Will COVID-19’s hybrid meeting legacy last?










Year three of the COVID-19 pandemic and yet much now feels unrestricted and ‘back to normal’. This can certainly be said of meetings—at least in Europe and the USA—which, throughout 2020 and some of 2021, took place online, but have returned to in-person in recent months. However, transatlantic, intra-European and American travel, though possible and permitted, has not been plain sailing (flying?), even this year. Therefore, many societies, within interventional radiology (IR) or otherwise, for 2021/2022, have opted for a hybrid setup, where delegates have had the choice of accessing sessions, or to travel to the physical venue. Several society spokespeople relay to Interventional News their plans for the hybrid and in-person evolution of some of the IR calendar’s main meetings, based on how those from the last couple of years have panned out.





PARAG J PATEL (MEDICAL COLLEGE of Wisconsin, Milwaukee, USA), president of the Society of Interventional Radiology (SIR), provides the perspective of a society that has, deliberately, not offered hybrid attendance options. The reason being, he explains, that “this allows us to provide a consistent experience to all who participate, ensuring valuable learning, interactions with speakers, and connection to the materials.” So, this year’s Society of Interventional Radiology annual meeting (SIR; 11–15 June, Boston, USA) was in-person only, and 2021’s exclusively online, after the 2020 meeting, scheduled for late March, was cancelled. However, Patel notes, the SIR 2022 plenary sessions were available via livestream, and saw 230 viewers tune in.
This reflects where the society stands on the question of a hybrid future for meetings right now, and Patel details how the hybrid model has, by no means, been discounted by SIR, which is “exploring the possibility of deploying hybrid models at future meetings to allow more IRs to participate in the way in which they prefer to or are able to attend. We know that travel and time off can be a challenge, and hybrid models enable accessibility from an attendance standpoint.”
on page 4

Continued
www.interventionalnews.com
Profile:
Dimitrios Filippiadis page 14 November 2022 | Issue 88
Josef
Roesch Lecture page 11 Report on rural IR practices page 7
by egos, or other factors that may render patient outcome a secondary consideration. In contrast, Verhoeven relayed how, at his hospital, “it is completely irrelevant who is doing what”, elaborating on this to say that “we decide together as a team who is the best suited” for taking on each individual case. This statement then gave way to Ricke making the point that different people’s definitions of collaboration will be different, and that what multidisciplinary involvement looks like in a particular hospital needs to be defined— ‘involved’ does not necessarily mean doing the procedure, as he added that it could mean only taking part in decision-making beforehand.





In addition to keeping the patient at the forefront of a procedure and “[putting] ego aside”, as Valérie Vilgrain (Assistance Publique-Hôpitaux de Paris, Paris, France) drove home in her presentation, Ricke summed up another takeaway from the session as a whole: “What I have learned today is that we need communication training in medical school.” He went on to contextualise this by making clear that “Nuernberg is not the rule” and that collaboration may not occur in a multidisciplinary manner as effectively in other hospitals. His hope, therefore, is that by starting early, the next generation of clinicians can learn while still at medical school to communicate in a way that is conducive to collaborative, yet patient-centred work.
Antonin Krajina (Charles University Hospital, Hradec Kralove, Czechia) then called upon the societies, such as those represented round the discussion table, to “take responsibility for interdisciplinary education.” Examples of this already occurring were heralded throughout the session, including the European Society for Minimally Invasive Neurological Therapy’s (ESMINT) theoretical stroke course (EXMINT).
Stroke treatment and by whom it is delivered formed a further part of discussion during the session, with
the panel shining a light on the differences in stroke thrombectomy services between the UK and The Netherlands in particular. Beyond the theory, as courses such as EXMINT teach, there is a question of how much training an interventionalist should be required to do before they can independently carry out thrombectomies for stroke patients. Wim van Zwam (Maastricht University Medical Center, Maastricht, The Netherlands) explained how “in The Netherlands, we have a requirement that if you want to do thrombectomies, you have to do at least 25 under the guidance of an experienced interventionalist, and your centre has to do at least 50 thrombectomies per year. These are very simple and straightforward guidelines.” However, Van Zwam acknowledged that, while there are more centres that can and want to do stroke thrombectomy than the country needs in The Netherlands, such is not the case in the UK. Uberoi labelled the latter as a “chicken and egg situation”, whereby “until you start doing the procedure, how can you have enough cases to train in it.”
Van Zwam followed up to ask whether a solution


News in brief The latest stories from the interventional world




could be to allow adequately trained cardiologists to perform stroke thrombectomy, to which Uberoi responded: “I do not really think the patients care who does their procedure], as long as it gets done and it is a safe service. Ultimately, you want the best trained person, but there has got to be a reality check in terms of what is achievable. Do you want zero service, or could a ‘silver’ or ‘bronze’ service be good enough to improve outcomes without compromising safety? That is the kind of balance I feel we need to look at in the UK.”
The session closed with all participants agreeing that “the clinical aspects of patient care are the same whether you are a vascular surgeon, interventional cardiologist or interventional radiologist.” This can, therefore, be a unifying motivation in multidisciplinary collaboration scenarios, and, as Vilgrain summarised, “we are better doctors when we work together”. This necessitates leaving egos at the door and working communication skills into education for medical students and trainees.
n SURVIVING AND THRIVING IN IR: Matthew Gibson (Royal Berkshire Hospital, Reading, UK) speaks to Interventional News on the topic of the British Society of Interventional Radiology (BSIR; 2–4 November, Glasgow, UK) annual meeting’s Wattie Fletcher Lecture: How to survive and thrive as an interventional radiologist. He discusses the impact of serious adverse events on physicians, why burnout is such a pressing concern in interventional radiology (IR), but, also how, in spite of this, it is possible to retain one’s enthusiasm and sense of humour in the job.
For more on this story go to page 7.
n BELOW-THE-KNEE VASCULAR TRIAL DATA: The Cardiovascular and Interventional Radiological Society of Europe (CIRSE) annual meeting (10–14 September, Barcelona, Spain) saw the presentation of data from two key studies of below-the-knee (BTK) treatments. The SAVAL trial compared a drug-eluting stent system with percutaneous transluminal angioplasty for critical limb-threatening ischaemia, while the MOTIV BTK postmarket trial is evaluating safety and efficacy for the treatment of patients with rest pain or minor tissue loss due to the presence of BTK lesions.
For more on this story go to page 10.
n INSIGHT INTO IR’S TECHNOLOGICAL FUTURE:
A series of speakers took to the CIRSE stage to present their observations and predictions for IR as a specialty from a technological perspective. Key takeaways for delegates included how artificial intelligence is not a threat to existing IR practice, but a tool that interventional radiologists can harness to advance services for patients—and that this is defined as ‘hybrid intelligence’.
For more on this story go to page 13.
Published by: BIBA Publishing, which is a subsidiary of BIBA Medical Ltd
BIBA Medical, Europe, 526 Fulham Road, Fulham, London, SW6 5NR, United Kingdom Tel: +44 (0) 20 7736 8788
BIBA Medical, North America, 155 North Wacker Drive, Suite 4250, Chicago, IL 60606, United States Tel: +1 708-770-7323
Printed by: Buxton Press
www.interventionalnews.com
Reprint requests and all correspondence regarding the newspaper should be addressed to the editor at the United Kingdom address.
© BIBA Medical Ltd, 2022. All rights reserved.
Write to us!
If you have comments on this issue or suggestions for upcoming editions, write to clare@bibamedical.com
Next issue: February 2023
2 November 2022 | Issue88 facebook.com/interventionalnews linkedin.com/company/interventional-news/ @in_publishing
Cover Story
Luigi Solbiati Fernando Gómez Muñoz
Editors-in-chief: Professor Andy Adam, Dr Brian Stainken Publisher: Roger Greenhalgh Content director: Urmila Kerslake Editor: Clare Tierney Editorial contribution: Jocelyn Hudson, Will Date, Bryan Kay and Jamie Bell Design: Terry Hawes, Wes Mitchell and David Reekie Advertising: Michael Broughton michael@bibamedical.com Subscriptions: subscriptions@bibamedical.com News or advertising queries: Tel: +44 (0)20 7736 8788
“Put ego aside” to keep patient outcome the priority during multidisciplinary collaboration
What I have learned [...] is that we need communication training in medical school.”
Continued from page 1
Stefan MüllerHülsbeck
Jens Ricke
Raman Uberoi
Eric
Verhoeven
Valérie Vilgrain
Wim van Zwam
LEARNING WITH A


COLLABORATIVE APPROACH IS1381GB0822MVI www.terumolearningedge.eu www.terumo-europe.com Discover our new educational website
Will COVID-19’s hybrid meeting legacy last?
In contrast, the European Society of Radiology (ESR)’s director of communications David Zizka tells Interventional News, that his society has taken a hybrid approach to its annual meeting, the European Congress of Radiology (ECR) since 2013 when it started streaming educational content. “Our participants are used to having the option to attend the event either onsite or online, but in many cases, they choose to attend in both ways,” Zizka notes, qualifying this statement with the following: “What we have learned this year is that there is no strict distinction between an onsite or online visitor anymore, as many of our participants visit us in Vienna, but not for the entire five days, and then continue their ECR experience online.”
Concerns for superiority of in-person experience not universal Patel expresses concerns that moving away from in-person only, may not be solely positive for the SIR meeting—as the rationale for not offering SIR 2022 in a hybrid format suggests. “We want to ensure that what we deliver does not create silos in the audience based on the format through which the attendee chose to participate. There is a risk with a hybrid approach that one group receives a lesser experience because they are not in the audience,” Patel acknowledges, before highlighting what underpins this reservation. “We do not just want to broadcast content to a passive audience. We want to actively engage our audience in discussion and learning, whether in-person or online.”
Zizka appears not to share such concerns, stating that “we are stepping away from differentiating participants according to [whether they are online or onsite attendees], as ECR is not a single event anymore but a
year-long one with a variety of ways of participating.”
He expands upon this assertion, pointing to the fact that “watching sessions on-demand during the actual congress period and especially afterwards for the rest of the year has become very popular amongst our participants.”
Adding his voice to the discussion, the Radiological Society of North America (RSNA) associate executive director for meetings services and corporate relations John Jaworski, whose opinion comes from the position of having 40% of RSNA attendees come from outside of North America, is therefore aware of the constraints that prevent people from travelling to the physical event space. Luckily, he acknowledges that “RSNA is fortunate to have a great team able to support both [the in-person and virtual] events,” which enables the society to fulfil the important objective of “[reaching] a greater number of healthcare professionals across the globe and providing them with important educational content to assist in patient care.”
Shared observations of post-pandemic attendance upswing Patel underlines that all societies are having to consider how to keep optimal engagement from attendees the foremost priority. Interestingly, Zizka underlines that there was already “a regressive trend in onsite meeting attendance before COVID-19”, but that a reduction in appetite for attending in person may have been “accelerated” by the pandemic. In the eyes of the ESR spokesperson, “onsite attendance must be a special experience for the participant [if the meeting has a remote attendance option], something that adds unique benefit in comparison to online-only participation,” justifying this with the point that offering hybrid meetings means “you will see a decrease in onsite participation.”
But, right now, in the immediate aftermath of lockdowns, Patel recounts witnessing “a chorus of excitement and eagerness to be completely in-person,” at SIR 2022. “Screen fatigue is real,” Patel adds, attributing the “[palpable] desire to continue to meet
in person” to this fact. Jaworski has observed the same enthusiasm for the in-person RSNA annual meeting: “Currently, our in-person registration is up 54% from this time last year, while our virtual meeting is on a par with 2021,” he relays to Interventional News. This follows an RSNA 2021 meeting for which attendance was “in line with our expectations”—30,000 attendees, of whom 6,000 attended virtually.
ECR received similarly positive feedback about their 2022 meeting, including from those who made last-minute decisions to attend remotely instead of in Vienna, and vice versa. “A big benefit of our registrations system is that every ECR ticket allows for full onsite and online access,” Zizka emphasises, “so participants can make that decision at any time without any bureaucratic efforts.”
Priorities for a bright future of IR meetings


Quizzed on how SIR plans on fulfilling the aforementioned goal of maintaining high levels of engagement, Patel refers to the possibility that SIR 2023 will livestream “at least some in-person sessions and in ways to ensure that any online audiences are actively engaged in the lessons happening on site in Phoenix.” After the fact, an on-demand library will enable attendees to revisit sessions, or view those they missed, Patel adds, stating that this “will also be available for purchase after the meeting for those who could not attend in person.”
The priority for the RSNA meeting logistics-wise, Jaworski brings to Interventional News’ attention, is to “better connect the virtual attendee to the in-person meeting.” For him this means “[looking] at almost every session like a TV studio and [considering] what the virtual attendee will be seeing and hearing.” One example of a simple but pivotal consideration in this regard is checking that in-room microphones are switched off during breaks “so personal conversations are not broadcast virtually”. Jaworksi adds that the RSNA is also “working on a way to better connect the virtual attendee with the speaker during session question and answer sessions, which will require some re-training of session moderators.” Finally, he alludes to the longer-term goal of RSNA “[improving] virtual networking between attendees and engagement opportunities with virtual exhibitors.”
Patel appears optimistic about the future of SIR meetings, in whatever variation on a hybrid form they may take, based on the 4,000-strong attendance at the 2022 meeting. Even if in-person attendance is set to decrease, as Zizka predicts, he believes that the strategies the ESR is adopting will mitigate this, at least in part, with “state-of-the-art online participation possibilities that live up to the latest technical trends, and [by reinventing] our event every year [to make it] a unique experience […] that people are always drawn to take part in onsite.” Jaworksi sees the meetings trend going the way of fewer attendees overall “in the short-term”, before increased comfort with travel leads to an uptick in attendance once more. “Nothing is better than faceto-face meetings for connecting with colleagues and developing relationships,” he professes, suggesting too that “competition from virtual meetings will lead to better in-person meetings […] with experience and engagement opportunities for attendees, such as interactive and hand-on experiences.”
November 2022 | Issue884 Cover Story
Continued from page 1
Onsite attendance must be a special experience for the participant [...] something that adds unique benefit.”
“The SIR 2022 plenary sessions were available via livestream and saw 230 viewers tune in.” “Currently, [RSNA] in-person registration is up 54% from this time last year, while our virtual meeting is on a par with 2021.” The societies let their statistics speak
An insight into treating liver tumours with thermal ablation
Amanda Smolock
Comment & Analysis
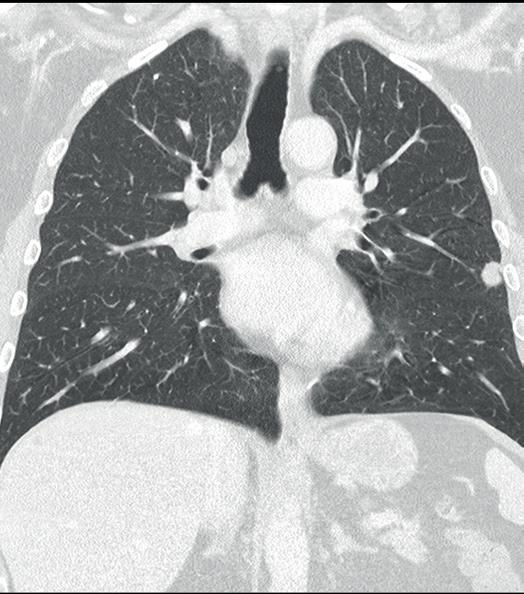
Amanda Smolock (Medical College of Wisconsin, Milwaukee, USA) discusses how her practice operates, using microwave ablation nearly exclusively for primary and metastatic liver tumours targetable under ultrasound (US) and/or computed tomography (CT) guidance.
Patients are typically discussed at a multidisciplinary liver tumour conference and referred to the interventional radiology (IR) clinic for evaluation. At consultation, a full history and physical exam is completed along with updated laboratory studies, including complete blood count, liver function studies, and coagulation tests. Patients with good performance status and preserved liver function are considered appropriate for percutaneous liver ablation. Contrastenhanced (CE) CT images or magnetic resonance images (MRI) are obtained within one month of evaluation and procedure. US assessment is performed at the clinic visit to ensure sonographic visibility and percutaneous approach for ablation. The approach is communicated with the procedure team and helps to streamline preparation on the procedure day.
Procedures are scheduled for general anaesthesia in the interventional CT suite and proper patient positioning for the procedure is a team effort: a posteriorly located tumour may require oblique positioning of the patient, and safe positioning of arms overhead improves CT image quality.
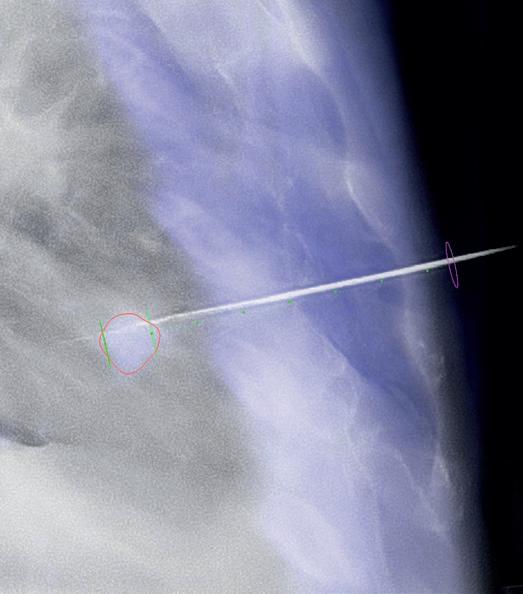
Non-contrast and multiphasic CE-CT are typically obtained prior to probe placement. This helps to review anatomy pre-procedure, confirm tumour location and size, and optimise the percutaneous approach. When possible, probes are placed under direct US guidance. Few cases have tumours visible only on CT or only after lipiodol staining with transarterial chemoembolization (TACE). In these cases, CT navigation software is used to optimise probe placement, which is often best in double oblique approaches to maximise both safety and efficacious tumour treatment. Respiratory manoeuvres in concert with the anaesthesiology team are utilised as
needed to accurately and precisely target tumours with ablation probes. A non-contrast CT is obtained to confirm and document probe position. Hydrodissection and/or biopsy, if being performed, are done after securing ablation probe position(s). CT and US are complementary imaging to confirm appropriate tumour targeting and predict ablation zone coverage. Activated probes and ablation zone formation are monitored in real time with US and intermittent CT. This allows for confirmation of ablation zone formation and coverage.
Another CE-CT is obtained at the conclusion of the ablation. Total contrast volume is split between pre- and post-ablation CE-CT, not to exceed 150–200ml of iodinated contrast agent. Post-ablation CE-CT assesses ablation zone coverage of the tumour with adequate margins and also evaluates for any complications. If margins are inadequate, additional ablation can be performed at this time.
A recent addition to our practice is MR-guided cryoablation. This technology allows ablation of small liver metastases that are visible only on MRI. Patient positioning and tumour targeting require additional considerations to maintain safety in the MR environment.
Patients receive a check-up telephone call from a nurse the day after the procedure and are then seen one month post-procedure in clinic along with CE-CT/MR. Follow-up with imaging occurs every three months, which may be extended to every six months after one year of documented complete response.
Amanda Smolock is assistant professor at the Division of Vascular and Interventional Radiology, Department of Radiology, Medical College of Wisconsin (Milwaukee, USA).
Disclosures: For relevant disclosures, see interventionalnews.com

