BETTER EYESIGHT: WHAT YOU AND MODERN MEDICINE CAN DO TO IMPROVE YOUR VISION
William A. Haseltine Ph.D. And Kim Hazel MPH
ACCESS Health Press
Copyright ©
2023
by William A. Haseltine, PhD
Cover art by Kim Hazel
All rights reserved. No part of this book may be used or reproduced by any means, graphic, electronic, or mechanical, including photocopying, recording, taping, or by any information storage retrieval system, without the written permission of the publisher except in the case of brief quotations embodied in critical articles and reviews.
All author proceeds from the sale of this book will be donated to the nonprofit global think tank ACCESS Health International.
iv
Recent Books by William A. Haseltine
TheCOVID-19Textbook:Science,MedicineandPublicHealth; WilliamA.HaseltineandRobertoPataraca(2023)
ScienceasaSuperpower:MyLifelongFightAgainstDiseaseAnd TheHeroesWhoMadeItPossible;WilliamA.Haseltine(2021)
MyLifelongFightAgainstDisease:FromPolioandAIDSto Covid-19;WilliamA.Haseltine(2020)
WorldClass.Adversity,TransformationandSuccessandNYU LangoneHealth;WilliamA.Haseltine(2019)
AgingWell;JeanGalianaandWilliamA.Haseltine(2019)
VoicesinDementiaCare;AnnaDirksenandWilliamAHaseltine (2018)
EverySecondCounts:SavingTwoMillionLives.India’sEmergency ResponseSystem.TheEMRIStory;WilliamAHaseltine(2017)
AgingwithDignity:InnovationandChallengeisSweden-The VoiceofCareProfessionals;SofiaWidenandWilliamA.Haseltine (2017)
ModernAging:APracticalGuideforDevelopers,Entrepreneurs, andStartupsintheSilverMarket;EditedbySofiaWidén,Stephanie Treschow,andWilliamA.Haseltine(2015)
ImprovingtheHealthofMotherandChild:SolutionsfromIndia; PriyaAnant,PrabalVikramSingh,SofiBergkvist,WilliamA. Haseltine&AnitaGeorge(2014)
AffordableExcellence:TheSingaporeHealthcareStory;WilliamA Haseltine(2013)
v
Living ebooks
A Family Guide to Covid: Questions and Answers for Parents, Grandparents,andChildren;WilliamA.Haseltine(2020)
ACovidBackToSchoolGuide:QuestionsandAnswersforParents andStudents;WilliamA.Haseltine(2020)
CovidCommentaries:AChronicleofaPlague,VolumesI,II,III, IV,V,andVI;WilliamA.Haseltine(2020)
MyLifelongFightAgainstDisease:FromPolioandAIDStoCovid19;WilliamA.Haseltine(2020)
Variants!: The Shape-Shifting Challenge of Covid-19 Vaccine Evasion&Reinfection;WilliamA.Haseltine(2021)
CovidRelatedPost-traumaticStressDisorder(CV-PTSD):WhatIt IsAndWhatToDoAboutIt;WilliamA.Haseltine(2021)
NaturalImmunityAndCovid-19:WhatItIsAndHowItCanSave YourLife;WilliamA.Haseltine(2022)
Omicron: From Pandemic to Endemic; William A. Haseltine (2022)
MonoclonalAntibodies:TheOnceandFutureCureforCovid-19; WilliamA.HaseltineandGriffinMcCombs(2023)
TheFutureofMedicine:HealingYourself:RegenerativeMedicine PartOne;WilliamA.Haseltine(2023)
ViroidsandVirusoids:Nature’sOwnmRNAs;WilliamA.Haseltine andKolomanRath(2023)
CAR T: A New Cure for Cancer, Autoimmune and Inherited Disease;WilliamA.HaseltineandAmaraThomas(2023)
vi
EndingHepatitisC:ASeven-stepPlanforaSuccessfulEradication Program: A Roadmap for Ending Endemic Disease Globally; WilliamA.HaseltineandKaelynVarner(2023)
Welcome to "Better Eyesight: What You And Modern Medicine Can Do To Improve Your Vision" a comprehensive guide to breakthroughs, challenges, and advances in the field of ophthalmology. This book aims to provide the latest information on cutting-edge eye care technologies, innovations, and the wide range of eye disorders and diseases that impact people globally.
The book delves into advances in eye care technologies, unveiling groundbreaking developments like brain implants, and gene therapy. It also explores various treatment options and procedures for different eye conditions. Specialized approaches for treating strabismus, stem cell therapies, gene therapies for retinal disorders, laser photocoagulation for diabetic macular edema, and photodynamic therapy for bullous retinal detachment are discussed in detail. The book takes a unique and comprehensive approach to color and night blindness.
Overall, it gives readers an in-depth understanding of the latest eye care technologies and treatment advances and offers valuable insights into common and rare eye conditions.
You can find more information about the eye and regenerative medicine by visiting
www.williamhaseltine.com/
Thank you for your interest.
vii
Acknowledgments
We thank the ACCESS Health US team, Courtney Biggs, Koloman Rath, Amara Thomas, Griffin McCombs, and Roberto Patarca, for their support in creating this book.
We also thank the expert ophthalmologists Kathryn Colby, MD, PhD, and Lynn K. Gordon, MD, PhD, for their time, expertise, and input in making this book up-to-date, accurate, and beneficial for the public. Their information was invaluable, and their insights helped shape the scope of the innovations covered in this book.
This work is supported by ACCESS Health International (www.accessh.org).
viii
Dedication
WilliamHaseltine,Ph.D.
To my wife, Maria Eugenia Maury; my children Mara and Alexander; my stepdaughters Karina, Manuela, and Camila; my grandchildren Pedro Agustin, Enrique Mattias, and Carlos Eduardo; and last but not least, our three dogs, Sky, Luna, and Ginger.
KimHazel,MPH
To my loving husband, Colin Purcell, for his unending support.
To my mom, Victoria Wilson, for her unconditional love.
To my friends Ami Hampton and Emily Trout for their undying positivity.
To my other moms, Teresa Hazel and Sandy Purcell for their unwavering belief in me.
To my friend and colleague Courtney Biggs for her guidance, support, and optimism.
ix
x Contents Introduction ................................ ................................ .............. 1 Chapter 1 : Eye Care Technologies and Special Topics 3 Retinal Imaging ............................................................................ 3 Diagnosing Other Diseases with Retinal Images ....................... 10 Partners to Retinal Imaging: Targeted Spectroscopy in the Eye Fundus & Electroretinography .................................................. 15 Migraines and the Eye ............................................................... 22 Brain Machine Interface & Implants ......................................... 27 Aging and the Eye ...................................................................... 35 Rare Eye Disease: Epidermolysis Bullosa .................................. 41 Organoids and Transplants ........................................................ 46 Visual Plasticity 50 Chapter 2 : Conjunctivitis ................................ ........................ 54 Allergic Conjunctivitis 55 Bacterial Conjunctivitis .............................................................. 59 Chapter 3 : Corneal Disorders and Diseases 63 Corneal Transplants ................................................................... 64 Corneal Infection from Contacts ............................................... 70 CRISPR for Herpetic Stromal Keratitis 74 Cell Therapy for Damaged Corneas .......................................... 77 Steven-Johnson Syndrome ......................................................... 82 Chapter 4 : Proptosis and Strabismus 86 Thyroid Eye Disease and Proptosis ............................................ 86 Strabismus .................................................................................. 89
xi Chapter 5 : Dry Eye Syndrome and Eye Floaters .................... 95 Eye Floaters .............................................................................. 110 Chapter 6 : Age - Related Macular Degeneration .................... 115 Research Leads Us To Insights ................................................ 118 Stem Cell Therapies 123 Gene Therapies ........................................................................ 133 Protein-Based Therapies .......................................................... 139 Geographic Atrophy Secondary to Age-Related Macular Degeneration ............................................................................ 150 Chapter 7 : Other Macular Issues ................................ .......... 156 Stem Cells for Stargardt's Macular Dystrophy ........................ 156 Macular Edema ........................................................................ 160 Diabetic Macular Edema ......................................................... 163 Chap ter 8 : Refractive Errors ................................ ................. 169 Binocular Vision Disorders ...................................................... 180 Amblyopia 185 Chapter 9 : Cataracts ................................ ............................. 190 Chapter 10 : Glaucoma 213 Chapter 11 : R etinal Detachment ................................ ......... 230 Chapter 12 : Retinitis Pigmentosa ................................ ......... 234 Chapter 13 : Understanding Retinopathy 240 Chapter 14 : Color Blindness and Night Blindness ............... 259 Color Perception 259 Color Blindness ........................................................................ 263 Color Blindness Due to Retinitis Pigmentosa ......................... 277 Night Blindness 281
xii Chapter 15 : Ocular Toxoplasmosis ................................ ....... 285 Chapter 16 : Uveitis ................................ ............................... 290 References ................................ ................................ ............. 298
Introduction

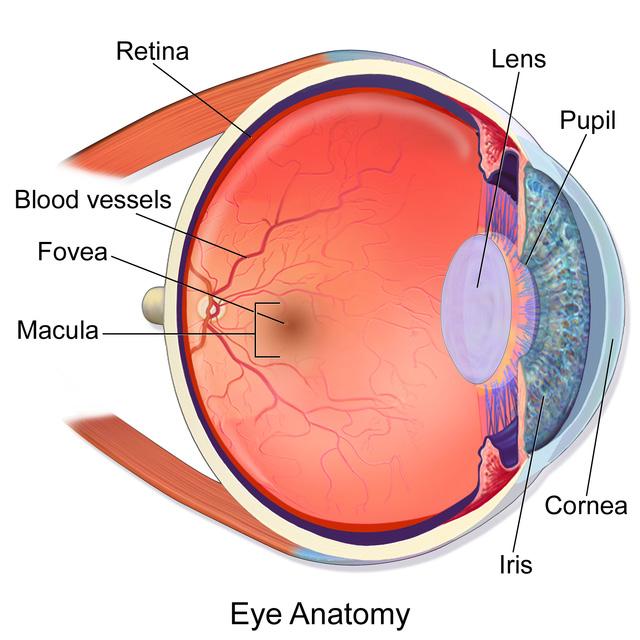
The human eye is an incredibly intricate and fascinating organ with an impressive ability to perceive and explore the world around us. Its complex structure includes several critical components, including the cornea, iris, lens, retina, and optic nerve, all working together seamlessly to capture light and transmit visual information to the brain.
The eye's ability to interpret the images it sees is essential for making sense of our surroundings. It allows us to appreciate the beauty of nature, recognize faces, and read words on a page. Furthermore, our eyes constantly adapt to changes in light levels, allowing us to see clearly in various environments, from bright sunlight to dimly lit rooms.
However, vision loss can occur due to various factors, such as aging, injury, disease, or genetics, resulting in a less vivid world or even completely obscured. Despite this, there are tireless efforts by dedicated doctors, researchers, and scientists to expand the boundaries of eye care and restore hope to those who have lost their vision.
Every new advance in vision restoration technology and every new treatment brings us closer to a brighter future. Such advances are not just about restoring sight but also about restoring hope and optimism for individuals, families, and entire communities whom the darkness of vision loss has burdened.
Contained within the pages of this book is a collection of stories that provide an in-depth look into the world of eye care. These stories
1
showcase the latest findings and breakthroughs in the field, offering a glimpse into the tireless work of professionals dedicated to improving eye health. Moreover, they highlight the incredible potential of human innovation and perseverance, demonstrating the power of the human spirit in the face of adversity.
"Better Eyesight: What You And Modern Medicine Can Do To
Improve Your Vision" is designed to guide readers through the intricacies of eye care, from the basic science behind vision and eye health to groundbreaking technologies, innovative treatment methods, and the inspiring stories of individuals whose lives have been transformed. We'll explore the complex machinery of the eye, analyze the mechanics of sight, and participate in the ongoing conversation about cutting-edge therapies, genetic interventions, and emerging practices in eye care.
Whether you're a medical professional, a researcher, a student, or someone struggling with vision health issues, this guide is essential for understanding the latest developments in eye care. Join us on a journey to explore scientific breakthroughs and personal stories that contributed to our understanding and approach to eye care. Each chapter of this journey will provide a glimpse into the vast landscape of ocular health and a profound appreciation for the power of healing, innovation, and human connection.
BetterEyesight 2
1
Eye Care Technologies and Special Topics

Retinal Imaging
The human eye is a marvelous work of art. Delicate as it is, it houses a complex system that enables us to see and experience the world around us. The core element of this intricate system lies within the retina - a delicate, light-sensitive tissue situated at the posterior part of the eye. Its crucial role is to convert incoming light into electrical signals, which are then elegantly processed by our brains, giving rise to our vivid perception of the world around us.
A healthy retina is paramount for crystal-clear eyesight. Any deviation from its optimal state can lead to an array of eye diseases, most of which can be diagnosed and tracked through retinal imaging. This type of imaging is a medical technology that enables ophthalmologists to capture and evaluate high-resolution, threedimensional retina pictures, providing critical insight into a patient's ocular health. Retina imaging technologies go beyond the traditional manual visual inspection with dilated pupils and instead offer a non-invasive and painless method to examine the retina, even when the patient is fully awake (Abramoff et al., 2010).
This imaging technology is essential in diagnosing and monitoring eye diseases such as diabetic retinopathy, age-related macular degeneration, and glaucoma. Even more surprising is that this
3
CHAPTER
technology can also lead to diagnoses of other conditions, such as neurodegenerative diseases like Alzheimer's, Parkinson's, and Huntington's.
Retinal imaging is a non-invasive procedure revolutionizing the field of ophthalmology (Nicolosi et al., 2023). It captures a digital image of the retina, optic disc, and blood vessels using a laser ophthalmoscope, providing a comprehensive view of the intricate structures within the eye. Unlike traditional ophthalmoscopy, retinal imaging offers a broader perspective, introducing more precision to eye exams and allowing for more accurate diagnoses (Cleveland Clinic, n.d.).
One of the most notable breakthroughs in retinal imaging is Optical Coherence Tomography (OCT) (Turbert, 2018). Built upon light wave technology, OCT unveils the intricate layers of the retina with remarkable detail (Kulkarni & Deshpande, 2019). By enabling ophthalmologists to examine the retina's microscopic structures, this technology plays a crucial role in the early detection and diagnosis of various ocular conditions (Soomro et al., 2020). The portability and cost-effectiveness of OCT are continually improving (Kulkarni & Deshpande, 2019), ensuring that this invaluable tool is more accessible than ever before.
BetterEyesight 4

SOURCE: Copyright © 2023 by the authors and MDPI, Basel, Switzerland
Compared to traditional retinal photography, OCT 3D retinal scanning offers a more comprehensive view of the retina's structure (Gabriele et al., 2010), making detecting potential eye diseases at an early stage easier. This technology allows healthcare professionals to examine the retina beyond its surface, gaining a better understanding of its layers and structures. The process is painless,
WilliamA.Haseltine,PhD 5
FIGURE 1: (A) The macular hole exhibits hyperautofluorescence on fundus autofluorescence (FAF) imaging. (B) A fundus photograph of the same eye. (C) An optical coherence tomography (OCT) scan of the same eye.
non-invasive, and takes less than five minutes to complete (Aumann et al., 2019).
To fully understand the Ocular Coherence Tomography or OCT process, it is essential to know the retina is scanned with a beam of light. As the light waves penetrate your retina, they are partially reflected by each distinct layer.
The reflected and incoming waves combine to form an interference pattern, generating a 3D image of your retinal structures. Creating a 3D image of the eye's posterior requires multiple high-resolution scans, with around 1,000 images captured during each scan (Gramatikov, 2014). These images are then processed and brought together to yield a comprehensive model showcasing the eye's intricate inner structures, including the fovea, optic nerve, and Henle fibers.
This image's quality and precision depend on the scanning technique employed by your doctor, which can vary depending on your specific needs. One promising method is called Polarizationsensitive Optical Coherence Tomography (PS-OCT). By utilizing the polarization properties of light, PS-OCT can provide highly detailed information about the thickness of your nerve fiber layer, the presence of fluid or blood accumulation, and the overall health of your retina.
A study by the Medical University of Vienna found that PS-OCT provides a highly effective method of detecting and monitoring diseases such as macular degeneration and glaucoma (Baumann, 2017). Another study by the Medical University of Vienna found that PS-OCT is particularly useful for evaluating retinal pigment
BetterEyesight 6
epithelial (RPE) lesions in patients with neovascular age-related macular degeneration (AMD) (Schütze et al., 2015).
Still, more research is needed to understand the full potential of PSOCT in clinical practice. Current data highlights that it could significantly improve the diagnosis and treatment of many eye conditions. When assessing retinal images, doctors look for signs of glaucoma, age-related macular degeneration, diabetic retinopathy, and retinal detachment.

SOURCE: Image by Matthew Strachovsky, M.D. published on navaophthalmic.com
For glaucoma diagnosis, doctors examine the optic nerve head for signs of damage. Any signs of disc cupping or thinning can be indicative of glaucoma. In age-related macular degeneration diagnosis, doctors examine the macula for a buildup of deposits called drusen, bleeding or fluid leakage, or loss of pigment in the
WilliamA.Haseltine,PhD 7
FIGURE 2: Diagram explaining what eye doctors look for in a retinal image
retina. For diabetic retinopathy diagnosis, doctors look for blood vessel abnormalities such as microaneurysms, hemorrhages, and neovascularization. Finally, for retinal detachment diagnosis, doctors look for any signs of detachment or tearing of the retina.
Apart from eye diseases, retinal imaging can also be used as a diagnostic tool for Alzheimer's disease. The retina is considered an extension of the brain, and many studies have shown a correlation between Alzheimer's disease and changes in the retina. Doctors use retinal imaging to identify specific biomarkers in the retina that may indicate Alzheimer's disease. These biomarkers include the thinning of distinct retinal layers and the accumulation of specific proteins.
Capturing a 3D retinal scan is incredibly detailed and comprehensive yet remains quick, safe, and entirely non-invasive. It ensures a painless and comfortable experience for patients. During the scan, patients rest their chin on a chin rest while the scanning device captures multiple images of their eyes. The captured images can be saved and stored for future reference, allowing for comparison with subsequent scans to monitor overall eye health.
3D retinal scans have revolutionized the diagnosis and treatment of eye conditions. They are instrumental in detecting severe eye conditions like glaucoma, macular degeneration, and diabetic retinopathy. These conditions often show no symptoms in their early stages, making them hard to see with traditional diagnostic techniques. 3D retinal scans can identify these problems early, enabling doctors to begin timely treatment and prevent significant vision loss.
BetterEyesight 8
A study by Fudan University in Shanghai explains how clinicians can use these images to diagnose different conditions (Xiaoxi et al., 2022). For instance, the thinning of the retinal nerve fiber layer, inner retinal layer, and choroidal layer, as well as reduced capillary density and abnormal vasodilatory response, have been linked to Alzheimer's disease. These abnormalities can be seen with retinal imaging, allowing earlier diagnosis.
A comprehensive study from 2020 also showed promising results in using non-invasive polarimetric imaging of retinal amyloid deposits as a potential low-cost method for detecting Alzheimer's disease (Snyder et al., 2021). This technique involves using light waves to detect abnormal protein deposits in the retina, which have been linked to the development of Alzheimer's disease.
In addition, a machine learning model has been developed using multimodal retinal imaging data to detect symptomatic Alzheimer's disease (Cheung et al., 2022). This model is based on the analysis of multiple imaging modalities, such as optical coherence tomography and fundus photography, to create a comprehensive picture of the retina and detect any abnormalities that may indicate the presence of Alzheimer's disease.
These advances in retinal imaging technology offer a non-invasive and cost-effective approach to early detection of Alzheimer's disease, potentially allowing for earlier intervention and improved patient outcomes. These scans can also detect other diseases like neurodegenerative diseases such as Parkinson's disease, Lewy body dementia, frontotemporal dementia, Huntington's disease, and multiple sclerosis (Kashani et al., 2021).
WilliamA.Haseltine,PhD 9
Diagnosing Other Diseases with Retinal Images
The eyes are connected to various body organs (American Academy Of Ophthalmology, 2015), such as the skin, joints, and gastrointestinal system. Through this interbody link, the eyes can show signs of diseases such as diabetes, high blood pressure, and cancer. High blood pressure can cause changes to the blood vessels in the eyes, leading to blurry vision or even blindness (The American Heart Association, 2018).
When it comes to the eyes, several signs may indicate the presence of cardiovascular disease. One of these symptoms is double vision or diplopia. This means a person sees two images of a single object instead of one. Double vision can occur in one or both eyes and be constant or intermittent. It may also be accompanied by other symptoms such as headaches, dizziness, and difficulty with balance and coordination.
Another indicator is a yellowish ring around the cornea, an arcus senilis. This ring is usually seen in older adults. Still, when present in younger people, it may suggest high cholesterol levels, which can increase the risk of heart disease.
BetterEyesight 10

SOURCE: EyeNet Magazine by American Academy of Opthalmology
High blood pressure is another sign of cardiovascular disease, and it can cause damage to the blood vessels in the retina. This can result in changes such as narrowing or ballooning. Individuals with cholesterol deposits in or around their eyes are at an increased risk of stroke and heart attack. Moreover, high blood pressure can cause changes in the blood vessels in the retina, leading to the appearance of narrowed, thickened, or even ruptured blood vessels. These
WilliamA.Haseltine,PhD 11
FIGURE 3: A patient with hypertension
changes can be detected through an eye exam and may signal an increased risk of stroke or heart attack.

Retinal vein occlusion is an eye condition that affects the veins in the retina. This condition is often associated with vascular disease.
12
BetterEyesight
FIGURE 4: These diagnostic imaging scans showcase occlusions in arterial (2a) and venous (2b) systems, represented by the black areas.
SOURCE: © AMERICAN ACADEMY OF OPHTHALMOLOGY 2023
It occurs when blood flow through the retinal veins is blocked, causing swelling and bleeding in the eye. Retinal vein occlusion is a severe manifestation of vascular disease. It can be an indicator of significant atherosclerosis in the body. Those with this condition are at a higher risk of developing other cardiovascular problems, such as heart attack or stroke (American Academy Of Ophthalmology, 2015).
It has been found that age-related macular degeneration (AMD), which is a common cause of vision loss for older adults, is linked to cardiovascular disease and stroke. A study by Mount Sinai revealed that patients with cardiovascular disease were three times more likely to suffer from a specific type of AMD, which indicates a close relationship between these two disorders (Mount Sinai, 2022).
Moreover, the appearance of small, yellowish deposits, called drusen, in the retina could also indicate cardiovascular disease. These deposits can cause impaired vision and are commonly seen in individuals with age-related macular degeneration, which has been associated with an increased risk of cardiovascular disease.
Similarly, diabetes can cause damage to the tiny blood vessels in the retina, leading to vision loss. Abnormalities in the retina can also indicate other health conditions, including neurodegenerative diseases such as Parkinson's disease, Lewy body dementia, frontotemporal dementia, Huntington's disease, and multiple sclerosis (Kashani et al., 2021).
For example, in Parkinson's disease, retinal changes such as thinning of the retinal nerve fiber layer and macular modifications can occur. Similarly, in Lewy body dementia, retinal thinning and reduced blood flow to the retina have been observed. In
13
WilliamA.Haseltine,PhD
Huntington's disease, retina degeneration can lead to vision deficits. In multiple sclerosis, a chronic autoimmune disease affecting the central nervous system, microcystic macular edema or outer retinal disruption can be potential biomarkers for early detection.
Early detection and intervention can lead to effective treatment and management strategies, potentially slowing the progression of these diseases and improving patients' quality of life. With the help of retinal imaging, doctors can detect these diseases early, allowing for timely intervention and better outcomes (Xiaoxi et al., 2022b).
Researchers are developing systems that can automatically scan retinal photos for signs of various diseases, including cardiovascular disease. These systems can analyze extensive datasets of retinal images with documented disease outcomes by leveraging machine learning algorithms. By discerning nuanced patterns or abnormalities, they have the potential to indicate the presence of diseases.
Studies have shown that this approach has yielded promising results (Muchuchuti & Viriri, 2023). If successful, it can significantly improve the efficiency and accuracy of retinal screening, leading to earlier disease detection and better patient outcomes, particularly in the case of cardiovascular diseases (Choudhary et al., 2023).
Retinal imaging also has some limitations that are worth mentioning. One of the primary limitations of retinal imaging is that patients with cataracts or other media opacities may face challenges with the procedure (Patel et al., 2020). This is because these conditions can scatter light in the eye, interfering with the quality of the retinal image captured. Additionally, the cost of retinal imaging may be a barrier for some patients. However, recent
BetterEyesight 14
technological advances have made it more affordable (Gulledge, 2011).
It is also essential to note that retinal imaging is just one tool used for diagnosing and monitoring eye conditions. While it provides valuable information about the retina's health, it cannot replace a thorough bedside examination performed by an experienced ophthalmologist. Therefore, retinal imaging should be used as a complementary tool to a comprehensive eye exam rather than a replacement for it.
Partners to Retinal Imaging: Targeted Spectroscopy in the Eye Fundus & Electroretinography
A promising technology in diagnostic imaging is targeted spectroscopy in the eye fundus (Lapointe et al., 2023). It allows for simultaneous eye fundus imaging and analysis of high-quality spectra from specific eye regions. This non-invasive approach provides valuable information about the eye fundus's structure, composition, and function, making it a handy tool for various applications.
Targeted ocular spectroscopy is an advanced imaging system using state-of-the-art technology to analyze the eye fundus comprehensively. This system combines two advanced technologies: the confocal scanning laser ophthalmoscope (CSLO) and the Fourier-transform spectrometer (FTS) (Fromow-Guerra, 2012).
The CSLO technology allows imaging of the eye's fundus, which is the eye's interior surface that consists of the retina, optic disc, and macula. The FTS collects spectra from specific regions of interest
WilliamA.Haseltine,PhD 15
within the imaged area, using Fourier transform spectroscopy to measure light intensity at different wavelengths. This allows the identification and quantification of various chemical compounds in the imaged area. One such compound is lipofuscin, a metabolite that increases in the retina as a person ages. The FTS can also detect other biomolecules like melanin, hemoglobin, and cholesterol (Shi, Hu et al., 2022).

SOURCE: Journal of Biomedical Optics
The combination of CSLO and FTS technologies in targeted ocular spectroscopy provides a detailed analysis of the eye fundus, which helps detect and monitor various eye diseases such as agerelated macular degeneration, glaucoma, and diabetic retinopathy
BetterEyesight 16
FIGURE 1: The targeted spectroscopy in the OEMI-7 eye model consists of four distinct regions: A, representing the blood vessels; B, the retina near the optic nerve head; C, the optic nerve head itself; and D, the retina far from the optic nerve head
(Lapointe et al., 2023). This advanced imaging system has revolutionized the field of ophthalmology and is a valuable tool for clinicians and researchers.
The combination of imaging and spectral analysis provided by this system offers a wealth of information on the composition and function of the eye fundus. For instance, it can detect changes in the concentration of oxygen, lipids, glucose, and other metabolites in the retina. It can also provide information on blood flow, inflammation, and other physiological parameters for assessing disease progression and treatment efficacy.
A recent study on the eye has shown that ocular spectroscopy can effectively analyze different eye regions, such as the optic disc, blood vessels, retina, and macula, by identifying distinct spectral signatures (Lapointe et al., 2023 These signatures correspond to the variations in tissue composition and function in each region, making ocular spectroscopy a precise and unique method for eye analysis.

SOURCE: Translational Vision Science & Technology
17
WilliamA.Haseltine,PhD
FIGURE 6: Color-coded oximetry vessel map
Ocular oximetry is an algorithm that measures blood oxygen saturation levels in healthy patients' optic nerve heads and parafovea (Garg et al., 2021). This is essential for detecting and monitoring diseases like glaucoma and diabetic retinopathy. The results of this algorithm have shown significant differences in oxygen saturation levels between various regions of the eye, providing valuable insights into the physiology and pathology of ocular diseases.
Numerous clinical trials have been conducted to evaluate the effectiveness of targeted ocular spectroscopy. One study aimed to determine if targeted ocular spectroscopy could be used to track the progression of age-related macular degeneration (AMD) (Flores et al., 2021). The results of the study showed that changes in the spectral signatures of the macular pigment were strongly associated with changes in the severity of the disease. This suggests that targeted ocular spectroscopy is a valuable tool for monitoring the progression of AMD.
Another study investigated the use of targeted fluorescence spectroscopy to detect and quantify the levels of specific intracellular proteins associated with glaucoma (Fernández-Vega Cueto et al., 2021). The study found that targeted fluorescence spectroscopy was highly influential in detecting the presence of these proteins, which could potentially be used as a biomarker for glaucoma diagnosis and monitoring.
Targeted ocular spectroscopy is a promising technology that can help diagnose and monitor ocular and neurological diseases. Despite some limitations, such as the ability to detect spectral changes in small retinal structures, this technology has already shown significant success in clinical trials. Researchers and clinicians can use it to measure oxygen saturation in vivo and
BetterEyesight 18
identify intracellular proteins associated with specific diseases. As this field progresses, we can expect more breakthroughs in diagnosing and treating ocular and neurological diseases.
Another promising technology, not unlike the imaging technique just discussed, is electroretinogram. It provides a glimpse into the cellular orchestra, enabling our sense of sight through light-induced responses. This tool helps to assess the functionality and health of retina cells. It is crucial for early detection and diagnosis of eye diseases (Yang et al., 2021). Electroretinography provides objective and quantifiable assessments of visual function and retinal wellbeing (Wolpert & Tsang, 2011). With the help of such evaluations, ophthalmologists can make informed decisions about patient care and treatment strategies, leading to optimal outcomes.
The procedure consists of multiple steps. Firstly, numbing drops are given to the patient to ensure comfort during the test. Then, a small speculum gently holds the patient's eyes open. Subsequently, an electrode is placed on each eye to measure the retina's electrical activity in response to light. After that, a light stimulus is presented, and the resulting electrical response is captured by the electrodes and displayed on a monitor for viewing and recording. The test is conducted in both light and dark rooms to allow the patient's eyes to adjust.
WilliamA.Haseltine,PhD 19

FIGURE 7: A: Device positioning for eye recordings using electroretinography (ERG). B: Example ERG responses to standard light-adapted flash stimuli. C: Device screen showing ERG recording setup, with visible eye and detected pupil (highlighted by blue circle).
D: Responses to standard light-adapted 30 Hz flicker stimulus.
SOURCE: Copyright © 2023 Omar A. Mahroo
An electroretinogram output consists of two essential components: the A-wave and the B-wave (Mahroo, 2023). The A-wave is a positive wave mainly from the eye's cornea. At the same time, the B-wave is a negative wave that represents the electrical response of the retina's rods and cones to light. By carefully analyzing these waves, ophthalmologists can detect any abnormalities in the structure and function of the retina, facilitating early detection and diagnosis of eye diseases.
BetterEyesight 20
The beauty of electroretinography lies in its effectiveness (Yang et al., 2021). Even before symptoms manifest, the test can pinpoint dysfunctions within the eye, establishing electroretinography as one of ophthalmology's most proactive diagnostic measures. Beyond its fundamental diagnostic capabilities, electroretinography boasts several advantages over other tests.
Electroretinography features a heightened level of sensitivity that allows it to identify even the slightest abnormalities in the retina (Yang et al., 2021). It can also discern between various retinal disorders. Another advantage is that the testing method is noninvasive, making it a safe and comfortable option for patients (Hong et al., 2022).
The introduction of multifocal electroretinography has further broadened the horizons of this testing method (Mahroo, 2023). This technique allows clinicians to map localized functional issues within the retina, providing intricate retinal assessments with exquisite detail. With this level of precision, clinicians can develop highly targeted treatment plans that address specific retinal issues, resulting in better patient outcomes.
However, like all medical procedures, this test has some limitations (Justus, 2021). The traditional full-field electroretinography resolution may not be able to identify localized retinal abnormalities (Ramkumar et al., 2015). Also, patient cooperation can sometimes be a hurdle. While this test provides a spectrum of diagnostic insights, it may not always give a definitive diagnosis.
Despite these limitations, the future of electroretinography looks promising, with the potential for advances. The field is constantly evolving with technology-enhancing precision (Mahroo, 2023).
WilliamA.Haseltine,PhD 21
This progress is essential as accurate diagnosis and treatment planning play a crucial role in safeguarding our vision, one of our most precious senses.
Approximately 285 million people worldwide are visually impaired, with the leading causes being cataracts, glaucoma, diabetic retinopathy, and age-related macular degeneration (Lee & Mesfin, 2020). Timely detection and diagnosis of eye diseases are crucial for successful treatment and prevention of vision loss. The high prevalence of eye diseases globally highlights the importance of diagnostic tools such as electroretinography.
Furthermore, electroretinography's significance also lies in its promise for the future. Continued research and development may offer even greater detail and specificity in diagnosing and managing retinal conditions. For patients with vision impairments and those at risk for retinal diseases, the advancements in electroretinography represent a beacon of hope an assurance that the vigilant eyes of science protect our sight.
Migraines and the Eye
A new study published in the journal Headache sheds light on the link between migraines and the eye, revealing new potential biomarkers for this complex condition (Podraza et al., 2023). If you are one of the more than one billion people who suffer from migraines, you know they can come with a variety of sensations and pains (American Migraine Foundation, 2019). If you don’t live with migraines, imagine this.
You’re sitting at your desk, your eyes glued to the computer screen, and you feel a strange sensation creeping up on you. Suddenly, your
BetterEyesight 22
vision becomes fuzzy and distorted, and despite your best efforts, the sensation persists.
In disbelief, you watch flashing lights and zigzag patterns dance before your eyes, accompanied by a tingling sensation that spreads across your face and hands. The aura envelopes you, making it hard to focus on your work. You realize this is a migraine aura, a warning sign that an overwhelming headache may be coming. Migraines can be debilitating, affecting approximately 12% of the population globally (Cleveland Clinic, 2021). Intense headaches often characterize them but can cause visual disturbances, such as flashing lights or blurry vision. A lesser-known aspect of migraines is their potential impact on the retina, the thin layer of tissue that lines the back of the eye.
Over the years, multiple theories have been proposed to explain the mechanisms underlying this debilitating condition (Glover & Sandler, 1989). One of the most well-accepted hypotheses is the neurovascular theory, which proposes that both neural and vascular components interact to trigger a migraine attack (Mason & Russo, 2018). The theory suggests that an initial neuronal event within the brain leads to a cascade of events culminating in a neurovascular headache.
Another theory that holds considerable clout is the neurogenic theory, which maintains that migraines are primarily a neurogenic process with secondary changes in cerebral perfusion (Spekker et al., 2021). This robust theory suggests that neuronal hyperexcitability, neurogenic inflammation, and neurovascular disorders all play a role in the development and maintenance of migraines.
WilliamA.Haseltine,PhD 23
While still theoretical, emerging research investigating the molecular and genetic bases of migraines may, in time, provide us with even more insights into the complex physiological mechanisms underlying this enigmatic and enervating condition. For now, it's essential to explore the types of migraine and how we can "see" them in the retina.
Migraines are a type of headache that can be debilitating and affect people's quality of life. They are classified into two main types: migraines with and without aura. An aura is a sensory experience that precedes or accompanies a migraine episode and can manifest differently in different people.
Visual auras are the most common type of aura experienced by people with migraines. These can include seeing flashing lights, zigzag patterns, or blind spots in their vision. Some people may see bright lines or spots that move across their field of vision. Visual auras can last for several minutes to an hour and can be followed by a headache.

SOURCE: By Migraine Canada
BetterEyesight 24
FIGURE 8: Types of Migraine Auras
Various types of auras can cause sensory disturbances such as tingling or numbness in the face or hands. This sensation can be similar to pins and needles or an electric shock. During an aura, some individuals may experience difficulty speaking or expressing themselves. They may also have trouble remembering words or names. Migraines associated with these symptoms are commonly referred to as hemiplegic migraines (National Organization for Rare Disorders, Inc., 2015).
It's important to note that not everyone with migraines experiences auras. However, for those who do, they can be a helpful warning sign that a headache is on its way.
The relationship between migraines and the retina has been a research topic for several years, with evidence pointing to reduced blood flow and abnormal vascular function in the retina during migraine episodes (Demircan et al., 2015). However, the traditional methods for studying the retina are limited in their ability to capture these phenomena, leading researchers to explore new imaging technologies such as optical coherence tomography angiography (OCTA).
The study published in Headacheused technology called OCTA to look at the tiny blood vessels in the eyes of people who get migraines. They compared people with migraines during and between attacks, as well as healthy people. The study found less blood flow to the retina during migraine attacks. This was true for both migraines, with or without an "aura."
The interictal analysis, performed when the patient is not experiencing a migraine episode, revealed a significant difference in the blood perfusion of the foveal region between patients with
WilliamA.Haseltine,PhD 25
migraines with aura and those without aura. The fovea is a small, central retina area that provides sharp and detailed vision.

SOURCE: Headache: The Journal of Head and Face Pain published by Wiley Periodicals LLC on behalf of the American Headache Society.
The study suggests that distinct retinal vascular signatures might be potential biomarkers for migraines. The finding of lower blood perfusion in the foveal region in patients with migraines with aura compared to those without aura suggests that there might be a correlation between this particular region of the retina and the occurrence of migraines with aura.
These findings have important implications for diagnosing and treating migraines, as they suggest that different types of migraines may have distinct physiological characteristics that can be identified through retinal imaging. This could lead to more accurate diagnoses and personalized treatment plans for migraine patients.
BetterEyesight 26
FIGURE 9: Visualization of the interictal foveal vessel flux index (VFI) in a representative healthy control (HC), migraine with aura (MA), and migraine without aura (MO) participant.
The study's sample size is small, including only 37 patients with migraines with aura, 30 with migraines without aura, and 20 healthy controls. Regardless of this limitation, the study's findings are significant, and they have the potential to lead to better diagnosis, treatment, and prevention strategies for migraines. Finding biomarkers to distinguish between migraines and track their progression over time could be a breakthrough. It's essential to continue research in this direction.
The researchers acknowledge that the mechanisms underlying migraines and their relationship with the retina are not fully understood. However, their study provides new clues and evidence for further exploration. In the future, doctors and researchers can use OCTA to track changes in the retina and adjust treatment plans accordingly. This could lead to a brighter future for those affected by migraines, offering new hope for relief and a better quality of life.
Brain Machine Interface & Implants
New brain implants allow blind users to see using prosthetic electrodes in their visual cortex. There are roughly 40 million people worldwide who have blindness and an additional 250 million with moderate-to-severe visual impairment (Orbis, 2022). Most blindness is brought about through injury or aging. In contrast, others are born with genetic conditions resulting in a lack of sight. While complete restoration of eyesight through medical intervention is still impossible, new brain implants may enable significant restoration.
WilliamA.Haseltine,PhD 27
The NeuraViPeR project was started in the EU in late 2020 to provide an affordable prosthetic vision replacement for more than 2.5 million blind Europeans.
The final product is scheduled for mass availability in 2025; detailed studies on the implants are still underway. However, the researchers behind the project have released other data I will piece together here (King, 2023).
The first human test subject for NeuraViPeR was fitted with a small implant in the brain’s visual processing cortex. In sight-abled people, when light hits the retina, photoreceptors in the eye translate the light to electrical signals interpreted by the brain in the visual cortex. Blindness typically involves the degradation of the retina or the optic nerve that connects the eyes to the brain. An implant to the visual cortex bypasses these damaged regions.
The patient’s implant consisted of just under 100 microelectrodes, which the user could activate and see despite their blindness. The implant was digitally connected to a pair of glasses fitted with a video camera that captured movement and relayed that information to the implant, just as our eyes do for the visual cortex.
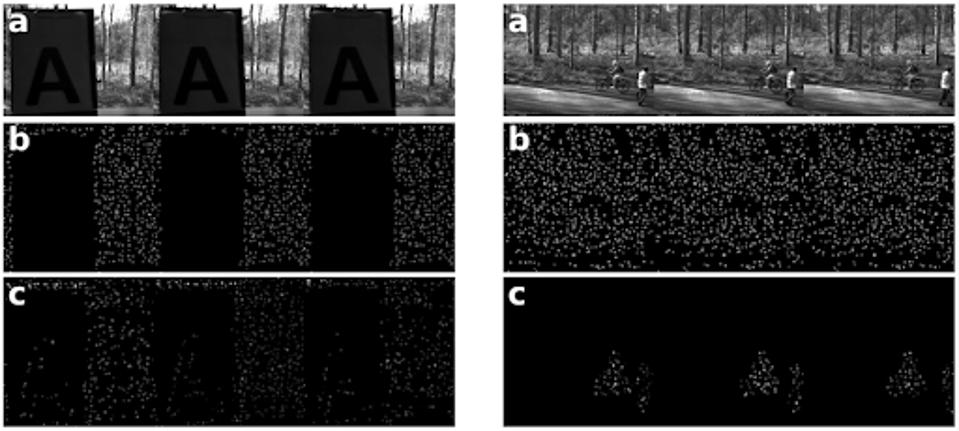
The electrodes then activate when the user’s glasses detect movement, resulting in sight for people who are blind. The following was taken from a preliminary study using the same technology.
BetterEyesight 28
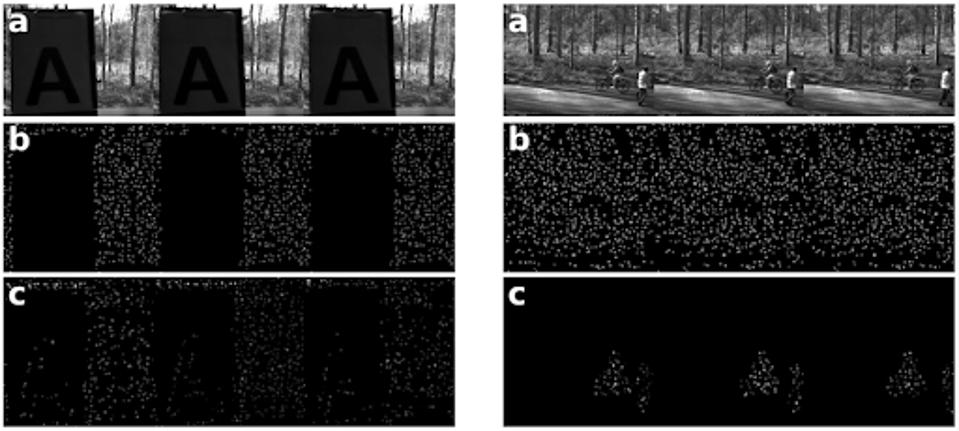
SOURCE: Rueckauer et al.
The electrodes are capable of detecting the edge of an object as well as the motion. Unfortunately, detailed imagery is complex, with only 96 electrodes within the implant. Normal human vision has a resolution of one million pixels. As such, detailed vision through an implant with a magnitude of fewer electrodes is not yet possible.
The researchers suggest that for a blind person to navigate a room or discern a face easily, the implant would need between 1,000 and 2,000 electrodes. The transfer of information between the visual processor and brain implant must also speed up. In addition to the image quality being low with only 96 electrodes, the frame rate is also low due to the slow processing of visual data through the implant.
A separate project, HyperStim, began in November 2022 to address processing speed alongside the NeuraViPeR project. Through an objective lens, the final version of the technology is still years away. The researchers must still create implants containing 10 to 20-fold
WilliamA.Haseltine,PhD 29
FIGURE 10: Image recognition by visual prosthetic using (B) edgebased recognition vs (C) event-based recognition as compared to (A) the original image.
denser electrode bunches and much faster processing systems for the implants.
However, blindness was once a life sentence, with little to no options in terms of therapy. NeuraViPeR and HyperStim are significant steps in the right direction. They may yield tangible blindness-inhibiting prosthetics in only a few short years.
Thanks to the work of scientists from the University Miguel Hernández, we are now further along the way to restoring vision for blind people (Fernández et al., 2021). In October, Fernández et al. successfully implanted an array of microelectrodes into the visual cortex of a fifty-seven-year-old woman who has been fully blind for the past sixteen years (Fernández et al., 2021). After training, the woman could visualize several complex patterns and identify some letters. This demonstrated the potential of array microelectrodes for restoring some rudimentary vision.
The ability to restore vision is one of the holy grails of regenerative medicine. I have previously written about the potential of optogenetics in this field. Still, this study presents real progress for using direct electrical stimulation in the brain instead.
Close your eyes and rub your eyelids. What do you see?
Most people will report seeing multi-colored dots or patterns of light. These dots of light are called phosphenes and are what researchers aim to induce in blind patients as a form of rudimentary vision. Past studies have used electrical stimulation directly on the brain's surface to induce phosphenes in blind individuals. However, there were significant limitations to this approach. When multiple electrodes were stimulated simultaneously, the phosphenes would
BetterEyesight 30
blur together rather than create two distinct shapes or dots. This made shape recognition difficult, if not impossible.
In addition, high levels of electrical current were required even to begin to stimulate phosphenes. This limited the clinical application of electrical stimulation in vision because high current levels can damage neurons or induce seizures.
To address these issues, Fernández et al. experimented with an array of electrodes that penetrate deeper into the brain. The theory was that if the electrodes could initiate the activity of neurons more deeply in the visual cortex, they would not require as much current to induce phosphenes in the patient’s vision. Electrodes with less current could also safely be placed closer together, potentially increasing visual resolution. This would allow patients to distinguish discrete shapes and patterns.
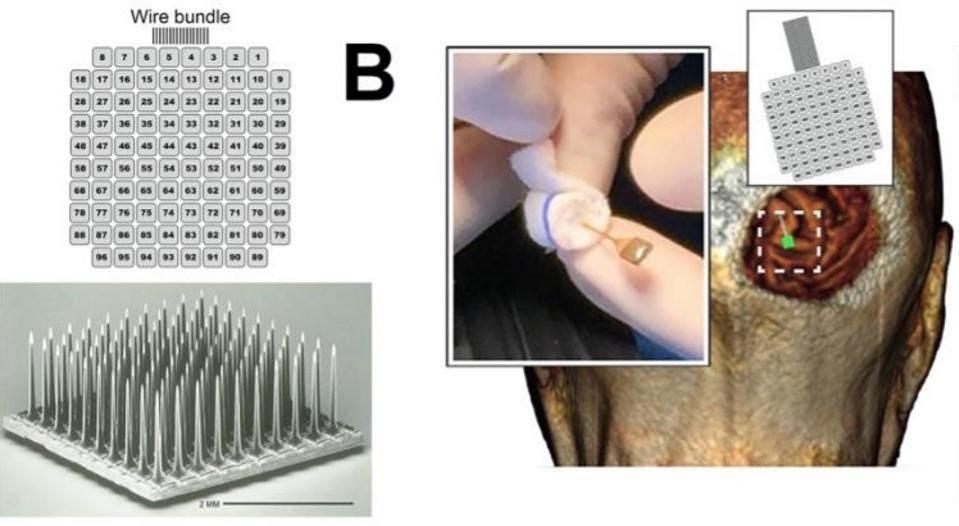
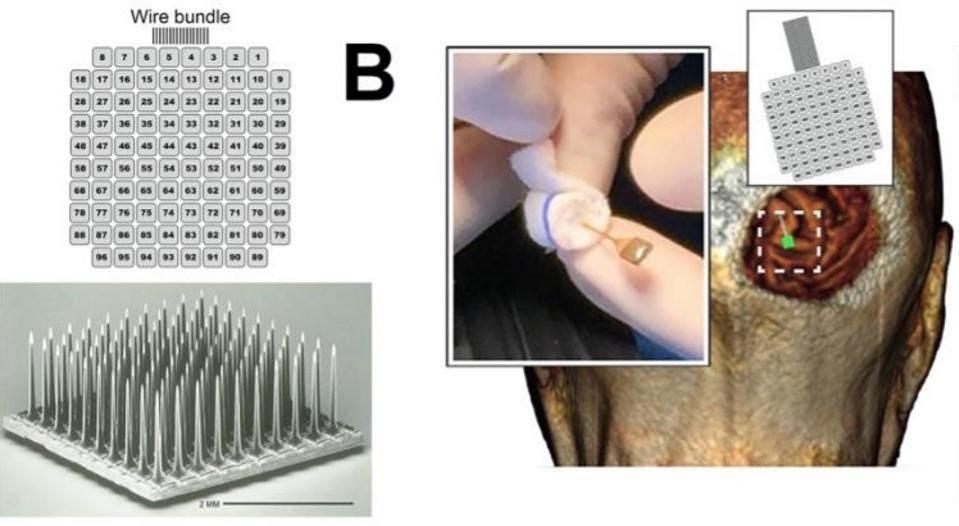
SOURCE: The Journal Of Clinical Investigation, Fernández, E. et al.
Recent experimentation provided an optimistic foundation for the penetrative electrode array system. The device was successfully
WilliamA.Haseltine,PhD 31
FIGURE 11: Microelectrode array and implantation
implanted in monkeys, allowing them to recognize simple shapes, motions, and letters.
One complication of electrically induced phosphenes in blind patients is that blind patients often experience spontaneous phosphenes regularly. The first step of the electrode implant experimentation was to see if the patient could discriminate between a spontaneous phosphene and an electrically induced one. To test this, researchers used an auditory tone that they played before they induced an electrical signal and when they were not inducing a signal.
The patient would press a button if she thought that she saw an electrically induced phosphene after the tone. After two months of daily experimentation, the patient began reliably differentiating between the two and correctly identified 947 out of 1000 electrically induced phosphenes.
One of the more crucial aspects of the experiment was whether penetrative electrode arrays produced higher-resolution images. To test this, researchers ran stimulation experiments with 50 pairs of electrodes. They found that in 23.6% of the simulations, the patient saw two discrete phosphene images. Surprisingly, electrodes that were just 400 micrometers apart were able to generate separate perceptions. These results demonstrate that the penetrative electrode array can achieve distinct images with electrodes five times closer than what has been achieved with direct surface stimulation, marking a vast improvement from previous methods.
Fernández et al. also found that the timing of electrode stimulation could be used to produce discrete images. This could be useful
BetterEyesight 32
when attempting to create more complicated patterns recognizable to the patient.
Further testing on the relationship between electrode current and the color and brightness of phosphenes showed that more significant currents produced brighter and whiter light. In comparison, smaller currents made phosphenes that were sepia in color and much dimmer. The patient could accurately differentiate between currents based on color and brightness.
After determining the vision characteristics produced by penetrative electrode arrays, researchers were ready to test the patient with complex 2D patterns. They simultaneously stimulated combinations of 3 to 16 electrodes to produce patterned stimuli. The patient would then draw what she saw. The overall success rate of these pattern recognition experiments was 81.4% and improved as training continued.

SOURCE: The Journal Of Clinical Investigation, Fernández, E. et al.
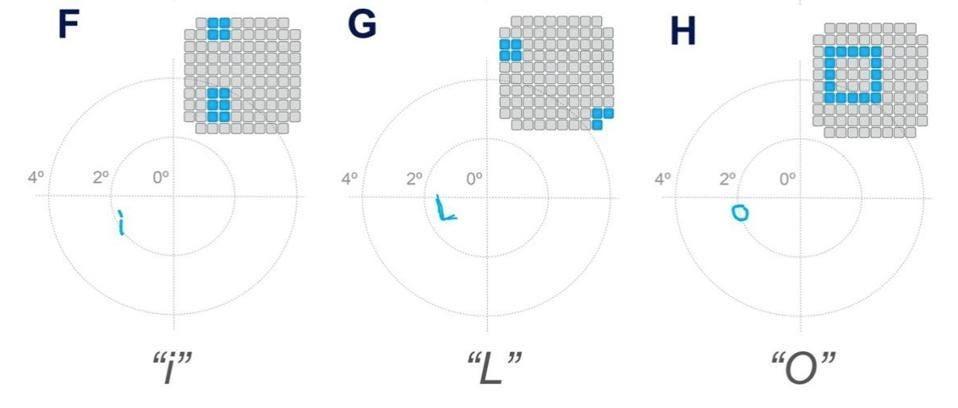
Motivated by the success of these results, Fernández et al. then tested the patient’s ability to recognize letters using the same experimental model. The patient was able to consistently recognize some letters, such as “I,” “L,” “C,” “V,” and “O,” but was
WilliamA.Haseltine,PhD 33
FIGURE 12: Pattern recognition test results.
inconsistent or unable to recognize others. Overall, her success rate for each trial always exceeded 70%.
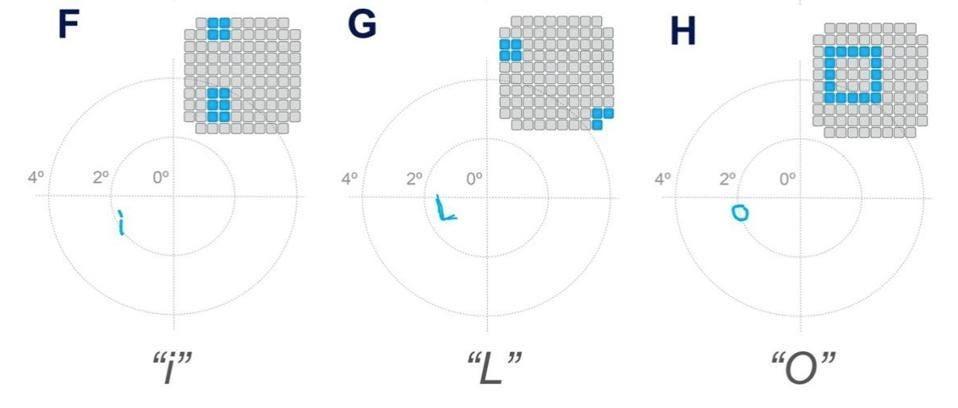
FIGURE 13: Letter recognition test results.
SOURCE: The Journal Of Clinical Investigation, Fernández, E. et al.
Finally, researchers experimented with a bio-inspired retina-like visual encoder to delve into the clinical applications of a penetrative microelectrode array system. The visual encoder is a pair of glasses that features a camera. The camera acts as an artificial retina. It records visual inputs in real-time and translates them into electrode stimulation patterns that can cause accurate phosphene visualizations in the patient. To investigate how the visual encoder could work with the microelectrode array system, the patient used the visual encoder to scan an image of black and white bars printed on cardboard. She was then asked to locate the borders between the black and white bars. They then repeated similar experiments using images on a computer monitor. After just two days of training, the patient could correctly locate features of an image 100% of the time.
BetterEyesight 34

SOURCE: The Journal Of Clinical Investigation, Fernández, E. et al.
Irrespective of damage done to the structures of the eye or the retina, this study offers a direct way of interfacing the visual world with the brain. The combination of neuroscience, microelectronics, and miniaturized high-powered computation made this study possible. These three fields are advancing at record speeds. As we develop a deeper understanding of each field, we can anticipate substantial progress in restoring vision to those with optical damage or even to those who have lost their eyes through the technology of direct brain stimulation.
Aging and the Eye
As we age, our vision changes, making us more susceptible to medical conditions. Some of the most common changes include difficulty seeing things up close, developing cataracts, and struggling to differentiate between colors. Even though these
WilliamA.Haseltine,PhD 35
FIGURE 14: Bio-inspired retina-like visual encoder.
changes can be frustrating, they are crucial to maintaining good eye health and preventing age-related eye problems.
Our eyes undergo natural physiological changes that can lead to various eye-related issues as we grow old. The lenses in our eyes become less flexible, making it harder to focus on objects. Also, the number of light-sensitive cells in our retina decreases over time, causing a decline in visual acuity. These age-related changes can give rise to various eye issues such as presbyopia, glaucoma, cataracts, and dry eyes.
Presbyopia is a gradual loss of the ability to see objects up close, typically affecting people in their 40s and beyond. It occurs due to a hardening of the lens in the eye and a decrease in its elasticity. As a result, it becomes more challenging to focus on nearby objects, such as reading material or computer screens.
Cataracts are another common age-related problem that affects many people. They occur when the proteins in the eye's lens break down and clump together, causing cloudiness and decreased vision. Cataracts can develop slowly and may not cause significant vision problems at first. However, as they progress, they can cause blurred vision, difficulty seeing in low-light conditions, and even blindness.
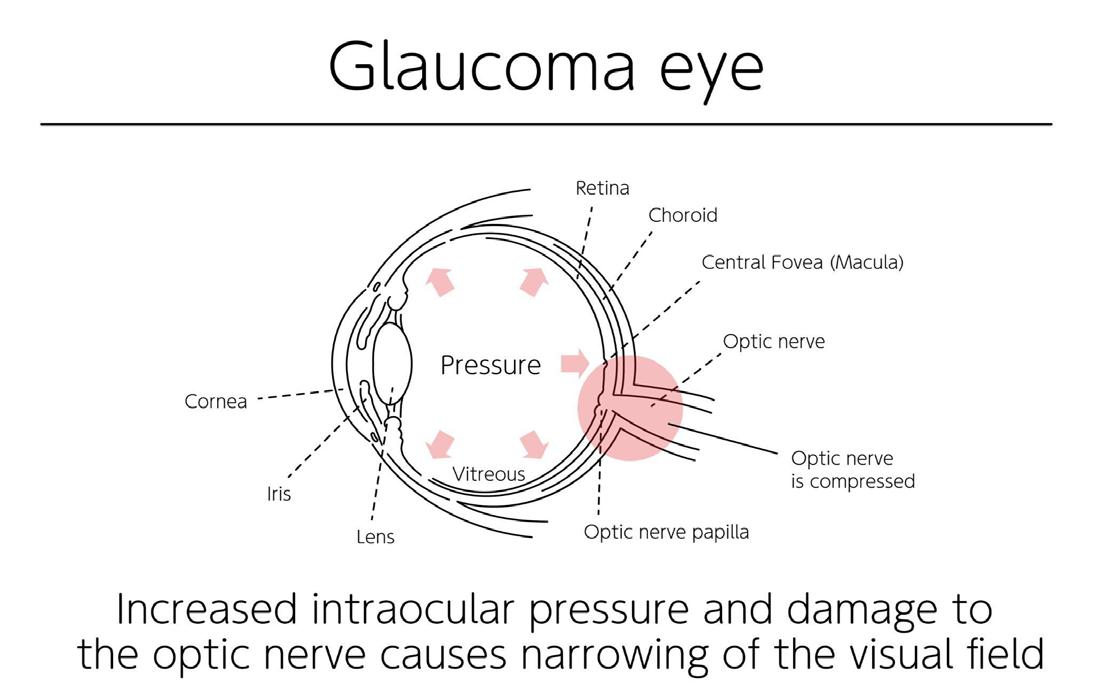
Glaucoma is a group of eye diseases that damage the optic nerve and can lead to vision loss or blindness. It typically occurs due to increased pressure within the eye, which can damage the optic nerve over time. Glaucoma can develop slowly and may not cause noticeable symptoms until significant vision loss occurs.
Finally, dry eyes occur when the eyes do not produce enough tears or when the tears evaporate too quickly, leading to discomfort and
BetterEyesight 36
vision problems. It is a common condition that can cause eye itching, burning, and redness.
A recent clinical trial has shown promising results in reducing keratoconus progression through corneal collagen crosslinking (Wittig-Silva et al., 2014). Keratoconus is a condition that causes the cornea to become thin and bulge outward, leading to distorted vision and increased sensitivity to light. The trial's results have opened up new possibilities for treating this condition and improving the lives of those affected.
In addition, gene therapy has shown potential in slowing the progression of retinitis pigmentosa. This degenerative eye disease affects approximately one in 4,000 people. Retinitis pigmentosa causes damage to the retina, leading to vision loss over time. While there is no cure for this disease, gene therapy offers hope for slowing its progression. This new therapy involves replacing or repairing faulty genes in the retina, which has shown promising results in animal studies.
As you advance in age, it is critical to be mindful of your eye health to preserve your vision. Along with scheduling regular eye exams, you can implement several other strategies to keep your eyes healthy.
Firstly, wearing sunglasses that offer adequate UV protection helps shield your eyes from harmful rays that could lead to the development of cataracts and other eye conditions. Secondly, quitting smoking is crucial as it has been linked to higher risks of age-related macular degeneration (AMD), cataracts, and other eye problems. Additionally, maintaining a healthy weight, consuming a balanced diet rich in fruits and vegetables, and taking supplements
WilliamA.Haseltine,PhD 37
such as omega-3 fatty acids and vitamins C and E have been shown to help prevent specific eye problems.
Staying hydrated is essential for maintaining healthy eyes and preventing dryness and irritation. Finally, using brighter lights in your home and keeping your living space clutter-free can help prevent accidents and reduce the likelihood of falls, which can be especially dangerous for older adults.
Although age-related eye problems are common, there are several measures you can take to minimize the risk of developing them (Jun, 2021). By leading a healthy lifestyle and scheduling regular eye exams, you can maintain good eyesight for many years. With ongoing research, new treatments and therapies may become available, providing even more options for protecting aging eyes.
The Eye's Microbiome and Its Importance for Our Health
In the depths of your eyes, a thriving metropolis of microorganisms exists, which could potentially revolutionize our understanding of eye health. Scientists are mapping this frontier, which may bolster our vision and eye health from this microscopic level (Willcox, 2013).
Although the words "bacteria" and "microorganism" may initially evoke thoughts of infection, these tiny creatures are the unsung heroes of our eyes' microbiome. Their constant watchfulness helps maintain good eye health by fighting off pathogens and regulating the immune system despite being invisible to the naked eye (Bunya & Rana, n.d.).
Recent research has shown that, contrary to popular belief, the eye is not an isolated organ and, much like our skin and gut, is host to various microorganisms (Peter et al., 2023). The ocular microbiome
BetterEyesight 38
is rich in microorganisms, especially on the conjunctival membrane (Leger et al., 2017). Although the ocular microbiome is less diverse than the skin microbiome, it still contains many microorganisms, approximately 1/100th of the total found on the skin (Mukamal, 2019).
The microbiome of our eyes is inhabited by four primary bacterial groups: Staphylococcus , Streptococcus , Propionibacterium , and Corynebacterium (Mukamal, 2019). Though these four aren't the only microorganisms in the eye microbiome, they are often found in the largest quantities.

