Offloading: The Comprehensive Guide
Editorial Summary
implication. Early detection and active management can delay or even prevent the onset of adverse outcomes. Protocols reflect the need for regular foot evaluations in every diabetic patient should have foot evaluation at yearly intervals. The cornerstone of the management are a multidisciplinary approach to prevention, including prevention of infection, appropriate wound care and management of non-viable tissue, and pressure reduction. The Triad of peripheral neuropathy, foot deformity and minor trauma have been found as risk factors in majority of cases of diabetic foot ulcers. Offloading the affected foot is a pivotal management strategy dispersing pressure away from the affected part. This article provides a concise overview of a variety of offloading techniques and their pros and cons.
Introduction
In patients with diabetes, 12-25% develop a diabetic foot ulceration (DFU) in their lifetime. This is a leading cause of diabetesrelated hospitalization and non-traumatic lower extremity amputation. DFU’s may lead to an increase in global morbidity, mortality, healthcare costs from hospitalizations, surgical and nonsurgical interventions, and amputations. Excessive pressure contributes delayed healing in up to 94% of these ulcerations. Pressure offloading can arguably be the most important principle implemented in treating diabetic foot ulcerations.1,2,3,4,5
Offloading Around the World
There are many different offloading techniques used around the world. Although Total contact casting (TCC) is the gold standard for offloading, it requires resources that may not be available in various countries. Fortunately, physicians are innovative and resourceful when it comes to caring for their patients and alternatives have been found.
Bohler Iron Walking Cast
Dr Lee Rogers
Chief-Podiatric Services, UT Health San Antonio
President, American Board of Podiatric Medicine
Associate Editor, Journal of The American Podiatric Medical Association San Antonio TX, United States
In India, the Bohler iron walking cast has been discussed in recent literature as a more effective offloading method because the entire plantar surface is off the ground. In this method, a lower leg cast is applied followed by an iron rod with a plantar platform. The iron rod is then applied with a clamp proximally and secured with more casting material. A modification is also utilized with roads and a distally placed hinge, to allow for a posterior platform for heel ulcerations.6


Mandakini Offloading System
The Mandakini offloading system is also discussed in Indian literature as an effective and cost-effective offloading technique. First, a pair of gloves is rolled together. The number of gloves used is dependent on the patient size. The gloves are then placed in an adhesive dynoplast, which is then applied to the foot. For distal lesions, it is applied proximally, and for rearfoot lesions, it is applied distal to the lesion. The device is then secured with a dressing. This technique is recommended to be changed every week for 4-6 weeks and authors noted complete healing without patient complaints with over 2 years of regular uses of the technique.7

48 Wound
- Vol 1 - December 2022
Masterclass
Foot complications are one of the most serious and debilitating consequences of Diabetes Mellitus. With global predictions of the number of diabetic patients near doubling by 2030, this condition is likely to be at the forefront of our clinical caseload. Aside from the morbidity and global healthcare burden in a diabetic patient with foot ulcers and amputations there is a significant financial
Figure 1: Bohler Iron Walking Cast. 6
Figure 2: Mandakini Offloading System. 31
© Copyright. Wound Masterclass. 2023 Images available from open access article: Venkatakrishnan S, Zachariah K, et al. A Description of a Modified Bohler Iron Walking Cast in the Management of Plantar Ulcers. J Foot Ankle Surg (Asia-Pacific) 2019;6(1):10–12. Images available from open access article: Kari SV. The economical way to off-load diabetic foot ulcers [Mandakini off-loading device]. Indian Surg. 2010 Apr;72(2):133-4. doi: 10.1007/s12262-010-0042-3. Epub 2010 Jul 1. PMID: 23133224; PMCID: PMC3452512.
The Samadhan Offloading System
The Samadhan is another instant offloading technique discussed in Indian literature. It is described as easy to apply, affordable, and effective. In this technique, the foam is painted with an adhesive liquid and rolled into a cylinder. The cylinder is then cut to fit the size of the ulcer and is applied proximal to the ulcer. The cylinder is then secured with coban or other dressing materials. In oral abstracts, this technique allowed for 73% healing compared to 13% in footwear. This technique can also be used with the patient’s footwear, as demonstrated in the picture.8