5Issue88 | November 2022 Comment & Analysis
JW MARRIOTT MARQUIS MIAMI, FL JANUARY 12-15, 2023


DAYS
FACULTY
BOARDS
PARTNERS
WORKSHOPS
RT & RN CREDITS
TRAINEE GRANTS

SUBMISSION OPEN MULTIDISCIPLINARY SESSIONS and JANUARY IN MIAMI

The SPECTRUM conference offers attendees a comprehensive review of a variety of oncological diseases, with the latest developments in surgical, medical, interventional, and radiation therapeutic options. A practical overview of how to incorporate these therapies into practice will be presented through a multidisciplinary lens, intended to achieve the highest levels of success in the fight against cancer.
In addition, SPECTRUM 2023 will dedicate 2 days to “ABLATION SPECTRUM” to bring you the most in-depth program on all types of tumor ablation. Hear from the pioneers and global leaders in tumor ablation along with case-based reviews. Learn about the latest advances in ablation, guidance and navigation and get a first-hand experience at the workshops.


OUR PARTNERS:
 JW MARRIOTT MARQUIS • MIAMI, FL
JW MARRIOTT MARQUIS • MIAMI, FL
More and Register at
thespectrumconference.org
MULTIDISCIPLINARY IO Learn
4
89
TUMOR
GLOBAL
HANDS-ON
NATIONAL
RESIDENT
ABSTRACT
Why laughter is not “frivolous”: Keeping burnout at bay in IR

Matthew Gibson (Royal Berkshire Hospital, Reading, UK) will be delivering this year’s British Society of Interventional Radiology (BSIR; 2–4 November, Glasgow, UK) Wattie Fletcher Lecture ‘Survive and thrive in interventional radiology [IR]’. Interventional News spoke with Gibson to glean some of the details of his talk, in which he will address the “psychological and non-medical stresses and strains of being an interventional radiologist and even suggest some things we can do to improve the situation.” From Gibson’s preview, it would appear that he intends to underline in the lecture how “just trying to get through to the next day is not enough” as an interventional radiologist. A selfprofessed enthusiast who, from personal experience, knows the value of enjoyment and laughter at work, Gibson makes a compelling case for thriving over mere survival in IR.
“Ihave an interest in several areas of IR, for example below-theknee angioplasty, dialysis access, and deep venous intervention but I am sure there are plenty of people better qualified than me to talk on these topics,” Gibson begins, talking through how he chose his lecture topic. He wanted to make it relevant and interesting to a wide audience. In a career of 25 years as a consultant interventional radiologist, he has “retained his enthusiasm for the job and IR in general”. This has surprised his contemporaries and younger colleagues, who have seen stress and burnout lay claim to many medical professionals’ enjoyment of their job. He felt he was well placed to produce a talk on the alltoo-common stresses of IR, rather than a more specific procedure or medical talk about a certain area of IR.
Before delving into burnout and the many contributing factors that make

this a reality for many interventional radiologists, Gibson states his keenness to work discussion of serious adverse events (SAEs) into his lecture. Namely, he expresses a desire to examine beyond the important impact of SAEs on the patient’s safety: the effect involvement in a SAE can have on medical professionals. “It is something we do not talk about enough, but SAEs produce a
definite adverse effect on medical staff”. This can result in, according to Gibson, damage to confidence and self-esteem and anxiety about making another mistake and, he adds, “you are more likely to be involved in another adverse event if you have already had one.”
“Death by 1,000 arrows” is the metaphor Gibson uses to characterise how the UK healthcare system investigates adverse events. “Although it is supposed to be a no-blame medical culture, being under investigation at any level can be damaging and upsetting. Anyone can refer a doctor to the General Medical Council [GMC], which can be extremely stressful,” Gibson relays, emphasising that doctors have taken their own lives after being referred.
Opening the issue of stress and burnout back up, Gibson again suggests that “[he does] not think we have talked about it enough in IR”, suggesting that this “[may be because] some of us think we are immune to it.” However, “we are all at risk”, he counters, moving on to list multiple explanations for this. Paperwork, emails, directly looking after our own patients”, work-life balance and “time poverty”. In addition, the public’s attitude plays a role, Gibson notes—“the medical profession is less respected than previously and patients and relatives may not understand the subtleties of why mistakes occur and the effect making mistakes, and being the subject of complaints, can have on the medical staff involved.”
In addition, lack of professionalism and rudeness at work “can make your IR team dysfunctional and negatively impact on patient care”.
Yet, there are positive steps that can be taken to mitigate the strain of working in modern medicine and IR, Gibson points out. “Governments,


Report highlights need for recruitment and retention of IRs in rural practices














A report from a joint taskforce of the American College of Radiology (ACR) and the Society of Interventional Radiology (SIR) recommends improved access to interventional radiologists in small and rural areas. The taskforce was formed to explore strategies for recruitment and retention of interventional radiologists in rural areas, which have the greatest challenges with access to interventional radiologic care.
“INTERVENTIONAL RADIOLOGISTS PLAY a key role in improving patient health outcomes and creating healthier communities,” said Alan H Matsumoto, vice chair of the ACR Board of Chancellors and a member of the joint taskforce. “The recommendations should be beneficial for practices in small and rural areas that hope to recruit interventional radiologists and provide the care patients deserve.”
The taskforce focused on improving training opportunities, creating templates to help radiology practices and hospitals provide interventional radiology (IR) services in small and rural communities, and developing appropriate financial models to recruit interventional radiologists to these areas and retain their services.
“Access to an interventional radiologist’s care can be the difference between life and death, yet millions of Americans living in rural communities do not have access to the image-guided treatments interventional radiologists perform to literally save life and limb,” said SIR President Parag J Patel, professor of radiology at the Medical College of Wisconsin (Milwaukee, USA). “Access to IR services improves the care offered within a hospital or health system. The recommendations outlined in this paper will help practices attract IR talent and expand IR services where they are often needed the most, eliminating IR deserts and improving patients’ access to the care they need.”
The report was published online in the Journal of the American College of Radiology (JACR)

employing organisations, managers, interventional radiologists and their team members can take steps to redress work-life imbalance, time poverty, improve resilience and, hopefully, reduce the risk of burnout and also improve patient safety.”
Interventional radiologists would also stand to gain from understanding that “being vulnerable is not a weakness,” Gibson advises, labelling this as “a real issue for us—we are expected to be invulnerable, to ride into high-stress situations and know what to do with no doubt in our mind.” Be this as it may, “you probably also need to be vulnerable at times in order to have a caring, empathetic relationship with your patients,” Gibson admits, elaborating on the importance of “shedding this armour”. Being invulnerable also “spills over into your private life—doctors can have issues with depersonalisation and desensitisation and thus cut themselves off from their loved ones.”
“Having a laugh with staff and patients might seem frivolous because medicine is a serious business, but it can have some very positive effects,” Gibson offers as part of the explanation for his having staved off burnout 30 years into his IR career.
“I cannot pretend that I have all the answers but stress and burnout are very much with us now and are probably only going to get worse.” This is what he expects the BSIR’s first survey into burnout among interventional radiologists to show and is why “it can be quite difficult to convince junior doctors or medical students how much of a privilege it is to care for patients.” Such, Gibson says, is his “humble opinion”, but he is convincing in how he conveys a need to address the issues that will form the basis for his lecture.
Issue88 | November 2022 7Burnout in IR
We are expected to be invulnerable, to ride into highstress situations and know what to do with no doubt in our mind.”
Matthew Gibson
2017 survey: 29% of rural practices could not provide all the necessary IR services Results: 2017 survey of SIR & ACR members agreed that IR services stabilise hospital radiology service contracts endorsed the value of IR services beyond the revenue they generate 76% 84%
New ablation confirmation software and liquid embolic agent at the frontline
The FIRST@CIRSE New Frontiers session at the Cardiovascular and Interventional Radiological Society of Europe (CIRSE) annual meeting (10–14 September, Barcelona, Spain) saw several presentations of new interventional oncology (IO) and embolization trial data, as well as news on studies that are in progress. Notable among them was an upcoming prospective randomised controlled trial (RCT) which aims to show that combined systemic therapy and yttrium-90 (Y90) radioembolization can improve survival for breast cancer patients with liver metastases; prospective multicentre results demonstrating that a new liquid embolic agent is both safe and effective for peripheral indications; and interim results that suggest new ablation confirmation software can reduce the minimum margin in treatment of liver malignancies.
Potential for Y90 embolization lies ahead Nima Kokabi (Emory University School of Medicine, Atlanta, USA) presented his and coauthors’ REMEMBR Y90 study (sponsored by Sirtex Medical), which aims to prove the safety and efficacy of radioembolization, in conjunction with systemic therapy, as a second- or third-line therapy for metastatic breast cancer to the liver. Expectations for the study include a possible increase in progressionfree and overall survival and reduction in treatmentrelated toxicity.
Y90 radioembolization has been used “primarily in salvage settings” and is responsible for a “[perceived] high rate of liver toxicity” and suboptimal survival benefits. Hence, this is the first RCT for evaluating its efficacy and safety when used in the earlier stages of breast cancer treatment metastatic to the liver, Kokabi began by explaining to CIRSE attendees.
Kokabi then outlined that the measure of efficacy—a primary endpoint—in the study is progression-free survival, that the safety profile—also a primary endpoint—of the treatment will be evaluated in terms of treatment-related toxicities, and that the study will also evaluate the “overall survival benefit of the addition of Y90 radioembolization to systemic therapy” as a secondary endpoint.

“Our hypothesis is that the combination therapy group will have a progression-free survival of 50% versus 20% for the systemic therapy group,” the presenter stated, adding that these figures are for the six months following treatment. “We need 50 patients [enrolled] to achieve our hypothesis goal—25 patients in each arm,” Kokabi went on to say.
Although not yet recruiting, once complete, Kokabi and colleagues hope that their study will show that, for patients with metastatic breast cancer to the liver, a combination of Y90 and systemic therapy, earlier in the course of the disease improves survival outcome and reduces treatment-related toxicity.

