page 2
Will the MDR transition fall short of mitigating impact on IR and beyond?
Profile: Theresa Caridi

page 16
In May 2021, the European Union (EU) Medical Devices Regulation (MDR) came into force to revise quality and safety standards for thousands of types of medical devices, and to reclassify in some cases. MDR was intended to come into effect in May 2020 after a three-year transition period, but this was delayed due to the COVID-19 pandemic. The transition period was recently extended again to allow device companies and manufacturers more time to plan their route to conformity with the new regulations, which many industry and healthcare stakeholders consider will make for slower implementation of new devices than under the MDR’s precursor, the Medical Device Directive (MDD). Interventional News sought out the views of interventional radiologists in Europe and the UK to capture the concerns within the sub-specialty relating to MDR, as well as those of industry.
In March 2023, European Council members voted to give producers of higher-risk medical devices until 31 December 2027, and those of mediumand lower-risk devices until 31 December 2028, to bring their products in line with the new rules on safety and quality. This gives manufacturers at least three years and six months’ extra time to adapt, as the conformity deadline initially adopted when MDR came into force was May 2024.
In December 2022, ahead of the March extension vote, EU health commissioner Stella Kyriakides was quoted explaining, in a European Council meeting, the rationale for going ahead with the vote. “We are […] experiencing [device] supply shortages on the global market. We are still feeling the impacts of the pandemic, and now also the Russian war in Ukraine, where several manufacturers of devices are located. This is creating additional complications.” Her words echo the reasoning stated in the regulation, published in the Official Journal of the European Union following the March vote: “In light of reports from healthcare professionals about the imminent risk of shortages of devices, it is necessary, as a matter of urgency, to extend the validity of [MDD] certificates.”
Philippe PereiraLegislative measures taken with mitigation in mind, in Switzerland
With a more regulated device landscape on the horizon, the Swiss Parliament voted to allow US Food and Drug Administration (FDA)-approved devices onto the market in Switzerland, in November 2022. Swiss Medtech were among the backers of this decision and shared in a press release from the time of the vote that “more than 1,000 of the approximately 5,000 foreign manufacturers have already stopped supplying Switzerland with their products—they are not prepared to meet the additional requirements for the limited Swiss market, and patients in Switzerland are the ones to suffer”. This statement summarises the challenges that many companies, health professionals, and others involved in the provision of healthcare by means of medical devices face now, with the MDR transition period already in motion.
Examining IR opinion
Philippe Pereira, an interventional radiologist and director of the Center for Radiology at SLK-Kliniken (Heilbronn, Germany), co-authored an editorial in December 2022 which looks ahead to the obstacles MDR will create for interventional


radiologists as the transition period ends and nonconforming devices are taken off the market.

Published in CardioVascular Interventional Radiology, the article warns that “taking devices with small profit margins, including orphan devices or devices for niche indications, such as those for many paediatric IR procedures, off the market instead of going through a costly and still uncertain rectification process has become an option.” The authors make the further point that this will increase the cost of devices that are recertified under MDR and put pressure on those manufacturers of surviving devices to increase their output. Should companies choose to apply for a recertification, Pereira et al set out their concern that “estimates of 13–18-month periods for the recertification could create a situation of safe devices becoming stuck in limbo between MDD certificate expiry and recertification, unavailable to patients and caregivers.” In their conclusion, the authors urge all
Continued on page 4
In March 2023, the European Council voted to extend the MDR transition
FEW ADVERSE EVENTS ARE connected to the use of inferior vena cava (IVC) filters when they are used to help prevent deep vein blood clots from developing into pulmonary embolisms (PE), according to the findings of the Predicting the safety and effectiveness of inferior vena cava filters (PRESERVE) trial, published jointly in the Journal of Vascular and Interventional Radiology (JVIR) and the Journal of Vascular Surgery Venous and Lymphatics (JVS-VL). The study and its findings have garnered attention, to the tune of presentations and discussions at some of the largest recent vascular and interventional radiology meetings.
PRESERVE is a multicentre, prospective, open-label, nonrandomised trial that studied the safety and efficacy of IVC filters from six manufacturers. It was a joint effort of the Society of Interventional Radiology (SIR) and the Society for Vascular Surgery (SVS), carried out in cooperation with the US Food and Drug Administration. PRESERVE was sponsored by the Inferior Vena Cava Filter Study Group Foundation—a foundation created by SIR and SVS to receive and distribute funds supplied by manufacturers to the contract research organisation and sites. The study was conducted at 54 sites in the USA between 10 October 2015 and 31 March 2019. During that time, filters were implanted in 1,421 patients, of whom 1,019 patients had an existing deep vein thrombosis (DVT) or pulmonary embolism (PE). Trial results suggest that IVC filters were effective in helping to prevent PEs in patients experiencing a DVT. Approximately half of the patients in the study had their filters removed within three months of placement, and only one of 23 incidences of PE occurred within the 30-day post-filter removal observation period, according to study authors.
“The question should not be only ‘should we place a filter?’ but ‘how should we offer comprehensive filterinclusive care of patients with venous blood clots, comprised of a detailed patient evaluation, a plan for retrieval after placement, and frequent followup with evaluation for filter removal or replacement,’” said Matthew S
Continued on page 6
New study demonstrates IVC filters “safe and effective” in treating venous thromboembolism
Interventional radiology: Beyond needles and images



Interventional radiology (IR) is unique amongst procedural disciplines because its ‘parent specialty’ is a diagnostic discipline that has no infrastructure for clinical practice. Charles Dotter, who performed the first angioplasty on 16th January 1964, recognised the risks inherent in this unique situation, stating: “If my fellow angiographers prove unwilling or unable to accept clinical responsibilities, they face forfeiture of territorial rights based solely on imaging equipment others can obtain and skills that others can learn.”

IR requires four sets of skills: first, its practitioners need to be able to interpret the radiological images that they need for their procedures. Second, they must have sufficient manual dexterity to master the necessary techniques. Third, they need to understand the pathology, physiology, and clinical aspects of the diseases that they encounter. Finally, they need to be able to assess a clinical situation and decide how best to treat the patient, sometimes quickly and based on incomplete information. The first two requirements pose no significant challenges. Image interpretation is the essence of radiology. And although not all radiologists are particularly dextrous, many have the practical skills for the performance of common interventional radiological procedures. Knowledge of pathology, physiology and clinical medicine is more problematic. In some countries, including the UK, substantial clinical experience used to be expected before beginning radiological training. In the 20th century, many British radiologists had a formal qualification in internal medicine before radiology training, but this is now unusual. As imaging became more complex, many training organisations sacrificed clinical experience in favour of more lengthy training in radiology. The ability to make swift decisions about treatment is a substantial challenge. Most diagnostic radiologists are thinkers and problem-solvers. Radiology attracts people who enjoy detecting abnormalities and using the related clues to suggest a possible diagnosis. This is a complex and immensely valuable skill and has placed imaging at the heart of modern medicine. Most radiologists have the mindset of a physician rather than a surgeon. A “surgical mindset”, however, is much more useful in IR, and not only because timely action is necessary in emergency situations. Diagnostic radiologists are not usually required to make decisions on clinical
Continued on page 6
Editors-in-chief: Professor Andy Adam, Dr Brian Stainken | Publisher:
Editor: Clare Tierney | Editorial contribution: Jocelyn Hudson, Will Date, Bryan Kay, Jamie Bell, Éva Malpass, Benjamin Roche, and Adam Pearce
Design: Terry Hawes, Wes Mitchell and David Reekie
Advertising: Michael Broughton michael@bibamedical.com
Subscriptions: subscriptions@bibamedical.com
If you have comments on this issue or suggestions for upcoming editions, write to clar












Interventional radiology: Beyond needles and images
Continued from page 2
are just as dependent on imaging as interventional radiologists but would find it impossible to serve their patients well without being able to practise as true clinicians.
Many interventional radiologists do not receive systematic training in all the procedures that they undertake in routine practice, especially the more complex ones. The disproportionate emphasis on diagnostic radiology training precludes the acquisition of sufficient clinical experience. The examination of the European Board of Interventional Radiology (EBIR) under the auspices of the Cardiovascular and Interventional Radiological Society of Europe (CIRSE) is a commendable effort but is a ‘voluntary supplemental examination’ which cannot be compared with equivalent tests undertaken by surgeons in their own disciplines. Interventional radiologists could point out that vascular surgeons undertaking IR procedures could be trained better, but that does not excuse the lack of a more robust system of training in IR.
The greatest responsibility for the failure of IR to establish itself as a real clinical specialty lies with institutions responsible for establishing curricula for training and holding examinations. The best decisions in medicine, whether large or small, are taken when considered from the patient’s perspective. Presidents and deans of radiological colleges should imagine that they are lying on a computed tomography (CT) table and are about to have percutaneous ablation of a small renal tumour. They have been asked to choose between two newly appointed staff interventional radiologists available to perform this procedure. One of them had two years of clinical experience, followed by three years of training in diagnostic radiology, which included studying subjects such as the appearance of unusual bone tumours, minutiae of mammography and details of interstitial lung disease. Then, as he was fortunate enough to train in a country where IR is recognised as a subspecialty, he studied this discipline for two years. This was far too short a period to master percutaneous ablation. This would be his first unsupervised procedure. The patient met this person only once, just before entering the CT unit, when informed consent was given. All previous clinical contact was through the patient’s oncologist, who is also going to be responsible for the patient’s care in hospital and the post-procedure follow up–an arrangement that can cause delays and confusion in dealing with recurrent or residual tumour. The second interventional radiologist has followed a curriculum established by a fictional college. After two years’ clinical training, she entered a dedicated course in IR, learning the aspects of imaging relevant to her chosen specialty. She studied, in detail, the procedures and equipment used in IR, and learned clinical skills, assisting her trainers with ward rounds and outpatient clinics. By the time she was appointed as permanent staff, she had carried out 20 percutaneous ablations. A primary clinical specialty of IR should have appropriate supporting staff and facilities, including dedicated CT equipment and other machines specially designed to guide procedures rather than provide images for diagnosis. Sharing CT units between diagnostic and interventional radiologists is as inefficient as running an outpatient clinic in an operating room. A more intense focus on the procedural and clinical skills required in IR would serve patients very well.
Continued from page 1
stakeholders to take action to mitigate the impact of MDR.
Stefan Weber, CEO of Cascination, gave his industry-specific take on the MDR situation to Interventional News. “Cascination started the transition to MDR early on and has already cleared several products under the new legislation. But I am sceptical MDR enhances patient safety as most products themselves do not change. I am certain it decreases innovation through an increased regulatory burden including product up-classification and everexcessive documentation.
“The approach of working with a system of notified bodies (over a central government agency) comes to a limit. On the one hand, different notified bodies potentially classify similar products into different risk classes therefore creating significant distortions in the market. On the other hand, notified bodies are under a significant conflict of interest between their for-profit orientation and their regulatory role. They grow at an alarming rate, with the costs being passed on to manufacturers, to hospitals and eventually to all EU citizens, either as taxpayers or health insurance purchasers.
“The system is largely out of balance; hence several European countries have to, or will, adopt accepting [US] FDA approvals. Manufacturers have stopped considering Europe as an attractive market. Unfortunately, as citizens, and future patients, we will see the full consequences only in a decade from now.”
Pedro Costa, who is CEO of Interventional Systems, also weighed in on his company’s response to the MDR and transition period. “Interventional Systems

perspective on the MDR situation when asked by Interventional News, which aligns with those of Pereira et al and Weber. Likening it to “an impending freight train coming down the tracks to a car stuck on the level crossing,” Morgan proceeds to provide context for his concern. “The requirement for medical device companies to secure approval based on data of usage for every single device in their inventory from the simplest guidewire to the most complex thrombectomy device via a very limited number of notified bodies seems unachievable, to say the least. Although originally intended to come into force for new devices next year, the EU seems to have kicked the proverbial can down the road by delaying implementation, but the problems have not gone away, they are just postponed.
“As interventional radiologists, we are already seeing limitations on the availability of devices that we need. It is often difficult to tell whether these are due to supply-side issues (container ships stuck in China, etc) or due to actual withdrawal of devices by companies from the market due to impending MDR. It is likely a combination of both factors. The effects of the MDR will inevitably adversely affect patient safety and patient care by restricting the devices available to interventional radiologists. This will initially impact on the availability of niche devices used in small patient groups.
“To mitigate the effects of withdrawal of devices from the market because of the MDR, interventional radiologists will do as they have always done—i.e. improvise using already-available devices used for other indications to get around problems. However, this is morally wrong in 2023, when we are meant to be improving patient safety, rather than risking it.”
In April 2022, MedTech Europe ran a survey of its industry members to assess the planned response to MDR among these companies. The Medical Devices Coordination Group task force on certification capacity monitoring—appointed by the European Commission and comprising members from all EU states— commissioned the survey, whose respondents number 475 companies in and outside the EU. Headline results include that “over half of all respondents plan portfolio reductions” and that those planning portfolio reductions “foresee on average 33% of their devices for discontinuation”.
Furthermore, the report states, “50% of respondents are deprioritising the EU market (or will do so) as the geography of choice for first regulatory approval of their new devices”.
has not been affected by the EU MDR challenges. We have been fully compliant since its first deadline, in 2021, and have already developed our secondgeneration robotic platform following the draft text. We have been fortunate as a company because our technological and clinical maturity allowed us to make no compromise on quality and compliance matters. As a Class I device manufacturer, we do not foresee a big impact for our patients and customers. The technology will continue to be available.
“As for the whole market, the extension is good news. It can alleviate the burden on highly innovative, early-stage companies in the space who would shift their focus to the USA or other fast-paced innovative geographies. And the companies and products will emerge on the other side of the extension better and safer.”
Robert Morgan, consultant radiologist at St Georges NHS Foundation Trust (London, UK) offered his


UK Government acts in response
There is also evidence to suggest that the impact of MDR is anticipated beyond continental Europe, which Morgan’s comment further supports. In February 2023, the UK’s Medical and Healthcare products Regulatory Authority (MHRA) shared in a press release that, currently, a CE-marked device can be placed on the UK market until 30 June 2023, but that “there are plans to extend acceptance of the CE-marking in the UK which, we will put into law in the coming months. We will publish guidance on this as soon as possible.”
In conclusion, the MedTech Europe survey data, and industry and interventional radiologists’ opinions in both continental Europe and the UK, suggest that the future impact that MDR will have is cause for concern. However, some companies, Interventional Systems being an example, have, thus far, been able to navigate the challenges posed by the new and tighter regulations on device safety and quality.
We are already seeing limitations on the availability of devices that we need.”ANDREAS ADAM Joint editor-in-chief
Will the MDR transition fall short of mitigating impact on IR and beyond?Robert Morgan Stefan Weber
















Continued from page 1
Johnson, an interventional radiologist and professor of radiology and surgery at Indiana University School of Medicine (Indianapolis, USA) and co-principal investigator on PRESERVE. “PRESERVE showed what questions we should ask as clinicians: ‘does this person continue to require protection against PE, and, in light of changing clinical status and available therapies, is the current filter needed?’ and then make an informed decision on how to continue care.”
David L Gillespie on the PRESERVE trial at VEITHsymposium 2022 “DVTs and PEs are a significant cause of death worldwide and understanding fully how tools like IVC filters can be used to prevent the progression of a DVT into a PE allow physicians to safely treat patients at risk of death from venous thromboembolism [VTE]” said David L Gillespie, a vascular surgeon at Beth Israel Deaconess Medical Center (Brockton, USA), and co-principal investigator on PRESERVE. “Now that the study is complete, we now have a
roadmap for better filter utilisation. We need to solidify a clearer set of practice guidelines for venous thromboembolic disease, based on its symptoms, location and complications. Further studies will focus on how the different manifestations of venous thromboembolic disease may benefit from filter-inclusive care.”
Speaking at VEITHsymposium 2022 (15–19 November, New York, USA), Gillespie outlined that “approximately ten years ago or so, the clinical management of patients with VTE and the prophylaxis of potential VTE in trauma patients was not well studied with regard to the use of IVC filters”. The result of the PRESERVE trial has been that “essentially, these filters are safe and effective for therapeutic [and prophylactic] use in the patient population [in question],” Gillespie continued, and this, despite the “challenges” of the COVID-19 pandemic, the “high dropout rate”, and the fact that “a large number of patients” had their filters removed.
PRESERVE and future directions discussed at SIR 2023
The Society of Interventional Radiology 2023 annual scientific meeting (4–9 March, Phoenix, USA), dedicated a session to examining the background, execution, and implications of this study for the future of VTE care. Johnson gave a presentation, of which one of the key takeaways was that, as he sees it, viewing VTE treatment as a question of “anti-coagulation versus filter [is] the wrong way to look at it”. He believes there is more nuance to it—“really, it is [a question of] anti-coagulate when
RESCUE trial shows reduction in segmental and main pulmonary artery occlusions
Robert A Lookstein, who is executive vice chair, Diagnostic, Molecular and Interventional Radiology at the Icahn School of Medicine at Mount Sinai Hospital (New York, USA) presented the results of a subanalysis of Thrombolex’s National Heart, Lung and Blood Institute (NHLBI)sponsored RESCUE trial during the latebreaking trial session at the Society for Interventional Radiology (SIR) annual scientific meeting (4–9 March, Phoenix, USA).
The core laboratory analysis of this investigational device exemption (IDE) trial demonstrated that pharmacomechanical catheter-directed thrombolysis (PMCDT) therapy using the Bashir endovascular catheter from Thrombolex led to a significant (71%; p<0.0001) reduction in segmental arterial occlusions after treatment, which correlated with the reduction in right ventricular to left ventricular (RV/LV) ratio (p=0.0026). There was also a significant reduction in main pulmonary artery (PA) occlusions (61%; p<0.0001) but this did not correlate significantly with the reduction in RV/LV ratio. The observed reduction in occlusions of both the
you can, use a filter when you have to, and get it out as soon as you possibly can”. Johnson acknowledged that there will always be patients who require filtration over a longer period, and in these cases, one might wish to remove the filter if it is “problematic—perhaps penetrating”, to then replace it with a new device.
Rounding off his time on the podium, Johnson asserted his stance on the efficacy of the IVC filter for VTE—“filters do prevent PE; I have no question that this study demonstrated this very well—[there was] a very low incidence of PE in a high-risk population”. He then ventured that where clots do occur in patients with filters placed, it could be that, rather than the filter having caused the clot, that its formation is “linked to patients’ underlying hypercoagulable state and contraindication to anticoagulation. It is not surprising that a person with VTE who cannot be anticoagulated develops another DVT, or a pre-existing DVT progresses. I do not believe that filters cause DVT.”
Rodney White (MemorialCare Long Beach & University of California Los Angeles, Los Angeles, USA) also shared his thoughts with delegates, from the SVS perspective. According to White, the core lab data yielded by the study will help inform guidelines, such as on how best to intervene to treat patients
main PAs and the segmental arteries explains why the overall reduction in PA obstruction as assessed by the refined Modified Miller Index is greater with the Bashir endovascular catheter than that which has been reported in contemporary thrombectomy or thrombolysis trials for the treatment of acute pulmonary embolism (PE).
The magnitude of effect of these other treatments on segmental arterial occlusions has not previously been reported.
The RESCUE trial is a prospective, multicentre trial evaluating the Bashir catheter in 109 patients with intermediate-risk acute PE at 18 sites in the USA. Of the 109 participants, 90% had elevated biomarkers and right ventricular dilatation. In the study protocol, the Bashir catheter was used to deliver 7mg of recombinant tissue plasminogen activator (r-tPA) into each PA over a five-hour infusion period, and 94% of patients had bilateral devices placed. The primary efficacy endpoint was the core lab-assessed change in the computed tomography angioplasty (CTA)-derived mean RV/LV diameter ratio at 48 hours (met for 107 patients), and the primary safety endpoint was serious adverse events, including major bleeding, at 72 hours. The median device placement time was 15 minutes, length of hospital stay, 2.8 days, and the number of patients seen at 30-day follow-up, 106.
“The RESCUE trial demonstrated rapid resolution of obstruction in the main, and especially segmental pulmonary arteries, with a <1% major bleeding rate. It is imperative that future endovascular PE trials assess the reduction in obstruction in more distal PAs since it has been shown that both the degree of residual PA obstruction and reduction in pulmonary vascular volumes, presumably due to reduced PA inflow, are significant predictors of late PE-related
with an IVC filter. He suggested the data will make it easier to find out “what parameters define filter penetration, what the incidence is, and what the consequences are and how to make it better. It may be that some devices are better than others”. A crucial question is what defines prophylaxis in the current treatment environment, White mused.
A further recommendation from White was that patients with IVC filters placed for VTE have a “dedicated case manager from the time treatment is initiated” so they can “stay in touch with the patient and their family”. Moreover, White made clear the importance of “dedicated IVC filter tracking systems” and filter removal clinics.
Concluding, White informed the audience that Gillespie will be compiling 24-month results for PRESERVE, which will include specific filter analysis, in turn having the potential to impact the definition of ‘prophylactic’ going forward. These longitudinal data will, White averred, “hopefully help [filter] manufacturers report and define indications with the [US] FDA”. Migration penetration will also be continually monitored in study patients, he added, before emphasising the “useful[ness]” of the SIR-SVS collaboration that led to the successful planning and execution of PRESERVE. The value lies, according to White, in being able to “get all stakeholders involved from the


