PATIENT CARE AND HUMANITARIAN EFFORTS IN GAZA P.26
FRESH FACES: FINDING JOY IN PEDIATRIC PRACTICE P.30
TRANSFORMATIONS: A BIKER’S QUICK RECOVERY POSTAMPUTATION P.34


PATIENT CARE AND HUMANITARIAN EFFORTS IN GAZA P.26
FRESH FACES: FINDING JOY IN PEDIATRIC PRACTICE P.30
TRANSFORMATIONS: A BIKER’S QUICK RECOVERY POSTAMPUTATION P.34

Powered exoskeletons and orthoses expand options for patients with limb difference P.16

THE PREMIER MEETING FOR ORTHOTIC, PROSTHETIC, AND PEDORTHIC









September 3–6, 2025, for an ideal combination of top-notch education and entertainment at the 108th AOPA National Assembly in Orlando, FL, at the Orange County Convention Center (OCCC).










EXHIBITS EDUCATION NETWORKING
Submit a presentation by March 12 to present.














Join our community of satisfied users and experience the difference.

Orthotists have an opportunity to play a key role in treating patients who benefit from powered orthoses and exoskeletons now that some of these devices qualify for Medicare reimbursement. Learn which types of devices are already being used in-home by some patients, what devices are under development, and how devices that offer powered assistance are a game changer for some individuals with limb difference.
By CHRISTINE UMBRELL

O&P professionals and humanitarian organizations are responding to a patient-care crisis in Gaza, where more than 10,000 new amputees need care following the destruction of the region’s only prosthetics hospital. Read about current aid efforts, challenges in delivering supplies, and ways that O&P professionals can contribute to these humanitarian efforts.
By JENNIFER DAVIS




Meet Steven Slawinski, CO, LO, FAAOP, who says treating cranial and scoliosis patients inspires him and spurs involvement in O&P advocacy initiatives.
Mike Zimmerman, CPO, LPO, set a fast but safe pace when treating a physically fit construction foreman who lost his leg after a motorcycle accident last year.


President
Rick Riley
O&P Boost, Bakersfield, CA
President-Elect
Kimberly Hanson, CPRH Ottobock, Austin, TX
Vice President
Matt Swiggum Proteor, Tempe, AZ
Treasurer
Chris Nolan
Össur, Foothills Ranch, CA
Immediate Past President
Mitchell Dobson, CPO Hanger Clinic, Austin, TX
Interim Executive Director
Teri Kuffel, JD
Arise Orthotics & Prosthetics, Spring Lake Park, MN
DIRECTORS
Jeff Erenstone, CPO
Mountain Orthotic and Prosthetic Services, Lake Placid, NY
Deanna Fish, MS, CPO Orthomerica Products Inc., Orlando, FL
Arlene Gillis, MEd, CP, LPO International Institute of Orthotics and Prosthetics, Tampa, FL
Adrienne Hill, MHA, CPO, LPO, FAAOP Kennesaw State University, Kennesaw, GA
Shane Kelly
Thuasne North America, Bakersfield, CA
Jim Kingsley
Hanger Clinic, Oak Brook Terrace, IL
Andrew L. Steele, MBA, CPO, LPO Clark & Associates Prosthetics and Orthotics, Waterloo, IA
Shane Wurdeman, PhD, CP, FAAOP(D) Research Chair
Hanger Clinic, Houston Medical Center, Houston, TX
AMERICAN ORTHOTIC & PROSTHETIC ASSOCIATION (AOPA)
330 John Carlyle St., Ste. 200 Alexandria, VA 22314 Office: 571-431-0876 Fax: 571-431-0899 AOPAnet.org
EXECUTIVE OFFICES
Teri Kuffel, JD, interim executive director, 571-431-0876, executivedirector@AOPAnet.org
Akilah Williams, MBA, SHRM-CP, director of finance and strategic operations, 571-431-0819, awilliams@AOPAnet.org
HEALTH POLICY AND ADVOCACY
Joe McTernan, director of health policy and advocacy, 571-431-0811, jmcternan@AOPAnet.org
Devon Bernard, assistant director of coding and reimbursement services, education, and programming, 571-431-0854, dbernard@AOPAnet.org
Morgan Fabber, MPH, manager of state and federal advocacy, 571-431-0814, mfabber@ AOPAnet.org
MEETINGS & EDUCATION
Ashley Vande Bunte, CMP, director, meetings and education, 571/431-0860, avandebunte@AOPAnet.org
Kelly O’Neill, CEM, assistant director, meetings and exhibitions, 571-431-0852, kelly.oneill@AOPAnet.org
Jules Gohng, meetings and education coordinator, 571-431-0843, jgohng@AOPAnet.org
MEMBERSHIP & COMMUNICATIONS
Joy Klapp, director of communications and membership, 571-431-0817, jklapp@AOPAnet.org
Betty Leppin, senior manager of member services, 571-431-0810, bleppin@AOPAnet.org
Madison McTernan, coordinator of membership and communications, 571-431-0852, mmcternan@AOPAnet.org
AOPA Bookstore: 571-431-0876
Reimbursement/Coding: 571-431-0833, LCodeSearch.com
O&P ALMANAC
AOPA, publisher
Josephine Rossi, editor, 703-662-5828, jrossi@contentcommunicators.com
Catherine Marinoff, art director, 786-252-1667, catherine@marinoffdesign.com
Bob Heiman, director of sales, 856-520-9632, bob.rhmedia@comcast.net
Christine Umbrell, editorial/production associate and contributing writer, 703-662-5828, cumbrell@contentcommunicators.com
PUBLISHER AOPA
EDITORIAL MANAGEMENT CONTENT
COMMUNICATORS LLC
ADVERTISING SALES RH MEDIA LLC
DESIGN & PRODUCTION MARINOFF DESIGN LLC
PRINTING SHERIDAN
O&P Almanac (ISSN: 1061-4621) is published bimonthly by the American Orthotic & Prosthetic Association, 330 John Carlyle St., Ste. 200, Alexandria, VA 22314. To subscribe, contact 571-431-0876, fax 571-431-0899, or email info@ aopanet.org. Yearly subscription rates: $59 domestic, $99 foreign. All foreign subscriptions must be prepaid in U.S. currency, and payment should come from a U.S. affiliate bank. A $35 processing fee must be added for non-affiliate bank checks. O&P Almanac does not issue refunds. Periodical postage paid at Alexandria, VA, and additional mailing offices.
Postmaster: Send address changes to: O&P Almanac 330 John Carlyle St., Ste. 200, Alexandria, VA 22314.
Copyright © 2025 American Orthotic and Prosthetic Association. All rights reserved. This publication may not be copied in part or in whole without written permission from the publisher. The opinions expressed by authors do not necessarily reflect the official views of AOPA, nor does the association necessarily endorse products shown in the O&P Almanac. The O&P Almanac is not responsible for returning any unsolicited materials. All letters, press releases, announcements, and articles submitted to the O&P Almanac may be edited for space and content. The magazine is meant to provide accurate, authoritative information about the subject matter covered. It is provided and disseminated with the understanding that the publisher is not engaged in rendering legal or other professional services. If legal advice and/or expert assistance is required, a competent professional should be consulted.
Share your message with AOPA membership— approximately 9,000 orthotic and prosthetic professionals, facility owners, and industry personnel. Contact Bob Heiman at 856-520-9632 or email bob.rhmedia@comcast.net. Learn more at bit.ly/AlmanacMediaKit25.








2.4%
2.4% FOR 2025
CMS in December released the official 2025 Medicare fee schedule for durable medical equipment, prosthetics, orthotics, and supplies. The fee schedule is effective for Medicare claims with a date of service on or after Jan. 1, 2025. As anticipated, the 2025 Medicare fee schedule for orthotic and prosthetic services increased by 2.4%. This represents a 3.0% increase in the Consumer Pricing Index for Urban Areas from June 2023 to June 2024, minus the total factor productivity adjustment of 0.6%.
A landmark study examining the extent to which microprocessor-controlled knee (MPK) provision to the level-K2 population of limb loss patients may be cost effective has been published by a team of recognized researchers that includes Allen Dobson, PhD, Joan Davanzo, PhD, and Andreas Kannenberg, MD (GER), PhD. The team conducted a retrospective cohort study using Medicare fee-for-service claims data from CMS.
Beneficiaries included in the study had a unilateral above-knee amputation and had been fit with a non-MPK (NMPK) prosthesis between Oct. 1, 2016, and Dec. 31, 2020. The researchers determined the K levels of each patient by studying the K modifiers. Because Medicare did not cover MPKs for K2 beneficiaries during that timeframe, only K2 NMPK and K3 MPK beneficiaries were included in the analysis. Propensity score weighting using inverse probability treatment weights was used to balance beneficiary characteristics.
The researchers used medical and prosthetic device cost analyses as the basis for a Congressional Budget Office-style score, which modeled, over a 10-year


period, the economic impact to Medicare of covering MPKs for the K2 population.
Providing MPKs to K2 beneficiaries who qualified for the technology would reduce the number of injured fallers by 18.5% and result in medical savings of $1,351 cost per member, per month, which amortizes the cost of the technology in 19 months, according to the study. “Medicare would save $410.3 million over 10 years if the K2 population was provided coverage of MPK prostheses,” reported the authors. The study was published in Prosthetics and Orthotics International in December.
To examine racial disparities— differences in healthcare access between racial groups—in lowerlimb prosthesis prescription practices among U.S. veterans, researchers from the Brown University School of Public Health and Providence VA Medical Center conducted a retrospective cohort analysis.
The team, led by Linda Resnik, PT, PhD, FAPTA, and Anthony I. Roberts, MS, studied the records of 12,143 White and 4,711 Black veterans who had undergone major lower-limb amputation between 2010 and 2022 in a veteran healthcare facility.
Nearly 12,000 veterans (11,969) had undergone transtibial amputation, and 4,885 had undergone transfemoral amputation.
Nationally, more than half (54.5%) of the veterans with limb loss had received a lower-limb prosthesis
prescription within 12 months of amputation. The researchers identified several racial disparities: Individuals with transfemoral limb loss faced greater racial disparities in prosthesis prescription. They also found that geographic variations in racial disparities exist at both regional and local levels.
“Significant geographic variations exist in racial disparities for lower-limb prosthesis prescriptions … with most areas favoring White veterans,” reported the authors. “Disparities were more pronounced for veterans with transfemoral amputations, highlighting the need for targeted interventions to improve equity in access to prosthetic care, especially for veterans with more proximal amputations and in regions and [areas] with the largest disparities.” The study was published in December in Archives of Physical Medicine and Rehabilitation
AOPA has announced a donation of $1 million over the next five years to the Orthotics and Prosthetics Foundation for Education and Research (O&P Foundation). This contribution underscores AOPA’s unwavering commitment to advancing innovation, education, and research in the O&P profession.

The donation will support the O&P Foundation’s mission to advance the art and science of orthotic and prosthetic rehabilitation by enhancing clinical practices through professional training awards, promoting educational opportunities through academic scholarships, strengthening the body of knowledge through research grants and fellowships, and inspiring excellence through recognition of scholarly achievements.

“AOPA’s mission has always been to strengthen the O&P profession,” said AOPA President Rick Riley. “On behalf of our members, AOPA’s Board of Directors approved this substantial multiyear donation to demonstrate the association’s commitment to a longterm strategic partnership with the O&P Foundation. We encourage others to similarly demonstrate their trust and support by donating to the O&P Foundation. Together we can accelerate research, education and training that will benefit O&P professionals and their patients in the future.”
“We are incredibly grateful for AOPA’s generous support,” said Chris Fairman, CPO, chair of the O&P Foundation. “This investment will enable us to expand our efforts and reflects a shared vision of elevating clinical standards, expanding educational opportunities, and strengthening the body of knowledge through research initiatives that directly benefit the patients we serve.”
with questions, bleppin@aopanet.org.

