PATIENT MINDSET TRAINING CLOSING THE WOMEN’S HEALTH GAP IDENTIFYING AND MANAGING SIPE AI AND MENTAL HEALTH AUTUMN 2024 PP100022780 This magazine is FREE for industry professionals. Subscribe: www.hospitalhealth.com.au/subscribe
TECHNOLOGY ISSUE











HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 2 Targeted prostate cancer treatment hopes to minimise side effects 34 This magazine is FREE for industry professionals. Subscribe: www.hospitalhealth.com.au/subscribe Eliminating parasitic diseases in remote communities 08 12 Open water swimming: identifying and managing SIPE 54 Enhancing IVF patient experience with AI Should chatbot psychologists become part of the health system? 20 Bridging the maternal care gap with technology TECHNOLOGY Technology to cut hospital readmission risks 58 iStockphoto.com/ipopba 24 Designing a ‘quiet hospital’ DESIGN IN HEALTH 30 Improving the patient journey 3D-printed skin could improve reconstructive surgery 42 16 TECHNOLOGY ISSUE PATIENT MINDSET TRAINING CLOSING THE WOMEN’S HEALTH GAP IDENTIFYING AND MANAGING SIPE AI AND MENTAL HEALTH AUTUMN 2024 PP100022780 This magazine is FREE for industry professionals. Subscribe: www.hospitalhealth.com.au/subscribe TECHNOLOGY ISSUE CONTENTS A DAY IN THE LIFE 38 ...of Sarah Morse


Antibacterial Hand Gel. Proven to increase skin hydration by 14% in settings that mimic hospital sta use – sanitising hands 20+ times per day over a two week period 1 .
• TGA Registered (Aust R 410937)
• Enriched with 4 moisturisers
• Quick drying
• 70% w/w ethanol – absolute
Found to have no impact to skin pH even with frequent and extended use1
Scan to try for yourself






























1. Ego Pharmaceuticals commissioned external dermal tolerability study. Average increase in skin hydration (corneometer), average change in pH (skin pH meter). Participant assessments. n=33. For the information of healthcare professionals only
CONTENTS











HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 4 The missing ingredient in hypertension guidelines 52 illness diagnosis 40 Mindset training to improve patient outcomes 45 ...with Sue Matthews, CEO of Royal Women’s Hospital 56 IN CONVERSATION CLINICAL SERVICES DAILY NEWS hospital_health /hospitalhealth hospitalhealth.com.au STRAIGHT TO YOUR INBOX hospitalhealth.com.au/ subscribe STRAIGHT TO YOUR PHONE SCAN to see the latest Hospital and Healthcare news STRAIGHT TO YOUR DESK hospitalhealth.com.au/ magazine 8,56 Contributing Editor Amy Sarcevic 20 Technology Deepak Biswal Founder and CEO CareMonitor. 6 Editor’s Welcome Mansi Gandhi Common pets and injury hospitalisations 50 38 Nursing Sarah Morse Founder and Director Unchained Solutions Women’s health Sue Matthews Royal Women’s Hospital Published bimonthly, Hospital + Healthcare is an independent voice for the hospital, health and aged-care professionals containing regular features on major projects, healthcare disciplines, eHealth, government updates, news, conferences and events.



Art/Production: Marija Tutkovska
Circulation: Dianna Alberry, circulation@wfmedia.com.au Copy Control: Mitchie Mullins copy@wfmedia.com.au
Advertising Manager: Kerrie Robinson +61 400 886 311 krobinson@wfmedia.com.au
PUBLISHED BY Westwick-Farrow Media A.B.N. 22 152 305 336
Generative artificial intelligence (AI) could power economic opportunities in Australia, contributing $13bn a year to the country’s health sector by 2030. This is according to estimates in a 2023 report by the Tech Council of Australia and technology company Microsoft.

sparked controversy in medical and public arenas. While the technology has a place in the system, there have been concerns about challenges for people with complex trauma, a potential slot machine effect and the need for safe relationships to facilitate healing. Read the article for insights from leading mental health professionals.
www.wfmedia.com.au
Head Office
Unit 5, 6-8 Byfield Street, North Ryde Locked Bag 2226 North Ryde BC NSW 1670 AUSTRALIA ph: +61 2 9168 2500
If you have any queries regarding our privacy policy please email privacy@wfmedia.com.au
Subscriptions for unregistered readersprice on application
While the technology has immense potential to help improve health outcomes and contribute to the economy, the Commonwealth Scientific and Industrial Research Organisation (CSIRO) recently highlighted how the current regulatory framework likely does not sufficiently address known risks presented by AI systems, particularly in high-risk settings.
Australia will certainly benefit hugely from AI in health care, but it is crucial to ensure the design, development and deployment of these systems in legitimate, but high-risk, settings is safe and can be relied upon, warned the agency. This must be done while ensuring the use of AI in low-risk settings can continue to flourish largely unimpeded, the agency suggested.
This issue’s lead article explores whether chatbot psychologists become part of the health system — an issue that
On a different note, as the popularity of open water swimming grows, we look at a rare but life-threatening condition — swimming induced pulmonary oedema (SIPE) — and the need to improve awareness and preventative treatments.
There are also insights on the role of patient mindset training for care teams in improving experiences and health outcomes, designing a ‘quiet’ hospital, bridging the maternal care gap with technology, improving patients’ healing journey with design, hypertension guidelines and more.
Happy reading!
Mansi Gandhi Editor, H+H hh@wfmedia.com.au

HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 6 TECHNOLOGY ISSUE PATIENT MINDSET TRAINING CLOSING THE WOMEN’S HEALTH GAP IDENTIFYING AND MANAGING SIPE AI AND MENTAL HEALTH AUTUMN 2024
This magazine is FREE for industry professionals. Subscribe: www.hospitalhealth.com.au/subscribe
PP100022780
TO CONTRIBUTE?
welcome articles and research reports from health professionals across Australia for review for the quarterly print publication and our daily web page. If you have a story you think
be of interest, please send an email to hh@wfmedia.com.au PRINT / DIGITAL / MOBILE VISIT WWW.HOSPITALHEALTH.COM.AU CONNECT. SEARCH ‘HOSPITALHEALTH’ Printed and bound by Bluestar Print Print Post Approved PP100022780 ISSN 2204-3438 PRINT ISSN 2204-3446 DIGITAL NOTICE: All material published in this magazine is published in good faith and every care is taken to accurately relay information provided to us. Readers are advised by the publishers to ensure that all necessary safety devices and precautions are installed and safe working procedures adopted before the use of any equipment found or purchased through the information we provide. Further, all performance criteria was provided by the representative company concerned and any dispute should be referred to them. Information indicating that products are made in Australia or New Zealand is supplied by the source company. Westwick-Farrow Pty Ltd does not quantify the amount of local content or the accuracy of the statement made by the source. Editor: Mansi Gandhi hh@wfmedia.com.au Contributing Editor: Amy Sarcevic Acting Publishing Director/MD: Janice Williams
Director/Production Manager:
WANT
We
would
Art
Linda Klobusiak
Welcome to our Autumn issue
iStock.com/gremlin

Should chatbot psychologists health system?
become part of the

This year, an announcement that chatbot psychologists could become part of Australia’s healthcare system within the next two years sparked controversy in medical and public arenas.
The bots, which mimic conversation with users via a voice- or text-based interface, can be programmed with human-like qualities, and deliver structured mental health programs.
But is the interaction meaningful enough to generate therapeutic outcomes?
Dr Cathy Kezelman AM, CEO and Executive Director of Blue Knot Foundation, believes AI has a place in health care, but is concerned about its impact on people with complex trauma.
“Complex trauma results from harmful interpersonal interactions and, for this reason, requires safe human relationships to facilitate the healing process.
“Supporting people to feel heard, and regain any trust that has been lost from their primary
betrayal, is, in my view, only possible when a committed human being walks alongside them.
“My concern with machines is that they will miss out on a lot of the sensitivities that are important for the therapeutic alliance and minimising the risk of additional trauma.”
Too attached?
Digital mental health specialist
Dr Simon D’Alfonso from the University of Melbourne shares similar concerns, but warns the opposite scenario could pose more harm.
When the world’s first chatbot ‘ELIZA’ was introduced in 1966, even its creator, Joseph Weizenbaum, was surprised to see people attribute human-like feelings towards it.
Known as the ‘ELIZA effect’, researchers have since warned about the dangers of projecting empathy and semantic comprehension onto programs with a textual interface.
“The trouble with some of the less structured bots is that people can get
tangled in unconstrained conversations and be led into an emotional rabbit hole,” D’Alfonso said.
“They can go too far in attaching human characteristics onto a non-sentient system, and often the depth of their exchanges isn’t justified by what the chatbot is capable of.”
Another danger of getting too wrapped up with a bot is a sense of loss when its functionality changes.
“Sometimes, manufacturers can suddenly change the parameters of these platforms and the user ends up feeling devastated,” D’Alfonso said.
Lacking substance?
Even with more structured bot varieties, D’Alfonso is concerned about the potential for adverse consequences.
“We are seeing increased scope for bots to converse in an open-ended fashion, as natural language processing models develop. But,
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 8
TECHNOLOGY
Amy Sarcevic

it’s unlikely you’ll ever find something with the cognitive complexity, semantic sophistication and emotional richness to carry out anything like a substantive psychotherapy dialogue.
“A lot of psychotherapy is reliant on facial exchanges, interpersonal presence and non-verbal cues. Acoustic and paralinguistic qualities — like a person’s pitch and intonation — all convey important information and play a role in the therapeutic alliance.”
That said, the notion of a digital therapeutic alliance (DTA) has recently emerged as a research topic. Although different to the traditional therapeutic alliance, research suggests DTA is a genuine phenomenon, which can develop with mental health apps or chatbots under the right conditions.
Studies show that by offering self-guided therapy, these technologies can effectively treat anxiety and depression.
D’Alfonso said the best results are likely to come if bots encourage users to set goals and tasks and offer a personalised experience. This type
of structured intervention could even foster an emotional connection with the bot, he said.
“There are going to be instances where a human client wants to interact with a chatbot and might even develop a bond with them.
“Of course, it won’t be an authentic two-way bond, because the bots aren’t capable of that. But it might just be enough to deliver therapeutic results, when used in conjunction with a goal-based framework.”
The slot machine effect?
Kezelman agrees that chatbots could elicit feelings of connection, but draws a parallel with social media to highlight the risks.
“You only have to walk past a bus stop to see how attached people can get to their technologies. But we know that many of these attachments can also be harmful.”
Indeed, research shows that social media has addictive properties, meaning some continue to use it despite negative consequences.
One study revealed that time spent on social media was linked with depression and suicidality. Despite this, some remained hooked, given its dopaminergic effects.
D’Alfonso agrees and warns about the potential for a ‘slot machine effect’, where people keep using a bot to feed their curiosity about its next move.
An adjunct solution?
Despite the potential for harm, both experts agree that chatbots could play a useful role in a constrained healthcare system.
“It’s certainly an appealing option when there are challenges around availability and cost with traditional therapy — I’m just not sure it should be the patient’s primary relationship,” Kezelman said.
Meanwhile, D’Alfonso sees the bots as more of an interim solution.
“Someone could chat a bit with the bot and then go and see their therapist. I don’t see them as a comprehensive replacement.”
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 9
iStock.com/Vertigo3d TECHNOLOGY

Aged Care: Fact vs Fiction
There’s no doubt that making the move to an Aged Care Residence can be a difficult decision, especially if it happens suddenly, due to changes in your patient’s circumstances or a decline in their health.
Whether they’re looking at options for themselves or their loved ones, having a clear understanding of what to expect gives confidence in their decision and makes it much easier to find the right fit. But finding accurate and helpful information can prove challenging due to some common misconceptions.
Myth 1: ‘An Aged Care Residence is like a hospital’ It’s true Aged Care Residences deliver nursing care to their residents, but at TriCare, it’s important our residents also feel like it’s their home. We pay attention to avoiding a sterile hospital feel. We take pride in beautiful accommodation, which provides a comfortable, warm environment, so residents feel relaxed and at home.
Rooms are tastefully furnished including everything needed to enjoy their own private space, with Premium Rooms much larger featuring hotel-style decor and furnishings. All residents have access to shared spaces and activities, which adds a strong sense of community and connection allowing for friendships and fun.
Myth 2: ‘Living in Quality Aged Care is not affordable’
The amount you pay for Aged Care depends on your individual financial circumstances and type of accommodation and services you choose. In Australia, the system has been designed to make Aged Care accessible to everyone. There are four possible fees you may be required to pay:
1) Care (set by the Commonwealth Government) includes:
Basic Daily Fee covers basic living costs like meals, cleaning, laundry, heating and cooling. The Government sets at 85% of the single person rate of the Age Pension and everyone is required to pay this.
Means-Tested Fee — an additional contribution to cost of care based on income and asset assessment. The Department of Human Services will decide if additional Means-Tested Care Fees apply.
2) Accommodation (set by the provider):
This fee covers cost of accommodation, including room, bathroom facilities and communal areas.
The amount charged will depend on choice of accommodation and will be charged as a RAD (lump sum), DAP (daily charge) or a combination of the two.
3) Additional and/or extra services (set by Government and provider):
This fee covers costs of things like higher standard room features, entertainment, food services such as alcohol and additional menu options, subscriptions to TV etc.
The first step is to check eligibility online at myagecare.gov.au or call them 1800 200 422, or call TriCare 1300 874 2273.
Myth 3: ‘You will lose your freedom and independence’
One of the biggest benefits of moving to Aged Care is the level of care available 24/7. In delivering TriCare’s support services, we encourage our residents to remain as independent as possible by completing tasks and activities that suit their ability. Providing this level of independence promotes a sense of pride and wellbeing that is beneficial to positive mental health.
Residents who do not have specific care needs in place to ensure their safety have the freedom to choose how they spend their day, enjoying quiet time or mingling in the communal facilities and taking part in activities such as painting and bingo as they wish. Family and friends are also welcome.
When considering Aged Care options, debunking myths �irst is a must. That way, patients and families have accurate information and details they need to make an informed choice on the best option for them.
» For more information visit: www.tricare.com.au
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 10 SPONSORED CONTENT
Beautiful room view, TriCare Kawana Waters.


Open water
swimming: identifying and managing SIPE
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 12 TECHNOLOGY
Mansi Gandhi

