neuronewsinternational.com This educational supplement has been sponsored by MicroVention
2022
Educational Supplement
www.neuronewsinternational.com December
|
What is the best approach to mechanical thrombectomy?
4–5 Insights from the ETIS registry
6–7
User experiences with acute ischaemic stroke devices
Since its inception in 1997, MicroVention has gradually expanded its offerings from cerebral aneurysms to include several other areas in neuroendovascular care—with ischaemic stroke being a key area of focus over the past 15 years. Among the more than 30 products the company has launched to date are the well-established ERIC family of stent retrievers, the SOFIA Plus aspiration catheter and, more recently, the BOBBY balloon guide catheter.


In this educational supplement, a number of esteemed neurointerventionists from across the globe have endeavoured to not only share experiences with these devices, either through daily usage in their centres or as part of clinical studies, but also to provide insights on wider considerations in the treatment of acute ischaemic stroke. These discussions range from health economics analyses, and the importance of real-world evidence in medical device evaluation, to the need for more open-minded philosophies in neurointerventional surgery.
ERIC SOFIA
BOBBY
MicroVention’s goal is to continue to be a leading global neuroendovascular company—a goal that it will accomplish in part by maintaining its pioneering work within stroke treatment, and producing reliable, easy to use and technologically advanced technologies supported by proven clinical data. Here, the company looks to bring together numerous aspects of its ischaemic stroke portfolio in one place while also facilitating conversations about how best to expand and optimise this field moving forward.
Standardised aspiration-first thrombectomy approaches bear direct cost benefits
There is a well-known economic benefit to mechanical thrombectomy versus standard medical care, according to John Thornton (Beaumont Hospital, Dublin, Ireland), who notes that it is a “very cost-effective treatment”. And, in addition to improved patient outcomes, there is a “general consensus” that these cost-related benefits are increased further if recanalisation is achieved at the first pass or, at least, with the lowest number of passes possible.
HAVING DEMONSTRATED THIS VIA a previous review of the Irish thrombectomy registry, which showed that there are economic benefits to achieving good recanalisation in fewer than four passes, Thornton and his colleagues then set out to optimise the cost
effectiveness of their centre’s acute ischaemic stroke treatments even further.
“We introduced a standardised approach to thrombectomy, with the intention of using an aspiration catheter first,” Thornton details. “It does not necessarily mean aspiration every
single time—but, there is an intention to use aspiration first, and it is really about having a standardised technique, and standardised equipment, so that everybody knows what they are going to do. And this worked very well.”
Highlighting a comparative analysis of two patient groups—including 127 patients treated before this switch was made and 127 patients treated once the standardised, aspiration-first approach was established, he adds: “We were able to demonstrate shorter procedure times, using fewer passes, and we got improved recanalisation overall.”
Thornton also notes a key difference between his team’s paper1 and previous studies like ASTER and COMPASS that have indicated non-inferiority between aspiration catheters and stent retrievers.
“Ours is not just a ‘pure’ aspiration study,” he states. “It is more about that standardised technique, with the intention—not an
2 December 2022 Introduction
Contents: 2–3
Mechanical thrombectomy
Clot location is important, but stroke operators also need an open-minded approach
While existing evidence suggests thrombectomy outcomes may differ depending on the location or even composition of the clot being treated, clinical studies are yet to elucidate the exact nature of this link and, as such, Tommy Andersson (Karolinska University Hospital, Solna, Sweden) believes operators must keep an open mind and be prepared to strategise based on the individual cases they face.
“TO ME, IT IS MORE ABOUT changing mindsets,” Andersson says. “I am becoming more and more irritated with hearing people say: I always start with aspiration. Or, I always start with a stent retriever. How can you say that? Why would you not adapt what you are doing to the situation— the patient, the location of the clot, [and] the problems you think you may encounter?”
Andersson feels a “false sense of success” is often created here too, as most clots are relatively easy for a skilled operator to treat and, therefore, any strategy—aspiration, stent retriever or a combined technique—is likely to work, while a small minority of more complex clots in challenging locations are where “more work needs to be done”.
“And, people say they always ‘start’ with a stent retriever, or aspiration, but what do they mean by start? What do they do after that?”