mortality. This novel approach with the Bashir catheter and low-dose tPA represents a major advance in the treatment of acute PE,” said Lookstein.

During the late-breaking session at SIR 2023, Lookstein emphasised that the safety profile observed during the trial was “very favourable”. Of note, the presenter added, “even though the Bashir endovascular catheters were selectively delivered preferentially to the lower lobe circulations, the effect of the reduction in pulmonary artery occlusions […] was seen uniformly across the entire pulmonary circulation”. Summarising the mechanisms behind PMCDT therapy with the Bashir catheter, Lookstein proceeded to describe to delegates “the synergistic pharmacomechanical effect of this combination technology, which enhances the luminal gain seen with the activation of the nitinol basket, increasing the surface area of thrombus that is exposed to the fibrinolytic agent, led to greater efficacy. We believe this novel mechanism of action led to an increased number of segmental vessels having restored circulation with this treatment.”
Concluding, Lookstein answered a question about total procedure time, which he stipulated as having been approximately six hours as per protocol. He noted, however, that there may be potential for this to be reduced, but that this would necessitate prospective research in order to be validated. A further comment from one of the delegates present drew attention to the fact that it was “interesting” that RESCUE found the bleeding rate to be “lower” than in some mechanical thrombectomy trials.

This novel approach [...] represents a major advance in the treatment of acute PE.”
New study demonstrates IVC filters “safe and effective” in treating venous thromboembolismRobert A Lookstein Top: Matthew Johnson, David L Gillespie and Rodney White
Study finds PAE “highly effective” long-term treatment up to six years for enlarged prostate
Prostate artery embolization (PAE) provides long-term effectiveness in treating urinary symptoms from an enlarged prostate gland, according to new research that was presented among the abstracts of the year at the Society of Interventional Radiology (SIR) annual scientific meeting (4–9 March, Phoenix, USA).
In the largest long-term North American study, 1,000 patients who underwent PAE reported significant sustained relief, up to six years, from lower urinary tract symptoms (LUTS) or urinary retention due to benign prostate hyperplasia (BPH).
“Our study shows that PAE is a highly effective treatment whose long-term outcomes include sustained LUTS relief and significant improvement in quality of life,” said senior author Shivank Bhatia, chair of Interventional Radiology (IR) at the University of Miami Miller School of Medicine (Miami, USA). “Of 18 million men in the USA eligible for BPH treatment, many avoid all treatments because of the widely known risks of surgery, particularly sexual side effects and leakage. PAE avoids these risks while achieving longterm clinical results.”

With PAE, interventional radiologists inject tiny particles into arteries that feed the prostate gland, reducing its blood supply and thereby shrinking it. Researchers characterised the treatment as showing “great short- to mid-term results” and positive longterm outcomes in self-reported symptom relief. In a media briefing organised by SIR ahead of the annual meeting, Bhatia responded to a question on the nature of the particle used for his six-year study—”they are acrylic polymer coated with gelatine”. He added
that while the particles are permanent, as opposed to resorbable, they carry a positive charge, where blood is negative, thereby ensuring that they do not move through the bloodstream “to the brain, but stay within the organ itself”.
Participants reported dramatic improvements on the 35-point International Prostate Symptom Score, which ranks symptoms as mild, moderate or severe. Preprocedure, patients reported a mean score of 23, in the “severe” range. But in less than a year, they achieved a score of six, with “mild” symptoms persisting throughout the six-year study – a response similar to that following surgery for BPH. However, PAE does not negatively impact sexual function. Study participants were also asked a quality-of-life question: “If you were to spend the rest
of your life with your urinary condition just the way it is now, how would you feel about that?” Preprocedure, the mean score was 5 or “mostly dissatisfied,” but within a year, the score was 1, or “mostly satisfied,” a ranking that also continued throughout.
PAE has a well established safety profile, as shown in repeated studies in the 10 years since it was first used. But interventional radiologists said most men are unaware of this treatment option. Most will avoid surgery and may instead take medication for years, even as BPH worsens, potentially leading to bladder failure.
“Patients choose PAE to avoid the side effects of current medications for BPH, which can include erectile dysfunction, painful or difficult urination, constipation, dizziness or fatigue,” said the study’s lead author Andrew Richardson, a senior resident at Jackson Memorial Hospital (Miami, USA). “PAE is an alternative not just to surgery but also to lifelong medication.”
Among the study’s findings was a persistent, years-long reduction in prostate size. However, Bhatia noted that prostate size reduction is not the only goal in long-term effectiveness. “Treatment should make the prostate softer as well as smaller –as opposed to smaller but remaining hard, which will still cause urinary symptoms.”
Richardson and Bhatia encourage patients to learn about all options for enlarged prostate symptoms, talk to various physicians and then decide what is best for them. Bhatia says, “One size does not fit all when it comes to treating BPH.”
Bhatia also informed delegates at the SIR 2023 closing plenary session that they were going to continue monitoring of the patient cohort from their study so as to add the existing data on reintervention rates.

PAE is an alternative not just to surgery but also to lifelong medication.”Shivank Bhatia
SIR 2023 puts spotlight on Latin American IR

A session at the recent Society of Interventional Radiology (SIR) annual scientific meeting (4–9 March, Phoenix, USA) put the focus on the landscape of interventional radiology (IR) in Latin America. Members from the affiliate societies Sociedad Iberoamericana de Intervencionismo (SIDI), which is region-wide and the Brazilian Sociedade Brasileira de Radiologia Intervencionista e Cirurgia Endovascular (SOBRICE) took to the podium to speak about IR in their respective countries, and SIR’s International Division councillor Constantinos Sofocleous (Memorial Sloan Kettering Cancer Center, New York, USA) shared with delegates the initiatives that SIR has implemented to strengthen IR worldwide, including in South and Central America.
“OUR MAIN GOAL IS TO EMPOWER interventional radiologists, wherever they are, wherever they practise,” Sofocleous stated, including strengthening local IR societies under that umbrella. “Hopefully we are able to create targeted training programmes,” he expressed, as well as “increasing awareness of IR not only among referral services, but also patients”. Citing an example of an SIR initiative geared towards fulfilling these goals, Sofocleous spoke about the Give Back Project, from which Latin America has benefited in the past. “We approve a project that an affiliate society has identified as
an important programme for their country, in a specific disease or field,” the speaker explained. “In partnership with SIR, certain faculty members will go and create a programme for the local population, with local faculty.” An example of this project’s work was the symposium on uterine fibroid embolization in September 2019 in El Salvador, Sofocleous shared, labelling it a “great success” that “needs to be replicated […] now we are post-pandemic”.
In addition, Sofocleous listed the “exciting” SIR International Scholar Programme, which takes place every year to provide “outreach to young people interested in IR”. These efforts, alongside others from SIR, will help “raise our voice at a governmental level”, Sofocleous concluded.
Another speaker in the session was SOBRICE President Gustavo Pipoca Andrade (Hospital da Restauração, Recife, Brazil), who walked the audience through the current state of Brazilian IR, before highlighting the challenges his country faces when it comes to improving recognition of the role it can play in healthcare. “We have 24 [IR training] centres certified by SOBRICE,” Andrade relayed, emphasising that this homogenisation of the qualification took place in 2002. In terms of numbers of practising interventional radiologists, the speaker admitted that there is “a long way to go” in Brazil— they comprise only 3% of radiologists.
Regional differences make for “completely different realities” in terms of healthcare, Andrade went on to underline—under 10% of those living in the north of Brazil have private health insurance, whereas in the wealthier southeast region, for example, this figure is over 30%. Showing the audience a heatmap of interventions performed across the country, Andrade demonstrated these are concentrated in the higherpopulation areas, with the number of training centres distributed accordingly too.
All is not equal where US IR procedure access is concerned
Nima Kokabi (Emory Healthcare, Atlanta, USA) addressed the “uncomfortable truth” of healthcare disparities in the USA specifically within interventional radiology (IR) in a presentation at the Society of Interventional Radiology 2023 annual scientific meeting (4–9 March, Phoenix, USA). He referenced a Journal of Interventional Radiology (JVIR) publication from 2022 to share with delegates the extent of the disparities at play within IR, before putting forward suggestions as to why IR care is as unequally received as it is in the USA, and what interventional radiologists can and should be doing to redress the imbalance.
‘UNEQUAL TREATMENT’ IS A
2003 US Institute of Medicine report on implicit bias and racial disparities in medicine in the USA, that Kokabi began by highlighting. The presenter lamented the fact that the reality of implicit bias and healthcare disparities has not changed as much as one might have hoped in the 20 years since the report was published. In Kokabi’s view, it contains “uncomfortable truths” that he believes all healthcare providers should have awareness of. A key point from the report, he went on, is that “although Black people are disproportionately [affected] by poverty […] that alone cannot explain why they are sicker and have shorter lives compared to their
white counterparts”. What is more, “even if they have the same income, age, and severity of condition”, this is still the case. “The lower quality of healthcare is down to us as physicians,” Kokabi opined.
Beyond healthcare more widely, Kokabi then drew audience attention to a recent JVIR article that dissects the disparities that exist within IR in the USA. The article examines the unequal treatment that members of minority groups receive across different disease areas, but Kokabi chose to home in on those most relevant to his practice—these included uterine interventions and hepatocellular carcinoma (HCC). “If you are Black,
“As a society we have tried to introduce IR everywhere in Brazil,” Andrade asserted. “We have almost everything—yttrium [Y]90, reversible electroporation, hybrid suites—much like the USA”. Yet, awareness of IR is not as good as it could be, he admitted. With this in mind, SOBRICE has

launched several campaigns to improve understanding of IR procedures. These include holding social media livestreams during which patients can ask interventional radiologists questions and an annual course for medical students. Andrade homed in on the importance of helping students understand that IR is more than “stopping bleeding or treating a tumour”. The speaker proceeded to clarify that “in Brazil, we do have industry—we produce wires, catheters, sheaths, coils, filters, stents, and prostheses.” There is also a SOBRICE-published, Portuguese-language collection of IR textbooks available to interventional radiologists and trainees, Andrade added, before leaving the audience with the fact that “finally, in the big centres, we are established as a clinical service, but beyond the big centres, we are not known yet and that is the biggest challenge”.
you are two to three times more likely to undergo hysterectomy for fibroids [over embolization],” Kokabi relayed, adding that those in the Hispanic and rural-dwelling communities also experience a “significantly higher rate” of hysterectomy. This is further exacerbated if you are Black and live rurally, Kokabi shared. When it comes to postpartum haemorrhage, the same phenomenon occurs, according to the article—the aforementioned communities have a higher likelihood of hysterectomy as opposed to embolization, with “Asians suffering from the same trend,” Kokabi said. In terms of HCC treatment, the presenter then conveyed, “if you are Black or Hispanic, even adjusting for tumour stage, you are less likely to receive any treatment”. In addition, Black, Native American, and Hispanic patients are less likely to undergo certain IR procedures, such as transarterial chemoembolization (TACE) and thermal ablation. Black patients with HCC also have a lower survival rate, which, Kokabi explained, is due to “more fragmented care, lower screening rates, and less access to treatment”.
The disparities extend beyond race, the JVIR article details, to patients of a less favourable socioeconomic background. Those with non-private medical insurance are “less likely to receive IR treatments”.
Regarding finding solutions to the disparities present in IR care, the article recommends “identifying and understanding the underlying causes” first. “If you are a realist or pessimist like myself, you know that finding solutions is very difficult […] it is hard to intervene and be successful,” Kokabi lamented. “One thing that we could all do better with is implicit bias and we are lying to ourselves if we say we are not affected by it.” The presenter urged delegates to seek out implicit bias training, which, in his experience is “very eye-opening—you realise things that you may not have thought you do subconsciously”.
Equally, Kokabi advocated for “[trying] to learn about those who you have biases towards” and then “[engaging] in dialogue with them”. He sees it as “the least we can do [to] reduce the gap [in IR service access],” the reasons for which he sees as being multifactorial. Kokabi suggested that “a lack of uniform access” to IR services in the USA is at play, as well as a lack of understanding from healthcare leaders and insurance companies of the value of IR, which creates inequalities in access. “We are not working hard enough,” were Kokabi’s concluding words, encouraging interventional radiologists to “do a better job” of promoting what IR can offer patients of all demographics.
Awareness of IR [in Brazil] is not as good as it could be.”
Gustavo Pipoca Andrade
PAIRS 2023: “[Opening] the gate” to IR in the Middle East and North Africa
Rana Tarek M Khafagy is a consultant interventional radiologist based at Ain Shams University Hospital (Cairo, Egypt). In her capacity as head of the Pan Arab Interventional Radiology Society (PAIRS) residents, fellows and students (RFS) section committee, she sat down with Interventional News at the PAIRS annual meeting (11–14 February, Dubai, UAE) to discuss her journey into interventional radiology (IR), and how it is for those in training now, both in her home country and across the Middle East-North Africa (MENA) region.
“At my institution, we have one department, radiology and IR
[…] During your residency and fellowship you are obliged to do rotations in [diagnostic and IR],” Khafagy explained, setting the scene for the discussion. However, she went on, “when I entered in 2014, the IR department was not open to [all] the residents and fellows. There were no women at that time in the IR unit—I had wanted to have training at the IR unit since my first year in residency, however only a few seniors agreed to help me. I used to finish my daywork duties in the department then go and stay there [and observe].”
The significance of being a woman in IR in the MENA region
Khafagy proceeded to recount how most of those in the IR unit at the time thought that “she [would] get bored and leave,” but, as is evident now given her position, she did not. “Most of the consultants were not accepting women in the unit,” she elaborated, describing the situation as “very challenging”. Khafagy believes that this is due to stereotyping women as unable to cope with the stress of a specialty like IR and the on-calls that they bring, and as too squeamish to deal with blood.
“However, to be honest,” she conceded, “I did meet some male consultants who supported me, including my mentor.”
In 2021, “another woman in my class and I became the first [women] to be consultants at the IR unit,” Khafagy shared. “Our presence as residents and fellows and now consultants has encouraged many women after us to join the IR unit and has helped to open the gate to them—if you were to come to the department now you would see a lot of women training at the IR unit.” Khafagy illustrated how much of the initial negativity towards female interventional radiologists at her hospital has dissipated since—women are now “welcomed” and “no one is offending [us], no one is avoiding [us]”.
On the subject of the IR procedures that she specialises in, Khafagy emphasised the importance of being
skilled in all of them, not only in women’s health-related procedures. For example, she does prostate artery embolization, and bronchial artery embolization, presenting on the latter at PAIRS 2023. However—and this is a point that was echoed in an information session later on during the meeting, on routes into IR in the MENA region—there is a particular demand in the region, given the religious and cultural environment, for female interventional radiologists, as female patients often require their doctor to be a woman. Therefore, women’s health procedures, such as uterine fibroid embolization make up more of a female interventional radiologist’s caseload than they do a male’s in the region.
Training in IR in the MENA region
Khafagy then moved on to discuss her role in PAIRS’ RFS section—“the team is very active and there are also many
females on the team.” Team members are “mainly from Egypt, Saudi Arabia, also from Algeria, Syria, Qatar, UAE and Morocco—many countries,” she detailed. There are even members involved in the section’s activities despite currently being based outside of the MENA region—“the UK, USA, Canada and Germany,” she added.
This prompted the question of whether she had spent time during her training outside of Egypt—“I spent a few months in the UK,” she replied. Contextualising this fact, she explained that it is “not that common to do fellowships abroad in Egypt” but more common in Saudi Arabia and the UAE. “Officially, in the UAE they do not have an IR training programme. So they have to go abroad, do their training and come back as a consultant.” The implications of this reality were addressed in the aforementioned information session— attendees expressed their concern that interventional radiologists-in-training often leave the region for an IR programme and do not return. Khafagy shed further light on this subject, clarifying that it is mainly in Saudi Arabia and Egypt, of all the MENA countries, that trainees embark on IR training.
Khafagy then segued into addressing awareness of her specialty in the MENA region—“Maybe five, six years