Regarded as one of the world’s most iconic ocean swims, the 20 km Rottnest Channel Swim (RCS) from Cottesloe Beach to Rottnest Island off the coast of Western Australia attracts thousands of participants each year.
This year, for the first time in the history of the 34-year-old event, the RCS organisers were forced to cancel the event mid-swim due to dangerous and unsafe weather conditions.
SIPE — what do we know?
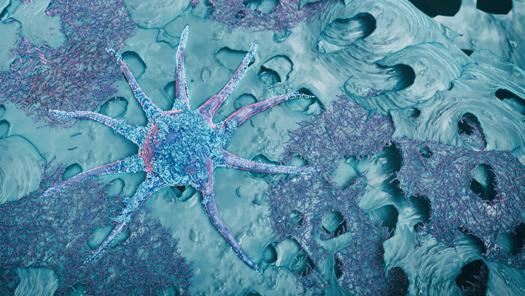
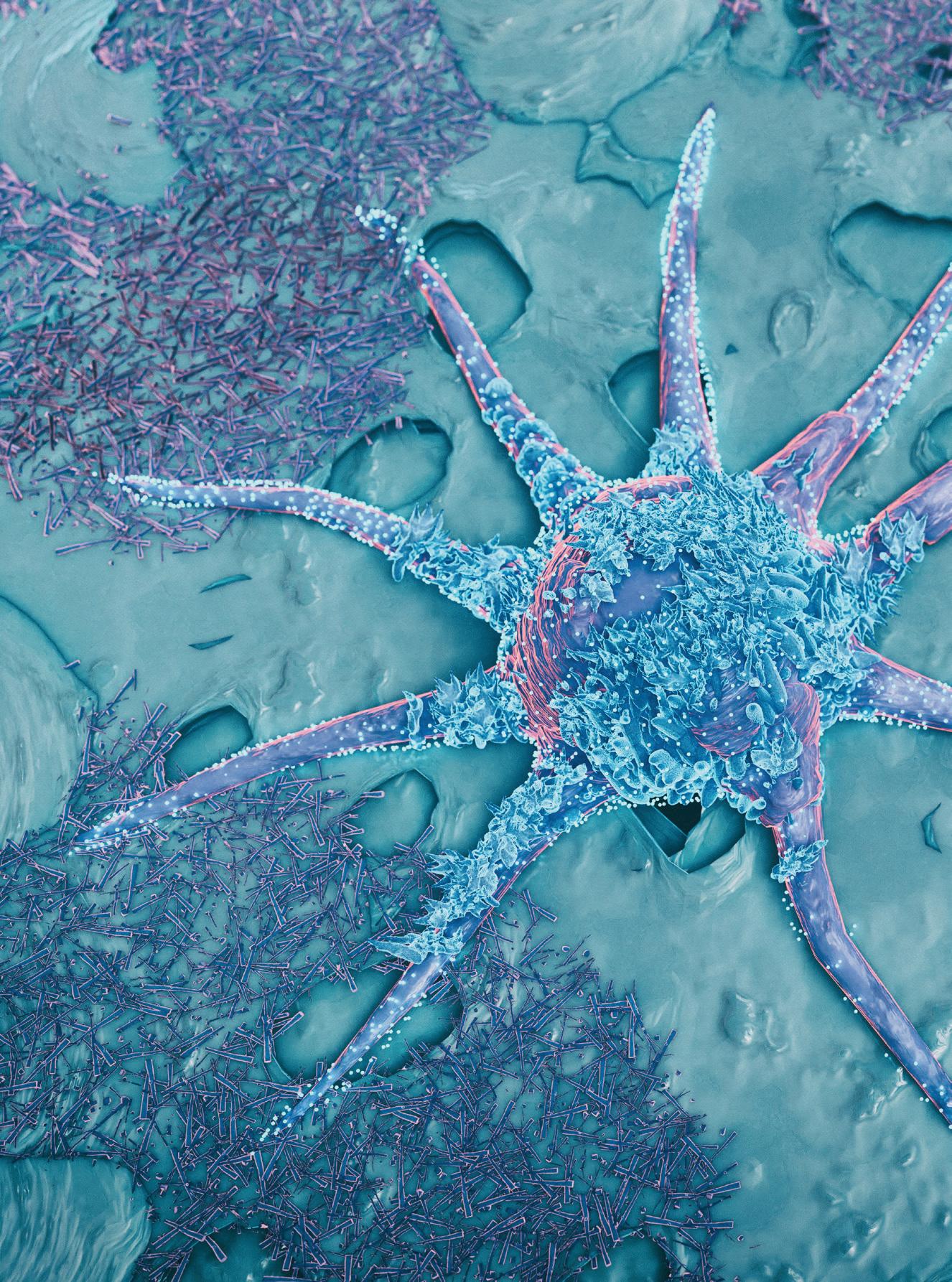
The race may have been called off, but research for a rare but life-threatening condition, swimming induced pulmonary oedema (SIPE), associated with open water swimming, did go ahead.
SIPE occurs when excess fluid accumulates in the lungs, causing acute shortness of breath during or immediately after swimming. It may include symptoms such as a whistling or crackling sound in the chest, an unexplained cough, coughing up phlegm or tightness in the chest.
It is a serious and potentially fatal condition, but there is not enough data on incidence rate and a lot remains unknown, particularly in terms of its pathophysiology, according to the researchers.
To get insights on the incidence rate of SIPE in public open water swimming, UWA researchers led by Associate Professor Louise Naylor, with support from Royal Perth Hospital, Fiona Stanley Hospitals and Curtin University, are conducting a study in both competitive and community-based marathon swimming events, specifically the RCS.
Identifying risk factors
The researchers are using the RCS cohort of 400+ athlete volunteers for their study for identifying risk factors. Dr Sebastian Knudsen, intensive care specialist at Royal Perth Hospital, was one of the solo participants at the event last year. Solo competitors typically spend between four (race leader) and 12 hours (last finishers) in water.
UWA senior researcher and PhD candidate Julie Collis, Naylor, Knudsen and team are hoping that their research will identify factors that can help people be screened and managed both in and out of the water.
In 2022, around 55% of surveyed swimmers who took part in the solo crossing for the swim reported at least one symptom of SIPE, and there have been individuals who have been hospitalised due to this condition at many crossings.
This study is being conducted in collaboration with Philips, with the company supplying a range of cardiac and lung ultrasound equipment (Philips Epiq CVx, Affiniti CVx ultrasound system, Compact 5500CV and Lumify systems) over the last two years.
Preventative treatments
Identifying risk factors for SIPE would allow the reduction in the risk of incidence occurrence via educating athletes
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 13 TECHNOLOGY iStock.com/inusuke


and support crew, potentially guiding preventative treatments in at-risk athletes, and allowing for more targeted research into the pathophysiology in the future, the researchers suggest.
Naylor and her team believe that a combination of water pressure on the body as well as exposure to cold and prolonged exercise forces blood from the extremities into the chest, thus increasing the pressure in the tiny capillaries in the lungs — this can lead to pulmonary oedema.
“With the increasing popularity of open water swimming, there is a growing need to better understand and raise awareness of SIPE and the associated risk factors for the condition.”
While the initial study target was to check for pre-clinical SIPE in 350–400 solo swimmers at the Rottnest Channel Swim, the numbers and study plans are being revised following the cancellation of the swim.
The RCS was suspended four hours after commencement, but the researchers were lucky to have a few participants who had almost hit Rottnest Island jump on a boat and reach the tent for testing.
“As part of the study, participants came in for pre-event testing, including an
echocardiogram at rest and under stress conditions. They were to be tested again immediately post-race when they arrived on Rottnest Island. Based on pilot work from last year, swimmers who had evidence of edema in the lungs (that is, preclinical or pre-symptomatic SIPE) were more likely to be female, had lower body fat and showed higher RV GLS (ie, 31 vs 29) compared to the group average after the marathon swim,” Naylor said.
The researchers will either be testing the same number of volunteer athletes at next year’s Rottnest Channel Swim or split this number amongst smaller events throughout the year. Collis said the study findings will help researchers determine any sport-specific cardiac adaptations to marathon swimming.
Need to raise awareness
With the increasing popularity of open water swimming, there is a growing need to better understand and raise awareness of SIPE and the associated risk factors for the condition, the researchers suggest.
Identifying risk factors for SIPE is a great first step, which would allow the reduction in the risk of a SIPE occurrence through athlete screening as well as potentially guiding preventative treatments in at-risk athletes, they said.
“Due to its somewhat insidious presentation and a lack of understanding around the condition, it is often overlooked until an athlete is extremely unwell. It is often only in retrospect that swimmers can say, ‘Oh, I was getting pain/shortness of breath/feeling unwell, but I just thought that was how I would feel after swimming 17km!’
“Added to this is the fact that many highlevel athletes will want to push themselves to the limit, and many more part-time athletes will be reluctant to stop given the huge sacrifices they have made to train for big events. Better knowledge of SIPE and its risk factors will help in making the big decision to pull a swimmer out of the water,” the researchers concluded.
The study authors have already been invited to attend and research other similar events and with the recent cancellation of RSC, they are investigating other options. “However, the logistics in trying to replicate an echo lab in the field on an island, with the correct scanning beds, participant privacy, machines etc are significant,” Collis said.
“For the baseline assessments, and last year post marathon I used the premium machines, The Epiq, as the 3D imaging provides a unique assessment of the cardiac mechanics and volumes. We had them barged over to the island ready for this year as well. We would need to review these logistics for smaller and subsequent events.”
SIPE may seem to be rare but UWA researchers suspect the cases are underreported with symptoms often easily ignored by participants. Their research hopes to change this, improving prognosis, prevention and outcomes.
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 14 TECHNOLOGY



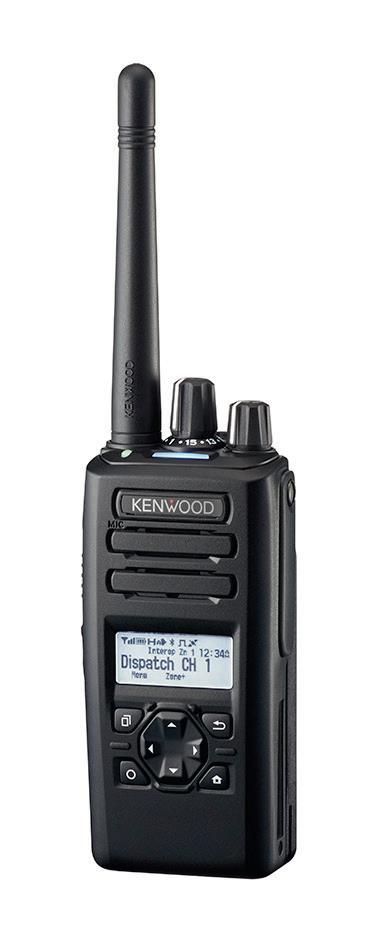

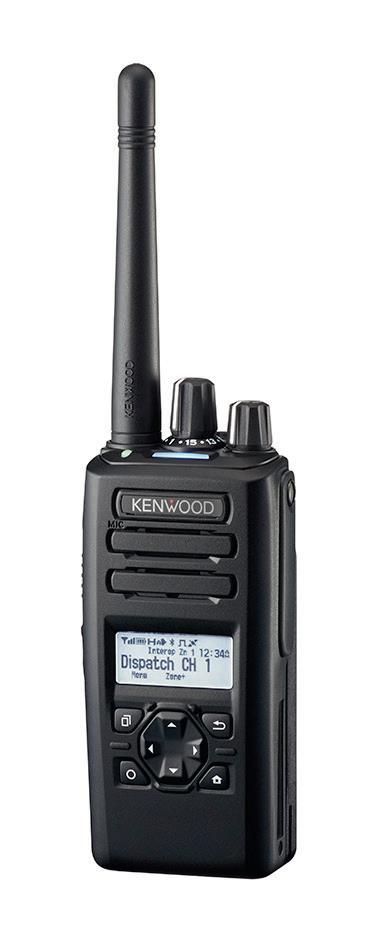
SUPPORTING PATIENT CARE, STAFF SAFETY, SECURITY AND EFFICIENCY
general enquiries, please contact our team via info@jvckenwood.com.au
For
www.au.jvckenwood.com
Long COVID may be no different to other post-viral syndromes, suggests latest research led by Queensland’s Chief Health Officer Dr John Gerrard.
People who tested positive for COVID-19 a year ago were no more likely to report moderate-to-severe functional limitations than people who had influenza, the research found.
Gerrard suggests it is time to stop using terms like “long COVID” as it wrongly implies there is something unique and exceptional about longer-term symptoms associated with the virus. “This terminology can cause unnecessary fear, and in some cases, hypervigilance to longer symptoms that can impede recovery,” Gerrard said.
The study by Queensland Health researchers suggests that in the highly vaccinated population of Queensland exposed to the Omicron variant[1], long COVID’s impact on
the health system is likely to stem from the sheer number of people infected with SARSCoV-2 within a short period of time, rather than the severity of long COVID symptoms or functional impairment.
Symptoms reported with the illness include fatigue, brain fog, cough, shortness of breath, change to smell and taste, dizziness and rapid or irregular heartbeat.
COVID-19 and influenza
The research, to be presented at this year’s European Congress of Clinical Microbiology and Infectious Diseases (ECCMID 2024) in Barcelona, Spain (27–30 April), adds to previous research by the same authors and published in BMJ Public Health which found no difference in ongoing symptoms and functional impairment when COVID-19 was compared with influenza,12 weeks post-infection[2]
To understand more about the impact of long COVID on the Australian state of
Queensland, researchers surveyed 5112 symptomatic individuals aged 18 years and older, comprising those with PCR-confirmed infection for COVID-19 (2399 adults) and those who were PCR negative for COVID-19 (2713 adults: 995 influenza positive and 1718 PCR negative for both but symptomatic with a respiratory illness) between 29 May and 25 June 2022.
Laboratory reporting for COVID-19 and influenza is mandated upon PCR test request under Queensland’s public health legislation, with the results recorded in the state’s Department of Health’s Notifiable Conditions System. A year after their PCR test, in May and June 2023, participants were asked about ongoing symptoms and the degree of functional impairment using a questionnaire delivered by SMS link.
Overall, 16% (834/5112) of all respondents reported ongoing symptoms a year later and 3.6% (184) reported moderate-to-
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 16 INFECTION CONTROL
“These findings underscore the importance of comparing post-COVID-19 outcomes with those following other respiratory infections, and of further research into postviral syndromes.”
severe functional impairment in their activities of daily life.
After controlling for influential factors including age, sex and First Nation status, the analysis found no evidence that COVID-19-positive adults were more likely to have moderate-tosevere functional limitations a year after their diagnosis than symptomatic adults who were negative for COVID-19 (3.0% vs 4.1%).
Moreover, results were similar when compared with the 995 symptomatic adults who had influenza (3.0% vs 3.4%).
Physiological data
Jeremy Nicholson, Professor of Medicine and Director of the Australian National Phenome Center at Murdoch University, said the research reports a year follow-up on 5112 symptomatic adult COVID-19 patients (omicron sub-variant of the SARS CoV-2) and 995 post-influenza patients from Queensland Australia. “The study indicates that 3–4% of people have significant
assertion that long COVID is the same as flu-related post viral syndrome is not proven, even if long COVID is indeed a post-viral syndrome (which it is),” Nicholson said.
Physician training programs
Marie-Claire Seeley from the Australian Dysautonomia and Arrhythmia Research Collaborative at the University of Adelaide and CEO of The Australian POTS Foundation said, “This abstract reveals a significant finding: approximately 4% of individuals, irrespective of the virus they contracted, may experience persistent health issues post-infection, resulting in chronic incapacitation. This implies that long COVID is not a standalone condition but rather part of a broader spectrum of post-viral syndromes.
“These findings align with previous Australian research published in the American Journal of Medicine in 2023. Adelaide researchers objectively demonstrated that 79% of long COVID patients met the criteria for postural orthostatic tachycardia syndrome (POTS), an autonomic nervous system disorder. Considering that POTS typically emerges following viral infection, this correlation is not unexpected. However, it’s concerning because POTS significantly impairs quality of life and functional capabilities, particularly affecting women during their childbearing years.
“Of further concern is the absence of specialised public autonomic physician training programs in Australia, unlike in the USA. This leaves us ill equipped to manage the increasing burden of post-COVID chronic autonomic disorders.”
iStock.com/mustafahacalaki
symptoms a year after either COVID-19 or influenza, hence the authors argue that they are effectively the same.”
“Unfortunately, this question cannot be simply answered in this work. The study is observational, based on reported symptoms with no physiological or detailed functional follow-up data. Without laboratory pathophysiological assessment of individual patients, it is impossible to say that this is indistinguishable from flu-related or any other post-viral syndrome,” Nicholson said.
“Also, there are many long-term effects of COVID-19 that do not have significant early-stage symptoms eg, heart disease, atherosclerosis and diabetes. These conditions do, however, have associated metabolic signatures which were not measured in the current study.
“The absence of evidence is different from evidence of absence, so the authors’
Further research needed
Interestingly, the Queensland Health analysis also found that those who were more likely to report moderate-to-severe functional impairment were those aged 50 years or older, and those who had symptoms of dizziness, muscle pain, shortness of breath, post-exertional malaise and fatigue.
“These findings underscore the importance of comparing post-COVID-19 outcomes with those following other respiratory infections, and of further research into post-viral syndromes,” Gerrard said.
The authors caution that the findings are associations and do not represent prevalence. They point to several limitations, including that participants who were hospitalised or had pre-existing illness were not identifiable within the cohort. They also note that the risk of long COVID has been lower during the Omicron wave compared with other SARSCoV-2 variants, and because 90% of people in Queensland were vaccinated when Omicron emerged, the lower severity of long COVID could be due to vaccination and/or the variant.
1. More than 90% of the population of Queensland had been vaccinated against COVID-19 before the community first experienced transmission of the Omicron variant in 2022.
2. Ongoing symptoms and functional impairment 12 weeks after testing positive for SARS-CoV-2 or influenza in Australia: an observational cohort study (bmj.com)
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 17 INFECTION CONTROL
How a Pharmaceutical Giant Ensures the Safety and Authenticity of Medicines Through Serialisation

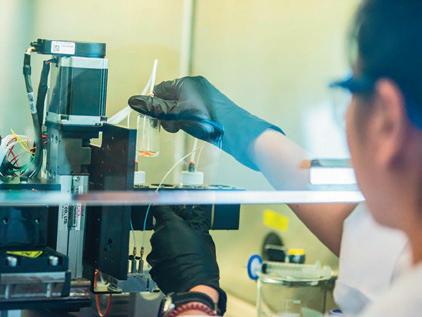
In an era where pharmaceutical traceability is paramount, Aspen Australia, a subsidiary of Aspen Pharmacare Holdings Limited, has emerged as a trailblazer in implementing robust global standards to combat the threat of falsified medicines. The company’s proactive approach to adhering to regulatory requirements and adopting GS1 standards has not only safeguarded its market presence but has also set a benchmark for the industry.
The Challenge
The pharmaceutical landscape is constantly evolving, with stringent regulations aimed at preventing the circulation of counterfeit drugs. As a Contract Manufacturing Organisation (CMO), Aspen Australia faced a significant challenge when awarded a contract manufacturing portfolio for new Middle Eastern markets. These markets demanded compliance with serialisation requirements, emphasising the GS1 DataMatrix barcode.
The Solution
Aspen embarked on a meticulous journey to implement a serialisation system, choosing a Point of Dispense Authentication (PoDA) model. This model focuses on serialisation at the sales unit level, ensuring traceability at the
point of dispensing. The selection criteria for the implementation encompassed flexibility, scalability, ease of use, ubiquity, innovation, technical implementation, customer service, and cost considerations.
How the System Works