Andersson queries. “With our knowledge of the first-pass effect and its proven benefits, we cannot afford to do something that we do not think is the very best option initially.”
He adds that operators often deem clot retrieval at the third attempt as “successful”—which is problematic, as “we know outcomes [are] better at the first pass”.
The role of location
According to Andersson, it is widely accepted that clot location is a “good indicator” of whether an operator may need to modify their strategy, but uncertainty remains and concrete evidence regarding which techniques are better suited to specific locations is minimal. He states that studies of this relationship could provide useful insight, but would likely also be hampered by variables like operator skill and differing healthcare settings, which are thought to influence procedural outcomes.

“For very proximal occlusions, I think aspiration works fine,” he adds, outlining his own paradigm for selecting an approach. “If it is in a bifurcation, I think two stent retrievers is probably the best option. If it is more distal but in a straight segment—for example, in the M1 MCA [middle cerebral artery]—I would
favour a combined technique. I think stent retrievers still have a huge role to play but, most of the time, in combination with aspiration or another device.” Andersson notes he would likely be less aggressive when treating red blood cell-rich clots, as “it will probably come out regardless of what I do”, but tends to be more aggressive with suspected fibrin-rich clots. “So, that is also something I would take into account, but it is more about optimising what we do and improving first-pass effect rates,” he adds. “If we can get closer to achieving recanalisation every time, and in fewer attempts, I think that will pay off for patients and improve their outcomes.”
Stent retriever or aspiration?
Andersson goes on to reference findings from the COMPASS study, which indicated comparable effectiveness and safety outcomes between first-line stent retriever and direct aspiration approaches. “The question [was] wrongly asked,” he claims. “It is not about which is better. I would say that it is sometimes better to use aspiration first, and sometimes stent retriever first is probably better.” He also laments the fact that COMPASS ultimately became about trying to prove which of the two approaches is better.
In Andersson’s view, it is important for operators to be well-versed in using as many techniques as possible—not just aspirationonly or a stent retriever, but a combination, or even a ‘double stent retriever’ approach—so they can select the optimal approach on a more individualised, case-by-case basis. “I think we are stepping into a new era, and we should take advantage of all the devices and tools that we have at our disposal today,” he concludes.
insistence—to use aspiration first. It was not considered to be a failure if, for example, you needed to deploy a stent.”
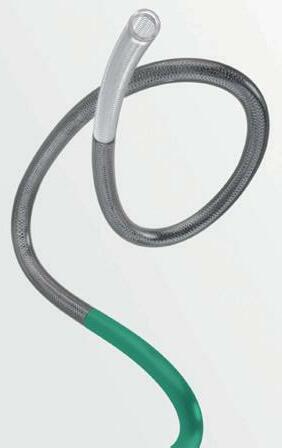
Here, Thornton touches on the role of the “fantastic” SOFIA catheter (MicroVention) in achieving these positive outcomes, adding that it facilitates rapid access to the intracranial vasculature, enabling a faster, better procedure. He also believes that advances in aspiration catheter technology have been pivotal in these improved results.
“When it was introduced, SOFIA was the largest catheter of its type at the time, and it had an incredible ability to be able to be advanced into the internal carotid artery [ICA] and middle cerebral artery [MCA] very easily—without causing trauma to the vessel and, actually, without having to use another catheter inside either,” Thornton elaborates. “It has got a lovely, soft tip. It moves quite well into the ICA or MCA, and you can quite
easily find yourself in a position to perform aspiration very quickly.”
Thornton then moves on to discuss costrelated considerations in the study, noting that Irish health agencies have assessed the improved 90-day modified Rankin Scale (mRS) scale scores seen with thrombectomy versus standard care, and calculated that its introduction into a service like the one at Beaumont Hospital was “very cost-efficient”.

“And, now, what we are doing is not simply looking at thrombectomy versus no thrombectomy,” he continues, “but we are looking at the quality of the thrombectomy and seeing if you can further improve cost-effectiveness. When we look at our own experience of standardising the technique, we found our procedures were shorter, with a better TICI [thrombolysis in cerebral infarction] score, in a faster
time—and those are some of the features that make recanalisation in 1–3 passes more cost-efficient.”