ago, if you asked medical students [in the region] if they knew anything about IR, they would definitely say no. As for now, I cannot say that everyone knows about it, but I believe they have heard about it. And this is very important regardless of the specialty they will go into eventually —they need to know about IR so they can refer patients.” The progress towards more widespread recognition of IR in the MENA region is, in part, due to the efforts of PAIRS, who “had a vision” that involved a focus on “promotion” of IR. An example of this is the ‘I am PAIRS’ campaign done in several Middle Eastern countries, for which Khafagy is a regional leader in Egypt, she shared. This has centred around gathering students at a dedicated event “so that [medical students] would know about [IR]”. Many of the students were “amazed, giving very good feedback,” Khafagy supplemented.
PAIRS’s residents, students and fellows focus
The inspiration for tailored RFS initiatives came from “peers at the Society of Interventional Radiology [SIR] and Cardiovascular Interventional Radiological Society of Europe [CIRSE],” Khafagy went on to say. The committee itself started as “just a little chat”—with Ayah Megahed (Yale New Haven Hospital, Bridgeport, USA). “She is a colleague of mine training in the USA and she is working for the SIR RFS. She said to me, why do we not have something like this for PAIRS?” Khafagy relayed by way of an origin story for the section. They agreed that the concept had “very good potential,” given the success of the US and European counterparts. “Being interested in working with the juniors and as a regional leader in Egypt of ‘I am PAIRS’, I spoke to Ayman Al Sibaie [Rashid Hospital, Dubai, UAE], the president of PAIRS and Karim Abd El Tawab [also Ain Shams University Hospital], the secretary,” Khafagy recounted, the PAIRS board was supportive and thus the PAIRS RFS section came into being. “I led it when I was a fellow and still [am leading it],” she added.
“Our vision, which is matching with PAIRS’s vision ‘Investing in Youth’ is mainly to increase awareness of IR among students and to support the residents and fellows because in a lot of countries, they are also involved in diagnostic work […] so we are working to encourage them [towards IR],” Khafagy summarised. Also of central importance to her though, as reflected throughout the discussion, is boosting the image of women in IR in the MENA region. She celebrated the fact that the section members say they “see many women presenting—this enhances their vision of women being able to [work in IR].” The goal is to continue what the section has achieved to date with supporting the students and juniors, Khafagy concluded.
Officially, in the UAE they do not have an IR training programme.”
Rana Tarek M Khafagy
Cement and screws: The importance of building (and formalising) evidence on MSK metastases
At the Society of Interventional Oncology (SIO) annual scientific meeting (19–23 January, Washington DC, USA), Sean Tutton (University of California San Diego Health, San Diego, USA) presented evidence on treatment for skeletal metastases, while urging those involved in these patients’ care, as well as collecting data on their experiences, to “harmonise the nomenclature” they use to optimise data and care quality.
Tutton began by suggesting that a reason for inconsistent terminology where bone cancer treatment is concerned, among interventional radiologists, is that it is a “young” part of the interventional radiology (IR) space. “We need to start talking about skeletal-related events—both the cancer as well as the cancer therapies are having a significant impact on the skeleton,” he urged. An example of why this issue is relevant for interventional radiologists, which Tutton gave, was that of a post-menopausal patient who, after chemotherapy, underwent “an 8% year-on-year bone loss”. This increases the risk of fracture, the speaker underlined.
Moving on to focus on pelvic metastases specifically, the presenter noted that they are the second most common type of skeletal metastasis after spinal. In Tutton’s view, it is crucial to understand that patients with cancer metastatic to the pelvis may experience
different types of pain—mechanical pain is not the same as bone-tumour interface pain, which, in turn, is not the same as neuropathic pain. “We address them differently,” Tutton emphasised.
Likewise, there are different classifications of disease stage depending on the type of skeletal metastasis. In the pelvis, the Harrington scale runs from one to four, with complete pelvic discontinuity at the end of the gradation, Tutton informed delegates. Treatment for these metastases differs based on the classification—Harrington 1 is “ablation alone”, 2 is a combination of ablation and osteoplasty, and for profound Harrington 3 and 4, the preferred treatment modality is “osteosynthesis, which is a combination of cement and screws,” the presenter outlined.
Tutton proceeded to run through the biomechanics behind using cement and screws, stating that he and IR and orthopaedic colleagues had seen in their experience that using screws alone is “very similar to not treating at all”. While “cement alone only deals with compressive forces”—and the pelvis also has to be able to deal with “bending, sharing and tortional forces,” Tutton detailed—cement and screws work in conjunction with one another to “shift the load-bearing away from the bad bone to the good bone”. He supplemented this by saying that “the key concept is that you are fixing bicortically if possible”. With the two materials combined, you achieve “the highest stiffness and greatest yield strength”. A further point Tutton made was regarding working with orthopaedic colleagues and how there, uniform nomenclature is key.
The speaker was keen to highlight that the cement plus screw combination is for progressive disease, with Nick Kurup and Matt Callstrom having reported on their experience with Harrington 1 and 2 lesions.
SBRT could be an “effective” treatment for patients with lung neuroendocrine tumours
Researchers at Moffitt Cancer Center (Tampa, USA) are investigating new treatment approaches for the primary lung neuroendocrine tumour patient population. In a new article published in the International Journal of Radiation Oncology, Biology and Physics, a team of physicians, led by Daniel Oliver and Stephen Rosenberg, suggests that stereotactic body radiotherapy (SBRT) could be an effective treatment for patients with early-stage lung neuroendocrine tumours.
SBRT IS A TREATMENT approach that delivers high doses of radiation to precise areas of a tumour, minimising damage to surrounding normal cells. Patients receiving SBRT often have less toxicity and sideeffects compared to treatment with conventional radiotherapy that is delivered in smaller doses each day over several weeks.
“SBRT is commonly used as a treatment for early stage non-small cell lung cancer, and our results show strong tumour control. This suggests that SBRT may also be effective
for lung neuroendocrine tumours,” said Oliver, assistant member of the Department of Radiation Oncology at the Moffitt Cancer Center. “In fact, SBRT is increasingly being used to treat early-stage lung neuroendocrine tumours in clinical practice, despite the lack of consensus recommendations for this approach and very limited data on its effectiveness and toxicity in lung neuroendocrine tumour patients.”
Because of the lack of data, Oliver and his team wanted to assess the efficacy and long-term outcomes of SBRT in patients with lung
Tutton labelled their use of balloon-assist osteoplasty and ablation as a “very novel way of dealing with periacetabular lesions”.
Regarding the body of data that exists within IR for treating skeletal metastases, Tutton acknowledged that there are “a lot of great retrospective data,” which help interventional radiologists build their “toolbox” and stipulate how to use cone beam computed tomography (CT), how to plot navigation lines and how to improve accuracy.
Speaking on his and colleagues’ experience, Tutton averred that the aforementioned pelvic procedures are “safe”, with no significant blood loss or infection reported. Following treatment, the patients he studied saw an improvement in terms of function and narcotic use. At one-year followup, the presenter shared that they were able to obtain “good data” on 42 of 105 participants—“we are in the process of reporting,” Tutton told attendees.
“The value” of studies like his is that “as we treat these patients and they survive, which is great […] 43% will need some form of additional procedure—you are going to need to see these folks [again],” was one of Tutton’s main messages for the audience. In order to add to their value, he opined that there needs to be, again, “harmonisation” of the outcome metrics, patient-reported and otherwise, “so that when we publish we all speak the same language”. In conclusion, Tutton expressed how patients living longer with pelvic metastases is a “huge win”, but that in order to give them the best possible quality of life, it is necessary to continue along “the right track” that IR is on with evidence surrounding osteosynthesis. “Skeletal metastases are common and devastating for quality of life,” so harmonised evidence reporting and use of nomenclature will contribute to “[allowing patients] to continue their cancer therapies and to get walking and actually enjoying life”.
3 6 9 YEAR YEAR YEAR 97% 91% 91%
Local control rates with SBRT
neuroendocrine tumours. They performed a retrospective analysis of 48 lung neuroendocrine tumours from 46 patients who were treated with SBRT from 11 institutions across the USA. The researchers discovered that SBRT provided strong local/regional tumour control—the three-, six-, and nine-year local control rates were 97%, 91%, and 91% respectively, and only one regional recurrence occurred. The treatment was also well tolerated with only one case of SBRT-related toxicities reported, which was considered low-grade.
“The current study is the largest and first multi-institutional series evaluating local control, toxicity and dosimetric outcomes with SBRT for early-stage lung neuroendocrine tumours. Our results suggest that while surgery provides excellent outcomes, SBRT should be considered another treatment option for this patient population,” said Rosenberg, study senior author and director of magnetic resonance imaging-guided radiotherapy in the Moffitt Cancer Center’s Department of Radiation Oncology.
As we treat these patients and they survive, which is great […] 43% will need some form of additional procedure.”
How dogs with seizures inspired novel neuro-oncology trial
On day two of the Pan Arab Interventional Radiology Society annual meeting (PAIRS; 11–14 February, Dubai, UAE), Riad Salem (Northwestern University, Chicago, USA) took to the podium to give insight into a new frontier in interventional oncology (IO)—yttrium 90 (Y90) microspheres to deliver targeted radiation to glioblastoma (GBM). Drawing on experience treating liver cancer in such a way, Salem introduced delegates to how this neuro-oncological concept came about and informed them of the currently recruiting FRONTIER trial—a feasibility study to evaluate the safety of the Therasphere GBM device in patients with recurrent GBM).
SALEM BEGAN BY CLARIFYING for the audience that the glass Theraspheres (Boston Scientific)
“are not an embolic-type therapy”, as some microspheres are, but rather, they deliver Y90 radiation. “Now the natural discussion [point would be] what about external beam radiotherapy [for GBM]?” Arguments against this approach, Salem countered, include the fractionated nature of the radiation, with multiple treatments, as well as the dose limits, “depending on how much brain you want to expose.” Nontarget radiation is, equally, a reason that limitations exist in external beam radiation, the speaker added. On the other hand, he acknowledged that radiotherapy delivered transarterially can “precisely deliver” radiation exactly as predicted by cone-beam computed tomography (CBCT). There are “no major issues with adjacency to other structures, so that provides you with a therapeutic option”.
“What have we learned in the liver?”
was Salem’s rhetorical question that reflected the subject of the session as a whole—IO outside the liver—and the answer was that “we can see exactly where [the Y90] has been deposited”. This means that one can accurately predict where necrosis will occur, the presenter explained, “in contradistinction” to external beam radiotherapy, which applies radiation to a “much larger area”. Applying these learnings in an area of “unmet need” is how the FRONTIER trial came about, as, Salem noted, “there are between 10,000 and 12,000 GBM cases in the USA and treating these patients can be “quite challenging”.
“One of the goals of treatment, initially, is debulking the tumour,” Salem went on, adding that unlike in the hepatic and other spaces, “R0 resections are rare because you want to limit how much brain you take out.” Recidivism around the area of resection is the result, the speaker detailed. “And there really are very few treatments that
are effective and accepted secondline standards of care,” according to Salem—“you can re-resect, re-radiate, but there is no protocol”.
“So, the options that we currently have are surgical,” but as seen on flare images with magnetic resonance imaging (MRI), “there is [often] disease around the tumour”. Whether micrometastases or oedema, there is “a challenge” associated with dealing with this in addition, according to Salem. “How much are the surgeons going to resect?” The need to cover this larger zone also means that external beam radiotherapy comes with the risk of non-target radiation, the speaker supplemented. Recurrence and recidivism are problems in this disease condition no matter the approach, in Salem’s opinion.
“Credit is due to the Hopkins group, who completed a six-canine study on

Why IR innovation need not cost the world: A global solution
The keynote lecture on day one of the Pan Arab Interventional Radiology Society annual meeting (PAIRS; 11–14 February, Dubai, UAE) advocated a simultaneously global and local approach when it comes to conducting research in interventional radiology (IR), and when innovating. Jafar Golzarian (University of Minnesota, Minneapolis, USA) talked delegates through the rationale for basing ideas for research and new medical devices or products on what is already familiar— or ‘local’—while bearing in mind that international collaboration with societies and individuals from other geographical regions can lead to more cost-effective innovations.
CITING THE USA AS AN EXAMPLE OF A country that invests a relatively large proportion of
According to the speaker, “it takes somewhere between US$5 and 10 million to get a US Food and Drug Administration [FDA] 510(k) class II approval” for a new medical device, hence the need, he believes, for a new way of innovating and researching in healthcare, and more specifically the IR field.

Golzarian conveyed his optimism despite this high financial burden on innovators—“innovation does not have to come with a cost”. Illustrating this, he cited the Fairembo concept—the use of suture fragments as an embolic—which is “feasible, safe” and “inexpensive”. With this in mind, Golzarian
dogs having seizures,” the presenter went on to say, which “opened the door” to using Y90 for GBM. Compared to humans, dogs’ cerebral anatomy does not allow for “selective injections” when delivering the Y90, yet, Salem shared, “the dogs were able to tolerate these hemispheric treatments”.
Regarding the FRONTIER trial, Salem confirmed that “in humans, of course, we want to get much more selective, and this is something we will be able to share once data start coming out”. In the Hopkins study, “all canines demonstrated initial reduction in tumour volume” and therefore, it is proof of concept, the speaker summed up.
“The FRONTIER trial is open and recruiting,” Salem told the audience, conceding that he was unable to divulge much more about the trial’s progress. Summarising the use of Y90 for GBM, the presenter relayed that “imaging is much more critical than in hepatic space and there is a level of cerebral vascular complexity that does not exist in the liver”. There are challenges to applying this product in the brain, such as the need to “re-engineer the microspheres” so as to use fewer than in the liver, however, “there is a lot of excitement [including] at the prospect of treating meningiomas [in the future]”.
urged budding innovators among the delegates to ask themselves “how can [their idea] help other people across the globe while being affordable?” Posing questions, he continued, is “important for the younger generation”, as is getting “frustrated” and “out of your comfort zone”, as this can often lead to finding a solution to the clinical problem that has elicited the questions and frustration in the first place. The solution, Golzarian supplemented, as exemplified by Fairembo, is to “always consider cost” and “material availability locally”. This being said, it is key not to sacrifice quality, were the presenter’s final words on innovation, before transitioning to speak on the similar issue faced by those wishing to pursue research—the high cost of doing so.
“Usually what people think,” the presenter averred, is that research is not worth their while—because of a “lack of ideas”, but also sometimes because they consider it to be too time-consuming and expensive. However, Golzarian assured, “research is not as complex as we think […] we need to demystify [it].” Conceding that multicentre, randomised trials are valuable, the speaker opined that, in IR, what is “probably most significant is real-world research”, but that knowing the outcomes of one’s procedure
The dogs were able to tolerate these hemispheric treatments.”Jafar Golzarian Continued over page
is vital. “Reflecting on complications is a very good start,” Golzarian shared.
Addressing the younger interventional radiologists in attendance once again, the speaker advocated for beginning a research endeavour with the procedures “you perform the most”, as well as doing a “thorough literature search”. Then, “you can start to fill the gap” if there seems to be one in the existing evidence. Golzarian then returned to a previous point—that “cost should always be a consideration”. This may prompt research into cheaper materials that could substitute those used currently, and, even better, those which could be “useful globally”.
A personal anecdote led Golzarian to emphasise
how crucial cost and collaboration considerations are when it comes to research—over the last 10 years, he has sought to conduct a trial with 110 patients
What the BCLC guidelines have omitted
Sarah White (Medical College of Wisconsin, Milwaukee, USA) opened the liver interventional oncology (IO) session at the Pan Arab Interventional Radiology Society (PAIRS) annual meeting (11–14 February, Dubai, UAE) with a presentation that set out what she believes to be the salient points of the latest Barcelona Clinic Liver Cancer (BCLC) guidelines. Last updated in early 2022, White emphasised the fact that “many key aspects of hepatocellular carcinoma [HCC] treatment are still missing”, including combination therapy with transarterial chemoembolization (TACE) and ablation and transarterial radioembolization (TARE).
White began by outlining a “historical overview” of the BCLC guidelines. “Initially published as a prognostic system in 1999,” it was not “designed” to stage liver cancers, the presenter shared with attendees. Neither was it formulated using “guideline methodology,” White added. “Many recommendations are not supported by high-quality data.” Other limitations include metastatic and nonmetastatic patients being combined into one category and treatment modalities “not [being] unique to disease stage,” White furthered, before stating that BCLC oncologic outcomes “are worse than other staging systems”. Providing a counterexample, White stated that the National Comprehensive Cancer Network (NCCN) guidelines, which have a “strict policy of who sits on the committee” and a “strict conflict of interest policy”, as well as a “methodological way to review all of the data [it deals with]”.
Nevertheless, the most recent update to the BCLC guidelines is “much more” in-depth compared to the first set, “largely because now we have nine drugs that we did not have in the past,” White attested.
What is new in the guidelines?
A first example of the 2022 additions is the focus on the “potential candidacy for liver transplantation” for patients with early-stage malignancies,
which, White said, before had “never really been put in the guidelines”. Within the scope of this addition are recommendations on eligibility for transplant and alternatives for those who are not suitable, for reasons such as heart disease, for example, the presenter relayed. “Ablation is really frontline for a patient who is not a transplant candidate, whereas before, it was resection that was frontline,” White said, expanding on the latest change to advice. Now, the consensus is that ablation and resection are “really on a par”, according to the speaker, with some concerns surrounding recurrence after resection, which was not the case two decades ago.
Next, White addressed what the guidelines now recommend for patients unable to have any of the aforementioned treatments. “You will see that the algorithm recommends TACE and TARE. What this really is talking about is when you cannot do ablation because of the location of the tumour.”

