

The New Order of Things:
UR Nursing was an early leader in the Nurse Practitioner movement. Today, the NP role is America’s fastest-growing profession.



UR Nursing was an early leader in the Nurse Practitioner movement. Today, the NP role is America’s fastest-growing profession.













EDITOR
Nora Williamson
Director of Strategic Communications, School of Nursing
ASSOCIATE EDITOR
Gianluca D’Elia
Communications Specialist, School of Nursing
ART DIRECTOR & DESIGN
Christine Kennedy
FEATURE PHOTOGRAPHY
Gianluca D’Elia John Schlia
Jeff Witherow Matt Wittmeyer
CONTRIBUTORS
Sam Coniglio Gianluca D’Elia
Robin Flanigan Nora Williamson
URMC COMMUNICATIONS
B. Chip Partner Assistant Vice President of Communications, URMC
Melissa L. Head ’99W (MS) Executive Director for Advancement
Andrea J. Allen
Senior Director of Advancement & Alumni Relations
NURSING Magazine is published twice a year for alumni, students, and friends of the University of Rochester School of Nursing. It is published by the University of Rochester Medical Center Departments of Communications, Alumni Relations, and Advancement.
ON THE COVER…
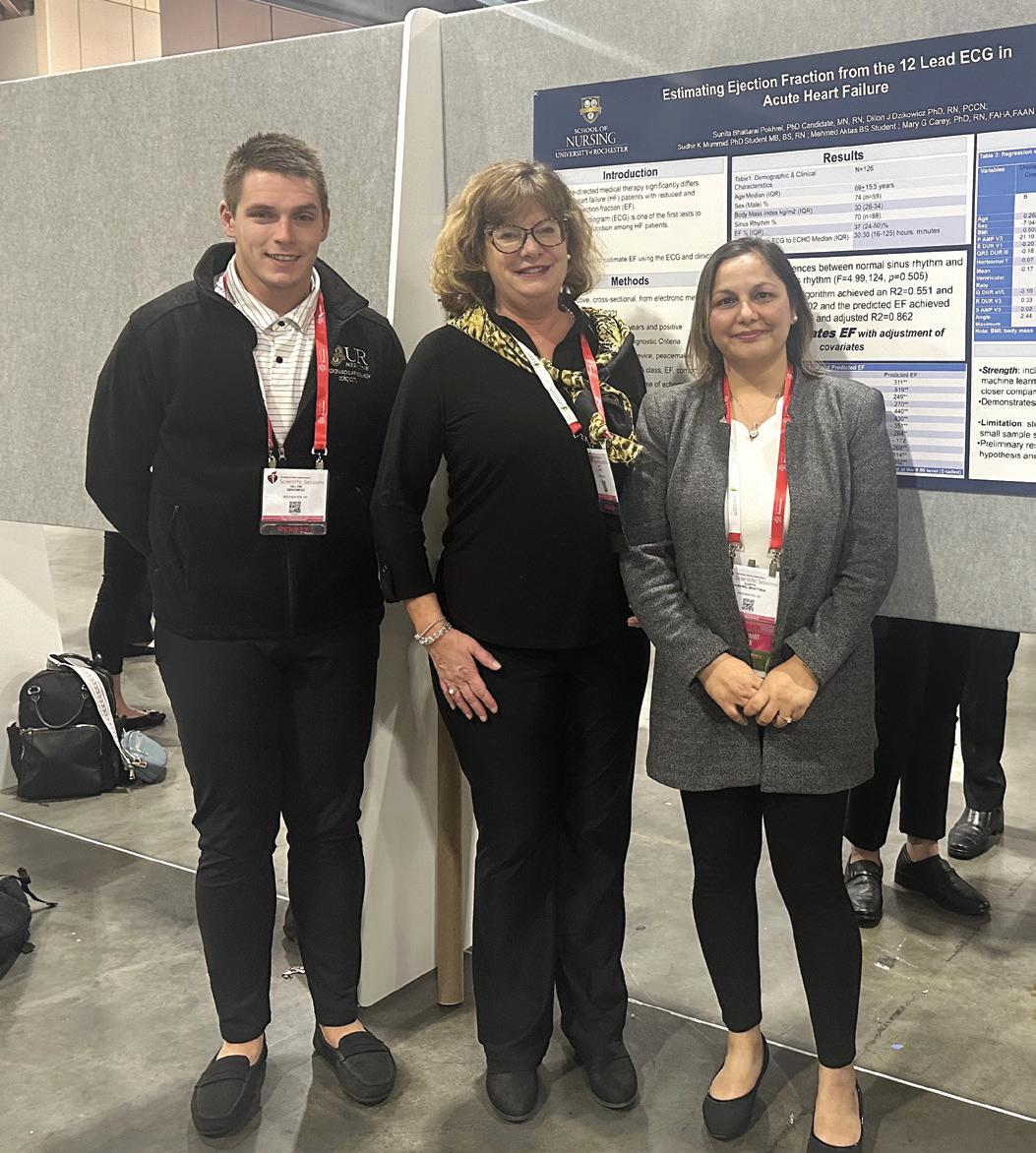
From left, Kara Mestnik, ’23N (DNP), APRN, FNP-C, a nurse practitioner at esophageal & thoracic surgery at the University of Rochester Medical Center; Cheryl Lustik, DNP, RN, MS, APN-C, chief advanced practice officer at URMC; and Kathleen Brennan, ’91N (MS), a nurse practitioner and educator who works on clinical placements for UR Nursing’s nurse practitioner students.
Photo by Matt Wittmeyer
WRITE TO US
We welcome your letters and feedback concerning stories in the magazine or issues related to the University of Rochester School of Nursing. Send your comments to: Editor,
Avenue, Box SON

Lisa Kitko, PhD, RN, FAHA, FAAN
Dean, School of Nursing
Independence Foundation
Chair in Nursing Education
Vice President, University of Rochester Medical Center
Professor of Nursing & Geriatric Medicine


Spring at the University of Rochester has been vibrant and productive for our faculty, staff, and students!
In the past six months, we have celebrated several milestones. Nearly 300 future nurse and health care leaders graduated at the historic Eastman Theatre, our accelerated students achieved a 100% pass rate on the Next Generation NCLEX exam, and we were again ranked among the top nursing schools in the nation for our master’s programs — No. 1 in Upstate New York!
I am also proud to share that our School of Nursing has faculty leads or team members at three new University-funded centers: the Center for Stress Resilience Science, the AI Horizons Institute, and the Center for Applied Biopsychosocial Research. These new hubs will allow us to support scholarship from diverse perspectives, including nursing, and further our contributions to cutting-edge research and practice. These achievements are due to the incredible efforts of our faculty, staff, and students, whose accomplishments are detailed in this magazine. They continue to embrace new challenges and forge new partnerships, shaping the future of nursing in Rochester and around the globe. Our cover story, “A New Order of Things,” highlights our innovative spirit as well as our shared commitment to advancing nurse practitioner education, built on a legacy of excellence. We are committed to inspiring future of generations of nurses to deliver critically important services to rural and underserved communities.
As Karen Keady, the Medical Center’s chief nursing executive, said in her graduation address, “The most significant growth comes outside of our comfort zones. It’s about saying ‘yes’ to opportunities that scare us, challenge us, and, ultimately, shape us into the leaders we aspire to be. It’s about working on and growing with teams that have a common goal and high trust and respect for its members.”
Our focused and formidable team is propelling our school and profession to new heights. We look forward to the next academic year and a summer of growth, driven by our strategic planning efforts that will set the vision for what we can achieve together.
THANK YOU FOR YOUR CONTINUED DEDICATION AND SUPPORT.
Warm regards,

Kevin Donohue, an accelerated bachelor’s graduate and former counselor at nearby Brighton High School, delivered the student speech on behalf of his cohort. “I’d like to think of myself as someone who feels a great deal of gratitude for the people who have had a positive impact on my journey to this point,” he said before sharing words of thanks for his family, classmates, and mentors, and encouraging his classmates to do the same.


Dave Bleck received his master’s degree in nursing education on the stage of Kodak Hall during the 2024 University of Rochester School of Nursing Graduation Ceremony.
Accelerated bachelor’s alumna Kelly Malepe, right, celebrated becoming a nurse with her family.

Accelerated bachelor’s alumnus Ward Kukol selected Associate Professor of Clinical Nursing Caroline Nestro as his pinner for the December 2023 ceremony. Nestro guided him on his path to pursuing psychiatric nursing.


Thaw Htoo, who now works in dialysis nursing at Strong Memorial Hospital, received his bachelor’s degree as a graduate of the Accelerated Bachelor’s in Nursing program on the stage of Kodak Hall.
Korie Kelly spoke on behalf of the RN to BS graduates at the December 2023 Pinning Ceremony. Kelly has been a registered nurse for more than 15 years at Highland Hospital, which supported her as she advanced her education. In her role as utilization management nurse manager, she leads a staff of 14 nurses. She discussed the most important lessons she learned throughout her degree program, such as letting failures pave the way for success, taking risks, and embracing diversity. “You may never feel 100 percent ready for the challenges ahead, but you will likely surprise yourself with what you are capable of and how resilient you are,” Kelly told her fellow graduates.




Outgoing Chief Nurse Executive Karen Keady, the School of Nursing’s assistant dean of clinical practice, delivered the 2024 keynote speech—her last address to nursing students before taking on a new role as system chief nursing officer for Vanderbilt Health in Nashville, Tennessee. “We have learned that the most significant growth happens outside of our comfort zones,” Keady said. “It’s about saying ‘yes’ to opportunities that scare us, that challenge us, and that, ultimately, shape us into the leaders we aspire to be.”

Sara Bird, a former lawyer from West Virginia, was selected by her classmates as the accelerated bachelor’s student speaker; spoke of nurses’ duty not only to provide high-quality care, but to advocate for inclusion, equity, and collaborative relationships. “We didn’t just learn how to listen to lung and heart sounds, take a manual blood pressure, interpret labs… we also learned how to be kinder, compassionate people to others because you cannot be a safe or effective nurse without upholding these principles,” said Bird, who is joining Strong Memorial Hospital’s med-surg flex team after graduation.

Instructor of Clinical Nursing Kaleigh Sullivan ’22N (MS), RN, was named the 2024 recipient of the Dean’s Award for Excellence in Teaching. Sullivan, who teaches psychiatric and mental health nursing courses for bachelor’s students, was praised for her approachable demeanor, genuine care for students, and teaching philosophy of being a “guide on the side.”

Graduate student speaker Samantha Loper, who will go on to work as a nurse practitioner for Strong Memorial Hospital’s cardiac surgery team after graduation, shared a personal story about her experience with a severe case of COVID that led to several months of complications while she was working toward her master’s.
“When you come face-to-face with the wall, you have two choices,” she told the Class of 2024. “One, you can give into it. Your second choice is to find that voice in the back of your heart and mind that says, ‘you can do this,’ and you dig deep and block out all distractions.”

The University of Rochester School of Nursing proudly announces that its graduates from the Accelerated Bachelor’s in Nursing program have achieved a remarkable 100 percent pass rate on the Next Generation NCLEX exam. This historic milestone was reached by graduates from the May 2023, August 2023, and December 2023 cohorts, marking a significant achievement for the School’s innovative educational initiatives.
The National Council Licensure Examination (NCLEX) is the test that all state boards of nursing use to determine qualification for licensure for graduates of nursing programs. The Next Generation (NGN) NCLEX – a new testing model introduced in Spring 2023 – was designed to address the need for newly licensed nurses to make complex clinical decisions. The revamped exam aims to better assess nursing candidates’ clinical judgment and decision-making abilities through real-world case studies.
“This achievement is not just a testament to the hard work of our students, but also to the dedication of our faculty and staff who have embraced these innovative teaching methods,” said Lisa Brophy, EdD, RN, MSBA, CNE, associate dean for undergraduate education.
“Our 100 percent pass rate on the Next Generation NCLEX demonstrates our ability to prepare nursing graduates to excel in their careers and provide high-quality care to their patients.”
The UR School of Nursing’s success is attributed to its Redefining Our Classroom Initiative (iROC), which has transformed traditional lecture-style learning into a dynamic, technology-driven environment. The iROC initiative focuses on enhancing critical thinking and clinical judgment skills, essential for the evolving health care landscape. This approach has earned the school recognition as an Apple Distinguished School.
As the School continues to evolve, it remains committed to supporting the success of its students through cutting-edge educational practices and a focus on diversity, equity, and inclusion. This commitment fosters a safe and supportive learning environment.
Students in the Accelerated Bachelor’s in Nursing program undergo rigorous training in a state-of-the-art learning environment, designed to replicate real clinical scenarios for hands-on learning. In just one-year, students are prepared to take the NGN NCLEX to become certified and begin practicing as RNs.
“Being able to make mistakes in a safe environment is crucial for learning and growth,”
said Luis Rosario-McCabe, DNP, RN, CNE, CNL, WHNP-BC, FNAP, co-director of the undergraduate programs. “Our NCLEX pass rates are a clear indicator of our effective preparation strategies.”