Thornton further notes that the switch to a standardised thrombectomy approach also resulted in his centre using less equipment than they had done previously, including fewer stent retrievers, as well as fewer microwires and microcatheters owing to SOFIA’s ability to be advanced without another device inside it and achieve successful clot retrieval.
This significantly reduces the cost of the procedure, adding to the overall costeffectiveness of mechanical thrombectomy, he concludes.
References
1. O'Neill, D; Griffin, E; Doyle, K M et al. A Standardized Aspiration-First Approach for Thrombectomy to Increase Speed and Improve Recanalization Rates. Am J Neuroradiol. 2019; 40(8): 1335–41.
3 December 2022
The future of ischaemic stroke care
ETIS registry
What is the ETIS registry, and why is it significant?
At this year’s LINNC Paris Course (30 May–1 June, Paris, France), Bertrand Lapergue (Foch Hospital, Suresnes, France) treated attendees to an update on the ETIS (Endovascular treatment in ischaemic stroke follow-up evaluation) registry—relaying that it is a “powerful academic research tool” with the ability to provide “effective device evaluation” while also “measuring and improving stroke care”. Here, ETIS coordinating investigator Lapergue discusses the registry's strengths and ultimate goals in greater detail.
ETIS IS AN ONGOING, prospective, multicentre registry, and it is also academic—which Lapergue points out is an important detail, as it means the subsequent data are not directly sponsored by industry.
Having been launched in 2013, the registry currently includes 29 of the 38 thrombectomy-capable centres across all of France, resulting in a total of roughly 15,000 consecutive stroke patients with a followup of three months.
“All of the thrombectomy cases [at these centres], regardless of the devices or strategy used, are collected within the ETIS registry,” Lapergue continues, noting that there are no specific inclusion criteria, and likening it to a “survey of practice” in France.
“It is important to be exhaustive, and to have consecutive patients, to avoid missing [cases],” he adds.
to smaller cohorts,” he adds.
As was the case with ERIC, for example, newer technologies can be compared to other, similar devices on the market too. And, whereas other studies may use historical cohort data to draw these comparisons, ETIS allows data from similar patient populations, over the same time period, to be contrasted.
The ETIS registry
Started in 2013
According to Lapergue, this is a vital detail, as operator skill and stroke care pathways improve over time, meaning there is “no direct comparison” between datasets collected years apart.
29 thrombectomycapable centres in France
15,000 consecutive stroke patients
Fewer than 10% of data missing
According to Lapergue, fewer than 10% of all data on these thousands of thrombectomy cases are missing, bolstering the comprehensive nature of this dataset.
Device evaluation
More than 45 peerreviewed publications since 2018
As such, the evaluation and development of thrombectomy devices is among the key functions of ETIS. Lapergue notes that the network has already played a role in assessing the ERICTM stent retriever and the SOFIA catheter (MicroVention), as well as other neurovascular technologies like Catch (Balt) and pRESET (phenox).
He believes that a major strength of the ETIS registry here is its high volume of treatments, with around 300 SOFIA cases being published previously, and another submission involving close to 700 cases with the device also now being prepared. “I think this makes our data more robust as compared
While device selection is up to the discretion of the operator within the ETIS registry, and other discrepancies may exist between the different stroke centres, Lapergue states that the large numbers of ETIS cases enable adjustments to be made via propensity score-based analyses, helping to “correct the nonrandomised aspect” of device evaluations.
Another point he is keen to emphasise is that specific or ‘true’ data from the registry are not shared directly with industry. Instead, an independent team within ETIS performs all of the statistical analyses and produces the resulting reports—as opposed to this being done by the device manufacturers themselves.

True data are shared with regulatory bodies, but not with companies, which Lapergue says helps to minimise biases or conflicts of interest.
Assessing changes in care
He also highlights the significance of an ongoing registry that has now been collecting and analysing data for the best part of a decade.
“We have several years of data, and we can [assess] the evolution of [treatment times], efficacy and safety with these
procedures,” Lapergue says. He notes a “dramatic improvement” in the efficacy of thrombectomies since 2013, with the firstpass effect rate increasing from 25% to 43% over this period and successful recanalisation (final thrombolysis in cerebral infarction [TICI] 2b–3) rising from 71% to 89%.
“With the quality of [newer] devices, and the experience and skill of the operators, we have increased recanalisation rates without any increase in complications,” he continues.
