Stroke community intensifies efforts to tackle “unacceptable” thrombectomy access disparities

A wealth of new data confirming the beneficial role mechanical thrombectomy can play in the treatment of acute ischaemic stroke came to light through the 2010s, but global healthcare systems are still fighting to make these procedures available for more patients, more of the time, and on a more universal basis. Around-the-clock services are yet to be established across the UK and, even in regions where this has been achieved, such as the USA and other parts of Europe, notable care disparities remain, with recent developments reflecting the urgent, worldwide need to rectify this.
In October, representatives of the Stroke Association were at 10 Downing Street in London, UK to hand over an open letter encouraging Prime Minister Rishi Sunak and the British government to prioritise a 24/7 thrombectomy service for eligible patients across the country.

The letter, and the benefits associated with this intervention, were backed by more than 9,000 signatures from among the stroke community—and supported by the World Stroke Organization (WSO), the British Heart Foundation and the Royal College of Radiologists, along with many other groups.


Sanjeev Nayak (University Hospitals of North Midlands NHS Trust, Stoke-on-Trent, UK), a consultant interventional neuroradiologist who played a leading role in establishing the first 24/7 thrombectomy service in the UK, and is now championing the Stroke Association’s attempts to make this a nationwide offering, recently spoke to NeuroNews to discuss this in more detail.

Having submitted the aforementioned letter to 10 Downing Street on 17 October, the charity is yet to receive a response from the British government, but a subsequent parliamentary reception held at the House of Lords saw various stakeholders involved in stroke thrombectomy care meet with UK members of parliament (MPs). Nayak noted that this event was well attended, with many MPs strongly supporting the need for a 24/7 thrombectomy service throughout the UK.
“The concept of a postcode lottery is no longer acceptable,” he added. “This life-changing service should be available round the clock throughout the UK. Last year, more than 6,000 patients in the UK missed out on this treatment—which meant they suffered significant physical disabilities because of severe stroke [that] could potentially have been prevented. The costs of stroke rehabilitation because of disability runs into [the] millions of pounds and this money can instead be used to fund the 24/7 stroke thrombectomy service within UK.”
In its letter addressed to the UK prime minister, the Stroke Association asserts that thrombectomies can save brains, save money and, ultimately, change lives, yet provision of these procedures is “patchy”, as treatment rates vary from 80% of patients who need them in London to 0–30% in other parts of England.
With National Health Service (NHS) England having missed its target of fully rolling out this treatment by 2022, and the current thrombectomy rate standing at 2.8%, the Stroke
Brain stimulation improves COVID-19 outcomes in randomised trial
IN THE RANDOMISED HDRECOVERY clinical trial, the use of high-definition transcranial direct current stimulation (HD-tDCS) has been found to be associated with a statistically significant increase in the number of ventilator-free days among critically ill COVID-19 patients.
Writing in the journal Brain Stimulation, Suellen Marinho Andrade (Federal University of Paraíba, João Pessoa, Brazil) and colleagues state: “HD-tDCS combined with concurrent rehabilitation therapy is a safe, feasible potential add-on intervention, and further trials should examine HD-tDCS efficacy in a larger sample of patients with COVID-19 and severe hypoxaemia.”
The authors begin by noting that HD-RECOVERY was conducted to evaluate the efficacy and safety of HD-tDCS alongside respiratory rehabilitation in patients with moderate-to-severe acute respiratory distress syndrome (ARDS) due to COVID-19.
In the trial, a total of 56 critically ill patients were randomised 1:1 to active (n=28) or sham (n=28) HDtDCS plus respiratory rehabilitation for up to 10 days—or until intensive
www.neuronewsinternational.com December 2022 | Issue 48 6
Featured in this issue:
The “incredible opportunity” offered by TENECTEPLASE page 11
Continued on page 4
So, you want to be a principal investigator?
Profile Shelley
page 16 Continued on page 23
Diederik Dippel
Renowden
“The
concept
of
a postcode lottery is no longer acceptable.” Sanjeev Nayak Image credit: Stroke Association
Left to right: Sanjeev Nayak, Stroke Association CEO Juliet Bouverie and stroke survivor Phil Woodford
World Stroke Day 2022: Leading organisations advocate greater public awareness
This year, on World Stroke Day (29 October), the Society of NeuroInterventional Surgery (SNIS) and World Stroke Organization (WSO) have urged the importance of public awareness, with the latter also announcing a new programme aimed at driving access to quality acute stroke care.
The WSO’s newly launched stroke certification initiative is a strategic response to the results of a World Health Organization (WHO)-WSO survey, which found that less than half (49%) of countries could provide comprehensive, evidencebased acute stroke care. The survey also identified a “huge gap” in provision of care in high- versus low- and middle-income countries. And, while 91% of high-income countries were able to provide access to specialist stroke unit care, the number was just 8% in low-income countries.
Research published by the WSO has also found that global rates of access to two treatments that constitute “fundamental markers of quality acute stroke stroke”—intravenous thrombolysis (IVT) and mechanical thrombectomy— stand at 46% and 30%, respectively.
“One in four of us will have a stroke in our lifetime, yet the majority of people globally lack access to effective treatment and stroke centre care,” said WSO president Marc Fisher (Beth Israel Deaconess Medical Center, Boston, USA). “On top of this, a lack of effective global prevention strategies has led us to a place where stroke is the second leading cause of death and the third leading cause of disability worldwide, with a soaring human and economic cost.”
“We have the knowledge and tools that could save millions of lives and hundreds of millions of dollars,” added incoming WSO president Sheila Martins (Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil). “Delivering quality stroke care is not just the right thing to do, it is the smart thing to do.”
As per a press release, the WSO’s Global Stroke Guidelines and Action Plan aim to help institutions and governments implement evidence-based criteria and standards for care developed by the organisation. Initially targeting hospitals in middle-income countries, the programme launched on 1 November with the primary aim of growing the global network of accredited stroke care providers.
Time is brain, so BE FAST World Stroke Day 2022 also saw US physicians from the Get Ahead of Stroke campaign urge the public to embrace the “simple truth” that strokes are emergencies— and they require calling emergency medical services (EMS) for immediate triage, transport and treatment.
SNIS doctors have long flagged that ‘time is brain’, citing the fact that, the quicker a patient gets to appropriate care, the more brain cells are saved and the greater the chance for survival and limiting disability. However, audience research shows that people often ignore stroke symptoms or drive themselves to the hospital, therefore missing vital in-transit assessment and triage by EMS personnel who coordinate with doctors and stroke care teams to ensure efficient transport, and the best course of treatment, an SNIS press release details.
“By knowing BE FAST, an acronym used to spot signs of stroke, you can save your life or the lives of others,” said SNIS president J Mocco (Mount Sinai, New York, USA). “If you notice any symptoms: loss of balance (B); loss of or blurry eyesight (E); face drooping (F); arm weakness (A); or speech difficulty (S), then it is time to call 911 (T). You may feel like you are overreacting, but you are not—stroke is an emergency, and delaying treatment can result in disability or death.”
In the past decade, new breakthroughs in stroke treatment like minimally invasive thrombectomy have dramatically increased the chances that patients experiencing severe strokes not only survive a stroke but come through without major, long-term disabilities and even return to their lives with minimal recovery time. Specialised care teams at Level 1 stroke centres, also known as comprehensive stroke centres, can perform thrombectomies 24/7/365 in the USA.
“This World Stroke Day, we want people to know that strokes can happen to anyone, at any age,” Mocco added. “If you notice something is not right, call 911 to ensure treatment begins right away.”
News in brief The latest stories from the neuro world

n WSC 2022: BREAKTHROUGHS IN THROMBECTOMY AND THROMBOLYSIS:
This year’s World Stroke Congress (WSC 2022) saw a number of data presentations elucidating the two leading interventional stroke treatments—with major trial updates on mechanical thrombectomy from MR CLEAN-LATE and ENCHANTED2, and discussions around the benefits of tenecteplase versus alteplase in intravenous thrombolysis.
For more on this story go to page 5.
n STUDY REVEALS IMPACT OF PANDEMIC ON ENDOVASCULAR ANEURYSM TREATMENTS:
A study published by Thanh Nguyen (top), Raul Nogueira and colleagues in the Journal of Neurology, Neurosurgery and Psychiatry has revealed that there was an increased rate of ruptured aneurysm coiling between 2019 and 2021, potentially indicating a shift towards endovascular techniques during the first year of the COVID-19 pandemic.



For more on this story go to page 13.
n INTERMITTENT DRG-S DEMONSTRATES PROMISE OF “TRUE LOW-ENERGY NEUROMODULATION”:
Intermittent dorsal root ganglion stimulation (DRG-S) has been shown to produce comparable results to continuous stimulation across a two-week period, as reported in Neuromodulation: Technology at the Neural Interface, indicating the potential it holds to “set a new bar for the meaning of true low-energy neuromodulation”.
For more on this story go to page 25.
Published by: BIBA Publishing, which is a subsidiary of BIBA Medical Ltd
BIBA Medical, Europe, 526 Fulham Road, Fulham, London, SW6 5NR, United Kingdom Tel: +44 (0) 20 7736 8788
BIBA Medical, North America, 155 North Wacker Drive – Suite 4250, Chicago, IL 60606, United States Tel: +1 708-770-7323
Printed by: Buxton Press
Reprint requests and all correspondence regarding the newspaper should be addressed to the editor at the United Kingdom address. © BIBA Medical Ltd, 2022. All rights reserved.
Write to us! If you have comments on this issue or suggestions for upcoming editions write to jamie@bibamedical.com
Make sure you get your copy of
Next issue March 2023
December 2022 | Issue48 2
facebook.com/neuronews https://www.linkedin.com/company/neuronews/ @NN_publishing www.neuronewsinternational.com Editor-in-chief: Prof Philip M Meyers Publisher: Roger Greenhalgh Content director: Urmila Kerslake Editor: Jamie Bell jamie@bibamedical.com Contributing writers: Will Date, Jocelyn Hudson, Bryan Kay and Clare Tierney Design: Terry Hawes, Wes Mitchell and David Reekie Advertising: Michael Broughton michael@bibamedical.com Subscriptions: subscriptions@bibamedical.com Please contact the NeuroNews team with news or advertising queries Tel: +44 (0)20 7736 8788
World Stroke Day
One in four of us will have a stroke in our lifetime
Kenneth Chapman

Association’s recent ‘Saving Brains’ report outlined several measures to help meet the revised 2029 target for a 24/7 service. These include urgent funding for infrastructure, equipment, training and support; developing a sustainable stroke workforce plan; NHS England addressing wider systematic challenges; and research funders improving access to and rates of thrombectomy.
“The input from the government is too little and I hope they can see the harm caused [by] not offering this service round the clock within the UK,” Nayak continued. “The biggest barrier is the lack of capital funding to run a 24/7 service. Every region in the UK has its unique requirements. Hence, capital funding should be provided to UK thrombectomy centres, which can then be used as per their local requirement. Also, investment must be made into the patient transfer pathways, and quicker transfer [facilitation] through road and air ambulance for thrombectomy patients should be prioritised. Time is brain and faster treatment times can lead to significantly better patient outcomes.
“I would like to see a 24/7 thrombectomy service throughout the UK by 2025. However, being more realistic, we should be able to achieve this in next five years.”
In addition to highlighting that the use of artificial intelligence (AI) has “revolutionised” stroke care, and claiming that “all stroke centres should avail such software to improve thrombectomy diagnosis and treatment”, Nayak pointed to the need for global partnerships in helping to develop more effective thrombectomy pathways— including the Society of Vascular and Interventional Neurology’s (SVIN) global ‘Mission Thrombectomy’ campaign (MT2020+), which the Stroke Association is currently in talks with and hoping to be a part of moving forward.
Across the pond
Another comment made by Nayak on this topic was that “the UK can learn from other countries where such treatments have been successfully implemented on a 24/7 basis”— something Dileep Yavagal (University of Miami, Coral Gables, USA) expanded on in conversation with NeuroNews
“Thrombectomy in the USA is provided 24/7—no exceptions or off hours for this emergency service—for all eligible patients at hospitals that are certified as thrombectomy stroke centres (TSCs),” he said. “The main difference is that availability of TSCs in the USA is market-driven and not centrally planned, as in Europe. TSCs have proliferated rapidly in all US states as the hospitals are highly reimbursed for each thrombectomy by Medicare, with federal insurance for patients >65 years,
as well as by private insurances.
“The other big difference [compared to Europe and the UK] is that denial or delay of thrombectomy is heavily punished by the medico-legal system. Another is the widespread adoption of a ‘bypass protocol’ by prehospital services, in which a non-TSC hospital is bypassed even if it is the closest hospital, and the suspected large vessel occlusion patient is taken to the nearest TSC as long as they are within 30 minutes’ travel time.”
While TSCs are now present in all 50 US states—a feat achieved within just a few years of thrombectomy becoming the standard of care in 2015—acute
SVIN 2022 saw presentations on mechanical thrombectomy being included and reimbursed within the Uruguayan National Stroke Plan; a novel Mechanical Thrombectomy Access Score (MTAS) to quantify regional barriers to thrombectomy access; and “highly successful” thrombectomy workshops teaching hands-on technical and workflow skills to neurointerventional teams from 10–15 countries in the Caribbean.
At the meeting, Yavagal himself announced the development of a pilot programme that will allow earlycareer neurointerventionists to observe thrombectomies at designated US centres using new remote proctorship technologies as well. All of these efforts are being supported by MT2020+.
“A recent global survey of 59 countries (conducted by MT2020+ and submitted for publication) showed that the median mechanical thrombectomy access rate globally is a dismal 2.79%,”
awareness are among his key priorities as president of the Radiology Society of Federation of Bosnia and Herzegovina.
Elsewhere in Europe, another significant development recently came from Hungary, with the country announcing plans to roll out a new, national imaging network across every one of its 39 stroke care units— including all seven of its comprehensive, thrombectomy-capable centres—by the end of 2022. Details of this programme, which is being supported by an AIpowered software technology called e-Stroke (Brainomix) and an automated radiology workflow solution (eRAD) to solve the system’s existing “lack of standardisation”, were discussed at an October press conference.
István Szikora (National Institute of Mental Health, Neurology and Neurosurgery, Budapest, Hungary), who played a key role in driving these plans forward, noted that there are “inherent disadvantages” to previously used ‘drip-and-ship’ models—the majority of which are time-related—but many of these can be overcome via the ‘mothership’ approach currently being introduced in his country, whereby patients are transported directly to a thrombectomy-capable centre.
stroke services in the USA are not free from their own difficulties. According to Yavagal, owing to variable distribution of TSCs, and them being concentrated in more densely populated, urban areas, the uniformity of time to thrombectomy access remains a key challenge.
“The large size of the USA and variable population centres are the geographical challenges that make it hard [to enable] uniform, 60-minute access to a thrombectomy centre for everyone,” he continued. “Currently, 21 states have >50% of their population living outside a 60-minute drive radius from a thrombectomy centre. Implementing public health interventions to ensure 60% access to 100% of the US population is a major priority for MT2020+.”
As chair of the MT2020+ campaign— which was founded by the SVIN in 2016 to accelerate access to stroke thrombectomy surgery—Yavagal is well placed, not only to comment on the current state of affairs in the USA, but also to discuss ongoing efforts to improve stroke interventions across the globe. These efforts were showcased recently at the 2022 SVIN meeting (16–19 November, Los Angeles, USA).
“We had a very informative and detailed update at the MT2020+ session,” Yavagal noted. “The campaign now has regional committees in over 90 countries—100% growth since 2020.”
Yavagal concluded. “More importantly, the disparity [between the country with] the highest thrombectomy access rate, Australia (46%), and the [country with] the lowest access rate, Bangladesh (0.1%), is a massive 460 times. This is after excluding eight countries that have zero access to mechanical thrombectomy. For a brain-saving and life-saving therapy, this is should be unacceptable for us as a global village.”
Across the globe
In a recent video interview with NeuroNews—which can be viewed online—Deniz Bulja (Sarajevo University Clinical Center, Sarajevo, Bosnia and Herzegovina) discussed the current situation in his country, noting that many eastern European regions face comparable challenges to their western counterparts when it comes to tackling gaps in thrombectomy services.

“I think we are facing similar problems [to those] that western Europe actually faced 5–10 years ago, or even before, when all of these major RCTs [randomised controlled trials] came along,” he said. “We are now walking this path and will, of course, overcome all of these obstacles—it takes time, but the people who are involved in endovascular stroke care are anxious to see it happen rather quickly.”
Bulja further noted that, on this front, educating physicians and raising public
To provide insights from the Asia-Pacific (APAC) region, World Federation of Interventional and Therapeutic Neuroradiology (WFITN) president Michihiro Tanaka (Kameda Medical Center, Kamogawa, Japan) also recently spoke to NeuroNews Tanaka pointed to similarities between stroke protocols in Japan, and those in the EU and North America, asserting that 24/7 thrombectomy services are “well developed” in his country, and highlighting the use of magnetic resonance imaging (MRI) for acute ischaemic stroke diagnosis in many Japanese hospitals. However, he stressed there are “plenty of issues” still to be tackled within the APAC region.

