




Heather and David Collings share their experience with preeclampsia and their son Lyndon's stay in the Sally and John Francis Tanner Neonatal ICU at Tanner Medical Center/Carrollton.







Heather and David Collings share their experience with preeclampsia and their son Lyndon's stay in the Sally and John Francis Tanner Neonatal ICU at Tanner Medical Center/Carrollton.

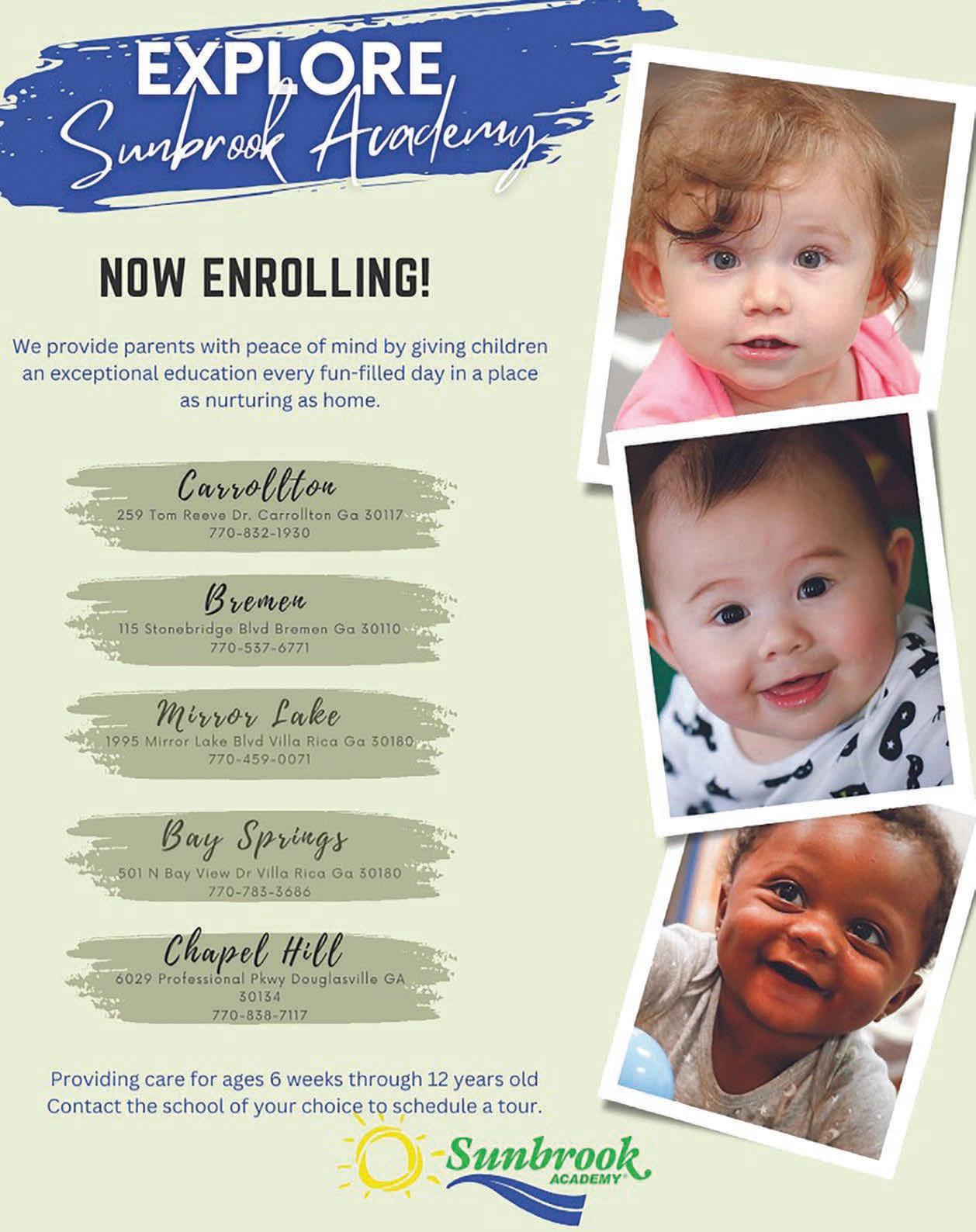
West Georgia Woman is a voice for and about the women who live and work in West Georgia.
Our mission is to engage, inspire, and cultivate a cohesive community for all women in West Georgia by sharing our hopes, our dreams and our lives.
This magazine would not be possible without the inclusion of our advertisers. Please be sure to show your support by doing business with these VIPs (very important partners) so we will be able to continue to share with you our stories about amazing West Georgia women!
Please be sure to tell them we sent you!
Inspiring women wanted. Do you know an interesting woman who should be on the cover of West Georgia Woman? Is there a special project or organization you would like us to feature in our magazine? Let us know! Email your suggestions to features@westgeorgiawoman.com.
Share your special events. Send your upcoming events to: calendar@westgeorgiawoman.com
Need to advertise? Email: Sales@westgeorgiawoman.com Call 404.502.0251
The views, opinions, positions or strategies expressed by the contributing authors are theirs alone, and do not necessarily reflect the views, opinions, positions or strategies of Angel Media, LLC., West Georgia Woman magazine or any employee thereof. Angel Media, LLC. makes no representations as to accuracy, completeness, correctness, suitability, or validity of any information in this publication and will not be liable for any errors, omissions, or delays in this information or any losses, injuries, or damages arising from its display or use.
Mail correspondence to:
West Georgia Woman Magazine
P.O. Box 2782
Carrollton, GA 30112
We welcome your comments and suggestions.
Contact us:
(404) 502-0251
Online: www.westgeorgiawoman.com
Follow us! @WestGaWoman




Publisher/Editor
Angela Dailey
angela@westgeorgiawoman.com
Copy Editor
Need a copy? We mail thousands of copies each month to households through Direct Mail or get yours from our racks at Kroger, Publix, Smith Brothers Supply Company, Southern Home and Ranch Center, Food Depot, Neva Lomason Library and the Tanner Health System Medical Pavilion in Carrollton; Piggly Wiggly in Bowdon, Buchanan, Franklin and Tallapoosa; Thriftown in Bremen; The Little Giant Grocery in Sargent; Fabiano’s Pizzaria, Leaf and Bean Coffee, Crook's Grocery (Temple Ave.) and Lee King pharmacy in Newnan; Tanner Health System's Villa Med and Villa West Office Buildings in Villa Rica; Kroger (Chapel Hill Rd. and Highway 5) and Food Depot on Hiram Douglasville Hwy and Highway 5 in Douglasville; Food Depot and Brickhouse Grille in LaGrange; Food Depot (Villa Rica Hwy) in Dallas; Kroger on Ridge Rd. in Hiram; WM Grocery and Chuckwagon restaurant in Roanoke, Al. and WM Grocery in Wedowee, Al. We have them in larger quantities at Publix (Bullsborough Drive), LeeKing and Thompson pharmacies in Newnan, the Apothecary Shoppe in Douglasville, Publix at Mirror Lake and New Georgia, CVS in Bowdon as well as hundreds of other retail locations and medical offices in 18 cities in eight counties in West Georgia and East Alabama.
Shala Hainer
shala@westgeorgiawoman.com
Photographer
Zachary Dailey
Dailey Life Photography
zachary@westgeorgiawoman.com
Healthy Woman Content Coordinator

