NEW REQUIREMENTS FOR SEVERAL CODES P.10

2024 AOPA NATIONAL ASSEMBLY: PREVIEW EDUCATIONAL SESSIONS P.26
TRANSFORMATIONS: PROSTHETIST RETURNS TRIATHLETE TO ACTIVITY WITH HELP FROM SEBCM LEGISLATION P.30


NEW REQUIREMENTS FOR SEVERAL CODES P.10

2024 AOPA NATIONAL ASSEMBLY: PREVIEW EDUCATIONAL SESSIONS P.26
TRANSFORMATIONS: PROSTHETIST RETURNS TRIATHLETE TO ACTIVITY WITH HELP FROM SEBCM LEGISLATION P.30

For O&P facilities, the benefits of artificial intelligence also bring questions P.16
SEPTEMBER 12-15, 2024
CHARLOTTE, NC

THE PREMIER MEETING FOR ORTHOTIC, PROSTHETIC, AND PEDORTHIC PROFESSIONALS.
Join us September 12–15, 2024, for an ideal combination of top-notch education and entertainment at the 107th AOPA National Assembly in Charlotte, NC.



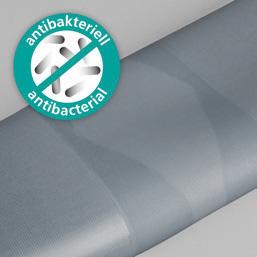
Part Number: RFX
Recommended for: K2-K4 activity levels
Features a centrally located internal fabric layer to withstand wear and tear around the brim line of the users' socket, alleviating some of the difficulty when dealing with reoccurring holes in higher active amputees.
OptiGel provides superior adhesion to the residual limb
Gray high-performance fabric limits vertical pistoning and increases control
30° pre-flexion to reduce bunching and discomfort behind the knee
Healthcare companies across the country are beginning to integrate aspects of artificial intelligence (AI) into their clinical practices—and O&P is no exception. Find out how AI will impact the provision of care as well as O&P documentation and reimbursement practices, and learn about the ethical challenges associated with the technology.
By CHRISTINE UMBRELL

Take a sneak peek at some of the most innovative and exciting educational sessions planned for the 2024 AOPA National Assembly in Charlotte, North Carolina, in September. View highlights from the Clinical, Digital, Business, Technical, and Pedorthic Tracks, and start setting your itinerary.


Meet Jonathan D. Day, PhD, CPO, and learn how he helped O&P advocate and para-triathlete Danielle Cummings return to an active lifestyle after undergoing osteomyoplastic transtibial amputation— using a prosthesis covered under new So Every BODY Can Move legislation.

Home of the original flexible clamshell side -specific anatomic RRD



Softie Guard the Incision Area From Micro Tears
The SOFTIE™ is constructed of firm but flexible Pelite, and comes with an anatomicallycorrect posterior strut, Velcro® compatible neoprene bands and a set of distal pads.
An economical alternative prefabricated prosthetic socket
Soft, non-constricting, easy to remove for wound concerns.



TransTibial

Adjustable Post-Op Preparatory Prosthetic System
This three-part post-operative preparatory prosthetic system allows the Prosthetist to provide a continuum of care, from the time of amputation, through early weight bearing, until the patient is ambulating independently.
All three sockets are part of a system that takes patients from post-op to definitive prosthesis.
TransFemoral
Adjustable Post-Op Preparatory Prosthetic System
Minimizes the effects of potential injury during both early and preparatory stages of rehabilitation. Adjustable, accommodates for compression and swelling. Permits measured and controlled weight bearing, through early ambulation.
Bridges the gap between postop and definitive prosthesis.




President
Mitchell Dobson, CPO, FAAOP Hanger Clinic, Austin, TX
President-Elect
Rick Riley
O&P Boost, Bakersfield, CA
Vice President
Kimberly Hanson, CPRH Ottobock, Austin, TX
Treasurer
Chris Nolan
Össur, Foothills Ranch, CA
Immediate Past President
Teri Kuffel, JD
Arise Orthotics & Prosthetics, Spring Lake Park, MN
Executive Director/Secretary Eve Lee, MBA, CAE
AOPA, Alexandria, VA
Arlene Gillis, MEd, CP, LPO International Institute of Orthotics and Prosthetics, Tampa, FL
Adrienne Hill, MHA, CPO(L), FAAOP Kennesaw State University, Kennesaw, GA
John “Mo” Kenney, CPO, LPO, FAAOP Kenney Orthopedics, Lexington, KY
James Kingsley
Hanger Clinic, Oakbrook Terrace, IL
Lesleigh Sisson, CFo, CFm Prosthetic Center of Excellence, Las Vegas, NV
Matt Swiggum Proteor, Tempe, AZ
Linda Wise
Fillauer Companies, Chattanooga, TN
Shane Wurdeman, PhD, CP, FAAOP(D) Research Chair
Hanger Clinic, Houston Medical Center, Houston, TX
AMERICAN ORTHOTIC & PROSTHETIC ASSOCIATION (AOPA)
330 John Carlyle St., Ste. 200 Alexandria, VA 22314
Office: 571-431-0876
Fax: 571-431-0899
AOPAnet.org
EXECUTIVE OFFICES
Eve Lee, MBA, CAE, executive director, 571-431-0807, elee@AOPAnet.org
Akilah Williams, MBA, SHRM-CP, director of finance and strategic operations, 571-431-0819, awilliams@AOPAnet.org
HEALTH POLICY AND ADVOCACY
Joe McTernan, director of health policy and advocacy, 571-431-0811, jmcternan@AOPAnet.org
Devon Bernard, assistant director of coding and reimbursement services, education, and programming, 571-431-0854, dbernard@AOPAnet.org
Sam Miller, manager, state and federal advocacy, 571-431-0814, smiller@AOPAnet.org
MEETINGS & EDUCATION
Ashley Vande Bunte, CMP, director, meetings and education, 571/431-0860, avandebunte@AOPAnet.org
Kelly O’Neill, CEM, assistant director, meetings and exhibitions, 571-431-0852, kelly.oneill@AOPAnet.org
MEMBERSHIP & COMMUNICATIONS
Joy Burwell, director of communications and membership, 571-431-0817, jburwell@AOPAnet.org
Betty Leppin, senior manager of member services, 571-431-0810, bleppin@AOPAnet.org
Nicole Ver Kuilen, manager of public engagement, 571-431-0836, nverkuilen@AOPAnet.org
Madison McTernan, coordinator of membership and communications, 571-431-0852, mmcternan@AOPAnet.org
AOPA Bookstore: 571-431-0876
Reimbursement/Coding: 571-431-0833, LCodeSearch.com
O&P ALMANAC
Eve Lee, MBA, CAE, executive director/publisher, 571-431-0807, elee@AOPAnet.org
Josephine Rossi, editor, 703-662-5828, jrossi@contentcommunicators.com
Catherine Marinoff, art director, 786-252-1667, catherine@marinoffdesign.com
Bob Heiman, director of sales, 856-520-9632, bob.rhmedia@comcast.net
Christine Umbrell, editorial/production associate and contributing writer, 703-662-5828, cumbrell@contentcommunicators.com
PUBLISHER EVE LEE, MBA, CAE
EDITORIAL MANAGEMENT CONTENT
COMMUNICATORS LLC
ADVERTISING SALES RH MEDIA LLC
DESIGN & PRODUCTION MARINOFF DESIGN LLC
PRINTING SHERIDAN
O&P Almanac (ISSN: 1061-4621) is published monthly, except for combined issues in June/July and November/ December, by the American Orthotic & Prosthetic Association, 330 John Carlyle St., Ste. 200, Alexandria, VA 22314. To subscribe, contact 571-431-0876, fax 571-431-0899, or email info@aopanet.org. Yearly subscription rates: $59 domestic, $99 foreign. All foreign subscriptions must be prepaid in U.S. currency, and payment should come from a U.S. affiliate bank. A $35 processing fee must be added for non-affiliate bank checks. O&P Almanac does not issue refunds. Periodical postage paid at Alexandria, VA, and additional mailing offices.
Postmaster: Send address changes to: O&P Almanac, 330 John Carlyle St., Ste. 200, Alexandria, VA 22314.
Copyright © 2024 American Orthotic and Prosthetic Association. All rights reserved. This publication may not be copied in part or in whole without written permission from the publisher. The opinions expressed by authors do not necessarily reflect the official views of AOPA, nor does the association necessarily endorse products shown in the O&P Almanac. The O&P Almanac is not responsible for returning any unsolicited materials. All letters, press releases, announcements, and articles submitted to the O&P Almanac may be edited for space and content. The magazine is meant to provide accurate, authoritative information about the subject matter covered. It is provided and disseminated with the understanding that the publisher is not engaged in rendering legal or other professional services. If legal advice and/or expert assistance is required, a competent professional should be consulted.
Share your message with AOPA membership— approximately 9,000 orthotic and prosthetic professionals, facility owners, and industry personnel. Contact Bob Heiman at 856-520-9632 or email bob.rhmedia@comcast.net. Learn more at bit.ly/24AlmanacMediaKit

The new Icon microprocessor knee features responsive sensors, streamlined setup, and the intuitive Stride Studio app. Our team has developed patented technology to put the Icon in a league of its own—providing remarkable accuracy, response time, and weight savings. Equipped with a long-lasting battery and IP68 rating, the Icon is the versatile solution for low to high activity users.


“I was surprised by the smoothness of the Icon’s microprocessor while walking. My favorite feature is that it’s waterproof in fresh water. During the summer months, I am always in and out of lakes, so being able to just jump right in without thinking twice is so nice.”
-Jake, Icon User