Carla DeLucia, EdD Associate Dean for Enrollment Management & Student Affairs

Carla DeLucia, EdD, assistant professor of clinical nursing, will serve as the associate dean for enrollment management and student affairs and continue to oversee the admissions and student affairs offices. In her new role, DeLucia will spearhead initiatives to strengthen the School’s recruitment and admissions efforts, adapt to market demands, and support student needs. She brings 17 years of experience in higher education administration, including expertise in predictive analytics and student financial services to the leadership role.
Lisa Brophy, EdD, RN, MSBA, CNE Associate
Dean
of Undergraduate Education
Lisa Brophy, EdD, RN, MSBA, CNE, assistant professor of clinical nursing, will serve as associate dean of undergraduate education. Brophy’s extensive experience in nursing practice, education, and leadership will be instrumental as she oversees the School’s undergraduate programs, including the accelerated nursing programs, RN to BS program, and the Center for Lifelong Learning. Brophy’s leadership will drive forward curricular innovations and enhance the quality of the School’s undergraduate offerings. She previously served as the assistant dean for education and co-director of the Accelerated Bachelor’s in Nursing program at the School.
Lydia Rotondo, DNP, RN, CNS, FNAP
Senior Associate Dean for Graduate Education & Innovation

education and technological integration. In her expanded role, Rotondo will focus on aligning the School’s priorities with the academic health system, promoting interprofessional education, and exploring innovative solutions to address workforce and community needs.
Professor Sally Norton, PhD, RN, FNAP, FPCN, FAAN, will serve as the senior associate dean for research.

Over the past five years, Norton has significantly advanced the School’s research mission, supporting faculty and students, and enhancing the School’s areas of research excellence. Norton will now oversee the PhD in Nursing & Health Science program, working closely with Program Director Marie Flannery, PhD, RN, to continue fostering research growth and mentorship within the School.


Professor Lydia Rotondo, DNP, RN, CNS, FNAP, will serve as senior associate dean for graduate education and innovation. Rotondo has been a transformative leader over the past 10 years as the School’s associate dean for education and student affairs, guiding the School through significant enrollment growth and championing competency-based
John Eaves, MBA, will serve as associate dean for operations and finance at the School, announced January 2024. With over 10 years of experience at the University and having served as interim associate dean since September, Eaves brings a wealth of financial expertise. In his new role, he will oversee operating and capital budgets, resource management, and administrative functions, working collaboratively with School leadership to advance the School’s education, research, and practice missions.

Craig Sellers, PhD, RN, AGPCNP-BC, GNP-BC, FAANP, a distinguished educator, researcher, and longtime specialty director of the School of Nursing’s adult master’s nurse practitioner programs, has devoted over four decades to nursing, including primary and palliative care for HIV/ AIDS patients and older adults. An expert in qualitative research methods, he is renowned for teaching students to apply these methods effectively. Sellers, who earned his PhD from the UR School of Nursing in 2009, practices at URMC’s Strong Memorial Hospital. His work has recently focused on training providers for community and geriatric care through a notable project, ENGOAL, enhancing health literacy among underserved older adults.
What motivated you to pursue a career in nursing and academia?
When I was in high school, I volunteered every weekend in the Emergency Department of our local hospital as part of our community engagement requirement. I continued volunteering when I came to Rochester and eventually discovered the UR School of Nursing. After a conversation with Eleanor Hall, chair of the Department of Nursing of the School of Medicine & Dentistry from 1957 to 1971. I transferred into the undergraduate nursing program. I spent the next decade at Strong Memorial Hospital, eventually moving to the Medical ICU and completed my master’s at the School.
During this time, I started to hear about what became known as the “AIDS epidemic,” and in 1991, I joined Community Health Network, a primary care clinic in Rochester, caring for people with HIV and AIDS. Those were difficult years due to the number of patients who were dying, and I developed an interest in caring for older adults and in palliative care.
I then joined the School’s PhD program, focusing on how people with HIV and AIDS made decisions about advanced directives and end-of-life care. This led to an opportunity to
become the specialty director for the Master’s ANP program, beginning my teaching career at the School.
What are some of the most rewarding moments of your career?
My favorite thing is running into NPs working in the community who have been my students. I can’t usually remember exactly when they were students here, but I’m not sure that matters much!
What advice would you offer to aspiring nurse educators?
Treat students as the adults they are. Guide them with your experiences and knowledge. Don’t forget about your own wellness along the way.
As you prepare to retire, what legacy or impact do you hope to leave behind in nursing education, and what are your plans for the future?
What’s my legacy? Well, that’s a difficult question to answer. I hope I have inspired my students to be thoughtful, curious, and caring clinicians—providers that people would want to take care of their own loved ones. I believe that both nursing and education are sacred callings. My goal has always been to leave things better off than when I found them.
I love to travel, so my next big trip is to visit Iceland. We’ll be renting a car and plan to drive around the whole circumference of the country, stopping along the way to see, well, the sights — waterfalls, glaciers, fjords, whales, and maybe even an active volcano!
Professionally, I plan to continue working as a per-diem NP in the Emergency Department at SMH— this will keep me up to date and grounded! I love editing, so I will continue reading manuscripts submitted to several journals and join the editorial board of a gerontology education journal. And, back to the wellness theme, I’m taking up mindfulness meditation and yoga to sustain me in my “older adult” years.

Karen Stein, PhD, RN, FAAN, a distinguished nurse researcher, spent her research career studying health risk behaviors among adolescent and young adult females, with a focus on identity development’s role. Her groundbreaking work extends to Western New York’s farmworker community, where she pioneered innovative mobile interventions promoting healthy eating. As a former editor of the Journal of the American Psychiatric Nurses Association and recipient of prestigious awards, Stein’s interdisciplinary collaborations and community-centered approach exemplify her dedication to the discipline of nursing and to the health and well-being of all members of communities, particularly those who are disenfranchised and vulnerable.
As you reflect on your tenure at the University of Rochester School of Nursing, what achievements or projects are you most proud of, and why?
I feel the greatest sense of accomplishment and pride in our work that has brought attention to the body weight/shape concerns of farmworker families, stemming from the challenges associated with dietary acculturation. Women in our groups expressed feelings of shame and guilt provoked by health care providers’ attitudes toward their and their children’s body weight. Women stated that while they were told that both they and their children needed to lose weight, they did not know how to make that happen. Providers made recommendations to “eat smaller portions” and “avoid sweets,” but did not provide the detailed information needed to make healthy choices in the U.S. eating environment. This disconnect led to unhealthy approaches to weight control. I believe that our work gave voice to body weight and related health concerns of this population—a voice needed to provide the farmworkers the support to improve their dietary intake while residing in the U.S.
What advice would you offer to aspiring nurse researchers, particularly those interested in exploring health risk behaviors and community-based interventions?
In my work, the first step was developing relationships with organizations including the Rural and Migrant Ministry and the Western Coalition of Farmworker Serving Agencies. In all cases, building the trust of community advocates was essential to reaching the populations. This work takes time and dedication but is essential for establishing a strong foundation for work with the community.
As you prepare to retire, what legacy or impact do you hope to leave behind in the field of nursing research, and what are your plans for the future?
The legacy that I hope to leave is my commitment to the discipline of nursing and a future of high-quality nursing research that meaningfully contributes to the health and well-being of all members of our communities, particularly those who are disenfranchised and vulnerable.
Of course, I am sad to leave this very important period my life. It has been a challenging journey with many successes, as well as many frustrations and disappointments along the way. Most important, the last thirty years have been amazingly stimulating, challenging, and filled with much joy and satisfaction.
Retirement for me will include continuing writing several papers I never quite got to! In addition, I serve on the board of directors of two nonprofit organizations (one serving New York and the other, international) that serve immigrant farmworkers in the US. Within that context, I will have the opportunity to work on measurement of program outcomes and outcome studies. Happily, I expect to spend a considerable amount of time working on my hobby of metal smithing. Last, but surely not least, I expect to spend as much time as possible with my two darling grandchildren, Mia and Ezra!
Visit our newsroom at son.rochester.edu/newsroom for the full faculty stories.
As part of the Boundless Possibility strategic plan, the University of Rochester is launching five new transdisciplinary centers or institutes aimed at supporting scholarship in areas that will bring the University even more distinction and reputation.
In early 2024, the University launched a planning funding competition, asking teams of scholars from multiple units across the institution to propose ideas for new centers and institutes.
Out of 42 submissions received, 10 potential transdisciplinary centers and institute were selected to receive planning funding for the 2024–25 academic year, with the goal of launching five shortly thereafter. School of Nursing faculty feature in three of the 10 receiving planning funding:
• Center for Stress Resilience Science — Harnessing a multitude of University expertise to become a global leader in understanding the impact of stress on health and well-being. A primary focus is to develop much-needed interventions for those bearing the brunt of stress by identifying underlying sociocultural factors and other mechanisms that perpetuate stress-related poor health and other disparities across the lifespan. Led by Kathi Heffner, PhD, professor of nursing, medicine, and psychiatry, with Associate Dean for Research Sally Norton, PhD, RN, FNAP, FPCN, FAAN, as a participating team member.
• AI Horizons Institute — Engaging synergistically in both foundational and use-inspired AI research to advance the state-of-the-art in generative AI, while striving to overcome the limitations of current technology by taking inspiration from neuroscience and psychology. The primary focus includes education and understanding of the ethical and societal implications of advanced AI. Michael Hasselberg, ’07N (MS), ’13N (PhD), URMC’s chief digital health officer and an associate professor of clinical nursing, is one of the co-leads; also participating are assistant professors Caitlin Dreisbach, PhD, RN; Dillon Dzikowicz, PhD, RN, PCCN; and Jinjiao Wang, PhD, RN.
• Center for Applied Biopsychosocial Research — Bringing together innovators across departments and schools to accelerate biopsychosocial discovery, while inspiring nascent visionaries whose research requires exceptional transdisciplinary mentorship. Attention will be placed on increasing research funding by opening new avenues at the intersections of science, engineering, education, business, and the humanities. Kathi Heffner, PhD, is co-lead.
Selected recipients will receive a funding of approximately $40,000 to spend a year developing what they think will be the best prospect for the University to advance its scholarly prominence. It is expected that one or more of these centers or institutes will be awarded larger-scale funding beginning in the 2025–26 academic year.
The University of Rochester School of Nursing, in partnership with nursing practice at the University of Rochester Medical Center (URMC), announced its extension of a free tuition program for UR nurses.
The School of Nursing Tuition Grant supplements University of Rochester employee tuition benefits to provide 100 percent tuition coverage in select bachelor’s, master’s, and advanced certificate programs.
By investing in the success of our nurses, we are directly enhancing the quality of care for our community, ensuring that every patient receives the most compassionate, knowledgeable, and advanced care possible.”
- Dean Lisa Kitko, PhD, RN, FAHA, FAAN
More than 675 URMC nurses and health care professionals have enrolled and benefited from the grant since its inception in 2019.
“The beauty of this program is that we’re not just opening doors, but we’re revolutionizing the future of nursing in our health care system. Our commitment goes beyond providing tuition-free education; it’s about supporting the full potential of our nurses toward earning their bachelor’s or master’s degrees,”said Dean Lisa Kitko, PhD, RN, FAHA, FAAN.
Open to eligible University of Rochester employees, the grant is available for new students in the RN to BS Online program, or the Clinical Nurse Leader, Nursing Education, and Leadership in Health Care Systems master’s programs.
The grant was first implemented in 2019 as a pilot program but was slated to end this past spring. The extension will cover new students who matriculate and begin their degree programs no later than the summer 2025 semester.
In addition to supporting the academic journeys of individual nurses, the grant was devised to bolster the strength of the workforce at Strong Memorial Hospital and other URMC facilities. By removing the financial barriers to degree programs, the grant aims to spur more nurses to pursue additional education to enhance their clinical practice, as well as prepare themselves for career advancement and positions of leadership.

