September - October 2022










Wound care providers know the magnitude of the silent epidemic of chronic wounds. Globally, over 40 million people live with chronic wounds.1 In some countries, wound care accounts for 35 - 65% of post-acute care.2 Government spending in the United States through Medicare is estimated at $96 billion annually.3 Beyond the size of the problem, health care providers face many challenges in providing proactive, optimized wound care resulting in delayed wound healing, poorer outcomes and lower quality of life for patients with wounds.
Similar to many other industries, wound care has the opportunity to address these challenges with technology designed specifically for the needs of clinicians and patients. Solutions that provide easyto-use tools at the point of care across the healthcare continuum help empower clinicians of all skill levels to effectively manage their patients’ wounds.
The introduction of smartphones into clinical care enables easy correction of a core challenge of wound care, accurate measurement. Disposable paper rulers became an industry standard, and length and width are widely accepted as critical measures of wound healing. However, Rogers4 highlighted that wounds are not rectilinear, and using length and width for area calculation can lead to a 41% overestimation of wound sizes. Beyond the two-dimensional surface area, wounds also have depth. Smartphones now have high-quality cameras and increased computing capacity. AI-powered applications can conduct threedimensional analysis of the wound bed and identification of the deepest point.5 Submillimeter accuracy can be achieved considering the entire visible wound bed and reducing the variability between clinicians. The ability to map a wound again increases the potential to precisely assess the wound volume and closure over time. Wound closing by secondary intention requires tissue granulation at the base of the wound to occur, followed by eventual reepithelialization.6 Thus, the surface area may lag behind depth or wound volume measurements. Wound
Mr David Mannion Dr José L. RamírezGarcíaLunatime and their potential to lead to inappropriate treatment changes or failure to identify chronic wounds.
Figure 1: Kong et al. (2021) implemented an AI-powered digital wound management solution (Swift Medical Inc., Toronto) with remote patient monitoring to precisely measure wounds taken by clinicians and patients. Their results highlight how the use of a specialized wound imaging platform enabled the acquisition of images by the patient comparable to those taken by the healthcare provider while allowing him to be remotely monitored during the COVID-19 pandemic.10


Accurate assessment over time can be further complicated by variability among clinicians. Technology can make wound assessments more consistent by reducing confounding factors such as skills and subjective judgement. Digital area and temperature measurement are two specific examples of wound documentation subject to variations. Wound size is essential to overall wound healing, and temperature indicates potential infection or delayed wound healing.7 Temperature is frequently measured subjectively in practice using palpation, and some clinicians are slowly adopting thermometry. Thermometry uses a laser to measure the temperature of a single point objectively. In contrast, thermography uses a thermal camera to measure an image that can collect temperature measurements for thousands of points.8 Wang and colleagues evaluated variation in measurement of size and temperature between clinicians across 42 wounds using traditional methods of a paper ruler and smartphone-based digital planimetry (area measurement) and thermography.9 The smartphone-based planimetry had a higher intraclass correlation coefficient and, thus, reproducibility than paper-based measurement. The smartphone-based thermography was equal to the clinically accepted reference thermometer. A notable difference was that non-expert clinicians also had higher interrater reliability. Therefore, this technology may address challenges caused by continuity of care and low wound care education in entry-level health professionals.
Patient self-monitoring is another theme across healthcare, and wound care is no exception. As shown in Figure 1, a smartphone app that securely enabled patients to upload wound photos to their medical records during the pandemic was deployed in Canada.10 The artificial intelligence (AI)-powered wound care app was simplified for patient use and would automatically enhance image quality and complete measurements for easy review
“This technology may address challenges caused by continuity of care and low wound care education in entry-level health professionals.”Digitizing Wound Assessment: Unlocking the Potential of the
by the clinicians. Patients responded positively, noting it saved time and money for them and their caregivers. Using the app reduced the need for travel to the clinic, reduced missed time from work and avoided the necessity to seek informal caregiver support for children. The clinicians could identify early warning symptoms of infection and recall patients as needed. Following this theme, a scoping review found that telehealth for wound care was not inferior to in-person care,11 indicating that clinicians will continue to adopt these methods beyond the pandemic. Making it easier for any clinician or patient to better monitor the wound allows clinicians to rethink their procedures and how frequently to schedule return visits.
