The challenges of CRT

Protecting access and why bariatric coding is crucial


Protecting access and why bariatric coding is crucial
Idon’t know how to design a Complex Rehab Technology (CRT) power wheelchair. I don’t know how to design a manual tilt-in-space wheelchair or an ultralightweight wheelchair.

But I know that creating these interventions requires the work of many professionals: engineers, of course, and clinicians. But wheelchair manufacturers also work with the U.S. Food & Drug Administration and the Centers for Medicare & Medicaid Services’ Pricing, Data Analysis and Coding (PDAC). They work with testing facilities, focus groups, CRT providers, consumers, caregivers, funding sources and referral sources.
All the work that goes into building CRT should be the “hard part.” Preserving low seat-to-floor height is hard. Keeping systems narrow enough to pass through doorways, but robust enough to accommodate larger consumers, is hard. Designing CRT that fits into a family’s busy lifestyle, transportability wise, is hard. Improving an ultralight’s rollability while keeping its weight down is hard. Doing all of this while keeping the CRT affordable probably seems impossible at times.
So once all that has been accomplished, and the FDA has given clearance, and the PDAC has responded, and seating team members have chosen what they believe will support the best outcomes — the rest should be easy.
After all, by this time, physicians have written prescriptions for medically necessary devices and components. Seating clinicians have worked with ATPs to configure and fit the equipment. The rest should just be follow-through documentation. Time consuming, yes. Still, this should be the “easy” and logical part of wheelchair provision compared to everything before it.
But in this ebook, we examine two current funding issues that are blocking access as surely as a brick wall would. The first challenge: Medicare Advantage plans (page 8) that, contrary to regulations, are routinely denying claims that traditional Medicare fee-for-service would pay.
The second challenge: CMS’s decision not to create a HCPCS code with a separate allowable for CRT seat elevation for bariatric clients (page 16).
Although there is Medicare funding for seat elevation, the lack of a bariatric code and corresponding allowable is preventing access. Although CMS requires Medicare Advantage plans to provide coverage equivalent to traditional Medicare’s, those Medicare Advantage plans’ policies, including copious prior authorization use and denials, are preventing access.
When technology that can support better functional outcomes is available, consumers should be able to access it efficiently. Anything less, with apologies to Pink Floyd, is another brick in the wall that’s denying access. m

Laurie Watanabe, Editor in Chief lwatanabe@wtwhmedia.com @CRTeditor

July/August 2024
mobilitymgmt.com
CO-FOUNDER & CEO, WTWH MEDIA Scott McCafferty
EDITORIAL
VP, EDITORIAL DIRECTOR Tim Mullaney
EXECUTIVE EDITOR Bob Holly EDITOR IN CHIEF Laurie Watanabe lwatanabe@wtwhmedia.com
ART VP, CREATIVE DIRECTOR Matt Claney mclaney@wtwhmedia.com
SALES VP OF SALES Sean Donohue
INTEGRATED MEDIA CONSULTANT Randy Easton
Mobility Management (ISSN 1558-6731) is published 5 times a year, March/April, May/June, July/August, September/ October, and November/December, by WTWH Media, LLC., 1111 Superior Avenue, 26th Floor, Cleveland, OH 44114.
© Copyright 2024 by WTWH Media, LLC. All rights reserved. Reproductions in whole or part prohibited except by written permission. Mail requests to “Permissions Editor,” c/o Mobility Management, 1111 Superior Avenue, 26th Floor, Cleveland, OH 44114.
The information in this magazine has not undergone any formal testing by WTWH Media, LLC, and is distributed without any warranty expressed or implied. Implementation or use of any information contained herein is the reader’s sole responsibility. While the information has been reviewed for accuracy, there is no guarantee that the same or similar results may be achieved in all environments. Technical inaccuracies may result from printing errors and/or new developments in the industry.
Corporate Headquarters: WTWH Media, LLC 1111 Superior Avenue, 26th Floor Cleveland, OH 44114 https://marketing.wtwhmedia.com/
Media Kits: Direct requests to George Yedinak, 312-248-1716 (phone), gyedinak@wtwhmedia.com.
Reprints: For more information, please contact Laurie Watanabe, lwatanabe@wtwhmedia.com.







Synchron has announced that a patient using its brain-computer interface has successfully used his thoughts to control the cursor of the Apple Vision Pro, a spatial computing system.
In a July 30 press release, Brooklyn-based Synchron said Mark, a 64-year-old with amyotrophic lateral sclerosis (ALS), “successfully used his direct thoughts to control the cursor on the Apple Vision Pro when he played Solitaire, watched Apple TV, and sent text messages using the Synchron brain computer interface, hands-free.”
Apple Vision Pro — which Apple says “seamlessly blends digital content with your physical space” using a headset — typically requires hand movements, eye movements, and/or voice to operate. The system provides access to digital content “while allowing users to stay present and connected to others,” the press release said.
Mark — whom Synchron identified by first name for privacy — had the Synchron Brain Computer Interface (BCI) implanted “in the blood vessel on the surface of the motor cortex of the brain via the jugular vein, through a minimally invasive endovascular procedure.”
“BCI is a platform to reconnect people with injury or disease to the fast-moving consumer technology landscape,” Tom Oxley, Synchron’s CEO/founder, said. “Vision Pro is a powerful system, but it relies on the use of hand gestures to exert control over the UI [user interface]. We are sending control signals directly from the brain to replace the need for hand gestures. We are moving towards a new Bluetooth standard for Human Computer Interactions that don’t require touch or
speech. This is a critical unmet need for millions with paralysis.”
“This is pretty cool,” Mark said about watching a video via Apple Vision Pro. “Using this type of enhanced reality is so impactful, and I can imagine it would be for others in my position or others who have lost the ability to engage in their day-to-day life. It can transport you to places you never thought you’d see or experience again.” m
A Synchron BCI, implanted in a blood vessel on the surface of the brain’s motor cortex, detects