Meri Wade
Healthy Woman Editorial
Dana Guthrie, Danielle Wong Moores (writers) Tony Montcalm, Alexis Casey and Ronda Faries (editing and captions)
Advertising Sales
Sales@westgeorgiawoman.com
West Georgia Woman is a monthly publication of Angel Media, LLC. All contents of this issue are copyright 2023. West Georgia Woman magazine, its logo and “Finding our voice. Knowing our value. Making a difference.” are trademarks of Angel Media, LLC. All rights reserved. Print or digital reproduction without permission is strictly prohibited.
All submissions will be included as space is available. West Georgia Woman reserves the right to reject or edit any submissions that are not in compliance with our editorial policy. If you wish to have your submission returned, please include a self addressed stamped envelope with your submission.
good enough health – she’d undergone a heart procedure in 2011.
“I had supraventricular tachycardia,” Heather said. “My heart would beat really fast on its own while I was at rest. I had surgery to correct that, and even after that, I was on medication to help with palpitations and different things.”
The couple found out they were expecting the week of Mother’s Day in 2018 after months of trying to conceive.
“Our pregnancy was actually very easy,” Heather said. “There were no complications, and I didn’t really even have any morning sickness. It was just easy.”
According to David, Heather did have a few weird cravings here and there, but other than that it was a textbook pregnancy.
By Dana GuthrieHeather and David Collings may be most wellknown across west Georgia as the owners and operators of D-BAT, a full-service baseball and softball training center with locations in Douglasville, Carrollton and Peachtree City.
Their passion for baseball and softball is core to their relationship, which began at the University of West Georgia.
“When we had a chance to purchase our first D-BAT franchise location, it was a perfect way to keep baseball in our lives,” David said.
Die-hard baseball fans, especially when it comes to the Atlanta Braves, the couple also have a dog named Wrigley, named for the iconic home of the Chicago Cubs, Wrigley Field.
They married in 2014, and four years later, they began thinking about expanding their family.

The challenges they would face in bringing that child into the world would test the limits of their faith and nearly cost Heather her life.
When the couple decided to have a baby, the first challenge was to make sure that Heather was in
“We had a baby shower at the University of West Georgia the weekend before Thanksgiving,” Heather said. “We went on a tour of the baby area at the Tanner Hospital in Carrollton that morning before the shower, and one of the nurses said that they had ‘better not see us anytime soon.’”
The following Monday, everything changed at a routine check-up. From that day on, there is little that Heather remembers, but David recalls the time clearly.
“When they took her blood pressure at the beginning of the appointment, it was a little high,” David said. “When they checked it again later in the appointment, it had risen even higher. They wanted to do lab work, but due to the holiday, the lab was closed, and they sent us to the hospital for blood work.”
Because of her heart issues, Heather had a urine protein test at the beginning of her pregnancy. Once they arrived at the hospital, they had her do another test and asked her to stay overnight. Her blood pressure steadily began to rise, and they started her on magnesium to control it while moving her over to the hospital’s labor and delivery unit as a precaution. By Wednesday, the doctors felt comfortable taking her off the magnesium.
But Heather would not leave the hospital until many weeks later.
“You can’t get out of bed while on the magnesium sulfate,” Heather said. “I do remember that being awful. I was so thirsty, and I remember wanting grape Fanta.”
As soon as Heather was off the magnesium, her blood pressure started to rise dangerously again. On Thanksgiving, the decision was made to induce labor – even though it would mean a premature delivery at only 33 weeks.
“They prepared us for the fact that our baby would be in the NICU and what to expect,” David said. “The prospect of losing them never entered my mind. Up until then, I was confident that even if the baby came early, it would be OK. Heather would be OK and everything would go back to normal. I was in shock.”
To make matters worse, Heather’s epidural didn’t take. While in active labor, there was one moment of levity with Heather’s obstetrician, Amy Goss, MD, with Tanner Healthcare for Women.
“There I am holding one of Heather’s legs, and Dr. Goss is looking after Heather, and Heather’s phone rings,” David said with a laugh. “It was Dr. Goss’ office calling to remind her of her appointment next week. Dr. Goss just smiled at us and said not to worry, that she would take care of it.”
GA LIC#CN004445
• LIGHT COMMERCIAL
• RESIDENTIAL
• AIR CONDITIONING
• HEATING
• SALES
• REPLACEMENT
• INSTALLATION
• PLANNED MAINTENANCE
• GAS OR ELECTRIC HEAT PUMP

• DEHUMIDIFICATION
• HUMIDIFIERS
• DUAL FUEL
• INDOOR AIR FILTRATION SYSTEMS


• ZONES
As if everything happening was not enough, the hospital’s fire alarm began to go off at the peak of Heather’s labor.
“Dr. Goss said not to worry and that we were not leaving without this baby,” David said. “She sent someone to find out what was going on, and there turned out to be a fire in the kitchen down below, but it was already under control. There was also construction going on in the room next to us with hammers and jack hammers daily.”
David said that the NICU team had told them they would be taking the baby as soon as he was born, if needed, and they did. The couple found out later that their son, Lyndon, stopped breathing once born, and had to be resuscitated.
“I stayed with Heather, and it was about two to three hours before I was allowed to go see him in the NICU,” David said.
By the next morning, Lyndon had improved so much that he began to earn his first awards in his life.
“One of the NICU nurses there does artwork,” Heather said. “She creates badges to show each
WELLS FARGO FINANCING OFFERED ON ALL NEW CARRIER EQUIPMENT
Ask about special financing with approved credit.



Service areas: Carroll, Haralson, Douglas, Paulding, Polk and Heard Counties

Keeping moms and babies safe and healthy during pregnancy, delivery and beyond
Prenatal and postpartum care keeps moms and babies safe, but complications like preeclampsia, blood clots and strokes can occur in any woman, regardless of her care. Black and Hispanic moms are especially at risk.

Some warning symptoms may appear during and right after pregnancy, and others may occur up to a year after delivery:
• A headache that won’t go away or gets worse over time
• Fever of 100.4 degrees or higher
• Trouble breathing
• Chest pain or a rapid heart rate
• Severe swelling, redness or pain of the leg or arm
• Changes in vision
• Dizziness or fainting
Seek care at your closest emergency department. Don’t wait, hoping symptoms will lessen or go away.
Partners, friends and family play a valuable role in ensuring moms get the medical attention they need, too.
Tanner Women’s Care is here to help.
Better birthdays for moms and babies.
LEARN MORE AT tanner.org/better-birth-days
milestone, like their first bottle. The badges look like little medals. She draws and colors them for the babies.”
David said it was almost a full 24 hours before enough of the magnesium sulfate was out of Heather's system for her to see her baby in person for the first time.
“The first time I saw him was hard,” David said. “I just wanted to hold him, but he was hooked up to all these wires and tubes, and I couldn’t. It was difficult to see him in that state. It’s not the picture I had in my head of what becoming a parent would be like.”
Heather doesn’t even remember seeing him after he was born because she was so ill.
“You picture how you want it to go, and ours was everything but that,” Heather said. “You almost feel like you did something wrong because it was my body that caused all of this, but I’m so grateful I was in a place where they could help him. The real first time it feels like I saw him was when I got to hold him on Saturday.”
While Heather’s blood pressure remained elevated, baby Lyndon was improving by the hour. The NICU team first thought he would be there for up to seven weeks, but he was ready to go home after four days.
Heather remained on two medications, five times per day. When the doctors and nurses were confident that Heather’s blood pressure was under control, the family was finally allowed to go home with two medications after a 12-day stay in the hospital. She continues to take one medication to this day.
“Dr. Goss was so calm, and that’s exactly what we needed,” Heather said. “She didn’t panic when the fire alarm was going off, when my blood pressure continued to rise, nothing.”
David credits Dr. Goss, the NICU team and the nurses at Tanner for keeping the family together in unimaginable circumstances.
“We always felt heard, and their confidence helped us,” David said.
Both Heather and David said that their families were pillars of strength and support during their ordeal. Heather’s father was diagnosed with early onset Alzheimer’s in 2015 at only 54 years old. He passed away in December 2019, and looking back at the time, if Lyndon had not come early, he would not have had one of each holiday with him prior to
his death.
“I question why my body did what it did,” Heather said. “I’m a person who always looks for answers, and had Lyndon not come early, he wouldn’t have celebrated both a Christmas and a birthday with my dad.”
They also credit their faith with helping them to endure and enjoy nightly prayer times with their son.
“If we try to put him to bed without it, he reminds us,” David said.
Both Heather and David said it was important to them to share their story because a situation like this can happen to anyone, and it’s important to be informed. “I had never even heard of preeclampsia before this,” David said.
For Heather, it was hard to process how her birth experience went in comparison to what is seen on social media – portrayals of perfect bodies right after birth or serene birth experiences. She said it’s important to normalize that things can and do veer from perfection, but if you are surrounded by care teams, family and friends with your best interests at heart, things can still turn out OK.
Still, the experience didn’t help the postpartum depression that Heather also endured after Lyndon’s arrival.
“I didn’t even know I had it,” Heather said. “The questions they asked me at my post-delivery visit,













