December - January 2023


December - January 2023

This Masterclass Guide is a concise overview aimed at exploring the use of Omeza® treatments and incorporating this into your clinical practice.
Wound healing is optimized by utilizing therapies that control bacterial burden, decrease tissue inflammation, support the extracellular matrix and establish a balanced healing environment.
Omeza® products are oil-based and contain no water (anhydrous). They were created to address the pathophysiologies associated with the development of chronic wounds.
■ All Omeza® products contain an anhydrous formulation of Omega-3, 6 and 9 oils designed to deliver nutrients for balanced wound healing
■ The Omeza® Lidocaine Lavage is a topical analgesic periwound prep designed to help manage debris and biofilm and reduce irritation
■ The Omeza® Collagen Matrix is a drug-device combination product comprised of hydrolyzed fish collagen, infused with cod liver oil and other plant derived oils

■ The Omeza® Skin Protectant is designed to help strengthen fragile skin, reduce inflammation, and promote remodeling when used daily on intact skin
■ Wound healing
■ Bacterial contamination
■ Diabetic foot ulcer
■ Venous leg ulcer
■ Omega fatty acids
■ Anti Inflammatory
■ Wound
■ Pressure Ulcer
■ Periwound
■ Anti-inflammatory
■ A drug-delivery device that delivers hydrolyzed fish collagen infused with cod liver oil, as well as other nutrients into the wound bed
■ When applied to a warm wound bed it softens, migrating into tunnels and crevices and conforming to the irregular wound topography
■ It is designed to promote the natural wound healing process via a bio-compatible structure that is naturally incorporated into the wound bed
Reduces pain and irritation
Strengthen and protect skin
• Always handle Omeza® Collagen Matrix using aseptic techniques
• Only content is sterile
• Prior to application of Omeza® Collagen Matrix, prepare the wound bed using standard methods to ensure wound is free of debris and necrotic tissue
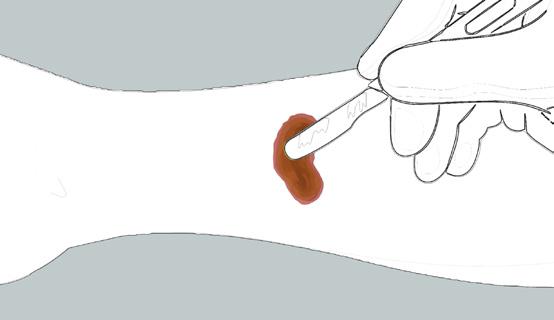
• Snap or cut open the tip of the Omeza® Collagen Matrix vial
• Slowly squeeze vial to apply directly to wound bed in stripes, or onto a suitable applicator (e.g. a tongue depressor)
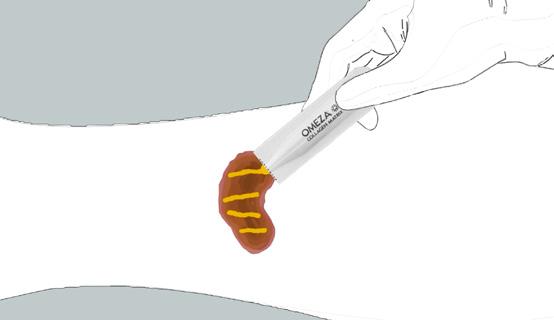
• After application, cover with the appropriate dressing to maintain matrix adherence and protect the wound area
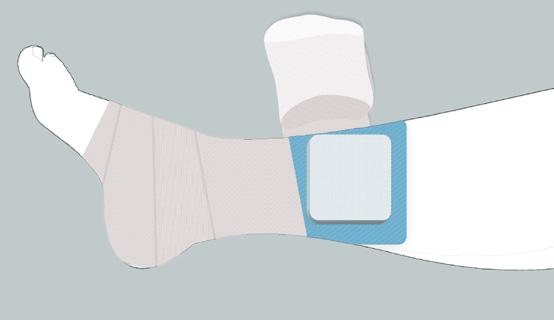
• The optimum dressing is determined by wound location, size, depth, and volume of exudate
■ Low dose of rapidly absorbing lidocaine reduces pain and irritation to aid in patient experience
■ Anhydrous formula designed to help inhibit growth of microorganisms
■ Peri wound prep oil rich in omegas known to decrease inflammation
■ Designed to improve skin elasticity and turgor of vulnerable skin
■ Soothing gel formula rich in omegas known to decrease inflammation
■ Designed to provide a low perfusion pulse during each application
Wounds That Are Suitable (Omeza® Collagen Matrix)