“Overall very good” results for new liquid embolic
Marc Sapoval (Hôpital Européen Georges Pompidou, Paris, France) took to the podium to present the full results from the EASYX-1 study (Antia Therapeutics AG), which evaluated, as a primary endpoint, the safety and efficacy of the Easyx liquid embolic agent for peripheral embolization.
The embolic agent is a “polyvinyl alcohol (PVA) co-polymer with iodine groups covalently bonded to the PVA,” Sapoval provided as background to begin his presentation.
The 50 patients who
genicular artery embolization (GAE) for knee osteoarthritis, were then presented by Adriaan Moelker on behalf of colleague Tijmen van Zadelhoff (Erasmus Medical Center, Rotterdam, The Netherlands). The aim of the treatment for the indication in question “is to reduce blood flow to the hyperaemic synovium,” Moelker provided as context, noting that “singlearm studies have shown promising results but do not account for a possible placebo-effect”—which is where this trial comes in.
Regarding methodology, Moelker relayed that 58 patients were randomised 1:1 to either GAE or a sham treatment, and the primary endpoint is the difference in the two groups’ patients’ knee injury and osteoarthritis outcome score (KOOS) pain subscale at four-month follow-up. Moelker also shared the secondary endpoints—number and severity of adverse events, and reduction of synovitis as seen on magnetic resonance imaging (MRI).
took part in the multicentre, prospective study had the following treated with Easyx: varicocele (n=15), angiomyolipoma (n=2), type 2 endoleak (n=8), acute bleeding (n=16), and portal vein embolization (n=9). The secondary endpoints evaluated included patient characteristics, technical and clinical success, and interventional radiologist satisfaction.
Sapoval reported to delegates an immediate technical success rate of 98% (n=49), a 100% clinical success rate for acute bleeding and type 2 endoleak embolization, which was 85.7% for patients with varicocele.
Portal vein embolization patients showed a “significant hypertrophy of future remnant liver at follow-up, and five of the nine patients could undergo preplanned hepatectomy,” the presenter elaborated, before concluding that “Easyx demonstrated its safety and efficacy with good results in common indications for liquid embolics.” Sapoval also acknowledged another “very important feature of this new liquid, [which] is that the beam-hardening artifacts are very, very reduced, and this can be very good when you do endoleaks.”
In terms of interventional radiologist satisfaction, it was “overall very good,” Sapoval summated, assessed as “greater than 90% for ease of use, ease of injection, cohesivity and overall angiographic results”.
Awaiting conclusive data from GAE trial
The primary results from the NEO trial (Cook Medical), a randomised sham-controlled trial of
The primary results, Moelker concluded, were that mean pain reduction after four months in the experimental group was 21.4 vs. 18.4 for the sham group, and “this showed [...] no statistical difference between either group”. Despite this result, with a “high placebo effect”, Moelker hypothesised that at one-year follow-up, “the placebo effect [may wear] off and the treatment effect [may persist], but we will have to wait for these data”.
Study yields “significantly [improved]” ablation margins
Bruno Odisio (MD Anderson Cancer Center, Houston, USA) then presented interim results from the COVERALL trial (National Institutes of Health), which he and colleagues are conducting to evaluate whether a new biomechanical AI-powered ablation confirmation software can improve the minimum ablative margin when treating malignant liver lesions. They expect that this “might translate to [improved] liver ablation efficacy and local tumour progression rates.”
“We know that ablation margins are the most important element to change the outcomes of liver tumours that are ablated—and it is the only thing that we can actually modify when we do liver ablations”. Odisio proceeded to explain the added value the software they studied brings when it comes to assessing minimum margins, as “with simple visual inspection, we tend to under- or over-judge [them] in approximately 44% of the patients”. This is important as “insufficient minimal ablation margin has been linked to treatment failure and local tumour progression”, hence studying the potential for improved minimum ablative margins with the proposed software.
The study is a single-centre, prospective, randomised, two-arm, phase II, intent-to-treat trial and 100 patients receiving microwave or radiofrequency ablation for primary and secondary liver tumours will be enrolled. Ablation confirmation for the experimental arm will be carried out using the biomechanical deformable image registration, versus standard-of-care visual inspection for the control arm, Odisio conveyed to delegates.
Marc Sapoval (far left) and Adriaan Moelker
The primary objective, the presenter continued, is to “evaluate if intraprocedural use of a biomechanical deformable image registration method during percutaneous ablation will increase the minimum ablative margins on a 3D computed tomography (CT)generated analysis.”
For the interim analysis, Odisio stated that they looked at the software’s efficacy in the treatment of 50 patients, which yielded a mean minimum ablative margin of 5.87mm and 2.2mm in the experimental arm (n=24) versus the control arm (n=26), respectively.
The presenter concluded that “intraprocedural use of [the software does] significantly [improve] minimum ablative margin”.
November 2022 | Issue888 CIRSE 2022
FIRST@CIRSE
Insufficient minimum ablation margin has been linked to treatment failure and local tumour progression.”
CIRSE audience privy to latest data on femoroand infrapopliteal treatments and vascular closure
CIRSE hosted another session of ‘firsts’—on data from studies of the latest in arterial interventions. Among this set of presentations were those of positive five-year effectiveness and safety results of femoropopliteal angioplasty with a paclitaxel-coated balloon catheter; 30-day safety data from a study of a “[responsive]” new self-expandable nitinol stent in femoropopliteal lesion treatment; and some “successful” results from a prospective registry assessing safety and efficacy using a vascular closure device for percutaneous lower limb endovascular procedures.
Five-year femoropopliteal angioplasty data
Ulf Teichgräber (Jena University Hospital, Jena, Germany) presented the long-term results of the EffPac trial (iVascular), which demonstrated that the paclitaxel-coated Luminor 35 balloon catheter is a “sustainably efficacious treatment approach” for patients with medium-length femoropopliteal lesions, as seen at five-year follow-up.
As the audience learned, the EffPac trial was a prospective, multicentre, randomised controlled trial (RCT) of 171 patients of Rutherford category 2–4 with medium-length femoropopliteal lesions. Patients received angioplasty using Luminor 35 (n=85) or balloon angioplasty; n=86) to assess the primary endpoint of safety and effectiveness of the former treatment method.
The secondary endpoints at five years included primary patency, freedom from clinically driven target lesion revascularisation (CD-TLR), and clinical improvement, Teichgräber noted.
Regarding the five-year outcomes, primary patency was 61.4% after treatment with Luminor and 53.5% after balloon angioplasty (log-rank p=0.040). Freedom from TLR was 82.1% and 73.7%, respectively (log-rank p=0.050). Incidence of primary clinical improvement was “similar between groups”, at (61% DCB vs. 64% POBA, p=0.94).
In conclusion, Teichgräber could declare that the EffPac trial “showed a sustained superior incidence of primary patency” with the Luminor 35 angioplasty compared to balloon angioplasty out to five years. No safety signal occurred and while freedom from TLR was reduced in the former group, at five years, this was no longer statistically significant. Clinical improvement in both groups


“remained stable” throughout the five years and there was no difference in all-cause mortality between both groups. Therefore, Teichgräber summarised, “Luminor 35 angioplasty is a sustainably efficacious treatment approach.”
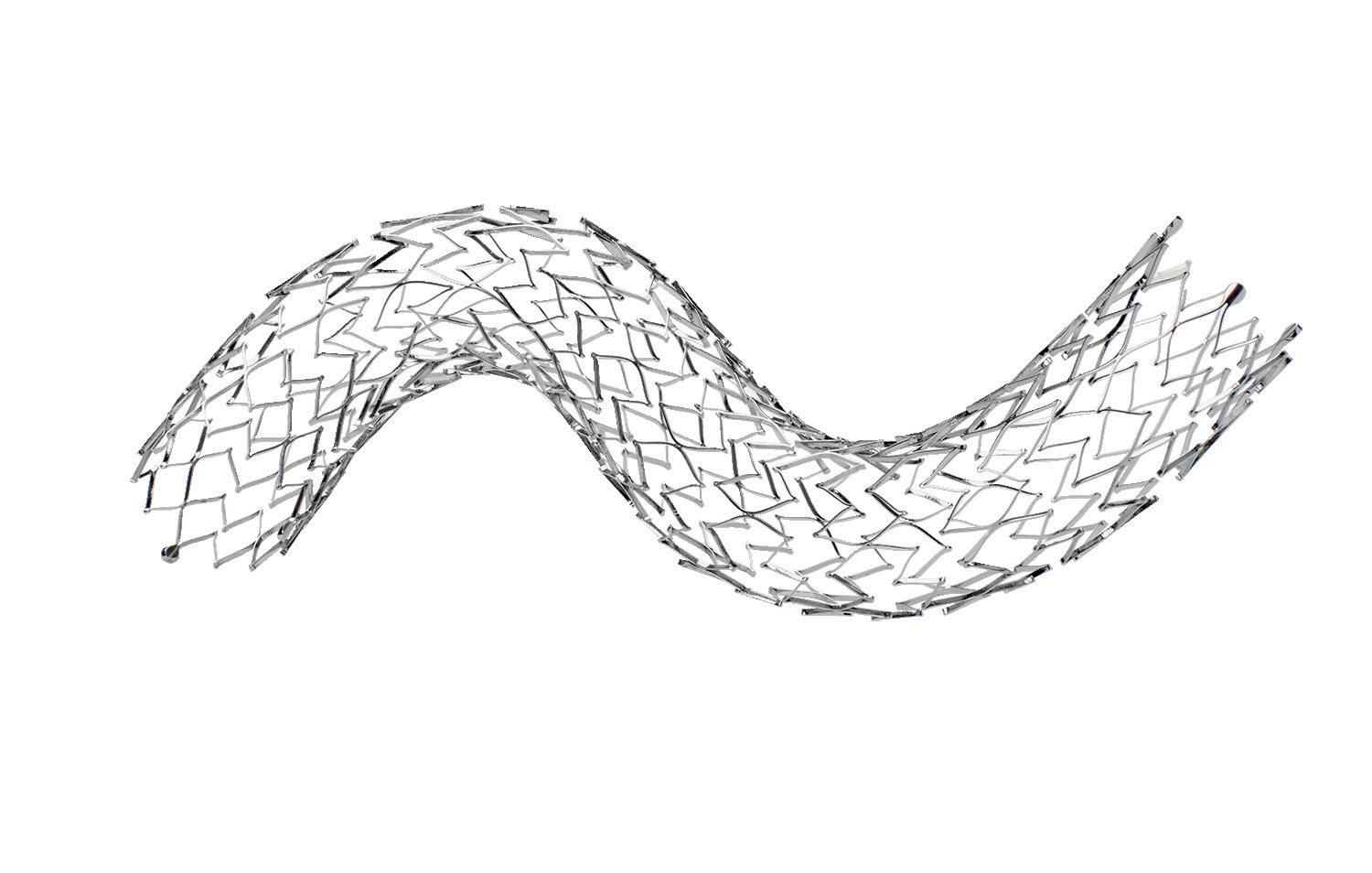
Preliminary results for femoropopliteal stent Koen Deloose (AZ Sint BlasiusDendermonde, Dendermonde, Belgium) shared the” 30-day safety results of PRIZER —a prospective, single-arm, multicentre study, assessing the safety and effectiveness of percutaneous treatment of femoropopliteal lesions with the Renzan stent (Terumo) in a total sample of 135 patients.

The trial of the “self-expandable interwoven nitinol dual-layer micromesh stent”, as Deloose described, evaluated 60 patients of Rutherford category 2–5 to obtain preliminary results. These were, “promising” with regard to safety profile, the presenter relayed, proceeding to define the safety endpoint—a composite of absence of death, TLR and index limb amputation. This was achieved in 58 (97%) patients and the single death that occurred was unrelated to the study, Deloose elaborated.
The presenter’s take-home messages included that “the interwoven Renzan stent responds perfectly well on our current expectations”, with a “clear functional improvement” seen in the aforementioned preliminary results at 30 days compared to at baseline.
Conclusions from vascular closure device registry
Delegates then learned of results of a prospective, multicentre, observational registry—FemoSeal CLOSE—which demonstrated the FemoSeal (Terumo)
vascular closure device’s safety and effectiveness when used following lower limb arterial endovascular procedures. Yann Gouëffic (Groupe Hospitalier Paris Saint-Joseph, Paris, France) presented, first explaining that “FemoSeal is an extravascular bioabsorbable polymer plug-based vascular closure device” intended to “achieve haemostasis by mechanically sealing the arteriotomy [from devices up to 7Fr] between two polymer bioabsorable discs”.
Gouëffic specified that 230 patients were enrolled in the trial and that “cessation of arterial bleeding achieved in interventional unit without any adjunctive treatment” constitutes the primary effectiveness endpoint. The primary safety endpoint, the presenter added, is freedom from any major vascular complication in the six hours immediately following the procedure. Minor access site complications and major complications out to 30 days are the secondary safety endpoints.
The study also collected data about time to haemostasis, ambulation and discharge, Gouëffic supplemented, with quality-of-life being assessed with the QoL EQ-5D-3L questionnaire, given at baseline, before discharge and at 30-day follow-up.
“Regarding the primary safety endpoint, freedom from access site-