In a new study of individuals with diabetes from the “45 and Up Study” in Australia, the risk of lower-limb complications—including peripheral neuropathy, ulcers, cellulitis, Charcot foot, osteomyelitis, peripheral vascular disease, and minor or major amputation—was 1.5 times higher in men than women
SOURCE: “SEX
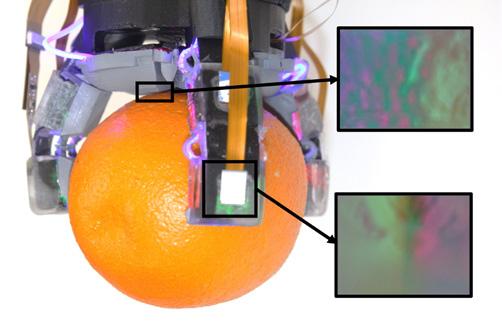
Researchers from the Massachusetts Institute of Technology (MIT) created a robotic hand with advanced tactile sensors, dubbed the GelPalm. The hand is designed to mimic the sensitivity and dexterity of a human hand and to handle objects with more detailed and delicate precision, according to the research team.
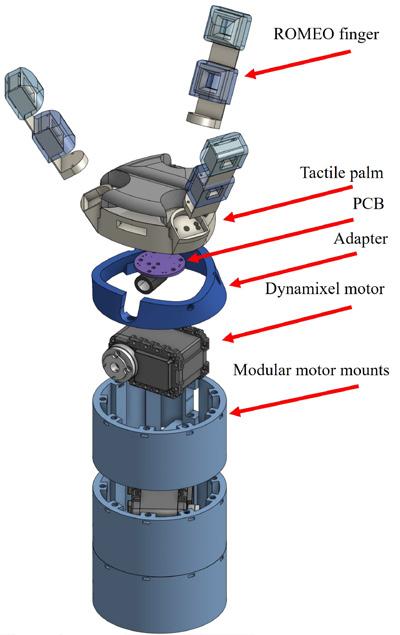
The device features a palm embedded with a gel-based, flexible sensor that leverages color illumination technology and a camera to generate 3D surface models for precise robotic interactions.
Led by Sandra Liu, MEng, PhD, and Edward Adelson, PhD, the research team also developed robotic phalanges called Robotic Module Endoskeleton Optical (ROMEO) fingers, to be used in conjunction with the GelPalm. The fingers are made of flexible materials and embedded with sensors; they feature “passive compliance” for natural adjustment to forces.
The GelPalm device has been designed to enable safer interaction with objects. “We draw inspiration from human hands, which have rigid bones
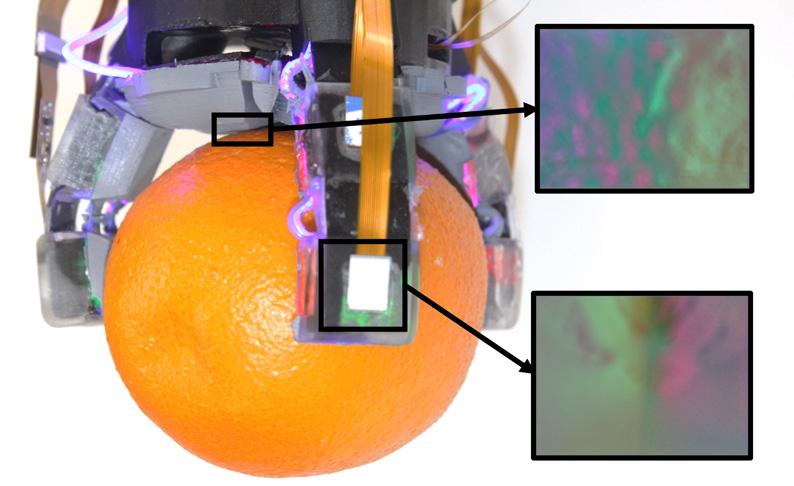
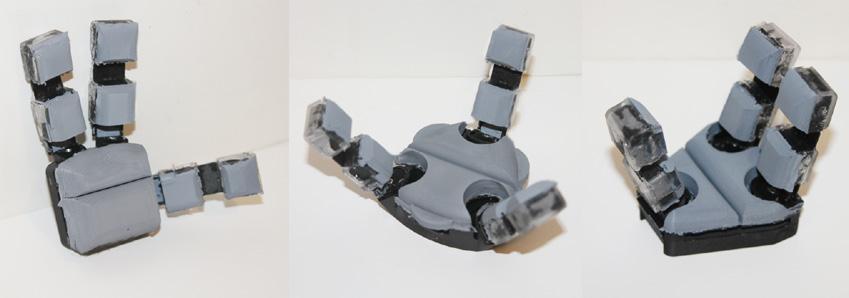
surrounded by soft, compliant tissue,” said Liu. “I hope we’re moving toward more advanced robotic hands that blend soft and rigid elements with tactile sensitivity, ideally within the next five to 10 years,” she said. “In developing GelPalm and the ROMEO fingers, I focused on modularity and transferability to encourage a wide range of designs. Making this technology low-cost and easy to manufacture allows more people to innovate and explore.” The research was published in arXiv.org
Recognizing that individuals with kidney failure face an increased risk of diabetesrelated foot complications, a multidisciplinary team of researchers conducted a study to investigate whether foot and ankle care by podiatrists before the onset of diabetic foot ulcers (DFUs) would improve patient outcomes.
“Up to 34% of adults with diabetes develop DFUs, and two-thirds of DFUs recur, even after healing,” noted the researchers. “These foot ulcers precede 80% of lower-extremity amputations and are associated with diminished physical function, reduced quality of life, and increased mortality risk.”
The researchers studied a national cohort comprising nearly 15,000 Medicare beneficiaries with diabetes aged 40 and older with kidney failure. They discovered that only 18.4% of patients
received care by podiatrists within the three months preceding the DFU diagnosis. They assessed two outcomes: amputation-free survival and time to major amputation.
Patients with kidney failure who were receiving dialysis who also received foot and ankle care from a podiatrist within the three months preceding a DFU diagnosis experienced reduced risk of major amputation and death, according to the researchers. In addition, the rate of major amputation—above-knee or below-knee amputation—also decreased.
“While future fully powered studies are needed to further support these findings,” they said, “these results suggest positive potential benefits for preventive foot and ankle care to mitigate complications in this high-risk population.” The study was published in March in JAMA Open Network
This September, take advantage of all that Charlotte, North Carolina, has to offer—extend your stay before or after the AOPA National Assembly, Sept. 12-15, or bring your family for some exciting adventures.
Charlotte is famous for its rich NASCAR history, entertainment options, and restaurants and breweries. Consider visiting some of these locations to make the most of your visit to Charlotte:
NASCAR Hall of Fame: This interactive museum celebrates the history of stock car racing and the sport’s legendary drivers. Visit nascarhall.com
2 3
Uptown Charlotte: This bustling urban center offers dining, museums, sporting events, rooftop bars, the Levine Museum of the New South, the Mint Museum Uptown, and much more. Visit uptowncharlotte.com
Freedom Park: This 98-acre park, centered on a 7-acre lake, offers paved trails, tennis and volleyball courts, playground equipment, and plenty of open spaces for picnics and relaxation. Visit charlottenc.gov/home
Carowinds Amusement Park: This fun-filled amusement park is home to more than 60 world-class rides, a waterpark, live entertainment, and more. Visit carowinds.com
NoDa Arts District: Charlotte’s historic arts district, NoDa, is a vibrant arts district featuring eclectic galleries, live music, and dining and brewery options. Visit noda.org
Daniel Stowe Botanical Garden: This can’t-miss outdoor experience features a world of natural wonder and beauty, offering displays of flora and peaceful walking paths. Visit dsbg.org
For details regarding the AOPA National Assembly, registration for the conference, accommodations, exhibitors, and more, visit aopaassembly.org. Book your hotel by Aug. 15 for the best rates. Questions? Contact assembly@AOPAnet.org or call 571-431-0876. 1 4 5 6 7
U.S. National Whitewater Center: Encompassing 1,300 acres on the Catawba River, the center attracts outdoor enthusiasts—offering whitewater rafting, kayaking, rock climbing, and zip-lining. Visit center.whitewater.org
Several members of Team Össur and Össur Ambassadors displayed award-winning performances at the 2024 Para Athletics World Championships in Kobe, Japan.
Össur athletes captured a total of 14 medals at this year’s Worlds, including five gold, six silver, and three bronze medals. Dutch athlete Fleur Jong successfully defended her gold medal in the T62/64 women’s long jump category with another first-place finish and a championship record of 6.53 meters. Marlene van Gansewinkel took the silver with a season-best of 5.45 meters.

Other medalists in various events included U.S. athletes Beatriz Hatz, Derek Loccident, Trenten Merrill, and Hunter Woodhall; Germany’s Markus Rehm; and Costa Rican athlete Sherman Guity.
“We continue to be inspired by the extraordinary accomplishments of the athletes who competed at this year’s World Championships,” said Sveinn Sölvason, president and chief executive officer of Embla Medical, the parent company of Össur. “Such extraordinary results are especially exciting, considering the next major international event that will take place in Paris this summer.”

The amount of data housed in the Limb Loss & Preservation Registry (LLPR) is rapidly expanding: Ten participating hospital systems and 23 participating O&P practices are currently providing data to the LLPR from 221 locations throughout the U.S. Data from nearly 500,000 unique patients and nearly 12 million episodes of care are housed in the registry.
SOURCE: “SUMMARY
A new study from Kaiser Family Foundation demonstrates the financial burdens associated with medical debts and notes that people in families with medical debt are more likely to forgo medical or dental care.
Likelihood of Delaying or Forgoing Healthcare
Had a medical problem but did not go to healthcare practitioner due to cost
Skipped a medical test, recommended treatment, or follow-up care due to cost
Did not fill a prescription due to cost
Experienced any of the above
The Orthotics and Prosthetics Foundation for Education and Research and the American Board for Certification in Orthotics, Prosthetics, and Pedorthics (ABC) have announced the recipients of the 2024 ABC Student Poster Prizes.
Megan Grunst, MPO, took first place for “Effects of Prosthetic Design Features on Osteoarthritis Risk in the Sound Limb: A Scoping Review.” Grunst is a recent graduate of Northwestern University Prosthetics-Orthotics Center (NUPOC) and an incoming prosthetic resident at the Minneapolis VA Medical Center. Pauline M. Porucznik, MPO, and Kate M. Grylicki, MPO, who both graduated from NUPOC and are current O&P residents, contributed to the poster.
Jacob Wilbert took second place for “Exposure to Orthotics and Prosthetics in Undergraduate Kinesiology Students in the Southeastern United
Household spends more than income
Very difficult to pay bills
Has no rainy-day fund
Probable or certain they could not find $2,000 in emergency
Strongly agree finances make them anxious Never or rarely have money left at end
States.” Wilbert recently graduated from Alabama State University’s P&O program and will continue to a combined O&P residency with Hanger Clinic in Knoxville, Tennessee.
Brogan Comstock took third place with “Tensile Strength Testing of Biopolyethylene and Recycled Polyethylene as Alternative Materials for AnkleFoot Orthoses.” Comstock is a second-year master’s student in O&P from California State University— Dominguez Hills.
Joe Fairley, CP, has been hired as the business development manager for Orten, the business unit of Proteor, as part of the digital services team. Fairley, a certified prosthetist and board-eligible orthotist, was previously the founder, chief executive officer, and owner of Ascent Fabrication and Amplify Prosthetics.
UPDATE ON GRACE PROSTHETIC FABRICATION
In the Member Spotlight on Grace Prosthetic Fabrication in the April 2024 issue of O&P Almanac, owner Tony Culver was mis-identified. Culver is the stepbrother of founder Ed Grace. O&P Almanac apologizes for the error and any confusion.
Hip-knee-ankle triple flexion with 125° knee flexion and 42° ankle ROM STABILITY
92% greater flat-foot time and 2X more toe clearance for optimal security
LIFE
Greater confidence with more shoe options, longer battery life, and ease while walking

855.450.7300 shop.proteorusa.com
BY DEVON BERNARD
Which codes now require prior authorization, WOPDs, or face-to-face encounters prior to payment?

As we hit the midyear mark for 2024, we have seen some updates that may impact O&P coding and reimbursement practices. We have seen a 2.6% fee increase; new fees for codes L8701, L8702, and K1007; the introduction of some new codes, including L5991, L5926, and L5783; the introduction of a new benefit category for lymphedema compression garments; policy article updates; and the conclusion of the first round of competitive bidding for select orthoses. Some big changes also loom on the horizon. By the end of the year, we may see the Lower-Limb Prosthesis Policy updated to consider coverage of microprocessor and
hydraulic/pneumatic technology for select K2 ambulators.
In addition, Medicare recently added new codes to the lists of codes requiring prior authorization, codes requiring written orders prior to delivery (WOPDs), and codes requiring face-to-face (F2F) encounters. This month’s Reimbursement Page explores these updates.
CMS on May 13 released an updated Master List—a list of all durable medical equipment and orthotic/prosthetic Healthcare Common Procedure Coding System (HCPCS) codes that meet specific criteria for high-risk
exposure to waste, fraud, and abuse and that Medicare believes may require additional conditions of payment—such as prior authorization, WOPDs, or F2F encounters. This most recent update added 76 codes, for a total of 512 codes. Eleven of those codes are O&P codes: L0457, L1681, L2006, L2280, L3761, L4000, L5615, L5926, L5991, L6026, and L7366
Codes on the Master List are not automatically subject to additional conditions of payment; inclusion means that they may be selected for these additional conditions of payment at a future date. In other words, the codes must be moved from the Master List to the Requires Prior Authorization
List or Requires WOPD List for these extra conditions to apply.
For a code to be added to the Master List, it must meet one of the following criteria:
• Have an average purchase fee of $500 or greater that is adjusted annually for inflation (in 2024, the fee would be $588 or greater)
• Any item with at least 1,000 claims and $1 million in payments during a recent 12-month period that is determined to have aberrant billing patterns
• Any item statutorily requiring a F2F encounter, a WOPD, or prior authorization.
When a code is placed on the Master List, it typically remains on the list for 10 years. However, that 10-year window can be expanded, if warranted by reports from the Comprehensive Error Rate Testing Program or the Office of Inspector General,
or if that code continues to have a high improper payment rate. A code also may be removed before the 10-year window expires; this typically occurs when the purchase amount drops below the required payment threshold.
In 2024, code L1833—knee orthosis (KO), adjustable knee joints (unicentric or polycentric), positional orthosis, rigid support, prefabricated, off the shelf—fell below the threshold and was removed from the Master List, and as such would no longer be subject to any special conditions of payment.
Six orthotic codes from the Master List will require prior authorization as a condition of payment effective Aug. 12, 2024. (See sidebar on page 12).
Unlike with previous implementations of the prior authorization condition of payment, these six codes will not be phased in; rather, they will be implemented nationwide for all claims with a date of service on or after Aug. 12, 2024.
In addition, for claims with a date of service on or after Aug. 12, 2024, code L1833—KO, adjustable knee joints (unicentric or polycentric), positional orthosis, rigid support, prefabricated, off the shelf—will no longer require prior authorization as a condition of payment as it was removed from the Master List. This brings the total number of O&P codes requiring prior authorization to 16.
As with the previous codes requiring prior authorization, the newly selected codes also will require Pricing Data Analysis and Coding (PDAC) contractor coding verification and will be listed on the PDAC Product