■ Partial, full-thickness wounds

■ Pressure ulcers
■ Venous ulcers








■ Diabetic ulcers
■ Chronic vascular ulcers
Wounds
Are Not Suitable (Omeza® Collagen Matrix)
■ Undermined wounds
■ Surgical wounds
■ Trauma wounds
■ Draining wounds
■ Known sensitivity to fish collagen or cod liver oil
■ Third degree burns


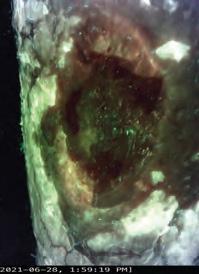
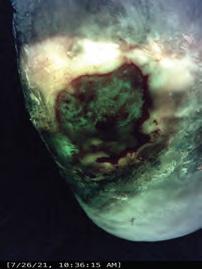
A case series to evaluate Omeza® products in combination therapy for the treatment of lower extremity ulcers of mixed etiologies exhibiting bacterial contamination as determined by a novel violet-light camera system and correlating biomarkers. Fluorescence images were acquired to assess the presence of bacteria at moderateto-heavy loads. Fluorescence imaging was implemented into the assessment to determine appropriate debridement level and location based on bacterial fluorescence signals.
The challenge of hard-to-heal wounds are a significant burden on the patient and the healthcare system. Omega-based wound treatments offer a treatment option for the management of partial, full-thickness wounds; pressure ulcers, venous ulcers; diabetic ulcers, chronic vascular ulcers; undermined wounds, surgical wounds; trauma wounds, and draining wounds.
A summary of the evidence of this innovative wound therapy is below.
■ A pilot study was conducted by Seo et al., into the Antibacterial Activity of Topical Fatty Acids
■ An ex vivo porcine skin explant model was used to establish a functional S. aureus biofilm for 5 days. The wounds were then treated with either an oil or with moistened gauze. The wounds were re-treated daily with either oil or more saline. Six explants per day from each group were harvested and viable total bioburden and biofilm were assessed
■ After the initial results, the experiment was run again with the added step of first soaking the explant in phosphate buffered saline with 0.05% Tween® 20 in order to see if the oil was masking the bacteria
■ At Day 0, the average bioburden was 4.8 log10 CFU/ml with 3.64 log10 CFU/ml of biofilm. After Day 1, total bacterial levels in the oil treated sample were reduced to 1.8 log10 CFU/ml while the control increased to 9.0 log10 CFU/ml. The levels of the oil-treated samples remained low and the control remained high every day thereafter
■ The results show the potential for a nutritive pro-healing oil to also have an antibacterial activity1
■ A 54-year-old male presented with a five-month history of Venous Leg Ulcer (VLU) to the left lower extremity

■ An omega-based protocol focused on wound and periwound preparation and care (protocol listed) performed once weekly
■ Pain and necessity for narcotic analgesics rapidly resolved.
■ Wound resolution was achieved at 11 weeks
■ The use of an omega-based complete care protocol resulted in expedited resolution of a chronic venous leg ulceration in a patient that had failed other advanced treatment modalities5,6,7,8,9,10,11,12
■ This patient (Figure 4) presented to the wound clinic with a hard-to-heal ulcer which has been present for four months, prior to commencing Omeza® therapy. The patient has a diabetic foot ulcer and Charcot foot arthropathy