“APAC is a very wide area, and the level of medical care in each country varies from country to country,” Tanaka continued. “In Japan and South Korea, patients with acute ischaemic stroke can be transported by ambulance on a priority basis, because they have well-developed medical insurance systems. However, in countries where medical insurance systems have not been established, it is still impossible to provide prompt treatment for acute ischaemic stroke.”
He went on to reference the WFITN’s own efforts, including recently published international recommendations for acute ischaemic stroke interventions, and an endowment fund to help develop and train young endovascular neurosurgeons and interventional neuroradiologists, particularly in low- and middle-income countries.
“[Everyone] in the world should be guaranteed to receive this innovative therapy [thrombectomy],” Tanaka added. “This is my message. I hope we can continue to collaborate to promote this mission for stroke patients and their families [across] the world.”

4 December 2022 | Issue48 Stroke Care
Continued from page 1
Stroke community intensifies efforts to tackle “unacceptable” thrombectomy access disparities
A recent global survey of 59 countries […] showed that the median mechanical thrombectomy access rate globally is a dismal 2.79%.”
Dileep Yavagal
Dileep Yavagal (left), Deniz Bulja and Michihiro Tanaka
World Stroke Congress bolsters evidence on optimal thrombectomy and thrombolysis approaches

While much-needed improvements to existing triage and transport protocols for acute stroke patients were a leading topic of focus on World Stroke Day (29 October 2022), the World Stroke Congress (WSC; 26–29 October, Singapore) programme saw stroke interventions themselves thrust into the spotlight, with much first-time data being presented on mechanical thrombectomy and intravenous thrombolysis (IVT) treatments alike.
Recent results from the MR CLEAN-LATE trial, which studied the efficacy and safety of thrombectomy—also referred to as endovascular therapy (EVT)—for acute ischaemic stroke in the anterior circulation 6–24 hours after symptom onset or last seen well, delivered by Susanne Olthuis (Maastricht University, Maastricht, The Netherlands), were among these presentations. In the trial, there was a 1.7 times higher chance for better functional outcome in patients who had collateral flow seen on imaging and treated with EVT, Olthuis reported.
Wim van Zwam (Maastricht University), who is also part of the MR CLEAN-LATE team, added: “MR CLEAN-LATE showed clear benefit for patients treated with EVT beyond the six-hour time window when selected on presence of collaterals only. This will open up these treatments in centres currently not able to perform CT [computed tomography] perfusion, will expand the indication beyond CT perfusion, and may speed up decision-making in centres currently using core and penumbra thresholds.”
In a social media post during WSC 2022, Tudor Jovin (Cooper University Health Care, Camden, USA) described these MR CLEAN-LATE data as “another win for the democratisation of thrombectomy”.
Further thrombectomy data
Following this, Yvo Roos (Amsterdam UMC, Amsterdam, The Netherlands) and Urs Fischer (University Hospital of Bern, Bern, Switzerland) presented pooled analyses of individual patient data from six randomised trials that compared direct mechanical thrombectomy against IVT plus thrombectomy (bridging thrombolysis), and found that direct thrombectomy is not non-inferior to bridging thrombolysis at a 5% margin. The researchers reported that IVT prior to mechanical thrombectomy is associated with a higher chance of successful reperfusion—but at the cost of a higher chance of any intracranial haemorrhage (ICH).
Another presentation saw results delivered from the ENCHANTED2 trial. This multicentre, prospective study showed that intensive blood pressure control (target systolic blood pressure [SBP] ≤120mmHg) in patients undergoing mechanical thrombectomy led to adverse effects, with a higher likelihood of poor functional outcome on the modified Rankin Scale (mRS) and more early neurological deterioration compared to less intensive blood pressure management (target 140–180mmHg) in the control arm.
Craig Anderson (The George Institute for Global Health, Sydney, Australia), who disclosed these findings as principal investigator of the study, stated: “While our study has now shown intensive blood pressure control to a systolic target of less than 120mmHg to be harmful, the optimal level of control is yet to be defined.”
Elsewhere, in the EXCELLENT registry, 46.8%
of patients achieved good clinical outcome following treatment with the Embotrap revascularisation device (Cerenovus) as a first-line therapy. According to Werner Hacke (University of Heidelberg, Heidelberg, Germany), who presented these results, evaluation of clot composition showed that the percentages of red blood cell and platelet content were strong predictors of clinical and recanalisation outcomes.
In a pre-planned post-hoc analysis of the RESILIENT trial—a study set up to compare stentretriever treatment and/or thromboaspiration versus best medical therapy for large vessel occlusion stroke—patients treated in the randomisation phase did not have a better outcome at 90 days when compared to ‘roll-in phase’ patients. Sheila Martins and Arthur Pille (both Hospital de Clínicas de Porto Alegre, Porto Alegre, Brazil) presented these findings, noting during a WSC 2022 session that the two likely reasons for this being the main finding were the strong effect of endovascular treatment, and good training before and during the roll-in period.
Late-breaking lytics research
Multiple studies investigating the use of tenecteplase as a newer-generation alternative to alteplase in IVT were also presented to attendees, with Mohammed Almekhlafi (University of Calgary, Calgary, Canada) delivering data from the AcT trial, and Vignan Yogendrakumar (Royal Melbourne Hospital, Melbourne, Australia) showcasing a pooled analysis of the Melbourne Stroke Registry, EXTEND-IA and EXTEND-IA TNK trials.
“In a [post-hoc] sub-analysis of the AcT trial, tenecteplase had similar rates of favourable functional outcome and reperfusion prior to thrombectomy,” noted Bruce Campbell (University of Melbourne, Melbourne, Australia). “In a pooled analysis of EXTEND-IA TNK and Australian statewide registry data, tenecteplase demonstrated increased rates of reperfusion prior to thrombectomy compared to alteplase across a spectrum of time from lytic to angiography up to four hours. Patients who achieved reperfusion prior to thrombectomy had improved functional outcomes compared to those who achieved reperfusion after thrombectomy.
“[…] The differences in time from lytic
administration to angiography between the two studies were thought likely to be contributing to the difference in results, as AcT almost exclusively included patients presenting to comprehensive stroke centres with rapid workflow from lytic to arterial access, whereas the Australian data included patients transferred between hospitals.”
A late-breaking clinical trials session saw further AcT data presented, with Dariush Dowlatshahi (University of Ottawa, Ottawa, Canada) reporting that—across more than 1,500 analysed patients—every 30-minute delay in onset-to-needle time was associated with a 9% decrease in the odds of achieving an mRS score of 0–1, while every five-minute delay in door-toneedle time was associated with a 3% reduction in the odds of mRS 0–1. Thus, the researchers concluded that, just as with alteplase, faster treatment leads to better clinical outcomes when acute ischaemic stroke patients are administered intravenous tenecteplase.
During a second late-breaking trials session, a pooled analysis of the NOR-TEST 1 and NOR-TEST 2 trials, both of which saw patients randomised to receive either 0.4mg/kg of tenecteplase or the standard 0.9mg/kg dose of alteplase, was presented by Vojtech Novotny (Haukeland University Hospital, Bergen, Norway). The key finding here was that, for ischaemic stroke with a National Institutes of Health Stroke Scale (NIHSS) score ≥6, the researchers determined no difference in efficacy of the two thrombolytic agents. However, mortality rates were higher in the tenecteplase group, leading them to conclude that a lower dose of tenecteplase should be considered in future studies.
Finally, Nadinda van der Ende (Erasmus MC University Medical Center, Rotterdam, The Netherlands) delivered data from the DUMAS trial at WSC 2022, with dual thrombolysis therapy with prourokinase and alteplase demonstrating a similarly low rate of ICH compared to alteplase alone (13% vs 14%, respectively). In
5 Issue48 | December 2022 Mechanical Thrombectomy
pooled analysis of EXTEND-IA TNK and Australian state-wide registry data, tenecteplase demonstrated
of reperfusion
to thrombectomy
to alteplase across
spectrum of
lytic to angiography
hours.”
a
increased rates
prior
compared
a
time from
up to four
Bruce Campbell
EVT associated with a higher chance for better functional outcome in patients with collaterals
1.7x
So, you want to be a principal investigator?
A career in clinical research is perhaps a less formulaic and well-trodden path than the one into medicine itself, typically requiring relatively young and inexperienced clinicians to show initiative, commitment and a great deal of patience. According to Diederik Dippel (Erasmus MC Stroke Centrum, Rotterdam, The Netherlands), lead investigator for MR CLEAN—one of the most impactful clinical trials in the recent history of neurointerventional surgery—the “best thing you can do” initially is embark on a master’s thesis and, after that, a PhD.
Speaking to NeuroNews, he describes his own early forays into clinical research, starting with the daunting set of circumstances he was faced with towards the end of his PhD studies. Having reached the end of the standard period PhD students in The Netherlands are given to complete their thesis, and on the verge of returning to daily clinical practice with much of his project investigating decision analysis still to do, Dippel reluctantly made a difficult choice in the name of furthering scientific comprehension.
“I informed my loved ones I was going to have to work on Sundays,” he recalls, “and I worked on Sundays for at least three years, researching and writing up to complete my thesis and get it published.”
However, while he notes that going above and beyond can be a necessary evil for committed researchers, Dippel is quick to point out this is certainly not something that is ‘expected’ of any PhD student—and those under his guidance are always encouraged and supported to finalise their projects within the allotted timeframe, wherever possible.
Battles, books and questions
In conjuring up several nuggets of wisdom for budding researchers, Dippel refers back to some of the earlier and less successful studies he was involved with long before the MR CLEAN days, including a series of trials investigating how paracetamol’s body temperature-lowering effects might influence stroke outcomes, and another assessing the use of ‘cooling devices’ to protect the brain from focal ischaemia. The former produced “very neutral results”, despite progressing to a large, randomised trial, while the latter was “very hard work” and ultimately found the approach in question was not feasible.
“One of my messages would be to pick your battles, and choose areas where there is real discussion and real benefit to be gained for patients in the long run,” he avers. “Do not do it just because it is interesting—try to find joy in a project that you think will really make a difference.”
Dippel also states that, despite his earlier projects being closer to the margin of stroke research and producing disappointing final results, he learned a lot from them, regarding how to “lay the groundwork” and the need for precision in such trials in particular. “You have to realise that almost all of your trials will be neutral or negative,” he adds. “A really positive trial that shows benefit and changes medical practice is very rare, so you have to have some stamina.”
For residents and trainees wanting to join research groups, he also emphasises the importance of reading
up on clinical methodology—citing Clinicals Trials: A Practical Approach by Stuart Pocock, first published in 1983, as an example, and suggesting that aspiring researchers would do well to familiarise themselves with clinical epidemiology books more broadly too. “Many of these books have been around for decades, but they are still the ones that give you a good basis to think about [clinical research],” Dippel notes.
Here, he alludes to the central roles writing and authorship play in clinical research—a detail that younger clinicians may not anticipate beforehand. Writing up many thousands of words is unavoidable and constitutes much of the “legwork”, Dippel claims, and the amount of input they have on this front will likely be reflected in the list of authors upon publication. He further notes that younger researchers in The Netherlands are often included as first or second author of their own projects, depending on the amount contributed by other, more experienced peers, but this
is unfortunately not so commonplace in every country.
“It can be a little bit boring, sometimes, as there is a lot of that legwork,” Dippel concedes, “but what I like about clinical research especially is that it is so diverse. Patient communication is sometimes forgotten, but it is important, because you have to talk to patients to gain their consent and answer their questions.

[Clinical research] also requires abstract thinking, writing, statistical analyses—it is very broad, which is wonderful.”
Another key piece of advice Dippel offers is to ask questions—not only in the context of research, but in clinical practice too, adding: “When you see decisions being made on treatments, or diagnostic procedures, ask yourself: why are we doing this? And you should not be satisfied with just any answer. You have to ask if there is evidence. Often, there is none, and then you have something you can keep in the back of your mind to explore or do something about later on.”
Medical students, residents and other less experienced researchers are typically involved in enrolling or randomising patients in clinical trials. Dippel believes this is a worthwhile pursuit, but also stresses the benefits of reading up on the protocol and reasons behind a given study, as well as attending any and all investigator meetings that are available. He further notes that, even after a larger trial has been published, local/participating investigators should consider how the data may help to answer other questions, and put themselves forward for any resulting sub-studies, as this offers another inroad for connecting with more experienced researchers.
6 December 2022 | Issue48 Education
One of my messages would be to pick your battles, and choose areas where there is real discussion and real benefit to be gained for patients in the long run.”
Diederik Dippel
And, perhaps most significantly of all, he encourages fledgling researchers to join in and, again, always ask questions. “Sometimes, they will be hesitant about asking a question because [they think] they may appear stupid but, mostly, when you do not understand something, you are not the only one. So, do not be afraid—I think that is important advice,” Dippel says. “Make yourself known, make yourself available, and stick out from the crowd by asking the right questions and being prepared. This is possible in an environment that aims for equality and collaboration, in our centre, but we also try to accomplish that [in the CONTRAST consortium] by not considering hierarchy and by addressing others by their name, never by their title.”
Importance of younger generations
Many universities offer medical students the opportunity to engage in master’s studies for half of or a whole year. Dippel notes that—in the medical space—these projects tend to be a meta-analysis, systematic review or small clinical study, with the student themself devising its protocol, sourcing the data and writing up the bulk of the report. “Some students really like it—they put all of their efforts in and they are successful,” he conveys. “Others, not so much, but it is a very nice timepoint in your career to find out if you would like to do research.”
Students and early-career clinicians alike also need to be “very careful” to preserve their time without overstretching themselves and creating problems at the clinic, Dippel asserts, adding: “Even writing the introduction and conclusion [of a paper] can take months if the clinic is consuming all of your energy. My experience is that, when you are a full-time doctor in a clinic that is not dedicated to research, you will [find it difficult]. There are lots of doctors that have the mindset of a researcher, and they may have one, two or three days per week for research. That is okay—
advisable, even, because you are a better doctor when you do research, and you think more clearly about clinical problems.”
He further notes that this goes both ways, as those who focus primarily on research will likely benefit from maintaining some amount of clinical practice alongside this. “But you have to create time for yourself to do it,” he continues. “This is often possible with research grants and having [at least] one day in the week that is your research day—but, otherwise, it will not work, in my opinion. I am in a lucky position, because we have a university clinic, and 50% of my time is spent on clinical work and the other 50% is research, but it can still be difficult to separate the two. In my environment, that is possible, but I know that in some other places it is very hard to say ‘sorry, this is my research day’; they start laughing and tell you to get back to work!”
Dippel describes the involvement of younger generations as a “win-win situation” for clinical research, providing a cheaper alternative to their older, more experienced counterparts while also equipping them with valuable education and practice for future projects. Here, he cites the fact that, after more than a decade as one of the research leads for the MR CLEAN trial, the subsequent MR CLEAN registry and then the CONTRAST consortium (a collaboration evaluating new acute stroke treatments), he is now set to front a national training programme for young, talented stroke researchers in The Netherlands.
Over the next five years, this programme plans to focus on involving postdocs in many sub-studies and cost-effectiveness analyses, giving them more substantial, coordinating roles in the numerous offshoots of the original MR CLEAN trial and the CONTRAST consortium. With Dippel and his colleagues—the “grumpy old men”, as he calls them in jest—taking a step back from these leading roles moving forward, the hope is to give burgeoning researchers increased responsibilities and hone their expertise for the future. And, supported by grants from the Dutch Heart Foundation, the programme is also looking to send young PhD students abroad, for one or two months at a time, enabling them to connect with other research groups and start up their own projects based around existing datasets.
“We are very lucky to have received these grants from the Dutch Heart Foundation, because that allows us to build the infrastructure to support this,” he concludes. “We—my co-lead for many years, Charles Majoie from Amsterdam University [Amsterdam, The Netherlands], and I—really take care that there is involvement of younger persons. I think that is the basis of how we work; if we do not have the younger people there, we are going nowhere, so it is very important.”