Specialized wound management systems can even improve the efficiency of seasoned clinicians in high-volume wound clinics. Well-designed digital solutions can improve the measurement, capturing a wound photo and documentation, meaning even highperforming wound centers have opportunities to optimize care. A study comparing paperbased ruler measurement to smartphonebased measurement found the digital method was 57% faster than manual methods.12 Furthermore, a recent study using an AIpowered smartphone app in a high-volume wound clinic demonstrated significant time savings compared to manual measurements and digital photography.13 The wound app was 77% faster than traditional paper ruler wound measurement, and in completing all steps of documentation, the AI-powered smartphone app saved 54% of the time. This efficiency applied to the wound clinic’s regular volumes and business schedule could save 21.8 - 51.7 days of a clinician’s time annually by adopting the app. This time presents opportunities for additional patient care in a clinicians’ day.
Adopting digital wound management solutions creates further opportunities for research and innovation in wound care by creating big data
sets. Information captured by digital wound assessment and saved to the patient’s record can be used to advance our understanding of wounds and is now beginning to be accepted by regulators (e.g., United States Food and Drug Administration) for coverage of treatments.14 Leveraging this real-world data requires appropriate methods, identifying useful sources, inclusion/ exclusion criteria, and relevant cohorts, data can be transformed into usable information for calculating end-point outcomes15. For example, a recent study used real-world data insights from over 1.5 million wounds and identified over 188,675 skin tears assessments to assess their prevalence in North America.16 This study was over ten times larger than any previously identified study, demonstrating the power of digitizing wound documentation and creating representative analyses. Furthermore, rich data such as wound photographs can be used to develop better assessment tools.
Artificial intelligence and machine learning (ML) offer new possibilities for advancing wound assessment. Changes in the different tissue types within the wound hint toward a healing wound but can be limited in utility by the knowledge, skill and experience of clinicians performing this assessment. AI is ideally suited to automatically identify tissue types and perform the task of quantifying the amount, which humans perform poorly. Even when clinicians know how to identify tissue types (e.g., granulation, eschar), humans cannot accurately identify the percentage of tissue type beyond a general estimate. AI can use an image to predict wound tissue composition pixel by pixel and provide highly accurate measurements. As an example of this, Ramachandram and colleagues17 demonstrated an AI tissue-typing (called AutoTissue) that achieved a high agreement compared to a panel of expert clinicians’ tissue ratings (Figure 2). Furthermore, this AI is designed to be deployed on a mobile app that runs on entry-
“Artificial intelligence and machine learning (ML) offer new possibilities for advancing wound assessment... AI can use an image to predict wound tissue composition pixel by pixel and provide highly accurate measurements.”
level smartphone models, therefore allowing it to be used seamlessly in clinical settings. This AI learned from thousands of wound images with labels for tissue types. The images had a wide variety of lighting conditions with diverse patient groups, reflecting the real world’s normal practices and ‘messy’ data. This type of model training results in a more robust prediction of tissue types than previous tools, which typically perform colour analyses that is trained on small data sets or in highly curated data sets. Wound tissues are not simply clear-cut red, black, or yellow. Instead, they are a mixture of cells often overlapping and presenting unique and complex patterns that AI can help analyze. Therefore, taking out the variability seen by clinicians’ assessments can improve documentation quality and, more importantly, increase the accuracy of wound assessment and prognostic scores that ultimately guide treatment.
More accurate wound healing prognostics are possible by leveraging big data available and objective wound assessments, such as AutoTissue. Gupta et al.18 used data from over 2.1 million wound evaluations to develop a model that identifies wounds at risk of delayed healing. Compared to commonly used wound scores such as the Pressure Ulcer Scale for Healing (PUSH) and Bates-Jensen Wound Assessment Tool (BWAT), their objective AI model performed better. Using advanced vision technology supports the concept of extracting objective information from wound imaging to help identify wounds that expert wound clinicians should review. Thus, AI-powered wound triage could identify hard-to-heal wounds, allowing wound specialists to be notified and assess wounds earlier if they change healing trajectory.

Embedding this AI in an app to be used across the continuum of care has significant benefits. Digitizing wound assessment and providing integrated AI tools empowers clinicians to work in new ways to optimize the entire health care team.