The Suvidha Offloading System
For the Suvidha system, the Gamgee pad pillows are applied first. The Gamgee pad is made of foam and folded in the shape of a “pillow” with a 2.5cm thickness and 1cm wound overlap. Paper tape is then used to wrap the “pillow”. This is done 2-3 times to make individual offloading components. The pillows are then placed around the wound with overlapping of 2cm at each junction. This is then secured using paper tape. Elastic plaster is then used to secure the pillows with 5cm of overlap. An elastic bandage is then used for additional security. A small prospective study examined this technique and found a 2-week healing time for 1x1cm hallux ulcerations and 12 weeks for 4x4cm midfoot ulcerations. Patients had high satisfactions with this technique. Overall, authors concluded that the Suvidha offloading footwear is a cost effective, easily replicable, and efficient dressing requiring only the readily available dressing materials. The results were thought to be comparable with other methods of offloading practiced worldwide.9



Offloading: The Comprehensive Guide Wound Masterclass - Vol 1 - December 2022 49
“Overall, authors concluded that the Suvidha offloading footwear is a cost effective, easily replicable, and efficient dressing requiring only the readily available dressing materials.”
Figure 3: Samadhan Offloading System. 8
© Copyright. Wound Masterclass. 2023 Images available from open access article: Shankhdhar LK, Shankhdhar K, Shankhdhar U, Shankhdhar S (2016) Instant Offloading of a Diabetic Foot Ulcer. Clin Res Foot Ankle 4:207. doi: 10.4172/2329-910X.1000207. Images available from open access article: Bhat, Sunay & Vinoth, D.. (2020). Studying the impact of the cost-effective Suvidha off-loading dressing in healing neuropathic ulcers in diabetic foot: a case series of 83 cases from South India. International Surgery Journal. 7. 2371. 10.18203/2349-2902.isj20202851.
Figure 4: Suvidha Offloading System. 9
The Importance of Offloading
So, with limited materials, increased clinic time, and other considerations, why is offloading so important? Here, we can see what havoc can occur when offloading isn’t a part of patient care. New ulcerations can develop. These new ulcerations or chronic ulcerations are always at risk for infection and/or amputation. If offloading isn’t implemented with every ulceration care plan, our patients are at an increased risk for morbidity and mortality.

Offloading Consensus
The International Working Group (IWGDF) on the Diabetic Foot has published evidencebased guidelines on the prevention and management of diabetic foot disease since 1999. In 2019, the IWGDF published a list of guidelines specifically for the offloading of the active diabetic foot ulcer.11


First Line of Offloading
The Science Behind Offloading
The thought behind offloading is to relieve the abnormal stresses that the foot experiences from the loss of protective sensation and biomechanical malfunction. The combination of loss of protective sensation and elevated mechanical stress can lead to tissue damage. The mechanical stress is thought to be due to increased compressive, frictional, and shearing forces during the gait cycle, causing repetitive microtrauma. This is the mechanism that is thought to cause many diabetic foot ulcerations. So, the goal of offloading is to distribute pressure away from the area of ulceration or pre-ulceration.10
The first recommendation from the IWGDF for a diabetic patient with a neuropathic forefoot or midfoot ulceration is the use of a nonremovable, knee-high offloading device with appropriate foot to device interface, such as TCC and nonremovable knee-high walking boots. When comparing these two non-removable devices, one study found that plantar pressure had greater reduction in a nonremovable knee-high walker device compared to the total contact cast. The total contact cast reduced forefoot ulcer pressures 84% whereas the nonremovable knee-high walker devices reduced the pressure by 92%. In the midfoot, nonremovable kneehigh walker devices reduced pressure by 77% compared to the 63% in the total contact cast. However, literature comparing these two nonremovable devices is limited.11