The Results
The Serialisation system’s workflow involves the automatic replenishment of productspecific serial number pools, the creation of serialised orders that reserve the required quantity of serial numbers and then download when assigned to a packing line. The GS1 DataMatrix barcode encoding the unique product identifier, expiry, batch/lot and serial number is printed, verified, and linked to production data at the line level. The serial numbers are then transferred by the Market Authorisation Holder (MAH) to the regulatory body’s database, ensuring authenticity can be verified at the point of sale.
The Challenges
The implementation journey was not without its challenges taking approximately two years, including an extensive validation process is a critical aspect. Aspen emphasises the need for adequate resourcing, stakeholder management, detailed process documentation, and sufficient time for training to ensure success.
Since the commercial launch in July 2020, Aspen’s serialisation system has enabled the supply of compliant products to several export markets. The use of GS1 DataMatrix and EPCIS standards ensures global traceability and addresses the issue of falsified medicines on a worldwide scale.
Conclusion
Aspen Australia’s success story exemplifies the importance of embracing global standards in the pharmaceutical industry. The adoption of GS1 standards has not only facilitated compliance with regulatory requirements but has also strengthened Aspen’s position as a trusted player in the global pharmaceutical market. The lessons learned from this implementation provide valuable insights for other companies navigating the complex landscape of pharmaceutical regulations and traceability. Learn more about the fight against falsified medicines while enhancing traceability across the supply chain: https://bit.ly/3PjrSyJ

HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 18 » For more information visit GS1 Australia www.gs1au.org SPONSORED CONTENT
© iStockphoto.com/PeopleImages

Bridging the maternal care gap with technology
Deepak Biswal*
In Australia, there has been a trend towards shorter postnatal stays between 2011 and 2021, with 27% of mothers discharged less than two days after giving birth in 2021 (17% in 2011) and 11% of mothers staying five or more days (18% in 2011). This is according to data from the Australian Institute of Health and Welfare (AIHW).
The World Health Organization (2022) recommends that after an uncomplicated vaginal birth in a health facility, healthy mothers and newborns should receive care in the facility for at least 24 hours after birth. Postnatal care in hospital allows health professionals to monitor the mother and baby after birth and provide mothers and their partners and/or family with advice and support around physical recovery, breastfeeding, parenting skills and linking to supports in the community (Rayner et al. 2008; World Health Organization 2022).
Quality of care
The average number of days women spend in hospital following childbirth has steadily declined from 3.0 days in 2011 to 2.5 days in 2021. Often some mothers are ready to leave a maternity ward in favour of the comforts of home, but others, especially those giving birth for the first time, report feeling confused, battered and out of their depth when asked to leave so soon after their baby’s arrival.
The decline in the number of working midwives is a contributing factor, with advocates blaming workload pressures and exposure to birth trauma, resulting in 25,557 practitioners working in midwifery in 2022 — a 4.8% decrease on 2016 figures.
This shortage is affecting the quality of care and potentially other outcomes, according to NSW Nurses and Midwives Association counsellor, lactation specialist and registered midwife Emma Gedge, who warned that specialist medical staff are increasingly lending their expertise to plug the midwifery gap, leaving them unable to properly respond to specialist care needs.
Based on data released by NSW Health, Gedge could be right. The ‘Mother and Babies 2021’ report found that the number of babies fully breastfed after they and their mothers are released from the hospital has declined for five years in a row in NSW, dropping from 78.5% in 2017 to 73.1% in 20212
Many hospitals are struggling to cope with the high demand and low midwife availability. Experts warn that early cost-containment and understaffing could lead to missed opportunities for education and support — opportunities that could mitigate the risk of a raft of complexities and challenges for mother and baby in the longer term if seized while mum and baby are under the care and supervision of healthcare professionals.
Midwives play a vital role in empowering women to recognise and evaluate their own risks, enabling informed decisionmaking throughout the perinatal journey. Results from focus groups with midwives and mothers revealed that nurturing connections, offering flexibility and ensuring care continuity are key elements of highquality midwifery-led care3. This approach gives women a genuine sense of choice and control over their maternity experience.

Technology to alleviate strain
Health care delivered via digitally enabled software and devices can alleviate some of the strain maternity wards are facing and the distress mothers are experiencing from the antenatal period right through the time that they are navigating the early stages of home life with their new addition.
Assiamira Ferrara, PhD, a Senior Research Scientist at Kaiser Permanente, a healthcare provider in Northern California, conducted a study on the impact of virtual visits on maternal healthcare outcomes during the pandemic. The study, published in JAMA Network Open4, revealed that telemedicine visits increased from comprising 11% to 21% of pregnancy appointments.
Surprisingly, despite no increase in overall appointments, health outcomes remained unaffected. A mixed-mode approach combining in-person and virtual visits yielded
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 20 TECHNOLOGY

comparable rates of preeclampsia, eclampsia, severe maternal morbidity, C-section delivery and preterm birth when compared to an inperson-only approach.
This approach could potentially overcome barriers for individuals with limited time due to inflexible work schedules, lack of transportation or childcare responsibilities.
Digitally enabled care
Local hospitals are introducing Hospital in the Home (HITH) programs for their maternity patients as an inpatient substitution service. Patients remain under the care of a treating hospital team, receiving the same treatment and considerations as they would in the hospital. Using a blend of capabilities like digital assessments, remote patient monitoring using Bluetooth-enabled home health monitoring devices and telehealth, for
example, clinicians and care teams can provide hospital-standard clinical care to the patient in their home.
A significant majority of Australian consumers, around 80%, are familiar with virtual care or have used it. Furthermore, 90% of those who have experienced virtual care express a level of satisfaction ranging from “somewhat” to “very”. In particular, convenience (72%), avoidance of in-person care settings (57%) and flexibility (50%) are frequently cited as the most notable advantages. This highlights a continued preference for easily accessible care options that eliminate the inconvenience of hospital visits or stays 5
While there is no silver bullet for the healthcare staffing crisis, digitally enabled maternal health care has the potential to bridge the gap between low midwife availability and high patient demand.
By facilitating real-time patient monitoring and continuous provider communication, timely intervention can be coordinated, easing the strain on the system and supporting new mums at a time when women experience uncertainty, anxiety and feelings of loneliness and social isolation in coping with the demands of caring for a newborn.
1. Mothers and Babies 2021 - HealthStats NSW
2. Exploring the qualities of midwifery-led continuity of care in Australia (MiLCCA) using the quality maternal and newborn care framework - ScienceDirect
3. Prenatal Health Care Outcomes Before and During the COVID-19 Pandemic Among Pregnant Individuals and Their Newborns in an Integrated US Health System
4. ‘It’s going to get worse’: Providers tap into health tech tools to prevent maternal health emergencies.
5. Virtual hospitals could cure many healthcare ills | McKinsey *Deepak Biswal is a founder and CEO of CareMonitor. His passion lies in using digital technology to create solutions that can help ease the burden of our healthcare system
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 21 TECHNOLOGY
iStockphoto.com/shironosov
IUnlocking Sustainable Growth for Disability Service Providers


n the ever-evolving landscape of delivering NDIS services, the importance of selecting the right partner cannot be overstated. Navigating a partner in the disability sector that will provide trustworthy advice, direction on managing industry compliance or enabling businesses to deliver high-quality care has proven to be a key challenge faced by many disability providers.
For too long business leaders have focussed on software as features and functionality, rather than understanding the overall value in the investment of a strategic partnership.
A tech partner is one that propels an organisation toward sustainable growth. Lumary understands this crucial distinction and is enabling NDIS service providers with a blend of cutting-edge technology, unwavering service and support, and a commitment to trust and security.
Trust and Security in Your Tech Partner
Over 200 healthcare providers are already benefiting from Lumary’s transformative end-to-end care management software and tech partnership. Lumary recognises the challenges faced by disability service providers in navigating the complexities of technology adoption for their workforce while ensuring data security and regulatory compliance. Their approach goes beyond offering a software tool as they strive to be a leading trusted tech partner, guiding organisations through every stage of their growth journey.
Lumary’s co-founder and CEO, Joseph Mercorella, states, “Empowering disability service providers to scale their businesses is at the heart of our mission. Our strategic tech partnership is designed to not only meet the immediate needs of our clients but also to fuel their long-term growth aspirations. We truly want to empower our customers to improve their operational e�iciency which elevates the wellbeing of their workforce and translates into improved personalised care for the participant.”
Ensuring Data Security
One of the primary concerns for any organisation entrusting its operations to a tech partner is data security. With Lumary’s certi�ication of ISO 27001 international standard for its NDIS care management software, organisations can rest assured that their sensitive information is safeguarded against potential threats. Lumary’s team of industry experts and tech engineers remain vigilant, staying abreast of the latest advancements and implementing robust security measures to strengthen digital infrastructure.
Streamlining Compliance with NDIA Integration
Furthermore, the NDIS landscape continues to evolve. With the introduction of PACE, the complex administration of the NDIS continues, and requirements for staying compliant with regulatory changes are becoming more prevalent. Navigating these changes is a significant administrative burden for any disability organisation. With Lumary’s care management platform and direct
integration with the NDIA’s provider portal organisations can streamline operations by automating the complexities of rate updates and claim processing.
And not to mention, peace-of-mind in managing NDIA compliance requirements. This proactive approach helps to shield organisations from potential pitfalls and reduce the administrative load, allowing them to focus on delivering exceptional care to their clients.
Driving Efficiency and Profitability
In the pursuit of efficiency and profitability, providers are often faced with a crucial decision: whether to customise technology to suit business needs or adapt one’s business to fit technology. A successful tech partnership goes beyond ‘plug-and-play’ software adoption. In some cases this may seem cost effective initially, however, providers increasingly find themselves quickly either outgrowing tech tools or troubled by data disparity in non-integrated tech stacks.
When disability providers look to embark on new business software solutions, their key success starts by refining their business processes to align with the supporting technology. Disability providers approaching digital transformation this way have high system adoption, increase scalability and achieve sustainable outcomes quicker and easier. Lumary’s enterprise care management platform has been developed in collaboration with leading disability providers and industry experts since the inception of
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 22 XXXXXXXXXXX 1 SPONSORED CONTENT


the NDIS, ensuring a best practice software solution that focuses on compliance and optimising workforce operations.
Custom software development, while offering a bespoke solution, requires substantial upfront investment and extended timelines. In contrast, Lumary’s purpose-built solution has evolved over time addressing specific sector needs and supporting disability providers to accelerate digital transformation with minimal disruption. In an already intricate industry, the choice of managing a custom-built software solution can significantly burden disability providers. It requires them to navigate sector changes and constantly adapt their custom technology to align with shifting NDIS requirements and regulations. This option can often incur draining effects on financial and workforce resources in the pursuit of maintaining compliance.
Working with a trusted tech partner and adopting their purpose-built software solutions ensures that financial and human resources remain focused on core healthcare delivery. With a long-term tech partnership, providers can confidently balance the ever-evolving landscape of disability care management, assured that their technology has proven the test of time by regularly adapting and updating to meet industry demands. This decision can drive longterm success and resilience, laying a solid foundation for growth and sustainability. By embracing technology like Lumary’s, organisations establish a pathway to efficiency, profitability, and service excellence.
Success Story: Concentric’s Transformation
Let’s delve into the success story of Concentric, a thriving multidisciplinary allied health practice and NDIS provider with over 34 locations across Australia. Concentric is one customer who has exemplified the transformative power of a long-term investment in Lumary as a trusted healthtech partner. Concentric is growing rapidly and after successfully implementing Lumary’s CM platform, they chose to adopt Lumary’s NDIA integration module in June 2023. Concentric CIO, Simon Baird says “Lumary’s technology has had a transformative impact on our organisational e�iciency and is setting us up for future expansion of services. The integration of Lumary’s NDIA Module has not only optimised our operational framework but has also notably improved our NDIA claims processing procedures.”
Lumary’s NDIA Integration Module enables data synchronisation between the NDIA (Proda & PACE) and Lumary’s software making for a much smoother pathway when claiming funds from the NDIA.
After approximately 6 months of implementing Lumary’s NDIA Integration Module, Concentric reported a 60% reduction in NDIA claim errors. This not only translates to a substantial financial improvement but
also signifies a significant decrease in the stress associated with hidden costs and the exhaustive efforts required to address unsuccessful and contested claims.
Reducing NDIA Claim Errors: A Financial Game-Changer
If you’ve ever dealt with NDIA claims, you know the frustration of encountering claim errors. These errors come at a high cost to organisations, and the more frequently they occur, the more the cost compounds. “This is a common issue and we’ve seen many businesses report error rates anywhere from 2% to 17% with NDIA claims.
This adds significant financial strain on any organisation,” says Lumary’s VP of Strategic Growth, Jason Collins.
“As an example, an organisation claiming $2 million per annum from the NDIA might find themselves investing valuable resources chasing after $340,000 per year. Despite the dedicated efforts of finance teams, numerous failed claims often result in hours of exhaustive investigations, follow-ups, and reclaim attempts. The hidden costs associated with these recovery efforts can be both crippling and immensely frustrating,” continues Collins.
With Lumary’s purpose-built NDIS software, providers can experience peace of mind knowing that their trusted tech solution is streamlining claim procedures, minimising errors, and seamlessly integrating while ensuring compliance with the NDIA. This allows organisations like Concentric to prioritise delivering exceptional services while continuing to scale their business.
Tech Partnership: Strategic Investment for Success
Indeed, the journey toward sustainable growth requires more than just technological know-how. It requires a partner who shares your vision, understands your challenges, and stands ready to support your aspirations.
Choosing a tech partner like Lumary means choosing to invest in your future. It means choosing to streamline your operations, enhance the quality of your services, and forge a path towards sustainable growth. With the right tech partner by your side, you gain more than just a mere software tool; you gain a strategic advantage that propels your organisation toward greater efficiency, profitability, and client satisfaction.
Seize the opportunity to elevate your organisation to new heights. Embrace the power of a Lumary partnership and embark on a journey toward sustainable growth and unparalleled success. Book a healthcare consultation with their team today and experience the difference firsthand. Together, create better wellbeing in people’s lives—one transformative partnership at a time.

HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 23 2 » For more information visit Lumary www.lumary.com


Designing a
‘quiet hospital’
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 24
Anew $145 million Northern Private Hospital has opened in Victoria, featuring the latest digital devices for patient safety and quality, and a new communication system, claiming to be the state’s first ‘quiet hospital’.
Northern Private Hospital CEO Shaune Gillespie said the technology meant less disruption for patients and faster communication between staff. Colocated with Northern Hospital Epping, the facilities are joined by a link bridge to allow the easy transfer of patients between sites.
“Gone are the days when patients, and even staff, had to buzz a noisy call bell for assistance and hope it gets heard. Now, the message goes directly to exactly who needs to hear it,” Gillespie said.
“Our smart comms devices link a patient’s call button, monitors and other safety equipment directly to the nurses looking after them.

They also allow our nurses to immediately, and silently, call for additional assistance.
“Northern Private will also accept referrals direct from GPs, helping to take pressure off local emergency departments and reduce wait times for patients,” he said.
The hospital is operated by Ramsay Health Care. Ramsay facilities provide a range of health care services, including primary care, complex surgeries as well mental health care and rehabilitation. The company employs over 86,000 people and treats 8.5 million patients in its hospitals and primary care clinics located in Australia, France, the United Kingdom, Sweden, Norway, Denmark, Germany, Italy, Malaysia, Indonesia and Hong Kong.

“Ramsay saw the need for better access to quality private healthcare services in the fastgrowing suburbs north of Melbourne,” Ramsay Health Care CEO Carmel Monaghan said.
Northern Private Hospital, located within the Riverlee New Epping estate, 22km from Melbourne’s CBD, features 70 patient beds, four operating theatres, a cardiac catheterisation lab, a sleep study unit, a day chemotherapy unit, an on-site pharmacy, pathology and medical imaging.
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 25 DESIGN IN HEALTH
The wide range of specialties available include general medicine, cancer care, cardiac care, ENT, orthopaedics, IVF and fertility, vascular care, urology, nephrology, gastroenterology, general surgery, thoracic surgery, respiratory and sleep services, and plastic and reconstructive surgery. The hospital will continue to evolve in the future to grow and meet the heath care requirements of the expanding community.
Northern Private Hospital was designed to support Ramsay’s commitment to sustainability and has a 4 Star Green Star Rating. The building was built using cooling beams and features solar panels, LED efficient lighting and double-glazed windows and equipment to help with water conservation.


HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 26 DESIGN IN HEALTH
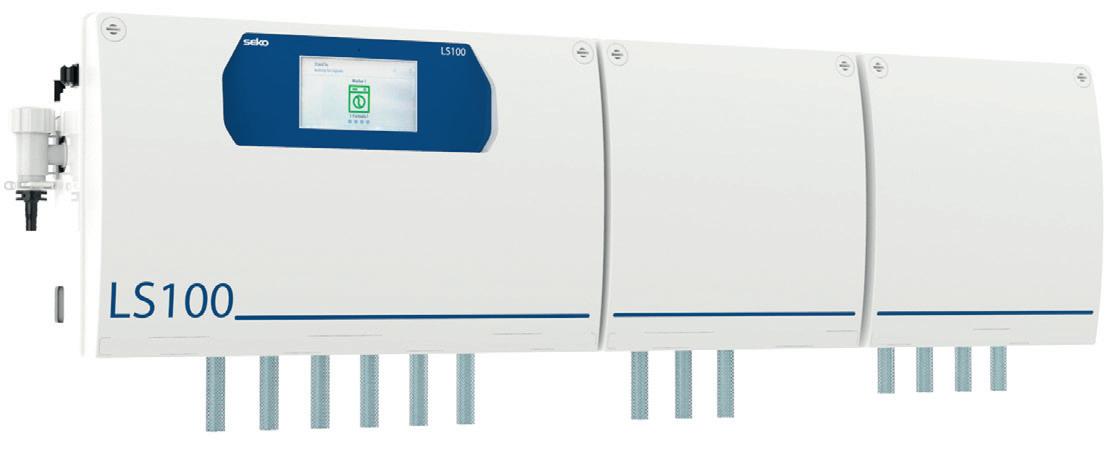
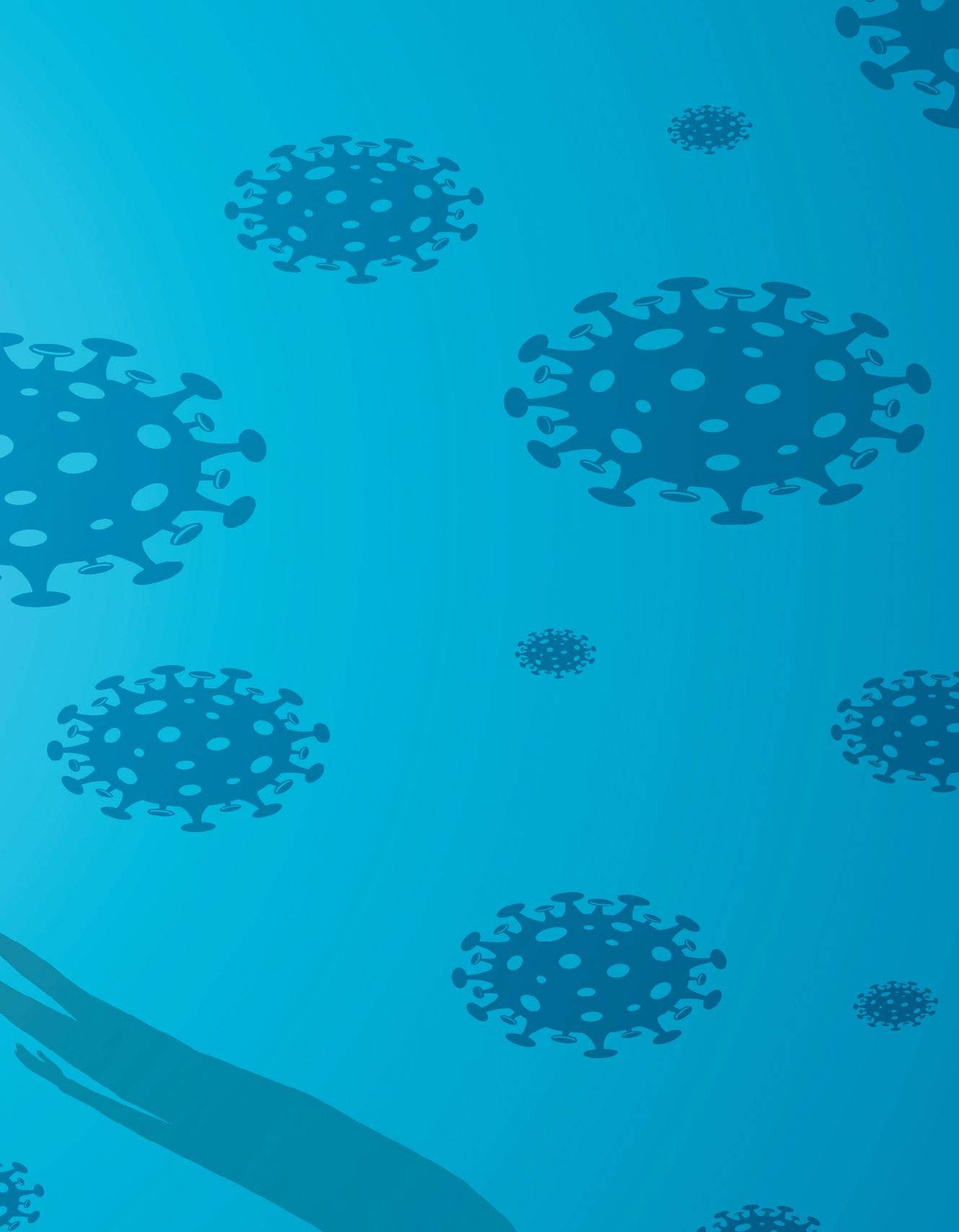
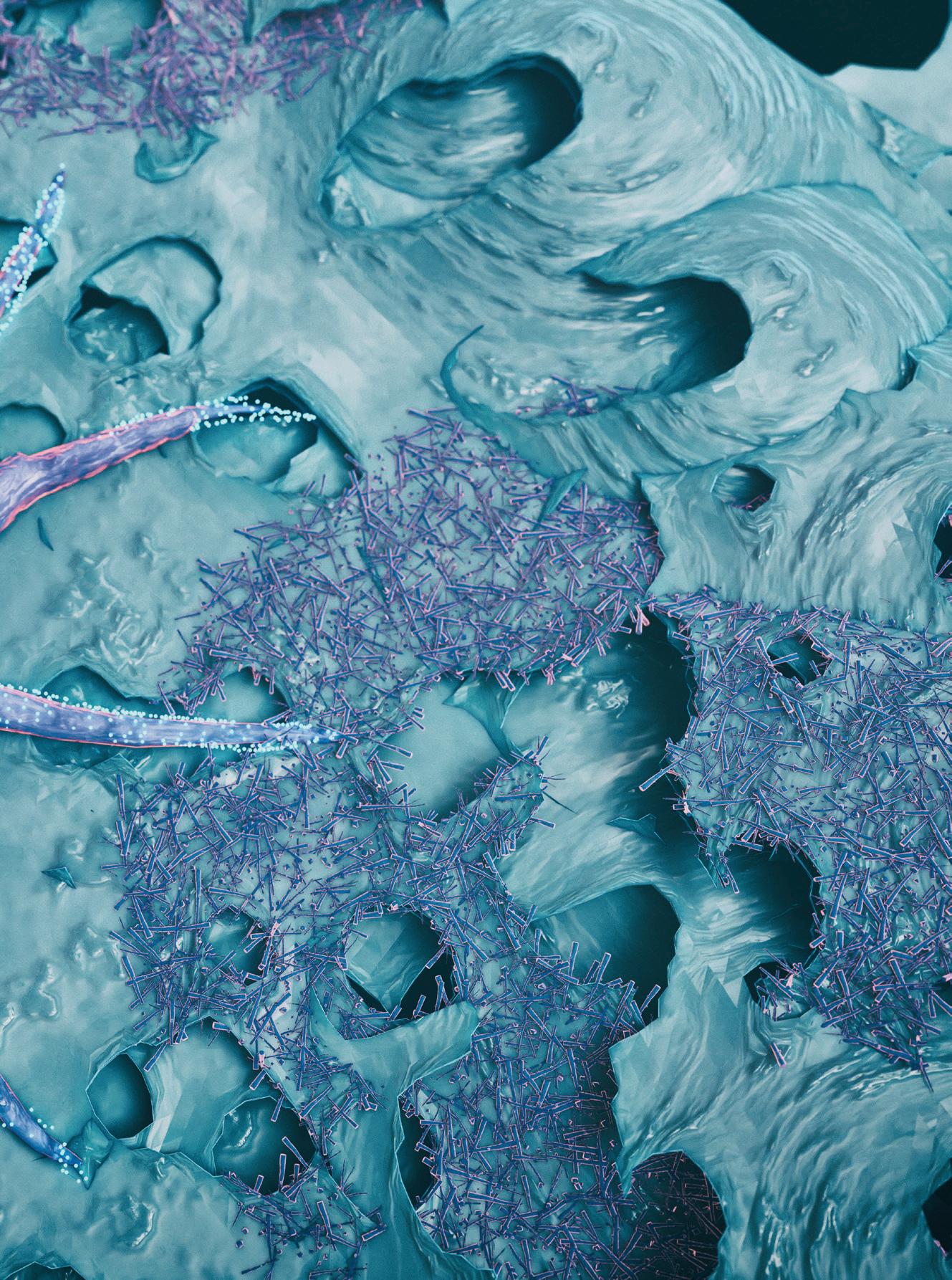
Keeping the healthcare sector clean
From hospital wards to dental surgeries, there’s nothing quite like the healthcare sector to challenge every aspect of cleaning and hygiene, with the protection of patients, visitors and staff vying for attention against budget limitations.
Therefore, it’s essential that on-site cleaning and hygiene equipment is capable of achieving and maintaining the highest standards in even the most demanding environments.
This begins with surface cleaning, where chemical dispensers used for dosing concentrated and pre-mixed solutions into sinks, spray bottles, mop buckets and scrubber dryers must combine precision and consistency with robustness and longevity.
In fast-paced environments such as operating theatres where excessive force and accidental collisions are common, a tough, impact-resistant dispenser casing helps to ensure consistent, reliable performance while reducing the cost of maintenance, repair and replacement.
When budget is tight it may be tempting to opt for lightweight dispensers but, while such systems are cheaper per unit, they are also unreliable and have a short lifespan, costing more in replacements in the long run compared with higher-quality, longer-lasting equipment.
In many cleaning stations it’s common to see concentrated chemical containers such as 20-litre drums stored unbunded on the floor, causing a potential leakage or trip hazard. Or, worse still, staff dosing detergent and other solutions manually, exposing them to potentially harmful concentrated chemical.
Integrated chemical storage can help solve this issue, enabling operators not only to save

space and make cleaning stations tidier and more presentable, but also providing vital health and safety benefits by keeping the chemicals off the floor and avoiding possible spillage and trip hazards.
Such systems typically feature a cabinetstyle enclosure where various-sized chemical containers can be stored and connected to the built-in dispenser. Lockable cabinets help to prevent theft and tampering and protect employees against exposure to harsh concentrated chemical.
Managers in the healthcare sector may also be responsible for their site’s on-premise laundry which, if not properly overseen, can be a source of excessive consumption and wastage of chemicals, water and energy.
To avoid this, and to ensure that bed linen, blankets, towels and uniforms are washed to the same high standard every time, it’s advisable to install trusted automatic chemical dosing systems that achieve accurate, consistent chemical dosing over the long term.
The same is true of on-site warewash machines handling high volumes of crockery, cutlery and glassware and in both cases the best systems are built with premium-grade components that offer superior chemical compatibility.
This means parts are more resistant to degradation from harsh concentrated detergents, helping to deliver repeatable results and extensive equipment lifespan while reducing maintenance requirement.
The integration of Internet of Things (IoT)enabled technology in some chemical dosing equipment is allowing managers and technicians to monitor detergent consumption statistics and system status at their

convenience via smart device, PC or laptop, with the only barrier being a Wi-Fi connection. As well as allowing operators to gain a clear understanding of their application’s cost, this cutting-edge connectivity also helps them to identify areas where chemical is being wasted and adjust programming accordingly.
Plus, technicians may be alerted to anomalies immediately, allowing them to schedule maintenance and avoid costly unplanned downtime as part of an efficient, well-run operation.
When it comes to maintaining exceptional standards in healthcare, it’s clear that a little investment can go a long way. Cleaning and hygiene expert SEKO knows this better than most as the company has been helping operators for decades with a dedicated range of chemical dilution, dispensing and dosing equipment.
These include the modular ProMax dilution system, which allows users to dispense premixed chemical solutions into spray bottles, mop buckets and scrubber-dryers, along with an IoT-enabled warewash and laundry dosing range that gives operators 24/7 access to wash data via the dedicated SekoWeb app and online platform.
Visit www.seko.com to explore the complete range.
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 27 SPONSORED CONTENT
» For more information visit www.seko.com
parasitic diseases

Eliminating in remote communities
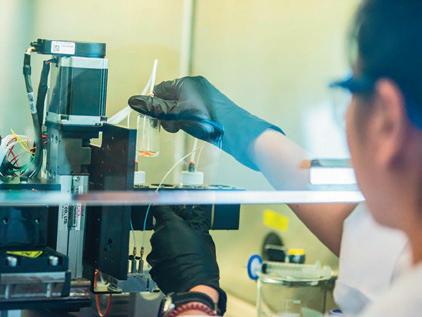
AQIMR Berghofer-led project aims to eliminate strongyloidiasis, a little-known and potentially fatal infection that thrives in communities with poor sanitation.
The multidisciplinary project team was recently awarded a $5 million Synergy Grant from the National Health and Medical Research Council (NHMRC).
Professor Darren Gray, project lead and Director of QIMR Berghofer’s Population Health Program, said an effort to control the parasitic worm Strongyloides stercoralis and eliminate its deadly diseases is long overdue and will have a profound impact on the health of Indigenous Australians.
“Strongyloidiasis is the most neglected of the neglected diseases. Despite being preventable and treatable, there is currently no global or national control strategy to manage its identification, prevention and management,” Gray said.
Australian First Nations communities have one of the highest rates of strongyloidiasis in the world, said Flinders University environmental health expert Professor Kirstin Ross in a new Royal Society article.
“This disease is transmitted when plumbing or other environmental health hardware components are failing,” said Ross, who is also part of the NHMRC project.
With an estimated prevalence of up to 60%, Aboriginal communities in northern Australia appear to have one of the highest
rates of strongyloidiasis in the world, according to Gray.
“Our project has the potential to eliminate this potentially fatal infection, which has a devastating effect on some of our country’s most vulnerable people,” Gray said.
Strongyloidiasis symptoms are highly variable but the infection can lead to life-threatening diseases including sepsis and pneumonia. It is caused by roundworms which enter the body through the skin and invade the lungs and gut.
Infestations are linked to faecal contamination and dogs may also play a role in the parasite’s life cycle. Addressing poor sanitation and hygiene, a lack of clean water and limited access to health care and health education are crucial to controlling the parasite.
Dr Catherine Gordon, a member of the QIMR Berghofer team and molecular parasitologist, said strongyloidiasis is notoriously difficult to detect.
“If you don’t look for this disease, you won’t find it. To date, there has been a lack of screening, testing and education.
“Our project will develop and validate new diagnostics including inexpensive and rapid diagnostic tests which can be conducted and assessed in the field,” Gordon said.
With the support of the NHMRC Synergy Grant, QIMR Berghofer’s cross-functional team will seek to determine the true burden
of the disease in East Arnhem Land and what role animals play in transmission.
The team will pilot an elimination program at two sites, combining treatment, improved sanitation and hygiene, community engagement, education, veterinary management and surveillance.
Gray said in addition to eliminating strongyloidiasis, this program is expected to reduce the impact of other common and preventable infections of poverty including scabies and group A streptococcus, ultimately reducing the burden of rheumatic heart disease.
The project is expected to have far-reaching consequences in the treatment and elimination of a number of serious diseases of poverty in Australia, South-East Asia and beyond.
“This research is a game changer for the control of infectious diseases of poverty globally and could ultimately contribute to the breaking of the poverty cycle by improving health and wellbeing and increasing educational attainment and economic output,” Gray said.
This research program brings together a multidisciplinary team of researchers, practitioners, policymakers and community, including partnerships with Strongyloides Australia, Miwatj Health Aboriginal Service, Animal Management in Rural and Remote Indigenous Communities, East Arnhem Regional Council, NT Health, NT Power and Water and NSW Health Pathology.
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 28 INFECTION CONTROL
iStock.com/simonbradfield

HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 30 DESIGN IN HEALTH
Artwork by First Nations artist Karen Lee Mungarrja, a Wiradjuri artist of the Tubba-Gah clan, Dubbo, NSW.
patient journey Improving the

Residents of Melbourne’s northern suburbs will have further access to health care and treatment, following the reopening of La Trobe Private Hospital. The hospital, located at La Trobe’s Bundoora campus, now comprises 34 beds, including four operating theatres and a four-bed high dependency unit. Clinical services offered at La Trobe Private include orthopaedics, general surgery, plastic surgery and urology, as well as a new radiology clinic and consulting suites.
Healthscope invested more than $25 million in the redevelopment to expand and enhance its longstanding partnership with La Trobe University, providing additional clinical education placements for La Trobe students as well as opportunities to receive professional learning experiences. Plans for the reopening of La Trobe Private Hospital were finalised in June 2021.
La Trobe University Vice Chancellor
Professor Theo Farrell said the hospital will bring a range of health and education benefits to the local community while continuing to strengthen the university’s teaching, learning and research capabilities. “La Trobe Private Hospital is driving healthcare innovation, as a place where world-class health care is combined with hands-on professional training and pioneering research,” Farrell said.
Healthscope CEO Greg Horan said the redevelopment of the hospital will provide critical new healthcare services in Melbourne’s northern corridor, as well as continuing Healthscope’s work to support and develop the next generation of healthcare professionals. “It’s very exciting to see this hospital now completed and fully operational,” Horan said.
The hospital also features artwork — ‘Murungidyal’ The Healing — by First Nations artist Karen Lee Mungarrja, a Wiradjuri artist of the Tubba-Gah clan, Dubbo, NSW.
The artwork, commissioned for Healthscope’s recent reconciliation action plan, features a Boab tree, eucalyptus leaves, circles, rainbows and a journey symbol. In Karen’s words, “This artwork tells a story representing the values of Healthscope and the importance of community in the journey of care. The eucalyptus leaves are
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 31 DESIGN IN HEALTH
Image courtesy of Healthscope.

a representation of their use in Smoking Ceremony to welcome people and their use as bush medicine to heal. Meeting circles represent both the community and the staff that come together to provide care. The Journey symbol represents both the diversity of people who come to Healthscope and the journey of their health care. The Rainbows are the symbol of hope.”
The new facilities will also enhance La Trobe’s research capabilities by strengthening its partnership with Healthscope that has already generated more than 60 publications in the past four years, many of which are co-produced with Healthscope staff and consumer representatives.
La Trobe Private Hospital’s services are complemented by its sister hospital,
Northpark Private Hospital, located just minutes away. Northpark Private Hospital offers a range of services, including ophthalmology, gynaecology, ENT and general surgery, along with maternity services and an early parenting unit. The hospital has also recently opened its expanded 56-bed mental health service which includes a dedicated older person’s mental health unit.
According to Healthscope, an important innovation at La Trobe Private was the implementation of a mobile CSSD (central sterile services department) where cleaning and sterilisation takes place at La Trobe Private Hospital’s sister hospital, Northpark Private Hospital, located a few minutes away. This service maximises efficiency across both hospitals.
“The hospital has also recently opened its expanded 56-bed mental health service which includes a dedicated older person’s mental health unit.”

HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 32
DESIGN IN HEALTH
Image courtesy of Healthscope.
Image courtesy of Healthscope.
External view of La Trobe Private Hospital.
From idea to action: Neat keeps it simple for Royal Australasian College of Surgeons

Technology and healthcare continue to blend in exciting ways — from the delivery of smarter medical devices and the integration of AI to telehealth, professional education and data analytics. The latest data from the Australian government shows that the global healthcare market is forecast to reach a value of US$505.4 billion by 2025.
Digital healthcare delivers better outcomes by empowering clinicians to focus on their patients remotely or at the bedside with the support of reliable and secure IT solutions. It is also changing the way healthcare professionals communicate and manage workflows. From the delivery of education and training through to improved collaboration when delivering multi-party patient treatment plans.
What’s clear is that technology also has an increasing business focus as healthcare providers seek to find new ways to improve clinician experiences and deliver more effective patient outcomes.
A great example of this in action is the Royal Australasian College of Surgeons (RACS) and their recent adoption of video collaboration technology to improve communication and workflow.
A reputable not-for-profit, known for its mentorship and development of surgeons, RACS plays a vital role in supporting the
health and well-being of its communities. It aims to improve surgical care, advocate for better health policies, promote research and innovation, and engage with the public. With nine offices across Australia and New Zealand, it needs to maintain relationships with health departments while also providing training, networking and examinations for prospective surgeons.
Given its operational complexity, RACS offices are often overbooked with different use cases and users — creating a minefield of miscommunication and confusion. Without a resolution, RACS could lose relationships with vital healthcare departments and would be unable to provide the best workshops and training for prospective surgeons.
RACS chose to partner with Neat, a Norwegian video technology company that offers digital solutions for meetings and collaboration, investing in the Neat Board for all offices. The Neat Board provides a full, responsive video meeting room experience, even for remote workers, enabling the college to meet the needs of its office-based team while also delivering a flexible solution for hybrid working.
The Neat Board — on wheels — allows RACS team members to effortlessly move their virtual meetings from room to room, providing a flexible communication solution that reduces confusion and increases workplace efficiency.

Neat also provides the equality that RACS advocates for, allowing employees to join meetings from a hybrid location. With Neat Symmetry, AI ensures employees are framed on screen equally so everyone can be seen and heard, while also eliminating those pesky technology errors that often appear in virtual meetings. This gives a voice to surgeons even if they aren’t on-site and allows the company to train their prospective surgeons with members of the FRACS tuning in from anywhere in the world.
Dubbed a ‘digital canvas’, the Neat Board also enhances ideation and creativity. Students and teachers alike can draw and brainstorm directly onto the Board, and save, upload, and share these ideas with remote-based participants.
In recent years, telehealth adoption has accelerated significantly and Neat devices are ideal for patient-healthcare provider communication. By removing noise and distractions, the Neat Frame’s HD camera and a three-mic audio system ensures everyone is seen and heard without distortion, enabling conversations to flow naturally, and reducing the risk of miscommunication.
Neat technology can enhance your healthcare organisation. Join us in revolutionizing healthcare delivery through innovative video collaboration solutions — together, we can enhance patient care and deliver better healthcare outcomes.
» For more information visit neat.no
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 33 SPONSORED CONTENT
RACS Surgeons-in-training in action with the Neat Board
Targeted prostate cancer treatment hopes to minimise side effects
The Icon Cancer Centres in Victoria are using focal low dose rate (LDR) brachytherapy to provide highly targeted radiation for prostate cancer.
LDR brachytherapy has been a standard treatment option for some years, and offers a similar side effect profile compared to external beam radiation and surgery, but the newer focal approach is designed to target the cancer more closely.
The focal treatment is said to be suitable for about 15–25% of prostate cancers that are confined to one area of the prostate and assessed on biopsy as low to intermediate risk.
The treatment, part of the LIBERATE registry, is aimed at examining oncologic outcomes and the possible reduction of the side effects such as erectile dysfunction, which are present in other treatments.
A targeted approach
Dr Andrew See, radiation oncologist at Icon Cancer Centres and co-lead of the LIBERATE registry, said, “Because of advances in diagnostics and imaging, we now have an unprecedented level of understanding of where the cancer is within the prostate, like
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 34 TECHNOLOGY
having precise GPS coordinates. We can go in with a very targeted approach just to treat that geographic area with a small margin.
“We’re treating only about 20% of the prostate using the brachytherapy seeds, instead of all of it, and you’re getting rid of the cancer with a 15-minute outpatient procedure, which is like a haircut, but you’re leaving 80% of their prostate untouched. Doing this minimises the risks of erectile dysfunction, urinary incontinence and bowel injury.”
Focal LDR brachytherapy treatment involves radioactive seeds being inserted into the prostate to deliver radiation directly to cancer cells, while minimising damage to the surrounding healthy tissue.
Studies into the procedure to insert the seeds have shown it is comparatively quicker, less
invasive and with a decreased likelihood of ongoing side effects, such as urinary incontinence and erectile dysfunction, than surgery or external beam radiation.1
See said, “All prostate cancer treatments come with some level of risk. With active surveillance men can feel a psychological burden of knowing they have cancer, and the ongoing testing can be fatiguing, even when their cancer is not symptomatic.
“We are always looking at how we can kill the cancer whilst reducing risks and side effects for patients.”
Brachytherapy seeds emit radiation for three months, with the cancer being destroyed during this time. The seeds then become inert and do not need to be removed.
Additional advantages
Focal LDR brachytherapy is said to have additional clinical advantage for patients should another prostate cancer be found later in life, with other treatment options remaining available.
“If a new cancer appears on the other side of the prostate, the patient can still have surgery if needed. Successful treatment via focal brachytherapy doesn’t prevent a new cancer occurring later on. We know from surgeon feedback that there is no issue removing the prostate if this occurs, and for those few patients we have still given them perhaps several years with their prostate and without issues of incontinence and sexual dysfunction that could occur from standard treatments of the whole gland,” See said.
So far, 110 men have contributed their data to the registry. See said early results are promising but they will have to wait some years for long-term data.
“The sense is that morbidity is definitely less, and tolerance is much better. Early oncological outcomes are still a few years off, but there’s been no reason not to be positive,” See said.
The importance of early detection
According to the Australian Institute of Health and Welfare2, prostate cancer is estimated to be the most commonly diagnosed cancer for males and for Australia overall in 2023, with an estimated total of 25,500 cases.
The majority of prostate cancers are diagnosed at stage I or stage II, and earlystage localised prostate cancer is most suitable for focal LDR brachytherapy.
Focal LDR brachytherapy treatment is available at Icon Cancer Centres located in Epworth hospitals in Geelong, Richmond and at Epworth Freemasons in East Melbourne.
See is co-leading the LIBERATE registry with urologist colleague Associate Professor Jeremy Grummet. He said, “As a surgeon, I also treat more aggressive prostate cancers with robotic prostatectomy, so I see the typical side effects our standard treatments so often cause. But seeing our patients after focal brachytherapy and their lack of side effects, it’s like chalk and cheese. As our study’s name implies, we are really trying to “liberate” prostate cancer patients from the burden of treatment side effects.”
Grummet, however, also stressed the importance of early detection. “Focal LDR brachytherapy is most suited to men whose prostate cancer is low–intermediate risk and these men are most likely to be asymptomatic. This highlights the importance of early detection,” he said.
It is recommended that men aged 50 and over or aged 40 and over with a family history of prostate cancer consider prostate specific antigen (PSA) testing.
2. https://www.aihw.gov.au/reports/cancer/cancer-data-inaustralia/contents/overview-of-cancer-in-australia-2023 iStock.com/koto_feja
1. https://bjui-journals.onlinelibrary.wiley.com/doi/full/10.1111/ bju.13252
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 35 TECHNOLOGY
Featured Products
Moisturising antibacterial hand gel
Introducing TGA registered Aqium Moisturising Antibacterial Hand Gel (Aust R 410937). Proven to increase skin hydration by 14 percent in settings that mimic hospital staff use — sanitising hands 20+ times per day over a two-week period1
Aqium Moisturising Antibacterial Hand Gel is enriched with four moisturisers, contains 70 percent w/w ethanol absolute and is quick drying.
The Dermal Tolerability Study commissioned by Ego also found Aqium Moisturising Antibacterial Hand Gel to have no impact to skin pH even with frequent and extended use1. And 94 percent of those surveyed felt Aqium Moisturising cared for their skin1
1. Ego Pharmaceuticals commissioned external dermal tolerability study. Average increase in skin hydration (corneometer), average change in pH (skin pH meter). Participant assessments. n=33. Ego Pharmaceuticals Pty Ltd www.egopharm.com




HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 36
Fill spray bottles, mop buckets and floor scrubbers automatically with a SEKO chemical dispensing system.
secure chemical
and dispensing
Reduced chemical
Customisable systems Wasted chemical Erratic cleaning performance Staff exposed to concentrated chemicals ProMax Perfect proportioning at the push of a button seko.com
Isn’t it time you wiped out manual chemical dispensing? SekureMax Safe,
storage
Consistent results
consumption
Hemodynamic monitoring solution
Getinge’s advanced hemodynamic monitoring solution PiCCO is designed to provide a minimally invasive measurement of cardiac output and its determinants (preload, afterload, contractility) as well as the quantification of pulmonary oedema through the measuring of the Extravascular Lung Water Index (ELWI)1. By indexing the ELWI to the patient’s predicted body weight, underestimation of lung water, particularly in obese patients, can be avoided.1
Getinge’s PiCCO is a clinically proven tool for hemodynamic assessment and management in a broad range of critically ill patients.1,2 With its combination of intermittent transpulmonary thermodilution and continuous pulse contour analysis, the PiCCO technology can be used to provide a complete picture of the hemodynamic situation. 1,2,3,
To allow easy integration into a user’s existing product portfolio, Getinge is partnering with various monitoring companies like GE, Philips, Dräger and Mindray, so its PiCCO haemodynamic monitoring can be implemented with the already familiar bedside user interface in a hospital.
The full reference list is available here: https://anz.getinge.com/picco-reference-list.
Getinge Australia Pty Ltd www.getinge.com/anz
Energy-efficient filters
Camfil Hi-Flo bag filters are designed to provide optimal energy-efficient air distribution, which should result in longer filter life and a lower total cost of ownership (TCO) for facilities. The filters are designed to remove airborne contaminants such as smoke, bacteria, fumes, fungi and virus-bearing droplet nuclei. They incorporate high-lofted, air-laid glass microfibre filtration media for consistent submicron particle capture, efficiency and low resistance to airflow throughout the life of the filter.
Available in various efficiencies, including M6, F7, F8 and F9 efficiencies to EN 779, Hi-Flo bag filters are used in supply and exhaust air applications, including pre-filtration within cleanrooms. Certain models are also available with an A+ Eurovent Energy Rating and/or ProSafe certification.
The filters feature a pocket design and are made with high-quality materials to enable optimal performance and energy efficiency. They are suitable for use in industrial, commercial, medical and institutional applications to improve indoor air quality and comfort. The filters have a recommended final pressure drop of 2x the initial pressure drop and are designed with a galvanised steel frame and PU-foam gasket.
Furthermore, the Hi-Flo series includes energy-efficient ventilation filters with performance standards that make them suitable for various commercial and industrial HVAC installations. These filters clean the air from particles in order to improve indoor air quality and workplace conditions.
Camfil Australia Pty Ltd www.camfil.com.au





HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 37
A Day in the Life of Sarah Morse
Registered nurse and a former (NSW) Young Australian of the Year

06:00 My day starts with morning cuddles as my six-year-old crawls into my bed as soon as she wakes up somewhere between 6:00 and 6:30. Warm sleepy cuddles are the best!
07:00 I’m off for some self-care and a walk around my local neighbourhood. I use this time to think and pray through my day and mentally prepare for what’s next. Today, I talk to my accountability buddy as I walk.
06:30 My alarm goes off, and I am officially awake. If I can, I start my day with prayer and meditation, but that doesn’t always happen. Cuddles for my 11-year-old when I get up.
08:30 The house is quiet as the girls head off to school. Breakfast and a quick shower to get ready for the day. Don’t forget the coffee!!
09:00 Morning meeting with my husband and co-founder of Unchained Solutions to discuss our team and any upcoming trainings.
10:30 As I drive across the city, I am grateful for this life I get to live, living all my passions at once, although the days are sometimes big and the juggle is real.
11:00 Arrive at a hospital for room set-up and AV check for my morning masterclass.
08:00 I arrive home to the final throes of my girls getting ready for school. I am grateful for the partnership with my husband who is awesome at the morning hustle! Kisses and hugs, and final checks of their bags to make sure they’ve got everything as they head out the door.
09:30 At my desk to brief my VA on social media and marketing, and answer any emails before heading out for the day. I fly through putting on my make-up, red dress and red sparkly shoes and am ready for today’s workshop.
11:30 Deliver my Culture of COURAGE masterclass to a room full of health professionals, inspiring them that they play a part in helping their teams to thrive. I invite them to journey on the road to recovery from burnout and moral injury to a thriving culture once more.
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 38 A DAY IN THE LIFE
06:30 07:00 08:00 08:30 09:00 09:30 10:30 11:00 11:30
06:00
From working as a health advisor at a safe house for human trafficking survivors in Spain to a palliative care nurse in Australia, former NSW Young Australian of the Year Sarah Morse has over two decades of nursing experience under her belt. With experience in cancer services and palliative care, she knows all too well how burnout impacts nurses and other health professionals. Following her personal experience, Sarah now works as a consultant, facilitator and keynote
speaker working with nurses and other health professionals to help them address burnout and moral injury, and to cultivate thriving workplaces.
She is also the Founder and Director of Unchained Solutions, a social enterprise aimed at inspiring Australian businesses to make an impact on modern slavery. Her service has landed her awards such as the Women’s Economic Forum Woman of Excellence and the Ausmumpreneur Women Will Change the World Award.