related major complications attributable to FemoSeal within six hours postdevice deployment was achieved in 95% of patients [n=215],” the presenter declared. “Successful puncture site haemostasis was achieved in 96% of the cases [n=219]”, and the figure for combined safety and efficacy was 95%.
Gouëffic concluded by labelling Femoseal a “safe and efficient vascular closure device” that “allows a short time to ambulation and haemostasis”.
Data updates for temporary nitinol stent plus drugcoated balloon in lower extremities
Marianne Brodmann (University of Graz, Graz, Austria) updated on the DEEPER LIMUS trial, which evaluated the safety of the Temporary Spur stent system (ReFlow Medical) when used alongside a sirolimus-coated balloon. It is a prospective, non-randomised, single-centre, single-arm pilot study, Brodmann also detailed, and there are “promising” primary and secondary endpoint data.
As rationale behind the study, the presenter recounted that “paclitaxelcoated devices were thought to be a promising solution to treat the high rates of morbidity and mortality associated with critical limb-threatening ischaemia (CLTI), but these have been called into question due to evidence suggesting increased mortality risk with their use in the lower extremities”. However, sirolimus-coated balloons may have less effective drug transfer.
The Temporary Spur Stent System may promote better drug uptake when used in conjunction with drug-coated devices.
The presenter then described the “self-expanding nitinol stent with an integrated balloon that is deployable and retrievable” that allows for “controlled penetration of plaque, calcium and the arterial wall, improving acute luminal gain and allowing better drug uptake”.
Brodmann then spoke to the primary safety endpoint, a composite of allcause mortality, major amputation and CD-TLR . This was calculated based on in-person patients visits in the six months post-procedure. This composite figure, calculable for 20 patients, Brodmann specified, was 15% (n=3).
One of the secondary endpoints was major adverse limb events of the target limb at six and 12 months, for which the results were 95% of 20 patients (n=19) and 93.8% of 16 patients (n=15). Primary patency by duplex ultrasound at six months is 85% (17/20), and is 82.3% (14/17) by angiogram at six months, with good correlation between the ultrasound and angiogram findings.
Brodmann’s conclusion was that the clinical data from DEEPER LIMUS are “promising”, as they show that the Temporary Spur stent system “may reduce vessel recoil, increase luminal gain, reduce dissection, and it allows continuous flow during treatment”.
Issue88 | November 2022 9CIRSE 2022
Ulf Teichgräber
Marianne Brodmann
Yann Gouëffic
Koen Deloose
SAVAL trial finds no gains with custom drug-eluting stents in PAD below the knee
At the Cardiovascular and Interventional Radiological Society of Europe (CIRSE) 2022 annual meeting (10–14 September, Barcelona, Spain), Hans van Overhagen (Haga Teaching Hospital, Den Haag, The Netherlands), as European principal investigator, presented the primary results of the SAVAL trial.
COMPARING THE SAVAL DRUG-ELUTING stent (DES) below-the-knee (BTK) vascular stent system (Boston Scientific) and percutaneous transluminal angioplasty (PTA) in the infrapopliteal lesions of chronic limb-threatening ischaemia (CLTI) patients, the trial failed to meet its primary effectiveness and safety endpoints.
The presenter explained that the SAVAL trial is a prospective, multicentre, randomised superiority trial of patients with symptomatic infrapopliteal artery lesions and Rutherford category 4–5 CLTI. The patients were assigned 2:1 to treatment with Saval DES or PTA.
Providing further details of the study, Van Overhagen stated that a total of 201 patients were enrolled and randomly assigned to treatment (n=130 DES, n=71 PTA) at 39 study centres in Belgium, France, The Netherlands, the USA, and Japan.
In terms of primary results, Van Overhagen reported a high technical success rate of 100% in the DES group and 98.7% in the PTA group.
However, “the primary effectiveness endpoint of superior 12-month primary patency was not met,” the
presenter relayed—the figure was 68% in the DES group and 71% in the PTA group. “The primary safety endpoint of non-inferior 12-month major adverse event (MAE)-free rate was [also] not met,” Van Overhagen supplemented, citing the results of 91.6% and 95.3% respectively for the DES and PTA groups, while freedom from all-cause mortality was 92.2% versus 89.9%.
Van Overhagen shared the rationale behind conducting the study: CLTI is a condition with “few effective endovascular options for infrapopliteal artery revascularisation” and DESs have yielded positive results in previous studies. This reflects what Van Overhagen highlighted in an earlier presentation he gave on DESs— both an endovascular approach and revascularisation are key to optimal treatment of CLTI.
In view of the primary results, Van Overhagen told delegates that “patient
Preliminary MOTIV BTK outcomes positive for bioresorbable scaffold use in below-the-knee lesions
Thomas Rand (Klinik Florisdorf, Vienna, Austria) recently presented on the preliminary results to 12 months of the Motiv bioresorbable scaffold (Reva Medical) postmarket trial at the recent Cardiovascular and Interventional Radiological Society of Europe (CIRSE) 2022 annual meeting (10–14 September, Barcelona, Spain). With the objective of evaluating safety and efficacy for the treatment of patients with rest pain or minor tissue loss due to the presence of lesions of a maximum length of 100mm at the level of the below-the-knee (BTK) arteries”, Rand shared in a FIRST@CIRSE session that at 12 months, primary patency—the efficacy endpoint—was 88%, and the technical success rate, 99%.
The MOTIV BTK study is a prospective, single-arm, multicentre trial, in which 58 patients with BTK artery lesions of a maximum length of 100mm have been enrolled. The study is being carried out on 60 limbs with 76 Motiv scaffolds, Rand specified. The Motiv scaffold has been approved for use in Europe since 2018 when, according to Reva Medical, the device became the first bioresorbable scaffold to receive CE mark for use below the knee.
“The special thing with the Motiv scaffold,” Rand opined, “is that it is sirolimus-eluting and bioresorbable,
so you have two good things.” The presenter noted that this is in keeping with the ‘leave nothing behind’ concept. “The scaffold itself is made from TyroCore, which is derived from tyrosine amino acid,” Rand then detailed, and this design is responsible for “low inflammation and irritation during degradation and [no calcification].” The thin struts “have been evaluated as best-in-class,” Rand supplemented.
Moving on to address the preliminary study outcomes, Rand described them as “really very good, [with] a 99% technical success in all patients.”
follow-up will continue through three years in-office with vital status assessment through five years, as specified in the study protocol […] We believe that given the impact of CLTI on limb and life, continued innovation to provide minimally invasive treatments is needed”.
In another session, Van Overhagen presented on the devices currently available and evidence to support the use of DESs specifically.
He began one presentation by underlining that the “cornerstone” of CLTI is revascularisation—”we try to get unobstructed blood flow all the way into the foot and avoid amputation”. The presenter went on to acknowledge that “we all know that endovascular treatment is less invasive. This is why, where possible, we use an endovascular approach”.
The presenter then proceeded to explain the origin of drug-eluting balloons (DEB) and DESs: “[they] have been introduced in order to try to reduce restenosis […] we try to diminish the amount of intimal hyperplasia”. The Dutch PADI trial, for which Van Overhagen was principal investigator, compared PTA with bare metal stents (BMS) to DES and, at two-year follow-up, there were almost twice as many major amputations in the former group, a trend which was also observed at five years.
“Our initial conclusions were that DES BTK in CLTI achieved improved patency, a trend towards fewer major amputations [and indicated] a need for dedicated self-expandable and longer stents,” Van Overhagen reported.
Further analysis out to ten years has also shown DES BTK to be safe and cost-effective, the presenter concluded.
Primary patency at six months was 90%, and the 12-month preliminary result 88%. The limb salvage rate until now at 12 months, as conveyed by Rand was 97%, and the 14% (n=8) death rate was entirely unrelated to the device or procedure. The freedom from clinically driven target lesion revascularisation (CD-TLR) was “a very nice” 98.3% at 12 months, Rand also underlined, with a “decline in Rutherford stages observed during this time.”
“As a conclusion, already, we can say with the Motiv scaffold we had excellent tracking and visibility and a problem-free delivery.” Rand proceeded to emphasise the scaffold’s ease of use and the 90% vessel patency rate, before sharing that the CD-TLR and limb salvage rates remained stable from six to 12 months.
“The major concept behind this study, which I really like, is the ‘nothing left behind’ concept, and this is really fulfilled in this study,” Rand finished by informing delegates.
Enrolment in MOTIV IDE clinical trial begins Following this presentation, Reva Medical announced that enrolment in the MOTIV pivotal trial has been initiated at clinical centres in both the USA and Europe. The study, which is being conducted under a US Food and Drug Administration (FDA) investigational device exemption (IDE), will evaluate the use of the Motiv sirolimus-eluting bioresorbable vascular scaffold for treatment in patients suffering from chronic limbthreatening ischaemia (CLTI).
The MOTIV study is a global, randomised controlled trial (RCT) that was designed to evaluate the safety and efficacy of the Motiv scaffold for the treatment of infrapopliteal lesions in patients with CLTI by randomised comparison with standard balloon angioplasty.
The study, led by coprincipal investigators Ehrin Armstrong (Adventist Health, St Helena, USA) and Andrej Schmidt (Universitätsklinikum Leipzig, Leipzig, Germany) will follow up to 292 patients at approximately 35 clinical centres in the USA and Europe.
November 2022 | Issue8810 Below-The-Knee Interventions
PERIPHERAL
The primary effectiveness endpoint of superior 12-month primary patency was not met.
68
%
71
%
in the DES group and
The figure was in the PTA group.
The special thing with the Motiv scaffold is that it is sirolimuseluting and bioresorbable, so you have two good things.”
Josef Roesch Lecture evidences need to “build on” interest in paediatric IR
Paediatric interventional radiologist Alex Barnacle (Great Ormond Street Hospital, London, UK) gave the Josef Roesch Lecture at the Cardiovascular and Interventional Radiological Society of Europe 2022 meeting (CIRSE; 10–14 September, Barcelona, Spain), choosing to present on the subject of ‘Developing excellence in interventional radiology (IR) for our youngest patients’. The presenter used various case examples to demonstrate to non-paediatric interventionalists that they “still need to think about [paediatric IR]—children grow up and graduate into adult practice”. A take-home message from Barnacle was how cross-specialty collaboration on issues such as establishing standards of practice, especially with the wider IR community, will help paediatric IR grow and “[change lives]”.
Barnacle’s presentation began with the story of a patient of hers, who was the first to receive orbital sclerotherapy at Great Ormond Street Hospital. Highlighting the life-changing impact of the treatment on her patient, Barnacle also underlined the importance of her network in providing the care her patient required—“[David Lord] talked me through [the procedure] over the telephone and we did [it].” This success is proof of the value of tapping into “the very small pool of expertise around the world”—Lord is based in Sydney, Australia—however “if we do not know each other, we cannot share our expertise and data,” Barnacle acknowledged. How crucial cultivating a network within paediatric IR is, is complemented by the need to communicate and work together with other specialties so that they better recognise where paediatric IR can play a key role in patient care.
“Just as with IR […] paediatric IR is massively under-recognised by other specialties,” Barnacle stated, going on
to explain the impact this has—“we get late referrals because other teams do not know what we can do”. An example of where increased awareness and implementation of paediatric IR expertise could make a difference to current practice is, as illustrated by Barnacle, central venous access. “We all know that children should not need to be going through repeated painful, distressing cannulations […] that will mentally and physically scar them and their families for the rest of their lives.” What is a “bread and butter” procedure for a paediatric interventional radiologist will enable their patients to “get on with dealing with [everything else] that they need to, without having to think about those repeated cannulations.”
In contrast to the day-to-day roles paediatric interventional radiologists can play, such as by providing central venous access, Barnacle touched on the “supportive care” that they can give patients with rarer conditions, including those with rapidly involuting congenital
Six-month data from the Surmodics SWING first-in-human trial presented at AMP Europe
Six-month data from the Surmodics SWING first-in-human (FIH) study of the company’s Sundance sirolimus drug-coated balloon (DCB) were shared at the 2022 Amputation Prevention Symposium (AMP; 9–11 October, Lugano, Switzerland).
THE SWING STUDY IS A prospective, multicentre, single-arm feasibility study to evaluate the safety and performance of the Sundance sirolimus DCB when used to treat occlusive disease of the infrapopliteal arteries.
The study’s primary safety endpoint data showed no perioperative deaths or major amputations at 30 days and just one major reintervention was reported among the 35 trial subjects, a Surmodics press release reports. Data for the primary efficacy endpoint
show a late lumen loss (LLL) of 1mm (±0.79mm) across 35 lesions at six months, indicating that the large luminal gain achieved immediately after the procedure was sustained six months post-treatment.
“At six months we observed a consistent improvement in Rutherford category and functional measures, as well as an excellent primary patency of 88.5%, which compares favourably to other DCBs used in the infrapopliteal circulation,” said SWING trial co-lead investigator Ramon Varcoe, vascular
haemangioma, and those who have swallowed button batteries, and may require dozens of interventions to “get through”.
Protocols and guidelines are also a factor in limiting the extent to which paediatric IR can fulfil its potential in such cases, as Barnacle also flagged. The presenter illustrated her point with a trauma case example, which saw the 15-year-old patient requiring a partial splenic embolization bypass a major trauma centre, as protocol would not allow (non-paediatric) interventional radiologists to carry out the treatment.
“[It] just feels wrong”, Barnacle admitted, before suggesting that, as with the “limited” existing standards of practice for paediatric IR, “we need more”. As a potential solution to the paucity of paediatric IR-specific practice guidelines, the presenter offered the approach of adding paragraphs to existing guidelines on how to nuance established adult practice for children.
A further barrier to widespread recourse to paediatric IR that Barnacle brought to the audience’s attention was the increase in paediatric contraindications for some devices—“we have had to change the inferior vena cava [IVC] filter we use,” the presenter lamented. This is symptomatic of a “small toolbox that is being emptied very quickly,” which, in addition to affecting paediatric IR practice, also has a knock-on effect for training, as device companies feel obliged to pull out of events such as the hands-on device training offered at meetings.
Nevertheless, Barnacle ended on a positive note, taking stock of the increasing interest in paediatric IR, of which there is ample
evidence. The scope of the paediatric IR programme at CIRSE is one such example, including a sell-out handson session in spite of one company pulling out for the aforementioned reason of contraindications. “Things are changing,” according to the presenter, proceeding to celebrate the fact that CVIR Endovascular’s most downloaded paper of the past year was on paediatric IR, and how the remote Society of Paediatric Interventional Radiology
surgeon at the Prince of Wales Hospital and associate professor of vascular surgery at the University of New South Wales (Sydney, Australia).


The SWING trial enrolled patients with stenotic or occluded lesions of the infrapopliteal arteries, a reference vessel diameter (RVD) of 2–4mm, and a total lesion length of ≤230mm for treatment with the Sundance sirolimus DCB at eight sites in Australia, New Zealand, and multiple locations in Europe. They will be followed for 36 months following the index procedure.
“The novel coating on the Sundance sirolimus DCB was evaluated in a challenging, predominantly CLTI
annual meeting in 2020 saw attendees from 43 different countries.

Key now, Barnacle believes, is to “build on this interest”, which, she believes, extends to trainees looking for more of a “human side” to their work and “greater job satisfaction”— requirements that, she opines, being a paediatric IR can meet. As relayed throughout her presentation, efforts to grow paediatric IR, and interest and awareness of it, can take the form of establishing clearer guidelines and protocols, drawing on professional networks to aid innovation and optimal patient care, and working with colleagues in other specialties “so that children get referred to us sooner—this is better than picking up the pieces,” Barnacle concluded.
“[After all], we are all here because we believe that minimally invasive procedures are the way to go.”
[chronic limb-threatening ischaemia] population with a high proportion of diabetes and moderate-severe calcification,” said trial co-lead investigator Andrew Holden, director of interventional radiology at the University of Auckland (Auckland, New Zealand). “This first-in-human study demonstrates that the Sundance sirolimus DCB could be a safe and promising treatment for occlusive disease of the infrapopliteal arteries.”
The Sundance sirolimus DCB utilises a “next-generation” coating technology consisting of microcrystalline sirolimus and a proprietary excipient to maximise drug transfer, which, according to Surmodics, enhances sirolimus delivery and sustains therapeutic levels in the artery.
In a press release, Surmodics notes that sirolimus is a potent anti-inflammatory and anti-proliferative compound, and has been used successfully in coronary drugeluting stents.
Issue88 | November 2022 11Paediatric IR
We are all here because we believe that minimally invasive procedures are the way to go.”
Alex Barnacle
Andrew Holden Ramon Varcoe
CIRSE hears how liver venous deprivation is “pushing limits”
Both the Andreas Gruentzig Lecture at this year’s Cardiovascular and Interventional Radiological Society of Europe meeting (CIRSE; 10–14 September, Barcelona, Spain) and a presentation of interim data at the ‘New Frontiers’ FIRST@CIRSE session informed delegates of the innovative future liver remnant (FLR) hypertrophy technique, liver venous deprivation (LVD). As Remon Korenblik (Maastricht University Medical Center, Maastricht, The Netherlands) and Boris Guiu (Hôpital Saint-Eloi, Montpellier, France) explained in the context of the data presentation and lecture respectively, LVD involves combining hepatic and portal vein embolization (HVE/PVE) to cause FLR growth. Guiu referred to the ongoing DRAGON 1 trial on which Korenblik presented as an example of “pushing the limits” and a key takeaway message from these presentations was that there is a “place [for] LVD in the future”, and that further studies will “define” exactly what that is.
DRAGON 1, as Korenblik conveyed to attendees, is a multinational, multicentre, prospective and single-arm trial, of which the purpose is to “assess training, implementation, safety and feasibility of combined PVE and HVE to accelerate FLR hypertrophy in patients with borderline resectable colorectal cancer liver metastases [CRLM]”.
Korenblik alluded to the importance of the trial—“the cornerstone [of CRLM] treatment is resection” but in cases of “insufficient FLR” this is not an option, hence, investigating whether the FLR can be increased in size, so that resection is possible.
The primary endpoint for the DRAGON 1 trial is “a composite of the safety of combined PVE and HVE, 90-day mortality, and one-year accrual monitoring of each participating centre.”
Secondary endpoints feature feasibility of resection, FLR hypertrophy, overall survival and disease-free survival.
The interim results from the trial so far, which Korenblik shared with delegates, seem to demonstrate that combined HVE and PVE “induces fast and extensive FLR hypertrophy and leads to high rates of resectability”. The definitive analyses after the DRAGON 1 trial completion are needed to confirm
these assumptions. “We also found this in a recent pooled analysis, which will be published shortly,” Korenblik reported, “in which we saw statistically significant higher resectability rates after PVE/ HVE compared to PVE alone.”
Next for the DRAGON Initiative, which is behind a series of trials to determine the safety and efficacy of combined PVE and HVE, is the beginning of recruitment for DRAGON 2, Korenblik asserted. This study “will investigate the efficacy and survival of patients after PVE alone compared to PVE and HVE combined in a multinational, multicentre randomised controlled trial”.
yielding “attractive initial results”, cohort studies have confirmed the technique’s outperformance of any other preparation technique, including ALPPS (associating liver partition and portal vein ligation for staged hepatectomy)—historically regarded as “the most efficient technique in terms of volumetric gain [in the FLR]”—or even hepatectomy, in terms of functional gain. Functional increase, Guiu duly noted, is, in addition to volumetric gain, “very important” in the context of liver preparation for hepatectomy.
“Now we are five or six years on [from the first study], we have now several [more…] from different teams,” Guiu elaborated for attendees. “All but one is showing that LVD outperforms PVE in terms of volumetric gain”, and the presenter went on to acknowledge that there is evidence that LVD also leads to fewer post-resection complications.
With “enthusiasm sparked” by the aforementioned findings, the next step, Guiu averred, is to go about obtaining multicentre, prospective study data. An example the presenter gave is the French HYPERLIV-01 randomised controlled trial comparing PVE with LVD, using glue in the hepatic veins in addition to proximal plugs. As Guiu noted, the trial “has already completed more than two-thirds of its accrual in 11 centres,” and the DRAGON Initiative will also provide key evidence of the value of performing LVD, through its series of trials, as relayed by Korenblik. “There is probably a place for LVD but we need definitely more data […] the objective is to define more precisely the place of this technique,” was Guiu’s conclusion regarding LVD versus PVE for FLR hypertrophy.
The presenter’s final remarks were on innovation within clinical practice more broadly and how to achieve “wide acceptance” of a new technique, such
ABRE clinical study 36-month data show sustained effectiveness of Abre venous selfexpanding stent system
Medtronic has announced the 36-month final results from the ABRE clinical study. The purpose of the ABRE clinical study was to evaluate the safety and effectiveness of the company’s Abre venous self-expanding stent system, intended for the treatment of symptomatic iliofemoral venous outflow obstruction.
THE STUDY RESULTS WERE presented in a late-breaking clinical trial session at the American Vein and Lymphatic Society (AVLS) 2022 annual meeting (13–16 October, New Orleans, USA). Stephen Black (Guy’s and St Thomas’ Hospital, London, UK), co-principal investigator for the ABRE study, presented the data.
“The 36-month ABRE data have continued to demonstrate the long-term durability of interventions in patients suffering from deep venous disease,” Black said. “The results show a sustained