Offloading: The Comprehensive Guide 50 Wound Masterclass - Vol 1 - December 2022
“If offloading isn’t implemented with every ulceration care plan, our patients are at an increased risk for morbidity and mortality.”
Figure 5a: New ulceration. 5b: Infection. 5c: Amputation.
5a 5b 5c © Copyright. Wound Masterclass. 2023
Figure 6: A Non-Removable, Knee-High Offloading Device with an Appropriate Foot to Device Interface.
Total Contact Casting
Total contact casts are the gold standard for offloading, and they were first developed for leprosy patients by Dr. Paul Brand. They are indicated for forefoot and midfoot plantar ulcerations and early Charcot immobilization. For offloading Charcot patients, the TCC was recommended for an average immobilization time of 4 months in recent literature with cast changes approximately every 14 days. Unfortunately, there are some contraindications to TCC’s, which have also been applied to nonremovable devices. Ischemia, heavy exudating ulcers, infection, and patient intolerance are considered contraindications for non-removable offloading devices. Additionally, caution should be used in bedridden patients and patients with peripheral artery disease. In bedridden patients, caution is used as total contact casts can transfer pressure to the heel and could cause more harm and potentially limb-threatening situations. In patients with peripheral vascular disease, it is typically cautioned that the patient should have palpable or dopplerable pedal pulses prior to cast application. However, one systematic review did find that an ankle-brachial index of greater than 0.55 is considered acceptable to total contact cast consideration.