“POP and circumstance”
Ask local officials to declare March as POP Month or designate a POP Day.
On the heels of POP Month is Limb Loss and Limb Difference Awareness Month in April, so start making plans to demonstrate how the limb loss community thrives and determine how your facility can participate during April.
The Occupational Safety and Health Administration (OSHA) launched a Severe Injury Report Dashboard in September featuring reports of severe workrelated injuries. Between Jan. 1, 2015, and April 30, 2024, a total of 24,188 workers experienced workplace-related amputation, as reported to OSHA. Access the dashboard to view yearly totals and geographical breakdowns at osha.gov/severeinjury-reports
Innovative healthcare models, such as telehealth, would aid in meeting the growing demand for O&P services, but many facilities are not engaging in this type of care, according to researchers from La Trobe University. The researchers explored the perspectives of orthotists and prosthetists to identify barriers and facilitators influencing the use of telehealth in the United States, and subsequently published a 23-page guide, “Telehealth for the O&P Profession.”
O&P care. However, some providers reported they offer the full spectrum of O&P care using telehealth, including initial consults, education, and even device delivery.
The researchers contacted orthotists and prosthetists certified by the American Board for Certification in Orthotics, Prosthetics, and Pedorthics and conducted 45-minute interviews with 30 clinicians. They found that many practitioners did not have a full understanding of telehealth, which limited their ability to see its value or discuss reimbursement or compliance with privacy regulations. Approximately one-third perceived they did not use telehealth to provide
The researchers recommended that O&P facilities consider best practices when developing telehealth procedures, focusing on scheduling, providing patients with clear instructions for each appointment, embedding processes that ensure timely communication, and developing policies that govern how health information and images are received and stored. “The profession requires a clear and strategic position on reimbursement for telehealth,” noted the researchers, as reimbursement was consistently described as a barrier to engaging in telehealth practices. The research team leveraged information from the interviews to create the “Telehealth for the O&P Profession” guide. The full study was published in October in PLOS One
The global compression therapy market size was valued at $4.18 billion in 2024 and is projected to reach $4.49 billion in 2025 and $6.72 billion by 2033.













CMS released a bulletin in January that outlines new Healthcare Common Procedure Coding System (HCPCS) Level II final coding, benefit category, and payment determinations for partial hand and finger prostheses, which are expected to become effective April 1. A collaborative team, led by Chris Baschuk, MPO, CPO, FAAOP(D), and involving AOPA, the O&P Alliance, the American Academy of Orthotists and Prosthetists (AAOP), Össur, Hanger, and other organizations, worked to advocate for and finalize the new codes.
The newly established codes address gaps in the HCPCS system by accurately describing the distinct components and fabrication processes essential for partial hand and finger prostheses. The finalized codes allow providers to bill for items such as diagnostic sockets and replacement sockets and bring the coding structure for partial hand prosthesis sockets and addition codes in line with other amputation levels. These elements in the fitting process previously had no consistent way of being covered by insurance and align with advancements in clinical practices and prosthetic technology, allowing for appropriate categorization and billing and improved patient care.
COST OF EMPLOYER PLANS ROSE 7% IN 2024
Family premiums for employersponsored health insurance rose 7% last year to reach an average of $25,572 annually, with workers contributing $6,296 to the cost of family coverage.
SOURCE:
“We are thrilled with CMS’s decision to create distinct codes for partial hand and finger prostheses,” said Baschuk, director of clinical services for Point Designs and chair of the Upper-Limb Prosthetics Society of AAOP. “This is a win for patients and clinicians alike, as it not only validates the specialized clinical work involved but also lays the groundwork for equitable access to these transformative devices.”
Highlights of the final CMS determination include the following:
• New HCPCS Level II Codes: Seven new codes have been established, including L6037 for postsurgical fittings and L6028 as a new base code for partial hand prostheses. These codes reflect the specific materials, designs, and applications unique to partial hand prostheses.
• Revised Descriptions: Existing codes such as L6698 now include broader applicability, allowing for the inclusion of locking mechanisms for partial hand prostheses.
• Recognition of Unique Clinical Needs: CMS’s determination acknowledges that partial hand prostheses require the same level of clinical care, technical expertise, and materials as other upper-limb devices.
More than 1,600 O&P Hanger employees, exhibitors, and industry experts travelled to Nashville Jan. 27-30 to take part in Hanger LIVE 2025, which offered educational sessions on a range of hot topics, networking opportunities, and exhibits. This year’s event, with a theme of “Future FWD,” featured the first-ever Global Partners Summit. Highlights included keynote session from Kaiser Permanante’s Robert Sallis, MD, along with Hanger Clinic’s Clinical and Scientific Affairs team, who spoke on the importance of movement, evidencebased care, and outcomes.
Several AOPA leaders participated in Hanger LIVE, including AOPA Interim Executive Director Teri Kuffel, JD; AOPA President Rick Riley; AOPA

Immediate Past President Mitchell Dobson, CPO; AOPA President-Elect Kimberly Hanson, CPRH; and AOPA Board Member Adrienne Hill, MHA, CPO, LPO, FAAOP. Hanger’s annual Partner Awards recognized four outstanding companies for their roles in supplying

products and services used to provide O&P care and improve patient outcomes in 2024: Ottobock took home the inaugural Clinical Evidence Award, which recognizes a partner that made a meaningful contribution through evidencebased published research, ultimately improving patient outcomes.
Infinite Biomedical Technologies LLC was honored with the Collaboration Award, which is granted to a partner that made outstanding contributions resulting in shared success.
WillowWood received the Innovation Award, which recognizes a company that exhibited expansive thinking in product innovation and technology, resulting in positive clinical outcomes.
College Park was honored with the Operational Performance Award, which recognizes a partner that outperformed industry benchmarks in quality, efficiency, and cost containment.

Allard USA has added Robert Nilsson to its team. Nilsson has developed expertise in building lasting relationships, solving complex challenges, and consistently delivering value to clients and organizations alike. In the past, he managed multistate territories and drove sales within the financial sector. Nilsson will leverage his expertise and sales experience at Allard.
The Board of Certification/Accreditation (BOC) announced the Board of Directors’ 2025 Executive Committee. Cameron Stewart, BOCO, BOCP, co-founder of Alcam Medical Orthotics and Prosthetics in Riverside, California, is chair. “I am deeply honored to serve as chairman of the BOC Board of Directors,” said Stewart. “This organization plays a vital role in advancing the standards and recognition of excellence in orthotics, prosthetics, and durable medical equipment (DME). I look forward to continuing our mission and ensuring BOC credentials remain a symbol of quality, competence, and commitment to patient care.”
Other members of the BOC Executive Committee include Abel Guevara III, DHA, MHIM, eFACHDM, RHIA, mMBA, CPhT-Adv, CDME, vice president of DME for MedicusRx in Houston, who serves as vice chair; Angela Presley, PhD, BOCPD, COF, program manager of entrepreneurship at Dartmouth College in Hanover, New Hampshire, who serves as secretary; Daniel Griffis III, PharmD, pharmacist in charge for Rainbow Drugstore in Brunswick, Georgia, who serves as treasurer; and L. Bradley “Brad” Watson, BOCO, BOCP, LPO, past president and regional manager for Clarksville Limb and Brace Inc., a Bionic Co., in Clarksville, Tennessee, who serves as member-at-large.
Two individuals have been elected as new members of the BOC Board of Directors: Sangeeta Bhambhani, a regional manager and O&P practitioner for Bionic Prosthetics & Orthotics in Mishawaka, Indiana, and Diana Klunk, a BOC-certified mastectomy fitter for Perfect Match Boutique in Camp Hill, Pennsylvania.
BOC also announced that Immediate Past Chair Wayne R. Rosen, BOCP, BOCO, LPO, CDME, FAAOP, retired from the board in 2024. “Wayne has been an instrumental leader on our Board of Directors and an important advocate for BOC and the O&P profession,” said Judi Knott, MA, MBA, CAE, BOC’s president and chief executive officer. “Wayne’s professionalism and commitment to mentoring and developing others has been tremendous. We are thankful for his many contributions to BOC.”

Jonas Holmstedt has been named the new chief executive officer (CEO) of Allard USA. Holmstedt succeeds Dennis Williams, who has transitioned to the role of senior advisor. In this capacity, Williams will focus on acquisition opportunities and the continued growth of Allard SmartFAB services in Chattanooga, Tennessee.
Holmstedt’s initial introduction to Allard began in 2012 when he
served as an advising attorney for global distributor relations. In 2017, he officially joined the Allard companies as a board member of Camp Scandinavia, and in 2021 he served as a board member of Allard Support for Better Life. “I have had the privilege of working closely with Jonas on numerous projects over the past 12 years,” said Peter Allard, sole owner and president of privately held Allard Support for Better Life. “He deeply understands our mission … and consistently demonstrates exceptional leadership and a true passion for the industry we serve.”
Marie Holmstedt has been named president and grant program administrator of Dralla Foundation, a nonprofit organization founded by Peter Allard.

Shane Wurdeman, PhD, CP, FAAOP(D), has been named chief clinical officer at Hanger Clinic. In this position, he leads the company’s Clinical and Scientific Affairs (CSA) Team and the Hanger Institute. Wurdeman succeeds James Campbell, PhD, CO, FAAOP, who will focus on his role as president of Hanger Venture, Hanger’s subsidiary that invests in entrepreneurs and small businesses to bring innovative O&P healthcare solutions to the market.
Wurdeman previously served as vice president of scientific affairs at Hanger. He currently serves as research chair on AOPA’s Board of Directors. He also cofounded the Orthotics and Prosthetics Foundation for Education and Research.
“Shane has dedicated his career to evidence-based advancements that have improved the lives of thousands of patients, both at Hanger Clinic and beyond,” said Pete Stoy, Hanger chief executive officer. “He’s the ideal choice to succeed Dr. Campbell as the leader of our CSA and Institute teams as we continually strive to positively impact the patients we’re privileged to serve.”
“I am honored to take on this new role,” said Wurdeman, “and look forward to advancing the work of the CSA team and the Hanger Institute as part of our commitment to serve as a leader in the O&P field, using leading-edge research to advance clinical practice and improving patient outcomes globally.”
Coyote® O&P Inc. has acquired the exclusive rights to manufacture, sell, and distribute the products of 5280 Prosthetics, a prosthetic manufacturer based in Littleton, Colorado. This acquisition grants Coyote O&P exclusive access to 5280 Prosthetics’ intellectual property and products, effective Dec. 9, 2024.
“We are excited to add vacuum suspension products … to our suspension products lineup,” said Matt Perkins, chief executive officer of Coyote O&P. “The intellectual property and existing products help give us a full lineup of suspension options, and we have big plans for more products and suspension options using the 5280 technologies.”
BY DEVON BERNARD