FIGURE 15:
based on 16S rRNA gene sequencing. Dong et al. (2011) examined a total of 115,003 sequences, Huang et al. (2016) analyzed 840,373 high-quality sequencing reads, and Zhou et al. (2014) generated 1,690,427 reads.
SOURCE: © 2020 by Petrillo et al.
Over the years, scientists have conducted numerous studies to unravel the connection between the ocular microbiome and various
WilliamA.Haseltine,PhD 39
Comparative ocular surface microbiota composition analysis
eye diseases (Xue et al., 2021). These studies have revealed that an imbalance in the microbial population in the eyes can trigger inflammation, leading to several conditions, such as chronic dry eye and blepharitis (Bunya & Rana, n.d.).
For example, chronic dry eye is a common condition that affects individuals of all ages. It occurs when the eyes fail to produce sufficient tears to lubricate the eye surface, resulting in dryness, irritation, and discomfort. Multiple factors, including age, medications, and environmental elements, can contribute to this condition. However, recent research suggests that an imbalance in the ocular microbiome may also play a role (Willis et al., 2020).
Researchers continue to delve into these clinical enigmas, aiming to identify the underlying causes of these conditions and develop targeted treatment approaches (Peter et al., 2023). The implications of this research can potentially revolutionize the treatment of ocular diseases.
The complexity of the eye's microbiome is being increasingly recognized, and with that recognition comes the responsibility to maintain its delicate balance. Age, ethnicity, geographic location, and lifestyle choices like wearing contact lenses can all affect the microbiome's equilibrium, leading to adverse health outcomes. Awareness of these factors can help prevent disruptions in the ocular microbiome's harmony.
Scientists are using their newfound knowledge to develop treatments that target imbalances in the microbiome. Different treatments, such as antibiotics, phage therapy, and probiotics, are available, each with unique challenges and opportunities. While antibiotics can eradicate harmful bacteria, they can also disrupt
BetterEyesight 40
beneficial ones (Xue et al., 2021). On the other hand, phage therapy offers precision in eliminating unwanted bacterial growth (Xue et al., 2021). Probiotics are also a potential solution as they can modulate the gut microbiome and improve ocular health (Petrillo et al., 2020).
Our understanding of the microbiome is evolving, leading us towards treatment and prevention. Through groundbreaking research, we are identifying pathways that could reduce the risk of eye diseases and maintain microbial equilibrium to prevent them from developing. This shift in perspective is significant as it acknowledges the potential of harnessing the microbiome's power to prevent diseases from taking root.
The ocular microbiome holds immense potential for researchers who seek to understand its impact on eye health. Our current knowledge is only the tip of the iceberg, and future studies will delve deeper into the microbiome's interactions with various eye conditions. These findings could lead to the development of novel treatments that enhance our quality of life.
Rare Eye Disease: Epidermolysis Bullosa
In a groundbreaking development, gene therapy delivered through eye drops has restored the sight of Antonio Vento Carvajal, a teenager who has been legally blind for most of his life (Ungar & Frisaro, 2023). Antonio was born with dystrophic epidermolysis bullosa, a rare genetic condition that causes blisters all over his body and eyes (Mayo Clinic, 2018). After participating in a clinical trial for topical gene therapy, which initially targeted his skin, Dr.
WilliamA.Haseltine,PhD 41
Alfonso Sabater had the idea to adapt the treatment for Antonio's eyes.
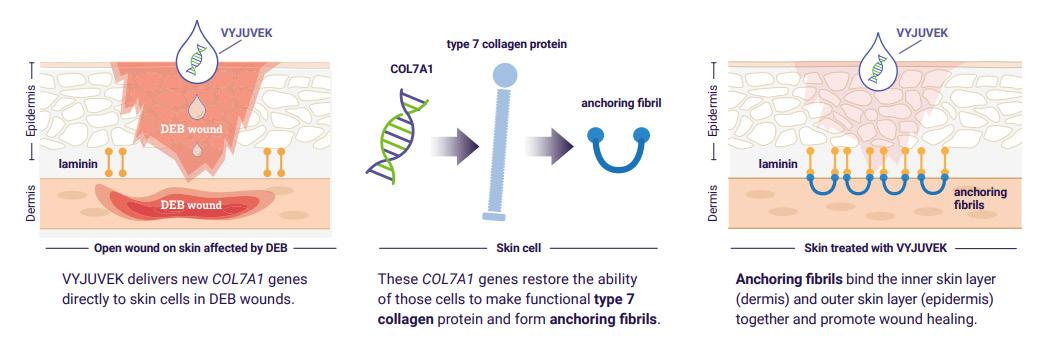
The Vyjuvek, formerly known as B-VEC, treatment uses an inactivated herpes simplex virus to deliver working copies of the gene responsible for Antonio's condition (Staff, n.d.). The results have been remarkable, with Antonio's vision significantly improving and the scarring in his eyes disappearing. This breakthrough offers hope for Antonio and opens the door to similar therapies that could benefit millions of people with other eye diseases.
Epidermolysis Bullosa, commonly called EB, is a group of rare inherited skin disorders that cause the skin to be very fragile. A faulty gene mutation in COL7A1 causes the condition. Those with EB find that any trauma or friction to the skin can cause painful blisters to form.

SOURCE: CDC Public Health Image Library
BetterEyesight 42
FIGURE 16: This image depicts the lower extremities of an infant, revealing bullous, erythematous lesions due to a condition known as epidermolysis bullosa (EB)
The severity varies from person to person and can range from mild to severe. There are also specific subtypes of the disorder that are host to different characteristics. Depending on the type and severity of EB, patients may also face complications such as infection, anemia, growth issues, and vision problems.
Most people with the disease are battling blisters across their hands and feet and thickened skin. As the skin constantly fights trauma, it will thicken over time, scar, and change color. Blisters can also form on the internal epidermis, such as in the mouth and through, making eating difficult.
Treatment for EB aims to relieve symptoms and prevent complications. Currently, it has no cure, so treatment focuses on supportive care. This care includes wound care, pain management, nutritional support, physical therapy, and psychological support.
One FDA-approved treatment for EB is currently available and making waves (Capaldo et al., 2023). This treatment is Vyjuvek or beremagene geperavec. It is a treatment specifically created for patients with dystrophic epidermolysis bullosa (DEB) and the first topical gene therapy to receive approval in the US.

SOURCE: © Krystal Biotech, Inc.
WilliamA.Haseltine,PhD 43
FIGURE 17: Adapted from De Rosa L, Latella MC, Secone Seconetti A, et al. Cold Spring Harb Perspect Biol. 2020
It is important to note that Vyjuvek is only approved for treating wounds related to dystrophic epidermolysis bullosa and is not a complete treatment for all types of epidermolysis bullosa.
Vyjuvek is a gene therapy gel that delivers a healthy copy of the gene, encoding the protein type VII collagen to targeted skin cells. The protein anchors the layers of skin together to promote healing.
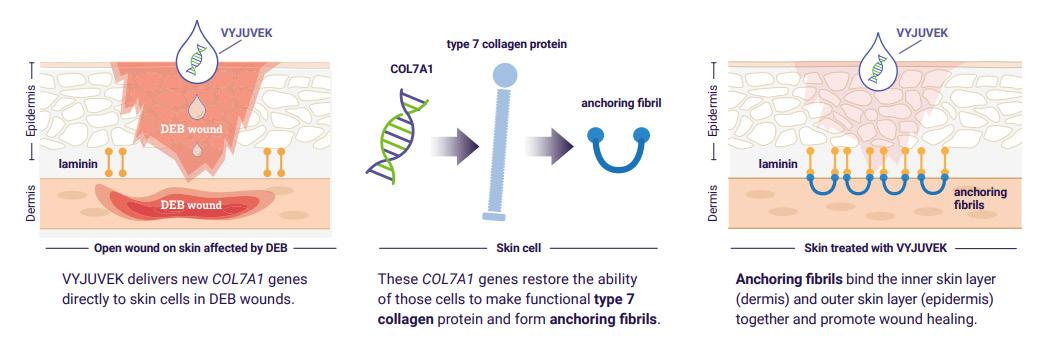
FIGURE18: Adapted from De Rosa L, Latella MC, Secone Seconetti A, et al. Cold Spring Harb Perspect Biol. 2020
SOURCE: © Krystal Biotech, Inc.
The drug delivers functional copies of the COL7A1 gene directly to the wound. It does this by using a modified herpes simplex virus type. The functional gene then produces a kind of collagen to start wound healing.
Before being approved by the FDA (FDA, 2019), Vyjuvek underwent two significant clinical trials (Staff, n.d.). These trials aimed to assess the drug's safety and effectiveness in treating wounds caused by DEB (Krystal Biotech, Inc., 2023-b). Seventeen patients participated in the studies, and the medication was well-tolerated, with no severe complications reported. A phase III trial was also completed (Krystal Biotech, Inc., 2023a). After three months of treatment, significantly more wounds treated with Vyjuvek had healed than those treated with a placebo. After six months, 65% of
BetterEyesight 44
wounds were healed in those using Vyjuvek compared to 26% in those using the placebo.
Given its positive safety record and promising trial outcomes, exploring alternative medicinal uses that could improve the quality of life for individuals affected by DEB seemed reasonable. The remaining questions are how they did it and how it restored a young boy's vision.
Initially, the Vyjuvek formulation utilized a gel infused with a herpes simplex virus type to deliver the COL7A1 gene to wounds. However, further modifications were necessary to accommodate its use in the eye.
The new version of the formula does not contain gel, but the original formulation remains unchanged. This latest version allows Vyjuvek to be given through eye drops, which deliver the COL7A1 gene directly to the eye. This process efficiently generates collagen seven within the cornea, crucial for maintaining its structural integrity. Insufficient levels of collagen seven can cause corneal dystrophy, leading to vision impairment. However, with Vyjuvek, restoring collagen seven levels and reversing the effects of corneal dystrophy is now possible, ultimately resulting in improved vision. This method has seen success in the recent trial with young Antonio. Still, only one case was under "compassionate use" approval from the US Food and Drug Administration (Hutton, 2023). Those involved in Antonio's case exercised extreme caution and were always considering the safety of the treatment. This caution was significant as Vyjuvek doesn't modify DNA, so it is not a one-time treatment like many gene therapies.
WilliamA.Haseltine,PhD 45
Ultimately, the trial was successful as Antonio's eye fully recovered from the surgery, and there has been continuous improvement every month without any scarring. The results were so promising that the medication is now allowed off-label use for the eyes.
Though there may not be specific plans for clinical trials of Vyjuvek for eye diseases at the moment, the success of this therapy in restoring vision in dystrophic epidermolysis bullosa patients opens up possibilities for future research and development in the field of gene therapy for other eye diseases.
Organoids and Transplants
One of the more significant advances in understanding human organs and cell biology is the ability to grow miniature versions of human organs in a cell culture. These are called organoids and are an emerging area of research that allows scientists to understand the root causes of diseases, how to treat them, and potentially how to rebuild the organs themselves.
Many organoids begin as pluripotent stem cells. Pluripotent stem cells are derived from the skin or blood and are reprogrammed into earlier embryonic stages of cell development. The embryonic cells can then be turned into almost any other cell in the body. If nudged in the right direction, these cells can develop into the equivalent of mini-functional organs or, in some cases, the specific tissue of an organ.
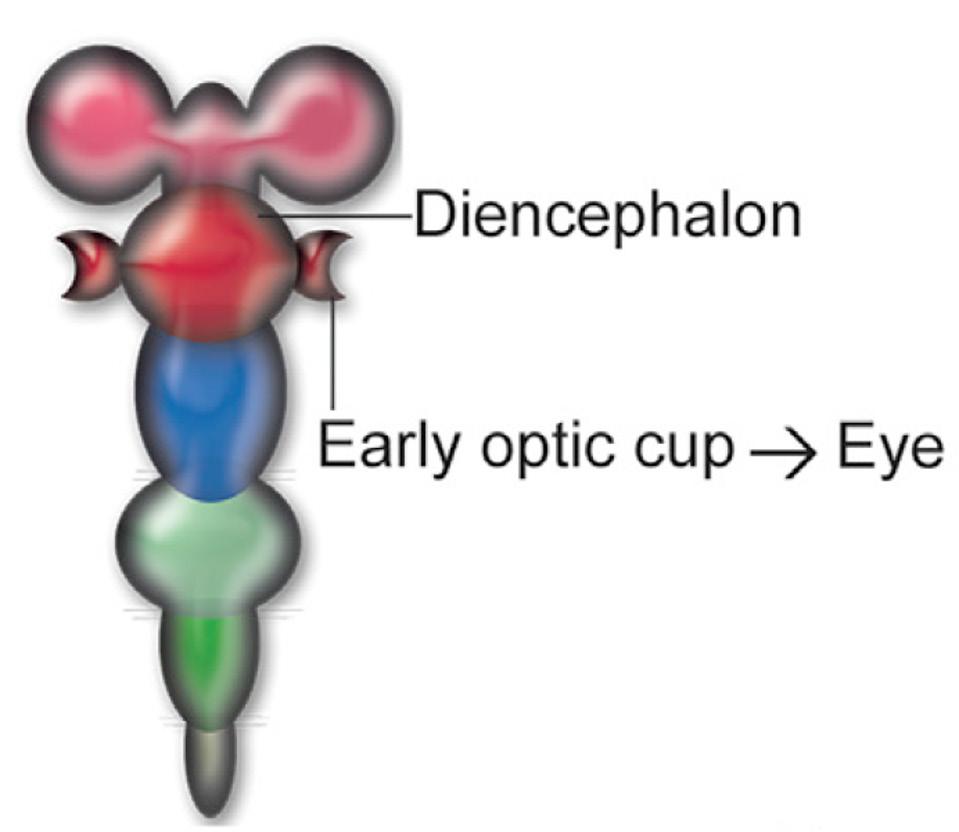
However, the brain is the most exciting and cryptic of all the organs of interest. A recent report published by scientists from the Institute of Human Genetics at Heinrich-Heine University displays
BetterEyesight 46
significant progress in developing brain organoids and, surprisingly, ones with rudimentary eyes (Gabriel et al., 2021).

SOURCE: Cell Stem Cell, G. Elke, W. Albanna, et al.
Our sensory organs, particularly our eyes and ears, are brain extensions. Though often considered discrete structures, the eye’s retinal cells are classified as neurons. Pure brain organoids have been grown in the past. However, because of the relationship between the eyes and the brain, researchers at Heinrich-Heine University were particularly interested in addressing whether we can grow brain organoids that contain these rudimentary optic structures.
The researchers began by first forming generic brain organoids. As expected, the organoids did not form any visible optic vesicles. However, they did display genetic markers for retinal and other eye cells. This prompted the researchers to alter their approach.
Previous studies have demonstrated that retinoic acid is a crucial signal for retinal cell development. Retinoic acid inhibits brain
WilliamA.Haseltine,PhD 47
FIGURE 19: Brain organoids with rudimentary eyes after 30 days of development
tissue growth, where the optic cup develops. With this information, researchers first conditioned pluripotent stem cells to differentiate into neural cells to form the generic brain organoid. As the brain organoid was forming, they introduced retinoic acid into the cell culture.
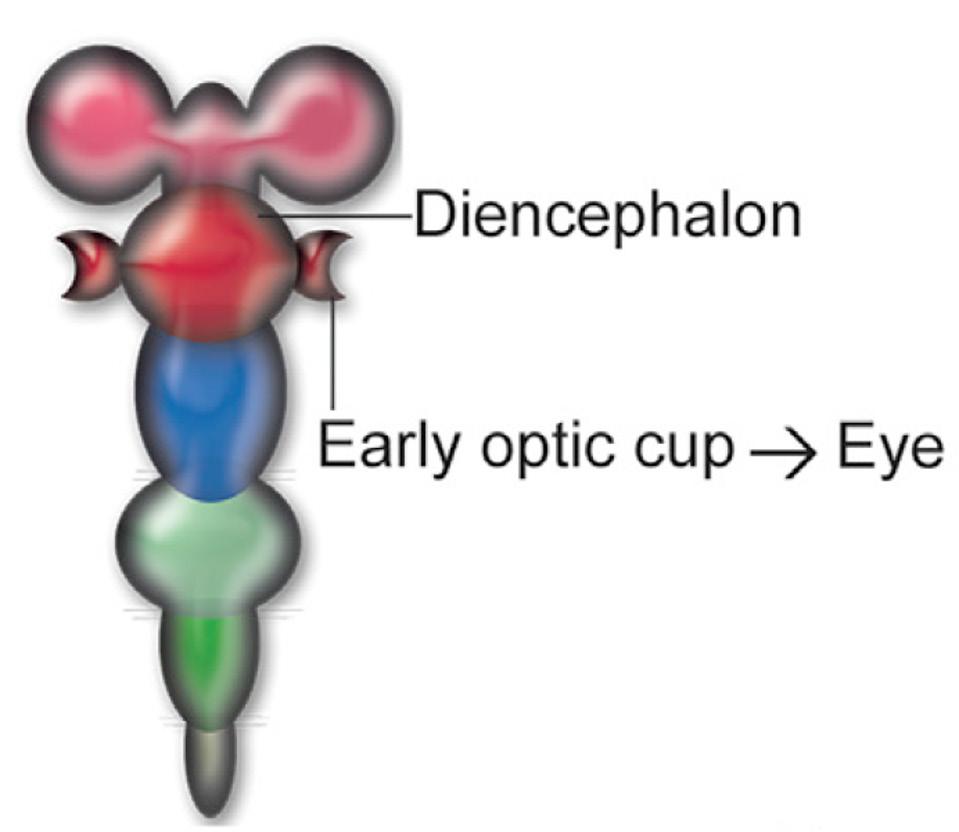
SOURCE: Cell Stem Cell, G. Elke, W. Albanna, et al.
To their surprise, after 60 days, the brain organoid formed highly pigmented areas that resembled a pair of eyes. Analysis of the organoid revealed that eight different cell populations were produced by adding retinoic acid. These included the generic brain organoid cell types, cells responsible for forming the optic cup, and cells necessary for retina development.
BetterEyesight 48
FIGURE 20: Diagram displaying optic cup placement

SOURCE: Cell Stem Cell, G. Elke, W. Albanna, et
al.
Not only this, but certain cells were responsive to light. In the human brain, particularly in the retina, cells will display higher or lower activity levels in the presence of light. These are called photosensitive cells. When photosensitive cells in the brain are suddenly exposed to bright lights, they are rendered inactive. After exposure to darkness, photosensitive cells reactivate and display normal responses to light. Researchers tested this ability in the organoids and found that they could recover their photosensitivity, matching the light reactions of eyes in vivo .
This study is an exciting step forward for brain research and research about the highly specialized organ of the eye. With this progress, the hope is that researchers will have the foundation to push further and begin to understand how eyes are generated. This may directly
WilliamA.Haseltine,PhD 49
FIGURE 21: Brain organoids with rudimentary eyes after 60 days of development.
impact our understanding of heritable diseases in the eyes and how to repair optic defects acquired during our lives.
Visual Plasticity
Visual plasticity is crucial in understanding how our eyes process visual information. Studies have revealed that not just the brain adapts to visual stimulation but also our eyes and their nerves (Rosa et al., 2013). Specifically, our retinal nerves adapt from light to dark environments.
This phenomenon is something that everyone can relate to daily. When we walk from outside on a sunny day into a dark room, our eyes take some time to adjust to the darker conditions. This is because our retinal nerves adapt to the new lighting conditions, allowing us to see the new environment properly.
The process of visual plasticity is complex, involving numerous interrelated components. However, we know that one of the critical factors involved is the retina, the specialized layer of cells at the back of the eye responsible for detecting and transmitting visual information. These cells allow our eyes to sense changes in light and darkness and send signals to our brain to process that information. Visual plasticity is a complex and dynamic process that refers to the brain's ability to adapt and change in response to visual stimuli. This adaptability occurs at various levels of processing, from the initial stages of visual perception to higher cognitive functions such as attention and memory.
At higher levels of processing, visual plasticity can involve changes in how visual information is integrated with other types of sensory and cognitive information. For example, the brain can adjust its
BetterEyesight 50
visual information processing to changes in auditory or tactile stimuli or cognitive factors such as attention, motivation, or emotion.
At the sensory level, visual plasticity involves changes in how visual information is processed and represented in the brain. For example, the brain can adjust its sensitivity to different wavelengths of light to optimize visual perception in other lighting conditions (Spring et al., 2019).
This adjusting sensitivity to light is one of the most well-known examples of visual plasticity. Our pupils immediately begin to enlarge or contract in response to fluctuations in light intensity. This rapid and automatic response allows our eyes to regulate the amount of light that enters and falls upon the retina, sending electrical impulses to the brain for visual processing.
The retina also undergoes changes to better process different lighting conditions. For example, the photoreceptor cells in the retina adjust their sensitivity in response to changes in light levels so that they can pick up more detail in dimmer lighting or reduce glare in brighter lighting. These adjustments are all made on the fly without us even realizing it's happening.
The eye plays a crucial role in visual plasticity as it gathers and transmits visual information to the brain. The retina, located at the back of the eye, contains photoreceptor cells called rods and cones that detect light and send signals to the brain through the optic nerve. The brain then processes this information to create the visual perceptions that we experience.
Studies have shown that the eye can change in response to visual stimuli, both through physical changes in the structure of the eye
WilliamA.Haseltine,PhD 51
and through changes in how the brain processes visual information (Hunter et al., 2019). For example, research has demonstrated that exposing mice to bright light can cause changes in the structure of the cells in the retina and changes in the levels of specific proteins (Rattner et al., 2008). These changes are involved in visual adaptation, allowing the animals to better adjust to changes in their visual environment.
A recent study published in Current Biology sheds new light on visual plasticity and its link to the eye (Maharjan et al., 2020). The study, conducted by researchers at the University of California, Berkeley, examined mice's visual systems to understand better the neural mechanisms involved in visual adaptation.
The researchers found that exposure to different types of visual stimuli caused changes in the activity of specific neurons in the retina and the brain. These changes were linked to changes in the behavior of the mice, suggesting that the visual plasticity that occurred was functionally relevant.
The study is critical because it provides new insights into how the brain processes visual information and adapts to changes in the visual environment. It also has potential implications for developing new treatments for vision-related disorders, such as amblyopia and age-related macular degeneration.
We can better understand how our brains process and interpret visual information through extensive research in this domain. By leveraging this knowledge, we can develop various techniques and tools to enhance our vision and cognitive abilities. This can lead to numerous benefits, such as improved learning, memory, visual acuity, and perception. With continued research, we can broaden
BetterEyesight 52
WilliamA.Haseltine,PhD
our knowledge of visual plasticity and uncover novel ways to enhance our brain function and overall well-being.
53
Conjunctivitis

Millions of individuals in the United States suffer from conjunctivitis (Ryder & Benson, 2020), commonly known as pink eye, which is the inflammation of the thin, transparent membrane covering the eye's white part. The cost of managing bacterial conjunctivitis in the United States annually amounts to 857 million US dollars (Ryder & Benson, 2020).
Although most cases of conjunctivitis are not severe, some types can lead to blindness if left untreated. Conjunctivitis can be classified into three main types: bacterial, viral, and allergic.
An allergic reaction causes the allergic type of conjunctivitis. It can cause symptoms such as redness, itching, tearing, and eye swelling. Treatment for allergic conjunctivitis involves avoiding the allergen, using antihistamine eye drops or oral medications, and sometimes using corticosteroid eye drops for severe cases.
Viral conjunctivitis is an eye infection primarily caused by the common cold or the herpes simplex virus, which is also responsible for cold sores. This highly contagious infection can spread through direct or indirect contact with an infected eye. Symptoms of the condition include redness, itching, burning, watery discharge, sensitivity to light, and sometimes, a gritty sensation. It typically begins in one eye and eventually spreads to the other. Unfortunately, there is currently no specific treatment available for viral conjunctivitis.
54
CHAPTER 2

SOURCE: ACCESS Health International
Bacterial conjunctivitis is caused by certain types of bacteria, including Streptococcus pneumoniae, Haemophilus influenzae, and Staphylococcus aureus. This kind of eye infection spreads quickly through direct or indirect contact. Symptoms include redness, swelling, itching, and discharge from the eye. The discharge may be transparent or yellow and can cause the eyelids to stick together, especially after waking up. The cornea may become infected in severe cases, leading to vision problems. Treating bacterial conjunctivitis often involves antibiotic eye drops or ointments, which help relieve symptoms and clear up the infection.
Allergic Conjunctivitis
Allergic conjunctivitis is a common and debilitating condition affecting millions globally. It is characterized by a chronic inflammation of the eyes, which is triggered by exposure to allergens
WilliamA.Haseltine,PhD 55
FIGURE 22: Diagram showing bacterial conjunctivitis in human eye
such as pollen, dust, and pet dander. While some over-the-counter and prescription antihistamine medications offer relief from symptoms, these treatments are often inadequate or cause side effects. For this reason, allergen immunotherapy has emerged as a promising treatment for managing allergic conjunctivitis.
Immunotherapy is a modern treatment that aims to boost the immune system's ability to identify, locate, and eliminate diseasecausing organisms and abnormal cells. This technique involves using drugs, vaccines, or other substances to stimulate or regulate the body's natural immune responses, intending to train the immune system to recognize and attack specific disease cells or agents.
It has been recognized as a potential treatment for various illnesses and disorders, including autoimmune disorders, infectious diseases, and allergies. In recent years, studies have found that immunotherapy can be highly effective in treating various forms of cancer, leading to long-lasting remissions and improved quality of life for cancer patients. While more research is needed to determine its full potential, immunotherapy is already considered one of the most promising approaches to treating various diseases.
Immunotherapy is an effective treatment method for individuals suffering from allergic conjunctivitis that reduces the sensitivity to allergens. This is achieved by administering small doses of the allergen over time, which helps to train the immune system to become less reactive to the substance.
Two main types of immunotherapy are used to treat allergic conjunctivitis: sublingual immunotherapy (SLIT) in the form of tablets and subcutaneous immunotherapy (SCIT) in the form of
BetterEyesight 56
injections. SCIT involves injecting allergens under the skin, while SLIT involves placing allergens under the tongue.
One study published in the Allergy, Asthma & Clinical Immunology journal (Dupuis et al., 2020) provided a detailed analysis of both forms of immunotherapy and their effectiveness in managing allergic conjunctivitis. The study found that subcutaneous therapy (SCIT) has strong evidence supporting its efficacy in improving symptoms of conjunctivitis caused by different allergens.
In contrast, the evidence for the tablet form (SLIT) is limited and varies depending on the allergen. For example, SLIT has shown significant efficacy in reducing ocular redness, itch, and tearing in pollen-induced allergic conjunctivitis. Still, its effectiveness in house dust mite-induced allergic conjunctivitis needs to be wellestablished.
Another study, published in the Current Opinion in Allergy and Clinical Immunology journal (Norris et al., 2020), also reviewed the findings of various clinical trials that examined allergen immunotherapy for treating allergic conjunctivitis. The study noted that subcutaneous immunotherapy (SCIT) carries a higher risk of systemic reactions, such as anaphylaxis, which can be lifethreatening.
On the other hand, sublingual immunotherapy (SLIT) has a higher rate of mild-to-moderate adverse events, particularly during the first month of treatment. SCIT is generally preferred for cost-benefit analyses as it offers greater efficacy and lower discontinuation rates.
A further study in the medical journal Allergy & Rhinology (Carr et al., 2016) explored the potential use of a sublingual immunotherapy
WilliamA.Haseltine,PhD 57
tablet as a treatment option for allergic conjunctivitis. The study involved 152 randomly assigned participants to receive either the sublingual immunotherapy tablet or a placebo for 12 months.
The study results showed that the participants who were given the sublingual immunotherapy tablet experienced a significant reduction in their symptoms of itching, tearing, and congestion. Specifically, the study found that the immunotherapy tablet was highly influential in managing these symptoms, with a statistically significant difference observed between the treatment group and the placebo group.
Another option for treatment is an antihistamine, and mast cell stabilizing eye drops provide relief from the symptoms. Antihistamine eye drops are a medication used to treat allergic conjunctivitis, in which the eyes become irritated and inflamed due to an allergic reaction. These eye drops contain antihistamines, which are drugs that work by blocking histamine receptors in the eyes. Histamine is a chemical released by the body in response to allergens, and it is responsible for causing symptoms like itching, redness, and swelling.
By blocking histamine receptors, antihistamine eye drops prevent the release of histamine and reduce the severity of allergy symptoms. This makes them an effective treatment option for people who experience allergic conjunctivitis. A study published by the University of Oulu (Honkila et al., 2022) found that eye drops containing antihistamines and steroids were highly effective in treating this condition, with symptom relief observed in as little as 24 hours.
BetterEyesight 58
Mast cell stabilizing eye drops work by preventing the activation and release of histamine, prostaglandins, and leukotrienes from mast cells, which reduces inflammation and alleviates allergy symptoms. Mast cell stabilizers take a few days to work but provide long-term relief from allergies.
Bacterial Conjunctivitis
Specific strains of bacteria such as Streptococcus pneumoniae, Haemophilus influenzae, and Staphylococcus aureus cause Bacterial Conjunctivitis Bacterial conjunctivitis. This highly contagious condition is easily transmitted through direct or indirect contact, leading to symptoms like redness, swelling, itching, and discharge from the eye. The discharge can cause eyelids to stick together, particularly after waking up. In severe cases, the infection can spread to the cornea, resulting in vision problems. Fortunately, antibiotic eye drops or ointments can alleviate symptoms and clear up the infection. A study published in the Journal of Ophthalmic & Vision Research (Azari & Arabi, 2020) has shown that antibiotic eye drops are highly effective in treating bacterial conjunctivitis. The study found that these eye drops successfully treated the infection in 96.8% of cases.
Antibiotic eye drops contain active ingredients that target the bacterial cell wall. The cell wall is an essential component of the bacteria's survival mechanism. Antibiotics bind to the bacterial cell wall, disrupting its integrity and causing it to rupture and die. As a result, the infection resolves, and the symptoms subside.
Bacterial conjunctivitis is commonly treated with polymyxin B, bacitracin, and erythromycin. The antibiotic choice depends on the
WilliamA.Haseltine,PhD 59
infection's severity, the patient's age, and any underlying medical conditions. Completing the entire course of antibiotics is crucial to effectively eliminate the disease, even if the symptoms have subsided. Failure to do so may cause a relapse of the condition and increase the risk of antibiotic resistance.
A newer option for treating bacterial infections is bacteriophagebased treatments. Bacteriophages are a type of virus that are naturally occurring organisms in our ecosystem. They hold a critical role in regulating and developing microbial communities. As such, they have been extensively studied and used in various fields, including phage display, cancer cell targeting, drug delivery, diagnostic applications, gene delivery, and nanoprobes. However, it is essential to note that using bacteriophages as therapeutic agents is still unproven. Definitive controlled clinical trials are needed to assess its general applicability.
Recently, research has explored their potential use in combatting the rising issue of antibiotic resistance, which has become a severe problem due to the overuse and misuse of antibiotics. Bacteriophages have also drawn attention as therapeutic agents to treat bacterial ocular infections, as indicated in a study published in the Frontiers in Pharmacology (Kaur et al., 2021). The authors demonstrated the efficacy of using bacteriophages to treat bacterial conjunctivitis in the survey.
Researchers have developed nanotechnology-based delivery strategies to deliver bacteriophages to the site of infection. A study published in The Journal of Microbiological Methods (Patil et al., 2023) revealed the promising results of nanotechnology in delivering bacteriophages to treat ear infections. In this study, the authors used chitosan nanoparticles to deliver bacteriophages to the
BetterEyesight 60
site of infection, which reduced the bacterial load and inflammation.
Another study published in the Nanomaterials journal (Paczesny & Bielec, 2020) explored the potential use of liposomes to deliver bacteriophages to the site of infection. The authors showed that the bacteriophages were stable and effective at killing pathogenic bacteria, offering a promising alternative to antibiotics.
Using bacteriophages in nanotechnology-based delivery strategies can provide several advantages. They are precise and only target the bacteria causing the infection, leaving other bacteria unharmed. This reduces the risk of developing antibiotic resistance and minimizes potential side effects. Furthermore, bacteriophages can penetrate biofilms that otherwise protect bacteria from antibiotics, as noted in the study.
Treatments
Significant advances in eye drop technology have transformed the treatment of eye diseases. Eye drops have a lower risk of adverse effects and provide the flexibility to develop combination eye drops that contain numerous active ingredients. Patients with sensitive eyes or long-term treatment requirements can benefit from improved treatment outcomes by creating preservative-free eye drops.
Ongoing research and development in this field are paving the way for even more improvements in eye drop technology. One such development is using nanoparticles to deliver medication directly to the eye, reducing the need for frequent administration and improving treatment outcomes. Another promising development is
WilliamA.Haseltine,PhD 61
gene therapy to treat genetic eye diseases, which could provide a permanent cure for these conditions.
Overall, the continued advances in eye drop technology are a promising sign for those with eye diseases. With further research and development, we can expect to see even more innovative treatments that will improve the quality of life for patients and reduce the burden of eye diseases on society.
BetterEyesight 62
CHAPTER 3
Corneal Disorders and Diseases

The cornea is a transparent, dome-shaped layer that covers the front of the eye, contributing up to two-thirds of the eye's focusing power (Sridhar, 2018). It consists of five layers, each with its specific function.

SOURCE: Yue Ruan, Subao Jiang, Aytan Musayeva, Norbert Pfeiffer, and Adrian Gericke
The cornea, the eye's transparent outer layer, has four main layers. The epithelium is the outermost layer that acts as a barrier to protect the cornea from any damage or infection.
Bowman's thin connective tissue layer is the next layer, which provides structural support to the cornea. The stroma is the thickest
63
FIGURE 23: The localization of limbal epithelial stem cells and the anatomy of the cornea.
layer, making up 90% of the cornea's thickness, and is responsible for most of the cornea's refractive power (Ophthalmic Consultants of Vermont, n.d.). Descemet's membrane is a thin layer between the stroma and the endothelium, the innermost layer that regulates the transport of fluids in and out of the cornea.
Corneal Transplants
Corneal transplant surgery has come a long way since its inception in 1905 (McGhee et al., 2013). This surgical procedure involves the replacement of a damaged or diseased cornea with a healthy one. It is one of the most frequently transplanted tissues worldwide, with the US alone performing an astonishing 48,000 procedures annually (Cleveland Clinic, 2023).
The advances in this field over the past century have significantly increased the rate of success and visual recovery. From the first crude techniques to modern-day precision surgeries, the evolution of corneal transplants has paved the way for innovative breakthroughs.
There are different types of corneal transplant procedures available, including penetrating keratoplasty (PK), which replaces all corneal layers; deep anterior lamellar keratoplasty (DALK), which involves the replacement of all layers except for the endothelium; and Descemet's stripping automated endothelial keratoplasty (DSAEK), which replaces only the endothelium (Colby, 2021).
BetterEyesight 64
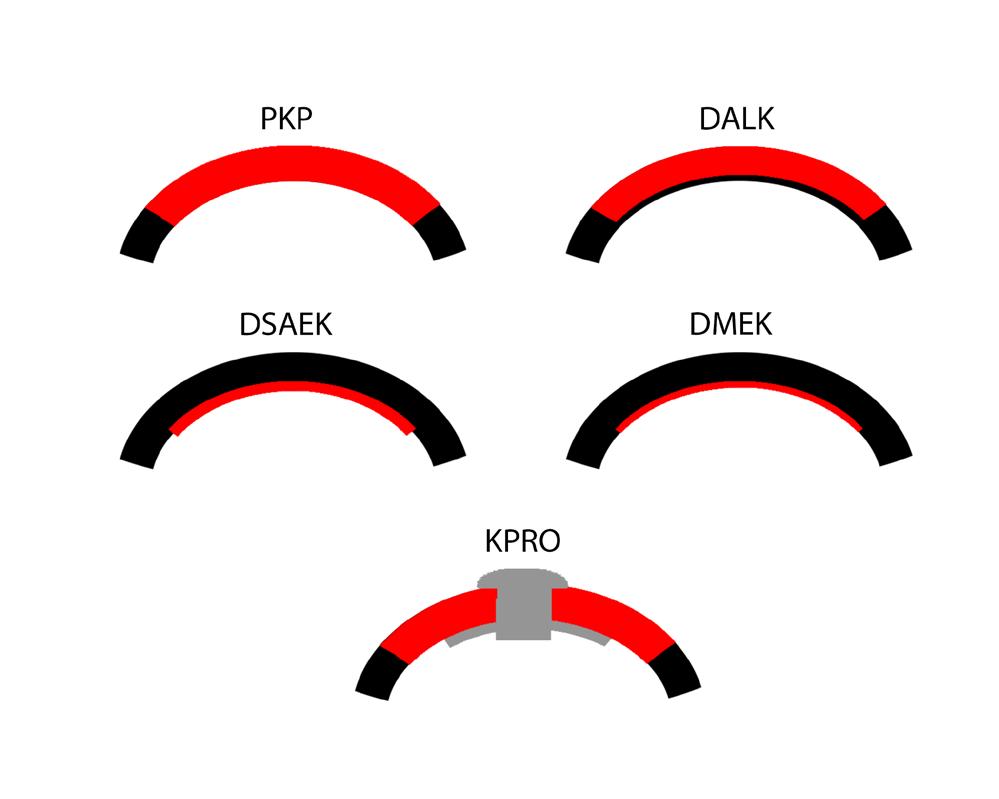
FIGURE 24: Diagram showing corneal tissue transplants (red) used in modern keratoplasty techniques: penetrating keratoplasty (PK), deep anterior lamellar keratoplasty (DALK), Descemet stripping automated endothelial keratoplasty (DSAEK), Descemet membrane endothelial keratoplasty (DMEK), and Boston Type I Keratoprosthesis (KPRO).
SOURCE: Donaghy CL, Vislisel JM, Greiner MA. An Introduction to Corneal Transplantation.
Corneal transplant is a standard treatment for several conditions, including keratoconus, a condition where the cornea becomes thin and cone-shaped; Fuchs' dystrophy, a condition that causes the endothelium to deteriorate; and corneal scarring due to injury or infection. The success rate of corneal transplants is high, and the procedure has helped restore vision in millions of people worldwide.
Corneal transplant surgeries are performed to help restore vision in individuals who have damaged or diseased corneas. The success rate of these surgeries varies depending on several factors, including the
WilliamA.Haseltine,PhD 65
reason for the surgery and the surgical technique used (Williams et al., 1995). For instance, transplants performed for keratoconus, where the cornea becomes thin and bulges outwards, typically improve visual acuity after healing (Williams et al., 1995).
However, the prognosis for long-term corneal clarity and vision can be poor. For example, transplants that are performed urgently for uncontrolled corneal infection or perforation following severe eye injury or for corneal scarring due to inflammatory diseases can have a poor outcome (Armitage et al., 2019). Until recently, traditional full-thickness corneal transplants were the cornerstone of treatment for such patients, but they had some drawbacks, notably a higher risk of rejection and complications (Dominika Szkodny et al., 2022).
Enter Deep Anterior Lamellar Keratoplasty (DALK), which is a cutting-edge, targeted approach to corneal transplantation that revolutionizes how ophthalmologists treat keratoconus and other corneal conditions. DALK is a regularly performed eye surgery that addresses damage to the outermost layers of the cornea, leaving the essential, healthy innermost layer untouched. This selective approach slashes the risk of rejection and other complications, making it an exciting and attractive option for people with corneal disorders (Karimian & Feizi, 2010).
DALK is an advanced surgical technique that selectively replaces only the front 95% of the cornea with donor tissue while preserving the thin back layers of the patient's cornea (Karimian & Feizi, 2010). This procedure is typically performed on patients with corneal scars or other abnormalities affecting the front of the cornea.
BetterEyesight 66

SOURCE: The Indian Journal of Medical Research
During the DALK procedure, the surgeon removes the outer layer (epithelium) and the abnormal front layers of the cornea, leaving the healthy back layers intact. The donor tissue is then carefully placed onto the remaining back layers of the patient's cornea and secured with sutures.
By preserving the delicate pump cell layer lining the back of the cornea (the corneal endothelium) and the thin back layers, DALK reduces the risk of complications while improving the patient's vision (Donaghy et al., 2015). The corneal endothelium is critical in maintaining corneal transparency and preventing swelling.
Compared to traditional full-thickness corneal transplants, which require the removal of the entire cornea, DALK only replaces the
WilliamA.Haseltine,PhD 67
FIGURE 25: Clinical pictures showing post-operative diffuse (left) and slit images (right) of automated lamellar therapeutic keratoplasty (with sutures). 10-0 nylon monofilament=0.020-0.029 mm thickness.
affected layers. This approach minimizes the risk of rejection by the patient's immune system, reduces healing time, and enables patients to return to their daily routines more quickly (Karimian & Feizi, 2010).
Several studies have explored the efficacy of Deep Anterior Lamellar Keratoplasty (DALK) as a treatment option for patients with keratoconus. This technique has a success rate of almost 90% in improving visual acuity among keratoconus patients (Atalay et al., 2021).
Comparative studies between DALK and traditional full-thickness corneal transplants further support DALK as a better option for keratoconus patients. Moorfields Eye Hospital's publication in Eye indicates that DALK patients experience faster healing times, better visual acuity, and fewer complications than those who undergo traditional transplants (Gore et al., 2012). This sentiment is echoed by another study that suggests that DALK has become an effective treatment for keratoconus (Tandon et al., 2019).
Long-term studies also point to the increasing use of DALK and other types of lamellar keratoplasty in treating the condition. Another study cited in Therapeutic Advances in Ophthalmology found that the graft rejection rate in patients receiving selective replacement was only 9%, denoting a high success rate (Atalay et al., 2021).
Selective replacement of the diseased corneal layer is a newer treatment option that only replaces the diseased portion of the cornea while preserving the healthy pump cell layer. This technique has shown great promise for patients with keratoconus as it reduces the risk of complications and improves visual acuity.
BetterEyesight 68
Additionally, patients who undergo DALK can return to their daily routines more quickly than with traditional corneal transplantation.
Other ongoing clinical trials investigate new therapies to treat corneal diseases affecting the endothelium (March de Ribot et al., 2023). Two such treatments being researched are Descemet's stripping only (DSO) (Hakim et al., 2023) and the implantation of cultured corneal cells (Nurković et al., 2020). Recent studies have demonstrated promising outcomes with these therapies, resulting in better patient outcomes and reduced surgical risks.
DSO is a surgical technique that selectively removes the diseased endothelium while preserving the healthy cornea. This procedure promotes the regeneration of healthy corneal endothelial cells, eliminating the need for a full transplant.
Cultured corneal cells, another promising therapy, involve the removal of a small sample of healthy corneal endothelium cells from the patient. These cells are then grown in a laboratory and implanted back into the patient's eye. This technique has shown better results than traditional corneal transplants, including faster healing times and improved visual outcomes.
Moreover, researchers are exploring new methods to improve the quality and availability of donor tissue (Wong et al., 2023). Tissue engineering is one such method that involves the creation of artificial corneal tissue in a laboratory. This tissue can replace damaged corneal tissue and is an attractive alternative to traditional donor tissue.
A cornea transplant is a safe and effective surgical procedure for treating corneal diseases and injuries. While some risks are still associated with the procedure, ongoing research and clinical trials
WilliamA.Haseltine,PhD 69
continuously improve outcomes and reduce risks. The future outlook for corneal transplant is positive with the emergence of novel therapies and advances in tissue engineering and stem cell research. However, ensuring an adequate supply of high-quality donor tissue remains a challenge, and ethical considerations must be addressed to maintain donor confidence and promote the continued success of corneal transplants.
Corneal Infection from Contacts
Contact lenses have become popular for people who want an alternative to glasses, as they provide greater comfort and convenience. However, contact lenses increase the risk of developing eye infections, including corneal diseases (Kates & Tuli, 2021).
Corneal infections caused by contact lenses can lead to severe complications, including permanent vision loss. Fortunately, the Orphan Drug for Acanthamoeba Keratitis (ODAK) Trial has shown that a new treatment protocol could be as effective as current treatments in treating corneal infections.
Corneal infections, like acanthamoeba keratitis, are a type of eye infection that can occur when microorganisms like bacteria, fungi, or amoeba penetrate the cornea. The cornea is the transparent outer layer of the eye that covers the iris and pupil and is critical in focusing light on the retina.
Contact lenses increase the risk of corneal infections due to several factors (Waghmare & Jeria, 2022). One of the primary factors is decreased oxygen permeability, which can cause corneal swelling and the accumulation of debris and microorganisms on the contact
BetterEyesight 70
lens. Other factors include poor hygiene, improper cleaning of contact lenses, and wearing contact lenses for an extended period.

SOURCE: Kates MM, Tuli S. Complications of Contact Lenses. JAMA. 2021;325(18):1912. doi:10.1001/jama.2020.20328
Symptoms of corneal infections can vary depending on the type of infection. Still, they typically include eye pain, redness, sensitivity to light, and blurred vision. In severe cases, corneal infections can lead to permanent vision loss or even require corneal transplant surgery.
WilliamA.Haseltine,PhD 71
FIGURE 26: Contact lens care poster
Acanthamoeba keratitis is an eye infection that commonly affects people who wear contact lenses. The risk is exceptionally high for those who fail to sanitize and store their lenses properly (Somani et al., 2021). Other factors that can increase the risk of infection include making homemade saline solutions or wearing contact lenses while swimming. Acanthamoeba organisms thrive in warm water, so using water sources properly is essential to reduce the risk of infection. People who work with vegetable matter or soil may also be at higher risk of acanthamoeba keratitis.
The symptoms of acanthamoeba keratitis may initially seem similar to other eye conditions like bacterial or viral keratitis, making its accurate diagnosis challenging. Some of the symptoms of this condition include eye pain, light sensitivity, eye redness, and vision loss. Acanthamoeba keratitis can lead to cornea scarring, resulting in permanent visual impairment (Bernfeld et al., 2023). In severe cases, surgical intervention may be required due to corneal perforation.
The treatment options available depend on the cause of the infection. The treatment usually involves topical or oral antibiotics, antifungal agents, or antiviral medication. In severe cases, surgical intervention may be necessary (Tuli & Gray, 2016). The type of surgery required depends on the severity of the infection and the extent of the damage to the cornea. Some common surgical interventions for corneal infections include corneal transplant, penetrating keratoplasty, and lamellar keratoplasty.
The treatment of Acanthamoeba keratitis is most effective when medical and surgical methods are used together (Shareef et al., 2023). Diagnosing the infection early and accurately is critical to get the best response to therapy. Medications like biguanides,
BetterEyesight 72
antiseptics, and antifungal agents may be necessary to treat the infection.
In severe cases, combination therapy may extend over several months. The use of steroids in treating Acanthamoeba keratitis is controversial, as it may delay healing or worsen the condition. For larger corneal ulcers or perforations, surgical interventions may be necessary.
The ODAK trial is an extensive study investigating the efficacy of a new treatment protocol for acanthamoeba keratitis, a rare but severe corneal infection commonly associated with contact lens wear (Dart et al., 2023). Traditionally, one of the treatments for this condition involves dual therapy (Oldenburg et al., 2011), a combination of PHMB 0.02%, and propamidine (Sowlati-Hashjin et al., 2020). However, the new treatment protocol utilizes a single agent, PHMB 0.08%, which was the trial's focus.
The trial was conducted over several months, and many participants were involved. The trial results showed that the new treatment protocol was highly effective, with a medical cure rate of over 86%. This is comparable to the current dual therapy, which has been the standard of care for many years. Notably, the new treatment protocol was found to be safe and well-tolerated by patients, indicating that it could be a viable alternative to traditional dual therapy.
The trial also revealed that the new treatment protocol was more accessible to administer than the dual therapy. Patients only needed to use a single agent, which simplified the treatment process and reduced the likelihood of errors in medication administration. Additionally, the new protocol was less expensive than the
WilliamA.Haseltine,PhD 73
traditional dual therapy, which could make it more accessible to a broader range of patients.
Based on the trial's findings, it is suggested that the new treatment protocol can potentially become the new standard of care for acanthamoeba keratitis. Patients with this condition could benefit from a more effective, streamlined, affordable treatment option.
The trial results provide hope for improved outcomes for patients diagnosed with this rare but severe corneal infection. Ultimately, further research is still necessary to enhance the management and treatment of corneal infections resulting from wearing contact lenses.
CRISPR for Herpetic Stromal Keratitis
The herpes simplex virus (HSV) is a highly prevalent virus that can cause various human infections. One of the most severe complications of HSV is herpetic stromal keratitis (HSK), which affects the eye's cornea and can lead to visual impairment or even blindness (Knickelbein et al., 2017). Unfortunately, current treatments for HSK are limited, and there is a pressing need for more effective therapies.
Fortunately, the gene-editing technology CRISPR-Cas9 has emerged as a promising approach for treating HSK caused by HSV. This revolutionary approach involves targeting and editing the viral genome to eliminate the virus from infected cells and tissues. The CRISPR-Cas9 system has shown great potential in laboratory studies, demonstrating high levels of efficacy against HSV (Ying et al., 2023).
BetterEyesight 74
Moreover, clinical trials are currently underway to evaluate the safety and efficacy of CRISPR-Cas9 for treating HSK caused by HSV (O’Hanlon Cohrt, 2020). These trials have shown promising results, with some patients experiencing significant improvement in their vision and reduced corneal inflammation (Wei et al., 2023). The outcomes of these trials are being closely monitored, and researchers are hopeful that CRISPR-Cas9 will be a game-changer in treating HSK and other viral infections.
CRISPR-Cas9 is a revolutionary tool in the world of gene editing. It is a targeted cutting and altering of the genetic code within organisms. This cutting-edge technology functions by using guide RNAs to target specific segments of DNA. Once the guide RNA is attached to the target gene, the Cas9 enzyme can cut the viral DNA in a precisely targeted manner.
This revolutionary technique boasts accuracy and efficiency (Medline Plus, 2022). Once the Cas9 enzyme makes the intended cuts, researchers can add, remove, or repair genes to eliminate genetic disorders or fight viral infections.
The ability of CRISPR-Cas9 to selectively target and cut genes that are responsible for causing diseases such as herpes simplex virus (HSV) infections is what makes it a game changer in the field of biomedicine. It is also a versatile and controllable technique that can be modified to target various genetic mutations.
Several studies have demonstrated the effectiveness of CRISPR in treating HSV infections (Yin et al., 2021). For instance, a study on mice with herpetic stromal keratitis illustrated that targeting HSV-1 with CRISPR-Cas9 can cure the condition. The mice were treated with a single intravenous injection of CRISPR-Cas9 targeting the
WilliamA.Haseltine,PhD 75
viral genome, significantly reducing viral replication and corneal pathology.
Similarly, in another study, a single HSV-1-targeting CRISPR was injected into the cornea of three patients with severe refractory HSK during corneal transplantation (Wei et al., 2023). The treatment was safe and effective, with no detectable CRISPR-induced off-target cleavages or systemic adverse effects observed in all three patients for an average of 18 months. The patients showed significant improvement in symptoms, with no recurrence of HSV infections.
When studying human corneal epithelial cells, researchers discovered that using the CRISPR/Cas9 system to decrease NECTIN-1 can significantly lower the risk of HSV infection (Li, Wei, et al., 2022). Studies show that NECTIN-1 is a crucial receptor for HSV's entry into cells. By reducing NECTIN-1 using the CRISPR/Cas9 system, viral replication and pathogenicity can be significantly decreased.
Several studies have shown that CRISPR/Cas9 editing machinery could control recurrent HSV ocular keratitis (Owens et al., 2018). The studies suggest that topical application of AAV-expressing CRISPR/Cas9 editing machinery can effectively prevent the spread of herpes simplex virus (HSV) in the eyes. Scientists use guide RNAs (gRNAs) to target specific genes in the virus and reduce the production of secreted virions that cause corneal pathology associated with HSV infections.
Recent clinical trials have shown promising results for using CRISPR-based therapies to treat herpes simplex virus (HSV) (O’Hanlon Cohrt, 2020). However, further research and
BetterEyesight 76
development are still needed before these therapies become widely available.
One of the significant concerns researchers are currently working on is addressing potential toxicity issues associated with using CRISPR. Obtaining FDA approval for human trials is also crucial (Yin et al., 2021). While the potential benefits of CRISPR-based therapies for HSV are exciting, ensuring they are safe and effective before they can be made available to the public is essential.
Recent research has explored various delivery methods for CRISPRbased treatments for herpes (Yin et al., 2021). These treatments can be delivered through viral vectors, such as adeno-associated viruses, which can enter the host cells and have the CRISPR/Cas9 components. Local administration methods or lentiviral delivery can also target latent HSV-1-containing neurons. However, there are still concerns about these delivery methods' long-term safety and efficacy in humans.
CRISPR-based therapies offer a promising avenue for improving the treatment of HSV infections and reducing the burden of associated diseases. However, more research and development are needed to address potential toxicity issues and optimize the delivery methods for CRISPR-based therapies. With continued efforts, CRISPRbased medicines can potentially revolutionize the treatment of HSV-caused corneal problems and other diseases caused by this virus.
Cell Therapy for Damaged Corneas
Imagine waking up in the morning with hazy vision or feeling as if there is a film over your eye. This is a reality for patients with corneal
WilliamA.Haseltine,PhD 77
endothelial cell disorders, such as Fuchs's endothelial corneal dystrophy and bullous keratopathy. These conditions are associated with corneal edema, resulting in corneal haziness, decreased vision, and potential blindness.
The recent development of cell therapies has shown promise in treating these conditions. One approach involves the injection of cultured human corneal endothelial cells supplemented with a rhoassociated protein kinase (ROCK) inhibitor, which has yielded positive results in small clinical trials.
The corneal endothelium is a thin layer of cells that forms the inner lining of the cornea. The human eye has approximately 7500 endothelial cells per square millimeter (Kannabiran et al., 2022). These cells play a crucial role in regulating the hydration of the cornea, which helps maintain its transparency. Any defects in these cells can lead to fluid accumulation within the corneal stroma, causing corneal opacity and reduced visual acuity. These defects are known as corneal endothelial cell disorders, which can cause corneal edema and vision problems.
The most common corneal endothelial cell disorders include Fuchs's endothelial corneal dystrophy, bullous keratopathy, pseudophakic bullous keratopathy, and pseudoexfoliation syndrome keratopathy. These disorders can be caused by age-related changes, trauma, inflammation, and genetics.
Corneal endothelial cell disorders have traditionally been treated through corneal transplantation. The process involves surgically removing damaged or non-functional corneal endothelial cells from the recipient's cornea and transplanting donor corneal endothelial cells to replace them. However, this procedure can be technically
BetterEyesight 78
challenging and has a high risk of rejection by the recipient's immune system. Additionally, there is a distinct shortage of available donors (Charters, 2023).
More recently, cell therapies have emerged as an alternative approach to restoring corneal transparency and improving visual outcomes for patients with these disorders (Wong & Mehta, 2022). Cell therapies involve transplanting healthy cells into the cornea and regenerating and replacing damaged or dysfunctional cells. Unlike traditional corneal transplantation, cell therapies do not return the entire cornea, only the damaged or non-functional cells. This makes the procedure less invasive and reduces the risk of rejection.
One of the critical advantages of cell therapies is that they can be tailored to the individual patient's needs. Cells can be harvested from the patient's body, cultured in the laboratory, and then transplanted back into the patient's cornea. This reduces the risk of rejection and eliminates the need for immunosuppressive drugs, which may have side effects.
A promising approach to cell therapy for corneal endothelial cell disorders is injecting human corneal endothelial cells supplemented with an ROCK inhibitor. In a recent study, this approach increased cell density after 24 weeks in 11 persons with bullous keratopathy (Kinoshita et al., 2018). Following treatment, all participants achieved a corneal endothelial cell density of more than 500 cells per square millimeter, with ten eyes having a density exceeding 1000 cells per square millimeter. Additionally, 91% of treated eyes achieved a corneal thickness of less than 630 μm, and 82% showed an improvement in visual acuity of two lines or more.
WilliamA.Haseltine,PhD 79