For stage B liver cancers, White proceeded to convey to delegates, “instead of having one category there
comparing prostate artery embolization [PAE] to a sham procedure. Despite generous funding from the Society of Interventional Radiology (SIR) Foundation, Golzarian admitted that “we could not find enough money”. With this in mind, the presenter concluded that he was “sure” that current prohibitive costs associated with research and innovation need not continue to pose a barrier to entry for aspiring investigators and innovators— rather it is a case of harnessing this issue creatively to seek a solution in international collaboration. The status quo is “not sustainable,” the speaker reaffirmed, and that this necessitates a “change in the landscape”.
are now three. There are now multiple treatment approaches, whereas it used to be straight to chemoembolization.”
The speaker also noted that for patients in this category, overall survival used to be 20 months with the old guidelines, but this is now “up to five years”. In summary, “no matter what [treatment you receive] the outcome is much better than it used to be,” White celebrated.
There is now also a “vast difference” when it comes to treatment guidelines for advanced-stage liver cancer, White said, elaborating by saying that “before, with portal vein invasion and metastatic implants, sorafenib was our only choice”. Overall survival was 11 months, whereas it is now greater than two years for these patients, the speaker underlined.
And what is missing?
“So, what did they fail to include?” White moved on to answer her own question, emphasising that one “really important” omission is the use of prospective data to compare ablation directly to resection. Moreover, she added, “the difference between ablation modalities—maybe that does not matter as long as you are in good hands, but there is no differentiation” between using a particular modality in a patient, versus choosing another.
“They [also] did not talk about liver-directed therapy [LDT] as a bridge to liver transplant,” White lamented. “At my centre, it is an 18-month waiting period,” she explained, going on to say that waiting for a patient with 3cm HCC for that duration may take them outside of the transplant criteria—LDT can ensure they remain eligible, on the other hand. LDT is also an option for those who are not on the transplant waiting list, White went on, as it can confer an increase in overall survival, yet this too is not referenced in the 2022 update. Likewise, LDT in
the setting of advanced or extrahepatic disease—the guidelines recommend “systemic therapy only”, the prudence of which in the context of an isolated lesion White invited the audience to question.
Adding to her list of important omissions in the most recent iteration of guidelines, White stated that radiation segmentectomy “either by itself or in addition to ablation” would have merited inclusion as “we have some pretty good data surrounding that”. Similarly, TACE and ablation for lesions over 3cm—“I do not think that anyone in this room would use a [single modality alone]” on a lesion greater than 3cm, White averred.
“They do not even talk about stereotactic body radiation therapy [SBRT], or the different TACE modalities. Drug-eluting beads are not the same as conventional TACE. And there is no stratification of when we should be using which one,” White continued. “[Neither do they] talk about radioembolization in the setting of intermediate disease [although] there are really good data,” the presenter said, rounding off the section of her presentation addressing the 2022 edition omissions.
On a final note, White acknowledged that “[failure] to mention any kind of combination therapy is likely because there are still data coming out—with many trials in the pipeline”. The speaker anticipated that the release of new data will continue to “drastically change the BCLC guidelines,” which, while evolving in line with research findings, “has many limitations as a staging system”.
They did not talk about LDT as a bridge to liver transplant.”
It takes somewhere between US$5 and 10 million to get a US Food and Drug Administration [FDA] 510(k) class II approval.”Sarah White
Registry reinforces safety, efficacy and efficiency of radial access in visceral interventions in embolization procedures
The final results of the RAVI prospective registry study demonstrated the safety and efficacy of radial access in visceral interventions in standard embolization procedures for uterine fibroids, benign prostatic hyperplasia, and hypervascular tumours. The findings of the Terumo Medical-sponsored study were presented at the Society of Interventional Radiology (SIR) 2023 annual scientific meeting (4–9 March, Phoenix, USA).
The results of the RAVI registry—the largest, prospective, multicentre, observational study in vascular and interventional radiology (VIR)— were shared on behalf of study investigators by Marcelo Guimarães, professor of radiology and surgery, Division of Vascular and Interventional
Radiology, Medical University of South Carolina (MUSC; Charleston, USA). It showed that radial access (RA) can be used as the primary access site for relevant and emerging embolization procedures, regardless of disease state (benign or malignant).
Of the 105 patients screened for the study, 99 were successfully enrolled in six US hospitals and treated between February 2020 and January 2022. In addition to MUSC, the other leading IR centres that participated were: Mount Sinai Hospital (New York); St Louis University (St Louis); University of North Carolina at Chapel Hill; Rush University (Chicago); and the University of California, Los Angeles.
74.7%
complications, stroke, myocardial infarction and death at 30 days. The procedural endpoint was defined as successful completion of the intended procedure using RA (i.e. without femoral bailout), which was achieved in 100% of patients. Technical success was 100%, defined as the successful embolization of the target lesion/organ. This prospective registry confirmed the safety and efficacy of RA at 30 days’ follow-up in visceral embolization procedures. Of the 99 patients in the study, 74 (74.7%) were able to be discharged the same day of their procedure, demonstrating that RA for embolization procedures can create efficiencies in cost management. In addition, newly presented one-year results focus on 70 patients where UFE was performed. The data showed that transradial UFE allows for fast recovery, low risk of bleeding and other complications, and demonstrates sustained increase in quality of life.
The primary safety endpoints included RA-related
Injectable tissue provides significant, long-term relief for chronic back pain
A minimally invasive treatment that injects allograft disc tissue into the spine to relieve pain associated with degenerative disc disease provides significant improvement in pain and function over a sustained period, according to new research presented at the Society of Interventional Radiology (SIR) annual scientific meeting (4–9 March, Phoenix, USA).
THE TREATMENT, KNOWN AS viable disc allograft supplementation, injects specialised cells and fluid into a patient’s damaged disc. The cells of the injected fluid encourage the cells in the damaged disc to regenerate with healthy tissue.
“The significant improvement in pain and function is promising for patients living with chronic low back pain—a condition that can greatly impact a person’s quality of life,” said lead author Douglas Beall, chief of radiology at Clinical Radiology of Oklahoma (Oklahoma City, USA). “This treatment may help patients return to normal activity for a longer period of time.”
Fifty patients at nine sites participated in this three-year voluntary extension of the randomised controlled ‘Viable allograft supplemented disc regeneration in the treatment of patients with low back pain’ (VAST) trial, with 46 receiving allograft treatment and four receiving saline. The treatment group was similar to the patient population at the start of the trial in age, sex, race, ethnicity, body mass index and smoking status. Pain levels were evaluated using the visual analogue scale and functionality was measured using the Oswestry Disability Index (ODI).
Sixty percent of patients who received allograft treatment for chronic low back pain reported a greater-than-50% improvement in pain and 70% of
patients reported more than a 20-point improvement in their ODI scores. There were no persistent adverse events reported.
“Existing treatment for chronic low back pain due to degenerative disc disease is often ineffective or the effects are short-lived,” said Beall. “We need better treatments for this condition since conservative care is not providing the long-term outcomes that patients deserve. Injectable allograft treatment might be the answer for many people.”
Use of allograft could even help decrease opioid use among patients with chronic low back pain, researchers said, which would be especially meaningful for younger patients who have years of function and quality of life to look forward to. In a media briefing held by SIR ahead of the annual meeting, Beall expanded on this to say that the treatment’s potential impact is “huge”, as this type of chronic back pain is “maybe one of the most common disease processes known to man”.
LEAD RESEARCHERS
“We are proud to announce the oneyear results from the biggest cohort of patients where UFE is performed using radial access,” said Guimarães. “Safety and effectiveness of this procedure, as shown in this study, should affirm our belief that radial access could become preferred for all common embolization procedures.”
Clifford Weiss and Daniel Giraldo Herrera (Johns Hopkins University School of Medicine, Baltimore, USA) presented their recent bariatric arterial embolization (BAE) study at the Society of Interventional Radiology (SIR) annual scientific meeting (4–9 March, Phoenix, USA). Their research found that the procedure was associated with “significant” weight loss that did not affect muscle mass, as detected by whole-body magnetic resonance imaging anthropometry. The authors note in the study abstract that the purpose of their research was “to evaluate the early effects of BAE on multicompartment fat and muscle body composition”, which constitutes the pilot phase of the BEATLES trial (bariatric embolization of arteries with imaging visible embolics).
BEATLES is a US Food and Drug Administration (FDA)-approved, physician-initiated investigational device exemption (IDE) study that, Weiss, Herrera, et al stipulate in their abstract, “evaluates tightly calibrated 100–200μm radiopaque microspheres” (BT-001933-01, Boston Scientific). Adult participants with obesity—defined as those with a body mass index [BMI]≥35 kg/ m²—were scanned at zero (baseline),
three, and six months post-BAE from neck to knee using a Siemens Skyra 3T magnetic resonance imaging (MRI) scanner. The researched employed a dual-echo Dixon waterfat vibe protocol, and a single-slice multiecho Dixon proton liver density acquisition.
Anthropometrics were gathered using AMRA Researcher (AMRA Medical), a semi-automated cloudbased MRI segmentation tool, and statistical testing was performed via repeated measures correlation (Rrm).
Regarding the results, the researchers shared in their write-up that seven patients (six female, one male) with a mean age of 39.6±11.0 years and Centers for Disease Control and Prevention-defined class II–III obesity underwent BAE. At zero, three, and six months, mean body weight was 125.9±24.4, 113.5±21.2, and 110.7±23.3kg (Rrm=-0.694 [95% confidence interval (CI) -0.921–0.113], p value=0.012). Weight-tothigh muscle volume ratios were 10.3±1.9, 10.0±0.5, and 9.2±1.3 kg/L (Rrm=0.89 [95% CI 0.64–0.97], p value =0.001), respectively. Weiss, Herrera, et al were able to conclude that “BAE with 100–200μm microspheres is associated with significant postprocedural musclesparing weight loss via subcutaneous and intramuscular fat reduction.”

Injectable allograft treatment might be the answer for many people.”
Bariatric arterial embolization associated with “significant” muscle-sparing weight loss
Percentage of patients in the study who were able to be discharged the same day of their procedure
ET2023
EUROPEAN CONFERENCE ON EMBOLOTHERAPY


June 21 – 24, Valencia | Spain
Join us for the embolotherapy congress of the year !


ET 2023 will unite interventionists from around the world for the most comprehensive knowledge and data exchange in embolization treatment.

Register now to secure your spot at ET 2023 and catch the early fee !
Browse the full programme and put together your personal itinerary.
Your stay in Valencia
Located on Spain’s beautiful Costa del Azahar, Valencia unites the best of Spain’s rich history and avantgarde architecture. Not to mention its world-famous paella !
Accommodation
CIRSE’s travel partner, Kuoni Tumlare, has secured a great number of hotel rooms near the congress centre for ET 2023 participants and offers an easy-to-use booking tool.
Getting there
Attendees of ET 2023 can enjoy reduced rates when traveling with the Lufthansa Group. Scan the QR code to get the discount code !
New study examines extent of interventional radiology recognition among US public
The Journal of Vascular and Interventional Radiology (JVIR) published a paper in January 2023 examining the potential barrier that the name of the interventional radiology (IR) specialty poses to the US public’s understanding of the role of interventional radiologists. Mina Makary et al (The Ohio State University Wexner Medical Center, Columbus, USA) found that “less than half” of those surveyed were able to identify interventional radiologists as doctors. Their findings also revealed that most IR referral patients who ended up having surgery “stated that a lack of IR awareness played a role in their decision”. The authors make recommendations in their paper, titled ‘Public awareness of IR: Populationbased analysis of the current state and pathways for improvement’, of how to improve recognition and understanding of IR among the general public, which include patient education delivered by primary care providers.

The authors embarked on the study in order to “evaluate IR awareness among the public and identify methods for improvement”. One thousand participants responded to 69 questions anonymously on Amazon’s Mechanical Turk crowdsourcing platform, which required either Likert Scale or free text answers. The authors justified their choice of platform “to obtain a more accurate and reliable assessment of the current rate of IR awareness”, compared to previous study samples. The questions prompted respondents on their “medical and IR-specific knowledge, preferred methods of medical information acquisition, and suggestions for improving IR awareness”.
Abbott acquires Cardiovascular Systems

Abbott and Cardiovascular Systems (CSI) have announced a definitive agreement for Abbott to acquire CSI. Under terms of the agreement, CSI stockholders will receive US$20 per common share at a total expected equity value of approximately US$890 million.
CSI IS A LEADER IN DEVICES for atherectomy, the procedural use of which can help maximise the benefits of standard balloon angioplasty or stent treatments in restoring blood flow in complex arterial disease. CSI also has an early-stage pipeline of complementary vascular intervention devices in development.

“The acquisition of CSI will add
With regards to study results, 39.8% of participants were able to place IR as a medical specialty in and of itself—this specialty status is the case in the USA, where it is not elsewhere, such as in the UK. This is “improved” from 2000, when data demonstrated that only 2% of the US population knew what interventional radiologists did. Less than half of respondents knew that IR involved medical procedures, with over half feeling that the name of the IR specialty was “too ambiguous” and 458 stated that they wanted to “learn more” about it. Makary et al also specify that they found “no correlation between age, income level, residence, or race” and level of IR awareness.
As stated above, there were respondents who themselves had been offered an IR procedure, numbering 113, and of these, 66 also had the option of undergoing surgery. Twenty patients then went on to say that their choice of surgery over minimally invasive IR treatment was influenced by a “lack of IR awareness”, which amounted to 71% of those who chose a surgical procedure. This is despite the finding that “92% of participants preferred undergoing a minimally invasive procedure over surgery”.
Regarding the solutions to the lack of awareness proposed to participants, in terms of an alternative name for IR, ‘minimally invasive radiology’ was “most preferred”, opted for by 21.3% of respondents. ‘Procedural radiologist’ and ‘radiological surgeon’ also featured among the top choices, garnering 18.4% and 14.6% of responses, respectively. “Short (<10-min) educational videos and increased patient education by primary care providers (PCPs) were among the most suggested ways to improve awareness,” the authors detail. Other suggestions posed to respondents, in order of popularity as per the study, included websites dedicated to the dissemination of information on IR, increased social media presence, and some form of advertising campaign promoting the specialty.
Based on their study, Makary et al were able to conclude that “a lack of IR awareness may underlie underutilisation. When presented
new, complementary technologies to Abbott’s leading vascular device offerings,” said Lisa Earnhardt, executive vice president, Medical Devices, Abbott.

“We are pleased to have reached an agreement with a leading global company that shares our passion for the development and commercialisation of innovative solutions for treating complex peripheral vascular disease and coronary artery disease,” said Scott Ward, CSI’s chairman, president, and chief executive officer.
Upon closing, the transaction is expected to be neutral to Abbott’s recently issued 2023 ongoing earnings per share guidance.
The transaction, which has been approved by the boards of directors of CSI and Abbott, is subject to the approval of CSI stockholders and the satisfaction of customary closing conditions, including applicable regulatory approvals.


JP Morgan Securities LLC is serving as financial advisor to CSI.
with the knowledge that IR improves patient outcomes, minimally invasive procedures with an interventional radiologist are more often desired by the public over surgical options.” Moreover, the authors posit that the current level of IR awareness among the general populace is “further exacerbated by low IR awareness within PCPs, which has led to low referral rates and underexposure of patients to IR”. Makary and his coauthors make the point that “initiating and maintaining professional relationships [between interventional radiologists and] local PCPs is the first step to improving patient referrals to IR. As IR awareness is low amongst PCPs, strong emphasis should be placed on educating PCPs about common pathologies such as peripheral artery and venous disease, fibroids, [and] chronic pain, that IR physicians treat.”
Speaking to Interventional News about the results, Makary noted how “the overall low level of awareness was not surprising as most patients who come to us for care are not familiar with our specialty or our procedures until we meet them and explain what we can offer.” However, he went on to add that he “did find it interesting that most found the name ‘interventional radiology’ ambiguous, and that ‘minimally invasive radiologist’ was the most preferred alternative”. Expanding on the appetite for a possible name change for the specialty, Makary expressed hope that his and colleagues’ work could “[support] the conversation [in the USA] regarding the identity and name of [the IR] specialty and [provide] helpful insight as the specialty evolves”—not just in terms of nomenclature, but also “educating the public and other healthcare providers about IR and the value of our care”.
Guerbet releases first batch of Elucirem for contrastenhanced MRI
GUERBET HAS ANNOUNCED
the first production batch has been manufactured and released for Elucirem (gadopiclenol) injection following US Food and Drug Administration (FDA) approval in September 2022, after priority review. The first patient has also now received a dosing. The highly stable macrocyclic gadolinium-based contrast agent (GBCA) has the highest relaxivity in its class for magnetic resonance imaging (MRI) and is indicated for use in adults and children aged two years and older.
Elucirem injection is used to detect and visualise lesions with abnormal vascularity in the central nervous system (brain, spine, and associated tissues) and the body (head, neck, thorax, abdomen, pelvis, and musculoskeletal system).
GBCAs improve the contrast between lesions and surrounding tissues by accelerating the relaxation of protons
thanks to interaction with gadolinium atoms. Gadopiclenol, the active drug substance of Elucirem, has been designed to enable twice as much interaction, resulting in the highest relaxivity among all non-specific GBCAs. This allows use at half the conventional gadolinium dose to reveal high-quality images.
The first dosing took place at the Hospital of the University of Pennsylvania (Philadelphia, USA), Guerbet has said in a press release. “Having the ability to use a lower dose of gadolinium, while seeing the diagnostic value and good tolerance during the magnetic resonance imaging [MRI] would be significant [...] for the practice of neuroradiology,” said Laurie A Loevner, division chief, Neuroradiology and professor of Radiology at the Perelman School of Medicine, University of Pennsylvania.
Theresa Caridi
“My interest in understanding and tackling health disparities has grown while here in Alabama as I have become increasingly aware of the imbalance of opportunities for patients in this state.” Theresa Caridi is an interventional radiologist based at the University of Alabama at Birmingham (UAB; Birmingham, USA), where she is Interventional Radiology (IR) Division director. Caridi’s career has also seen her practise across the USA, take on roles which have included the chair of the Society of Interventional Radiology (SIR) Foundation Board of Directors (2022–23), and has now led her, as a passionate patient advocate, to make the move away from academic IR into a principal industry position. She recounts some of the key points on her IR career journey to date for Interventional News.
What attracted you to a career in IR?
Some individuals know exactly what they want to do from the start, but I was not one of those people. I was fascinated by general surgery, but the environment was not ideal at the time I was a student. I was very fortunate to have the benefit of my dad’s perspective— he highlighted for me all those who were switching from surgery into IR and diagnostic radiology (DR). There really was not the reverse happening—nobody switched from radiology into surgery—which I found very telling.
I did a rotation in radiology, and I loved it, including the diagnostic component. It was so fascinating to piece the whole puzzle together for the teams in the hospital. I ultimately attended radiology residency and when I rotated through IR, I loved the ability to combine what I valued in diagnostic work with a procedural solution. I was fascinated by taking care of complex diseases through tiny incisions and sending patients home the same day with very few side-effects. It spoke to me that we could significantly impact someone’s health and healthcare in such a positive way. It could not be more at the forefront of medicine and ideal patient care.
Who were your mentors?
There have been many who have been pillars along my path—mentors, sponsors, and champions. I think it is important to have a variety of mentors of varying career stage, gender, and geography. I always want at least one strong critic who will have the difficult conversations. I am particularly grateful to Jim Benenati, Jim Spies, Cheri Canon, Frank Facchini, David Hahn, and too many peer mentors to count, including, but not limited to, many of the women in IR leadership. Now, I have mentees that began working with me as students and are graduating and becoming peer mentors themselves. Each reference point has its own value.
Could you describe a particularly memorable case of yours?
I was on call while 38–39 weeks pregnant with my second of three children. I was called in overnight for biliary sepsis in a patient with a bile leak needing diversion. The biliary system was non-dilated. My fellow at the time performed a single blind stick into a peripheral biliary duct. When we saw how tiny it was, I hip-checked him and moved my big belly over to first operator for the remainder of the case. I was so far from the table because of my term belly (I ended up having a 9lbs, 1 ounce bundle of joy) that we laughed quite a bit watching me in action. Fortunately, all went smoothly!
How does being associate professor of obstetrics and gynaecology (ob/gyn) complement being an IR? What led you to pursue both specialties?
I appreciate having a secondary appointment in ob/gyn. At the minimum, it is a symbol of the collaboration we have with our ob/gyn colleagues at UAB. They have truly met us in the middle where we have treatment overlap. It has been a phenomenal experience for me and I feel it has added a lot of value to a truly comprehensive women’s health practice in IR.
What was it that earned you the 2022 Brewer-Heslin Award for Professionalism in Medicine?
The Brewer-Heslin Award recognises those who exhibit excellence in patient care and is named for the late Alabama Governor Albert P Brewer, and Martin Heslin, a long-time UAB surgeon leader. Brewer made the gift for the endowment in appreciation of the professionalism he observed and admired in Heslin, who had been his surgeon. I was unaware of the nomination for this—it was all done behind the scenes— until I was notified of my award by the dean. As I understand it, my nomination was based on efforts made to create a comprehensive clinical IR service with a focus on quality and improving health disparities. It was really special to accept the award at the white coat ceremony. It is truly a reflection of great mentors, sponsors, champions, and a hard-working team.
How is practice in Alabama different to practising in Washington DC where you were based before coming to UAB?
The practice is very different in that UAB is a larger organisation with a much bigger catchment area. There is no patient population that we do not treat. My individual practice areas have been heavily supported by colleagues in ob/gyn, urology, and surgery, and I think that has a lot to do with tremendous leaders who have shown a true sense of collaboration.
My interest in understanding and tackling health