Another possibility for how wound care clinicians and teams organize themselves and achieve collective outcomes is the creation of collaborative digital wound records. One example is an inter-professional wound care team in Canada comprising ten home health provider organizations, eight hospitals and wound care centres. A regional health authority implemented a digital wound management solution to address chronic wounds in their population.19 The first phase of this project followed 248 patients that had chronic wounds. By continually monitoring the wounds for improvements using a smartphone app and escalating if no improvements were achieved in 14 days, the program attained a 3-month reduction in length of stay on home care, reduced emergency room visits by 7%, lowered readmission to home care by 50%, and savings of $1,000 (CAD) per patient per month. The savings resulted from decreased weekly visits and lower utilization of advanced wound care product spending. The wound care team reported that the digital wound management solution was intuitive, helped evaluate wound progress better, and supported better and faster decisions. Thus, it was concluded that a shared wound management tool could optimize clinician roles within and across organizations. Clinicians can quickly seek input when wounds are not progressing, and referral times can be decreased if rich standardized assessment documentation is captured in a shareable format.
Harnessing the power of digital wound assessment can translate to many positive outcomes. Home health can reduce hospitalization and less visit utilization per episode. In-patient settings can enable remote digital consultation models to provide prompt support from wound experts across their facilities. Clinicians can gain organizational support and funding by making the case through clinical and financial outcomes. Patients can be engaged in self-monitoring and self-care in the privacy of their own homes.
Digitizing Wound Assessment: Unlocking the Potential of the Wound Care TeamWound management solutions influence care beyond the initial assessment and achieve their highest potential using systems thinking. Clinicians need to understand the benefits of new digital tools in wound care to identify opportunities to supplement clinical skills and improve organizational outcomes.
The advancement of technology will continue to bring changes to wound care by challenging


and improving the methods of our current practice and developing new assessment capabilities. Over the past decades, different devices have come on the market, enriching the potential assessment of wounds. For example, bacterial fluoresces enables the ability to see microorganisms invisible to the human eye.20


Under violet light (405 nm) certain bacteria will fluoresce red or blue green
 Digitizing Wound Assessment: Unlocking the Potential of the Wound Care Team
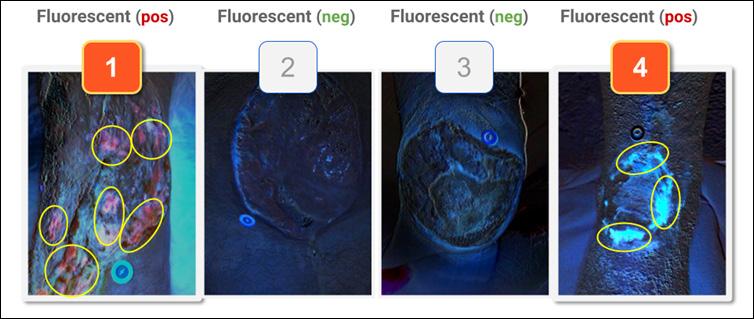
Figure 3: The diagnosis of infection is based on numerous considerations. Until recently, it has not been possible to ‘assess bacterial load’ at the point of care. 3a illustrates the typical visual scenario. 3b illustrates an Augmented visual assessment with bacterial fluorescence. The addition of bacterial fluorescent imaging to clinical signs and symptoms has been shown to outperform clinical signs and symptoms alone26. In a similar fashion, thermography provides an additional data point to aid in the determination of infection as illustrated in 3c and 3d.
Digitizing Wound Assessment: Unlocking the Potential of the Wound Care Team
Figure 3: The diagnosis of infection is based on numerous considerations. Until recently, it has not been possible to ‘assess bacterial load’ at the point of care. 3a illustrates the typical visual scenario. 3b illustrates an Augmented visual assessment with bacterial fluorescence. The addition of bacterial fluorescent imaging to clinical signs and symptoms has been shown to outperform clinical signs and symptoms alone26. In a similar fashion, thermography provides an additional data point to aid in the determination of infection as illustrated in 3c and 3d.
(See Figure 3). Thermography can reduce the subjective assessment of infection by human touch and give insights into areas of inflammation.21,22 Tissue oxygenation measurements of the skin show clinicians if the wound bed has sufficient perfusion.23,24 Moisture assessments can be an early indicator of pressure injury.25
Acquiring these technologies and seamlessly integrating them into practice seems out of reach due to the cost, multiple devices required that cost tens of thousands of dollars, and lack of interoperability. As technology develops, these medical imaging modalities are becoming integrated into wound management solutions in a form factor that can fit in your pocket.20 As illustrated in Figure 4, the ability to compare wound imaging modalities in seamless workflows will help advance assessment by clinicians. These changes bring the possibility of broad adoption of these advanced technology solutions.