Inflammation that occurs in parts of the body other than the brain and spinal cord has been associated with atrophy in the cervical spinal cord in patients with multiple sclerosis (MS), a new study said.
The study — “Systemic inflammation associates with and precedes cord atrophy in progressive multiple sclerosis” — was published this spring in the journal Brain Communications.
In discussing the study, Multiple Sclerosis News Today noted that even common infections — such as those from colds or urinary tract infections — were associated with “more damage to the nervous system in people with progressive forms of multiple sclerosis.”
Researchers used MRI technology to measure participants’ cervical cord and brain atrophy at the start and end of the study.
“Systemic inflammation predicted cervical cord atrophy,” the study’s abstract reported. “An association with brain atrophy was not observed in this cohort. A time lag between systemic inflammation and cord atrophy was evident, suggesting but not proving causation.”
Study participants had primary or secondary progressive MS for more than 2.5 years, and were less than 70 years old.
Lead researcher Ian Galea, a neurologist with the University of Southampton, said in an announcement, “Our results build on decades of research showing inflammation causes nerve cell loss in the lab. Now we’ve shown a connection between inflammation and loss of cells in the spinal cord in humans. In the future, research could help us understand what’s going on at a molecular level when this inflammation happens –which could perhaps help us develop new drug treatments.
“The results of this study suggest it is important for people with MS to minimize inflammation where they can. This includes receiving recommended vaccinations and seeking prompt attention for bladder infections. Following a healthy lifestyle could also be beneficial, as factors like smoking, alcohol and obesity are linked to inflammation. As health-care professionals we can help by talking about these things with our patients so they have the facts they need.” m







A new study published in Disability and Rehabilitation examined wheelchair riders who experience falls and fall-related injuries — and how those incidents impacted their lives going forward.
“Factors associated with fear of falling and fall-related injuries among people who use wheelchairs and motorized mobility scooters: a cross-sectional study” was published in the June 23 edition of the journal. The study’s authors were Sahel Moein, University of Illinois graduate student; Elizabeth W. Peterson, clinical professor, occupational therapy, University of Illinois Chicago; and Laura A. Rice, professor of health and kinesiology, University of Illinois Urbana-Champaign.
“Our research has shown that falls among wheelchair and scooter users are typically caused by interacting risk factors,” Peterson said in a July 30 news announcement from the University of Illinois Urbana-Champaign. “These may be physical, behavioral, environmental or psychological in nature.”
Risk factors include rough terrain, transfers Rice said risk factors for falling include driving or rolling over rough terrain; transferring between wheelchairs and other surfaces; and reaching “beyond one’s base of support.”
Rice added that while falls can cause fractures and other serious injuries, even smaller injuries can be significant. “While a cut or scrape may seem minor, for someone with diminished sensation, that can quickly turn into a bigger problem,” she noted.
The research team studied data from 156 full-time wheelchair or scooter riders with one or more falls in the last three years. Participants completed online surveys that asked about their histories, frequency of mobility device use, whether they’d received training on how to prevent falls, how often they’d fallen in the last year, how afraid they were of falling, and their levels of anxiety and depression.
Researchers found that 96% of the study participants — whose median age was 33 years old — reported falling at least once in the last year, with 74% sustaining injuries as a result. After falling, 94.6% said they were worried about falling again.
“Those who experienced fall-related injuries reported higher levels of anxiety and less frequent use of their wheelchairs or mobility scooters than their peers,” the announcement said.

Fear can lead to higher risk of falling
“But based on clinical experience and other research — especially among ambulatory people — I think it’s likely that a fear of further injuries is causing some people to limit their activities,” Rice said in the announcement. “This can lead to something called a ‘disuse disability cycle,’ where you get into this loop of stopping doing things, and then your physical capacity declines, and that puts you at more risk of falling. It’s a vicious cycle.”
Moein added that while seniors are more typically considered at higher risk for falls, “We also found that participants who experienced fall-related injuries were, on average, younger than those who did not experience such injuries. This is in contrast with many of the previous findings among community-dwelling adults, where older age was associated with falls and their consequences. So we believe that people who are younger have riskier behaviors, which put them at higher risk of experiencing injuries.”
The researchers suggested gauging wheelchair and scooter users’ fall risk and providing safety training accordingly. “The team is testing an intervention they designed to address the specific fall-prevention needs of wheelchair and scooter users,” the announcement said. “The intervention, which is delivered by occupational or physical therapists, addresses a variety of modifiable influences on fall risk.”
The intervention “uses self-management strategies like problem solving, resource utilization and action planning to build participants’ ability to prevent falls,” Peterson said. “Participants also engage in exercise, practice transfer and other wheelchair skills, and create plans to manage falls when they happen.” m
The National Coalition for Assistive & Rehab Technology (NCART) and U.S. Rehab are hosting a Sept. 24 legislative day on Capitol Hill. The in-person event in Washington, D.C., will be “focusing on educating members of Congress about the current economic issues challenging NCART members as they focus on providing equipment to consumers,” NCART said in its July 31 newsletter.
A major talking point on the Hill will be H.R. 5371, the bill that would provide Medicare beneficiaries a way to pay out of pocket to upgrade their ultralightweight wheelchairs to a titanium or carbon fiber frame. Currently, no pathway for upgrades exists. m