In his view, however, there are still future strides that can be made. While TICI scores and recanalisation serve as a “strong marker of efficacy”, Lapergue feels there is still scope to aim for improved TICI 2c/3 rates (>70% recanalisation) rather than settling for TICI 2b scores (>50%) moving forward—with industry collaboration to develop new devices set to be key here.
“I think, as well as device quality, the next stage may be stroke workup—because, if you look at the delay from stroke onset to groin puncture, it is very long,” he says (currently around 90–100 minutes, on average). “We have to improve on this,” he avers. “We [must] improve pre- and intra-hospital pathways for patients, because [right now] they are too long.”
Lapergue concludes by touching on the relevance of ETIS registry data undergoing remote monitoring to ensure a strong level of quality, but also the fact they are open source, as this empowers its function as a “tool for academic research”, noting that—as close to 50% of thrombectomies are ‘off-label’ procedures right now—it is vital to analyse the results extensively, furthering the existing knowledge base and informing clinical practice.
“We are reporting the data in real-time, meaning each centre can compare [its] results with the national [averages],” Lapergue adds.
To this end, the ETIS collaborators have published more than 45 peer-reviewed publications since 2018. “So, it is a huge research activity, and one that we are very proud of,” he states.
4 December 2022
Lapergue presenting at LINNC 2022
A closer look at the study supporting French reimbursement of SOFIA
SOFIA HAS FREQUENTLY been used for contact aspiration in thrombectomy procedures at Marnat’s centre—and many other French hospitals within ETIS—and is a “very good device”, in his view.
This was borne out by a retrospective study in which he and his colleagues examined ETIS data from 2013 to 2018.1 Some 2,600 patients across four stroke centres were included, with close to 900 of these undergoing contact aspiration thrombectomy, and 296 ultimately being treated with SOFIA. The study’s aim was to collect safety and efficacy data, and determine predictors of successful recanalisation with the catheter.
The key finding of their study was a final modified thrombolysis in cerebral infarction (mTICI) 2b/2c/3 rate of 86.1%. “This is in line with the best rates that have been published [to date],” he notes. Marnat et al also report a first-pass effect rate of 24.2%.
Another interesting finding, according to
Marnat, was that ‘rescue strategy’ (i.e. switching to a stent retriever) was required in just 29.7% of cases. And, as an “important objective” of the study was to assess the feasibility of minimising rescue therapies in daily practice, he describes this as a “very good result”.
Marnat says the 6Fr SOFIA catheter was also found to be more efficient than the device’s 5Fr iteration, and he therefore believes operators should prioritise deploying larger diameter catheters—provided the artery is large enough to safely support this. “Of course, if we need to go more distally, then it is very important to reduce the device diameter,” he says. “But, if both are feasible, then the larger one should be selected.”
Discussing specific cases in which contact aspiration, and SOFIA in particular, was shown to be particularly appropriate in their study, Marnat says the device is “perfectly adapted” to M1 and basilar artery occlusions
with embolic causes. He also claims this has “strong implications” for operative strategy, potentially making these cases easier for younger operators with less training, adding that a single-device strategy can reduce procedure times and lower costs too.
Marnat states that, while this large case series offered a “good study population”, two key factors led to SOFIA being used in just one third of these cases. Firstly, the device was not covered by reimbursement policies across French hospitals at the time, making physicians more likely to select alternatives that their centres would not need to pay for.
However, Marnat and colleagues' study did play a key role in MicroVention ultimately obtaining this reimbursement in France in April 2021. In addition, results from two further SOFIA studies—one sponsored by MicroVention itself, and another prospective, multicentre trial with hundreds of patients— are set to be published soon, expanding the existing data on the device’s performance.
The second factor he highlights is first-line contact aspiration being less well-established, and the wider use of a ‘stent retriever-alone’ technique, at the time of their study. But, the latter is now far less common in France following “important evidence” seen in the COMPASS and ASTER trials, Marnat claims.
References
1. Marnat, G; Barreau, X; Detraz, L et al. First-Line Sofia Aspiration Thrombectomy Approach within the Endovascular Treatment of Ischemic Stroke Multicentric Registry: Efficacy, Safety, and Predictive Factors of Success. Am J Neuroradiol 2019; 40(6): 1006–12.