13:00 Time for lunch and a change into my scrubs before heading to an afternoon shift at the hospital on a busy surgical ward.
14:30 Shift starts and I receive handover. It’s going to be a busy one! As I work, I remember the video I watched in orientation called “What if Disney ran your hospital” about how to create memorable moments for people in hospital. I do my best to personalise the experience for each person.
15:00 I prepare a patient for theatre. He is an elderly man with sky high blood pressure, which he says always goes up as soon as he gets to the hospital! He is asymptomatic, and I ring the anaesthetist, who is happy to continue.
15:30 A patient returns following reconstruction surgery of his nose after the removal of a BCC. He is in good spirits, despite his bandaged nose. As I am doing his post-op checks, I get notification that another patient has returned.
15:45 This time a 93-year-old man who is a high falls risk. He is slightly confused from the anaesthetic, and his daughters seek to reorientate him to the ward. I consult with his surgeon, who agrees that keeping him in hospital for a few extra nights is in his best interest.
17:00 The rest of the afternoon passes in flurry of patients coming and going for their day surgery procedures, and attending to their individual pre-op and post-op needs.
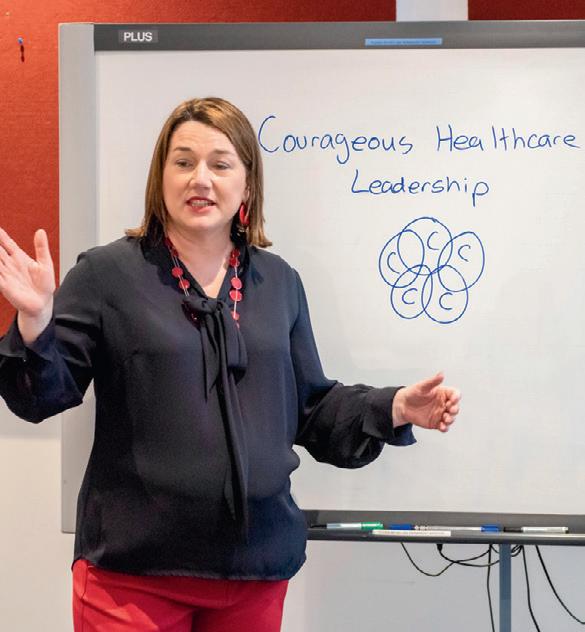

18:30 Time for dinner, and FaceTime to say goodnight to my girls. Sadly, I’m not there for bedtime tonight, but the cadence of my life where no two days are the same means that tomorrow I’ll be there during the day for school assembly, pick-up, homework and bedtime.
19:00 After dinner, my day only patients have left and I attend to my patients who are staying overnight.
22:00 I hand over my remaining patients and my shift finishes.
23:00 Home and showered. Time for a quick chat with my husband to debrief our days before falling asleep, excited to see what tomorrow will bring.
A Day in the Life is a regular column opening the door into the life of a person working in their field of health care. If you would like to share a day in your working life, please write to: hh@wfmedia.com.au
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 39 A DAY IN THE LIFE 15:00 17:00 22:00 23:00 18:30 19:00 15:30 15:45 13:00 14:30
Understanding vision shifts to support
early psychiatric illness diagnosis

Neuroscientists from the university have established a link between shifts in visual perception and the cadence of our steps while walking. Understanding how vision shifts as we walk could help develop early diagnostics for neuromuscular or psychiatric illness and understand changes in mobility as we age.
The research, published in Nature Communications, revealed that the brain processes vision in a rhythmic manner, rising and falling in sensitivity in a cycle that corresponds to the rhythm of our steps. When swinging from one step to the next, human perception is good and reactions fast. During footfall, however, our vision is not as sharp and reactions are slowed.
Lead author Dr Matthew Davidson said the research findings revealed the relationship between perception and movement and could bridge the gap between experimental psychology and natural, everyday behaviour.
The study also confirms the understanding of the visual brain sensing the environment in a strobe-like way; our perception takes regular samples of the world before stitching them together to create a seamless experience. The study found that shifts in our visual perception have important perceptions for understanding human behaviour.
The research was conducted by Dr Matthew Davidson with colleagues Professor David Alais and Professor Frans Verstraten from the University of Sydney. The study extends earlier research that showed that perception of vision and sound is cyclic, with the brain taking approximately eight samples per second.
Alais said the critical new finding in this study is that these oscillations in the brain’s sampling of the world slow down when walking to match the step cycle.
“Humans take about two steps per second when walking and generally keep to a consistent rhythm. The reported oscillations in visual sensitivity also occur at about two cycles per second and are locked to the step cycle. In some participants these rhythmic oscillations occur at four cycles per second but these were also locked to the step cycle,” Alais said.
Davidson added that using VR technology enabled the researchers to discover that vision moves through a good and bad phase on every step. It is unclear why the brain’s perceptual processes are so closely linked to walking. The researchers tracked 45 subjects walking back and forth along a 10-metre path in a virtual environment. During each walk — lasting about nine
seconds — subjects were required to respond to between zero and eight visual stimuli, with their eye and head movements tracked along with gait and walking information. Of the 45 subjects, insufficient data was collected for seven subjects. In the datasets for 38 subjects, reduced perception at footfall was recorded 83% of the time.
“One possible explanation is that vision becomes secondary to motor control while your foot is grounded and the next step is planned. Once you are in the swing phase between footfalls, the brain switches back to prioritising perceptual sampling of the world, creating an ongoing perceptual rhythm that harmonises with your step rate,” Alais said.
The researchers now plan to study whether the perception of sound and touch also modulate as we walk. “An obvious question is whether these oscillations in perception are more pronounced in the elderly given difficulties with balance and coordination as we age. It also raises the exciting possibility that we could develop cheap and easy diagnostic tests using VR headsets or use this information to develop tests for early onset of neuro-muscular disorders or some psychiatric illnesses, which can manifest in abnormal gaits,” Davidson said.
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 40 CLINICAL SERVICES
iStock.com/Zbynek Pospisil
Unlocking Hospital Performance:

In the fast-paced world of healthcare, where every decision can impact efficiency and effectiveness, using data to inform decision making is imperative. As healthcare leaders and executives, your mission is clear: to optimise operations, enhance patient care, and ensure the smooth functioning of your hospital or health system within existing resources. Achieving these goals requires more than just intuition — it demands actionable insights derived from data-driven solutions.
Enter SystemView by HealthCare Logic — the game-changing platform designed to revolutionise hospital performance management, now live in over 150 hospitals globally. As the only interactive and userconfigurable platform offering a standardised enterprise solution across all four performance domains of hospitals, SystemView empowers healthcare leaders like you to make informed decisions that drive tangible results.
Unparalleled Analytic Power
At the heart of SystemView lies its unmatched analytic power. Built on decades of industry expertise and innovation, this cutting-edge platform harnesses novel-algorithms and advanced predictive analytics provided in intuitive visualisations. Whether you’re analysing outpatient wait times, surgical efficiency, emergency department flow, or bed capacity, SystemView provides the comprehensive insights you need to optimise every aspect of your hospital’s operations.
Introducing SystemView by HealthCare Logic
Intuitive Interface, Infinite Possibilities
SystemView isn’t just powerful — it’s also remarkably easy to use. With a purposebuilt web interface that prioritises simplicity and functionality, SystemView ensures that even the most complex data sets are accessible and actionable. From clinical systems represented as visual reports to highfrequency data feeds with short time-lags, SystemView puts the information you need right at your fingertips, empowering you to drive meaningful change with confidence.
Real-Time Insights for RealWorld Impact
In today’s dynamic healthcare landscape, real-time insights are non-negotiable. That’s why SystemView offers near-real-time disaggregated data that directly impacts both clinicians and executives. By providing visibility into all relevant patient and clinical team-level data associated with hospital goals, SystemView enables proactive management, informed decision-making, and sustainable improvements in clinical team and hospital performance.
Real-world Insights
But don’t just take our word for it — here’s what healthcare leaders who have implemented SystemView have to say:
“It enables us to have conversations that are far more targeted with clinicians — more dynamic data, more timely information, and see if your strategy is giving you an improvement or not.” — Chief Operating Officer
“SystemView allows us to make more informed and faster decisions in delivering our health services. The system is significantly more advanced than most systems I’ve seen.” — Executive Director, Women’s, Newborn & Children’s Services
Your Path to Performance Excellence
Are you ready to unlock the full potential of your hospital or health system? Join the ranks of healthcare leaders who are transforming their organisations with SystemView. From seamless integration into existing workflows to ongoing support and training, HealthCare Logic is committed to partnering with you every step of the way to inspire improvement.
Experience the Future of Hospital Performance Management
Visit healthcarelogic.com/systemview to learn more and schedule a personalised demo today. Together, let’s redefine what’s possible in healthcare.

HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 41 » For more information visit Healthcare Logic www.healthcarelogic.com SPONSORED CONTENT
3D-printed skin could improve reconstructive surgery
Fat tissue holds the key to 3D printing layered living skin and potentially even hair follicles.
That’s according to an international team of researchers, who recently harnessed fat cells and supporting structures from clinically procured human tissue to precisely correct injuries in rats. Their findings, published in the journal Bioactive Materials, could have implications for reconstructive facial surgery and even hair growth treatments for humans.
“Reconstructive surgery to correct trauma to the face or head from injury or disease is usually imperfect, resulting in scarring or permanent hair loss,” said Professor Ibrahim T Ozbolat from The Pennsylvania State University (Penn State), who led the international collaboration. “With this work, we demonstrate bioprinted, full thickness skin with the potential to grow hair in rats. That’s a step closer to being able to achieve more natural-looking and aesthetically pleasing head and face reconstruction in humans.”
While scientists have previously 3D bioprinted thin layers of skin, Ozbolat and his team were able to intraoperatively print a full, living system of multiple skin layers, including the bottom-most layer or hypodermis. Intraoperatively refers to the ability to print the tissue during surgery, meaning the approach may be used to more immediately and seamlessly repair damaged skin, the researchers said. The top layer — the epidermis that serves as visible skin — forms with support from the middle layer on its own, so it doesn’t require printing. The hypodermis, made of connective tissue and fat, provides structure and support over the skull.
“The hypodermis is directly involved in the process by which stem cells become fat,” Ozbolat said. “This process is critical to several vital processes, including wound healing. It also has a role in hair follicle cycling, specifically in facilitating hair growth.”
The researchers started with human adipose, or fat, tissue obtained from patients undergoing surgery at Penn State Health Milton S. Hershey Medical Center. Dino J Ravnic, an associate professor at Penn State College of Medicine, led his lab in obtaining the fat for extraction of the extracellular matrix — the network of molecules and proteins that provides structure and stability to the tissue — to make one component of the bioink.
Ravnic’s team also obtained stem cells, which have the potential to mature into several different cell types if provided the correct environment, from the adipose tissue to make another bioink component. Each component was loaded into one of three compartments in the bioprinter. The third compartment was filled with a clotting solution that helps the other components properly bind onto the injured site.
“The three compartments allow us to coprint the matrix-fibrinogen mixture along with the stem cells with precise control,” Ozbolat said. “We printed directly into the injury site with the target of forming the hypodermis, which helps with wound healing, hair follicle generation, temperature regulation and more.”
They achieved both the hypodermis and dermis layers, with the epidermis forming within two weeks by itself.
“We conducted three sets of studies in rats to better understand the role of the adipose matrix, and we found the co-delivery of the matrix and stem cells was crucial to hypodermal formation,” Ozbolat said. “It doesn’t work effectively with just the cells or just the matrix — it has to be at the same time.”
They also found that the hypodermis contained downgrowths, the initial stage of early hair follicle formation. According to the researchers, while fat cells do not directly contribute to the cellular structure of hair follicles, they are involved in their regulation and maintenance.
“In our experiments, the fat cells may have altered the extracellular matrix to be more supportive for downgrowth formation,” Ozbolat said. “We are working to advance this, to mature the hair follicles with controlled density, directionality and growth.”
According to Ozbolat, the ability to precisely grow hair in injured or diseased sites of trauma can limit how natural reconstructive surgery may appear. He said that this work offers a hopeful path forward, especially in combination with other projects from his lab involving printing bone and investigating how to match pigmentation across a range of skin tones.
“We believe this could be applied in dermatology, hair transplants, and plastic and reconstructive surgeries — it could result in a far more aesthetic outcome,” Ozbolat said.
“With the fully automated bioprinting ability and compatible materials at the clinical grade, this technology may have a significant impact on the clinical translation of precisely reconstructed skin.”
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 42 INFECTION CONTROL
Miji Yeo, a postdoctoral researcher at Penn State, checks the bioink cartridges on a 3D printer developed to intraoperatively print layers of skin.
Michelle Bixby/Penn State.
University of Canberra Introduces CARAT: A Trailblazing Hub for Elder Rights and Recognition

As the Australian population ages, there will be increased demand for healthcare services that are tailored to the needs of elderly patients. In recent years, however, controversies in the quality of aged care at facilities across the nation have highlighted a clear disconnect between the needs of patients, and what universities see as best practice.
To tackle this disparity, researchers at the University of Canberra have teamed up, launching a brand new hub to advocate for the improvement of aged care services nationwide. The Centre for Ageing Research and Translation (CARAT) looks to transform the role that universities have in the care of elderly Australians, and positions the university as a leader, demonstrating what is possible in the aged care space.
Focus Areas of CARAT
CARAT has three core focus areas — with a notable focus on three core themes, that being dementia and cognition, workforce, and innovative models of care.
Each of these three areas recognises the multi-faceted problems that healthcare providers must tackle to provide the best patient care experience possible. Dementia, for example, is a widespread issue amongst older Australians, a leading cause of death for elderly women, and is only expected to grow in prevalence in the decades to come.
Understanding dementia on its own is helpful, however, understanding how best practice intertwines with other elements of research can assist researchers in determining the conditions necessary to support the health of aging Australia.
For example, it is well known that there is currently a high demand for aged care professionals around Australia, with many firms recruitment and retention for potential employees can sometimes be very difficult.
CARAT’s research endeavours to understand what’s possible, while considering the current and future requirements of aged care recruitment nationwide.
The team is led by Professor Diane Gibson, a globally renowned researcher specialising in ageing and aged care, particularly in the interface that research and policy provide. Overall, the CARAT team contains approximately 30 researchers across the university affiliated with the program, forming a multidisciplinary team that is already having a real-world impact.
Discussing the launch of CARAT at an event in February 2024, Professor Gibson was optimistic about the benefits that the program could bring to elderly Australians, saying “We look forward to further opportunities for our work to have a greater impact in improving the lives of older people across Australia and the world.”
Clinical Placements with Older People (CPOP)
One such program that is having an impact is a Commonwealth-backed initiative that looks to raise the profile of gerontological nursing in Australia.
With CARAT leading the initiative, the Clinical Placements with Older People (CPOP) program works with aged and healthcare providers to provide nurses with high-quality clinical placements that empower them to use the skills they’ve acquired in a highly relevant workplace.
Gerontological nursing qualifications empower nurses with skills that are specific to working in aged care. This includes specific training on aspects of care that are not typically covered in non-specialised nursing roles.
This can be beneficial for both nurses and patients alike and can help ensure that patients receive the best possible care available, and students are afforded the best possible opportunity to work on their nursing skills in a contextually relevant environment.
For many Australians, understanding the role that aged care will play in the lives of elderly relatives will be crucial in driving positive care outcomes.
This can be especially relevant for those undertaking a course such as a Master of Social Work, as CARAT’s work aspires to blur the line between the classroom and the aged care facility.