Certain rules and guidelines should be followed when treating and communicating with patients who have deficits in hearing, vision, or speech, as well as those patients who have limited English proficiency (LEP). An individual with LEP is defined as a person whose primary language is not English and who has a limited ability to read, write, speak, or understand English. This limited ability may require some additional aids to ensure effective communication and understanding of the care being provided.
As a refresher, the Americans With Disabilities Act (ADA) is the governing rule as to when an interpreter is required and who is required to pay for their services.
Specifically, Section C, Part 360.303, of Title III, Auxiliary Aids and Services, offers this guidance. This section states that you have a duty to make available or provide appropriate aids or services, when they are needed, to provide effective communication with people who are deaf, have hearing loss, are blind, have vision loss, and/ or have a speech disability. Section 1557 of the Affordable Care Act (ACA) strengthens some of the provisions of the ADA regarding the meaningful use of aids and interpreters for patients with LEP.
Several aids and services are considered appropriate when treating patients with these types of impairments, and each has its own merits and limitations.
Some examples of appropriate aids and services for an individual who has hearing loss or is deaf include written materials/
exchange of written notes, computer-aided transcription services, video remote interpreting services, and the option of qualified interpreters. A qualified interpreter is defined as someone “who is able to interpret effectively, accurately, and impartially, both receptively and expressively, using any necessary specialized vocabulary.”
An individual does not need to be certified to meet this definition, unless your state requires the use of certified individuals.
For LEP patients, a “qualified interpreter” should meet three requirements: They must be proficient in speaking and understanding English and at least one other language; they must be able to interpret accurately, effectively, and impartially between both languages (including using specialized vocabulary and terminology when needed); and they must adhere to ethical principles,
including client confidentiality. As an alternative to using qualified interpreters for LEP patients, you may consider using a translator or translation services or software.
Family members, friends, and companions would not be considered qualified interpreters for LEP patients in most cases because they may be emotionally involved or could have interests that conflict with the patient’s—and thus would be unable to interpret “effectively, accurately, and impartially.” In addition, using such individuals as interpreters can cause problems when it comes to maintaining patient confidentiality. However, there are certain scenarios in which a family member, friend, or companion may be an acceptable alternative to a qualified interpreter—for example, in the case of an emergency.
In some cases, you may use a bilingual staff member as an interpreter, but there are some restrictions to this option. One restriction states that “interpreter” must be part of the staff member’s official job description in order for them to carry out this responsibility.
Given all of the options, how do you know which method to use? This depends on the effectiveness of the communication required. The key to communicating effectively is to consider the nature, length, complexity, and context of the communication and the patient’s normal and preferred method(s) of communication; for patients with LEP, this could include the type of dialect spoken by the patient.
For example, if the patient is in the office to set up an appointment, to ask a few general questions, or to take part in a follow-up appointment, you may be able to rely on notes, brochures, translated materials, or a similar method. However, if the patient is there for their first fitting or the appointment requires a full exam and testing, then notes may not be adequate to explain the situation or allow the patient to ask complex questions. In such a case, an interpreter may be required, or you may
need to find a different method with which the patient is comfortable. You should be cognizant of the patient’s normal means of communication and preferences.
The patient may prefer one method over the other, or they may demand that you provide an interpreter; however, you are not always required to provide the method selected or preferred by the patient. You should consider their preference and try and accommodate their choice, but the final deci sion rests with you—as long as the method chosen results in effective communication.
In addition, the ADA—and to a degree Section 1557 of the ACA—states that you are not required to provide a particular auxiliary aid or service if it causes an undue burden to your business. An undue burden can be something that involves significant difficulty (hiring an interpreter on short notice) or expense. An undue expense doesn’t solely mean the interpreter is more expensive than the item/service you are providing; an undue expense consid ers your overall financial resources and overall expenses.











Anatomically side-specific (liner, pads are optional)
Early ambulation
Note that you may request or require advance notice from patients and individ uals requesting interpreters or any of the other possible aids and services. However, you may not require excessive or abusive advance notices. The advance notices must be reasonable and should be based on the time needed to find and hire a quali fied interpreter or to find alternate aids or services. Remember also that you must be able to accommodate any walk-in or imme diate requests to the best extent
You are required to pay for whichever auxiliary aid or service you and your patient elect to use; this is considered part of doing business.
Several new updates and implementation dates related to Section 1557 of the ACA are in effect or about to take effect. The updates strengthen the nondiscrimination protec tions for patients to ensure they are not discriminated against based on their race, color, national origin, sex, age, or disability.


Dynamic size variations for volume control
Antibacterial & Accessible (hygiene & wound care)
Backup for definitive (adjustments)


To be compliant with these Section 1557 changes, you must take or have taken several key actions.
First, update your policies and procedures, and train your staff. In short, you must have policies for providing language assistance services for patients with LEP and for ensuring effective communication and reasonable modifications for people with disabilities—for example, explaining the types of aids and services you provide and how you will make them available. You also must train staff on these policies and procedures.
If you need assistance with updating or creating these policies and procedures, the Office of Civil Rights (OCR) has templates available for download; visit the “For Providers” page under “Civil Rights” on the Department of Health and Human Services website: hhs.gov/civil-rights/for-providers/ resources-covered-entities/index.html. If you use these templates, be sure that you have read and understand them, and that you are not committing yourself to anything you will not be able to provide or accomplish. The updates to your facility’s policies and procedures and the subsequent training should be completed by July 5, 2025.
Second, create and post a “notice of availability of language assistance services and auxiliary aids and services”; this must be accomplished by May 5, 2025. This notice does not have to be overly detailed and could be as simple as the following:
ATTENTION: If you speak [insert language], free language assistance services are available to you. Appropriate auxiliary aids and services to provide information in accessible formats also are available free of charge. Call 1-xxx-xxxxxxx (TTY: 1-xxx-xxx-xxxx) or speak to any member of our staff.
Note that you must follow some rules regarding this notice: The notice must be provided annually to your patients, and upon request. It should be posted in your facilities in a clear and prominent location and on your website, and should be
presented in a font size that is at least 20 points. The most important rule is that the notice should be able to be provided in at least the 15 most commonly spoken languages in the states in which your facilities operate, as well as in alternate formats for individuals with disabilities.
The OCR resources web page listed previously provides a template for a notice of availability of language assistance services and auxiliary aids and services in English and more than 40 other languages. To determine the top 15 languages spoken in your state, visit lep.gov or search the CMS website.
Finally, create, update, and post a “notice of nondiscrimination.” At this point in time, the notice should already be completed. Your notice should include a standard statement of nondiscrimination, such as: “We do not discriminate based on race, color, national origin, sex, age, or disability.” It should include a statement about your provision of accessibility services and aids, including language assistance for individuals with LEP. The notice does not need to be overly complex; it could be as simple as the following:
Discrimination is against the law. [Name of your organization] complies with federal civil rights laws and does not discriminate on the basis of race, color, national origin, age, disability, or sex. [Name of your organization] also provides reasonable modifications, auxiliary aids, and services for people with disabilities, and provides language assistance services to people whose primary language is not English.
Consider including information on how an individual can file a complaint with OCR if they feel they are being discriminated against; this could take the form of a link to the OCR complaint page, ocrportal.hhs. gov/ocr/smartscreen/main.jsf. As with the notice of availability of language assistance services and auxiliary aids and services, the notice of nondiscrimination should be provided annually or upon request
If your organization employs 15 or more people, you must assign an individual to be a “coordinator” responsible for ensuring compliance with all of these updates.
and must be posted in clear and prominent locations within your facilities and on your website, and presented in a font size that is at least 20 points. The OCR offers sample notices in English and more than 40 languages, but it is not required that this notice be made available in the top 15 languages spoken in your state. If your organization employs 15 or more people, you must assign an individual to be a “coordinator.” The coordinator is responsible for ensuring compliance with all of these updates and handling any grievances and complaints from patients about having meaningful access to qualified interpreters, aids, and services. Include the coordinator’s information and your organization’s grievance procedures on your notice of nondiscrimination.
Take the time to update your policies, procedures, trainings, and notices to ensure your compliance and to enhance your services to patients who may need qualified interpreters or other aids and auxiliary services.

Reach him at dbernard@AOPAnet.org
Drop-in vacuum for easy sealing
Holds vacuum longer
Vacuum runs less often

Smart app and manual control
PATENT: US9119735 B2


BY CHRISTINE UMBRELL

Some powered exoskeletons and orthoses are now covered by Medicare. Here’s how the technology could transform orthotic patient care
Powered exoskeletons are wearable structures that support and assist movement and augment the capabilities of the human body—and as such, they are braces, as categorized by CMS in November 2023. With the updated classification and associated payment decisions, finalized last April, orthotists have an opportunity to partner with allied healthcare professionals to treat patients who may benefit from both lower-limb and upper-limb powered orthoses.
Prior to the introduction of powered exoskeletons, mobility options for people
f With the recent classification of some powered orthoses and exoskeletons as braces, orthotists have an opportunity to partner with allied healthcare professionals to treat patients who may benefit from active assistance.
f Orthotists are skilled at interfacing with orthotic hardware, and with the added software component in powered orthoses, they can finetune device settings and provide patients with greater functionality.
with spinal cord injury were largely limited to wheelchairs. When robotic exoskeletons first came to market, they were used primarily in clinical settings, such as physical therapy offices. “They were on the market and in rehab clinics” prior to the November 2023 final rule, “but now patients can take them home” and leverage them in their day-today activities, explains Kinsey Herrin, MSPO, CPO, FAAOP, senior research scientist at Georgia Tech’s School of Mechanical Engineering and a leader at the university’s Exoskeleton and Prosthetic Intelligent Controls (EPIC) Lab.
f Powered lower-limb exoskeleton devices are already on the market, and more patients are using them in their home and community settings in addition to their wheelchairs.
f Previously wheelchair-bound patients may find that the ability to stand and walk helps prevent secondary complications such as bladder infections, neuropathic pain, spasticity, and muscle atrophy.
f Classifying certain upper-limb exoskeletons as braces has had a positive impact for many individuals, including some stroke survivors who may now access powered devices to help them move their arms.
f In the future, orthotists will likely fit patients with a wider array of powered orthoses, including smaller powered devices that focus on single or double joints.
CMS released a final rule in November 2023 that included powered orthoses and exoskeletons in the brace benefit category for Medicare coverage and payment purposes. Fee schedules for these devices were released in April 2024.
The lower-extremity article addresses code K1007: “bilateral hip, knee, ankle, foot device, powered, includes pelvic component, single or double upright(s), knee joints any type, with or without ankle joints any type, includes all components and accessories, motors, microprocessors, sensors.” This device must support “the weak legs for a patient that can perform ambulatory functions with the device. Ambulation may include the assistance of a cane, crutches, or a walker to return to mobility activities of daily living.”
The article also states that K1007 is to be considered a custom-fitted item and must adhere to the rules of custom fitting: Adjustments must be made at the time of fitting; the adjustments must go beyond minimal self-adjustment; and the adjustments must be made by someone with specialized training. Regarding fabrication, the coding article states that K1007 is a complete item, and no other codes may be used.
The upper-extremity article states that “upper-extremity powered exoskeleton devices are used for chronic upper-limb weakness; these custom-fabricated orthotic devices are used to support and assist movement, thereby promoting functional activities of daily living,” and this currently includes codes L8701 and L8702.
In addition to being custom fabricated, L8701, “powered upper-extremity range-of-motion assist device, elbow, wrist, hand with single or double upright(s), includes microprocessor, sensors, all components and accessories, custom fabricated,” and L8702, “powered upper-extremity range-of-motion assist device, elbow, wrist, hand, finger, single or double upright(s), includes
With the increased availability of powered exoskeletons, orthotists should educate themselves about the various features and capabilities available. They should also understand how each device can be customized for the individual user—enabling patients to experience varying levels of functionality.

A patient uses an Indego exeskeleton.
microprocessor, sensors, all components and accessories, custom fabricated,” are all inclusive, and no other add-on codes may be used. They also must include an adjustable microprocessor control feature that utilizes electromyography signals. These signals are derived from intact muscle tissue, which controls the motors and results in support and movement of the limb through functional motion.
The coding bulletin also requires that, effective for claims with a date of service on or after June 1, 2024, all items billed with the K1007, L8701, or L8702 code must be reviewed and verified by the Pricing, Data Analysis, and Coding (PDAC) contractor and placed on the PDAC Product Classification List. For details, see the advisory articles “Powered Lower-Extremity Exoskeleton—Correct Coding ” and “Powered Upper-Extremity Exoskeleton—Correct Coding.”