SOURCE: Copyright © 2018, Massachusetts Medical Society
By replenishing the density of healthy endothelial cells, these therapies offer the possibility of restoring corneal transparency and improving visual outcomes. Furthermore, since these cell therapies eliminate the need for corneal transplantation, they can reduce the risk of graft rejection and decrease the technical complexity.
BetterEyesight 80
FIGURE 27: The cell therapy approach used in the ROCK Study by Aurion Biotech
The study does not provide detailed information on the long-term outcomes and complications associated with injected cultured CEC therapy. However, other ongoing clinical trials have shown promising results. One study found that refined human CEC transplantation could promote long-term corneal clarity without significant immunologic or safety concerns (Numa et al., 2021). Another study investigated the effects of injecting human corneal endothelial cells cultured on a Descemet's membrane (DM) substrate and found promising results in patients with Fuchs's endothelial corneal dystrophy (De et al., 2021).
While cell therapies show great potential in treating corneal endothelial cell disorders, several challenges still need to be addressed before they can become the standard of care. One issue is the limited availability of suitable donors for cell transplantation. Additionally, the cost of producing cultured cells for transplantation can be prohibitive. As more clinical trials are conducted, addressing these challenges and developing strategies to overcome them will be necessary.
It's essential also to consider the long-term safety of cell therapies. Although the initial outcomes may seem optimistic, tumors can be developed using cultured cells. Long-term follow-up studies are necessary to ensure the practicality and safety of these therapies over time.
Despite these challenges, the future looks bright for cell therapies in treating corneal endothelial cell disorders. Further research is needed to refine the best cell sources, optimize culture conditions, and develop standardized protocols for transplantation. Increased collaboration between clinicians, scientists, and industry partners
WilliamA.Haseltine,PhD 81
will be necessary to move these therapies from the laboratory to the clinic.
Steven - Johnson Syndrome
Steven-Johnson Syndrome (SJS) is a rare and life-threatening disorder that severely affects the skin and mucous membranes. SJS often results from an adverse reaction to medication or infection, causing detachment of the skin layers and the development of blisters and sores on the mucous membranes. The impact of SJS on the eyes is particularly prominent, resulting in severe eye pain, light sensitivity, vision loss, and, in some cases, blindness. However, advances in care and treatment options for SJS have vastly improved patient outcomes, including the ability to preserve eye health (Thuma et al., 2021).
Novel treatments, such as intravenous immunoglobulin (IVIG) and systemic corticosteroids, have demonstrated promising results in treating SJS and reducing its associated ocular damage (Chang et al., 2022). The development of new treatments provides hope for SJS patients. Early intervention is critical to improving clinical outcomes and mitigating long-term effects (Slentz et al., 2013).
Stevens-Johnson syndrome (SJS) is a rare but life-threatening medical condition that can cause several ocular complications. The condition can affect people of any age, but it is most commonly found in children and young adults.
One of the most significant corneal complications associated with SJS is the development of fluid-filled blisters called bullae on the cornea's surface. These bullae can cause considerable pain and discomfort, and their rupture can lead to corneal ulceration and
BetterEyesight 82
perforation. Moreover, the rupture of these bullae can cause the cornea to become thin and fragile, increasing the risk of further complications (Wang et al., 2014).
SJS can also cause inflammation of the iris, the colored part of the eye. This inflammation can lead to iritis, which can cause eye pain, redness, and sensitivity to light. In some cases, SJS can also cause conjunctivitis, inflammation of the thin, clear tissue covering the white part of the eye.

others.
SOURCE: Ophthalmic Atlas Images by EyeRounds.org, The University of Iowa.
In addition to bullae formation, SJS can cause significant damage to the corneal epithelium, the cornea's outermost layer. This damage can lead to long-term changes in the corneal surface, including scarring and irregular astigmatism. Such changes can
WilliamA.Haseltine,PhD 83
FIGURE 28: This slit-lamp photograph showcases the enduring effects of SJS/TEN, encompassing limbal stem cell deficiency and symblepharon, among
cause vision problems that persist even after the acute phase of the condition has resolved (Ma et al., 2021).
The primary treatment for SJS is to identify and eliminate the medication or other factors that caused it. Once the causative agent is removed, supportive care becomes essential to minimize the risk of complications and promote healing (Oakley & Krishnamurthy, 2020).
Supportive care may include pain management with nonsteroidal anti-inflammatory drugs (NSAIDs) or opioids, nutritional support, and fluids to prevent dehydration. Hospitalization is often required as SJS can rapidly progress and lead to life-threatening complications such as sepsis, organ failure, or pneumonia. In the hospital, patients are closely monitored and treated with intravenous fluids, antibiotics, and corticosteroids to reduce inflammation and promote healing.
SJS can cause severe damage to the cornea, which can lead to vision problems and even blindness if not treated promptly. Eye drops and ointments can manage pain and inflammation to protect the cornea from further damage and promote healing; bandage contact lenses can be worn. However, severe cases may require surgery to repair corneal perforation or remove damaged tissue.
Researchers are conducting several clinical trials to explore new treatments for SJS and its associated ocular complications. These trials are focused on developing targeted therapies that can help reduce inflammation and promote healing.
There is a promising treatment for severe ocular complications caused by Stevens-Johnson syndrome (SJS). This treatment involves mesenchymal stem cells, multipotent stromal cells capable of
BetterEyesight 84
differentiating into various cell types. Mesenchymal stem cells have anti-inflammatory and antioxidant properties that help corneal healing. Recent research has shown that using mesenchymal stem cells in a patient with SJS-induced corneal damage has significantly improved corneal clarity and reduced pain (Park et al., 2020). This approach offers a potential solution for treating severe ocular complications associated with SJS.
Another promising treatment is a topical gel containing an antiinflammatory agent and a neuroprotective peptide. In a small study, SJS patients treated with this gel significantly reduced ocular symptoms (Matsumoto et al., 2023). The gel was safe and welltolerated, with no adverse effects reported. This treatment may offer a viable alternative for SJS patients who are unable to tolerate traditional therapies.
Even though these trials are still in the initial stages, the outcomes have been promising. These studies bring hope to SJS patients who are experiencing severe eye-related complications and could create a path for more efficient treatments in the future. As the research progresses, the ultimate objective is to reduce or even avoid the harmful effects of SJS on the cornea.
WilliamA.Haseltine,PhD 85
Proptosis and Strabismus

Thyroid Eye Disease and Proptosis
Thyroid eye disease (TED) is an autoimmune disorder that causes inflammation of the muscles and tissues around the eyes. This can lead to proptosis or bulging of the eyes, diplopia or double vision, and a significant reduction in the patient's quality of life. TED is often connected to Graves' disease (Johnson & Heiting, 2020).
In this autoimmune condition, the thyroid gland overproduces hormones. Still, it can also occur in patients with Hashimoto's thyroiditis or as a result of radiation therapy to the head and neck.
Thyroid eye disease can be explained simply by saying that it is a disease where autoantibodies target specific eye cells, causing them to bulge out and compress the optic nerve. This can lead to vision problems and even blindness in severe cases.
In more detail, the immune system produces autoantibodies that activate specific receptors. These receptors then trigger the release of cytokines, which are chemical messengers that cause inflammation and fibrosis in the eye tissues. As a result of this inflammation, the extraocular muscles become inflamed and swollen, leading to a range of symptoms, including proptosis or bulging of the eyes, double vision, and exposure keratopathy.
86
CHAPTER 4
Proptosis occurs due to the swollen muscles pushing the eyeball forward, leading to an abnormal eye protrusion. Double vision and exposure keratopathy can occur due to the abnormal position of the eyeball caused by the swollen muscles. Exposure keratopathy is when the cornea, the transparent outer layer of the eye, becomes dry and damaged due to inadequate protection from the eyelid.
Currently, the mainstay of treatment for TED is glucocorticoids, such as prednisone or methylprednisolone, powerful antiinflammatory drugs that can help reduce swelling and inflammation. However, these drugs can also cause significant side effects, including weight gain, mood changes, and increased risk of infection.
In addition to glucocorticoids, doctors may also recommend other treatment options based on the severity of the condition and the patient's needs. Radiotherapy, which uses high-energy radiation to target the tissues in and around the eyes, can effectively reduce inflammation and swelling. Immunosuppressants, such as mycophenolate or azathioprine, may also suppress the immune system and prevent further damage to the eye tissues.
In some cases, surgery may be necessary to correct the position of the eyes or to reduce pressure on the optic nerve. This can involve decompression surgery to remove bone from around the eyes or to remove fat from behind the eyes to create more space. In rare cases, doctors may recommend orbital radiotherapy, which is a type of radiation therapy that targets the eye socket to reduce inflammation and swelling.
Teprotumumab, a fully human monoclonal antibody, is a novel treatment option for TED. Its mechanism of action involves binding
WilliamA.Haseltine,PhD 87
to and blocking the activity of IGF-1 R, preventing the activation of fibroblasts and thereby reducing inflammation and fibrosis. The FDA approved this medication in January 2020 (Pluchino, 2020) for treating active TED based on the results of two randomized, double-masked, placebo-controlled, parallel-group, multicenter trials.
A recent study published in the International Journal of Ophthalmology reviewed the efficacy and safety of teprotumumab for the treatment of TED, incorporating data from three clinical trials involving 341 patients (Lin et al., 2023). The analysis found that teprotumumab was significantly more effective than a placebo in reducing proptosis, or the protrusion of the eyes, in both the intention-to-treat and per-protocol populations.
Patients treated with teprotumumab also showed improvements in diplopia response, overall response, and the clinical activity score, a measure of disease activity. Additionally, patients receiving teprotumumab experienced more significant gains in proptosis and quality of life than those receiving a placebo.
Despite these positive outcomes, the analysis also revealed that patients treated with teprotumumab are at a higher risk of adverse events, including serious complications such as muscle spasms and gastrointestinal reactions. However, these side effects were generally tolerable and manageable in clinical trials.
The findings on teprotumumab as a treatment for TED are highly promising, with evidence indicating that it may offer a safer and more efficient alternative to glucocorticoids. Although the studies analyzed had relatively short follow-up periods and small sample
BetterEyesight 88
sizes, these limitations do not negate the potential benefits of teprotumumab.
Indeed, future research should prioritize examining this treatment's long-term safety and efficacy by studying patients' experiences with chronic-inactive TED. Additionally, identifying biomarkers that predict response to treatment is a crucial avenue for advancing our understanding of TED and optimizing treatment outcomes. These areas of study offer significant potential for improving patient outcomes and increasing medical knowledge.
Strabismus
Strabismus is a visual disorder that affects people globally and has an estimated prevalence of 1.93% (Buffenn, 2021), which means that about 2 in every 100 people have this condition. It occurs when the eyes are misaligned and do not point in the same direction, leading to physical changes in appearance, disrupted visual development and function, negative impacts on overall health, and psychological distress.
Individuals who have strabismus face several challenges. They are at an increased risk of vision loss and injury (Buffenn, 2021). Furthermore, they often find it difficult to receive appropriate care and lack proper information among ophthalmologists and primary care providers. Although the exact cause of this condition is unknown, it may be due to muscle tension, nerve damage, or abnormalities in the brain that control eye movement. Some research suggests that genetics may also play a role (Wilmer & Backus, 2009) in the development of strabismus.
WilliamA.Haseltine,PhD 89
Various risk factors can lead to strabismus, such as premature birth, low birth weight, and cerebral palsy. Strabismus is also more common in certain pediatric conditions, including Down syndrome, retinopathy of prematurity, and hydrocephalus. While strabismus can be a purely cosmetic concern in some cases, untreated patients can experience functional vision loss and visual input suppression in one of the eyes, leading to permanent vision impairment.

SOURCE: Wikimedia Commons
Strabismus can be classified into different types, including esotropia, exotropia, hypertropia, and hypotropia. Esotropia involves an inward deviation of one or both eyes. In contrast, exotropia involves an outward variation of one or both eyes. Hypertropia and hypotropia involve upward and downward deviation of one or both eyes, respectively.
BetterEyesight 90
FIGURE 29: Depiction of a person suffering from Strabismus or crossed eyes. The three types of Strabismus or crossed-eyes have been shown
Paralytic strabismus is another type, resulting in an inability to move eyes correctly. This condition is also known as paralytic squint and is often characterized by double vision or diplopia. Paralytic strabismus can be caused by the involvement of the third, fourth, or sixth cranial nerves and can be either congenital or acquired. In children, paralytic strabismus is often caused by congenital malformations that affect the muscles responsible for eye movement. This can include conditions such as Duane syndrome, which affects the eye's ability to move inward or outward, or congenital fibrosis syndrome, which affects the eye's ability to move in any direction.
In adults, paralytic strabismus is usually the result of trauma, infections, or neurological disorders. Trauma to the eye or head can cause damage to the muscles responsible for eye movement, resulting in paralytic strabismus. Infections such as botulism, Lyme disease, or herpes simplex virus can also cause this condition.
Neurological disorders such as multiple sclerosis, stroke, or brain aneurysms can also lead to paralytic strabismus. These conditions affect the brain's ability to control eye movement, leading to misalignment or abnormal eye movements.
Strabismus treatment is a comprehensive approach with multiple objectives. The primary goals of this treatment are to improve the alignment of both eyes, enhance visual clarity, and foster binocular vision. Proper alignment ensures that both eyes work harmoniously, reducing eye strain and discomfort while improving visual coordination. Optimizing optical clarity provides a more immersive and wholesome visual experience, enabling patients to see objects clearly without distortions. Lastly, promoting binocular vision offers
WilliamA.Haseltine,PhD 91
enhanced depth perception and a comprehensive understanding of spatial relationships.
Treatment options for paralytic strabismus include eye exercises, corrective lenses, prism glasses, and eye surgery. Eye exercises are often recommended to strengthen the muscles responsible for eye movement, which can improve the alignment of the eyes. Corrective lenses may also be prescribed to help correct refractive errors, which can contribute to the development of strabismus. Prism glasses may be recommended to help align the eyes by bending light rays, which can help reduce the severity of the condition.
In addition to traditional methods such as glasses or contact lenses to correct refractive errors, other specialized approaches can be employed to address the issue of eye misalignment. These methods may include special drops, lenses, or even eye patching, which have proven effective in straightening misaligned eyes. In some cases, surgery may be considered the most optimal and effective long-term solution for treating strabismus. One novel treatment approach related to surgery is the use of adjustable stitches.
The sutures play a crucial role in strabismus surgery. The stitches allow for precise adjustments of extraocular muscles to optimize alignment during postoperative recovery. A comprehensive study by the American Academy of Ophthalmology (Heidary et al., 2022) evaluated the impact of adjustable sutures on motor alignment outcomes in patients undergoing strabismus surgery.
The technique used in this surgical procedure involves the flexibility of adjusting sutures either immediately after the surgery or within a few days, with or without sedation, to ensure optimal
BetterEyesight 92
results. It is worth noting that both adjustable and non-adjustable suture techniques have yielded favorable outcomes in motor alignment in most cases, indicating the effectiveness of both approaches. However, the study suggests further research into the viability of these sutures before making them a common practice. Additionally, another treatment option is to avoid surgery entirely by using Botox.
Botulinum toxin type A (BTXA) is a neurotoxin commonly used for treating strabismus, a condition where the eyes don't align correctly. By injecting BTXA into the extraocular muscles, we can restore ocular alignment. Generally, the effects of this injection become apparent within 1 to 3 days.
The technique for administering BTXA may vary based on whether an open or closed conjunctival-based approach is used and whether electromyographic guidance is employed. This procedure can be conducted in an operating room or an office setting. Evaluating the injection of BTXA for horizontal strabismus is crucial to identify any temporary or permanent adverse effects associated with this treatment.
Based on a review by the American Academy of Ophthalmology (Binenbaum et al., 2021), extraocular muscle injection of BTXA is an effective method for achieving successful motor outcomes, akin to eye muscle surgery for horizontal strabismus. The consistency of results across the studies included in the review is notable. Three of five comparative studies indicated successful motor outcome rates of approximately 60%.
Strabismus is a complex condition affecting individuals of all ages and significantly impacting their quality of life. While the exact
WilliamA.Haseltine,PhD 93
cause of this condition is unknown, various risk factors can lead to the development of strabismus. If left untreated, strabismus can lead to permanent vision impairment.
The primary goals of strabismus treatment are to improve the alignment of both eyes, enhance visual clarity, and foster binocular vision. Treatment approaches may include traditional methods such as glasses or contact lenses, specialized techniques such as special drops, lenses, or even eye patching or surgery.
Recent advances in strabismus surgical procedures, such as adjustable sutures, have shown promising results in achieving optimal outcomes. Similarly, Botulinum toxin type A (BTXA) injections are an effective treatment alternative for horizontal strabismus.
As the research progresses, we will likely see novel approaches and improvements in current treatments that will provide better vision and outcomes to those with strabismus.
BetterEyesight 94
Dry Eye Syndrome and Eye Floaters

Burning, itching, watering eyes. Few things are a bigger nuisance than irritated eyes, so it's no surprise there are so many options for dry eye relief. Dry eye disease is a condition that afflicts millions of people worldwide, causing constant discomfort and affecting their quality of life. One of the key culprits behind this condition is meibomian gland dysfunction, which hinders eye lubrication and moisture by preventing the normal secretion of oil from the meibomian glands in the eyelids.
Despite the prevalence of dry eye disease and meibomian gland dysfunction, it remains a mystery as to what exactly causes this condition and how we can address it effectively. However, recent research (Baudouin et al., 2016) has made significant strides in understanding the underlying mechanisms of the disease, offering a ray of hope for those suffering from it.
Dry eye disease is a chronic, multifactorial condition that affects the eye's surface. It's a common issue among people of all ages and genders worldwide. Typically, dry eye disease is a result of meibomian gland dysfunction.
The International Workshop on Meibomian Gland Dysfunction defines this dysfunction as a chronic abnormality of the glands characterized by blockages and changes in secretion. This leads to tear film alterations, inflammation, and other eye-related issues.
95
CHAPTER 5

Opthalmology
SOURCE: © American Academy of Ophthalmology 2023
Meibomian gland dysfunction manifests in various forms, each with distinct characteristics. The low-delivery state can be obstructive or hyposecretory, while the high-delivery state presents another scenario. These conditions have underlying causes ranging from hyperkeratinization to hormonal fluctuations. Moreover, the dysfunction can also be classified based on the quantity and quality of meibum, which leads to foam formation in the tear film.
Age-related meibomian gland dysfunction adds another layer to the mix. Cell signaling and lipid synthesis changes can occur as we age,
BetterEyesight 96
FIGURE 30: Meibomian Glands diagram by the American Academy of
contributing to gland atrophy. Reactive oxygen species may also play a role.
Dry eye disease is like a self-sufficient cycle, causing tear film breakup, drying, inflammation, and more. The condition persists in a vicious cycle even after removing or reducing the initial cause. This happens when the compromised eye surface is continuously exposed to environmental challenges. Understanding the mechanisms of meibomian gland dysfunction and dry eye disease can help us develop more targeted treatments.
One of the entry points into this relentless cycle is the dysfunction of the meibomian gland. When the meibomian gland experiences dropout, blockage, or inflammation, it triggers bacterial growth and spread. These bacteria produce lipases and esterases, increasing the meibum's viscosity and melting temperature. Consequently, the meibum secretion onto the tear film's surface is reduced. This defines the self-sustaining circle of Meibomian gland dysfunction.
Insufficient meibum leads to a decrease in lipid content within the tear film. This, in turn, causes increased tear evaporation, hyperosmolarity, and inflammation, perpetuating the cycle of dry eye disease.
The concept of a double vicious cycle demonstrates how the disease mechanisms of dry eye disease and meibomian gland dysfunction intertwine to create a chronic condition known as meibomian gland dysfunction-associated dry eye disease.
WilliamA.Haseltine,PhD 97

SOURCE: Baudouin et al., 2016 © British Journal of Ophthalmology 2016
Meibomian gland changes are a gateway to dry eye disease, perpetuating a vicious double cycle of dysfunction. Advanced imaging techniques, such as in vivo confocal microscopy, optical coherence tomography, and keratography, offer valuable insights into the intricate link between dry eye disease and Meibomian gland dysfunction.
The coexistence of dry eye disease and Meibomian gland dysfunction can contribute to the deterioration of the eye's surface. Research has shown that when the ocular surface is exposed to stress, it triggers the production of cornified envelope precursors by the ocular epithelium.
BetterEyesight 98
FIGURE 31: The pathology of dry eye disease by the British Journal of Ophthalmology
These precursors then lead to the keratinization of meibomian gland orifices. Consequently, this can result in meibomian gland inflammation, blockage, atrophy, loss of mucin-filled goblet cells, and entrapment of mucin within the remaining goblet cells, all contributing to the development of dry eye disease.
Treatment
Dry eyes can be a debilitating condition that can significantly impact a person's quality of life. Fortunately, various treatment options are available to help interrupt the vicious cycle of dry eye disease.
For those suffering from dry eye and blepharitis, implementing proper eyelid hygiene is one of the most critical steps in managing these conditions. Regularly cleaning the lids and lashes can help remove excess oils and debris contributing to ocular irritation. While anti-inflammatory therapies like oral tetracycline derivatives or topical cyclosporine eye drops can effectively reduce inflammation and improve tear production, patients have another essential option.
Enter Avenova, a lid hygiene product that directly tackles one of the root causes of dry eye and blepharitis: the overpopulation of bacteria that live on the lids and lashes. Studies have shown that Avenova kills harmful bacteria (Singh, 2017) and helps neutralize bacterial toxins and enzymes like lipase, contributing to these lid conditions. This makes Avenova ideal for controlling eyelid conditions like meibomian gland dysfunction-associated dry eye disease. Moreover, using tear substitutes is another essential aspect of treating dry eye. These drops or ointments are designed to maintain a healthy tear film and alleviate dryness, burning, and irritation
WilliamA.Haseltine,PhD 99
symptoms. Some of the newer tear substitutes on the market also possess osmo-protective properties, which help reduce hyperosmolarity a key factor contributing to dry eye disease.
Overall, it's clear that a multi-pronged approach that includes proper eyelid hygiene, anti-inflammatory therapies, and tear substitutes is crucial for managing dry eye. Still, there are some other cutting-edge options out there as well, such as intense pulsed light therapy and vector thermal pulsation.
Intense pulsed light therapy or vectored thermal pulsation may be recommended for those with more severe dry eye disease. It uses a noncoherent polychromatic light source with a 500–1200 nm wavelength spectrum. This therapy helps to reduce inflammation of the glands and improve abnormal telangiectatic vessels through the photothermal effect.
Vector thermal pulsation is a therapy for obstructive meibomian gland dysfunction. It enhances tear film stability by improving the flow of meibomian gland secretions. It's a non-invasive treatment option when traditional approaches like heat and eyelid massage aren't practical. This therapy clears meibomian gland obstruction using pulsating pressure and heat.
Each eye receives vectored thermal pulsation for 12 minutes using a temperature- and pressure-controlled device. Adverse effects like eyelid pain, conjunctival congestion, and ocular burning may occur but usually resolve in 4 weeks. Vectored thermal pulsation improves symptoms and signs based on tear break-up time, corneal fluorescein staining, and meibomian gland secretion scores.
Artificial tears are one of the most commonly used treatments for dry eyes (Fletcher et al., 2017). These eye drops add moisture to the
BetterEyesight 100
eyes and improve tear film stability, temporarily relieving mild dry eye symptoms.
The drawback to artificial tears is that they can only provide temporary relief and do not treat the underlying issues. This reprieve from symptoms also leads to frequent use of these tears, which often contain preservatives that may cause eye irritation and redness with prolonged use. Some people also experience changes in vision or eye pain after using artificial tears for an extended time. Moreover, additional therapies may need to be administered with artificial tears to maximize the treatment's effectiveness.
Anti-inflammatory eye drops, on the other hand, target the root causes of dry eyes, providing more comprehensive relief than artificial tears. One such medication is Xiidra®, a lifitegrast ophthalmic solution (Semba & Gadek, 2016) specifically designed to treat the signs and symptoms of dry eyes.
Clinical trials involving 2133 patients with dry eyes evaluated Xiidra®'s effectiveness in managing dry eyes. These trials typically involve a group of randomly assigned participants to receive either Xiidra® or a placebo. The participants' symptoms and eye health are monitored over a period of time to assess the drug's efficacy. The trials measured the improvement of dry eye disease using an inferior fluorescein corneal staining score and patient symptoms reported via an eye dryness score.
The medication effectively reduces dry eye symptoms and improves eye health, as found in three studies (Haber et al., 2019) conducted to ensure the safety and efficacy of the drops: OPUS-1, OPUS-2, and OPUS-3. Xiidra outperformed placebo remedies significantly in all three studies, reducing the signs and symptoms of dry eye disease.
WilliamA.Haseltine,PhD 101
Patients who received ongoing lifitegrast treatment exhibited a reduction in dry eye disease symptoms at 3, 6, and 12 months following the initial treatment. Also, symptom questionnaire scores showed a consistent decline at 3, 6, and 12 months after the index compared to before.
In addition to these clinical trials, a pooled analysis (Keating, 2017) of five randomized controlled trials published in Drugs evaluated the safety and tolerability of the medication. Xiidra® was generally well tolerated, with mild side effects like eye irritation and redness. While Xiidra® may have limitations and potential side effects, it offers hope for individuals seeking long-lasting relief from dry eye disease.
Xiidra® works by targeting the interaction between two proteins (Semba & Gadek, 2016). It specifically targets the interaction between lymphocyte function-associated antigen-1 (LFA-1) and intercellular adhesion molecule 1 (ICAM-1). Both of these proteins play a role in inflammation and immune responses.
LFA-1 is expressed on the surface of specific white blood cells, while ICAM-1 is on the surface of various cells in the eye. When LFA-1 and ICAM-1 interact, it can lead to inflammation and worsening dry eye symptoms. By blocking this interaction, Xiidra® helps reduce inflammation and improve tear production.
102
BetterEyesight

FIGURE 32: Immunologic
SOURCE: Semba C, Gadek T For Dove Press
The development of lifitegrast, the active ingredient in Xiidra®, targeted the interaction between lymphocyte function-associated antigen-1 (LFA-1) and intercellular adhesion molecule 1 (ICAM-1) to reduce inflammation and immune responses associated with dry eye disease.
The figure below illustrates the evolution of the lifitegrast design. The first two domains of ICAM-1 were determined by X-ray crystallography and are shown in a space-filling model represented by part a. The binding residues in domain one are superimposed on a ribbon diagram of the first two domains of ICAM-1, as defined by part b of the figure.
WilliamA.Haseltine,PhD 103
synapse.
The six amino acid side chain binding residues identified by alanine point mutagenesis of the ICAM-1 epitope that binds to LFA-1 are depicted in another space-filling depiction, as seen in part c. The molecular structure of lifitegrast is represented using a space-filling model, as seen in part d of the figure. Part e shows the threedimensional structural form of lifitegrast. Finally, the structural formula of lifitegrast is shown in part f of the image.

SOURCE: Semba C, Gadek T For Dove Press
Lifitegrast binds to the integrin LFA-1 found on the surface of white blood cells. By binding to this protein, lifitegrast blocks the interaction between LFA-1 and ICAM-1, disrupting the subsequent cycle of t-cell-mediated inflammation that can lead to dry eye disease.
Blocking the interaction reduces the migration of white blood cells into ocular tissues and alleviates dry eye inflammation. Lifitegrast also facilitates the cell-mediated elimination of cytotoxic T-cells, granulocytes, and monocytes. This elimination of cytotoxic cells
BetterEyesight 104
FIGURE 33: The evolution of the lifitegrast design targeting LFA-1.
further reduces inflammation by reducing the production of inflammatory cytokines.
In addition to its anti-inflammatory properties, lifitegrast increases tear production by upregulating the expression of MUC5AC, a gene associated with mucous secretion in the conjunctival epithelium. Increased mucus production leads to increased moisture on the ocular surface and relief from dryness.
Can Omega-3 Fatty Acids Help Treat Dry Eyes?
Omega-3 fatty acids have been touted as essential nutrients for overall health. Still, it is important to look critically at the potential benefits of omega-3s for eye health. While studies show that consuming omega-3 fatty acids may help reduce the risk of developing macular degeneration and glaucoma, it is essential to note that these studies are not conclusive.
Omega-3s are crucial components found in the membranes of human cells. These fats are polyunsaturated, characterized by double bonds in their chemical structure. Polyunsaturated fats are different from other fats, like saturated fats, because their chemical structure is different. Also, saturated and trans fats are unhealthy when consumed in large quantities. Polyunsaturated fats, on the other hand, are known as healthy fats.
SOURCE: Wikimedia Commons
There are three unique types of these omega-3 fatty acids. The first is eicosapentaenoic acid, also called EPA. Fish and fish oil
WilliamA.Haseltine,PhD 105
FIGURE 34: Chemical structure of eicosapentaenoic acid (EPA)
supplements contain EPA. It is the omega-3 that plays an essential role in preventing heart disease. Additionally, it serves as an FDAapproved medication to lower triglyceride levels.

SOURCE: Wikimedia Commons
The second of the omega-3s is alpha-linolenic acid or ALA. Plant foods such as flaxseed and soybeans are commonly rich in this nutrient. ALA helps reduce blood clots, supports growth and development, and decreases inflammation in the body. Upon consumption, it can undergo conversion into two essential fatty acids: EPA and docosahexaenoic acid (DHA). However, this process is inefficient, resulting in a minimal conversion of the total ALA to EPA and DHA.
SOURCE: Wikimedia Commons
DHA is the last of the three omega-3s and the most critical for sight. Studies suggest that our eyes may benefit from a diet high in DHA. Moreover, DHA is typically abundant in the retina and brain. In the retina, DHA maintains photoreceptors, which are the cells that help us process light. Similarly to EPA, docosahexaenoic acid is in fish and various types of seafood.
BetterEyesight 106
FIGURE 35: Chemical structure of α-linolenic acid (ALA) with three double bonds on carbons numbered 9, 12, and 15.
FIGURE G: Chemical structure of docosahexaenoic acid (DHA)
Low levels of EPA and DHA have been associated with common eye conditions, such as macular degeneration, glaucoma, and diabetic retinopathy (Sala-Vila et al., 2016). Alzheimer's disease often manifests with low levels of DHA, contributing to the prevalence of visual impairments among affected individuals. Unfortunately, these omega-3s are unattainable through the body's natural production. Instead, acquiring these omega-3s from dietary sources or supplements is necessary. Some studies have found that omega-3 supplementation has improved visual acuity and slowed the progression of retinal diseases and dry eye disease. A comprehensive multicenter randomized clinical trial (Oydanich et al., 2020) supported this outcome, which examined the impact of omega-3s on visual health outcomes and dry eye disease compared to placebo.
The trial provided further evidence for the effect of omega-3s on these measures. The randomized trial followed 535 participants and reported support for the claim that omega-3 supplementation positively impacts severe dry eye disease compared to a placebo. The study did not illustrate the statistical significance of their finding, however. As a result, it is essential to consider more evidence before recognizing this as a steadfast fact.
Three other studies found similar results across ten years. The first and most recent, published in 2018 (Titiyal et al., 2018) in the Indian Journal of Ophthalmology, found that daily supplementation of omega-3s for three months in 518 participants reduced symptoms and signs of dry eyes compared to a placebo. The second trial (Epitropoulos et al., 2016), by The Eye Center of Columbus, had a lower participant count and also found that omega-3 supplements increased tear film stability, which is vital for
WilliamA.Haseltine,PhD 107
dry eye disease treatment. The final study was the largest of the three.
It was a cross-sectional study published in the AmericanJournal of Clinical Nutrition (Miljanovic et al., 2005). It featured 32,470 participants. The results were that the women with the highest dietary omega-3 intake had a 17% lower risk of dry eye disease than those with the lowest intake. The study found this association for DHA with the highest intake, leading to a 12% lower risk of dry eye disease.
Omega-3 supplements are effective in preventing and alleviating dry eye disease. However, their impact is a subject of further investigation regarding more severe conditions like age-related macular degeneration.
Interestingly, a three-month period of omega-3 supplementation resulted in a noteworthy reduction in intraocular pressure among adults in a randomized clinical trial from Australia. The study that found this result confirmed their statistically significant results (Downie & Vingrys, 2018). However, considering it is still one of the first of its kind, it is crucial to remain skeptical until further research is published.
Observational studies have shown that dietary consumption of omega-3 fatty acids may confer protection against age-related macular degeneration and reduce the risk of advanced macular degeneration (Zhang et al., 2020). However, no current randomized clinical trial data explicitly supports this or increasing omega-3 intake to combat age-related macular degeneration.
Further to that point, for a boost in DHA to help treat or prevent retinal disorders like age-related macular degeneration or retinitis
BetterEyesight 108
pigmentosa, it must first travel to the intestine, where it is absorbed and then to the bloodstream. From there, it needs to travel in the bloodstream into the retina. This means that the supplement would need to pass not only the intestinal barrier but also the blood-brain barrier.
The brain barrier serves as a vital protective shield, shielding the delicate neural tissue of the brain from the bloodstream. However, not all omega-3 supplements effectively traverse this barrier, potentially rendering them ineffective in delivering DHA to the retina.
You may now be thinking, "Well if omega-3 doesn't work as a supplementtocombatretinaldisorders,williteven workas adrug?"
Currently, no FDA-approved Omega-3 drugs for ocular disorders exist. Still, the question is significant as many research groups are working to determine how effective these fatty acids are and how to convert them from nutraceuticals to proper pharmaceuticals for eye diseases.
How soon can we expect omega-3 medications in eye treatments, considering the FDA's approval of their efficacy in addressing cardiovascular conditions and managing triglycerides?
The approval process for new drugs is lengthy, complex, and expensive. Hence, an exact estimate is impossible, but study results show that omega-3 fatty acids may protect from age-related macular degeneration (Lawrenson & Evans, 2015). With the creation of new supplements (Johnson, 2023), the odds are good that we will see these sooner rather than later. Still, more research is needed before omega-3-based treatments for retinal disorders are found on pharmacy shelves.
WilliamA.Haseltine,PhD 109
Dry eye disease is a multifactorial condition affecting millions worldwide. Meibomian gland dysfunction is a prevalent cause of dry eyes, characterized by chronic abnormality and blockages in the glands. Understanding the vicious cycle of meibomian gland dysfunction-associated dry eye disease is essential for developing effective treatments.
By understanding the mechanisms of meibomian gland dysfunction and dry eye disease, we can take significant steps toward reducing the prevalence and severity of this chronic condition. We can look forward to more targeted and effective treatments as research continues.
Eye Floaters
Have you ever noticed specks or strings drifting across your vision?
If so, you may be one of the estimated 70% of people worldwide who experience eye floaters at some point (Woudstra-de Jong et al., 2023). While this condition is not typically considered severe, it can still be frustrating and uncomfortable, affecting your vision and quality of life.
Usually, the brain ignores these floaters, and they go unnoticed. However, when they increase in number or become more concentrated in a particular area, they can cause annoyance or discomfort.
There are several treatments available to help ease the symptoms of eye floaters. This article will discuss the different options and advances in artificial intelligence that can educate patients and enhance the management of this common condition.
BetterEyesight 110
Eye floaters are specks or strands that can appear in the field of vision and move around when the eyes move. These floaters are caused by the shrinking of the vitreous, a gel-like substance that fills the eye. The vitreous becomes more liquid and less gel-like as we age, causing the collagen fibers to clump together and form specks or strands.

SOURCE: Exeter Eye - Ophthalmic Surgeons
While most floaters are harmless and do not require treatment, some may indicate a severe eye condition, such as retinal detachment or inflammation. Aside from that, eye floaters can be distracting and, at times, concerning significantly when their numbers increase. Some individuals may experience significant interference with their vision, compromising their quality of life and overall well-being.
WilliamA.Haseltine,PhD 111
FIGURE 37: Diagram of floaters but Exeter Eye
Fortunately, several current treatments address eye floaters, with various approaches depending on the individual's condition and overall severity of symptoms.
Laser Floater Treatment (LFT) is a non-surgical procedure performed in the office that is used as one of the current treatments for eye floaters. LFT uses laser light to dissolve eye floaters, reducing their visibility in the patient's field of vision. It has emerged as a viable alternative for people who are hesitant to undergo surgery, as it poses minimal risk of complications and is a less invasive option than surgical treatments.
Studies have shown that LFT is effective in treating eye floaters. One such investigation, which assessed the safety and effectiveness of YAG laser vitreolysis as a treatment for vitreous floaters, concluded that LFT is a suitable option for patients hesitant to undergo surgery due to its minimal risk of complications (Katsanos et al., 2020). The study also found that LFT shows promising results in improving subjective and objective outcomes for symptomatic floaters. However, given the limited available evidence, further research is needed to determine the exact role of YAG laser vitreolysis in treating vitreous floaters.
Another current treatment option for eye floaters is vitrectomy, a surgical procedure that involves removing the vitreous, the jelly-like substance inside the eye where the floaters are suspended. This approach is relatively uncommon and is typically reserved for extreme cases where the floaters interfere significantly with the individual's vision. Vitrectomy carries some risks, including infection and retinal detachment.
BetterEyesight 112
Eye floaters can also be treated through medical management and patient education, especially if an underlying medical condition causes them. For instance, if the floaters result from inflammation or bleeding due to diabetes, controlling or treating the underlying condition can help alleviate the floaters.
Educating patients regarding eye floaters and related disorders is paramount to successful treatment. Patients should understand the condition, including its causes and available treatment options. Additionally, they should be informed about the risk factors, such as age, eye trauma, and specific medical conditions that can lead to eye floaters. By being mindful of these risk factors, patients can take preventative measures to avoid the development of eye floaters.
The study published in Investigative Ophthalmology & Visual Science examined AI chatbots for patient education on retinal floaters (Wu et al., 2023). The study assessed multiple AI chatbots and their ability to help provide practical and actionable patient education. It also highlights AI systems' accuracy in answering questions related to floaters from a retinal specialist point of view.
The researchers found that both ChatGPT™ and Google Assistant™ had weak scores, indicating the bots were inadequate in providing in-depth specialist information. Additionally, while AI chatbots can be a helpful tool for patient education, they should not replace the need for a qualified healthcare professional. Patients must be encouraged to seek medical advice and not rely solely on AI chatbots for diagnosis and treatment.
Eye floaters are a common condition that can be uncomfortable and negatively impact one's quality of life significantly as the number of floaters increases. Fortunately, several treatments are available for
113
WilliamA.Haseltine,PhD
eye floaters, including Laser Floater Treatment (LFT). Studies show that LFT effectively treats vitreous floaters and has promising results in improving subjective and objective outcomes for symptomatic floaters.
As technology advances and shapes the healthcare industry, the future of eye floater treatment looks promising. Integrating artificial intelligence and human expertise can improve patient care by providing accurate and tailored information and guidance to patients and caregivers, helping them make informed decisions about their health. We can look forward to a future where AI and human expertise work together to provide the best possible patient care.
BetterEyesight 114
CHAPTER 6
Age - Related Macular Degeneration

The field of regenerative medicine is rapidly advancing, offering new hope to individuals suffering from visual disorders. Specifically, there's a growing potential to restore vision and transform lives with breakthrough treatments.
The human eye, an intricate sensory organ responsible for our ability to perceive the world, has numerous complex structures, such as the cornea, iris, lens, retina, and optic nerve. With these complex structures comes the potential for diseases and disorders that can lead to blindness and visual impairments.
Cataracts, glaucoma, diabetic retinopathy, and age-related macular degeneration are the most common optical conditions affecting millions worldwide. While cataracts result in lens clouding, leading to blurry vision, glaucoma is caused by damage to the optic nerve, leading to loss of peripheral vision. People with diabetes can also get diabetic retinopathy. This condition affects the blood vessels in the retina and leads to vision impairment if left untreated.
A recent review examined age-related macular degeneration and regenerative medicine's role in treating it (Guymer & Campbell, 2023). Age-related macular degeneration, a leading cause of vision loss among people over 50, affects the retina's center, leading to blurry or distorted vision.
Age-related Macular Degeneration (AMD), a chronic eye condition, affects 196 million people worldwide as of 2020. Its
115
prevalence is rising, with an expected increase to 288 million by 2040. AMD's impact is extensive, causing a decrease in people's quality of life, mobility, and independence. In turn, this leads to an increased rate of falls and depression.
This disease has become an important global cause of disease burden and a leading driver of health outcome inequalities, disproportionately affecting countries with low income and low human development index values.
The disease burden in Africa is over twice that of the Americas. Moreover, Asia, which constitutes around 60% of the global population, is projected to carry more than a third of all cases of AMD. Despite considerable progress in treatment, age-related macular degeneration still poses a significant public health challenge.
The Beckman Initiative for Macular Research proposed a clinical classification system for AMD in 2013, which is now commonly used in research and clinical settings. This classification system requires only clinical examination or color fundus images, making it universally accessible and applicable.
Color fundus images capture intricate details of the fundus. The photos can give insights into the retina, blood vessels, macula, and optic disc. With this, doctors can identify vascular abnormalities, monitor disease progression, and evaluate treatment efficacy. These images are essential in diagnosing and treating AMD.
BetterEyesight 116

SOURCE: ACCESS Health International
Neovascular AMD, also known as wet macular degeneration, is defined as the presence of neovascularization under the retinal pigment epithelium.
Geographic atrophy, also known as dry macular degeneration, involves the loss of photoreceptors and retinal pigment epithelium and presents as a sharply defined pale area with exposed underlying choroidal blood vessels.
WilliamA.Haseltine,PhD 117
FIGURE 38: A diagram of a healthy macula, dry macular degeneration, and wet macular degeneration
Both age-related macular degeneration (AMD) types can be asymptomatic in their early stages. Still, they may cause night blindness and difficulty adjusting to dim lighting. Early detection and monitoring are crucial for identifying neovascular complications and ensuring timely medical intervention. Age-related macular degeneration develops due to oxidative damage to the retina over time. This damage affects various eye structures, including photoreceptors, Bruch's membrane, choriocapillaris, and the retinal pigment epithelium.
Retinal pigment epithelial (RPE) cells accumulate intracellular debris, mainly lipofuscin or drusen, as we age. This buildup leads to oxidative damage and the aggregation of debris into sub-RPE deposits, which manifests as drusen--the hallmark of AMD. This buildup over time is why age is the predominant risk factor for the condition.
Although age is a significant risk factor for macular degeneration, other factors, such as diet and genetics, can also play a role. While lifestyle factors like diet fall under modifiable risk factors, less controllable factors like genetics can't be changed easily.
Smoking poses the most significant risk of all preventable factors, tripling the probability of developing the condition. Nevertheless, quitting smoking can help reduce this risk. Regular physical activity may offer minor protection, but research has proved it a significant mitigating factor in developing macular degeneration.
Research Leads Us To Insights
Although progress has been made in treating age-related macular degeneration, there are still deficiencies in our understanding of the
BetterEyesight 118
disease and its management. Currently, research is focused on early intervention trials to slow down or prevent disease progression.
To improve trial accessibility and efficiency, regulatory agencyendorsed primary endpoints play a crucial role. However, thus far, no such metrics for disease progression have been approved, latestage age-related macular degeneration being a notable exception. Contrast sensitivity, best-corrected visual acuity, and geographic atrophy lesion growth rate remain the only benchmarks recognized by these agencies.
Researchers are actively investigating methods to streamline early intervention trial progress. They are concentrating on developing clinical endpoints by gathering feedback from patients and through anatomical and functional markers. To achieve this objective, experts have collaborated to form a consensus group to establish a more comprehensive grading of age-related macular severity that accounts for early biomarkers and surrogate endpoints.
Innovation in technology and strategies such as AI integration into screening tools, developing advanced home-based monitoring tools, and prioritizing marginalized and vulnerable groups show promise in the fight against age-related macular degeneration and other retinal disorders.
Effective therapies for macular degeneration have the potential to unlock a new era of transformative outcomes, significantly reducing the disease burden on aging populations. Investing in developing treatments for age-related macular degeneration can create farreaching impacts that benefit millions globally.
Artificial Intelligence for Age-Related Macular Degeneration
WilliamA.Haseltine,PhD 119
Identifying those at high risk of age-related macular degeneration is challenging due to a shortage of specialists and clinical expertise to evaluate retinal imaging. However, emerging technologies like artificial intelligence/machine learning (AI/ML) have paved the way for more accurate and efficient screening methods. These AI systems can autonomously evaluate one's risk for developing late age-related macular degeneration and help with prompt diagnosis and treatment. As this technology advances, early intervention can be a game-changer for patients at high risk of disease, helping them maintain their vision and quality of life.
iHealthScreen develops AI and machine learning-based diagnostic systems for identifying age-related macular degeneration (IHealthScreen , n.d.). Their flagship product, iPredict™, enables primary care providers to screen patients for age-related macular degeneration and predict which individuals with early disease are more likely to experience vision loss.
The system was developed using over 93,000 color fundus photos from the landmark Age-related Eye Disease Study (AREDS) and trained using deep-learning algorithms (The AREDS Study Group, n.d.). The resulting model was validated and tested using an additional 23,495 images from AREDS.
To use iPredict™, primary physicians use a fully automated fundus camera to capture color images of a patient's retinas. These images are then securely sent to a centralized server and analyzed using iPredict™. Based on the analysis, a report classifies the patient as either referable or non-referable for age-related macular degeneration. The system assigns a prediction score for referable
120
BetterEyesight
patients, quantifying their risk of developing the late-stage disease within the next year or two.
In clinical trials, iPredict™ predicted a 2-year risk for progression to late age-related macular degeneration with 86% and 84% accuracy. The system's accuracy in a non-specialist setting is being evaluated in four primary care clinics in the New York City area. iPredict's screening model has been prospectively validated and submitted to the FDA for clearance to market the system to primary care practices by the end of 2023.
In collaboration with National Center for Biotechnology Information colleagues, NEI researchers developed another AIbased system for predicting late age-related macular degeneration. Both iHealthScreen and the NIH system are trained to look for reticular pseudodrusen, a type of lesion that causes a spotted pattern in the macula and is associated with a higher risk for progression to late disease.
Early detection and treatment of age-related macular degeneration are crucial for preventing irreversible vision impairment. AI-based tools can aid in disease management. A recent analysis focused on using AI-based algorithms for detecting the disease in fundus images. The study found that the algorithms were almost as practical as retinal specialists in detecting the disease.
The AREDS database - with 130,000+ fundus photographs - is frequently used in AI studies of age-related macular degeneration identification. While widely appreciated by researchers, it's noteworthy that the database was established in the 80s and lacks the nuanced understanding of hard drusen and age-related changes in the current clinical classification of the illness. Therefore, some
121
WilliamA.Haseltine,PhD
obsolete images may compromise their suitability for large-scale AI models. Furthermore, note that some of the photographs were digitized from the film.
The study discovered that the diagnostic prowess of AI needs to be improved in studies that employ larger validation datasets. It's crucial to note that said models were evaluated only on research data sets. AI-based screening in larger populations differs significantly under distinct settings and conditions, necessitating a cautious approach. The performance of AI-based algorithms varied considerably in the studies included owing to various factors, including algorithm architecture, data size for training and validation, image quality, and lack of reference standards for defining age-related macular degeneration.
Artificial Intelligence can potentially detect age-related macular degeneration from multimodality imaging data, including fundus photographs, spectral domain optical coherence tomography (SDOCT), and angio-OCT. Integrating AI-based software into a fundus camera can help ophthalmologists reduce their workload, lower the likelihood of misdiagnoses, and detect early-stage macular degeneration more efficiently, especially in remote areas lacking skilled specialists. Nonetheless, AI algorithms are typically developed to detect only one disease or sign and trained on limited data sets. Their effectiveness relies on the quality of the image for accurate diagnosis.
There are additional challenges to implementing AI software, such as the feasibility and performance of the software compared to clinical physicians, patient trust in machines, and the potential issues of a "black box" system, where physicians might miss falsenegative cases. Patients must understand that referrals are necessary
BetterEyesight 122
if age-related macular degeneration symptoms develop. Moreover, these techniques are not yet suitable for primary care screening due to their higher cost than non-mydriatic automatic cameras, nor are they helpful for retinal specialists who can read the images themselves.
Nevertheless, research in this field holds great promise for the early diagnosis and treatment of age-related macular degeneration, which can improve patient outcomes and even save lives.
Stem Cell Therapies
Is it possible to restore vision with our cells? Can you believe that soon we may witness this reality in front of our eyes? Seeing may be believing, but this scientific breakthrough will allow us to believe in something we've never seen before.
Of the 2.2 billion cases of vision impairment, over one billion could have been prevented or are currently neglected (World Health Organization, 2023). Digging deeper, at least eight million people face total blindness from age-related macular degeneration.
With numbers like these, it's no surprise there is an increasing focus on the potential of stem cell therapies to restore vision loss. At least ten clinical trials look at stem cell therapies for vision loss. There are also a variety of preclinical studies underway, one of which we will look at in further detail in this piece.
One such intervention is stem cell therapy. More specifically, research by Thomas Jefferson University (Hinkle et al., 2021) and published in Stem Cell Research &Therapy reports that induced pluripotent stem cells are a promising approach for treating age-
WilliamA.Haseltine,PhD 123
related macular degeneration. Their promise comes with their potential to develop into any cell type.
To better understand how stem cells can treat age-related macular degeneration, it is first essential to comprehend their characteristics and location. Stem cells are functionally undifferentiated, immature cells with complex structures. This means stem cells can be differentiated or specialized into any cell type in the human body.
As a stem cell becomes differentiated or more specialized, it can only become certain cell types. The process of stem cell differentiation is similar to going from high school to college to graduate school, where the student focuses on their preferred area of expertise.

SOURCE: ACCESS Health International
BetterEyesight 124
FIGURE 39: An infographic showing undifferentiated stem cells becoming differentiated cell types
Stem cells also have the potential to repair tissue and restore function after injury or disease. Because of this potential, they may be able to replace or repair damaged cells in the retina. But how do researchers know what type of stem cells to use (Öner, 2018)?
Different types of stem cells are categorized based on their ability to differentiate or specialize. One type of stem cell is the totipotent stem cell, which can develop into any tissue in the body, including organs and blood vessels. The embryo contains these stem cells during early development. Another type is pluripotent stem cells, derived from adult tissue and can become any cell type in the body except for a complete organ. Multipotent stem cells are even more specialized and can only differentiate into specific tissue types, such as muscle or skin.
Induced pluripotent stem cells are a particular type of stem cell that shows promising results for treating retinal degenerative diseases like age-related macular degeneration. These induced pluripotent stem cells, often called iPSCs for short, are created by reprogramming adult cells from a patient. The reprogramming of cells starts with extracting some adult cells from the body, such as those found in the hair, and then applying Yamanaka factors (“Yamanaka Factors,” n.d.).
The Yamanaka factors are a mix of four transcription factors that allow the cells to revert to an embryonic state. This process essentially "resets" the adult cell and enables it to become any cell in the body, including those in the eye. From here, scientists can grow large numbers of iPSCs for use in research or potential therapies.
WilliamA.Haseltine,PhD 125

SOURCE: ACCESS Health International
Scientists are researching several conditions and drug development applications for these cells (Tartaglia, 2018), highlighting the characteristics that make them an ideal therapy for macular degeneration.
As macular degeneration advances, it can lead to damage in the retinal pigmented epithelium (RPE) and subsequent vision loss. However, there is a promising solution - the development of iPSCderived RPE transplants. These transplants, created from induced
BetterEyesight 126
FIGURE 40: An infographic showing the process of creating induced pluripotent stem cells
pluripotent stem cells, have been developing for over a decade (Singh & MacLaren, 2018). They succeeded without significant systemic complications (Schwartz et al., 2015).
The possibilities introduced by iPSC therapies are so promising the National Institute of Health is planning the first major U.S. clinical trial using them (Sharma et al., 2019). Also, researchers in London and California plan to launch a Phase 2 clinical trial for stem cell therapy in treating age-related macular degeneration (da Cruz et al., 2018). Clinical trials aim to determine efficacy and safety, but induced pluripotent stem cell therapy for macular degeneration is a new treatment with risks and side effects.
Immunosuppression and immune reactions pose inherent risks in cell-based therapies (NYSCF, 2021). It is necessary to deliberately suppress the immune system during cell-based treatments to prevent potential attacks on the administered cells. Interestingly, using iPSCs offers an alternative to this requirement as it allows for the extraction of cells directly from the patient, subsequently reintroducing them. This approach effectively circumvents the immune system's response to foreign cells, eliminating potential red flags.
Alas, immunosuppression or immune response are not the only risks, and one risk that is more common to induced pluripotent stem cells is the risk of tumor formation (Begley, 2017). iPSCs are more likely to form teratomas than other types of cells used in cell therapies. Teratomas are tumors that contain cells from multiple germ layers and can be dangerous.
Despite these potential risks, iPSC therapy has shown promise as a possible treatment option for macular degeneration, and ongoing
WilliamA.Haseltine,PhD 127
clinical trials will help us to see a future free from vision loss due to retinal degenerative diseases like age-related macular degeneration.
Research such as a study by Duke-NUS Medical School, the Singapore Eye Research Institute, and the Karolinska Institute study further supports these findings (Goon Tay et al., 2023). This preclinical study has produced significant vision recovery in a trial using stem cells to form light-detecting or photoreceptor cells in the eye.
In this study, the researchers introduced a human retina-specific protein called LN523 to cultivate human embryonic stem cells. This protein has been reported to be enriched in the retina and brain, suggesting that it might help to create an ideal retinal environment, facilitating the differentiation of pluripotent stem cells into photoreceptor cells.
The study results showed that introducing LN523 into the retinal matrix led to the differentiation of embryonic stem cells into photoreceptor progenitors within 32 days of culture. Furthermore, the researchers found that the embryonic stem cell-derived photoreceptor progenitor cells could engraft in the genetic retina degeneration rodent model and rabbits with a degenerated retina. This means these stem cells can live in mouse and rabbit retinal matrixes, allowing them to create more photoreceptor cells and replace those lost to degeneration.
The researchers used a retinal test called a full-field electroretinogram to investigate the functional recovery of the transplanted rodent retina. They found that short-term functional recovery was detected despite cell engraftment in a confined targeted host retina region. The transplanted human photoreceptor
BetterEyesight 128
progenitors expressed mature markers. They exhibited synaptic connectivity with the host's inner retina after 3 to 5 months posttransplantation.
These findings suggest that LN523 can be a promising approach for differentiating stem cells into photoreceptor progenitors for cellbased therapy in patients suffering from retinal degenerative diseases. The researchers plan to refine the protocol and test against cells in photoreceptor degeneration that are more closely related to the human eye. If practical, they hope to start clinical trials.
The study faced limitations, including the lack of a method to purify photoreceptor progenitor cells and the ability to perform cell transplantation in a fully depleted photoreceptor retina to demonstrate clinical applicability. Additionally, the full-field electroretinogram used in the study only detected short-term functional improvement post-transplantation.
Despite certain limitations, studying cell transcriptomic profiles and post-transplanted animal models showed partial improvement in vision and no teratoma growth. This indicates that the retinaspecific laminin-based, LN523, photoreceptor differentiation method could be a safe avenue for treating retinal degenerative conditions.
While more work remains, this study presents a promising opportunity for sorting photoreceptor progenitor cells. Such advances could significantly improve functional retina outcomes after transplants, laying the groundwork for future discoveries in mechanistic pathways involved in the progression of macular degeneration. Ultimately, such progress may enable the discovery
WilliamA.Haseltine,PhD 129
of alternative therapies for individuals suffering from retinal degenerative diseases.
Stem cell therapies are also being investigated for treating advanced macular degeneration and geographic atrophy. Geographic atrophy is an advanced form of dry age-related macular degeneration. It causes the death of cells in the retina's macular region, leading to central vision loss. Geographic atrophy is characterized by gray or white patches in the macula, the part of the retina responsible for central vision.