For nearly two decades, the School of Nursing’s Leadership in Health Care Systems (LHCS) program has prepared students from various backgrounds to take on roles as executives, managers, program coordinators, and other key leadership positions.
The broad, interdisciplinary focus of the master’s program attracts both nurses and non-nurse health care professionals alike. Victoria Thomas, RDH, BS, is among those who joined from outside the nursing profession.
Looking for a change after two decades as a dental hygienist, she earned a bachelor’s in Allied Health at nearby SUNY Empire that opened her up to new possibilities and led her to consider what to do next.
Thomas, who works down the street from Helen Wood Hall as a research coordinator at the Eastman Institute for Oral Health (EIOH), utilized University employee tuition benefits and the School of Nursing tuition grant to take the next step in her career.
“I have grown personally and professionally through this program, and I would not have had this opportunity without the School of Nursing Tuition Grant. I am so grateful to have been accepted into this program …. The faculty at UR Nursing have real-world knowledge, expertise in their fields, and are unbelievably supportive and accommodating. I am excited to share that I will walk at the graduation ceremony this spring and complete my final class this summer.”

In a significant step toward addressing the region’s critical need for adolescent eating disorder treatment, New York State Assemblymember Jen Lunsford announced $80,000 in funding to support efforts by the Healing Connection, the School of Nursing, and other local partners to open an adolescent residential treatment facility.
The addition of a residential program would help the Healing Connection, a local eating disorder treatment program, close a gap in the continuum of care. This continuum typically includes five parts: inpatient, partial hospitalization, residential treatment, intensive outpatient, and outpatient care. However, there are no residential treatment programs for adolescents in Upstate and Western New York.
Easier access to the full continuum of care, including 24/7 residential treatment, gives patients and their families the best opportunity to combat the illness.
“Currently, adolescents need to travel at least five hours away for eating disorder residential treatment, and the majority have to go out of state, leaving behind their families, friends, and health care team,” said Mary Tantillo, PhD, PMHCNS-BC, FAED, CGP, a professor of clinical nursing and director of the Western New York Comprehensive Care Center for Eating Disorders. “Residential treatment closer to home allows for continuity of connections with family, friends, and providers, while also offering opportunities for new connections with peers and staff in the treatment setting.”
“We are grateful for Assemblywoman Lunsford’s support of residential programming, which will be life-changing and life-saving for many adolescents, including those who often cannot access treatment due to a lack of financial means,” she added.
The new state funding will be allocated toward the facility’s operating expenses.
“We are blessed here in the Finger Lakes to have so many resources that help families find the connections they need to help those suffering from eating disorders,” Assemblymember Lunsford said. “This funding represents a significant step forward in our commitment to recovery and healing, and will provide a safe haven for people on the path toward a healthier future.”

Visit nyeatingdisorders.org to learn more about local resources for treatment and recovery.


The School of Nursing welcomed its Summer 2024 cohort of UR Nursing Scholars at an Admitted Student Day in March. The UR Nursing Scholars program has admitted more than 100 students to the 12-Month Accelerated Bachelor’s program, offering 100 percent tuition coverage in exchange for a three-year work commitment at select UR Medicine hospitals.


for local

The 11th annual See What
Day, a collaboration between UR Nursing and the Children’s School of Rochester, introduced sixth-graders to a day in the life of nurses, dieticians, and physical therapists at Strong Memorial Hospital. Pictured is Instructor of Clinical Nursing Sharon Gilbride teaching a student how to swaddle a baby.
Faculty and staff diversity officers Chen Zhang, Jonathan Wetherbee, Peter Bertoldo, and Maria Quiñones-Cordero celebrate the Year of the Dragon at the School of Nursing’s annual Lunar New Year Celebration on Feb. 8.

Bachelor’s student Mona Sepulveda ’99


Every year, I Heart SON Day brings the community together to write thank-you notes to alumni and supporters of the school and to share what they love most about the School.

Students from East High School, led by recent Master’s in Nursing Education alumni Dave Bleck and Caitlyn Paris-Woods, visit an operating room as part of a full-day field trip for the School of Nursing and East’s “Pathways to Nursing” course. The 10-week program equips high-schoolers with clinical, research, and professional skills to prepare them for health-related college majors and jobs.






Assistant Professor Meredith Kells, Professor Emeritus of Pediatrics Richard Kreipe, and adolescent medicine nurse practitioners Amy Realbuto and Heather Wensley attend the Society for Adolescent Health & Medicine’s annual meeting.

UR Nursing alumna Kai Mbeke (second from left) and Professor of Clinical Nursing Susan Blaakman (second from right) attended the New York State Office of Mental Health Chief Nursing Officers Annual Education Conference. Blaakman presented “Road to Joy: Mapping the Path in Mental Health Nursing” as a plenary speaker.
Heather Wensley, a DNP alumna and nurse practitioner on Golisano Children’s Hospital’s Adolescent Medicine team, earned first place in the DNP student poster category at ENRS for a presentation of her recent scholarly project, “A Clinic-Based Parent-Peer Support Program for Parents of Transgender and Gender-Diverse Youth Date.”

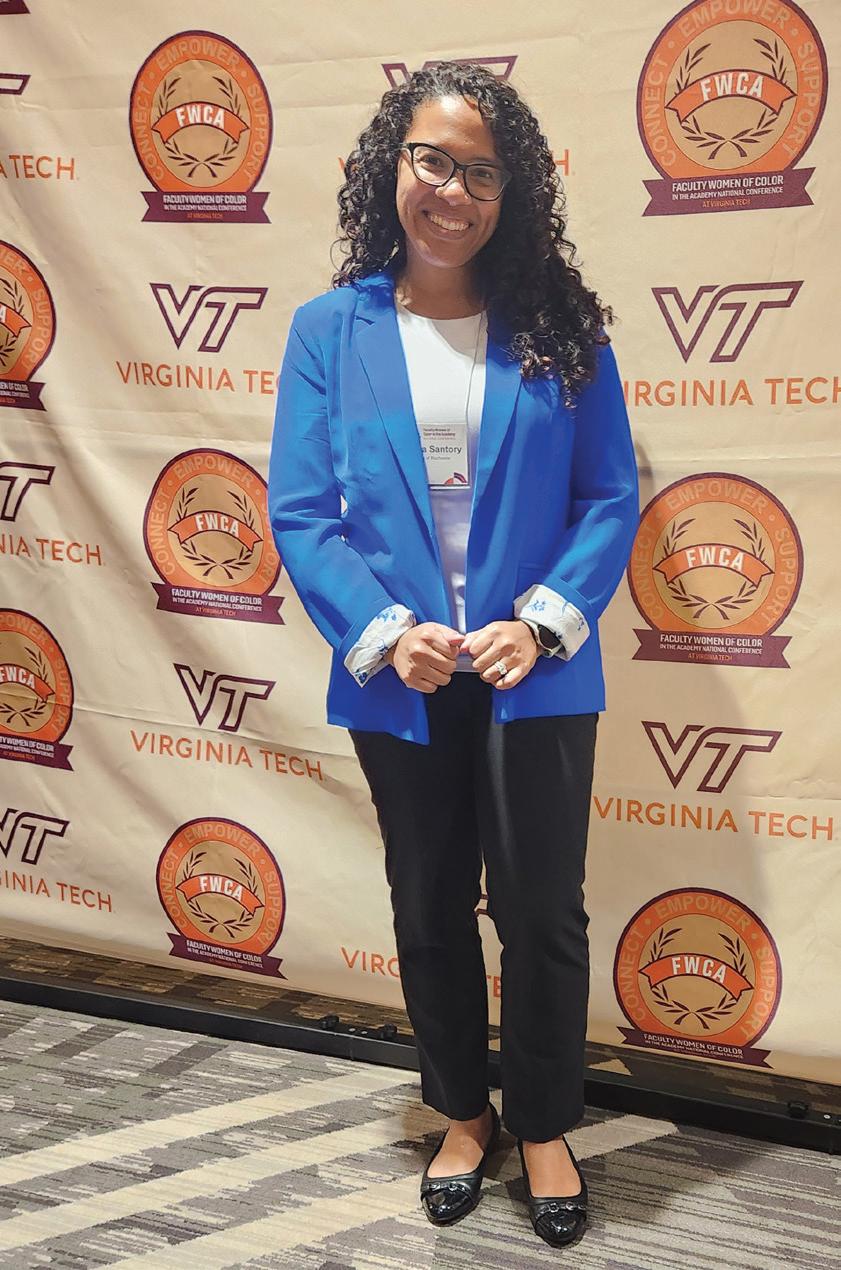
Instructor of Clinical Nursing Kristina Santory attended the Faculty Women of Color in the Academy conference in Arlington, Virginia, and had an on-demand presentation titled “Surviving to Thriving: Cultivating Self-Care and Resilience in Early Career Academia.”

PhD student Wonkyung Chang won first place in the poster presentation category at the American Psychiatric Nurses Association New York chapter’s annual conference. Her study, “Unhealthy Alcohol Use among Gay, Bisexual, and Other Men Who Have Sex with Men,” seeks to understand how social, psychological and cultural factors contribute to the prevalence of heavy drinking among sexual minority men.
PhD students Zhihong Sandy Zhang, Yuri Choi, and Erin Vernetti presented posters at ENRS.

Erin Baylor and Kimberly Buholtz, UR Nursing’s director and assistant director of simulation, presented at the International Meeting on Simulation in Health Care in San Diego. Both delivered podium presentations, spoke on a panel about the International Nursing Association of Clinical Simulation and Learning (INACSL) endorsement process, and they led a workshop together, titled—“Spice Up Your Simulations or You’ll Be Chopped.”

Faculty and students travelled to Boston for the Eastern Nursing Research Society (ENRS) annual conference in March: (L to R) Caitlin Dreisbach, Heather Wensley, Chen Zhang, Lisa Kitko, Erin Vernetti, Carol Li, Yuri Choi, and Meredith Kells.


DNP alumna Christine Boerman (right) and UR Medicine Chief Digital Health Officer Michael Hasselberg ’07N (MS), ’13N (PhD) (second from left) were among the URMC nurses who attended ViVE, a leading health care business event, in Nashville. Boerman, who graduated this past May, developed a nursing innovation fellowship at Strong Memorial Hospital as her DNP scholarly project. She received a registration scholarship from ViVE, and the School of Nursing supported her travel to the conference.
Assistant Professor of Clinical Nursing
Maria Marconi was the keynote speaker at the University of Oklahoma’s 21st annual evidence-based practice symposium, “Unleashing the Power of Evidence-Based Academic Assessment.” Across the three-day conference, she spoke at the University’s campuses in Tulsa, Oklahoma City, and Lawton, and consulted with graduate and undergraduate programs on academic assessment planning.
Three University of Rochester School of Nursing faculty members have been recognized as distinguished fellows of the National Academies of Practice (NAP).
The following three associate professors will be inducted into the NAP at its annual awards and induction ceremony in March: Erin S. Baylor, DNP, RN, PNP-BC, ONP, CHSE; Luis A. Rosario-McCabe, DNP, RN, CNE, CNL, WHNP-BC; and Tara M. Serwetnyk, EdD, RN, NPD-BC.
The NAP’s distinguished fellowship honors individuals who have made significant, enduring contributions to health care practice, research, education, and public policy. The NAP is a non-profit organization founded in 1981 to advise governmental bodies on health care, foster collaboration, and advance patient-centered care. Distinguished practitioners and scholars are elected by their peers from multiple different health professions to join the interprofessional group.
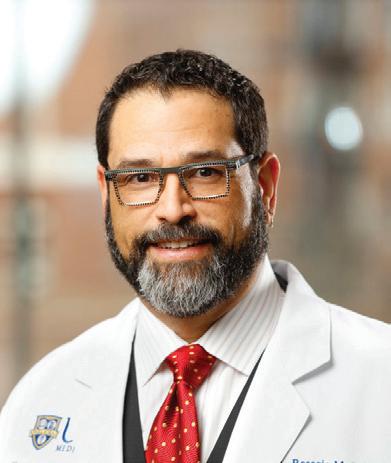
Rosario-McCabe has provided obstetric and gynecological care to women of all ages for more than 30 years and has worked alongside community and state leaders and in interprofessional teams to address health care disparities.
A focus on marginalized communities is at the heart of Rosario-McCabe’s work. He led the establishment of a dedicated transgender clinic within Strong Memorial Hospital’s Obstetrics & Gynecology Department, and continues to serve as a leader in gender-affirming care, regularly leading workshops and presentations on interprofessional LGBTQ+ health care. Rosario-McCabe is also co-director of the Accelerated Bachelor’s Program for Non-Nurses.
“Reflecting on my 30-plus-year career in nursing, I am reminded of the butterfly effect in chaos theory, where a small change in one area can cause a more significant impact on another,” Rosario-McCabe said. “I’ve witnessed the power of interprofessional collaboration in providing quality, person-centered care, reinforcing the belief that we are stronger together. Recognition by my peers as a distinguished fellow is an honor and strengthens the impact of my work. I look forward to my involvement with the NAP in shaping health care practice, policy, and education at a national level.”