Six orthotic codes from the Master List will require prior authorization as a condition of payment:
• L0631—Lumbosacral orthosis (LSO), sagittal control, with rigid anterior and posterior panels, posterior extends from sacrococcygeal junction to T-9 vertebra, produces intracavitary pressure to reduce load on the intervertebral discs, includes straps, closures, may include padding, shoulder straps, pendulous abdomen design, prefabricated item that has been trimmed, bent, molded, assembled, or otherwise customized to fit a specific patient by an individual with expertise
• L0637—LSO, sagittal-coronal control, with rigid anterior and posterior frame/panels, posterior extends from sacrococcygeal junction to T-9 vertebra, lateral strength provided by rigid lateral frame/panels, produces intracavitary pressure to reduce load on intervertebral discs,
includes straps, closures, may include padding, shoulder straps, pendulous abdomen design, prefabricated item that has been trimmed, bent, molded, assembled, or otherwise customized to fit a specific patient by an individual with expertise
• L0639—LSO, sagittal-coronal control, rigid shell(s)/panel(s), posterior extends from sacrococcygeal junction to T-9 vertebra, anterior extends from symphysis pubis to xyphoid, produces intracavitary pressure to reduce load on the intervertebral discs, overall strength is provided by overlapping rigid material and stabilizing closures, includes straps, closures, may include soft interface, pendulous abdomen design, prefabricated item that has been trimmed, bent, molded, assembled, or otherwise customized to fit a specific patient by an individual with expertise
L1843—Knee orthosis (KO), single upright, thigh and calf, with adjustable flexion and extension joint (unicentric or polycentric), medial-lateral and rotation control, with or without varus/ valgus adjustment, prefabricated item that has been trimmed, bent, molded, assembled, or otherwise customized to fit a specific patient by an individual with expertise
• L1845—KO, double upright, thigh and calf, with adjustable flexion and extension joint (unicentric or polycentric), medial-lateral and rotation control, with or without varus/valgus adjustment, prefabricated item that has been trimmed, bent, molded, assembled, or otherwise customized to fit a specific patient by an individual with expertise
• L1951—Ankle-foot orthosis, spiral, Institute of Rehabilitative Medicine type, plastic or other material, prefabricated, includes fitting and adjustment.
Classification List. Currently, L0631, L0637, L0639, and L1843 already require PDAC verification so only the L1845 and L1951 will need to be reviewed and added to the PDAC coding verification list.
To meet this requirement and allow time for the verification process, the durable medical equipment Medicare administrative contractors and PDAC have announced that all items using codes L1843 or L1951 will require PDAC coding verification by Dec. 1, 2024. Any items currently verified and listed as L1843 or L1951 on the PDAC Product Classification List will not need to be reverified.
AOPA is currently verifying whether the emergent care exemption and the ST modifier would be available for these six new codes. While the ST modifier will
allow claims to be processed immediately, without a prior authorization, claims are still subject to a prepayment review. In 2022 and 2023, 100% of claims would have been subject to prepayment review; however, CMS stated that, starting in 2024, only 50% of the claims would be subject to prepayment review.
CMS also announced in May that eight O&P HCPCS codes will require a F2F encounter as a condition of payment for claims with a date of service on or after Aug. 12, 2024 (see sidebar on page 14)
A F2F encounter does not mean a mandatory visit with the orthotist for delivery or evaluations; rather, it refers to the patient
having an encounter/visit with the ordering/referring physician or other eligible professional (nurse practitioner, physician assistant, etc.) prior to the order being written. A F2F encounter has five key requirements:
• The encounter must occur within six months prior to the physician, or other eligible professional, writing the order; not adhering to this timetable is a common denial reason in audits
• The encounter or visit must be used by the eligible practitioner to gather information associated with the diagnosis, treatment, or management of a clinical condition for which the orthosis is being ordered; this includes things such as physical exams, diagnostic tests, progress notes, treatment plans, etc.
• All findings and notes must be documented in the patient’s medical record— and not on an order or a letter of medical necessity
• All documentation of the encounter must be kept on file and made available upon request
• The use of telehealth is acceptable for the F2F encounter provided that all of the regulatory requirements for a telehealth visit have been met; currently, the exemptions and expansion of telehealth created by the COVID-19 public health emergency are still active, but they are set to expire at the end of 2024.
When CMS updated the required F2F encounter list, it announced that eight new orthotic codes will require a WOPD as a
condition of payment for claims with a date of service on or after Aug. 12, 2024. The eight codes are the same as the eight new F2F encounter codes: L0635, L0636, L0638, L0639, L0640, L0651, L1845, and L1852.
Previously, L1833 was subject to the F2F encounter/WOPD requirement. However, because it has been removed from the Master List, this is no longer the case and, as of May 13, L1833 no longer requires a F2F encounter or WOPD as a condition of payment. With the addition of the eight codes and the removal of L1833, the total number of O&P services requiring a F2F encounter and WOPD is 23, as of Aug. 12, 2024.
The WOPD requirement is relatively self-explanatory. The core elements of a standard written order (SWO) and WOPD are the same; however, a SWO must be










on file prior to billing and a WOPD must be on file prior to delivery. In most cases, with the WOPD, the treating practitioner must document and communicate to you—the supplier—that they have had a F2F encounter with the patient within the six months prior to the date on the written order.
A SWO/WOPD must include the following elements to be considered valid for Medicare purposes:
• Patient name or Medicare Beneficiary Identifier
• Order date
• General description of the item (narrative description, HCPCS code/descriptor, brand name/model number, etc.)
• Quantity to be dispensed
• Treating practitioner’s name or National Provider Identifier
• Treating practitioner’s signature.




• Reimbursements for prosthetic & orthotic L codes
• 25% increased stiffness over standard polypropylene
• Available in cut-to-size blanks



With the increase in separation of the types of items being ordered and delivered (i.e., custom fabricated, custom fitted, off the shelf, etc.) and sometimes not knowing which base code will be provided and billed until the time of delivery, you should consider moving away from simply using HCPCS codes and descriptors with your orders. At a minimum, remove the phrases “off the shelf” or “customized to
fit a specific patient by an individual with expertise.” Doing so may save some time and headaches down the road, including the possibility of having to get a new and revised order if something changes at the time of delivery.
The Aug. 12, 2024, implementation deadline is around the corner, so be sure to update your policies and procedures and educate your staff and referral sources.
Everyone at your facility should be ready for the newest implementation of WOPD, F2F encounter requirements, and the expansion of the prior authorization program.

Devon Bernard is AOPA’s assistant director of coding and reimbursement services, education, and programming. Reach him at dbernard@AOPAnet.org
The following eight Healthcare Common Procedure Coding System codes will require face-to-face encounters as a condition of payment:
• L0635—Lumbosacral orthosis (LSO), sagittal-coronal control, lumbar flexion, rigid posterior frame/panel(s), lateral articulating design to flex the lumbar spine, posterior extends from sacrococcygeal junction to T-9 vertebra, lateral strength provided by rigid lateral frame/panel(s), produces intracavitary pressure to reduce load on intervertebral discs, includes straps, closures, may include padding, anterior panel, pendulous abdomen design, prefabricated, includes fitting and adjustment
• L0636—LSO, sagittal-coronal control, lumbar flexion, rigid posterior frame/ panels, lateral articulating design to flex the lumbar spine, posterior extends from sacrococcygeal junction to T-9 vertebra, lateral strength provided by rigid lateral frame/panels, produces intracavitary pressure to reduce load on intervertebral discs, includes straps, closures, may include padding, anterior panel, pendulous abdomen design, custom fabricated
• L0638—LSO, sagittal-coronal control, with rigid anterior and posterior frame/panels, posterior extends from sacrococcygeal junction to T-9 vertebra, lateral strength provided by
rigid lateral frame/panels, produces intracavitary pressure to reduce load on intervertebral discs, includes straps, closures, may include padding, shoulder straps, pendulous abdomen design, custom fabricated
• L0639—LSO, sagittal-coronal control, rigid shell(s)/panel(s), posterior extends from sacrococcygeal junction to T-9 vertebra, anterior extends from symphysis pubis to xyphoid, produces intracavitary pressure to reduce load on the intervertebral discs, overall strength is provided by overlapping rigid material and stabilizing closures, includes straps, closures, may include soft interface, pendulous abdomen design, prefabricated item that has been trimmed, bent, molded, assembled, or otherwise customized to fit a specific patient by an individual with expertise
• L0640—LSO, sagittal-coronal control, rigid shell(s)/panel(s), posterior extends from sacrococcygeal junction to T-9 vertebra, anterior extends from symphysis pubis to xiphoid, produces intracavitary pressure to reduce load on the intervertebral discs, overall strength is provided by overlapping rigid material and stabilizing closures, includes straps, closures, may include
soft interface, pendulous abdomen design, custom fabricated
• L0651—LSO, sagittal-coronal control, rigid shell(s)/panel(s), posterior extends from sacrococcygeal junction to T-9 vertebra, anterior extends from symphysis pubis to xyphoid, produces intracavitary pressure to reduce load on the intervertebral discs, overall strength is provided by overlapping rigid material and stabilizing closures, includes straps, closures, may include soft interface, pendulous abdomen design, prefabricated, off the shelf
• L1845—Knee orthosis (KO), double upright, thigh and calf, with adjustable flexion and extension joint (unicentric or polycentric), medial-lateral and rotation control, with or without varus/ valgus adjustment, prefabricated item that has been trimmed, bent, molded, assembled, or otherwise customized to fit a specific patient by an individual with expertise
• L1852—KO, double upright, thigh and calf, with adjustable flexion and extension joint (unicentric or polycentric), medial-lateral and rotation control, with or without varus/valgus adjustment, prefabricated, off the shelf.





CHRISTINE UMBRELL

Healthcare companies—including O&P facilities—face opportunities and challenges in leveraging artificial intelligence

What can artificial intelligence (AI) do for my organization? That’s the question healthcare professionals across the country are asking as ChatGPT, Google Gemini, and other chatbots take over the internet and infiltrate the workplace. The answer, according to AI experts, is: More than you could possibly imagine. Healthcare facilities of all types and sizes are embracing aspects of AI to build more efficient, outcome-driven practices equipped to deliver optimal patient care. With the capacity to learn and establish correlations between incoming patient data and corresponding outcomes, AI can provide healthcare professionals with the ability to improve patient interventions, including orthotic and prosthetic care.
As O&P companies shift toward AI-driven practices that facilitate predictive healthcare and aid clinicians in diagnoses, documentation, and other aspects of their work, they will need to not only understand
f Healthcare organizations of all types and sizes are exploring and adopting aspects of artificial intelligence (AI)—IT systems that can sense, comprehend, act, and learn.
f Some healthcare facilities leverage AI to establish correlations between incoming patient data and corresponding outcomes to facilitate predictive healthcare and improve patient interventions.
what AI can do but also consider what constitutes ethical use of AI, as well as privacy and security considerations for facilities and patients.
At a basic level, AI can be defined as “IT systems that sense, comprehend, act, and learn; intelligence demonstrated by software with the ability to depict or mimic human brain functions,” says Tom Lawry, managing director of Second Century Tech and a former Microsoft executive who served as the company’s national director of AI for health and life sciences. Lawry spoke at the AOPA Leadership Conference in January and is author of Hacking Healthcare—How AI and the Intelligent Health Revolution Will Reboot an Ailing System.
f Within O&P, AI may be used to augment the clinician’s work—potentially improving the workflow, reducing the need for trial-and-error, and fostering more personalized O&P care.
f AI also may facilitate more effective administrative services, aid in documentation practices, and optimize healthcare resources to improve efficiencies.