perfect.












“His first Christmas, he was just a month old and he won’t even remember it, but I felt like it had to be perfect,” Heather said.
The couple agrees that it’s OK to ask for help and to take advantage of the excellent resources available.

Both Heather and David believe that they are blessed to have had the Tanner “family” to care for them before, during and after their pregnancy.
They will be celebrating Lyndon’s fifth birthday this year and are grateful to be a Tanner NICU

Learn more about Tanner Healthcare for Women – including the health system’s maternity and NICU services – at TannerWomensCare.org.
770.462.5005

Christy Skinner and Shellie Cloud are often mistaken for one another.
“You didn’t realize that she’s a foot taller and she’s a Yankee?” joked Skinner.
They’ve been there for each other in the best of times and – now – in the worst.
In 2021, Skinner’s close cousin, William Downs, was diagnosed with cancer. Although he responded well to therapy at first, the cancer was later found to have spread to multiple organs. He reluctantly went on hospice, but asked Skinner to be with him. And Skinner asked Cloud, her friend, to help.
A few months later, Cloud’s daughter, Katie, was undergoing oral surgery when a terrible complication occurred: Katie, who is globally developmentally delayed and nonverbal, aspirated some of the blood. By the time she came out of surgery, it was too late. She, too, went on hospice, and Cloud turned to Skinner.
The two women have been friends for more than a decade. They’ve also been coworkers, both working as hospice nurses for Tanner Hospice Care. That they were able to be there for one another both personally and professionally during one of

the worst times in their lives, amid the tears, “was a beautiful experience.”
“Just knowing that I could call on someone – and I did,” said Cloud. “I was a wreck. Looking back on it, I couldn’t have done it without her.”
It takes a special nurse to serve in hospice care.
“It takes a compassionate heart,” said Skinner, a registered nurse who was recently promoted to Tanner’s hospice administrator. “Compassionate nurses are everywhere, but hospice is different. You’re dealing with a delicate situation. We know that our patients aren’t going to get better; we’re caring for them until they pass away. Our goal is to keep them comfortable and peaceful until then and to help them have the best quality of life in the time they have left, whether that’s days or weeks or months or years. We’re also there for families who are dealing with some of the worst days of their lives.”
Skinner said she always knew she wanted to be a nurse. “I felt like God called me to this field,” she
said. “He opened up many doors for me to be able to go to nursing school,” including a Tanner nursing scholarship.
Although Skinner worked elsewhere for a time, she came home to west Georgia as soon as she could. She’d never worked in hospice – her only related experience was a short stint in home health as an occupational health nurse – but Tanner Hospice Care had an opening, and she decided to give it a try.

“It just fell into place,” Skinner said. “I never gave a thought of leaving to do anything else because it felt like home, and it became a passion.”
For Cloud, who grew up in Ohio, her call to nursing happened a little later in life. Cloud’s daughter, Katie, was born with a disorder that caused daily seizures.
Cloud was a full-time mother and caregiver to her daughter until Katie was 14, and Cloud decided to go to nursing school.
“In a way, I felt it would prepare me better for her future, but I also felt it would give me something to do,” she said. “I knew Katie would pass before me, so it would give me something to fill my days.”
Cloud’s first job was at the emergency department at Grady Memorial Hospital, but within her first few
weeks, her mother’s health began to decline and she went on hospice at Tanner.
“Her hospice nurse came in, and I just fell in love with her,” said Cloud. “She had this way of helping me be calm about the whole situation. My mom was on hospice for about three months, but I thought, ‘Man, I want to do what she does. I want to be that for other people.’”
Cloud applied to Tanner Hospice Care as a parttime nurse, which became a full-time position by the time she was hired. Now, she’s an on-call nurse, working Wednesdays and Thursdays from 5 p.m. to 8 a.m. and Saturdays from 10 a.m. to 6 p.m.
Tanner Hospice Care is staffed by eight fulltime nurses, four on-call nurses, one administrator and three case managers, as well as certified nurse assistants helping with hygiene care. With other hospice agencies opening in Carrollton and surrounding areas over the past several years, what continues to set Tanner Hospice Care apart is that it’s a “smaller, more intimate” hospice, said Skinner.
“We see patients often, and we get to know them and their families,” she said. “We’re in those homes with patients and families two or three times a week. We’re often seeing patients more than their own families.”
While hospice may represent “the end” for many patients and families, Skinner said it’s much more than that.
At Tanner, after an initial referral, a nurse meets with the patient and family to explain the benefits of hospice specifically for them and what their team can do to help. They assess the patient’s needs – whether that’s medication for pain or anxiety, equipment or something else.
They also educate loved ones on how to help care for the patient, from how to change incontinence briefs in bed or how to position someone to change the sheets.
“We’re developing a plan of care so that we can fully meet that person’s needs individually –whatever we can do to add comfort for the patient but also have ease of care for their loved ones,” said Skinner.
With Tanner’s on-call team, patients and their loved ones also have around-the-clock access to a nurse so they can ask questions, voice concerns or ask for a visit in the middle of the night, said Skinner.
“They have that peace of mind that they’ve got somebody they can call to help them through whatever it is they’re dealing with,” she said.
Ultimately, it’s about hope, peace and joy in whatever time remains.
Caring
Safety Supervision/Transportation
Safety Supervision/Transportation
Dressing/Bathing Assistance
Dressing/Bathing Assistance
Medication Reminders
Medication Reminders
Meal Preparation
Meal Preparation
Hospice Support
Hospice Support

1-800-381-9165
1-800-381-9165
lreaves@nwga-rightathome.com
lreaves@nwga-rightathome.com
jdeville@nwga-rightathome.com
jdeville@nwga-rightathome.com
“I think, with hospice, that hope is very important,” said Cloud. “We focus on that hope as much as we can to help a patient and a family do the things they want to do, and I think that’s not well understood.”
“We hear it sometimes from other doctors: ‘You guys are the symptom management experts,’” said Skinner. “I don’t know if ‘expert’ is the right word, but we try to pull together our skills and resources to manage symptoms so patients have quality of life. We tell them to live the best life they can with what time they have left. You can still be living while you’re dying.”
“I think we alleviate fears so people can enjoy the final days, weeks or months of a person’s life – and be able to say goodbye,” said Cloud.
For Skinner’s cousin, William, – a diesel mechanic in the prime of his life – his cancer diagnosis came out of the blue.