1. Las Heras, K., Igartua, M., Santos-Vizcaino, E., & Hernandez, R. M. (2020). Chronic wounds: Current status, available strategies and emerging therapeutic solutions. Journal of Controlled Release, 328, 532–550. https://doi.org/10.1016/j.jconrel.2020.09.039
2. Welsh, L. (2018). Wound care evidence, knowledge and education amongst nurses: A semi-systematic literature review. International Wound Journal, 15(1), 53–61. https://doi. org/10.1111/iwj.12822
3. Vaughan, G., Prizeman, G., Eustace-Cook, J., & Byrne, G. (2021). Use of mHealth apps by nurses in the management of chronic wounds: A scoping review protocol. JBI Evidence Synthesis, 19(10), 2783–2789. https://doi.org/10.11124/JBIES-20-00401
4. Rogers LC, Bevilacqua NJ, Armstrong DG, Andros G. Digital planimetry results in more accurate wound measurements: a comparison to standard ruler measurements. J Diabetes Sci Technol. 2010 Jul 1;4(4):799-802. doi: 10.1177/193229681000400405. PMID: 20663440; PMCID: PMC2909508.
5. Lakdawalla, A., Phan, C., & Allport, J. (2020). Clinical Validation of Digital Wound Management as an Efficient Tool for Assessing and Monitoring True Wound Depth. 1. https://f. hubspotusercontent40.net/hubfs/2024649/+%20Conference%20Assets/SAWC%20-%20 AutoDepth.pdf
6. Beitz, J. M. (2022). Wound Healing. In L. L. McNichol, C. R. Ratliff, & S. S. Yates (Eds.), Wound, Ostomy, and Continence Nurses Society Core Curriculum: Wound Management (2nd ed., pp. 38–54). Wolters Kluwer.
7. Sibbald, R. G., Mufti, A., Armstrong, D. G., & Smart, H. (2021). Nontouch Infrared Skin Thermometry: An Underutilized Tool. Advances in Skin & Wound Care, 34(11), 614–615. https://doi.org/10.1097/01.ASW.0000795248.80980.89
8. Ramirez-GarciaLuna, J. L., Bartlett, R., Arriaga-Caballero, J. E., Fraser, R. D. J., & Saiko, G. (2022). Infrared Thermography in Wound Care, Surgery, and Sports Medicine: A Review. Frontiers in Physiology, 13, 838528. https://doi.org/10.3389/fphys.2022.838528
9. Wang SC, Anderson JAE, Evans R et al (2017) Point-of-care wound visioning technology: Reproducibility and accuracy of a wound measurement app. PLoS One 12(8): e0183139. https://doi.org/10.1371/journal.pone.0183139
10. Kong, L. Y., Ramirez-GarciaLuna, J. L., Fraser, R. D. J., & Wang, S. C. (2021). A 57-YearOld Man with Type 1 Diabetes Mellitus and a Chronic Foot Ulcer Successfully Managed with a Remote Patient-Facing Wound Care Smartphone Application. American Journal of Case Reports, 22. https://doi.org/10.12659/AJCR.933879
11. Kostovich, C. T., Etingen, B., Wirth, M., Patrianakos, J., Kartje, R., Baharestani, M., & Weaver, F. M. (2022). Outcomes of Telehealth for Wound Care: A Scoping Review. Advances in Skin & Wound Care, 35(7), 394–403. https://doi.org/10.1097/01.ASW.0000821916.26355.fa
12. Au, Y., Beland, B., Anderson, J. A. E., Sasseville, D., & Wang, S. C. (2019). Time-Saving Comparison of Wound Measurement Between the Ruler Method and the Swift Skin and Wound App. Journal of Cutaneous Medicine and Surgery, 23(2), 226–228. https://doi. org/10.1177/1203475418800942
13. Mohammed, H. T., Bartlett, R. L., Babb, D., Fraser, R. D. J., & Mannion, D. (2022). A time motion study of manual versus artificial intelligence methods for wound assessment. PLOS ONE, 17(7), e0271742. https://doi.org/10.1371/journal.pone.0271742
14. Fife, C. E., & Eckert, K. A. (2017). Harnessing electronic healthcare data for wound care research: Standards for reporting observational registry data obtained directly from electronic health records: Standards for reporting observational data from electronic health records. Wound Repair and Regeneration, 25(2), 192–209. https://doi.org/10/f99qmb
15. Madu, T. (2021). Conducting meaningful real-world data analysis in wound care—A guide. Journal of Wound Care, 30(2), 93–94. https://doi.org/10/gn7ksq
16. Fraser, R. D. J., Gupta, R., & Mohammed, H. T. (2022). Analysis of real-world data from North American skilled nursing facilities’ skin and wound records for skin tear prevalence, healing and treatment. Journal of Wound Management, 13.