7 Issue48 | December 2022 Education
There are lots of doctors that have the mindset of a researcher, and they may have one, two or three days per week for research. That is okay—advisable, even, because you are a better doctor when you do research, and you think more clearly about clinical problems.”
Direct thrombectomy fails to show non-inferiority versus bridging therapy in early time window
THE INTERNATIONAL DIRECT-SAFE TRIAL has produced results indicating that intravenous thrombolysis (IVT) plus mechanical thrombectomy— commonly referred to as bridging therapy—should continue to be recommended as the standard treatment approach in large vessel occlusion (LVO) acute ischaemic stroke patients who present within 4.5 hours of symptom onset.
The trial’s findings, which ultimately did not show non-inferiority with direct mechanical thrombectomy compared to bridging therapy, have been published in The Lancet by Peter Mitchell (University of Melbourne, Melbourne, Australia) and colleagues, who note that “additional information from our study should inform guidelines to recommend bridging therapy as standard treatment”.
“The benefit of combined treatment with IVT before endovascular thrombectomy in patients with acute ischaemic stroke caused by LVO remains unclear,” they write at the outset of their publication. “We hypothesised that the clinical outcomes of patients with [LVO stroke] treated with direct endovascular thrombectomy within 4.5 hours would be non-inferior compared with the outcomes of those treated with standard bridging therapy (IVT before endovascular thrombectomy).”
This hypothesis was investigated via the DIRECTSAFE study—an international, multicentre, prospective, randomised, open-label, blinded-endpoint trial in which adult patients who presented within this early, 4.5-hour time window from stroke onset were recruited from 25 acute-care hospitals in Australia, New Zealand, China, and Vietnam.
Eligible patients—those with stroke and an LVO in their intracranial internal carotid artery, middle cerebral artery (M1 or M2), or basilar artery, confirmed by non-contrast computed tomography (CT)
SWIFT-DIRECT
and vascular imaging, were randomly assigned via a web-based, computer-generated randomisation procedure to either direct endovascular thrombectomy or bridging therapy on a 1:1 basis. Patients assigned to bridging therapy received alteplase- or tenecteplasebased IVT as per standard care at each site; and thrombectomy was also per standard of care, using the Trevo device (Stryker) as a first-line intervention.
The primary efficacy endpoint for DIRECT-SAFE was functional independence (modified Rankin Scale [mRS] score 0–2) or return to baseline at 90 days, with a non-inferiority margin of –0.1, analysed by intention to treat and per protocol. The intention-totreat population was included in the safety analyses, Mitchell and colleagues note.
Between 2 June 2018, and 8 July 2021, 295 patients were randomly assigned to direct thrombectomy (n=148) or bridging therapy (n=147). Functional independence occurred in 55% of 146 patients in the
direct thrombectomy group (n=80) and 61% of 147 patients in the bridging therapy group (n=89).
The researchers further detail that safety outcomes were similar between the two groups, with symptomatic intracerebral haemorrhage occurring in 1% of patients in the direct group (n=2) and 1% of 147 patients in the bridging group (n=1). In addition, 15% of patients in the direct group died (n=22) compared to 16% in the bridging group (n=24).
Speaking to NeuroNews following publication of this paper, Mitchell highlighted an additional takehome message from the study beyond the fact that eligible LVO stroke patients should receive IVT with alteplase or tenecteplase.
“A further, surprising finding of our study—that we cannot exclude being due to chance—is the differential response observed in Asian region versus non-Asian region patients,” he noted. “For reasons covered in the paper, we had hypothesised that the benefit of direct therapy may be larger in Asian region patients. [However], we observed an even lower proportion of patients in Asian regions treated with direct therapy achieving the primary outcome compared to the bridging therapy group.
“On the basis of the DIRECT-SAFE trial, patients with LVO ischaemic stroke eligible to receive thrombolytic therapy and mechanical thrombectomy should continue to receive bridging therapy. The DIRECTSAFE investigators, together with the investigators of the other randomised trials into direct endovascular thrombectomy, have joined together to further investigate subgroups and outcomes with individual, patient-level meta-analysis—the IRIS collaboration.
“The ongoing research of the IRIS collaboration with increased numbers and statistical power may allow more insight into which patient subgroups show non-inferiority, and at what non-inferiority margin, [with] direct treatment, potentially allowing more individualised treatment decisions. For example, patients with large core infarcts presenting at later time intervals—yet still within guidelines for receiving intravenous thrombolytic therapy—with likely need for stent placement and antiplatelet medication, may be more safely treated with direct thrombectomy.”
important effect”—also noting that “exploratory analysis of secondary clinical outcomes indicated a potentially favourable effect of IVT with shorter in-hospital delays”.
A RECENT SUB-ANALYSIS of the SWIFT-DIRECT trial, which is published in the Journal of NeuroInterventional Surgery (JNIS), has found “no evidence” that the effect of bridging intravenous thrombolysis (IVT) on functional independence outcomes is modified by overall or inhospital treatment delays, indicating that the effect of IVT plus thrombectomy is preserved over time and all IVT-eligible patients should therefore be treated with this combined approach.
However, writing in JNIS, Urs Fischer, Thomas Meinel (both University Hospital of Bern, Bern, Switzerland) and colleagues state that, due to its “low power”, this subgroup analysis “could have missed a clinically
The authors hypothesised that treatment delays might be an ‘effect modifier’ for the risks and benefits of IVT before a mechanical thrombectomy in acute ischaemic stroke patients. To assess this, they used the dataset from the international SWIFT-DIRECT trial, which randomised 408 patients to receive IVT plus thrombectomy, or thrombectomy alone.
Fischer initially presented preliminary results from SWIFT-DIRECT alongside Jan Gralla (University Hospital of Bern, Bern, Switzerland) at the 7th European Stroke Organisation Conference (ESOC 2021; 1–3 September, virtual), with full results being published in The Lancet in July of this year.

In their more recent JNIS sub-analysis, Fischer, Meinel and colleagues set out to assess the relationship between assignment to IVT plus thrombectomy, and expected onset-to-needle (OTN) and door-to-needle (DTN) times, via regression models. Their primary
outcome was functional independence at three months—categorised as a score of 0–2 on the modified Rankin Scale (mRS)—while secondary outcomes included mRS shift, mortality, recanalisation rates and (symptomatic) intracranial haemorrhage at 24 hours.
The researchers included 408 patients (median age=72 years, 51.2% female)—207 of these received IVT plus thrombectomy and 201 received thrombectomy alone. The expected median OTN and DTN times were 142 minutes and 54 minutes in the IVT plus thrombectomy group, and 129 minutes and 51 minutes in the thrombectomy-alone group, respectively.
Overall, Fischer, Meinel and colleagues found that OTN times had no significant bearing on functional and safety outcomes, as well as the recanalisation rates, associated with bridging IVT in their sub-analysis. They report similar findings regarding in-hospital delays, as DTN times were not found to have significantly affected functional outcomes
following bridging IVT treatments. However, mRS shift and mortality analyses suggested greater benefits when bridging IVT was administered after shorter average in-hospital delays.
The authors note that “good overall data quality” within the context of a prospective, multicentre randomised controlled trial (SWIFT-DIRECT) and a prespecified, deposited statistical analysis plan were among the key strengths of their investigation, but concede that limitations should be considered too—including the fact that the original study was “neither designed nor powered to detect an interaction effect” between treatment delays and bridging IVT outcomes.
“Until further evidence regarding potential heterogeneity of the IVT effect size before mechanical thrombectomy becomes available from individual patient metaanalysis of comparable trials,” Fischer, Meinel and colleagues conclude, “IVT should be eligible patients, and neither OTN nor DTN should influence treatment decisions regarding bridging IVT.”
8 December 2022 | Issue48 Research Updates: Ischaemic Stroke
sub-analysis finds effect of bridging thrombolysis is preserved over time
ISCHAEMIC STROKE
On the basis of the DIRECT-SAFE trial, patients with large vessel occlusion ischaemic stroke eligible to receive thrombolytic therapy and mechanical thrombectomy should continue to receive bridging therapy.”
Urs Fischer
BAOCHE trial results supporting thrombectomy for basilar artery stroke published in NEJM
Results from the BAOCHE randomised controlled trial (RCT), which found that the addition of thrombectomy to standard medical care within 6–24 hours in basilar artery occlusion stroke patients improved functional outcomes at 90 days—as compared to standard care alone—have now been published in the New England Journal of Medicine (NEJM).
THESE INITIAL FINDINGS were presented earlier this year at the European Stroke Organisation Conference (ESOC 2022; 4–6 May, Lyon, France), and more recently at the LINNC Paris Course (30 May–1 June, Paris, France), by Tudor Jovin (Cooper University Health Care, Camden, USA).
At the outset of their NEJM report, Jovin and colleagues note that, although improved clinical outcomes have been observed with endovascular thrombectomy in anterior circulation stroke, the effects and risks of these procedures at 6–24 hours after symptom onset in patients with acute ischaemic stroke caused by basilar artery occlusion have not yet been extensively studied.
Therefore, in an open-label, multicentre RCT conducted in China over a five-year period, they set out to
elucidate the effectiveness and safety of thrombectomy in this location by randomly assigning patients with basilar artery stroke who presented between six and 24 hours after symptom onset to receive either standard medical therapy plus thrombectomy, or a control group consisting of standard medical therapy only.
According to Jovin et al, the BAOCHE trial’s original primary outcome (90-day modified Rankin Scale [mRS] score of 0–4) was changed to a good functional status (mRS 0–3) at 90 days. Here, they clarify that this change was made to the primary outcome during the trial as new data from randomised trials became available that indicated an mRS score of 0–3 is “most indicative of treatment benefit”. The primary safety outcomes were
US study bolsters recent evidence supporting tenecteplase in ischaemic stroke care
Tenecteplase, a newer-generation intravenous thrombolysis (IVT) drug, has outperformed the traditional treatment (alteplase) for ischaemic strokes in several key areas, demonstrating better health outcomes and lower costs, according to a recent study published in the journal Stroke
The study was led by a team of neurologists at Dell Medical School at the University of Texas at Austin (Austin, USA) and, starting in September 2019, was carried out over a 15-month period across 10 Ascension Seton hospitals in central Texas.
“The Dell Med Neurology Stroke Program was one of the first in the USA to make this change,” said Steven Warach (Dell Medical School, Austin, USA), lead author of the study. “Based on even the earliest results from this study, other experts across the country were convinced and made the switch from alteplase to tenecteplase at their own stroke centres— including at Ascension hospitals nationwide.”
Both tenecteplase and alteplase are federally approved for use in dissolving clots in blocked heart arteries. However, tenecteplase—the newer of the two drugs—is also being used by clinicians, off-label, to treat ischaemic strokes, because clinical trials in this space have indicated that it may be at least as effective as alteplase. Tenecteplase is delivered via a single five- to 10-second intravenous injection, meaning that, crucially, it is the easier of the two to administer as well.
symptomatic intracranial haemorrhage (ICH) at 24 hours and 90-day mortality.
A total of 217 patients were randomised 1:1 and included in the analysis, with 110 in the thrombectomy group and 107 in the control group. The researchers note that randomisation occurred at a median of 663 minutes after symptom onset, and intravenous thrombolysis was used in 14% of patients in the thrombectomy group and in 21% of those in the control group.
Jovin et al also detail that enrolment in BAOCHE was halted at a prespecified interim analysis timepoint because of the superiority demonstrated by thrombectomy at that stage. The researchers relay that the percentage of patients with a 90-day good functional status was almost twice as high in the thrombectomy group (46%) compared to the control group (24%), also noting an adjusted rate ratio of 1.81 here (95% confidence interval [CI], 1.26–2.60; p<0.001). In addition, the results for the original primary effectiveness outcome (mRS 0–4) were 55% in the thrombectomy group and 43% in the control group (adjusted rate ratio, 1.21; 95% CI, 0.95–1.54).

In the aforementioned study, researchers compared its performance with alteplase, which is widely considered the standard drug for IVT stroke treatments and is injected over a period of 60 minutes.
“When it comes to treating patients with a stroke, every second matters,” said Warach. “The shorter preparation and injection time with tenecteplase not only eliminates a lot of dosing errors related to alteplase, but it is also more efficient. We were able to deliver the clot-busting medicine more quickly after patients arrived in the emergency department and, for patients who needed to be transferred to another hospital for more advanced care after receiving the clot-buster, we were able to initiate the transfer sooner in those treated with tenecteplase.”
For patients who come into the emergency department after a stroke, Warach and his colleagues’ study found that the doorto-needle time—the time between a patient’s arrival and the moment they receive treatment—was, on average, six minutes quicker with tenecteplase. And, for patients who also required surgical removal of a stroke-causing blood clot via a mechanical thrombectomy procedure, tenecteplase sped up the process of transferring the patient to a thrombectomycapable stroke centre by 25 minutes.
The researchers saw further improvements in clinical outcomes for those patients who received tenecteplase, including a 5% increase in patients who were able to walk independently at the time of hospital discharge to home, and a 4% decrease in occurrences of adverse events like brain haemorrhages, discharge to hospice care or death. Warach and colleagues also noted potential economic benefits that were seen in their study, as tenecteplase treatments cost the hospitals about US$2,500 less than alteplase per patient.
Regarding the prespecified safety outcomes, symptomatic ICH rates were higher in the thrombectomy group, occurring in six of 102 patients (6%) versus in one of 88 (1%) in the control group (risk ratio, 5.18; 95% CI, 0.64–42.18), while 90-day mortality was similar between the two groups at a rate of 31% in the thrombectomy group and 42% in the control group (adjusted risk ratio, 0.75; 95% CI, 0.54–1.04). The researchers further note that procedural complications occurred in 11% of the patients who underwent thrombectomy in BAOCHE.
These outcome data lead Jovin et al to conclude that, among patients with stroke due to basilar artery occlusion who presented 6–24 hours after symptom onset, endovascular thrombectomy led to a higher rate of good functional status at 90 days versus standard medical therapy alone. However, they also highlight the higher ICH incidence, and occurrence of procedural complications, associated with thrombectomy—and acknowledge that the generalisability of their findings outside of the Han Chinese population studied is somewhat limited.
“If this price differential continues, the magnitude of savings could equate to [a number] in excess of US$150 million every year in the USA,” said David Paydarfar (Dell Medical School, Austin, USA), coauthor of the study. “This is a great example of valuebased care—better care, for less money.”
The researchers conclude their Stroke study by adding that evaluation in larger, multicentre cohorts is recommended to determine if these observations generalise.
These findings follow The Lancet’s publication of positive data from the AcT study earlier this year. In what was claimed to be the largest stroke trial ever conducted in Canada, researchers showed that tenecteplase is an effective treatment for acute ischaemic stroke, with 0.25mg/kg of the drug working “as well as, if not better than” 0.9mg/kg of alteplase across 1,600 patients.
The Dell Med Neurology Stroke Program is now working with colleagues in the state-funded Lone Star Stroke Research Consortium—a clinical research network focused on innovations in the prevention, diagnosis, treatment and rehabilitation of stroke patients in Texas—to disseminate its study findings across the state, in an attempt to help more stroke centres make the switch to tenecteplase. Warach is also working with Lone Star Stroke colleagues to build a state-wide database to “further confirm their results and answer lingering questions”, according to a University of Texas at Austin press release.
“For example, we have such a large Latinx population in Texas,” he stated, “I would like to know if we are seeing the same advantages from tenecteplase in that community as we are in the larger population. The more data we have, the more questions we can answer.”
9 Issue48 | December 2022 Research Updates: Ischaemic Stroke
US$150 million each year in the USA US $2,500 less than alteplase Per patient, tenecteplase treatments cost hospitals Could equate to savings in excess of
Tudor Jovin