“It’s an exciting time to be an orthotist—and to be a patient who could benefit from powered assistance,” says Herrin, whose lab is affiliated with the Human Augmentation Core in the Institute for Robotics and Intelligent Machines at Georgia Tech.
Kinsey Herrin, MSPO, CPO, FAAOP
Herrin’s lab focuses on control of powered devices, with staff studying how to optimize device hardware and software to help users more easily integrate into their everyday environments. “Our research aims to enable a future in which patients can wear their exoskeletons from the moment they wake, receiving seamless, task-based assistance throughout their day until they go to bed at night,” she says.
In addition to full-body exoskeletons, many powered devices are coming to market that focus on specific areas of the body—devices that can be used for just one or two joints, says Herrin. Patients can get extra power that is unavailable in traditional passive orthotic systems, she says.
For 30 years, The Bremer Group Company has established a reputation for supporting practitioners and patients with quality back braces, and exceptional customer service. The VertAlign® Spinal Support System embraces these 7 Cs.
For more information call 800-428-2304 or visit www.bremergroup.com.



These developments bring a bevy of opportunities for patients— and for orthotists who are interested in learning about these devices and how they may benefit specific patients. “Because clinicians haven’t been able to provide these types of devices” in the past, “it will take time for orthotists to get educated on the options and who’s a candidate” for specific powered devices, says Herrin.
Orthotists are skilled at interfacing with orthotic hardware, “and with the added software component, they can fine-tune device settings and provide patients with greater functionality, ultimately enhancing their mobility and quality of life,” Herrin says. Both the hardware and software must be optimized to ensure the best patient solution: “It’s in the orthotist’s scope of practice to both fit and program these devices.”
Herrin believes orthotists should consider powered devices as one more tool in their toolbox. “It will be similar to how clinicians treat patients now,” she says—evaluating patients and their individual needs. “If there’s weakness, there’s potential for benefit” from a powered device, she says. Powered devices may enhance the lives of a broad spectrum of patients—from those with neurological disorders like stroke and multiple sclerosis, to individuals with joint weakness, to “anyone with abnormal movement patterns.”
Two companies currently offer personal in-home powered lower-limb exoskeleton devices, according to Michael Glover, PT: Eksobionics and Lifeward Inc. Glover, a physical therapist and neurological clinical specialist with a career focus in acquired brain injury, joined Eksobionics in 2012 with a goal of bringing robotics into standard clinical practice, and he currently serves as director of clinical operations. The company offers exoskeletons designed for rehab purposes, “but now we also have a device that is designed for the home and community environment,” he says. “That’s the device that received reimbursement last year.”

Glover notes that progress in some aspects of orthotics has been relatively stagnant, but powered orthoses mark a turning point. Devices such as rigid orthoses and knee-ankle-foot orthoses (KAFOs) “have been relatively similar for quite some time—decades in some cases,” he says. “When you’re looking at this from an energy expenditure and gait kinematics perspective, taut and hinged-knee orthoses cause the user to extend a significant amount of energy beyond typical gait”; powered orthoses give the human body the opportunity to walk in a typical gait pattern without having to teach compensatory strategies that often are required with bracing. “These powered braces offer the joint kinematics at the hip and the knee to promote a more typical and efficient gait pattern, so users are able to walk farther without having to expend so much energy.”
Approximately 100 people have acquired Eksobionics’ personal exoskeleton to date, according to Glover. “The U.S. Food and Drug Administration has approved these devices for home use since the mid-2010s, but most of them were cost-prohibitive; most people paid out of pocket because they weren’t covered by private insurers or Medicare,” he says. In 2023, Eksobionics and Lifeward approached CMS and other officials in Washington, DC, to explain the medical and psychological benefits of the technology. They emphasized how exoskeletons can help prevent or ameliorate secondary complications. AOPA and the O&P Alliance supported these efforts.
Glover says that because exoskeletons give users the ability to stand or walk, they may prevent issues such as bladder infections, bowel disfunction, sexual disfunction, neuropathic pain, spasticity, muscle atrophy, and bone density loss. “There’s a tremendous number of things that happen to individuals who are in a seated position because they’re not able to walk,” he explains. Powered exoskeletons “give them the opportunity to stand and be more mobile—and ultimately have a healthier lifestyle, which improves quality of life because they have less of those secondary complications.”
CMS ultimately placed powered lower-limb exoskeletons into brace category K1007. “Being placed in that brace category means it doesn’t conflict or compete with the reimbursement and financial benefit that users receive for using a wheelchair.”
The Motion Foot SLX has a 17 degree hydraulic range of motion that smooths out aggressive terrain, cushions heel strike, and actively clears the toe with ease. For the K3 patient that needs a smooth ride for those long hikes or a day at the office, the Motion Foot SLX won’t leave them disappointed.

Want to see it in action? Scan the QR code to schedule a demo now!

That’s an important point for potential beneficiaries to understand, says Kathleen O’Donnell, vice president of marketing at Lifeward. “An exoskeleton is a medical device that can be used in addition to—not as an alternative to—a wheelchair,” she says. Powered exoskeletons “help people with spinal cord injury in weightbearing exercises and in moving around in their daily environment—in getting mobile.”

Kathleen O’Donnell
Powered exoskeletons help patients achieve extremely individualized goals, according to Glover. “The exoskeleton is designed to help people stand and ultimately walk. But not everyone who has a spinal cord injury is motivated to do walking activities,” he explains. “Some just want to stand in their kitchen and prepare a meal or wash dishes at their sink without having to be in a seated position,” he says. Glover worked with one exoskeleton user whose goal was to return to the woodworking activities he loved—but he had been unable to use his workshop because it was designed before his injury. “Others just talk about going to social events” and standing face-to-face with others.
Medicare approves exoskeletons on a case-by-case basis, says O’Donnell. To qualify, patients must, at a minimum, have a spinal cord injury of T7 or below, be able to manage crutches for balance support, be between 5’2” and 6’3” in height, and be under 220 pounds. “We start by making sure potential users have spinal cord injury, trunk control, and arm and hand function,” she says.
For individual patients considering whether an exoskeleton might work for them—and be reimbursable by Medicare—Lifeward staffs an internal team that discusses the internal and external parameters on an individualized basis, says O’Donnell. Before proceeding, “we want to know they’ll be successful in the exoskeleton.”
Orthotists have an opportunity to play a key role on healthcare teams working with exoskeleton patients. Prior to CMS’s classification, most exoskeletons were provided to patients who had been introduced to the devices by their physicians or physical therapists, explains Jeannine Lynch, vice president, market access and strategy, for Lifeward Inc. Now, orthotists may educate patients with spinal cord injury about these braces and become involved in the fitting process.
Just as physical therapists typically consult with orthotists when ordering an AFO or KAFO for a patient, “the way we are looking at collaboration and partnerships with different O&P groups for exoskeletons is very similar,” says Glover. For example, “if a PT has a spinal cord patient in their facility [who is an appropriate candidate for a powered exoskeleton], the orthotist could come in and help with the measurement and fit, and the physical therapist would train the gait with the patient on that device,” he says. The orthotist could continue to work collaboratively to ensure the device continues to fit and perform appropriately as the patient uses the device and progresses.
Lynch and O’Donnell suggest that orthotists partner with therapists who use exoskeletons during individual PT appointments. “This is a new category, so we’re still learning,” Lynch says, but she believes orthotists’ expertise could be helpful in sizing and measurements for new exoskeletons, as each device is custom fitted for the patient. In addition, orthotists’ knowledge and experience could add value during delivery, assembly, and configuration, as well as final adjustments.

Orthotists also can work with allied health professionals to raise awareness of exoskeletons and ensure candidates for the technology understand that it is covered by Medicare, says Lynch—whether they have recent spinal injuries or have been injured for several years and are just learning about the technology.
“There are potential long-term opportunities here,” adds Glover. “But it’s so new in this space that there’s going to be a lot of learning and education into this new option.” He notes the reimbursement for the orthotist’s work is yet to be determined. “Right now, the exoskeleton manufacturers do a lot of the upfront work in working with patients to determine the appropriate device and get it to the patient. But I would imagine that with scale, there’s potential we could have relationships with orthotists grow, as the companies grow and as reimbursement gains traction.”
The November 2023 CMS final rule has implications beyond lowerlimb devices. Classifying upper-limb exoskeletons with codes L8701 and L8702 as braces has had a positive impact for many patients, including some stroke survivors, says Erin O’Brien, CPO, FAAOP, a full-time clinical education specialist for Hanger.

CUSTOM: FOOT ORTHOTICS • AFO’S • RICHIES
One size does not fit all. At Hersco, our team of professionals works to fabricate orthotics from your scans and casts to match your patients’ specific needs. Customer service is at the heart of everything we do and we work endlessly to help you be as effective and efficient as possible. When you want the job done quickly and accurately, Hersco is here to help.


“In the upper-limb orthotic space, there are very few options to restore function,” explains O’Brien, who oversees Hanger’s national program for powered upper-extremity exoskeletons, which includes the MyoPro brace. “Most upper-limb orthotic devices focus on maintaining or increasing range of motion through static or dynamic positioning. However, these orthoses don’t assist with activities of daily living or other bimanual tasks,” O’Brien says.

With the April 1, 2024, fee schedule change came the opportunity for some Medicare beneficiaries with upper-limb involvement to access powered devices to help them move their arm again. “The functional deficits that result from neurologic injury can now be minimized through the restoration of volitional movement of the elbow and hand,” O’Brien says. This means that patients can regain independence in many daily tasks, “which can help improve their physical and mental health.”
O’Brien, who has reviewed dozens of patient cases for clinical candidacy, notes that upper-extremity exoskeletons can improve safety during mobility tasks for many patients that use assistive devices when walking. “Because a large portion of clinical candidates have upper-limb weakness subsequent to a cerebrovascular accident (CVA), they often have lower-limb weakness and gait abnormalities as well,” she says. “By improving their upper-limb function, and therefore their ability to hold onto and manipulate
an assistive device, an upper-limb device can impact their safety and independence.”
Orthotists should do their homework to learn about the powered upper-limb options available—and in development—and consider which patients are appropriate candidates for the technology. “As with any prosthetic or orthotic device, appropriate patient selection is imperative for success. Each type of exoskeleton will have its own set of patient indications and contraindications for a device to function as intended,” O’Brien says. “While it may seem that every post-CVA patient is a candidate for a powered upper-extremity exoskeleton to improve arm function, the number of patients that fulfill all the candidacy qualifications is much smaller.
“As a field, we need to ensure that only appropriate patients are fit with this technology to ensure that the short- and long-term functional outcomes are positive,” O’Brien adds. By applying patient selection appropriately, “the field will ensure that insurance coverage continues to improve, which will, in turn, lead to additional technology advancement.”
While larger powered exoskeletons receive a lot of attention, Herrin believes orthotists also will increasingly fit patients with smaller powered devices that focus on single or double joints, such as powered ankle exoskeletons, hip exoskeletons, knee-ankle exoskeletons, and more. “Many of these devices have only been used in PT facilities so far, so it’s important to integrate the orthotist into the picture, given our skillset in tailoring assistive technology for patients in their homes and communities,” says Herrin.

Many iterations of powered devices are currently in R&D. The EPIC team is developing a task-agnostic exoskeleton controller to more seamlessly modulate assistance across a broad range of activities without any user-specific calibration. The controller leverages deep learning, based on real-time estimates of the user’s lower-limb joint movements, to help coordinate assistance across the hip and knee and reduce user energy expenditure, according to Herrin.
O’Brien also expects that exoskeleton technology will continue to advance and “provide options for additional patients with different presentations.” For example, she is hopeful that a wrist-hand-finger orthosis model of a powered exoskeleton will be developed to assist those with isolated hand and wrist deficits. “There are a multitude of presentations that can be assisted utilizing powered joints,” she says. “There is certainly space in the pediatric domain for powered assist for the upper and lower extremities as well.”
As technology improves and the number of devices increases, O’Brien believes “more and more patients will be candidates for powered orthoses. However, for these patients to access the devices it will be critical that clinicians are measuring the impact these devices are having on patients’ lives in order to help payors understand their value.”
Christine Umbrell is a contributing writer to O&P Almanac Reach her at cumbrell@contentcommunicators.com

Fabtech Systems pioneered the technology behind one of the most effective braces for complex foot and ankle challenges. Trust the original innovators to deliver exceptional care. Choose Fabtech CFAB to design and build a brace that ensures your patients receive the highest standard of support and relief.