Your father, James G Caridi is a posthumous recipient of an SIR Gold Medal this year—what is it like being a second-generation interventional radiologist? Are there any downsides to it as well as the obvious positives?
disparities has grown while here in Alabama as I have become increasingly aware of the imbalance of opportunities for patients in this state. There are so many individuals and organisations doing good work here to bridge these gaps, including our team, which has looked at disparities in fibroid treatments and interventional oncology therapies.
Being second-generation to someone like my father is all an upside. Dad believed in helping others, even if in a small way. This made him beloved as a physician and patient advocate, which was only enhanced by his own personal diagnosis. I love that I learned so much about being a patient advocate from him.
Where being a second-generation IR is challenging is similar, I would imagine, as in any career – in the stages of defining yourself, your path, and your individual impact. It is been many years since I have
It is my goal to stay true to my purpose and show other women in IR that this path is possible!”
Current Appointments
2021–present: Associate professor, obstetrics and gynaecology, University of Alabama at Birmingham (UAB; Birmingham, USA)
2020–present: Associate professor and division director, interventional radiology (IR), UAB
2020–present: Associate professor, radiology, UAB
Past Appointments
2013–2020: Assistant professor,
radiology, MedStar Georgetown University Hospital (Washington DC, USA) and MedStar Montgomery Medical Center (Olney, USA)
Selected Society Positions/ Memberships
2022–2023: Chair, Society of Interventional Radiology (SIR) Foundation
Fellow, SIR (FSIR)
Member, Radiological Society of North America (RSNA)
Member, Cardiovascular and Interventional Radiological Society
felt that burden. Dad and I had a tremendous mutual respect for one another’s careers and allowed plenty of space between our paths.
What inspired a pivot from a purely academic career to a role in industry? Are there other women in IR who have done this?
I have partnered a fair amount with industry as an individual and via national society work. I have always felt that we need strong industry colleagues and physicians to partner to provide the best products for our patients. Our corporate partners have incredible minds and resources. I think we need to continue to align and have patient-centred voices in leadership within these corporate entities. I admire the companies who are seeking this physician perspective. It was a very difficult decision to pivot away from academia and a traditional IR practice, but I feel it absolutely suits where I am in my career. I have an opportunity for a major stretch— to understand the corporate world, while bringing the physician/patient voice, and all the while, get to continue to have a clinical IR practice. I am thrilled and filled with gratitude to have this opportunity. I am unaware of other women in IR that have truly worked as a leader in the medical device world. I am amongst amazing male colleagues as I make this pivot, many of whom gave me guidance as I considered this decision. It is my goal to stay true to my purpose and show other women in IR that this path is possible!
What are your hobbies and interests outside of medicine?
I take pride in being a partner to my husband Reggie and a mother of three children (Corinne who is eight years old, Jude, five, and Giuliana, two). I love nothing more than to fill the bellies of loved ones with food from my kitchen (my staple is preparing Italian food, as this is my heritage). Breaking bread with friends and family is the best. A perfect day for me involves exercise, scenic views, time with my family, cooking and sharing wonderful food, and reading (on a chill day) or seeing live entertainment—maybe a concert, Broadway musical, or a ballet—on a more elaborate day.
of Europe (CIRSE)
Member, American College of Radiology (ACR)
Medical Education
2012–2013: Vascular and interventional radiology fellowship, University of Pennsylvania (Philadelphia, USA)
2008–2021: Diagnostic radiology residency, University of Florida (Gainesville, USA)
IO beyond interventional oncology: Progress in immuno-oncology



arm). Although the comparator arm is not the current standard of care (ipilimumab plus nivolumab) and the data are immature for evaluating overall survival benefit, authors reported a difference in two-year survival of 10% (54.4% vs. 44.1%).

Point of View




Recent advances in immuno-oncology are transforming the practice of medical oncology. Currently, antibodies directed against negative regulators of T-cell function, the so-called checkpoint inhibitors, oncolytic virus, and engineered cell therapies such as chimeric antigen receptor (CAR)-T products have received market approval in treating more than 16 types of haematological and solid malignancies and two tissue-agnostic cancer indications including tumours with microsatellite instability (dMMR/MSI-H) and high tumour mutation burden (TMB).
In 2022, the first randomised phase III trial of adoptive cell therapy with tumour-infiltrating lymphocyte (TIL) treatment was presented. This trial was led by The Netherlands Cancer Institute in collaboration with the National Center for Cancer Immune Therapy in Copenhagen, Denmark and compared the
ex vivo modified patient’s own immune cells versus ipilimumab alone in patients with stage IV melanoma. TIL treatment led to a significant progression-free survival benefit of four months (seven versus three months) and in 20% of patients, the metastases disappeared completely (vs. 7% in the ipilimumab
Reprogramming patient or donor T-cells that are designed to express chimeric antigen receptors on their surface (the so-called CAR-T cell) to recognise and target specific tumourassociated antigens has revolutionised haematologic malignancies such as leukaemia and lymphoma, leading to six approved CAR-T cell treatments since 2017. Several clinical trials are underway focusing on this type of therapy option for solid tumours. A recent phase I trial of CAR-T cell and mRNA vaccine targeting carcinoembryonic antigen claudin 6 (CLDN6) in solid tumours that expressing this protein showed a highly impressive objective response rate of 57% and a disease control rate up to 85% in patients with testicular cancer.
Since 2021, two bispecific antibodies, a new form of immunotherapy, have been approved for the treatment of advanced uveal melanoma (Kimmtrak) and metastatic non–small cell lung cancer with certain EGFR mutations (Rybrevant). These antibodies bind onto two specific proteins—one on the surface of the cancer cell and one on the T-cell. Thus, they bring the two cells closer together, allowing the T-cell to better recognise and kill the cancer cell.
Although personalised immunotherapy is an obvious strategy to pursue, its high cost as well as frequent serious toxicities, including cytokine-release syndrome, make them not applicable to all cancer patients. Combining immune therapies with other types of treatment—such as chemotherapy, targeted therapy, radiotherapy, and interventional radiology—many of which are standard of care, can provide additional benefit, as has been shown in several trials. Finally, it is increasingly obvious that other characteristics of the host including sex, microbiome, obesity, and smoking play a role in inducing different responses in immunotherapies.
For the future, the challenge remains—learn how we can identify the patients who will respond to current immune-based cancer therapies and increase the rate of durable clinical responses.

The author declared no relevant disclosures. Antonia Digklia is a specialist in medical and interventional oncology at the Centre hospitalier universitaire de Lausanne (Lausanne, Switzerland).



Antonia Digklia
Immune therapies with [IR…] can provide [...] benefit.”


Progress travelled on the Road2IR in sub-Saharan Africa
Fabian M Laage Gaupp is assistant professor of radiology and biomedical imaging at Yale School of Medicine (New Haven, USA) and a recipient of the Yale Institute for Global Health’s winter 2023 Spark Awards. This monetary prize will see Laage Gaupp and his team at Road2IR make frequent trips to Uganda to help set up the country’s first interventional radiology (IR) training programme—based on the sub-Saharan region’s very first, which the organisation established in Tanzania in 2018. Laage Gaupp, who is one of Road2IR’s founding members, speaks to Interventional News about the challenges of growing IR in sub-Saharan Africa and the impact Road2IR’s work to date has had on healthcare in this region.
recently. We graduated the first class of three fellows in 2021, the second class of seven in 2022, and are about to graduate the third class of three in August 2023. The reason why the second class was so large is that several Tanzanians, who were supposed to do IR training in China, got kicked out of the country when the pandemic started, and we took them into the programme in Tanzania. This should serve as a cautionary tale for countries relying on China and other nations to train their physicians. The safest way is always to train in-country and every country should aim to have at least one IR training programme of its own.
What are the challenges associated with trying to help establish IR services in a less economically developed part of the world?

is still not a focus for global health, unfortunately.
What are your immediate plans for putting the Spark Award funding to use?
What prompted the foundation of Road2IR?
Why were you so keen to dedicate yourself to this outreach work?
Road2IR started as a WhatsApp group in 2017 when I first visited Tanzania with my friend and mentor Dr Frank Minja, who is himself a neuroradiologist, originally from Tanzania. During that visit, I met three peers in Tanzania, who were in their second year of radiology residency at the time—Drs Azza Naif, Erick Mbuguje, and Ivan Rukundo. Together, we assessed the current status of IR in Tanzania—it was non-existent. We came up with the goal of establishing an IR service and training programme in Tanzania, which would make it the first and, at the time, only, IR training programme in all of sub-Saharan Africa (a region with over one billion people). In October 2018, we started doing a two-week teaching trip to Tanzania every month. Another year later, Muhimbili University of Health and Allied Sciences (Dar es Salaam), the university affiliated with Muhimbili National Hospital, where Azza, Erick, and Ivan were training in diagnostic radiology, started a two-year Masters of Science course in IR. Those three enrolled as the first trainees and graduated in September 2021. We have come a long way, with several thousand procedures performed, 10 interventional
radiologists graduated (eight from Tanzania, one from Rwanda, and one from Nigeria), and growing demand and procedure numbers. The reason why I do this is because I see the extreme demand for IR in Tanzania and sub-Saharan Africa overall and I know that we can have immense impact, even with relatively limited resources. All the advantages IR provides in countries like the USA are even more pronounced in sub-Saharan Africa, where surgical and anaesthesia complication rates are often higher.
How did the COVID-19 pandemic impact your work over in Tanzania? In spite of this, what has Road2IR achieved since its inception in 2018?
The COVID-19 pandemic only halted our progress for about six months (March until October 2020). We decided early on that we could not justify stopping an entire service line and training programme because of a viral disease with relatively low mortality. At the time, the IR service in Tanzania was already saving lives every day, so stopping it was not an option. We resumed our monthly teaching trips in November 2020, and have done at least one trip per month since. This is in contrast to many other global health organisations, who seemed to remain in a state of paralysis until
Our main challenge has always been, and remains, disposable equipment. This is an obvious problem, since there was never any demand and, therefore, nobody to supply equipment. Now that demand is growing, we are trying to convince equipment companies supplying this part of the world. So far, some companies have been eager to expand their market to sub-Saharan Africa, while others, not so much. This probably depends on their overall strategy, their willingness to take risk, and their size—some companies can barely keep up with demand in the USA. That being said, I do think it is important that companies make an effort to supply their products to subSaharan Africa. The demand is huge and we as IR physicians cannot do our work without equipment. If Western companies do not act, Chinese and Indian companies will certainly take the market. Tanzania is an example of how quickly a supply chain can be established—we can get a company’s entire device catalogue approved in a week by the Tanzanian health authorities, who have been supportive collaborators with us throughout the process. All we need is for companies to be open-minded.
How was the Road2IR open letter to the World Health Organisation (WHO) in 2021 received?
To be honest, I have no idea. WHO never responded. Prior to the letter, we have reached out to WHO for several years. At one point, we had a Zoom call with some of their radiology and surgery leadership and discussed extensive plans and suggestions. After that, they never followed up and it went nowhere. Sadly, I think that WHO has no real understanding or appreciation of what IR is and how much impact it could have in resource-limited settings. I am hoping that with a growing body of evidence on IR in these settings, WHO will take note. We could greatly benefit from their support, but IR
I will travel to Tanzania and Uganda every few months in the coming year to help set up the partner programme in Uganda. We are essentially creating a copy of the Tanzania programme, but now have the advantage of having a regional partner programme in Tanzania. This means that we will not only have visiting teams going to Uganda from Europe and the USA, but also from Tanzania. This should help the Uganda programme evolve even more quickly and robustly. I am really excited for the next year and I am hopeful that, by 2024, we can do most basic IR procedures in Uganda and, by 2025 or 2026, we will be able to do most complex procedures there. In addition, Ivan Rukundo is now back in his homeland Rwanda and has started the first IR service in this country of 10 million. He is getting over 100 phone calls from referring physicians a day! As you can see, demand for IR is high everywhere, and we are trying to reach the goal set by the Society of African Interventional Radiology and Endovascular Therapy (SAFIRE) of at least one interventional radiologist per million people. This means we need at least 60 in Tanzania, at least 40 in Uganda, and at least 10 in Rwanda.
Further discussion: IR societies and funding awards
Probed further on SAFIRE’s role in expanding IR coverage in sub-Saharan Africa, Laage Gaupp states how it is a very new society, having had its first official meeting in 2021 in Cape Town, South Africa. Nonetheless, he asserts his belief that there is “lots of promise and potential” as far as the society’s work is concerned. Laage Gaupp suggests that SAFIRE plans to set up a continental examination board to allow for uniform IR training standards.
Regarding the continued work of Road2IR, the Spark Award is one of several funding sources that the organisation has secured, Laage Gaupp avers. For example, it has recently received £25,000 from the UK’s Academy of Medical Sciences, but in order to continue to gain muchneeded financial backing, Laage Gaupp stipulates the need to tailor funding applications to the promise of solving disease-specific problems, as opposed to a larger gap in procedural medicine.
Our main challenge [...] remains disposable equipment.”Evaluating a patient for nephrostomy tube placement, Muhumbili National Hospital, Dar es Salaam, Tanzania
Non-surgical treatment significantly reduces knee pain in adults, especially those over 50
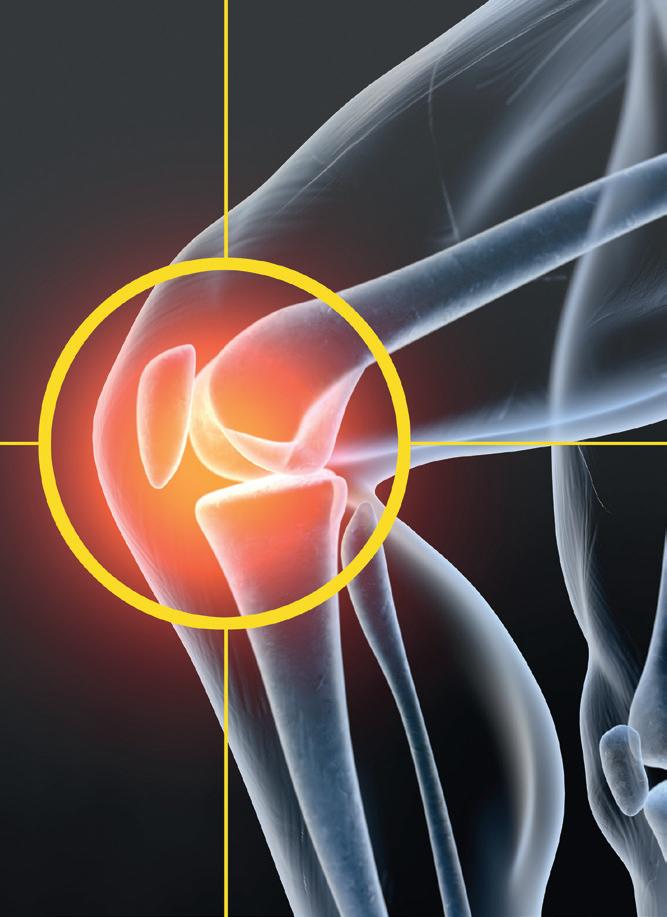
Genicular nerve radiofrequency ablation is a minimally invasive treatment for knee pain due to osteoarthritis of the knee, and can significantly reduce pain, especially for adults who are 50 years and older, according to new research presented at the Society of Interventional Radiology (SIR) annual scientific meeting (4–9 March, Phoenix, USA). This is the first time a study has examined patient demographics, prior surgical history and other clinical characteristics that may predict the level of pain reduction after treatment.
“WE KNOW THIS TREATMENT HAS CLEAR benefits in reducing pain and improving the ability to do everyday activities for patients,” said Kaitlin Carrato, chief resident in interventional radiology (IR) at MedStar Georgetown University Hospital (Washington DC, USA). “But now that we know it
is particularly helpful for those over 50 years old, it may mean that those with chronic pain conditions, like arthritis, would benefit more from this treatment than patients suffering acute pain, such as an injury.”
Interventional radiologists perform genicular nerve radiofrequency ablation by image guidance to place probe needles next to the nerves of the knee that can send pain signals to the brain. The probes generate radio waves, creating a ball of heat to dull or destroy the pain nerve endings. These nerves do not control muscles or affect balance, making the procedure safe. Furthermore, patients leave with plasters, not stitches. The treatment in other studies has been shown to last for approximately six months and up to two years.
The study examined pain reduction for 36 patients using the visual analogue scale (VAS) and the Western Ontario McMaster Universities Osteoarthritis (WOMAC) pain scale. Researchers evaluated whether pain reduction levels were influenced by demographics and clinical characteristics, such as age, gender, body mass index, history of prior surgery and history of fibromyalgia.
Before treatment, patients had a mean baseline VAS of 8.58 and a mean baseline WOMAC of 66.6. After treatment, all study participants experienced a
Cryoablation for renal cell carcinoma: Where do we stand? Where are we going?
Christos Georgiades
Point of View
Christos Georgiades (Johns Hopkins University, Baltimore, USA), delves into the various national society guidelines for treating renal cell carcinoma (RCC), what the ‘gold standard’ of treatment is currently considered to be, and what he believes is the route to ensuring the best outcomes for patients.
The answer to the question of “where do we stand on cryoablation for stage 1A RCC?” can best be found by deploying the ultimate litmus test. Ask those who treat RCC what they would choose for themselves if their life depended on it. And in the case of RCC, it would. I would not be going out on a particularly long limb if I presumed to answer for them—“cryoablation”. This, however, may not satisfy the data-driven, or more accurately, data-dominated decision-makers. So, let us look at the ‘guidelines’. With or without qualifications, all major relevant associations—the National Comprehensive Cancer Network, American Urological
Association (AUA), European Association of Urology (EAU), Society of Interventional Radiology (SIR), and the Cardiovascular and Interventional Radiological Society of Europe (CIRSE)—include ablation as a treatment option for stage 1A RCC. The guidelines worth exploring a bit deeper, however, are those from the American Society of Clinical Oncology, which recommends ablation for stage 1A RCC “if a complete ablation can be achieved”. The wisdom of this last statement is that it gets to the heart of an important issue. Implicitly, it brings up the crucial factor for good oncologic outcomes—operator experience. While no study addresses this issue rigorously,
statistically significant reduction in pain. The mean VAS of 8.58 decreased to 5.02, while the mean WOMAC score decreased from 66.6 to 41. The greatest increase in functionality and decrease in pain was recorded for patients 50 and older compared to younger participants.
“Roughly one in four US adults have knee pain,” said John B Smirniotopoulos, an interventional radiologist at MedStar Georgetown University Hospital. “This treatment can offer many of those people a chance to enjoy everyday activities and regain a higher quality of life by decreasing the pain that they experience on a daily basis.”

