18 minute read
Women's Health


Advertisement


Jacqueline Rose Menopause Coach, Women's Hormonal Health Specialist, Yoga for Women's HealthCertified Instructor.
REFRAMING WOMEN’S HEALTH –A CALL TO RESET THE PARADIGM
You know how once you see something in a different light, you can never un-see it. You can never go back to the way you used to view it. It happens many times in life. Someone behaves in an unexpected way and you never see them the same way again. Or you hear a new approach to an old theory and it changes your frame of reference. It changes everything. And from then on, your thoughts are altered and you can’t go back. This has happened to me over the last few years with how I view and understand women’s health issues. And it is slowly happening with the women I work with, who are not willing to accept the old medical paradigms.
Let me give you two examples.
Case Study 1:
A dear friend recently told me about a visit to the pediatrician with her 17-year-old daughter. Her daughter was generally healthy, normally had a regular cycle but hadn’t had a period in 4 months, was feeling run down, exhausted, and experiencing some mild digestive issues. The mother didn’t know what to do and how to help her daughter, especially as she was having a busy and stressful time at school. So she went to the doctor, thinking she was doing exactly the right thing. But then she told me how the doctor had responded to them.
“Let’s get some basic baseline blood tests done. But it could just be stress, or maybe you are eating something different, or maybe you are not sleeping as much. It will probably get better in a few months, it’s probably really nothing. It’s totally normal for girls to have breaks between their periods. ” So on the one hand – this doctor did nothing wrong. She ordered the standard tests, she asked some basic questions, and she assessed in her mind no serious issue. She checked everything off her checklist and her job was done. BUT – with my new insight about women’s health issues, when I heard this story I got really angry.
experience. It was a standard 10-minute appointment with the doctor having little time to really join some of the dots of the girl’s health and wellbeing status and consider what this girl was really experiencing. There were no other recommendations made, no talking about her mental health, lifestyle, or practical and tangible things that this young girl could do. Assuming that please Gd her blood tests all come back clear, she was basically told to just wait around for her period to eventually come back and that this was just “normal teenage stuff” .

For me, THIS IS JUST NOT GOOD ENOUGH!
It is not the doctor’
s fault. She did what she has been trained to do.
After speaking to my friend and understanding more of her daughter’s situation, I think stress is playing a big role in her irregular periods. Dealing with stress, looking at what she’s eating, assessing her gut health how much is she sleeping, is she moving at all or sitting for hours revising for exams – these are questions that the doctor ran through but didn’t stop to delve into and explain how significant they are to teen health.
I feel so sad, angry, and disappointed at the dis-service that this girl experienced by her doctor who did not ask the right questions didn’t think about root-cause triggers, and did not take the time to look at the larger picture. The doctor just related to the symptoms as presented. And this is the way the Western medical healthcare system is structured and has worked for years.
I believe, however, that there is a different way for women to be supported. I believe that our bodies are complex structures, that we each have our own health story and there is a detailed spider’s web of a health story to unravel. It requires taking a much more holistic approach when dealing with our health issues. It requires time, attention, and understanding. It requires the doctor to ask questions and have time to listen to the answers! It also requires US to be proactive, to ask questions, and if we don’t feel that we have been seen or heard, if we are not satisfied with the response, we need to keep asking.
Case Study 2:
A woman came to see me who was really struggling with menopause symptoms, she was all over the place and about to get separated from her spouse.
She told me that at the age of 48 her life was not going well. She had low energy, and could not get motivated to be productive in her work life. And the lack of focus and concentration wasn’t helping.
She wasn’t sleeping well and felt overwhelmed with the demands of her personal and professional life. Her libido was through the floor, her husband was driving her mad, she was moody the whole time, her body hurt her and she just wanted out. And worst of all was that she had been a “superwoman” in the years leading up to these changes – she was the doer, the one that everyone relied on. She felt frustrated and confused.
She had been to her doctor. He had ordered some blood work and to check her hormones to see if she was peri-menopausal. He then basically recommended a variety of different pills – sleeping tablets for when she couldn’t sleep, anti-anxiety to regulate her moods. He basically told her “it will eventually pass. This is just normal for women of your age. And if things get worse, come back in 6 months.