Tenecteplase offers “incredible opportunity” to optimise thrombolytic stroke treatments
Earlier this year, results from the Canadian AcT (Alteplase compared to tenecteplase) randomised controlled trial (RCT) were delivered for the first time at the European Stroke Organisation Conference (ESOC 2022; 4–6 May, Lyon, France). And, alongside other first-time data presentations from studies like NOR-TEST 2 and TWIST, these results represented a major step towards validating the benefits of tenecteplase, a newergeneration intravenous thrombolysis (IVT) drug, over alteplase, the longstanding ‘go-to’ in thrombolytic stroke treatments. That is according to AcT principal investigator Bijoy Menon (University of Calgary, Calgary, Canada), who recently sat down with NeuroNews to discuss these findings and their wider implications—as well as what the future of IVT treatments may look like globally.
Firstly, could you briefly summarise the purpose, design and key results of the AcT trial?
Although tenecteplase was of increasing interest as a thrombolytic agent in patients with acute ischaemic stroke, because of its use as a single bolus, there was no phase 3 RCT showing evidence that it could replace alteplase as the thrombolytic agent of choice in our routine practice. The AcT trial sought to generate this evidence that would help change practice. The primary goal of the trial was to show that tenecteplase at a dose of 0.25mg/kg body weight was comparable to alteplase in all acute stroke patients otherwise eligible for thrombolysis as per Canadian acute stroke guidelines. The Canadian acute stroke guidelines are very similar to the European, American and Australian acute stroke guidelines.
The design of the trial was therefore pragmatic, with all acute ischaemic stroke patients who would otherwise be thrombolysed as part of standard care being eligible for enrolment. Comparability was to be shown via non-inferiority—if the lower 95% confidence interval [CI] of the difference in primary outcome rates between tenecteplase versus alteplase was greater than −5%, then tenecteplase would be considered non-inferior. The trial had a prospective randomised open blinded-endpoint (PROBE) design with blinded-endpoint assessments. The primary efficacy outcome was 90-day modified Rankin Scale (mRS) 0–1 rate collected centrally in a blinded manner, and key safety outcomes included symptomatic intracerebral haemorrhage rates at 24 hours and 90day mortality. Other pragmatic outcomes included return to baseline function at 90 days and ambulatory status at discharge.
The trial enrolled 1,600 patients. The primary outcome rate with tenecteplase
was 36.9% compared to 34.8% with alteplase (unadjusted risk difference 2.1%; 95% CI, −2.6 to 6.9), with the −2.6% lower 95% CI for the risk difference easily being greater than the −5% non-inferiority margin. The two drugs were comparable for all secondary and safety outcomes too. No statistical heterogeneity was seen across any relevant subgroups. The AcT trial therefore provides robust evidence that we can switch standard of care within 4.5 hours of stroke symptom onset to tenecteplase, given its ease of use when compared to alteplase.
What is the relevance of these findings and how are they set to impact clinical practice?
The AcT trial was designed to build evidence that would be considered robust and generalisable (i.e. evidence that mirrors real-world practice).
This is why large, pragmatic trials are important—their results can be directly applied to your practice. This impact of the trial’s pragmatic design is reflected by the fact that practice is now changing in Canada and across the world.
What are the major benefits tenecteplase offers, and why they are so crucial in stroke care?
The major benefits with tenecteplase are a) ease of use as a single intravenous bolus injection administered over 5–10 seconds, compared to a bolus and an hour-long infusion with alteplase, and b) easy workflow given that patients need not be transferred within and between hospitals when being administered thrombolysis using complicated intravenous lines and infusion pumps. These advantages would translate to faster treatment times, reduced overall treatment costs and, potentially, better outcomes for acute stroke patients.
Other studies have investigated a higher dose of tenecteplase than the one seen in AcT and produced more negative results. What is the significance of this?
Thrombolysis has risks; the most important amongst them being bleeding that is dose related. The evidence from the NOR-TEST 2 trial (Norway) and from the earlier phase 2 trials suggest that a higher dose of tenecteplase (0.4mg/kg body weight) causes more harm without any additional benefit. The body of evidence up to now, including from AcT, therefore suggests that we should be using tenecteplase at a dose of 0.25 mg/kg body weight for IVT.
to using tenecteplase because of tenecteplase’s ease of use. I see no reason why this will not happen in stroke given the AcT results—also published in The Lancet earlier this year. Transition always takes time though, as systems have to adapt; but this is a matter of time.
The recent study out of Dell Medical School (Austin, USA) is a real-world observational study—rather than an RCT—that is showing the efficacy and safety of tenecteplase. Such studies show the real-world benefits of tenecteplase in different settings and are therefore very helpful. The TECNO trial (Switzerland) is testing the utility and safety of intra-arterial tenecteplase. Such studies are important in helping expand indications and use of tenecteplase.
Other studies like the recent TWIST trial (Norway), and the ongoing TIMELESS (USA and Canada) and ETERNAL (Australia) trials, help us understand the utility of tenecteplase in the extended time window too. The ongoing ATTEST 2 (UK) and TASTE (Australia) phase 3 trials—along with the recently completed TRACE phase 3 trial (China)—will provide more evidence around tenecteplase use in acute stroke patients. All these trials are likely to help us transition globally to a more efficient thrombolysis paradigm in acute stroke.
For acute stroke treatments, is tenecteplase likely to replace alteplase completely in the future?
Yes, and we only have to look at the practice in cardiology to understand why. After the large ASSENT-2 RCT, which was published in The Lancet in 1999 and compared tenecteplase to alteplase in patients with acute myocardial infarction, demonstrating that mortality and bleeding risks were equivalent, practice changed completely
Some centres are already making the switch, but how long do you think it may be before, globally, tenecteplase becomes more widely used? There is a supply shortage of tenecteplase in Europe and some other parts of the world that is limiting this switch; otherwise, I see this transition happening very soon. In Canada and the USA, where there is no shortage of tenecteplase, this switch is happening right as we speak. Many hospitals and health systems have already moved to a tenecteplase-only IVT protocol, with others following suit. The transition will also accelerate once national guidelines reflect this new evidence, and the supply issues are being addressed too. Overall, I see us having moved to tenecteplase globally as the IVT drug of choice in acute stroke patients within the next 2–3 years.
Can you provide insight on which direction you feel tenecteplase research should now take in order to further bolster these promising findings?
We need to develop robust evidence for thrombolysis in many conditions where, previously, because of restrictive trial criteria within the initial alteplase thrombolysis trials, evidence was weak.
We also need to better understand the utility and safety of tenecteplase in patients undergoing endovascular therapy (EVT); those who may be on newer anticoagulants or antithrombotics; those with other risk factors like renal dysfunction, high blood pressure or high blood glucose; and even in the elderly. We need to better understand how to use thrombolysis when modern imaging information on risk and futility is available. And we need to understand if the effect of thrombolysis with tenecteplase can be enhanced and whether concomitant therapies might improve outcomes further. As Dickens said: “These are the best of times…”; we have an incredible opportunity here, if only we can make use of it.

11 Issue48 | December 2022 Intravenous Thrombolysis
How important do you think further recent/ongoing studies are in building on the positive data seen in AcT?
Overall, I see us having moved to tenecteplase globally as the intravenous thrombolysis drug of choice in acute stroke patients within the next 2–3 years.”
Bijoy Menon
Similar complication rates observed following DAPT discontinuation within and past 90 days in Pipeline Shield treatments
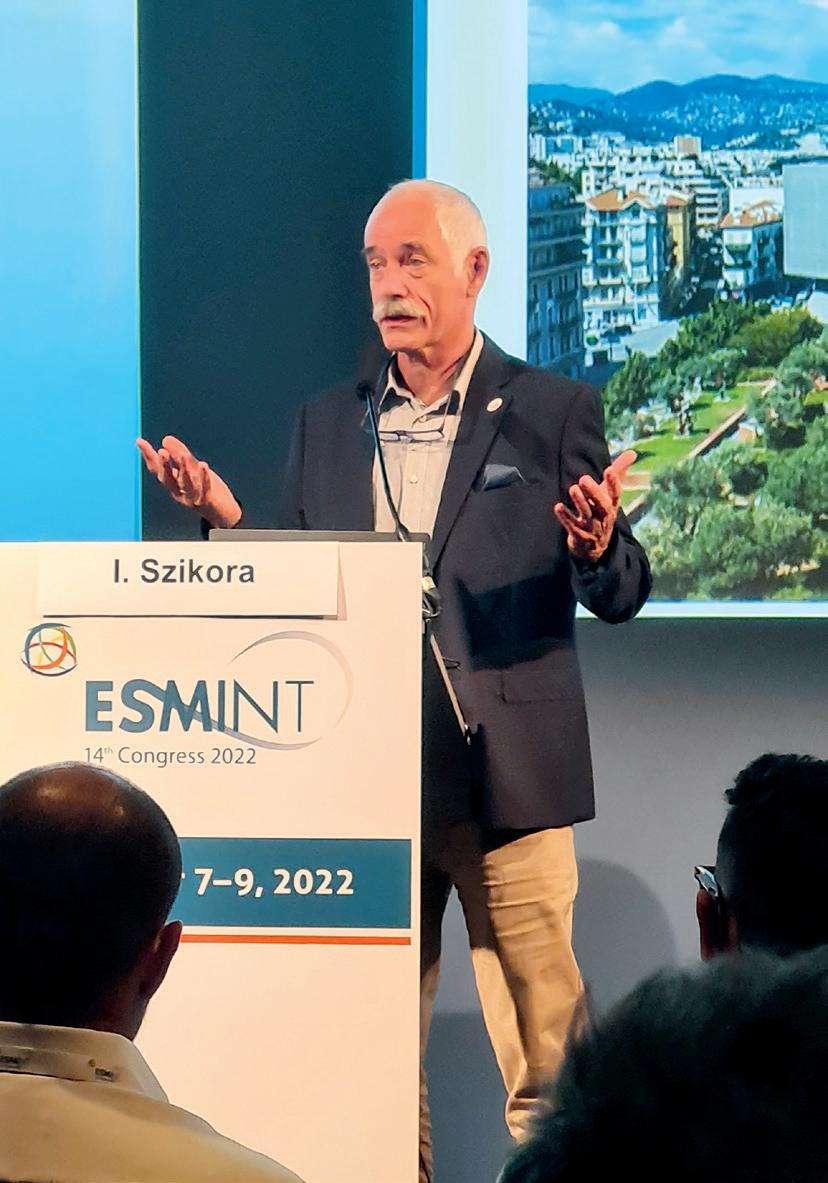
The duration of dual antiplatelet therapy (DAPT), either 30–90 days or more than 90 days, following implantation of a flow diverter in cerebral aneurysm patients has been found to have no significant effect on major complications and adverse events. Lower incidences of reported neurological death or major ischaemic stroke were also observed after the discontinuation of DAPT—regardless of whether a shorter (<90 days) or longer DAPT protocol was used—as per a global analysis presented for the first time at the 2022 European Society of Minimally Invasive Neurological Therapy (ESMINT) congress (7–9 September, Nice, France).
These findings were delivered by István Szikora (National Institute of Mental Health, Neurology and Neurosurgery, Budapest, Hungary) who, speaking to NeuroNews following the session, said: “This study was not designed to compare coated versus non-coated devices, as it only analysed the events [seen with] the Pipeline Shield—the coated version of Pipeline [Medtronic]. The results suggest that elongated DAPT, such as over three months, is likely not needed for the majority of aneurysms. The data presented here may help to design more accurate observational studies to analyse the need for DAPT in association with such devices.”
At the outset of his presentation, Szikora informed the ESMINT audience that DAPT is considered necessary following flow diverter implantation, primarily as a means for preventing thromboembolic complications and reducing in-stent stenosis risks— but there is currently a lack of guidelines regarding the optimal duration for which these treatments should be administered. In addition, studies from the cardiovascular space have highlighted increased bleeding complications, problems with patient compliance and higher costs as potential drawbacks associated with DAPT.
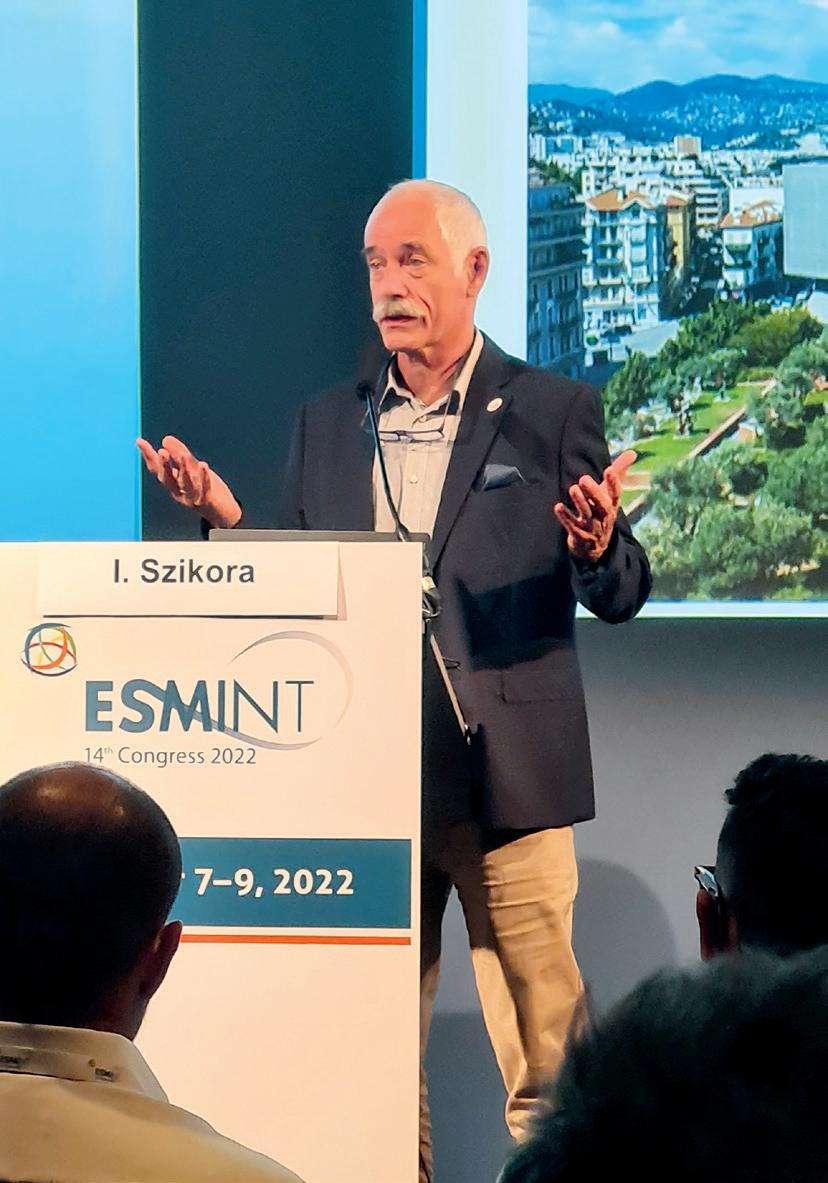
As such, Szikora and his co-investigators set out to analyse the duration of DAPT regimens, within a realworld setting, using three global, postmarket studies of the Pipeline Shield flow diverter: INSPIRE-A, SHIELD OUS and PFLEX. Combining these studies gave the investigators a total population of 750 patients, of which 714 were deemed eligible and had available follow-up data at six months. Szikora detailed that these patients were categorised into different groups based on the length of time for which they received DAPT—with 22 patients receiving DAPT for 0–30 days, 105 patients for 31–90 days (a patient number that Szikora noted was “surprisingly low”) and 605 for >90 days.
“We also had a group of patients who were on DAPT for more than 180 days [containing 353 patients], but this group also included those who were in the third group [>90 days], so there is an overlap between groups three and four,” the speaker added.
Szikora and colleagues analysed all major complications and adverse events across these patient groups—including neurological deaths, major/all ischaemic strokes, thromboembolic complications, significant stenoses and any other major complications. Regarding baseline data, such as age, sex and comorbidities, as well as aneurysm characteristics, no significant differences between the
four patient categories were found.
Reporting results from these analyses, Szikora noted a rate of 13% for all major complications/stroke and neurological deaths from 0–30 days, describing this as a high number, but adding that this was a result of three patients dying from bleeding complications within a matter of days following the flow diverter implantation procedure.
“But, comparing [all complications] within 90 days, and after 90 days, we did not find any significant differences,” he continued. “Going further, regarding complication rate by incidence time […], we found that the great majority of the total number of [all
thromboembolic complications] occurred within the first 30 days—regardless of how long DAPT was administered for.”
Szikora went on to state that—again, regardless of DAPT duration—a similar preponderance of major bleeding complications, neurological deaths and major/all ischaemic strokes was seen from 0–30 days. He further noted that data on significant stenoses differed slightly, as this is not routinely assessed within the first 30 days post-implantation, but that, based on patients’ first follow-up angiographies, no significant difference was found between the four groups here either.
Detailing the “most significant finding” of this analysis, the speaker reported that—in addition to the vast majority of complications and adverse events occurring within the first 30 days—all but one of these complications/events occurred before the discontinuation of DAPT, with the single event that occurred post-DAPT continuation being seen after more than 350 days in a patient who had received DAPT for over 200 days. He went on to state that, overall, patients who received DAPT for 31–90 days did not have a higher incidence of reported safety events after DAPT discontinuation as compared to those in the longer DAPT duration categories (>90 days and >180 days).
According to Szikora, limitations of this analysis included its retrospective nature, the fact the DAPT duration categories do not precisely reflect those commonly seen in clinical practice (three or six months), the different sample sizes between these categories, and a lack of standardisation due to DAPT regimens being at the treating physician’s discretion— although he claimed the latter was also beneficial in removing the “ethical dilemma” of mandating specific treatment protocols in assessing the significance of DAPT duration.
Briefly touching on future research directions, Szikora noted that these findings highlight the need for prospective studies to assess the impact of DAPT duration on safety outcomes, as this will “help to drive guidelines” in the neurointerventional space. However, responding to a question from session moderator Marios Psychogios (University Hospital Basel, Basel, Switzerland) regarding the timepoint at which patients should be randomised to receive single antiplatelet therapy (SAPT) or DAPT in future studies, Szikora said that, at this point, “we do not have enough scientific evidence to randomise”.
“I believe that these are interesting observations,” he continued, “but we must accept that none of these studies [INSPIRE-A, SHIELD OUS and PFLEX] were designed to answer this question. It would be absolutely irresponsible to start designing a randomised study based on [our analysis]. It is an important piece of information, but we need to continue analysing these data.”
Szikora also reiterated that, in future trials, it would be appropriate to select DAPT timeframes that more accurately reflect everyday clinical practice—for example, three months, as typically prescribed at his own centre—and future analyses may even benefit from excluding patients who receive DAPT for much shorter periods of time—for example, 30 days or less.
12 December 2022 | Issue48 Research Updates: Aneurysms
The results suggest that elongated dual antiplatelet therapy [DAPT], such as over three months, is likely not needed for the majority of aneurysms. The data presented here may help to design more accurate observational studies to analyse the need for DAPT in association with such devices.”
István Szikora
Increased coiling rate suggests shift towards endovascular techniques during COVID-19 pandemic
A global study published in the Journal of Neurology, Neurosurgery and Psychiatry (JNNP) has revealed that, while ruptured aneurysm clipping rates remained largely unchanged, there was an increased rate of ruptured aneurysm coiling between 2019 and 2021—which the authors believe indicates a shift towards endovascular techniques during the first year of the COVID-19 pandemic.
IN THEIR JNNP REPORT, THANH Nguyen (Boston University School of Medicine, Boston, USA), Raul Nogueira (University of Pittsburgh Medical Center, Pittsburgh, USA) and colleagues also note that, over the same period, there was a decrease in aneurysmal subarachnoid haemorrhage (aSAH) admissions volume, driven by a decrease in mild-to-moderate aSAH presentations. However, they observed no significant difference in aSAH inhospital mortality between the pandemic and pre-pandemic years—except within a subgroup analysis of higher aSAH mortality in hospitals with the highest COVID-19 burden—attesting to “resilience in the care of patients with aSAH amidst the pandemic”.
The researchers set out to evaluate differences in the incidence and severity of aSAH presentation, and ruptured
aneurysm treatment modality, during the first year of the COVID-19 pandemic (1 January 2020 to 28 February 2021) compared with the preceding year (1 January 2019 to 29 February 2020). They conducted a cross-sectional, retrospective study including 49 countries and 187 centres, with primary objectives being to evaluate changes in the volume of non-traumatic SAH, aSAH hospitalisations and aSAH in-hospital mortality, and secondary objectives being to evaluate the severity of aSAH admission presentation, the modality treatment of aSAH, and the associations between COVID-19 admission volumes and aSAH volumes, over the same period.
“Our primary hypothesis was that, similar to the first wave, there would be a decrease in SAH and aSAH hospitalisations between the first year
of the COVID-19 pandemic and the preceding year,” Nguyen, Nogueira and colleagues write. “Our secondary hypothesis was that there could be a shift toward increased use of ruptured aneurysm coiling, as we had observed in the first wave of the pandemic.”
Across the total study period (1 January 2019 to 31 May 2021), there were 20,680 non-traumatic SAH admissions and 344,491 COVID-19 admissions among participating centres, the authors detail. Of these, there were 16,247 aSAH admissions, and 8,300 endovascular coiling procedures and 4,240 aneurysmal clipping procedures over the study period.
Reporting their results, Nguyen, Nogueira and colleagues note observed declines in aSAH admissions (–6.4%, p=0.0001) during the first year of the pandemic compared with the prior year—with this being most pronounced in high-volume SAH and high-volume COVID-19 hospitals. There was a trend towards a decline in mild (−5%, p=0.06) and moderate (−8.3%, p=0.06) presentations of SAH too, but no difference in higher SAH severity.
According to the researchers, ruptured aneurysm clipping rates remained unchanged before and during the first year of the pandemic (30.7% vs 31.2%, p=0.58), whereas ruptured aneurysm coiling increased (53.97% vs 56.5%, p=0.009). There was no difference in aSAH in-hospital mortality rates between these two time
Adjunctive therapy demonstrates comparable aneurysm occlusion rates to established flow diverters
The Neqstent coil-assisted flow diverter (Cerus Endovascular) has demonstrated comparable occlusion rates to those seen with other, similar flow diversion technologies, as well as positive device stability and safety outcomes. These new data were presented by Thomas Liebig (Ludwig Maximilian University, Munich, Germany) at this year’s European Society of Minimally Invasive Neurological Therapy (ESMINT) congress (7–9 September, Nice, France).