Baylor serves as director of simulation and leads the Pediatric Nurse Practitioner master’s program. Through her leadership roles at the School, she has incorporated best practices in interprofessional education through several innovative, experiential learning opportunities. Among her recent accomplishments of which she is most proud is the implementation of the Community Action Poverty Simulation as part of the curriculum for bachelor’s and NP students, as well as simulations focused on telehealth, pediatric trauma, delivering difficult news, and Objective Structured Clinical Examinations (OSCEs).
In recent years, Baylor also helped the School launch New York’s first advanced certificate program in Pediatric Acute Care Nursing. She continues to serve vulnerable populations in the region as a primary care provider.
“This is a humbling and exciting way to be recognized, and it blends all of the areas of my work that I take pride in and feel passionate about,” Baylor said. “I have been working as a pediatric nurse practitioner for almost 30 years and teaching at the School of Nursing for 20 years now, and it is incredibly meaningful to see my passions for patient care and education recognized by my peers.”
Serwetnyk, director of academic innovation, leads the Redefining Our Classroom Initiative (iROC), which has leveraged technology to shift the traditional classroom into a dynamic learning environment. Her leadership has helped the School of Nursing achieve designation as an Apple Distinguished School — an honor that recognizes centers for innovation, leadership, and educational excellence — and recognition as the American Associate of Colleges of Nursing’s 2023 Innovations in Professional Nursing Education Award winner. Serwetnyk has focused her research on original teaching strategies to improve outcomes and has presented nationally on education technology, instructional design, student engagement, and active learning strategies.
In addition to her work at the School, she led research at the University of Rochester Medical Center to evaluate training outcomes for online and hybrid American Heart Association courses, leading to the implementation of URMC’s Resuscitation Quality Improvement program. Serwetnyk started her career at Golisano Children’s Hospital, where she started as a staff nurse and also served as pediatric burn coordinator and a nurse leader.
“I am honored to join this distinguished group of leaders who are working collaboratively to impact the health care system and positively influence health outcomes,” Serwetnyk said. “I truly value the interprofessional relationships I have made throughout my career as a nurse and recognize the importance of interprofessional education as we prepare future nurses for today’s complex health care environment. I look forward to establishing new relationships with other health professionals who share my passion for innovation, interprofessional collaboration, and scholarship.”

A new research study aims to address stigma and discrimination related to HIV prevention and treatment in Ghana—with promising potential to improve HIV care in marginalized communities worldwide.
A University of Rochester School of Nursing researcher has earned a $2.3 million National Institutes of Nursing Research grant to address stigma and discrimination related to HIV, sexual orientation, and gender expression and improve health outcomes among those who are most disproportionately affected by the HIV epidemic in Ghana.
Assistant Professor of Nursing and Public Health Gamji Rabiu Abu-Ba’are, PhD, MA, will lead a five-year study to implement and test a unique multilevel intervention program. The program will provide comprehensive support and care to health care facilities and young men in order to to address the social determinants of health that lead to disparities in HIV care.
“This study bridges a vital gap in HIV prevention and treatment by ensuring that the most advanced biomedical interventions are not just developed, but are accessible and effective for those at the highest risk,” said Abu-Ba’are. “It’s about transforming scientific breakthroughs into tangible health benefits for communities that need them the most — by understanding their unique experiences, steering us closer to a world where HIV is no longer a public health crisis, but a manageable health condition.”
The project, “Status-neutral community-based multilevel intervention to address intersectional stigma and discrimination, and increase HIV testing, PrEP, and ART uptake among YGBMSM in Ghanaian Slums,” will receive more than $2.3 million over five years from the National Institutes of Nursing Research. It aims to revolutionize HIV care for young gay, bisexual, and other men who have sex with men in Ghana’s slums, where social and economic challenges compound the risk of HIV.
Ghana is among the most rapidly urbanizing African nations, with more than half of the population currently living in its metropolitan areas. The United Nations predicts that Ghana’s
Visiting international scholar Edem Yaw Zigah, Assistant Professor Gamji Rabiu Abu-Ba’are and postdoctoral research associate Osman Wumpini Shamrock are all members of the Behavioral, Sexual, and Global Health Lab.
two of every five city dwellers live in slum settlements, where there is often little to no access to health care and sexual health services.
Sexually active minority men living in slums are among the hardest hit by these challenges.
Researchers will explore the program’s potential to reduce stigma and discrimination and to increase HIV self-testing and Pre-exposure Prophylaxis (PrEP) uptake among young sexually active minority men. As part of the study, the program will include comprehensive training for health care workers and the integration of PrEP and Antiretroviral Therapy (ART) into the treatment plan. The program has already shown early efficacy in boosting HIV testing.
Co-investigators on the grant are Natalie Leblanc, PhD, MPH, RN, and Jim McMahon, PhD, with the University of Rochester School of Nursing, Kwasi Torpey, PhD, MPH, FGCOP, FWACP, and Chris Guure, PhD, with the University of Ghana, and LaRon Nelson, PhD, RN, FNP, FNYAM, FAAN, and Jeon Sangchoon, PhD, with the Yale School of Nursing.
Abu-Ba’are is the principal investigator of the Behavioral, Sexual, and Global Health Lab that operates out of the University of Rochester School of Nursing and or Jama’a Action, a community health organization based in Accra, Ghana. His research develops and refines interventions to reduce intersectional stigma and optimize outcomes among HIV high-risk populations in socially vulnerable communities in Sub-Saharan Africa, Western Europe, and the United States.
Earlier this year, the NIH Fogarty International Center awarded $619,800 to Abu-Ba’are support a three-year study on the feasibility of a group intervention program called “Lafiya” (“wellness” in the West African Hausa language) to improve HIV self-testing among young sexually active minority men in urban areas of Ghana.
Faculty and students from the University of Rochester School of Nursing received international recognition from the American Heart Association for their research and leadership.
In April, Dean Lisa Kitko, PhD, RN, FAHA, FAAN was named chair-elect of the American Heart Association Council on Cardiovascular and Stroke Nursing (CVSN). This council serves as a home for cardiovascular nursing science, provides resources for nurses’ professional development at all stages and career paths, and advocates for nursing and cardiovascular and stroke conditions across the lifespan.
“Engaging with the CVSN Council embodies my passion for making a tangible difference in cardiovascular health outcomes and promoting excellence in nursing science,” Kitko said in an announcement from the CVSN Council.
“Involvement in the CVSN Council allows me to collaborate with fellow experts, exchange insights, and collectively address the multifaceted challenges in cardiovascular and stroke care.”
Kitko was named a fellow of the American Heart Association (AHA) in 2015 and has been involved with the organization both locally and nationally for several years. An award-winning nurse scientist, Kitko sheds light on the role of family caregivers in managing heart failure. She has contributed to the development of interventions and support programs aimed at addressing the needs of both heart-failure patients and their caregivers, and her work has been supported by the National Institutes of Health and AHA.
In November, Professor of Nursing Mary Carey, PhD, RN, FAHA, FAAN, and Michele Pelter, PhD, RN, FAHA, an associate professor of physiological nursing at University of California, San Francisco, received the 2023 Research Article of the Year Award.
The award-winning article, “An annotated ventricular tachycardia (VT) alarm database: Toward a uniform standard for optimizing automated VT identification in hospitalized patients,” was published in the Annals of Noninvasive Electrocardiology earlier this year.
VT is a life-threatening abnormal heart rhythm, and computer accuracy in identifying VT is less than 10 percent, jeopardizing patient safety and contributing to alarm fatigue among health care providers. A team of researchers collaborated across the University of Rochester, UCSF, University of Pittsburgh Medical Center, and the University of North Carolina - Chapel Hill to create a database of over 22,000 ventricular tachycardia alarms from 500,000 hours of ECG monitoring to train computer algorithms to better recognize and predict fatal VT arrhythmias among hospitalized patients.
The study found that creating high-quality, well-annotated datasets for algorithm development and testing can ultimately improve patient outcomes and reduce alarm burden.
PhD candidate Sunita Pokhrel Bhattarai, PhD, MS, RN, won the AHA Council on Cardiovascular and Stroke Nursing’s Early Career Research Travel Grant. The award recognizes promising and outstanding investigators in the early stages of their careers and provides travel assistance to participate in AHA scientific meetings. She successfully defended her dissertation, “Estimating Left Ventricular Ejection Fraction from the 12-Lead Electrocardiogram in Acute Heart Failure Patients: A Retrospective Study,” in the spring semester.
Assistant Professor Dillon Dzikowicz, PhD, RN, PCCN, was named a recipient of the American Heart Association’s Second Century Early Faculty Independence Award. The grant funding will support the project “Re-designing STEMI/NSTEMI Classification: Secondary Screening for an Occluded Culprit Artery in NSTEMI.” The study will train, test, and validate a machine learning algorithm to identify acute coronary occlusion among heart attack patients without obvious signs on the electrocardiogram.
Assistant Professor Lauren Ghazal, PhD, FNP-BC, has been chosen as a STAT Wunderkind, a “next-generation scientific superstar,” in a national contest that singles out young, high achievers from top research institutions.
Ghazal, a researcher and family nurse practitioner, joined the University in July 2023 as an assistant professor at the School of Nursing and associate member of the Wilmot Cancer Institute’s Cancer Prevention and Control Program.
As a nurse scientist, Ghazal utilizes her professional and personal experiences in cancer care, nursing, and economics to research the cancer survivorship needs of adolescents and young adults, with a focus on the financial impacts of cancer on these age groups. It’s an area of research that holds personal meaning for Ghazal, a cancer survivor who was treated for lymphoma in her 20s.
“I’m honored and proud to be recognized for my work in and dedication to advancing adolescent and young-adult cancer care delivery — especially at a time when I am launching a new career in a new place,” Ghazal said. “I feel blessed to contribute to nursing science as a patient, provider, and researcher and hope to continue this important work in a long career.”

“Our generation of assistant professors is pushing boundaries in a good way, and that’s something I really value at the University of Rochester,” Ghazal said. “There are groundbreaking researchers doing great science here — in ways that haven’t been done before. I’m excited to learn from my colleagues, and to know that we have the people and infrastructure here to move adolescent and young adult research forward.”
STAT, a respected news agency that exclusively covers health and medicine, created the annual “Wunderkind” award to celebrate early-career researchers who are not yet independent scientists or program leaders.
Alongside her new colleagues at Wilmot, Ghazal is working to expand adolescent and young adult cancer research at the University of Rochester Medical Center. She is a co-principal investigator on a Patient-Centered Outcomes Research Institute (PCORI) engagement award for a project to build a research base to support studies on cancer survivorship disparities in the LGBTQ+ community.