I was angry with her but not surprised. I hear this the whole time. Women who are peri-menopausal or close to menopause do not feel seen or heard. The complexities of their symptoms are not being recognized. The way these symptoms impact their personal and professional lives is not being understood. Being given band-aid medicine that treats the symptoms doesn’t really address the full extent of their challenges. Six months of suffering and struggling until she can go back to the doctor again to see if he will recommend anything helpful. Once again THIS IS JUST NOT GOOD ENOUGH! Of course, it is not his fault. He is doing what he has been trained to do. Work through the checklist of questions, ascertain if he can make a diagnosis based on the symptoms, and treat with appropriate drugs. But, it ignores the overall health and wellbeing of the patient. It ignores the physical, emotional, and mental health relationships. It ignores her experience of struggle, confusion, and suffering and how that impacts all areas of her health and wellbeing. And in this particular situation, it totally ignores the complex ways that menopause can show up, how it can affect your life, and practical strategies that can be easily implemented to support women. There is no understanding of menopause management and the deep way it affects women. Before I continue I want to add here a BIG DISCLAIMER: I am NOT an anti-Western medical care system. It is amazing and miraculous. The healthcare professionals are doing the best they can, within the framework in which they work and the training they have received. I have seen first-hand how this medical care system saves lives day after day. However, time and time again, I hear how this approach is failing women and their health concerns. How women are sent away to “just deal with it” . How it’s assumed “eventually things will sort themselves out, and if not just come back in 6 months' time. ” I hear about women with endometriosis and polycystic ovaries syndrome who don’t get diagnosed for years. I have heard stories, too many to count, of women who are put on anti-depressants for their
menopause symptoms, because they have been misdiagnosed.
Part of the reason for this approach is the traditionally low percentage of medical research which includes women's data sets. For decades, until US Federal Law legislation changed in 1993, a lot of clinical research and studies were done solely or largely on men and the results were extrapolated to women. Women were excluded from clinical drug trials and so dosages were male-driven. Women’s health issues have just not been recognized, researched, or taken seriously enough. And treatment options are still way behind where they need to be. But in 2021, things are changing, albeit slowly.
There is another way to approach women’s health and I have seen it in action and that is a Functional Medicine approach. It looks at the body as a number of integrated systems working together in a delicate balance. Rather than using the symptoms as the marker for treatment, Function Medicine looks and the root causes of ill health and addresses what needs to change at the source.
There are some amazing doctors out there who think differently. Who understands that women know what’s going on in their bodies and that if a woman has actually made time to come and get checked, that means she is struggling. I know there are health professionals out there who get how women’s hormones impact everything going on in our bodies. I know that a functional, integrative approach to women’s health is possible, to look at the whole body and assess what’s really going on.
I also know that unfortunately, it’s on us to get educated, informed AND proactive about our own health journey. Today it’s not enough just to go see your doctor. Today you need to be more forceful to get the answers you want and deserve. Today you need to search for the “right doctor” who understands and embraces a different approach to women’s health and healthcare treatment. Who understands how to look at health differently – to look at the root causes and not just at the symptoms!
In addition, there is a growing body of evidence-based research into the benefits of integrating an alternative, holistic approach to health and wellbeing. Things like yoga, mindfulness, alternative therapies, deep breath work, supplements, plant-based medicine, self-care, etc need to be included in our health management protocols.
I am NOT proposing giving up on our Western medical healthcare system. Not at all. However, I am saying that we need to start seeing it for what it really is – ONE pathway on our health journey.
We need to start assessing how it supports us and how it’s failing us. We need to ask our healthcare professionals within this system to do better for us. And we need to get proactive to find the doctors and medical professionals who are pushing the envelope in thinking about healthcare in a different way. Who understands that the old system needs a reboot, and who understands that women’s healthcare needs to be done differently! Because once you realize how your needs can be met, you can’t go back to the way you received treatment before.