Finally, adjunct procedures to total contact casting have been noted to be effective in reduce time to healing. Achilles lengthening in combination with total contact casting has been shown to rapidly increase healing in forefoot ulcers and lead to a 2-fold decrease in recurrence.12,13,14,15,16
What Does a TCC Do?
TCCs have been shown to bear approximately 30% of the plantar pressure load and are aimed to redistribute these pressures on the foot. The cast is also designed to have increased padding, which creates a cavern for the foot to sit in and allow for less pressure to prominent areas. Additionally, TCCs can be cumbersome, which can decrease walking, stride length, and ultimately reduce the forces applied to the foot.17,18,19,20
Examining the Gold Standard Offloading Effects on Foot Areas
Because patients can ambulate in TCCs, it is important to know the benefit of TCCs in each area of the foot. Overall, TCCs lead to an 8492% reduction in plantar pressures. If this is broken down into the individual areas of the foot, there is a 32% reduction at the 5th MPJ, a 63% reduction at the 4th MPJ, a 69% reduction at the 1st MPJ. There is a 65% reduction of pressure at the hallux, and 45% reduction at the heel. However, as previously stated, pressure reduction at the heel is debated within the literature.21,22,23,24
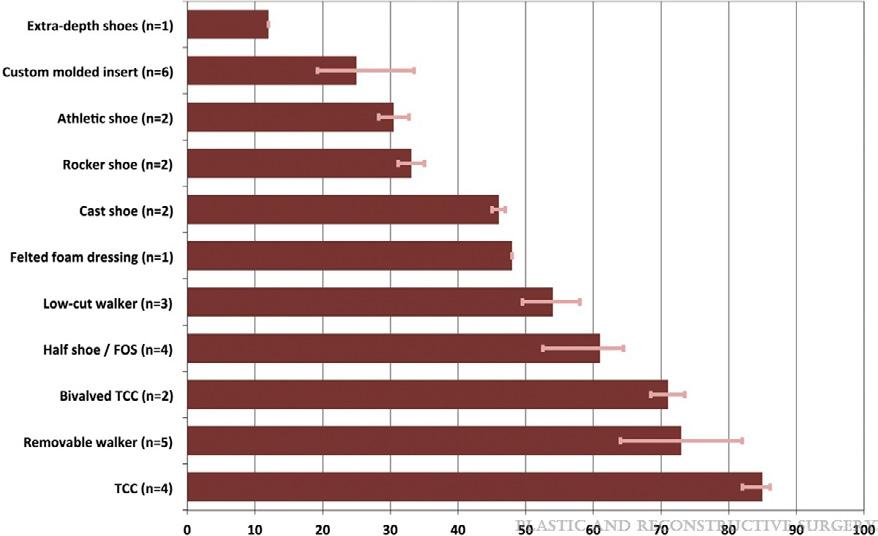
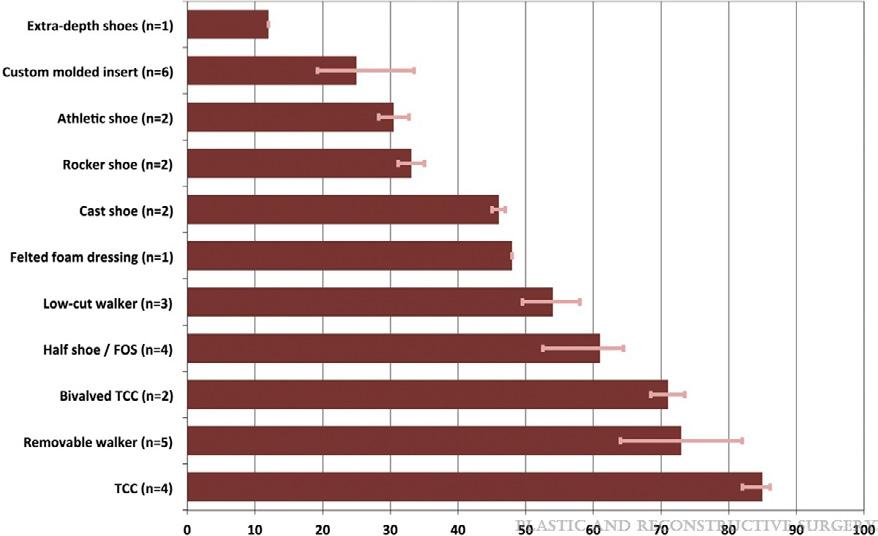
Percentage Offloaded at Ulcer Site
In a literature review, Bus examined the offloading capacities for various devices based on the patient’s peak plantar pressures. He found that total contact cases had the highest average of offloading power by having the highest peak pressure reduction percentage (87%), followed by removable devices, and so on down the line. It was noted that nonischemic, noninfected ulcerations should heal within 6-8 weeks with proper offloading and wound care.25
Non-removable Device Cautions
When assessing if a patient is a good candidate for a non-removable offloading device, it is important to consider a few patient aspects. Even though complication rates are noted to be around 5% in literature, clinical judgement and evaluation is needed to minimize any risk of
Offloading: The Comprehensive Guide Wound Masterclass - Vol 1 - December 2022 51
“Achilles lengthening in combination with total contact casting has been shown to rapidly increase healing in forefoot ulcers and lead to a 2-fold decrease in recurrence.”
12,13,14,15,16
65% 32% 64% 69% 45%
© Copyright. Wound Masterclass. 2023
Figure 7: Offloading Effects on Foot Areas.
complication to the patient. Complications were noted to be 1.55 times higher in patients with a BMI of 30 kg/m2 or more, 1.27 times higher in patients with moderate glycemic control, and 1.48 times higher in patients with poor glycemic control.
One of the main concerns for diabetic patients is their increased fall risk and gait alterations. Due to the neuropathy, their proprioception and muscle strength are altered. This can lead to mediolateral instability, especially in the ankle, and falls. Studies have also shown gait alterations with unilateral offloading in diabetic patients leading to slower gait, unsteadiness, limp, and decreased stride length. So, patients with peripheral neuropathy may need gait training or a contralateral shoe lift if a total contact cast or non-removable weightbearing device is being considered. Total contact casts and non-removable devices can also cause proximal joint pain or new ulcerations due to rubbing and different force distributions. Finally, some patients may not want a nonremovable device. This may be due to several different factors such as scratches from the device, anxiety, general intolerance, etc. For any number of reasons, the patient can simply prefer to have a removable device over a nonremovable device.26,27,28,29
How Do TCC’s Work?
They act as an exoskeleton, removing plantar pressure and transferring it to the tibia. They immobilize the ankle, reducing the plantarflexory forces at the midfoot and forefoot. TCC’s reduce the contact time of the affected foot on the ground. They’re irremovable, forcing adherence and also cumbersome and cause patients to take fewer steps per day.