Tom Lawry
f AI technology introduces a suite of ethical challenges— particularly in the areas of bias and fairness; transparency and accountability; privacy and security; and informed consent.
f O&P facilities that choose to leverage AI may gain a competitive advantage—as long as they focus on responsible AI principles and “ethical AI” in healthcare.
Lawry notes that AI can not only boost the accuracy of predictive models but also improve the workflow in health and medicine by either automating or augmenting the way work is done. Because the jobs of most healthcare professionals—including orthotists and prosthetists—cannot be automated, he categorizes healthcare providers as “knowledge workers”—possessing skills that cannot be automated but may be augmented. For example, he says that AI can assist in providing clinical decision support: “Rather than having to go through a whole litany of things to try and determine what to do with a patient, AI points clinicians to various things that help them make the right decisions for a patient.”
Most healthcare knowledge workers are challenged by everaccelerating technological advances, rendering their jobs more complex, Lawry explains, so AI may help these professionals improve clinical and operational workflow processes. “AI can help on the administrative side with things like optimizing, coding, and improving reimbursement,” he suggests.

“If you’re creating a prosthetic device, the ability to have AI help analyze individual patient data could enhance the creation of a highly customized prosthesis that takes into account specific anatomical needs and lifestyle requirements,” Lawry explains. “The clinician developing the device is already very good at [such a task], but AI can help make them better or help them optimize their time.”
Other tasks that may be facilitated by AI include assisting in analyzing medical imaging data, such as scans, to aid in the design and fabrication of O&P devices, Lawry says. He also suggests leveraging AI-powered sensors that are built into prostheses and orthoses to track usage patterns, provide data analysis, and assess pressure points, “even allowing for constant remote monitoring of patients’ progress, say following surgery or at initial use of a prosthesis.”
Similarly, business expert Chuck Gallagher believes AI has the potential to drive almost limitless advances in the provision of healthcare services. Gallagher, who will deliver the AI-themed keynote presentation at the AOPA National Assembly
in September, says AI poses “great potential for transformative changes in healthcare.” AI may offer more effective administration services and optimize healthcare resources—through process improvement, but also by using novel technologies such as machine learning and natural language processing to facilitate personalized care and early diagnosis of disease.
AI may, for example, “be better than a person at reading X-rays,” he says, because it may be able to identify finer areas of distinction. “From a practical perspective,” Gallagher explains, “an X-ray is a black-and-white image. A radiologist is trained to look for areas that may be a tumor. An AI may not see a ‘tumor,’ but it may see shades a human cannot see” and point out areas that may need further attention.
As AI facilitates more accurate predictive healthcare, O&P professionals will be empowered to provide more personalized care. Currently, U.S. healthcare faces a growing need to manage an aging population with increased healthcare needs, says Shane Wurdeman, PhD, CP, FAAOP(D), vice president of scientific affairs at Hanger. “The O&P landscape is not sheltered from this and will need to determine how to be more effcient and effective with limited resources,” he says. AI will provide guidance on best clinical options for patients, taking into account their individual needs, according to Wurdeman. Most importantly, “AI will facilitate the movement from what is the ‘best technical option’ to instead what is the ‘best unique clinical option’ for each person.” (See the sidebar “AI at Work” on page 20.)

Given the advantages AI offers for O&P practices, Wurdeman and his Hanger colleague Molly McCoy, CPO, clinical documentation specialist, are part of a large, cross-functional team at Hanger—which includes clinicians, software engineers, scientists, compliance experts, and more—preparing to leverage the technology on a more consistent basis. Over the past year, “Hanger has diligently been working on building an AI model for Hanger Clinic by leveraging current GPT-4 large language model technology,” says Wurdeman. “Essentially, we are educating ChatGPT about all things O&P. We will launch Hanger Clinic’s AI assistant this year to help reduce the burden of clinical documentation for our clinical staff and facilitate ease of access for patients.”
Smaller O&P companies also may find ways to leverage AI to set their facilities apart, according to Lawry. “Remember AI is a tool, and if you can figure out how to leverage AI to be better at what you do, that’s not something that’s reserved for big companies,” he notes. “That’s for any organization or individual that has an understanding of what AI can do, and that has an expertise in serving O&P patients.” In fact, “much of what we’re seeing” in healthcare in general “is actually smaller organizations using AI as a differentiation point—and getting out ahead of some of the larger organizations in healthcare today.”

CUSTOM: FOOT ORTHOTICS • AFO’S • RICHIES
One size does not fit all. At Hersco, our team of professionals works to fabricate orthotics from your scans and casts to match your patients’ specific needs. Customer service is at the heart of everything we do and we work endlessly to help you be as effective and efficient as possible. When you want the job done quickly and accurately, Hersco is here to help.


Many O&P companies are already embracing AI, as the technology can help remove the trial-and-error “that can result from working with medically complex patients for whom we may be missing historical information,” says Molly McCoy, CPO, clinical documentation specialist at Hanger. “More specifically, we will begin to integrate medical records, outcomes, and practice workflows to improve prognostication and enhance clinical practice,” she says.

McCoy offers the following example of how AI could positively influence O&P clinical care: “The best clinical option for many patients with amputation through the femur is often a microprocessor-controlled knee (MPK) because of the stability and intuitive use, among other features. For patients with medical complexity, we need to explain how that MPK will support overall health that is specific to a patient’s comorbid conditions,” she says.
“So, how can we impact health with an MPK for a patient—let’s call her Ms. Jones—who had an amputation at age 20 and now, at 60 years old, also has congestive heart failure and diabetes that are well managed medically most of the time? It can be difficult to
In addition to facilitating predictive healthcare and improving patient care, the most significant impact of AI may be in the area of O&P documentation, according to Wurdeman. “The burden of clinical documentation is expanding exponentially and creates greater pressure for a solution to assist clinicians in their ability to help patients,” he says. “The result of the need—combined with the advent of the large language models that we are seeing become more common—presents an opportunity for a solution to a growing challenge.”
This may eventually lead to more appropriate reimbursement: “With reduction in time-consuming tasks for both providers and payors—combined with improved guidance and prognostication for better clinical outcomes—there becomes a real opportunity for improved reimbursement,” suggests Wurdeman.
“Implementing AI in O&P to help write more effective documentation makes sense in light of the fact that payors have been using precursor AI technology—such as natural language processing—for years, and they are increasingly using cutting-edge AI technology in processing claims,” agrees McCoy. As a result, “denials are becoming more detailed, patient specific, and medically focused. In order to respond to
weed through a large amount of medical records to find that she has these comorbidities, and often even harder to know what the pertinent side effects are from these comorbidities and medications during a clinical appointment.
“If AI pre-reads Ms. Jones’ medical records, it could potentially highlight that she has congestive heart failure and diabetes that are medically managed with medication, and she has struggled in the past with some medication side effects—something she might not think to mention during her appointment for prosthetics,” says McCoy. “The AI could also tell you the most common side effects of heart failure medications: feeling tired, dizziness, wheezing/ shortness of breath, low blood pressure, and a slow heart rate.
“When Ms. Jones arrives for her evaluation, you might ask if or when she has these side effects. You would then potentially use the AI to help write a note about your recommendation: ‘Ms. Jones needs to stay physically active to help manage her diabetes. At the same time, she needs the extra safety and stability provided by an MPK because when walking she occasionally has dizziness and feels tired from her heart medication,’” suggests McCoy. “The end result is communication of the component choice with medically relevant, patient-specific information—with little to no extra time spent hunting for the information, wordsmithing the note, or a lengthy Q&A session.”

or avoid such denials, we need to implement AI to be at least as efficient—if not more—in clinical reasoning communication.”
McCoy emphasizes that “clinical documentation is clinical care,” explaining that “AI can enhance our ability to understand our patients at a deeper level by enabling use of medical records information, incorporating patient-reported outcomes data into our decision-making, and helping us create better patient results and more effective documentation,” she says. “When used correctly, AI creates the potential for more heartfelt improvements than just time efficiency. It can empower the patient to be more of a participant in their care and an acting team member in the design process.”






Business expert Chuck Gallagher will share his expertise on the topic of artificial intelligence (AI) during the keynote address at this year’s AOPA National Assembly in Charlotte, North Carolina. He will deliver his presentation, “The AI Revolution: Unlocking the Future of Business,” during the Opening Remarks and Keynote Presentation beginning at 8 a.m. Friday, Sept. 13.
“We will pull back the curtain and think of practical, real-world applications of AI,” says Gallagher. He will explain what it takes to harness the boundless power of AI to the benefit of O&P companies—and will provide live demonstrations of AI applications and other cutting-edge technologies. Plan now to attend this important keynote presentation to stay at the forefront of AI advancements and acquire the insights necessary to fuel innovation and expansion at your O&P organization. “We’ll be doing it live,” says Gallagher, “and we’ll have fun.”
AI also may enhance the O&P research and development process, ultimately reducing the time it takes to implement new strategies and launch new devices. “By nature, scientists are trained to be skeptical, and adapting to new technology can present challenges,” explains Wurdeman. AI creates an opportunity “to quickly analyze large data [sets] and look at practice patterns in somewhat real-time to facilitate rapid changes.”
Faster data analysis “can help advance care techniques and reduce the average 17-year timeframe it takes for new findings to be integrated into clinical practice,” Wurdeman adds. To accomplish such a time reduction would require acceptance from the research community, he says, as well as “an acknowledgment that a different way to do research can be just as effective while also being more efficient.”
While AI has many positive usages within healthcare, the technology also introduces a suite of ethical challenges “that need to be solved if the application in healthcare will be fair and proper,” says Gallagher. Some of the popular commercial chatbots, including the recently released Google Gemini, have been found to have some built-in biases, according to Gallagher.
Compliance and clinical risks will need to be managed with human intervention and AI, according to Wurdeman. “For example, there are cases where AI may be able to determine a patient has a certain condition because of other active health conditions. However, it would be inappropriate for an AI model to present any new information that was not actually discussed by the patient and clinician.”


From a clinical perspective, AI users must recognize that the ability to provide clinical guidance is based on the quality of information used to build the underlying model, he says. “In other words, the more thorough and thoughtful information provided, the better the result.” Wurdeman says it’s important to recognize that AI models will be built based on data that trains the model; however, because much of that data stems from convenience samples, it may not represent certain populations. “If not used cautiously, it could possibly lead to greater disparities in certain areas.”
“Ethically, clinicians should spend effort getting a patient’s individuality into any AI model they use,” says McCoy. “AI can bring efficiency that frees clinical time, and using that time to improve the AI results—versus letting the AI work independently—will pay bigger efficiency dividends over time and reduce ethical issues.”
Gallagher points to four specific issues where healthcare professionals will need to be vigilant to ensure ethical use of AI-driven healthcare. First is “bias and fairness,” or the degree to which the data used to train AI systems is biased. “This is problematic in the healthcare sector, where bias in AI algorithms will result in different treatments and care,” he says.
Second, healthcare professionals should consider “transparency and accountability” when leveraging AI, Gallagher says. “It is important that AIs are made transparent regarding the decisions made so that they can be scrutinized and explained.”
Third, privacy and security are important considerations: “Healthcare providers should protect sensitive data from unauthorized access or breaches that would expose sensitive patient information,” Gallagher says.



or the active users with foot drop less support is needed during stance phase e flexibility – greater ROM


Artificial intelligence (AI) offers a “real solution” to the growing paperwork that clinicians must complete daily, with many apps and IT platforms available to assist in capturing patient histories, taking notes, completing documentation, and more. But the risks need to be considered when using these AI technologies, says Mary Mason, MD, MBA, founder of the Little Medical School and a speaker at the upcoming AOPA National Assembly in Charlotte, North Carolina.