LIEBIG BEGAN HIS PRESENTATION BY outlining the use of Neqstent as an adjunctive therapy in the treatment of intracranial aneurysms, claiming that this technique intends to provide stable aneurysm neck coverage for the placement of embolisation coils as well as long-term aneurysm occlusion. He also described Neqstent as the “smaller brother” of Cerus’ Contour device, owing to the latter having a higher mesh density.
The CAFI study—for which Liebig is the principal investigator—was set up to assess the performance of the 7mm, 9mm and 11mm iterations of the Neqstent device. According to Liebig, this prospective, multicentre, single-arm study was conducted across several European centres, including in Austria, Denmark, Germany and Switzerland, while some cases from Canada were also added.
All 38 patients enrolled in the CAFI study had nonruptured bifurcation aneurysms, with Liebig noting a female predominance, an average age of roughly 60 years, and no neurological deficits, in the intention-totreat cohort. He added that the most common aneurysm locations were the anterior communicating artery (Acom) and basilar artery tip, followed by the middle
cerebral artery (MCA), and that—on average—the aneurysms seen in the study were “not very large”.
“The majority [of patients] were treated with a 7mm or 9mm device, and this was successful at the first attempt in almost 90% of cases,” Liebig reported. “In two patients, it was not possible to place the device due to anatomical issues.” He later detailed difficulties in expanding the device in one
periods (19.1% vs 20.1%, p=0.12), the researchers add.
Nguyen, Nogueira and colleagues conclude by stating that there was a decline in non-traumatic SAH and aSAH admissions during the first year of the COVID-19 pandemic—and this decline was “likely driven by an observed trend in the decline of patients presenting with mild-to-moderate aSAH”, and is concordant with decreases seen in other urgent cases, such as ischaemic stroke.
Ruptured aneurysm treatments
of these two cases, illustrating a problem that may be encountered when treating aneurysm recurrences following prior implantation of a Woven EndoBridge (WEB; Microvention) device—something that has also previously been observed with Contour.
The primary safety endpoint was ischaemic event with ongoing symptoms at last follow-up, he continued, and—across the 36 patients who successfully underwent Neqstent implantation—this occurred in two patients within the first six months after the procedure. There were no non-accidental or neurological deaths.
“In terms of device stability, there was only one case where the device, together with the coils, had moved up at followup—leading to a neck remnant that did not [require] treatment,” Liebig added.
Occlusion rates were assessed using both the Raymond-Roy (RR) and WEB occlusion scales, according to the speaker, who reported that Neqstent yielded similar occlusion results to those seen previously with the Contour and WEB devices, demonstrating a combined RR1+2 rate of 86.2% and a WEB occlusion rate of 83.4% at the six-month follow-up timepoint.
He added that six-month follow-up data were available for all 36 patients, but 12-month follow-up data are currently only available for six of the included patients.
“We have to collect a few more 12-month followups,” Liebig concluded, “but we are fairly happy with our results so far—especially [the fact] there was only one device movement leading to a neck remnant.”
13 Issue48 | December 2022 Research Updates: Aneurysms
We have to collect a few more 12-month follow-ups, but we are fairly happy with our results so far—especially [the fact] there was only one device movement leading to a neck remnant.”
30.7% 31.2% Clipping rate before first year of pandemic Clipping rate during first year of pandemic 53.97% 56.5% Coiling rate before first year of pandemic Coiling rate during first year of pandemic
Thomas Liebig
Process times and regional variation are main areas of concern for thrombectomy care in England
Technical and clinical outcomes associated with mechanical thrombectomy treatments in England are currently “acceptable”, but ‘drip-and-ship’ patients, process times and variation between units all represent concerns in stroke care moving forward, as per discussions at this year’s European Society of Minimally Invasive Neurological Therapy (ESMINT) congress (7–9 September, Nice, France).
These messages were delivered by Phil White (Newcastle University, Newcastle upon Tyne, UK), whose presentation pertained to ‘the current situation in the UK’—although the speaker prefaced his talk by noting that he would primarily be focusing on England, as the constituent parts of the UK operate independent healthcare policies and, as such, “have all approached stroke thrombectomy in a different way”.
Drawing on data from the Sentinel Stroke National Audit Programme (SSNAP), White reported that monthly thrombectomy rates have steadily increased over the past few years— largely driven by level 1a evidence favouring thrombectomy from the 2016 HERMES collaboration paper—and, after ‘flatlining’ through much of 2020 due to the COVID-19 pandemic, these numbers have picked up again recently, reaching roughly 200 procedures per month at the start of this year.
Existing problems
White also noted that the “main shortfall” in thrombectomy volumes across England stems from discrepancies between ischaemic stroke patients who are admitted directly to a comprehensive stroke centre (CSC), and those in drip-and-ship cohorts who are treated with intravenous thrombolysis (IVT) at a frontline hospital before being transported to a CSC, to undergo a thrombectomy.
The speaker went on to state that a theoretical maximum thrombectomy rate of 10% (across the total number of stroke admissions) has been devised, meaning roughly 8,000 eligible patients should be receiving this treatment each year in England. In reality, of those patients admitted directly to a CSC, around 6% currently undergo a thrombectomy—which White said compares reasonably with the rates seen in countries like Germany (8%) and Ireland (9%).
However, at 3%, the national average in England is “much lower”, he continued, and, while this represents solid progress and a sixfold increase
from a baseline rate of <0.5% in 2016, this average is being lowered by a “pretty miserable” 1.5% thrombectomy rate within drip-and-ship cohorts. Here, there can be significant difficulties with identifying and referring patients at primary stroke centres, he added.
White alluded to the impact of the pandemic on these figures, reporting a 28% “overnight” reduction in thrombectomy rates following the first COVID-19-related lockdown in 2020, with the “erratic and slow recovery of activity” across the UK healthcare system—but particularly within emergency and ambulance services— leading to process times being badly affected and some areas still struggling today.
In addition, nearly half of all centres in England (46%) tightened their patient acceptance criteria during the pandemic, according to White, which exacerbated these effects.
Given the fairly low thrombectomy numbers seen across England, White posed the question of whether the outcomes associated with the procedures are ‘acceptable’. He asserted that, in both a clinical and a technical sense, they are, owing to reasonable levels of efficacy and procedural safety observed
across real-world populations—and, although there is “probably too much variation” across the country right now, a lack of statistical outliers here suggests ‘the law of small numbers’ could be a key contributor.
Touching on further real-world stroke data, White reported a median thrombolysis in cerebral infarction (TICI) 2b–3 rate of 79%, which is in line with other real-world literature, and a ‘good’ modified Rankin Scale (mRS) score (≤3) at discharge—a “reasonable but imperfect” outcome marker, according to White—of 53%, as well as 20% technical complication and 17% 30-day mortality rates, both of which are essentially in line with previous trial data.
However, regarding processes, such as ‘door-to-puncture’ and ‘door-indoor-out’ times, he said the healthcare system “can do much better”, adding that “we have gone backwards, and have not really [returned] to where we were before the pandemic”.
Expanding on these process times in England, White reported that the national median door-to-puncture time is more than three hours (192 minutes) and, while this figure drops to a “more acceptable” 50 minutes in CSCs, the wide range of timings here (36–106 minutes) is less positive.
The speaker went on to detail “particularly troublesome and worrying” door-in-door-out times, with a postpandemic national median of 155 minutes (up from a pre-pandemic average of 130 minutes) that is “not going down”. He also noted that this falls short of a 90-minute interim
target devised from modelling by his research group, and is “way off” the ideal target of 60 minutes that he and his collaborators have proposed.
“This really reflects things that happen outside of the CSC,” White stated. “There is some impact on doorin-door-out times, but not very much, [from] what happens in CSCs.”
Looking forward
White concluded his ESMINT presentation by stating that “we have made modest progress in England”, and that some areas have performed better than others, with comprehensive 24/7 coverage established across Greater London, but “much lower” thrombectomy rates in other regions and potentially “unacceptable” variation between units.

He also reiterated the fact that low procedure volumes, particularly in dripand-ship patients—who are simply “not getting here [to CSCs] fast enough”— suggest system-wide issues, while process times are too long and have declined in recent years as well.
Speculating on what is driving these problems, White said: “This is multifactorial—there is inertia in our system, and it is a disruptive innovation that requires a lot of things to change. And, without upfront capital and personnel investment to facilitate development, [it will] be difficult.”
The speaker also highlighted the ongoing impact of COVID-19 on this state of affairs, before adding that “we have had a sustained lack of investment since the financial crisis of 2008, lagging well behind the [healthcare] inflation rate in terms of money being spent on the system” and, while the number of interventional neuroradiologists in England has progressed, Brexit has created “well-reported difficulties” in the recruitment and retention of EU staff.
Responding to a question from session moderator Vladimir Kalousek (Clinical Hospital Sisters of Mercy, Zagreb, Croatia) on UK training protocols and which physicians are allowed to perform thrombectomies, White noted that guidance published in early 2017 allows any radiologist to be trained in mechanical thrombectomy—but, nearly six years on from this, a mechanism relating to non-radiologists is yet to be fully signed off by the UK General Medical Council (GMC).
Here, White further commented that, in spite of the “pressing need” here, this process has been “very slow” for a variety of reasons and, although England has doubled its number of interventional neuroradiology trainees since 2016 and there is also a small handful of UK neurosurgeons who currently perform thrombectomies, the country is still short of interventional and general radiologists, holding one of the lowest per-person rates across Europe.
“Anybody with appropriate training can do it—but the credentialing process to do it with GMC approval is still ongoing,” he added, drawing the discussion to a close.
14 December 2022 | Issue48 ESMINT Congress
There is some impact on door-in-door-out times, but not very much, [from] what happens in comprehensive stroke centres.”
Phil White
Physicians should prioritise firstpass optimisation over speed in thrombectomy procedures
Achieving clot retrieval with the fewest possible number of passes is critical in mechanical thrombectomy, and may even hold greater importance than how quickly the procedure is completed—despite the age-old mantra that ‘time is brain’. That is according to a recent presentation from the European Society of Minimally Invasive Neurological Therapy (ESMINT) congress (7–9 September, Nice, France), delivered by outgoing ESMINT president Jens Fiehler (University Medical Center HamburgEppendorf, Hamburg, Germany), who also claimed that, “at any given time, reperfusion is still better than no reperfusion”.
FIEHLER BEGAN WITH A NOD TO THE undoubted relevance that time to recanalisation has, referencing previous studies that have demonstrated the direct influence reperfusion times have on computed tomography (CT) perfusion imaging outcomes.
“We definitely have a time dependency and we all know that complete reperfusion is the desired outcome for thrombectomy,” he said. “And, Osama Zaidat’s group [Mercy Health, Toledo, USA] made it clear, really for the first time, that it is also about having complete reperfusion as early as possible.”
Moving on to discuss the lauded ‘first-pass effect’ in thrombectomy, defined as complete reperfusion (thrombolysis in cerebral infarction [TICI] 2c–3) with a single device pass, the speaker noted a “huge difference” between achieving recanalisation at the first pass versus with two or more passes. “Any TICI 3 is already 6% worse [on average] than first-pass TICI 3, and any TICI 2b is worse still,” Fiehler asserted.
Here, he also touched on the fact that several publications have shown higher reperfusion rates are achieved with each successive retrieval attempt— “obviously”, because they are essentially “adding up”—but that, in reality, the rate of good clinical outcomes does not actually improve beyond the third attempt. And, despite the fact that successful reperfusion will naturally always lead to improved outcomes when compared directly to no reperfusion, Fiehler stated that average outcomes associated with four-plus attempts are “no better than if we
Basecamp
Vascular announces firstin-human cases with
steerable mechatronic guidewire
Basecamp Vascular (BCV) has announced a “major step” in the development and evaluation of steerable mechatronic guidewires for stroke treatment via its GECKO system.
A FIRST-IN-HUMAN CASE WITH the device was conducted by Michel Piotin (Foundation Rothschild Hospital, Paris, France), and presented for the first time at the 2022 European Society of Minimally Invasive Neurological

did not try at all”.
“But the problem is that we cannot go back in time,” he continued. “We cannot say ‘what if we did not try it’—we did try it, because, at any given time, reperfusion is likely better than no reperfusion.”
According to Fiehler, prior research has found that failed reperfusion attempts may be harmful as well, with one study involving TICI 0 patients demonstrating a 40% rate of good outcome in 0–1 attempts versus just 4% with two or more attempts.
“So, we can actually harm patients [if we are not] successful,” he noted.
Outlining another illustration of this problem, Fiehler claimed that, while TICI 3 reperfusion at both the first and second pass results in better outcomes than first-pass TICI 2b reperfusion, outcomes following TICI 3 in three or more passes are “no better” than those seen with first-pass TICI 2b.
“The conclusion is that you need to be pretty sure that, with the second retrieval attempt, you [will] achieve TICI 3,” he explained. “And, if you do not, then you made the wrong decision and you should have stopped right away.”
Referencing a study published by him and his colleagues, Fiehler noted a trend towards elapsing
Therapy (ESMINT) congress (7–9 September, Nice, France).
“Physicians face many challenges with neurovascular pathologies in navigating to the treatment site rapidly and safely,” said Piotin. “GECKO, through its design versatility and electronic navigation, facilitates the management of complex arterial manoeuvres, saving time and minimising device exchanges.
“We are very pleased to be the first users and look forward to realising the many benefits of this device in our patients.”
As per a BCV press release, more than 12.2 million people suffer a stroke globally each year, while the estimated global cost of the condition is more than US$721 billion.
A key issue in stroke treatment—the release continues— is speed to
time being linked to poorer outcomes—even within a group of patients who underwent successful recanalisation at the first attempt. He also informed the ESMINT audience that the issue becomes “really complex” when attempting to analyse which of these two factors, time elapsed or number of passes, independently affects patient outcomes more profoundly. “But, the conclusion was that it is not so much the time that makes the difference—it is the number of passes,” he added.
Fiehler conceded that interpreting many of the ‘per-pass’ data these arguments are based on is “very difficult” as well, owing to the variability that can be found across multicentre, self-assessed studies. He cited the fact that different operators will likely define success differently and make contrasting decisions about, for example, whether or not to continue following the first two or three unsuccessful retrieval attempts, and their decision-making process will also be influenced by the individual patient in front of them.