Mary-Therese Dombeck, PhD, DMin, LMFT, LMHC, taught full-time at the University of Rochester School of Nursing until 2021 — when she was 85. But the beloved teacher, colleague, researcher, and mentor still hasn’t retired completely.
The now 89-year-old professor emeritus of nursing, who has served under five deans, says she can’t imagine life without working part-time where she has been affiliated since the mid-1970s.
“I feel like I grew up there,” says Dombeck, who earned a master’s degree in psychiatric and adult mental health nursing of adults at the School of Nursing in 1978. “It’s like my home.”
Dombeck joined the faculty in 1979 as senior associate in nursing and went on to become professor of nursing. She has served on every School committee since and chaired several.
Her scholarly endeavors on ethnography and hermeneutics combine social anthropology and theology — she has degrees in both disciplines — and have been published in national and international peer-reviewed research and clinical journals. Since 1980, she has taught an expansive array of courses — including psychiatric nursing, group and family psychotherapy, cultural diversity, and spiritual issues in health care, among others — and developed most of them.
Dombeck’s academic work has been featured in more than 30 publications, and she has presented nationally and internationally on the study of dreams, gender identity in nursing, and religious and spiritual needs in health care.
“I think of Mary as a lifelong MasterClass,” says Professor Emeritus of Nursing Tobie Olsan, PhD, RN, CNL, FNAP, who met Dombeck in graduate school and has worked alongside
her in multiple capacities since. Yet “despite her high intellect and sophisticated understanding of systems, she’s always humble and kind.”
When asked how she feels about the seminal work that has resulted from fusing nursing and spirituality, Dombeck says: “I’ve never thought about it like that. I was just following my own path.”
It’s a path that leads back to her childhood.
At the time Dombeck was born in Cairo, Egypt, most women there lost children because of exceptionally poor health conditions. Dombeck says she watched her mother, Esther, successfully raise four children using scrupulously clean cooking methods that were difficult to duplicate. She considered her mother to be endowed with the capabilities of a good nurse.
Another formative memory involved Esther taking her to their church sanctuary on Sundays for a short prayer, freshly baked bread in hand, before distributing the bread to poor sections of the city.
“I can’t imagine what I would have been without those experiences,” Dombeck recalls. “I wanted to be like my mother. She was indomitable, yet always very kind.”
Holly Brown, DNP, RN, PMHNP-BC, PMHCS, executive director of the Golisano Institute for Developmental Disability Nursing at St. John Fisher University, has some adjectives of her own to describe her former School of Nursing teacher and colleague.
“Mary is patient, reflective, curious, and constant,” Brown says. “She has the ability to bring really dense, really complicated concepts down to a usable level for the average person.”
Olsan recalls Dombeck using pragmatic language to move her from the “quantitative realm,” in which she felt comfortable to more conceptual places, gently quelling her anxiety in the process.
“Mary hands-down makes doctoral study and learning a safe space to be,” Olsan says. “We talk about ‘safe spaces’ now; she invented that. And her pearls of wisdom just sort of stick with you and help you beyond the date of your graduation — invaluable.”
Pragmatic doesn’t mean basic, however. Dombeck is known for engaging others on a deeper, more meaningful level.
“I don’t do small talk,” she says. “If we’re going to talk, let’s talk.”
In fact, she was talking about diversity long before it became a cultural conversation. As a result, two awards are named after her: the Mary Dombeck Diversity Enhancement Faculty Award and the Mary Dombeck Diversity Enhancement Staff Award.
Dombeck has received numerous awards herself throughout her career, including the School of Nursing’s Culture Diversity Advancement Award.
With experience comes perspective, and one of the occupational shifts Dombeck has been most appreciative of over the years is the increase both in male nurses and those from different ethnic backgrounds.
“It’s not just white women anymore,” she says, “and that’s for the best because we’re more like the people we serve.”

To get even more in touch with those people, in 2014 Dombeck formed a spirituality subcommittee within the Council for Diversity and Inclusion to focus on how spiritual, religious, and moral beliefs, relate to the perception of health, illness, healing, suffering, and dying.
In addition to being the founding owner of Crossbridge Counseling, Dombeck has been known as the School of Nursing’s “unofficial chaplain” for decades, presiding at memorial services and offering prayers at graduation and other events.
Now that she teaches only two psychotherapy courses at the School of Nursing, Dombeck has more time for resting, ballroom dance lessons, get-togethers with family and friends, and facilitating dream interpreting groups. (Her aunt was a well-known dream interpreter in Egypt.)
“It is a happy balance so far,” she says. “I will continue to evaluate when it is time to stop working year by year.”
Those who know her have a difficult time picturing the School of Nursing without Dombeck, whose name is rarely uttered without a trailing list of glowing attributes.
“Mary is present, wise, aware, constant, unflappable,” Brown says. “That woman is like Yoda — for real.”

“I’ve often thought of Mary as my spirit guide.”
Tobie Olsan, professor emeritus of nursing

Kamila Barnes ’11N (MS), ’13N (DNP), has seen the dangers of Black maternal health inequity firsthand in her work as a family nurse practitioner.
Barnes, the founder and owner of Barnes Health Affiliates, LLC, remembers seeing a patient who’d recently delivered her baby through a cesarean section surgery and noticed uneven bumps on her C-section scar. A different provider had told the woman that her experience was normal. But Barnes found that it wasn’t that simple: An abscess was pushing through the wound.
“This was someone who could have developed sepsis, which could lead to death,” said Barnes, who is now chair of the National Black Nurses Association’s Black Maternal Health Task Force and an associate professor of nursing at Hofstra University.
Situations like this are a difficult reality for many Black parents. In the US, Black women are more than twice as likely to experience severe pregnancy-related complications, and nearly three times more likely to die, according to the Centers for Disease Control and Prevention. Racial disparities in maternal health are intertwined with structural racism dating back to slavery, as well as with implicit biases that continue to affect our interactions in health care settings today.
Research has shown that the legacy of racist policies in the US continues to impact maternal health today. Public health researchers here at the University of Rochester Medical Center, for example, found that redlining policies of the 1930s and ’40s
— which effectively trapped people of color in low-income and segregated neighborhoods and denied them the ability to build intergenerational wealth — are associated with worse outcomes in pregnancy and childbirth among Black women today.
Barnes is a maternal health advocate who has worked to reduce maternal-child health disparities through her clinical, scholarly, and community service work. An alumna of the School of Nursing’s DNP program, her scholarly project focused on addressing health disparities among Rochester’s teen parent population. She shared her expertise and insights on how nurses are uniquely positioned to improve Black maternal health outcomes:
What are some of the most pressing factors that impact Black maternal health today?
One of the major issues is us Black women not being heard. When you read articles about Black maternal health, there are often anecdotes from family members and partners that say, “She complained of unusual leg swelling and pain, and was told that it’s just how pregnancy is.” You read cases where they go to the doctor with bad headaches and vision changes, and they’re told, “Oh, you’re just pregnant,” or “You’re just anxious.”
Everything is also connected historically. It is well-documented that Black people were once deemed to not feel pain or experience symptoms in the same way as white folks, and we were deemed to have thicker skins. There has been an attitude toward Black women to not take our symptoms seriously, and that leads to mortality.
What guided you toward your own interest in maternal health advocacy?
I started my nursing career on a med-surg floor, working with a general population. When I decided to go back to school, I was trying to decide what to focus on, and I thought, “What are some things that keep me up at night?”
I started looking into maternal-child health disparities. I was surprised by the disparities that exist for Black women in maternal health outcomes. I understood that socioeconomic disadvantages and social determinants of health could affect outcomes, but there were significantly higher mortalities for
Black women with a higher education level and socioeconomic status in comparison to non-Hispanic white women who hadn’t graduated high school.
I continued to dig deeper and explore why those differences existed, even when someone is highly educated or has insurance. I started looking into the history of systemic racism and implicit biases in health care, along with the disadvantages outside of health care systems that we face in our communities. That became the impetus for dedicating my career to Black maternal health.
How can nurses advocate for Black maternal health through their roles?
It’s important for nurses to understand the power that they have in making changes to help the populations that they serve.
Without mentorship, some of us might go into the profession thinking, “I’m just going to go work somewhere, see patients, and go home.” Because I’ve been passionate about community work, it has afforded me the opportunity to have mentors. And because I’ve had mentors, I’ve had a better view of how powerful we are as a profession. We are over four million strong, which means that we even have a few nurses serving in Congress right now. Nurses can have a seat at different tables and be part of the decision-making process.
You don’t have to aspire to be a vice president or a director, but if you start by saying, “I don’t like the way things are going on my unit or in my clinic — how about I lead a patient safety initiative? How about I start a maternal health committee to focus on bettering outcomes or patient experiences?” That in itself is advocating for patients and communities. You can make small changes, even within your working environment, that can lead to better outcomes.
It’s also important to find a way to navigate the system you work in and to advocate for patients. We all go through ethics training, whether it’s for nursing, social work, medicine, or any field in health. But we often forget those ethics when we start practicing for a variety of reasons: Maybe we’re scared to speak up — or scared we’re going to be outcasted for speaking up. But without accountability, and without nurses who are always there with the patient as advocates, we’re not going to see better outcomes.
How can we ensure that nurses understand this issue as early as possible, especially for those who are new to the profession?
The essentials of education for both undergraduate and graduate nursing programs include population health and addressing social determinants of health. Integrating small or large activities or assignments into the curriculum exposes students to ways they can use their roles to change health outcomes. If you’re administering the curriculum for a course,
encourage students to identify a topic they’re passionate about and do a project that involves advocacy. We can also lead simulations on other topics outside of just medical treatment. I recently took the initiative to plan a midwifery panel event for undergraduate students. It’s important for students to know information about pregnancy, pregnant populations, and vulnerable populations as well, no matter what specialty area you work in. You have to be able to know how to communicate within a team about things that are not normal. Even for those who aren’t considering a career in women’s health, you are going to be taking care of a woman of childbearing age at some point in your experience.
• Baby Love Program at Golisano Children’s Hospital
• UR Medicine Maternal & Fetal Care
• Nurse Family Partnership
• Postpartum Resource Center of New York
• Doula Cooperative of Rochester
• Rochester Black Nurses Association


UR Nursing was an early leader in the Nurse Practitioner movement. Today, the NP role is America’s fastest-growing profession.
In the mountainous, woodland towns of rural Boulder County, Colorado, Loretta C. Ford, EdD, RN, PNP, FAAN, FAANP, had an important realization about her work as a public health nurse.

Often working independently, Ford would make house calls to children and families who might not have seen a provider otherwise, visit nursing homes, collect statistics, and even test the water quality in local wells. The more her role grew, the more she noticed how nurses could help address deficits in care if they were given more specialized training and decision-making power.
Alongside pediatrician Henry Silver, MD, she would go on to co-found the nation’s first pediatric nurse practitioner program at the University of Colorado in 1965 — forever changing the practice and study of nursing.
The nurse practitioner (NP) title added a sense of legitimacy to the duties that Ford already knew nurses could perform, both independently and as collaborators on health care teams.
“We were the ‘Lone Rangers.’ We had to make decisions,” Ford once said in an interview with CNN.
These words resonate with many University of Rochester School of Nursing alumni who have joined the NP profession.

Michael Hasselberg, ’07N (MS), ’13N (PhD), remembers starting his first NP role in a rural Finger Lakes village where nearly everyone knew each other, and patients felt a deep sense of gratitude for his presence in the community. Without him, access to specialty care was sparse.
By title, he was a psychiatric NP fresh out of his master’s program at the University of Rochester, but both Hasselberg and his patients knew that didn’t capture the full extent of his role: Practicing autonomously, he set up a psychopharmacology clinic, made
visits to jails and nursing homes, and served as the only psychiatric provider for six counties.
“It was probably the best thing that ever happened to me in my career,” recalled Hasselberg, whose rural experiences continue to shape his work today as University of Rochester Medical Center’s (URMC) chief digital health officer. “The disparities in rural communities struck me, and ended up becoming my ‘why’ for the rest of my career.”
The demand for NPs is growing rapidly, and not just in rural areas. Today, the nurse practitioner role ranks No. 1 in U.S. News & World Report’s 100 Best Jobs List, and rivals only wind turbine technicians as the nation’s fastest-growing occupation. Patients are more likely than ever to receive care from NPs and physician assistants in nearly every type of health care setting. And in 27 states, NPs have full practice authority, allowing them to open independent practices.
Today, many nurses see the NP role as a pathway to maximize their impact on patients, practice with greater authority, and grow as health care leaders.
“One of the most unique opportunities NPs have is that they get the training and experience of being a registered nurse on the frontlines of care, and then they can take it to a whole new level, functioning similarly to our partner disciplines like medicine, physical therapy, or psychology,” Hasselberg said.
This is one of the many qualities that draws nurses to the role, said Cheryl Lustik, DNP, RN, MS, APN-C, chief advanced-practice officer at the Margaret D. Sovie Center for Advanced Practice at URMC. She oversees professional development opportunities and senior leadership representation for more than 1,000 nurse practitioners and physician assistants — collectively known as advanced practice providers (APPs).