Clinicians can choose from many AI options to reduce the administrative burdens related to patient interactions, says Mason, but “we must pause and consider the ramifications of introducing” information related to clinician/patient interactions into an AI engine, she says. “As patient data and details of a [clinical visit] are fed into an AI engine, the product is learning from this and remembers it.”
Mason says it’s important that patients are informed when their private healthcare information is fed into AI engines, and that O&P business owners and managers determine who has access to patients’ private data within AI applications. Clinicians
Finally, “informed consent” is a requirement: “Patients should be informed of how their data will be used in artificial systems, and consent should be obtained,” he says. (See the sidebar “Attend ‘AI in the Doctor’s Office’ at the Assembly.”)
Gallagher offers several strategies to implement “ethical AI” in healthcare. He suggests ensuring algorithms are trained on diverse and representative data sets to reduce bias. He also recommends that technologists, healthcare professionals, ethicists, and patients collaborate to build ethical AI solutions. In addition, “the ethical implications of AI systems must be continuously monitored and evaluated throughout their lifecycle,” he says. Plus, “including patients and the public in discussions on the ethical use of AI in healthcare is central to building trust and ensuring that AI solutions are tuned to societal values.”

should consider whether patients understand what they’re consenting to when agreeing to share data with AI applications.
“There’s so much excitement about AI—but there are also a lot of gaps,” Mason says. “Clinicians need to raise their hand and advocate for their patients.” Learn more during Mason’s presentation, “AI in the Doctor’s Office,” which will take place Saturday, Sept. 14, at 10:30 a.m.

The bottom line is that healthcare professionals should be aware of the risks inherent in AI usage and find ways to mitigate those risks.
Given all that AI can offer—and the precautions necessary to move forward in an ethical manner—“organizations and individuals need to decide if they’re going to lean into this, or resist,” says Lawry. “The competitive advantage for those who get in early is strong. It’s not a matter of whether AI is going to impact clinical practices—it’s a matter of how and when.”
Lawry encourages organizations to focus on “responsible AI principles” to ensure adequate oversight: “We need to look at which decisions that are being made should always have a human in that loop when making the final decision—for example, a decision around a diagnosis, or a treatment path,” he notes.
“Cautious excitement will allow clinicians to embrace opportunities to help their patients and themselves, while ensuring they don’t make mistakes that compromise their values or integrity,” says Wurdeman. “If clinicians remain diligent in their role of caring for patients, there is opportunity to use AI to enhance the human connection that is essential to O&P care.”
Christine Umbrell is a contributing writer to O&P Almanac Reach her at cumbrell@contentcommunicators.com



Turbomed’s premium foot drop or thosis sits on the outside of the shoe to facilitate maximized ankle movement while reducing the risk of injury .

PDAC validated (L1951)
Simplified assembly
18% more dorsi-flexion power
35% more media-lateral strength

Prepare now for this year’s “Ignite 24”-themed AOPA National Assembly by previewing the hot topics scheduled for the conference
Invest in your O&P professional development by exploring the expansive slate of top-tier O&P educational sessions featured at the AOPA National Assembly in Charlotte, North Carolina, Sept. 12-15. There’s something to spark everyone’s interest at this year’s Assembly—whether you’re an O&P clinician, business owner, manufacturer, student, educator, researcher, or advocate.
The National Assembly Planning Committee has been working at top speed to bring you an entertaining, enjoyable, and innovative experience that will broaden your knowledge and inform you of the latest trends and hot topics. By participating in the wide range of sessions offering more than 100 CE credits within Clinical Care, Digital Care, Business, Technical, and Pedorthic Education Tracks, you’ll hear key perspectives from top minds during unique panel sessions, access timely updates and tips on cutting-edge
technologies, improve your techniques to better serve patients, and boost your business practices.
Here’s a preview of some of the most highly anticipated educational sessions planned for the Assembly—be sure to consider these sessions when developing your personal conference schedule.
This year’s Clinical Track, featuring orthotic, prosthetic, and combined sessions, offers a wide variety of topics critical to optimal provision of O&P services. In addition to a one-day track devoted to the specialty of upper-limb prosthetics, which will take place beginning 8:30 a.m. Sept. 13, sessions will focus on topics ranging from new socket technologies to orthotic applications of exoskeletons to osseointegration, and much more.
“We have three talks in our track that relate directly to reimbursement change within our profession,” says Tyler Klenow, MBA, MSPO, CPO, LPO, chair of the Clinical Track programming for the Assembly Planning Committee.
“Powered Upper-Extremity Bracing,” at 10:30 a.m. Sept. 13, will provide an overview of the quickly advancing space of motorized braces for the upper extremity and will feature an expert-packed panel discussion—including Ghaith Androwis, PhD; Harry Kovelman, MD; Jonathan Naft, CPO; Jason George, PhD; and Ajay Seth— highlighting key topics related to recent changes to L codes, benefit categories, and reimbursement.
At the “Adjustable-Volume Sockets: Who, What, When, Why, and How To Get Paid” session at 3:45 p.m. Sept. 13 and led by Klenow; Joe Mahon, CP; Jimmy Capra; and Billy Lester, you’ll access information about the new L code for adjustable-volume sockets, proper patient indications, clinical applications, the reimbursement pathway, practice benefits, and more.
“MPK K2: Benefits and Reimbursement Update,” at 3:45 p.m. Sept. 14, will give an overview of the existing evidence that helped achieve the recent proposed changes in the Medicare Local Coverage Determination for coverage of microprocessor-controlled knees in the K2 population. Al Dobson, PhD; Andreas Hahn, PhD; Andreas Kannenberg, MD(GER), PhD; and Shane Wurdeman, PhD, CP, will lead the discussions.
AOPA National Assembly
accessibility, and delve into the innovative modular design of the Zeus myoelectric hand—removing the need for loaner hands and empowering individuals with limb differences.
“Revolutionizing Prosthetic Care: Smartphone Gait Data for Practical Evidence and Benchmarking” will follow Mullen’s presentation. Patrick Tarnowski, PT, MBA, will introduce attendees to a new generation of technologies that increase accessibility of gait analysis tools for O&P providers in their own clinics.
A combined Digital/Pedorthic Track session, “Foot Orthotics Using Digital Technology,” Sept. 13 at 3:45 p.m., will feature several presentations with dual purpose. Be sure to check out Amit Bhanti’s case study, “How CPO Has Implemented the Latest Advancements in Telehealth, Artificial Intelligence, Data Analytics, and 3D Printing,” where Bhanti will highlight his company’s partnership with Hike Medical and use of a telehealth platform to streamline evaluation, billing, fitting, and compliance.

Another important session, to be held at 11 a.m. Sept. 15, will focus on “Medical Necessity in Prosthetics and Orthotics: Moving From Device Deliverers to Healthcare Providers.” Here, you’ll experience short panel presentations from Molly McCoy, CPO; Jeffrey Heckman, DO; Kannenberg; and Dave McGill, JD. These experts will offer best practices on documenting “medical necessity” and discuss the shift from fee-for-service to value-based care and appropriate provision of healthcare.
Of course, you won’t want to miss the “best-of-show” Thranhardt lectures, set to start off the educational programming during the Sept. 14 General Session (see sidebar).
Access key information to keep abreast of digital trends, adopt new technologies, and become more efficient at O&P care by attending sessions in the Digital Track.
Headlining the digital-themed sessions is Joshua Steer, PhD, this year’s Hans Georg Näder Digital Education Award winner. His presentation, “Insights Into Transtibial Prosthetic Socket Design From Expert UK Clinicians’ Digital Records,” scheduled for Sept. 13 at 10:30 a.m., will introduce a method to compare rectifications made by experienced prosthetists across a range of patient demographics and limb shapes, to improve understanding of socket design strategies.
Immediately following Steer’s presentation is a session by Sarra Mullen, CP, “Digital Health: Remote Visits and Modular Design in a Myoelectric Hand.” Mullen will explore the cutting-edge advancements in digital health technology that are revolutionizing the field of prosthetics. Discover how remote visits enhance patient care and
Also of note is the combined Digital/ Technical/Clinical Track session, “Taking the Leap: Advancing O&P With Digital Tools, Digital Workflow, and 3D Printing,” presented by Brent Wright, CP, BOCO, and Jeffrey Denune, CP, LP, at 9:15 a.m. Sept. 15. This innovative presentation will be followed by the fan-favorite interactive “O&P Digital Care Showcase,” beginning at 11 a.m. During this hands-on event, participants will learn about computer-based 3D design software tools utilizing provided prosthetic, orthotic, and pedorthic patient cases—and exhibitors will present a fabricated mold, device, or 3D print. Watch, compare, and learn!
The AOPA National Assembly is renowned for its comprehensive and forward-focused business-themed educational sessions. This year, top O&P business experts will offer Hamontree presentations Sept. 14 at 2 p.m. The Sam E. Hamontree, CP(E), Business Education Award was created to recognize the best business education paper, idea, and/or proposal submitted for presentation. The audience will be invited to cast their vote for the 2024 Hamontree Award winner via the Assembly App. Four presentations will compete for the Hamontree Award. Ernst Bastian, CO, will present “Can a Small Fish Make a Splash in a Big Pond?” where he will share the advantages of working in a small company and offer strategies for building and maintaining positive relationships. Ashlie White, MSHLS, MA, will share highlights from the Amputee Coalition’s newly released study of amputation statistical trends in the session, “Prevalence of Limb Loss and Limb Difference in the United States: Implications for Public Policy.” David Holzman, CFA, will delve into trends in the O&P mergers and acquisitions (M&A) space in “How Merger and Acquisitions Are Changing the O&P Landscape and What Independents Should Consider When Developing a Transition Plan.” Finally, Mike Schlesinger will offer tips for successful transactions in “Beyond the Sales Price—Top 10 Key Steps for Owners To Understand and Consider for an Efficient and Successful Transaction.”