Leiomyosarcoma is a rare cancer that grows in the smooth muscles of the body – the intestines, stomach, bladder and blood vessels. An initial surgery removed the primary cancer, and a second
Website:
rightathome.net/northwest-georgia
rightathome.net/northwest-georgia
Website: www.rightathome.net/northwest-georgia
surgery removed a tumor in the brain.
Then the cancer returned, showing up in his stomach, liver and lungs.
His doctor suggested hospice.
“He didn’t really want to initially, but then he asked me to be his nurse,” said Skinner. In other words, he said, “I’m not going to go on hospice if you can’t be my nurse.”
Emotionally, Skinner couldn’t do his initial assessment; the two cousins had grown up together like brother and sister, and she wasn’t sure if she could handle it.
“I knew I was going to need the help of my coworkers to help me take care of him,” Skinner said.
Skinner leaned on Cloud for help with his needs at home and advice on helping him get his pain and nausea under control.
“I was too close to it,” she said. “Sometimes I needed a different perspective and somebody else taking a look at him.”
During his last few weeks, Skinner, Cloud and the Tanner team helped him feel well enough to do activities he enjoyed. He got out of the house to go fishing and worked on a few vehicles.

The longtime truck driver – who had driven through every state in the continental U.S. except Vermont – was planning a trip to that state when his health suddenly declined. He died peacefully at home.
“He tried to go out and do everything he could at the end,” Skinner said. “And he still had a great attitude. We sat at the table and laughed and talked about our childhood and memories of the past. His wife and sister both said they thought that was probably as therapeutic to him as the medicine. And we had time to come to terms with it.”
A few months later, just before Christmas 2021, Cloud’s daughter, Katie, had all four of her wisdom teeth removed. During the oral surgery, she couldn’t follow commands to bite down on gauze to put pressure on the wounds and stop the bleeding. Unknown to anyone at that point, the blood drained into her lungs.
That night, Cloud said she knew something was wrong. By the next day, her oxygen saturation had started dropping, and she rushed her daughter to an emergency department. The doctor took a chest X-ray, but there was nothing they could do.

The hospice administrator at the time told Skinner what was going on.
“I was like,
The Rapha Clinic of West Georgia (Rapha) is a faith-based, non-profit, charitable ministry serving uninsured adults in West Georgia (Carroll, Douglas, Haralson, Heard, and Paulding counties). Volunteer professionals provide high quality medical and dental care to those most in need. In addition to the best healthcare, Rapha patients receive spiritual support and guidance without forcing beliefs. At Rapha, we believe that good health is everyone’s responsibility.
The Rapha Clinic of West Georgia (Rapha) is a faith-based, non-profit, charitable ministry serving uninsured adults in West Georgia (Carroll, Douglas, Haralson, Heard, and Paulding counties). Volunteer professionals provide high quality medical and dental care to those most in need. In addition to the best healthcare, Rapha patients receive spiritual support and guidance without forcing beliefs. At Rapha, we believe that good health is everyone’s responsibility.
‘No, this can’t be happening,’” said Skinner. “It had been one of my fears. We knew that Katie’s health was fragile.”
“Shellie and I have worked together for so long, I felt like I have watched Katie through the years. She was part of us. When Shellie would have to bring her to staff meetings, I’d go over there and talk to her and pat on her and love on her a little bit.”
Then the administrator told Skinner, “Shellie wants you to be Katie’s nurse.”
As hard as it was, Skinner said, “I knew that I needed to be there. Shellie needed us as much as Katie needed us.”
“Emotionally, I was a wreck,” said Cloud, wiping away tears as she spoke. “I realized that all my knowledge was not helpful. I just know and trust Christy.”
With Skinner’s help and the support of other coworkers, Cloud spent the next seven days being Katie’s mom while Skinner and other hospice nurses handled Katie’s medications, calling her doctor and doing everything they could do to keep Katie comfortable in her last days.
“I’ve seen these nurses in action at work,” said Cloud. “They do this for everybody. I wasn’t anyone special. They just happened to know me longer than they know some of these other patients and families, but they do what they do.”
“I couldn’t have done it without them,” Cloud said, echoing the sentiments shared by Skinner during her cousin’s hospice care.
Please support us by attending our Annual Fundraiser concert, Sound of Medicine on September 10, 2021 at Mill Town Music Hall spotlighting some of West Georgia’s greatest musical performers who happen to be in healthcare.
770.562.4501
www.RaphaClinic.org
Please support us by attending our Annual Fundraiser concert, Sound of Medicine on September 10, 2021 at Mill Town Music Hall spotlighting some of West Georgia’s greatest musical performers who happen to be in healthcare.
“You know, maybe that was the whole purpose of me falling in love with hospice: knowing I would need them someday.” WGW
Learn more about Tanner Hospice Care at TannerHospiceCare.org.







Adriana Bailey, 22, carries on helping others after overcoming cancer
 By Dana Guthrie
By Dana Guthrie
When Adriana Bailey, 22, first started experiencing shortness of breath, she dismissed it as a minor inconvenience.
The full-time college student at Auburn University was close to finishing her degree, raising a beautiful daughter and engaged to the man of her dreams. The Alabama native had no idea her life was about to change.

“My first visit to Tanner Medical Center/East Alabama was on June 14, 2022,” Bailey said. “I woke up that morning and I couldn’t breathe. It was more than just shortness of breath, which I’d been having for more than a week. I blew it off because I was so busy, but that day was different. I was having trouble even getting breath into my body.”
Both her fiancé and her father encouraged her to go to the emergency room, which she finally did.
“They did a lot of tests, including a CT scan, an EKG and several other tests,” Bailey said. “After about four hours, a nurse practitioner named Suzanne Brown asked if I had any family with me, which I thought was weird. I told her my fiancé was on his way and she told me ‘OK,’ and left.
“It was weird, but I had no idea they were about to tell me I had cancer.”

“It didn’t register to me what she was saying,” Bailey said. “She assured me that more tests would be needed to confirm a diagnosis and to not worry or stress until the tests could show what was going on.”
After sharing the news with her parents, Bailey came to Tanner Cancer Care in Carrollton, meeting with medical oncologist Brad Larson, MD, with Northwest Georgia Oncology Centers. He confirmed that he believed she had a type of lymphoma called Hodgkin’s disease, but that a biopsy would be needed to confirm the diagnosis.
He showed her the CT scan showing a 6-millimeter mass pushing on her left lung, causing her breathing issues.
After referring her to a cardiothoracic surgeon in Rome, a biopsy date was set. With a team of doctors behind her, they began to set up a treatment plan.
Part of the mass was removed in the biopsy, but with part of the mass still residing inside, it was decided that Bailey would undergo several cycles of chemotherapy.
After four cycles, a PET scan would be performed to see how she was responding and whether radiation would be needed. Radiation was not an
ideal option as the side effects on someone her age could be devastating.
“With all of this information being thrown at me, I didn’t really know how to respond,” Bailey said. “Both of my parents were crying, and it wasn’t until that moment that I really began to process what was happening to me and accept it. I was devastated that I would not be able to complete my degree in December 2022. I had worked so hard, and I had this plan laid out for my life and it was suddenly interrupted with all these things completely out of my control.”