BY JENNIFER DAVIS


When bombing damaged Sheikh Hamad bin Khalifa al-Thani Hospital for Rehabilitation and Prosthetics in October 2023, individuals in Gaza who required amputation lost a critical resource for protecting and enhancing their mobility.
Established in 2016 with funding from Qatar, the hospital was the first of its kind, fitting people with prosthetic devices and providing rehabilitation care in the Gaza Strip. Intense bombing in retaliation for the Hamas-led Oct. 7, 2023, attack on Israel, was the death knell for the hospital, which previously suffered damage in a 2021 bombing.
The loss of medical facilities dedicated to prosthetic care and rehabilitation dovetailed with an exodus of O&P specialists and a massive surge in individuals requiring amputation to create a healthcare emergency that will impact the Gaza Strip for generations to come. An estimated quarter of those injured in Gaza by late July—approximately 22,500—have life-changing injuries
that require long-term rehabilitation services, according to the World Health Organization (WHO). Severe limb injuries make up an estimated 13,455 to 17,550 cases, WHO reports.
“The World Health Organization estimates that over 10,000 people are newly amputated; among them, 4,000 are children, making it the highest percentage of pediatric amputees in the world,” says Raghad Weshahi, CPO, a member of Prosthetics for Palestine, a volunteer initiative formed in October 2024 to work with local Palestinian providers to meet the growing needs of amputees.
The three-phase ceasefire agreement between Israel and Hamas, which took effect Jan. 19, 2025, stemmed the violence in Gaza and brought increased opportunities for sorely needed humanitarian aid to the region—at least into March. But leaders have not agreed to specific terms for the second and third phases of the deal, yielding an extremely fragile peace.

Founder and executive director of the nonprofit HEAL Palestine, Steve Sosebee, was in the Palestinian territories the week after the ceasefire agreement took effect. While there may have been an increased flow of aid into the area, Sosebee says it’s not nearly enough to meet the housing, medical, and humanitarian needs of the general population, which was cut off from receiving supplies and aid throughout the conflict.
“It’s absolutely catastrophic with the complete destruction of the healthcare system,” he says.
For now, the most effective way to get people with traumatic injuries the treatment they need is to take them out of Gaza.
According to data published by the United Nations Office for the Coordination of Humanitarian Affairs, 12,000 patients in Gaza need medical evacuation abroad, and just 458 patients, including 276 children, had been exceptionally evacuated as of Jan. 15. Since its founding in January 2024, HEAL Palestine has evacuated 30 children from Gaza to the United States for free care they can’t get at home. HEAL Palestine will continue to evacuate as many children as possible to receive medical care until Gaza’s medical resources can be rebuilt, says Sosebee.
The Ottobock Global Foundation is another of just a few nongovernmental organizations that have been successful in evacuating patients from Gaza. The foundation, associated with medical technology company Ottobock
and its global patient-care network, has evacuated 38 children from Gaza for treatment in Egypt and Turkey.
“Since the security situation can change daily, we are continuing to provide care abroad for the time being and hope that more children can be rescued from the crisis area,” says Christin Franzel, a member of the foundation’s executive board.
New York-based Penta Medical Recycling has worked with nonprofits like the Palestine Children’s Relief Fund and Anera to improve access to prostheses.
During the conflict, all channels the nonprofit typically uses to transport its donated, recycled prosthetic supplies shut down, says Penta Executive Director Anna Szczepanek. “Even before the war, it was extremely challenging to get equipment into that part of the world—and it’s even more challenging now.”
The ceasefire agreement provides hope for improved access into the region. The United Nations World Food Programme reports it brought more food to people in Gaza during the first four days of the ceasefire than what it could previously dispatch on average per month.
However, Szczepanek does not expect to be able to bring in the metal components for devices as easily. There are restrictions on items entering the Gaza Strip that might be considered for dual use—both to meet civilian needs, but also to potentially fulfill military purposes.



Penta currently is in talks with various groups to see how aid can be provided to patients as quickly as possible, whether equipping mobile clinics run by the Royal Medical Services in Jordan or providing devices for Palestinian children evacuated to the United States for treatment by groups like HEAL Palestine.
“We have a lot of feelers out,” Szczepanek says. “We’re looking for ways to get equipment into the hands of people who can use it.”
The Limbs for Life Foundation, a nonprofit organization primarily focused on providing funding for uninsured or underinsured U.S. residents in need of lower-extremity prostheses, receives several emails a day from international patients seeking assistance. Requests have come from Gaza, Ukraine, and almost anywhere a disaster has occurred, says Executive Director Randy Titony.
The organization also receives calls for advice from companies like Amparo Prosthetics, whose Confidence Socket is used in the Jordanian Royal Medical Services mobile clinics, looking for opportunities for collaboration and creative solutions to assist in Gaza.
In addition to funding prostheses for patients within the U.S., Limbs for Life provides used prosthetic components for individuals outside the U.S. who can find a local provider to build and fit a prothesis. Its Oklahoma warehouse is packed with devices donated by families or clinics, overstock equipment, older models of devices, and samples.
“Our system is really successful in recycling these components,” Titony says. “The pilon is stainless steel. Feet are carbon fiber.”
Amparo is interested in replicating some of the Limbs for Life Foundation’s efforts for collecting and redistributing donated devices and exploring partnerships that could help them ramp up new programs. Titony says Limbs for Life also regularly provides supplies to U.S. prosthetists who are doing mission work abroad and stands ready to fulfill any request for parts and supplies it can.
Anera, a nonprofit providing humanitarian assistance and sustainable development to vulnerable communities in Palestine, Lebanon, and Jordan, has encountered numerous individuals in need of orthotic or prosthetic care during the physiotherapy clinics it offers in field health centers in Khan Younis, Deir Al Balah, and Gaza, according to Lubna Iskandar, Anera’s health program manager.
The group is working to coordinate existing resources and practitioners in the region to create a framework for onsite O&P care in the future. Anera developed lists of needed prosthetic and orthotic items and submitted them to Israeli authorities for approval, to smooth the way for importing devices. Anera also is working with Palestinian organizations that can manufacture equipment needed for 3D-printed or quick-fit prostheses and attempting to line up staffing for future clinics.
“We’re in communication with the remaining experts in Gaza and are laying the groundwork to organize a training of trainers, if and when we receive the approvals to import prosthetic items,” Iskandar says. “Our model depends on doing most of the work in Gaza to enable tailoring and maintenance.”
Prosthetics for Palestine, a project of nonprofit Physicians for Palestine, also is working toward building back services on the ground in Gaza, so the intensive care needs and multiple follow-up appointments required by most people with limb loss can be met.
Many of the amputees in Gaza had traumatic amputations that could have been prevented in better equipped locations, Prosthetics for Palestine leaders say. If the patients are not evaluated and fitted properly, ulcers, residual limbs with skin breakdowns, and other complications are likely to arise.
Just 600 to 700 out of an estimated 10,000 people needing care have been evaluated and are ready for fitting, according to a Prosthetics for Palestine partner orthopedic limb surgeon in Gaza.
The group is raising funds and putting processes in place to accept donated supplies and deliver them to Gaza in two phases. The first, partnering with Limber P&O, will focus on below-theknee prostheses that can be built using an iPhone and a 3D printer, with the hope that printing onsite will facilitate entry of supplies into Gaza. The second phase will shift to manufacturing traditional prostheses and expand the types of amputations that can be treated. Gently used and donated supplies will be incorporated into both phases.
“It is our goal to work hand-in-hand with local providers to supply them with quality prostheses, both 3D-printed and traditional pieces, and offer support with additional materials, supplies, and training, to uplift them in being self-sufficient,” says Natalya Beranek, CPO, of Prosthetics for Palestine.



As efforts to provide quality, ongoing O&P patient care to residents of Gaza depend upon an end to attacks and destruction, some professionals from within the industry are banding together to campaign for peace.
The Ceasefire Collective is a growing group of O&P professionals and advocates that’s worked since November 2023 to support of a permanent ceasefire in the Palestinian territories. “We can provide all of the physical aid in the world but, if hostilities continue, then we’re not helping to address the cause,” says Westin Humble, a member of the group who recently began working as a software engineer after spending more than a decade employed in the O&P field.
Nearly three dozen CPOs and professionals in related fields joined the Ceasefire Collective’s effort, petitioning their professional organizations to express their desire for a permanent ceasefire.
“Prosthetists and orthotists rarely have an opportunity to prevent the injuries that lead patients to seek our care, but in calling for a ceasefire, we do,” the Collective states in its communication to professional associations.
Emily Lipski, CPO, the founder of a pediatric practice in Puerto Rico, helped mobilize the members of the Collective and is amassing a collection of prosthetic componentry to donate to Prosthetics for Palestine once they’re prepared to receive and disperse donated devices.
“Gaza is now home to the largest cohort of child amputees in the world,” Lipski says. “As prosthetists, we understand the unique challenges for folks with traumatic limb loss and the distinct prosthetic care needs of children.”
Davis is a contributing freelance writer for O&P Almanac
The organizations mentioned in this article have provided the following information for members of the O&P community who would like to assist their humanitarian efforts:
y Anera is looking for volunteers who can assist “training the trainers” to increase the number of skilled professionals in Gaza. Anera also can receive medical missions. For more information, email Lubna Iskandar at lubna@anera-jwg.org.
y To learn more about the Ceasefire Collective’s efforts to promote peace in Gaza, email opceasefirecollective@ gmail.com
y In addition to donations to its Global Healing Program, HEAL Palestine welcomes technicians, surgeons, and rehabilitation specialists interested in working to rebuild artificial limb and orthotic services in Gaza. Visit healpalestine.org and fill out the contact form if you’d like to volunteer.
y Limbs for Life Foundation and Penta Medical Recycling accept donations of used prostheses as well as financial contributions. Visit their websites to learn more.
y Ottobock Global Foundation is grateful for private individuals who support its relief campaigns. Visit ottobockglobal-foundation.com/#donation to give.
y Prosthetics for Palestine invites O&P professionals to host house party fundraisers to benefit its work. Visit prostheticsforpalestine.org to access its online house party toolkit. Or, fill out the contact form on the website to find out how to serve as a clinical volunteer.