17. Ramachandram, D., Ramirez-GarciaLuna, J. L., Fraser, R. D. J., Martínez-Jiménez, M. A., Arriaga-Caballero, J. E., & Allport, J. (2022). Fully Automated Wound Tissue Segmentation Using Deep Learning on Mobile Devices: Cohort Study. JMIR MHealth and UHealth, 10(4), e36977. https://doi.org/10.2196/36977
Digitization and technological advancement will continue to transform the standard of care for wound assessment. Technology is a tool to empower clinicians to perform assessments that maximize the scope of practice and potential of their wound care team. Healthcare organizations face increasing pressures. Technology needs to be integrated into their medical records and designed with empathy for the needs of clinicians and patients. Adopting digital tools into clinical practice will provide deeper insights into wound healing and help health care providers address the global burden of chronic wounds. The world has moved into the digital age. It is time for wound care teams to move there as well.
18. Gupta, R., Goldstone, L., Eisen, S., Ramachandram, D., Cassata, A., Fraser, R. D. J., Ramirez-GarciaLuna, J. L., Bartlett, R., & Allport, J. (2022). Towards an AI-based Objective Prognostic Model for Quantifying Wound Healing [Preprint]. https://doi.org/10.36227/techrxiv.21067261.v1
19. Barker, M., Perron, M., Parrott, W., & Fraser, R. D. J. (2021). Interprofessional Virtual Wound Care Impact in an Integrated Health Care System during COVID-19. https://doi.org/10/gn9nbr
20. Ramírez-GarcíaLuna, J. L., Martínez-Jiménez, M. A., Bartlett, R., Wang, S. C., Fraser, R. D. J., Saiko, G., & Gergory C Berry. (2022). Is My Wound Infected? https://doi.org/10.13140/RG.2.2.17235.66088
21. Chanmugam, A., Langemo, D., Thomason, K., Haan, J., Altenburger, E. A., Tippett, A., Henderson, L., & Zortman, T. A. (2017). Relative Temperature Maximum in Wound Infection and Inflammation as Compared with a Control Subject Using Long-Wave Infrared Thermography. Advances in Skin & Wound Care, 30(9), 406–414. https://doi.org/10.1097/01.ASW.0000522161.13573.62
22. Lin, Y.-H., Chen, Y.-C., Cheng, K.-S., Yu, P.-J., Wang, J.-L., & Ko, N.-Y. (2021). Higher Periwound Temperature Associated with Wound Healing of Pressure Ulcers Detected by Infrared Thermography. Journal of Clinical Medicine, 10(13), 2883. https://doi.org/10.3390/jcm10132883
23. Lee, L.-L., & Chen, S.-L. (2022). Assessment of Hyperspectral Imaging in Pressure Injury Healing. Advances in Skin & Wound Care, 35(8), 429–434. https://doi.org/10.1097/01. ASW.0000831888.39420.a6
24. Saiko, G., Lombardi, P., Au, Y., Queen, D., Armstrong, D., & Harding, K. (2020). Hyperspectral imaging in wound care: A systematic review. International Wound Journal, 17(6), 1840–1856. https://doi.org/10.1111/ iwj.13474
Serena, T. E., Harrell, K., Serena, L., & Yaakov, R. A. (2019). Real-time bacterial fluorescence imaging accurately identifies wounds with moderateto-heavy bacterial burden. Journal of Wound Care, 28(6), 346–357. https://doi. org/10.12968/jowc.2019.28.6.346
25. Moore, Z., McEvoy, N. L., Avsar, P., Byrne, S., Vitoriano Budri, A. M., Nugent, L., O’Connor, T., Curley, G., & Patton, D. (2022). Measuring subepidermal moisture to detect early pressure ulcer development: A systematic review. Journal of Wound Care, 31(8), 634–647. https://doi. org/10.12968/jowc.2022.31.8.634
26. Serena, T. E., Harrell, K., Serena, L., & Yaakov, R. A. (2019). Real-time bacterial fluorescence imaging accurately identifies wounds with moderateto-heavy bacterial burden. Journal of Wound Care, 28(6), 346–357. https://doi. org/10.12968/jowc.2019.28.6.346
27. Ramírez-GarcíaLuna, J. L., Fraser, R. D. J., Bartlett, R., Saiko, G., Wang, S. C., & Berry, G. K. (2022). Infrared Thermal Imaging: A New Paradigm For Wound Care. https://doi.org/10.13140/RG.2.2.19985.30560