Charcot foot (Charcot arthropathy) is a serious condition affecting diabetic foot patients. Diabetic Charcot foot occurs in people who have neuropathy and an injury occurs which causes the bone to fracture or dislocate in the foot. Often the injury occurs without the knowledge of the patient. The symptoms that occur include swelling, heat, and occasionally some redness to the foot. Some patients experience some pain while some patients experience no pain at all.
■ At commencement of Omeza® therapy his ulcer measured 3.0cm x 1.0cm and 0.2cm. Within 8 weeks of weekly therapy with Omeza® products he was completely healed
Biofilm Study Venous Leg Ulcer Study Diabetic Foot Ulcer with Charcot Foot■ No preparation needed
■ Easy to apply - snap and squeeze
■ Readily available for patients
■ Easy to store
■ Increases practice efficiency
■ Off-the-shelf, single use vials
“After 37 years of wound care experience, having tried everything in a wound care center setting I can only suggest... drop what you are using and try Omeza. The results are astounding. The simplicity of application and alleviation of patient responsibility cannot be overstated. Recommend highly!”
Dr Gregory A Black, DPM Sylvania, OH Sylvania Podiatry
“I went into our case study looking to improve skin and wounds on long term, “non-healable” patients that reside in nursing homes my company serves. The response to the Omeza treatment protocol was greater than expected and healed 3 wounds that were present for greater than a year without having to change the behavior of the patient or the facility. I also introduced it to my clinic and some skeptical nurses are now demanding it for our tough stasis dermatitis patients.”
Carmen Hudson, MD, FACS, CWSP Medical Director – United Wound Healing
References
1. Seo S, Jeong S, Gibson DJ. A pilot study of the antibacterial activity of topical fatty acids. Poster presented at the Symposium on Advanced Wound Care Spring/Wound Healing Society meeting. San Antonio, TX. May 7–11, 2019.
2. Laboratory testing University of Florida. Data on file.
3. Independent clinical and consumer use testing performed by Princeton Consumer Research. Data on file.
4. Independent testing performed by Augustine Scientific. Data on file
5. Mostow EN, et al; OASIS Venus Ulcer Study Group. Effectiveness of an extracellular matrix graft (OASIS Wound Matrix) in the treatment of chronic leg ulcers: a randomized clinical trial. J Vasc Surg. 2005 May;41(5):837-43.
6. Raffetto JD, et al; Why Venous Leg Ulcers Have Difficulty Healing: Overview on Pathophysiology, ClinicaConsequences, and Treatment. J Clin Med. 2020 Dec 24;10(1):29.
7. Calistru AM, Baudrier T, Gonçalves L, Azevedo F. Thrombophilia in venous leg ulcers: a comparative study in early and later onset. Indian J Dermatol Venereol Leprol. 2012 May-Jun;78(3):406.
8. Zutt M, et al; Thrombophilia in patients with chronic venous leg ulcers-a study on patients with or without post-thrombotic syndrome. J Eur Acad Dermatol Venereol. 2011 Dec;25(12):1432-9.
9. Mackenzie RK, Ludlam CA, Ruckley CV, Allan PL, Burns P, Bradbury AW. The prevalence of thrombophilia in patients with chronic venous leg ulceration. J Vasc Surg. 2002 Apr;35(4):718-22.
10. Falanga V, Sabolinski M. A bilayered living skin construct (APLIGRAF) accelerates complete closure of hard-to-heal venous ulcers. Wound Repair Regen. 1999 Jul-Aug;7(4):201-7.
11. Jia YC, Qiu S, Xu J, Kang QL, Chai YM. Docosahexaenoic Acid Improves Diabetic Wound Healing in a Rat Model by Restoring Impaired Plasticity of Macrophage Progenitor Cells. Plast Reconstr Surg. 2020 May;145(5):942e-950e.
12. Babaei S, et al; Omegaven Improves Skin Morphometric Indices in Diabetic Rat Model Wound Healing. J Am Coll Clin Wound Spec. 2018 Apr 28;9(1-3):39-45
Useful Links
Use
QR code for more information about Omeza® treatments

Click here to request more information from
How