Jacqueline Rose
www.theyogaroom120.com/

MANAGING PESKY LEAKAGE
Dr. Elaine Mele PT, PYT, FNCP Physical Therapist Yoga Therapist Functional Nutrition Provider
How to get on top of the drops”
Has it happened to you? Jamming through your HIIT class or out for a much-needed run and just as you start to pump up the intensity...feeling good...feeling strong…oops there goes a warm trickle down your leg.
Or maybe you are out with your girlfriends’ sharing a good hearty laugh and you feel a couple of drips.
Or you are stuck in traffic and you have to GO. RIGHT. NOW.
How did you feel when this happened? Did you experience embarrassment, shame or exasperation?
Well, guess what, you are NOT ALONE. Stress urinary incontinence (SUI) which is defined as urine leakage that occurs during loaded, physically stressing activity occurs within 4-10% of women (1).The incidence increases to about 50% for those who have given birth and it can rise again during perimenopause with an average of 30–50% experiencing some form of incontinence (2). So you can see leaky episodes are pretty prevalent.
There are different types of incontinence, the 2 most common are:
Stress Urinary Incontinence (SUI): which is urine leakage that occurs when the body experiences a physical “stress” such as during sneezing, coughing, laughing or high impact exercise like running.
Overactive Bladder (OAB): which is an increase in urinary frequency (peeing more than 8-9 times per day) or in urge (being unable to hold your urine until you get to a toilet or needing to urinate multiple times overnight)
You can also have mixed incontinence, a combination of the two, but we’ll just keep it simple here today.
We know that incontinence in women is common, but is it an acceptable, “normal” side effect of pregnancy or aging that we just have to suck up and deal with? No.
This is treatable and not something to be ashamed of.
Before we talk about how to fix the problem we must first understand how and why it happens.
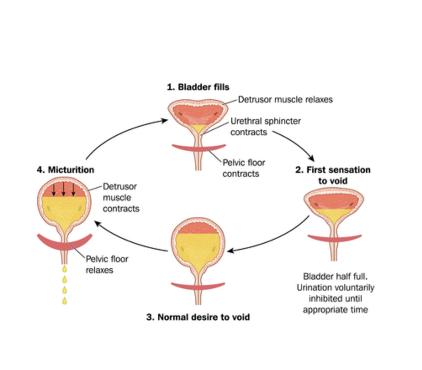
Most of us already know the bladder holds urine in our bodies. The main muscle of the bladder is called the Detrusor, it contracts and squeezes the bladder to initiate urination. Coming out of the bladder is a tube called the urethra. The urethra has a sphincter that acts as a gatekeeper, it opens to release urine and closes to keep urine from leaking out. The pelvic floor lies underneath all of this, like a hammock, to support the entire structure. The pelvic floor must stay somewhat contracted or engaged to work with the urinary sphincter to keep any urine from leaking out. It also must be able to relax to allow urine flow when the time is right. If the Detrusor muscle contracts and the sphincter is not closed, leakage occurs. Alternatively, if the Detrusor contracts and the pelvic floor coordination is delayed, leakage can occur.
A nerve feedback loop also exists between the bladder and the brain sending messages back and forth regarding the volume of fluid in the bladder and the urge to urinate. The brain receives a message that the bladder is at a certain volume and then the brain “decides” whether it is time to urinate. It will then send a signal to the muscles and sphincter around the bladder to relax, allowing urine to flow out. Sometimes we can unconsciously train the brain to signal urination in habitual situations such as soon as we pull into our driveway or when we get to work, whether or not our bladder is actually full and ready to empty.
Certain foods can also “irritate” this feedback loop causing the pathway to be overactive, thus increasing the signals to the bladder that it's time to void, increasing the frequency and urge of urination. Overurination, or urinating more than the average of five to seven times per day can lead to weakness in the pelvic floor, disruption of the system’s natural cycle and rhythm and it can also increase the risk of developing a UTI (urinary tract infection), which we all know are not fun!
During perimenopause, we also have the additional influence of Estrogen. The natural and progressive decrease in estrogen during this time leads to thinning of the vaginal tissues and a loss of elasticity (ability to bounce back from a stretched position).
This can lead to a weakened pelvic floor. A weak pelvic floor cannot fully support the organs nor maintain the appropriate tension required to prevent leakage.
The other important area to consider with incontinence is the internal pressure system created during breathing. We have two diaphragms that help maintain the pressure system, the respiratory diaphragm that sits just under your rib cage and the pelvic floor (diaphragm) that sits at the base of your pelvis.
www.elainemele.com elaine@elainemele.com
These structures move in tandem in a very coordinated manner. When we inhale and draw in breath both diaphragms drop or relax creating a negative pressure system to draw air into the lungs. On the exhale, the air is released by both diaphragms lifting up and contracting, forcing pressure up and out. If our diaphragms are not coordinated properly we could experience an increase in downward pressure that stresses the urinary system causing leakage. For an animated explanation of this check out this YouTube video by my colleague, Julie Wiebe, PT https://www.youtube.com/watch?v=eRAaJN3FC6A
So, you can see that we have a complex system at work that affects how, when, and why we pee. The processes leading to incontinence can be multi-faceted and is not a one-size-fits-all problem, but there are a few simple things you can try first to address unwelcome leakage:
Avoid bladder irritants
Certain food and beverages will cause the bladder and nerve pathways to become hypersensitive and create a situation where the urgency to go is greater.
Foods that are considered bladder irritants include:
Coffee Soda (any and all) Artificial sweeteners and processed foods Energy drinks; and Acidic fruits and juices like orange and grapefruit
Make sure you fully empty your bladder