Mickey
Elmo while
The Fresh Faces column introduces readers to prominent O&P professionals who are making an impact with their contributions to the orthotics and prosthetics profession. This month, we speak with Steven Slawinski, CO, LO, FAAOP, clinic director of Orthopediatrics Specialty Bracing in Marlton, New Jersey.
Steven Slawinski, CO, LO, FAAOP, started in the orthotics and prosthetics field as an orthotic technician at a central fabrication site in Philadelphia in 1999. He joined Orthopediatrics Specialty Bracing (OPSB–formerly Boston Orthotics & Prosthetics) in 2008 as a technician and orthotic fitter, then attended Northwestern University’s O&P program and earned his orthotic certification in 2011.
Slawinski, who enjoys working with pediatric patients, specializes in cranial and spinal deformities. He is the current director of OPSB’s Cranial Remolding Program and is a member of the Scoliosis Program team. He is involved in creating and revising treatment standards, as well as education and training of clinical staff and allied health professionals. He devotes a great deal of time to volunteering for AOPA and other O&P organizations to increase access to and improve care for pediatric patients.
O&P Almanac: What brought you to a career in O&P?
Steven Slawinski, CO, LO, FAAOP: I started in the O&P field at a central fabrication site as an after-school job when I was 16 years old, pouring plaster and learning to hand-modify check sockets and anklefoot orthoses. Honestly, I had no intention of remaining in the field after college. However, upon graduating, I knew I wanted to work in pediatrics but was still not sure in what capacity.
I always enjoyed the artistic nature of the fabrication process and how you create something completely unique with your hands, so I decided to return to O&P and sought a position with a company that focused on pediatrics. Ultimately, I found a home with Boston Brace in Massachusetts in 2008, about 10 years after first being introduced to the profession.
O&P Almanac: Why did you decide to specialize in orthotics, and why do you enjoy working with pediatric patients?
Slawinski: My areas of interest are specific to cranial and spinal deformities. Having a strong technical background provides me with a unique clinical perspective that I have embraced to provide a high level of care.
Working with the pediatric population inherently limits your exposure to prosthetics, so it wasn’t necessarily a conscious choice to specialize in orthotics. I get along better with babies and kids—probably because I still act like one in many ways.
As for cranial remolding, when my patient schedule was almost exclusively infants, I got to make babies smile all day by making silly faces and impersonating Mickey and Elmo. Who doesn’t love a smiling baby? Also, adults don’t find me nearly as amusing, so it was a natural fit. There is also the visual effect of treatment in a relatively short period of time, which is appealing from an outcomes standpoint.
O&P Almanac: What are some of the innovations and processes you have been involved in developing?
Slawinski: I have been fortunate to be involved in the development and implementation of the Boston Brace 3D thoracolumbosacral orthosis as part of my company’s scoliosis program. We are continuously improving the design through weekly meetings where we discuss feedback from our own clinical staff.
As director of the Cranial Remolding Program, I am in a unique position to be involved in the clinical training and education, as well as the fabrication of our own cranial remolding orthosis, the Boston Band.
Bridging the gap between the clinical and manufacturing realms provides a distinct perspective that allows process improvement on both sides that are not so obvious when only seeing a problem from one of

those viewpoints. Functioning as the manufacturer as well as the clinical staff allows us to optimize the outcomes and experience for all of our patients.
O&P Almanac: Why is advocacy, such as involvement in the So Every BODY Can Move (SEBCM) initiative, a priority for you?
Slawinski: I have worked on SEBCM [a grassroots advocacy initiative aimed at ensuring equitable access to the O&P care needed for physical activity] initiatives in both New Jersey and Pennsylvania, but currently I am focusing on leading the efforts in New Jersey.
I found out about SEBCM through AOPA when the association was recruiting volunteers to initiate efforts on a state level. I was compelled to act when the inequity in coverage was underscored in a meeting I was attending. Having no experience doing
any advocacy work was apparently not a disqualifier; determination and persistence have made the difference to this point. It is an entirely separate world that works in a way that can be frustrating from an outsider’s perspective, but I have learned so much being involved in this initiative over the past 18 months. I will be able to use that knowledge when we look to introduce legislation in New Jersey aimed at Medicaid parity.
In New Jersey, an identical bill must move through both the state Senate and state Assembly. Through our team’s efforts, the Senate bill passed the floor vote earlier this year, and the Assembly bill has one more committee hearing before it will be voted on and then sent to the governor’s desk to be signed into law. We would not have made this progress if not for the dedication of each team member, along with the support we have received from AOPA and the Amputee Coalition.
O&P Almanac: What is involved in your role as chair of AOPA’s Member Services Committee, and what are your plans for that committee in 2025?
Slawinski: The Member Services Committee reviews the existing programs available to AOPA members, as well as generates and evaluates new potential services that would be beneficial and impactful. As chair, I help guide the meetings, but it’s very much a collaborative effort between all of the committee members.
As for plans this coming year, AOPAversity, the site that houses AOPA’s CEU library, will be free to access for all AOPA patient-care facility members, which is an incredible feature for anyone with a certification.


few years now, which is another extraordinary group of individuals that I thoroughly enjoy spending time with. It’s rewarding to be able to give back and contribute to the next generation of clinicians entering the profession.
I also moderate a few different support groups for parents of children with plagiocephaly and scoliosis. As a parent myself, I am fortunate to be in close vicinity to the best children’s hospitals in the country, but there are families that drive hours to get to a facility that may only see a couple kids each year with their child’s presentation. Being able to help those families by answering their questions and providing recommendations virtually is quite gratifying.
O&P Almanac: What are the biggest challenges and opportunities for the future of O&P?
O&P Almanac: Tell us about any other volunteer activities you participate in to help further the O&P profession.
Slawinski: Being part of the [American Academy of Orthotists and Prosthetists’] Craniofacial Society leadership team has opened many doors through networking, and [I’ve had several] opportunities to publish some of the innovations and unique cases that I’ve been involved in.
I have been volunteering with the American Board for Certification in Orthotics, Prosthetics, and Pedorthics (ABC) as an examiner for the CPM exams for the past
Slawinski: Generating interest in orthotics and prosthetics as a profession has been a challenge, but groups like ABC’s #WhatIsPOP? are working to address that through outreach and education, which is great to see.
Another challenge is healthcare as a system, as evidenced by the need for such initiatives as So Every BODY Can Move The overwhelming majority of those in this profession are here to help people, so it can be disheartening when our patients are denied services because the insurance company doesn’t cover something their healthcare providers deem medically necessary.
With that being said, there are opportunities to expand coverage and services for our patients, so we need to remain committed as a profession to advocacy efforts whenever and wherever possible. It is often an uphill battle, but if it’s worth doing, it’s going to take some deliberate effort.
There are no prerequisites to volunteering; it’s a commitment any of us can make to help however we can. I would encourage everyone to look for an opportunity to volunteer if you don’t already. It’s a great approach for a newer clinician to grow their network and develop skills that will be practical throughout their career, or it can be novel territory—like legislative advocacy—that can energize your passion for the profession if you’ve been in the field for a couple decades. I would be happy to answer any questions about the organizations I am involved in, so feel free to reach out and connect.

works with a lower-extremity patient.





Pennsylvania clinician sets fast, but safe, pace for fitting a physically fit lower-limb loss patient

The Transformations column features the success story of an O&P clinician who has worked with an inspiring or challenging patient. This month, we speak with Mike Zimmerman, CPO, LPO, East Region regional manager for Union Orthotics and Prosthetics, about his experience with a construction foreman who lost his left leg below the knee in a motorcycle accident.
Prosthetist Mike Zimmerman, CPO, LPO, has been treating Derrick Konop for less than a year, but his patient has made great strides in that time.
One year ago, 40-year-old Konop, who is married with two children, spent his days working a full-time job as a construction foreman for a crew that does asphalt milling, managing a residential moving company he owns with his wife, and visiting the gym almost daily. Those activities were brought to an abrupt halt last May, when Konop suffered an amputation due to a motorcycle accident. Six months later, he was back to full speed at both of his jobs and the gym—thanks to his prosthesis and individualized care from Zimmerman at Union Orthotics and Prosthetics.
On May 24, 2024, Konop was riding his motorcycle on a back road in Pennsylvania when he saw some rabbits crossing the road and slowed to about 15 MPH to let them pass. Another motorcycle rider came flying up behind him and tried to pass him in a non-passing zone. “He sideswiped me,” Konop recalls. The force with which the other biker hit Konop nearly severed his left foot. “My foot got caught in the side of my motorcycle, which broke my ankle and pulled my foot almost all the way off,” Konop says. He was flown to UPMC Presbyterian Medical Center, where he underwent immediate surgery, but the doctors were


unable to save his foot because the damage was too severe, and his leg was amputated below the knee.
Konop spent six days in the hospital, taking time each day to move his leg to do his own “physical therapy” while in bed. Once home, he spent another 10 days on blood thinners, which prevented him from going to the gym. As soon as he was finished with the prescription, Konop says, “I got into a wheelchair and rolled back to the gym.”
Even before receiving a prosthesis, he worked diligently at the gym to get the rest of his body into top physical shape and prepare for an artificial limb. “My main goal was to get back to work,” Konop says. “So, I stayed active while I was in the wheelchair and hopped around in a walker,” focusing on upper-body but adding some lower-body exercises.
“Before I got my prosthesis, I noticed my left quad and glute muscles were getting smaller just because I wasn’t walking around,” Konop recalls. He incorporated upper-leg exercises into his workout


regimen, with the intention of strengthening his left residual limb so it would be easier to walk.
For his prosthetic needs, Konop was initially seen in the hospital by another prosthetist from Union O&P, who fit him with a rigid dressing. Upon his discharge, Zimmerman took over as Konop’s prosthetist, as Zimmerman is head of the Greensburg, Pennsylvania, location of Union O&P, near Konop’s home. Zimmerman held long discussions with Konop about abilities and goals. He quickly recognized that Konop was more physically fit than many prosthetic patients and worked to ensure his patient was on a fast track to mobility. Zimmerman, who graduated from Northeast Metro Technical College with a degree in prosthetics technology before becoming certified in orthotics and prosthetics, has been with Union O&P for the past 14 years. He has seen all types of patients—with Konop toward the high end of the activity scale. Zimmerman enjoys


working with highly active patients but says it’s important to manage expectations.
“For patients that are active, part of my job is to pull the reins back and to get them to go through the whole process,” says Zimmerman. Working with Konop, “I have to slow him down” and let him progress through the necessary steps to recovery. “He wants to go straight from A to Z, but there are many steps in between” that Konop must navigate to ensure optimal and long-lasting outcomes.
With Konop eager to be fit with a prosthesis, Zimmerman took measurements in July, then fit Konop with a diagnostic leg in August. Given Konop’s physical condition and high level of activity both at home and work, Zimmerman fit him with a lightweight anatomical foot that offers energy return and smooth rollover as well as shock absorption and rotation capabilities. Zimmerman has had to work closely with Konop, adding padding to his socket—and replacing it altogether on two occasions—as his residual limb has gotten much smaller in the aftermath of his accident.


Because Konop was so active in the gym prior to amputation, his calf muscles were extremely large but have decreased in size after the amputation. “With the muscle atrophy from not being able to use my calf muscle anymore, the size and shape keep going down,” Konop says.
“For the first fitting, he was so bulbous” that Zimmerman had to make a very big socket. But the circumference decreased quickly, Zimmerman says. “It was surprising to Derrick—but it’s just part of the process,” he says.
Konop eventually experienced a hematoma, which served as a turning point, as it caused the fluids to drain more quickly— and Zimmerman was able to fit him with a prosthesis knowing he was closer to his final size.
Zimmerman is still working with Konop to determine which suspension system works best and is most comfortable. “He’s trying everything out,” says Zimmerman. “He started with a negative pressure system, and now he’s on a pin using a suspension


sleeve because he doesn’t like the pistoning,” he says. “He likes the pin because he can don and doff the prosthesis quickly and easily when at home.”
Fortunately, Zimmerman is quick with adjustments because he does all fabrication on site, without having to send devices out when changes are needed. His facility houses a fabrication area and employs a full-time technician. At Union O&P, “we do have a central fab site, but we can do a lot of our own fabrication in this office.”
Konop is back to doing “every single thing” he did prior to amputation. “My life is exactly the same—it just takes me a couple of extra minutes in the morning” to don his prosthesis, says Konop. “I walk around and sometimes completely forget I even have it.”
Despite initially being told by a physical medicine and rehab (PM&R) physician at the hospital that he shouldn’t plan to return
to work as a foreman—where he also operates a large asphalt milling machine—until 2025, Konop was determined to get back on the job.
In September, Zimmerman fit Konop with his final prosthesis. In October, Konop returned to the PM&R physician, who evaluated Konop and watched him walk— and jog—proficiently on his prosthesis. He agreed Konop could return to work immediately—several months ahead of schedule.
Konop and Zimmerman credit the quick return to life-as-usual to a positive practitioner-patient relationship and frequent check-ins. Konop reaches out to Zimmerman whenever he notices a change in his leg or prosthesis fit, and Zimmerman makes frequent adjustments to ensure an optimal fit as Konop’s anatomy evolves.
Konop is grateful for Zimmerman’s individualized approach to care and willingness to move swiftly—but carefully—through the various stages of prosthetic fitting and adjustment. “Mike is on it right away” when Konop contacts him with a problem.
Zimmerman says Konop will likely experience a bit more shrinkage over the next few months. “He’s not cylindrical yet, and that will take a long time,” he says, so he will likely fit Konop with one more socket before summertime.
As for Konop’s personal goals, “I was never a runner, but now I want to run an amputee marathon” or take part in another type of athletic event geared toward individuals with amputation, he says. “I want to be able to show people what I can do with just one foot.”
He also has been invited to speak at his employer’s annual safety meeting in February to share his story about overcoming adversity. “Everyone has been pretty impressed with my recovery—a lot of people didn’t think I would come back to work at all, or thought I wouldn’t come back until next year,” he says.
“The important thing is to keep positive,” says Konop. “Obviously, [amputation] is life changing. But if you learn how to use a prosthesis and keep a good state of mind, there’s light at the end of the tunnel.” Plus, he adds, “I think I look pretty cool with a fake foot.”
“TurboMed has made me more confident with my disability. The braces help me keep up with my friends and family, as well as do activities that I struggled with before. They are so comfortable, and I love that I can wear any shoes with them. I wouldn’t change it for anything else.”
–Davi Keynes-Levinson, CMT patient and proud Turbomed ambassador