Real-world registries provide “very useful” adjunct to randomised trials
Raphaël Blanc (Rothschild Foundation Hospital, Paris, France) highlights the benefits of a large, real-world registry like ETIS, with particular focus on how such networks can supply valuable data on new thrombectomy devices.


“ERIC [MICROVENTION] HAS BEEN on the market in France for quite a long time, and has been used very regularly within the ETIS registry since the beginning,” says Blanc, who is also the scientific coordinator for the registry. In this time, many data have been collected on the device as a first-line treatment and as part of a rescue strategy.
ETIS has enabled retrospective comparisons to similar devices like Solitaire (Medtronic) and Trevo (Stryker), with these comparisons demonstrating ERIC's safety and effectiveness in stroke treatments.
Blanc references the benefits of propensity score-based analysis here—as seen in a paper where ERIC demonstrated equivalent angiographic and clinical outcomes to more established stent retrievers—allowing direct comparisons to even larger case numbers
and cohorts.1
Owing to strict data monitoring and large patient numbers, ETIS has allowed the prospective collection of “very robust and complete” controlled data, according to Blanc, who also notes that these data have greatly improved the understanding of ERIC and its performance.
“A registry like ETIS can provide real-life data,” he adds. “And, because those data are controlled and monitored, and we have a large number of cases, they lead to analyses that are quite robust in a real-world setting.
“In France, two thirds of stroke centres are now participating in ETIS, so it is a very wide, national registry including multiple centres and numerous operators. This is very useful in providing information on the
real-life usage of devices.”
A high volume of patients and cases allows evaluations to be performed in a short period of time too, which Blanc feels is beneficial for patients, doctors and companies alike. Such registries offer a beneficial adjunct to randomised trials, he adds.
“From a purely scientific and statistical point of view, it does not compare to randomised trials,” Blanc concludes. “But, it can give us robust data, and help provide specific insights to inform or refine the design of future trials.”
References
1. Ducroux, C; Renaud, N; Bourcier, R et al. Embolus Retriever with Interlinked Cages (ERIC) versus conventional stent retrievers for thrombectomy: a propensity score-based analysis. J Neurointerv Surg. 2021; 13(3): 255–60.
care 5 December 2022
The future of ischaemic stroke
Gaultier Marnat (University Hospital of Bordeaux, Bordeaux, France) discusses the SOFIATM catheter (MicroVention) and details a retrospective study of the device based on the multicentre ETIS registry.
User experiences
Positive SOFAST findings may accelerate first-line aspiration thrombectomy uptake
Principal investigator Dheeraj Gandhi (University of Maryland, Baltimore, USA) discusses the SOFAST study and its potential impact on mechanical thrombectomy practices moving forward.
Could you summarise the study's purpose and design?

SOFAST is a postmarket, prospective, multicentre, single-arm, observational study that aims to collect real-world evidence on the safety and effectiveness of aspiration thrombectomy. The first cohort focused on the SOFIA Flow Plus 6Fr aspiration catheter (MicroVention) as a first-line treatment, with the intent to evaluate prespecified endpoints. The study’s primary endpoint is the proportion of patients achieving successful recanalisation of the target vessel (mTICI ≥2b), and there are multiple secondary endpoints related to safety, and functional and technical outcomes, such as first-pass effect and time to successful recanalisation. The second cohort of the study will collect similar data on all MicroVention devices (including the BOBBY balloon guide catheter) used for mechanical thrombectomy to assess treatment outcomes relative to patient, disease and procedural characteristics.
What is the latest status update?
The study aims to enrol a total of 1,000 subjects between cohorts one and two. We are making excellent progress and, as of June
2022, have completed our target enrolment for cohort one (107 subjects). The data are being collected and analysed, and a report is expected by the end of this year. Cohort two started in June 2022 and 14 subjects have been enrolled so far. Our research team has been very active—we aim to activate a total of 50 centres within the next few months for cohort two.
Could you describe your experiences with SOFIA to date?