While Bailey was assured that the disease was caught early and her prognosis for recovery was good, it was hard for her to accept deviating from her plan to graduate even though Dr. Larson recommended she delay her last semester.
With her daughter Anastasia, who was only a year old at the time, Bailey was also worried about the toll this would take on her. Thankfully, Bailey had a superstar of a fiancé who was with her every step of the way.
“He is such a strong man and was with me all of the time,” Bailey said. “I was still dealing with postpartum depression at the time of my diagnosis, which just seemed overwhelming. The way he took care of me and our daughter was heroic.
“We had savings, and he quit his job for a while to take care of us after I gave birth to my daughter, Anastasia in June 2021. Lots of men won’t do that. Some people criticized him for that, saying he wasn’t correctly providing for his family. He not only provided for my physical care and mental health during this time, but he did again during this process as well. He held me when I cried a lot. He was there for all of it. My doctor’s appointments, the biopsy,


my chemo appointments. He’s been the rock for me in the process, and I could not have done it without him.
“My mom also helped out a lot. She took a leave from work and took my family and me into her home from October to January of 2022. While I rested during the day, she took care of my daughter. The days I couldn’t get up out of bed from the chemo, she was there and did everything she could for me. She is the best mother and deserves the world.”
The Tanner staff across the board were also instrumental in getting Bailey through this process.
“For those who may be facing the same thing I did, I would tell them to have faith in their doctors and find a village and support team,” Bailey said. “I have so much love for all of them. Let people help you. It was hard for me to accept help at first, but I realized it came out of a place of genuine love and care for my well-being. I was unemployed going through this, and when people tried to give me money, I didn’t want to accept it. I was also able to rely on my faith in God. When I was first diagnosed, I didn’t really have any faith in God. I had strayed from church and religion, but through this process I found Him. I learned to trust Him and His plan and not the strict plan I had laid out for myself.”
Bailey added that it was extremely difficult for her to withdraw from school for that semester during her treatment and recovery. She was focused on her studies, and it was her dream to graduate with her class because she loved school and learning so much.
She even completed part of her college studies while still in high school so she could earn her degree early. When it came to the day she needed to withdraw, she couldn’t bring herself to do it. Her
fiancé had to push the enter button for her to complete the online form for withdrawal as she just couldn’t do it herself.
“I can’t say enough about Dr. Larson,” Bailey said. “He is an amazing doctor and has helped us so much. He answered every question we had and explained everything to us in a nonmedical way. He creates that bond with his patients, and he always greets us with a fist bump. He is just a good doctor and relates to you.”
Chemotherapy treatments are hard on the body, but Bailey has nothing but praise for the Tanner staff who helped her in those moments.

“The nurses, Britney, Kylie and Michelle – they are amazing,” Bailey said. “The second you walk in, they ask if you need a blanket, a snack, a pillow. They want you to be as comfortable as possible because they know how hard it is. They have conversations with all their patients or allow you to be alone. They see to your needs.
“One of the chemo drugs I had to take can cause burns and sores in your mouth, so they recommended


“He held me when I cried a lot. He was there for all of it. My doctor’s appointments, the biopsy, my chemo appointments. He’s been the rock for me in the process, and I could not have done it without him.”
– Adriana Bailey
to eat something cold while I was receiving that treatment,” said Bailey. “They gave me ice cream and popsicles to help alleviate that. I can’t say enough about those three women.”
Bailey does have one amusing moment about her journey: It’s a tradition to ring the bell when you are declared cancer free.
“On my last treatment day, they knew I was already cancer-free as I had a recent PET scan,” Bailey said. “There was no cancer in that scan, but I needed the last treatment to complete the cycle. On my last treatment, my fiancé came with me, and I presented the nurses with a few gifts for their kindness. My mom also surprised me that day by bringing my daughter and other family members to watch me ring the bell. When it came time to ring the bell, I rang it and I’m standing there all happy and everyone was kind of laughing. I looked up and realized the bell was half hanging off the wall. In my enthusiasm, I broke the bell.”
With successful treatment and the support of her Tanner care team, Bailey has now completed her degree at Auburn and is employed with AltaPointe Health.
“I am a care coordinator working with children and adolescents,” Bailey said. “After they see their therapists, I develop their homecare plans.”
Bailey’s experience with getting her own mental health treatment inspired her desire to go into the field of psychology.
“I’ve always been passionate about mental health after my own struggles in high school,” Bailey said. “My parents are from a different generation where those types of things were not really talked about. I didn’t really get the professional help that I needed at the time. That’s why I want to help children and teenagers who are in a place like I was. I was dealing with anxiety during those formative years.”
Bailey believes her experiences give her a unique perspective beyond what she learned in the classroom and is ready to do all she can to help young people get the treatment they need. WGW
To learn more about how you can support lifesaving care for local patients at Tanner Health System’s Roy Richards, Sr. Cancer Center, scan the QR code and make your impact today.

“Everyone helps each other for the common goal of caring for our patients. We provide a level of care that’s the best in the region. We care.”
We’re one of the largest employers in west Georgia and east Alabama, with more than 4,000 team members.
Making sure each one of them is empowered to be themselves makes us a destination not just for care, but a career.
To be a healthcare provider of choice, we have to be an employer of choice.
#ExperienceTanner for yourself. careers.tanner.org

Paying attention to symptoms paid off for heart attack survivor Penny Freeman
 By Danielle Wong Moores
By Danielle Wong Moores
As Penny Freeman laid in her bed, there was a thought that wouldn’t leave her mind: “If I fall asleep now, I’m not going to wake up.”
She forced herself out of bed – but couldn’t make herself believe that she might be having a heart attack.
“I’m usually the caregiver,” said Freeman.
She’s a mom to 15-year-old twin boys, a 37-yearold son and a daughter-in-law, plus a grandmother to two grandchildren, all of whom recently moved into the same sprawling, two-level home in Bowdon.