Total Contact Cast Applications
Total contact casting (TCC) is a bespoke
designed cast which as its mechanism works by taking the weight off the foot (off-loading) in patients with diabetic foot ulcers (DFUs). Reducing pressure on the wound by taking weight off the foot has proven to be very effective in DFU treatment. Since the 1960’s TCC has been used for offloading DFUs in the US, with many clinicians regarding it as the "reference standard" for off-loading the sole of the foot.
The general principles of total contact cast application include minimal amount of padding should be used on the leg, a single layer of cotton padding is sufficient during application. Folds and creases should be avoided in the stockinette to avoid sources of friction. Bony prominences should also be well padded to avoid any friction or unwanted pressure. Padding can be added between the toes to avoid rubbing of the digits and toe caps can be used to avoid friction on toes in casts. And finally, the duration of the cast should be determined by patient characteristics, such as wound characteristics, patient activity level, etc. could determine if a patient needs a cast change sooner versus later. Typically, the initial cast is changed in approximately 3 days of its application. This is to ensure that no issues are arising, as there is a high potential for reduced oedema or change in limb shape. Total contact casts are then typically changed every 1-2 weeks to monitor the wound and managed swelling.27

Offloading: The Comprehensive Guide 52 Wound Masterclass - Vol 1 - December 2022
“One of the main concerns for diabetic patients is their increased fall risk and gait alterations. Due to the neuropathy, their proprioception and muscle strength are altered. This can lead to mediolateral instability, especially in the ankle, and falls.”
© Copyright. Wound Masterclass. 2023
Figure 8: How do TCCs work?
Second Line of Offloading
If a patient does not qualify or does not tolerate a non-removable offloading device, a removable knee-high device with an appropriate foot to device interface is recommended as the second line choice of treatment. Some studies found that this device is effective because of the reduced walking done in these devices and that the removable offloading device should distribute the peak pressures in a very similar fashion to the non-removable devices. However, one caveat is that patients are to ideally to wear the device constantly and rarely off the devices. One study found that patients only wore their removable offloading device during 28% of their daily activity. Another study found that patients wore their removable cast walker during 55% of their daily activity. A third study compared a removable device with and without cohesive bandaging. The cohesive bandaging kept patients from removing the device, and patients who could not remove their device had a higher portion of healed ulcers at 12 weeks of treatment. This study concluded that the modification of cohesive bandages increased patient compliance to allow for increased ulcer healing. Because of compliance concerns, the selection of the removable offloading device is important, and the factors of the removable device should be carefully considered for each patient. Patient compliance, design of the device, and its ability to maintain a good foot to device interface are key components in removable offloading devices.26,27,28,29