» For more information visit: studyonline.canberra.edu.au
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 43 SPONSORED CONTENT
iStock.com/Rawpixel
Josh Young

Mindset training to improve patient outcomes
A new pilot study explores the effectiveness of patient mindset training for care teams to improve experience and outcomes.
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 45 CLINICAL SERVICES
iStock.com/Rudzhan Nagiev
Past research has shown that what patients think, believe or expect regarding medical care can influence care outcomes. They are also reported to have better outcomes when they have more adaptive mindsets about their treatments (eg, “this treatment will be effective”), their bodies (eg, “my body is capable”), their illnesses (eg, “diabetes is manageable”) and their care team (eg, “I am in good hands”).
To leverage the potential power of mindset in medical care, researchers from Stanford University developed and conducted ‘Medicine Plus Mindset’ training at five primary care clinics in the Bay Area.
As a part of the project, participants received two-hour training and a follow-up session a month later to reinforce the training. They reported a better understanding of mindset and a greater appreciation for its influence, and reported using the training when communicating with patients.
“The goal of what we’re trying to do is say these mindsets do actually matter for things like patient experience and patient satisfaction,” said the lead author of the study, Kari Leibowitz. “But they also matter for objective things like patient health outcomes.”
“Care teams have an intuitive sense that their patients’ mindsets matter and, in their best moments, they are shaping patient mindsets for the better,” said senior author Alia Crum, Associate Professor of Psychology in the School of Humanities and Sciences.
“But they don’t often realise the science behind just how important mindsets are. They also typically don’t have a framework for how to identify those mindsets and cultivate them in their patients skilfully, ethically and deliberately.”
Findings of the study have been published in Patient Education and Counselling
The impact on care outcomes
“Mindsets are core assumptions that we have about things in the world and how they work,” Leibowitz said.
“Medicine is effective, medicine is harmful. Cancer is a catastrophe, cancer is an opportunity.” Those mindsets, Leibowitz said, can cause a cascade of psychological processes, which can positively or negatively affect patient outcomes.
As such, small changes in a care provider’s words can change patient mindsets for the better. For instance, a provider might say “the vast majority of patients do not experience side effects from this treatment” instead of “a small percentage of patients experience side effects from this treatment”.
Additionally, when treating a patient with a chronic illness, such as diabetes, a provider might say “this diet has really worked for people in your situation” instead of simply prescribing the diet.
If a patient is experiencing side effects of a treatment, they might benefit from knowing that those could be signs that the treatment is working, not merely an unfortunate consequence.
“One thing that I like about the Medicine Plus Mindset program compared to scripted responses is that it creates some flexibility for me to understand who I’m speaking to.”
However, medical care staff generally receive no formal training on shaping patient mindsets. In this study, a team of researchers and clinicians delivered the Medicine Plus Mindset training to primary care staff, including all members of the care team, from physician to front desk staff.
The training included information about strategies and opportunities for shaping patient mindset and tips for communicating warmth and competence, and care teams were encouraged to share their experiences seeing mindset affect patient outcomes.
Pilot study
The team first conducted a pilot study, delivering the training to 27 staff members at two Bay Area clinics. After completing training development, they delivered the training to 186 staff members at Stanford Primary Care and in a primary care clinic within the Alameda Health System.
The Medicine Plus Mindset training differs from standard medical communication training in that it doesn’t focus on specific scripts. Instead, it focuses on underscoring the value of mindsets in shaping health outcomes and providing high-level frameworks for which mindsets matter most.
“One thing that I like about the Medicine Plus Mindset program compared to scripted responses is that it creates some flexibility for me to understand who I’m speaking to,” said Larry Kwan, a study co-author and Clinical Assistant Professor at Stanford Medicine. “Scripting doesn’t allow for that.”
The researchers taught care teams that they ultimately want to help patients cultivate useful mindsets about their treatment, the capability of their care team, their bodies and their illnesses.
The care teams also worked together to share ways that they have successfully changed patient mindsets in the past.
We are not mindset experts, but all of the providers are experts in their jobs and in providing patient care, Leibowitz said. “The tool is meant to be used flexibly, and these team members can draw on their own experience, insight and wisdom to figure out ways to deploy it.”
Care team experiences
After the initial training and follow-up session, the researchers evaluated the training by assessing self-reported care team reaction (directly after the training), learning outcomes (before and one month after the training) and behaviour (before and one month after the training).
Participants overwhelmingly reported the training as being both “very enjoyable” and “very useful”. They also reported increases in the belief that patient mindsets influence healthcare outcomes, and in their ability to shape patient mindsets.
“After the training, our participants felt like they were better able to recognise and shape patient mindsets in practice,” Leibowitz said.
In the weeks following the training, care team members reported using the training to shape patient mindset; they also reported increased satisfaction in their own jobs. The research team also anecdotally noted that the training was particularly helpful to those in nonprovider roles, such as medical assistants. “They play a really big role in the encounter, but maybe don’t always feel like they have the opportunity to make a big difference,” Leibowitz said.
“A lot of them reported feeling like now they can really see how their words and actions make a difference.”
Addressing limitations
While care teams reacted positively to the training, there are limitations. High medical staff turnover could limit the effectiveness of the training and busy schedules could limit the time available for training. However, physicians and care teams still rate the training highly.
Future areas of study include evaluating the effects of mindset training on patient health outcomes and implementing the training outside of primary care.
“Patient mindsets are being shaped from the moment they walk in the office to how they are treated at the pharmacy,” Crum said. “That’s why we wanted the training to be as inclusive as possible. We all have a role to play.”
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 46 CLINICAL SERVICES
Adopting AI in Australian Healthcare: What Does It Look Like?

Rapid innovation in Artificial Intelligence (AI) technologies is rapidly transforming many industries, such as consumer retail and logistics. However, AI is experiencing a new frontier of challenges in the healthcare sector.
There has been a call for the ethical and responsible adoption of AI technologies such as Large Language Models (LLMs) within the healthcare sector, notable from leading industry body, the Australian Medical Association (AMA).
This has fuelled debate within the healthcare space on the role of AI in the workforce, with new graduates from a Masters in Healthcare Leadership to well-heeled industry participants debating the role these powerful technologies should have in today’s techheavy medical landscape.
AMA Calls for Oversight
The AMA has long been considered a leading body in advocacy for new and changing practices in the medical sector. Releasing a position paper on the role of AI in August 2023, the peak body representing physicians called for the responsible implementation of such technologies within the industry.
In particular, the AMA noted that while AI technologies are powerful, ultimately, they should not be considered as a replacement for traditional practitioner-led medical treatment. Instead, the paper called for the
implementation of models that enhance human clinical practice.
Additionally, the position paper called for the considered development of patient-oriented models — emphasising that models and practices created should fundamentally prioritize patient-centered care. The position paper considers a range of key areas in the development of AI, including maintaining privacy controls on healthcare data, no matter whether it is identifiable or not.
Fundamentally, it’s important to consider the role of AI in patient-oriented healthcare. AI can be a powerful tool — with new and emerging platforms providing valuable insights in fields as varied as cancer detection, robotic surgery, and medication development.
AI mustn’t be used as a tool to replace the role of medical staff. While other industries, notably those involved in software development, have experienced significant layoffs due to the presence of AI in the workforce, the AMA highlights that it’s important that AI tools on their own are not sufficient to provide well-informed medical treatments.
Identifying AI Views in Healthcare
How does the broader healthcare industry feel about the implementation of AI? It’s important to understand how the industry perceives AI
and applications, particularly as it develops and becomes further enmeshed in healthcare. For one researcher at Southern Cross University, identifying industry attitudes towards AI and helping professionals understand how AI will impact their roles is a crucial part of researcher Lucy Shinner’s remit. As part of her doctorate, she pioneered the development of a tool, known as the Shinners Artificial Intelligence Perception (SHAIP) questionnaire, which allowed for Dr Shinner to gather key insights on the perceived role and impact of AI within the healthcare sector.
Dr Shinner’s work has proved critical in breaking down barriers between what’s perceived and possible in the world of AI and healthcare. Commenting on the role of AI in healthcare, she noted that “There are a lot of trust issues and this often comes down to understanding just how AI works”, highlighting that “The trick will be empowering healthcare professionals to come up with the ideas and get involved in or lead the development of new technology that will improve care delivery.”
Dr Shinner’s work is crucial in understanding how practitioners perceive the influence of AI within the workforce. As the healthcare sector continues to embrace the role of AI platforms, it will be critical for peak bodies and researchers to come together to identify ways that it can be used to drive successful patient outcomes.

HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 47 SPONSORED CONTENT
» For more information visit: online.scu.edu.au
Josh Young
Featured Products
Vacuum cleaner
The upgraded Nilfisk GD930 Pro HEPA vacuum is designed to help users to clean faster and efficiently. Featuring a 5x larger HEPA filter, the vacuum is designed for increased lifespan and is quieter than before, allowing users to clean anytime without disrupting anyone. New fleece bags are said to improve filtration by up to 10% and increase performance levels over normal paper bags.
The GD930 is durable, tough and built for long lifespan, saving on total overall costs and reducing on environmental waste. The detachable cord is designed to eliminate costly repairs and downtime with seamless, fast replacement by the operator.
The vacuum offers smart efficiency with the quick-start cord release and enhanced cable management allowing users to get moving on the job quickly.
The HEPA filter is set in the lid for faster access and the storage on top of the lid allows for quick startup and parking when performing multiple tasks.
The vacuum has a high filling capacity 15L container/dust bag offering increased productivity, timesaving and cost benefits.
The highly visible orange cable can help users avoid trip and fall accidents. The device features lightweight aluminium accessories, rubber grip for comfortable handling and lower noise output.
Nilfisk Pty Ltd
www.nilfisk.com/en-au
Air sampling unit
The Orum International TRIO.BAS unit, distributed by Cell Biosciences, is designed to help healthcare facilities to continuously monitor air quality, identifying potential sources of airborne pathogens and assessing the effectiveness of infection control measures.
The air sampling method involves the collection of air samples to detect and quantify microbial contaminants, such as bacteria and fungi, present in the ambient air. The approach is particularly designed for sensitive areas like operating rooms, isolation units and patient care areas, where microbial contamination poses a significant risk to vulnerable individuals.
Regular microbial active air sampling helps in preventing the spread of infections and enables healthcare professionals to implement targeted interventions, providing a safer environment for both patients and staff. This technique is designed to contribute to the overall improvement of healthcare facility hygiene, fostering a healthier and more secure


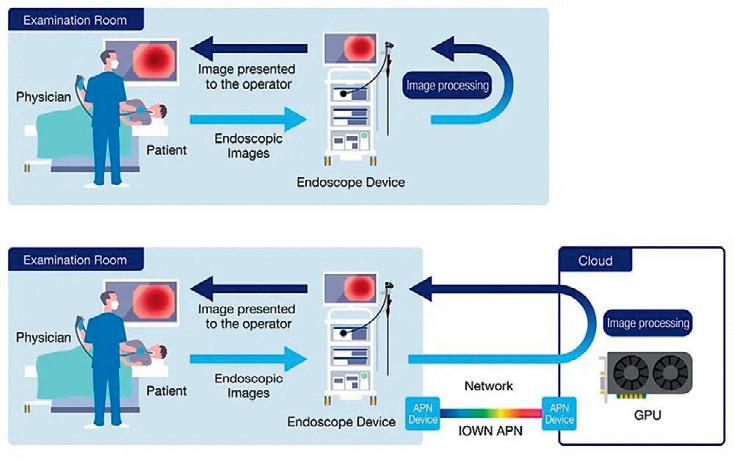
Cloud endoscopy system
NTT Corporation (NTT) and Olympus Corporation (Olympus) have jointly begun a demonstration experiment of a cloud endoscopy system that enables image processing on the cloud.
NTT’s IOWN APN technology and Olympus’s advanced technology for endoscopes will be used in a demonstration experiment of a cloud endoscopy system that enables real-time image processing of endoscopes on the cloud.
Through this demonstration experiment, the two companies will establish a reference model for the commercialisation of the cloud endoscopy system, overcome the current limitations of processing performance of endoscopic equipment, improve maintainability and provide a flexible and rapid market response to the market.
Based on the knowledge gained from the demonstration experiment, the companies will jointly consider the commercialisation of the cloud endoscopy system. Furthermore, NTT will establish a reference model for a network for medical devices that will solve various technical problems when medical devices are brought to the cloud, while Olympus will contribute to the establishment of an optimal network for the cloud endoscopy system and its reference model.
Olympus Australia Pty Ltd
www.olympusaustralia.com.au
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 48
Video conferencing device
Neat Frame is an ‘all-in-one’ portable video conferencing device featuring personal, portrait-orientated HD video framing technology and front-facing speakers designed to deliver a rich sound quality.
The device is suitable for healthcare professionals who need a reliable telehealth device that delivers seamless connectivity for face-to-face consults with patients and colleagues, while also allowing them to easily share digital content.
With its AI-powered 15.6″ portable touchscreen and an auto-framing camera, Neat Frame is designed to ensure that patients are seen and heard without distortion, allowing conversations to flow naturally. It removes distracting background noises, reducing the risk of miscommunication between patient and doctor.
The device set-up is simple for time-poor and overburdened hospital staff and IT teams. Being portable, Neat Frame can also move easily from space to space in hospitals, to reduce expenditure and increase the usability per patient.
Neat neat.no




Common pets and injury hospitalisations
Cats and dogs, the most common domestic pets in Australia, were responsible for 12,000 — over half (53%) of all — injury hospitalisations related to contact with animals in 2021–22, according to AIHW.
The Australian Institute of Health and Welfare’s (AIHW) latest report titled Contact with animals explores who is commonly injured and the types of animals responsible. The report describes patterns and trends in hospital admissions due to contact with animals between July 2012 and June 2022. It does not include data on emergency department presentations.
“During this 10-year period, hospitalised injuries due to contact with animals gradually increased. The age standardised rate of these injuries increased from 66.5 per 100,000 in 2012–13 to 90.5 in 2021–22,’ said AIHW spokesperson Dr Sarah Ahmed.
“There were 23,380 hospitalisations due to contact with animals in 2021–22, with a notable increase of 2230 (or 10%) hospitalisations from 2019–20 to 2020–21. The Pets and the Pandemic survey by Animal Medicines Australia indicates increased pet ownership throughout the COVID-19 pandemic.
Injury types
In 2021–22, the most frequent type of injuries caused by contact with animals were open wounds (13,419 cases, 57%) followed by fractures, toxic effects and superficial and soft tissue injuries. The body parts most commonly
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 50
iStock.com/dusanpetkovic
CLINICAL SERVICES
injured were the upper limbs (nearly half of these injuries) and head and neck.
Allergic reactions to animals sent 1180 cases to hospital, the majority being males who were twice as likely as females to be hospitalised for this reason. Anaphylactic reactions to bites and stings have the potential to be fatal; however, the report does not include information on deaths.
“Although owning a pet comes with a risk of injury, research has shown that interactions between humans and animals can provide benefits to our health and wellbeing,” Ahmed said.
“Over two in three Australian households are estimated to own a pet, so unsurprisingly common domestic pets account for the largest proportion of animals involved in injury hospitalisations.”
“Two in three pet owners are female and are 1.2 times as likely as males to be hospitalised due to a common pet-related injury.”
Two in three pet owners are female and are 1.2 times as likely as males to be hospitalised due to a common pet-related injury.
With 5030 injury hospitalisations, livestock made up almost a quarter (22%) of all injury hospitalisations due to contact with animals in 2021–22. Horses (22%), cows (13%) and sheep (3%) were the livestock most frequently contributing to injury hospitalisations. Females were twice as likely to be injured than males.
Venomous vs non-venomous animals
In 2021–22, the crude rate of injury hospitalisations due to venomous animals was 11.1 per 100,000, as compared to 72.8 per 100,000 for non-venomous animals.
“Australia is home to some of the most venomous animals in the world; however,
Australians are 6.6 times as likely to be hospitalised due to injury involving nonvenomous compared to venomous animals,” Ahmed said.
Injuries from marine animals most frequently occurred in summer during leisure activities. Sea creatures were responsible for 525 injury hospitalisations during 2021–22, making up 2.2% of all injury hospitalisations due to contact with animals. Males were more than twice as likely to be injured than females.
In 302 cases, 58%, these marine animals were venomous. The most common venomous marine animals contributing to these hospitalisations were jellyfish (23% of marine animals), stingrays (18%) and stinging fish (16%). Stings from the Irukandji jellyfish made up over three in four hospitalisations from all jellyfish.
LEARN MORE ABOUT

AND WHY CUSTOMERS RAVE ABOUT OUR QUALITY, ERGONOMICS, AND SERVICE.
Our team and valued partners are available to demo products and explore total solutions tailored to your needs. Start exploring

HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 51 CLINICAL SERVICES
Reach out to your local Ergotron Representative | Email: robin.burgess@ergotron.com | Mobile +61421080303
The missing ingredient in hypertension guidelines
New research suggests it’s time to update the hypertension treatment guidelines with recommendations on low-sodium potassiumenriched salt
In Australia and New Zealand, most people consume excessive amounts of sodium, with the estimated average said to be about 3600 mg/day.
High levels of sodium intake and low levels of potassium intake are widespread, and both are linked to high blood pressure (hypertension) and greater risk of stroke, heart disease and premature death. Using a salt substitute where part of the sodium chloride is replaced with potassium chloride addresses both problems at once, suggest researchers.
Salt and substitutes
A global collaboration of researchers from the US, Australia, Japan, South Africa and India reviewed 32 separate hypertension treatment guidelines - two from global organisations, five from regional organisations and 25 from country organisations — published from 1 January 2013 to 21 June 2023. The research has been published in the American Heart Association’s journal Hypertension
They found all guidelines referred to sodium reduction, with most recommending reducing salt intake. Many also recommended increasing dietary potassium intake, but only two — the Chinese and European guidelines — made a specific recommendation for using potassium-enriched salt.
Professor Garry Jennings, Chief Medical Advisor at the National Heart Foundation said as many as one in three Australian adults have high blood pressure — equivalent to 6.8 million people.
“It’s concerning that we have not made much progress in lowering that figure in the last decade, despite all the tools at our disposal. We know that reducing sodium and increasing potassium helps improve blood pressure control, but people find it hard to make the necessary changes to their diet.”
• Mean global sodium intake was recently estimated to be 4.3 g/ day, or about 10.8 g/day of salt — more than double the WHO recommendation for adults of less than 2000 mg/day sodium (equivalent to <5 g/day).
• In Australia and New Zealand, most people also consume excessive amounts of sodium — the estimated average is about 3600 mg/day.