result in both technical aspects, but more importantly, in patient outcomes.”
The ABRE study included a complex set of patients. Within this patient group, 47.5% of patients were categorised as having post-thrombotic syndrome (PTS) and 35.8% of PTS patients presented with a complete venous occlusion confirmed by the core lab. The mean lesion length of subjects was 112.4mm and 44% of patients had stents that extended below the inguinal ligament.
Of note, the study results showed: Overall, effectiveness following
measured by EQ-5D and VEINESQoL quality of life.
Sustained and clinically meaningful improvements through 36 months as measured by Villalta and VCSS venous functional assessments indicate less severity of PTS disease and venous disease overall.
November 2022 | Issue8812 Venous Updates
Boris Guiu in both technical aspects, but more importantly, in patient outcomes.”
Tech advancements set to continue to enhance IR practice
The Cardiovascular and Interventional Radiological Society of Europe (CIRSE) 2022 annual meeting (10–14 September, Barcelona, Spain) saw presenters explore artificial intelligence (AI), its current role in interventional radiology (IR), and how the two will evolve together to shape innovative practice in a session named “IR: The most tech of the medical specialties”. Among the key takeaways was reassurance that AI will not “replace” human interventional radiologists, rather that it is a question of understanding how AI can be useful in IR and combining it with the knowhow and abilities of interventional radiologists to achieve ‘hybrid intelligence’.
DISCUSSION OF VIRTUAL REALITY (VR) and augmented reality (AR) also featured in the session, as well as wider commentary on what it takes to become a technological innovator in the IR space.
AI can lead to “truly patientfocused, individualised medicine”
The first speaker, Fernando Gómez Muñoz (Netherlands Cancer Institute, Amsterdam, The Netherlands; Hospital Clinic and Hospital Sant Joan de Déu, Barcelona, Spain), provided an overview of how AI is currently being applied in IR and how he predicts this landscape will look in the coming years. Referring to the results for ‘artificial intelligence interventional radiology’ that a pubmed. gov search yields, the presenter demonstrated that AI in IR has been a topic of growing research focus—in 2016 there were 16 publications on the subject, and in 2021, 290.
Defining AI as “a combination of algorithms to provide machines with the capability to solve problems in a similar way to humans”, and machine learning as “a subtype of AI that uses computer algorithms to build predictive models,”
Gómez Muñoz gave the example of how the latter can be used to predict type 2 endoleaks. The importance of this capability is, he shared with delegates, that “if you can predict [these], you can embolize the vessels that may cause the endoleak beforehand, avoiding a more complex procedure later, or an aneurysm rupture, which can happen if there is no adequate follow-up”.
Among the other applications of AI is in predicting local tumour progression post-thermal ablation, classifying peripheral arterial disease (PAD) in conjunction with computed tomography (CT) angiography, 3D planning for ablation procedures, as well as intraprocedural verification. The presenter then spoke to the advantages that AI offers for limiting unnecessary radiation exposure, such as during fluoroscopy-guided endoscopic procedures. Gómez Muñoz relayed his experience using verification software after ablation of liver tumours. It can “lead to early retreatment in some situations”, he explained, and can
“dramatically reduce the recurrence rate of colorectal liver metastases”.
A further take-home message from Gómez Muñoz’s presentation was that he sees haptic perception in robots as a key area of future development with relevance to IR procedures. “Pressure, vibration, temperature and viscosity” are among the types of perception that the presenter hopes to see in robots used in IR settings, bringing the interventional radiologists who will make use of these innovations in a position to practise, increasingly, “truly patient-focused, individualised medicine”.
VR: the potential to reduce radiation exposure
Bradford Wood (National Institutes of Health Center for Interventional Oncology, Bethesda, USA) focused on VR in IR now, and its future directions.
An important message he had for delegates was regarding the precise ways in which VR can benefit IR, which “can be poor” when reproducibility is concerned: by standardising practice and “equalising” the care patients receive.
VR also has the potential to reduce interventional radiologists’ and patients’ radiation exposure through providing real-time mapping during cases, such as in conjunction with cone beam CT, to increase accuracy. This will also, in turn,
reduce procedural complications and the time the given procedure takes. Related to this, VR can track patient movements so registration—the matching of images to the patient—remains accurate throughout the procedure.
However, Wood admitted that there are hurdles to adopting VR technologies in an IR practice. For example, goggles—a common means of accessing VR for use in a procedure—can bring on cybersickness, which discourages its use. However, handheld and projectorbased tools, and even smartphone apps, can be a way around this ergonomic issue.
Cost-effectiveness, Wood explained, is another barrier to healthcare providers incorporating VR into IR procedures, even though the benefits of increased accuracy and therefore reduced radiation exposure and intraprocedural complications, as Gómez Muñoz outlined, are highly valuable.
Technological innovations at lower cost
Luigi Solbiati (Humanitas University, Milan, Italy) gave his presentation on technological innovations in IR, what it takes to get them off the ground, and the obstacles that innovators can come up against in trying to do so. Solbiati also covered the benefits and pitfalls involved in developing these types of innovations and what he foresees the next disruptive IR technologies being. In terms of the latter, Solbiati cited histotripsy as already showing significant “world-changing” potential as a non-invasive, non-thermal, nonionising procedure, where high-intensity focused ultrasound (HIFU) has been less successful.
Image fusion technology, which came into being around 20 years ago, was an example Solbiati gave of game-changing technology innovation in IR—“nowadays, we have wonderful rooms where you can do [ultrasound, angiography, CT and cone beam CT] together”.
However, he was keen to acknowledge the lack of accessibility of these types of advancements throughout the world, due to the cost involved. Therefore, Solbiati concluded, “we should find alternative solutions”.
Among these, he listed “the fusion of real-time ultrasound (US), contrastenhanced CT and positron emission tomography (PET) in the US room,” which he qualified by stating that it is “a simple and significantly lower-cost alternative to interventional PET-CT rooms.”
The presenter also opined that robots that facilitate remote needle placement will be a crucial future development in AI for IR, and that ablation confirmation software that should become mandatory after every ablation.
Solbiati himself, as highlighted by his co-presenters, has successfully created technology that can thermally ablate liver tumours using AR alone, and no radiation. One of the ideas behind this is to solve the aforementioned issue of the high cost associated with installing sophisticated multifunction CT suites.
To round off the session, moderator Laetitia Saccenti (Hôpital Paris Saint-Joseph, Paris, France) asked a question on behalf of those who may be concerned about AI capabilities exceeding those of interventional radiologists, and thus reducing or eliminating the scope of human practitioners’ roles in IR. “You cannot change the way things are going, you just have to surf the wave […] the more you learn, the more useful [a tool] it will be,” Gómez Muñoz answered.
Wood reiterated that “[AI and VR] will not replace” interventional radiologists. Certainly, a key takeaway from all three speakers was that technology will evolve to complement the work of interventional radiologists; enhancing what they are able to achieve as opposed to rendering their role obsolete.


Issue88 | November 2022 13Tech in IR
Luigi Solbiati
Fernando Gómez Muñoz
You cannot change the way things are going, you just have to surf the wave.”
Dimitrios Filippiadis
“The spine is an area where interventional radiologists play a crucial role in both diagnosis and therapeutic management of a variety of pathologies”. Dimitrios Filippiadis is associate professor of diagnostic and interventional radiology (IR) at the National and Kapodistrian University of Athens (Athens, Greece) whose practice centres around musculoskeletal (MSK) interventions and diagnostics, and interventional oncology (IO) and cancer pain management. Beyond this, he is passionate about IR education, which has seen him, this year, take up the position of the Cardiovascular and Interventional Radiological Society of Europe (CIRSE) Online Education Committee chair. From his research on discomanometry, to personal experience at the forefront of adopting ablation procedures within Greece, Filippiadis speaks to Interventional News about the “intrinsic rewards” and “lifelong memories” that being an interventional radiologist has given him in his decorated career thus far.
What attracted you to a career in IR?
When I started my residency in diagnostic radiology, I had a lot of second thoughts about sitting in front of a computer monitor dictating reports. Then, a fellow resident came to me and suggested I register for a postgraduate course in IR, which was organised by Professor Dimitrios Kelekis in Greece. From the introductory courses onwards, I knew that this was the clinical career path I wanted to follow. Some years later, a visit to Strasbourg on a CIRSE grant made me realise that interventional oncology (IO) and pain management would be my specialist practice.
Who are, or were, your mentors?
I was fortunate enough to have had wonderful mentors early on in, and throughout, my career. During my residency, Alexis Kelekis introduced me to spinal and MSK procedures and influenced me greatly. Elias Brountzos taught me that providing patient care is one aspect of our work, with the other being to bolster the IR community by volunteering our time and expertise to help our specialty to flourish further. Nikolaos Kelekis gave me the opportunity to work almost exclusively in the field of ablation and I will always be grateful to him for this chance. Last but not least, even though I have never worked with him, Loukas Thanos, a Greek pioneer in the field of ablation, has had a great influence on my career.
Could you describe a particularly memorable case of yours?
I will never forget the first time I treated a paediatric cancer patient. He was 16 years old with a history of right paraganglioma and right nephrectomy due to renal cell carcinoma (RCC) and presented with an endophytic RCC lesion in the lower pole of his left kidney. The stress obtaining the parents’ consent and preparing for the ablation was unbearable, at least for me. The night before the ablation, I was not able to sleep, imagining only the worst-case scenario. However, after the procedure, when I informed the parents that everything had run smoothly, that we had totally ablated the tumour without any adverse events, they started crying. It is a moment I will never forget.
What led you to pursue your PhD in quantitative discomanometry? How is it complementary/relevant to your role as an interventional radiologist?
The spine is an area where interventional radiologists play a crucial role in both diagnosis and therapeutic management of a variety of pathologies. Specifically for intervertebral disc herniation, what I have always found fascinating is the fact that the success rate of percutaneous decompression techniques is around 80% no matter which technique you use. Discomanometry could serve as a diagnostic tool to escalate patients,
leading to an improved patient-specific, or even better, hernia-specific, approach.
Your paper on pain management in cancer patients, recently published in Current Oncology Reports, is one of many you have authored on the subject—what innovations do you see on the horizon in this area?
Management of cancer pain is one of the most interesting topics in my everyday clinical practice. We have published numerous papers on the topic, but myself and the rest of the co-authors are actually particularly proud of this publication, which has been included in the National Comprehensive Cancer Network 2021 guidelines for adult cancer pain. As far as innovations in the field of pain management are concerned, I am convinced that cryoneurolysis is the ideal technique for pain palliation, as it offers more confined and more organised nerve regeneration alongside pain reduction. Although, at present, there is no standardised ablation protocol, given the wide range of variables that affect intraprocedural temperature at the ablation site, a more palatable solution will be a new device with information-gathering capabilities, to form and perform individual cryoneurolysis protocols.
You were appointed to the position of associate professor of diagnostic and interventional radiology at the National University of Athens Medical School— what has changed the most about your practice since your early senior consultant days over a decade ago? Being an educator offers intrinsic rewards and brings with it lifelong memories. Providing real-life clinical experiences and context to medical students is an essential part of today’s medical education— whereas I had only very minimal obligations towards medical students and teaching when I started as a senior consultant. Integrating the role of medical students into the healthcare system provides added value, both to clinical care and medical education. You need to change your workflow in order to allow students to contribute before, during, and after visits, and to engage them holistically in patient care. Last but not least, you need to strike a balance between apprenticeship and an academic model, and choose which approach works best for whom.
You were at the forefront, at your centre, when it came to integrating microwave and navigation-guided ablation into IR services, yours being the first in Greece to adopt both procedures— why do you think it is important to lead the charge in adopting new techniques
and procedures?
New techniques and procedures go hand in hand with IR, which is a discipline born of innovation; adopting new technologies is essential for the growth and flourishing of our specialty. Early adoption results in improved efficacy, ability to offer what no one is offering at the moment, and empowering practice with new and improved systems that make for better services. From our first experience with microwaves in 2008 to today, it has been evident for us that this technology offers unique advantages and has a role in today’s ablation practice. Ideally, when it comes to locoregional therapies, we want to have all the ablation techniques available in our armoury and to be able to take a lesion-tailored approach. Application of navigation tools as well as simulation and verification software significantly contribute to standardisation of ablation; I strongly believe that in the near future, these
14 November 2022 | Issue88Profile
Andy Watt/NB Illustration
PROFILE
tools and software will be part of all interventional radiologists’ everyday practice. The tools will prove their value by allowing for better comparison of percutaneous ablation to surgical and radiation oncology.
In (also) becoming the first Greek hospital to enrol in the International Accreditation System for Interventional Oncology Services (IASIOS), what has the impact on your practice and patients been?
Even though the second department of radiology is in the process of acquiring the IASIOS accreditation, the benefits for patients and in terms of practice performance are more than evident. The whole process of patient care and treatment is improved. During the IASIOS accreditation process, we have analysed our service, improved its coordination and monitoring, and the end result is improved delivery of high-quality IO care, with the patient receiving the best possible treatment for an optimal, individual clinical outcome. This improvement has been throughout the department, affecting not only IO but all IR services.
You recently became the CIRSE Online Education Committee chairperson— what do you hope to do in this role that has not been done before?
Education extends beyond practical knowledge. Educated physicians develop thinking and skills, which help them make good decisions for the benefit of the patients. The Online Education Committee deals with the CIRSE Library, Academy and Webinars as well as with everything included in these three main pillars of virtual and online education provided by our scientific society. To leave your own footprint on this position I must admit is a very difficult task, since my predecessor Stefan Müller-Hülsbeck has done a superb job in organising almost everything from scratch. I am positive though, that along with my deputy chairperson Julien Garnon and all the members of the Committee, we will rise to the challenge and structure education in order to foster a love of learning among our IR community.
What are your hobbies and interests outside of medicine?
Before and during my medical studies, I worked as a DJ. What I have left from these days and nights are thousands of vinyl records and CDs of all kinds of music, which I love listening to in my free time. Apart from listening to music, I love reading books, especially historical novels (Bernard Cornwell, Wilbur Smith and Ken Follett are my favourite authors). My other main hobbies are playing basketball and swimming, especially on my beloved island of Lefkada where we have a beach house.
Current appointments
2022–present: Associate professor of diagnostic and interventional radiology, National and Kapodistrian University of Athens (Athens, Greece)
2022–present: Chairperson, CIRSE Online Education Committee
Past appointments
2009–2016: Senior consultant, IR, Second department of radiology, Attikon Medical School (Athens, Greece)
2016–2022: Assistant professor of diagnostic and interventional radiology, National and Kapodistrian University of Athens
Medical education

1992–1998: Medical degree, Charles University (Prague, Czech Republic)
2002–2009: Radiology specialty training, Oncologic Hospital of Athens (Athens, Greece)
2004–2006: Postgraduate course in IR, National University of Athens Medical School
2007–2012: PhD in quantitative discomanometry, National University of Athens Medical School
Society positions (selected)
CIRSE (Cardiovascular and Interventional Radiological Society of Europe)
SIO (Society of Interventional Oncology)
RSNA (Radiological Society of North America)
SIR (Society of Interventional Radiology)
15Issue88 | November 2022 Profile
SYMPOSIUM ON ENDOVASCULAR THERAPY
IN 2023, I’D LIKE TO
Discover best techniques and devices to treat cardiovascular disease.
Utilize multidisciplinary teams to improve patient outcomes of endovascular therapy.