Always a highlight of the Assembly, the award-winning Thranhardt presentations recognize individuals committed to advancing O&P education and research, and memorialize Howard R. Thranhardt, CPO.
This year, the Thranhardt sessions will be featured during the General Session beginning at 8 a.m. on Sept. 14. Plan to be in attendance for these highly regarded presentations:
• “Assessing Outcomes With Microprocessor Knee Utilization in a K2 Population (ASCENT K2): Findings From a Clinical
Beyond the Hamontree presentations, several additional business-themed sessions will offer knowledge of business best practices and efficiency tips. Don’t miss a special presentation from Dale Berry, CP, LP, FAAOP; Kimberly Hanson; and Mitchell Dobson, CPO, FAAOP, titled, “ALJ Law Judge Trial—Simulation Proceedings,” Sept. 14 at 10:30 a.m. This one-of-a-kind session will provide a simulation of an ALJ trial and identify key elements of the process and procedure—from the viewpoints of the plaintiff (prosthetic provider), defendant (Medicare), and adjudication law judge. Presenters will explain the most common prior errors, omissions, and misconceptions of the ALJ to provide real-life examples of effective trial procedures.
The Technical Track offers an interesting array of choices—you’ll want to attend several of these sessions to enhance your technical fabrication skills and acquaint yourself with some of the latest O&P products.
In the session titled “Optimization of User-Adjustable Lower-Extremity Prosthetic Designs,” presented Sept. 13 at 10:30 a.m., Mike Marten, RTP, will share fabrication techniques to fine-tune different lower-extremity prosthetic designs.
Gary Bedard, CO, will speak on “Maximizing the Tuning of AnkleFoot Orthoses With the Material Science of Custom Fabrication,” Friday, Sept. 13, at 2 p.m. Bedard will explain how recent advances in material science illustrate a means to optimize thermoplastic fabrication for a best practice approach.
In a combined Technical/Pedorthic Track session, Dennis Janisse, CPed, will present “Hands-On, Total-Contact Foot Orthosis Materials/Fabrication” Sept. 14 at 10:30 a.m. Designed specifically for pedorthists and technicians, this session will demonstrate fabrication techniques and material selection when fabricating a total-contact foot orthosis.
Trial of 107 Individuals With Above-Knee Amputation,” presented by Shane Wurdeman, PhD, CP, and Andreas Kannenberg, MD(GER)
• “Reduction in Falls and Fall-Risk With Increased Walking Speed Found Following One Year of C-Brace Use: Interim Results From the C-Brace Registry,” presented by Tyler Klenow, MBA, MSPO, CPO, LPO, and Russell Lindstrom, MS.
The 2024 pedorthic-focused education promises to equip attendees with the knowledge they need now to manage and treat conditions of the foot, ankle, and lower extremities.
Among the many highlights, Brian Lane, CPed, will discuss “Filling the Pedorthic Prescription: How To Decide What Orthosis To Use” Sept. 13 at 2 p.m. Lane will explain the many factors to be considered—patient condition, insurance and reimbursement, vague prescriptions, and more—and share challenges and best practices.
Dennis Janisse, CPed, will lead a discussion of subtalar-control foot orthoses (SCFOs) during “Options When You Need More Control SCFOs” Sept. 14 at 3:45 p.m. Janisse will explore the function of the SCFO as well as the many different types and design variations available.
Erick Janisse, CO, CPed, will speak on “Functional Orthoses Vs. Total Contact” Sept. 13 at 2:45 p.m. He will compare and contrast the design features of functional and total-contact orthoses, including a discussion of which designs are better suited for certain pathologies. He also will lead the session “Foot Orthotic Management of the Diabetic Foot” Sept. 14 at 2:45 p.m. This session will examine several different designs, materials, and orthosis modifications that may be effectively utilized to prevent or minimize diabetic foot complications, and will delve into the interaction and interface between orthoses, footwear, and hosiery.
During the session “12 Tips To Successfully Dispense Foot Orthotics,” Sept. 14 at 2 p.m., Seamus Kennedy, BEng (Mech), CPed, FAAOP, will offer suggestions to make the process of providing foot orthoses easier, smoother, and more efficient.
The 2024 Assembly will offer all of the topics outlined above— and so much more. Visit AOPA’s Assembly website to access the Assembly Preliminary Program and view all of the sessions planned for Charlotte—and to view details about hotels, registration, exhibitors, and much more.
Increase suction suspension even more with the new air expulsion valve release button for all Coyote Air-Locks.

Air expulsion built into the release button.
Quiet expulsion.
Increases negative pressure in the socket.

All Air-Locks can be easily retrofit.
Sold Separately


The Transformations column features the success story of an O&P clinician who has worked with an inspiring or challenging patient. This month, we speak with Jonathan D. Day, PhD, CPO, clinical associate professor at the College of Medicine at the University of Oklahoma Health Sciences and prosthetist to para-triathlete Danielle Cummings.
Six months ago, Danielle Cummings became the first person in New Mexico to receive an activity-specific prosthesis covered by insurance—just a few days after the state’s So Every BODY Can Move (SEBCM) legislation went into effect requiring that state commercial plans and state employee plans cover such devices.
A second-year medical student at the University of New Mexico School of Medicine, Cummings was glad to be fit with a running leg that would enable her to compete in triathlons. Her journey to that moment—and to pain-free mobility—was a long one, facilitated in part by her prosthetist, Jonathan D. Day, PhD, CPO.
Seven years ago, Cummings, who has always been active, suffered a bad fall while rock-climbing. “I essentially shattered the talus bone in my ankle,” she
recalls. Despite the severity of the injury, her surgeons and physicians did not recommend amputation; instead, she endured multiple surgeries, tested several orthoses, and tolerated lots of steroid injections over the six years following the accident. “The chronic pain was horrendous and only worsened with each new surgery or orthosis.”
Cummings committed to physical activity despite the pain, swimming and biking to stay in shape. She also tried running a few times, facilitated by a specialized brace, with limited results. Along the way, she joined in the SEBCM initiative in New Mexico, helping advocate for coverage of activity-specific devices for individuals with limb loss and difference as an orthosis user.
Last year, as Cummings completed her first year of medical school, the pain became unbearable. “I was unable to sleep, and I could barely eat because the pain was
so bad,” she notes. She met with several surgeons to discuss possibilities but learned she was not a great candidate for fusion or ankle replacement due to her young age and desire to live a very active life, so options were limited.
“My treating physician was a podiatrist, and he did not do amputations, so I started meeting with other physicians,” Cummings says. Because she was already involved in New Mexico’s SEBCM movement, she met several prosthesis users who shared stories of amputation giving them their lives back. “I spoke with many people who had similar injuries to mine who had chosen amputation and were now pain-free and back to being active,” Cummings recalls. “I saw the life they were getting to live—and that is what I craved for myself.”

She decided to explore whether amputation was a possibility. After several physicians in New Mexico warned her that amputation surgery would “ruin my life,” Cummings was introduced to a physician who had undergone an Ertl procedure—now known as an osteomyoplastic transtibial amputation—20 years prior. The procedure can be used to create a highly functional residual limb via creation of a tibiofibular bone bridge, which provides a stable, broad tibiofibular synostosis capable of distal weight bearing.
Cummings was connected with William Ertl, MD, an orthopedic surgeon at the University of Oklahoma Medical Center and grandson of Janos Ertl, MD, who developed the Ertl procedure in 1920. After speaking virtually with William Ertl and Day—a prosthetist and clinical associate professor at the College of Medicine at the University of Oklahoma Health Sciences (OUHSC)— Cummings felt optimistic that amputation could alleviate her pain and confident that she would adjust to life with a prosthesis. She decided to travel to Oklahoma for the procedure.
Despite a packed medical school schedule, Cummings was given approval to take six weeks off to undergo osteomyoplastic transtibial amputation surgery on July 7, 2023. In conjunction with the procedure, Ertl performed a targeted muscle reinnervation (TMR) behind Cummings’ knee—a nerve transfer for neuroma prevention, which has been found to reduce pain in some patients. Day was well-prepared to fit Cummings with a prosthesis postamputation as he frequently collaborates with Ertl. Day, who has been faculty at the OUHSC College of Medicine since 2000, completed a doctorate degree in rehabilitation science at OUHSC last year. His research focuses on postamputation healing and readiness for prosthetic treatment. Day currently treats both orthotic and prosthetic patients, but his “specialty” is prosthetics, and his practice merged with Ertl’s orthopedic practice about 20 years ago. “We’ve had a blended practice, where we see patients together,” Day explains.
Day worked closely with Cummings and Ertl to ensure a smooth transition to prosthesis use. “We started care preoperatively, then postoperatively we were in conversation regarding goals for prosthetic use and function, and insurance authorization prior to release,” he recalls.
Cummings returned to class Aug. 21 on crutches without a prosthesis and received her initial prosthesis shortly thereafter—a low-profile Torsion Ossur foot, as well as a patient-adjustable heel-height foot. “I juggled the medical school load, research projects, multiple physical therapy appointments, and traveling back and forth to Oklahoma about once a month from August through December,” Cummings recalls—all while excelling academically.
Day, for his part, worked many hours to ensure Cummings’ treatment was comprehensive and appropriate—often spending concentrated time during week-long visits. “Because Danielle lives in New Mexico, she would fly in on Sunday, and we would spend a week together” fitting her prosthesis. “She was blocked for several hours of my schedule those weeks, spending one to three hours each day” to ensure the most appropriate fit.
Once she began walking with her prosthesis, Cummings knew that amputation had been the right decision: “I truly feel like it saved my life, and now I have my life back.” She finally felt free from the excruciating pain—and the mental weight of worrying how much pain each step would bring. “All of my pain is gone, and I feel like I have my brain back,” she says. “The mental clarity in studying has been a game-changer.”
She was able to use her everyday prosthesis to continue being active— and even to ski. She enjoyed biking and swimming, but she also sought access to an activity-specific prosthesis, which would allow her to run and participate in triathlons. Six months postamputation, she had atrophied and matured to the point

where she needed another socket on her daily use prosthesis—and she was also cleared by Ertl to run. “That’s when we submitted paperwork for her running leg,” recalls Day.
Cummings, who played an instrumental role as a consumer-advocate in pushing for New Mexico’s SEBCM legislation, was thrilled to become the first recipient of an activity-specific prosthesis under the recently enacted law. Her insurance company agreed to cover the device in January after receiving a four-page letter of medical necessity written collaboratively by Day and Ertl. “We explained that we were requesting coverage of a running leg, and that the patient would be running three to five times a week, with a goal of running triathlons,” Day says. They also noted they could provide a history of Cummings’ past activities and explained that using the running leg would save wear-and-tear on her everyday prosthesis.
After receiving approval and being fit with the running prosthesis, “it took a month of figuring the prosthesis out” to optimize it for Cummings to use, explains Day. Because the proximal socket was loose, padding was added to tighten the proximal posterior. He used silicone tape to reduce the rotational instability.
By April, Cummings was competitionready: She competed against able-bodied athletes in her first triathlon, using her activity-specific prosthesis during the run, a cycling-specific device on the bike,

and no prosthesis on the swim. She took fourth place in her age group, and 21st out of 130 women. She easily qualified for an upcoming national Paratriathlon event, finishing 22 minutes under the qualifying time.

She recently began training with USA Paratriathlon and is running approximately 15 to 20 miles each week, on top of swimming and biking. She’ll race in the national Paratriathlon event this summer.
Two months ago, Cummings completed her second year of medical school with Phase 1 Honors. She is giving back to her community by assisting in important research studies. “I have been a part of multiple research projects on chronic pain and opioid use and traumatic orthopedic fractures,” she says. She also volunteers at two free healthcare clinics for uninsured or homeless populations: One Hope and Albuquerque Opportunity Center Clinic.
As they look to the future, both Cummings and Day will continue to advocate for greater access to appropriate O&P care. Cummings shared her own experiences during the 2024 AOPA Policy Forum in April, speaking to attendees about her journey to becoming an individual living with limb loss, her work with SEBCM, and her experience being the first person in New Mexico to get an activity-specific prosthesis with insurance. “I discussed how important movement
is for medicine, and for physical and mental health,” she says.
A future physician herself, Cummings is “leaning into” emergency medicine as a potential career choice. “I love to be active and on my feet, and I want a career that will challenge me mentally,” she says. “I thrive in fast-paced environments where I have to think quickly as well as collaborate with multiple people,” she says. “I also love that I get to be a source of encouragement for patients that come in with severe traumatic injuries” and potentially give hope to injured patients, to “show people that you can still succeed and pursue what you love.
“My injury taught me how much patients crave authenticity and empathy that can really only be given when someone has also been through a challenging time with their health,” Cummings adds. “My injury has given me a great ability to better connect with patients, and I am forever grateful for that.”
As a prosthetist, Day hopes to abolish “this concept that is still pervasive among some surgeons, that amputation is failure, that amputation isn’t a path to an outcome that is quality-of-life driven,” he says.
“Amputation in many cases allows patients to stop taking pain meds and to stop having to deal with pervasive pain,” Day adds. “Danielle is a perfect example of the opposite—we have made her quality of life so much better” with a prosthesis. “Now, she can do whatever she wants.”