• Sodium reduction is listed as a ‘best-buy’ chronic disease intervention by the WHO, proposing that all member states reduce mean population intake by 30% by 2025.
Guidelines and recommendations
Professor Alta Schutte, at The George Institute for Global Health and UNSW Sydney, said that despite data from randomised controlled trials demonstrating the health benefits of potassium-enriched, sodiumreduced salt substitutes, they are rarely used.
“We found current clinical guidelines offer incomplete and inconsistent recommendations about the use of these salt substitutes,” she said.
“Given the wealth of evidence available, we feel it’s time to include salt substitutes in treatment guidelines to help address spiralling rates of uncontrolled high blood pressure around the world and reduce preventable deaths.”
The study authors proposed the following wording for inclusion in clinical guidelines for blood pressure control:
• Strong recommendation for patients with hypertension — Potassiumenriched salt with a composition of approximately 75% sodium
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 52 CLINICAL SERVICES

chloride and 25% potassium chloride should be recommended to all patients with hypertension, unless they have advanced kidney disease, are using a potassium supplement, are using a potassium sparing diuretic or have another contra-indication.
• Conditional recommendation for the general population — If you have to add salt to foods, potassium-enriched salt with a composition of approximately 75% sodium chloride and 25% potassium chloride can be recommended for use by the general population in settings where there is a low likelihood that people with advanced kidney disease (stage 4-5) will be undiagnosed by the health system and contraindications to use can be printed on product packaging.
Potassium-enriched salt can be used at home and in commercial settings as a direct replacement for regular salt (sodium chloride) when seasoning, preserving or manufacturing foods. Importantly, while other salt reduction strategies make foods taste less salty, switching to potassium-enriched salt is undetectable by most people.
“Unwanted taste effects are the main reason why efforts to reduce salt intake have failed for more than two decades. The willingness of patients to keep using potassium-enriched salt removes that barrier, which is why it can be a game-changer,” Schutte added.
Barriers to uptake
Jennings said that while potassium-enriched salt substitutes could provide a simple solution, a shift in the food environment would be needed to fully realise the benefits.
“We would need to see low-sodium, potassium-enriched salts more widely available on supermarket shelves across the country, but they would also need to be affordable for most Australians.”
Another barrier to uptake has been concerns about causing elevated levels of potassium in the blood (hyperkalaemia) in people with advanced kidney disease.
Professor Bruce Neal, Executive Director at The George Institute Australia and Professor of Clinical Epidemiology at Imperial College London, said it is clear that patients with advanced kidney disease should not use potassium-enriched salts, but this applies to a very small proportion of the population, and these patients are already advised to avoid salt.
“No issues with serious harm from hyperkalaemia were recorded in any of the trials to date, though all were done in clinical settings. Our recommendation for use in hypertension is based on patients being managed by a healthcare worker. Healthcare workers know not to recommend potassium-enriched salt in the presence of kidney disease and risks for these patients can be avoided.”
The authors argued that given potassium-enriched salt substitution is one of the few dietary interventions patients comply with long-term, it is logical to at least consider the use of potassium-enriched salt for all those with hypertension.
“We strongly encourage clinical guideline bodies to review their recommendations about the use of potassium-enriched salt substitutes at the earliest opportunity — if the world switched from using regular salt to potassium-enriched it would prevent millions of strokes and heart attacks every year at very low cost,” Schutte said.


HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 53 CLINICAL SERVICES
iStock.com/Motortion

Enhancing IVF patient experience with AI
Reproductive health provider Virtus Health is deploying RingCentral MVP and RingCentral Contact Centre solutions at its facilities in Australia and Europe.
The NYSE-listed RingCentral provides AI-first global enterprise cloud communications, video, webinars, hybrid events and contact centre solutions. The company’s integrated and secure unified communications as a service (UCaaS) and contact centre as a
service (CCaaS) platform will assist Virtus in delivering personalised patient care, tailored to individual circumstances and needs.
Virtus will roll out these solutions over the next six months at its 62 fertility clinics, day hospitals, and diagnostics and pathology facilities.
While the deployment was initially planned to commence in Australia, the relocation of Virtus Health’s Complete Fertility Centre in the UK to a brand-new premises in Southampton presented the opportunity to pilot the RingCentral solution ahead of the Australian rollout. Once the solutions have been rolled out, Virtus is expecting significant savings annually in business communications costs.
The RingCentral platform will unify and consolidate Virtus’s telephony and contact centre functionality, providing high availability and reliability, visibility and reporting on all calls and voice traffic across the organisation, and the ability to manage call flows and queues centrally between the contact centre and individual sites. It is also a suitable platform to support Virtus Health’s hybrid working environment, and the integration of any future Australian and international acquisitions, according to the company.
The five-year contract includes the provision of devices and project services to design and deploy the integrated UCaaS and CCaaS environment for approximately 1700 employees and a centralised contact centre supporting staff and patients across 62 sites globally. The solution will be deployed over Virtus Health’s global SD-WAN, ensuring quality of service and optimised performance.
The RingCentral for Salesforce integration will ensure calls are routed to the appropriate clinics and teams, that patient information is readily accessible and Virtus can personalise the patient experience.
Shaun Thurling, Head of Information Technology, Virtus Health, said, “Reproductive health care, especially IVF, is a very personal journey and so patient experience is our most important outcome. RingCentral was the best fit to support our key patient care goals, providing the ideal solution for a seamless interconnection between our centralised contact centre and decentralised clinical environment.
“The recent success of our UK deployment has proven that and given us valuable insights to assist in the global deployment over the next four months. We look forward to the additional functionality and patient care capabilities we will gain through the initial rollout, as well as further innovations and integrations to be delivered by RingCentral over our five-year partnership,” Thurling said. John Poli, Industry Principal, Healthcare at RingCentral, said the company has established “a highly available platform with the level of security and data privacy that is meeting the needs of healthcare providers in Australia and around the world. I look forward to seeing Virtus Health become the industry benchmark in using communications technologies to support personalised patient care.”
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 54 TECHNOLOGY
iStock.com/Cinefootage Visuals
Stay a Step Ahead of Hidden Threats of Winter Infections

As the winter season looms, healthcare facilities brace themselves for heightened challenges in combating infectious diseases, especially the hidden threats posed by pathogens lurking on surfaces. GAMA Healthcare is proud to unveil the ‘Stay a Step Ahead’ of Winter Infections campaign, dedicated to equipping healthcare professionals with essential Infection Prevention and Control (IPC) knowledge and resources to effectively combat winter infections and ensure the safety of patients and residents.
At the core of our campaign lie three critical focus areas: surface decontamination, patient and resident hand hygiene, and antimicrobial resistance (AMR). These areas have been identified as pivotal in curbing infection transmission, mitigating the risk of healthcare associated infections (HAIs), and addressing the threat posed by hidden pathogens during the winter months.
Surface decontamination: In healthcare settings, stringent surface decontamination practices are paramount in preventing the spread of infections. High-touch surfaces such as bed rails, keyboards, and tables serve as breeding grounds for harmful pathogens, facilitating infection transmission. Inadequate room cleaning can elevate the risk of patients and residents being exposed to previous occupants’ microorganisms by up to 73%. Ensuring proper surface cleaning is critical to preventing infections. This IPC awareness campaign underscores the importance of
adhering to rigorous cleaning protocols and employing effective disinfectants to mitigate this risk effectively, emphasising the significance of maintaining hygienic environments in healthcare settings.
Patient and resident hand hygiene: Maintaining optimal hand hygiene among patients and residents is another cornerstone in breaking the chain of infection. Studies reveal that 39% of patients carry at least one pathogen on their hands, including formidable foes like rhinoviruses, Gramnegative and Gram-positive bacteria, and even hepatitis A.
Promoting and monitoring hand hygiene practices have been shown to substantially reduce HAI rates. Through a range of educational resources and initiatives, our campaign aims to raise awareness about the importance of proper hand hygiene practices, empowering healthcare professionals to advocate for and support these protocols among those under their care.
Antimicrobial resistance (AMR):
The emergence of antimicrobial resistance presents a formidable challenge to healthcare systems worldwide. Antibiotic misuse and overuse have fuelled the proliferation of resistant pathogens, rendering infections increasingly difficult to treat. By preventing HAIs, we can significantly curb the spread of resistant microbes. This campaign emphasizes the crucial role of implementing robust infection prevention strategies and surveillance measures to combat AMR
Wozniak, T. M., Dyda, A., Merlo, G., & Hall, L. (2022). Disease burden, associated mortality and economic impact of antimicrobial resistant infections in Australia. The Lancet Regional Health - Western Pacific, 27, 100521. https://www.thelancet.com/journals/ lanwpc/article/PIIS2666-6065(22)00136-5/fulltext
Loveday, H., Tingle, A., & Wilson, J. (2020). Using a multi-modal Strategy to Improve Patient Hand Hygiene. American Journal of Infection Control, 49(6). https://www.ajicjournal.org/article/S0196-6553(20)31064-6/fulltext
Carling, P. C., & Huang, S. S. (2013). Improving Healthcare Environmental Cleaning and Disinfection Current and Evolving Issues. Infection Control & Hospital Epidemiology, 34(5), 507–513. https://www.cambridge.org/core/journals/infection-control-andhospitalepidemiology/article/abs/improving-healthcare-environmental-cleaning-and-disinfectioncurrent-and-evolving-issues/14 9C7D943A348162ACAC18B69FC46225
and drive down infection rates. Statistics reveal that over 1,000 deaths in Australia are attributed to AMR-associated cases, primarily arising from resistant HAIs. Alongside other antimicrobial stewardship measures, employing appropriate disinfectants and techniques can effectively mitigate the risks of both HAIs and AMR. A comprehensive approach to address this pressing healthcare challenge is needed to safeguard patient wellbeing and healthcare sustainability.
FREE Infection Prevention Resources
As part of the ‘Stay a Step Ahead’ of Winter Infections, download educational resources and tools such as educational posters, articles, interactive crossword puzzles and more, all of which are designed to enhance knowledge and raise awareness of infection prevention practices.

Engage in IPC Knowledgesharing competition
Healthcare professionals are invited to participate in our IPC Hot Tips Competition, which provides a platform to raise awareness about hidden infection threats, patient and resident hand hygiene, and AMR management strategies. Share your insights and ideas for infection prevention for a chance to WIN.
Educational Webinar
To further support our IPC colleagues, we will be hosting a webinar on winter preparedness, providing valuable insights and strategies for combating winter infections effectively.


HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 55 » For more information visit www.gamahealthcare.com.au
SPONSORED CONTENT
iStock.com/fi lo
OIn Conversation
...with Sue Matthews, CEO of Royal Women’s Hospital
Amy Sarcevic

ne day, an hour after the final call for visitors to leave, Professor Sue Matthews — now CEO of Royal Women’s Hospital — found a man by his wife’s bedside in the gynaecology ward she was working at. After asking the man politely to leave, Matthews noticed he had tears in his eyes.
“My wife and I have just spent seven years and $35,000 trying to obtain the dream we just lost. You want me to leave her to grieve alone?” he said. It was in reference to the dilation and curettage procedure his wife had just endured following a miscarriage.
The moment struck an emotional chord with Matthews, who vowed from then onward to rethink the way women’s health is managed — both under her watch and in a broader, societal context.
“I will never forget it. What seemed like a simple procedure from a medical perspective was life-altering for the woman and her husband. I realised then that we had been doing things wrong for years, by asking the women’s partners to leave,” she said.
Since then — and following an extensive career in forensic sexual assault — Matthews has advocated passionately for the better treatment of women in the healthcare system.

She now sits on several committees, including the National Women’s Health Advisory Council and Victoria’s Women’s Health Advisory Committee, where she also chairs the Women’s Pain Inquiry.
In each role, she takes a stand against inequities in women’s health care. Medically, these include the 20–30% higher rates of misdiagnosis among women and the four additional years it takes for women to get diagnosed, relative to men.
Experientially, they include issues like medical gaslighting and pain minimisation.
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 56 IN CONVERSATION
Stigma, politicisation and research bias
When asked where these inequities stem from, Matthews points to historically biased practices within governments and medical research.
“We have seen recently, in the USA, how women’s health — in particular their sexual and reproductive health — is often politicised, in a way that men’s never is,” she said.
“We have also seen in our lifetime terms like ‘hysteria’ — which stems from the Greek word ‘uterus’ — being used as formal medical diagnoses.
“What’s less visible is the ongoing exclusion of women in medical trials. This is often justified on the basis of women’s hormonal volatility — but, in my view, this is the very reason women should be the focus of medical trials.”
Lessons hard-earned
Indeed, although 70% of the people who experience chronic pain are women, 80% of pain studies are conducted on men or male mice.
This has already seen catastrophic health outcomes for women.
In 2016, researchers noticed that a sleeping pill, widely prescribed in the USA, was
causing a spike in road accidents the morning after women had taken it.
The drug was being metabolised differently by women, but this side effect had been missed in the trial regime, given the exclusion of women participants.
Major health issues, like heart attacks, are also rarely considered through a woman’s lens.
“When we hear the term heart attack, we tend to conjure up an image of a person clutching their chest when, in reality, women can experience cardiac arrest very differently. For women, it often presents as indigestion, shoulder, neck or tooth pain,” Matthews said. A consequence of this is that women’s pain is often not taken as seriously, she added.
“Women presenting with pain can be perceived as hysterical and are more likely than men to be given antidepressants or antianxiety medication, instead of the treatment they actually require.”
Driving change
While Matthews is excited to see women’s health issues being taken more seriously over time, she says there is a way to go before they are given equal weight to men’s. To help drive this change, she is advocating

for the inclusion of women participants in all future medical research.
“This is one of the most impactful ways we can improve health equity for women,” she said.
“At the very least, the public should be made aware if a drug has been approved on the basis of male-only trials.”
However, her efforts do not stop at the broader, policy level.
Just this month, Matthews sent an email to key government leaders reporting that a national shortage in migraine medication would disproportionately affect women. She also works tirelessly to ensure that daily care at the Royal Women’s Hospital is delivered without bias or judgment.
“The reason we have a standalone women’s hospital is not just to provide four walls of care. It is to make sure we are adequately supporting the most vulnerable patients and advocating for health equity,” she said.
A mother to two girls and a grandmother to one, Matthews said her drive to improve health equity will never wane.
And, on days where she feels disheartened by the slow pace of change, she thinks back to that night on the gynaecology ward and remembers her ‘why’.
HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 57 IN CONVERSATION
iStock.com/Jorm Sangsorn
hospital readmission risks Technology to cut
A new study has found that virtual care technology can help improve the quality and sustainability of home-based acute care models.
The study, by Telstra Health and Mackay Hospital and Health Service (part of Queensland Health), analysed 151 adult and 26 paediatric patients admitted to the Mackay Hospital in the Home (MHITH) program between 1 August 2020 and 30 June 2021. All patients assessed used virtual care technology for the majority, or all, of their home-based acute care.
The study measured readmissions within 28 days, unplanned emergency department (ED) presentations, transfers-in to facility-based hospital beds and average length of stay among the patients.
Findings from the study showed use of virtual technology was associated with a statistically
significant reduction in risk of hospital readmission within 28 days — from 43% to 21%.
In addition, the risk of hospital readmission within 28 days for the same diagnosis-related group (DRG) dropped from 18% to 4%, and length of stay in hospital for the top three DRGs by volume decreased from a mean of 7.2 days to 4.0 days, saving the health provider an average of $3698 per admission.
Use of virtual care technology was also associated with reduced rates of unplanned ED presentations and transfers-in to traditional hospital beds compared to usual care for adults.
Vickie Irving, Head of Clinical Innovation & Effectiveness and Deputy Chief Health Officer
at Telstra Health, said, “We’re proud to provide one of Australia’s first evidence-based studies to show the beneficial impacts virtual care technology can have for both healthcare providers and patients — from cost savings to reducing the risk of hospital readmission.”
The study was co-authored by Cathie La Riviere, Manager Virtual Health at Mackay Hospital and Health Service; Judi Cavanagh, Program Officer at Mackay Hospital and Health Service; Vickie Irving, Head of Clinical Innovation & Effectiveness and Deputy Chief Health Officer at Telstra Health; James Brown, Commercial Strategy Manager at Telstra Health; and Brian Dorricott, former Head of Data Science at Telstra Health.
In 2020 Mackay Base Hospital implemented Telstra Health’s virtual care technology as part of the Care in the Right Setting Hospital in the Home (HiTH) program. Designed to deliver inpatient standard of care to patients at home, the program combines the use of virtual health monitoring devices and a dedicated patient app for recording vital signs and data with home visits and video consultations from the clinical team.
“Despite evidence that Hospital in the Home (HITH) models of care are a safe, reliable and cost-effective alternative to in-hospital care for suitable patients, we know there is suboptimal uptake in Australia,” Irving said.
“We wanted to assess the clinical and financial impacts of virtual care technology on HITH models of care. The statistically significant results in the study show clinical, economic and consumer benefits are associated with embedding virtual care technology in HITH service models. These important findings raise considerations for health systems facing capacity constraints and rising costs.”
The study has been published in the Asia Pacific Journal of Health Management

HOSPITAL + HEALTHCARE AUTUMN 2024 hospitalhealth.com.au 58 TECHNOLOGY
iStock.com/Willowpix








www.WFMedia.com.au/subscribe FREE to industry and business professionals The magazine you are reading is just one of 11 published by Westwick-Farrow Media. To receive your free subscription (magazine and eNewsletter), visit the link below.