Compare simple and complex arterial access during diverse endovascular procedures performed by worldrenowned specialists.
Access the most relevant and pertinent data that I can utilize in challenging situations in my practice.
CHECKED YES TO ANY/ALL OF THE ABOVE? JOIN US.
16 –19 JANUARY 2023 LOEWS MIAMI BEACH FLORIDA INTERNATIONAL
iset.org
Renal denervation back on track with studies adding “important data to the field”
More than eight years after results of the SYMPLICITY HTN-3 trial led the authors of a New England Journal of Medicine (NEJM) editorial to observe that the “renal denervation train” had reached a “grinding halt”, investigators have expressed renewed optimism that the procedure is back on track as a promising treatment option for hypertension.
This comes on the back of a release of data from two sham-controlled renal denervation trials at the 2022 Transcatheter Cardiovascular Therapeutics meeting (TCT; 16–19 September, Boston, USA), including long-term results from the SYMPLICITY HTN-3 trial, and primary results from the RADIANCE II trial—described as “important data for the field” by discussants in a late-breaking clinical science session at which the data were presented.
Deepak Bhatt (Brigham and Women’s Hospital Heart & Vascular Center and Harvard Medical School, Boston, USA), who presented the long-term findings from SYMPLICITY HTN-3, acknowledged in his presentation that at six months, though renal denervation using the Symplicity (Medtronic) radiofrequency renal denervation system had been shown to be safe, the trial’s efficacy endpoint was not met.
At TCT 2022, Bhatt shared new data from the trial, which enrolled a total of 535 patients with treatmentresistant hypertension from 88 centres across the USA, all of whom were randomised 2:1 to undergo renal denervation (364) with an early generation of the Symplicity system or a sham procedure (171). All patients received stable, maximum tolerated doses of three or more antihypertensive drugs. The latest analysis included 101 patients from the sham control arm who crossed over to receive renal denervation after six months.


Despite the trial’s primary endpoint failure at six months, the long-term data presented by Bhatt point towards significantly greater reductions in office systolic blood pressure in patients who had undergone renal denervation versus those receiving a sham procedure at one (-18.9mmHg vs. -6.3mmHg, p<0.0001), two (-24.1mmHg vs. -4.3mmHg, p<0.0001) and three (-26.4mmHg vs. -5.7mmHg, p<0.0001) years, while the number of antihypertensive drugs were shown to be similar between patients in each arm of the trial.
Noting that the earlier data from the trial should confer a degree of caution to the interpretation of the long-term findings, Bhatt concluded that the latest data support the notion that durable blood pressure reductions with radiofrequency renal denervation in the presence of maximal medical therapy are “safely achievable”.
“I think the results that I have presented here and which were published in The Lancet are very encouraging, and I think it helps unify the field and more recent findings with renal denervation,” Bhatt told Interventional News, adding that the analysis complements other studies in renal denervation to have met their primary endpoints. “Viewed in that context, [and] examining the totality of data [indicating] that there is really something there,” he added, “renal denervation is, in fact, reducing blood pressure. It does not mean it should replace medicines or lifestyle modifications, but in the right patient, I think it could be a useful adjunct.”
In what is seen as a further positive development for proponents of renal denervation, the same TCT 2022 late-breaking clinical science session saw Ajay Kirtane (Columbia University Irving Medical Center New York-Presbyterian Hospital, New York, USA) present
the primary results from RADIANCE II, looking at the blood pressure-lowering efficacy of ultrasound renal denervation using the Paradise (Recor Medical) system at two months.
Through the trial, investigators from 60 study centres in eight countries screened 1,038 individuals for trial eligibility, with 224 patients with uncontrolled hypertension ultimately randomised 2:1 to undergo renal denervation with the Paradise system (150) or a sham procedure (74).
Patients were required to remain off antihypertensive medications throughout the two months of follow-up unless specified blood pressure criteria were exceeded. At the two-month primary efficacy endpoint, Kirtane reported, patients treated with renal denervation had a mean reduction in daytime ambulatory systolic blood pressure of -7.9mmHg, compared to a reduction of -1.8mmHg in the sham control group, corresponding to a statistically significant between-group difference of -6.3mmHg (p<0.0001).
Similar reductions in blood pressure were observed in nighttime and 24-hour measures, as well as measurements taken at home and in the physician office. There were also no major adverse events in either group through 30 days, Kirtane reported. The trial’s primary safety endpoint will be measured at six months, and patients will be followed for a total of five years.
“The reason that we did the RADIANCE II trial is to try and build upon prior trials, such as RADIANCE-HTN SOLO and TRIO, which had demonstrated that renal denervation could lower blood pressure in comparison with a sham,” Kirtane commented to Interventional News, referring to earlier studies to have assessed the use of the Paradise system. “I think it pretty clearly showed that renal denervation lowered blood pressure at two months in comparison with the sham, especially on a backdrop of patients with no medication.
“We have also shown that, in a backdrop of a combination therapy with three separate agents, renal denervation can lower blood pressure, and in many ways this is a confirmatory trial, but a larger trial that will hopefully lead to regulatory approval in the USA.”
In discussions that followed Kirtane’s presentation at TCT, speakers welcomed the findings of RADIANCE
II, and their wider importance to the understanding of renal denervation as a treatment for hypertension. “We should not forget that this is the sixth sham-controlled trial that showed and confirmed the efficacy of this approach using different modalities, but also using different patient populations,” said Felix Mahfoud (Saarland University Hospital, Hamburg, Germany), who has himself been heavily involved in renal denervation research including as an investigator in the RADIANCE-HTN SOLO and TRIO trials.
Mahfoud asked Kirtane to offer his view on what is required for the treatment to find its way into clinical practice, to which Kirtane responded that additional safety and, importantly, clinical outcomes data will be vital. “That is important, because while blood pressure is recognised as a surrogate of adverse events, and we know that for patients that are uncontrolled that lowering blood pressure is a good thing, I think we have seen enough examples in our field of potential questions to clinical efficacy that the onus is on us to do those kinds of trials,” Kirtane said.
Naomi Fisher (Brigham and Women’s Hospital and Harvard Medical School, Boston, USA) offered her perspective on the trial as a specialist in hypertension, describing the condition as the “number one global burden of disease risk factor in the world”.
RADIANCE II
The change in ambulatory systolic blood pressure was -7.9 mmHg for the ultrasound renal denervation group compared to -1.8mmHg for the sham group.
“We need innovation,” she commented. “Our control rates are poor and they are only falling, if you look at large statistical datasets showing that we are doing a worse and worse job as time goes on. We have had pharmacology around since the 1950s for high blood pressure, our last new drug class was introduced in 2007, that is how long ago that we had an innovation.
SYMPLICITY HTN-3
“Finally, we have evidence for an innovative therapy that is really desperately needed to help control blood pressure.”
At 12 months, renal denervation patients had significantly greater office systolic blood pressure reductions compared with sham control after crossover imputation (-18.9 mmHg vs -6.3 mmHg, p<0.0001, respectively).
Issue88 | November 2022 17Renal Denervation
The results of these two key trials were presented at TCT 2022

19-23 JANUARY 2023 AW S H I N G TON, DC | WASHINGTON HILTON REGISTER NOW at www.sio-central.org/sio2023
FLASH results demonstrate “excellent safety profile” of the FlowTriever system in full US cohort
Results of the FLASH registry demonstrate the “excellent safety profile” of the FlowTriever system (Inari Medical) in 800 “real-world” patients. This is according to Catalin Toma (University of Pittsburgh Medical Center, Pittsburgh, USA), who presented outcomes for the full US cohort of FLASH at the 2022 Transcatheter Cardiovascular Therapeutics meeting (TCT; 16–19 September, Boston, USA). The results were simultaneously published in EuroIntervention.
TOMA REPORTED A 1.4% MAJOR BLEEDING rate and 0.4% rate of other major adverse events (MAEs) in what the presenter described as the largest prospective interventional study in pulmonary embolism (PE). Allcause mortality was <1% at the 30-day visit in this “real-world” population with prevalent baseline predictors of mortality, the presenter added, noting also that haemodynamics improved ontable, acute vitals and right ventricular (RV) strain normalised, and clinical recovery continued through six months.
The presenter noted that acute all-cause mortality following PE has remained high (>10%) over two decades, adding that, following PE, the 30-day readmission rate is nearly 25%, and up to half of patients report persistent dyspnoea, exercise intolerance, and/or functional limitations
at three to six months.
According to Toma, guidelines suggest considering advanced therapies, including mechanical thrombectomy, when thrombolytics fail or are contraindicated, or haemodynamic deterioration occurs. However, he said, major bleeding risks with thrombolyticbased treatment strategies remain a concern, and their use is limited by corresponding contraindications and consequent intensive care unit (ICU) monitoring.
Mechanical thrombectomy can rapidly extract thrombus and relieve RV strain without thrombolytics, the presenter said, stating that “additional data on the risk-to-benefit ratio could shift the standard of care”.
 One example
One example
Randomised trial finds carotid endarterectomy or stenting not superior to best medical therapy in asymptomatic patients
of a mechanical thrombectomy device is FlowTriever, he highlighted, noting that this system is 510(k)-cleared by the US Food and Drug Administration (FDA) and CE mark-approved for the treatment of PE.
FLASH is a prospective, multicentre, single-arm registry designed to evaluate the safety and effectiveness of the FlowTriever system for treatment of PE through six months, with the decision to intervene being at the discretion of treating physicians or local PE response team (PERT). The primary endpoint is an MAE composite endpoint of device-related mortality within 48 hours, major bleeding within 48 hours, and intraprocedural device- or procedurerelated adverse events.
At TCT, Toma reported a primary MAE rate of 1.8% (14/788), which combined a 0% rate of device-related deaths (0/788), 1.4% rate of major bleeding (11/788), and 0.4% rate of intraprocedural adverse events (3/788).
Regarding all-cuase mortality, he noted rates of 0.3% at the 48-hour visit (2/794), 0.8% at the 30-day visit (6/734), and 5% rate at the six-month visit (28/588). Importantly, the procedure led to significant improvement in invasive haemodynamics with decreased pulmonary
pressures and improved cardiac output. Finally, Toma revealed that the rate of all-cause readmissions at the 30-day visit was 6.2%, with 1.4% related to PE treatment (10/711) and 4.8% unrelated to PE treatment (34/714).
Looking ahead, Toma highlighted that “data from the ongoing PEERLESS randomised controlled trial will provide important evidence regarding the safety and effectiveness of FlowTriever mechanical thrombectomy compared with catheter-directed thrombolysis”.
Five-year outcomes of a multicentre, randomised controlled trial (RCT) indicate that carotid endarterectomy (CEA) or carotid artery stenting (CAS) are not superior to best medical therapy (BMT) alone for moderate-to-severe asymptomatic carotid artery stenosis.
TILMAN REIFF (UNIVERSITY HOSPITAL of Heidelberg, Heidelberg, Germany) and colleagues recently reported this key conclusion from the SPACE-2 trial in The Lancet Neurology. The authors claim that—to the best of their knowledge—this is the first randomised trial to directly compare CEA plus BMT, CAS plus BMT, and BMT alone over a five-year period in patients with asymptomatic carotid artery stenosis.
“The optimal treatment for patients with asymptomatic carotid artery stenosis is under debate,” the investigators write, noting that, since BMT has improved over time, the benefit of CEA or CAS is “unclear”. They add that randomised data comparing the effect of CEA and CAS versus BMT alone are lacking, and therefore aimed to directly compare CEA plus BMT with CAS plus BMT and both with BMT only in the SPACE-2 trial.
SPACE-2 was a multicentre RCT carried out at 36 study centres in Austria, Germany, and Switzerland, Reiff et al detail in their report. The researchers enrolled participants aged 50–85 years with asymptomatic carotid artery stenosis at the distal common carotid artery or the extracranial internal carotid
artery of at least 70% according to European Carotid Surgery Trial criteria (equivalent to at least 50–99% according to North American Symptomatic Carotid Endarterectomy Trial [NASCET] criteria).
Reiff and colleagues note that SPACE-2 was initially designed as a three-arm trial including one group for BMT alone. However, the design was amended due to slow recruitment to become two substudies with two arms each comparing CEA plus BMT with BMT alone (SPACE-2a) and CAS plus BMT with BMT alone (SPACE-2b).
The authors report that a total of 513 patients across SPACE-2, SPACE-2a, and SPACE-2b were recruited and surveyed between July 2009 and December 2019, of whom 203 (40%) were allocated to CEA plus BMT, 197 (38%) to CAS plus BMT, and 113 (22%) to BMT alone. The median follow-up was 59.6 months.
Lancet paper, Reiff and colleagues report that the cumulative incidence of any stroke or death from any cause within 30 days or an ipsilateral stroke within five years—the primary
Tilman Reiff
efficacy endpoint—was 2.5% (95% confidence interval [CI], 1–5.8) with CEA plus BMT, 4.4% (95% CI, 2.2–8.6) with CAS plus BMT, and 3.1% (95% CI, 1–9.4) with BMT alone.
The investigators also relay that, in both the CEA and CAS group, five strokes and no deaths occurred in the 30-day period after the procedure. During the five-year follow-up period, they note, three ipsilateral strokes occurred in both the CAS plus BMT and BMT alone groups, with none in the CEA plus BMT group.
Reiff et al conclude that CEA plus BMT or CAS plus BMT were not found to be superior to BMT alone regarding risk of stroke or death within 30 days or ipsilateral stroke out to five years. However, they stress that their results “should be interpreted with caution” due to the small sample size.
In a commentary on Reiff and colleagues’ work, also published in The Lancet Neurology, Alison Halliday (University of Oxford, Oxford, UK) underscores the importance of randomised trials in this field of study. Halliday, who is principal investigator of the Asymptomatic Carotid Surgery Trials, remarks: “Despite its relatively small sample size, SPACE-2 provides important long-term followup data because of the randomised trial methodology. Large procedural registries usually cease follow-up within days or a few months, and patients on medical treatment alone cannot be meaningfully compared without randomisation.
“The future of interventions for carotid artery stenosis on randomised comparisons of different treatment approaches to [minimise bias] and, at the same time, that enough patients are included. Alternatively, individual patient meta-analysis of similar trials can be used to support future interventions. SPACE-2 is of value to future individual patient meta-analyses of these three treatment options.”

Issue88 | November 2022 19Pulmonary Embolism
Data from the ongoing PEERLESS randomised controlled trial will provide important evidence regarding the safety and effectiveness of FlowTriever mechanical thrombectomy compared with catheter-directed thrombolysis.”
Catalin Toma
Regency Paris Etoile
Hot Topic Meeting on Embolotherapy for Joint Disease and MSK Sports Injuries

GEST is proud to announce the launch of its first focused, hot topics meeting fully dedicated to the Embolotherapy for Joint Diseases and MSK Sport Injuries. This in-person event will be a classic GEST program full of interactions, panels, masterclasses and more!