The Sovie Center promotes a culture of continuous education, in which APPs “have options for career advancement and opportunities for additional education, training, mentorship, or skill development, which hopefully helps them feel more satisfied in their specific role,” Lustik said.
URMC hires about 100 APPs per year, Lustik said. And that investment in non-physician providers has a significant community impact.
“When we support professional growth for APPs within our organization, it enhances our patients’ care,” Lustik said. “Providers are growing their knowledge and skills, which ultimately means that they can take care of more


complex patients.”
This can lead to increased access to care and better patient outcomes and satisfaction overall.
With the number of NPs in the US expected to grow by 45 percent over the next decade, it may be hard to believe now that Loretta Ford’s pioneering ideas weren’t fully embraced 60 years ago.
When she joined the UR School of Nursing as its inaugural dean in 1972, she spent years pushing for national and state recognition of the NP role, even testifying to Congress to advocate for more financial and educational support for non-physician health care providers.
“Introductions of new roles into health care systems may shake things up a bit,” she told the US House Subcommittee on Health and the Environment in 1976. “There is a need to change the organizations and structures by which health care is delivered so that the system of care is so well-articulated

between and among units, that the training and skills of all health professionals are wisely utilized in team relationships to serve people.
Ford’s advocacy helped pave the way for the University to shape the profession and become an early leader in the NP movement.
In the 1970s, the School’s Family Health Nurse Clinician Program became one of the only master’s programs in the country to prepare nurse practitioners in primary care. And in 1989, the School of Nursing launched the nation’s first Acute Care NP program, just a year after New York passed landmark legislation to authorize NPs’ title and scope of practice. The role itself was developed by nurses in Strong’s surgical nursing unit. Graduates of the new master’s program would be able to use the newly state-legislated title of “nurse practitioner.”
The School continues to address emerging needs in health care today. It was among the first 50 nursing schools to introduce a Doctor of Nursing practice program, as part of a national effort led by the the American Association of Colleges of Nursing (AACN) to prepare advanced-practice nurses for clinical leadership roles and to improve health care safety and quality.
In 2021, UR Nursing launched New York’s first pediatric acute care NP certificate, which prepares NPs to care for children of all ages with complex, acute, critical and chronic illnesses, disabilities, or injuries.

Julie Gottfried, DNP, RN, CNS, CPNP-AC/PC, co-founder and specialty director for the certificate program, said she is confident in NPs’ ability to improve access to care for vulnerable populations.
“The role of the nurse practitioner is integral in addressing health disparities in our society today,” said Gottfried, who has worked with children in both primary care and hospital settings.
In part, she credits this ability to nurses’ holistic approach to care.
“In the provider role, I’m able to pull together the pieces, look into the community I serve, and find local sources of specialized care. I consider how I can help my patient — who, for example, may or may not have transportation to get to various appointments — access the resources that are right there in the community.”

Researchers from the University of Rochester School of Nursing were among the first to quantify the impact of NPs in improving primary-care capacity. A 2019 study showed that the growing supply of NPs offset a low supply of physicians in underserved communities across the U.S.

“This has great implications,” said Ying Xue, DNSc, RN, a nursing workforce expert and the Loretta C. Ford Endowed Professor in Primary Care Nursing. “Having NPs present in areas with low access to health care addresses big obstacles. Filling the gap regarding access to health care providers can eventually address health disparities.”
A strong focus on health equity remains at the core of NPs’ work at the University of Rochester today, and opportunities to make direct impacts and implement positive changes are motivating future generations of nurses to pursue the NP profession.
Jose Perpignan Jr., ’16N, ’24N (MS), dreamed since he was a child of working in a role where he could bridge the gap between underserved communities and quality care, when he watched his father volunteering in their Brooklyn, New York, neighborhood as part of a volunteer ambulance service.

“I’ve seen what it looks like when you pour into the community you’re from, and when you don’t have to be a victim of not having the care you should receive,” said Perpignan, who earned his Family NP master’s degree in the spring.
As a bachelor’s student, he supported his mother through a diagnosis with soft tissue sarcoma. The first provider she visited told her that she’d have to have her leg amputated, but that couldn’t have been the only option, he remembered thinking. Upon seeking a second opinion, Perpignan’s mother was told that she’d soon be able to run around and dance with her grandchildren.

“This also motivated me to want to become an NP,” he said. “I wanted to be in a position where I could educate myself, learn, grow, and be able to provide the care and treatment that patients need.”

Susan Blaakman, PhD, RN, PMHNP-BC, FNAP, FAAN, has seen positive, nurse-led changes firsthand as a longtime faculty member and director of UR Nursing’s Psychiatric Mental Health NP program.
One of UR Nursing’s latest NP-led initiatives, the grant-funded Project ENACT (Educating NPs to Address Childhood Trauma), has helped expand the behavioral health workforce serving at-risk children and adolescents. It has trained 70 NPs since its launch and added 18 new clinical sites where students could put the program’s trauma-informed care curriculum into practice.
Project ENACT, which is supported by the Health Resources and Services Administration (HRSA), couldn’t have come at a better time: Adolescents’ socioemotional development was disrupted by the COVID-19 pandemic, and they have faced higher rates of depression, anxiety, and suicidal behavior. Paired with a shortage of mental health workers, especially in low-income areas and communities of color, the need is urgent.
“Health equity is really about bringing services to the most vulnerable in our communities, particularly folks that are historically marginalized and have experienced systemic racism and discrimination. If you have a mental illness, that can sometimes add its own marginalization,” Blaakman said.
Similar strides have been made across several specialty areas at UR Nursing and URMC. Most recently, the University’s Highland Family Medicine family nurse practitioner Residency Program received a $2.4 million HRSA grant to support continued training of more Family Nurse Practitioners to practice in underserved settings and help meet the needs of culturally diverse and clinically complex patients.
385,000 strong
NPs will continue to make a positive impact on many issues health care faces today, such as physician shortages in primary care and specialty practices, the country’s rapidly

aging population and its demand for health care services, and care access overall, said Cheryl Lustik, of the Sovie Center for Advanced Practice.
“It’s exciting to say that this group of health care providers can help improve access and health outcomes and that they’re leveraged in a way in which they really are looked at as providers, respected both by the patients and the physicians that they’re working with.”
In the past year, the profession grew by 8.5 percent to 385,000 NPs.
Many NPs are inspired by Loretta Ford herself, who said in her 1972 installation speech that together, “we will create a new order of things” at the School of Nursing.
“What I have tried to do in my role as a nurse practitioner is to push the envelope, and maybe raise the ceiling, similar to Dr. Ford’s vision of what we as NPs could do for patients,” said Heather Wensley ’11N (MS), ’24N (DNP), a nurse practitioner on Golisano Children’s Hospital’s Adolescent Medicine team who specializes in gender health and eating disorders.
“Our work is important within the walls of the clinic, but it’s also important out in the community,” she said, emphasizing NPs’ ability to advocate for change.

When Ford was first considering whether to move to Rochester and take the School of Nursing dean position, she was encouraged by URMC’s “hope for the future” of the nursing profession and respect for interprofessional collaboration, she said in a summer 2023 interview in her Florida home. Throughout its history, the School has built a solid foundation as an institution that was ahead of the times, and looking ahead, she said, it will continue to be both an agent and acceptor of change.
“I think the University of Rochester School of Nursing is well positioned to take the future on and to create the future that we really need for this nation,” Ford said. “I expect great things to continue at Rochester.”



Heather Wensley, ’11N (MS), ’24N (DNP), grew up with a mother who worked as a surgical technician, often loving to tag along on weekends when she was paged for emergencies. She remembers sitting by the TV in the physician’s lounge of their small Pennsylvania town’s hospital, watching health care workers rush by the doorway, off to scrub into life-saving surgeries.
Those early memories helped Wensley discover her dream of becoming a provider, though she wasn’t sure if that would lead her to nursing or medical school at first.
“I could see the dedication that they had to their patients, and from an early age, I knew that I wanted to get into health care,” she recalled. “I wanted to make an impact on somebody and their family like that.”
Choosing a bachelor’s in nursing paid off in the long term, she said: Understanding the work of a registered nurse and spending time with patients in their most vulnerable moments ultimately helped Wensley become a better pediatric nurse practitioner.
After earning her master’s in 2011, she discovered her passion for working with adolescents through her role as a high-school NP in the Rochester City School District.
“I love their spirit and energy. They have a lot to offer the world, and they have a vision for what they want the world to be like for themselves and the next generation,” she said.
Wensley later returned to Golisano Children’s Hospital
(GCH) in 2020 to join its Adolescent Medicine team, specializing in gender health and eating disorders. Alongside fellow alumna Amy Realbuto, ’06N (MS), she serves as a leader on an interdisciplinary team where NPs are empowered to practice at their full scope and “walk alongside our physician colleagues,” she said. “Our adolescent medicine team is amazing and what makes it so special is the respect and collaboration we all have with each other. We all continuously learn from each other and recognize the unique expertise that we all have. Everyone is vital to the care we provide.”
She shared her gratitude for Susan Michelle Yussman, MD, MPH, chief of the Adolescent Medicine division at URMC, for empowering NPs to practice to the top of their licenses while prioritizing their wellness and ensuring that they’re happy in their roles.
Wensley also credits the School of Nursing’s inaugural dean, Loretta C. Ford, EdD, RN, PNP, FAAN, FAANP, co-founder of the nurse practitioner role, as one of her greatest inspirations to “push the envelope,” find new ways to reduce health disparities, and maximize the impact of her NP position — and that shows in the work she has done throughout her NP career.

Exemplifying nurses’ holistic approach to patient care, she created GCH’s first peer support group for parents of transgender

“It’s a gift to be able to sit alongside people in hard moments in their lives, and to be able to do this work.”
Heather Wensley ’11N (MS) ’24N (DNP)

and gender-nonconforming youth as her Doctor of Nursing Practice (DNP) scholarly project, which she successfully defended in the Spring 2024 semester. Trained to consider biological, social, and other factors that affect a patient’s health, Wensley recognized that the entire family unit is an integral part of teenagers’ development and wellness.
“I believe that people and parents are doing the best they can with the resources they have available. Parents love their children,: she said. “Sometimes they just need somebody to talk to and to talk some of these thoughts and feelings through.”
Research shows that parental support is associated with higher quality of life and protection against depression for transgender youth. The peer support group seeks to help parents better support, understand, and care for their children.
“It has been really special to be a part of it,” Wensley said of the group. “Seeing people connecting with a stranger who has walked through some of the same things that they’re going through helps them know they’re not alone. To hear others’ success stories, and that everything is going to be OK, is really helpful for parents to hear throughout their child’s journey.”
Recently, she has been working with Assistant Professor of Nursing Meredith Kells, PhD, RN, CPNP, FSAHM, to develop an eating disorder (ED) screening tool to introduce at local school districts. She hopes it will address some

pressing issues in ED care: These disorders are starting to develop among children ages 9 to 11 more frequently, and across all age groups, youth of color at risk for EDs are more likely to go undiagnosed.

“To begin to eliminate implicit bias in screenings and eliminate these disparities, we hope to develop standardized ED risk screening tools for younger children, working with both city and suburban schools to ensure all children receive the care they need,” she said.
Being an advocate beyond the Medical Center campus is an equally important part of her role as bedside care.
“The work we do is important within the walls of the clinic, but it’s also important out in the community, which is one of the reasons why I love adolescent medicine,” she said.

The specialty has a uniquely broad reach into adolescents’ lives, with nurses working not only in traditional clinical environments but in schools and community agencies as well.
“Some of the days can be heavy, and you just feel for these patients and these families so much,” she said. “But patients really can get better, and when they do, it’s all worth it. It’s a gift to be able to sit alongside people in hard moments in their lives and to be able to do this work.”

The Dean’s Diamond Circle awards dinner celebrates the significant contributions of School of Nursing alumni, former faculty, and supporters. This year’s dinner was held on April 12, 2024, at Monroe Golf Club.
At the event, School of Nursing Dean Lisa Kitko was officially installed as the Independence Foundation Chair in Nursing Education. The Independence Foundation, through its generous grant, has established and expanded professorships at the School of Nursing, recognizing individuals like Dean Kitko for their exceptional leadership and dedication to advancing health care and fostering cultural change within the community.
“Dean Kitko is a natural choice for this honor, and together we offer our enthusiastic congratulations for her remarkable achievements and this well-deserved recognition,” said David C. Linehan, MD, CEO of the University Rochester Medical Center, dean of the School of Medicine and Dentistry, and senior vice president for health sciences. “Investing in nursing education is key to the health of our community.”