That new home was just remodeled, and Freeman and her family had been staying with other relatives. All the stress meant that while Freeman was caring for her family, she wasn’t taking the best care of herself.
High blood pressure runs in her family, with her mother and older son both on medications.
“I was not very good with my blood pressure medication for about nine months prior,” said Freeman. “I got on this, ‘Why am I taking so many meds? I don’t feel bad.’”
One Saturday morning, Freeman woke up not feeling normal.
She already knew her blood pressure was high; she’d been scheduled to have a tooth pulled the previous Tuesday and the practice “wouldn’t touch me,” she said. “My blood pressure was outrageous. I knew that I needed to follow up with a doctor and get back on my meds.”
She’d started taking her medications again on her own and was working on the doctor’s appointment – since the move, she needed to change physicians. But then came that odd feeling on Saturday morning. It wasn’t pain, “but I wasn’t feeling well.”
Freeman tried to go about her day. She and her sons went to Carrollton to get lunch at Zaxby’s. But she couldn’t get over the feeling that something was wrong.
“God was trying to tell me something,” she said.
Finally, she called her daughter-in-law, Christian Parlier, an ICU nurse, to ask if she should go to urgent care or come back home. They talked about her symptoms, until Parlier finally asked, “does it feel like pressure, like someone’s sitting on your chest? Then you need to go to the hospital immediately.”
Terrified, Freeman did a U-turn on Highway 27 and drove herself and her sons to the emergency department at Tanner Medical Center/Carrollton.
“I was so worked up, I just patted my chest,”
Freeman said. “I couldn’t talk because when I would start to talk, I would start crying. When my daughterin-law was like, ‘yes, get to the hospital,’ it was, ‘Oh my God, am I really having a heart attack?’”
The man at the desk understood her hand signals and asked if she was having chest pain.
Freeman nodded, and after getting her name and date of birth, Tanner’s emergency department staff immediately got her into a room and started an electrocardiogram to check her heart’s electrical activity and ran bloodwork.
Her son arrived to pick up his brothers while her daughter-in-law came to stay with her. It felt like only minutes before Rajat Jhanjee, MD, a board-certified cardiologist and electrophysiologist at Tanner, introduced himself and told her that her bloodwork showed specific biomarkers that indicated she’d experienced a heart attack.
Freeman still assumed she’d be monitored and would go home the next day.
“I was feeling fine,” she said, “but my daughterin-law told me, ‘That’s because they gave you medication, and that’s why you’re feeling OK.’”
Freeman spent Sunday anxious to get home, and on Monday she had an echocardiogram and underwent cardiac catheterization to further examine her heart and potentially place a stent.
The staff told her, “When you wake up, if everything’s OK, you’ll be back in the room you were in. If we have to go ahead and put in a stent, you’ll still go back to the third floor, but to a different room.”
Instead, Freeman woke up still in the cath lab.
“You’ve got several blockages,” she remembers them telling her. “We think the surgeon should take a look.”

For Freeman, who’d only ever had one other surgery in her life – to remove a cyst from her left wrist when she was in the eighth grade – the prospect of open-heart surgery was a shock.
“It didn’t feel real to me,” she said.

She met Tanner cardiothoracic surgeon Omar Lattouf, MD, physician assistant Gene Coughlin, PA, and nurse practitioner Cody Connell, NP-C, who explained what would happen next.
“Coronary artery bypass surgery treats blockages in the arteries of the heart by using blood vessels from elsewhere in the body to replace damaged vessels,” said Dr. Lattouf.
With three blockages in her coronary arteries, Freeman would undergo a triple bypass, using blood vessels taken from her legs.
Dr. Latouff gave her options: “We could do the surgery tomorrow or wait until Friday.”
“Let’s get it over with,” she said.
She was moved to cardiac ICU where her prep began, including more tests and bloodwork, shaving and a shower with a special soap.

She met with anesthesiology, and Connell sat down with her and her daughter-in-law – who was able to spend the night with her in her room – to explain what would happen during the procedure.
Her anxiety could have crept up again, but Freeman credits her nurses, Joni Cox, RN, and Michelle Harper, RN, who chatted with her about family, their jobs and their lives.
“They were so calm, and their calmness helped me to be calm,” said Freeman. “They were so encouraging and just the sweetest. Very easy to talk to, and it just helped me keep my mind off things.”
The morning of surgery, she bathed one more
time and received medication to help her relax. Her nurses covered her in warm blankets and she was wheeled down to the cardiothoracic operating suite.
The next thing she knew, she woke up in recovery.
Freeman remembers a nurse calling her name and waking up still intubated. She was asked to breathe “like she was breathing through a straw.” She drifted back to sleep and woke up again in her room, without a breathing tube, and being fed ice chips by her nurse.
During her recovery, dry mouth was the hardest part, she said. Because she couldn’t drink yet, she used ice chips and a special sponge applicator to rub water on her lips and her mouth.
She also remembers being told that Dr. Lattouf typically keeps his patients in the operating suite a little longer to ensure there are no complications.
“Thank goodness he does,” said Freeman, as she “threw” a blood clot, and Dr. Lattouf reopened her to remove it.
The next day, it was time to get up and walk. During her surgery prep, Connell had given Freeman a heart-shaped pillow that he drew on with a marker to show her where her blockages were and how they would build the bypass vein with an artery from her leg.
“That pillow was my friend” during recovery, said Freeman, who hugged it to help support her chest muscles when she was rocking in bed to sit up and then get to standing.
During the next three days, Freeman walked as much as she could. She had four drainage tubes to help the incision heal, and they were finally removed.
Her daughter-in-law bought a recliner for Freeman to sleep in during her first days at home and found a shower chair. Her nurses told her that she was a “star patient,” and when on Sunday, Coughlin told her she could go home that day or stay one more night, Freeman immediately said, “home today please.”
At home, Freeman had a strong support system around her – her brother, her sons and daughter-inlaw and her mother.
The first few days were hard.
“Everything bloomed while I was in the hospital,” she said – and her pillow was a life-saver as she hugged it when she had to sneeze or cough due to allergies.
She was on her pain medications for only about a day longer and had a machine that provided suction
Your heart matters, so our team of cardiovascular experts do their best to keep it from missing a beat.
We bring you the latest advances in cardiac testing, treatment and rehabilitation — detecting heart disease early and managing your condition.
Should you have a heart attack, our team of interventional cardiologists are available around the clock at our accredited chest pain centers to provide life-saving angioplasty and stenting.
And open-heart surgery is now available in Carrollton, so our team can save even more hearts and change even more lives.
Get care your heart will love, right here at home.
Learn more and find a trusted expert at TannerHeartCare.org

on her incision for about a week. She slept a lot, but by that weekend, “I was feeling really good.”
The wound dressing and suction machine came off next, and that next week she was listening in on meetings and calls at work and was easing in by doing a little laundry.

By the third week, “I was back at it,” she said.
Today, Freeman still has a little lingering swelling in her left leg where the blood vessels were removed for her bypass. Cardiac rehab at Tanner is helping;

she’s going three times a week and is up to seven minutes on each machine and is lifting three pounds.
She’s also changed her diet – “I was a salt girl,” she said. Potato chips and salting her watermelon are no longer parts of her diet. “I’m just trying to eat better, take my meds and take care of myself. I’m paying attention to that.”
In the meantime, she was cleared by her doctors at Tanner to go to Six Flags Over Georgia – she and her family are season passholders – and she just
We make it easy and convenient to get yours.
• Easy scheduling through your Tanner MyChart app
• Extended, convenient hours at multiple locations
• Close-to-home access aboard the Mammography on the Move mobile mammography unit, serving west Georgia and east Alabama
• Clear 3-D imaging for reliable results at Carrollton, Villa Rica and Bremen locations
And if an issue is found, you’ll have continuity of care through Tanner Cancer Care — with treatment options within three days.
Get hours, locations and more at tanner.org/mammography or call 770-812-9721.

Breast Health-WGW-2023-HalfPage.indd 1
returned from a cruise to Aruba, Bonaire and the Dominican Republic.