Scan code to register today


MSK 2023 January 20-21, 2023 • Paris, France
Hyatt
Micromate™ reduces complications, radiation exposure and procedure time for increasingly “challenging” cases
Marco van Strijen is an interventional radiologist at St Antonius Ziekenhuis (Nieuwegein, The Netherlands) who specialises in non-vascular interventions and interventional oncology. Image-guided procedures feature heavily in his practice, Van Strijen tells Interventional News, enabling him to “[draw] needle paths, [define] targets and [introduce] needles”. Micromate (Interventional Systems) provides robotic assistance for these tasks, Van Strijen reports, detailing how “it is three years that we have been using Micromate”, following on from a successful stint with the early prototype that “functioned so well” that “the rest was history”.
On how Micromate fulfils its role within his practice, Van Strijen begins by acknowledging that for any percutaneous biopsy “it is very important to have a stable needle”, and therefore, “a device that helps you keep the needle stable while advancing the device through the skin to the desired target,” such as Micromate does, is valuable. “This is especially true in […] areas where there is not that much overlying skin or soft tissue [to] hold your needle while you are trying to centre it in the direction of your target,” Van Strijen adds, before exemplifying how unwieldy some of the former approaches to intraprocedural needle stabilisation were: “we were using our own hands, sterile towels draped around the needle insertion point, or sterile forceps, making adjustments until we had the needle in a holding position, but these were not that stable, especially when you have a patient who is still breathing or maybe even starts to move because of their discomfort on the table: you always have the risk of dislodging the needle.”
carcinoma—in which Micromate was used under live imaging, the procedure time was 43% faster than previously reported, Interventional Systems states. The radiation level decrease measured 70%. Greater needle stability facilitates greater procedural accuracy, which, Van Strijen shares, makes “[working] in areas that rely on needles being positioned to millimetre or sub-millimetre accuracy” possible. For example, this could be “in the vicinity of critical structures such as the neck or the face or close to the major vessels of the thorax”. Van Strijen asserts that “this is where this type of robotic device comes in very handy.”
To the question posed by Interventional News of how Micromate reduces complications in lung biopsy cases, such as the aforementioned, Van
Strijen states that “a quick inand-out is the ideal strategy”, and with Micromate, the biopsy is possible “during one single breath-hold”. The incidence of pneumothoraces, which Van Strijen notes is the “most encountered complication in this procedure”, is “[reduced] significantly” by virtue of being able to avoid unnecessary pleura punctures. Where the needle is less stable, the necessary multiple attempts and sometimes, leaving the needle in, can cause tears in the pleura, Van Strijen explains.
Micromate may be responsible for something akin to his team becoming victims of their own success, Van Strijen then admits—”I think that by having this type of technology available, we are challenged quite a bit by our referring clinicians who are asking for more and more challenging lesions to be biopsied.” In practice this means “trying to get histology from a lesion of just a few millimetres,” in contrast to a decade ago, when, Van Strijen says “a two- or threecentimetre lesion was common”.
Likewise, because of the development of robotic technology, Van Strijen now carries out biopsies “next to very challenging structures—close to major vessels, close to the beating heart”.
Van Strijen is also keen to mention a further advantage of Micromate and the impact it has in his teaching hospital. “This type of device should be very easy to use, one that any user immediately understands without a lot of training—after only one or two demo cases,” he opines. And, with Micromate satisfying such an expectation, Van Strijen sees it as “[bridging] the gap between inexperienced and experienced users […] Young doctors are challenged in trying to perform the same procedures as their tutors,” but, as Van Strijen informs Interventional News, “one of the things I find very helpful [about Micromate]” is how doctors of different levels of experience can use it successfully.”

Van Strijen then enumerates the precise advantages of having a completely stable needle, as achieved with Micromate—“not only will it help in reducing the number of [needle] re-positionings, but it reduces the need for imaging, as you can advance the needle as quickly as possible. And this is [of…] benefit in reducing the amount of radiation, not only for the patient but also for yourself as the operator.” Furthermore, Van Strijen speaks of the procedural time reduction that this results in, and, consequently, the discomfort the patient is subjected to on the table.
In a particular case of Van Strijen’s—that of a percutaneous lung biopsy close to the pleura in a 52-year-old patient referred with suspected rectal

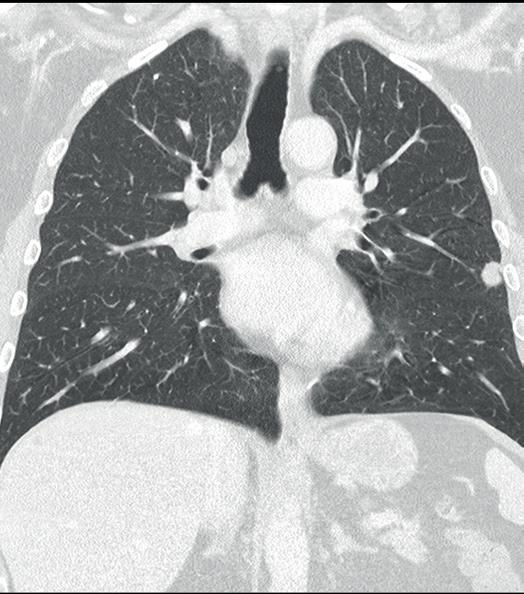

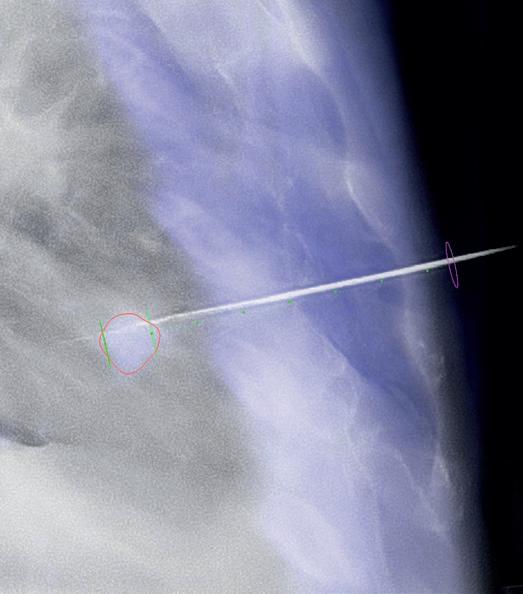


21AdvertorialIssue88 | November 2022
THIS
ADVERTORIAL IS
SPONSORED
BY INTERVENTIONAL SYSTEMS
I think that by having this type of technology available, we are challenged quite a bit by our referring clinicians who are asking for more and more challenging lesions to be biopsied.”
1-3) Preoperative CT scan views. The lateral left lung lesion is clearly visible; 4) Definition of the planned needle path. The red contour corresponds to the borders of the segmented lesion; 5) Alignment of Micromate to the planned needle path under live imaging; 6) Insertion of the biopsy needle through the guidance needle and tissue harvesting.
Marco van Strijen
4 5 1 2 3 6
The IR event of 2023 is taking place in Phoenix. Will you be there?




Don’t miss these program highlights:
The 2023 Dotter Lecture and award ceremonies that recognize and celebrate your peers
Plenary sessions that are a hallmark of SIR productions
Categorical courses delivered by key opinion leaders and rising stars


Hands-on and Angio-club workshops for one of a kind learning experience
Sessions by Clinical Specialty Councils to help you improve your practice across all clinical pathways and so much more!

Register by Jan. 13 for maximum savings!
#SIR23PHX sirmeeting.org
Program updates and registration
New mechanical thrombectomy systems unlock possibilities for the treatment of venous thromboembolism

Mechanical thrombectomy with the ClotTriever and FlowTriever systems (Inari Medical) opens up new possibilities for the management of deep vein thrombosis (DVT) and pulmonary embolism (PE), widening the treatment window and eliminating the sideeffects associated with lysis. This is according to Bernhard Gebauer (Charité – University Medicine Berlin, Berlin, Germany) and Gerd Grözinger (University of Tübingen, Tübingen, Germany), who discussed developments in the diagnosis and treatment of venous thromboembolism at this year’s Cardiovascular and Interventional Radiological Society of European (CIRSE) annual meeting (10–14 September, Barcelona, Spain). In the discussion, both interventionalists focused on the benefits of mechanical thrombectomy, in particular with the ClotTriever and FlowTriever systems, and how these technologies have opened up new possibilities in their treatment algorithms.
AT THE OUTSET OF THE DISCUSSION, both physicians gave an overview of general trends in the treatment of DVT and PE. Grözinger was keen to get Gebauer’s take on why the prognosis for PE “has not significantly improved” in recent years.

Gebauer, who is head of the Interventional Radiology Department at Charité, stressed that this is a “severe” disease, with most patients experiencing impaired heart function. The main reason why prognosis has not improved, he believes, is because the treatment options on anticoagulation or lysis are “very limited”. Gebauer explained that often thrombus is old and organised, and when this is the case anticoagulation or lysis are not effective. “I think that removing the thrombus and getting away from the underlying disease is probably helping us to improve treatment for these patients in the future,” he remarked, pointing to the benefits of mechanical thrombectomy in this patient population.
Gebauer also commented on the option of systemic thrombolysis. He noted that, while this method is now recommended in the guidelines for some patient groups, the high dose of medicine needed for the technique to work could result in complications, including risk of bleeding. He also pointed out that the technique is not a suitable option for many patients. “A lot of patients we treat have had trauma or recent surgery, and so giving them thrombolysis is
contraindicated,” he noted. In addition, he mentioned that physicians will sometimes experience the “very serious event” of severe cerebral bleedings from thrombolysis in these patients. Grözinger, who is deputy medical director at the University of Tübingen, added that treatment with thrombolysis might also be suboptimal for old and organised thrombus. Mechanical thrombectomy might be a solution here, Gebauer suggested.
This technology also shows potential in DVT, the experts pointed out when discussing the perfect time window for treating this condition. The ClotTriever has the potential to overcome the “strict timeframe” of two weeks for treatment that used to exist, Grözinger
said, referencing its ability to deal with thrombus of various ages. “The time window has extended tremendously.”


The experts considered which patients benefit the most from interventional treatment for either a DVT or PE, especially with regard to long-term outcomes. Gebauer expressed his opinion that patients with older thrombus in whom guideline-recommended therapies give suboptimal results are the patients who benefit the most from these new therapies. “The direct removal of thrombus leads to improvement in these patients,” he noted.
For pulmonary embolism, which Gebauer stressed is “more of an emergency”, he believes that intermediate high-risk (IHR) patients benefit the most from intervention. “High-risk patients have a very high mortality rate, and in these patients, you can also improve the mortality, however they would still have a high mortality rate because of their underlying disease and impaired cardiac function,” he explained.
Grözinger added that there is another set of patients in whom he would always recommend intervention: “If we see the pelvic veins are involved, we would rather go straight to interventional treatment,” he said, “especially with these new devices where you can more or less eliminate bleeding risks and other side-effects without lysis”. He summarised that the approach at his institution centres on a “strong belief” in lysis-free thrombectomy.
Despite it having been established that patients with older thrombus benefit more from mechanical thrombectomy than from conservative treatments, Gebauer underlined the fact that patient selection is not simple. “It is not easy to identify the correct patients because very often you do not know the thrombus age itself,” he said. He stated that imaging can provide some “hints” as to the age of the thrombus, and that sometimes onset of patient symptoms can also help in identifying the right patients for treatment.
According to Grözinger, magnetic resonance (MR) venography is more reliable than onset of symptoms and patient history in determining thrombus age in DVT. He noted the example of an MR venography showing organised thrombus and vessel wall scars despite the patient saying that symptoms began three to five days earlier. “In cases such as this, there is a fresh part of the thrombus, but the underlying disease is often much older,” he explained. This is where these new treatment options unlock the possibilities for the treatment of venous thromboembolism.
Indications for use: The ClotTriever® Thrombectomy System is indicated for (1) the non-surgical removal of thrombi and emboli from blood vessels, and (2) injection, infusion and/or aspiration of contrast media and other fluids into or from a blood vessel. The ClotTriever thrombectomy system is intended for use in the peripheral vasculature including deep vein thrombosis (DVT).
Indications, Contraindications, warnings and instructions for use can be found in the product labeling supplied with each device.
Caution: Federal (USA) law restricts this device to sale by or on the order of a physician.
All trademarks are property of their respective owners.
The FlowTriever® Retrieval/Aspiration System is indicated for (1) the non-surgical removal of emboli and thrombi from blood vessels; and (2) injection, infusion and/or aspiration of contrast media and other fluids into or from a blood vessel. The FlowTriever system is intended for use in the peripheral vasculature and for the treatment of pulmonary embolism.

Indications, Contraindications, warnings and instructions for use can be found in the product labeling supplied with each device.
Caution: Federal (USA) law restricts this device to sale by or on the order of a physician.
All trademarks are property of their respective owners.
Inari Medical, Inc. headquarters: 6001 Oak Canyon, Suite 100 | Irvine CA 92618
Inari Medical Europe GmbH, a subsidiary of Inari Medical, Inc. | Messeplatz 10 | 4058 Basel, Switzerland
Issue88 | November 2022
I think that removing the thrombus and getting away from the underlying disease is probably helping us to improve treatment for these patients in the future.” Bernhard Gebauer
The time window [for deep vein thrombosis treatment] has extended tremendously.”
— Gerd Grözinger
ClotTriever device
THIS ADVERTORIAL IS SPONSORED BY INARI MEDICAL

LEADERS IN ONCOLOGIC INTERVENTIONS www.ecio.org ECIO 2023 April 16-19 Stockholm, Sweden European Conference on Interventional Oncology C RSE Cardiovascular and Interventional Radiological Society of Europe Submit your abstract for ECIO 2023 and showcase your work to the world’s largest IO community ! Accepted papers will be • featured at the congress • published in a dedicated CVIR supplement • accessible via the congress platform • included in the CIRSE Library Abstract submission for ECIO 2023 is open until January 12. ecio.org/submit GET EXPOSUREGLOBALFOR YOUR WORK!
Product News

Cordis acquires MedAlliance
Cordis announced its acquisition, subject to customary closing conditions, of MedAlliance.
A press release notes that the agreement includes an initial investment of US$35 million and US$200 million payment upon closing in 2023, regulatory achievement milestones up to US$125 million and commercial milestones up to US$775 million through 2029. Cordis will immediately begin co-promotion of MedAlliance’s Selution SLR drugeluting balloon in markets where it is commercially available.
The Selution platform leverages spherical MicroReservoirs made from biodegradable polymer mixed with the drug to control the sustained release of sirolimus. According to Cordis, Selution SLR is the only drug-eluting balloon using MicroReservoirs and is designed to provide the longest and most effective pharmacokinetics release profile of any device on the market.
Selution SLR received CE mark approval for the treatment of peripheral arterial disease in February 2020 and for the treatment of coronary artery disease in May 2020. In addition, MedAlliance has obtained
investigational device exemptions for peripheral below-the-knee (BTK) and superficial femoral artery (SFA) interventions.
Penumbra and Asahi Intecc partner to introduce Indigo System to Japan
Penumbra and Asahi Intecc, a Japanese medical device manufacturer, announced that they will collaborate to introduce Penumbra’s Indigo Aspiration System into the Japanese market upon regulatory approval.
Penumbra’s Indigo Aspiration System can be used to remove emboli and thrombi from vessels of the peripheral arterial and venous systems, and for treatment of pulmonary embolism.Indigo enables the restoration of blood flow in such cases as acute limb ischaemia and venous thrombus.

differentiate between clot and blood, designed to reduce blood loss and the need for clot-dissolving drugs, which may lower the risk of bleeding complications.
New liquid embolic multicentre trial successfully enrols final patient
for tumour embolization and other uses where there is a desire for distal vessel bed penetration.
Interim results of the GPX study have been presented at recent annual congresses including Global Embolization Symposium & Technologies (GEST), Society of Interventional Radiology (SIR), and Leipzig Interventional Course (LINC).
 Indigo Aspiration System
Indigo Aspiration System
The Indigo System combines hypotube-based Indigo Aspiration Catheters with Lightning Intelligent Aspiration, a computer-aided clot detection technology that can
Fluidx Medical has shared completion of trial enrolment for its GPX embolic device. In this multicentre trial, GPX was used to treat a variety of primary and metastatic tumours, renal adenoma tumours, and a range of other arterial and venous applications. “We are pleased to announce the enrolment of the final patient in the trial and look forward to participating in future trials using this promising technology,” stated the trial’s principal investigator, Andrew Holden (Auckland City Hospital, Auckland, New Zealand.) “In the trial, GPX showed significant potential to advance liquid embolics, penetrating very distally, providing profound embolization, and demonstrating excellent radiopacity which helped to avoid non-target embolization and preserve healthy adjacent tissue.”
GPX has shown promising results
Truveta announces collaboration with Boston Scientific to advance postprocedure patient insights and help address healthcare disparities
Truveta announced a strategic collaborative agreement with Boston Scientific to improve long-term patient care and gain insights into healthcare disparities. Through this collaboration, Boston Scientific researchers will be able to access data from Truveta, which contain de-identified medical records from more than 65 million US patients.
Truveta data provide the most upto-date picture of US health across age, race, ethnicity, geography, socioeconomic factors, and more. Data are updated daily and include the full Electronic Medical Record (EMR), including device-specific data, not just the medical bill from claims data, all de-identified and aggregated.
These clinical data are linked across providers and with medical claims when care is provided outside Truveta’s network.
Available in print and digital formats and through our social channels
Visit venousnews.com and click ‘Subscriptions’ for complimentary print subscription* and e-newsletter subscription**