BetterEyesight 130
FIGURE 41: Two images highlight the relationship between features in the fellow eye and the affected eye's geographic atrophy (GA) progression rate. The top images display bilateral GA, which increases the risk for higher GA lesion progression rates in both eyes. The bottom
images show GA in the left eye and intermediate age-related macular degeneration (AMD) in the right eye, indicating a relatively lower GA lesion progression rate in the affected eye. Analysis of fundus autofluorescence and OCT images from both eyes helps predict and manage GA progression.
SOURCE: American Academy of Ophthalmology
Currently, no approved treatments for geographic atrophy exist. The lack of adequate and effective treatment options significantly impacts the quality of life for those affected. Also, the damage caused by geographic atrophy is irreversible. Fortunately, several clinical trials are ongoing to slow the progression of age-related macular degeneration, and some methods can provide some relief to those with geographic atrophy.
One of these approaches is to reduce oxidative stress in the retina, which will slow the progression of geographic atrophy (Wang et al., 2021). One can use antioxidants like vitamins C and E to mitigate oxidative stress. These powerful agents act as protective shields against free radicals. Free radicals are particles produced by the body's metabolism. Other supplements, such as zinc, have also shown some promise in supporting retinal function.
Different approaches for macular diseases include laser photocoagulation and photodynamic therapy (Johns Hopkins Medicine, n.d.). These make use of lasers and light to target abnormal blood vessels selectively. Laser photocoagulation seals leaking blood vessels in the retina. At the same time, photodynamic therapy uses light alongside a laser to do the same. Ultimately, both treatment methods focus on minimizing the amount of light reaching the retina, thereby reducing the damage to cells and blood vessels in the macula.
WilliamA.Haseltine,PhD 131
Further treatments for macular degeneration are currently being studied. These additional approaches include complement inhibitors that prevent inflammation and cell damage and stem cell therapies that replace the damaged cells.
Research by the National Natural Science Foundation of China has shown that stem cells can regenerate retinal pigment epithelium and photoreceptor cells (Noble et al., 2022), essential components in a healthy retina. Geographic atrophy and dry macular degeneration impact these retinal cells, so stem cell therapies may be an ideal approach to reversing the once irreversible vision loss associated with them.
The results of stem cell therapies for age-related macular degeneration and geographic atrophy are promising. Animal studies and clinical trials have seen improved vision; further clinical trials are underway.
One example of a recent clinical trial currently investigating stem cell therapy for geographic atrophy is OpRegen (Hoffmann-La Roche, 2023). This trial tests the safety and tolerability of embryonic stem cell-derived retinal pigment epithelium cells. The trial showed that this treatment has a favorable safety profile with no reports of inflammatory or immune responses. Also, there was a marked increase in visual function.
Still, careful consideration is needed when determining the appropriate cell type for each patient, as derivation and transplantation techniques must be optimized. Furthermore, longterm clinical trial data is necessary to evaluate the feasibility of wideuse stem cell therapies for retinal disorders.
BetterEyesight 132
Gene Therapies
Gene therapy can potentially address many acute and chronic diseases. Applying gene therapy and gene editing to restore vision has been especially fruitful. According to the World Health Organization (WHO), age-related macular degeneration affects over 196 million people globally (World Health Organization, 2023). The incidence of the disease will likely increase in the coming years due to aging populations in many countries.
These findings have prompted researchers to develop intervention strategies based on individual polygenic risk scores. However, interpreting these scores at a personal level may be challenging. As a result, more traditional approaches to gene therapy and gene editing have been considered for age-related macular degeneration.
Gene therapy and gene editing are two different approaches to treating genetic mutations. Gene therapy replaces a defective gene with a functional one through a delivery vector. Gene editing, on the other hand, involves manipulating the target gene at the DNA or genomic level. CRISPR-based gene technologies permit both the substitution of entire genes and the editing of small region target sequences. CRISPR-based treatments have been studied for retinal disorders such as retinitis pigmentosa.
Over the past five decades, gene therapy has evolved from a simple concept to the subject of over 1400 clinical trials across the globe, offering a degree of innovation and intervention never seen before. More particularly, viral vector gene therapy has emerged as an innovative treatment option for retinal diseases such as wet and dry age-related macular degeneration, paving the way for revolutionary treatment plans that could significantly improve patient outcomes.
WilliamA.Haseltine,PhD 133
BetterEyesight
In gene therapy, a vector is a vehicle that delivers therapeutic genes or nucleic acids to target cells to treat genetic disorders or diseases. Typically, vectors can be divided into two categories: viral and nonviral vectors. Viral vectors utilize modified viruses to deliver the desired gene to the target cells. In contrast, nonviral vectors use alternative methods to provide genes to target cells.
Messenger RNA (mRNA) has emerged as a nonviral gene therapy vector that shows promising potential in inducing cellular and therapeutic immune responses. Through its versatile protein delivery mechanism and dendritic cells' potent antigen-presenting abilities, mRNA can deliver genetic information to treat various inherited and acquired diseases. mRNA is also often used alongside CRISPR for retinal disorders, cancer treatment, and other CAR T therapies.
The inability to integrate into the host genome and the strictly transient expression are additional benefits that make mRNA therapy a promising avenue for safe and effective gene therapy. However, viral vectors often have greater efficiency in transferring genes to target cells than nonviral vectors, and researchers have therefore been working on modifying viral vectors to reduce the risks involved in their use in human subjects.
The concept of using viruses as vectors dates back to the 1970s. However, it wasn't until the 1980s that scientists could manipulate viral genomes without adverse effects. Recently, the spotlight has fallen on adeno-associated viral, or AAV, vectors. AAVs are a class of small DNA viruses that infect humans and other primates without causing illness. These developments have enabled new applications in gene therapy, with their use surging in clinical trials.
134
Scientific research has discovered that in mouse muscle tissue, in vivo administration of AAV vectors can provide long-term transgene expression and effective relief. By requiring a helper virus to replicate, AAV vectors present a significant advantage because they are unlikely to be associated with a disease. Thus, essential proteins coding for viral replication and integration can be removed from the AAV genome.
Moreover, AAV vectors have demonstrated a capacity to elicit a relatively mild immune response, mitigating the chance of producing a host immune response while substantially decreasing the overall vector dose required for therapeutic efficacy. This lessened risk inherent in AAV vector therapeutics makes them particularly promising for clinical trial exploration.
The suitability of eyes as targets for gene therapy stems from the fact that individual genes are responsible for different conditions, making it possible to replace a single gene to minimize payload delivery for AAV vectors and avoid potential errors arising from large transgenes. Furthermore, the potential of a single gene therapy dose presents a marked improvement over frequent intravitreal injections to treat retinal diseases.
One of the landmark breakthroughs in gene therapy occurred when three clinical trials evaluated the efficacy of adeno-associated virus serotype two vectors carrying a functional copy of the retinal pigment epithelium-specific 65-kDa protein gene, or RPE65. This gene encodes the RPE65 protein, critical in the biological conversion of light photons into electrical signals transmitted to the brain via the optic nerve.
WilliamA.Haseltine,PhD 135
This groundbreaking research led to the FDA's approval of the firstever ocular gene therapy: Voretigene Neparvovec-rzyl, also called Luxturna. Spark Therapeutics develops Luxturna to treat confirmed cases of inherited retinal dystrophy caused by RPE65 mutations. Approved by the United States Food & Drug Administration in December 2017, Luxturna is a one-time subretinal injection of a functional copy of the RPE65 gene that becomes transduced into the retinal cells.
The injection of Luxturna delivers a functional copy of the RPE65 gene to the retinal cells, allowing the production of RPE65-specific protein, which is crucial for the retinoid cycle. By restoring the retinoid process, Luxturna aims to improve vision and preserve existing vision. Today, Luxturna is being administered at ten treatment centers in the United States, and it remains a significant breakthrough in gene therapy.
Since the approval of Luxturna, other clinical trials evaluating gene therapies have reported positive results, indicating that gene therapy could revolutionize age-related macular degeneration treatment plans.
Researchers are also exploring subretinal and suprachoroidal injections and using adeno-associated viruses (AAVs) as vectors for gene delivery. Potential therapies, including ADVM-022, RGX-314, GT-005, and HMR59, have shown encouraging results in preclinical and clinical trials, with sustained expression of therapeutic proteins and reduced need for repeated injections. Moreover, they have exhibited a relatively low incidence of adverse events, making them viable candidates for widespread use.
136
BetterEyesight
ADVM-022 is a promising gene therapy developed by Adverum Biotechnologies to treat neovascular age-related macular degeneration. The treatment aims to deliver a protein via a single intravitreal injection, thereby reducing the need for repeated injections every 4-8 weeks.
Preclinical studies in nonhuman primates have demonstrated sustained expression for up to 30 months after a single intravitreal injection of ADVM-022. Further trials found that a single intravitreal injection of ADVM-022 significantly reduces the frequency of anti-VEGF injections.
While inflammation has been the main adverse event in the trial, no ADVM-022-related non-ocular adverse events have been reported. The lower dose of ADVM-022 has been associated with fewer cases of inflammation, and all treatment-related ocular adverse events have been mild or moderate.
RGX-314 is another promising gene therapy for treating neovascular age-related macular degeneration. It is developed by REGENXBIO Inc. The treatment employs an adeno-associated virus vector-based gene delivery system that expresses a monoclonal antibody fragment resembling ranibizumab, a well-established anti-VEGF therapy.
RGX-314 is delivered either subretinally or suprachoroidally and offers the potential for sustained anti-VEGF antibody production while reducing the burden of multiple intravitreal injections. RGX314 is generally well-tolerated, with no reports of an abnormal immune response, drug-related ocular inflammation, or postsurgical inflammation made thus far.
GT-005 targets dry age-related macular degeneration patients. Dry macular degeneration accounts for most age-related macular
137
WilliamA.Haseltine,PhD
degeneration cases, and currently, no effective therapies are available. Advanced dry macular degeneration, or geographic atrophy, is a debilitating eye condition that can lead to permanent vision loss due to the irreversible degeneration of retinal pigment epithelial cells and their overlying retinal photoreceptors.
GT-005 employs an adeno-associated viral vector (AAV) to enhance CFI expression levels. An AAV is a small virus modified to deliver therapeutic genes to cells; in the case of GT-005, the AAV deposits therapeutic genes in the cells of the retina. This design allows the therapy to be a one-time treatment delivered under the retina. GT005 is currently undergoing evaluation in Phase I and II trials. Thus far, no GT-005-related severe adverse events (SAEs) have been observed.
The other primary gene therapy currently being investigated for treating dry age-related macular degeneration is HMR59 by Hemera Biosciences. HMR59 focuses on preserving vision in those with late-stage geographic atrophy. Its purpose is to enhance the capacity of retina cells to produce a soluble version of CD59 protein.
CD59 is one of the proteins that protect the retina from damage from the complement system. As we know, any imbalance in the complement system can lead to the death of light-sensitive cells in the back of our eyes and vision loss. By increasing the activity of CD59 using gene therapy, HMR59 can protect these vital cells from destruction due to complement-induced damage.
Like GT-005, HMR59 is a one-time treatment. Researchers administer the medication by injecting it into the transparent gellike substance inside the eye. At the time of writing, HMR59 phase
BetterEyesight 138
I studies are complete, and phase II has begun. There is also another phase I trial starting to see if there are any beneficial effects of HMR59 on wet age-related macular degeneration.
HMR59 is another new retinal gene therapy in the form of an AAV2 vector-based treatment. This therapy is administered intravitreally, seven days after a single intravitreal injection of anti-VEGF treatment. HMR59 intends to provide protection against the complement cascade and reduce the incidence of macular neovascularization. Clinical trials have shown promising results, and ongoing studies will be evaluated for long-term safety and efficacy.
Despite the immense potential of gene therapy, there are still many issues that must be addressed for it to become widely used. However, recent improvements, such as dose optimization, efficient administration routes, effective management post-injection, and long-term benefits, have yielded promising results, offering hope for the future of gene therapy.
The discussed advances in gene editing and therapy have made retinal gene therapies a dynamic and ever-evolving field. There's much to anticipate in improved conditions and the clinical potentials that lie ahead.
Protein - Based Therapies
No approved protein-based therapies for treating dry macular degeneration exist. Still, ongoing research and clinical trials hold promise. Scientists are studying potential protein-based treatments such as antioxidative therapy and complement cascade inhibition therapy.
WilliamA.Haseltine,PhD 139
BetterEyesight
Before we explore the complement therapies, it is essential to understand currently accepted antioxidative treatments and the complement system. Antioxidant therapy aims to decrease oxidative stress and inflammation in the retina, contributing to dry macular degeneration. Antioxidative treatment focuses on improving retinal defenses against oxidative damage through the dietary intake of antioxidants, developing antioxidant-based drugs, and gene therapies.
Antioxidants neutralize harmful free radicals produced by the body and reduce oxidative damage in cells. They can be enzymatic or non-enzymatic. Enzymatic antioxidants include proteins like superoxide dismutase, catalase, and glutathione peroxidase. Each plays a role in the body's natural defense against oxidative stress.
Antioxidative therapy concerning age-related macular degeneration focuses on improving retinal defenses against oxidative damage through the dietary intake of antioxidants, developing anti-oxidantbased drugs, and gene therapies. This type of therapy is a broader range of approaches and includes more than just protein-based therapies; the complement cascade inhibition therapies, on the other hand, are more specific.
The complement system and its related cascade are vital to the immune system. It consists of proteins that activate a response when the body encounters an antigen. The complement system has three major pathways: the classical, alternative, and lectin pathways. About half of all dry age-related macular degeneration patients have gene mutations that affect complement regulation (Geerlings et al., 2017), particularly in the genes involved in the alternative pathway.
140
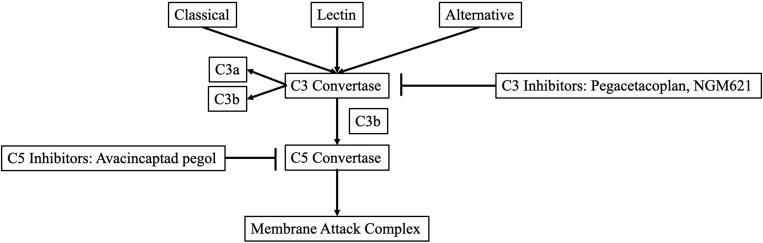
SOURCE: Clinical Ophthalmology
All the paths converge and form a C3 convertase, breaking into C3 and C3b. C3 is involved in tissue damage and inflammation, while C3b is needed to create C5 convertase. C5 is an inflammatory molecule. When C3, C3b, and C5 team up, they make a membrane attack complex or MAC. This MAC damages cells and attracts cells to form swelling, which is necessary for the immune response.
The imbalance of the complement system is a significant factor in age-related macular degeneration. However, developing complement inhibitors for macular degeneration treatment is challenging due to the complexity of the complement system and the variability in individual responses to these inhibitors.
Ongoing research and clinical trials actively explore the potential of complement inhibitors as a viable therapeutic approach for dry agerelated macular degeneration. The current focus revolves around rigorously evaluating the effectiveness of complement inhibitors. This evaluation requires robust and sensitive measures to gauge disease progression and treatment response.
The design of clinical trials carefully considers these factors in conjunction with outcome measures. Despite the challenges,
WilliamA.Haseltine,PhD 141
FIGURE 42: Development of geographic atrophy therapeutics in targeting the complement cascade.
continuous research and clinical trials persist in investigating complement inhibitors as a promising therapeutic option for dry age-related macular degeneration.
Nearly 40 clinical trials have examined or are exploring a minimum of 14 distinct complement inhibitors for age-related macular degeneration (Qin et al., 2021). Unfortunately, several of these trials have yielded disappointing results. For instance, lampalizumab, an anti-factor D antibody, did not meet expectations in two phase III trials focused on geographic atrophy. However, amidst these setbacks, two complement inhibitors, namely APL-2 and Zimura, have exhibited remarkable efficacy in inhibiting the progression of geographic atrophy during phase II clinical trials.
APL-2 is also known as pegcetacoplan and works by inhibiting the C3 complement. In a phase II trial, APL-2 showed promising results by reducing the growth rate of geographic atrophy by 29% monthly and 20% every other month compared to the placebo group (Qin et al., 2021).
Zimura, on the other hand, acts as a C5 inhibitor. When patients received a monthly dosage of Zimura along with anti-VEGF, approximately 60% experienced a visual acuity improvement of three lines or more. This outcome is better than those who received anti-VEGF alone (Qin et al., 2021).
Zimura is unique because it is effective for both wet and dry macular degeneration subtypes. The effectiveness of Zimura as a new medication for addressing dry age-related macular degeneration will rely on the outcome of the ongoing phase III clinical trials.
BetterEyesight 142
Of course, dry macular degeneration is not the only type of agerelated macular degeneration, and there are protein-based options for wet macular degeneration. Wet age-related macular degeneration is characterized by the growth of abnormal blood vessels beneath the retina, which can lead to fluid leakage, scarring, and, ultimately, vision loss. This debilitating consequence has prompted extensive research and the development of innovative treatment approaches.
Currently, the primary treatment option for wet age-related macular degeneration involves the injection of anti-vascular endothelial growth factor. Anti-VEGF therapy is a type of treatment that targets the activity of vascular endothelial growth factor (VEGF). This protein promotes the formation of blood vessels. The therapy is based on administering drugs, such as monoclonal antibodies or tyrosine kinase inhibitors, that block the function of VEGF or its receptors, known as VEGFRs.
Anti-VEGF therapy has revolutionized the treatment of ocular diseases like wet age-related macular degeneration. By restraining the activity of VEGF, this therapy can suppress the growth and spread of tumors and hinder the formation of new blood vessels. VEGF-A is responsible for normal and abnormal vessel growth and leads to the activation of VEGF receptors on endothelial cells. It is crucial to understand that various types of VEGFs attach to different receptors, thereby promoting the generation of vessels. However, if this process is unregulated, it can harm photoreceptors, leading to irreversible vision loss.
Anti-VEGF drugs have been extensively studied and have shown efficacy in various cancer types and visual conditions. However,
WilliamA.Haseltine,PhD 143
some patients may eventually develop drug resistance or experience adverse effects.
One of the most well-known drugs in this class is ranibizumab, which was first approved in 2004. This monoclonal antibody binds specifically to VEGF-A, preventing it from interacting with receptors on the surface of vascular endothelial cells in the eye. Doing so can block the formation of new blood vessels, a hallmark of several eye diseases, including age-related macular degeneration.
Aflibercept is another drug that targets the VEGF pathway, but it works slightly differently than ranibizumab. Rather than blocking VEGF-A directly, it binds to all isoforms of VEGF and placental growth factor, another member of the VEGF family. This broader binding profile allows aflibercept to inhibit angiogenesis, or the formation of new blood vessels, more comprehensively than ranibizumab.
Faricimab is a newer drug that has shown great promise in clinical trials. Rather than targeting VEGF directly, it works by inhibiting both VEGF-A and Ang-2, another protein involved in angiogenesis. This dual inhibition has yielded superior outcomes compared to drugs targeting only VEGF-A.
Finally, brolucizumab is a drug approved more recently, in 2019. Like ranibizumab, it explicitly targets VEGF-A but has some unique features that distinguish it from other drugs in this class. Specifically, it has a smaller molecular size than different monoclonal antibodies, allowing it to penetrate tissues more quickly and persist for extended periods.
BetterEyesight 144
With all these options to halt the onset of wet macular degeneration, we now have renewed hope for millions affected by this devastating disease, especially as more clinical trials are underway.
While ranibizumab and other drugs have proven effective in treating wet AMD, ongoing research focuses on developing newer, more targeted VEGF inhibitors.
Several VEGF inhibitors are developing and showing promising results in early studies. For instance, a 2020 meta-analysis demonstrated that long-term anti-VEGF treatment patients were almost nine times more likely to gain 15 or more letters on the bestcorrected visual acuity test than those receiving placebo injections (Wong et al., 2014).
Clinical trials show that repeated injections of anti-VEGF drugs into the gel-like substance inside the eye, known as the vitreous, significantly improve patient vision (Kaiser et al., 2021). This discovery makes it possible to manage the disease as a chronic illness rather than an unpreventable, blinding condition.
The regulatory approval process for anti-VEGF agents is rigorous, and these drugs are monitored closely for safety and efficacy. The increase of the vascular endothelial growth factor family is crucial to developing neovascular diseases, which is the main characteristic of wet age-related macular degeneration.
These therapies offer considerable visual results and provide opportunities for enhancing visual outcomes in patients with wet age-related macular degeneration. Thus, proactive and targeted disease management through anti-VEGF therapies has become a significant focus of wet age-related macular degeneration treatment.
WilliamA.Haseltine,PhD 145
These anti-VEGF injections can be expensive, require frequent administration, and cause adverse effects such as vision problems, eye infections, and retinal detachment. This has driven research into alternative therapies for macular degeneration, one of which is DARPins.
Macular degeneration is an age-related eye disease that affects the macula, which is the part of the retina responsible for sharp, central vision. The disease causes a progressive loss of vision that starts in the center of the visual field and can advance to total blindness.
There are two types of macular degeneration: dry and wet. Dry macular degeneration is the most common form. It is characterized by the slow breakdown of cells in the macula and the accumulation of debris in the retina. Wet macular degeneration, on the other hand, is less common but more severe, as it is characterized by the growth of abnormal blood vessels underneath the retina. These blood vessels can leak and cause permanent damage to the retina, leading to rapid vision loss.
Designed Ankyrin Repeat Proteins (DARPins) are synthetic proteins that show promise as a treatment. These engineered proteins exhibit powerful therapeutic potential as they can target the factors contributing to blood vessel growth and leakage, which are characteristic traits of macular degeneration.
With their innovative design, promising preclinical and clinical data, and potential to provide a new chapter in treating retinal disorders, DARPins hold great promise for improving outcomes for patients with wet age-related macular degeneration and related conditions.
146
BetterEyesight
DARPins, a class of engineered proteins, hold immense promise and have garnered significant attention due to their versatility and potential biomedical applications. These proteins are derived from ankyrin repeat motifs, which naturally occur in protein domains across various organisms.

SOURCE: European Bioinformatics Institute
Ankyrin repeats consist of approximately 33 amino acids. These repeats intricately fold into specific shapes, forming highly stable protein domains. This inherent stability allows ankyrin repeats to play crucial roles in diverse cellular processes, contributing to their functional diversity.
DARPins are created by repeating and rearranging these units to achieve specific binding properties and target recognition. This
WilliamA.Haseltine,PhD 147
FIGURE 43: Cartoon representation of the molecular structure of protein registered with 2qyj code
modular design empowers DARPins to be customized and optimized for various applications, including therapeutic agents or diagnostic tools. The exceptional specificity and affinity of DARPins make them an ideal option for binding to complex molecules, such as disease-specific biomarkers and specific protein receptors.
DARPins offer a multitude of advantages over antibody treatments for retinal disorders. Their compact structure allows better tissue penetration, including the retina, resulting in improved therapeutic delivery. Furthermore, DARPins can be engineered with exceptional affinity and specificity for target molecules, enhancing their therapeutic efficacy while minimizing off-target effects. They also exhibit remarkable stability, resisting degradation by proteases, making them a superior choice for retinal disorder treatment.
While assessing the advantages, we must also consider the potential drawbacks. It is crucial to recognize the intricacies involved in manufacturing, which demands specialized facilities and expertise. Additionally, ongoing clinical development, regulatory approval, and managing risks associated with immunogenicity and delivery challenges require further research and advances in protein engineering to fully unlock the potential of DARPins and overcome limitations related to their utilization.
BetterEyesight 148

44: Representations of a single designed ankyrin repeat domain and a multidomain DARPin® drug candidate. Molecular model of MP0250, a DARPin® drug candidate consisting of four DARPin® domains (molecular weight approximately 62 kDa). The scaffold is dark blue, and the potential target interaction residues of the individual domains are orange (human serum albumin [HSA]), cyan (hepatocyte growth factor [HGF]), and red (vascular endothelial growth factor [VEGF])
SOURCE: Beyond Antibodies: The Darpin® Drug Platform. Biodrugs.
Among the DARPins currently in clinical trials for retinal diseases, some of the most notable candidates include abicipar pegol, RG7716, and conbercept.
Abicipar pegol is a therapeutic agent targeting vascular endothelial growth factor-A (VEGF-A) in treating neovascular age-related macular degeneration and diabetic macular edema. Clinical investigations have reported that abicipar pegol demonstrated comparability to ranibizumab regarding efficacy, with a similar safety profile. However, there are some potential limitations to the therapy, such as an increased incidence of intraocular inflammation observed in some patients compared to other anti-VEGF treatments.
WilliamA.Haseltine,PhD 149
FIGURE
RG7716 is a bispecific DARPin binding to VEGF-A and Angiopoietin-2 (Ang-2). This unique feature holds promise in effectively blocking pathological angiogenesis, thus preventing blindness. Clinical trials have reported that RG7716 shows a statistically significant improvement in best-corrected visual acuity (BCVA) over the currently accepted therapy of aflibercept injections in patients with neovascular age-related macular degeneration. However, RG7716 has been associated with mild to moderate fever in some patients, and its use is not recommended for patients with a history of significant infusion reactions.
Conbercept is an innovative fusion protein that combines a DARPin domain, specifically designed to target VEGF receptors, with a domain derived from a human immunoglobulin. Clinical trials have shown its efficacy in treating various retinal disorders, including neovascular age-related macular degeneration and macular edema associated with retinal vein occlusion. Conbercept has also exhibited higher binding affinity to VEGF than other antiVEGF agents, resulting in superior inhibition of pathological angiogenesis. However, a potential limitation of the therapy is that it is administered through intravitreal injection, which can cause adverse effects such as intraocular inflammation or endophthalmitis.
Geographic Atrophy Secondary to Age - Related Macular Degeneration
Dry age-related macular degeneration is a progressive condition characterized by the gradual deterioration of the macula, the area responsible for sharp central vision. As the cells in the retina in this
BetterEyesight 150
area die and are not regenerated, visual acuity deteriorates progressively.
The dry subtype is the most common form for about 80% of all macular degeneration cases (Boyd & Vemulakonda, 2019). It occurs when tiny yellow deposits known as drusen accumulate beneath the retina. These drusen are waste products that gradually enlarge, leading to the death of retinal cells in the macula and resulting in blurred vision. The progression of the disease typically unfolds slowly over time, with three stages: early, intermediate, and late.

SOURCE: ACCESS Health International
Late-stage dry macular degeneration can lead to the onset of geographic atrophy. Geographic atrophy causes retinal cells to waste away and die, creating patchy areas in the retina that cause blind
WilliamA.Haseltine,PhD 151
FIGURE 45: A comparison of normal vision and vision with age-related macular degeneration.
spots in vision. These areas of dead and dying cells appear in retinal images and resemble a map, which is why it's called geographic atrophy. It can impact one or both eyes. It is estimated to affect around 1% of the population in the United States (The AREDS Research Group, 2009) and over 8 million people globally (Krogh Nielson et al., 2023).
Although the exact cause of geographic atrophy is unclear, it likely results from genetic and environmental factors. Risk factors associated with age-related macular degeneration and geographic atrophy include smoking, age, and family history. Fortunately, there is now an FDA-approved treatment for geographic atrophy.
In 2023, the FDA approved pegcetacoplan or Syfovre® for treating dry age-related macular degeneration (Pavluk, 2023b). This medication works by inhibiting a protein found in the complement system. The complement system is part of the immune system and is responsible for attacking foreign bodies. It recognizes, tags, and eliminates any foreign particles. In dry macular degeneration, an overactive complement system damages retinal cells, leading to blind spots in vision.
Syfovre® prevents the complement system's C3 protein from becoming out of control. Properly managing this slows down retinal damage, halting the progression of geographic atrophy.
BetterEyesight 152

FIGURE 46: Structure of Pegcetacoplan
SOURCE: Wikimedia Commons
Clinical trials of Syfovre® showed that injections can slow the growth of sores, thus preserving vision. The medication is injected directly into the clear gel-like substance that fills the eye. As with any injection, the risk of inflammation and infection is increased. Apellis has reported an increased incidence of eye inflammation during clinical trials, which led some experts to question the risk-tobenefit profile of the drug.
One such expert, Demetrios Vavvas, an ophthalmology professor at Harvard Medical School and the director of the Retina Service at Massachusetts Eye and Ear, expressed his concern in an interview where he said, "As the potential benefit goes up, the risks go up, and the benefits are potential. The risks are real" (Fidler, 2023).
Vavvas' concerns were validated on July 29, 2023 (Pavluk, 2023a), as Apellis' lead researchers presented the safety and efficacy of Syfovre® at the American Society of Retinal Specialists Annual Conference (American Society of Retina Specialists, n.d.). The presentation led to the safety committee advising the American Society of Retinal Specialists to publish a letter of concern regarding increased cases of ocular inflammation. More specifically, six instances of occlusive retinal vasculitis were reported.
WilliamA.Haseltine,PhD 153
Retinal vasculitis is a potentially blinding inflammation of the eye, and at least one of the six impacted individuals reported significant vision loss after receiving their injection. Apellis said that the incidence of this particular eye inflammation aligns with their findings in clinical trials with an estimated rate of 0.01% per injection (Pavluk, 2023a).
Still, there is cause for concern, considering individuals must receive these injections every 25 to 60 days, depending on severity, for this treatment to be effective. The inflammation and retinal vasculitis cases have not been tied to any particular batch of medication or manufacturing issues (Fidler, 2023). However, patients reported the effects two weeks after their first Syfovre® injection.
Apellis is currently investigating these reports concerning their geographic atrophy medication, but what if we could treat dry agerelated macular degeneration before it becomes geographic atrophy?
Two studies conducted by the National Eye Institute, a branch of the National Institute of Health, explore the relationship between vitamins and eye health. More specifically, these studies, known as Age-Related Eye Disease Studies, or AREDS and AREDS2, determined whether vitamins and minerals could slow the progression of age-related eye diseases like dry macular degeneration (The AREDS Study Group, n.d.).
The initial AREDS study indicated that vitamins C and E, copper, and zinc successfully slowed the progression of macular degeneration. AREDS2 expanded this by including lutein, zeaxanthin, and omega-3 fatty acids, ultimately showing an even
BetterEyesight 154
more pronounced effect in slowing down the disease. Although nutritional supplements cannot cure macular degeneration, they are a viable option to slow its progression. Acknowledging that dietary supplements do not effectively manage late-stage dry macular degeneration or geographic atrophy is also essential. This is why gene therapies are being investigated as potential treatments for the disease.
WilliamA.Haseltine,PhD 155
CHAPTER 7
Other Macular Issues

Stem Cells for Stargardt's Macular Dystrophy
Stem cells are undifferentiated cells that can develop into specialized cells. They repair or replace damaged tissue, are a promising area of medical research, and treat diseases like leukemia and spinal cord injuries.
In ophthalmology, stem cell therapies are a promising treatment for retinal diseases. They involve transplanting stem cells into the eye to replace damaged or diseased retinal cells. The ultimate goal is to regenerate healthy retinal cells, which can reverse vision loss and improve the overall quality of life for patients suffering from retinal diseases. In previous chapters, we have discussed the use of stem cell therapies in treating various optical disorders, such as retinitis pigmentosa and age-related macular degeneration.
Despite being experimental, stem cell therapies for retinal diseases have exhibited promising results in preclinical studies and earlystage clinical trials. However, further research is imperative to ensure the safety and effectiveness of these therapies before their widespread implementation.
156
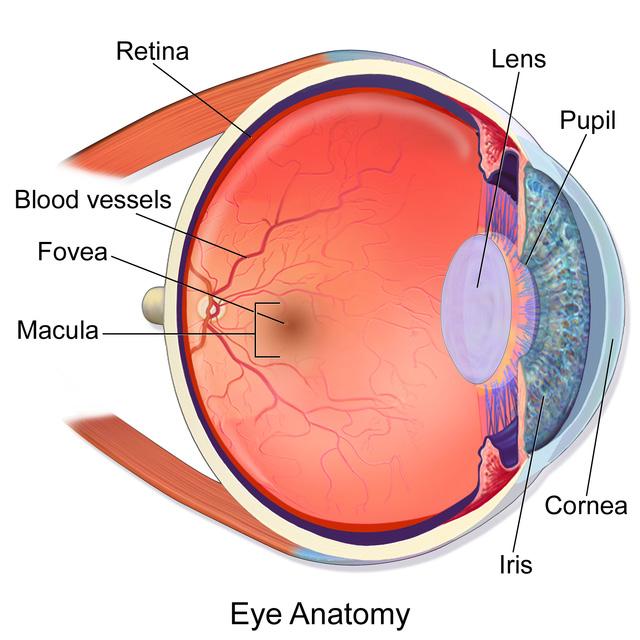
SOURCE: Blausen.com staff (2014). "Medical gallery of Blausen Medical 2014". WikiJournal of Medicine 1 (2).
DOI:10.15347/wjm/2014.010. ISSN 2002-4436.
Stargardt's Macular Dystrophy (SMD) is a rare genetic disorder that predominantly affects the macula, a small region at the back of the eye's retina responsible for central vision. This disorder, also known as Stargardt disease, is named after the German ophthalmologist Karl Stargardt, who first discovered it in 1901.
SMD is an inherited retinal disorder passed through an autosomal recessive pattern. The condition results from mutations in the ABCA4 gene, which codes for the protein responsible for transporting wastes from the retina's photoreceptor cells. When this gene gets mutated, abnormal accumulation of toxic molecules in
WilliamA.Haseltine,PhD 157
FIGURE 47: Anatomy of the eye
the photoreceptors leads to their degeneration, ultimately causing vision loss.
Patients with SMD often experience a gradual loss of central vision, essential for reading, driving, and recognizing faces. The initial symptoms usually surface during early to mid-adolescence, with most patients experiencing significant visual impairment by their twenties. The age of onset, the rate of progression, and the severity of the symptoms vary significantly from one individual to another, making it challenging to predict the rate of vision loss.
Central vision loss is not the only consequence of SMD. Patients with this disorder may also experience other vision issues, such as sensitivity to light, reduction in color perception, and the appearance of blind or blank spots in their visual field. Unfortunately, there is currently no cure for Stargardt's Macular Dystrophy. Nonetheless, early diagnosis through genetic testing and regular check-ups with an ophthalmologist can help slow the progression of vision loss through early intervention.
Stargardt's Macular Dystrophy shares similarities with retinal disorders such as age-related macular degeneration and retinitis pigmentosa. AMD, like SMD, affects the macula but is more prevalent and is associated with aging.
Conversely, RP involves the photoreceptor cells in the peripheral part of the retina, leading to gradual night blindness and eventual loss of central vision. Despite these differences, these conditions culminate in vision loss, making them a significant concern to the affected individuals, their families, and the healthcare system.
Researchers are currently investigating the use of stem cells to treat SMD (MD Stem Cells, 2023). Several clinical trials (Fondation
BetterEyesight 158
Stargardt, 2018) are underway in which scientists use different types of stem cells, such as embryonic stem cells, induced pluripotent stem cells, and adult stem cells (Hinkle et al., 2021). These trials aim to replace the damaged cells in the retina with healthy cells derived from stem cells. This replacement can help in halting or even reversing the progression of the disease, potentially restoring some degree of vision to the patients.
Although the clinical trials are still in their early stages, stem cell therapy could offer a promising solution for treating SMD and other retinal diseases. However, it may take several years before this treatment becomes widely available, and more research is needed to demonstrate its long-term safety and effectiveness.
Stem cell therapies have emerged as an advanced treatment for several retinal diseases. These therapies involve using stem cells to replace or repair damaged cells and tissues in the eye to restore or enhance vision. One of the most significant advantages of stem cell therapies is their ability to target a wide range of retinal diseases, including age-related macular degeneration, retinitis pigmentosa, and diabetic retinopathy. Stem cell therapy is versatile, and it has the potential to benefit a large number of patients suffering from these debilitating conditions.
For stem cell therapies to become available to the general public, several challenges must be overcome. One significant challenge is ensuring that the transplanted stem cells integrate seamlessly with the patient's eye and do not cause any harm. Additionally, the cost of these therapies remains a concern, which may restrict many patients from accessing them.
WilliamA.Haseltine,PhD 159
Despite these challenges, the progress made in clinical trials is highly promising. Researchers have shown that stem cell therapies can improve vision in some patients, and they continue to explore new ways to optimize these treatments. With continued research and development, stem cell therapies have the potential to revolutionize the way we treat retinal diseases and improve the lives of millions of patients worldwide.
Macular Edema
Picture the world around you without the ability to read, drive, or even recognize your loved ones' faces. This is the reality for those suffering from macular edema, a debilitating condition caused by fluid accumulation in the macula, the central area of the retina responsible for providing precise and detailed vision.
With symptoms such as distortions, blurriness, and loss of sight, macular edema can profoundly impact a person's quality of life and daily activities. Finding effective treatments is critical to preserving patients' vision and enhancing their well-being.
Thanks to recent medical breakthroughs, there are now multiple ways to treat macular edema, including medications, laser therapy, and surgery. These treatments can target underlying causes such as diabetes, high blood pressure, age-related macular degeneration, and inflammatory eye diseases.
Macular edema is a condition caused by multiple factors, with inflammation being one of the primary contributors. Inflammation triggers the release of cytokines and growth factors, which cause leakage from the blood vessels in the retina. Among these growth factors is vascular endothelial growth factor (VEGF), which plays a
160
BetterEyesight
significant role in forming new blood vessels and angiogenesis. When someone has macular edema, their body makes too much VEGF. This can cause new blood vessels to grow and leaky blood vessels in the eye.
Besides inflammation, oxidative stress is also a significant contributor to macular edema. The cells in our eyes are susceptible to damage from oxidative stress, which can result in inflammation. This inflammation can be dangerous and lead to the breakdown of the blood-retinal barrier (BRB), which prevents fluid leakage from the blood vessels. When the BRB is compromised, fluid can seep into the retina, leading to swelling and, eventually, vision loss.
It is important to note that macular edema can occur due to various underlying conditions, such as diabetes, ocular hypertension, and age-related macular degeneration. These underlying conditions can cause changes in the retinal microenvironment, leading to the release of pro-inflammatory cytokines, growth factors, and free radicals that contribute to the development of macular edema.
The treatment options for macular edema vary depending on the underlying condition, the severity of the edema, and the patient's overall health. In some cases, addressing the underlying condition, such as controlling blood sugar in diabetes, is enough to resolve the edema. However, in many cases, more aggressive treatment is necessary.
Current treatment options for macular edema include laser photocoagulation, corticosteroids, and anti-VEGF agents. Laser photocoagulation involves using a high-energy beam of light to target the blood vessels in the retina, causing them to seal off and prevent further leakage corticosteroids, such as triamcinolone,
WilliamA.Haseltine,PhD 161
work by reducing inflammation and swelling in the macular tissue. However, corticosteroids have risks associated with their use, such as elevated intraocular pressure and cataract formation.
Anti-VEGF agents, such as aflibercept and ranibizumab, are currently the first-line treatment for macular edema. These drugs work by binding to and neutralizing the excess VEGF in the eye, reducing vessel permeability and preventing neovascularization. These agents are delivered through intravitreal injections, which involve injecting the drug directly into the eye. While anti-VEGF agents have successfully improved vision and slowed disease progression, they come with limitations, such as frequent injections, and possible adverse effects, such as inflammation and endophthalmitis.

SOURCE: Advances in Novel Pharmaceutical Options in Ophthalmology
BetterEyesight 162
FIGURE 48: Molecular mechanism of action of faricimab leads to decreased vascular leakage and inhibited neovascular processes.
The advent of bispecific antibodies, such as faricimab, offers a new therapeutic strategy in macular edema treatment. Faricimab targets both the VEGF and the angiopoietin-Tie pathways, providing a complete blockade of neovascularization and vascular leakage.
Numerous studies, including Phase III trials (TENAYA, LUCERNE, RHINE, and YOSEMITE), have demonstrated the efficacy and safety of faricimab in treating macular edema associated with w-AMD and diabetic macular edema (DME) (Ferro Desideri et al., 2023). In these trials, faricimab has been shown to maintain clinical efficacy over more extended treatment regimens than aflibercept.
In addition to improving vision outcomes, treating macular edema has significant economic benefits. A recent study estimated the total direct and indirect benefits of DME treatment to be 63.0 billion and 4.8 billion, respectively, over 20 years (Mulligan et al., 2023). This value includes improved quality of life, employment outcomes, and disability outcomes associated with DME treatment.
Diabetic Macular Edema
Diabetic macular edema is a severe complication of diabetes that affects a person's vision and can lead to blindness if left untreated. Diabetic macular edema (DME) is a leading cause of vision loss among people with diabetes, and its prevalence is increasing. More specifically, the University of Toronto found that the pooled prevalence of DME was approximately 5.5% among people with diabetes (Im et al., 2022). However, the good news is that effective treatments are available, including laser photocoagulation therapy.
WilliamA.Haseltine,PhD 163
Laser therapy, specifically subthreshold and multimodal imagingguided laser therapy techniques, has emerged as an essential treatment option for DME. These cutting-edge therapies are more precise, less invasive, and offer significant advantages over traditional laser therapy. They can reduce the need for frequent follow-up appointments, improve treatment outcomes, and significantly reduce patient treatment burden.
Diabetic macular edema (DME) is a severe complication of diabetes that can lead to vision loss and blindness if left untreated. It is a type of macular edema that occurs when fluid accumulates in the macula, which is the central part of the retina responsible for sharp, detailed vision.
DME is caused by damage to the retina's blood vessels due to high blood sugar levels over time. This damage causes the blood vessels to leak fluid into the macula, leading to swelling and distortion of the central vision. Symptoms include blurred or distorted vision, difficulty reading or recognizing faces, and dark or empty spots in the central vision. If left untreated, it can cause permanent damage to the retina and lead to severe vision loss or blindness.
The condition is chronic and progressive, so early detection and prompt treatment are essential to prevent severe vision loss. Fortunately, effective treatments are available, including medications that can be injected into the eye to reduce swelling and improve vision.
The first-line treatment is anti-vascular endothelial growth factor (VEGF) therapy, which involves injections into the eye to prevent the growth of abnormal blood vessels that can contribute to edema.
BetterEyesight 164
However, laser photocoagulation therapy can also be used as an alternative or in conjunction with anti-VEGF therapy.
Laser photocoagulation therapy involves using a laser to create thermal burns on the retina, which seal leaking blood vessels and reduce edema. The treatment has been used for DME for over 30 years and effectively reduces vision loss. Focal laser photocoagulation is the most commonly used technique, which targets microaneurysms or tiny fluid-filled sacs on the retina. The treatment is usually performed in an outpatient setting and can be completed in a single session.
Despite the effectiveness of laser photocoagulation therapy, its use has declined with the advent of anti-VEGF therapy. However, recent research by Nagoya City University has shown that laser therapy remains a practical therapeutic approach to chronic refractory edema (Nozaki et al., 2023). The key to successful laser therapy is identifying microaneurysms using multimodal, highly accurate, and minimally invasive coagulation techniques.
The image that is displayed below provides a comprehensive summary of the different types and settings of laser therapies that are currently available. In particular, the figure highlights two different types of laser therapy: focal and subthreshold.
WilliamA.Haseltine,PhD 165
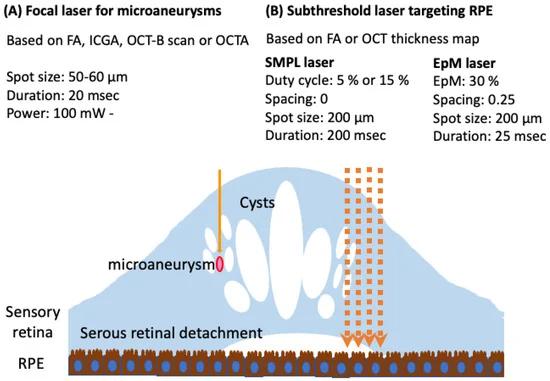
FIGURE 49: A concise overview of current laser therapies. Focal laser targeting microaneurysms recommends a short duration of application with the assistance of fluorescein angiography, indocyanine green angiography, optical coherence tomography B-scan, or OCT angiography. Alternatively, subthreshold laser targets the retinal pigment epithelium with the help of FA or OCT thickness map.
SOURCE: © 2023 by Nozaki, M., Ando, R., Kimura, T., Kato, F., & Yasukawa, T.
Focal laser therapy is used to target microaneurysms in the eye. It is recommended that the duration of laser application should be kept short. The planning aspect of this therapy will involve the use of several imaging techniques such as fluorescein angiography (FA), indocyanine green angiography (ICGA), optical coherence tomography (OCT) B-scan, or OCT angiography (OCTA) to ensure accuracy.
BetterEyesight 166
Subthreshold laser therapy targets the retinal pigment epithelium (RPE). During the planning stage of this therapy, the image of the FA or OCT thickness map would be used to ensure the correct positioning of the laser.
Furthermore, subthreshold laser therapy is a relatively new technique that uses lower energy levels than conventional laser therapy. This technique treats various retinal diseases, including diabetic macular edema and retinal vein occlusion. Subthreshold laser therapy has several advantages over traditional laser therapy.
Firstly, it reduces the frequency of anti-VEGF injections, often required in conjunction with laser therapy. This reduces the treatment burden on patients and improves their quality of life. Secondly, subthreshold laser therapy has the potential to provide longer-lasting treatment, which reduces the need for frequent follow-up appointments (Sabal et al., 2023).
Multimodal imaging-guided laser therapy is another promising technique that combines various imaging modalities, such as optical coherence tomography (OCT), fundus photography, and fluorescein angiography. This technique allows for better visualization of microaneurysms, small bulges in the retina's blood vessels that can cause vision loss.
Visualizing these microaneurysms makes it easier to target them with laser therapy. This technique can optimize anti-VEGF therapy and reduce treatment burden. Additionally, multimodal imagingguided laser therapy can treat other retinal diseases, such as agerelated macular degeneration and retinal vein occlusion (Kim et al., 2023).
WilliamA.Haseltine,PhD 167
While anti-VEGF therapy remains the first-line treatment, laser therapy can be used as an alternative or in combination with antiVEGF therapy. Using precise, minimally invasive coagulation techniques, such as multimodal imaging-guided and subthreshold laser therapy, can improve treatment outcomes and reduce treatment burden.
Further studies are needed to determine the optimal timing and settings for laser photocoagulation therapy and the potential of new laser technologies in managing DME. Nevertheless, laser photocoagulation therapy remains a valuable treatment option for DME, and its use should be considered in the management of this chronic and progressive condition.
BetterEyesight 168
CHAPTER 8
Refractive Errors

The eye is a complex organ that gives us a window into the world. Yet, over 2 billion people around the globe have impairments that dramatically affect their ability to see near or far (World Health Organization, 2023). One billion of those people have issues with vision that could have been prevented or not addressed (World Health Organization, 2023).
The personal impacts of vision impairments are significant. Whether young or old, struggling with sight can impact the quality of life. In children, unaddressed refractive disorders can lead to delayed motor development. Adults can also face higher rates of unemployment and depression in relation to their challenges of seeing clearly. Older adults experience significant personal impacts from vision impairment and loss, such as social isolation and a higher risk of falls and injury.
Over 84 million people struggle with refractive errors specifically (World Health Organization, 2023). These errors arise when the shape of your eye hampers the proper focus of light on the retina, a light-sensitive tissue layer at the back of your eye. Four main types of refractive errors affect vision: myopia, hyperopia, astigmatism, and presbyopia. The prevalence of myopia alone is expected to double by 2050 and impact 5 billion people worldwide (Wisse et al., 2019).
169

SOURCE: ACCESS Health International
Myopia, or nearsightedness, makes it difficult to see distant objects. It occurs when the eye is too long, causing light entering your eye to focus in front of your retina instead of directly on it. This results in a blurry image being transmitted to your brain. Myopia is usually corrected by wearing glasses or contact lenses with concave (curved inward) lenses to bend the light.The prevalence of myopia is rapidly increasing globally, and by 2050, almost half the world's population is projected to suffer from this condition, and it is becoming increasingly prevalent among children (Kaiti, 2022). Childhood myopia can significantly increase the risk of developing severe visual
BetterEyesight 170
FIGURE 50: An infographic illustrating how an image is perceived in the retina in different visual defects like hyperopia, myopia, and astigmatism.
impairments later in life, such as myopic macular degeneration and retinal detachment.
Conversely, hyperopia, or farsightedness, makes it hard to see closeup objects. This type of sightedness is caused by an eye that is too short and causes light entering the eye to focus behind the retina instead of directly on it again, resulting in a blurry image. Hyperopia can be corrected with glasses or contacts with convex (curved outward) lenses.
People with astigmatism may experience blurry or distorted vision for objects far away and nearby due to the cornea or lens having an abnormal shape. Astigmatism can be present at birth or develop during childhood or young adulthood and is often accompanied by nearsightedness or farsightedness. Astigmatism is usually corrected with glasses. Contact lenses can also correct this condition, though they are more expensive and take longer to receive than lenses designed for myopia or hyperopia.
Presbyopia is a standard refractive error among middle-aged and older adults that affects near vision. According to the World Health Organization, approximately 826 million presbyopia cases exist worldwide, making it one of the leading causes of vision issues (World Health Organization, 2023). It occurs when the lens in the eye loses flexibility with age, making it difficult to focus on close objects. Those with presbyopia often use bifocal or multifocal lenses to help with distance and near vision.
Currently, the most common method for diagnosing refractive errors is through a subjective manifest refraction test, which an eye care provider typically administers.
WilliamA.Haseltine,PhD 171
However, in recent years, there has been a rise in the popularity of self-eye exams for refraction. A self-eye exam entails using digital technology to perform a visual acuity test from home. This approach can benefit those who cannot visit an eye care provider due to scheduling conflicts or geographical limitations. Still, these exams do not offer screening or diagnosis of eye health or other diseases and do not replace an eye health exam with a licensed provider.
One self-eye exam option is the Visibly Digital Acuity Product (Visibly’s Approach to the Future of Eyecare - a Call to Action , 2022), which the FDA recently approved (FDA Office of Media Affairs, 2022). This web-based, self-guided software application is designed for adults aged 22 to 40 who can perform a self-test at home to evaluate visual acuity with or without correction. The application is intended to provide supportive recommendations alongside the patient's medical history, corrective eyewear prescriptions, and subjective vision data.
While the Visibly Digital Vision Test web application is a powerful tool for assessing visual health, it can never replace the need for a thorough eye exam by a licensed eye care professional. It is designed to be used with professional care as a supplementary tool, providing valuable insights into your overall eye health. This comprehensive test suite includes evaluations for visual acuity, color vision, contrast, brightness perception, and stereopsis for depth perception. Clinical trials have supported web-based eye testing as a valid and safe method for measuring visual acuity and refractive error, particularly for mild myopia. A recent study by the University Medical Center Utrecht in the Netherlands found that web-based eye testing can be a reliable substitute for the subjective manifest refraction test (Wisse et al., 2019). The study evaluated a web-based
BetterEyesight 172
tool for measuring visual acuity and refractive error in clinical trials.
The study found that the web-based test was just as practical as the traditional subjective manifest refraction method, with a strong correlation to the reference test and little difference in uncorrected visual acuity between the two methods.
The web-based tool's prescription effectively improved visual acuity, especially for people with mild myopia. This indicates that the webbased refraction assessment method validated by the trial is convenient and user-friendly for achieving accurate visual acuity correction in screening applications.
Another clinical trial, conducted at the University of California, San Francisco, also aimed to compare the accuracy of a home vision screening test with the standard Snellen visual acuity test conducted by an in-office technician to screen and prioritize patients remotely (Chen et al., 2021). The study involved patients who had scheduled ophthalmology appointments at the clinic. The home vision test used a modified eye chart in a PDF format that could be either printed or viewed on a monitor.
The results indicated that there was a minimal difference on average between the two methods. The study found a high level of agreement between the results obtained from the home vision test and those obtained through in-office measurement. While self-eye exams can be a convenient and helpful tool, they should be considered supplementary and never replace a thorough eye exam by a licensed eye care professional.
The standard treatment for refractive vision errors is glasses and contacts. Today, many of us wear glasses, whether for fashion or
WilliamA.Haseltine,PhD 173
necessity. Americans spend over $15 billion annually on eyewear in the US (American Academy of Ophthalmology, n.d.).
The origins of glasses and refractive lenses date back to ancient civilizations such as the Egyptians and Romans, who used polished stone or crystal lenses to magnify objects. While these early lenses lacked the corrective power of modern lenses, they paved the way for clear vision for many people.
Eye doctors prescribe precise lens dimensions for glasses to improve vision clarity. Glasses come in various styles and can be customized with plastic, metal, or titanium. Different lens styles include singlevision plastic to multifocal HD options. However, glasses can be expensive and prone to smudging, fogging, scratching, and breaking. Hence, eyeglasses are not the only option for individuals with vision impairments.
Contact lenses are a popular alternative to glasses and have come a long way since their invention in the late 1800s. While early contact lenses were made of glass, modern lenses are much smaller and more comfortable. They sit directly on the surface of your eye and correct how light enters the retina. They also offer better peripheral vision than glasses. Contact lenses can be used for nearsightedness, farsightedness, astigmatism, and presbyopia. However, the lenses for astigmatism and presbyopia come with a more significant price tag and must be oriented correctly in the eye.
There are also more permanent solutions to refractive problems, like surgery. Refractive surgery offers an effective solution to reduce or even eliminate the glasses or contact lenses requirement. Different refractive surgeries, such as LASIK (laser-assisted in situ
BetterEyesight 174
keratomileusis), are available, which reshape the cornea to correct the refractive error.
LASIK, or laser-assisted in situ keratomileusis, is a refractive surgery to fix vision problems (NYU Langone Hospitals, n.d.). It is the most widely performed surgery for refractive errors. Around 25 million people have undergone LASIK surgery since it became a steadfast treatment in 1989 (Bayba & Huang, 2023).
The surgery is usually done as an outpatient procedure and takes about 10-15 minutes per eye. During the process, numbing eye drops ensure patient comfort. Most people experience improved vision immediately or within a day or two after surgery, which is generally painless.
LASIK surgery starts by creating a corneal flap wherein the surgeon delicately forms a thin, hinged layer on the cornea's surface using a laser (National Eye Institute, 2019). This meticulously crafted flap unveils the underlying corneal tissue. From here, the surgeon can precisely remove exact amounts of corneal tissue using computerguided laser eye mapping to correct refractive errors.
WilliamA.Haseltine,PhD 175

SOURCE: ACCESS Health International
Once the cornea has been reshaped, the surgeon delicately repositions the flap back over the eye without stitches. This flap will act as a protective bandage, helping to speed up the healing process and ensure optimal recovery. This natural corneal healing highlights one of the more significant concepts of regenerative medicine - the body healing itself.
Success rates for these surgeries are substantial at 96%. Yet, there is still a decline in patients opting for these elective procedures. An important factor in deciding whether to undergo LASIK surgery is fear. Unsurprisingly, many of us fear anything coming in contact with our eyes and the idea of a laser being used on our eyes. At the same time, we are awake, and watching is too much to bear for some.
BetterEyesight 176
FIGURE 51: Diagram of LASIK surgery
Another significant factor is cost. LASIK prices vary, but generally, it costs roughly $4,400 for both eyes to be treated in the United States (Vision Center & Huang, 2023). While the cost of LASIK has decreased in recent years, other economic factors have also changed. These financial challenges put the surgery out of reach for a large portion of the population.
Another advance to watch is customized corneal ablation surgery or advanced surface ablation (Mehta & Mehta, 2020). This type of refractive surgery uses advanced imaging technology to create a personalized treatment plan for each patient. A laser reshapes the cornea by mapping its unique shape and curvature, similar to LASIK. This corneal ablation surgery provides an option for longterm relief for those not candidates for LASIK.
There are other options for refractive errors in children, as surgery is not commonly viable. Recent research on low-dose atropine as a potential treatment option for myopia in children has shown promising results, generating considerable interest. Atropine, a medication derived from plants like belladonna, has been widely used for over a century with various medical applications. Once absorbed in the gut, it is distributed throughout the body, metabolized in the liver, and excreted in urine.
Atropine works by blocking specific receptors in the body that respond to acetylcholine (McLendon & Preuss, 2023). It is a competitive antagonist that competes with acetylcholine to bind to the receptors. This medication acts at the nerve endings without blocking the transmission of impulses along the nerve fibers. It has multiple effects on the body, including inhibition of secretions, reduction of muscle tone, relaxation of smooth muscles, increased heart rate, and elevated respiratory rate.
WilliamA.Haseltine,PhD 177
SOURCE: Ben Mills on Wikimedia Commons
When applied to the eyes, atropine reduces the contraction of the ciliary muscle and causes the pupil to dilate. This action reduces the eye's ability to focus on nearby objects, making it primarily useful for diagnosing or treating eye conditions. For diagnostic purposes, atropine is helpful in cases where the doctor needs to examine the retina or the optic nerve. It can effectively dilate the pupil, allowing for a better view of the inside of the eye (Mayo Foundation for Medical Education and Research (MFMER), 2023).
In addition to its diagnostic uses, atropine can be used therapeutically to treat conditions like uveitis, where eye inflammation can cause pain and discomfort (Duplechain et al., 2020). Atropine can also treat amblyopia, commonly known as lazy eye, by blurring the vision in the good eye, which ultimately helps to improve vision.
But can atropine be used to treat myopia or induce myopia in children and teenagers?
BetterEyesight 178
FIGURE 52: Skeletal formulae and ball-and-stick models of the D and L isomers of the atropine molecule
There have been clinical trials conducted on the use of low-dose atropine as a potential treatment for myopia. The most commonly studied concentration of atropine is 0.01%. It is important to note that the effectiveness of low-dose atropine in myopia treatment has produced diverse outcomes in the studies conducted.
A study recently published in JAMA Ophthalmology investigated the effectiveness of 0.01% atropine in slowing down myopia progression or axial elongation (Repka et al., 2023). The results of the survey revealed that low-dose atropine did not significantly slow the progression of myopia or axial elongation when compared to the placebo group.
However, another study published in JAMA Opthalmology found that low-dose atropine (0.01%) significantly reduced myopia progression and axial elongation after three years (Zadnik et al., 2023). A similar result was seen in a review of clinical trials conducted in 2022 (Kaiti, 2022).
It is suggested that the effectiveness of atropine in slowing down the progression of myopia can vary in different populations. So, while low doses of atropine may not significantly help some groups, they could be beneficial in reducing myopia progression in others. Still, it is essential to remember that atropine simply slows myopia progression (Parry et al., 2016). It does not entirely stop it or reverse it.
Additional studies are necessary to establish the efficacy of atropine as a remedy for myopia in diverse populations. Until this research is completed thoroughly, atropine will not be granted FDA approval for treating myopia. Therefore, it must be employed off-label for now (Parry et al., 2016).
WilliamA.Haseltine,PhD 179
Research on the effectiveness of atropine in slowing myopia progression has generated mixed results. While some studies have suggested that low-dose atropine may provide a viable treatment option for myopia, others, particularly in the US population, have not found a significant benefit. However, some experts, like Michael F. Chiang, MD, director of the National Eye Institute, suggest continuing research to determine the most effective concentration of atropine for specific populations (National Eye Institute, 2023).
Binocular Vision Disorders
Binocular vision disorders can affect how the eyes team up, resulting in various vision issues such as Strabismus, Amblyopia, and Convergence Insufficiency. Proper coordination between the two essential functions of binocular visual function, accommodation and convergence, is crucial to see objects clearly and in three dimensions. Treatment options for accommodative and vergence dysfunction include lenses, prisms, and vision therapy. However, recent studies suggest virtual reality is an effective treatment option for those with binocular vision disorders.
Vision disorders can affect how the eyes work together. Strabismus causes misalignment, making the eyes not look in the same direction. Amblyopia results in weak vision in one eye. Convergence Insufficiency hampers the ability to focus on nearby objects, affecting reading and close work. Recent studies suggest that up to 17.6% of the general population may have convergence insufficiency. In comparison, up to 20.2% could be affected by accommodative dysfunction (Li et al., 2022).
BetterEyesight 180
Binocular visual function is the ability of both eyes to work together in harmony, providing a single, clear image of the surrounding environment. This process involves two essential functions: accommodation and convergence. Accommodation is how the eyes adjust the focus to see objects at varying distances. It consists of a change in the shape of the eye's lens, which focuses light onto the retina. The convergence process involves turning both eyes inward to focus on an object nearby. This ensures that both eyes focus on the same thing, which helps to create a single, clear image.
Accommodation and convergence are crucial components of binocular vision, as they allow us to see objects clearly and in three dimensions. Proper coordination between these two functions is essential, as any lack of coordination can result in blurred vision and difficulty seeing. Both processes require a complex interplay between the visual, neural, and brain systems, and any abnormalities in these systems can disrupt binocular vision, leading to various vision issues such as Strabismus, Amblyopia, and Convergence Insufficiency. Understanding the complexities of binocular visual function is essential to diagnose and treat vision disorders effectively.
Several options are available when treating accommodative and vergence dysfunction, including lenses, prisms, and vision therapy. The best treatment approach may involve a combination of these options tailored to the individual's needs and condition.
Corrective lenses, such as soft or hard contact or prescription eyeglasses, are commonly suggested to address accommodative and vergence dysfunction. These lenses magnify visual clarity and improve focusing ability. In addition, prism lenses rectify alignment issues and alleviate eye fatigue.
WilliamA.Haseltine,PhD 181
Prism lenses fix double vision by bending light rays to present a unified image. They can be combined with glasses to help postsurgery and following head trauma. Different prism lenses can correct vertical/horizontal misalignment and image distortion.
Individuals with trouble with eye coordination and focusing ability due to accommodative and vergence dysfunction can benefit greatly from vision therapy. This treatment option involves targeted exercises and activities designed to enhance binocular vision, which improves visual alignment and coordination. Vision therapy takes place in a clinical setting with the guidance of a trained therapist, or individuals can choose a personalized program for home-based therapy sessions. This office-based vergence/accommodative therapy (OBVAT) is a type of vision therapy that has proven very effective in improving binocular function, especially for patients with convergence insufficiency.
A recent study by Sichuan University in China found that virtual reality is a viable treatment option for those with binocular vision disorders (Li et al., 2022). This pilot randomized controlled trial sought to compare the efficacy of virtual reality-based vision therapy to office-based vergence and accommodative therapy (OBVAT) in young adults dealing with convergence insufficiency or accommodative dysfunction. The randomly assigned participants participate in the virtual reality-based vision therapy group or the office-based vergence/accommodative therapy group.
182
BetterEyesight

SOURCE: BMC Ophthalmology by Springer Nature
The virtual reality-based vision therapy uses an innovative technique that presents slightly different images to each eye, resulting in improved visual dissociation. This approach exposed participants to separate images on a virtual reality screen, inducing horizontal vergence demands. These images depicted human and animal figures and objects like gourds. A deliberately blurred background and concurrent stimuli movement was implemented to enhance visibility, necessitating adjustments in vergence. Notably, participants received training to improve both convergent and divergent capabilities.
The vision therapy lasted 12 weeks, and each group had an hourlong session weekly. The assessments occurred at the study's onset
WilliamA.Haseltine,PhD 183
FIGURE 53: A simplified schematic representation of the VR imaging principles presented in Li, S., Tang, A., Yang, B. et al.
and after 6 and 12 weeks of treatment. They measured binocular visual functions like vergence and accommodation and used a subjective questionnaire-based approach. The study evaluated parameters like distance and near horizontal heterophoria, the ratio of accommodative convergence to accommodation (ACA), monocular accommodative amplitude, and monocular accommodative facility.
After the treatment, patients who received virtual reality-based vision therapy and OBVAT demonstrated significant improvement in convergence insufficiency and accommodative dysfunction. This finding suggests that virtual reality-based vision therapy and OBVAT are innovative and valuable supplementary treatment options for young adults suffering from these conditions. However, it is essential to note that the OBVAT group improved better in a monocular accommodative facility than the virtual reality-based vision therapy group. Nevertheless, this study confirms that virtual reality is a viable new treatment option for binocular vision disorders.
A separate study by Imam Khomeini International University found that a contrast-based virtual reality game can positively impact amblyopia treatment (Fateme Hosseinnia et al., 2020). It explores experimental approaches to improve adult visual function, including a clinical trial video game. The therapy involves evaluating optical parameters and using a 3D video game set with a virtual reality set and an Android device.
It concludes that the proposed 3D video game exhibits potential as an effective treatment for amblyopia in adults. These findings underscore the capacity of innovative technologies in the medical realm, paving the way for enhanced treatment options and, ultimately, more favorable patient outcomes.
BetterEyesight 184
Unlike traditional therapy, virtual reality-based vision therapy offers a more engaging and immersive experience that can enhance patient compliance and motivation during therapy sessions. These studies have shown that virtual reality-based vision therapy effectively improves convergence insufficiency and accommodative dysfunction, suggesting its potential as an alternative to traditional treatment.
It is also important to note that optimizing, diversifying, and personalizing virtual reality-based vision therapy can further enhance its effectiveness and reduce patient response time. Future research should explore different training strategies and protocols within virtual reality-based vision therapy to maximize its benefits and tailor the treatment to individual patient needs.
Amblyopia
Amblyopia, also known as lazy eye, is a common condition affecting up to 3 out of every 100 children (National Eye Institute, 2019b). The condition arises due to abnormal visual development in one eye, leading to reduced vision. Early detection and treatment are essential in preventing long-term vision problems. This article will provide an overview of amblyopia and discuss the current and emerging treatment options.
Amblyopia is a condition where one eye has reduced visual acuity compared to the other. The condition usually occurs during early childhood and can be caused by various factors, including refractive errors, strabismus, and other structural abnormalities in the eye. In most cases, amblyopia develops because the brain and the affected
WilliamA.Haseltine,PhD 185
eye do not work together correctly, leading to the use of the stronger eye and neglect of the weaker eye, which deteriorates over time. Research has shown that amblyopia develops due to a lack of visual experience during early childhood (University of California San Francisco, 2021). The brain becomes more responsive to the visual input from the stronger eye, leading to a preference for that eye and, subsequently, the weakening of the other eye. If left untreated, this neural plasticity results in permanent visual acuity loss in the affected eye.
The treatment for amblyopia aims to stimulate and improve the visual development of the weaker eye. Current treatments include patching, atropine eye drops, and optical penalization.
Patching is a commonly used method to treat amblyopia, and it involves covering the stronger eye with an eye patch. This treatment promotes the use of the weaker eye and helps it develop properly. The patch is usually worn for several hours a day, and the duration of the treatment depends on the severity of the condition.
A study published in the American Family Physician Journal suggested clinical trials indicate that in children with moderate amblyopia, patching for two hours daily is as effective as patching for six hours (Bradfield, 2013). Daily atropine is also as effective as daily patching in this group.
Atropine eye drops are applied to the stronger eye and work by blurring its vision. This encourages the use of the weaker eye, which is then forced to work harder, leading to better vision in the affected eye. Atropine eye drops are usually used when patching is impossible or when the patient has difficulty wearing the patch.
BetterEyesight 186
Optical penalization is another treatment that can be used to treat amblyopia. This method uses a lens that blurs the vision in the stronger eye while keeping the weaker eye clear. This treatment also forces the weaker eye to work harder, leading to better vision. Optical penalization is usually preferred over atropine eye drops (Li et al., 2019).
Although these methods have effectively treated amblyopia, they can be challenging due to the child's discomfort, low compliance, and disruptive effect on daily activities (Boyd, 2020). These treatments have been found to have limited effectiveness in children older than ten years. A study published in the American Academy of Family Physicians journal also suggested that children younger than seven years benefit most from treatment (McConaghy & McGuirk, 2019). Therefore, exploring new treatment options that can improve compliance, accelerate visual recovery, and provide long-term benefits is essential.
Recent advances in neuroscience have led to innovative approaches to treat amblyopia. These treatments include virtual reality therapy and binocular treatments.
Binocular treatment uses metaplasticity to promote full recovery. This method involves using a local anesthetic, tetrodotoxin, to silence activity in both retinas. It can be delivered through intraocular injections. Research has shown that this approach is practical for both juvenile and adult animals, providing a treatment strategy that does not depend on compliance and promotes the recovery of binocular vision, regardless of age (Bossi et al., 2017).
Virtual Reality (VR) therapy is an innovative treatment method for amblyopia that involves using specialized VR headsets to create an
WilliamA.Haseltine,PhD 187
immersive visual experience. This experience stimulates the weaker eye and enhances its function, making it a promising and effective treatment option.