She’s still a caregiver, but she also recognizes that she, too, deserves attention.
“I think that as moms, we take care of everyone else and not ourselves,” she said.
Her best advice is, "Know your body. Recognize when something is not right. It’s really just paying attention to how you’re feeling.”
She also gives credit to Tanner.
“I felt like their only patient when I was there,” said Freeman. “I was a priority from the minute I walked in the door, touching my chest and not being able to speak, to when I left. The
nurse manager came and checked on me, the anesthesiologist came the day after. Dr. Jhanjee saw me over several days. They were all so super nice and caring toward me – calm and soothing. If I started getting nervous, they brought something to help with my anxiety. When they had to get me up, they were very patient and didn’t rush me. I could go at my own pace. I would recommend anyone to go there; they were fabulous."
Her daughter-inlaw works at another local hospital, “but I’m trying to get her to move to Tanner,” she joked. WGW
More on Tanner’s heart care services – including openheart surgery –can be found at TannerHeartCare.org.
Kaylee and Zack Cargle grateful for team who helped welcome Henry into the world
 By Dana Guthrie
By Dana Guthrie
When Kaylee and Zack Cargle found out they were expecting their first child, there was nothing but joy in their lives.
“Zack and I ran in the same circle of friends, and I really met him through my best friend Amy,” Cargle said. “We started dating after Amy’s wedding when Amy’s mom told Zack ‘enough already, go ask her out,’ and it just worked.”
The couple had always been told that it would be difficult – if not impossible – to conceive a child. Despite discovering that she was pregnant in August 2022 while recovering from COVID-19, her doctors assured her that her pregnancy would not be affected.
As the weeks and months passed, their growing excitement mounted until a routine doctor visit changed everything.
Getting pregnant was supposed to be hard for Cargle – she’d previously been diagnosed with polycystic ovarian syndrome (PCOS). PCOS is a hormone condition that can make it harder to become pregnant. It can cause irregular periods, excess hair growth and put women at risk for other conditions like diabetes and high blood pressure.
“I thought that I would have a hard time getting pregnant with PCOS, so we were surprised it happened so quickly,” Cargle said. “I have had so many problems, and getting diagnosed with PCOS can be difficult. I had a great gynecologist when I was 18 years old who took the time to listen to me. She was very much ‘women forward’ in her thinking, and I was not dismissed like so many people are who may have PCOS. They are often told all their problems will be fixed by just losing weight, and that’s not true.”
Cargle started treatment for PCOS her freshman year of college and, despite having a dedicated doctor and the right diagnosis, she still struggled with some of the symptoms of PCOS and the side effects of some of the treatments.
“It’s hard to talk about it, honestly,” Cargle said. “The weight gain, the excess facial hair that can happen. But these things need to be talked about. I was also on the verge of being pre-diabetic as well. I also had a weird thing where my feet would swell all the time. It’s related to the other stuff, it’s just one additional challenge I’ve had with my body. PCOS isn’t talked about enough, and it needs to be. It helps so much to have doctors who want to listen to you and help you through what you’re dealing with.”
While recovering from COVID-19, Cargle noticed that she still wasn’t feeling like she normally did. Even her missed periods were not an unusual occurrence due to her PCOS. She began to think, “what if…?”
“Since we had been tracking my ovulation in order to help our odds, the kits also came with pregnancy tests,” Cargle said. “I thought I’d been pregnant the month before, but I wasn’t. I took the test and couldn’t believe what I was seeing: It was two lines instead of one. My husband was still sound asleep and I ran out there waving this stick in my hand yelling, ‘Zack, Zack, Zack, Zack, Zack!’ He was so excited when he woke up to realize what I was saying.”


Tiffany Stanfill, MD, of Tanner Healthcare for Women in Villa Rica, assured Cargle that her recent recovery from COVID-19 should have no repercussions on her pregnancy, but there was one danger on the horizon that Cargle did not see coming: preeclampsia.
Preeclampsia’s biggest symptom is high blood pressure. It begins after 20 weeks of pregnancy in women whose blood pressure had previously been in the standard range. Untreated, it can lead to serious or fatal complications for both the mother and baby.
Along with high blood pressure, preeclampsia signs and symptoms may include:
• Excess protein in urine or other signs of kidney problems

• Decreased levels of platelets in blood
• Increased liver enzymes that indicate liver problems

• Severe headaches
• Changes in vision, including temporary loss
of vision, blurred vision or light sensitivity, floaters in the eyes
• Shortness of breath, caused by fluid in the lungs
“We made it to week 32 with a textbook pregnancy,” Cargle said. “I had two appointments near that time where I had slightly elevated blood pressure. I deal with swelling in my feet and legs regularly, and I knew that it would get worse with pregnancy, and it did.
“It was a Monday when Dr. Stanfill wanted me to do the 24-hour urine test. We were on our way to Charleston for a short trip that my parents received as a Christmas gift. She said it was OK to go, but to take it easy. About two and a half hours into the drive, Dr. Stanfill called and told me that I had preeclampsia. It wasn’t bad enough for me to cancel the trip, but I did need to be careful.”
When Cargle returned, she began seeing her care team twice per week and was put on modified bed rest. She also began medication to help control her blood pressure and learned to take her blood pressure at home.

Additionally, she began taking shots to help mature her baby’s lungs in case of a premature delivery. On March 8, 2022, Cargle was in the
waiting room for her scheduled appointment and started feeling unwell. Her care team admitted her for observation.
“We had a little freak out, and we called our parents,” Cargle said. “We knew this might be a possibility, but it was still unnerving. We had planned on an early induction around 37 weeks due to my hypertension, but moving that date up was scary. I had to stay in the hospital from then on. We had ups and downs. I missed my brother and sister-in-law’s wedding. I watched it online, but I cried the whole time. They came in to take my blood pressure while the ceremony was starting, and they couldn’t get a good read because I was a mess. I was sad and happy at the same time.”
Cargle finally made it to her induction date, but it was not easy. By that time, the protein in her urine was in the 4,000 range, and she was carrying more than 30 pounds of extra fluid on her body, making it impossible to walk.
“It looked like I had a water balloon on my belly under where the baby sat,” Cargle said. “My hands were so swollen that I couldn’t make a fist. I hadn’t hardly moved at all, and now it was time to have a baby. It was like being on the couch for years and then getting up to run a full marathon.”
To make a tense situation even more harrowing, during the delivery, the cord became wrapped around the baby’s neck.
Although the situation was serious, when Cargle realized the care team was able to dislodge the cord, she was able to to regain her positive attitude.
“I try to joke when a situation is hard,” Cargle said. “That’s how I cope and deal with it. Between pushes, I was trying to make jokes because it made me feel better.”
“We knew we were in good hands. I can’t say enough about Dr. Stanfill. She just cares so much. I think she even traded weekends with another doctor just so she could be there for my delivery. She would check on me even when it wasn’t her rounds to be making. She listened to me and to all my fears. She is so passionate about what she does, and she cares about her patients. She has so much heart.”
about Dr. Stanfill. She just cares so much. I think she even traded weekends with another doctor just so she could be there for my delivery. She would check on me even when it wasn’t her rounds to be making. She listened to me and to all my fears. She is so passionate about what she does, and she cares about her patients. She has so much heart.”
Cargle also said that Dr. Stanfill was mindful of Cargle’s anxiety –something she’d been dealing with even before her pregnancy.
– Kaylee CargleAfter two and a half hours, Dr. Stanfill told Cargle that she could have three more pushes along with the use of a vacuum, and that if the baby still wasn’t moving along as it should, they would have to have a C-section.
“Thankfully, with the help of the vacuum, those pushes were all we needed,” Cargle said. “It was also heartbreaking because Henry didn’t cry and was gray. We knew he had a heartbeat, and I held him for a few seconds on my chest before he was taken to the nursery. We were all crying because the thing you wanted to hear most was that cry, and we didn’t hear it.”
Cargle said the staff at the Maternity Center at Tanner Medical Center/Villa Rica were the most kind and caring group of people in the world. She’s grateful for their care of Henry.
Despite being a little jaundiced, Henry would be fine – but Cargle was not out of the woods.
Cargle developed pneumonia because she had aspirated at some point. While Henry was born on March 19, Cargle would remain hospitalized another week.
“God was very good to us,” Cargle said. “God had us at the right place with the right doctors. We knew we were in good hands. I can’t say enough
“She remained calm, cool and collected,” Cargle said. “She would always be honest with me but would never talk to me in a way that would add to my anxiety.”
Cargle has nothing but praise for the entire staff at the Maternity Center at Tanner Medical Center/Villa Rica, especially the nurses. She said that even when it wasn’t their “time” to have her as a patient, they would still drop by and check in on her.
“They are all incredible,” Cargle said. “God knew I needed Dr. Stanfill and the staff at Tanner with me in this process.”
Cargle isn’t sure when they will add another baby to their family, but Dr. Stanfill assured her that she would be with her as they now know what to watch out for when they decide to do so.