Sounds like an obvious suggestion but, let’s face it, many women...
are often multi-tasking while they pee, thinking about the next five things on the to-do list don't always pay attention to or, in some cases, lack of sensation when the bladder is empty
Full bladder emptying should occur without bearing down or using force, so this doesn't mean wringing out your pelvic floor to squeeze out every last drop. It just means be patient and let your urine stream come to a complete and natural stop on its own.
Maintain healthy bowel movements
Nothing is off-topic here! Constipation will increase the pressure on your bladder since the rectum sits directly behind it. This will cause the whole system: the pelvic floor, urinary sphincter, and detrusor muscle to have to work harder to overcome the extra load, increasing the risk of leakage.
The goal is to have at least one healthy bowel movement per day. Healthy poop is log-shaped and firm but not hard. To avoid or mitigate constipation, drink plenty of clear, non-sugary, noncaffeinated fluids, such as water. The recommendation is to drink a minimum of 65 ounces per day, but optimally you imbibe half of your body weight in ounces of fluid (ie: 75 ounces for a 150lb woman), eat at least 25 g fiber per day that is sourced from whole grains, fruit and vegetables and aim for 30-60 minutes of daily exercise. That’s all I have to say about poop, for now!
In order to maintain a nice healthy pressure management system that we discussed earlier, it is important to be aware of our breath. This is something that you can practice outside of your workouts when you are in a relaxed state before you try and practice it in a “loaded” situation.
*Try this* Pick an exercise that is easy for you such as an unloaded (unweighted) squat.
Slowly move into a squat position while you inhale, pause.
Now to start to exhale slowly as you begin to return to a standing position. Keep exhaling the whole way through until you are fully standing. If you can, also envision the pelvic floor (ie: your perineum or space between your vagina and anus) lifting up and drawing in, like an elevator rising from the ground floor, throughout the exhale. Avoid clenching these muscles, that will be counterproductive. Just begin with envisioning a gentle engagement and lift.
It is important that the pelvic floor is also able to relax, so when you initiate the next inhale and lower back into a squat, imagine that the perineal space is widening out in all four directions as you move back down.
Repeat a few more times and again over the next few days until you are comfortable with the timing and coordination of the breath cycle. Then go ahead and try it with an added load by adding weight to the exercise, it can be a literal weight or a laundry basket or your child. Start with the smallest weight first. See if you can avoid leaks with just this simple exercise and then gradually increase the load. The more you practice this pattern of breathing during exertion, it will eventually become natural where you won't have to think about it every time and hopefully, your leakage will decrease dramatically! Won't that be great?!?
Give these four things a try and let me know how it goes!
If you continue to struggle with increased urinary frequency, and urine leakage during exercise or exertion you may need to see a healthcare provider that specializes in Women's
Health. You can also reach out to me at elaine@elainemele.com for a free 20-minute
consultation to discuss your needs.
Reference:
Dr. Elaine Mele
www.elainemele.com elaine@elainemele.com