Turbomed’s premium foot drop orthosis sits on the outside of the shoe to facilitate maximized ankle movement while reducing the risk of injury.
New MONOCORE TechnologyTM for a drill-less, one-piece design
New height-adjustable calf culf with pressure screws
Overhauled simplified instructions
FACILITY:
Burton Prosthetics


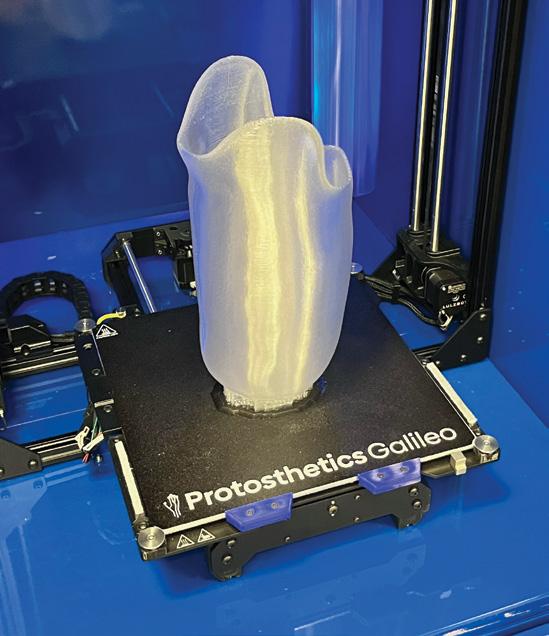
Jeremy Burton, BOCO, COF
LOCATION: Omaha, Nebraska
HISTORY: 19 years
Burton Prosthetics dates back to the early 2000s, when Russ Burton, CPO-E, who grew up in the O&P industry, opened his own facility in a garage near his home in Omaha, Nebraska. In 2008, the facility’s growing business required a new home, so Burton moved the company to a storefront in the city, adding new practitioners and staff. In 2012, Burton retired and sold his business to three of his clinicians: Tadd Meyer, CP; Paul Monestero, BOCOP; and Burton’s son, Jeremy Burton, BOCO, COF, the third generation of Burtons in the field.
“We are a locally owned facility with about 75 years of combined experience, which is valuable in our town,” says Meyer. “Our facility includes a modern, on-site fabrication lab with two great technicians, so we can control every facet of the design, fabrication, and fitting of prostheses.”
“We’re big believers in AOPA. It promotes a higher level of professionalism in our field, advancing it through education, literature, and research. And we’re glad AOPA advances our cause in Washington.”
—Tadd Meyer, CP
The company offers a full range of prostheses and serves adult, pediatric, and geriatric patients. “We do a lot of sports prostheses, and we fit quite a few transtibial amputees,” says Meyer. “We’ve had partial-hand amputees and we also fit upper- and lower-extremity orthoses, as well as a lot of spinal, cervical, and fracture bracing. We want to do it all!”
The facility welcomes new technology and houses a 3D printer on site for printing test sockets from scans. Meyer says the facility will soon add the capability to make 3D-printed ankle-foot orthoses. “We also print flexible inner sockets and some co-poly preparatory sockets,” says Meyer. “We’re still learning, but 3D printing helps with fabrication time and keeps dirt and debris to a minimum, and we’re getting good results so far.” He notes that the facility has been designing a lot of three-quarter brims for transfemoral amputations recently. “We’ve found that if you fit and cast them correctly, you don’t have to have a lot of proximal support, and it’s far more comfortable” for the patient.
Clinicians use direct-socket technology with some below-knee limb loss patients. “Once we get a gel liner on the patient, we can form a carbon shell over the top of the limb with a vacuum and use resin to
laminate and harden it. It will set in about 10 minutes, and if we have the componentry, we can fit them that day,” Meyer says. “It’s not for every situation, but when a patient needs to be fitted more quickly, it’s a good solution. If there is a lot of swelling in the residual limb, we can shrink the socket later after the swelling goes down. It’s solid enough to walk on, and it looks good.”
Burton Prosthetics has patented a transtibial socket that provides better support to the knee and posterior part of the knee, allowing it to bend more freely and create more control of the prosthesis, according to Meyer.
The facility is committed to the greater community as well and supports the Amputee Wellness Alliance of the Midlands. The organization aids limb loss patients in obtaining professionally fitted prostheses, particularly for sports, as well as for children. “We donate our time to help them serve the community,” Meyer says. Burton also supports Dear Diabetes, a club that offers diabetes education, and donates funds to several area organizations.
One of Meyer’s most memorable patients is Jen Rolf, a below-knee limb loss patient he has been working with for about 20 years. “She first started with a long residual limb and needed several revisions. But Jen always persists,” he says. “Jen ran a gym out of her home, she models for RUSH Feet, and she helps a lot of amputees who contact her. She has a presence on Instagram and Facebook, and she is so inspiring.”
Meyer sees a strong future for Burton Prosthetics. “We are always thinking about growing, and we are always curious about new technologies,” he says. He has considered adding more locations but decided that the facility is stronger under one roof. Instead, the business expands its reach by serving patients through clinics and hospitals throughout the area.
“We are about more than providing the nuts and bolts,” Meyer says. “We work for our patients in every way we can.”
Deborah Conn is a contributing writer to O&P Almanac. Reach her at deborahconn@verizon.net

BY DEBORAH CONN
OWNERS: Privately held



EWhy Am I an AOPA Member?
“AOPA keeps us connected to industry stakeholders and gives us the platform to communicate with them about our solutions, visions, and outcomes.”
—Kim De Roy
LOCATION: Carlsbad, California
HISTORY: Five years
levate Movement was founded in 2019 by Arni Thor, a 23-year veteran of orthotic design. His focus, and that of his collaborators, was to bridge the gaps in drop foot care.
“Arni had helped develop carbon-fiber ankle-foot orthoses (AFOs) in the early 2000s for Össur, and he noted that there had been no further development since then,” explains Kim De Roy, Elevate’s chief executive officer. Thor realized there was an opportunity to innovate in the reimbursable segment of the market, making the solutions more useful to clinicians and therapists and more functional to users. What makes Elevate’s solutions different, De Roy notes, is that they address drop foot right from the initial, acute phase all the way through the long term.
At the very start, patients who have suffered a stroke can receive the Sstep, a textile sock that places the foot in the right position without the need for shoes. The earlier treatment starts, the better for the patient, according to De Roy, as the product helps patients get on their feet almost immediately.
“The Sstep features an innovative support mechanism that gently lifts the drop foot to avoid toe stubbing, trips, and falls,” De Roy says. Both in the hospital, and then at home, the sock has been designed to allow the patient to walk around safely without having to don an AFO and shoe. Later in life, the sock is useful in the shower or at the beach, where users can walk on the sand, in the water, or on a boardwalk without shoes.
The second phase of acute drop foot begins after the patient is discharged from inpatient rehab and can receive an AFO. “Because clinicians only have 48 hours to deliver the device, most patients get off-theshelf orthoses,” says De Roy. “But many of them are unstable and need a custom-made device. Our custom-fabricated modular system and templates allow the O&P professional to build an AFO well within the two days available.”
The benefit, he says, is increased stability from the use of custom-fabricated thermoformable parts, which clinicians can gradually remove as patients progress
in rehabilitation. “Because the device can adapt to the patient’s needs, clinicians don’t have to fight for a redetermination of the patient to qualify for an entirely new device,” says De Roy.
For the long term, patients can use the sock in the comfort of their home, which allows them to be more independent. “It could make the difference between staying at home or having to go to a skilled nursing facility,” De Roy notes.
In designing Elevate’s products, Thor sought to serve the needs not only of patients, but of clinicians and business owners as well. “Elevate is all about taking what is a very basic product to more of a holistic, comprehensive treatment plan and protocol, so that all stakeholders—patients, clinicians, neurologists—benefit from our designs,” De Roy says.
Elevate offers several variations on its AFO, including the FreeFlow, a carbon-fiber AFO in a posterior design; the Glide, an anterior carbon-fiber AFO; the Helix Band, which offers multiplanar support with the FreeFlow and Glide; and the Swift, a device that progresses from triplanar stability to dynamic stability and then to flexible dynamics.
Based in Carlsbad, California, Elevate Movement has eight employees representing more than 100 years of experience in all phases of O&P. The company outsources manufacturing, with staff on the ground to monitor quality.
The company considers itself a clinical partner of O&P facilities and will accompany clinicians to rehab facilities. Elevate offers continuing education classes for physical therapists (PTs) to educate them about its products and will guide both clinicians and PTs through the process to improve patient outcomes.
As technology evolves, De Roy notes that the strength of Elevate’s solution is its simplicity. “Affordability and access to a device can be compromised by the cost of high tech,” he says. “We will keep our products simple and reasonably priced.”
Deborah Conn is a contributing writer to O&P Almanac. Reach her at deborahconn@verizon.net


































































































































ACCESS YOUR PERSONAL ACCOUNT, VIEW VIDEOS, PRINT CERTIFICATES, OR REVIEW CE CREDIT HISTORY 24/7.
Log in at https://aopahub.aopanet.org. Your username is the email used to create your profile. If you do not currently have an AOPAversity account, visit www.AOPAnet.org/education to create a profile.

Meet up in Orlando next September for the 2025 AOPA National Assembly! Network with O&P stakeholders, take part in educational sessions on the latest hot topics, browse the exhibit hall to see cutting-edge products, and much more.
The 2025 AOPA National Assembly will take place Sept. 3-6 at the Orange County Convention Center. Extend your trip to enjoy all that Orlando has to offer—bring friends or family!

Orlando is one of the most popular travel destinations in the United States and is home to several exciting theme parks—including Disney World, Universal Studios, and Gatorland, the first theme park in Orlando.