We adopted the SOFIA Flow Plus catheter shortly after its introduction and use this device for aspiration as a primary approach in suitable ischaemic stroke patients. The simplicity and speed of this approach belies its inherent safety. Favourable SOFIA characteristics include a larger 0.070 inchwide lumen, enabling effective aspiration, and a uniquely engineered, soft, steamshapeable tip and torqueable shaft. It has a hybrid coil and braid design that provides catheter stability while facilitating navigation of tortuous distal vessels for direct aspiration, or deployment of adjunctive treatment devices. And, it can frequently be navigated safely, by itself, to the middle cerebral artery, thereby saving precious time and additional
Why ERIC is my go-to stent retriever for the majority of cases
Yaakov Amsalem (Shaare Zedek Medical Center, Jerusalem, Israel) discusses his experiences with the ERIC stent retriever (MicroVention)—and why it has now been his go-to device for time-critical mechanical thrombectomy procedures for several years.
BACK IN 2008, AT A TIME WHEN acute ischaemic stroke patients were severely underserved across the country, Amsalem set up the first thrombectomycapable medical centre in all of northern Israel. From this centre, based in Haifa, he worked alone, providing 24-hour stroke

care to a population of roughly two million people.
At the time, this was one of only four thrombectomy-capable centres anywhere in Israel, and Amsalem notes that he was performing as much as half of the total number of thrombectomy procedures in
expense. A soft, atraumatic tip enhances safety, and reduces the risk of complications like dissection or intracranial haemorrhage.
Why are studies like this and supporting data so important?
Although tremendous progress has been made over the last decade in establishing mechanical thrombectomy as a standard of care for emergent large vessel occlusion (ELVO) acute ischaemic stroke, there is still a lack of uniformity and clarity on optimal approaches for performance of these procedures. While five randomised controlled trials (RCTs) published in 2015 utilised stent retrievers as the primary option, subsequent RCTs have demonstrated that aspiration can achieve equivalent outcomes, but with faster recanalisation and substantially reduced costs. More real-world data are necessary to corroborate these findings and assess the incremental effectiveness of devices with favourable material characteristics like SOFIA Flow Plus.
What impact do you think SOFAST will have further down the line? Broader implications will depend on its outcomes. We anticipate having cohort one results soon, which will help guide us further. SOFIA Flow Plus, with its stated advantages, could lead to superior outcomes regarding recanalisation and first-pass effect, while also enhancing the safety of thrombectomy procedures. Positive SOFAST findings may encourage other centres to adopt this approach, even if they have previously been skeptical of using aspiration thrombectomy as a first-line tool. The second, larger cohort will allow us to generate and test various research questions, and assess the outcomes from treatment relative to patient, diseasespecific, and procedural, characteristics.
Israel each year—primarily using the Solitaire (Medtronic) and Merci (Concentric Medical) stent retriever devices.
Amsalem claims that, after the first couple of years, he was treating 80–100 patients annually and, following improved education and integration of emergency medical services (EMS), began seeing better results with thrombectomies.
Access to endovascular stroke care has grown markedly in recent times and, according to Amsalem, there are now 10 thrombectomy-capable centres in Israel performing more than 800 of these procedures each year.
Some six years ago, Amsalem set up one of these units himself in Jerusalem. Having primarily used Solitaire and, subsequently, the Catch device (Balt) as well up to this
6 December 2022
STRAIT: New study may aid acceptance of balloon guide catheters in stroke treatment
Earlier this year, the first patient was enrolled in the observational STRAIT study by principal investigator Tobias BoeckhBehrens (Technischen Universität München, Munich, Germany) at his centre. Here, Boeckh-Behrens provides an update on the study and discusses its potential significance further down the line.

Could you briefly summarise the purpose and design of this study?
The purpose of STRAIT is to evaluate the performance of the new BOBBYTM balloon guide catheter (BGC; MicroVention). This prospective, single-arm, multicentre observational study is being conducted in up to nine centres across Germany and Switzerland. We plan to enrol a total of 270 patients with anterior circulation large vessel occlusions (LVOs) during the next one-and-ahalf years. We will be focusing especially on technical performance, with core labcontrolled successful recanalisation as a primary endpoint, although all kinds of clinical variables will of course be analysed as well. To achieve comparable results to historical cohorts, our key inclusion criteria for the use of BOBBY and study enrolment more or less match the ‘classical’ ones—for example, ASPECTS ≥6; NIHSS ≥5; and time from symptom onset up to eight hours.