SOURCE: Ophthalmology, the journal of the American Academy of Ophthalmology
Studies have shown that VR therapy has higher compliance rates and shorter treatment periods than traditional methods (Shao et al., 2023). It also improves vision in amblyopia children (Ainhoa Molina‐Martín et al., 2023). The immersive and engaging experience provided by VR therapy makes it more enjoyable for children, resulting in better treatment outcomes. Additionally, VR therapy can be customized to meet each child's needs, making it a practical and personalized option for treating amblyopia.
The field of Amblyopia management is rapidly evolving. Technological and neurological advances promise to improve the diagnosis, treatment, and outcomes of lazy eyes. As researchers delve
BetterEyesight 188
FIGURE 54: An example of the video modifications used in the treatment.
into the underlying mechanisms of the condition, they are discovering innovative ways to promote neural plasticity and improve visual recovery. With the availability of new treatments, the scientific community can work towards a better understanding of the condition and continue to develop viable treatment options for patients.
WilliamA.Haseltine,PhD 189
CHAPTER 9
Cataracts

Our eyes support the most significant of our senses: sight. Sight informs a large percentage of how we perceive the world around us. It is also one of the most poetic senses, yet some things can create a cloudy haze that obscures our environment.
One of the most prevalent causes of foggy and hazy vision is cataracts. In the US, cataracts affect over 24 million people (American Academy of Ophthalmology, n.d.). According to the World Health Organization, approximately 65.2 million people have cataracts globally (World Health Organization, 2019). However, the outlook of a cataract diagnosis is still manageable with current and future treatment options like surgery and novel gene therapies.
Cataracts are a disorder that clouds the eye and thoroughly obstructs vision. It does this by impacting the lens in the eye. The lens consists mainly of water and proteins. As we age, the protein in the lens may clump together and form cataracts.
190

SOURCE: ACCESS Health International
Vision issues often present themselves in various ways, with symptoms that can develop gradually over time or occur suddenly with visible changes. These symptoms can subtly affect eyesight, causing blurry vision and difficulty seeing clearly at night or even leading to double vision, which may occur in one eye.
Additionally, colors that used to be bright and vivid may appear faded and less vibrant, indicating a possible vision issue. However, with numerous treatment options available for cataracts, those experiencing vision problems can find relief and regain clear sight.
Various factors, such as prolonged exposure to ultraviolet sunlight, diabetes, smoking habits, physical injuries, accidents, and specific medications, influence the formation of cataracts. These elements can contribute to the gradual clouding of the eye's natural lens, leading to impaired vision and potential blindness if left untreated.
WilliamA.Haseltine,PhD 191
FIGURE 55: Diagram of Cataract Eye
Typically, cataracts arise due to the breakdown of the lens microarchitecture. The formation of cellular compartments can cause fluctuating optical density, which results in light scattering and a cloudy lens appearance. The lens consists of specialized elongated and tightly packed cells called lens fibers. These fibers are infused with crystallin proteins that maintain transparency and refractive properties.
In the case of cataracts, crystallin proteins may become damaged or misfolded, which can cause clumping. Such clumps can accumulate and disrupt the structure and function of the lens. Consequently, this leads to light scattering and a cloudy appearance.
It is important to note that changes in specific molecules within lens cells can serve as a biomarker for early detection of cataract development. There can be inherited cataracts occurring alone or in combination with other systemic disorders. Such cataracts exhibit phenotypic and genotypic heterogeneity.
Thus far, 115 genes linked to syndromic and non-syndromic variants and 38 disease-causing genes have been identified in isolated cataracts (Berry et al., 2020). This discovery highlights the complexity of the condition and the need for a thorough investigation of the genetic makeup to facilitate proper diagnosis and management. In addition, it is crucial to understand the underlying molecular mechanisms of cataracts to develop new therapeutic strategies.
Treatments
One of the most widely used and highly effective methods for treating cataracts is a surgical procedure called cataract extraction.
BetterEyesight 192
This technique involves the precise removal of the cloudy lens, which is then replaced with an intraocular lens implant. It has been adopted by medical professionals due to its remarkable safety and efficacy, as evidenced by the thousands of surgeries performed annually in the United States alone (Kauh et al., 2016).

SOURCE: ACCESS Health International
Cataract removal is the most commonly performed surgical intervention among all medical specializations. It has a projected annual incidence of 3.7 million cases in the United States, 7 million in Europe, and 20 million globally (Rossi et al., 2021).
It is a surgical procedure that involves removing and replacing the opaque lens with an intraocular lens or IOL. The Intraocular Lens (IOL) is a permanent implant made of high-quality plastic placed inside the eye. IOLs, such as standard mono-focal, premium multifocal, and toric lenses, are available. Each lens type fulfills specific visual requirements and tasks.
WilliamA.Haseltine,PhD 193
FIGURE 56: Cataract Surgery Diagram

SOURCE: ACCESS Health International
A standard monofocal lens typically replaces the natural lens removed during cataract surgery for those with mild or single-vision prescriptions. They focus on either up-close, medium-range, or distance vision. Most people have them set for clear-distance vision and wear glasses for reading or close work.
Those with presbyopia often use multifocal lenses, supporting both near and far vision. During an adjustment period, the brain learns to select necessary vision information for objects at different distances. Insurance coverage for multifocal IOLs may be limited, and these lenses tend to be pricier than mono-focal lenses.
The toric lenses are for use in patients with astigmatism. An astigmatism is when the cornea is curved unevenly, causing light to be scattered instead of focused. Toric lenses are more precise and customized for each patient's unique needs. They correct near, intermediate, or farsightedness.
BetterEyesight 194
FIGURE 57: Cataract Surgery Flow Diagram.
Like all medical procedures, complications can arise when receiving an intraocular lens implant. One such complication is the posterior capsule (behind the intraocular lens), which may become cloudy months or years after cataract surgery. If this happens, the surgeon will perform a simple laser to clear the capsule.
There are currently no permanent nonsurgical options for treating cataracts. Nevertheless, various nonsurgical alternatives may help alleviate cataract symptoms, slow their progression, and reduce their severity. Some of these options include consuming nutritional supplements such as carotenoids, vitamins E and C, and organic compounds.
Future options may include eye drops, as some eye drops work to dissolve cataracts. A group of professionals from the University of California, San Diego, strives to replicate the clinical trials' outcomes to present an alternative surgery (Zhao et al., 2015).
Researchers have developed a new medication that utilizes a naturally occurring steroid called lanosterol. This steroid has shown potential in preventing the clustering of flawed crystallin proteins that lead to cataracts in the non-congenital form of the disease. The next step for the scientists is to determine the precise mechanism behind how the lanosterol-based eye drops work and to conduct further research through human trials.
This discovery could revolutionize how cataract treatments are conducted, offering a promising alternative to surgery. Speaking of game-changing alternatives, gene therapies also hold promise as a future innovation for treating cataracts.
In essence, gene therapy is a cutting-edge approach that aims to address genetic mutations responsible for various illnesses in
WilliamA.Haseltine,PhD 195
patients. Gene therapy strives to replace or repair defective genes. It does this by introducing fresh genes into the body. This transformative process involves using specially engineered viruses as vectors to deliver healthy genes into the patient's cells, targeting the root cause of genetic diseases.
Studies have revealed that specific genes play a crucial role in the formation of cataracts in both humans and rodents (Shi et al., 2022). These genes include GJA1, GJA3, and GJA8, which encode proteins known as connexins. In particular, Cx43, Cx46, and Cx50 are the connexins produced by these genes. Among these, Cx46 and Cx50 are predominantly present in the cells of the lens fibers, whereas Cx43 is common in the cells of the lens epithelium.
Any disruption in the expression of these genes can significantly contribute to the onset of severe cataracts in both humans and mice. Such findings highlight the importance of these genes in maintaining proper lens function and preserving visual acuity. Overall, these genes play a crucial role in maintaining the integrity of the lens, highlighting the importance of these genes in preventing cataracts.
There needs to be more information on gene therapies specifically for cataracts. Still, discovering these genes and the success of gene therapies for other eye disorders, such as age-related macular degeneration, provide hope for those facing vision impairment due to cataracts.
Cataract surgery is a procedure that aims to improve visual acuity and quality of life. Intraocular lenses provide patients with various options depending on their visual needs, such as mono-focal,
BetterEyesight 196
multifocal, or toric lenses. However, complications such as posterior capsule opacification may arise, requiring additional treatment.
While there are currently no permanent nonsurgical options for treating cataracts, promising research indicates that eye drops containing lanosterol and gene therapy could potentially revolutionize cataract treatment, providing a much-needed alternative to surgery. With continued research advancements, we hope to see significant improvements in preventing, diagnosing, and treating cataracts, ultimately preserving and restoring visual function for millions worldwide.
By now, you know that cataracts are a critical issue as they are the leading cause of blindness globally (Adelson et al., 2021). This fact is interesting since cataract surgery is one of the most cost-effective medical interventions available (Adelson et al., 2021). Since cataract surgery has been proven safe and effective in restoring vision, Whydocataracts continue to bea globalvision crisis?
Disparities in Care
To answer this question, it's essential first to clarify what disparities exist around cataract care. First, cataract disease is disproportionately prevalent in countries with lower socioeconomic status, leading to a significant inequality gap (Fang et al., 2022). Second, developing nations face lower cataract surgical rates than their developed counterparts, meaning fewer surgeries occur in the countries that need them most (Wang et al., 2016). These alarming statistics highlight the issues of limited healthcare accessibility and inadequate community outreach efforts.
The cost of cataract care varies significantly, leading to disparities in treatment access. In the United States, bilateral cataract surgery
WilliamA.Haseltine,PhD 197
costs between $2,410 and $5,243 (Rebenitsch et al., 2014). However, the same surgery can cost $7,300 in Spain, $4,300 in Turkey (Rebenitsch et al., 2014), and around $1,500 in China (Xu et al., 2016). In Colombia, the surgery costs around $2,000 (OPHTHALMON SA, 2022). In India, the average cost ranges from $41 to $125 (Ophthalmology Times, 2014). Additionally, India's Aravind Eye Care Systems offers no-cost options to patients through their pay-what-you-can and "no questions asked policy."
The Aravind model relies on three primary factors to be effective. Firstly, the hospital sees many patients, which allows them to benefit from economies of scale. Secondly, they have reduced material costs by creating manufacturing channels for operation materials such as lenses and sutures. Thirdly, Aravind prioritizes the patients and community and organizes outreach events and vision camps while subsidizing patients' travel costs to the surgery centers.
Aravind Eye Care System
Dr. Govindappa Venkataswamy, a skilled ophthalmologist, was conscious of the widespread issue of blindness in his country early on and performed over 100,000 eye surgeries throughout his career to address it. His passion for helping the underprivileged led him to create Aravind Eye Care. This sustainable and replicable solution has benefited many.
Founded in 1976 with 11 beds, Aravind Eye Hospital has blossomed into a visionary institution. The overall mission of Aravind is to eliminate needless blindness while providing high-quality, highvolume, compassionate care to all.
Shortly after the development of Aravind, Dr. Venkataswamy began to wonder how Aravind could be scaled up. He is quoted asking, "If
BetterEyesight 198
Coca-Cola can sell billions of sodas and McDonald's can sell billions of burgers, why can't Aravind sell millions of sight-restoring operations, and, eventually, the belief in human perfection? With sight, people could be freed from hunger, fear, and poverty. You could perfect the body, then perfect the mind and the soul, and raise people's level of thinking and acting." (Center for Global Development, n.d.).
Since then, Aravind has grown and scaled up tremendously. It now encompasses five hospitals nationwide in India. The organization has also seen a six-fold increase in annual cataract surgeries, skyrocketing from 29,928 in 1988 to 180,991 in 2007 (Natchiar et al., 2008). In 2023, the clinic held over 5.7 million outpatient visits and over 700,000 surgeries (Aravind Eye Care Systems, 2023).
Aravind Eye Hospitals prioritizes equity by providing free or heavily subsidized treatment to 50% of patients while maintaining financial self-sustainability (Aravind Eye Care Systems, n.d.). Due to their high patient volume, the hospitals benefit from economies of scale. They also follow a standardized protocol for eye screening camps. This protocol ensures a comprehensive examination, including refraction, intraocular pressure measurement, and fundus examination.
Furthermore, Aravind has placed significant emphasis on cataract care. It has been at the forefront of innovative surgical techniques that have greatly expanded access to life-changing procedures for numerous individuals.
Aravind recognized the importance of intraocular lens prices to surgery costs. Hence, they found a way to manufacture them in India and established a new manufacturer called Aurolab. The first
WilliamA.Haseltine,PhD 199
product created by Aurolab was polymethyl methacrylate (PMMA) IOL. This lens changed the affordability of IOLs, dropping prices from hundreds of dollars to below $10 per lens (Sriram, 2022).
Today, with a remarkable price tag of just $3, this lens has significantly changed the affordability of cataract surgery in India (Sriram, 2022). This allows the total surgery expenses to fall to as low as $10 per cataract operation for the hospital (Center for Global Development, n.d.). This is part of why Aravind can offer their services at no cost to those in need and at a standardized cost for those who can afford it or want upgraded lenses (Abhilasha & Harvard University, 2013).
To put this in perspective, in the United States bilateral cataract surgery can cost anywhere between $2,410 to $5,243 (Rebenitsch et al., 2014), whereas in India, the same procedure now costs $41 to $125 (Ophthalmology Times, 2014). It’s also important to note that at Aravind, a financially well-off patient covers the treatment costs for multiple disadvantaged patients with a single payment (Sriram, 2022).
Furthermore, labor costs are minimal, with surgeons charging only $2.25 per patient and other staff charging $4.81 per patient (Ophthalmology Times, 2014). In contrast, in the US, Medicare pays $1,766 for the surgery center and $760 per surgeon (Ophthalmology Times, 2014). Also, the average surgery time in the US is 21 minutes, while at Aravind, it only takes 6 minutes (Ophthalmology Times, 2014).
Over time, the manufacturing operations at Aurolab rapidly expanded from 35,000 lenses in 1992-1993 to an impressive count of nearly 600,000 (Center for Global Development, n.d.). Around
200
BetterEyesight
60% of Aurolab's intraocular lenses are supplied to nongovernmental organizations in India and other developing nations (Sriram, 2022).
Aravind’s Aurolab doesn’t stop at producing lenses. They also make sutures, needles, and solutions for surgery to keep costs as low as possible. Aurolab’s needles have been crafted to deter suture reuse and minimize expenses in ophthalmic surgery. Furthermore, they offer a wide selection of absorbable and non-absorbable options, catering to a diverse range of surgical requirements.
Aurolab exports its products to over 130 countries, making surgery more affordable globally. Still, making intraocular lenses more affordable is only one significant factor that allows Aravind to perform so many cataract surgeries safely and efficiently.
Aravind recognizes that the quality of training for its cataract surgeons is crucial to providing the highest standard of surgical care (Aravind Eye Care Systems, n.d.). Therefore, they emphasize improving the quality of training for eye specialists worldwide. This emphasis ensures that Aravind's cataract surgeons are well-equipped to provide the best possible care to their patients while also setting a high benchmark for eye care professionals globally.
Aravind's success is also attributed to efficient service delivery systems and innovative operating practices, such as implementing an 'assembly line' system in operating rooms. Aravind doctors perform over 2,000 surgeries annually, surpassing the average of around 300 at other Indian hospitals (Business Model Toolbox, n.d.). An Aravind surgeon can skillfully conduct 50 cataract operations in a single day (Mehta & Shenoy, 2011).
WilliamA.Haseltine,PhD 201
Each operating room has two beds in the system, with one patient waiting while the other undergoes surgery. After each surgery, the surgeon quickly performs a series of sanitation steps before moving on to the next patient. Surgery can sometimes take as little as five minutes from start to finish (Solo Eyewear, 2012).
Their surgical efficiency also stems from their strategic approach of allowing surgeons to dedicate their full attention to surgeries. Recognizing the scarcity and high expenses associated with ophthalmologists, who often perform routine tasks like measuring intraocular pressure and assessing refractive errors, Aravind implemented a ground-breaking solution. They introduced a new group of mid-level ophthalmic personnel, which significantly boosted the productivity of each ophthalmologist by over four times (Ravilla & Ramasamy, 2014).
Further to that, they also implement regular assessments and meetings to determine surgeon fatigue and effectiveness (Mehta & Shenoy, 2011). They also implemented a salary setup that does not link a surgeon's salary to the number of patients seen, allowing surgeons to take the necessary time and precautions with each patient rather than worrying about their pay.
At this point, it is also critical to note that while scaling up their total number of procedures, Aravind did not suffer a drop in quality or patient outcomes. Aravind's rate of complications is half that of the United Kingdom's National Health Service (McKinsey's Health Systems, 2011).
Ensuring high-quality community eye care entails more than just achieving optimal visual outcomes. It encompasses various aspects, such as the efficiency of the caregiving process, patient treatment
202
BetterEyesight
adherence, and the reduction of multiple visits. An effective community eye care program should be accessible, affordable, and tailored to the community's needs while staying up-to-date with technological advancements, promoting positive health-seeking behaviors, and creating demand for healthcare among those in need.
The success of Aravind's cataract operation program has demonstrated that quality care can be provided on a large scale with appropriate technology and processes, leading to affordable costs. In the past, cataract surgery was categorized based on social classes. However, with the introduction of the assembly line system, locally made intraocular lenses, and other surgical consumables, along with the training of local surgeons and nurses, it is now possible to achieve similar results to those in developed countries.
Aravind’s success also inspired other groups across India, such as L V Prasad. Established in 1987, the L V Prasad Eye Institute (LVPEI) is a prominent world-class eye health facility in Hyderabad, India ( L V Prasad Eye Institute, 2022). As a World Health Organization Collaborating Centre for Prevention of Blindness, LVPEI provides comprehensive patient care, sight enhancement, and rural eye health programs. One of the critical components of LVPEI’s success is its unique pricing structure, which allows it to offer fee waivers and discounts to needy patients while maintaining high-quality care.
LV Prasad isn’t the only group that has replicated Aravind’s success. Aravind has mentored other groups throughout India, Asia, and Africa. The hospitals mentored by Aravind have witnessed a remarkable surge in productivity upon replication. Numerous facilities observed a substantial 40-50% increase in output in the
WilliamA.Haseltine,PhD 203
subsequent year. At the same time, some even doubled their output within a single year (Ravilla & Ramasamy, 2014).
The projected tripling of global blindness by 2050 (The International Agency for the Prevention of Blindness (IAPB), n.d.), with South Asia and sub-Saharan Africa being the most heavily impacted regions, underscores the significance of Aravind's work and business model. Others, such as LV Prasad, have also found the secret to cataract surgery success. The hospitals can offer free or lowcost, high-quality healthcare to 50-60% of their patients using the profits earned from the 40-50% of patients who pay for their services (Honavar, 2022).
It is only natural to see the success in India and wonder why it is so expensive to get this same surgery here in the United States and why the model isn't implemented in more countries.
Cataract Care in Other Parts of the World
US healthcare payers provide financial coverage for medical services by compensating providers, negotiating lower prices, and promoting preventative care. Cataract treatment and surgery can be expensive, with varying coverage. Medicare covers only 80% of senior citizens.
According to Medicare's national average, the price of a surgeon's time in the United States for both ambulatory and hospital settings is around $746 for a patient (Gillette, 2023). Facility fees can range from $1,000 to $2,100. In addition to these, patients have to pay for supplies and materials like lenses, as mentioned earlier. For those without insurance, the surgery costs around $4,000 (Brown et al., 2019).
BetterEyesight 204
Several factors contribute to the overall cost of cataract surgery in the US. These include the surgical facility, the chosen procedure, the type of intraocular lens (IOL) employed, the utilization of technologies such as laser assistance, the qualifications of the surgeon, the medications administered on the day of the procedure, the inclusion of additional eye correction services, and the possibility of post-surgical complications.
Suppose the surgery is complete within 20 minutes without any complications. In that case, the cost can range from $46 for a single surgeon with an available anesthesiologist to $120 for two surgeons and a dedicated anesthesiologist (Rossi et al., 2021). In the United States, this amounts to 1.2 million physician hours or 132 million dollars (assuming an average cost of $110 per hour), almost twice as much in Europe (Rossi et al., 2021).
Regardless of the reason behind the expenses related to cataract surgery, these higher prices lead to low rates of corrective surgery, meaning more people are living with untreated cataracts (Koo & Ansari, 2020). About 5 million cataract surgeries occurred in the US in 2022 (Basaldua, 2021), while India boasts over 8.34 million during 2022 (Jha, 2023). China, another major country with yet another approach to cataract care, lags behind the US and India in cataract surgical rates (Xiang et al., 2023).
Despite the Chinese government's notable efforts, China's cataract surgical rate is significantly lower than its poorer neighbors, such as India and Vietnam (Sun Yat-sen University & ClinicalTrials.gov, 2021). The main reason for this is the lack of trained surgeons. Despite having over 36,000 ophthalmologists in China, only onethird are qualified to perform cataract surgeries independently (Sun Yat-sen University & ClinicalTrials.gov, 2021). This shortage of
WilliamA.Haseltine,PhD 205
ophthalmologists in China creates a need to improve the country's ophthalmic service capacity to meet the demand for cataract surgeries (An et al., 2019).
The cost of surgery in China can vary from $536 to over $1000 (Fang et al., 2010). While this may seem like a reasonable price here in the United States, many are unwilling to pay this price in China.
A study assessed the impact of Helen Keller International's (HKI) low-cost surgery program and found that 80% of the participants expressed willingness to cover the surgical expenses (Fang et al., 2010).
However, only 56% of them were willing to pay $66 or more, which is the subsidized price offered by HKI (Fang et al., 2010). Visually impaired individuals were more inclined to pay for the surgery, with an average contribution of up to $32 (Fang et al., 2010). This information highlights the significant financial barrier posed by the high cost of cataract surgery in rural China, especially compared to the average surgery cost in the country.
A study published in the BMC Public Health Journal suggests that the increased costs of cataract surgery in China are similar to those observed in the United States and India, mainly due to the type of intraocular lens (IOL) used (Fang et al., 2010). The research also reveals that the variation in total patient costs in China is primarily attributed to the expense of different IOL types.
The multi-focal and adjustable intraocular lens costs over $1,100, making it too expensive to be reimbursed (Fang et al., 2010). Consequently, most patients opt for a single-focused intraocular lens. The study focused primarily on surgical variations in four hospitals across China. The providers did not use multi-focal or
BetterEyesight 206
adjustable intraocular lenses in the three hospitals that were studied (Fang et al., 2010).
All four providers used imported lenses (Fang et al., 2010). Although domestic lenses were available, these hospitals did not use them. This was because patients widely believed imported lenses offered better quality than domestic ones.
Still, cost and lack of trained professionals are two reasons China and Asia experience lower surgery uptake rates. Another component is culture. In some Asian developing countries, the head of the household often decides whether to undergo cataract surgery due to cultural norms (Koo & Ansari, 2020). Additionally, older adults are often reluctant to receive treatment due to fear and unfamiliarity with the procedure. This fear can lead to delayed diagnosis of cataracts, resulting in poorer outcomes upon surgery.
It is interesting to note that treating or not treating cataracts can have a significant economic impact. When discussing health issues and disparities, we often overlook a healthier population's impact on generating more resources through gainful employment. This impact is part of why William Nordhaus, the Nobel Prize-winning economist, has suggested that 50% of the wealth created in the United States in the 20th century came about due to advances in health and healthcare (Brown et al., 2019).
One analysis suggests that cataract surgery in the first eye can provide a monetary return on investment of $372,543 for the direct medical costs of surgery expended in 2018 (Brown et al., 2019). Another similar analysis suggests that eliminating cataract-related blindness and low vision in India will require an investment of approximately $2.6 billion but would result in a net gain of $13.5
WilliamA.Haseltine,PhD 207
billion (Le et al., 2016). Furthermore, the contribution to a country's GDP strongly suggests that cataract surgery makes the nation wealthier (Brown et al., 2019).

SOURCE: ACCESS Health International
Cataract treatment impacts more than just economies. It also has a significant public health impact. Every year, over 26 million people who were either blind or had low vision regain their sight through cataract surgery, dramatically improving their quality of life and independence (Chen, Xu, et al., 2021). Moreover, cataract surgery reduces the risk of falls in elderly patients, leading to fewer hospitalizations (Feng et al., 2018).
Therefore, it is crucial to address the inequalities and make cataract surgery more accessible and affordable to enhance the health and
BetterEyesight 208
FIGURE 58: Comparison of vision with and without cataracts
well-being of people worldwide, particularly as the global population ages.
Pediatric Cataracts
Pediatric cataracts are a rare but severe condition that can cause permanent vision loss in children. Though it mainly affects young ones, it can have a devastating impact on their developing visual system. Early detection and timely treatment are crucial, as good eyesight is essential in almost every aspect of life. There are two types of pediatric cataracts, making accurate diagnosis imperative for effective treatment.
Thankfully, several treatment options are available for pediatric cataracts, including some innovative therapies currently undergoing clinical trials. This article will provide everything you need about pediatric cataracts, including their different types and the latest treatment options.
Pediatric cataracts are a condition that causes cloudiness or opacity in the lens of a child's eye. This cloudiness can affect vision and may lead to blindness if left untreated. Unlike adult cataracts, which can usually be treated with surgery, pediatric cataracts require specialized care and treatment.
The effects of pediatric cataracts on a child's vision can vary depending on the severity of the condition. Some children may experience blurred vision or a decrease in visual acuity. In contrast, others may have difficulty focusing or may see double. Pediatric cataracts can sometimes cause the eyes to appear misaligned or cause uncontrolled eye movements.
WilliamA.Haseltine,PhD 209
There are two main types of pediatric cataracts: congenital and acquired (Struck, 2015). Congenital cataracts are present at birth and may be caused by genetic factors, maternal infections, or metabolic conditions. Acquired cataracts, on the other hand, develop after birth and can be caused by external factors such as trauma or certain diseases.
Treatment options for cataracts may include surgery, glasses, or contact lenses, depending on the severity and underlying cause of the condition. In the case of pediatric cataracts, the primary treatment is a surgical procedure called cataract extraction. This surgery is typically performed under general anesthesia. During the process, the cloudy lens is carefully removed from the eye. An intraocular lens (IOL) may sometimes be implanted in the eye to replace the affected lens.
Modern surgical techniques, such as micro-incision cataract extraction and primary intraocular lens (IOL) implantation, have shown effectiveness in clinical trials for children between two months to 16 years old (Demirkılınç Biler et al., 2018). The Toddler Aphakia and Pseudophakia Study (TAPS) revealed that IOL implantation was relatively safe for children above six months but younger than two years (Heidar, 2017). IOL placement in the bag was the most preferred site. However, if the support for the posterior capsule is insufficient, putting the IOL in the ciliary sulcus is also an option.
While surgical management is the primary focus of such trials, a few studies have looked into the long-term outcomes of pediatric cataract surgery and primary intraocular lens (IOL) implantation in children (Demirkılınç Biler et al., 2018). For instance, the Infant Aphakic Treatment Study (IATS) aimed to assess the effectiveness
BetterEyesight 210
of primary IOL implantation in infants below six months of age who underwent cataract-removal surgery, with varying results (Infant Aphakia Treatment Study Group et al., 2010).
The study found that while primary IOL implantation could potentially offer improved visual outcomes and a reduced incidence of strabismus, the infants who received it experienced more adverse events and additional intraocular surgeries than those who did not, some of which included glaucoma, corneal edema, and retinal detachment. The study's authors attribute such adverse events to the complexity of the surgery, making it challenging to avoid complications entirely.
There is limited non-surgical treatment available for pediatric cataracts. However, some treatments provide hope for improving visual outcomes in children. It is possible to manage some pediatric cataracts without surgical intervention. Small, partial, or paracentral cataracts can be monitored through observation. Pharmacologic pupillary dilation can also help improve pupil size and enable children to see better (NHS, 2018).
Furthermore, the cause of cataracts is highly variable, with bilateral congenital cataracts being the most common cause of treatable childhood blindness. Currently, 42 known genes may lead to cataract formation in humans or mice, with even more genes expected to be involved in cataract formation, as there are still families with cataracts from unknown gene mutations and cataractous mouse mutant lines that have yet to be characterized at the molecular level (Churchill & Graw, 2011).
The course and prognosis of pediatric cataracts are also challenging to predict, as the likelihood and rate of progression depend on
WilliamA.Haseltine,PhD 211
several factors, such as the presence of other ocular or systemic abnormalities. Nevertheless, ongoing research and clinical trials offer hope for better managing and treating pediatric cataracts.
BetterEyesight 212
CHAPTER 10
Glaucoma

Glaucoma is a leading cause of irreversible blindness and disability worldwide. It is a group of eye conditions that damage the optic nerve, which connects the eye to the brain, leading to vision loss. According to a systematic review and metaanalysis of the global causes of blindness and distance vision impairment by Brien Holden Vision Institute, glaucoma is the second leading cause globally (Bourne et al., 2017).
The global prevalence of glaucoma is expected to increase from 76 million people in 2020 to 111.8 million by 2040 (Tham et al., 2014). This increase in the prevalence of glaucoma will have a significant economic impact on healthcare systems and individual patients.
Glaucoma is a disease that damages the optic nerve, which is responsible for transmitting visual information from the eye to the brain. This condition is caused by a build-up of fluid pressure inside the eye, known as intraocular pressure (IOP). When the intraocular pressure is abnormally high, it can put excessive stress on the optic nerve and cause damage over time.
213
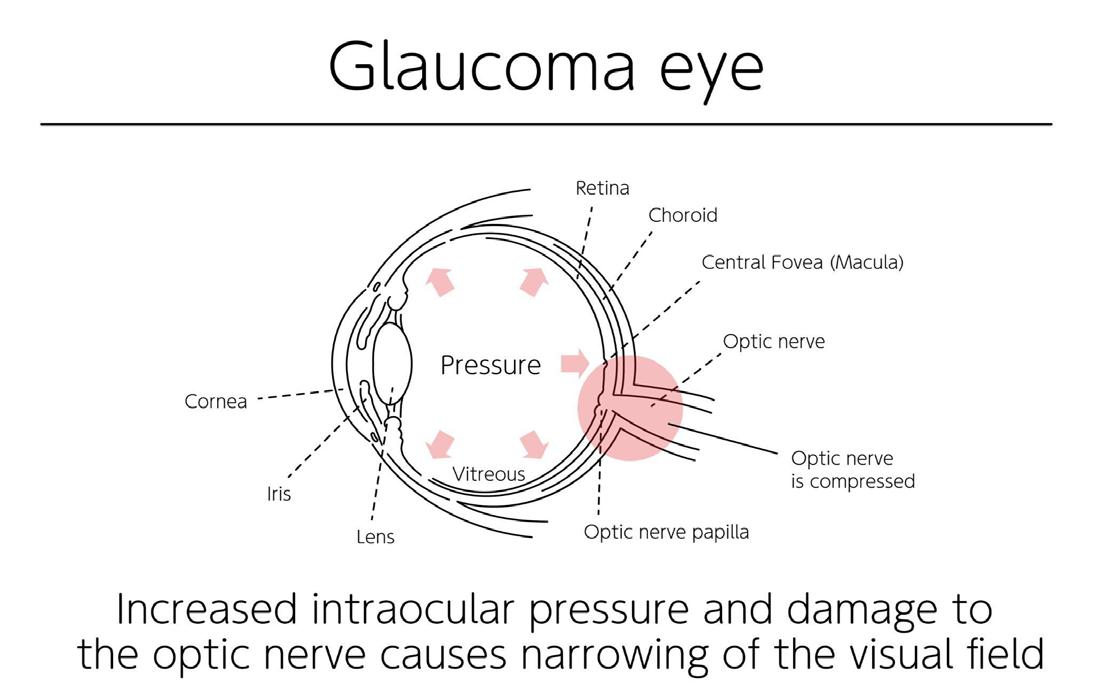
SOURCE: ACCESS Health International
There are two main types of glaucoma: open-angle glaucoma and angle-closure glaucoma. Primary open-angle glaucoma is the most common type, accounting for over 70% of all glaucoma cases (Allison et al., 2020). POAG prevalence varies globally, but it is suggested that 57.5 million individuals have the disease worldwide (Allison et al., 2020). The disease's prevalence increases with age, with individuals over 60 at the highest risk (Allison et al., 2020) Also, those with severe OAG are at an increased risk of falls or fractures due to impaired vision and decreased mobility (Shih et al., 2021).
BetterEyesight 214
FIGURE 59: Diagram of an eye with Glaucoma

SOURCE: Wikimedia Commons
The most common signs and symptoms of POAG are changes in peripheral vision, eye redness, eye pain, halos around lights, blurred vision, and tunnel vision (Mayo Clinic, 2022). However, these symptoms often occur late in the disease course, indicating the risk of severe vision loss.
The disease usually results from inadequate drainage of the aqueous humor through the trabecular meshwork, which leads to increased eye pressure (Mahabadi et al., 2020). Unfortunately, the impacts of POAG on daily life can be challenging, as vision loss can lead to difficulties in driving, reading, and performing daily tasks.
Furthermore, individuals diagnosed with severe disease and disease progression face the most significant burden regarding eye-related
WilliamA.Haseltine,PhD 215
FIGURE 60: Glaucoma vs Normal Vision
expenses (Shih et al., 2021). This includes costs associated with treatments, medications, and frequent doctor visits.
Although the exact biological mechanisms responsible for glaucoma are not fully understood, researchers believe that damage to the optic nerve is caused by a combination of factors, including oxidative stress, inflammation, and abnormal blood vessel growth. Early diagnosis and treatment of glaucoma are essential for preventing vision loss, as the condition often has no symptoms until it has progressed to an advanced stage.
Traditional methods for diagnosing glaucoma and detecting its progression using standard technology are challenging in clinical practice. However, using artificial intelligence (AI) and deep learning (DL) algorithms in healthcare can improve the diagnosis and screening of glaucoma.
In their recent article, a team from Nanjing Medical University in China explained and illustrated the process of using artificial intelligence and deep learning-based algorithms to diagnose eyerelated disorders and diseases (Zhang et al., 2023).
BetterEyesight 216

SOURCE: Copyright © 2023 Zhang, Tang, Xia and Cao.
Generally speaking, diagnosing glaucoma using AI involves carefully processing various data, like optic disc photos, visual fields, and intraocular pressure. The algorithm eliminates noise, artifacts, and irrelevant information to ensure accurate results while learning distinctive features and patterns associated with glaucoma through training. It is rigorously tested in the validation phase to confirm its effectiveness. If successful, it undergoes further evaluation in the testing phase to ensure reliable diagnoses.
When the algorithm is implemented in clinical practice, clinicians collect data such as optic disc photographs, visual fields, and intraocular pressure readings from patients and preprocess the data before applying the algorithm to diagnose glaucoma.
WilliamA.Haseltine,PhD 217
FIGURE 61: A flowchart depicting constructing and evaluating a deep learning model.
One of the essential roles of deep learning in glaucoma diagnosis is the ability to screen and differentiate normal eyes from those with early stages of glaucoma. Deep learning models trained with fundus photographs can identify characteristic fundus lesions in glaucoma, including retinal nerve fiber layer abnormalities (Zhang et al., 2023). This would allow diagnosing glaucoma earlier and potentially decrease the risk of visual impairment.
Furthermore, deep learning algorithms trained with optical coherence tomography (OCT) data can detect microstructural damage due to glaucoma and its progression over time. According to research conducted by Wake Forest School of Medicine in North Carolina, deep learning algorithms are proving to be more accurate than manual or automated segmentation methods in identifying early signs of glaucoma (Thompson et al., 2022).
Deep learning can also detect glaucoma from fundus image regions outside the optic nerve head (ONH), as seen in a study done by a team in Sydney, Australia (Akter et al., 2022). This is highly promising for the broader clinical applicability of deep learning in computer-aided glaucoma screening and follow-up. It can also provide a comprehensive assessment of the retina, allowing clinicians to detect early signs of glaucoma that may have gone unnoticed.
Duke Eye Center of Duke University reviewed the advantages of using sophisticated deep learning algorithms for glaucoma diagnosis (Thompson et al., 2020). They found that these algorithms can deliver diagnoses significantly faster than conventional methods, greatly enhancing efficiency and expediting treatment plans. Additionally, these algorithms' accuracy surpasses traditional methods, enabling early detection and intervention, which can
BetterEyesight 218
effectively halt disease progression. This improves patient outcomes and reduces healthcare costs associated with late-stage treatments.
Deep learning algorithms have tremendous potential for improving medical care access, especially for underserved populations living in remote areas without access to ophthalmologists. These algorithms allow patients in these areas to receive timely and accurate diagnoses, leading to better healthcare outcomes and reducing healthcare disparities (Campbell et al., 2021). These algorithms enable eye care services to be accessed equally, regardless of location.
Moreover, healthcare professionals can use deep learning algorithms to minimize diagnostic variability, leading to more reliable and precise assessments (Aggarwal et al., 2021). This, in turn, instills greater confidence in the accuracy of medical diagnoses and propels improved patient care.
Despite the promising results, several challenges must be addressed when implementing deep learning algorithms for detecting glaucoma in clinical practice.
One of the primary challenges stems from the need for more standardization in the data sets used to train these algorithms (R Krishnadas, 2021). Since different research studies and healthcare institutions may use varying data collection techniques and formats, it becomes crucial to establish standardized data sets that can be used uniformly to train learning algorithms specifically for diagnosing glaucoma (Leonard, 2022).
In addition to data standardization, another obstacle lies in the accessibility of these algorithms to all healthcare providers. While they have shown great potential in detecting glaucoma, their
WilliamA.Haseltine,PhD 219
deployment and usage may not be feasible for all healthcare professionals, especially those serving underserved populations. Hence, there is a need to develop user-friendly interfaces and tools that enable healthcare providers from diverse backgrounds to utilize deep learning algorithms effectively in detecting glaucoma among underserved populations.
Glaucoma is a significant cause of blindness and disability worldwide. Its prevalence will increase in the coming years, significantly impacting healthcare systems and individual patients. Advances in artificial intelligence and deep learning algorithms in healthcare have shown great potential for improving the accuracy of diagnosing glaucoma and detecting its progression. These algorithms can provide faster and more accurate diagnoses, potentially improving access to care for underserved populations and reducing diagnosis variability.
However, some challenges must be addressed before deep learning algorithms can be widely implemented in clinical practice for detecting glaucoma. These include focusing on data standardization and improving accessibility. By addressing these challenges, we can pave the way for widespread and accurate implementation of deep learning algorithms in clinical practice for the early detection and management of glaucoma.
Treatments
Effective therapies that can slow down the advancement of the disease are crucial to bringing about significant clinical benefits, preserving vision, and alleviating the substantial economic burden faced by patients and healthcare systems alike. Different treatments are available to manage glaucoma and prevent vision loss. These
BetterEyesight 220
treatments include medication, surgery, and device-based therapies, such as laser trabeculoplasty.
Medications are usually the first line of treatment for glaucoma. They work by lowering pressure and preventing further damage to the optic nerve. Prostaglandin analogs, beta-blockers, alphaagonists, and carbonic anhydrase inhibitors are commonly prescribed medications for glaucoma.
Surgical options are available for those with more advanced glaucoma or those who cannot tolerate medications.
Trabeculectomy is a surgical option that creates a new drainage channel to reduce intraocular pressure. It facilitates the drainage of the aqueous humor, specifically.
During this treatment, a surgeon creates a small opening, or "shunt," in the sclera and removes a portion of the trabecular meshwork, the sieve-like structure through which the aqueous humor flows out of the eye. This new channel allows excess fluid to drain, thus decreasing the pressure that can damage the optic nerve.
Trabeculectomy is highly effective in lowering intraocular pressure. It is often considered when other methods, such as medications or laser therapy, have failed to control glaucoma (Binibrahim & Bergström, 2017). However, the procedure carries some risks, including infection, excessive bleeding, and vision loss.
Compared to traditional incisional surgery, minimally invasive glaucoma surgery is less invasive and has a shorter recovery time (Beckers et al., 2021). They also have a lower risk of complications, such as bleeding or infection, and may not require general anesthesia (Beckers et al., 2021). These procedures typically involve
WilliamA.Haseltine,PhD 221
using canal-based or suprachoroidal-based devices inserted into the eye to reduce intraocular pressure.
Canal-based devices increase the drainage of aqueous humor, the fluid that fills the front of the eye. On the other hand, suprachoroidal-based devices work by shunting fluid from the front of the eye to the space between the sclera and the choroid, a layer of blood vessels in the eye.
It is worth noting that MIGS devices that form a bleb have been associated with substantial intraocular pressure reductions (Gurnani & Tripathy, 2022). A bleb is a fluid-filled pocket that forms under the conjunctiva, the thin membrane covering the eye's white part. The formation and management of the bleb play a critical role in surgical success. Surgeons can effectively regulate intraocular pressure and improve patient outcomes by carefully managing the bleb.
Researchers have developed a minimally invasive glaucoma surgery device known as the MicroShunt, which has shown promising results in reducing intraocular pressure and the usage of glaucoma medication (Beckers et al., 2021). The MicroShunt procedure involves creating a small incision on the eye's surface. Then, the device is placed under the conjunctiva, the white part of the eye, and connected to the anterior chamber, which is the space between the iris and the cornea. The device allows excess fluid in the eye to drain, which reduces intraocular pressure and prevents further damage to the optic nerve.
Studies conducted in the Dominican Republic have shown that MicroShunt has a high success rate of 95% in reducing pressure at year 3 (Beckers et al., 2021). However, it is essential to note that, like
BetterEyesight 222
any surgical procedure, there are potential adverse events, such as the device touching the iris, temporary low intraocular pressure, shallow or flat anterior chamber, and temporary choroidal effusion.
Still, MIGS devices like the MicroShunt offer a promising option for POAG patients as they are less invasive and effective than traditional glaucoma surgeries. While there are potential risks and complications associated with any surgical procedure, the MicroShunt has demonstrated effectiveness in reducing IOP and preserving vision. Early detection and treatment of POAG is crucial for the best possible outcomes. MIGS devices like the MicroShunt provide an alternative treatment option for those with this condition.
Another option for the treatment of glaucoma is laser therapy (Sarenac et al., 2022). These are promising treatment options for glaucoma patients due to their ability to improve fluid drainage from the eye, thereby reducing intraocular pressure. There are two primary laser therapies for glaucoma: laser trabeculoplasty and selective laser trabeculoplasty.

WilliamA.Haseltine,PhD 223
FIGURE 62: Glaucoma surgery diagram
SOURCE: ACCESS Health International
Laser trabeculoplasty involves using a laser to open up the drainage channels in the trabecular meshwork, allowing for better fluid outflow. On the other hand, selective laser trabeculoplasty selectively targets and treats specific areas of the trabecular meshwork while leaving other sites untouched. This precision laser energy targeting can lead to fewer side effects than traditional laser therapies (Sarenac et al., 2022).
Ongoing research aims to improve the efficacy of glaucoma treatments, reduce their side effects, and extend their duration of activity. Furthermore, the genetic basis of glaucoma is being explored through genome-wide association studies, which may lead to new and more effective treatment options (Sharif, 2023). Promisingly, gene therapy options are now emerging as a new avenue for treating glaucoma.
Gene therapy aims to alter the genes responsible for glaucoma to prevent further damage to the optic nerve. By targeting the specific genes that contribute to this condition, gene therapy can potentially halt or even reverse the progression of glaucoma.
Gene therapy is an innovative and promising approach to treating glaucoma. This therapy involves introducing healthy genes into the eye cells to repair or replace damaged genes responsible for the disease. One study published in the Journal of Clinical Investigation demonstrated the efficacy of gene therapy in reducing intraocular pressure (IOP) and preventing optic nerve damage in animal models of glaucoma (Sharif, 2023).
Researchers have also focused on targeting specific genes and pathways involved in the development of glaucoma, such as
BetterEyesight 224
oxidative stress and inflammation. Additionally, advancements in genetic engineering technology, such as CRISPR-Cas9 and optogenetic techniques, can potentially develop more precise and effective gene therapies for glaucoma and related ocular disorders (Abdelnour et al., 2021).
Stem cell-based treatments, specifically RGC (retinal ganglion cell) replacement therapy, are also being investigated (Coco-Martin et al., 2021). Retinal Ganglion Cells (RGCs) are specialized neurons that play a critical role in the visual system by transmitting information from the retina to the brain via the optic nerve. These highly complex cells comprise more than a dozen molecularly, functionally, and topographically unique subtypes. Each subtype has distinct morphology, connectivity, and response properties, allowing it to perform different visual system functions.
RGCs are the final output neurons of the retina. They are responsible for encoding visual information into electrical signals sent to the brain. These signals are then processed by higher visual centers in the brain, which enables us to see and perceive the world around us.
Despite their complexity, RGCs have been a promising target for therapeutic intervention as they do not regenerate naturally once they deteriorate. Any damage to these cells can result in permanent vision loss. Scientists are actively working to develop new therapies that can help protect and restore RGCs in individuals with retinal degenerative diseases such as glaucoma and age-related macular degeneration.
However, the limited availability of RGCs in stem cell-derived cultures makes the integration of RGCs into the host retina a
WilliamA.Haseltine,PhD 225
complex task. Organoids offer a promising alternative to traditional branch cell-based transplantation methods.
Organoids are self-organizing three-dimensional structures that closely resemble the complexity and organization of the retina. They are generated by culturing stem cells in a controlled environment that mimics the developmental process of the retina. Recent advances in organoid protocols have made it possible to create RGCs from both human and mouse stem cells, overcoming the limitations of traditional stem cell-based transplantation methods.

BetterEyesight 226
FIGURE 63: Cell delivery can be either suprachoroidal, intravitreal, or subretinal.
SOURCE: Multidisciplinary Digital Publishing Institute (MDPI)
Subretinal space and vitreous cavity transplantation are two potential methods for RGC replacement. Subretinal space transplantation involves transplanting cells into the subretinal area, which is located between the retinal pigment epithelium and the photoreceptor layer. The transplanted cells can integrate into the host retina and potentially restore vision.
Vitreous cavity transplantation, on the other hand, involves transplanting cells into the vitreous cavity of the eye, which is the gelatinous substance located behind the lens. The transplanted cells can secrete neurotrophic factors that promote the survival of the remaining RGCs and stimulate the regeneration of damaged ones.
Numerous studies are currently investigating the possibility of using RGC replacement therapy as a treatment for glaucoma. One such study was conducted on rats with glaucoma, and it showed significant improvement in visual function and RGC survival when RGC-like cells were transplanted into them (Luo & Chang, 2024). These RGC-like cells were differentiated from human-induced pluripotent stem cells, which can develop into any cell in the human body.
The study demonstrated that human-induced pluripotent stem cells could be a potential source for RGC transplantation in glaucoma patients. However, further research is necessary to determine the safety and effectiveness of this therapy before it can be implemented in clinical practice.
Still, despite the promise of studies, there are some challenges. A review done by a team in Spain assessed these challenges and more (Coco-Martin et al., 2021). One of the significant challenges is
WilliamA.Haseltine,PhD 227
understanding the origin of RGCs and how to replicate their natural development in laboratory settings.
Another area for improvement is the difficulty in scaling up the production of RGCs and ensuring they can be produced in large quantities. Additionally, once produced, there are challenges in integrating and ensuring the survival of transplanted RGCs in the host tissue
Regrowing RGC axons is also a significant challenge, as it requires identifying the factors that promote axon growth and determining how to apply them effectively. Finally, achieving functional RGC replacement is a significant hurdle, as it involves creating RGCs that can function as well as, or better than, the RGCs they are replacing.