Third Line of Offloading
For the patient who cannot tolerate or is contraindicated to wear a knee-high removeable offloading device, the third line choice of offloading is an ankle-high offloading device. Traditionally, literature has also found that a kneehigh device is more effective than an ankle-high device. However, recent literature has contradicted these findings by concluding that there was no difference between a knee-high and an ankle-high removable offloading device.
One study compared custom-make knee-high removable devices, custom-made ankle-high devices, and prefabricated ankle-high devices. No significant differences were found between ulcer healing rates between any of the devices. Literature has claimed that the key component for knee and ankle-high devices is the fixation of the ankle joint. Because of this, ankle-high devices have shown a reasonable time to healing if the devices are used regularly, and ankle offloading devices more effectively reduced plantar pressures than custom-made or standard footwear. Anklehigh devices are also noted to be 20% lighter than knee-high walkers, which may lead to increased patient compliance and facilitate gait better than a knee-high walker. It has also been noted that these devices have a low adverse event rate and comfort was shown to be equivalent to therapeutic footwear.
Offloading: The Comprehensive Guide Wound Masterclass - Vol 1 - December 2022 53
“For the patient who cannot tolerate or is contraindicated to wear a knee-high removeable offloading device, the third line choice of offloading is an ankle-high offloading device.”
Figure 9: Knee-high removable offloading device with appropriate foot-device interface.
© Copyright. Wound Masterclass. 2023
Figure 10: Ankle-high removable offloading device with appropriate foot-device interface.
Fourth Line of Offloading
Some patients are still either unable or unwilling to tolerate an ankle-high offloading device.

In this case, a felted foam in an appropriately fitting shoe can be a lower fourth line alternative for knee or ankle high devices. Studies have found that when felted foam was applied to an ulceration in a surgical shoe, planter pressures were reduced and lead to shorter healing time than in a half shoe alone. However, there has not been any difference found between felted foam applied directly to the foot and felted foam fitted to a post-operative shoe. Some authors have made note that adhering the felted foam to the foot may increase compliance and provide offloading when the patient does not wear the shoe.
Even still, evidence for the use of felted foam to offload diabetic foot ulcerations is low, and more studies are needed in this area.

Heel Ulceration Offloading
For heel ulcerations in the diabetic patient, the offloading device needs to be carefully considered and it is often a difficult task to undertake. Studies have not found significant differences between TCCs and therapeutic footwear in heel ulceration closure. The literature is mixed at this time as to the effects of total contact casts compared to removable knee-high walkers on heel ulceration outcomes, and no known studies has tested the efficacy of heel pressure relief in specific heel offloading shoes. Crutches to prevent heel strike have been found to be effective. In patients that are non-ambulatory, pressurerelieving mattresses, heel-offloading shoes, or pillows should be employed. Overall, some evidence had found that using knee-high offloading devices may be more effective in time-to-healing and reducing plantar pressures at the heel, but the evidence is low and heel ulceration relapse is the most difficult to prevent.

Conclusion
Ideally, offloading devices should be tailored to each patient as much as possible. If this is not possible, standard offloading options can be entertained to provide some plantar pressure relief. The first line of treatment is a knee-high, nonremovable device, followed by a removable knee-high device, an ankle high removable device, and finally felted foam in therapeutic shoes. While offloading can be a tricky aspect of wound care to master, it is a key to the healing and prevention of diabetic neuropathic ulcerations.
Offloading: The Comprehensive Guide 54 Wound Masterclass - Vol 1 - December 2022
“Evidence for the use of felted foam to offload diabetic foot ulcerations is low, and more studies are needed in this area.”
© Copyright. Wound Masterclass. 2023
Figure 11: Felted foam padding in combination with therapeutic footwear or post-operative shoe.
1. Hoffstad O, Mitra N, Walsh J, Margolis DJ. Diabetes, lower-extremity amputation, and death. Diabetes Care. 2015 Oct;38(10):1852-7.
2. Fleischli JG, Lavery LA, Vela SA, Ashry H, Lavery DC. 1997 William J. Stickel Bronze Award. Comparison of strategies for reducing pressure at the site of neuropathic ulcers. J Am Podiatr Med Assoc. 1997 Oct;87(10):466-72.
3. Armstrong DG, Boulton AJM, Bus SA. Diabetic Foot Ulcers and Their Recurrence. New England Journal of Medicine. 2017;376(24):2367-75.
4. Lazzarini PA, Pacella RE, Armstrong DG, Van Netten JJ. Diabetes-related lower-extremity complications are a leading cause of the global burden of disability. Diabetic Medicine. 2018;35:1297-9.
5. Walsh, J. W., Hoffstad, O. J., Sullivan, M. O., & Margolis, D. J. (2016). Association of diabetic foot ulcer and death in a population‐based cohort from the United Kingdom. Diabetic Medicine, 33(11), 1493-1498
6. Venkatakrishnan, S., Zachariah, K., Chinnappan, P., & Rawat, N. (2019). A description of a modified Bohler iron walking cast in the management of plantar ulcers. J Foot Ankle Surg (Asia-Pacific), 6(1), 10-12.