Eileen K. Fry-Bowers, ’97N (MS)
Eileen K. Fry-Bowers, PhD, JD, RN, CPNP, FAAN, a pioneering leader in pediatric nursing practice, research, policy, and education, is the recipient of this year’s Distinguished Alumnus Award.
As dean of the University of San Francisco School of Nursing and Health Professions and a fellow of the American Academy of Nursing, she leads strategic initiatives that expand clinical training, promote health equity, and improve care quality and accessibility. Her roles as past chair and vice chair of the American Academy of Nursing expert panel on child, adolescent, and family health reflect her dedication to best practices in pediatric care.
A pediatric nurse practitioner, Fry-Bowers has directly impacted patient care, using her clinical knowledge to inform policy, publish scholarly articles, and serve in editorial roles. Her research on COVID-19’s impact on vulnerable children and families has been recognized by Congress for its significance.
Eileen K. Fry-Bowers holds a bachelor’s degree from Loma Linda University School of Nursing, a master’s degree from the University of Rochester School of Nursing, and a Juris Doctor from Whittier Law School. She earned her doctorate from UCLA School of Nursing, where she was awarded a Chancellor’s Fellowship and named a University of California Regents Scholar. Her extensive clinical experience spans acute care, specialty clinics, and military institutions. A veteran of the United States Navy Nurse Corps, Fry-Bowers has held faculty and leadership positions across nursing, medicine, and public health, contributing significantly to child health policy and advocacy.



Jonathan G. Terry
Jonathan G. Terry, a dedicated supporter and close friend of the University of Rochester School of Nursing, is the recipient of this year’s Humanitarian Award. For many years, Terry has shown a steadfast commitment to the betterment of the community through insightful guidance, visionary leadership, and generous support. His extensive involvement includes being an inaugural member of the School’s National Council and a staunch advocate for its values.
Terry honors the philanthropic legacy of his late father, George Spencer Terry, Jr. and his mother, Elizabeth (Ann) Gay Terry. In 2004, he founded the Terry Family Talent Foundation, which funds research and education initiatives at the School and charities across the Finger Lakes region.
In 2010, Terry co-founded Allergy Advocates New York in memory of his sister, Ruthie T. Cornell, who passed away due to an anaphylaxis attack in 2009. The organization raises awareness about the dangers of untreated allergic reactions and advocates for related medical and legislative issues.
A graduate of Baldwin-Wallace College, the University of Missouri-Kansas City, and Parsons School of Design, Terry worked as a lighting designer in the entertainment and architectural industries for 27 years. His foundation supports arts and education in the Finger Lakes Region, and at the University of Rochester School of Nursing, it sponsors the George Spencer Terry, Jr. B’49 Endowed Fund in Nursing and the Elizabeth “Ann” Gay Terry B’40 Endowed Fund in Nursing.


McCollister “Mac” Evarts, ’57M (MD), ‘64M (RES)
Dr. C. McCollister “Mac” Evarts, a transformative leader in medical education and a pillar of orthopaedics, is the recipient of this year’s Legacy Award. A graduate of the University of Rochester School of Medicine and Dentistry, Evarts completed his orthopaedics residency at Strong Memorial Hospital. His visionary leadership and commitment to education have left an enduring impact on the University of Rochester Medical Center and the School of Nursing.
Appointed founding chair of the Department of Orthopaedics in 1974, Evarts established a strong foundation for growth. As an ingenious surgeon and skilled administrator, he served as CEO of the Medical Center from 2003 to 2006, launching initiatives that continue to benefit the University. His collaboration with Dr. Loretta C. Ford, founding dean of the School of Nursing, exemplified their shared dedication to advancing nursing education.
Evarts championed the School of Nursing during a pivotal growth period, affirming that outstanding nursing education is essential for any leading academic medical institution. He also helped expand the UR Well program, providing opportunities for students to aid underserved communities, and helped establish the American Cancer Society’s B. Thomas Golisano Hope Lodge.
For
In 2007, Evarts and his wife, Nancy, a 1954 graduate of the School of Nursing, supported the beloved Evarts Lounge. In 2014, he established an endowed professorship in orthopaedics, furthering his commitment to health, medicine, education, and community. Evarts’ influence extends beyond Rochester. At Penn State Health Milton S. Hershey Medical Center, he revamped the medical school curriculum, expanded the faculty, and led the construction of a biomedical research facility. Elected to the National Academy of Medicine in 1997, he continues to educate and mentor at Penn State College of Medicine.
honoring her exceptional contributions to nursing research, education, and interprofessional collaboration.

Frank Dimino
Frank DiMino, an esteemed entrepreneur and philanthropist, is the recipient of this year’s John N. Wilder Award. Born in Grotte, Sicily, he immigrated to the United States in 1934 and settled in Rochester. After his father returned to Sicily, DiMino became the primary support for his family, demonstrating resilience and determination.
He married his wife, Helen, in 1947, and they raised six children together. DiMino began investing in real estate, eventually expanding his small construction company into one of the largest in Western New York. Over the years, he owned and operated diverse businesses, including a thoroughbred horse boarding facility, an 18-hole golf course, apartment complexes, a construction company, and the largest active landfill in New York State.
In 2018, at 92, DiMino retired from active business management to focus on philanthropy. His generous support has significantly benefited the University of Rochester School of Nursing, particularly in the expansion of Helen Wood Hall, a hub for the School’s internationally recognized, innovative nursing education.
A self-made and highly respected businessman, DiMino embodies the spirit of “ever better.” His philanthropy is driven by a profound respect for nurses, acknowledging their essential role in health care. His contributions have profoundly impacted the University and the broader community and demonstrate his commitment to giving back.

Judith Gedney Baggs, ’84N (MS), ’90N (PHD)
Judith Gedney Baggs, PhD, RN, a distinguished researcher renowned for her work in interprofessional collaboration and end-of-life decision making in intensive care units (ICUs), is the recipient of this year’s Dean’s Medal. Currently, she is a faculty member at Oregon Health & Science University (OHSU) and the deputy editor-in-chief of the Journal of Interprofessional Care. Baggs’ academic journey began with a bachelor’s degree in English. After raising three children, she found her true passion in health care, earning an associate degree in nursing and starting her career in the ICU. In 1978, she moved to Rochester, completed a bachelor’s program, and received her master’s degree from the University of Rochester School of Nursing, where her interest in research was sparked.
In 1990, Baggs earned her doctorate at the University of Rochester, focusing on nurse-physician collaboration and its impact on ICU patient outcomes. She later delved into palliative care, exploring ICU end-of-life decision-making to improve the process for patients and families.
Baggs worked at the University of Rochester Medical Center for 12 years as an ICU staff nurse and later spent 15 years at the School of Nursing, serving as professor and associate dean of academic affairs. Later, she held positions as senior associate dean for academics and director of the PhD program at OHSU School of Nursing. Although semi-retired since 2018, Baggs remains professionally active, supporting OHSU faculty and editing the Journal.
In choosing a career, Jane Tuttle, PhD, ’79N, ’84N (MS), thought about how she loves people and loves science, so nursing was the perfect fit. She credits the University of Rochester School of Nursing for shaping her career significantly.
Tuttle appreciates the lifelong learning aspect of nursing education, which allowed her to adapt her path. She found the flexibility and support she needed at Rochester, becoming an advocate for nurse practitioners.
Arriving at the school as a practicing nurse and adult learner, Tuttle completed a tailored program, maximizing her learning from the outset. Her UR education was instrumental in securing positions in Washington, DC, and, later, at Georgetown University and Yale School of Nursing. Returning to Rochester with her PhD, she directed the UR School of Nursing’s family nurse practitioner program for over two decades.
“What is unique about Rochester is the mentoring, the reputation, the way we work in an interdisciplinary way across the University and Medical Center,” Tuttle reflects. “I feel very fortunate to have had a long career in teaching.”
The separate division of adolescent health at the University of Rochester drew Tuttle’s interest, leading her to focus her work on adolescents. She saw them as underserved in health care during crucial developmental years.
Tuttle has directed her giving toward scholarships, emphasizing her commitment to supporting students, especially those facing financial challenges.
“As a faculty member, students are what it’s all about,” she says. “That’s why we do what we do. They need the support, especially those who don’t have family to fall back on. When I started out, I was a young single mom and didn’t have a lot of resources.”
Now, Tuttle and her husband value being members of the Wilson Society, staying connected with alumni, and contributing to the future of the school.
“I knew I wanted to recognize the University of Rochester in my will in memory of my dear friend Eleanor Hall, who was instrumental in founding the School of Nursing here,” Tuttle shares. “When she died, I became a member of the bequest society in her honor.”

The society, formerly named the Eleanor Hall Bequest Society, has been incorporated into the University’s Wilson Society; however, Hall, chair of the Department of Nursing of the School of Medicine and Dentistry from 1957 to 1971, is still remembered profoundly. Tuttle often walks by the portrait of Hall at the school and feels she can hear her mentor’s voice, guiding her in her practice.
Encouraging fellow alumni to join her as donors, Tuttle emphasizes the University of Rochester’s commitment to excellence and innovation.
“The University of Rochester is always on the cutting edge. I am so proud of how highly regarded we are,” Tuttle reflects. “I feel lucky that I found nursing and that the University of Rochester has been a real home to me over all these years.”
A planned gift to the University of Rochester is one of the easiest ways to ensure the greatest and most lasting impact on the programs you care about. Contact giftplanning@rochester.edu to learn more about how to join the Wilson Society, which honors those who have included the University of Rochester in their philanthropic planning.
Polly Straub Spengler, ’81N (MS), retired after 42 years of nursing.
Cheryl Field, ’89N, MS, RN, CRRN, published a new book Prepared! A Healthcare Guide for Aging Adults, as a step-by-step guide to help individuals navigate the complex world of health care as an older adult and reduce the feelings of fear and uncertainty, replacing them with confidence and reassurance.

Cheryl Thompson, ’92N (MS), published a new book, Inside My Husband’s Closet, which tells the story of the year after her husband came out to only her as transgender and how she processed her own feelings and looked to the future.
Mary Ellen Wilson, ’00N (MS), earned the Emergency Nurses Association (ENA) Lifetime Achievement Award in 2003 for almost four decades of exemplary leadership in emergency nursing. Throughout her career, she has been dedicated to promoting safe patient care through educational initiatives and organizational contributions. Her extensive involvement, from teaching courses to chairing conferences, has helped advance the status of emergency nursing, culminating in her presidency of the ENA in 2004, and reflecting her enduring commitment to the field.
Ivelisse Vicente, ’02N, see 2020s.
Andrew Wolf, ’03N (MS), ’16W (EdD), ’19N (PMC), was selected to participate in the American Association of Colleges of Nursing’s (AACN) Advancing Academic Leadership for Deans Program, which serves as a vital resource for new or transitioning nursing deans and chief academic officers, aiming to enhance their executive leadership skills for sustained success. Wolf is currently the Chief Nursing Officer and Director of the Malek School of Nursing Professions at Marymount University, a role he has held since June 2023.
Suzanne O’Brien, ’11N (PhD), is the second co-principal investigator of a research team at Binghamton University that is developing an app to help older adults maintain their balance. If the team successful, O’Brien hopes to apply the same research to assist more patient groups, such as those with Parkinson’s Disease and stroke.

Kamila Barnes, ’11N (MS), ’13N (DNP), associate professor of nursing for the Hofstra Northwell School of Nursing and Physician Assistant Studies, received the President’s Award from the Theta Chi Chapter, Inc. of Chi Eta Phi Sorority, Inc., a professional organization for nurses. The honor was given in recognition of her dedication to the growth of the chapter.


Orlando Harris, ’10N (MS), ’14N (PhD), was named one of the UC San Francisco School of Nursing’s 24 People to Watch in 2024 as a result of to his research and advocacy for sexual and gender minorities. This year, he continues his already accomplished career by co-leading the new California Center for HIV Syndemic Policy Research, which aims to expose the root causes of HIV and syndemic conditions and serve as a leading community-academic collaborative center that pushes boundaries in HIV policy and practice.