More beneficiaries are leaving traditional Medicare. They may not receive equivalent coverage
By Laurie Watanabe
If you are a senior or are senior adjacent — if you have family or friends who are seniors, or work with seniors, for example — you’re likely very familiar with Medicare Advantage (MA) plan sales pitches delivered as robocalls, mailings or commercials featuring senior celebrities. And you’ve likely heard the range of enticing offers that MA plans make, from gym memberships to mealdelivery services, gift cards and cash rebates.
All those ubiquitous sales pitches are working. Last August, KFF (formerly the Kaiser Family Foundation) reported that 30.8 million people — 51% of the Medicare-eligible population — were enrolled in MA plans for 2023. And MA plans are hugely lucrative businesses, accounting for $454 billion of total Medicare spending in 2023, KFF added.
But as popularity of MA plans has grown, so has controversy surrounding plans’ denial rates, and accusations that MA plans are stalling or blocking access to medically necessary services and
equipment. A November 2023 story in Politico said, “A bipartisan group of lawmakers is increasingly concerned that insurance companies are preying on seniors, and, in some cases, denying care that would otherwise be approved by traditional Medicare.”
So how are MA plans impacting Complex Rehab Technology (CRT) clients?
Noel Neil, JM, CDME, VP of auditing and corporate compliance for ACU-Serve Corp., pointed out an April 2022 study from the Office of the Inspector General (OIG): “Some Medicare Advantage Organization Denials of Prior Authorization Requests Raise Concerns About Beneficiary Access to Medically Necessary Care.”
“A central concern about the capitated payment model in MA is the potential incentive for MA Organizations (MAOs) to deny beneficiary access to services and deny payments to providers in an attempt to

Complex Rehab Technology (CRT) isn’t the only health-care industry deeply concerned over the dubious practices of Medicare Advantage (MA) plans.
For example, in April 2022, the Office of the Inspector General (OIG) released the report “Some Medicare Advantage Organization Denials of Prior Authorization Requests Raise Concerns About Beneficiary Access to Medically Necessary Care.” And in February 2023, KFF (formerly Kaiser Family Foundation) published the report “Over 35 Million Prior Authorization Requests Were Submitted to Medicare Advantage Plans in 2021.”
The two reports confirmed that large numbers of MA prior authorizations have been denied, and that a significant number of those denials were questionable, either because they were later overturned on appeal, or because traditional Medicare fee-forservice would have approved the claims.
KFF: Vast majority of appealed denials are overturned
The KFF report said of MA plans, “While prior authorization has long been used as a tool to contain spending and prevent people from receiving unnecessary or lowvalue services, there are some concerns that current prior authorization requirements and processes may create barriers and delays to receiving necessary care, as well as exacerbate complexity for patients and their providers.”
While 82% of appeals were fully or partly overturned, only 11% of prior authorization denials were appealed in the first place — meaning that the vast majority of denials went unchallenged.
The OIG report, in explaining the reason for the study, said, “A central concern about the capitated payment model used in Medicare Advantage is the potential incentive for Medicare Advantage Organizations (MAOs) to deny beneficiary access to services and deny payments to providers in an attempt to increase profits. Although MAOs approve the vast majority of requests for services and payment, they issue millions of denials each year, and CMS [Centers for Medicare & Medicaid Services] annual audits of MAOs have highlighted widespread and persistent problems related to inappropriate denials of services and payment.”

The study said 13% of prior authorizations denied by MAs “met Medicare coverage rules; these services likely would have been approved for beneficiaries under original Medicare.” Some denials were tied to “clinical criteria not contained in Medicare rules,” such as requiring an x-ray before authorizing more advanced imaging.
The report noted that prior authorization usage is relatively uncommon for traditional Medicare beneficiaries, while “virtually all Medicare Advantage enrollees — 99% — were enrolled in a plan that required prior authorization for some services in 2022.”
“Prior authorization may play a role in helping Medicare Advantage plans reduce costs and maintain profits,” KFF said.
In its 2021 research, KFF added that more than 35 million prior authorization requests were submitted to MA plans, and more than 2 million prior authorizations were fully or partly denied.
MA plans also claimed that some prior authorizations lacked sufficient approval, “yet our reviewers found that the existing beneficiary medical records were sufficient to support the medical necessity of the services,” the OIG report said.
The OIG report concluded that MA plans’ prior authorization histories “provide an opportunity for improvement to ensure that MA beneficiaries have timely access to all necessary health-care services, and that providers are paid appropriately.” OIG recommendations included new guidance on how MA plans can appropriately use clinical criteria when determining medical necessity, and updating MA audit protocols to address the report’s issues. m
increase profits,” the OIG said. “Although MAOs approve the vast majority of requests for services and payment, they issue millions of denials each year, and CMS [Centers for Medicare & Medicaid Services] annual audits of MAOs have highlighted widespread and persistent problems related to inappropriate denials of services and payment.”
“Basically, the OIG concluded that Medicare Advantage plans are intentionally denying claims for services,” Neil said. “And when providers appeal them, [denials] are often overturned.”
Jim Stephenson, senior market access manager for Permobil Americas, noted that MA plans are required to adhere to CMS policy.
“The regulation is that if traditional Medicare would have covered it, then the Medicare Advantage plans have to,” Stephenson said. “They can do more; they can’t do less.”
Despite that requirement, seating teams and home medical equipment suppliers are reporting very different experiences.
One example is noninvasive ventilation, commonly prescribed for patients as their amyotrophic lateral sclerosis (ALS) progresses.
“Some of the MA plans are looking in the medical records to show that the patients have actually tried a BiPAP before the doctors prescribed vents,” Neil said. “And that’s not necessarily a requirement of the NCD [national coverage determination]. So they’re not taking into consideration patients’ extenuating circumstances, where the physician documents clearly that a BiPAP would not be able to help the patients because of their unique circumstances — maybe because of their CO2 retention and the tidal pressure that’s not available in a