SOURCE: Neural Regeneration Research19(4):807-810, April 2024.
BetterEyesight 228
FIGURE 64: This illustrative graph displays three commonly used types/formats of donor cells in retinal ganglion cell (RGC) replacement studies.
However, recent advances in stem cell technologies and organoid protocols discussed before offer new solutions to these limitations. For example, organoid protocols enable the generation of RGCs that more closely resemble those found in the human retina, thus improving the accuracy and efficacy of transplantation (Luo & Chang, 2024). Additionally, stem cell technologies have been used to create RGCs capable of integrating into the host tissue and regenerating axons.
RGC replacement therapy shows potential as a new therapeutic approach for treating glaucoma. Although there are challenges to overcome regarding scaling up RGC production and achieving reliable and functional integration, recent advancements in stem cell technologies and organoid protocols offer promising solutions. Clinical trials investigating the potential of RGC replacement therapy have reported positive outcomes, providing hope for restoring vision in glaucoma patients.
WilliamA.Haseltine,PhD 229
Retinal Detachment

The human eye is a miraculous work of nature, enabling us to perceive the world in all its beauty. However, sometimes, even the most intricate mechanisms of the eye can malfunction, leading to debilitating conditions such as retinal detachment.
This medical emergency demands immediate attention and is characterized by sudden vision loss, floaters, flashes of light, and more. Bullous retinal detachment is a specific type that forms a blister, potentially causing significant damage, often leading to permanent vision loss. While current surgical methods offer successful outcomes, they require a long and invasive recovery period.
Patients suffering from bullous retinal detachment may have a new, non-invasive alternative to surgical intervention in the form of photodynamic therapy (PDT). This therapy shows a lot of promise in improving patients' visual prognosis. In this article, we delve into the details of PDT, exploring how it works and the current limitations of this treatment.
Retinal detachment is a medical emergency that requires immediate attention. It is a condition that occurs when the retina, the thin layer of tissue at the back of the eye, separates from the underlying tissue. This separation can be caused by injury, disease, or other factors. The most common symptom of retinal detachment is sudden, painless vision loss, often described as a curtain-like
230
CHAPTER 11
shadow that moves across the field of vision. Other symptoms may include flashes of light, floaters, or the appearance of a veil or cobweb in the affected eye.
Bullous retinal detachment is characterized by forming a large, fluid-filled blister or bulla in the retina. This blister can cause significant damage to the retina and can lead to permanent vision loss if left untreated. Bullous retinal detachment is often caused by trauma to the eye. Still, it can also be the result of underlying medical conditions such as diabetes or high blood pressure. Treatment for bullous retinal detachment may include surgery to repair the damaged retina and restore vision or laser therapy to prevent further damage.
Currently, the most common methods of treating it involve surgical intervention such as scleral buckling or vitrectomy. In scleral buckling, a silicone band or sponge is placed around the eye to push the wall of the eye against the detached retina and help hold it in place. In vitrectomy, the surgeon removes the vitreous, clear gel from the eye and replaces it with a gas or oil bubble to help push the retina back in place.
While these procedures can be successful in many cases, they are invasive and require significant recovery. Patients may experience discomfort, blurred vision, and sensitivity to light during recovery, which can last several weeks. However, with proper care and followup appointments with their doctor, patients can expect to regain their vision and return to normal activities over time.
Photodynamic therapy (PDT) is a non-invasive treatment option that has shown promise in managing various retinal diseases, including bullous retinal detachment. PDT involves using a
WilliamA.Haseltine,PhD 231
photosensitizing agent, such as indocyanine green (ICG), injected into the patient's bloodstream. The photosensitizer is then activated by a low-power laser, which causes damage to the blood vessels that supply the affected area of the retina. This damage leads to the formation of a clot, which seals off the area and prevents any further fluid leakage or bleeding.
A study published in Graefe's Archive for Clinical and Experimental Ophthalmology evaluated the efficacy of half-dose PDT for treating bullous retinal detachment (Gao et al., 2018). Six patients with bullous retinal detachment received half-dose photodynamic therapy (PDT). The treatment was guided by a medical imaging technique called indocyanine green angiography (ICGA).
It uses laser spots that cover multiple areas. After the treatment, the patient's retinas were reattached, and the fluid underneath the retina disappeared. Three months later, the patient's vision improved significantly. One patient needed a second treatment because the sub-retinal fluid persisted, but eventually, their detachment resolved successfully.
While the results of this study are promising, there are several limitations to consider. The sample size was small, and there was no control group for comparison. Additionally, the follow-up period was relatively short, at only six months, so it is unclear how these patients will fare in the long term. Further research is needed to determine the optimal dosages and treatment parameters for bullous retinal detachment.
Despite these limitations, PDT offers a non-invasive alternative to surgical intervention for treating bullous retinal detachment. It is
BetterEyesight 232
less invasive and may recover faster than traditional surgical approaches. Additionally, PDT is effective in treating other retinal diseases, such as age-related macular degeneration, so there is potential for its use in a wide range of conditions.
In conclusion, photodynamic therapy has demonstrated promising results in managing bullous retinal detachment. Its non-invasive nature and efficacy in other retinal diseases make it an attractive alternative to traditional surgical approaches. While further research is needed to determine the optimal treatment parameters, this therapy offers hope for improved visual outcomes for patients with this condition.
WilliamA.Haseltine,PhD 233
Retinitis Pigmentosa

Retinitis Pigmentosa is a rare genetic disorder causing severe vision loss that progressively damages the retina. Those impacted feel imprisoned by tunnel vision in an ever-narrowing bubble of sight. Daily tasks become more challenging as the condition progresses, and simple activities feel like insurmountable obstacles. Walking down a street, for instance, becomes intimidating, as you may not be able to see the sidewalk or other people walking nearby, leading to the possibility of tripping or colliding with someone.
Retinitis pigmentosa (RP) is an inherited eye disease that affects over one million individuals worldwide. The condition is the leading cause of inherited blindness in developed countries. It is estimated to impair the vision of 1 in every 4,000 people (Qin et al., 2023).
It is characterized by the progressive and irreversible degeneration of photoreceptor cells, which are the cells lining the back of the eye responsible for converting light into electrical impulses sent to the brain. The disease typically affects both eyes, and most people with retinitis pigmentosa experience symptoms such as night blindness, tunnel vision, and loss of peripheral vision.
Genetic mutations cause the condition and can be passed down from parents to their children. There are at least 100 genes attributed to the disease (Qin et al., 2023). One such gene is phosphodiesterase 6b, also known as PDE6b. It is a protein-coding
234 CHAPTER
12
gene that plays a critical role in the phototransduction pathway. It converts light into an electrical signal the brain can interpret as vision.
In individuals with retinitis pigmentosa caused by mutations in the PDE6b gene, the gene is either absent or non-functional. As the disease progresses, cone photoreceptor cells, responsible for color vision, are affected. The loss of cone cells contributes to the severe and irreversible deterioration of vision in individuals with retinitis pigmentosa.
Treatment
Stem cell and gene therapies have been making significant progress in restoring vision loss due to age, disease, or trauma. Traditional gene replacement and CRISPR-Cas gene editing approaches have been used for gene therapy for retinal degenerative diseases.
CRISPR, or Clustered Regularly Interspaced Short Palindromic Repeats, is a revolutionary gene-editing technology that allows scientists to target and modify specific DNA sequences precisely and efficiently. CRISPR uses specialized cellular machinery to make precise cuts in the DNA strand, opening up the possibility of replacing or removing faulty genes and treating various genetic disorders.
The potential uses of CRISPR are vast and varied, ranging from developing new crops to treating life-threatening genetic diseases. In the medical field, CRISPR has shown great promise in treating degenerative eye diseases.
Researchers in China have developed a new, highly versatile form of CRISPR-based genome editing that has successfully restored the
WilliamA.Haseltine,PhD 235
vision of mice with retinitis pigmentosa, a leading cause of blindness in humans. The study will be published in the Journal of Experimental Medicine, focusing on using CRISPR to replace the gene causing retinal degeneration (Qin et al., 2023).
In the study, the researchers developed a CRISPR-based genomeediting tool named PESpRY. The system corrected the mutation in the PDE6b gene. The correction restored the gene's activity in the retinas of mice, prevented the death of rod and cone photoreceptors, and restored their normal electrical responses to light. The geneedited mice retained their vision even into old age, as shown in behavioral tests, such as finding their way out of a visually guided water maze or head movements in response to visual stimuli.
In addition, the researchers found that their PESpRY system led to the preservation of photoreceptors in the mice. This resulted in the rescue of visual function in the mice, supported by detailed electroretinograms and behavioral assessments.
The new system is a breakthrough that offers enormous potential. Its ability to enable practical and versatile genome editing within the body holds great promise for treating inherited retinal disorders, such as retinitis pigmentosa. With further research, the hope is to test these gene therapies in humans to see if we can overcome inherited retinal degeneration. It will be a significant advance in gene therapy.
A similar breakthrough, which relied on optogenetics, was described in a paper published in Nature Medicine (Sahel et al., 2021). While he could identify the notebook 92% of the time, he could only touch the smaller staple box 36% of the time and was
BetterEyesight 236
even reported to be able to see the white stripes of a pedestrian crosswalk.
The team of international scientists discovered that activity in the visual cortex of his brain changed depending on whether or not an item was there, demonstrating its relationship to the retina using non-invasive electroencephalography (EEG) readings. The results were described as "remarkable." “I think that a new field is being born,” University of Basel professor and researcher Botond Roska told reporters during a recent conference call announcing the team’s results.
Scientists have utilized optogenetic therapies to restore vision for over a decade in people with degenerative eye diseases, such as retinitis pigmentosa (Saey, 2015). It combines optics and genetics, allowing researchers to regulate individual neurons in vitro using visible light. Brain cells are first exposed to light-sensing molecules, which are then activated by light pulses from fiber-optic threads. The chemical turns light into an electrical impulse, also causing the neuron to fire. This allows researchers to stimulate specific neurons on demand, potentially affecting the subject's behavior and responses. The method is based on algal proteins that move in response to light sources. In the therapy, scientists injected these genes into the retina's remaining functional ganglion cells, causing them to create the light-sensitive protein ChrimsonR.
“It’s exciting. It’s really good to see it working and getting some definite responses from patients,” says David Birch, a retinal degeneration expert at the Retina Foundation of the Southwest in Dallas. Birch has conducted clinical trials of other optogenetic therapies but was not involved in this study.
WilliamA.Haseltine,PhD 237
As part of their PIONEER 1/2a investigation, the University of Basel-UPMC team used GenSight Biologics technology to apply the core theories of optogenetics to the retina. The two-pronged approach was adopted using both biological and technological components. The biological aspect addressed the RP issue as the researchers targeted the patient’s retinal ganglion cells for genetic therapy that would make them photoactivatable.
Normally, the rods and cones are photosensitive. Still, given that RP had essentially damaged and destroyed the patient's rods and cones, the ganglion cells (mainly focusing on carrying electrical charges generated by those photoreceptive cells) would have to be modified (Bi et al., 2006). To do this, the researchers isolated a gene from a light-sensing species of green algae into one of the patient's eyes. This leads to the gene encoding a photoactivatable protein called ChrimsonR.
“These proteins are very special,” Dr. José-Alain Sahel, Distinguished Professor and Chairman of the Department of Ophthalmology at the University of Pittsburgh School of Medicine, co-founder of Gensight Biologics and co-lead investigator for the PIONEER study, told Engadget. “They were discovered in the late ‘90s and early 2000s. These proteins exist in algae, capturing light and triggering an electrical response that enables the algae to move towards or retract from light, and it's a single protein, so it's a very fast response.”
After a few months, the ganglions produced sufficient amounts of ChrimsonR. The technological aspect came in because ChrimsonR is most responsive to light in the 590nm wavelength (amber). As this is far brighter than ambient lighting can produce, Gensight (founded by Dr. Sahel and his colleagues) developed a proprietary
BetterEyesight 238
set of goggles that collect image data from an incorporated event camera and beam high-intensity, 590nm wave light directly into the patient’s eyes.
“We developed a bioinspired camera that functions at every single pixel by detecting any change in light sensitivity,” Sahel explained. “These cameras can detect very low levels of changes, can function at low levels applied and high levels of light. We are functioning pixel by pixel, and we are processing the image in real-time.”
This is the first reported case of partial functional recovery in a neurodegenerative disease after optogenetic therapy. However, this current PIONEER study is a very preliminary start to this form of therapy. Before optogenetics can become a standard treatment for some forms of blindness, further positive clinical trial findings are needed.
For now, Dr. Sahel and his colleagues are bringing in additional volunteers for training, testing stronger virus dosages, and updating their goggles to thin spectacles that are more comfortable and deliver more information to the retina. Compared to the Orion Visual Cortical Prosthesis System, which requires probes to implant a control unit chip in your skull, optogenetic therapy can be a less invasive approach. Sahel and Roska stress that the treatment is not a cure for blindness.
“For now, all we can say is that there is one patient … with a functional difference,” Roska says. Sahel adds, “it’s a milestone on the road to even better outcomes.”
WilliamA.Haseltine,PhD 239
Understanding Retinopathy

Diabetic retinopathy, a condition that develops in people with diabetes, is a silent thief that robs them of their vision. It is one of the leading causes of blindness in the working population worldwide, and its prevalence is steadily rising (Lee et al., 2015). In 2021, diabetic retinopathy affected an estimated 9.6 million people in the US, comprising 26.43% of those with diabetes (Lundeen et al., 2023).
It is a diabetes-related complication that impacts the blood vessels in the retina. The retina, located at the back of the eye, is responsible for visual perception. High blood sugar levels can cause damage to the blood vessels in the retina, leading to a range of symptoms and complications. The disease can progress through two main stages: non-proliferative diabetic retinopathy (NPDR) and proliferative diabetic retinopathy (PDR), with the latter being the more severe. Several factors can elevate the risk of developing diabetic retinopathy. These include uncontrolled blood sugar levels, high blood pressure, high cholesterol, obesity, pregnancy, and smoking. As the duration of diabetes increases, the likelihood of diabetic retinopathy also rises (Bhavsar et al., 2023). Timely identification and intervention are critical in mitigating vision impairment and reducing the complexities associated with this ailment.
Several pathways and mechanisms that play a significant role in the development and progression of diabetic retinopathy are identified.
240 CHAPTER
13
A study by the University of Malaya outlines these pathways and mechanisms (Safi et al., 2014). One of the critical pathways is the polyol pathway, which converts excess glucose to sorbitol and fructose. This process leads to osmotic stress and oxidative damage in the retina.
Another important pathway is the protein kinase C (PKC) pathway, which produces vascular endothelial growth factor (VEGF), leading to abnormal retina growth. In addition, non-enzymatic glycation, inflammation, oxidative stress, and activation of the reninangiotensin system (RAS) are also implicated in the development of diabetic retinopathy. Failure to address these pathways and mechanisms can result in retinal damage and vision impairment if left unattended.
Early screening and proper management can prevent or slow its progression, underscoring the importance of screening programs. Screening programs play a critical role in preventing complications of diabetic retinopathy, and the efficacy of these programs can be enhanced through artificial intelligence (AI).
In recent years, AI has emerged as a tool in the early detection and treatment of diabetic retinopathy. AI-powered computer-aided diagnosis systems are being developed to analyze retina images and identify abnormalities indicative of diabetic retinopathy. These systems use machine learning algorithms to recognize and classify features such as microaneurysms, hemorrhages, and exudates. By analyzing these features, AI can evaluate the severity of the condition and recommend appropriate treatment (Rajesh et al., 2023).
WilliamA.Haseltine,PhD 241

SOURCE: Copyright © 2023, American Diabetes Association
Retina images are captured and uploaded to a cloud server during a typical eye exam. These images are later analyzed by artificial intelligence using advanced machine learning algorithms, which generate comprehensive reports for clinicians. These reports highlight any potential abnormalities, which can be further evaluated by either AI or humans to determine the risk of disease or disease progression.
BetterEyesight 242
FIGURE 65: Example workflow of using AI model for DR screening
For patients at an elevated risk of developing the condition, it becomes possible to implement early interventions to prevent potential vision loss. This proactive approach can significantly contribute to preserving and safeguarding one's eyesight.
A recent study published in JAMA NetworkOpen evaluated an AI algorithm's ability to analyze non-invasive retinal imaging (Kanagasingam et al., 2018). The algorithm achieved an impressive sensitivity of 87.2% and a specificity of 90.7% in predicting the future development of diabetic retinopathy compared to a highly rigorous reference standard set by expert human graders.
Furthermore, a review by a team from the University of Washington in Seattle assessed the performance of various AI algorithms designed explicitly for diabetic retinopathy (Rajesh et al., 2023). The AI output was evaluated against the reference standard established by ophthalmologists. The findings revealed that the algorithms consistently outperformed the specialists in multiple studies. However, the review does express apprehension regarding the limitations and accessibility of these technologies in clinical practice.
By merging the power of AI technology with the expertise of healthcare professionals, more accurate diagnoses and effective treatment plans can be developed. Artificial intelligence can assist in the early identification of medical conditions like diabetic retinopathy. This can result in timely interventions and ultimately improve patient outcomes.
Early detection of diabetic retinopathy is vital for successful treatment and improved patient outcomes (Vashist et al., 2011). Not only does it reduce the need for frequent checkups (Tung et al.,
WilliamA.Haseltine,PhD 243
2008), but it also aids in lowering healthcare costs (Avidor et al., 2020). Early detection can also reduce the risk of vision loss for diabetics by 95% (Lahr, 2019).
Healthcare providers can use predictive AI models and diagnostic assistance to accurately identify patients who require monitoring and direct them to appropriate care. A team from New York conducted a study that showed how diabetic retinopathy risk can be determined by fundus photography (Rom et al., 2022). By training AI on a machine learning algorithm, the images can be assessed for risk.
AI systems can help reduce the workload of healthcare professionals (Hamid Shamszare & Choudhury, 2023), enabling them to spend more time on quality patient care, which is critical given the growing shortage of medical personnel. At the same time, the AI takes on the laborious task of analyzing medical images (Rom et al., 2022). This approach optimizes healthcare resources by prioritizing patients needing immediate attention while avoiding unnecessary checkups that can drain time and finances. Additionally, leveraging predictive AI models aids in identifying potential health risks early on, resulting in further enhancements to patient outcomes (Wang et al., 2023).
The use of AI in managing diabetic retinopathy has been a topic of debate due to its controversial effectiveness. While AI can screen patients for diabetic retinopathy, researchers have reported that relying solely on AI may lead to overdiagnosis and overtreatment of patients (Wang et al., 2023). AI algorithms may classify lesions as clinically significant when they are not (Kanagasingam et al., 2018).
BetterEyesight 244
Another limitation of AI in diabetic retinopathy management is its ability to analyze retina images and make thorough treatment recommendations (Rajesh et al., 2023). While AI can detect certain features of the retina, it cannot evaluate the patient's medical history, current symptoms, or other factors that may be critical in making treatment decisions.
Therefore, healthcare professionals should view AI as a supplementary tool (Wang et al., 2023) to provide personalized care to patients with diabetic retinopathy and not as a replacement for human clinicians.
By leveraging AI's capacity to identify high-risk groups and facilitate early diagnosis and monitoring, we can reduce the prevalence of vision loss and blindness among diabetic individuals. But it doesn't stop there.
These systems can also enhance screening accuracy, efficiency, and affordability, making them accessible to a broader population. However, for optimal patient and societal benefits, it is imperative that AI technology adheres to sound ethical guidelines and integrates effectively into healthcare settings.
Our aim should be to refine the AI system's diagnostic accuracy further and combine it with interventions promoting healthy lifestyles, thus preventing diabetic retinopathy's development and progression.
Treatments
Effectively managing this condition requires maintaining tight control over blood glucose and blood pressure levels. This is typically the first course of action that most doctors recommend to
WilliamA.Haseltine,PhD 245
prevent or slow down the progression of the disease. Early detection can help slow its passage in the initial stages by closely monitoring your blood glucose and blood pressure.
Laser treatment is frequently used in later stages to stop further damage and prevent vision loss (National Eye Institute, 2022). It targets and halts the growth of new, fragile blood vessels that can bleed within the eye. The procedure involves multiple treatments that may be necessary to ensure the best outcome, and the frequency of treatment depends on the severity of the condition (NHS Choices, 2020). It is a safe and effective outpatient procedure that does not require hospitalization (Healthwise, 2023). However, laser treatments are limited in their ability to restore vision that has already been lost and may cause some degree of vision loss following the procedure due to the destruction of healthy tissue in the treated area.
When laser treatment fails, or in cases of advanced retinopathy, antiVEGF medication is a viable treatment option (Zhao & Singh, 2018). These medications are directly injected into the eye's vitreous, a gel-like substance. They prevent the growth of new blood vessels and reduce fluid buildup. Anti-VEGF medication works by blocking the action of VEGF protein, which stimulates the development of new blood vessels in the retina. As a result, antiVEGF medication can prevent abnormal blood vessel growth in the retina (Simó et al., 2014). Anti-VEGF treatment for diabetic retinopathy requires frequent and costly injections, leading to issues with compliance and accessibility for some patients.
Another option is steroids. Steroid implants can be placed in the eye to reduce inflammation and swelling (Rittiphairoj et al., 2020), which can cause vision loss in patients with diabetic retinopathy,
BetterEyesight 246
particularly those with macular edema. In cases where laser treatments are not an option due to the severity of the retinopathy, eye surgery may be performed to remove blood clots or scar tissue accumulated in the eye due to retinopathy (NHS Choices, 2020). This procedure can help restore vision in less severe cases of diabetic retinopathy. It's essential to mention that while steroid implants may help treat diabetic retinopathy, they come with certain limitations. They can cause an increase in intraocular pressure, lead to cataract formation, and other complications that require careful monitoring and management by a qualified healthcare professional.
In addition to the standard treatments currently available for diabetic retinopathy, researchers are exploring new and innovative methods to combat this eye disease. One such cutting-edge treatment is gene therapy, which involves the insertion of healthy genes into the retina to replace faulty ones responsible for developing diabetic retinopathy. Although gene therapy is still experimental, it has shown promising results in treating and managing this condition (Wang et al., 2020).
Another potential treatment option being explored by researchers is stem cell therapy (Leng et al., 2021). It involves replacing damaged or dead cells in the retina with stem cells. However, certain challenges limit its effectiveness, such as the risk of immune rejection of the transplanted cells, difficulty selecting the appropriate type of stem cells, and the potential for tumor growth. Although still in the early stages of development, stem cell therapy holds great promise as a future treatment option for individuals with diabetic retinopathy.
WilliamA.Haseltine,PhD 247
Researchers are also investigating using a protein called NOX4 as a potential therapeutic target for diabetic retinopathy (Wang, Li, Luo, et al., 2023). NOX4 is recognized for its involvement in the development of this disease. By targeting this protein, researchers hope to develop new treatments to manage and treat diabetic retinopathy effectively.
One of the critical molecular players in diabetic retinopathy is a protein called NOX4, a member of the NADPH oxidase family of enzymes that generate reactive oxygen species (ROS) in cells.

FIGURE 66: Illustration of NOX4
SOURCE: Biozentrum
NOX4 is expressed in retinal cells, including vascular cells, affected by diabetic retinopathy. Studies have shown that NOX4 promotes oxidative stress and inflammation in the retina, leading to damage to the blood-retinal barrier (BRB) and the development of early and advanced stages of diabetic retinopathy (Liu, 2022). NOX4 also
BetterEyesight 248
activates several signaling pathways (Anilkumar et al., 2008) that contribute to the disease's pathogenesis, including the AGE-RAGE pathway, the protein kinase C (PKC) pathway, and the vascular endothelial growth factor (VEGF) pathway.
Therefore, NOX4 has emerged as a promising therapeutic target for treating diabetic retinopathy. Several preclinical studies, such as one by the University of Crete, have shown that inhibiting NOX4 activity can reduce oxidative stress, inflammation, and vascular dysfunction in the retina, preventing the development and progression of diabetic retinopathy (Stavroula Dionysopoulou et al., 2023).
Among the numerous NOX4 inhibitors developed for this purpose, an inhibitor called GLX7013114 has emerged as an up-and-coming candidate. The previously mentioned study by the University of Crete delved deeper into the effects of this NOX4 inhibitor in vivo using two experimental models of diabetic retinopathy (Stavroula Dionysopoulou et al., 2023).
The study found that when administered topically as eye drops, GLX7013114 exhibited considerable beneficial effects in reducing oxidative stress, neurodegeneration, and neuroinflammation in the diabetic retina. Additionally, the NOX4 inhibitor mitigated the diabetes-induced increase in vascular endothelial growth factor (VEGF) levels and proinflammatory cytokine levels in the retinal tissue. Furthermore, GLX7013114 exhibited neuroprotective, antiinflammatory, and vasculoprotective properties, which can protect retinal ganglion cell function.
Another study published in RedoxBiologyalso found similar results (Wang, Li, Luo, et al., 2023). The study highlights NOX4's
WilliamA.Haseltine,PhD 249
importance in controlling redox signaling in high glucose and regulating oxidative stress. The article also briefly discusses NOX4's relationship with diabetic macroangiopathy and outlines potential areas for future research.
These encouraging findings highlight the exciting prospects of GLX7013114 as a possible therapeutic intervention for diabetic retinopathy. The continued research and development in this field hold promise for preventing and managing this visually impairing condition, ultimately improving the lives of individuals affected by diabetic retinopathy.
Researchers are exploring alternative therapeutic targets that can complement or replace NOX4-based treatments to counteract the effects of AGEs and develop more effective treatments for diabetic retinopathy (Kupis et al., 2022). Among these targets are protein kinase C and advanced glycation end products.
Protein kinase C encompasses a group of enzymes that play a crucial role in orchestrating diverse cellular functions like cell growth, differentiation, and programmed cell death. These enzymes wield significant influence over fundamental cell processes, working together harmoniously to ensure proper cellular functioning. Multiple signals, such as hormones, growth factors, and stress, activate them. Once activated, they phosphorylate target proteins, modulating their activity and function. There are several isoforms of protein kinase C, each with a distinct expression pattern and localization within the cell.
Recent research has shown that protein kinase C plays a significant role in developing diabetic retinopathy and other diabetic microvascular complications (Pan et al., 2022). In diabetic
BetterEyesight 250
retinopathy, protein kinase C is activated by high glucose levels, leading to increased vascular permeability, inflammation, and oxidative stress. This, in turn, contributes to the development of retinal edema, hemorrhages, and neovascularization. Protein kinase C has also been implicated in other microvascular complications of diabetes.
In the case of diabetic retinopathy, advanced glycation end products are believed to contribute to microvascular damage and inflammation in the retina. AGEs are compounds formed when proteins and sugars undergo glycation. They play a significant role in diabetic complications such as neuropathy, nephropathy, and retinopathy. This irreversible process creates cross-linked molecules resistant to the body's natural turnover and removal mechanisms. AGEs contribute to microvascular damage, inflammation, and abnormal blood vessels in diabetic retinopathy.
Ongoing scientific research is expected to provide in-depth insights into the intricate molecular mechanisms involved in diabetic retinopathy, a common complication of diabetes. By understanding these mechanisms, researchers can develop more effective inhibitors that can help prevent or treat the condition. These advances in research offer exciting prospects for the potential treatment of diabetic retinopathy, which could improve the quality of life for millions of people living with this condition.
Retinopathy of Prematurity
Retinopathy of prematurity (ROP) is a disease that has become increasingly common and significant in recent years. As a result of advances in neonatal care, more premature infants are surviving. Still, they are also at higher risk of retinopathy of prematurity
WilliamA.Haseltine,PhD 251
(AlajbegovicHalimic et al., 2015). This disease can lead to blindness and other visual impairments, causing lifelong consequences for individuals and their families (Jefferies, 2010). However, there is hope. Advances in treatment methods and ongoing research are improving the outcomes for premature infants with ROP.
Retinopathy of prematurity (ROP) is a condition that occurs when abnormal blood vessels grow in the retina, which is the lightsensitive layer of tissue at the back of the eye. This condition mainly affects premature infants, especially those born before 31 weeks of pregnancy or weighing less than 3 pounds at birth (Boyd & Vemulakonda, 2018). The development of ROP is due to abnormal retinal development, which is likely associated with varying levels of oxygen exposure during pregnancy (de las Rivas Ramírez et al., 2022).

by interrupted blood vessel development in two phases. In phase I, infants receive excess oxygen that stops normal vessel growth and causes vessel loss. In phase II, the infant is placed back into room air, causing abnormal blood vessel growth and activating certain proteins. The genes encoding Ang, EPO, IGF, and MMP are upregulated.
SOURCE: Copyright © 2022 by Juhee Ryu
ROP has five stages, ranging from mild, in which the blood vessels grow only to the edge of the retina, to severe, in which the blood
BetterEyesight 252
FIGURE 67: Retinopathy of prematurity (ROP) is caused
vessels grow through the retina and cause retinal detachment, leading to possible blindness (Molinari et al., 2017).
Treatment options for ROP depend on the severity of the condition and the stage at which it is detected (National Eye Institute (NEI), 2019). In mild cases, the condition may resolve on its own without treatment. However, in more severe cases, treatment options may include laser therapy, cryotherapy, or surgery. In some cases, followup care, such as eye exams and monitoring, may be necessary to prevent further vision loss.
Laser therapy is the standard treatment for ROP, which involves using a laser to produce minor burns on the outer edges of the retina (Stuart, 2014). This procedure stops the growth of abnormal blood vessels and prevents further complications such as retinal detachment, scarring, and blindness.
Laser therapy is performed under local anesthesia and takes only a few minutes. The physician will use an ophthalmoscope to direct the laser beam to the affected areas of the retina. The procedure may cause mild discomfort, but infants generally tolerate it well.
Studies have shown that laser therapy is highly effective in treating ROP (Stuart, 2014). The results depend on the severity of the condition and the timing of the treatment. In some cases, multiple sessions may be required to achieve optimal results.
Anti-VEGF drugs are a type of medication that can be administered via injections to help block the growth of blood vessels. These drugs are designed to work by inhibiting the protein VEGF, which plays a crucial role in forming new blood vessels. VEGF is responsible for promoting the growth of blood vessels by signaling specific cells to divide and multiply.
WilliamA.Haseltine,PhD 253
However, in some cases, such as when VEGF levels are too high, this can lead to the growth of abnormal blood vessels that can cause health problems. By inhibiting the action of VEGF, anti-VEGF drugs can help prevent the development of these abnormal blood vessels, which can be beneficial in treating ROP (Stuart, 2014).
In severe cases of ROP, surgical interventions such as scleral buckle or vitrectomy may be required. A scleral buckle is a silicone band placed around the eye, which helps to relieve traction on the retina. A vitrectomy involves removing the vitreous gel, the transparent substance inside the eye, and replacing it with a saline solution.
Clinical trials are being conducted to investigate new ROP treatment and prevention methods (Ryu, 2022). Some studies examine the use of stem cells to repair damaged retinal tissue. At the same time, others explore the use of gene therapy to suppress abnormal blood vessel growth. Further studies investigate the effectiveness of early vitamin A supplementation in reducing the incidence of ROP in premature infants.
Although some trials have reported promising outcomes, more research is needed to verify the safety and efficacy of these new methods. Nevertheless, advances in treatment methods, such as laser therapy, have significantly improved outcomes for premature infants with ROP, leading to better visual acuity and fewer cases of blindness.
With continued advancements in medicine and research, there is reason to be optimistic about the future of ROP treatment and outcomes for premature infants.
BetterEyesight 254
Familial Exudative Vitreoretinopathy
Familial exudative vitreoretinopathy (FEVR) is a rare genetic disorder that affects the development of the blood vessels in the retina. This inherited disorder causes the blood vessels in the retina to develop abnormally, leading to abnormal connections between the arteries and veins in the eye. This can cause the leaking of blood and other fluids into the retina, resulting in vision problems such as blurry or distorted vision, partial or complete vision loss, and even blindness.
Familial exudative vitreoretinopathy (FEVR) is an inherited disorder that affects the development of the blood vessels in the retina. Specifically, the blood vessels in the retina fail to develop normally, causing abnormal connections between the arteries and veins. This can result in blood and other fluids leaking into the retina, leading to vision problems such as blurry or distorted vision, partial or complete vision loss, and even blindness.

WilliamA.Haseltine,PhD 255
FIGURE 68: The image depicts the changes that occurred in the retina of the right eye of a patient suffering from a rare genetic disease known as Familial Exudative Vitreoretinopathy (FEVR) over three years. It shows the development of exudate and the dragging of the retina.
SOURCE: Janeannyoung by Wikimedia Commons
FEVR is a condition that can affect people differently. Some may experience mild vision issues, while others may have more severe symptoms. The symptoms can also vary between the eyes and even among family members with the condition (RESERVED, 2014). It is possible for an illness not to affect vision in some cases. However, those who have symptomatic FEVR generally encounter issues with their peripheral vision, experience flashes, or see floaters at a young age. FEVR may also be linked to other health problems like hearing loss or skeletal abnormalities.
The research paper published in the Molecular Genetics and Metabolism Reports journal provides valuable insights into the role of the Endoplasmic Reticulum (ER) membrane protein complex (EMC) in regulating retinal angiogenesis (Li et al., 2023). The study highlights how EMC malfunction can lead to familial exudative vitreoretinopathy (FEVR).
This study's findings are essential for diagnosing, managing, and treating FEVR and retinal vascular diseases. The protein EMC1 is necessary for retinal vascularization and is critical in the Wnt/βcatenin signaling pathway. Identifying EMC1 could lead to new drug targets and treatments. The study also used WES analysis to find genetic variants in the EMC1 gene, which could help in genetic counseling and selecting patients for gene replacement therapy.
The study sheds light on the molecular basis of retinal angiogenesis and the relationship between EMC proteins and signaling pathways in retinal development. Finding new candidate genes through WES analysis could help identify pathogenic genes for other genetic
BetterEyesight 256
diseases, improving our understanding of disease mechanisms and enabling targeted therapies.
While there is no cure for FEVR, early diagnosis and treatment can help manage the symptoms and prevent further vision loss (Sızmaz et al., 2015). Familial exudative vitreoretinopathy (FEVR) is treated according to the severity of the eye condition.
If the case is mild, the doctor may not suggest any treatment and simply observe the patient. In moderate to severe cases, the goal is to prevent the progression of neovascularization, which can cause hemorrhage and exudation. Laser photocoagulation or cryotherapy may be used to manage neovascularization. At the same time, antivascular endothelial growth factor (VEGF) therapy may reduce hemorrhage and exudation.
If there is ongoing fibrovascular proliferation, surgery may be needed to address potential complications like retinal detachments. The surgery may involve the removal of the lens or vitrectomy, which is the removal of the vitreous gel in the eye. Prompt intervention is essential to prevent complications like vitreous hemorrhage, retinal detachment, and neovascular glaucoma.
Timely diagnosis and appropriate management of FEVR are imperative to prevent complications and preserve vision. Although no definitive treatment exists, a personalized approach based on the patient's eye condition and stage can provide the best outcome.
Familial exudative vitreoretinopathy (FEVR) is a rare genetic disorder that affects the development of the blood vessels in the retina. This inherited disorder can cause vision problems such as blurry or distorted vision, partial or complete vision loss, and even blindness. While there is no cure for FEVR, early diagnosis and
WilliamA.Haseltine,PhD 257
treatment can help manage the symptoms and prevent further vision loss.
The current treatment strategies for FEVR involve laser photocoagulation or cryotherapy to manage neovascularization and anti-vascular endothelial growth factor (VEGF) therapy to reduce hemorrhage and exudation. Surgery may be necessary to address potential complications like retinal detachments, vitreous hemorrhage, and neovascular glaucoma.
Further research on the molecular basis of retinal angiogenesis can help develop targeted therapies and improve patient outcomes. Comprehensive eye exams, genetic testing, counseling, and timely interventions can significantly impact the management of FEVR.
BetterEyesight 258
Color Blindness and Night Blindness

Imagine standing atop a mountain, gazing out at a breathtaking sunset. The sky is ablaze with a riot of colors - reds, oranges, yellows, and purples - all merging and blending to create a stunning display of natural beauty. From the deepest blues of the ocean to the lush greens of the forests, colors are an essential part of our world, adding depth and dimension to everything around us. Yet, the intricacies of color perception are often overlooked.
Each color we see results from a complex interplay of light and our brain's interpretation. The colors we perceive are not static but constantly shifting, changing with the light source and our biases. Cultural, biological, and individual factors influence how we perceive color, making color perception a multidimensional phenomenon.
In this chapter, we explore the intricacies of color perception, including color blindness and the impact of color on mood and psychology.
Color Perception
Color perception is a complex process involving light interaction with specialized photoreceptor cells in the retina. The visible light spectrum contains all the colors from violet to red. When light shines on an object, the physical properties of that object determine
259 CHAPTER
14
how it absorbs, reflects, and emits light, affecting how we visually perceive the object.
The perception of color involves the interaction of light with specialized photoreceptor cells in the retina called cones. Most mammalian retinae only contain two types of cones, sensitive to short and medium-wavelength light. Humans, however, have an additional cone sensitive to long-wavelength light at the red end of the visual spectrum. This additional cone allows us to see a broader range of colors than most mammals.

SOURCE: © 2000-2023 AAV Media, LLC
The first step in the visual cycle is the retinal's light-mediated conformational change, which activates an associated opsin that acts as a protein-coupled receptor. Each cone type is associated with a different opsin with other genetic bases. These cones are responsible
BetterEyesight 260
FIGURE 69: image diagram of the eye in detail showing rods and cones
for color perception, and the specific wavelengths of light they absorb determine the perceived color.
Multiple factors can influence our perception of colors; sensory inputs are vital contributors to our perception of colors. One such input is what we see and the context in which we see it. The color's surroundings can significantly impact our perception of it.
For example, the perceived brightness of a color can be influenced by the background on which it is placed. Researchers have found that a red square set on a white background may appear brighter than the same red square placed on a black background (Welbourne, 2016). This effect, known as simultaneous contrast, occurs because the color receptors in our retinas are stimulated differently based on the surrounding colors.
The context in which a color appears can also alter how we perceive its hue. The shade of blue may appear greener when surrounded by yellows than pinks. Thus, our perception of colors is determined by the colors themselves and the context in which they are presented, highlighting the complex and multifaceted nature of color perception.
Furthermore, research published in Frontiers in Psychology has shown that smells can impact our perception of colors (Ward et al., 2023). In some cases, specific odors can be strongly associated with particular colors, and the presence of these odors can subtly alter our color perception. For example, the smell of lemons may cause us to perceive yellow as brighter or more intense. Similarly, the scent of lavender may make us perceive shades of purple as more calming or soothing. This phenomenon can be seen in the visual below.
WilliamA.Haseltine,PhD 261

SOURCE: © 2023 Ward, Ashraf, Wuerger and Marshall.
The figure showcases the angle data for each odor relative to the control, revealing a general shift toward warm colors in the presence of any fragrance. While four odors (lemon, caramel, cherry, and coffee) align with their anticipated crossmodal correspondences, the expected green-blue color trend for peppermint was not observed. Error bars (dashed lines) denote the standard mean error. These findings were statistically validated, indicating a significant impact of odor on color perception and suggesting a potential crossmodal integration mechanism.
Our brains can change and adapt based on our experiences, known as brain plasticity. This phenomenon can potentially improve our
BetterEyesight 262
FIGURE 70: Angle for each of the odors relative to the control. Error bars (dashed lines) denote the standard mean error.
color perception, especially in cases of color blindness. According to recent studies, experience actively influences circuits for color vision, which can alter color perception and persist even after the incident has ended (Neitz et al., 2002).
In the study, researchers focused on color-deficient adults with inherited photopigment defects. Despite the defects, these individuals still experienced vivid color sensations. This indicates that their brains adapted to the neural circuitry associated with color vision.
The researchers found that these color-deficient adults had altered weightings of inputs to chromatic channels, which points to a significant neural adjustment due to their inherited photopigment defect. This finding shows that chromatic experience can change color perception, and this change persists even after the experience has been discontinued.
This study provides compelling evidence that experience plays an active role in shaping the neural circuits associated with color perception. The ability of the visual system to adapt and change in response to experience offers great promise for the treatment of genetic disorders and the recovery from neurological damage.
Color Blindness
Color blindness is when individuals have difficulty distinguishing between specific colors, usually red and green. This condition occurs when there is a defect in the M or L cone opsins on the X chromosome. In addition, S cone opsin defects can also occur, although less frequently. While color blindness cannot be cured, improving color discrimination is possible.
WilliamA.Haseltine,PhD 263
Color blindness can significantly impact how people perceive and experience the world around them, affecting their emotions and communication. For instance, people with color blindness may find it challenging to convey the right mood or tone in a conversation because they cannot distinguish specific colors. For example, colorblind individuals have trouble differentiating between red, blue, and green hues.
Approximately 8% of men and 0.5% of women with Northern European ancestry have some form of color blindness (Wood, 2023). Color blindness is often hereditary, but it can also result from an injury or a disease affecting the retina or the optic nerve.
This vision disorder occurs when the photopigments, the lightsensitive chemicals in the retina, are not working correctly or are absent. These photopigments are responsible for interpreting the signals from the cones of the light-sensitive cells in the eye and converting them into electrical messages that are sent to the brain. The brain then interprets these signals as different colors.
The human eye has three cones responsive to red, green, and blue light, respectively. These cones are accountable for our ability to perceive various colors, hues, tints, and shades. These cones are most sensitive to light wavelengths between 400-700 nanometers, which correspond to the visible light spectrum.

BetterEyesight 264
FIGURE 71: A linear representation of the visible light spectrum.
SOURCE: Gringer on Wikimedia Commons.
Individuals with normal vision possess all three types of cones, which allow them to see a broad range of colors. However, people with color blindness have a deficiency in one or more types of cones, which can lead to difficulty distinguishing specific colors. For instance, a person with red-green color blindness may have difficulty differentiating between shades of red and green.
There are three primary types of color blindness: protanopia, deuteranopia, and tritanopia.

SOURCE: All About Vision
Protanopia is the most common form of color blindness, affecting around 1% of men (Birch, 2010). It is caused by the absence of redsensitive cones in the retina, which makes it difficult to differentiate between red and green colors. As a result, people with protanopia
WilliamA.Haseltine,PhD 265
FIGURE 72: Visual representation of primary types of color blindness
tend to confuse red and green hues and perceive them as shades of yellow or gray.
Deuteranopia, affecting around 5% of men, is caused by the absence of green-sensitive cones in the retina (Seltman, 2023). This type of color blindness makes it difficult for an individual to distinguish between red and green colors and perceive them as shades of gray or blue.
Tritanopia is a rare type of color blindness, affecting less than 1% of the population (Medline Plus, 2015). It is caused by the absence of blue-sensitive cones in the retina, which makes it difficult to differentiate between blue and yellow colors. People with tritanopia tend to confuse blue and green hues and perceive them as shades of pink or purple.
Another type of color blindness is Blue Cone Monochromacy (BCM) (Genetic and Rare Diseases Information Center, 2016). This rare condition affects about one in every 100,000 people (Kohl & Orphanet, 2013). BCM is a genetic disorder resulting from the absence or damage of the genes responsible for the blue photopigment in the retina cones. This leads to reduced color perception and poor visual acuity, making daily activities such as selecting matching clothes, identifying objects in traffic lights, or distinguishing between colors more difficult.
Recent advances in gene therapy offer a promising solution to this condition. Gene therapy can potentially restore the function of the missing or damaged genes in the retina, allowing for improved color perception and visual acuity. This means that individuals with BCM can look forward to a brighter future where they can better
BetterEyesight 266
enjoy life's colorful moments and engage in activities they previously found difficult.
Blue cone monochromacy (BCM) is a rare X-linked retina disorder. It causes a complete or near-complete loss of function in the L- and M-cones responsible for color vision. As a result, individuals with BCM rely only on their S-cones, which detect short-wavelength light, to see the world around them.
It is important to note that individuals with BCM do not see the world in just one color, blue. Instead, they see the world in shades of blue, yellow, and gray without perceiving red, green, or other distinct colors. This significantly impacts their ability to distinguish colors, recognize faces, and perform tasks that rely on color vision, such as driving.
Blue cone monochromacy (BCM) is caused by mutations in the OPN1LW and OPN1MW genes found on the X chromosome. These genes encode proteins that are needed in the process of converting light into electrical signals that the brain uses for visual processing. The proteins are called L- and M-cone opsins, which play a crucial role in this process.
When there are mutations in these genes, the L- and M-cone opsins' structure and function can be affected. This impairment can result in a loss of L- and M-cones or in their dysfunction. The loss of Land M-cones or their dysfunction compromises the power of the retina to distinguish colors and process visual information accurately.
WilliamA.Haseltine,PhD 267
Treatments
While there is no cure for color blindness, several devices and products can assist individuals in experiencing more enhanced and nuanced color vision.
Tinted glass lenses are a wearable device that is the most commonly used corrective device for color deficiencies. The lenses work by selectively filtering out specific wavelengths of light, enhancing color contrast, and improving perception. By doing so, the lenses enable individuals to distinguish between previously indistinguishable colors.
One of the most popular of these devices is the EnChroma glasses, which employ a special filter to intensify the perception of red and green colors (Enchroma, n.d.). The glasses work by blocking specific wavelengths of light and amplifying others, making colors appear more vibrant and distinct.

SOURCE: KK99LIUC on Wikimedia Commons
BetterEyesight 268
FIGURE 73: Visual of how EnChroma and other color blind lenses work
Another product that can be helpful for people with color blindness is ColorLite (ColorLite, n.d.). This software program modifies the colors on a computer screen to make them more distinguishable. The software adjusts the color contrast of text, images, and videos, making it easier for people with color blindness to distinguish between colors.
While these lenses are effective, they are not a permanent solution. Additionally, they can be inconvenient since they must be worn regularly to maintain effectiveness. Despite these limitations, tinted glasses remain a popular option for individuals with color blindness who want to improve their color perception.
Recent technological advances have led to the use of contact lenses that incorporate special filters (Badawy et al., 2018). These filters selectively block specific wavelengths of light, enhancing the ability of individuals with CVD to differentiate between colors. The filters can be customized to each individual's needs, allowing for a more personalized approach to correcting CVD.
Compared to tinted glasses, contact lenses are more comfortable and less obtrusive. They provide a more natural viewing experience since they sit directly on the eye rather than in front of it. Additionally, contact lenses can be worn during sports or other physical activities where glasses might be less practical.
With the advent of 3D printing technology, researchers and clinicians are developing new and innovative ways to address the needs of those suffering from color blindness.
Researchers from Khalifa University have developed a new technique that involves creating a contact lens with a unique design that can help correct color blindness (Salih et al., 2023). The lens
WilliamA.Haseltine,PhD 269
filters out specific wavelengths of light to enhance contrast between colors, much like how the glasses lenses work. This innovative approach has significant potential to change the lives of those suffering from color blindness.
Creating contact lenses to correct color blindness is a complex and fascinating process that requires specialized knowledge and skills. The first step involves using a 3D printer to create a mold of the contact lens. This mold is then filled with a technical organic material developed to correct different types of color blindness. The material is carefully selected based on its optical properties and ability to adhere to the mold surface.
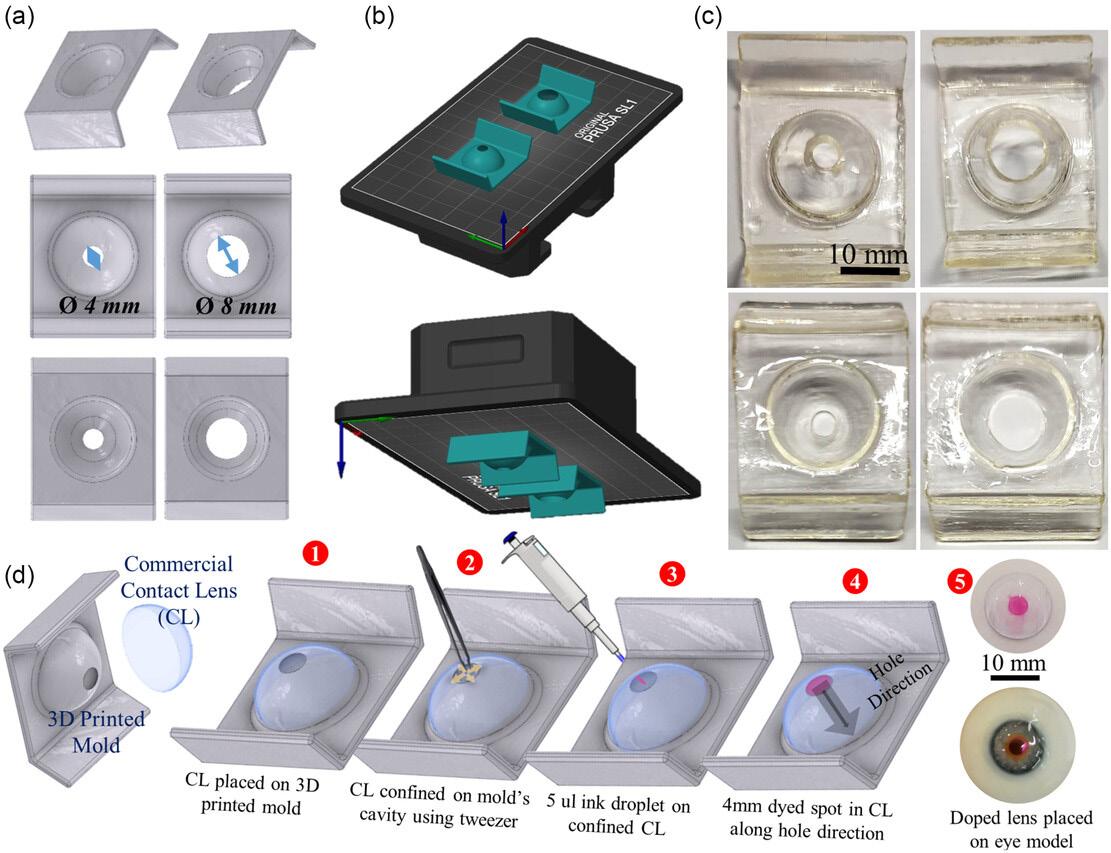
BetterEyesight 270
FIGURE 74: a) First, the molds for the contact lenses are designed using computer-aided design (CAD) software. b) Then, the design is sliced, and print parameters are adjusted for the 3D printing process. c) Digital photos show the 3D-printed molds with different hole sizes. d) The commercial contact lenses are tinted using a specific method: the lens is
placed in the mold with its center aligned (1), a portion of the lens is confined using a tweezer (2), and 5 μL of ink is deposited on this confined area (3). The spot is left to dry for 10 min before the final tinted lens is ready for display or testing on an eye model. (4-5)
SOURCE: © 2023 The Authors. Advanced Engineering Materials published by Wiley-VCH GmbH
The next step is to cure the material by exposing it to heat or UV light. The curing process ensures that the material retains its shape and properties and is firmly attached to the mold surface. Once the material has cured, the mold is removed, leaving behind a solid piece of the color-correcting material with the shape of the contact lens.
The final step is to polish the lens to a smooth finish. This involves using specialized tools and techniques to remove any imperfections and to create a lens surface that is perfectly smooth and transparent. This process is critical to ensure the lens provides clear and accurate vision. The result is a custom-designed contact lens tailored to the individual's eye.
Recent studies have shown promising results for 3D-printed contact lenses as a solution for color blindness. One study by the Journal of Macromolecular Materials and Engineering investigated using 3Dprinted hydrogel contact lenses with embedded color-correcting dyes (Saba Hittini et al., 2023). The study found that the lenses effectively improved color vision in individuals with red-green color blindness.
Another study published in ACS Biomaterials Science & Engineering focused on developing tunable light-filtering technology for 3D-printed contact lenses (Muhammed Hisham et al., 2023). The study found that by incorporating pH-sensitive dyes
WilliamA.Haseltine,PhD 271
into the lenses, the colors perceived by the wearer could be adjusted based on the pH level of their tears. This technology can potentially provide personalized color correction tailored to each individual's needs.
However, it's important to note that these lenses are currently only tailored to specific types of color blindness. Therefore, individuals with different color deficiencies may not benefit from this technology. Furthermore, these lenses are still in the experimental stages and are unavailable commercially.
The development of 3D-printed contacts for color blindness is a significant milestone in personalized care. These contacts can potentially revolutionize how we treat color blindness, offering a more effective and customized solution. This is a step forward in the right direction. With further development and refinement, 3Dprinted contacts can become a widely adopted solution for color blindness.
3D contacts aren’t the only contacts making progress in treating color blindness.
Gold contacts are a promising new development that offers hope for those seeking a more effective treatment
Gold is highly suitable for making contact lenses because it is biocompatible and has excellent optical properties. Researchers have used these properties to create gold nanocomposite contact lenses that incorporate gold nanoparticles into the contact lens matrix. These gold nanoparticles are engineered to selectively filter out specific wavelengths of light, which can help improve color differentiation and perception in individuals with color vision deficiency (CVD).
BetterEyesight 272
A recent study was published in ACS Nano to investigate the efficacy of these gold nanocomposite contact lenses in treating color blindness (Salih et al., 2021). The study recruited participants with CVD to wear gold contact lenses and complete various color-related tasks. The study showed that the gold contact lenses significantly improved color discrimination in individuals with mild to moderate color blindness. Furthermore, the contact lenses were well-tolerated and had no adverse effects.

FIGURE 75:
SOURCE: Copyright © 2021 American Chemical Society.
273
WilliamA.Haseltine,PhD
(a) transmission spectra of the nanocomposites; (b) solutions before polymerization (scale: 10 mm); (c) steps in polymerizing the solutions and obtaining the lenses; (d) polymerized lenses at different nanoparticle concentrations (scale: 10 mm).
While the results of this study are promising, some limitations need to be addressed. Firstly, the study's sample size was relatively small. Therefore, further research with a larger sample size is necessary to ensure the effectiveness of gold contacts. Additionally, the study only focused on individuals with mild to moderate CVD, and it remains to be seen if these contacts will be effective in individuals with severe CVD.
Despite these limitations, gold nanocomposite contact lenses represent an exciting development in CVD correction. With further research and development, these lenses could provide a more natural and permanent solution for color blindness.
Furthermore, this research opens the possibility of developing other nanocomposite materials to correct visual impairments. For example, these materials could create contact lenses that correct visual acuity or sharpness. The potential applications of nanocomposite materials in the field of ophthalmology are vast and exciting, and it will be fascinating to see how the area develops in the future.
Gene therapy is another potential treatment option for color blindness. Researchers have used gene therapy to restore color vision in monkeys and have made significant strides in developing a treatment for humans. The therapy involves using viral vectors to introduce the correct genes to the retina to replace the malfunctioning ones.
Advantages of these treatments include potentially restoring or enhancing color vision, which could significantly improve the quality of life for affected individuals. A recent West Virginia University study evaluated gene therapy's safety and efficacy as a
BetterEyesight 274
potential cure for blue cone monochromacy (BCM) (Sechrest et al., 2023), a spiritual successor to a similar treatment conducted on monkeys in 2009 (Science, 2009).
This previous therapy involved using a virus to deliver the red-green opsin gene to the retinas of squirrel monkeys born entirely colorblind. According to the results, the monkeys gained full-color vision within weeks after receiving treatment.
Fast forward to the present day, and the groundwork laid out by the monkey study paved the way for this recent research exploring gene therapy for BCM. For this study, a virus containing a functional copy of the blue cone photopigment gene was delivered to the retinas of two BCM patients. While the trial was small-scale and limited to a six-month follow-up period, the results were highly encouraging. Both patients experienced significant improvements in color vision, visual acuity, and light sensitivity.
Another study by Adverum Biotechnologies also focused on gene therapy options for BCM (Hanna et al., 2023). It used ADVM-062, a vector optimized for cone-specific expression of human L-opsin. Unlike existing therapies that involve subretinal vector injection, ADVM-062 can be administered using a single intravitreal (IVT) injection, which poses less risk to the central retinal structure of BCM patients.
WilliamA.Haseltine,PhD 275

SOURCE: © 2023 Adverum Biotechnologies Inc.
Preclinical studies have demonstrated that ADVM-062 effectively transduces gerbil cone photoreceptors and produces a de novo response to long-wavelength stimuli. In non-human primates, ADVM-062 showed cone-specific expression and transduction of foveal cones at specific doses. These findings hold promise for developing a safe and effective treatment for this debilitating and rare disease.
It is important to note that although gene therapy results offer hope for those with BCM, this technology is still in its early stages of development and requires further research to ensure its safety and
BetterEyesight 276
FIGURE 76: The Process of Gene Therapy for BCM.
long-term effectiveness in treating inherited genetic diseases. Nevertheless, this research is a significant advance in gene therapy. It demonstrates the potential of this technology to cure genetic diseases that were previously thought to be untreatable.
Color Blindness Due to Retinitis Pigmentosa
Color blindness is a visual deficiency that impairs the ability to distinguish specific colors. This condition can become an independent ailment or a result of retinal diseases such as retinitis pigmentosa (RP). It is a degenerative disease that progressively destroys the light-sensitive cells in the retina, leading to varying levels of vision loss.
Retinitis pigmentosa is a disease that can cause total blindness over time. The disease affects the cells in the retina that detect light and color and can lead to color blindness. As the disease progresses, the person's vision can become more limited, resulting in "tunnel vision," where only a tiny circle in the center of their vision is visible. Color blindness and other visual impairments caused by retinitis pigmentosa can also occur.
Retinal implants have recently gained attention as a potential treatment for RP-induced color blindness. These implants restore vision by bypassing the non-functioning photoreceptor cells and stimulating the remaining functional cells. While they are not perfect solutions for individuals with color blindness as a primary disorder, they show promising results in treating retinitis pigmentosa, which can cause it in its advanced stages.
Retinal implants have emerged as a revolutionary treatment option for various retinal diseases, including retinitis pigmentosa (RP), an
WilliamA.Haseltine,PhD 277
inherited disorder that causes blindness. These devices can replace the functions of deteriorated phototransducing cells present in the retina.
Two major types of retinal implants have been developed: bioelectronic and photovoltaic. Bioelectronic implants capture light from an image, transform it into electrical impulses, and transmit it to the remaining cells in the retina. This type of implant is designed to stimulate the inner retinal neurons and has shown promising results in restoring partial vision in patients. These bioelectronic implants convert visual information into electrical signals that the brain can interpret, bypassing the damaged cells in the retina.
The second type of implant, photovoltaic retinal prostheses, employs light as the source of stimulation. These prostheses can potentially restore high-resolution responses to single-pixel stimulation in blind retinas. Photovoltaic implants use tiny solar cells to power up the implant and stimulate the retina, which enables color vision. Photovoltaic implants also involve fewer electrical wires and lower energy requirements, which allows them to operate for longer durations without disturbing the patient's comfort levels.
Regarding color blindness, photovoltaic retinal implants have the edge over bioelectronic implants. As the latter relies on detecting electrical impulses and transmitting them to the brain, it may not be as effective in restoring normal color vision in those with vision impairments. On the other hand, the photovoltaic implant efficiently converts light energy into electrical energy, stimulating the remaining healthy cells in the retina and restoring color vision entirely.
BetterEyesight 278
Numerous studies have explored the feasibility of using electrical stimulation strategies to provide chromatic information to patients to partially restore color perception. These studies have shown promising results and could significantly improve the quality of life.

B-C: These fundus images are from the implant eye of Subject 4 (B) and Subject 5 (C), who reported blue/purple sensations at higher stimulation frequencies.
D-E: These images are from the implanted eye of Subject 6 (D) and Subject 7 (E), who did not report blue/purple sensation at higher stimulation frequencies.
F: The perceptual threshold of 19 electrodes in blue-sensing subjects versus 15 in non-blue-sensing subjects. This suggests that individual differences in perception may be related to electrode placement.
SOURCE: © 2020 by the American Academy of Ophthalmology
WilliamA.Haseltine,PhD 279
FIGURE 77: A: This image shows the placement of an intraocular implant in Subject 3's eye, with a close-up of the retinal area near the electrode array.
A study published in ScienceDirect found that electrical stimulation of the retina of blind RP patients resulted in the restoration of partial color vision, specifically along the blue-yellow axis (Yue et al., 2021). The researchers used a retinal implant that delivered controlled electrical currents to the residual inner retina, which allowed the perception of chromatic content. The study involved 12 patients; all reported seeing blue-yellow colors after activating the retinal implant. Although the restored vision was imperfect, the researchers were encouraged by the results and believed this technology could improve prosthetic eyes for RP patients.
The second study, published in Nature, explored using a photovoltaic retinal prosthesis to restore high-resolution responses in blind retinas (Chenais et al., 2021). The researchers created a photovoltaic pixel measuring 0.1mm², implanted onto the retina to stimulate the remaining cells. The study involved five blind patients. All reported seeing flashes of light when the photovoltaic pixel was activated. The researchers found that the responses to the single-pixel stimulation were high-resolution, indicating that the photovoltaic prosthesis could be an effective treatment option for RP patients.
However, despite the potential benefits of retinal implants in partially restoring color perception in RP patients, the current success rate is still limited. Certain device risks associated with retinal implants include overstimulation, which could cause damage to the retina, and the delamination of implanted components. Additionally, previous retinal implants have produced poor results, and wearers are still considered legally blind.
BetterEyesight 280
More research and development are necessary to enhance the efficacy of retinal implants for color blindness in RP patients. Innovative implant technologies could provide alternative or supplementary methods to current retinal implants.
Night Blindness
Imagine sitting in a movie theater, waiting for the movie to start. As the lights dim and the trailers begin, you start feeling anxious. The darkness envelops you, and you realize you can hardly see the screen before you. Every time the scene fades to black, you frantically search for any source of light.
This is the reality for people with night blindness. This condition deprives people of their ability to see in low-light conditions. However, night blindness is not limited to movie theaters; it affects tasks like driving at night or walking after dusk.
Nyctalopia, commonly known as night blindness, is a condition that affects an individual's eyesight in low or dim light conditions. This makes it challenging to see clearly in the dark, leading to difficulties driving or moving around in low-light settings. Night blindness is a relatively rare genetic condition, with an estimated prevalence of 1 in 7,000 to 10,000 individuals in the US (Elsevier, n.d.).
Despite the challenges of night blindness, there is hope for those living with this condition. Scientists have been working on gene therapies to help improve the vision of those affected by night blindness. These gene therapies are a promising solution because they target the genetic mutations that cause night blindness rather than treating symptoms.
WilliamA.Haseltine,PhD 281
Night blindness is a condition that affects a person's ability to see in low-light conditions, which can make it challenging to navigate in the dark. The condition is caused by mutations in the genes responsible for producing the photoreceptor rods in the retina.
Photoreceptor rods are cells located in the retina and responsible for detecting light. These cells are essential in low-light conditions as they help us see in the dark. However, individuals with night blindness cannot produce enough of these cells or have defective rods, which results in poor night vision.
Several underlying factors, such as vitamin A deficiency or retinitis pigmentosa, can cause this condition (Mehra & Le, 2020). Vitamin A is a crucial nutrient for producing rhodopsin, a protein found in photoreceptor rods in the eye that enables us to detect light. Without enough vitamin A, the production of rhodopsin is impaired, causing defective rhodopsin in individuals with night blindness, which makes it hard for them to see in low-light conditions.

FIGURE 78: Rhodopsin structure and crystals.
SOURCE: Copyright © 2013 Elsevier, Inc.
BetterEyesight 282
Rhodopsin is a protein found in the eye's retina that is critical for vision (Palczewski, 2014). It consists of a molecule called retinal, which is bound to a protein called opsin. When light enters the eye and strikes the retina, it undergoes a chemical reaction that causes a change in the shape of the retinal. This change in form triggers a cascade of events that ultimately leads to the generation of an electrical signal transmitted to the brain via the optic nerve. The brain interprets this signal as visual information, allowing us to see the world around us.
Treatments
One of the most effective treatments is vitamin A supplementation (Mehra & Le, 2020). This treatment is particularly effective for those whose night blindness is caused by a deficiency of this essential nutrient. Vitamin A plays a crucial role in the retina's function and is responsible for vision in dim light (Clifford et al., 2013). Therefore, supplementing with vitamin A can improve night vision and alleviate the symptoms of night blindness. For people with a genetic form of night blindness, taking vitamin A supplements may not be a practical solution. In such cases, other alternatives, like night vision aids, can be considered. Night vision aids, such as goggles or glasses, amplify the available light, making it easier to see in low-light conditions. These devices can be helpful for those who work in low-light environments or enjoy outdoor activities at night. However, it's important to note that while night vision aids can be effective, they can also be expensive and challenging to wear.
Researchers are currently exploring new treatments to tackle this condition to improve night vision in affected individuals. One such
WilliamA.Haseltine,PhD 283
treatment option is gene therapy, which involves introducing healthy genes into the body to replace the faulty ones responsible for night blindness. Early-stage trials have shown that gene therapy has a lot of potential to improve night vision (Botto et al., 2022), with some individuals experiencing a significant improvement in their eyesight. However, this treatment is still in its infancy and requires further study before it can be widely available.
Stem cell therapy is also currently being explored as a potential treatment option for this condition. This therapy involves using stem cells to develop new rods in the retina, which can potentially restore night vision in affected individuals. Although this treatment option is still in its early stages of development, it has shown promising results in animal studies (Neuroscience News, 2023).
New treatment options bring a promising outlook for treating night blindness. As research continues to advance, there is a positive outlook that better treatment options will become available, ultimately improving the quality of life for individuals suffering from night blindness.
BetterEyesight 284
Ocular Toxoplasmosis

Ocular toxoplasmosis may not be a term that immediately comes to mind when one thinks of eye infections. Still, it is a prevalent condition responsible for posterior uveitis and potential vision loss. Caused by the parasite Toxoplasma gondii, this infection can be acquired through contaminated soil, water, food, and even from infected cats and rodents.
The conventional therapy for this infection has been known for its severe adverse effects and toxicity (Ozgonul & Besirli, 2016), making alternative therapies a critical and compelling area of research. This article will explore the emerging alternative therapies for ocular toxoplasmosis, including intravitreal therapy and singleagent treatment with trimethoprim-sulfamethoxazole, and their potential to transform the treatment landscape for this debilitating eye condition.
Ocular toxoplasmosis is an infection caused by the protozoan parasite Toxoplasma gondii. One of the most common causes of posterior uveitis is inflammation in the layer of tissue at the back of the eye. Ocular toxoplasmosis may first affect only one eye. However, it can come back and affect both eyes.
285
CHAPTER 15

FIGURE 79: a Fundus photograph of active ocular toxoplasmosis chorioretinitis. b Resolved vitritis and resolving lesion two weeks after starting dual therapy with trimethoprim-sulfamethoxazole and prednisone. c Fibrosis and vitreoretinal adhesion with a new focus of active retinitis closer to the fovea (white arrow).
SOURCE: © 2016 S. Karger AG, Basel
The condition typically presents as necrotizing retinochoroiditis, an inflammation affecting both the retina and choroid, the two layers of tissue that comprise the back of the eye.
Studies have shown that approximately 50% of patients with ocular toxoplasmosis develop uveitis (Kalogeropoulos et al., 2021), which is a common complication of the condition. Uveitis is an inflammation of the uvea, the middle layer of tissue in the eye that contains the blood vessels that supply the retina. In some cases, uveitis can cause permanent damage to the eye, leading to vision loss.
Treatments
The conventional therapy for this infection involves oral pyrimethamine, sulfadiazine, and a systemic corticosteroid. Pyrimethamine is an anti-parasitic agent that aims to arrest the multiplication of the parasite during the active period of retinochoroiditis, while sulfadiazine has a complementary role in
BetterEyesight 286
the treatment. However, this conventional combination therapy has the downside of causing severe adverse effects and toxicity, making it a less desirable option.
To address this issue, multiple studies have been conducted to find alternative therapies for ocular toxoplasmosis. A systematic review and meta-analysis published by the Journal of the Brazilian Society of Tropical Medicine (Amaral et al., 2023) supports alternative treatment regimens for ocular toxoplasmosis. The article discusses the limitations of the common oral combination therapy and the benefits of locally delivered drugs to treat the condition. It also mentions that oral sub-doses of trimethoprim-sulfamethoxazole can reduce the recurrence of ocular toxoplasmosis.
Over the past few years, there has been a marked increase in the research on intravitreal therapy (Melo et al., 2023). This approach involves the direct injection of medication into the eye, allowing for more targeted treatment and fewer systemic side effects that can affect the whole body.
Combining clindamycin with dexamethasone has received the most attention among the studied regimens. This particular regimen has been extensively researched, and the results have been promising (Abdala & Muñoz, 2014). Clindamycin is a broadspectrum antibiotic that is effective against many types of bacteria. At the same time, dexamethasone is a steroid that helps reduce inflammation and swelling.
When used together, these medications have been shown to effectively treat various ocular conditions, including endophthalmitis, uveitis, and retinal vein occlusion (American Academy of Ophthalmology, 2011). Moreover, the combination is
WilliamA.Haseltine,PhD 287
associated with fewer complications and improved safety compared to other treatments.
In addition to intravitreal therapy, different alternative therapeutic regimens have emerged as effective in the treatment of ocular toxoplasmosis. These alternative regimens have shown promising results in effectively managing the condition. One such option is single-agent treatment with trimethoprim-sulfamethoxazole. This treatment effectively prevents disease recurrences and is beneficial in long-term management.
It is worth noting that trimethoprim-sulfamethoxazole is a sulfa drug combination that is used to treat a wide range of bacterial infections. It works by inhibiting the growth of bacteria by blocking the production of folic acid, which is essential for the bacteria to multiply and survive. In the case of ocular toxoplasmosis, this treatment has proven effective in reducing the severity of the condition and preventing it from recurring.
In light of the challenges posed by the severe adverse effects of conventional therapy for ocular toxoplasmosis, there is a growing need for alternative treatment options that are safer, more tolerable, and more effective. Fortunately, recent research has shown great promise in intravitreal therapy and other alternative therapeutic regimens, such as single-agent treatment with trimethoprimsulfamethoxazole.
These emerging therapeutic options represent a significant breakthrough in ocular toxoplasmosis management and hold great promise for the future. With continued research and development in this field, there is every reason to believe that the outlook for
BetterEyesight 288
ocular toxoplasmosis will continue to improve, ultimately leading to a brighter future for patients suffering from this condition.
WilliamA.Haseltine,PhD 289
CHAPTER 16
Uveitis

Uveitis is a type of eye inflammation that affects the middle layer of tissue in the eye wall called the uvea. This disorder can occur suddenly, and symptoms may worsen quickly, affecting one or both eyes. The signs and symptoms of uveitis can include eye redness, pain, light sensitivity, blurred vision, floaters, and decreased vision.
Approximately half of all cases of uveitis are of unknown origin. In contrast, the other half may be related to autoimmune or inflammatory disorders such as systemic lupus erythematosus, sarcoidosis, or Crohn's disease.
Uveitis is a complex medical condition that causes inflammation in different eye parts, leading to a wide range of symptoms that can significantly impair vision and quality of life. There are four main categories of uveitis, each with unique signs and complications.