Why are such studies important in providing supporting data alongside a new device like the BOBBY balloon guide catheter? Firstly, the field of neurointervention in general is an extremely innovative and rapidly evolving area, especially regarding developments in material properties. Therefore, neurointerventionists are consistently faced with newly developed products, and we
point, his practice changed rapidly following the introduction of the ERIC stent retriever product, which he used for the first time in March 2015.
“Since then, I have used ERIC in about 90% of cases,” he notes. “I am a very active, ambitious person, so I want to see results immediately. And, with Solitaire, it always took [multiple] passes to take the thrombus out. I looked for a new device and, when I found ERIC, I saw that it was less aggressive towards the vessel, and the rate of success was very high from the beginning as well.”
benefit a lot from gaining as much information as possible regarding their respective performance. Such information is what we are trying to provide with this study. Secondly, although there is a lot of available evidence indicating patient benefit associated with the usage of BGCs, there is still a relevant proportion of interventionists who do not use BGCs as a standard approach. Therefore, I believe all manner of additional evidence on the possible benefits of BGC usage is generally important.
should lead to a higher proportion of optimal placements of the ballooned tip in the distal part of the cervical internal carotid artery with no need for additional supportive devices like, for example, long sheaths. The second advantage is that BOBBY allows and is designed for combined usage with the 6Fr SOFIA Plus distal aspiration catheter. Owing to its particularly good navigability and softness, SOFIA is the favoured catheter in many centres that use distal aspiration as part of their standard thrombectomy approach. Of course, higher patient numbers in STRAIT are now needed to confirm this initial, personal impression.
Even in the short window of time since the BOBBY device became available, and enrolment of the first STRAIT patient in April 2022, we have already been able to gain a good impression of the catheter’s specific characteristics. In my personal view, it has two major advantages that might hold the potential to overcome some of the oftenheard reservations regarding BGC usage. The first is a good balance between the rigidness of the first generation of available BGCs, and the ‘floppyness’ of subsequent generations. This provides stable support at the aortic arch, on the one hand, while maintaining very good navigability of the distal soft tip—also in tortuous anatomies—on the other. This
microcatheter (MicroVention), which is “much smaller” than the catheters used with Catch or Solitaire. He notes: “When I started using the device, I found that it removed the thrombus at the first or second pass, in most cases, and I said: okay, it works!”
What do you think the future implications of STRAIT will be?
My hope is that the study will be able to confirm those aforementioned advantages. If this is the case, I think STRAIT has the potential to change clinical practice in favour of a better acceptance and wider use of BGCs in stroke treatment. The main reservations with the use of BCGs, in general, are access problems, safety and lack of compatibility with distal aspiration catheters. If these points can be addressed and essentially ‘ruled out’, BGC acceptance should substantially improve—which, in turn, would probably further improve patient outcomes after interventional LVO stroke treatments.
such as stroke neurologists, to perform the procedure. Amsalem also notes that ERIC allows him to perform faster thrombectomy procedures—in as little as five minutes, in some cases—and these time savings are critical in acute stroke treatment.
“My technical success rate with ERIC is more than 90%—much more, in fact,” Amsalem continues. “Clinically, there are a lot of factors, but it is very rare that I see dissections, [postprocedural] bleeding or distal emboli.”
Amsalem also relays another important factor—the compatibility of all the sizes of ERIC with the 17-inch Headway
As such, he claims that thrombectomies using ERIC are low risk, and very easy to manage, adding that this simplification may enable a wider variety of specialities,
He concludes by noting that he “always” uses the SOFIA catheter (MicroVention) for mechanical thrombectomy. Here, Amsalem cites the “huge advantages” offered by SOFIA’s navigability and trackability, and its superior flexibility compared to other catheters, emphasising that its deployment alongside ERIC will “very rarely” fail to successfully remove a clot in one or two passes. All rights reserved. Published by BIBA Publishing, London T:+44 (0)20 7736 8788, publishing@bibamedical.com. The opinions expressed in this supplement are solely those of Microvention and the featured physicians and may not reflect the views of NeuroNews
7
December 2022
The future of ischaemic stroke care
Could you describe the device's key features and benefits it provides?