“Theoretically, the only way to solve this is to have a randomised controlled trial […] and I think the most sensible approach would be to have a randomised trial after the third failed attempt,” Fiehler opined. “Similar things are already happening with ICAD [intracranial atherosclerotic disease] patients—for instance, the ANGEL-REBOOT study in China is randomising stenting versus doing nothing after two failed attempts—and I think this could help us better understand the problem.”
Fiehler concluded that first-pass TICI 3 should always be the operator’s goal and, responding to a query from the audience regarding aspiration versus other thrombectomy techniques, stated: “If you are successful at the first pass with aspiration, that is wonderful, but the problem is more to do with how often we get there. My own thinking regarding these data is that [we should] put everything into the first attempt—rather than simply doing a quick aspiration first and then making a more technical effort later.”
intervene, as each minute represents nearly two million lost neurons. During stroke intervention, complications can arise that delay access to the clot and cause issues in patient recovery, with current approaches sometimes involving excessive time and devices to obtain access to the stroke location, depending on anatomical complexity.
“Because ‘time is brain’, at BCV, we developed the GECKO—a sterile, Class 3, single-use, steerable mechatronic guidewire intended to facilitate the access and positioning of a catheter to reach the obstructing clot,” added Raphaël Blanc (Foundation Rothschild Hospital, Paris, France), CEO of BCV.
GECKO was designed to allow faster navigation and reduce complications, especially in tortuous
vessels, according to the release. The system is compatible with existing catheters and image-guided platforms, and has potential applications in any procedure requiring guidewire access, including cardiovascular, urological, gynaecological, oncological and bariatric procedures.
Elsewhere in the ‘Start-Up Alley’ portion of the ESMINT 2022 programme, Oxford Heartbeat’s PreSize neurovascular technology, intended for artificial intelligence (AI) software simulation in flow-diverting stent deployment; Intradys’ Lumys mixed reality platform, designed to provide live communication during procedures; and Artiria Medical’s own efforts to develop an augmented neurovascular guidewire technology, all featured.
15 Issue48 | December 2022 ESMINT Congress
Michel Piotin
We are very pleased to be the first users and look forward to realising the many benefits of this device in our patients.” Michel Piotin
Michel Piotin
Jens Fiehler
Shelley Renowden
Through her many years as a consultant neuroradiologist at the North Bristol NHS Trust (Bristol, UK), as well as organising the European Course in Minimally Invasive Neurological Therapy (ECMINT) and making leading contributions to the UK Neurointerventional Group, Shelley Renowden has played a significant role in growing the specialty of interventional neuroradiology (INR) across the UK. In recent years, her work in training future generations of INRs has also expanded overseas through the European Society of Minimally Invasive Neurological Therapy’s (ESMINT) education committee. Renowden discusses these efforts, the formative years of her career, and some of the most pressing matters in the neurointerventional field right now, with NeuroNews
What initially attracted you to medicine, and the field of neuroradiology specifically?
I was attracted to a career in medicine because I considered it to be challenging, very varied, stimulating, and fun, while meeting lots of people. Who wants a boring career spanning 35 years or more? I went into radiology for the same reasons—on my elective, it was a radiologist who stimulated me the most by a long way and, when doing my internship, it was the radiologists who seemed to be the most knowledgeable and human!
I went into academic radiology, not only doing cross-sectional imaging (my chosen specialty at that time—I did actually declare at one point that I would never do another cerebral angiogram!), but also working towards an MD in vasomotor control mechanisms in the human umbilical artery and a chance ‘throwaway’ remark one day catapulted me into neuroradiology. The neuroradiology consultant in the University Hospital of Wales (Cardiff, UK), Margaret Hourihan, was due to go on maternity leave and could not find a locum for her period of absence. As a lecturer, I asked her if she wanted me to do it. She was delighted, and I did a consultant neuroradiology locum for four months and absolutely loved it. After that, I obtained a neuroradiology training post at the Radcliffe Infirmary (Oxford, UK) where I spent four wonderful, stimulating, exciting, inspiring and enjoyable years.
ECMINT was the dream of James Byrne and the ESMINT board. James had already booked St Anne’s College (Oxford, UK) and had a curriculum sketched out, but we organised the first course within three months—I do not know how we achieved that! Firstly, it is important because it is a very intense theoretical course. Every cycle comprises four courses, each of which is nearly one week long and encompasses all the knowledge necessary for the practice of INR, with detailed vascular anatomy, embryology, pharmacology, pathophysiology and haematology techniques (also neurosurgery and radiosurgery where applicable),

Margaret Hourihan brought me into neuroradiology and encouraged me. The neuroradiologists at the Radcliffe Infirmary provided a wonderful training— particularly Andrew Molyneux, guiding me into neurointervention, and Philip Anslow, the best diagnostic neuroradiologist and teacher I have ever met (and great fun). He encouraged my diagnostic skills in paediatric neuroradiology, epilepsy and the skull base, which I did whilst also expanding the INR service in Bristol many years ago. My interventional training in Oxford and my supportive neurovascular surgical colleagues in Bristol (Richard Nelson and also, later, David Porter), and as well as highly specialised and dedicated neurovascular nurses and radiographers, have enabled the development of a nationally acclaimed UK neurovascular centre and the training of INRs—our first being Marcus Bradley, who is still a current source of great support.
With James Byrne, I embarked upon the first Oxford MSc course in endovascular surgery (along with the fabulous Paul Brennan from Dublin, Ireland), and I will always be enormously grateful and indebted to James, because he asked me to help him start up and run ECMINT. This has had a major impact on my career and I only wish it had come earlier. I also need to include Anil Gholkar, who provided invaluable support and advice in my earlier professional years. I thank them all.
and now medical statistics and an expanding spinal component as well. It comprises a series of lectures and tutorials given by European experts, and formative quizzes and exams. Attendance for an entire cycle and passing the course exams are an entry criterion for the European Diploma in Neurointervention (EDNI). I wish it had existed in my formative years, because it would have made life so much easier and I would almost certainly have been a better INR. I have learnt so much from ECMINT, and it also provides a base for INRs to meet from all over world, to discuss and form long-lasting professional relationships. St Anne’s College just buzzes with energy and enthusiasm during the week of the course. One feels totally rejuvenated and exhilarated even after an extremely intense week.
What do you feel has been the most important development in the INR field during your career?
I have been very lucky to be involved in INR during a period of great development and transformation, so I must include two.
First, Guglielmi detachable coil (GDC)embolisation of intracranial aneurysms, leading to the ISAT study—this was a major contribution to the management of intracranial aneurysms that significantly enhanced and consolidated the field of INR. It paved the way for advances in other endovascular devices to manage more complex
aneurysms (and, of course, the Solitaire stent [Medtronic] went on to be a major player in stroke thrombectomy). Currently, the vast majority of aneurysms are treated endovascularly.
Second—obviously—thrombectomy for large vessel occlusion in hyperacute ischaemic stroke, which significantly improves outcomes for many thousands of patients (and their families) worldwide each year and lessens the stroke burden on society.
What is the most significant unmet need in neuroradiology right now?
Probably, in many countries, effective and more efficient management of the entire stroke service is an important need. In no other area of medicine (except perhaps major trauma) is an efficient collaborative team effort so important but, on a global scale, we may still be a little way off from “drip and drive” at the moment.
16 Interview December 2022 | Issue48
Who have your mentors been and how have they impacted your career?
How was the ECMINT course set up, and why is it an important offering in this space?
PROFILE
alisonlang.com
The necessary role models are out there. Assertiveness and leadership training are critical in the training of most female INRs, to enable their development and to lead the way.”
Current (or recent) roles:
Consultant neuroradiologist, North Bristol NHS Trust (Bristol, UK)
Examiner, Endovascular Neurosurgery MSc, Oxford University (Oxford, UK)
Societies:
2012: Chairperson at the inaugural World Arteriovenous Malformation (AVM) Congress
2014–2020: ESMINT Executive Board member and chair of Education Committee

2016–2019: Examiner for the European Diploma in Neurointervention
2019: World Federation of Interventional and Therapeutic Neuroradiology (WFITN) Scientific Committee member
ECMINT course co-director and organiser
Besides your own work, what is the most interesting piece of neurointervention research you have seen in the past year?
Neuroprotection—because, despite thrombectomy, around 50% of patients do not achieve independence. I think neuroprotection in conjunction with revascularisation is a potentially exciting and certainly interesting advance in stroke management and, possibly, in delayed cerebral ischaemia in subarachnoid haemorrhage too, where changes at a cellular level are similar. Many agents and methods are currently being trialled and investigated.
How would you assess the representation of female physicians in INR?
Diversity in any group is important and this is increasingly recognised. The number of female physicians in INR is growing—although still not enough— and I only have to look at the numbers of female attendees at ECMINT to see that. Role models and support for women are necessary. A great professional WhatsApp group has mushroomed in the space of one year and currently includes more than 700 women from all over the world, providing not only support but also a valuable source of education and advice. The necessary role models are out there. Assertiveness and leadership training are critical in the training of most female INRs, to enable their development and to lead the way.
What advice would you give to people embarking on a career in neuroradiology?
I would advise them to be thorough in their work and not take shortcuts. I recommend thoughtful, questioning and regular reading. One should listen to and be able to discuss with colleagues. Include others, be respectful and supportive, and do not show irritation. I also urge leading multidisciplinary meetings, teaching and lecturing, ‘putting yourself out there’ and involvement in professional societies from an early stage.
What are your interests outside of the field of medicine?
Sport is important for brain health and general wellbeing, and I go to the gym two or three times each week and have a weekly intensive tennis lesson— which completely suits my competitive spirit! I also love cooking, trying out new recipes and entertaining my friends. I have always loved learning languages and, for the last few years, I have had weekly Spanish lessons. My progress is not nearly as fast as I would like—I really need to visit Spain to practise. We have a cavapoochon, a highly intelligent, communicative and very spoilt dog who requires a lot of attention.
Honours (selected):
Education and update course founder, UK Neurointerventional Group
Fellow, European Board of Neurointervention
More than 100 published academic papers
Journal referee for British Journal of Neurosurgery; JNNP; Journal of Neurology; Neuroradiology; World Neurosurgery
Contributor to eBrain
17 Interview Issue48 | December 2022
Fact file
Abnormal DW-MRI foci “significantly more frequent” with radial versus femoral access
A prospective analysis of 200 consecutive diagnostic cerebral angiograms has indicated that the number of diffusionweighted magnetic resonance imaging (DW-MRI) restriction foci was “significantly more frequent” when transradial access was used—as compared to the more established transfemoral access approach.
AS PER A RECENT PUBLICATION FROM Vinicius Carraro do Nascimento (Gold Coast University Hospital, Southport, Australia) and colleagues in the Journal of NeuroInterventional Surgery (JNIS), the occurrence of clinically symptomatic events within in this analysis was minimal. However, the authors note that the increasingly widespread use of radial access may lead to this becoming more clinically relevant in the future. Carraro do Nascimento and colleagues begin their report by stating that the aforementioned approach
has grown in popularity in recent times, with a ‘radial first’ access strategy via the radial artery being used in both neuroangiography and neurointerventions.
“Recent studies have shown that transradial arterial access for cerebral angiography has been associated with reduced access site complication rates and improved patient satisfaction compared with transfemoral access,” they write. “The goal of this study was to evaluate the presence of abnormal [DW-MRI] foci following DSA [digital subtraction angiography] and correlate their frequency with transradial access or transfemoral access.”
As such, they prospectively analysed 200 consecutive adult DSAs, performed from January 2021 to January 2022, at a single tertiary centre. Of these 200 consecutive diagnostic cerebral angiograms, 51% were performed via transradial access and 49% were performed via transfemoral access.
Some 17.5% of the transradial access angiograms demonstrated at least one hyperintense focus on DW-MRI, Carraro do Nascimento and colleagues report. Meanwhile, of the transfemoral access procedures, 5.2% were considered positive. One patient (0.5%) in the transradial access group experienced a minor neurologic deficit postoperatively that had not completely resolved at 90 days after the procedure—and no
RAPID Aneurysm programme shows positive early performance in retrospective study
RAPID Aneurysm, a semi-automated artificial intelligence (AI) software programme (RapidAI), is highly accurate in detecting cerebral aneurysms on computed tomography angiography (CTA) imaging, according to a retrospective study published recently in the Journal of Stroke and Cerebrovascular Diseases by investigators Jeremy Heit (Stanford University School of Medicine, Stanford, USA) and colleagues.
DETAILING THEIR OBJECTIVES in this first-of-its-kind evaluation, Heit and colleagues initially note that cerebral aneurysms may result in significant morbidity and mortality, and, as such, identifying them on CTA studies is “critical” to guide patient treatment. They also state that AI platforms to assist with automated cerebral aneurysm detection are “of high interest”, which led them to assess the performance of the RAPID Aneurysm programme in the detection of these aneurysms.
In the study, RAPID Aneurysm was used to retrospectively detect the presence of cerebral aneurysms on CTA studies performed between January 2019 and December 2020.
The ‘gold standard’ here was aneurysm presence and location— as determined by the consensus of three expert neuroradiologists. Aneurysm detection accuracy; sensitivity and specificity; positive and
negative predictive values; and positive and negative likelihood ratios; were all determined by the programme.
Heit and colleagues report that 51 patients (mean age=56 years, 24 women [47.1%]) with a single CTA were included, and a total of 60 aneurysms were identified for the analysis.
RAPID Aneurysm had a sensitivity of 0.95 (95% confidence interval [CI], 0.863–0.983), a specificity of 1 (95% CI, 0.996–1), a positive predictive value of 1 (95% CI, 0.937–1) and a negative predictive value of 0.997 (95% CI, 0.991–0.999).
The authors further state that the programme demonstrated an accuracy of 0.997 (95% CI, 0.991–0.999) for cerebral aneurysm detection, with their findings suggesting that the adoption of aneurysm detection platforms like RAPID Aneurysm “may be a valuable tool to assist radiologists in their interpretation
“Several other studies have used automated, computer-assisted or AI techniques to detect the presence
neurologic deficits occurred in the transfemoral access group.
“Despite the proven benefit of transradial access over transfemoral access in neurointervention, the number of [DW-MRI] restriction foci were significantly more frequent during cerebral angiography when [the former] was selected,” the authors conclude. In their JNIS report, Carraro do Nascimento and colleagues also posit that further studies contrasting these two main access techniques “will be beneficial” for cerebral angiography.
“This study raises a degree of awareness to the fact that a transradial approach may carry a very small but definite risk of neurological complications,” said Carraro do Nascimento, discussing the wider implications of the study with NeuroNews. “By no means are we against the technique. In fact, at our institution, transradial access is used in a significant number of cases. Most of our elective cerebral angiograms and a significant number of elective cases are performed via radial access. The important factors of our study are that there is no perfect/riskfree approach in neurointervention; and a radial approach can be seen as an alternative, rather than ‘radial only’, for neurointerventions. We are in the process of expanding our data, with the aim to publish the results of a larger cohort.”
of cerebral aneurysms on CTA or MRA [magnetic resonance angiography] examinations,” Heit et al continue. “Few studies have used these techniques to detect cerebral aneurysms on CTA studies—and these studies reported sensitivities of 82–98% and specificity of 0–19% for cerebral aneurysm detection. The sensitivity (95%) and specificity (100%) of RAPID Aneurysm in our study compares favourably with these prior studies.
“A well-validated AI programme that detects cerebral aneurysms is expected to be an asset to radiologists. AI programmes that detect cerebral aneurysms on CTA have been shown to improve radiologists’ sensitivity for the detection of aneurysms. It will be of interest to conduct additional studies to see how RAPID Aneurysm affects radiologists’ performance in interpreting CTA studies in future [research].”
While their concluding message is that “RAPID Aneurysm is accurate in the detection of cerebral aneurysms”, however, Heit et al go on to highlight several limitations of their study, including its retrospective design and relatively small case numbers—which may introduce bias—as well as the fact it was comprised of a limited number of CT vendors, potentially limiting the generalisability of their findings, and the absence of <3mm aneurysms and ruptured cerebral aneurysms in
their dataset.
“Whether RAPID Aneurysm improves the performance of human radiologists was not assessed in this study and requires further investigation,” they add.
Speaking to NeuroNews, Heit said: “I believe we are on the cusp of seeing a sea change in our healthcare system through the adoption and implementation of AI.

“We have an ageing population that will severely strain the ability of our healthcare system to provide for them. We have fewer people going into medical school and [the US] Congress has not increased funding for residency training programmes to increase the number of physicians to care for this ageing population. I think it is very likely that these pressures will help to usher in the rapid adoption of AI in the healthcare system, which will be needed to meet these significant workforce challenges.
“More evidence that AI solutions lead to improvements in care and cost efficiency is needed to help make this transition, and there will need to be changes in reimbursement to hospital systems and physicians to implement these AI platforms.
“It will certainly be interesting to watch this space in the coming years, but I am hopeful that healthcare can do more with less by leveraging AI technology.”