BiPAP. So to jump through that hoop, there has to be documentation that the patient tried the BiPAP, which is against the whole clinical premise, because if the doctor knows that a therapy cannot treat the patient’s symptom or condition, why would they try it?”
“You’ve got people [at MA companies] who don’t get to see these clients,” Stephenson said. “Sure, everybody’s heard of ALS. But if you haven’t been around it or seen it personally, you have no idea what it means.
“[MA plans] don’t understand the equipment. All they’re doing is looking at policy guidelines versus dollars going out the door, and weighing whether or not it’s worth it to them [to cover equipment recommended by clinicians]. They’re not thinking about it from a perspective of ‘This human being needs this help.’ It should be that simple.”
Seating options via switches
Stephenson said another common example of blocked access involves power seating options, such as tilt and recline, and how they’re operated by power wheelchair riders.
“[MAs’] issue is about being able to operate the seating through the joystick in the
[elevating legrests], a switch for seat elevation.
“In their philosophy, they feel like [electronics] should not be covered. And even with Medicare approval, we’re still seeing instances where [a Medicare Advantage plan] is denying those, saying that they’re not medically necessary. So providers are still taking a large volume of those to the ALJ [administrative law judge] on appeal.”
Based on common MA denial tactics, what can seating teams and providers do to advocate for optimal technology for clients?
In explaining why MA plans so frequently deny what traditional Medicare approves, Stephenson said, “Private insurance companies are being contracted by government entities. And they’re trying to match their own policies with the policies that they’re supposed to be following.
“They’re coming in with a preconceived notion about how this process works, but they’re being pushed into a system that does things a bit differently. So it’s a challenge.”
Because MA plans are required to cover what traditional Medicare would cover,
The regulation is that if traditional Medicare would have covered it, then Medicare Advantage plans have to. They can do more; they can’t do less — Jim Stephenson
expandable controller and harness,” he said. “When you justify the fact that [the clients] do truly clinically need to operate their seating through the drive control, [MA plans] cover all that. But then they’ll deny one of the seating systems so that they don’t have to pay for the expandable controller and harness.”
This scenario has happened often enough that Stephenson has detected a pattern of which seating systems are denied. “It’s usually recline. You can count on it almost every time.”
“They feel the electronics should not be payable,” Noel said of MA plans. “They believe that the power seating option should come with a switch, and a patient should be able to operate a switch: for tilt, a switch. A switch for the recline, a switch for the ELRs
Stephenson agreed that getting a prior authorization from traditional Medicare could be helpful.
“Yes, I suggest that,” he said. “Because at that point, you can send in an affirmative prior authorization from Medicare to one of these Advantage plans. Then they’re at a point of either ‘We will follow what Medicare does’ or ‘We knowingly will go against the contract.’ And then you’ve got proof of them not doing what they’re supposed to do.”
Another possible best practice is suggested by statistics (see “Denials” sidebar).
As Neil mentioned, appealing MA denials often results in full or partial overturning … if the provider, the rest of the seating team, and the consumer have the time, energy and resources to fight that fight.
In June, the bipartisan, bicameral Improving Seniors’ Timely Access to Care Act was reintroduced in the House (H.R. 8702) and Senate (S. 4532). The American Medical Association (AMA) said an earlier version of the bill had 378 cosponsors in the House and Senate, as well as endorsements from more than 500 organizations, including the AMA.
The new version of the bill addressed and significantly reduced the original $16 billion score from the Congressional Budget Office, the AMA added.
A summary of the bill listed on congress.gov says the bill “establishes several requirements and standards relating to prior authorization processes under MA plans.
“Specifically, MA plans must (1) establish an electronic prior authorization program that meets specified standards, including the ability to provide real-time decisions in response to requests for items and services that are routinely approved; (2) annually publish specified prior authorization information, including the percentage of requests approved and the average response time; and (3) meet other standards, as set by [CMS], relating to the quality and timeliness of prior authorization determinations.”
Stephenson suggested that the root of the problem could be a culture clash that occurs when private payers enter the traditional Medicare space in an effort to grow their own businesses and profits.
“The inherent problem with our entire health-care system is that they’re allowed to be for-profit,” Stephenson said. “That should not be. If you’re making all this money to provide health care for these people, then you should be spending every dollar of that money on their health care.” m
Read a case example of a Medicare Advantage denial escalated to the departmental appeals board — and how it was ultimately resolved — as related by ACUServe’s Noel Neil.

Complex Seating. Simplified.