7. Shankhdhar, L. K., Shankhdhar, K., Shankhdhar, U., & Shankhdhar, S. (2015). Offloading a diabetic foot ulcer in the developing world. Podiatry Today, 28(10), 18-24 Agrawal, V. P. (2012). Are we forgetting to offload the Diabetic foot Ulcers in Rural setup?. J Clin Biomed Sci, 2(4), 206.
8. Shankhdhar, L. K., Shankhdhar, K., Shankhdhar, U., & Shankhdhar, S. (2016). Instant Offloading of a diabetic foot ulcer. Clin Res Foot Ankle, 4(3).
9. Bhat, S. N., & Vinoth, D. (2020). Retracted: Studying the impact of the cost-effective Suvidha off-loading dressing in healing neuropathic ulcers in diabetic foot: a case series of 83 cases from South India. International Surgery Journal, 7(7), 2371-2377.

10. Armstrong DG, Boulton AJM, Bus SA. Diabetic Foot Ulcers and Their Recurrence. New England Journal of Medicine. 2017;376(24):2367-75.
11. Bus, S., Armstrong, D., Gooday, C., Jarl, G., Caravaggi, C., Viswanathan, V., &Lazzarini, P. (2019). IWGDF guideline on offloading foot ulcers in persons with diabetes
12. Guyton, G. P. (2004). The total contact cast: indications and technique. Techniques in Foot & Ankle Surgery, 3(3), 186-191.
13. Lin, S. S., Lee, T. H., & Wapner, K. L. (1996). Plantar forefoot ulceration with equinus deformity of the ankle in diabetic patients: the effect of tendo-Achilles lengthening and total contact casting.
14. Mueller, M. J., Sinacore, D. R., Hastings, M. K., Strube, M. J., & Johnson, J. E. (2003). Effect of Achilles Tendon Lengthening on Neuropathic Plantar Ulcers*: A Randomized Clinical Trial. JBJS, 85(8), 1436-1445.
15. Griffiths, D. A., & Kaminski, M. R. (2021). Duration of total contact casting for resolution of acute Charcot foot: a retrospective cohort study. Journal of foot and ankle research, 14(1), 1-12.
16. Riopelle, A., LeDuc, R., Wesolowski, M., Schiff, A. P., &Pinzur, M. S. (2021). Risk of Complications With the Total Contact Cast in Diabetic Foot Disorders. Foot & ankle specialist, 14(1), 25-31
https://www.aofas.org/news/press-releases/2020/11/10/tips-for-diabetic-foot-care
17. Myerson M, Papa J, Eaton K, Wilson K. The total-contact cast for management of neuropathic plantar ulceration of the foot. J Bone Joint Surg Am. 1992 Feb;74(2):261-9.
18. Armstrong DG, Nguyen HC, Lavery LA, van Schie CH, Boulton AJ, Harkless LB. Off-loading the diabetic foot wound: a randomized clinical trial. Diabetes Care. 2001 Jun;24(6):1019-22.
19. Armstrong DG, Lavery LA, Wu S, Boulton AJ. Evaluation of removable and irremovable cast walkers in the healing of diabetic foot wounds: a randomized controlled trial. Diabetes Care. 2005 Mar;28(3):551-4.
20. Snyder RJ, Frykberg RG, Rogers LC, Applewhite AJ, Bell D, Bohn G, Fife CE, Jensen
J, Wilcox J. The management of diabetic foot ulcers through optimal off-loading: building consensus guidelines and practical recommendations to improve outcomes. J Am Podiatr Med Assoc. 2014 Nov;104(6):555-67.