290
FIGURE 80: patient with uveitis
SOURCE: Anastassiya Bezhekeneva
The most common type of uveitis is anterior uveitis, which affects the iris and ciliary body at the front of the eye. This type of uveitis, also known as iritis, is characterized by eye pain, redness, sensitivity to light, and blurred vision. Sometimes, the pupil may become smaller and irregular, leading to vision problems.
Intermediate uveitis affects the vitreous and the retina at the back of the eye, and it's often associated with systemic diseases such as sarcoidosis or multiple sclerosis. This uveitis can cause floaters, blurred vision, and difficulty seeing in low-light conditions. It can lead to retinal detachment and permanent vision loss in severe cases.
Posterior uveitis affects the choroid, retina, and optic nerve at the back of the eye, and it's often caused by infections or autoimmune diseases such as toxoplasmosis, herpes, or Behcet's disease. This type of uveitis can cause a gradual loss of vision, floaters, and sensitivity to light. In some cases, it can also lead to macular edema, scarring, or retinal detachment.
Finally, panuveitis affects all parts of the uvea, from the front to the back of the eye. This type of uveitis is often the most severe. It can cause a wide range of symptoms, including pain, redness, blurred vision, floaters, and photophobia. Panuveitis is often associated with systemic autoimmune diseases such as lupus, rheumatoid arthritis, or sarcoidosis, and it can lead to severe complications such as glaucoma, cataracts, or retinal detachment.
WilliamA.Haseltine,PhD 291
Treatments
As uveitis can cause severe complications that lead to permanent vision loss, early diagnosis and treatment are essential. Therapy aims to treat the inflammation and check the eyes regularly to prevent further damage and vision loss. Ophthalmologists typically prescribe eye-drop medications that reduce inflammation and dilate the pupil. In some cases, injections or pills may also be necessary. While these treatments can effectively control symptoms, they do not adequately relieve severe cases.
Several hydrogel formulations have been researched for their potential use in treating uveitis because of their unique biodegradability properties, biocompatibility, and ability to sustain drug release. Hydrogels are polymeric materials that absorb and retain water, making them an ideal carrier for therapeutic agents. Moreover, these hydrogels can also provide sustained release of therapeutic agents, resulting in longer-lasting treatment effects and a reduced need for frequent dosing.

SOURCE: Journal of Materials Chemistry B
A recent study published in the Journal of Materials Chemistry B investigated the potential of using an injectable, thermo-sensitive and biodegradable in situ hydrogel to deliver indomethacin to treat uveitis (Zou et al., 2019). The hydrogel exhibited good biocompatibility and sustained release of indomethacin for over two
BetterEyesight 292
FIGURE 81: Example of Hydrogels releasing drugs
weeks. However, the study was limited to in vitro testing. It only evaluated the hydrogel's ability to release indomethacin over two weeks. The study did not examine the hydrogel's impact on other ocular tissues or the eye as a whole. Therefore, further research is needed to determine any potential side effects before it can be used as a treatment option for uveitis.
Researchers from Nantong University also recently studied using hydrogels made from γ-cyclodextrin for treating anterior uveitis by delivering flurbiprofen to the eyes (Fang, Wang, et al., 2022). The study found that the hydrogels improved the anti-inflammatory effects of flurbiprofen when given to rabbits. Still, it is essential to note that the study only tested on rabbits, and the length of the study did not allow for long-term effects to be evaluated.

SOURCE: Carbohydrate Polymers
WilliamA.Haseltine,PhD 293
FIGURE 82: Preparation of γ-cyclodextrin-based polypseudorotaxane hydrogels and topical delivery of FLB to treat anterior uveitis.
Multifunctional hydrogel eye drops have also been investigated for treating uveitis through synergistic therapy mechanisms. Synergistic therapy mechanisms refer to the combined effects of multiple therapeutic agents that work together in a complementary fashion to enhance the overall therapeutic outcome. Simply put, it is the idea that two or more medications or substances can work together to produce a more significant effect than what would be possible if they were used alone.
A recent study in The American Chemical Society's Nano Journal has shown that hydrogel eye drops with multiple functions can effectively alleviate uveitis (Li, Chen, et al., 2023). To test the hydrogel eye drops, researchers induced uveitis in mice and administered the drops. The results showed that the eye drops significantly reduced inflammation and prevented the formation of cataracts. The hydrogel eye drops achieved this by slowly releasing therapeutic agents, which provided long-lasting relief to the eyes. Additionally, the eye drops targeted only the inflamed areas of the eye, reducing the risk of side effects that can happen with other treatments.
However, it is essential to note that the study was conducted on animals. It still needs to be determined if the hydrogel eye drops will also work in humans. More research is necessary to confirm their safety and effectiveness for human use.
When treating noninfectious uveitis, corticosteroids are often used as the primary medication. These drugs help reduce the release of inflammatory chemicals that cause the condition. Still, they can also disrupt the immune system, causing side effects like cataracts, glaucoma, and an increased risk of infections (Yasir & Sonthalia, 2019).
BetterEyesight 294
To mitigate these risks, other medications are often combined with corticosteroids to lower the dosage and duration of treatment. For instance, immunosuppressive drugs may be used to reduce the activity of the immune system, thereby reducing the inflammation caused by the condition. Additionally, nonsteroidal antiinflammatory drugs (NSAIDs) may be used to relieve pain and inflammation.
Recent advances in pharmacological strategies have led to new treatments targeting the molecules responsible for inflammation.
Biological agents are particularly effective in treating noninfectious uveitis. These agents target specific molecules involved in the inflammatory process, reducing the overall inflammatory response. Some biological agents to treat noninfectious uveitis include tumor necrosis factor (TNF) inhibitors, interleukin (IL)-6 inhibitors, and IL-1 inhibitors.
TNF inhibitors block TNF's activity, a molecule produced by immune cells that plays a vital role in the inflammatory response. Similarly, IL-6 and IL-1 inhibitors target IL-6 and IL-1, which are also involved in the inflammatory process. By specifically targeting these molecules, these biological agents can effectively reduce inflammation and improve the symptoms of noninfectious uveitis.
These agents have effectively controlled inflammation and reduced corticosteroid dependency (Valenzuela et al., 2020). However, they can be expensive and carry potential side effects, including an elevated risk of infection and malignancy.
Noninfectious uveitis can be managed using different types of medication. These include corticosteroids, biologic agents, and immunosuppressants like methotrexate and mycophenolate
WilliamA.Haseltine,PhD 295
mofetil. These medications suppress the immune system and are often used with corticosteroids to reduce their dosage. Methotrexate and mycophenolate mofetil have been proven effective in controlling inflammation (National Eye Institute, 2019b). However, it's essential to consider their potential side effects, such as liver toxicity and increased susceptibility to infections.
Surgery can be used for both diagnostic and therapeutic purposes. For instance, if uveitis leads to the formation of cataracts, surgery may be necessary to remove them. Similarly, suppose fluid buildup in the eye causes pressure. Surgery may be required to relieve this pressure and prevent further damage (Hassman et al., 2017).
Laser therapy is a focused treatment that can help with specific issues related to uveitis. This therapy can treat cystoid macular edema and neovascularization, two complications that can result from uveitis. In the case of cystoid macular edema, laser therapy can reduce swelling and fluid leakage in the macula, an integral part of the retina responsible for central vision. Laser therapy can also prevent the growth of abnormal blood vessels in the eye that can cause bleeding or scarring (Hassman et al., 2017).
When it comes to treating uveitis, there are several factors to consider, such as the root cause of the inflammation, the severity of the condition, and the overall health status of the patient. Sometimes, a combination of treatments may be necessary to achieve the best possible outcome. The primary goals of uveitis treatment are to preserve vision, manage inflammation, and minimize any side effects associated with therapy.
BetterEyesight 296
To avoid the long-term side effects of commonly used corticosteroids in treating uveitis, alternative medications like biological agents are becoming increasingly popular. These medications can help preserve vision while reducing the risk of side effects.
WilliamA.Haseltine,PhD 297
References