www.symmetric-designs.com
Fit a custom molded back in one appointment
Single tool adjustment
Completely ventilated custom seating
HCPCS Coded E2617 and E2609
Demos available
Beat the heat with for fully ventilated custom seating! StimuLITE ®
Back Kits available with a full range of sizes, shapes, padding/covers and mounting options.
Admittedly, the typical Complex Rehab Technology provider is already burdened with so much claims-related work that requesting additional documentation from them is not an easy ask.
The funding project by the Clinician Task Force (CTF), however, is a vital one, according to CTF Executive Director Cara Masselink, Ph.D., OTR/L, ATP. The CTF is examining the funding decisions of various Medicare Advantage (MA) plans to better understand which plans are denying power wheelchair claims — and whether traditional Medicare would have approved those claims.
“I think there’s a lot to protect in this industry,” Masselink told Mobility Management. “Not only the client, but also DME suppliers.”
Examining MA plans’ history of denials
“We are hearing from a lot of people in the industry that MA plans are denying power wheelchair bases and power options that traditional Medicare would likely cover,” Masselink said in explaining the reason for the CTF’s ongoing project. “We’ve heard about this for years, and it’s been a long-standing issue.”
The CTF, in collaboration with the National Coalition for Assistive & Rehab Technology (NCART) and other industry partners, came up with a multi-pronged plan. “One of the prongs is looking at and trying to understand if these are really claims that Medicare would cover,” Masselink said about MA denials. “As a group, we felt the Clinician Task Force was probably the best group to carry this forward, because our sole focus is protecting access and looking at equity.”
The CTF is asking providers to provide, at regular intervals, information such as the MA plans they work with and the plans they’ve chosen not to work with, if applicable.
“For the study, we are asking suppliers to — when there is a power chair base — to concurrently submit the claim to the [traditional Medicare] prior authorization process, and get a decision from Medicare as well,” Masselink said. “Then we are asking for information on that claim to be copied and pasted into a spreadsheet, and we are looking at trends in the data that we get: diagnoses, HCPCS codes, denial reasons, and plans. [We’re] trying to understand a little bit better when [claims to MA plans] are approved and when they are not.”
Most claims have been for Group 3 power chairs
Thus far, the focus has been on Group 3 power chairs of all types: no power options, single power option, multiple power options.
“Most of the data we’ve received has been Group 3, but we are not limited to that [group of HCPCS codes],” Masselink said. “Most of the data we’ve received are Group 3 with tilt and recline.
“Most of the diagnoses [received from submitted info] are stroke right now, but not all of them. I would love to see a broader range of diagnoses represented in the data that we have. We know people who have had a stroke need power wheelchairs, but a lot of people with multiple sclerosis and other neurological conditions do, too. That information isn’t very broadly represented in our data right now.”
And the CTF would also welcome data on clients with neuropathy, diabetes-related amputations, and other diagnoses more typically seen for Group 2 claims. “We have opened it up for any power wheelchair claim,” Masselink confirmed.
Tracking data to protect access
She added that the CTF has tried to make the participation process as simple as possible.
“What we asked [participating] companies to do is to assign a random ID to the client in the entries that they give to us,” Masselink said. “They should keep a log that relates the random ID to the patient in their database. They move information from the claim and denial to a spreadsheet with the random ID. And then, on a monthly basis, we’re asking those companies to email us the spreadsheet.”

“We’re hoping they can copy and paste information from the claim and denial, updating it if or when new information comes in. We’re trying to reduce administrative burden as much as possible. We don’t want companies to worry about ‘Did we send this one in already?’”
Data from providers will be compared to look for trends.
“I think the lowest denominator for privacy in geographic location that we are gathering is at the state level,” Masselink said. “We’re trying to show that this is representative across or happening across the United States, or look at where it’s happening more often so that we can try to understand it better.”
Providers who want to participate can scan the QR code in this story for more information.
“We understand that this is extra [effort],” Masselink said. “But we’re not going to make a change if we all don’t come together and do this. The people who are processing the claims and submitting them to insurance are the best people to get us this information.
“The starting point is being able to get this information together so that we can write a letter to Medicare and say, “This is what we’re seeing and this is what we think is happening. Can we talk about why, and can we talk about ways that we can make this better for Medicare and for people who need this equipment?’ The DME MACs have been receptive to that information and to our collaboration in the past. So we feel like this is a fairly reliable approach hopefully to make some change.”
The more providers who participate, the better. And the faster, the better, as well.
“We’d like to get moving on this; we can’t keep this out there forever,” Masselink said. “The faster we can get a reasonable amount of claims, a reasonable amount of data, the quicker we’re going go to Medicare.” m
Scan this QR code for more information on the CTF research project.