During a dedicated media briefing held by SIR, Smirniotopoulos commented on how “rewarding” it is to see the patients return to the clinic for follow-up at regular intervals following their ablation treatment. The progress seen now, overall, at over a year in most cases is “possibly to a degree that [patients] did not expect and maybe that we did not even expect”.
The researchers are currently conducting long-term studies into this treatment that dive deeper into what other factors could predict how well the treatment will work. The same treatment is also conducted with shoulder, hip and sacroiliac joints, where the spine connects to the pelvis.
there is a common understanding among interventional radiologists and urologists on “where we currently stand”— for stage 1A RCC, an experienced interventional radiologist will deliver the same oncologic outcomes as an experienced surgeon. Yet, admittedly, this is not the case everywhere. Many places, especially community settings, lack experienced interventional radiologists. But then again, the same holds true for surgeons experienced in partial nephrectomy, the current ‘gold standard’ of treatment. Which brings us to the second part of the question— “where are we going?”
Twenty years ago, partial nephrectomy was the new ‘gold standard’ for treating stage 1A RCC. Yet, due to the unavailability of experienced surgeons, nearly 54% of patients had radical nephrectomy, which led to them unnecessarily losing a lot of healthy nephrons. Today, after a 20-year push for nephron-sparing options, the situation is not much better, with about 42% of patients with stage 1A RCC still receiving radical nephrectomy. What a disappointment! More relevantly, while 3% of such patients were treated with ablation 20 years ago, today, and despite the evolving guidelines, only 12% are. One could very well argue we are going nowhere. But at the same time, it ought to be clear where we should be going. If we are truly committed
to patient care, our collective efforts should be focused towards offering all stage 1A RCC patients a nephronsparing option, whichever one that may be. The practical solution is neither easy nor obvious. The most feasible and logical answer seems to be the setup and promotion of regional centres that provide these nephron-sparing options—small, incentivised groups of interventional radiologists and urologists working together to offer nephronsparing options to their respective population parcel. A committed effort by the AUA/EAU and SIR/Society of Interventional Oncology (SIO)/CIRSE/ European Society of Interventional Oncology (ECIO) would indeed have tremendous benefits for patients, many of whom would be spared short-term complications and, importantly, potential renal failure and the need for chronic renal replacement treatment.
In closing, reading between the (guide)lines, one appreciates the essence of them can be distilled down to the oncological equivalence of ablation and surgery for stage 1A RCC. This is provided that interventional radiologists possess the necessary expertise to maintain published oncological outcomes. More crucially, however, the question “where are we going?” reveals a failing, an opportunity, and a challenge to interventional radiologists and urologists—make nephron-sparing options available to the nearly-50% of stage 1A RCC patients who unnecessarily undergo radical nephrectomy.
Disclosures:
Georgiades is a consultant for Boston Scientific. Christos Georgiades is professor of vascular and interventional radiology at Johns Hopkins University.
Many places [...] lack experienced interventional radiologists.”
Humacyte publishes six-year outcomes in study of HAV for peripheral arterial bypass
Humacyte, a clinical-stage biotechnology platform company developing universally implantable bioengineered human tissues and advanced tissue constructs and organ systems at commercial scale, has announced the publication of “Six-year outcomes of a phase two study of human-tissue engineered blood vessels for peripheral arterial bypass,” in the Journal of Vascular Surgery-Vascular Science

THE PUBLICATION DESCRIBES
the long-term analysis of the company’s phase two clinical trial evaluating the bioengineered human acellular vessel (HAV) as a conduit in patients with symptomatic peripheral artery disease (PAD). The researchers concluded that “the infection-resistant, off-the-shelf human acellular vessel could provide a durable alternative conduit in the arterial circuit setting, to restore lower extremity blood supply in patients with peripheral
artery disease”.
This paper reports a 60% overall secondary patency rate for the phase two study at 72 months, including all patients originally enrolled, and was estimated by Kaplan Meier analysis. There was no evidence of graft rejection or infection. Additionally, no patients underwent amputation of the affected limb out to six years—a meaningful clinical and qualityof-life result, as amputation is a common outcome in many severe PAD patients.
Furthermore, no patients reported pain at rest or ischaemic ulcers on the affected legs. Researchers reported that “these data have demonstrated the durability of the HAV and suggest the occurrence of cellular remodelling by the host.”
Piotr Gutowski (Pomeranian Medical University, Szczecin, Poland), lead manuscript author, commented: “Synthetic grafts can be limited due to poorly matched mechanical compliance, risk of infection, and variable patency rates. Furthermore, cryopreserved allogenic grafts are limited due to poor durability, thrombosis, and mechanical degradation. The HAV is designed to be consistent in size, durable in highpressure circulation, show no clinical immunological response, and remodel with the patient’s own cells.”
“With an increasing global prevalence of PAD and more than 200 million people living with the disease, there still remains a major unmet need for longterm solutions,” said Laura Niklason, chief executive officer of Humacyte. “Key findings of this publication show that the HAV was durable and performed
Large bore mechanical thrombectomy reduces adverse outcomes in high-risk PE patients

LARGE BORE MECHANICAL thrombectomy with the FlowTriever system (Inari Medical) in patients with high-risk pulmonary embolism (PE) was associated with a significantly lower occurrence of meaningful in-hospital adverse clinical outcomes compared to other contemporary treatments, data presented at the American College of Cardiology (ACC) 2023 Scientific Sessions (4–6 March, New Orleans, USA) indicate.
These were among the results of the FLAME study, a prospective, non-randomised study of interventional treatment in high-risk PE, a patient population with a historical mortality rate of 25-50%, which were presented at ACC 2023 by Mitchell Silver (OhioHealth Heart and Vascular, Mansfield, USA).
The study collected data on patients treated with the FlowTriever and on those treated with other therapies in a context arm. The primary endpoint measured a composite of meaningful in-hospital clinical outcomes, including mortality, major bleeding, clinical deterioration, and escalation to an alternate therapy.
Silver reported that FLAME was stopped early after meeting the pre-specified interim
the FlowTriever arm, in which a mortality rate of 1.9% was recorded, compared to 29.5% in the context arm. In all, the composite primary endpoint occurred in 17% of patients in the FlowTriever arm, compared to 63.9% in the context arm.
“The remarkably low mortality seen with FlowTriever demonstrates the benefit of rapidly identifying PE patients and getting them to an interventionalist for assessment,”
Silver was quoted as saying in a press release issued shortly after the presentation of the results at ACC 2023. “It is time for our hospital systems to develop standardised care pathways for PE, similar to what has been done in other major cardiovascular diseases such as heart attack and stroke.”
“High-risk PE persists as one of the deadliest cardiovascular diseases,” James Horowitz (NYU Grossman School of Medicine, New York, USA), FLAME national principal investigator was also quoted as saying in the same release. “Outcomes have remained unchanged for decades. The FLAME data show that [the] FlowTriever is an important new treatment option that offers a dramatic improvement in survival.”
well in a medically complex patient cohort for long-term treatment of PAD. The HAV is designed to be available off-the-shelf, has the potential for a regenerative capacity and low infection risk, all of which are particularly important in this patient group.”
The HAV has been evaluated in eight clinical studies in the USA, Europe, and Israel.
New VOYAGER PAD analysis confirms consistent benefit of low-dose rivaroxaban plus aspirin following lower extremity revascularisation
Data from a new prespecified analysis of the phase three VOYAGER PAD clinical trial show that low-dose rivaroxaban plus aspirin resulted in a 33% reduction in acute limb ischaemia and a 15% reduction in major adverse limb and cardiovascular events, with or without dual antiplatelet therapy (DAPT). The data were presented at the American College of Cardiology’s 72nd annual scientific session (ACC; 4–6 March, New Orleans, USA).
THE NEW FINDINGS REINFORCE THE benefits of the Xarelto (rivaroxaban; Janssen Pharmaceutical Companies of Johnson & Johnson) vascular dose (2.5mg twice daily plus aspirin 100mg once daily) over standard of care (aspirin alone), demonstrating consistent benefit at 30 days, 90 days and up to three years following lower extremity revascularisation in patients with peripheral arterial disease (PAD).
“These data demonstrate an evolution in the medical therapy of patients undergoing lower extremity revascularisation for symptomatic [PAD],” said Marc P Bonaca (University of Colorado Anschutz Medical Campus, Aurora, USA), lead study author of the VOYAGER PAD analysis. “We hope these data assist clinicians in understanding how to implement antithrombotic therapy in practice and overall support initiation of rivaroxaban in the first days after revascularisation regardless of whether or not DAPT is utilised.”
Those treated with Xarelto plus aspirin after lower extremity revascularisation saw a 33% reduction in acute limb ischaemia, with a trend toward greater benefit observed early (≤30 days hazard ratio [HR]=0.45; 95% confidence interval [CI] 0.24–0.85) vs. late (>90 days HR=0.75; 95% CI 0.60–0.95).
Xarelto plus aspirin was more effective than antiplatelet therapy alone in preventing acute limb ischaemia after lower extremity revascularisation (Kaplan-Meier estimate from 0 to 90 days 1.02% vs. 2.10%, respectively, and 4.3% and 5.7% from 91 days to three years). The hazard ratio for the rate of thrombolysis in myocardial infarction (TIMI) major bleeding at 0 to 90 days was 2.01 (range 0.9–4.47) and from days 91 up to three years was 1.28 (range 0.82–1.99), neither of which were statistically significant.
FlowTriever arm— mortality rate of 1.9% was recorded, compared to 29.5% in the context arm
The HAV is designed to […] show no clinical immunological response, and remodel with the patient’s own cells.”
Piotr Gutowski
ESC and EAPCI publish renal denervation consensus statement
Renal denervation represents another treatment option in patients with uncontrolled resistant hypertension and may be used in selected patients deemed intolerant to antihypertensive drugs.
These are among the messages of a new consensus statement published in EuroIntervention following a review of evidence by the European Society of Cardiology (ESC) Council on Hypertension and the European Association of Percutaneous Cardiovascular Interventions (EAPCI).
Early excitement over the potential for renal denervation as a treatment for hypertension was dampened following the release of initial results of the SYMPLICITY HTN-3 trial in 2014 in which it was shown that, at six months, renal denervation did not elicit significant incremental blood pressure lowering benefit compared with a sham procedure.
Subsequently, joint ESC and European Society of Hypertension (ESH) guidelines on the management of arterial hypertension, published in 2018, advocated against the routine use of device-based therapies for hypertension, until further evidence of their safety and efficacy came to light. However, newer
sham-controlled trials have revitalised hope in the potential of renal denervation, with a number showing statistically significant and clinically meaningful reductions in blood pressure.

In producing the latest consensus statement, the ESC and EAPCI expert panel have reviewed evidence from several “second-generation” randomised, shamcontrolled trials, which, they say, demonstrate the safety and the blood-pressure lowering efficacy of radiofrequency and ultrasound renal denervation. The second generation of trials have involved either the Symplicity Spyral (Medtronic) multi-electrode radiofrequency device or the Paradise (ReCor Medical) ultrasound system.
“Since the publication of the 2018 ESC/ESH Guidelines for the Management of Arterial Hypertension, several high-quality, randomised, sham-controlled trials have been published, demonstrating a bloodpressure-lowering efficacy over 24 hours for both radiofrequency and ultrasound renal denervation in a broad spectrum of patients whose hypertension ranges from mild-to-moderate to severe and resistant,” Emanuele Barbato (University of Rome, Rome, Italy) and colleagues write in EuroIntervention
“This expert group proposes that renal denervation is an adjunct treatment option in uncontrolled resistant hypertension, confirmed by ambulatory blood pressure measurements, despite best efforts at lifestyle and pharmacological interventions,” the statement notes. Renal denervation may also be used in patients who are unable to tolerate antihypertensive medications in the long term, the writing committee has concluded.
The authors of the paper suggest that a shared decision-making process, taking into account the patient’s global cardiovascular risk and the presence
Results on ReCor Medical’s Paradise ultrasound renal denervation system published in two JAMA Network publications
ReCor Medical and parent company, Otsuka Medical Devices, have announced that primary endpoint results from the RADIANCE II pivotal trial have been published in the Journal of the American Medical Association (JAMA). Study results showed that the Paradise ultrasound renal denervation (uRDN) system successfully reduced blood pressure compared to sham. In addition, pooled analysis results from the combined primary efficacy endpoint and safety data from RADIANCE SOLO, RADIANCE TRIO, and RADIANCE II were concurrently published, showing a consistent blood pressure-lowering effect across a range of hypertension.
RADIANCE II IS A RANDOMISED, sham-controlled US Food and Drug Administration (FDA) investigational device exemption pivotal trial of the Paradise uRDN system for treating patients with uncontrolled hypertension.
Conducted as an international multicentre study at more than 60 study centres in eight countries, 224 patients with uncontrolled hypertension were randomised 2:1 to uRDN or a sham. Patients were to remain off antihypertensive medications throughout the two months of followup unless specified blood pressure criteria were exceeded. At the two-
month primary efficacy endpoint, patients treated with the Paradise uRDN system had a mean reduction in daytime ambulatory systolic blood pressure of -7.9mmHg, compared to a reduction of -1.8mmHg in the sham arm, corresponding to a statistically significant and clinically relevant between-group difference of -6.3mmHg (p<0.0001). The study also achieved its primary safety composite outcome with no major adverse events observed.
Concurrently published in JAMA Cardiology, the RADIANCE pooled analysis includes data from more than 500 patients randomised in the three studies from RADIANCE-HTN TRIO,
of hypertension-mediated organ damage, should be followed when considering renal denervation as a treatment option.
Furthermore, they state that interventionalists require expertise in renal interventions and specific training in renal denervation procedures. “Centres performing these procedures require the skills and resources to deal with potential complications,” Barbato et al state.
Presently both the Symplicity Spyral and Paradise system carry a CE mark, and Medtronic and ReCor both filed premarket approval applications to the US Food and Drug Administration (FDA) in late 2022 for their respective devices.