18 December 2022 | Issue48 Research Updates: Imaging
It will be of interest to conduct additional studies to see how RAPID Aneurysm affects radiologists’ performance in interpreting computed tomography angiography studies in future [research].”
Vinicius Carraro do Nascimento
Jeremy Heit
Vessel-wall imaging could hold the key in “known yet understudied” phenomenon of spontaneous recanalisation
Following the publication of a case report in Topics in Magnetic Resonance Imaging, researchers from Malaysia have indicated that the use of vessel-wall imaging (VWI) “could potentially serve as an imaging method to presumptively diagnose spontaneous recanalisation in patients with acute ischaemic stroke”, although additional studies to investigate and validate this further are needed, they add.

s spontaneous recanalisation in acute ischaemic stroke is an understudied subject, there is not much in the present literature to refer to, to better understand this phenomenon,” first author of the study, Mohamad Syafeeq Faeez Md Noh (University of Putra Malaysia, Serdang, Malaysia), told NeuroNews

“If the utilisation of advanced VWI is possible [and it is done] when patients present with acute stroke, and they happen to have spontaneous recanalisation, it may be possible to look at the patient characteristics— underlying medical conditions that contribute to or oppose spontaneous recanalisation, and sites of occlusion [most often] associated with spontaneous recanalisation compared to sites that are not—and corroborate in a bigger sample size or study population as to the kinds of clots that are likely to recanalise spontaneously.
“Utilisation of VWI not only gives information regarding the lumen, but it also allows the interrogation of the vessel wall, to look at whether it is just inflammation of the wall or whether there is plaque that is causing the acute stroke clinically. This is a step forward compared to luminal imaging, which is limited by just visualising the lumen, and looking at whether it is patent or occluded.”
In their report, Noh and colleagues detail the case of a 66-year-old man who was referred to their centre from an outside hospital following an acute onset of syncope and suspected of having a possible middle cerebral artery (MCA) syndrome. However, despite no imaging or intravenous thrombolysis (IVT) treatment being performed at the outside hospital, the patient’s symptoms resolved within three hours after initial presentation, during transfer to their centre, with his National Institutes of Health Stroke Scale (NIHSS) score
decreasing from five—on examination at the emergency department—to zero.

In addition, subsequent imaging found vessel-wall enhancement at the suspected vessel involved, as well as evidence of acute infarcts at the supplied territory, but no atherosclerotic plaque or vessel occlusions. Stroke interventions via IVT or mechanical thrombectomy were therefore deemed unnecessary, and the patient was “eventually discharged well”.
Noh et al determined this to be a case of spontaneous recanalisation—a “rather understudied and poorly understood” phenomenon whereby the vascular occlusion causing an acute ischaemic stroke appears to ‘self-canalise’. More specifically, given the change in this patient’s NIHSS score, they postulate that “there was a high likelihood of a transient large vessel occlusion
involving the M1 segment of the left MCA vessel, with spontaneous recanalisation while being transferred to our centre”.
“This was evident by the noneccentric wall enhancement and thickening seen with no plaque present, and the acute infarcts on the DWI/ADC [diffusion-weighted imaging/apparent diffusion coefficient] sequence,” they continue. “We do acknowledge that this is a single case study, which would need to be corroborated by larger studies in the future. It is with exactly that in mind that we hope our limited experience opens up more areas of study and that VWI is routinely incorporated in the practice of stroke medicine in many more centres throughout the world.”
In conversation with NeuroNews, Noh noted that—within the specific context of spontaneous recanalisation— conventional, luminal imaging methods carry limitations. Computed tomography (CT) and magnetic resonance (MR) angiographies “may give a false impression of an occluded vessel”, despite blood flow beyond the plaque being reduced yet present if performed at a moment when the atherosclerotic plaque and adjacent vessel wall are inflamed, according to Noh. “And a cerebral angiography is, of course, much more invasive compared to CTA or MRA, and it is not without risks,” he added.
Noh further stated that clots with an embolic source (as opposed to a local thrombosis), MCA clots (as opposed to internal carotid artery [ICA] clots) and stage three hypertension have all previously been put forward as concatenate to an increased likelihood of spontaneous recanalisation occurring—but, due to a lack of large, well-designed studies on this phenomenon to date, these findings are all preliminary.
“For clinicians and researchers managing and studying acute stroke, these are important points to take into account when practising on a daily basis, as well as when considering going

into research, and designing studies or clinical trials,” he said. “Knowledge of the factors contributing to or opposing spontaneous recanalisation in acute ischaemic stroke definitely helps patients too, in terms of the treatment they [receive], and possibly saves them from unnecessary therapy; for instance, objective evidence of spontaneous recanalisation in a patient clinically presenting with acute stroke may [preclude] the administration of IVT, which is not without risks.”
In Topics in Magnetic Resonance Imaging, Noh et al conclude that “our experience could potentially aid in the understanding of spontaneous recanalisation in patients with acute ischaemic stroke—particularly in the postulation of the pathophysiology”. They also reiterate the potential held by the relatively new, adjunctive technique of VWI in cases where conventional imaging has found no clear sign of plaque or stenosis, stating that evidence of wall enhancement at the suspected vessel could be combined with clinical symptoms to determine the site of initial occlusion.
19 Issue48 | December 2022 Research Updates: Imaging
“A
Utilisation of vessel wall imaging not only gives information regarding the lumen, but it also allows the interrogation of the vessel wall, to look at whether it is just inflammation of the wall or whether there is plaque that is causing the acute stroke clinically.”
NIHSS score of 5 at the emergency department Spontaneous recanalisation during transfer NIHSS score of 0 at the radiology department
Mohamad Syafeeq Faeez Md Noh
Endarterectomy and TCAR ‘continue to show superior outcomes’ to transfemoral stenting
Researchers led by a vascular team in Indianapolis found that carotid endarterectomy (CEA) remains the mostused strategy in carotid revascularisation, with CEA and transcarotid artery revascularisation (TCAR) showing decreased odds of stroke or death compared to transfemoral carotid artery stenting (TF-CAS).
THOSE WERE AMONG THE MAIN FINDINGS delivered by Hanaa Dakour Aridi (Indiana University, Indianapolis, USA) during the 2022 annual meeting of the Midwestern Vascular Surgical Society (MVSS;15–17 September, Grand Rapids, USA) after an analysis of regional variation in patient selection, practice

New study
case for expanding coverage for carotid artery stenting
Research from Ochsner Health (New Orleans, USA) published in the Journal of the American College of Cardiology (JACC) is likely to influence expanded insurance coverage for carotid artery stenting.
THE PAPER, “CAROTID ARTERY stenting: JACC state-of-the art review”, details significant advances in the field of carotid stenting. It concludes that the technique “has achieved parity with carotid surgery for stroke prevention,” and that the data “support updating the national coverage decision for carotid stenting from the Centers for Medicare
increase in the percentage of CEA cases.”
Aridi reported that she and her team found no significant differences in stroke and death between CEA and TCAR across the three regional volume groups.
“However, TF-CAS was associated with higher odds of stroke and death compared to CEA, and TCAR was associated with a decreased odds of stroke or death compared to TF-CAS,” she added. “These variations were also seen when we analysed the regions individually.”
Despite significant variation in clinical practice, Aridi concluded that “no significant regional variation was observed in the outcomes of carotid revascularisation”.
“TCAR and CEA continue to show superior outcomes to TF-CAS across all regional groups,” she continued. “Our study identifies some gaps in adherence to societal guidelines, mainly in terms of intraoperative procedural variability that can potentially lead to worse outcomes. It also highlights the need for uniformity in management of patients with carotid artery disease.”
Raghu Motaganahalli (Indiana University School of Medicine, Indianapolis, USA), the study’s senior author, told NeuroNews: “What we are seeing is TCAR has grown at the cost of CEA, not at the cost of TF-CAS. We would love to see growth happening at the cost of TF-CAS because it is probably at a higher risk of stroke and complications.”
patterns and outcomes based on techniques used in carotid revascularisation logged in the Vascular Quality Initiative (VQI) from 2016–2021.
The research team divided 19 geographic regions into three quantiles based on the average annual volume of carotid procedures performed: low (956 cases), medium (1,533) and high (1,845) centres. They looked at a total of 126,768 carotid revascularisation cases, with most patients being asymptomatic. CEA was the most common procedure (>60%) across all regional groups, with 13% performed using TF-CAS and 17% with TCAR.
“Overall, there was a trend towards increased utilisation of TCAR since its introduction in 2016 up to 2021,” Aridi said, addressing the MVSS 2022 audience. “This seems to have been mirrored by an
and Medicaid Services [CMS] to equal coverage for carotid surgery”.
“Carotid artery stenting is a minimally invasive procedure compared to open surgery,” explains first author Christopher White (John Ochsner Heart and Vascular Institute, New Orleans, USA). “Overall, stenting and surgery are equivalent in patients who are good candidates for both, and the patient and their doctor should discuss which one is better for the individual patient.”
The paper analyses several large, multicentre randomised controlled trials encompassing data from over 25 years and more than 10,000 patients to demonstrate that carotid artery stenting can be just as effective as surgery when it comes to long-term stroke prevention and durability.
The paper suggests that the current CMS coverage decision regarding carotid stenting is outdated and places Medicare patients at a disadvantage by restricting their options for less invasive treatment, and recommends expanding coverage to be equivalent to open
surgery.
“The current literature supports equivalent results for carotid stenting and carotid surgery in patients who are suitable candidates for both procedures,” says White. “Some patients will not be good candidates for stenting and should receive surgery, while some patients will be poor candidates for surgery and should receive stents.”
Current coverage is likely to be expanded in the near future to include coverage for carotid stenting that is equal to carotid surgery for those who are symptomatic with a carotid stenosis
≥50% and ≤99%, and those who are asymptomatic patients with carotid stenosis ≥70% and ≤99%.
“We believe our multidisciplinary paper, written by neurologists, neurosurgeons, vascular surgeons, and cardiologists, will be an important summary of the most recent evidence that will support CMS in reimbursing both procedures on an equal basis,” says White.

20 December 2022 | Issue48 Carotid Disease CAROTID
makes
Our study identifies some gaps in adherence to societal guidelines, mainly in terms of intraoperative procedural variability that can potentially lead to worse outcomes.”
≥70% ≤99% AND ASYMPTOMATIC patients with carotid stenosis ≥50% ≤99% AND SYMPTOMATIC patients with carotid stenosis
Hanaa Dakour Aridi
Hanaa Dakour Aridi takes to the MVSS 2022 podium
EXPANDED CAROTID STENTING COVERAGE
Christopher White
patients
Five-year outcomes of a multicentre, randomised controlled trial (RCT) indicate that carotid endarterectomy (CEA) or carotid artery stenting (CAS) are not superior to best medical therapy (BMT) alone for moderate-to-severe asymptomatic carotid artery stenosis.
Tilman Reiff (University Hospital of Heidelberg, Heidelberg, Germany) and colleagues recently reported this key conclusion from the SPACE-2 trial in The Lancet Neurology. The authors claim that—to the best of their knowledge—this is the first randomised trial to directly compare CEA plus BMT, CAS plus BMT, and BMT alone over a five-year period in patients with asymptomatic carotid artery stenosis.
“The optimal treatment for patients with asymptomatic CAS is under debate,” the investigators write, noting that, since BMT has improved over time, the benefit of CEA or CAS is “unclear”. They add that randomised data comparing the effect of CEA and CAS versus BMT alone are lacking, and therefore aimed to directly compare CEA plus BMT with CAS plus BMT and both with BMT only in the SPACE-2 trial.
SPACE-2 was a multicentre RCT carried out at 36 study centres in Austria, Germany, and Switzerland, Reiff et al detail in their report. The researchers enrolled participants aged
50–85 years with asymptomatic carotid artery stenosis at the distal common carotid artery or the extracranial internal carotid artery of at least 70% according to European Carotid Surgery Trial criteria (equivalent to at least 50–99% according to North American Symptomatic Carotid Endarterectomy Trial [NASCET] criteria).
Reiff and colleagues note that SPACE-2 was initially designed as a three-arm trial including one group for BMT alone. However, the design was amended due to slow recruitment to become two substudies with two arms each comparing CEA plus BMT with BMT alone (SPACE-2a) and CAS plus BMT with BMT alone (SPACE-2b).
“Originally, we planned to recruit 3,640 patients; however, the study had to be stopped prematurely due to insufficient recruitment,” the authors write. They report that a total of 513 patients across SPACE-2, SPACE-2a, and SPACE-2b were recruited and surveyed between 9 July 2009 and 12 December 2019, of whom 203 (40%) were allocated to CEA plus BMT, 197
Smartphone video may offer noninvasive stroke screening option
Motion analysis of video recorded on a smartphone accurately detected narrowed carotid arteries, according to new research published in the Journal of the American Heart Association.
“BETWEEN 2% AND 5% OF STROKES EACH year occur in people with no symptoms, so better and earlier detection of stroke risk is needed,” said lead study author Hsien-Li Kao (National Taiwan University Hospital, Taipei, Taiwan).
“This was an exciting ‘eureka’ moment for us. Existing diagnostic methods—ultrasound, CT and MRI—require screening with specialised medical imaging equipment and personnel. Analysis of video recorded on a smartphone is non-invasive and easy to perform, so it may provide an opportunity to increase screening. Though more research and development are needed, the recordings and motion analysis may be able to be implemented remotely, or a downloadable app may even be feasible.”
(38%) to CAS plus BMT, and 113 (22%) to BMT alone. The median follow-up was 59.6 months.
In their paper, Reiff and colleagues report that the cumulative incidence of any stroke or death from any cause within 30 days or an ipsilateral stroke within five years—the primary efficacy endpoint of the study—was 2.5% (95% confidence interval [CI], 1–5.8) with CEA plus BMT, 4.4% (95% CI, 2.2–8.6) with CAS plus BMT, and 3.1% (95% CI, 1–9.4) with BMT alone.
The investigators also relay that, in both the CEA and CAS group, five strokes and no deaths occurred in the 30-day period after the procedure. During the five-year follow-up period, they note, three ipsilateral strokes occurred in both the CAS plus BMT and BMT alone groups, with none in the CEA plus BMT group.
Reiff et al conclude that CEA plus BMT or CAS plus BMT were not found to be superior to BMT alone regarding risk of stroke or death within 30 days or ipsilateral stroke during the fiveyear observation period. However, they stress that their results “should be interpreted with caution” due to the small sample size.
Indeed, they note that the small sample size of the trial was its “main limitation”. They outline the crux of the issue here: “With the low number of observed outcome events, only a few further events would be needed to change the results significantly.”
Despite this, they highlight that the present analysis “reveals important
This study, conducted between 2016 and 2019, used motion magnification and pixel analysis to detect the minute changes in pulse characteristics on the skin’s surface captured in a smartphone video recording.
A group of 202 Taiwanese adults (average age of 68 years; roughly 79% men) who received care at a single Taiwanese hospital participated in the study. Among the participants, 54% had significant carotid artery stenosis, meaning they had at least 50% blockage that was previously diagnosed by ultrasound, while 46% did not have significant stenosis. Recordings were captured with participants laying on their back, with their head tilted back in a custom-made box that minimised outside movement. An Apple iPhone 6, 64GB, was mounted to the box to capture a 30-second video recording of the person’s neck. The older generation phone was used as researchers believed it would be more common to the average user, Kao explained.
Researchers found that the video motion analysis algorithm had an 87% accuracy rate of detecting stenosis in the group known to have carotid artery stenosis. All study participants also had standard Doppler ultrasound testing to confirm narrowing in their arteries and to gauge and validate the estimates from the video motion analysis.
“More research is needed to determine whether video recorded on smartphones is a promising approach to help expedite and increase stroke
indications for possibly relevant existing associations, can be used for further pooled analyses, and provides data for future meta-analyses in a topic area in which currently only few randomised trials are available”.
In a commentary on Reiff and colleagues’ work, also published in The Lancet Neurology, Alison Halliday (University of Oxford, Oxford, UK) underscores the importance of randomised trials in this field of study. Halliday, who is the ACST principal investigator, remarks: “Despite its relatively small sample size, SPACE-2 provides important long-term followup data because of the randomised trial methodology. Large procedural registries usually cease follow-up within days or a few months, and patients on medical treatment alone cannot be meaningfully compared without randomisation.