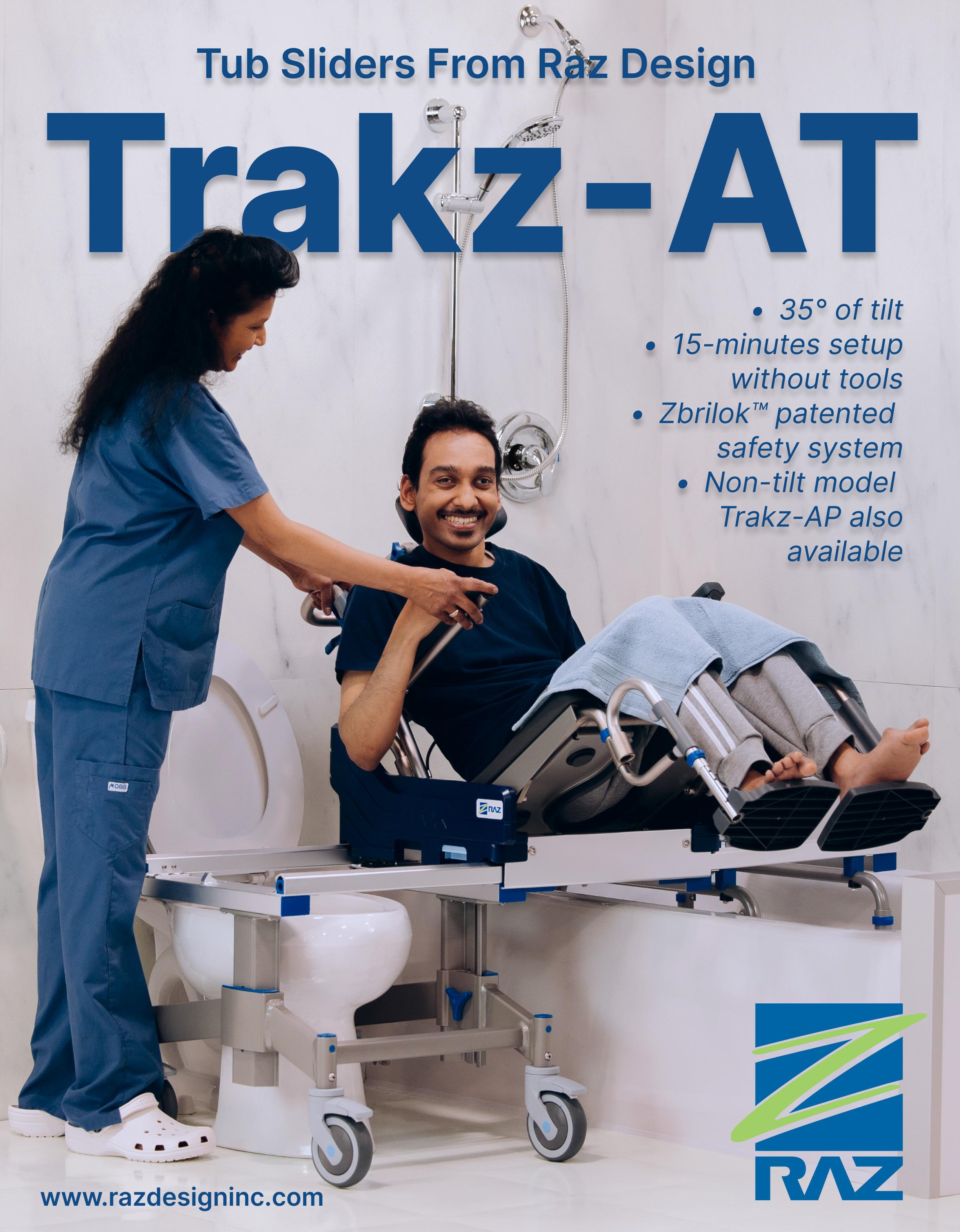
It’s all about access, engineering … and physics
By Laurie Watanabe
This spring’s coding and funding decision by the Centers for Medicare & Medicaid Services (CMS) for power seat elevation was a textbook case of good news and bad news.
The good news: CMS, citing how seat elevation can support and facilitate transfers and reaching tasks, affirmed the medical necessity of seat elevation for Medicare power wheelchair beneficiaries.
But the bad news: The initial allowable was $2,000.34 for HCPCS code E2298. (In June, CMS revised the allowable to $2,013.96.)
And E2298 was the only HCPCS code created. Despite Complex Rehab Technology (CRT) industry testimony that a second bariatric code and accompanying allowable were needed to ensure access to the technology, CMS contended the one code and allowable were entirely sufficient.
Design differences in bariatric seating, mobility
Just as designing pediatric wheelchairs isn’t as simple as shrinking an adult-sized wheelchair, successfully designing a heavy-duty
wheelchair and seating system is much more complicated than making those systems wider, deeper and able to support more weight.
When engineering a bariatric power wheelchair and seating, “the user weight can be the least of our concerns,” said Brad Peterson, VP of sales USA at Amylior. “You can make something to support a [heavyduty] weight; it can be big and robust. However, the bigger challenge can be safely accommodating their shape and the distribution of the weight, which can be widely variable from person to person. All the while, we must also take into consideration maneuverability, environmental access, transfer, stability, performance and comfort just as we do systems for more standard weights. Yes, everything needs to be bigger and stronger but in a smaller, lower and more stable package! It can be quite a balancing act.”
“There are differences in the design, materials used and engineering to provide support and durability for higher weight capacities,” said Leslie Wade, MOT, OTR/L, ATP, regional clinical education manager, Permobil. “Generally, heavy-duty power chairs
feature larger batteries, more powerful motors, and advanced suspension to provide a smoother ride. The goal is to design power chairs that are safe and functional for our users with higher weight capacities.”
Asked also if manufacturers need to consider additional factors when designing bariatric seat elevation equipment, Jeff Rogers, director of power product management for Sunrise Medical, said, “I think there are two parts to this question. One: How do you first get 450 lbs. up that high — because that’s what the weight capacity is. Second: Once that weight is elevated, what do you do with it? From a QUICKIE standpoint, we don’t have a heavy-duty elevation [system] at this time because there are challenges with this. Could we develop one? Yes. Would it be really expensive right now? Yes. That’s been why we don’t have one currently in the market: The challenge is managing that weight. Getting it elevated is one thing, but managing the stability of the base is another. Because the physics are: If I put 450 lbs. up 12" in the air, there is a little thing called momentum which is much different than it is when the seat is in the home position.”
Rogers compared the low profile of a sports car, whose weight is low to the ground, versus a higher-profile SUV. “Which one is going to be more susceptible to
price, which is just not going to happen. Because not only does the seating system have to change, but the base will likely change as well to accommodate the weight being higher than a traditional HD base.”
The complexity of seat elevation
While CMS representatives seem to believe that seat elevation is substantially less complex than power tilt or recline, Peterson disagreed.
“Of course, you need a system that has a stronger actuator (motor) for heavy-duty weights. That’s the most basic thing because you’re lifting up to 150 lbs. more weight between the standard weight and the heavyduty weight chair. So there is more weight, and oftentimes a lot more asymmetrical loads that are biased to the front.
“That puts different loads on the lifting actuators from a durability and stability standpoint. And we have to make sure it still supports tilt, recline, power elevating legs and back-mounted accessories such as backpacks, ventilators, oxygen, etc. These add weight but also greater asymmetrical and cantilevered loads, all supported by the power seat elevation system.”
“When designing heavy-duty power wheelchairs, stability is critical, especially when using power seat functions, such as seat elevate,” Wade said. “Heavier weight can potentially affect the stability of the power
If I put 450 lbs. up 12 inches in the air, there is a little thing called momentum that is much different than it is when the seat is in the home position
— Jeff Rogers
the bariatric consumer, manufacturers need to ensure that the power chair remains safe to drive and can navigate varied terrain while in a raised position.
“Our number one job is to keep the individual safe,” he said. “So, when someone’s driving a power chair, we must try to predict what environments they’re going to put this chair into. We can say in the owner’s manual, ‘Don’t drive on a given slope.’ But we also know people don’t pull out a protractor and measure every angle they drive on. So we try to prepare for as much of the unknown as possible. With a combination of mechanical features, as well as electronic features that limit the drive of that chair in certain scenarios, we can give the best ride experience, regardless of where they are. The chairs are getting smarter and smarter.”
While power tilt and power recline are acknowledged by CMS to be seating systems, seat elevation is defined as an accessory.
Julie Piriano, PT, ATP/SMS, senior director of payer relations & regulatory affairs for the National Coalition for Assistive & Rehab Technology (NCART), was the industry’s primary presenter during November’s Healthcare Common Procedure Coding System Public Meeting, 2nd 2023 Biannual HCPCS Coding Cycle. (At that time, Piriano was employed by Pride Mobility Products/Quantum Rehab.)
Seat elevation, Piriano believes, is a hybrid technology: “The industry recognizes that CRT power seat elevation is an accessory to a CRT power wheelchair, as it is a component that cannot be used without the chair,” she pointed out.
tipping over?” Rogers asked. “A large SUV. Even though it may be bigger, heavier, and have a wider stance, when you put that much weight that high in the air, you’re going to have challenges.”
Rogers said that fact is one of multiple challenges to designing a functional, safe seat elevation system. “That’s one thing that we have to overcome,” he said. “To say it’s going to be the same as building a standardcapacity [system] — that’s not the case. We’re now forced with trying to figure out a way to build this technology at the same
wheelchair. When there is a heavier load — e.g., 350 lbs. — positioned in seat elevate, the center of gravity is raised more than compared to a lighter weight (e.g., 175 lbs).
“To make the base more stable, manufacturers may design their power wheelchairs with wider bases, enhanced anti-tip mechanisms, as well as lower centers of gravity. Manufacturers may also limit the wheelchairs’ movement when the seat is elevated to prevent instability and risk of tipping.”
Rogers said that in addition to elevating
“However, like power tilt and power recline, we also contend that CRT power seat elevation is a complete system that moves the chair frame relative to the base and compromises the stability of the chair much more than either of the other two power seating systems combined. There are additional mechanical and/or electrical safety mechanisms inherent in the design of a CRT power seat elevation system, and they require more rigorous stability testing protocols not required of an accessory that is an addition to a power seating system, such as power elevating legrests (ELRs) or a power centermount foot platform.”