Jahaira Capellan, ’12N (MS), ’20N (PhD), received the Change Maker Award, which is one of several awards bestowed by University of Rochester President, Sarah Mangelsdorf as part of her Presidential Stronger as One Diversity Awards celebration. Capellan was honored for her “exceptional commitment, unwavering passion, and remarkable efforts in advancing equity and inclusion in research and healthcare” as she focused her research on better understanding the parenting practices and needs of the Spanish-speaking Puerto Rican community of Rochester.
Sheniece L. Martin-Stancil-El ’19N (MS), ’21N (DNP) recently published an expansion of her master’s CNL capstone project, Comprehensive Approach to Opioid Management in a Primary Care Network.
Ashley Jackson, ’23N (MS), began a new job as a pediatric nurse practitioner at Adirondack Pediatrics in Glens Falls, NY.

Ivelisse Vicente, ’02N, and Nicaury Kim ’23N (MS), collaborated on an abstract that was presented at the Association of Perioperative Registered Nurses in March. It was Kim’s first time being a poster presenter and was part of her capstone project, which started at Sawgrass Surgical Center in 2023 and aims to recycle unrepairable surgical tools such as forceps, needles, and scissors to be donated to medical missions.
Alumna Jessica Tambe, ’22N (MS), RN, SCRN, earned national recognition for her work as a neuroscience nurse educator at Strong Memorial Hospital. Tambe, a graduate of the Master’s in Nursing Education (MNE) program, was named the recipient of the Excellence in Neuroscience Education Award at the American Association of Neuroscience Nurses’ annual conference in Salt Lake City, Utah. The award recognizes nurses whose contributions inspire, develop, and support nurses in the provision of care to neuroscience patients.


“Receiving an award like this shows that anytime I’ve wondered, ‘Am I really making a difference?’ I really am,” Tambe said. “I couldn’t have done it without the School of Nursing. It’s so much more than a degree. The MNE program helped me realize how many opportunities are out there in nursing education.”





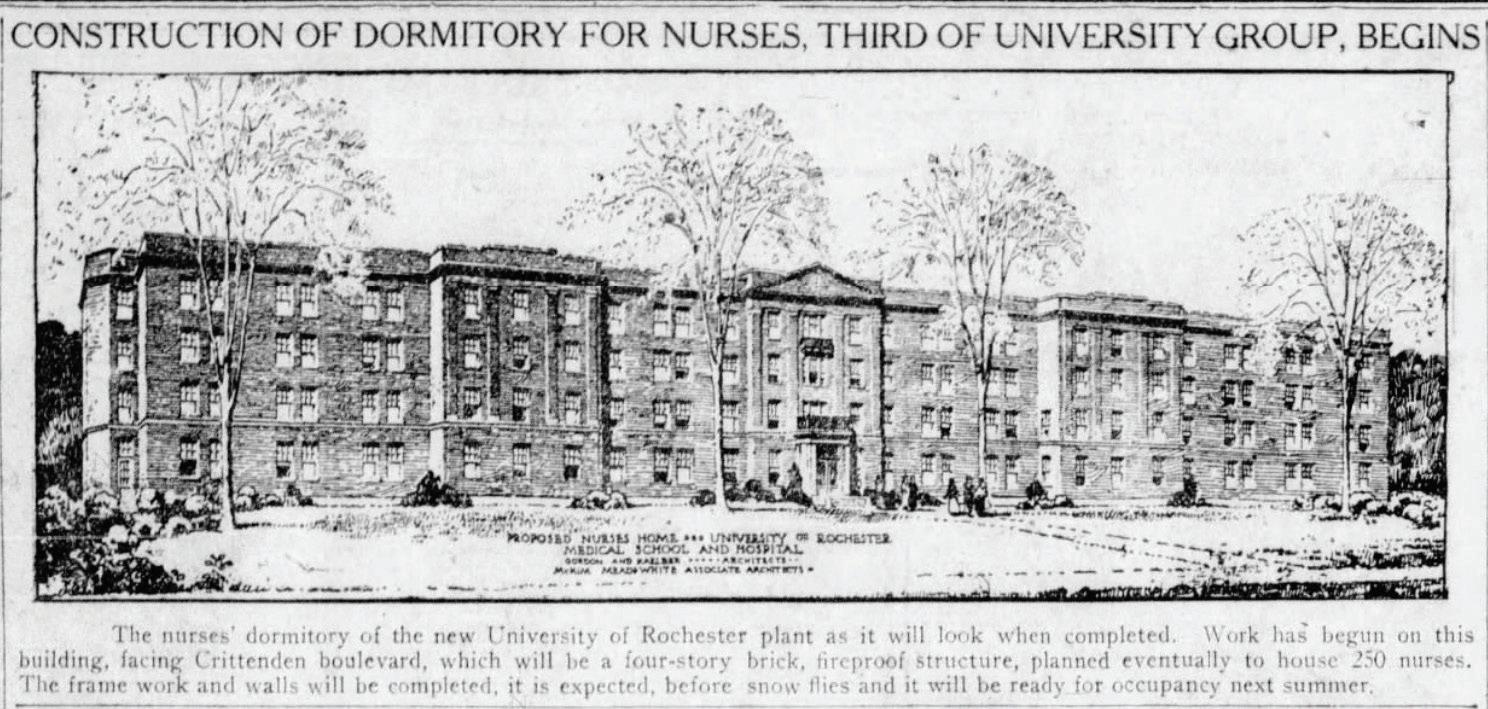
One hundred years ago, on June 4, 1924, construction began on an “attractive, fireproof, four-story building” designed to house 250 nurses in preparation for the opening of Strong Memorial Hospital. The Democrat and Chronicle named Helen Wood Hall in 1934, it honored Helen Wood, the first director of the School of Nursing (1925–1931).

The Epsilon Xi Past Presidents’ Council celebrated its 10th anniversary at its annual meeting on April 13. It was formed in 2014 to maintain the connection among former leaders, as well as to support the activities of the current board of our chapter of Sigma Theta Tau, the International Honor Society of Nursing. Each annual meeting includes a presentation from the current Epsilon Xi leadership. Members of the Past Presidents’ Council have raised dollars for nursing scholarships, collaborated with the Gandhi Institute, and sponsored presentations from the URMC DICE committee and the Black Nurses’ Association.






In 1972, the School of Nursing became an independent school within the University, and Helen Wood Hall was converted from a residence hall to a school of nursing. Dormitories were converted to offices, classrooms, and clinical lab space.
The University of Rochester School of Nursing is preparing to celebrate its centennial in September 2025, marking since the admission in 1925 of its first class of 16 nursing students. Opportunities to celebrate and honor the school’s history will be forthcoming.

Pictured from left: Tobie Olsan ’95N (MS), ’03N (PhD), first Epsilon Xi President Maureen Friedman ’74N, ’91N (PhD), Cindy Gibson ’89N (MS), Jane Tuttle ’79N, ’84N (MS), current Epsilon Xi President Melanie Bobry ’09N, ’22N (MS), ’22W (AC), special guest Dean Lisa Kitko, Maria Marconi ’77H (DPL), ’14W (EdD), Cathy Peters ’81N (MS), ’00N (PMC), Harriet Seigel ’59, ’60N, ’76N (MS), and Luis Rosario-McCabe ’94N, ’95N (MS), ’17N (DNP), ’15N (PMC).
Missing from photo: Madelinie Schmitt ’65N, ’70 (MA), Lisa Norsen ’77N, ’83N (MS), ’07N (PhD), ’92 (PMC), Jamie Oliva ’ 98N (MS), ’16N (PhD), and Shannon Moreland ’04N, ’08N (MS), ’14N (DNP).
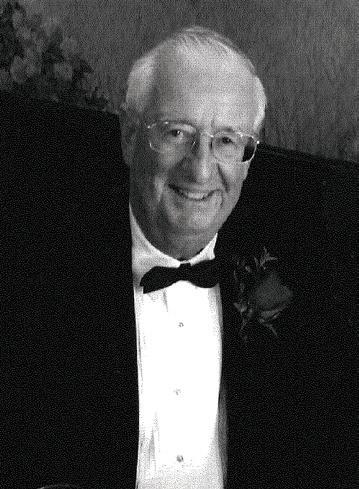

Richard Mulvey, a longtime friend and supporter of the School of Nursing, passed away on Dec. 6, 2023, at the age of 94. Mulvey received the School of Nursing’s Legacy Award in 2013.
Mulvey married Ann in 1982. During Ann’s long career as a nurse, she worked in hospitals, schools, and a private practice office. Ann Mulvey died in 2008 after battling cancer. To honor her memory and her decades of service to the nursing profession, Richard established the Ann Marshall Mulvey, ’55N, Nursing Endowed Scholarship.
Betty (Morehouse) Zeth ’48N passed away on Nov. 21, 2023.
Crystal (Isham) Michel ’48N passed away on Oct. 30, 2023.
Joanne (Menke) Zimmerman ’50N passed away on Feb. 16, 2024.
Elizabeth (Lilygren) Bonvin ’51N passed away on Oct. 21, 2023.
Barbara (Strider) Kuehn ’51, ’52N passed away on Feb. 23, 2023.
Hollis (Troy) O’Brien ’51, ’52N passed away on Dec. 24, 2023.
Phyllis (Padgett) Beard ’53N passed away on Nov. 3, 2023.
Janet (Dapson) Hall ’53, ’54N passed away on April 3, 2024.
Joyce (Popo) Bell ’54N passed away on Dec. 24, 2023.
Word has reached us of the passing of the following alumni and faculty. The School of Nursing expresses its sympathy to their loved ones.

Mulvey was a US Army veteran and attorney who formerly served as Ithaca, New York’s, city prosecutor and judge, and as Tompkins County District Attorney. Dick and Ann moved to Naples, FL., in 2000, where he practiced probate law until his retirement in 2004.
Residual funds from Mulvey’s charitable gift annuities will continue to support future generations of nursing students. We are grateful for his commitment to helping aspiring nurses make their dreams a reality.
Lois (Treadwell) Miller ’55, ’56N passed away on Oct. 4, 2023.
Ann (Vonderahe) Clough ’57N passed away on Oct. 27, 2023.
Bonnie (Fay) Collipp ’57N passed away on Nov. 21, 2023.
Ruth (Gillette) Hennessey ’57N passed away on Nov. 3, 2023.
Joan (Zabadal) Hoeffel ’56, ’57N passed away on Dec. 10, 2023.
Ann (Steger) Smith ’58N passed away on Oct. 27, 2023.
Virginia (Reed) Fisher ’59N (DPL), ’59 passed away on Oct. 25, 2023.
Ann (Van Rennsselaer) Egan ’61N, ’61 passed away on Dec. 19, 2023.
Patricia (Hager) Hinckley ’63N passed away on March 13, 2024.
Carol G. Bailey ’65N passed away on Oct. 1, 2023.
Rosemarie (Radesky) DeRose ’65N passed away on Oct. 20, 2023.
Connie (Durfee) Marion ’65N passed away on Feb. 23, 2024.
1970s
Carol Susan (Gustafson) Giffi ’73N, ’85N (MS) passed away on Nov. 2, 2023.
Christine (Fliss) Kogut ’77N passed away on March 3, 2024.
Joanne E. Layton ’81N (MS) passed away on Nov. 17, 2023.
Judy Feret ’75, ’83N (MS) passed away on March 5, 2024.
Janice Mary (Hanlon) Spiess ’01N passed away on March 10, 2024.
Cynthia A. MacDonald ’12N passed away on Oct. 18, 2023.












Did you receive a promotion? Move to a new city?
Publish your research findings? We want to hear from you! Submit your news and we will share it with your classmates and the UR Nursing community in the next NURSING Magazine. Fill out the alumni class notes form online or mail to:




School of Nursing Office of Advancement and Alumni Relations
Larry & Cindy Bloch Alumni & Advancement Center
P.O. Box 278996 | Rochester, NY 14627-8996
Name Class Year (include maiden name, if applicable)
Address
City State, Zip
Phone ( ) - Cell Phone ( ) -
Occupation
Employer
Family information (Spouse, children’s names)


601 Elmwood Avenue, Box 643
Rochester, New York 14642
Change Service Requested

Moved by a growing need for mental health support she noticed while working as a family nurse practitioner in palliative care and hospice settings, Ann Quinn earned her second master’s degree in the Psychiatric Mental Health NP program this spring. She hugs Professor of Clinical Nursing Susan Blaakman on the stage of Kodak Hall as she graduates on May 17, 2024.