21. Myerson M, Papa J, Eaton K, Wilson K. The total-contact cast for management of neuropathic plantar ulceration of the foot. J Bone Joint Surg Am. 1992 Feb;74(2):261-9.
22. Armstrong DG, Nguyen HC, Lavery LA, van Schie CH, Boulton AJ, Harkless LB. Off-loading the diabetic foot wound: a randomized clinical trial. Diabetes Care. 2001 Jun;24(6):1019-22.
23. Armstrong DG, Lavery LA, Wu S, Boulton AJ. Evaluation of removable and irremovable cast walkers in the healing of diabetic foot wounds: a randomized controlled trial. Diabetes Care. 2005 Mar;28(3):551-4.
24. Snyder RJ, Frykberg RG, Rogers LC, Applewhite AJ, Bell D, Bohn G, Fife CE, Jensen J, Wilcox J. The management of diabetic foot ulcers through optimal off-loading: building consensus guidelines and practical recommendations to improve outcomes. J Am Podiatr Med Assoc. 2014 Nov;104(6):555-67.
25. Bus, Sicco A. PhD The Role of Pressure Offloading on Diabetic Foot Ulcer Healing and Prevention of Recurrence, Plastic and Reconstructive Surgery: September 2016 - Volume 138 - Issue 3S - p 179S-187S
26. Bus, S., Armstrong, D., Gooday, C., Jarl, G., Caravaggi, C., Viswanathan, V., &Lazzarini, P. (2019). IWGDF guideline on offloading foot ulcers in persons with diabetes.
27. Guyton, G. P. (2004). The total contact cast: indications and technique. Techniques in Foot & Ankle Surgery, 3(3), 186-191.
28. Hingorani, A., LaMuraglia, G. M., Henke, P., Meissner, M. H., Loretz, L., Zinszer, K. M., ... & Murad, M. H. (2016). The management of diabetic foot: a clinical practice guideline by the Society for Vascular Surgery in collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine. Journal of vascular surgery, 63(2), 3S-21S.
29. Hochlenert, D., & Fischer, C. (2020). Ventral Windowed Total Contact Casts Safely Offload Diabetic Feet and Allow Access to the Foot. Journal of Diabetes Science and Technology, 1932296820964069
30. Singh S, Yoong M, Kaur A . Offloading techniques for diabetic foot. J Diabetes Metab Disord Control. 2017;4(3):84-88. DOI: 10.15406/jdmdc.2017.04.00112
31. Kari SV. The economical way to off-load diabetic foot ulcers [Mandakini off-loading device]. Indian J Surg. 2010 Apr;72(2):133-4. doi: 10.1007/s12262-010-0042-3. Epub 2010 Jul 1. PMID: 23133224; PMCID: PMC3452512.
Offloading: The Comprehensive Guide Wound Masterclass - Vol 1 - December 2022 55 References woundmasterclass.com Introducing Wound Masterclass Video woundmasterclass.com/Video © Copyright. Wound Masterclass. 2023 Image licenced from Adobe Stock. Credit: BillionPhotos.com
 Dr Anthony Tickner
Medical Director, Saint Vincent Hospital Wound Healing Center Vice President, Massachusetts Foot & Ankle Society President & CEO-Associated Foot Specialists, P.C. Westford MA, United States
Dr Anthony Tickner
Medical Director, Saint Vincent Hospital Wound Healing Center Vice President, Massachusetts Foot & Ankle Society President & CEO-Associated Foot Specialists, P.C. Westford MA, United States