Unveil new realms of freedom with the E-Motion® DuoDrive™, fusing revolutionary power assist with your manual wheelchair. Its lightweight, dual-mode design seamlessly transforms mobility, empowering you to navigate effortlessly, conquer inclines, and extend your adventures.
Two Driving Modes: Easily switch between manual and Cruise Mode for a customized travel experience.
Extended Battery Life: A single charge delivers up to 12 hours of uninterrupted movement.
Advanced Slope Capability: Master inclines with the DuoDrive's robust electric motors.

While physics is a complex subject — a challenging combination of math and science, according to Carnegie Mellon University, that concerns matter and energy — we frequently encounter physics in our everyday lives, sometimes without even thinking about it.
Imagine that you see a long-handled ax on the ground and want to pick it up, but only have one hand free. Where do you grab that ax — nearer the head of the ax, or nearer the end of the handle or haft?
If you would grab the ax nearer the head … that’s physics.
So what does physics have to do with seat elevation on power wheelchairs — and specifically with seat elevation for clients with body weights in the bariatric category?
It’s related to the need for stability of the seating system and the power base, and related to how that balance is achieved.
Julie Piriano, PT, ATP/SMS, is now the senior director of payer relations & regulatory affairs for the National Coalition for Assistive & Rehab Technology (NCART). But last November, while employed by Pride Mobility Products, Piriano was the industry’s primary speaker at the Healthcare Common Procedure Coding System Public Meeting, 2nd 2023 Biannual HCPCS Coding Cycle, hosted by the Centers for Medicare & Medicaid Services (CMS).
Piriano and the industry’s other speakers that day — Brad Peterson from Amylior; Bill Ammer from Ammer Consulting; and Peter Thomas from the ITEM Coalition and Powers Pyles Sutter & Verville — urged CMS to provide Medicare coverage for a heavy-duty seat elevation code.
A separate heavy-duty code — along with adequate funding for it — was essential, speakers said, to preserve access to seat elevation for bariatric consumers.
And here’s where physics comes in, to explain why heavy-duty seat elevation needs to be funded independently from standard-weight seat elevation.
Hammer vs. sledgehammer
Piriano used an example she attributed to Ammer to explain weight, balance and stability.
“If you take a hammer, and you hold it up by the head of the hammer, and you wave it around, you’ve got good control of the hammer,” Piriano said. “If you hold it at the bottom of the handle, and you raise it over your head, and you wave it around, it is very hard to control. That’s the center of gravity change and the instability that it creates.
“If you then take a sledgehammer and hold it at the bottom of the handle, and now you wave the sledgehammer …?”
That real-world example demonstrates how much more challenging it is to stabilize and control higher weights versus lower weights, especially when the weight is being vertically raised, as happens with bariatric seat elevation. m
And seat elevation’s classification as solely an accessory causes complications for documentation for ELRs and power articulating footplates (AFPs), Piriano added.
“In addition, if CRT power seat elevation is not deemed a power seating system, then the addition of power ELRs or a power AFP is not covered or reimbursable for a beneficiary who needs leg elevation in conjunction with their CRT power seat elevation system, as these accessories can only be billed as an addition to a power seating system,” she explained.
Reimbursement, meanwhile, remains a work in progress for both heavy-duty seat elevation and standard-weight seat elevation, which received a paltry $13.62 increase in June.
“We have informally been meeting with CMS on this topic,” she said. “But then we submitted a new HCPCS code application to the alphanumeric coding workgroup, so that it goes back into the formal process and is added to their statement of work. So they have to address it. We had to do it in a way that said, ‘We are seeking a revision to the code.’
“And we gave them the new code description, which then allows them to make changes, because we weren’t asking for a new code. And we weren’t removing a code. The only other option was revision.”
Ultimately, the CRT industry’s concern is that the lack of a bariatric seat elevation code will prevent bariatric wheelchair riders from accessing crucial technology that can help with transfers and other activities of daily living.