“To date, there are at least 18 societal and/or expert consensus documents published, and the increasing number of citations seems to parallel the mounting evidence for renal denervation therapy,” David Kandzari (Piedmont Heart Institute and Cardiovascular Services, Atlanta, USA), a member of the writing committee for the ESC/EAPCI consensus statement and prinicipal investigator in the SPYRAL HTN-ON MED trial, told Interventional News. “In all, these documents are important for providing clinicians with guidance regarding the evidence basis for renal denervation safety and effectiveness, patient selection, and procedural technique. Many of the documents also underscore the need for shared-decision making and accounting for patient preference.
“The ESC/EAPCI document offers the most contemporary evidence and informed clinical considerations for renal denervation, including recommendations for not only patient selection but also for institutions related to renal denervation programme development, patient selection, and operator proficiency.”
which studied patients with resistant hypertension, and RADIANCE-HTN SOLO and RADIANCE II, which studied patients with mildmoderate hypertension.
The combined dataset showed an overall reduction in daytime ambulatory systolic blood pressure in the uRDN group of -8.5mmHg with a difference between treatment and sham at two months of -5.9mmHg (p<0.0001), favouring uRDN. Blood pressure results were similarly positive in the 24-hour, night-time, home, and office measures. A favourable safety profile was consistently observed post-uRDN treatment across the studies.
“The results of the RADIANCE clinical trials are meaningful in that they solidify the role of the Paradise uRDN system as a therapy for hypertension treatment in addition to medications
and lifestyle modification. Having three consistent sham-controlled clinical trials demonstrating the Paradise uRDN system can safely lower blood pressure in a range of patients is a very high bar to have met,” said co-principal investigator Ajay Kirtane (New York-Presbyterian Hospital, New York, USA).
Co-principal investigator Michel Azizi (Université Paris Cité, Hôpital Européen Georges Pompidou, Paris, France) added: “The results [of the pooled analysis] are in line with the 2023 consensus statement of the European Society of Cardiology (ESC) Council on Hypertension and the European Association of Percutaneous Cardiovascular Interventions (EAPCI). The publication of these results will bring the evidence of the performance of uRDN in the treatment of hypertension to a broad audience of physicians.”
These results are in line with the new 2023 consensus statement of the European Society of Cardiology Council on Hypertension and the European Association of Percutaneous Cardiovascular Interventions.”Paradise system Kidney model
Squid liquid embolic agent deemed safe and effective for high-grade DAVFs
The Squid liquid embolic agent (Balt) has been deemed safe and effective in treating highgrade dural arteriovenous fistulas (DAVFs), and serves to expand the armamentarium for neurointerventionists treating DAVFs and other intracranial vascular malformations.
MARKUS MÖHLENBRUCH (HEIDELBERG
University Hospital, Heidelberg, Germany) and colleagues recently published the results from a prospective, observational multicentre study of this endovascular embolisation treatment in the Journal of NeuroInterventional Surgery.
“Squid is a promising liquid embolic agent for the embolisation of high-grade DAVFs,” they write. “In this prospective, multicentre study, embolisation using Squid was associated with an acceptable complication rate and a high occlusion rate.”
The study’s authors begin their report by noting that endovascular embolisation became established as a feasible treatment option for cranial DAVFs—primarily following the introduction of the Onyx liquid embolic agent (ev3/Medtronic) in the mid-2000s—and that newer agents like the novel, non-adhesive, precipitating Squid have aimed to overcome existing shortcomings and further improve the success of DAVF embolisation.
“The two major innovations of the new liquid embolic, Squid, in comparison with Onyx, are the size of the tantalum grains, which are admixed to the agent, and the availability of the low-viscosity version, Squid 12,” they write, but note that all other components of the two agents are identical.
As such, Möhlenbruch and colleagues set out to assess the safety, efficacy and short-term outcomes of DAVF treatment with this liquid embolic via the prospective, observational LIQUID study, which was conducted across eight German neurovascular centres. The primary outcome measures were safety—defined as morbidity and mortality—and the occlusion rate 90–180 days after treatment.
A total of 53 patients (mean age=59.8 years, 22.6% female) with high-grade (Cognard type ≥3) DAVFs were treated with the Squid liquid embolic agent across 55 treatment sessions. Of the included DAVFs, 56.6% were Cognard type III, 41.5% were type IV, and 18.9% were ruptured, the authors report. The Squid 18 was used in 83.6% of treatments while the Squid 12 was deployed in 32.7%.
Outlining results from the LIQUID study, Möhlenbruch and colleagues state that the overall rate of intraprocedural or postprocedural adverse events was 18.2%, and procedure-related adverse events resulting in permanent morbidity were observed in 3.6% of cases. One patient (1.8%) died unrelated to the procedure due to pulmonary embolism.
In addition, the immediate complete occlusion rate using Squid only was 92.5%. In one patient, after partial embolisation with Squid, transvenous
Systematic review deems coated stents plus SAPT feasible in ruptured aneurysms
A systematic review and meta-analysis of the “scarce” existing literature has adjudged flow diversion with a coated stent plus single antiplatelet therapy (SAPT) to be “feasible” in the treatment of ruptured intracranial aneurysms, despite thromboembolic complications occurring in a “significant number of patients”— all of which were associated with aspirin-based SAPT.
THESE FINDINGS HAVE BEEN published in World Neurosurgery by Matthias Gawlitza (University Hospital Leipzig, Leipzig, Germany) and colleagues, who also note a low rate of haemorrhagic complications across the patient cohort involved.

At the outset of their report, the authors state that, owing to the increased risk of major bleeding events in patients with ruptured aneurysms who undergo flow diversion alongside dual antiplatelet therapy (DAPT), surfacemodified flow diverters that can be implanted with SAPT would represent “a major step forward” in this setting.
“Flow diverters coated with antithrombogenic substances were recently introduced and have shown encouraging results in the preclinical setting,” Gawlitza et al further note.
“Our aim was to analyse their clinical application in patients with ruptured intracranial aneurysms using SAPT.”
The authors also highlight three surface-modified or ‘coated’ flow diverters designed to reduce
thrombogenicity that have gained CE-mark clearance, and are currently under “intensive clinical and scientific investigation”—the Pipeline Embolisation Device (PED) Shield (Medtronic), equipped with a phosphorylcholine coating, and the P48 hydrophilic coating (HPC) and P64 HPC flow-modulation devices (Phenox/ Wallaby Medical).
“Hydrophilic polymer and phosphorylcholine coating for flow diverters are major technical advances with encouraging preclinical data proving reduced thrombus formation, both in vitro and in vivo,” they add. “Quickly after market launch, the first case reports and small series about their use in ruptured aneurysms under SAPT were published, specifically addressing their potential to reduce complications associated with DAPT in critically ill patients with SAH [subarachnoid haemorrhage].”
With these devices as their central focus, Gawlitza et al set out to assess the safety and efficacy of flow diverters
coiling was performed to achieve complete occlusion, resulting in an overall, immediate complete occlusion rate of 94.3%. The final complete occlusion rate at 90–180 days was 93.2%, the authors add, noting that this core laboratory-rated rate of occlusion is “slightly higher than previously published occlusion rates on endovascular embolisation of DAVFs”.
Regarding functional outcomes, Möhlenbruch and colleagues report that—after a mean follow-up of 5.5 months—the modified Rankin Scale (mRS) score was stable or improved 93% of the time. However, a worsening mRS score was deemed to have been related to the procedure in one patient (1.8%).
“Squid, which features several modifications compared with the established agent, Onyx, expands the armamentarium of liquid embolic agents for the treatment of DAVFs,” they continue.
Despite this, the authors also point out that, even with these potential advantages in mind, impedance of a plug formation; early distal embolisation; and a potentially higher ability to diffuse into collateral meningeal arteries, constitute three major drawbacks associated with embolisation utilising low-viscosity agents. And, while none were directly observed in the LIQUID study, these drawbacks should be known and considered by interventionists using Squid 12.
Möhlenbruch and colleagues go on to briefly acknowledge their study’s limitations, including a relatively low number of patients, the fact that 9.3% of patients did not have data available for follow-up, and the lack of a control group involving other embolic agents. As such, while they claim that this is the largest study reporting on DAVF embolisation using Squid to date—and the first ever prospective study on the endovascular treatment of high-grade DAVFs in “the era of liquid embolic agents”—the scope for comparisons between Squid and other agents is limited.
with antithrombogenic coating in the treatment of ruptured aneurysms under SAPT. To do this, they performed a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)-compliant systematic review and meta-analysis covering three major databases up to March 2022.
Five studies reporting 43 patients with a total of 46 intracranial aneurysms were identified and deemed eligible for inclusion in the analysis. The authors also note that more than one stent was implanted in 16% of patients, and additional coil embolisation was performed in some 53.8%. SAPT with one of several different acetylsalicylic acid regimens was used in 86% of patients, while antiplatelet protocols were variable overall.
The pooled risks of thromboembolic (23.9%), haemorrhagic (9.4%) and overall (28.3%) complications were calculated “in the absence of publication bias, with low-to-moderate study heterogeneity measures”, Gawlitza et al report. All complications occurred in patients under SAPT with acetylsalicylic acid (ASA)—more commonly referred to as aspirin.
Adequate aneurysm occlusion was described in 65.5% of patients in the study, the authors also state, adding that moderate heterogeneity was observed in few retrospective observational studies, encompassing “a limited number of patients” treated with variable SAPT regimens.
“Flow diversion for ruptured aneurysms under SAPT using stents with hydrophilic polymer and phosphorylcholine coating is feasible, and is associated with low rates of haemorrhagic complications,” Gawlitza et al conclude. “However, thromboembolic complications are frequent and may limit the use of this technique to selected cases. The literature is scarce, with few heterogeneous studies encompassing a limited number of patients treated with highly variable SAPT regimens. However, although more and better data are necessary to conclude on the appropriate medication, it should be noted that all reported thromboembolic complications occurred under SAPT with ASA, which therefore should be used with caution as [the] primary SAPT agent.”
Thrombectomy appears comparable to medical management in treating ACA occlusion stroke
MECHANICAL THROMBECTOMY
appears to be a safe and technically feasible treatment option for ischaemic strokes caused by primary isolated anterior cerebral artery (ACA) occlusions in more distal locations. The procedure—which is more traditionally used in large vessel occlusions (LVOs) of the middle cerebral artery (MCA) and internal carotid artery (ICA)—has also demonstrated similar clinical outcomes to best medical management with or without intravenous thrombolysis (IVT).
These are the key findings of an international registry study published recently in the journal Radiology by Lukas Meyer (University Medical Center Hamburg-Eppendorf, Hamburg, Germany) et al.
As Meyer and his co-authors point out in their introduction, despite thrombectomy being a potential therapeutic option in distal occlusion stroke, current evidence supporting its benefits specifically for primary, isolated distal medium vessel occlusions (MeVOs) in the ACA is, to their knowledge, “generally unknown”. They aimed to elucidate this issue
through a case-control study of the TOPMOST registry—an international, retrospective, multicentre, observational registry of patients treated for distal cerebral artery occlusion stroke. Meyer et al analysed the clinical and safety outcomes of thrombectomy for primary, isolated ACA occlusions of the more distal A2–A4 segments, compared to best medical management with or without IVT, in daily clinical practice between January 2013 and October 2021.
In this study, endovascular reperfusion was evaluated using the modified thrombolysis in cerebral infarction (mTICI) scale. The number of reperfusion manoeuvres was counted— including first-pass effect (mTICI 3 after first attempt)—and a final reperfusion result of mTICI 2b–3 was considered a successful thrombectomy, with intervention times and the rate of intervention-related serious adverse events also being detailed.
Regarding clinical measures, early outcome was assessed via the median improvement of National Institutes of Health Stroke Scale (NIHSS) scores at
Study finds “dismally low” global access to thrombectomy and “enormous disparity” between countries
The Society of Vascular and Interventional Neurology (SVIN) has released its first global analysis of access to mechanical thrombectomy for the treatment of large vessel occlusion (LVO) stroke. Findings from MT-GLASS—a study conducted as part of the SVIN Mission Thrombectomy 2020-plus (MT2020+) initiative— have been published in the journal Circulation
THE MT-GLASS STUDY LOOKED AT worldwide access to life-saving thrombectomy treatments, and the factors that contribute to global access, including income class of the country, based on the World Bank classification; proportion of gross domestic product (GDP) spent on healthcare; availability of thrombectomy infrastructure, including operators and centres; availability of reimbursement for thrombectomy; and other relevant stroke systems of care policies. The study ultimately found an “extremely low” global rate of mechanical thrombectomy access, with an “enormous disparity” between countries by income level.
“The study findings validate why we founded Mission Thrombectomy in 2016 and our continued mission that has now grown to include 95 countries,” said Dileep Yavagal (University of Miami, Coral
24 hours, while functional outcomes were defined as favourable (modified Rankin Scale [mRS] score of 0–2) or excellent (mRS 0–1) at 90 days. Safety was assessed by the occurrence of mortality—during hospitalisation and at day 90—as well as symptomatic intracerebral haemorrhages (ICHs).
From a total of 154 patients who met the inclusion criteria, Meyer et al detail that 110 patients (median age=76 years, 50 men) underwent propensity score matching, with 55 having received a thrombectomy and 55, best medical management. Distal MVOs were located in the A2 (53% of patients), A3 (45%) and A4 (2%) segments.
Prior to propensity score matching, the authors observed a median time from symptom onset to groin puncture of 195 minutes across 94 patients who received a thrombectomy. The median number of reperfusion attempts was one, and successful thrombectomy (mTICI grade 2b–3) was achieved in 81% of patients. Complete reperfusion (mTICI 3) was achieved in 67% of patients— including a first-pass effect rate in 41%. Symptomatic and asymptomatic bleeding events were observed in 2% and 14% of patients, respectively, before propensity score matching.
The authors report a median 24hour NIHSS-point decrease of 2 in the thrombectomy cohort compared to 1 in the best medical management cohort. In addition, the distribution of mRS scores at 90 days showed “no evidence of a statistically significant difference”
Gables, USA), corresponding author of the study, chair of the MT2020+ initiative, and past president and cofounder of SVIN. “The global access to thrombectomy is dismally low, with the countries’ income level, prehospital protocols to bypass non-thrombectomy centres, and operator and thrombectomy centre availability, all playing critical roles in thrombectomy access.”
MT-GLASS was conducted throughout 75 countries using the Mission Thrombectomy global network of regions between November 2020 and February 2021, and received 887 responses from 67 countries, an SVIN press release details.

It found a median global thrombectomy access rate of 2.79% (interquartile range, 0.7–11.74%), and revealed a <1% rate of thrombectomy access in 18 countries and 0% in seven countries. In addition, there was a 460-fold disparity between the highest and lowest non-zero thrombectomy access regions, while low-income countries had an 88% lower rate of access compared to high-income countries.
The global rate of availability for thrombectomycapable operators and centres were found to be 16.5% and 20.8%, respectively, of what is considered to be the “optimal” rate, the authors report. Multivariable regression analyses showed that country income level (low/lower-middle versus high); operator and centre availability; and presence of prehospital acute stroke bypass protocols, were all “significantly associated” with increased odds of thrombectomy access.
“Mechanical thrombectomy has proven to be a highly effective therapy for mitigating death and disability since 2015, and it is the largest advancement
between the thrombectomy and non-thrombectomy cohorts regarding mRS scores of 0–1 (38% vs 33%, respectively) and 0–2 (49% in both groups).
Functional outcomes stratified across several subgroups—including age, sex, occlusion site, NIHSS on admission, and whether IVT was given—showed no evidence of a difference in 90-day mRS score distributions between the two cohorts. Ninety-day mortality rates were similar with (22%) and without (31%) thrombectomy too, as were inhospital mortality rates (11% and 10%, respectively).
“We did not find a treatment effect in favour of one therapy option after propensity matching,” Meyer et al conclude. “These results show the potential efficacy of [best medical management] in the subgroup of ACA distal medium vessel occlusion. Mechanical thrombectomy may be considered a technically feasible treatment option for acute ischaemic stroke due to primary isolated occlusions in the A2 and A3 segments because it can lead to high rates of successful reperfusion associated with favourable long-term outcome and did not result in increased rates of symptomatic bleeding events if patients were treated at tertiary stroke centres.
“Nevertheless, patient selection for treatment allocation requires further investigation to identify patients who will benefit the most from available treatment options.”
in stroke treatment in 30 years,” said SVIN president Ameer Hassan (Valley Baptist Neuroscience Institute, Harlingen, USA). “Given the widely distributed global burden of stroke, it is critical to have rapid access to mechanical thrombectomy, worldwide, in an equitable manner. In the USA, stroke is now the number-five killer—but, in the rest of the world, it is still number two! The findings highlight distressing results on a global scale, and represent many lives that could have been saved or significantly improved with better access to thrombectomy treatments.”
“We believe that insights gained from this study would inform global interventions to improve access to this life-saving treatment and enable researchers to study nuances of the obstacles to it further,” added Kaiz Asif (University of Illinois, Chicago, USA), corresponding and first author of the study. “While we continue to work on innovations in surgical treatments and technologies, we are also determined to expedite their dissemination— through Mission Thrombectomy—to a large majority across the world to whom they are not yet available.”
It is critical to have rapid access to mechanical thrombectomy, worldwide.”
Ameer Hassan
CX 2023 highlight: The BASIL-2 trial
Data and discussion on revascularisation treatment strategies for patients with chronic limb-threatening ischaemia (CLTI) will take centre stage at the CX 2023 Consensus update, with results from the BASIL-2 (Bypass versus angioplasty in severe ischaemia of the leg-2) randomised controlled trial (RCT) to be presented for the first time. Chief investigator Andrew Bradbury (University of Birmingham, Birmingham, UK) speaks to Interventional News about the background, context and significance of the trial ahead of this year’s meeting.


BRADBURY NOTES THAT BASIL-2 HAS ITS origins in the original BASIL-1 trial, the short-term results of which were published in The Lancet in 2005. BASIL-1 triallists randomised (1999–2003) patients with severe limb ischaemia, mainly due to femoropopliteal disease, to either a plain balloon angioplasty-first or a bypass surgery-first revascularisation strategy. With “fairly limited followup,” Bradbury recalls, there did not seem to be much of a difference in the primary outcome of amputationfree survival. There was, however, a suggestion that the data from both groups were “beginning to diverge,” which prompted the team to follow the patients up for longer. Reporting the key finding from these later outcomes, Bradbury summarises that “people randomised in BASIL-1, and who were likely to live for more than two years, and who had a good vein, were best served by having a vein bypass first rather than a plain balloon angioplasty first”.
outcome being amputation-free survival (time to major—above-the-ankle—amputation, or death from any cause, whichever occurs first).
Considering the BASIL-2 trial in its wider context of randomised data in this space, Bradbury notes that the investigators have been in “friendly dialogue” with the BEST-CLI team “from the get-go”. Results of the BEST-CLI trial were presented late last year, with the headline finding being that surgical bypass with adequate single-segment great saphenous vein is a more effective revascularisation strategy for patients with CLTI who are deemed to be suitable for either an open or endovascular approach.
First presentation 11:10–11:40
Tuesday 25th April Kensington 1
Speaking on his motivation for starting the BASIL-2 trial, Bradbury recollects how it became clear there were a number of gaps in peripheral arterial disease (PAD) research during his involvement in the UK National Institute for Health and Care Excellence (NICE) guideline expert group on PAD. One such gap had to do with infrapopliteal, or below-the-knee, disease, and Bradbury notes that NICE made a research recommendation to undertake an RCT to compare a ‘vein bypass-first’ with a ‘best endovascular treatmentfirst’ strategy for people who required an infrapopliteal procedure. This is what BASIL-2 endeavoured to achieve.