*Available
worldwide
25Issue88 | November 2022 Market Watch
for US and EU readers only **Available
A trusted provider of latest news, review of cutting-edge research, congress coverage and opinion from thought leaders
A specialised news source in the venous arena
Editorially independent
Subscribe
today
Industry News
Cardiovascular Systems announces full market release of the 2.00 Max Crown for peripheral orbital atherectomy systems
Cardiovascular Systems Inc (CSI) has announced the full market release of the 2.00 Max Crown for peripheral orbital atherectomy systems (2.00 Max Crown).
CSI notes in a press release that the 2.00 Max Crown is uniquely designed to enable simultaneous modification of both intimal and medial calcium. The device features an increased 70-micron diamond coated crown that creates more efficient engagement in mixed plaque, helping to achieve optimal luminal gain in mild to moderately calcified lesions above the knee.
Amit Srivastava (Bay Area Heart Center, St Petersburg, USA), who was one of the first physicians in the USA to incorporate the 2.00 Max Crown into his practice, commented: “The new 2.00 Max Crown greatly expands the lesions that can be treated with CSI’s orbital atherectomy. This device delivers exceptional luminal gain in mixed morphology lesions above the knee.”
Bentley acquires GoBack catheter from Upstream Peripheral Medical Technologies
Bentley announced that it has acquired the rights of the GoBack catheter from Upstream Peripheral Technologies.
The GoBack catheter will simplify crossing and re-entry in occluded arteries. A press release notes that the product’s unique feature is a curved nitinol needle that can be manipulated by the physician using the device handle. Thanks to its small profile, the device can even be used in the smaller arteries in the lower leg.
The GoBack catheter is CE-marked and US Food and Drug Administration
Calendar of events
12–15 January 2023
SPECTRUM 2023 Miami, USA thespectrumconference.org
16–19 January 2023
International Symposium on Endovascular Therapies (ISET) 2023 Miami Beach, USA iset.org/2023
19–23 January 2023
SIO (Society of Interventional Oncology) 2023 Washington D.C., USA sio-central.org
(ChEVAR) with the Endurant II/IIs stent graft system.
Used together, the Endurant II/IIs stent graft and Radiant covered stent offer a standardised, fully on-label, off-the-shelf solution for short-neck, juxtarenal abdominal aortic aneurysms (AAA). This enables safe and effective endovascular repair in both urgent and elective juxtarenal AAA cases.
The Radiant product’s design offers ccurate delivery and deployment, while providing the flexibility and radial strength necessary for a chimney covered stent.
The covered stent is intended to maintain perfusion to the renal arteries when used in combination with the Endurant II/IIs stent graft system for AAA patients with inadequate sealing zones.
OptaBlate bone tumour ablation system
Featuring four probes and Stryker’s patented microinfusion technology, OptaBlate allows physicians to customise their procedure and reduce ablation time by three minutes.
(FDA) cleared. Launched in 2019, the device is now available in 23 countries. It is Bentley’s intention to extend the global availability to all of the 80 markets in which the company is already active, the press release details.

Currently produced in Israel and initially shipped from there, a production transfer to the Bentley production facility in Hechingen, Germany will be completed by 2025.
Medtronic receives CE mark for the first balloonexpandable covered stent indicated for ChEVAR Medtronic has received CE mark for its Radiant balloon-expandable covered stent, the first and currently, only, covered stent indicated for use in chimney endovascular aneurysm repair

With this CE mark, Medtronic will roll out a comprehensive training programme and continue to invest in clinical data to optimise ChEVAR outcomes.
The product comes from the longterm collaboration between Medtronic and Getinge, leveraging Getinge’s proven Advanta V12 design and eight sizes of the Getinge (Atrium Medical) stent portfolio. It will be produced by Getinge and distributed by Medtronic.
Stryker receives FDA clearance for OptaBlate bone tumour ablation system
Stryker has announced that its OptaBlate bone tumour ablation system has received 510(k) clearance from the US Food and Drug Administration (FDA). The addition of the OptaBlate technology to Stryker’s Interventional Spine portfolio expands on its core competencies in vertebral augmentation and radiofrequency ablation,completing its portfolio of treatment options for metastatic vertebral body fractures.

“Stryker’s new bone tumour ablation (BTA) system is a significant improvement on existing technology,” said Anthony Brown, a vascular and interventional radiologist at Radiology Imaging Associates (Englewood, USA).
Key features of the system include treatment of two vertebral body levels at once using a bipedicular approach, and microinfusion technology, which keeps the zone hydrated, reducing impedance errors and preventing charring.
Xeltis presents “promising” first-in-human data on restorative haemodialysis access graft
Xeltis has shared in a press release what it describes as “very promising” preliminary efficacy and safety results from one of the centres participating in the AXESS study—a first-in-human (FIH) clinical trial of its restorative haemodialysis access graft, Axess.
These data were presented at the Porto Vascular Conference (PVC; 7–8 October 2022, Porto, Portugal).
During haemodialysis, the Axess device demonstrated 100% cumulative primary and secondary patency, with an average follow-up time of 5.8 months and no device-related complications, in patients implanted by Matteo Tozzi and his team at the University of Insubria (Varese, Italy)—one of six European sites participating in the trial.
Xeltis’ Axess device is a synthetic, bio-restorative vessel graft that enables early puncturing needed to connect to the haemodialysis machine. It is also designed to turn into a patient’s own living blood vessel, like an arteriovenous fistula, as its porous structure gets gradually colonised by patient’s own tissue cells.
20–21 January 2023
GEST MSK Hot Topic Meeting 2023 Paris, France eventcreate.com/e/gestmsk2023
23–24 January 2023
Mediterranean Interventional Oncology (MIO) 2023 Rome, Italy & Digital miolive.eu
11–14 February 2023
Pan-Arab Interventional Radiology Society ( PAIRS) 2023
Diubai, United Arab Emirates pairscongress.com
1–5 March 2023
European Congress of Radiology (ECR) 2023 Vienna, Austria myesr.org/congress
4–9 March 2023
Society of Interventional Radiology (SIR) Annual Meeting 2023 Phoenix, USA sirmeeting.org/index.asp
16–19 April 2023
European Conference on Interventional Oncology (ECIO) 2023 Stockholm, Sweden ecio.org/attend/ecio-2023
25–27 April 2023
Charing Cross (CX) Symposium 2023 London, UK cxsymposium.com
18–21 May 2023
Global Embolization Oncology Symposium Technologies (GEST) 2023 New York, USA annual.thegestgroup.com/GEST23
6–9 June 2023
Leipzig Interventional Course (LINC) 2023 Leipzig, Germany leipzig-interventional-course.com
21–24 June 2023
European Conference on Embolotherapy (ET) 2023 Valencia, Spain etconference.org/attend/et-2023
9–13 September 2023
Cardiovascular and Interventional Radiological Society of Europe (CIRSE) 2023 Copenhagen, Denmark cirsecongress.cirse.org
26 Market Watch November 2022 | Issue88
C M Y CM MY CY CMY K
Radiant balloon-expandable covered stent
Bentley CEO and directors with Arnold Schwarzenegger double

Consensus Update Vascular & Endovascular SEE YOU IN 2023 CXSYMPOSIUM.COM Peripheral Arterial Consensus Aortic Consensus Acute Stroke Consensus Venous & Lymphatic Consensus Vascular Access Consensus The Hurting Leg Consensus INNOVATIONEDUCATION EVIDENCE 25–27 APRIL 2023 TUESDAY-THURSDAY LONDON, UNITED KINGDOM CONTROVERSIES CHALLENGES CONSENSUS
Predictably pr e c ise.
NEUWAVE ™ offers a comprehensive solution that enables you to ablate lesions of many shapes and sizes with predictability and precision. 1,2*
Scan the code to get in touch. Together, we’re rede ning ablation
. *Refer to IFU for Ablation Zone Sizes. Based on benchtop testing and clinical effect is unknown. 1. Laeseke PF, Lee FT Jr, van der Weide DW, Brace CL. Multiple-Antenna Microwave Ablation: Spatially Distributing Power Improves Thermal Profiles and Reduces Invasiveness. J Interv Oncol. 2009;2(2):65-72. 2. Harari CM, Magagna M, Bedoya M, et al. Microwave Ablation: Comparison of Simultaneous and Sequential Activation of Multiple Antennas in Liver Model Systems. Radiology. 2016;278(1):95-103 Please refer always to the Instructions for Use / Package Insert that come with the device for the most current and complete instructions. © Ethicon Endo Surgery (Europe) GmbH 2022, 213460 220513 EMEA/UK























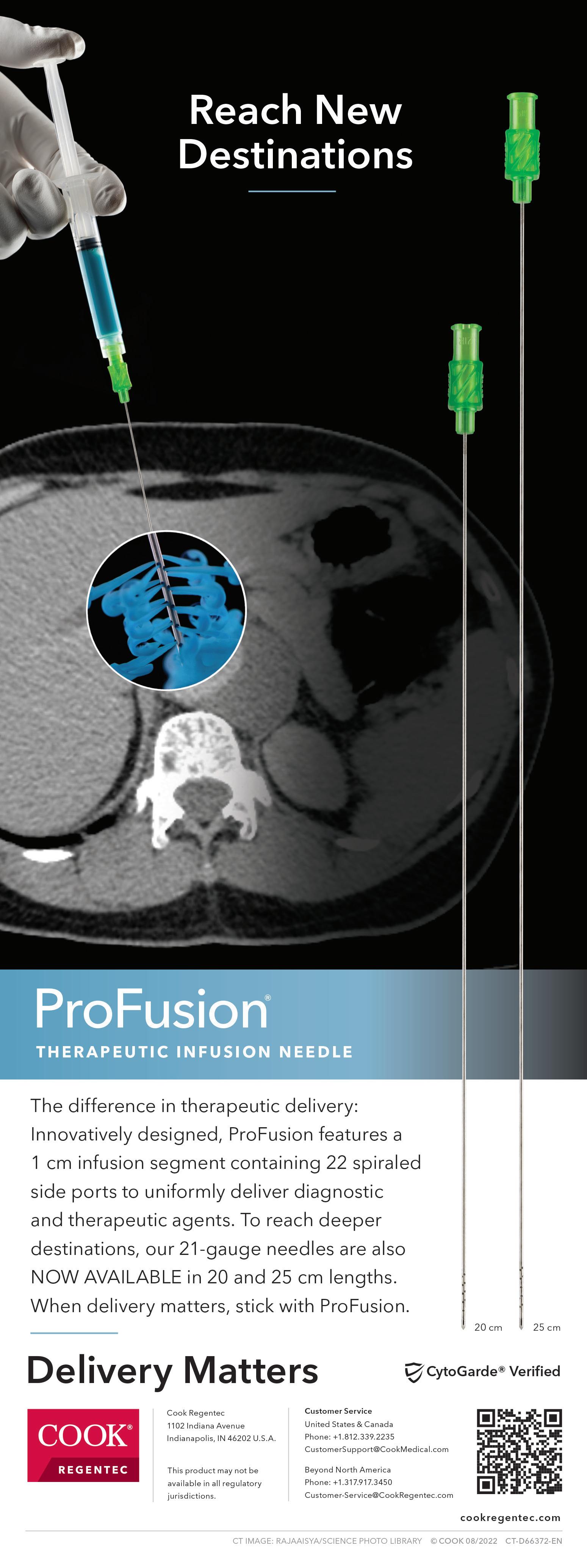







 JW MARRIOTT MARQUIS • MIAMI, FL
JW MARRIOTT MARQUIS • MIAMI, FL



























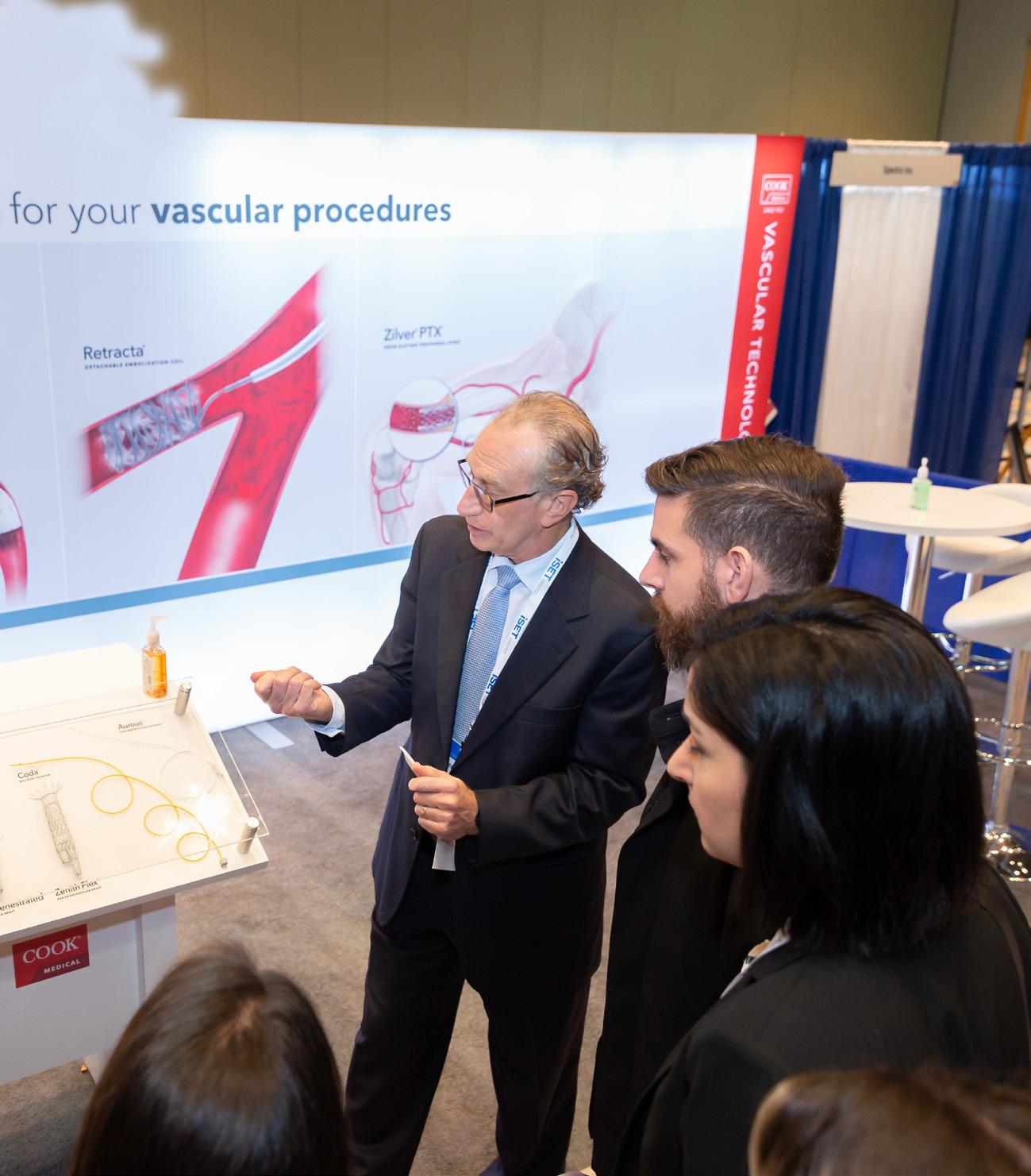



 One example
One example