The Call for Presentations for the 2025 AOPA National Assembly is now open. AOPA encourages individuals to submit expert content by the March 12 deadline. The Assembly educational program will consist of general sessions as well as five concurrent breakout tracks. Please note that all submitters must create a new account to submit proposals for 2025, regardless of whether you submitted a proposal in a previous years.
Visit bit.ly/3ZxhJnH or email assembly@ aopanet.org for details.
Take part in the webinar
Registration is now open for AOPA’s Virtual Coding & Billing Seminar, designed to equip O&P professionals with the tools and knowledge to excel in today’s dynamic reimbursement environment. This seminar will take place March 24 and 25 from noon to 4 p.m. ET each day.
You’ll learn information in key areas of coding and billing:
• Hot topics, including the latest updates on HCPCS codes and reimbursement policies
• Expert tips for navigating Medicare audits and appeals
• Strategies to minimize denials and maximize reimbursements
• Coding and documentation best practices.
• Interactive Learning: Engage with experts in a virtual format
• Convenience: Participate from your home or office
• Practical Tools: Gain actionable insights to streamline your billing processes.
Let Joe McTernan; Devon Bernard; Jon Naft, CPO; Curt Bertram, CPO; and Lesleigh Sisson, CFm, CFo, help you navigate coding and billing challenges!
Visit aopanet.org or email info@aopanet.org
Designed to provide fast and reliable access to the latest HCPCS codes for orthoses, shoes, prostheses, and modifiers, this is a must-have, essential resource for streamlining your billing and coding process. The popular Quick Coder comes laminated so it is durable, long-lasting, and easy to store. The 2025 Quick Coder includes the new codes that are active as of April 1. Price is $45 for AOPA members and $95 for nonmembers.
How does your organization stack up against other O&P businesses? Find out by purchasing AOPA’s brand new “2024 O&P Operating Performance Report” and “2024 Compensation and Benefits Report.” These timely, in-depth reports provide up-to-date insights and data, empowering you to make informed decisions, drive growth, and stay ahead in a rapidly evolving landscape. The reports feature key performance metrics; information on trends and opportunities; and data-driven insights. Executives and leadership teams, operations and finance professionals, marketing and sales team, and clinic managers will gain a strategic advantage from accessing these reports.
Secure yours today: https://aopahub.aopanet.org/merchandise.
Purchase the full reports on the AOPA Hub, aopahub.aopanet.org, and contact Betty Leppin with questions, bleppin@aopanet.org


Embrace the comfort of custom-fit with Mt Emey®’s Custom Shoe (Medical) Program. Our precise 3D scanning captures your unique foot contours, promising a perfect fit without the wait or waste. From stylish athletics to roomy comfort designs, our handcrafted shoes adapt to your needs. Satisfaction guaranteed before payment. Plus, qualified wholesale accounts receive a free 3D scanner. Step into the Mt Emey difference— where every shoe is made for you.



The Coyote® Knee Cover is offered at a great price! The contoured shape was designed to fit the C-Leg 4 and help mimic the natural look of a leg while adding a cosmetically pleasing finish, and extra protection to the surface of the prosthetic knee. Its cushioning also helps stabilize patients when kneeling, enhancing both comfort and functionality. Available in multiple designs and colors, the Knee Cover includes fun and convenient features to suit every style.
For more information, contact Coyote at 208-429-0026 or visit coyote.us
For more information, call 1-888-937-2747 or visit emeys.com




Designed in partnership with COAPT, Fillauer’s Myo/One™ Electrode System is a streamlined, waterproof system that can reduce hours of trial and error into a couple quick minutes. Designed around one small preamplifier that provides two channels of EMG signal for myoelectric devices, the system replaces cables, fabrication aids, sealing rings, and multiple devices with one simple cable. Myo/One is a convenient, small, versatile, package which is compatible with almost all dual-site myoelectric devices and provides a much simpler system for dual-channel direct EMG control. Visit our website at fillauer.com to learn more.

Download the Hersco App on your iPhone and connect to the lab anytime. The Hersco app and order portal makes scanning and ordering seamless. Scan patients for foot orthotics, Richie Braces, and ankle gauntlets, and submit at your convenience. Our digital workflow allows you to easily track jobs, re-order devices, and manage your account. Download the app and get your username and password.
Our 3D printers produce accurate and precise orthotics, reducing landfill waste by over 90%!
Email us today at fastorthotics@hersco.com or call 800- 301-8275 to get a free product sample. Visit hersco.com
Located in Watchung, NJ.
A prime location, offering convenient access situated between major interstates Routes 78 and 22, ample parking, and excellent visibility. Offering the perfect blend of accessibility, functionality, and aesthetics to meet your needs. The property is just 45 minutes from the bustling business district of lower Manhattan, making it an ideal spot for companies looking to maintain close ties to the city while enjoying a suburban location. For more information, contact Kathy Shafer at 908-763-5505.




-A myoelectric arm orthosis that may help a user improve function in arms and hands paralyzed by a stroke, BPI, cerebral palsy, or other neuromuscular disease or injury.
Provide the MyoPro®: www.myomo.com/sign-up



Spinal Technology is the global leader in custom spinal orthoses design and fabrication, specializing in adolescent idiopathic scoliosis. Our expertise in patient assessment, orthosis design, and X-ray evaluation is trusted worldwide. We use advanced 3D technology in fabrication, combining it with traditional methods for optimal results. Our commitment extends to education, providing resources for practitioners and patients. We’ve manufactured over a million braces since 1991, continuously refining our expertise to achieve the best possible spinal corrections. Our collaborative approach aims to enhance the lives of all patients.
Visit spinal.tech/experiencematters or call 508-957-8311.
*Ask about our 2025 special mini-inventory discount package, including product training and virtual fitting help.
For 30 years, The Bremer Group Company has established a reputation for supporting practitioners and patients with quality back braces, and exceptional customer service.
For more information, call 800-428-2304 or visit www.bremergroup.com .



Turbomed’s leading line of foot drop ankle-foot orthoses sit completely outside the shoe for an invisible, painless support that will follow you as long and as far as you want. Their unique design acts as an exoskeleton to the impaired limb, keeps the foot at 90 degrees, and provides the user with unparalleled levels of function. Each model takes minutes to assemble and is easily transferrable to most shoes, boots, and sandals through an innovative lace clip design.
The Xtern Summit is the lightest model, has the most dorsiflexion power, and features a see-through design. The Xtern Frontier was designed for patients with reduced hand dexterity and requiring front leg support. Visit turbomedusa.com, and think outside the shoe!




ABC: Application Deadlines, Exams Dates, O&P Conferences, and More! Check out ABC’s Calendar of Events at abcop.org/calendar for the latest dates and event details, so you can plan ahead and be in the know. Questions? Contact us at info@abcop.org or visit abcop.org/contact-us
The Pedorthic Footcare Association: Diabetic Wound Prevention, Management, and Healing Program 10-session online education program series. Approved CEs by ABC and BOC, monthly classes are 1.5 hours each. For more information and to register, visit pedorthics.org/page/diabetic_series_10.
March 12
Deadline to Submit Proposal for 2025 AOPA National Assembly. Visit aopanet.org or email assembly@aopanet.org
March 24-25
AOPA Virtual Coding & Billing Seminar. Noon to 4 p.m. ET each day. To register, visit aopanet.org
June 13–14
27th Annual PrimeFare East—NEW VENUE! Downtown Marriott Hotel and Convention Center, Chattanooga, TN. Contact Cathie Pruitt at 901-359-3936, primecarepruitt@gmail.com, or visit primecareop.com
September 3–6
AOPA National Assembly. Orlando. For more information, visit aopanet.org
2026
September 22–25
AOPA National Assembly. Long Beach, CA. For more information, visit AOPAnet.org
Advertise O&P events for maximum exposure with O&P Almanac Contact Bob Heiman at bob.rhmedia@comcast.net or learn more at bit.ly/ AlmanacMediaKit25. Announcement and payment may also be sent to O&P Almanac, Calendar, P.O. Box 34711, Alexandria, VA 22334-0711, or emailed to jklapp@AOPAnet.org along with VISA or MasterCard number, cardholder name, and expiration date. Make checks payable in U.S. currency to AOPA. Note: AOPA reserves the right to edit calendar listings for space and style considerations.
ALPS South LLC 1 800-574-5426 easyliner.com




A large number of O&P Almanac readers view the digital issue— If you’re missing out, visit issuu.com/americanoandp to view your trusted source of everything O&P.
Scan the QR to start advertising in the O&P Almanac or visit bit.ly/AlmanacMediaKit25
Apis Footwear Co. 29 888-937-2747 apisfootwear.com
ComfortFit Orthotic Labs 3 888-523-1600 comfortfitlabs.com
Coyote Prosthetics & Orthotics 15 800-819-5980 coyote.us
Cypress Adaptive 9 888-715-8003 cypressadaptive.com
Fabtech Systems 25 800-322-8324 fabtechsystems.com
Ferrier Coupler Inc. 43 810-688-4292 ferrier.coupler.com
Fillauer Companies Inc. 21 423-624-0946 fillauer.com
Flo-Tech O&P Systems Inc. 13 800-356-8324 1800flo-tech.com
Hersco 23 800-301-8275 hersco.com
Myomo 33 888-669-1033 myomo.com
OrthoFeet Inc. C4 800-524-2485 https://orthofeet.shoes
Spinal Technology Inc. 5 508-957-8281 spinal.tech/almanac
The Bremer Group Co. 19 800-428-2304 bremergroup.com
TurboMed Orthotics 37 888-778-8726 turbomedorthotics.com
If you are interested

With the arrival of the new year, many states have already launched their 2025 legislative sessions. AOPA is keeping track of bills that could affect the provision of orthotic and prosthetic care throughout the country. While some states recently enacted legislation related to the So Every BODY Can Move (SEBCM ) initiative, several others are introducing SEBCM -related bills this year.
Maryland’s SEBCM bill, which was signed into law last May, went into effect Jan. 1, 2025. The legislation, which impacts state commercial plans and Medicaid, has already received a notable amount of news coverage in print and media outlets. Sheryl Sachs, MSPO, CPO, Maryland’s state lead for the project and a member of AOPA’s Government Relations and State Representatives committees, has been featured in several articles and on sites such as CBS News.
Policy changes are already being seen due to Minnesota’s SEBCM legislation, which was signed into law last May and took effect Jan. 1, 2025. Blue Cross Blue Shield of Minnesota’s commercial policies around “Myoelectric Prosthetic and Orthotic Components
for the Upper Limb” and “Microprocessor-Controlled Prostheses for the Lower Limb” have been updated with similar language changes to include running, biking, and swimming under potential physical needs that can be considered under the coverage of a prosthesis. In prior versions of these policies, prostheses “chiefly for convenience including participation in recreational activities” were deemed not medically necessary.
In New Jersey, Assembly Bill 3856— the state’s SEBCM bill—passed the Assembly Financial Institutions and Insurance Committee in December 2024. It has been referred to the Assembly Appropriations Committee. One of the bill’s primary sponsors, Assembly Member Antwan L. McClellan, is a member of this committee. The companion bill, Senate Bill 1439, passed in June of 2024.
Bill S1616/A2520 was introduced in January. If passed, Medicaid managed care organizations would be required to cover DMEPOS services at no less than 100% of established New York Medicaid fee rates. Matt Johnson, MPT, CEEAA, a member of the AOPA State Representatives committee, has helped organize outreach to representatives. New York residents are encouraged to write to their legislators. Visit AOPA’s LinkedIn page and the Co-OP for links.
The Texas Department of Licensing and Regulation (TDLR) implemented continuing education (CE) requirement changes. As of Jan. 6, 2025, TDLR will no longer confirm CE credits before renewing prosthetist or orthotist licenses. Now instead, you could be randomly selected for an audit of CE hours after you’ve renewed your license. Keep your CE records up to date.
Multiple states have introduced SEBCM legislation in 2025 in pursuit of creating equitable and life-changing access to prosthetic and orthotic care and devices for physical activity.
As of Jan. 23, 10 states have introduced bills in 2025 relating to increasing coverage of prosthetics and orthotics: Georgia, Massachusetts, New Hampshire, Maryland, Connecticut, Nebraska, Oregon, Indiana, Washington, and Tennessee. Visit soeverybodycanmove.org for details.