FACILITY:
Miller Prosthetics and Orthotics


PT,
“We strive to run a strong and efficient business, and the business-oriented tracks at the AOPA National Assembly are extremely helpful. The annual survey helps us compare industry statistics with our own business to focus on areas to improve. And we’ve learned a lot from the Policy Forum about how to discuss issues with our delegates and senators. It’s also a great opportunity for high-level networking.”
—Mark Miller, CPO
OWNER:
Mark Miller, CPO, and Nancy Miller
LOCATION: Belpre, Ohio, and Parkersburg, West Virginia
After 24 years in O&P, Mark Miller, CPO, launched his own facility with his wife, Nancy Miller, in 2012. The couple started with one office in Parkersburg, West Virginia, and opened a second office in Belpre, Ohio, in 2015, just a few miles across the bridge spanning the Ohio River. In 2017, they built a new, and primary, facility in Belpre.
Miller Prosthetics and Orthotics has two certified prosthetist/orthotists and one certified orthotist among its 10 employees, and the facility serves patients of all ages. Nancy Miller oversees the business end of the company, while Mark Miller focuses on serving patients.
Miller P&O embraces advanced technologies—for example, using Össur direct technology for transtibial sockets, which allows clinicians to fabricate the socket directly on the residual limb. “We do a lot of 3D scanning and printing. I rarely touch plaster anymore, and we operate a paperless office,” says Mark Miller. “The technology allows us to get people turned around pretty quickly.” He may scan a patient on a Tuesday, create a 3D-printed socket overnight, fit them with a diagnostic device on Wednesday, print a second diagnostic device and fit them Thursday, and have the definitive socket ready by Saturday.
The Millers relocated their Parkersburg office in 2021. The new building encompasses far more space than they needed, so they built their office in the front and turned the back into a large, open gym. They founded a 501(c)(3) nonprofit called the Amputee Center, where individuals with limb loss can meet for peer support, exercise, and socializing. The space is stocked with Amputee Coalition materials and other printed resources. Visitors have free access to fitness classes and programs at the center—whether or not they are Miller P&O patients.
The center’s showpiece is an aerial gym featuring a variety of harness equipment. “One therapist had the idea to bring in bungee fitness. She thought it would be good for amputees to be hooked to the ceiling so they wouldn’t worry about falling,” says Miller. “It’s more than a harness; it lets patients move and bend their knees. Some just use a handle to help them maintain their balance.”
HISTORY: 12 years

The center also offers fitness classes to everyone in the community at nominal fees, with offerings of tai chi; aerial, chair, and regular yoga; ballroom dancing; and bungee fitness.
Every Thursday afternoon, the center hosts open hours, where at least one individual with limb loss is available as a resource. “Some folks are facing amputation and want to talk with someone who’s been through it; others may have different kinds of questions,” Miller says.
The center holds a mixer once a month and bestows a gold medal on one of the participants for achieving their goal that period. “We got the idea at the Rio Paralympics,” says Miller. “The goal can be as simple as walking on a walker, or mowing the lawn, or completing a hike—it’s up to the person.”
Support for the center comes from a combination of grants, sponsorships, and fundraising. Each year it holds the Amputee Fun Fest as its major fundraiser, which features a stage, live music, food trucks, and vendors.
One of Miller’s favorite patient success stories is that of a woman with bilateral above-knee amputations. “She had experienced limited success with stubbies. We fit her with new sockets and Ottobock knees that lock when she stands up and unlock to allow her to sit at a controlled rate with hydraulics,” he says. “She has been doing really well, and she feels like a big factor has been the support she’s received at the Amputee Center. She had been relying on people to give her rides, but she just got her license and drives herself with hand controls.”
For many years, Miller P&O had a mascot, a congenital three-legged dog, whom Miller fit with a prosthetic leg and later became a certified therapy dog. “Keating traveled everywhere with us,” recalls Miller. “He wore a pirate costume, and we put his image on T-shirts. When people saw the pirate dog, they thought of us. Sadly, he is no longer with us, but patients still remember him fondly.”
Deborah Conn is a contributing writer to O&P Almanac. Reach her at deborahconn@verizon.net





































































































































Dralle Advisors assists clients offering the Pro Armour Plus prosthetic cover (on the foot) and the Ethnocare Overlay.
“As a past president of AOPA, I fully believe in its vision, and I couldn’t be more excited about the success of the So Every BODY Can Move advocacy initiative it founded. To witness the incredible impact, community, and education it has created across the country has been thrilling.”
—Traci Dralle, CFm
BY DEBORAH CONN
Traci Dralle, CFm
DLOCATION: Chattanooga, Tennessee
HISTORY: 10 months
ralle Advisors may be a newcomer in the orthotics and prosthetics arena, but its founder, Traci Dralle, CFm, brings a wealth of experience to her new role. Dralle served as president of Fillauer Cos. for 10 years, and before that spent nine years at Trulife as vice president of sales and marketing. She was on the AOPA Board of Directors for six years, serving as president in 2021.
“While I was at Fillauer, I kept getting asked for guidance from other manufacturers, startups, and newcomers to the U.S. market, and I decided I wanted to do something different—something that would make the greatest impact on patients,” she says. She left Fillauer in July 2023 to start her own consulting firm, “where I can offer my knowledge, expertise, and guidance to multiple organizations to make sure that patients have access to high-quality O&P products.” She launched Dralle Advisors Sept. 1, and introduced the company at the AOPA National Assembly in Indianapolis.
Dralle works primarily with O&P manufacturers, basing her work on three pillars: helping companies simplify, optimize, and grow. “Right now, most of my clients are startups in the O&P space. One of the most important things I do is try to simplify the process of going to market. It’s so easy to complicate anything— even with just one product,” she says. “I focus on the who, what, why, when, where questions. I help manufacturers clarify their goals: Are they revenue based? Focused on product development? And then I help them figure out the best way to get their product to market.”
Dralle has one hard-and-fast rule: “I have to believe in the product. It has to provide good value and quality, and there has to be a need for it.”
One of Dralle’s clients is Ethnocare, a company based in Montreal that developed the Overlay, a retrofit solution that transforms traditional sockets into adjustable ones. The Overlay is made of a breathable fabric and features an adjustable air expansion system, fitting over the liner and into the socket. “I’m helping with their sales and marketing strategy, primarily internationally, but in the U.S. as well,” Dralle
says. “Lots of startups rely on distributors to get their products to market, but you have to know the right distributors. It’s important that the distributor is a partner with your company—it’s a two-way street, give and take. Anyone can say, ‘We’re the biggest in this country,’ but nobody knows. When I can set a company up with the right partners from the start, patients will have immediate access to its products, benefiting the company, clinicians, and patients alike.”
The focus on digitalization in the O&P industry and advances in scanning and 3D printing will only grow in the coming years, predicts Dralle. “I think what I do will stay important even as that takes over—companies will still have the same goals and same mission, but manufacturing will occur in a new way,” she says. She plans to work with startups as well as existing companies that are making investments in these types of changes. “Companies that have been in business for a long time are looking at how they manufacture or develop products, how they get to market—for example, clinics may buy a license to print their own products,” she says.
“This also has implications for including small countries without access to technology. If you drop off an electric or even solar-powered 3D printer in a developing country, they will be able to print a foot, socket, and components right there, allowing someone to go back to work. The opportunities are exciting!”
Dralle considers her company to be in “phase 1,” which she plans to continue for the rest of 2024. She has a phase 2 plan to expand the business beyond advising business owners and executives. “I want to also be able to support and encourage leaders and future leaders at all levels,” she says. “Many great ideas do not start at the top. They just end up there for approval.”
The journey so far has been rewarding. “I really enjoy the people I’m working with, and I love that they get to shine,” she says. “Their success is my success, and that brings me joy.”
Deborah Conn is a contributing writer to O&P Almanac. Reach her at deborahconn@verizon.net
Are you ready to take your career and your business expertise to new heights?
The Certificate in O&P Business Management can help you do just that!
















This joint certificate program will provide you with:
• Basic business acumen
• Practical knowledge to apply immediately to your work
• Techniques for developing better business practices
• How to think about improving your company’s returns
A comprehensive certificate program for business owners, managers, and practitioners of O&P patient care facilities, O&P manufacturers and distributors to explore crucial business challenges as they relate to O&P.
To complete the certificate program, you must register and complete one core course and one elective course from each of the four areas of learning within a four-year period


Certificate in O&P Business Management

Take part in the virtual event Aug. 19-20
Sign up for the next AOPA Virtual Coding & Billing Seminar, slated for Aug. 19-20. You’ll learn how to get claims paid, survive audits, collect interest from Medicare, and file successful appeals. Earn CEs!
Visit AOPAversity online at bitly.aopaversity for details and to register. For questions regarding seminar content, email Devon Bernard at dbernard@aopanet.org
AOPA will offer six webinars throughout 2024—in February, April, June (postponed), August, October, and December. Webinars are $99 for members and $199 for nonmembers. All webinars are live, but everyone who registers will receive access to the recordings. Earn 1.25 CE credits by attending or listening to the recording and returning the provided quiz within 30 days and scoring at least 80%.
Topics from the first three webinars include the following:
• February: “Changes & Updates to Medicare Policies: Do You Still Know the Rules?”
• April: “The Three ‘C’s of O&P”
SEPTEMBER 12-15, 2024 | CHARLOTTE, NC
The 2024 AOPA National Assembly, with a theme of “Ignite 24,” takes place Sept. 12-15 in Charlotte, North Carolina. Plan now to attend this year’s Assembly. Why attend?
• Earn continuing education credits
• Hear from physicians, researchers, and top-notch practitioners
• Participate in hands-on learning and demonstrations
• Network with an elite and influential group of professionals
• Explore the largest O&P exhibit hall in the western hemisphere, featuring devices, products, services, tools, and the latest technology from exhibitors around the world.
Registration is now open! Register and learn more at AOPAAssembly.org
FUN FACT
Charlotte boasts a growing film industry and has become a sought-after filming location. “The Hunger Games,” “Homeland,” “Days of Thunder,” “Sully,” and “Talladega Nights” were all filmed in part in Charlotte.

• June: “Regulatory Hot Topic: Requirements When Treating Patients With Limited English Proficiency”
To purchase the February, April, or June webinar or register for future sessions, access your AOPA Connection account or visit aopanet.org. Questions? Contact Devon Bernard at dbernard@aopanet.org
So Every BODY Can Move (SEBCM) is at the forefront of the national disability rights movement, focusing on creating equitable and life-changing access to prosthetic and orthotic care for physical activity in 28 states by the 2028 Paralympic Games.

SEBCM, developed through a partnership between AOPA, the National Association for the Advancement of Orthotics and Prosthetics, the American Academy of Orthotists and Prosthetists, and the Amputee Coalition, advocates for a policy solution rooted in dignity and justice by empowering state-by-state legislative action, expanding access to medically necessary orthotic and prosthetic care for physical activity.
For more information and to get involved, log on to soeverybodycanmove.org, a dynamic platform featuring a user-friendly interface, engaging content, an interactive state map, and much more.
The officers and directors of the American Orthotic & Prosthetic Association (AOPA) are pleased to present these applicants for membership. Each company will become an official member of AOPA if, within 30 days of publication, no objections are made regarding the company’s ability to meet the qualifications and requirements of membership.
Agility Prosthetics & Orthotics
347 W. O’Brien Drive, Ste. 1 Hagatna, Guam 96910 671-682-0140
agilitygu.com
Dianna M. Le, CPO International Member
Alt-Bionics
14838 Vance Jackson Blvd., Ste. 532
San Antonio, TX 70433 210-854-6392 altbionics.com
Ryan Saavedra Supplier Startup
Orthotic & Prosthetic Specialists Inc.
101 Highland Park Place Covington, LA 90433 985-898-6319 orthprosla.com
Michael Relle, CPO, FAAOP Patient-Care Facility

Orthotic & Prosthetic Specialists Inc.
1241 Coursey Blvd., Ste. C Baton Rouge, LA 70816 225-333-1893
Michael Relle, CPO, FAAOP Patient-Care Facility—Affiliate
Radii Devices Ltd. Engine Shed Station Approach BST, United Kingdom BS1 6QH 795-678-7704 radiidevices.com
Joshua Steer, PhD Supplier Startup
Vessl Prosthetics
99 Bowman Drive
Ilderton, ON Canada N0N 2A0 519-476-6410
vesslpro.com
Sydney Robinson, MSc Supplier Startup


Ypsilon® FLOW ½ & ToeOFF® FLOW 2 ½
FLOW AFOs are Allard’s newest generation of AFOs fabricated with a new proprietary formula that offers increased ROM in the sagittal plane and smoother transition (flow) throughout the gait cycle. The footplate is shaped to allow more clearance for the forefoot in the shoe toe box. Plus, both Ypsilon® FLOW ½ and ToeOFF® FLOW 2 ½ are designed to accommodate lower shoe heel heights, fitting more shoe styles. For more information call 888-678-6548 or email info@allardusa.com. Request your free magnetic level!