“This is where we say, ‘Let’s use gravity,’” said Rogers about how seat elevation can help with transfers.
“Anytime we can get your starting point higher than your finish point of your transfer, gravity is going to help you, and your caregiver doesn’t have to lift you up and over.
“I’ve seen plenty of moms trying to take care of a son or daughter who may be bariatric. They’re going to blow out their backs trying to lift this person daily. If I offer a device to assist them, I save the caregiver from possible injuries.”
And if seat elevation isn’t available to this population?
“Then we’re going to have people who will be sitting for longer than they should or will be stuck in a situation that they can’t get out of,” Rogers said. “Riders are stuck at home sometimes because they’re afraid to go anywhere because they can’t transfer. This most definitely impacts the quality of life of our riders, and they deserve better.”
Peterson pointed out that demand for bariatric CRT is only expected to grow, especially for larger weight capacities.
“There are also people who weigh more than 450 lbs.,” Peterson said. “If you look at the tilt code, the recline code, if you look at other mainstream chairs in the very heavyduty code, they’re oftentimes tilt-only chairs, or they’re 25° of tilt, nothing else. Because they’re not designed to be able to give the benefit of full tilt, full recline, full power legs, just because of [the clients’] size. Because there’s no extra funding. Suffice it to say that the needs of someone who weighs 585 lbs.


are much different than someone who weighs 185 lbs.”
Because of current Medicare policy — and one allowable for seat elevation of all weight capacities — Peterson expects bariatric clients to be denied access.
“We’re one of the only ones who will do seat elevation for consumers over 400 lbs., but we limit it to 5" or 7", just from the stability standpoint,” Peterson said regarding Amylior’s current offerings. “So right there, these people are not going to be able to get that funded because it doesn’t [elevate] 11".”
Peterson recalled a CMS representative “saying that a lot of people have a hard time thinking about putting someone who weighs 300 lbs., 11" in the air and driving at 3.5 mph. So think of doing the same thing with someone who weights 485 or 500 lbs.
“We need to be able to engineer and design specifically to that weight and make the system itself specifically to what they need, and we can’t do that with a code that says, ‘Any type’ [of seat elevation].” m
If you look at mainstream chairs in the very heavy-duty code, they’re oftentimes tilt-only or they’re 25° of tilt, nothing else
— Brad Peterson
At the Nov. 30, 2023, Healthcare Common Procedure Coding System Public Meeting, 2nd 2023 Biannual HCPCS Coding Cycle, representatives from the Centers for Medicare & Medicaid Services (CMS) described power seat elevation as staying in one plane — solely moving up and down — compared to power tilt, which moves through more than one plane.
That distinction seemingly impacted CMS’s decision-making process while determining whether to define seat elevation as a seating system or a seating accessory, and while calculating allowables.
But is seat elevation as simple as moving vertically?
Seat elevation is a highly complex system
“No, not necessarily,” said Julie Piriano, PT, ATP/SMS, senior director of payer relations & regulatory affairs for the National Coalition for Assistive & Rehab Technology (NCART). “When the tilt function is deployed, rotation occurs around a fixed point, but the user’s center of gravity moves in a horizontal direction, as there is a sliding motion that helps keep the center of gravity close to its
which it operates at full speed. If the chair drives at a reduced speed (creep mode) in a tilted position, the chair is re-tested for dynamic stability in its least stable configuration in which it still drives. For chairs with a tilt system that goes into drive lock-out where the chair cannot move in a tilted position, no further testing is required.”
Moving in multiple directions to elevate
Complex Rehab seat elevation does not simply lift the seating and consumer straight up and only straight up, as if rising on a post the way a typical office chair does.
Additionally, while all seat elevation systems lift the wheelchair rider, different systems achieve that lifting in different ways.
“While many seat elevation systems raise the system’s center of gravity directly upward from its home position, some seat elevation systems may move slightly forward or rearward while elevating to align the center of gravity to its most stable position over the base,” Piriano said. “Regardless of which mechanism is used to elevate the seat 10" or greater, raising the seat height creates a much less stable system than tilt, recline, or a combination of tilt and recline.”
More evidence of seat elevation’s complexity: The amount of required stability testing for power chairs with that option.
“The mandatory testing performed by an independent test lab is much more extensive for chairs with a CRT [Complex Rehab Technology] seat elevation system because of the industry’s established performance characteristics of 10" of elevation, the ability to ascend and descend while driving, the ability to move on horizontal surfaces while fully elevated and compatible with other power seating systems such as tilt and/or recline,” Piriano said. “This is an important distinction for CRT power seat elevation systems, as it is essential for these chairs to be tested in their least stable configuration with all power seating systems deployed while still permitting the chair to move.” m