Roundtable discussion 12:00–13:00
Tuesday 25th April Kensington 1
Bradbury notes that there are a number of differences between the two trials, highlighting for example that BASIL-2 included a different group of patients. “Only about 40% of [BEST-CLI] patients have a below-the-knee intervention,” he says. “We are focused in BASIL-2 on below the knee, and [BEST-CLI] did not pre-specify an only below-theknee analysis.” While BEST-CLI is “not exclusively a femoropopliteal trial,” it has similarities to BASIL-1 in that it is more of a femoropopliteal trial with or without infrapopliteal disease, whereas BASIL-2 is specifically looking at infrapopliteal revascularisation, Bradbury explains.
BASIL-2 and BEST-CLI are both RCTs, however Bradbury is keen to stress the limitations of this high level of evidence. “An RCT is not a GPS, it is more like a wobbly compass near the North Pole,
and all it can try and do is push you in a certain direction of travel,” he comments. He adds that while both the BASIL-2 and BEST-CLI teams are “huge enthusiasts” for RCTs, this type of research must still be scrutinised.
Looking ahead to CX, Bradbury expresses his excitement at the prospect of presenting the BASIL-2 data for the first time at what he describes as “the big UK vascular and endovascular meeting”. “I am really looking forward to seeing everyone at CX 2023 and it is going to be a great meeting. It is a pleasure and a privilege for us to be part of it and have the opportunity to present our trial data for the first time.”
Bradbury hopes that once the audience hear the results, as well as the limitations, which “every RCT has,” they will “go away and reflect” on the data and think about them “in the context of their own practice, their own healthcare system and come to a decision as to whether these new data are going to influence their practice, or not, as the case may be”.
Join the conversation at CX 2023
During the CX session, Bradbury will deliver the results of the BASIL-2 trial, with co-investigators Catherine Moakes, Gareth Bate and Matthew Popplewell (all University of Birmingham, Birmingham, UK) and Lewis Meecham (University Hospital Cardiff, Wales) set to present on the journey from BASIL-1 to BASIL-2, methodology, study limitations and future work, among other topics. Attendees in London and remote participants will have the opportunity to pose questions to the BASIL-2 investigators.
A roundtable discussion is planned to include invited commentary from the US Food and Drug Administration (FDA) and UK Secretary of State for Health.
“Endovascular techniques and technologies for lower limb revascularisation are very different now from what they were 15–20 years ago when we did BASIL-1,” Bradbury remarks, noting for example better guidewires, better balloons, more skilful entry and retrograde cannulation to name just a few developments. As a result, the team are keen to see how the two treatment modalities compare in this new treatment landscape.
In addition, the question at the centre of BASIL-2 represents a “massive global problem” and therefore an important one to solve, Bradbury comments. He elaborates: “I have had the opportunity to visit hospitals in many different countries, and vascular wards wherever you go are essentially full of people with CLTI.” Bradbury explains that BASIL-2 is his and his team’s “attempted contribution” to try and improve the evidence base for the treatment of these patients who are “very challenging” and often “very poorly,” with multiple comorbidities.
BASIL-2 is a superiority trial, Bradbury explains, noting that the hypothesis the investigators started with was that vein bypass would be superior due to the fact that BASIL-1 “seemed to show that vein bypass had advantages over endovascular intervention”. He adds that it is a pragmatic trial, and thus surgeons and interventional radiologists are permitted to use their preferred techniques and equipment, with the primary
It is a pleasure and a privilege for us to be part of [CX 2023] and have the opportunity to present our trial data for the first time.”BASIL-2 Podium











“Intuitive” new biopsy system delivers on reducing “inherent” procedural risk and ensuring sample quality
Consultant interventional radiologist Damian Mullan (The Christie NHS Foundation Trust, Manchester, UK) speaks to Interventional News about his experiences with Merit Medical’s Temno Elite™ biopsy system at his hospital, the largest single-site cancer centre in Europe. Among the benefits of using the product for cancerous and noncancerous soft tissue biopsies alike, Mullan emphasises its ability to yield a larger and less fragmented sample with better macroscopic and microscopic visibility compared to other biopsy needles. This advantage is complemented by the intuitiveness of the design, allowing even those using the system for the first time to do so while reaping the benefits of the Temno Elite’s “unique” features.
Mullan first outlines the obstacles that he and colleagues have historically faced when it comes to carrying out soft tissue biopsies.
“Our main challenge is getting a sufficient volume of tissue to satisfy needs for histological diagnosis, for clinical trials and for tissue banking. A good-quality sample is vital, as every biopsy has inherent risks, and you do not want to repeat a biopsy simply because the sample is insufficient despite accurate biopsy placement. The Temno Elite enables the clinician to take a good-quality sample first time, and in a safe manner for the patient”, according to Mullan.
Moving on to speak on the key features Temno Elite boasts, Mullan mentions the “cored-out” bevel, which “produces up to a 72% larger sample than previous side-notch needle systems. This can provide a similar bulk of tissue with fewer biopsy passes or allow confidence that a smaller gauge biopsy will give you a similar bulk of tissue to current needle systems. You now do not have to upsize your needle and puncture hole to get a better quality sample,” he underlines.
In addition, he explains how the sample assist feature is key to allowing delivery of a nonfragmented sample to your histopathologist. “It allows you to atraumatically slide the biopsy sample off the bevel, avoiding having to scrape it off with a scalpel or swirl in formalin, and this avoids fragmentation. A non-fragmented sample is crucial for liver and renal biopsy where you are looking for a continuous piece of tissue to ascertain the number of continuous portal triads or the ratio of glomeruli to fibrosis.” In combination, he summarises, these two features aid the diagnostic yield when sampling, for cancer and non-cancer patients alike. He adds: “It is visually and microscopically better and appears as if you are getting a sample from a traditional forward-cutting needle—they are good, solid cores.”
Ease of use is a further consideration that the Temno Elite accounts for, Mullan avers, dubbing it “very intuitive”. This is in contradistinction, he notes, to “some other needle systems, which, if you handed to a colleague with no experience of that system, they would find it difficult to understand how to load and fire the system until they had used it 10 or 20 times. However, if you hand over a Temno Elite, it is a case of ‘point-and-click biopsy’, it is ergonomic intuition.” Mullan describes the new system overall, in this regard, as “a nice, stepwise evolution of the previous Temno systems. You do not need instruction or repetition to become
immediately familiar with it”. Regarding the safety profile, Mullan refers to unique advantages offered by the Temno Elite. Lung biopsy, specifically, is “a procedure that can carry significant morbidity.” There are well recognised



72% LARGER SAMPLES1



to do a procedure, which is in a controlled, concise, methodical and safe fashion.”
Mullan follows this up by stating that the Temno Elite is geared towards use for multiple types of biopsy, with a range of gauge and length options. “The quality of the sample and the size means that it is relatable to any biopsy, [not only lung and liver] because you will get a better quality sample than with traditional flat-cutting bevel needles. It is an evolution of previous needle systems, so it is not too different, just better. Across the board, whether for renal, peritoneal, [or others], it does seem to give a better sample.”


On the topic of testing, Mullan proceeds to share his experience—“we have performed bench-side tests, ex vivo, with a calf’s liver to assess the number of portal triads, and it did give us a significant increase in the number compared to older flat-cutting bevel systems.” In theory and in practice, “fragmentation is significantly less with the Temno Elite system”.


Commenting on real-life use, Mullan explains how the cored-out bevel does make the needle tip slightly more prone to bending and distortion (in comparison to a flat bevelled needle), but “only if you are aggressive with manipulation in tissue. One would argue that any biopsy should be precise and targeted, avoiding excess
Total Core biopsy technology for superior samples Sample Assist feature for procedure control

Product & Industry
IceCure Medical receives regulatory approval in China for commercial use of its IceSense3
disposable cryoprobes
IceCure Medical, developer of minimally invasive cryoablation technology, the ProSense System (marketed under the brand name IceSense3 in China), has announced the National Medical Products Administration (NMPA) of China has approved the company’s IceSense3 disposable cryoprobes for commercial use, to be used in combination with the company’s IceSense3 console.
With this latest approval, the company and its partners in China can address a significant market with its proven technology to treat malignant and benign tissue of the breast, lung, bone, liver, and kidneys.
“With approximately 430,000 new breast cancer cases in 2022 alone, and a healthcare system readily adopting new technologies that produce improved outcomes, we see China as a prime market for our cryoablation system,” stated Eyal Shamir, IceCure’s chief executive officer.
Getinge receives US FDA premarket approval for the iCast covered stent system
Getinge‘s iCast covered stent system has received premarket approval from the US Food and Drug Administration (FDA) for the treatment of patients with iliac arterial occlusive disease.
“The global market for covered stents is growing at an annual rate of 5%. Getinge will continue to ramp up capacity throughout the year in order to meet the demand,” says Elin Frostehav, president of acute care therapies at Getinge.
The iCast covered stent system, which is sold outside the USA under the brand name Advanta V12, has been used by clinicians for 20 years and is the most clinically evaluated balloon expandable polytetrafluoroethylene (ePTFE)-covered stent in the world, with clinical data published in more than 550 articles.
SurgVision’s Explorer Air II granted US FDA 510(k) clearance
SurgVision has announced that it has received 510(k) clearance from the US Food and Drug Administration (FDA) for the Explorer Air II for use with pafolacianine (Cytalux, On Target Laboratories) during intraoperative fluorescence imaging.
This is designed to achieve highsensitivity and imaging fidelity, meeting the needs of oncological intraoperative fluorescence imaging. The system allows real-time imaging during surgery and its prototype has

been tested by academic centres for a variety of indications.
The Explorer Air II is also cleared in the USA and CE-marked in the EU for visual assessment of blood flow and tissue perfusion.
Currently, the identification of tumours during surgery or interventional endoscopy relies on visual inspection and palpation. Tumour tissue is sometimes difficult to distinguish from healthy tissue. As a consequence, surgical resection of the tumour is often incomplete.
Noninferiority study comparing outcomes of Focal One HIFU vs radical prostatectomy yields positive results
EDAP TMS has shared news of a presentation of positive results from a large, multicentre, noninferiority study comparing Focal One high-intensity focused ultrasound (HIFU) versus radical prostatectomy (RP) at the 38th annual congress of the European Association of Urology (10–13 March, Milan, Italy).
The study, which ran from April 2015 to September 2019, compared Focal One HIFU versus RP as a first-line treatment for patients with localised prostate cancer (grade groups <3). A total of 3,328 patients from 42 treatment centres were included: 1,967 were treated with Focal One HIFU and 1,361 underwent radical prostatectomy surgery. Patients were followed for 30 months.
Among the data that the study produced were the following points:
At 30 months, the salvage treatmentfree survival rate was higher in the HIFU arm (90.1%) compared with RP arm (86.8%);
Risk of salvage treatment was greater than 1.2-fold higher after RP (HR: 0.75, 95% CI [0.64-0.96], p = 0.02);
ICS score, a measure of urinary incontinence, was significantly lower after HIFU (0 vs 1, p < 0.001);
IIEF-5, a measure of erectile function, decreased significantly less after HIFU than after RP despite (median Δ = -4 vs -9 p < 0.001);
Postprocedural benefits of HIFU for both erectile function and urinary continence were demonstrated despite patients in the HIFU-treated group being an average of 9.6 years older (median age was 74.7 years for HIFU vs 65.1 years for RP, p>0.0001).
UK MHRA awarded £10 million to fast-track patient access to medical products
A total of £10 million has been awarded to the Medicines and Healthcare products Regulatory Agency (MHRA)—an executive agency of the UK Department of Health and Social Care (DHSC)—to help bring innovative new medicines and medical technologies to UK patients more quickly, His Majesty’s (HM) Treasury has announced.
Over the next two years, the MHRA will use the money to support development of a thorough but shortened process to speed up the approval process for cutting-edge treatments developed in the UK with the greatest opportunity to meet the country’s healthcare priorities, such as cancer vaccines and artificial intelligence (AI)-based therapeutics for mental ill-health.
It will also support the establishment of an international recognition framework, allowing the MHRA to capitalise on the expertise and decision-making of trusted regulatory partners, and provide patients with fasttrack access to best-in-class medical products that have been approved in other countries.
The first regulatory partners that the MHRA intends to build new recognition routes with are the Food and Drug Administration (FDA) in the USA and the Pharmaceuticals and Medical Devices Agency (PMDA) in Japan.
Shockwave Medical announces US launch of new peripheral IVL catheter
Shockwave Medical has announced the full US commercial availability of the Shockwave L6 peripheral intravascular lithotripsy (IVL) catheter following clearance by the US Food and Drug Administration (FDA).
A press release details that the Shockwave L6 catheter is purpose-built to modify calcification in otherwise difficult-to-treat lesions in large peripheral vessels, including the iliac and the common femoral arteries.
“The Shockwave L6 catheter pushes the boundaries of what IVL can help physicians achieve for patients with severe peripheral arterial disease,” said Frank Arko (Sanger Heart and Vascular Institute, Charlotte, USA).
“The characteristics of the new catheter allow physicians to optimise IVL therapy in large peripheral vessels, which represent over 20% of peripheral interventions performed in the USA each year. The Shockwave L6 catheter may also be beneficial when IVL is utilised to facilitate transfemoral access for large bore procedures like TAVR [transcatheter aortic valve replacement], TEVAR [thoracic endovascular aortic repair] and EVAR [endovascular aortic repair] to minimise the risks of rupture and dissection.”
According to Shockwave Medical, the L6 IVL catheter’s compact emitter
configuration, in conjunction with four new device sizes (8, 9, 10 and 12mm diameters), enables effective delivery of sonic pressure waves in larger vessels.
Merit Medical expands SwiftNinja steerable microcatheter offering
Merit Medical has announced the expansion of its SwiftNinja steerable microcatheter product line. New sizes include a low-profile 2.4Fr distal diameter option in 125cm and new, longer 150cm lengths.
The 180-degree articulating microcatheter is designed to provide access to challenging peripheral and coronary vasculature without the use of a guidewire. It is part of the broader Merit Vascular portfolio that includes sheath introducers, inflation devices, embolics, and other procedural solutions.
“Unlike conventional microcatheters that are limited to a set shape, the steerable SwiftNinja is really a game-changer,” said Jason Hoffmann, interventional radiologist at New York University (New York, USA), and consultant for Merit Medical. “The tip shape and angle can be changed in real time while inside a patient, allowing for shorter procedures with less radiation exposure. Without the need for a guidewire, there is the potential for significant cost savings as well— all of which benefit the patient. The SwiftNinja has paved the way for better embolization care.”
NeoDynamics granted Chinese patent for FlexiPulse needle design
NeoDynamics, a medical device company dedicated to advancing the diagnosis and care of cancer, recently announced that the company has been granted a Chinese patent for the needle design employed in the NeoNavia FlexiPulse probe.
The front-loaded, open-tip sampling needle is designed to enable maximum tissue yield, with minimal patient trauma. The patent is an important milestone that opens up for a future commercial launch in China and strengthens the protection of the NeoNavia biopsy system. NeoNavia with FlexiPulse addresses biopsies in the axillary lymph nodes, which can be a technically and anatomically challenging site due to the proximity to blood vessels and nerves.
The Chinese patent comes on top of a similar patent granted in the USA in August 2021, followed by US Food and Drug Administration (FDA) clearance received in September 2022.
Argon Medical launches Traveler portal vein access series
Argon Medical introduces the Traveler portal vein access series as the newest addition to its portal vein access product portfolio. The product line is designed to meet the needs of physicians accessing the portal vein
Product & Industry News





fibrotic liver parenchyma and reach the portal vein, even when there is very distorted anatomy” said Donna D’Souza, an interventional radiologist at the University of Minnesota (Minneapolis, USA).
The Traveler Series, which includes Traveler 16, Traveler 21, and Traveler 38, is now available in the USA and Canada.
blocked vein with four occluded stents.
Williams made the following comment on the procedure—“I had crossed the segment in this patient three years ago, but today it would have been impossible with existing devices. The patient’s leg was in a desperate condition. Traversa not only made this procedure possible, but also much easier and impressively faster.”
Microbot Medical’s Liberty robotic system remote controller receives design patent allowance in Japan
through the liver during transjugular intrahepatic portosystemic shunt (TIPS) procedures. Traveler supplements Argon’s 2021 launch of Scorpion, which also supports TIPS procedures.
Traveler is designed to improve component visualisation and durability, which are common challenges of the TIPS procedure. “Several innovative features of the Traveler set make it easier to access the portal vein compared to other sets on the market. Firstly, the metal cannula is very robust, and the shaping tool allows it to be curved to great degrees without compromising component integrity. Secondly, the puncture needle is longer and seems sharper, making it easier to pass through severely
Conference calendar
25–27 April
Charing Cross (CX) Symposium 2023 London, UK cxsymposium.com
10–13 May
Venous Symposium 2023 New York, USA venous-symposium.com
18–21 May
Global Embolization Oncology Symposium Technologies (GEST) 2023 New York, USA annual.thegestgroup.com/GEST23
VeinWay crossing tool sees first-in-human compassionate use for venous recanalisation

In a first-in-human, compassionate use case approved by the US Food and Drug Administration (FDA), University of Michigan Health (Ann Arbor, USA) interventional radiologists David M Williams and Minhaj




Khaja successfully used VeinWay’s Traversa for venous recanalisation to save a patient’s leg that was close to being amputated.

Traversa, a newly developed tool for crossing tough occlusions in veins, enabled the physicians to recanalise a previously uncrossable vascular pathway, which included a 20cm-long
Khaja said that “the device allowed us to take the path that we wanted rather than being forced to troubleshoot the path chosen by the sharp recanalisation devices available today. With Traversa, we were able to choose the angle and the length of the throw of the needle. This enabled us to pick the pathway and if we did not like it, we were able to readjust. I think that allowed us to safely get through the occlusions and the stents.”
Microbot Medical has announced that Japan is the most recent global jurisdiction to recognise the interface design of the Liberty robotic system’s remote controller. The design patent, which was issued by the Japan Patent Office (JPO), complements similar design patent allowances in the USA and Europe, further strengthening the company’s global intellectual property (IP) portfolio.
“We believe the ability to perform an endovascular procedure remotely, while reducing radiation exposure and the physical strain due to wearing a lead vest for an extensive period of time, is a major benefit to the physician and patients,” commented Eyal Morag, the company’s chief medical officer. “By eliminating these issues, it allows the healthcare provider to better focus on delivering the best patient care to achieve better outcomes.”
During the recent animal study, as well as other physician-sponsored lab sessions in Europe and the Americas, when using the Liberty robotic system, physicians were given the option to use the remote-controlled activation from the safety and convenience of the interventional suite control room.
1–3 June
International Conference on Complications in Interventional Radiology (ICCIR) 2023 Poertschach, Austria cirse.org/events/iccir
6–9 June
Leipzig Interventional Course (LINC) 2023 Leipzig, Germany leipzig-interventional-course.com
21–24 June
European Conference on Embolotherapy (ET) 2023 Valencia, Spain etconference.org/attend/et-2023
9–13 September
Cardiovascular and Interventional Radiological Society of Europe (CIRSE) 2023 Copenhagen, Denmark cirsecongress.cirse.org
8–10 November
British Society of Interventional Radiology (BSIR) 2023 Newport, UK bsir.org/meetings/bsir-asm-2023
25–29 January
Society of Interventional Oncology (SIO) 2024 Long Beach, USA sio-central.org
23–28 March
Society of Interventional Radiology (SIR) 2024 Salt Lake City, USA sirmeeting.org