Embrace the comfort of custom-fit with Mt Emey®’s Custom Shoe (Medical) Program. Our precise 3D scanning captures your unique foot contours, promising a perfect fit without the wait or waste. From stylish athletics to roomy comfort designs, our handcrafted shoes adapt to your needs. Satisfaction guaranteed before payment. Plus, qualified wholesale accounts receive a free 3D scanner. Step into the Mt Emey difference— where every shoe is made for you.


With a focus on low-impact K2 users, College Park combines some of its most popular and trusted technology in the new Terrain iW. This lightweight foot offers triaxial movement on an Intelliweave® composite base. Featuring anatomical ankle motion, flexible springs, and a durable heel wedge, the Terrain iW was designed for ultimate comfort and stability.
To learn more or request a demo, please visit college-park.com/ terrain-iw


Coyote’s Dynamic Strut was designed with varying thicknesses to flex and move, helping the patient navigate real-world conditions. The strut excels at creating a comfortable natural gait for daily use, walking, working, hiking, biking, and golf. It works great with a thermoformed orthosis and provides the needed energy response.
• Comfortable natural gait
• Works great with thermoformed braces
• Provides energy response
For more information, call 1-888-937-2747 or visit emeys.com
• New smaller size available. Contact Coyote at 208-429-0026 or visit www.coyote.us


Minimizing the effects of micro tears and/or injury to the incision bed rest holds a high priority. FLO-TECH® designed the and SOFTIE-TF to aid against distal end breakdown, access for wound care, and daily hygiene. We incorporated struts to maximize extension control. Our SOFTIES healing and increase the quality of rehabilitation for surgical amputees. The sockets are soft, non-constricting to remove for examinations. Having an inventory of and SOFTIE-TF ™ sockets allows you to fit any patient at a ’s notice. They easily fit most sizes including XL.
Minimizing the effects of micro tears and/or injury to the inclusion area at the bed rest holds a high priority.
FLO-TECH® designed the SOFTIE™ and SOFTIE-TF™ to aid against distal end breakdown, easy access for wound care, and daily hygiene. We incorporated posterior struts to maximize extension control.

Our SOFTIES assist healing and increase the quality of rehabilitation for postsurgical amputees. The sockets are soft, nonconstricting, and easy to remove for examinations. Having an inventory of SOFTIE™ and SOFTIE-TF™ sockets allows you to fit any patient at a moment’s notice. They easily fit most sizes, including XL. Visit 1800flo-tech.com

Hersco is delighted to offer HP’s advanced 3D-printing technology for custom orthotics. 3D printing has unique design capabilities not possible with other methods—reducing landfill waste by 90%! The accuracy of 3D is unparalleled, specs exceed direct-milled polypro, and manual plaster fabrication. Among the benefits: a 90% reduction in landfill waste, many new design possibilities for posting, and the ability to vary thickness and flexibility across the shell. The PA-11 polymer is a biobased renewable material that has been tested and proven in research and industry. Call today, 800-301-8275, for a free sample.



Engineered to exceed expectations, giving you more of what you need to live the life you want. PROTEOR QUATTRO™ MPK is designed to be MORE INTUITIVE for elevated security and dependability with patented valve technology for effortless transitions between activities, hyperresponsive sensors read body movements, and exclusive stumble recovery determines appropriate resistance to recover more naturally. MORE PERSONALIZED with up to 20 customizable modes and the shortest MPK available; allows a wider selection of ankles/feet. MORE ADAPTABLE for fewer interruptions with a 2-3+ day battery life PLUS Battery Booster allows charging ON THE GO. Visit shop.proteorusa.com

Turbomed’s leading line of foot drop ankle-foot orthoses sit completely outside the shoe for an invisible, painless support that will follow you as long and as far as you want. Their unique design acts as an exoskeleton to the impaired limb, keeps the foot at 90 degrees, and provides the user with unparalleled levels of function. Each model takes minutes to assemble and is easily transferrable to most shoes, boots, and sandals through an innovative lace clip design.
The Xtern Summit is the lightest model, has the most dorsiflexion power, and features a see-through design. The Xtern Frontier was designed for patients with reduced hand dexterity and requiring front leg support. Visit turbomedusa.com, and think outside the shoe!
A large number of O&P Almanac readers view the digital issue— If you’re missing out, visit issuu.com/americanoandp to view your trusted source of everything O&P.
Scan the QR to start advertising in the O&P Almanac or visit bit.ly/24AlmanacMediaKit

Allard USA 23 866-678-6548 www.allardusa.com ALPS South LLC 1 800-574-5426 www.easyliner.com
Apis Footwear Co. 11 888-937-2747 www.apisfootwear.com
College Park Industries 5 800-728-7950 www.college-park.com
ComfortFit Orthotic Labs 33 888-523-1600 www.comfortfitlabs.com
Coyote Prosthetics & Orthotics 29 800-819-5980 www.coyote.us
Fabtech Systems 21 800-322-8324 www.fabtechsystems.com
Ferrier Coupler Inc. 39 810-688-4292 www.ferrier.coupler.com
Flo-Tech O&P Systems Inc. 3 800-356-8324 www.1800flo-tech.com Hersco 19 800-301-8275 www.hersco.com Naked Prosthetics 15 888-977-6693 www.npdevices.com Ottobock C4 800-328-4058 www.professionals.ottobockus.com Procomp 13 www.fabwithprocomp.com
PROTEOR USA 9 855-450-7300 www.proteorusa.com
TurboMed Orthotics 25 888-778-8726 www.turbomedorthotics.com
Contact Bob Heiman at bob.rhmedia@comcast.net

June 28–29
PrimeFare East. Sheraton Grand Hotel Downtown Nashville. In-person meeting. For information, contact Cathie Pruitt at 901-359-3936, primecarepruitt@ gmail.com, or visit primecareop.com
June 30
Application Deadline for AOPA 2025 Call for Volunteers. Visit aopanet.org/volunteer or contact info@aopanetorg
July 1–31
ABC: Application Deadlines, Exams Dates, O&P Conferences, and More! Check out ABC’s Calendar of Events at ABCop.org/calendar for the latest dates and event details, so you can plan ahead and be in the know. Questions? Contact us at info@abcop.org; ABCop.org/contact-us
August 19–20
AOPA Virtual Coding & Billing Seminar. To register, visit aopanet.org

September 12–15
AOPA National Assembly. Charlotte, NC. For more information, visit aopanet.org

October 18–19
PrimeFare Central. Renaissance Hotel and Convention Center, Tulsa OK. In-Person Meeting. Contact Cathie Pruitt at 901-359-3936, primecarepruitt@gmail.com, or visit primecareop.com
November 18-19
AOPA In-Person Coding & Billing Seminar. Alexandria, VA. To register, visit aopanet.org


The Pedorthic Footcare Association: Diabetic Wound Prevention, Management, and Healing Program. 10-session online education program series. Approved CEs by ABC and BOC, monthly classes are 1.5 hours each. For more information and to register, visit pedorthics.org/page/.Diabetic_ Series_LMS_List

Advertise O&P events for maximum exposure with O&P Almanac Contact Bob Heiman at bob.rhmedia@comcast.net or learn more at bit.ly/24AlmanacMediaKit. Announcement and payment may also be sent to O&P Almanac, Calendar, P.O. Box 34711, Alexandria, VA 22334-0711 or emailed to jburwell@AOPAnet.org along with VISA or MasterCard number, cardholder name, and expiration date. Make checks payable in U.S. currency to AOPA. Note: AOPA reserves the right to edit calendar listings for space and style considerations.
If you are interested
Through efforts by Jim Kaiser, CP, LP, and the Illinois Society of Orthotists and Prosthetists (ISOP), Illinois Medicaid will implement a 7% increase in Medicaid O&P reimbursement rates in 2025, accomplished via inclusion in a larger omnibus bill, Senate Bill (SB) 3268, that was enacted into law June 7. ISOP is seeking to implement a 21% total rate increase through staggered 7% increases in 2025, 2026, and 2027 and plans to work with the Illinois Healthcare and Family Services Department and the Illinois General Assembly to accomplish this goal.
SB 455, legislation introduced by Sen. Sue Prentiss that would require New Hampshire Medicaid to reimburse for O&P services at 90% of Medicare, has passed the New Hampshire House Health, Human Services, and Elderly Affairs and Finance committees after an amendment was added that would set that 90% reimbursement rate to the 2024, rather than the prevailing, Medicare rate. Next up will be a House floor vote, which may be followed by a signature from Gov. Chris Sununu.
SB 3468 and Assembly Bill 3408, bills that would require that Medicaid managed care organizations reimburse for O&P at no less than 100% of Medicaid fee-for-service rates, passed an Assembly floor vote and committees in both legislative chambers. Unfortunately, the bill was unable to be considered for a Senate floor vote before the end of the session. Advocates in the state, led by Matthew Johnson, MPT, CEAA, are currently pushing legislators to convene a special session to provide additional time to consider the bill.
With the help of SEBCM lead advocate Sheryl Sachs, MSPO, CPO, Maryland’s So Every BODY Can Move Act, Senate Bill (SB) 614/House Bill (HB) 865, which would ensure coverage of activity-specific prostheses by state-regulated commercial plans and Maryland Medicaid, has officially been signed into law by Gov. Wes Moore. Maryland is the sixth state to enact activity-specific O&P legislation. The law will officially take effect in January 2025.
Massachusetts House Bill 4096, legislation requiring that state commercial plans, public employee plans, and Massachusetts Medicaid provide coverage for activity-specific O&P, has successfully passed through the Joint Healthcare Financing Committee. Supported by SEBCM lead advocate Maggie Baumer, JD, the bill now heads to the House Ways and Means Committee.
The omnibus spending package containing Minnesota’s SEBCM bill was officially passed by both chambers, and the bill was signed into law by Gov. Tim Walz, making Minnesota the seventh state to enact activity-specific O&P legislation. The bill, supported by Teri Kuffel, JD, and the Minnesota Society of Orthotists, Prosthetists, & Pedorthists, implements insurance fairness at Medicare coverage levels, covers
activity-specific and showering/bathing O&P, and ensures nondiscrimination standards in O&P care—all for both state-regulated commercial plans and Minnesota Medicaid.
SB 177, a bill introduced by Sen. Sue Prentiss that would ensure activityspecific prosthetic coverage in state commercial plans for patients under 19 years of age, has passed through the New Hampshire legislature and will now head to Gov. Chris Sununu’s desk for his signature. If enacted, New Hampshire will become the eighth state to enact activityspecific O&P legislation.
SB 1439, legislation supported by SEBCM lead advocate Steve Slawinski, CO, FAAOP, would ensure coverage of activity-specific O&P in state-regulated commercial plans and public employee plans. The bill has passed through the Senate Commerce Committee and will move on to the Senate Budget and Appropriations Committee.
With the help of the Pennsylvania Orthotic Prosthetic Society, another SEBCM bill has been introduced. HB 2399 would ensure that state-regulated commercial plans cover custom O&P, including activity-specific orthoses and prostheses, if deemed medically necessary by the treating physician.