“I know I can put my complete trust in her and in the Tanner staff,” Cargle said. “Some of the nursing staff had also dealt with preeclampsia in their own pregnancies, and they would just come by and talk to me and tell me they understood what I was going through. That is something you can’t teach in a classroom, that compassion for patients and a willingness to step outside a daily duty and come to you on a personal level. I could not have made it without that encouragement.” WGW
Learn more about Tanner Healthcare for Women – including the health system’s maternity and NICU services – at TannerWomensCare.org.
Women’s Health at Villa Rica Focuses on Medicine and Then Some
 By Danielle Wong Moores
By Danielle Wong Moores
Alcha Strane, MD, is only 5 feet, 4 inches tall. But she knew that if she wanted to earn a full scholarship to college, she had to play a Division I sport. So, the petite powerhouse got it done playing collegiate basketball.
“Yes, I know,” she said with a laugh. “If I have a goal, I’m going to get it done. It’s not an ‘if,’ it’s a ‘when.’ I’m an unrealistic optimist.”
Dr. Strane credits her determination and drive to a work ethic instilled in her by her parents, Cheryl and Albert, and a strong faith in God.
That determination and drive are also what make Dr. Strane a great physician to her patients.
A board-certified obstetrics and gynecology specialist at Tanner Healthcare for Women in Villa Rica, Dr. Strane is building a holistic practice that cares for girls and women ages 7 to 97, at all stages of life, offering not only medicine but also health and wellness.

Educating her patients and encouraging them to be their own best advocate are her main goals.
Her favorite moments are when patients say, “thank you so much for listening and taking in what I had to say and planning for me. I’ve seen so many doctors; no one ever taught me that. No one has ever said it that way, and I really get it now.”
“That’s the best feeling for me,” she said.
In deciding to pursue medicine, “my mom was a big influence,” said Dr. Strane, “and the other women in my family.”
On the one hand, her mother specializes in women’s health and holistic medicine and has been Dr. Strane’s role model on caring for the entire woman, not just her medical needs. On the other hand, Dr. Strane watched her aunts and a grandmother struggle with obesity and diabetes.
Despite briefly considering orthopedic surgery, she realized during medical school at Morehouse School of Medicine that what she really cared about most was helping women with their health needs.
Dr. Strane came to Morehouse after putting herself through college playing Division I basketball for Oregon State University and the University of San Diego.
Being a scholar-athlete had a price: Her science grades weren’t where they needed to be.
Morehouse’s post-baccalaureate program gave her a way to take intensive science courses and demonstrate that she had the focus and drive to succeed in medical school. For most students, it’s a
homelifegroup@kw.com


two-year program; Dr. Strane got it done in one.
That she was meant to be an OB/GYN was confirmed during her third year of medical school.
“I did my first delivery, and it was just amazing,” said Dr. Strane. “I delivered the baby because all the residents in training were off taking an exam, and it was just me and the attending physician. That’s unheard of as a medical student, so that was a huge blessing for me.”
Another sign was the fact that she could stay cool and give direction under that kind of pressure, which an OB/GYN she worked with pointed out.
“They said, ‘I think you’re more OB/GYN than you realize,’” said Dr. Strane. “It turns out they were right.”
After finishing her residency in obstetrics and gynecology at Wellstar Kennestone Hospital in Marietta, where she served as chief resident, Dr. Strane said she was looking for a place that felt like family.
She found that at Tanner.
In her practice at Tanner Healthcare for Women in Villa Rica, Dr. Strane treats vaginal issues and

abnormal bleeding, counsels girls when they begin their periods, supports infertility and pregnancy care, handles incontinence, prolapse and fibroids, and supports women experiencing menopause.
She also provides coverage in Tanner’s emergency departments and is a primary care doctor offering annual physicals.
But her practice doesn’t focus only on medicine.
“It’s more looking at the person as a whole – mind, body, spirit –and making sure that the decisions we’re making for your health aren’t just medicine,” said Dr. Strane. “I’m not just going to prescribe antidepressants; I’m going to suggest we talk to a counselor or see if there are any other strategies if you’re having mental health issues. Or physically, it’s not just about weight loss medications, but what dietary changes should we make and how can we teach you to shop healthier and cook healthier.”
Being pregnant during her residency only added to her training as OB/GYN.
While she’s not saying that you must carry a child to be a successful OB doctor, “I never would have known a lot of things my pregnant people are going through if I hadn’t gone through it,” said Dr. Strane, who with her wife, Tori Lewis, is mom to 17-monthold son Kai.
Dr. Strane made deliberate choices when it came time for the delivery so she would know what her patients were going through. She experienced having her water broken and had Pitocin to induce contractions, both without pain relief; she chose IV medication; and she had an epidural.
“I wanted to know what each of them felt like and what worked for me and how it made me feel,” she said. “I did it so I would know which ones I could speak to.”
Days in the clinic are busy for Dr. Strane’s growing practice, and every patient gets the benefit of her focus and her time. For her, it’s all about education, advocacy and a holistic view of the patient.

“I believe in education for my patients,” she said. “It’s a buzzword, but shared decision-making? I’ve always been into that. I want to give you the options, I want to give you the education behind
why I’m telling you these options and I want you to make the choice. The reason I’m like that is because the outcomes are better when you make your own decision and you know why, instead of me just telling you.”
The advocacy piece goes back to her family. She still has family members call and put her on speakerphone while they’re at their physician’s office, so Dr. Strane can ask questions that might be overlooked and offer clarification when it’s difficult to quickly process information.
Dr. Strane conducted research into Black maternal mortality for about a decade during medical school and residency, educating patients to learn to advocate for themselves and creating an app to teach residents about unconscious bias and how to listen.

“I want to be that family member for my patients and give them questions they might not have thought about or give them the space to ask those questions and feel safe doing it,” said Dr. Strane. “This is not easy stuff. Each patient has a story that we want to listen to so we can understand them as a whole.” WGW
Follow Tanner Healthcare for Women on Instagram and Facebook.
“I want to be that family member for my patients and give them questions they might not have thought about or give them the space to ask those questions and feel safe doing it.”






We’re making your health our priority with the highest quality services and care, keeping you and your family healthy. From our top-notch physicians, nurses and clinical staff to our growing list of advanced medical services, innovative diagnostic imaging and state-of-the-art surgical care, we’re here for you.





We offer:

• Behavioral health
• Breast health
• Cancer care
• Emergency care
• Gastroenterology care
• Gynecology care
• Heart care
• Maternity care


• Neurology care
• Obstetrics
• Orthopedics
• Primary care
• Pediatrics
• Urology care
• And more