Dart, J. K., Papa, V., Rama, P., Knutsson, K. A., Ahmad, S., Hau, S., ... & Minassian, D. C. (2023). The Orphan Drug for Acanthamoeba Keratitis (ODAK) Trial: PHMB 0.08%(Polihexanide) and Placebo versus PHMB 0.02% and Propamidine 0.1%. Ophthalmology .
Genetic and Rare Diseases Information Center. (2016). Bluecone monochromatism|GeneticandRareDiseasesInformation Center(GARD) – an NCATSProgram . Nih.gov. https://rarediseases.info.nih.gov/diseases/917/blue-conemonochromatism
Heidar, K. Cataracts in Children, Congenital and Acquired. American Academy of Ophthalmology. 2017.
Infant Aphakia Treatment Study Group, Lambert, S. R., Buckley, E. G., Drews-Botsch, C., DuBois, L., Hartmann, E., Lynn, M. J., Plager, D. A., & Wilson, M. E. (2010). The infant aphakia treatment study: design and clinical measures at enrollment. Archivesofophthalmology(Chicago,Ill.:1960) , 128(1), 21–27. https://doi.org/10.1001/archophthalmol.2009.350
Leger, A. J. S., Desai, J. V., Drummond, R. A., Kugadas, A., Almaghrabi, F., Silver, P., ... & Caspi, R. R. (2017). An ocular commensal protects against corneal infection by driving an interleukin-17 response from mucosal γδ T cells. Immunity , 47(1), 148-158.
L V Prasad Eye Institute . (2022). Lvpei.org. https://www.lvpei.org/
298
Abdala, C. A., & Muñoz, M. P. (2014). INTRAVITREAL CLINDAMYCIN AND DEXAMETHASONE FOR OCULAR TOXOPLASMOSIS. InvestigativeOphthalmology &VisualScience , 55(13), 2849–2849.
https://iovs.arvojournals.org/article.aspx?articleid=2268215
Abdelnour, S. A., Xie, L., Hassanin, A. A., Zuo, E., & Lu, Y. (2021). The Potential of CRISPR/Cas9 Gene Editing as a Treatment Strategy for Inherited Diseases. Frontiers in Cell andDevelopmentalBiology , 9 .
https://doi.org/10.3389/fcell.2021.699597
Abhilasha, & Harvard University. (2013, December 8). Aravind Eye Care’sGrandVisionforIndia . Technology and Operations Management. https://d3.harvard.edu/platformrctom/submission/aravind-eye-cares-grand-vision-for-india/
Abramoff, M. D., Garvin, M. K., & Sonka, M. (2010). Retinal Imaging and Image Analysis. IEEEReviewsinBiomedical Engineering , 3 , 169–208.
https://doi.org/10.1109/rbme.2010.2084567
Adelson, J. D., Bourne, R. R. A., Briant, P. S., Flaxman, S. R., Taylor, H. R. B., Jonas, J. B., Abdoli, A. A., Abrha, W. A., Abualhasan, A., Abu-Gharbieh, E. G., Adal, T. G., Afshin, A., Ahmadieh, H., Alemayehu, W., Alemzadeh, S. A. S., Alfaar, A. S., Alipour, V., Androudi, S., Arabloo, J., & Arditi, A. B. (2021). Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the Right to Sight: an analysis for the Global Burden of Disease Study. TheLancet Global
WilliamA.Haseltine,PhD 299
Health , 9(2), e144–e160. https://doi.org/10.1016/S2214109X(20)30489-7
Aggarwal, R., Sounderajah, V., Martin, G., Ting, D. S. W., Karthikesalingam, A., King, D., Ashrafian, H., & Darzi, A. (2021). Diagnostic accuracy of deep learning in medical imaging: a systematic review and meta-analysis. NpjDigital Medicine , 4(1).
https://doi.org/10.1038/s41746-021-00438-z
Ainhoa Molina‐Martín, Leal-Vega, L., Dolores, Martínez-Plaza, E., María Begoña Coco-Martín, & Piñero, D. P. (2023). Amblyopia Treatment through Immersive Virtual Reality: A Preliminary Experience in Anisometropic Children. Vision , 7(2), 42–42.
https://doi.org/10.3390/vision7020042
Akter, N., Fletcher, J., Perry, S., Simunovic, M. P., Briggs, N., & Roy, M. (2022). Glaucoma diagnosis using multi-feature analysis and a deep learning technique. ScientificReports , 12(1).
https://doi.org/10.1038/s41598-022-12147-y
AlajbegovicHalimic, J., Zvizdic, D., AlimanovicHalilovic, E., Dodik, I., & Duvnjak, S. (2015). Risk Factors for Retinopathy of Prematurity in Premature Born Children. MedicalArchives , 69(6), 409.
https://doi.org/10.5455/medarh.2015.69.409-413
Allison, K., Patel, D., & Alabi, O. (2020). Epidemiology of Glaucoma: The Past, Present, and Predictions for the Future. Cureus , 12(11).
https://doi.org/10.7759/cureus.11686
Amaral, L., Rodrigues, M., Fernandes-Cunha, G., Silva-Cunha, A., Paulo, M., & Sílvia Ligório Fialho. (2023). Clinical outcomes of intravitreal treatment for ocular toxoplasmosis: systematic review and meta-analysis. RevistaDaSociedade
BetterEyesight 300
BrasileiradeMedicinaTropical , 56 .
https://doi.org/10.1590/0037-8682-0552-2022
American Academy Of Ophthalmology. (2015, December 1). The Heart andtheEye:SeeingtheLinks . American Academy of Ophthalmology.
https://www.aao.org/eyenet/article/heart-eyeseeing-links
American Academy of Ophthalmology. (n.d.). Eye Health Statistics - AmericanAcademyofOphthalmology . Www.aao.org.
https://www.aao.org/newsroom/eye-healthstatistics#:~:text=Refractive%20Errors
American Academy of Ophthalmology. (2011, February 7). Intravitrealclindamycin,dexamethasoneappears a good alternativeto conventionaltherapyforoculartoxoplasmosis
American Academy of Ophthalmology.
https://www.aao.org/education/editors-choice/intravitrealclindamycin-dexamethasone-appears-goo
AMERICAN MIGRAINE FOUNDATION. (2019). TheFacts AboutMigraine . American Migraine Foundation.
https://americanmigrainefoundation.org/resourcelibrary/migraine-facts/
American Society of Retina Specialists. (n.d.). AnnualMeetingTheAmericanSocietyofRetinaSpecialists . Www.asrs.org. Retrieved November 29, 2023, from
https://www.asrs.org/annual-meeting
An, L., Catherine Lingxue Jan, Feng, J., Wang, Z., Zhan, L., & Xu, X. (2019). Inequity in Access: Cataract Surgery
Throughput of Chinese Ophthalmologists from the China National Eye Care Capacity and Resource Survey.
WilliamA.Haseltine,PhD 301
OphthalmicEpidemiology , 27(1), 29–38.
https://doi.org/10.1080/09286586.2019.1678654
Anilkumar, N., Weber, R., Zhang, M., Brewer, A., & Shah, A. M. (2008). Nox4 and Nox2 NADPH Oxidases Mediate Distinct Cellular Redox Signaling Responses to Agonist Stimulation. Arteriosclerosis,Thrombosis,andVascularBiology , 28(7), 1347–1354.
https://doi.org/10.1161/atvbaha.108.164277
Aravind Eye Care Systems. (n.d.). OurStory . Aravind Eye Care System. https://aravind.org/our-story/
Aravind Eye Care Systems. (2023). Activity Report 2022-2023. In online.pubhtml5.com .
https://online.pubhtml5.com/idml/xvjq/#p=18
Armitage, W. J., Goodchild, C., Griffin, M. D., Gunn, D. J., Hjortdal, J., Lohan, P., Murphy, C. C., Pleyer, U., Ritter, T., Tole, D. M., & Vabres, B. (2019). High-risk Corneal Transplantation. Transplantation , 103(12), 2468–2478.
https://doi.org/10.1097/tp.0000000000002938
Atalay, E., Özalp, O., & Yıldırım, N. (2021). Advances in the diagnosis and treatment of keratoconus. TherapeuticAdvances inOphthalmology , 13 , 251584142110127.
https://doi.org/10.1177/25158414211012796
Aumann, S., Donner, S., Fischer, J., & Müller, F. (2019). Optical CoherenceTomography(OCT):PrincipleandTechnical Realization(J. F. Bille, Ed.). PubMed; Springer.
https://www.ncbi.nlm.nih.gov/books/NBK554044/
Avidor, D., Loewenstein, A., Waisbourd, M., & Nutman, A. (2020). Cost-effectiveness of diabetic retinopathy screening
BetterEyesight 302
programs using telemedicine: a systematic review. Cost EffectivenessandResourceAllocation , 18(1).
https://doi.org/10.1186/s12962-020-00211-1
Azari, A. A., & Arabi, A. (2020). Conjunctivitis: A Systematic Review. JournalofOphthalmic&VisionResearch , 15(3), 372–395.
https://doi.org/10.18502/jovr.v15i3.7456
Badawy, A.-R., Hassan, M. U., Elsherif, M., Ahmed, Z., Yetisen, A. K., & Butt, H. (2018). Contact Lenses for Color Blindness. AdvancedHealthcareMaterials , 7(12), 1800152.
https://doi.org/10.1002/adhm.201800152
Basaldua, B. (2021, May 5). TheFuture ofCataractSurgery . IOR Partners | Office-Based Surgery. https://iorpartners.com/thefuture-of-cataract-surgery/
Baudouin, C., Messmer, E. M., Aragona, P., Geerling, G., Akova, Y. A., Benítez-del-Castillo, J., Boboridis, K. G., Merayo-Lloves, J., Rolando, M., & Labetoulle, M. (2016). Revisiting the vicious circle of dry eye disease: a focus on the pathophysiology of meibomian gland dysfunction. BritishJournalof Ophthalmology , 100(3), 300–306.
https://doi.org/10.1136/bjophthalmol-2015-307415
Baumann, B. (2017). Polarization Sensitive Optical Coherence Tomography: A Review of Technology and Applications. AppliedSciences , 7(5), 474.
https://doi.org/10.3390/app7050474
Bayba, M., & Huang, M. (2023, April 14). LASIKStatistics - Safety andSuccessRates in 2023 Vision Center.
https://www.visioncenter.org/resources/lasik-
WilliamA.Haseltine,PhD 303
statistics/#:~:text=LASIK%20surgery%20boasts%20a%20succes s
Beckers, H. J. M., Aptel, F., Webers, C. A. B., Bluwol, E., Martínez-de-la-Casa, J. M., García-Feijoó, J., Lachkar, Y., Méndez-Hernández, C. D., Riss, I., Shao, H., Pinchuk, L., Angeles, R., Sadruddin, O., & Shaarawy, T. M. (2021). Safety and Effectiveness of the PRESERFLO® MicroShunt in Primary Open-Angle Glaucoma. OphthalmologyGlaucoma .
https://doi.org/10.1016/j.ogla.2021.07.008
Begley, S. (2017, April 26). Cancer-causing DNAfoundin stem cellsusedinsome clinicaltrials . STAT.
https://www.statnews.com/2017/04/26/stem-cells-cancermutations/
Bernfeld, E., Feldman, B. H., Kozak, A., Door , W. T., Bunya, V. Y., Halfpenny, C., Hong, A., Ortiz-Morales, G., & Bernal, M. D. (2023, May 7). AcanthamoebaKeratitis - EyeWiki .
Eyewiki.aao.org.
https://eyewiki.aao.org/Acanthamoeba_Keratitis
Berry, V., Georgiou, M., Fujinami, K., Quinlan, R., Moore, A., & Michaelides, M. (2020). Inherited cataracts: molecular genetics, clinical features, disease mechanisms and novel therapeutic approaches. BritishJournalofOphthalmology , 104(10), 1331–1337.
https://doi.org/10.1136/bjophthalmol2019-315282
Bhavsar, A. R., Atebara, N. H., & Drouilhet, J. H. (2023). Diabetic Retinopathy: Practice Essentials, Pathophysiology, Etiology. EMedicine .
https://emedicine.medscape.com/article/1225122overview?form=fpf
BetterEyesight 304
Bi, A., Cui, J., Ma, Y.-P., Olshevskaya, E., Pu, M., Dizhoor, A. M., & Pan, Z.-H. (2006). Ectopic Expression of a Microbial-Type Rhodopsin Restores Visual Responses in Mice with Photoreceptor Degeneration. Neuron , 50(1), 23–33.
https://doi.org/10.1016/j.neuron.2006.02.026
Binenbaum, G., Chang, M. Y., Heidary, G., Morrison, D. G., Trivedi, R. H., Galvin, J. A., & Pineles, S. L. (2021). Botulinum Toxin Injection for the Treatment of Strabismus: A Report by the American Academy of Ophthalmology. Ophthalmology , 128(12), 1766–1776.
https://doi.org/10.1016/j.ophtha.2021.05.009
Binibrahim, I., & Bergström, A. (2017). The role of trabeculectomy in enhancing glaucoma patient’s quality of life. OmanJournalofOphthalmology , 10(3), 150.
https://doi.org/10.4103/ojo.ojo_61_2016
Birch, J. (2010). Worldwideprevalenceofred-green color deficiency Journal of the Optical Society of America. A, Optics, Image science, and vision. 29. 313-20. 10.1364/JOSAA.29.000313.
https://www.researchgate.net/publication/223985289_Worldwi de_prevalence_of_red-green_color_deficiency
Bossi, M., Tailor, V. K., Anderson, E. J., Bex, P. J., Greenwood, J. A., Dahlmann-Noor, A., & Dakin, S. C. (2017). Binocular Therapy for Childhood Amblyopia Improves Vision Without Breaking Interocular Suppression. InvestigativeOpthalmology &VisualScience , 58(7), 3031. https://doi.org/10.1167/iovs.1620913
WilliamA.Haseltine,PhD 305
Botto, C., Rucli, M., Tekinsoy, M. D., Pulman, J., Sahel, J.-A., & Dalkara, D. (2022). Early and late stage gene therapy interventions for inherited retinal degenerations. Progress in RetinalandEye Research , 86 , 100975.
https://doi.org/10.1016/j.preteyeres.2021.100975
Bourne, R. R. A., Flaxman, S. R., Braithwaite, T., Cicinelli, M. V., Das, A., Jonas, J. B., Keeffe, J., Kempen, J. H., Leasher, J., Limburg, H., Naidoo, K., Pesudovs, K., Resnikoff, S., Silvester, A., Stevens, G. A., Tahhan, N., Wong, T. Y., Taylor, H. R., Bourne, R., & Ackland, P. (2017). Magnitude, temporal trends, and projections of the global prevalence of blindness and distance and near vision impairment: a systematic review and meta-analysis. TheLancet GlobalHealth , 5(9), e888–e897.
https://doi.org/10.1016/s2214-109x(17)30293-0
Boyd, K. (2020, March 4). Amblyopia:WhatIsLazyEye? American Academy of Ophthalmology.
https://www.aao.org/eye-health/diseases/amblyopia-lazy-eye
Boyd, K., & Vemulakonda, G. A. (2018, April 28). WhatIs RetinopathyofPrematurity(ROP)?American Academy of Ophthalmology.
https://www.aao.org/eye-health/diseases/whatis-retinopathy-prematurity
Boyd, K., & Vemulakonda, G. A. (2019, May 10). WhatIs MacularDegeneration?(D. Turbert, Ed.). American Academy of Ophthalmology.
https://www.aao.org/eyehealth/diseases/amd-macular-degeneration
Bradfield, Y. S. (2013). Identification and Treatment of Amblyopia. AmericanFamilyPhysician , 87(5), 348–352.
https://www.aafp.org/pubs/afp/issues/2013/0301/p348.html
BetterEyesight 306
Brown, G. C., Brown, M. M., Busbee, B. G., & Rapuano, S. B. (2019). A Cost-benefit Analysis of 2018 Cataract Surgery in the United States. ClinicalResearchinOphthalmology , 2(1).
Buffenn, A. N. (2021). The Impact of Strabismus on Psychosocial Heath and Quality of Life: A Systematic Review. Surveyof Ophthalmology , 6
https://doi.org/10.1016/j.survophthal.2021.03.005
Bunya, V. Y., & Rana, V. (n.d.). OcularSurfaceMicrobiomeEyeWiki . Eyewiki.aao.org.
https://eyewiki.aao.org/Ocular_Surface_Microbiome
Business Model Toolbox. (n.d.). AravindBusinessModel . Business Model Toolbox. https://bmtoolbox.net/stories/aravind/
Campbell, J. P., Mathenge, C., Cherwek, H., Balaskas, K., Pasquale, L. R., Keane, P. A., & Chiang, M. F. (2021). Artificial Intelligence to Reduce Ocular Health Disparities: Moving From Concept to Implementation. Translational VisionScience&Technology , 10(3), 19.
https://doi.org/10.1167/tvst.10.3.19
Capaldo, G., Perla, C., Majors, S., & Dreisbach, E. N. (2023, May 19). FDAapproves Vyjuvekfordystrophicepidermolysis bullosa . Www.healio.com.
https://www.healio.com/news/dermatology/20230519/fdaapproves-vyjuvek-for-dystrophic-epidermolysis-bullosa
Carr, W., Schaeffer, J., & Donnenfeld, E. (2016). Treating allergic conjunctivitis: A once-daily medication that provides 24-hour symptom relief. Allergy &Rhinology , 7(2), 107–114.
https://doi.org/10.2500/ar.2016.7.0158
WilliamA.Haseltine,PhD 307
Center for Global Development. (n.d.). CASE19:Treating cataracts inIndia . Center for Global Development | Ideas to Action. https://www.cgdev.org/page/case-19-treating-cataractsindia
Chang, H.-C., Wang, T.-J., Lin, M.-H., & Chen, T.-J. (2022). A Review of the Systemic Treatment of Stevens–Johnson Syndrome and Toxic Epidermal Necrolysis. Biomedicines , 10(9), 2105.
https://doi.org/10.3390/biomedicines10092105
Charters, L. (2023). A closer look at how cell therapy for corneal endothelial disease is gaining traction.
Europe.ophthalmologytimes.com , 19 , 30–31.
https://europe.ophthalmologytimes.com/view/a-closer-look-athow-cell-therapy-for-corneal-endothelial-disease-is-gainingtraction
Chen, T. A., Li, J., Schallhorn, J. M., & Sun, C. Q. (2021).
Comparing a Home Vision Self-Assessment Test to OfficeBased Snellen Visual Acuity. ClinicalOphthalmology , Volume15 , 3205–3211.
https://doi.org/10.2147/opth.s309727
Chen, X., Xu, J., Chen, X., & Yao, K. (2021). Cataract: Advances in surgery and whether surgery remains the only treatment in future. AdvancesinOphthalmologyPracticeandResearch , 1(1), 100008.
https://doi.org/10.1016/j.aopr.2021.100008
Chenais, N. A. L., Airaghi Leccardi, M. J. I., & Ghezzi, D. (2021). Photovoltaic retinal prosthesis restores high-resolution responses to single-pixel stimulation in blind retinas. CommunicationsMaterials , 2(1).
https://doi.org/10.1038/s43246-021-00133-2
BetterEyesight 308
Cheung, C. Y., Ran, A. R., Wang, S., Chan, V. T. T., Sham, K., Hilal, S., Venketasubramanian, N., Cheng, C.-Y., Sabanayagam, C., Tham, Y. C., Schmetterer, L., McKay, G. J., Williams, M. A., Wong, A., Au, L. W. C., Lu, Z., Yam, J. C., Tham, C. C., Chen, J. J., & Dumitrascu, O. M. (2022). A deep learning model for detection of Alzheimer’s disease based on retinal photographs: a retrospective, multicentre case-control study. TheLancetDigitalHealth , 0(0).
https://doi.org/10.1016/S2589-7500(22)00169-8
Choudhary, A., Ahlawat, S., Urooj, S., Pathak, N., Lay-Ekuakille, A., & Sharma, N. (2023). A Deep Learning-Based Framework for Retinal Disease Classification. Healthcare , 11(2), 212.
https://doi.org/10.3390/healthcare11020212
Churchill, A., & Graw, J. (2011). Clinical and experimental advances in congenital and paediatric cataracts. Philosophical Transactions oftheRoyalSocietyB:BiologicalSciences , 366(1568), 1234–1249. https://doi.org/10.1098/rstb.2010.0227
Cleveland Clinic. (n.d.). RetinalImaging:WhatIt Shows&Why It’sImportant . Cleveland Clinic.
https://my.clevelandclinic.org/health/diagnostics/25046-retinalimaging
Cleveland Clinic. (2021, March 3). MigraineHeadaches: Symptoms,Causes,Treatment &Prevention . Cleveland Clinic.
https://my.clevelandclinic.org/health/diseases/5005migraine-headaches
Cleveland Clinic. (2023, March 9). CorneaTransplant . Cleveland Clinic.
https://my.clevelandclinic.org/health/treatments/17714cornea-transplant
WilliamA.Haseltine,PhD 309
Clifford, L. J., Turnbull, A. M. J., & Denning, A. M. (2013). Reversible night blindness – A reminder of the increasing importance of vitamin A deficiency in the developed world. JournalofOptometry , 6(3), 173–174.
https://doi.org/10.1016/j.optom.2013.01.002
Coco-Martin, R. M., Pastor-Idoate, S., & Pastor, J. C. (2021). Cell Replacement Therapy for Retinal and Optic Nerve Diseases: Cell Sources, Clinical Trials and Challenges. Pharmaceutics , 13(6), 865.
https://doi.org/10.3390/pharmaceutics13060865
Colby, K. (2021). Update on Corneal Transplant in 2021. JAMA , 325(18), 1886.
https://doi.org/10.1001/jama.2020.17382
ColorLite. (n.d.). ColorBlindGlasses|ColorBlindness
Correction|Colorlite Colorlite | Color Blind Glasses | Color Blind Test.
https://www.colorlitelens.com/
da Cruz, L., Fynes, K., Georgiadis, O., Kerby, J., Luo, Y. H., Ahmado, A., Vernon, A., Daniels, J. T., Nommiste, B., Hasan, S. M., Gooljar, S. B., Carr, A.-J. F., Vugler, A., Ramsden, C. M., Bictash, M., Fenster, M., Steer, J., Harbinson, T., Wilbrey, A., & Tufail, A. (2018). Phase 1 clinical study of an embryonic stem cell–derived retinal pigment epithelium patch in agerelated macular degeneration. NatureBiotechnology , 36(4), 328–337.
https://doi.org/10.1038/nbt.4114
de las Rivas Ramírez, N., Luque Aranda, G., Rius Díaz, F., Pérez Frías, F. J., & Sánchez Tamayo, T. (2022). Risk factors associated with Retinopathy of Prematurity development and progression. ScientificReports , 12(1).
https://doi.org/10.1038/s41598-022-26229-4
BetterEyesight 310
De, M., Presa, L., & Holland, E. (2021). InjectableCorneal EndothelialCellsThepotentialtransformationofthe management ofendothelialcellfailure0 .
https://aurionbiotech.com/wpcontent/uploads/2022/04/Corneal-Physician-InjectableCorneal-Endothelial-Cells.pdf
Demircan, S., Ataş, M., Arık Yüksel, S., Ulusoy, M. D., Yuvacı, İ , Arifoğlu, H. B., Başkan, B., & Zararsız, G. (2015). The Impact of Migraine on Posterior Ocular Structures. Journalof Ophthalmology , 2015 .
https://doi.org/10.1155/2015/868967
Demirkılınç Biler, E., Yıldırım, Ş., Üretmen, Ö., & Köse, S. (2018). Long-term Results in Pediatric Developmental Cataract Surgery with Primary Intraocular Lens Implantation. TürkOftalmolojiDergisi , 1–5.
https://doi.org/10.4274/tjo.80947
Dominika Szkodny, Wróblewska-Czajka, E., Wylęgała, A., Nandzik, M., & Wylęgała, E. (2022). Incidence of Complications Related to Corneal Graft in a Group of 758 Patients. JournalofClinicalMedicine , 12(1), 220–220.
https://doi.org/10.3390/jcm12010220
Donaghy, C., Vislisel , J., & Greiner , M. (2015, May 21). Deep AnteriorLamellarKeratoplasty(DALK) . Webeye.ophth.uiowa.edu.
https://webeye.ophth.uiowa.edu/eyeforum/tutorials/corneatransplant-intro/3-DALK.htm
Downie, L. E., & Vingrys, A. J. (2018). Oral Omega-3 Supplementation Lowers Intraocular Pressure in
WilliamA.Haseltine,PhD 311
Normotensive Adults. TranslationalVisionScience& Technology , 7(3), 1. https://doi.org/10.1167/tvst.7.3.1
Duplechain, A., Conrady, C. D., Patel, B. C., & Baker, S. (2020). Uveitis . PubMed; StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK540993/
Dupuis, P., Prokopich, C. L., Hynes, A., & Kim, H. (2020). A contemporary look at allergic conjunctivitis. Allergy,Asthma& ClinicalImmunology , 16(1). https://doi.org/10.1186/s13223020-0403-9
Elsevier. (n.d.). NightVision - an overview|ScienceDirectTopics . Www.sciencedirect.com. Retrieved December 14, 2023, from
https://www.sciencedirect.com/topics/biochemistry-geneticsand-molecular-biology/night-vision
Enchroma. (n.d.). Homepage Test . EnChroma. Retrieved December 14, 2023, from
https://enchroma.com/es/pages/homepage-test
Epitropoulos, A. T., Donnenfeld, E. D., Shah, Z. A., Holland, E. J., Gross, M., Faulkner, W. J., Matossian, C., Lane, S. S., Toyos, M., Bucci, F. A., & Perry, H. D. (2016). Effect of Oral Re-esterified Omega-3 Nutritional Supplementation on Dry Eyes. Cornea , 35(9), 1185–1191.
https://doi.org/10.1097/ico.0000000000000940
Fang, G., Wang, Q., Yang, X., Qian, Y., Zhang, G., & Tang, B. (2022). γ-Cyclodextrin-based polypseudorotaxane hydrogels for ophthalmic delivery of flurbiprofen to treat anterior uveitis. CarbohydratePolymers , 277 , 118889.
https://doi.org/10.1016/j.carbpol.2021.118889
BetterEyesight 312
Fang, J., Wang, X., Lin, Z., Yan, J., Yang, Y., & Li, J. (2010). Variation of cataract surgery costs in four different graded providers of China. BMCPublicHealth , 10(1).
https://doi.org/10.1186/1471-2458-10-543
Fang, R., Yu, Y.-F., Li, E.-J., Lv, N.-X., Liu, Z.-C., Zhou, H.-G., & Song, X.-D. (2022). Global, regional, national burden and gender disparity of cataract: findings from the global burden of disease study 2019. BMCPublicHealth , 22(1).
https://doi.org/10.1186/s12889-022-14491-0
Fateme Hosseinnia, Khaleghi, A., & Mahmoudi, K. (2020). Using Gamification Based on Virtual Reality Mobile Platform for Treatment of Adults with Amblyopia. AdvancesinIntelligent SystemsandComputing , 836–843. https://doi.org/10.1007/978-
3-030-49932-7_78
FDA. (2019). EpidermolysisBullosa:DevelopingDrugsfor Treatment ofCutaneousManifestationsGuidance for Industry
https://www.fda.gov/media/128419/download
FDA Office of Media Affairs. (2022, August 16). FDARoundup: August16,2022 . FDA.
https://www.fda.gov/news-events/pressannouncements/fda-roundup-august-16-2022
Feng, Y. R., Meuleners, L., Fraser, M., Brameld, K., & Agramunt, S. (2018). The impact of first and second eye cataract surgeries on falls: a prospective cohort study. ClinicalInterventions in Aging , Volume13 , 1457–1464.
https://doi.org/10.2147/cia.s164419
Fernández, E., Alfaro, A., Soto-Sánchez, C., Gonzalez-Lopez, P., Lozano, A. M., Peña, S., Grima, M. D., Rodil, A., Gómez, B., Chen, X., Roelfsema, P. R., Rolston, J. D., Davis, T. S., &
WilliamA.Haseltine,PhD 313
Normann, R. A. (2021, December 1). Visualpercepts evoked withan intracortical96-channelmicroelectrodearray inserted in humanoccipitalcortex. Www.jci.org.
https://www.jci.org/articles/view/151331/pdf
Fernández-Vega Cueto, A., Álvarez, L., García, M., ÁlvarezBarrios, A., Artime, E., Fernández-Vega Cueto, L., CocaPrados, M., & González-Iglesias, H. (2021). Candidate Glaucoma Biomarkers: From Proteins to Metabolites, and the Pitfalls to Clinical Applications. Biology , 10(8), 763.
https://doi.org/10.3390/biology10080763
Ferro Desideri, L., Traverso, C. E., Nicolò, M., & Munk, M. R. (2023). Faricimab for the Treatment of Diabetic Macular Edema and Neovascular Age-Related Macular Degeneration. Pharmaceutics , 15(5), 1413.
https://doi.org/10.3390/pharmaceutics15051413
Fidler, B. (2023, February 17). Apelliswins FDAapprovaloffirst drugfortype ofvision loss BioPharma Dive.
https://www.biopharmadive.com/news/apellis-fda-approvalsyfovre-geographic-atrophy/643111/
Fletcher, J., deLeeuw, A., & Corte, R. (2017, February 17). The besteye dropsfordryeyes in 2022:Productsandhowto choose . Www.medicalnewstoday.com.
https://www.medicalnewstoday.com/articles/best-eye-drops-fordry-eye
Flores, R., Carneiro, Â., Tenreiro, S., & Seabra, M. C. (2021). Retinal Progression Biomarkers of Early and Intermediate AgeRelated Macular Degeneration. Life , 12(1), 36–36.
https://doi.org/10.3390/life12010036
BetterEyesight 314
Fondation Stargardt. (2018, May). Clinicaltrials . Stargardt Foundation. https://www.stargardt.fr/en/current-research-andtrials/clinical-trials/
Fromow-Guerra, J. (2012, September). TheEvolutionofConfocal ScanningLaserOphthalmoscopy . Retina Today.
https://retinatoday.com/articles/2012-sept/the-evolution-ofconfocal-scanning-laser-ophthalmoscopy
Gabriel, E., Albanna, W., Pasquini, G., Ramani, A., Josipovic, N., Mariappan, A., Schinzel, F., Karch, C. M., Bao, G., Gottardo, M., Suren, A. A., Hescheler, J., Nagel-Wolfrum, K., Persico, V., Rizzoli, S. O., Altmüller, J., Riparbelli, M. G., Callaini, G., Goureau, O., & Papantonis, A. (2021). Human brain organoids assemble functionally integrated bilateral optic vesicles. CellStemCell , 28(10), 1740-1757.e8.
https://doi.org/10.1016/j.stem.2021.07.010
Gabriele, M. L., Wollstein, G., Ishikawa, H., Xu, J., Kim, J., Kagemann, L., Folio, L. S., & Schuman, J. S. (2010). Three dimensional optical coherence tomography imaging: Advantages and advances. Progress in RetinalandEye Research , 29(6), 556–579.
https://doi.org/10.1016/j.preteyeres.2010.05.005
Gao, T., Qu, J., Xiao, J., Hu, J., & Zhao, M. (2018). Photodynamic therapy for bullous retinal detachment: a single-center experience of case series with a 6-month follow-up study. GraefesArchiveforClinicalandExperimental Ophthalmology , 256(8), 1429–1439.
https://doi.org/10.1007/s00417-018-4015-8
WilliamA.Haseltine,PhD 315
Garg, A. K., Knight, D., Lando, L., & Chao, D. L. (2021). Advances in Retinal Oximetry. TranslationalVisionScience& Technology , 10(2), 5. https://doi.org/10.1167/tvst.10.2.5
Geerlings, M. J., de Jong, E. K., & den Hollander, A. I. (2017). The complement system in age-related macular degeneration: A review of rare genetic variants and implications for personalized treatment. MolecularImmunology , 84 , 65–76.
https://doi.org/10.1016/j.molimm.2016.11.016
Gillette, H. (2023, February 27). Costofcataractsurgery: With insurance, withoutinsurance, andhelp(W. C. Lloyd III, Ed.). Www.medicalnewstoday.com.
https://www.medicalnewstoday.com/articles/cataract-surgerycost#medicare
Glover, V., & Sandler, M. (1989). Can the vascular and neurogenic theories of migraine finally be reconciled? Trends inPharmacologicalSciences , 10(1), 1–3.
https://doi.org/10.1016/0165-6147(89)90089-8
Goon Tay, H., Andre, H., Chrysostomou, V., Adusumalli, S., Guo, J., Ren, X., Sheng Tan, W., Tor, J. E., Moreno-Moral, A., Plastino, F., Bartuma, H., Cai, Z., Bo Tun, S. B., Barathi, V. A., Wei, G. T. S., Grenci, G., Chong, L. Y., Holmgren, A., Kvanta, A., & Guy, C. J. (2023). Photoreceptor laminin drives differentiation of human pluripotent stem cells to photoreceptor progenitors that partially restore retina function. MolecularTherapy , 31(3), 825–846.
https://doi.org/10.1016/j.ymthe.2022.12.012
BetterEyesight 316
Gore, D. M., Shortt, A. J., & Allan, B. D. (2012). New clinical pathways for keratoconus. Eye , 27(3), 329–339.
https://doi.org/10.1038/eye.2012.257
Gramatikov, B. I. (2014). Modern technologies for retinal scanning and imaging: an introduction for the biomedical engineer. BioMedicalEngineeringOnLine , 13 , 52.
https://doi.org/10.1186/1475-925X-13-52
Gulledge, M. (2011, August 26). DigitalRetinalImaging:PracticeBuildingInvestment . Review of Optometric Business.
https://reviewob.com/digital-retinal-imaging-practice-buildinginvestment/
Gurnani, B., & Tripathy, K. (2022). MinimallyInvasive Glaucoma Surgery PubMed; StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK582156/
Guymer, R. H., & Campbell, T. G. (2023). Age-related macular degeneration. TheLancet , 401(10386), 1459–1472.
https://doi.org/10.1016/S0140-6736(22)02609-5
Haber, S. L., Benson, V., Buckway, C. J., Gonzales, J. M., Romanet, D., & Scholes, B. (2019). Lifitegrast: a novel drug for patients with dry eye disease. TherapeuticAdvancesin Ophthalmology , 11 , 251584141987036.
https://doi.org/10.1177/2515841419870366
Hakim, F. E., Nagra, A. K., & Dhaliwal, D. K. (2023). Descemet Stripping Only: Long-Term Outcomes. Cornea .
https://doi.org/10.1097/ICO.0000000000003421
Hamid Shamszare, & Choudhury, A. (2023). Clinicians’ Perceptions of Artificial Intelligence: Focus on Workload, Risk,
WilliamA.Haseltine,PhD 317
Trust, Clinical Decision Making, and Clinical Integration. Healthcare , 11(16), 2308–2308.
https://doi.org/10.3390/healthcare11162308
Hanna, K., Nieves, J., Dowd, C., Bender, K. O., Sharma, P., Singh, B., Renz, M., Ver Hoeve, J. N., Cepeda, D., Gelfman, C. M., Riley, B. E., & Grishanin, R. N. (2023). Preclinical evaluation of ADVM-062, a novel intravitreal gene therapy vector for the treatment of blue cone monochromacy. MolecularTherapy , 31(7), 2014–2027.
https://doi.org/10.1016/j.ymthe.2023.03.011
Hassman, L., Bessette, A., & Kuriyan, A. E. (2017, September 1). Treatment ofUveiticMacularEdema . Retinalphysician.com.
https://www.retinalphysician.com/issues/2017/september2017/treatment-of-uveitic-macular-edema
Healthwise. (2023, June 6). LaserPhotocoagulationforDiabetic Retinopathy|Kaiser Permanente . Healthy.kaiserpermanente.org.
https://healthy.kaiserpermanente.org/health-wellness/healthencyclopedia/he.laser-photocoagulation-for-diabeticretinopathy.tf4075
Heidary, G., Aakalu, V. K., Binenbaum, G., Chang, M. Y., Morrison, D. G., VanderVeen, D. K., Lambert, S. R., Trivedi, R. H., Galvin, J. A., & Pineles, S. L. (2022). Adjustable Sutures in the Treatment of Strabismus. Ophthalmology , 129(1), 100–109. https://doi.org/10.1016/j.ophtha.2021.07.026
Hinkle, J. W., Mahmoudzadeh, R., & Kuriyan, A. E. (2021). Cellbased therapies for retinal diseases: a review of clinical trials and direct to consumer “cell therapy” clinics. StemCell
BetterEyesight 318
Research&Therapy , 12(1). https://doi.org/10.1186/s13287021-02546-9
Hoffmann-La Roche. (2023, October 23). SafetyandEfficacy
StudyofOpRegenforTreatment ofAdvancedDry-FormAgeRelatedMacularDegeneration - FullText ViewClinicalTrials.gov Clinicaltrials.gov.
https://classic.clinicaltrials.gov/ct2/show/NCT02286089
Honavar, S. (2022). Self-sustainable and inclusive eye care –Where equity meets excellence. IndianJournalof Ophthalmology , 70(5), 1441.
https://doi.org/10.4103/ijo.ijo_1008_22
Hong, E., Glynn, C., Wang, Q., & Rao, S. (2022). Non-Invasive Electroretinogram Recording with Simultaneous Optogenetics to Dissect Retinal Ganglion Cells Electrophysiological Dynamics. Biosensors , 13(1), 42.
https://doi.org/10.3390/bios13010042
Honkila, M., Koskela, U., Kontiokari, T., Mattila, M.-L., Kristo, A., Valtonen, R., Sarlin, S., Paalanne, N., Ikäheimo, I., Pokka, T., Uhari, M., Renko, M., & Tapiainen, T. (2022). Effect of Topical Antibiotics on Duration of Acute Infective Conjunctivitis in Children. JAMANetworkOpen , 5(10), e2234459.
https://doi.org/10.1001/jamanetworkopen.2022.34459
Human brain organoids assemble functionally integrated bilateral optic vesicles. (2021). CellStemCell .
https://doi.org/10.1016/j.stem.2021.07.010
Hunter, J. J., Merigan, W. H., & Schallek, J. B. (2019). Imaging Retinal Activity in the Living Eye. AnnualReviewofVision
WilliamA.Haseltine,PhD 319
Science, 5(1), 15–45. https://doi.org/10.1146/annurev-vision091517-034239
Hutton, D. (2023, April 25). ARVO2023:KrystalBiotech announces clinicaldataon topicalapplicationofB-VECto treat ocularcomplicationsinpatient withdystrophic epidermolysisbullosa Ophthalmology Times.
https://www.ophthalmologytimes.com/view/arvo-2023-krystalbiotech-announces-clinical-data-on-topical-application-of-bvec-to-treat-ocular-complications-in-patient-with-dystrophicepidermolysis-bullosa
iHealthScreen. (n.d.). Ihealthscreen.org. Retrieved December 4, 2023, from https://ihealthscreen.org/
Im, J. H. B., Jin, Y.-P., Chow, R., & Yan, P. (2022). Prevalence of diabetic macular edema based on optical coherence tomography in people with diabetes: A systematic review and meta-analysis. SurveyofOphthalmology , 67(4), 1244–1251.
https://doi.org/10.1016/j.survophthal.2022.01.009
Jefferies, A. (2010). Retinopathy of prematurity: Recommendations for screening. Paediatrics&ChildHealth , 15(10), 667–670.
https://doi.org/10.1093/pch/15.10.667
Jha, D. (2023, June 9). Record 83.4 lakh cataract surgeries executed in 2022-2023: Government. TheTimes ofIndia .
https://timesofindia.indiatimes.com/india/record-83-4-lakhcataract-surgeries-executed-in-2022-2023government/articleshow/100857963.cms?from=mdr
Johns Hopkins Medicine. (n.d.). LaserPhotocoagulationforAgeRelatedMacularDegeneration Www.hopkinsmedicine.org.
https://www.hopkinsmedicine.org/health/treatment-tests-and-
BetterEyesight 320
therapies/laser-photocoagulation-for-agerelated-maculardegeneration
Johnson, A. (2023, March 27). Newformofomega-3could prevent visualdeclinewithAlzheimer’sdisease . EurekAlert!
https://www.eurekalert.org/news-releases/983049
Johnson, A., & Heiting, G. (2020, February 26). ThyroidEye Disease . All about Vision.
https://www.allaboutvision.com/conditions/thyroid-eye-disease/
Jun, A. S. (2021, August 8). BestWaytoAge-ProofYour Vision Www.hopkinsmedicine.org.
https://www.hopkinsmedicine.org/health/wellness-andprevention/best-way-to-age-proof-your-vision
Justus, M. S. (2021, February 9). Theincreasingpotentialof electroretinographyinophthalmicdiagnostics . Ophthalmology Times. https://europe.ophthalmologytimes.com/view/theincreasing-potential-of-electroretinography-in-ophthalmicdiagnostics
Kaiser, S. M., Arepalli, S., & Ehlers, J. P. (2021). Current and Future Anti-VEGF Agents for Neovascular Age-Related Macular Degeneration. JournalofExperimental Pharmacology , Volume13 , 905–912.
https://doi.org/10.2147/jep.s259298
Kaiti, R. (2022). Role of Atropine in the control of Myopia Progression- A Review. BeyogluEyeJournal .
https://doi.org/10.14744/bej.2022.07742
Kalogeropoulos, D., Sakkas, H., Mohammed, B., Vartholomatos, G., Malamos, K., Sreekantam, S., Kanavaros, P., &
WilliamA.Haseltine,PhD 321
Kalogeropoulos, C. (2021). Ocular toxoplasmosis: a review of the current diagnostic and therapeutic approaches. InternationalOphthalmology , 42(1), 295–321.
https://doi.org/10.1007/s10792-021-01994-9
Kanagasingam, Y., Xiao, D., Vignarajan, J., Preetham, A., TayKearney, M.-L., & Mehrotra, A. (2018). Evaluation of Artificial Intelligence–Based Grading of Diabetic Retinopathy in Primary Care. JAMANetworkOpen , 1(5), e182665.
https://doi.org/10.1001/jamanetworkopen.2018.2665
Kannabiran, C., Chaurasia, S., Ramappa, M., & Mootha, V. V. (2022). Update on the genetics of corneal endothelial dystrophies. IndianJournalofOphthalmology , 70(7), 2239–2248.
https://doi.org/10.4103/ijo.IJO_992_22
Karimian, F., & Feizi, S. (2010). Deep Anterior Lamellar Keratoplasty: Indications, Surgical Techniques and Complications. MiddleEast AfricanJournalof Ophthalmology , 17(1), 28–37. https://doi.org/10.4103/09749233.61214
Kashani, A. H., Asanad, S., Chan, J. W., Singer, M. B., Zhang, J., Sharifi, M., Khansari, M. M., Abdolahi, F., Shi, Y., Biffi, A., Chui, H., & Ringman, J. M. (2021). Past, present and future role of retinal imaging in neurodegenerative disease. Progress in RetinalandEye Research , 83 , 100938.
https://doi.org/10.1016/j.preteyeres.2020.100938
Kates, M. M., & Tuli, S. (2021). Complications of Contact Lenses. JAMA , 325(18), 1912.
https://doi.org/10.1001/jama.2020.20328
BetterEyesight 322
Katsanos, A., Tsaldari, N., Gorgoli, K., Lalos, F., Stefaniotou, M., & Asproudis, I. (2020). Safety and Efficacy of YAG Laser Vitreolysis for the Treatment of Vitreous Floaters: An Overview. AdvancesinTherapy
https://doi.org/10.1007/s12325-020-01261-w
Kauh, C. Y., Blachley, T. S., Lichter, P. R., Lee, P. P., & Stein, J. D. (2016). Geographic Variation in the Rate and Timing of Cataract Surgery Among US Communities. JAMA Ophthalmology , 134(3), 267–276.
https://doi.org/10.1001/jamaophthalmol.2015.5322
Kaur, S., Kumari, A., Kumari Negi, A., Galav, V., Thakur, S., Agrawal, M., & Sharma, V. (2021). Nanotechnology Based Approaches in Phage Therapy: Overcoming the Pharmacological Barriers. Frontiers inPharmacology , 12
https://doi.org/10.3389/fphar.2021.699054
Keating, G. M. (2017). Lifitegrast Ophthalmic Solution 5%: A Review in Dry Eye Disease. Drugs , 77(2), 201–208.
https://doi.org/10.1007/s40265-016-0681-1
Kim, L. A., Tripathy, K., Bhagat, N., Lim, J. I., Karth, P. A., FRCS Glasgow, & Madadi, S. (2023, August 16). Sub-Threshold Laser - EyeWiki . Eyewiki.aao.org. https://eyewiki.aao.org/SubThreshold_Laser
King, A. (2023, August 22). Restoringsightto theblindwith cutting-edgebrainimplants|ResearchandInnovation . Ec.europa.eu. https://ec.europa.eu/research-andinnovation/en/horizon-magazine/restoring-sight-blind-cuttingedge-brain-implants
WilliamA.Haseltine,PhD 323
Kinoshita, S., Koizumi, N., Ueno, M., Okumura, N., Imai, K., Tanaka, H., Yamamoto, Y., Nakamura, T., Inatomi, T., Bush, J., Toda, M., Hagiya, M., Yokota, I., Teramukai, S., Sotozono, C., & Hamuro, J. (2018). Injection of Cultured Cells with a ROCK Inhibitor for Bullous Keratopathy. NewEngland JournalofMedicine , 378(11), 995–1003.
https://doi.org/10.1056/nejmoa1712770
Knickelbein, J. E., Bunya, V. Y., Woodward, M. A., & Weissbart, S. B. (2017, February 17). Herpessimplexvirus stromal keratitisandendotheliitis - EyeWiki . Aao.org.
https://eyewiki.aao.org/Herpes_simplex_virus_stromal_keratitis _and_endotheliitis
Kohl, S., & Orphanet. (2013, August). Orphanet:Bluecone monochromatism Www.orpha.net.
https://www.orpha.net/consor/cgi-
bin/OC_Exp.php?Expert=16&Lng=GB
Koo, E. H., & Ansari, Z. (2020). Commentary on ten-year incidence of cataract surgery in urban southern China: the Liwan Eye Study. AnnalsofEye Science , 5 , 21–21.
https://doi.org/10.21037/aes-2020-01
Krogh Nielson, M., Shah, Y. S., Kim, L. A., Tripathy, K., Do, D. V., Bhagat, N., & Lim, J. (2023, August 29). Geographic Atrophy - EyeWiki(K. Tripathy, Ed.). Eyewiki.aao.org.
https://eyewiki.aao.org/Geographic_Atrophy
Krystal Biotech, Inc. (2023a, February 17). Ph3Efficacyand SafetyofB-VECfortheTreatmentofDEB - FullText ViewClinicalTrials.gov . Clinicaltrials.gov.
https://classic.clinicaltrials.gov/ct2/show/NCT04491604
BetterEyesight 324
Krystal Biotech, Inc. (2023b, August 18). ALong-term Treatment
WithB-VECforDystrophicEpidermolysisBullosa - FullText View - ClinicalTrials.gov . Clinicaltrials.gov.
https://classic.clinicaltrials.gov/ct2/show/NCT04917874
Kulkarni, S., & Deshpande, M. (2019). Recent advances in retinal imaging and diagnostics. CommunityEye Health , 32(107), S9–S10.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7041830/
Kupis, M., Samelska, K., Szaflik, J., & Skopiński, P. (2022). Novel therapies for diabetic retinopathy. CentralEuropeanJournalof Immunology , 47(1), 102–108.
https://doi.org/10.5114/ceji.2022.112993
Lahr, J. (2019, November 11). Visionbenefitscan leadtoearly detectionofdiabeticretinopathy . EyeMed Vision Benefits.
https://eyemed.com/en-us/blog/health-wellness/vision-benefitscan-lead-to-early-detection-of-diabetic-retinopathy-17546
Lapointe, N., Akitegetse, C., Poirier, J., Picard, M., Sauvageau, P., & Sauvageau, D. (2023). Targeted spectroscopy in the eye fundus. JournalofBiomedicalOptics , 28(12), 126004.
https://doi.org/10.1117/1.JBO.28.12.126004
Lawrenson, J. G., & Evans, J. R. (2015). Omega 3 fatty acids for preventing or slowing the progression of age-related macular degeneration. CochraneDatabaseofSystematicReviews
https://doi.org/10.1002/14651858.cd010015.pub3
Le, H.-G., Ehrlich, J. R., Venkatesh, R., Srinivasan, A., Kolli, A., Haripriya, A., Ravindran, R. D., Thulasiraj, R. D., Robin, A. L., Hutton, D. W., & Stein, J. D. (2016). A Sustainable Model For Delivering High-Quality, Efficient Cataract Surgery In
WilliamA.Haseltine,PhD 325
Southern India. HealthAffairs , 35(10), 1783–1790.
https://doi.org/10.1377/hlthaff.2016.0562
Lee, R., Wong, T. Y., & Sabanayagam, C. (2015). Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye andVision , 2(1).
https://doi.org/10.1186/s40662-015-0026-2
Lee, S. Y., & Mesfin, F. B. (2020). Blindness . PubMed; StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK448182/
Leng, Y., Li, X.-J., Li, C.-Y., & Bai, D. (2021). Insights into stem cell therapy for diabetic retinopathy: a bibliometric and visual analysis. NeuralRegenerationResearch , 16(1), 172.
https://doi.org/10.4103/1673-5374.286974
Leonard, C. Y. (2022, November 10). WhatLiesAheadforAI in Glaucoma?Www.reviewofophthalmology.com.
https://www.reviewofophthalmology.com/article/what-liesahead-for-ai-in-glaucoma
Li, S., Tang, A., Yang, B., Wang, J., & Liu, L. (2022). Virtual reality-based vision therapy versus OBVAT in the treatment of convergence insufficiency, accommodative dysfunction: a pilot randomized controlled trial. BMCOphthalmology , 22(1).
https://doi.org/10.1186/s12886-022-02393-z
Li, S., Yang, M., Zhao, R., Peng, L., Liu, W., Jiang, X., He, Y., Dai, E., Zhang, L., Yang, Y., Shi, Y., Zhao, P., Yang, Z., & Zhu, X. (2023). Defective EMC1 drives abnormal retinal angiogenesis via Wnt/β-catenin signaling and may be associated with the pathogenesis of familial exudative vitreoretinopathy. Genes&Diseases , 10(6), 2572–2585.
https://doi.org/10.1016/j.gendis.2022.10.003
BetterEyesight 326
Li, T., Qureshi, R., & Taylor, K. (2019). Conventional occlusion versus pharmacologic penalization for amblyopia. Cochrane DatabaseofSystematicReviews .
https://doi.org/10.1002/14651858.cd006460.pub3
Li, X., Chen, Z., Bai, J., Li, X., Chen, X., Li, Z., Pan, H., Li, S., Gao, Q., Zhao, N., Chen, A.-L., Xu, H., Wen, Y., Du, L., Yang, M., Zhou, X., & Huang, J. (2023). Multifunctional Hydrogel Eye Drops for Synergistic Treatment of Ocular Inflammatory Disease. ACSNano .
https://doi.org/10.1021/acsnano.3c08869
Li, Y., Wei, Y., Li, G., Huang, S., Xu, J., Ding, Q., & Hong, J. (2022). Targeting NECTIN-1 Based on CRISPR/Cas9 System
Attenuated the Herpes Simplex Virus Infection in Human Corneal Epithelial Cells In Vitro. TranslationalVision Science&Technology , 11(2), 8–8.
https://doi.org/10.1167/tvst.11.2.8
Lin, F., Yao, Q., Yu, B., Deng, Z., Qiu, J., & He, R. (2023). The Efficacy and Safety of Teprotumumab in Thyroid Eye Disease: Evidence from Randomized Controlled Trials. International JournalofClinicalPractice , 2023 , e6638089.
https://doi.org/10.1155/2023/6638089
Liu, J. (2022, November 24). Identificationofpotentialferroptosisrelatedbiomarkersanda pharmacologicalcompoundin diabeticretinopathybasedon machinelearningandmolecular docking(X. Li, Y. Cheng, K. Liu, H. Zou, & Z. You, Eds.). Frontiers in Endrocrinology.
https://www.frontiersin.org/articles/10.3389/fendo.2022.988506
/full
WilliamA.Haseltine,PhD 327
Lundeen, E. A., Zeb Burke-Conte, Rein, D. B., Wittenborn, J. S., Jinan Saaddine, Lee, A. Y., & Flaxman, A. D. (2023). Prevalence of Diabetic Retinopathy in the US in 2021. JAMA
Ophthalmology
https://doi.org/10.1001/jamaophthalmol.2023.2289
Luo, Z., & Chang, K.-C. (2024). Cell replacement with stem cellderived retinal ganglion cells from different protocols. Neural RegenerationResearch , 19(4), 807.
https://doi.org/10.4103/1673-5374.381494
Ma, D. H.-K., Tsai, T.-Y., Pan, L.-Y., Chen, S.-Y., Hsiao, C.-H., Yeh, L.-K., Tan, H.-Y., Lu, C.-W., Chen, C.-B., & Chung, W.H. (2021). Clinical Aspects of Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis With Severe Ocular Complications in Taiwan. Frontiers in Medicine , 8 , 661891.
https://doi.org/10.3389/fmed.2021.661891
Mahabadi, N., Foris, L. A., & Tripathy, K. (2020). OpenAngle Glaucoma PubMed; StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK441887/
Maharjan, R., Diaz Bustamante, L., Ghattas, K. N., Ilyas, S., AlRefai, R., & Khan, S. (2020). Role of Lifestyle in Neuroplasticity and Neurogenesis in an Aging Brain. Cureus .
https://doi.org/10.7759/cureus.10639
Mahroo, O. A. (2023). Visual electrophysiology and “the potential of the potentials.” Eye , 37(12), 2399–2408.
https://doi.org/10.1038/s41433-023-02491-2
March de Ribot, F., Chowdhary, A., Y. Bunya, V., Feng, S., & Shaik, N. (2023, August 7). ClinicalTrialsin Cornea -
BetterEyesight 328
EyeWiki . Eyewiki.aao.org.
https://eyewiki.aao.org/Clinical_Trials_in_Cornea
Mason, B. N., & Russo, A. F. (2018). Vascular contributions to migraine: time to revisit?. Frontiers in cellularneuroscience, 12 , 233.
Matsumoto, K., Ueta, M., Inatomi, T., Fukuoka, H., Mieno, H., Tamagawa-Mineoka, R., Katoh, N., Kinoshita, S., & Sotozono, C. (2023). Topical Betamethasone Treatment of StevensJohnson Syndrome and Toxic Epidermal Necrolysis with Ocular Involvement in the Acute Phase. AmericanJournalof Ophthalmology , 253 , 142–151.
https://doi.org/10.1016/j.ajo.2023.05.010
Mayo Clinic. (2018). Epidermolysisbullosa - Symptomsand causes. Mayo Clinic.
https://www.mayoclinic.org/diseasesconditions/epidermolysis-bullosa/symptoms-causes/syc20361062
Mayo Clinic. (2022, September 30). Glaucoma - Symptomsand causes. Mayo Clinic.
https://www.mayoclinic.org/diseasesconditions/glaucoma/symptoms-causes/syc-20372839
Mayo Foundation for Medical Education and Research (MFMER). (2023, September). AtropineSulfate(Ophthalmic Route)SideEffects - MayoClinic . Www.mayoclinic.org.
https://www.mayoclinic.org/drugs-supplements/atropinesulfate-ophthalmic-route/side-effects/drg-20313091?p=1
McConaghy, J. R., & McGuirk, R. (2019). Amblyopia: Detection and Treatment. AmericanFamilyPhysician , 100(12), 745–750. https://www.aafp.org/pubs/afp/issues/2019/1215/p745.html
WilliamA.Haseltine,PhD 329
McGhee, C., Crawford, A., & Patel, D. (2013). A brief history of corneal transplantation: From ancient to modern. Oman JournalofOphthalmology , 6(4), 12.
https://doi.org/10.4103/0974-620x.122289
McKinsey's Health Systems. (2011). Drivingdownthecost of high-qualitycare Lessons fromtheAravindEyeCareSystem
https://www.mckinsey.com/~/media/mckinsey/dotcom/client_s ervice/Healthcare%20Systems%20and%20Services/Health%20 International/Issue%2011%20new%20PDFs/HI11_18%20Arav indEyeCareSys_noprint.ashx
McLendon, K., & Preuss, C. V. (2023, June 23). Atropine . Nih.gov; StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK470551/
MD Stem Cells. (2023, June 6). StemCellOphthalmology
TreatmentStudyII - FullText View - ClinicalTrials.gov . Clinicaltrials.gov.
https://classic.clinicaltrials.gov/ct2/show/NCT03011541?term= stargardt&draw=6&rank=44
Medline Plus. (2015, January 1). Colorvisiondeficiency: MedlinePlusGenetics Medlineplus.gov.
https://medlineplus.gov/genetics/condition/color-visiondeficiency/
Medline Plus. (2022, March 22). Whatare genome editingand CRISPR-Cas9?Medlineplus.gov; Medlineplus.
https://medlineplus.gov/genetics/understanding/genomicresear ch/genomeediting/
BetterEyesight 330
Mehra, D., & Le, P. H. (2020). Physiology,NightVision . PubMed; StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK545246/
Mehta, K., & Mehta, C. (2020, April 5). AdvancedCustom Ablation:NewTechnologyforBetterQualityofVision . Www.eophtha.com.
https://www.eophtha.com/posts/advancedcustom-ablation-new-technology-for-better-quality-of-vision
Mehta, P. K., & Shenoy, S. (2011). InfiniteVision . BerrettKoehler Publishers.
Melo, L. A. de, Paiva, M. R. B. de, Fernandes-Cunha, G. M., Silva-Cunha, A., Mol, M. P. G., & Fialho, S. L. (2023). Clinical outcomes of intravitreal treatment for ocular toxoplasmosis: systematic review and meta-analysis. Revista Da SociedadeBrasileiradeMedicinaTropical , 56 .
https://doi.org/10.1590/0037-8682-0552-2022
MiljanovicB., Trivedi, K. A., Dana, M. R., Gilbard, J. P., Buring, J. E., & Schaumberg, D. A. (2005). Relation between dietary n−3 and n−6 fatty acids and clinically diagnosed dry eye syndrome in women. TheAmericanJournalofClinical Nutrition , 82(4), 887–893.
https://doi.org/10.1093/ajcn/82.4.887
Molinari, A., Weaver, D., & Jalali, S. (2017). Classifying retinopathy of prematurity. CommunityEye Health , 30(99), 55–56.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5806220/
Mount Sinai. (2022, July). BlindingEye DiseaseIsStrongly AssociatedWithHeartDiseaseandStroke|Mount Sinai - New York . Mount Sinai Health System.
WilliamA.Haseltine,PhD 331
https://www.mountsinai.org/about/newsroom/2022/blindingeye-disease-is-strongly-associated-with-heart-disease-and-stroke
Muchuchuti, S., & Viriri, S. (2023). Retinal Disease Detection Using Deep Learning Techniques: A Comprehensive Review. JournalofImaging, 9(4), 84.
https://doi.org/10.3390/jimaging9040084
Muhammed Hisham, Salih, A. E., & Butt, H. (2023). 3D Printing of Multimaterial Contact Lenses. ACSBiomaterialsScience& Engineering , 9(7), 4381–4391.
https://doi.org/10.1021/acsbiomaterials.3c00175
Mukamal, R. (2019, January 29). MicrobiomeoftheEye . American Academy of Ophthalmology.
https://www.aao.org/eye-health/anatomy/microbiome-of-eye
Mulligan, K., Jae Hong Kim, Tysinger, B., Blim, J., Emerson, G. G., Ferrone, P. J., Kim, J. E., Seabury, S. A., & Hahn, P. F. (2023). The Broader Economic Value of Treatment for Diabetic Macular Edema. DiabetesCare , 46(6), 1196–1203.
https://doi.org/10.2337/dc22-2527
Natchiar, G., Thulasiraj, R., & Sundaram, R. M. (2008). Cataract surgery at Aravind Eye Hospitals: 1988–2008. CommunityEye Health , 21(67), 40–42.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2580063/
National Eye Institute. (2019a, June 26). SurgeryforRefractive Errors|NationalEye Institute . Nih.gov.
https://www.nei.nih.gov/learn-about-eye-health/eye-conditionsand-diseases/refractive-errors/surgery-refractive-errors
BetterEyesight 332
National Eye Institute. (2019b, July 2). Amblyopia(LazyEye)| NationalEye Institute . Nih.gov. https://www.nei.nih.gov/learnabout-eye-health/eye-conditions-and-diseases/amblyopia-lazyeye
National Eye Institute. (2019c, September 23). Twocommonly useddrugsforuveitisperformequallywell National Institutes of Health (NIH).
https://www.nih.gov/news-events/nihresearch-matters/two-commonly-used-drugs-uveitis-performequally-well
National Eye Institute. (2022, February 2). LaserTreatment for DiabeticRetinopathy|NationalEye Institute . Www.nei.nih.gov.
https://www.nei.nih.gov/learn-about-eyehealth/eye-conditions-and-diseases/diabetic-retinopathy/lasertreatment-diabetic-retinopathy
National Eye Institute. (2023, July 13). Low-doseatropine eyedropsno betterthanplaceboforslowingmyopia progression National Institutes of Health (NIH).
https://www.nih.gov/news-events/news-releases/low-doseatropine-eyedrops-no-better-placebo-slowing-myopiaprogression
National Eye Institute (NEI). (2019, July 10). Retinopathyof Prematurity|NationalEye Institute . Www.nei.nih.gov.
https://www.nei.nih.gov/learn-about-eye-health/eye-conditionsand-diseases/retinopathy-prematurity
National Organization for Rare Disorders, Inc. (2015). Hemiplegic Migraine - NORD(NationalOrganizationforRareDisorders) . NORD (National Organization for Rare Disorders); NORD.
https://rarediseases.org/rare-diseases/hemiplegic-migraine/
WilliamA.Haseltine,PhD 333
Neitz, J., Carroll, J., Yamauchi, Y., Neitz, M., & Williams, D. R. (2002). Color Perception Is Mediated by a Plastic Neural Mechanism that Is Adjustable in Adults. Neuron , 35(4), 783–792.
https://doi.org/10.1016/s0896-6273(02)00818-8
Neuroscience News. (2023, April 14). StemCellTherapyCould RestoreVisionto ThoseWithMacularDegenerationand OtherBlindingEye Diseases Neuroscience News.
https://neurosciencenews.com/amd-vision-stem-cell-23015/
NHS. (2018, October 3). Childhoodcataracts - Treatment . Nhs.uk.
https://www.nhs.uk/conditions/childhoodcataracts/treatment/
NHS Choices. (2020). Treatment - Diabeticretinopathy . NHS.
https://www.nhs.uk/conditions/diabetic-retinopathy/treatment/
Nicolosi, C., Vicini, G., Bacherini, D., Giattini, D., Lombardi, N., Esposito, C., Rizzo, S., & Giansanti, F. (2023). Non-Invasive Retinal Imaging Modalities for the Identification of Prognostic Factors in Vitreoretinal Surgery for Full-Thickness Macular Holes. Diagnostics , 13(4), 589.
https://doi.org/10.3390/diagnostics13040589
Noble, W., Xu, H., Huang, X., & Gao, H. (2022). a section of the journal Frontiers in Neuroscience Editorial: Stem Cell-Based Therapy in Retinal Degeneration. Frontiers in Neuroscience| Www.frontiersin.org , 1 , 879659.
Norris, M. R., Khaimov, M., & Bielory, L. (2020). Use of allergen immunotherapy for treatment of allergic conjunctivitis. CurrentOpinioninAllergy&ClinicalImmunology , 20(6), 609–615.
https://doi.org/10.1097/aci.0000000000000692
BetterEyesight 334
Nozaki, M., Ando, R., Kimura, T., Kato, F., & Yasukawa, T. (2023). The Role of Laser Photocoagulation in Treating Diabetic Macular Edema in the Era of Intravitreal Drug Administration: A Descriptive Review. Medicina , 59(7), 1319.
https://doi.org/10.3390/medicina59071319
Numa, K., Imai, K., Ueno, M., Kitazawa, K., Tanaka, H., Bush, J. D., Teramukai, S., Okumura, N., Koizumi, N., Hamuro, J., Sotozono, C., & Kinoshita, S. (2021). Five-Year Follow-up of First 11 Patients Undergoing Injection of Cultured Corneal Endothelial Cells for Corneal Endothelial Failure. Ophthalmology , 128(4), 504–514.
https://doi.org/10.1016/j.ophtha.2020.09.002
Nurković, J. S., Vojinović, R., & Dolićanin, Z. (2020). Corneal Stem Cells as a Source of Regenerative Cell-Based Therapy. StemCellsInternational , 2020 , 1–11.
https://doi.org/10.1155/2020/8813447
NYSCF. (2021, March 30). Envisioning a BrighterFuturefor MacularDegenerationPatients:ExpertsUnpackthePathto a CellTherapy . New York Stem Cell Foundation.
https://nyscf.org/resources/envisioning-a-brighter-future-formacular-degeneration-patients-experts-unpack-the-path-to-acell-therapy/
NYU Langone Hospitals. (n.d.). EyeSurgeryforRefractiveError . Nyulangone.org. https://nyulangone.org/conditions/refractiveerror/treatments/eye-surgery-for-refractive-error
O’Hanlon Cohrt, K. (2020, November 17). News:CRISPR-Cas ClinicalTrialUpdate . CRISPR Medicine.
WilliamA.Haseltine,PhD 335
https://crisprmedicinenews.com/news/crispr-cas-clinical-trialupdate/
Oakley, A. M., & Krishnamurthy, K. (2020). StevensJohnson Syndrome(ToxicEpidermalNecrolysis) . PubMed; StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK459323/
Oldenburg, C. E., Acharya, N. R., Tu, E. Y., Zegans, M. E., Mannis, M. J., Gaynor, B. D., Whitcher, J. P., Lietman, T. M., & Keenan, J. D. (2011). Practice Patterns and Opinions in the Treatment of Acanthamoeba Keratitis. Cornea , 30(12), 1363–1368.
https://doi.org/10.1097/ico.0b013e31820f7763
Öner, A. (2018). Stem Cell Treatment in Retinal Diseases: Recent Developments. TürkOftalmolojiDergisi , 48(1), 33–38.
https://doi.org/10.4274/tjo.89972
Ophthalmic Consultants of Vermont. (n.d.). WhatIs TheCornea? Ophthalmic Consultants of Vermont.
https://ocvermont.com/corneal-surgery/what-is-the-cornea/
Ophthalmology Times. (2014, May 6). Cataractsurgery costs, complicationslowat Aravind . Ophthalmology Times.
https://www.ophthalmologytimes.com/view/cataract-surgerycosts-complications-low-aravind
OPHTHALMON SA. (2022, December 15). Thetop 10cheapest destinationsforyour Cataractsurgery Ophthalmon.com.
https://www.ophthalmon.com/2022/12/15/top-10-cataractsurgery-destinations/
Orbis. (2022, June 20). Globalblindnesswasslowingprior to pandemicstudyreveals . Orbis.
BetterEyesight 336
https://www.orbis.org/en/news/2021/new-global-blindnessdata#:~:text=2021%20has%20seen%20the%20official
Owens, C. M., Diner, B., Fusco, R., King, E., Friedland, A., Singhal, P., Kiran Gogi, Harbinski, F., Shen, S., Stefanidakis, M., Barrera, L., Bumcrot, D., Neumann, D., & Albright, C. (2018). CRISPR/Cas9 Targeted Disruption of Herpes Simplex Virus type 1 in a Rabbit Latency Model Reduces Viral Reactivation and Associated Corneal Pathology. Investigative Ophthalmology&VisualScience , 59(9), 374–374.
https://iovs.arvojournals.org/article.aspx?articleid=2689104
Oydanich, M., Maguire, M. G., Pistilli, M., Hamrah, P., Greiner, J. V., Lin, M. C., & Asbell, P. A. (2020). Effects of Omega-3 Supplementation on Exploratory Outcomes in the Dry Eye Assessment and Management Study. Ophthalmology , 127(1), 136–138.
https://doi.org/10.1016/j.ophtha.2019.07.009
Ozgonul, C., & Besirli, C. G. (2016). Recent Developments in the Diagnosis and Treatment of Ocular Toxoplasmosis. OphthalmicResearch , 57(1), 1–12.
https://doi.org/10.1159/000449169
Paczesny, J., & Bielec, K. (2020). Application of Bacteriophages in Nanotechnology. Nanomaterials , 10(10), 1944.
https://doi.org/10.3390/nano10101944
Palczewski, K. (2014). Chemistry and Biology of the Initial Steps in Vision: The Friedenwald Lecture. Investigative Opthalmology&VisualScience , 55(10), 6651.
https://doi.org/10.1167/iovs.14-15502
WilliamA.Haseltine,PhD 337
Pan, D., Xu, L., & Guo, M. (2022). The role of protein kinase C in diabetic microvascular complications. Frontiers in Endocrinology , 13 .
https://doi.org/10.3389/fendo.2022.973058
Park, S.-Y., Oh, I. Y., Kim, J.-H., Kim, H.-J., Seo, B., Kwon, O. Y., Song, W.-J., Kwon, H.-S., Cho, Y. S., Moon, H.-B., & Kim, T.B. (2020). Therapeutic Effects of Mesenchymal Stem Cells on a Stevens-Johnson Syndrome/Toxic Epidermal Necrolysis Model. JournalofKoreanMedicalScience , 35(15).
https://doi.org/10.3346/jkms.2020.35.e130
Parry, N., David Epley, K., Michael Siatkowski, R., & Tan, D. (2016, December). Howto Use Low-DoseAtropineto Slow MyopicProgressionin Kids . American Academy of Ophthalmology.
https://www.aao.org/eyenet/article/how-to-uselow-dose-atropine-to-slow-myopic-progre
Patel, S. N., Shi, A., Wibbelsman, T. D., & Klufas, M. A. (2020). Ultra-widefield retinal imaging: an update on recent advances. TherapeuticAdvancesinOphthalmology , 12 , 251584141989949.
https://doi.org/10.1177/2515841419899495
Patil, R., Dehari, D., Chaudhuri, A., Kumar, D. N., Kumar, D., Singh, S., Nath, G., & Agrawal, A. K. (2023). Recent advancements in nanotechnology-based bacteriophage delivery strategies against bacterial ocular infections. Microbiological Research , 273 , 127413.
https://doi.org/10.1016/j.micres.2023.127413
Pavluk, L. (2023a). ApellisProvidesUpdateon ReviewofRare SafetyEvents withSYFOVRE®(pegcetacoplaninjection)for GeographicAtrophy|ApellisPharmaceuticals,Inc. Apellis Pharmaceuticals, Inc. https://investors.apellis.com/news-
BetterEyesight 338
releases/news-release-details/apellis-provides-update-reviewrare-safety-events-syfovrer
Pavluk, L. (2023b). FDAApprovesSYFOVRETM (pegcetacoplan injection)as theFirst andOnlyTreatmentforGeographic Atrophy(GA),a LeadingCauseofBlindness|Apellis Pharmaceuticals,Inc. Apellis Pharmaceuticals, Inc.
https://investors.apellis.com/news-releases/news-releasedetails/fda-approves-syfovretm-pegcetacoplan-injection-firstand-only
Peter, V. G., Morandi, S. C., Herzog, E. L., Zinkernagel, M. S., & Zysset-Burri, D. C. (2023). Investigating the Ocular Surface Microbiome: What Can It Tell Us? ClinicalOphthalmology (Auckland,N.Z.) , 17 , 259–271.
https://doi.org/10.2147/OPTH.S359304
Petrillo, F., Pignataro, D., Lavano, M. A., Santella, B., Folliero, V., Zannella, C., Astarita, C., Gagliano, C., Franci, G., Avitabile, T., & Galdiero, M. (2020). Current Evidence on the Ocular Surface Microbiota and Related Diseases. Microorganisms , 8(7), 1033.
https://doi.org/10.3390/microorganisms8071033
Pluchino, K. (2020, March 24). FDAapproves firsttreatment for thyroideye disease . FDA. https://www.fda.gov/newsevents/press-announcements/fda-approves-first-treatmentthyroid-eye-disease
Podraza, K. M., Nitin Bangera, Feliz, A., & Charles, A. (2023). Reduction in retinal microvascular perfusion during migraine attacks. Headache:TheJournalofHeadandFace Pain .
https://doi.org/10.1111/head.14654
WilliamA.Haseltine,PhD 339
Qin, H., Zhang, W., Zhang, S., Feng, Y., Xu, W., Qi, J., Zhang, Q., Xu, C., Liu, S., Zhang, J., Lei, Y., Liu, W., Feng, S., Wang, J., Fu, X., Xu, Z., Li, P., & Yao, K. (2023). Vision rescue via unconstrained in vivo prime editing in degenerating neural retinas. JournalofExperimentalMedicine , 220(5).
https://doi.org/10.1084/jem.20220776
Qin, S., Dong, N., Yang, M., Wang, J., Feng, X., & Wang, Y. (2021). Complement Inhibitors in Age-Related Macular Degeneration: A Potential Therapeutic Option. Journalof ImmunologyResearch , 2021 , 1–15.
https://doi.org/10.1155/2021/9945725
R Krishnadas. (2021). The many challenges in automated glaucoma diagnosis based on fundus imaging. IndianJournal ofOphthalmology , 69(10), 2566–2566.
https://doi.org/10.4103/ijo.ijo_2294_21
Rajesh, A. E., Davidson, O. Q., Lee, C. S., & Lee, A. Y. (2023).
Artificial Intelligence and Diabetic Retinopathy: AI Framework, Prospective Studies, Head-to-head Validation, and Cost-effectiveness. DiabetesCare , 46(10), 1728–1739.
https://doi.org/10.2337/dci23-0032
Ramkumar, H. L., Epley, K. D., Shah, V. A., Rajapuram Kumar, U., Tripathy, K., Prakalapakorn, S. G., Hyde, R. A., Lim, J. I., Karth, P. A., & Rodriguez, S. (2015, October 17).
Electroretinogram - EyeWiki Aao.org.
https://eyewiki.aao.org/Electroretinogram
Rattner, A., Toulabi, L., Williams, J., Yu, H., & Nathans, J. (2008).
The Genomic Response of the Retinal Pigment Epithelium to Light Damage and Retinal Detachment. TheJournalof
BetterEyesight 340
Neuroscience , 28(39), 9880–9889.
https://doi.org/10.1523/jneurosci.2401-08.2008
Ravilla, T., & Ramasamy, D. (2014). Efficient high-volume cataract services: the Aravind model. CommunityEye Health , 27(85), 7–8.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4069777/
Rebenitsch, R., Camejo, M., & Rupani, M. (2014). A comparative analysis of the cost of cataract surgery abroad and in the United States. IndianJournalofOphthalmology , 62(6), 748.
https://doi.org/10.4103/0301-4738.136288
Repka, M. X., Weise, K. K., Chandler, D. L., Wu, R., Melia, B. M., Manny, R. E., Kehler, L. A. F., Jordan, C. O., Raghuram, A., Summers, A. I., Lee, K. A., Petersen, D. B., Erzurum, S. A., Pang, Y., Lenhart, P. D., Ticho, B. H., Beck, R. W., Kraker, R. T., Holmes, J. M., & Cotter, S. A. (2023). Low-Dose 0.01% Atropine Eye Drops vs Placebo for Myopia Control: A Randomized Clinical Trial. JAMA Ophthalmology
https://doi.org/10.1001/jamaophthalmol.2023.2855
RESERVED, I. U. -- A. R. (2014, January). Orphanet: Familial exudative vitreoretinopathy Www.orpha.net.
https://www.orpha.net/consor/cgibin/OC_Exp.php?Expert=891&Lng=GB
Rittiphairoj, T., Mir, T. A., Li, T., & Virgili, G. (2020). Intravitreal steroids for macular edema in diabetes. Cochrane Database of Systematic Reviews .
https://doi.org/10.1002/14651858.cd005656.pub3
Rom, Y., Aviv, R., Ianchulev, T., & Dvey-Aharon, Z. (2022). Predicting the future development of diabetic retinopathy using
WilliamA.Haseltine,PhD
341
a deep learning algorithm for the analysis of non-invasive retinal imaging. BMJ Open Ophthalmology , 7(1), e001140.
https://doi.org/10.1136/bmjophth-2022-001140
Rosa, A. M., Silva, M. F., Ferreira, S., Murta, J., & Castelo-Branco, M. (2013). Plasticity in the Human Visual Cortex: An Ophthalmology-Based Perspective. BioMed Research International , 2013 , 1–13.
https://doi.org/10.1155/2013/568354
Rossi, T., Romano, M. R., Iannetta, D., Romano, V., Gualdi, L., D’Agostino, I., & Ripandelli, G. (2021). Cataract surgery practice patterns worldwide: a survey. BMJ Open Ophthalmology , 6(1), e000464.
https://doi.org/10.1136/bmjophth-2020-000464
Ryder, E. C., & Benson, S. (2020). Conjunctivitis PubMed; StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK541034/
Ryu, J. (2022). New Aspects on the Treatment of Retinopathy of Prematurity: Currently Available Therapies and Emerging Novel Therapeutics. International Journal of Molecular Sciences , 23(15), 8529.
https://doi.org/10.3390/ijms23158529
Saba Hittini, Salih, A. E., Alam, F., Shanti, A., Lee, S., Kyriaki Polychronopoulou, Habiba Alsafar, Fahad Almaskari, & Butt, H. (2023). Fabrication of 3D‐Printed Contact Lenses and Their Potential as Color Blindness Ocular Aids. Macromolecular Materials and Engineering , 308(5).
https://doi.org/10.1002/mame.202200601
Sabal, B., Teper, S., & Wylęgała, E. (2023). Subthreshold Micropulse Laser for Diabetic Macular Edema: A Review.
BetterEyesight 342
Journal of Clinical Medicine , 12(1), 274.
https://doi.org/10.3390/jcm12010274
Saey, T. H. (2015, May 15). How to rewire theeye Science News.
https://www.sciencenews.org/article/how-rewire-eye
Safi, S. Z., Qvist, R., Kumar, S., Batumalaie, K., & Ismail, I. S. B. (2014). Molecular Mechanisms of Diabetic Retinopathy, General Preventive Strategies, and Novel Therapeutic Targets. BioMed Research International , 2014 .
https://doi.org/10.1155/2014/801269
Sahel, J.-A., Boulanger-Scemama, E., Pagot, C., Arleo, A., Galluppi, F., Martel, J. N., Esposti, S. D., Delaux, A., de Saint Aubert, J.B., de Montleau, C., Gutman, E., Audo, I., Duebel, J., Picaud, S., Dalkara, D., Blouin, L., Taiel, M., & Roska, B. (2021). Partial recovery of visual function in a blind patient after optogenetic therapy. Nature Medicine , 27 .
https://doi.org/10.1038/s41591-021-01351-4
Sala-Vila, A., Díaz-López, A., Valls-Pedret, C., Cofán, M., GarcíaLayana, A., Lamuela-Raventós, R.-M., Castañer, O., ZanonMoreno, V., Martinez-Gonzalez, M. A., Toledo, E., Basora, J., Salas-Salvadó, J., Corella, D., Gómez-Gracia, E., Fiol, M., Estruch, R., Lapetra, J., Fitó, M., Arós, F., & Serra-Majem, L. (2016). Dietary Marine ω-3 Fatty Acids and Incident SightThreatening Retinopathy in Middle-Aged and Older Individuals With Type 2 Diabetes. JAMA Ophthalmology , 134(10), 1142.
https://doi.org/10.1001/jamaophthalmol.2016.2906
Salih, A. E., Alam, F., Elsherif, M., Hittini, S., & Butt, H. (2023). Low‐Cost Customized Color‐Blind Contact Lenses using 3D
WilliamA.Haseltine,PhD 343
Printed Molds. Advanced Engineering Materials .
https://doi.org/10.1002/adem.202300004
Salih, A. E., Elsherif, M., Alam, F., Yetisen, A. K., & Butt, H. (2021). Gold Nanocomposite Contact Lenses for Color Blindness Management. ACS Nano , 15(3), 4870–4880.
https://doi.org/10.1021/acsnano.0c09657
Sarenac, T., Bečić Turkanović, A., Ferme, P., & Gračner, T. (2022). A Review of Selective Laser Trabeculoplasty: “The Hype Is Real.” Journal of Clinical Medicine , 11(13), 3879.
https://doi.org/10.3390/jcm11133879
Schütze, C., Teleky, K., Baumann, B., Pircher, M., Götzinger, E., Hitzenberger, C. K., & Schmidt-Erfurth, U. (2015). Polarisation-sensitive OCT is useful for evaluating retinal pigment epithelial lesions in patients with neovascular AMD.
BritishJournalofOphthalmology .
Schwartz, S. D., Regillo, C. D., Lam, B. L., Eliott, D., Rosenfeld, P. J., Gregori, N. Z., Hubschman, J.-P., Davis, J. L., Heilwell, G., Spirn, M., Maguire, J., Gay, R., Bateman, J., Ostrick, R. M., Morris, D., Vincent, M., Anglade, E., Del Priore, L. V., & Lanza, R. (2015). Human embryonic stem cell-derived retinal pigment epithelium in patients with age-related macular degeneration and Stargardt’s macular dystrophy: follow-up of two open-label phase 1/2 studies. The Lancet , 385(9967), 509–516.
https://doi.org/10.1016/s0140-6736(14)61376-3
Science. (2009, September 16). Gene Therapy Gives Monkeys
Color Vision .
Www.science.org.
https://www.science.org/content/article/gene-therapy-givesmonkeys-color-vision
BetterEyesight
344
Sechrest, E. R., Chmelik, K., Tan, W. D., & Deng, W.-T. (2023). Blue cone monochromacy and gene therapy. Vision Research , 208 , 108221. https://doi.org/10.1016/j.visres.2023.108221
Seltman, W. (2023, September 1). What Is Color Blindness? WebMD; WebMD.
https://www.webmd.com/eye-health/colorblindness
Semba, C., & Gadek, T. (2016). Development of lifitegrast: a novel T-cell inhibitor for the treatment of dry eye disease. Clinical Ophthalmology , 2016:10 , 1083.
https://doi.org/10.2147/opth.s110557
Shao, W., Niu, Y., Wang, S., Mao, J., Xu, H., Wang, J., Zhang, C., & Guo, L. (2023). Effects of virtual reality on the treatment of amblyopia in children: A systematic review and meta-analysis.
Journal of Pediatric Nursing , 72 , 106–112.
https://doi.org/10.1016/j.pedn.2023.07.014
Shareef, O., Shareef, S. M., & Saeed, H. N. (2023). New Frontiers in Acanthamoeba Keratitis Diagnosis and Management. Biology , 12(12), 1489–1489.
https://doi.org/10.3390/biology12121489
Sharif, N. A. (2023). Elevated Intraocular Pressure and Glaucomatous Optic Neuropathy: Genes to Disease Mechanisms, Therapeutic Drugs, and Gene Therapies. Pharmaceuticals , 16(6), 870–870.
https://doi.org/10.3390/ph16060870
Sharma, R., Khristov, V., Rising, A., Jha, B. S., Dejene, R., Hotaling, N., Li, Y., Stoddard, J., Stankewicz, C., Wan, Q., Zhang, C., Campos, M. M., Miyagishima, K. J., McGaughey, D., Villasmil, R., Mattapallil, M., Stanzel, B., Qian, H., Wong, W., & Chase,
WilliamA.Haseltine,PhD 345
L. (2019). Clinical-grade stem cell–derived retinal pigment epithelium patch rescues retinal degeneration in rodents and pigs. Science Translational Medicine , 11(475), eaat5580.
https://doi.org/10.1126/scitranslmed.aat5580
Shi, Y., Hu, Y., Jiang, N., & Yetisen, A. K. (2022). Fluorescence Sensing Technologies for Ophthalmic Diagnosis. ACSSensors
https://doi.org/10.1021/acssensors.2c00313
Shi, Y., Li, X., & Yang, J. (2022). Mutations of CX46/CX50 and Cataract Development. Frontiers in Molecular Biosciences , 9 .
https://doi.org/10.3389/fmolb.2022.842399
Shih, V., Parekh, M., Multani, J. K., McGuiness, C. B., Chen, C.C., Campbell, J. H., Miller-Ellis, E., & Olivier, M. M. G. (2021). Clinical and Economic Burden of Glaucoma by Disease Severity. Ophthalmology Glaucoma .
https://doi.org/10.1016/j.ogla.2020.12.007
Simó, R., Sundstrom, J. M., & Antonetti, D. A. (2014). Ocular AntiVEGF Therapy for Diabetic Retinopathy: The Role of VEGF in the Pathogenesis of Diabetic Retinopathy. Diabetes Care , 37(4), 893–899.
https://doi.org/10.2337/dc13-2002
Singh, I. P. (2017). NovaBay’s Avenova Offers Key Benefits in Glaucoma Care .
https://cdn.shopify.com/s/files/1/0569/8895/8888/files/Dr._Sing h_-
_Avenova_Offers_Key_Benefits_in_Glaucoma_Care.pdf?v=16 74259302
Singh, M. S., & MacLaren, R. E. (2018). Stem Cell Treatment for Age-Related Macular Degeneration: the Challenges.
BetterEyesight 346
Investigative Ophthalmology & Visual Science , 59(4), AMD78–AMD82.
https://doi.org/10.1167/iovs.18-24426
Sızmaz, S., Yonekawa, Y., & T. Trese, M. (2015). Familial Exudative Vitreoretinopathy. Turkish Journal of Ophthalmology , 45(4), 164–168.
https://doi.org/10.4274/tjo.67699
Slentz, D. H., Hemmati, H. D., Scott, I. U., & Fekrat, S. (2013, December 1). Management of Stevens-JohnsonSyndrome and Toxic Epidermal Necrolysis . American Academy of Ophthalmology.
https://www.aao.org/eyenet/article/management-ofstevensjohnson-syndrome-toxic-epider-2
Snyder, P. J., Alber, J., Alt, C., Bain, L. J., Bouma, B. E., Bouwman, F. H., DeBuc, D. C., Campbell, M. C. W., Carrillo, M. C., Chew, E. Y., Cordeiro, M. F., Dueñas, M. R., Fernández, B. M., Koronyo-Hamaoui, M., La Morgia, C., Carare, R. O., Sadda, S. R., van Wijngaarden, P., & Snyder, H. M. (2021). Retinal imaging in Alzheimer’s and neurodegenerative diseases. Alzheimer’s & Dementia : The Journal of the Alzheimer’s Association , 17(1), 103–111. https://doi.org/10.1002/alz.12179
Solo Eyewear. (2012, February 3). Aravind Eye Hospital . SOLO Eyewear. https://www.soloeyewear.com/blogs/news/5474302aravind-eye-hospital
Somani, S. N., Ronquillo, Y., & Moshirfar, M. (2021). Acanthamoeba Keratitis . PubMed; StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK549863/
Soomro, T., Shah, N., Niestrata-Ortiz, M., Yap, T., Normando, E. M., & Cordeiro, M. F. (2020). Recent advances in imaging
WilliamA.Haseltine,PhD 347
technologies for assessment of retinal diseases. ExpertReviewof Medical Devices , 17(10), 1095–1108.
https://doi.org/10.1080/17434440.2020.1816167
Soucy, J. R., Aguzzi, E. A., Cho, J., Michael James Gilhooley, Keuthan, C., Luo, Z., Aboozar Monavarfeshani, Saleem, M. A., Wang, X.-W., Wohlschlegel, J., Fouda, A. Y., Ashok, A., Moshiri, A., Alain Chédotal, Reed, A. A., Amjad Askary, Su, A.J. A., Anna La Torre, Archana Jalligampala, & Ariadna SilvaLepe. (2023). Retinal ganglion cell repopulation for vision restoration in optic neuropathy: a roadmap from the RReSTORe Consortium. Molecular Neurodegeneration , 18(1).
https://doi.org/10.1186/s13024-023-00655-y
Sowlati-Hashjin, S., Carbone, P., & Karttunen, M. (2020). Insights into the Polyhexamethylene Biguanide (PHMB) Mechanism of Action on Bacterial Membrane and DNA: A Molecular Dynamics Study. TheJournalofPhysicalChemistryB , 124(22), 4487–4497.
https://doi.org/10.1021/acs.jpcb.0c02609
Spekker, E., Tanaka, M., Szabó, Á., & Vécsei, L. (2021). Neurogenic Inflammation: The Participant in Migraine and Recent Advancements in Translational Research. Biomedicines , 10(1), 76.
https://doi.org/10.3390/biomedicines10010076
Spring, K. R., Fellers, T. J., & Davidson, M. W. (2019). ThePhysics of Light and Color - Human Vision and Color Perception | Olympus Life Science Olympus-Lifescience.com.
https://www.olympus-lifescience.com/en/microscoperesource/primer/lightandcolor/humanvisionintro/
BetterEyesight 348
Sridhar, M. S. (2018). Anatomy of cornea and ocular surface. Indian Journal of Ophthalmology , 66(2), 190–194.
https://doi.org/10.4103/ijo.IJO_646_17
Sriram, P. K. (2022, October 18). Aurolab: India’s Revolution in Affordable Eye Care . American Academy of Ophthalmology.
https://www.aao.org/young-ophthalmologists/yoinfo/article/aurolab-india-revolution-affordable-eye-care-one
Staff, B. (n.d.). Vyjuvek (Beremagene Geperpavec) for Epidermolysis Bullosa . Epidermolysisbullosanews.com.
https://epidermolysisbullosanews.com/kb103/
Stavroula Dionysopoulou, Pernilla Wikström, Bucolo, C., Giovanni Luca Romano, Micale, V., Svensson, R., Dimitris Spyridakos, Mastrodimou, N., Georgakis, S., Panayotis Verginis, Walum, E., & Thermos, K. (2023). Topically Administered NOX4 Inhibitor, GLX7013114, Is Efficacious in Treating the Early Pathological Events of Diabetic Retinopathy. Diabetes , 72(5), 638–652.
https://doi.org/10.2337/db22-0515
Struck, M. C. (2015). Long-term Results of Pediatric Cataract Surgery and Primary Intraocular Lens Implantation From 7 to 22 Months of Life. JAMAOphthalmology , 133(10), 1180–1183. https://doi.org/10.1001/jamaophthalmol.2015.2062
Stuart, A. (2014, February 1). CurrentROPTherapies:HowLaser andAnti-VEGFCompare American Academy of Ophthalmology. https://www.aao.org/eyenet/article/currentrop-therapies-how-laser-antivegf-compare
Sun Yat-sen University, & ClinicalTrials.gov. (2021, March). ChinaOLIMPICS:ChinaOphthalmicLearning and Improvement Initiative in CataractSurgeryTrial - FullText
WilliamA.Haseltine,PhD 349
View - ClinicalTrials.gov . Clinicaltrials.gov.
https://classic.clinicaltrials.gov/ct2/show/NCT03458442
Tandon, R., Singh, R., Gupta, N., & Vanathi, M. (2019). Corneal transplantation in the modern era. IndianJournalofMedical Research , 150(1), 7.
https://doi.org/10.4103/ijmr.ijmr_141_19
Tartaglia, C. (2018, November 30). FateTherapeuticsAnnounces FDAClearanceofLandmarkINDforFT500iPSC-derived, Off-the-ShelfNKCellCancerImmunotherapy . Fate Therapeutics. https://ir.fatetherapeutics.com/newsreleases/news-release-details/fate-therapeutics-announces-fdaclearance-landmark-ind-ft500
Tham, Y.-C., Li, X., Wong, T. Y., Quigley, H. A., Aung, T., & Cheng, C.-Y. (2014). Global Prevalence of Glaucoma and Projections of Glaucoma Burden through 2040. Ophthalmology , 121(11), 2081–2090.
https://doi.org/10.1016/j.ophtha.2014.05.013
The American Heart Association. (2018, December). Theeyes haveit forhighbloodpressure clues . Www.heart.org.
https://www.heart.org/en/news/2018/12/13/the-eyes-have-it-forhigh-blood-pressure-clues
The AREDS Research Group. (2009). Change in Area of Geographic Atrophy in the Age-Related Eye Disease Study. ArchivesofOphthalmology , 127(9), 1168.
https://doi.org/10.1001/archophthalmol.2009.198
The AREDS Study Group. (n.d.). Age-RelatedEye Disease Studies(AREDS/AREDS2)|NationalEye Institute Www.nei.nih.gov. https://www.nei.nih.gov/research/clinicaltrials/age-related-eye-disease-studies-aredsareds2
BetterEyesight 350
The International Agency for the Prevention of Blindness (IAPB). (n.d.). ProjectedChangein VisionLoss 2020to 2050 . The International Agency for the Prevention of Blindness.
https://www.iapb.org/learn/vision-atlas/magnitude-andprojections/projected-change/
Thompson, A. C., Falconi, A., & Sappington, R. M. (2022). Deep learning and optical coherence tomography in glaucoma: Bridging the diagnostic gap on structural imaging. Frontiers in Ophthalmology , 2 .
https://doi.org/10.3389/fopht.2022.937205
Thompson, A. C., Jammal, A. A., & Medeiros, F. A. (2020). A Review of Deep Learning for Screening, Diagnosis, and Detection of Glaucoma Progression. TranslationalVision Science &Technology , 9(2), 42.
https://doi.org/10.1167/tvst.9.2.42
Thuma, T., Rosenberg, E., & Jeng, B. H. (2021, January 1). A Primeron Stevens-JohnsonSyndrome . American Academy of Ophthalmology. https://www.aao.org/eyenet/article/a-primeron-stevens-johnson-syndrome
Titiyal, J. S., Falera, R. C., Kaur, M., Sharma, V., & Sharma, N. (2018). Prevalence and risk factors of dry eye disease in North India: Ocular surface disease index-based cross-sectional hospital study. IndianJournalofOphthalmology , 66(2), 207–211.
https://doi.org/10.4103/ijo.IJO_698_17
Tuli, S., & Gray, M. (2016). Surgical management of corneal infections. CurrentOpinioninOphthalmology , 27(4), 340–347.
https://doi.org/10.1097/ICU.0000000000000274
Tung, T.-H., Shih, H.-C., Chen, S.-J., Chou, P., Liu, C.-M., & Liu, J.-H. (2008). Economic evaluation of screening for
WilliamA.Haseltine,PhD 351
diabetic retinopathy among Chinese type 2 diabetics: a community-based study in Kinmen, Taiwan. Journalof Epidemiology , 18(5), 225–233.
https://doi.org/10.2188/jea.je2007439
Turbert, D. (2018, April 27). WhatIsOpticalCoherence Tomography?American Academy of Ophthalmology.
https://www.aao.org/eye-health/treatments/what-is-opticalcoherence-tomography
Ungar, L., & Frisaro, F. (2023, July 24). Genetherapyeyedrops restoreda boy’ssight.Similartreatments couldhelpmillions
AP News.
https://apnews.com/article/gene-therapy-blindnessrare-diseases-58f81838894dfb8568affde0b7e4d2f1
University of California San Francisco. (2021, January).
AmblyopiaandVisualDevelopment . Horton Lab.
https://hortonlab.ucsf.edu/blog/amblyopia-and-visualdevelopment
Valenzuela, R. A., Flores, I., Urrutia, B., Fuentes, F., Sabat, P. E., Llanos, C., Cuitino, L., & Urzua, C. A. (2020). New Pharmacological Strategies for the Treatment of NonInfectious Uveitis. A Minireview. Frontiers inPharmacology , 11 .
https://doi.org/10.3389/fphar.2020.00655
Vashist, P., Gupta, N., Singh, S., & Saxena, R. (2011). Role of early screening for diabetic retinopathy in patients with diabetes mellitus: An overview. IndianJournalofCommunity Medicine , 36(4), 247.
https://doi.org/10.4103/0970-0218.91324
Visibly’sApproachto theFuture ofEyecare - ACallto Action (2022, November 2). Visibly - the World’s First Online Vision
BetterEyesight 352
Test. https://www.govisibly.com/2022/11/visiblys-approach-tothe-future-of-eyecare-a-call-to-action/
Vision Center, & Huang, M. (2023, September 13). Costof LASIKEyeSurgeryin 2021(With&WithoutInsurance) . Vision Center. https://www.visioncenter.org/lasik/cost/
Waghmare, S. V., & Jeria, S. (2022). A Review of Contact LensRelated Risk Factors and Complications. Cureus .
https://doi.org/10.7759/cureus.30118
Wang, D., Li, J., Luo, G., Zhou, J., Wang, N., Wang, S., Zhao, R., Cao, X., Ma, Y., Liu, G., & Hao, L. (2023). Nox4 as a novel therapeutic target for diabetic vascular complications. Redox Biology , 64 , 102781.
https://doi.org/10.1016/j.redox.2023.102781
Wang, J. W., Rixen, J. J., Goins, K. M., & Kitzmann, A. S. (2014). OcularManifestationsofStevens-JohnsonSyndrome . Uiowa.edu.
https://webeye.ophth.uiowa.edu/eyeforum/cases/192-StevensJohnson.htm
Wang, J.-H., Roberts, G. E., & Liu, G.-S. (2020). Updates on Gene Therapy for Diabetic Retinopathy. CurrentDiabetes Reports , 20(7).
https://doi.org/10.1007/s11892-020-01308-w
Wang, P., Chin, E. K., & Almeida, D. (2021). Antioxidants for the Treatment of Retinal Disease: Summary of Recent Evidence. ClinicalOphthalmology , Volume15 , 1621–1628.
https://doi.org/10.2147/opth.s307009
Wang, W., Yan, W., Fotis, K., Prasad, N. M., Lansingh, V. C., Taylor, H. R., Finger, R. P., Facciolo, D., & He, M. (2016).
WilliamA.Haseltine,PhD 353
Cataract Surgical Rate and Socioeconomics: A Global Study. InvestigativeOphthalmology&VisualScience , 57(14), 5872–5881.
https://doi.org/10.1167/iovs.16-19894
Wang, Z., Li, Z., Li, K., Mu, S., Zhou, X., & Yu, D. (2023). Performance of artificial intelligence in diabetic retinopathy screening: a systematic review and meta-analysis of prospective studies. Frontiers inEndocrinology , 14
https://doi.org/10.3389/fendo.2023.1197783
Ward, R. J., Ashraf, M., Wuerger, S., & Marshall, A. (2023). Odors modulate color appearance. Frontiers inPsychology , 14
https://doi.org/10.3389/fpsyg.2023.1175703
Wei, A., Yin, D., Zhai, Z., Ling, S., Le, H., Tian, L., ... & Hong, J. (2023). In vivo CRISPR gene editing in patients with herpes stromal keratitis. medRxiv , 2023-02.
Wei, A., Yin, D., Zhai, Z., Ling, S., Le, H., Tian, L., Xu, J., Paludan, S. R., Cai, Y., & Hong, J. (2023). In vivo CRISPR gene editing in patients with herpetic stromal keratitis. MolecularTherapy:TheJournaloftheAmericanSocietyof GeneTherapy , 31(11), 3163–3175.
https://doi.org/10.1016/j.ymthe.2023.08.021
Welbourne, L. (2016). Peripheralfactorsaffectinghumancolour perception .
https://etheses.whiterose.ac.uk/14319/1/LaurenWelbourne_Ph D_Thesis_Corrected.pdf
Willcox, M. D. P. (2013). Characterization of the normal microbiota of the ocular surface. ExperimentalEye Research , 117 , 99–105.
https://doi.org/10.1016/j.exer.2013.06.003
BetterEyesight 354
Williams, K. A., Muehlberg, S. M., Lewis, R. F., & Coster, D. J. (1995). How successful is corneal transplantation? A report from the Australian corneal graft register. Eye , 9(2), 219–227.
https://doi.org/10.1038/eye.1995.43
Willis, K. A., Postnikoff, C. K., Freeman, A., Rezonzew, G., Nichols, K., Gaggar, A., & Lal, C. V. (2020). The closed eye harbours a unique microbiome in dry eye disease. Scientific Reports , 10(1), 12035.
https://doi.org/10.1038/s41598-02068952-w
Wilmer, J. B., & Backus, B. T. (2009). Genetic and environmental contributions to strabismus and phoria: evidence from twins. VisionResearch , 49(20), 2485–2493.
https://doi.org/10.1016/j.visres.2009.08.006
Wisse, R. P. L., Muijzer, M. B., Cassano, F., Godefrooij, D. A., Prevoo, Y. F. D. M., & Soeters, N. (2019). Validation of an Independent Web-Based Tool for Measuring Visual Acuity and Refractive Error (the Manifest versus Online Refractive Evaluation Trial): Prospective Open-Label Noninferiority Clinical Trial. JournalofMedicalInternet Research , 21(11), e14808.
https://doi.org/10.2196/14808
Wittig-Silva, C., Chan, E., Islam, F. M. A., Wu, T., Whiting, M., & Snibson, G. R. (2014). A Randomized, Controlled Trial of Corneal Collagen Cross-Linking in Progressive Keratoconus. Ophthalmology , 121(4), 812–821.
https://doi.org/10.1016/j.ophtha.2013.10.028
Wolpert, K., & Tsang, S. (2011). Electroretinography. In www.intechopen.com . IntechOpen.
https://www.intechopen.com/chapters/17262
WilliamA.Haseltine,PhD 355
Wong, E. N., & Mehta, J. S. (2022). Cell therapy in corneal endothelial disease. CurrentOpinioninOphthalmology , 33(4), 275–281. https://doi.org/10.1097/icu.0000000000000853
Wong, J. O., Puente, M. A., Bunya, V. Y., Halfpenny, C., Syed, Z. A., & Patel , R. (2023, October 3). CornealDonationEyeWiki Eyewiki.aao.org.
https://eyewiki.aao.org/Corneal_Donation
Wong, W. L., Su, X., Li, X., Cheung, C. M. G., Klein, R., Cheng, C.-Y., & Wong, T. Y. (2014). Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: a systematic review and meta-analysis. TheLancet GlobalHealth , 2(2), e106–e116. https://doi.org/10.1016/s2214109x(13)70145-1
Wood, J. (2023, May). DOYOUSEEWHAT I SEE?ALOOK
ATCOLORDEFICIENCIESINKANSAS .
https://soar.wichita.edu/server/api/core/bitstreams/a222c5d8cd9c-491f-8079-0aed1d4c6bd8/content
World Health Organization. (2019, October 8). Worldreport on vision . Www.who.int.
https://www.who.int/publications/i/item/9789241516570
World Health Organization. (2023, August 10). Blindnessand VisionImpairment . World Health Organization.
https://www.who.int/news-room/fact-sheets/detail/blindnessand-visual-impairment
Woudstra-de Jong, J. E., Manning-Charalampidou, S. S., Vingerling, H., Busschbach, J. J., & Pesudovs, K. (2023).
Patient-reported outcomes in patients with vitreous floaters: A
BetterEyesight 356
systematic literature review. SurveyofOphthalmology , 68(5), 875–888. https://doi.org/10.1016/j.survophthal.2023.06.003
Wu, G., Tien, K., Zhao, W., Cheng, E., & Lee, D. A. (2023). Can AI chatbots provide accurate information about retinal floaters for our patients? InvestigativeOphthalmology&Visual Science , 64(8), 4204–4204.
https://iovs.arvojournals.org/article.aspx?articleid=2790033
Xiang, Y., Wang, X., Cao, X., Fang, W., Chen, Y., Ran, J., Long, Z., Tan, Q., Lai, Z., Liu, L., Zhao, D., Li, X., Tang, B., Wan, W., & Hu, K. (2023). Efficacy of cataract surgeries performed during blindness prevention programs in Chongqing, China: a multicenter prospective study. BMCOphthalmology , 23(1).
https://doi.org/10.1186/s12886-023-03082-1
Xiaoxi, M., Wang, X., Xiao, Y., & Zhao, Q. (2022a). Retinal examinationmodalitiesin theearlydetectionofAlzheimer’s disease:Seeingbrainthroughtheeye. 10(3), 185–187.
https://doi.org/10.2478/jtim-2021-0053
Xiaoxi, M., Wang, X., Xiao, Y., & Zhao, Q. (2022b). Retinal examination modalities in the early detection of Alzheimer’s disease: Seeing brain through the eye. JournalofTranslational InternalMedicine , 10(3), 185–187.
https://doi.org/10.2478/jtim-2021-0053
Xue, W., Li, J. J., Zou, Y., Zou, B., & Wei, L. (2021). Microbiota and ocular diseases. Frontiers in cellularandinfection microbiology , 1047.
Xu, X., Ma, Y.-Y., & Zou, H.-D. (2016). Cost-Utility Analysis of Cataract Surgery in Advanced Glaucoma Patients. Journalof
WilliamA.Haseltine,PhD 357
Glaucoma , 25(7), e657–e662.
https://doi.org/10.1097/ijg.0000000000000313
Xue, W., Li, J. J., Zou, Y., Zou, B., & Wei, L. (2021). Microbiota and Ocular Diseases. Frontiers in CellularandInfection Microbiology , 11 .
https://doi.org/10.3389/fcimb.2021.759333
Yamanaka factors. (n.d.). Longevity.Technology - LatestNews, Opinions,AnalysisandResearch .
https://longevity.technology/yamanaka-factors/amp/
Yang, J.-J., Huang, C.-H., Yang, C.-H., Yang, C.-M., Lin, C.-W., Ho, T.-C., Lin, C.-P., Hsieh, Y.-T., Yeh, P.-T., Lai, T.-T., Chen, P.-L., & Chen, T.-C. (2021). The Clinical Contribution of Full-Field Electroretinography and 8-Year Experiences of Application in a Tertiary Medical Center. Journalof PersonalizedMedicine , 11(10), 1022.
https://doi.org/10.3390/jpm11101022
Yasir, M., & Sonthalia, S. (2019, March 24). Corticosteroid AdverseEffects . Nih.gov; StatPearls Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK531462/
Yin, D., Ling, S., Wang, D., Dai, Y., Jiang, H., Zhou, X., Paludan, S. R., Hong, J., & Cai, Y. (2021). Targeting herpes simplex virus with CRISPR–Cas9 cures herpetic stromal keratitis in mice. NatureBiotechnology , 39(5), 567–577.
https://doi.org/10.1038/s41587-020-00781-8
Ying, M., Wang, H., Liu, T., Han, Z., Lin, K., Shi, Q., Zheng, N., Ye, T., Gong, H., & Xu, F. (2023). CLEAR Strategy Inhibited HSV Proliferation Using Viral Vectors Delivered CRISPRCas9. Pathogens , 12(6), 814–814.
https://doi.org/10.3390/pathogens12060814
BetterEyesight 358
Yue, L., Castillo, J., Gonzalez, A. C., Neitz, J., & Humayun, M. S. (2021). Restoring Color Perception to the Blind. Ophthalmology , 128(3), 453–462.
https://doi.org/10.1016/j.ophtha.2020.08.019
Zadnik, K., Schulman, E., Flitcroft, I., Fogt, J. S., Blumenfeld, L. C., Fong, T. M., Lang, E., Hemmati, H. D., & Chandler, S. P. (2023). Efficacy and Safety of 0.01% and 0.02% Atropine for the Treatment of Pediatric Myopia Progression Over 3 Years. JAMAOphthalmology .
https://doi.org/10.1001/jamaophthalmol.2023.2097
Zhang, A. C., Singh, S., Craig, J. P., & Downie, L. E. (2020). Omega-3 Fatty Acids and Eye Health: Opinions and SelfReported Practice Behaviors of Optometrists in Australia and New Zealand. Nutrients , 12(4), 1179.
https://doi.org/10.3390/nu12041179
Zhang, L., Tang, L., Xia, M., & Cao, G. (2023). The application of artificial intelligence in glaucoma diagnosis and prediction. Frontiers inCellandDevelopmentalBiology , 11 .
https://doi.org/10.3389/fcell.2023.1173094
Zhao, L., Chen, X.-J., Zhu, J., Xi, Y.-B., Yang, X., Hu, L.-D., Ouyang, H., Patel, S. H., Jin, X., Lin, D., Wu, F., Flagg, K., Cai, H., Li, G., Cao, G., Lin, Y., Chen, D., Wen, C., Chung, C., & Wang, Y. (2015). Lanosterol reverses protein aggregation in cataracts. Nature , 523(7562), 607–611.
https://doi.org/10.1038/nature14650
Zhao, Y., & Singh, R. P. (2018). The role of anti-vascular endothelial growth factor (anti-VEGF) in the management of
WilliamA.Haseltine,PhD 359
proliferative diabetic retinopathy. Drugs in Context , 7 , 1–10.
https://doi.org/10.7573/dic.212532
Zou, M., Jin, R., Hu, Y., Zhang, Y., Wang, H., Liu, G., Nie, Y., & Wang, Y. (2019). A thermo-sensitive, injectable and biodegradable in situ hydrogel as a potential formulation for uveitis treatment.
JournalofMaterialsChemistryB , 7(28), 4402–4412.
https://doi.org/10.1039/C9TB00939F
BetterEyesight 360