“The future of interventions for carotid artery stenosis depends on randomised comparisons of different treatment approaches to ensure that bias is minimised and, at the same time, that enough patients are included. Alternatively, individual patient metaanalysis of similar trials can be used to support future interventions.
“SPACE-2 is of value to future individual patient meta-analyses
treatment options.”
screening,” Kao said. “Carotid artery stenosis is silent until a stroke happens. With this method, clinicians may be able to record a video of the patient’s neck with a smartphone, upload the videos for analysis and receive a report within five minutes. The early detection of carotid artery stenosis may improve patient outcomes.”
There were several limitations to the study including the small number of study participants, all of whom were considered at high risk for a cardiovascular event. In addition, neck length and neck angle were not analysed, which may affect the results of the video analysis. Skin colour is not likely to hinder applications to a broader population since a standard lighting method was used for this assessment, according to Kao.
21 Issue48 | December 2022 Carotid Disease
Randomised trial finds carotid endarterectomy or stenting not superior to best medical therapy in asymptomatic
With this method, clinicians may be able to record a video of the patient’s neck with a smartphone, upload the videos for analysis and receive a report within five minutes.”
Tilman Reiff
Collavidence: A global project looking to break down longstanding barriers in stroke research
As per its own mission statement, Collavidence wants to “make medical research collaboration and funding easier, more accessible and more transparent”, paying mind to gender and age disparities, economic barriers, and many other challenges currently facing stroke research. Mayank Goyal, Collavidence founder and president, and Rosalie McDonough, the project’s CEO (both University of Calgary, Calgary, Canada), spoke to NeuroNews to discuss Collavidence’s motivations and longterm goals, as well as detailing a recent shift in how they plan to go about realising these aspirations.
Having officially launched earlier this year, Collavidence now has more than 400 registered users from 44 different countries across the Americas, Europe, Asia, Africa and Australia—and these numbers are “growing steadily”, according to Goyal. In the space of just a few months, it has received 16 project submissions and managed to successfully help generate funding for five of them to date.
During the initial months since its launch, Collavidence has been financially supported by industry partners and foundations, but also wealthy individuals via social entrepreneurship or ‘impact investment’, recently closing its first pre-seed round of fundraising. Goyal notes that “our supporters are not only seeking a return on investment, but also a feeling that they are contributing to a social good; they believe in what we are doing”.
“I do think we are in the middle of a sea change with shifting demographics that has been further accelerated by the pandemic,” he adds. “More and more people are getting into focused philanthropy, and want to be involved and see where their money goes. This is obvious through the growth in crowdfunding over the past few years. We are hoping to capture this change [and target it] towards accelerating stroke research. And, because of the way our platform is set up, we are hoping it provides greater opportunities to younger researchers and leads to more gender equality.”
Goyal is quick to point out that Collavidence is a start-up—but an unconventional, ‘mission-driven’ one. In other words, it is “for-profit with a purpose”, as 100% of the money raised for projects on the platform goes to its researcher(s), with Collavidence itself currently not taking any commission. The initiative has primarily been launched off the back of ‘bootstrapping’ from its founding team and is now relying on a mix of philanthropic
donations and grants, and investment dollars, for growth. However, Goyal further notes that, given Collavidence’s value lies with its userbase, he and McDonough, along with chief scientific officer Johanna Ospel (University Hospital of Basel, Basel, Switzerland), chief knowledge officer Aravind Ganesh (University of Calgary) and the rest of the team, are now focusing all of their efforts on community building, recently introducing the concept of ‘working groups’ to that end.

The benefits of working groups
“These working groups are more of a collaborative module whereby you may not have a formalised idea of what you want to research,” says McDonough.
“It may just be something you have experienced in your practice, or you might be interested in a topic and find that there are [limited] data on it. As a clinician scientist, you could say ‘I had a patient last week with this rare [condition] and I was unsure how to treat them—I wonder if anybody else has run into this problem’. And then you create a working group around this and invite your colleagues and friends in the field to join, and the discussion happens in a very public way.
“From there, people who have had the same problem might see the discussion happening and request to join too, and you have this ‘snowball effect’—essentially like a Reddit [page] or a forum for medical research, which, interestingly enough, does not exist. We have all of these fragmented WhatsApp groups where physicians from around the world discuss challenging cases, or existing data, or new publications they have read, but that remains exclusive and anecdotal. We want to transfer that onto Collavidence.”
McDonough also states that, by creating a platform for this discussion, Collavidence is hoping to build more of an initial “buzz” around the given

topic so that, when those involved begin sharing a developed, formalised research proposal, potential donors will see that a large group of dedicated people, potentially hundreds, have already shown an interest. “If they can see all of those comments and the iterations a research idea has gone through, they would be more likely—we assume— to support the project financially,” she notes.
Bridging gaps in gender, experience and income
“There is a huge funding gap [in medical research],” McDonough continues. “The supply and demand issue is very prevalent, and things are actually getting worse.” She goes on to state that the rate of successful applicants is roughly 20%, if not lower based on the given year, adding that there are a number of different reasons for this, including the “huge problem” of budget cuts and a “hypercompetitive environment” whereby only ‘the best’ applicants—often those who have secured research funding in the past—are successful. “That is a problem,” McDonough says, “because it is disincentivising the young academic workforce.”

Age- and career stagerelated disparities are one of three key areas Collavidence is seeking to tackle in stroke research and, in addition to enabling younger, less experienced clinicians to find their feet, another major motivation for starting the project was to bridge funding gaps in areas outside of the western world. As many of these countries do not even have granting agencies, they are almost wholly dependent on philanthropic work that is usually apportioned on a very personal basis, according to McDonough.
The third and final overarching group Collavidence is hoping to aid is women. On this front, McDonough highlights conscious efforts to have an even split
of male and female members within its team, hopefully giving more of a voice to one of several “very disadvantaged” groups in stroke research.
“At the end of the day, when you are in a position of privilege, you can only do so much to imagine another person’s perspective,” Goyal adds.
“The best approach is to have people who represent [those perspectives].” To that end, Collavidence’s scientific review committee features physicians from across multiple continents, and Goyal says it will attempt to continue making the group as geographically and racially diverse as possible, while maintaining equitable gender representation.

What does the future hold?
Many of the aforementioned goals are reflected in those 400-plus users Collavidence has accrued since its launch: around 13% are from low- and middle-income countries, some 33% are women, and more than half are either early-career (42%) or junior (11%) staff.
“The founders are very fortunate to have a strong, global network within the stroke research world,” Goyal notes. “Initially, we are going to use this network to get people on the website, as well as giving them personalised coaching on how to make their project more visible and raise money. We are also encouraging established researchers and clinicians to create working groups related to tough cases or patient management dilemmas they face in day-to-day practice. Over the next two years, we hope to reach 10,000 people actively using the website—not only to increase collaboration and evidence-based medicine, but also to have greater degrees of engagement from all personnel across the stroke chain of [care], including nurses, caregivers and family members.”
While McDonough adds that Collavidence will “always be pushing the stroke field ahead”, owing to the fact it is “really underfunded” despite its burden of disease, the project also intends to “organically go wherever the need is”, with those in psychiatry, mental health and cardiac research having already voiced an interest too.
“Change is tough,” Goyal concludes, alluding to what may be the biggest barrier facing Collavidence further down the road. “People are used to working in a particular way, and any deviation from the norm [means] overcoming hesitation and inertia. What we are trying to do is a culture shift and that is not easy. However, based on our initial experience, feedback and rapid growth, I do think we have had an excellent start.”
22 December 2022 | Issue48 Collaboration and Evidence
What we are trying to do is a culture shift and that is not easy. However, based on our initial experience, feedback and rapid growth, I do think we have had an excellent start.”
Mayank Goyal
Johanna Ospel
Rosalie McDonough
Aravind Ganesh
Mayank Goyal
care unit discharge. Patients in both groups underwent two 30-minute stimulation sessions each day.
The primary outcome of the study was ventilator-free days during the first 28 days, defined as the number of days free from mechanical ventilation. Secondary outcomes, such as delirium, organ failure, length of hospital stay and adverse effects, were also investigated.
Reporting their results, Andrade and colleagues state that active HD-tDCS induced more ventilator-free days than sham HD-tDCS. “This outcome suggests a clinically meaningful benefit of HD-tDCS in patients with severe COVID-19,” they assert. In addition, patients in the active group experienced lower rates of organ dysfunction and a reduced length of hospital stay, as compared to the sham group. The positive clinical response rate was also found to be higher in the active group.
There was no significant difference between the two groups regarding prespecified secondary outcomes at five days, the authors note, and adverse events were similar between groups—leading them to conclude that HD-tDCS plus respiratory rehabilitation was “tolerable and safe” in the study. “HD-tDCS was selected based on its established tolerability, portability, and focal cortical modulation, and shown here to be deployable to intensive care units,” they add.
Andrade and colleagues go on to state that, with regard to rates of delirium, active HD-tDCS was superior to sham HD-tDCS at 11 days, but not on day 28. “These time points reflect different clinical concepts and the presence of a ‘ceiling effect’ may explain these findings,” they write. “Future trials should consider monitoring delirium patients whose critical illness has resolved.”
Discussing safety outcomes, the authors note that all but one of the seven deaths through day 28 in the trial occurred in patients aged 69 years or older, with none being attributed to HD-tDCS treatment, while no serious
adverse events were attributed to the study treatment, nor occurred in the active group.
“HD-tDCS plus respiratory rehabilitation was tolerable and safe, with both groups presenting similar adverse events,” Andrade and colleagues posit. “Mild and transient scalp erythema was the only adverse event associated with active HD-tDCS, which is consistent with the general population non-significant-risk profile of tDCS. HD-tDCS was selected based on its established tolerability, portability and focal cortical modulation—and shown here to be deployable to intensive care units.”
The authors also note several underlying mechanisms that may explain the observed clinical benefit with HDtDCS. These include the interplay between the altered respiratory drive during mechanical ventilation and the corticospinal control of respiratory muscles, as previous studies have shown supra-threshold brain stimulation activates cortical projections directly stimulating the diaphragm; the boosting of motor learning and motor rehabilitation efficacy when paired with tDCS; and the enhancement of cerebral blood flow by tDCS.
Prior to concluding, the authors highlight several strengths of their study, including its pragmatic protocol—which is representative of a real-world setting—allocation concealment and blinding, high follow-up rate at 28 days, and robustness of their adverse events data. However, they also acknowledge a number of limitations, such as the inhospital study setting potentially limiting generalisability of the results to COVID-19 patients in other settings; the possibility of these results being influenced by COVID-19 treatment approaches changing over the course of the study; and the fact it was conducted prior to both widespread vaccination and circulation of the Delta (B.1.617.2) and Omicron (B.1.1.529) variants of the virus.
“The results of this trial support the early use of HD-tDCS associated with respiratory support of severe COVID-19 patients,” Andrade and colleagues summarise, before reiterating that additional research into the efficacy of brain stimulation in a large sample of pulmonary disease patients is warranted.

Non-invasive SCS demonstrates “lifechanging” potential in spinal cord injury patients
Onward Medical has announced that the Up-LIFT pivotal study evaluating its non-invasive, electrical spinal cord stimulation (SCS) ARC-EX therapy achieved its primary effectiveness endpoint of improvement in upper-extremity strength and function in patients with movement disabilities.
“RESTORING HAND AND ARM function after spinal cord injury [SCI] is life-changing, freeing people with paralysis to feed and care for themselves, and be more independent in everyday activities,” said Chet Moritz (University of Washington, Seattle, USA), the study’s co-principal investigator.
“We are grateful to the many therapists, clinicians and people with SCI who participated in this landmark study,” added co-principal investigator Edelle Field-Fote (Emory University, Atlanta, USA). “There was very low attrition over thousands of clinic visits—a testament to the collective enthusiasm for this compelling therapy and for everyone’s determination to find new treatment options for people with SCI.”
The Up-LIFT study is a prospective, singlearm pivotal study designed to evaluate the safety and effectiveness of ARC-EX therapy in treating upper-extremity functional deficits in people with chronic tetraplegia. The study enrolled 65 people at 14 leading SCI centres across the USA, Europe and Canada. Time since injury averaged 5.9 years (range 1–34 years) with an average subject age of 46.5 years.
Up-LIFT participants completed an average of 50 training sessions over a period of roughly four months. A series of comprehensive assessments were performed at baseline, and monthly thereafter, to detect changes in sensory and motor function of upper extremities that directly translate into improved functional performance in activities of daily living.
Rigorous measures, such as CUE-T, GRASSP, ISNCSCI iii, and pinch and grasp force, were used to detect clinically meaningful changes resulting from the combination of ARC-EX therapy with standard-of-care rehabilitation.
According to Onward, detailed results will be made available after review by the US Food and Drug Administration (FDA). The company plans to submit for regulatory approval in both the USA and Europe in the coming months, and is hopeful it can begin treating SCI patients with its ARC-EX therapy during the second half of 2023.
“The Up-LIFT study results represent a turning point in the field of SCI and paralysis science,” said Marco Baptista, chief scientific officer of the Christopher and Dana Reeve Foundation. “Functional recovery, once deemed impossible, may now be in reach.”
23 Issue48 | December 2022
Brain stimulation improves COVID-19 outcomes in randomised trial Continued from page 1 HD-tDCS plus respiratory rehabilitation was tolerable and safe, with both groups presenting similar adverse events.” HD-RECOVERY trial Randomised 1:1 56 critically ill patients Active HD-tDCS plus respiratory rehabilitation (n=28) for up to 10 days OR until ICU discharge Sham HD-tDCS plus respiratory rehabilitation (n=28) for up to 10 days OR until ICU discharge
Suellen Marinho Andrade
Systematic review finds “strong evidence base” supporting deep brain stimulation for OCD
Deep brain stimulation (DBS) can halve the symptoms of severe obsessive-compulsive disorder (OCD), according to the findings of a pooled data analysis of available evidence, which has been published online in the Journal of Neurology, Neurosurgery and Psychiatry (JNNP). The analysis also found that two thirds of those affected experienced substantial improvements within two years, but highlighted multiple potential complications and limitations of DBS for this indication as well.
While drugs and cognitive behavioural therapy (CBT) can be very effective in treating OCD and its symptoms, these approaches are not successful in roughly one in 10 cases—and this led researchers to further investigate DBS, which has emerged as an alternative treatment for those with severe OCD symptoms.
Various prior studies have suggested that the technique can be effective in people with OCD, but they have not always quantified the impact of potentially influential factors, according to the researchers.
In a bid to account for this, and to update the existing body of evidence, they systematically reviewed and pooled the results of 34 clinical trials published between 2005 and 2021, with the aim of critically assessing how well DBS alleviates OCD and associated depressive symptoms in adults.
The 34 studies included 352 adults with an average age of 40, and severe-to-extreme OCD— the symptoms of which had not improved despite treatment. In 23 of the studies, participants were
required to have had persistent symptoms for five or more years before consideration for DBS surgery. Of the remaining 11 studies, one had a requirement of more than a decade of symptoms and two or more years of failed treatment; another required at least one year of failed treatment; and five did not specify any requirements.
On average, symptoms had persisted for 24 years across studies included in the systematic review and meta-analysis. Coexisting mental health issues were reported in 23 studies and included major depression
Proof-of-concept study indicates utility of evoked-interference DBS in Parkinson’s disease
Closed-loop evoked-interference deep brain stimulation (DBS) has been shown to be potentially utilisable in characterising the role of oscillatory dynamics in Parkinson’s disease and other brain conditions—indicating that this DBS modality could play a role in developing personalised neuromodulation systems.
THIS IS THE KEY MESSAGE
delivered by David Escobar (Cleveland Clinic, Cleveland, USA), and colleagues from the University of Minnesota in Minneapolis, USA, in a recent proof-ofconcept, in-human study published in Brain Stimulation
Escobar and colleagues offer some initial context to their study, stating that the neural circuit dynamics underlying the manifestation of specific motor signs in Parkinson’s disease are yet to be demonstrated. And, while current theories propose that the amplitude and incidence of 13–35Hz ‘beta’ band oscillations play a role here, approaches to control basal ganglia neural activity in real time are needed to clarify whether a causal relationship between these oscillations and motor signs exists.
As such, they tested evokedinterference DBS in a 55-year-old male patient diagnosed with idiopathic Parkinson’s disease roughly six years before being implanted with a directional DBS lead in the unilateral
globus pallidus internus (GPi). The researchers subsequently evaluated the suppression and amplification capabilities of this approach.
“We used a feedback (closed-loop) control strategy in which stimulation pulses were delivered in the GPi with precise amplitude and timing relative to the targeted GPi oscillations to evoke neural responses that suppress or amplify these oscillations,” they write.
“The rationale behind this approach [...] is that synaptic-related neural responses evoked by electrical pulses can modulate spontaneous, synaptic-related oscillations via synaptic integration when the pulses are delivered with precise amplitude and timing relative to the phase of spontaneous oscillatory activity.”
Five days after this procedure, the patient was admitted at the University of Minnesota Clinical Research Unit (Minneapolis, USA), where experiments took place over the course of two days to ascertain identification and
(over half of the total participants), anxiety disorder, and personality disorder. The average monitoring period after DBS implantation was two years.
The final pooled data analysis, which included 31 studies involving 345 participants, showed that DBS reduced symptoms by 47%, and two thirds of participants experienced substantial improvement within the monitoring period. In addition, secondary analysis revealed a reduction in reported depressive symptoms, with complete resolution in nearly half of all participants and partial response in a further 16%.
Some 24 of the studies reported complete data on serious side-effects, including hardware-related complications; infections; seizures; suicide attempts; stroke; and the development of new obsessions associated with stimulation. Overall, 78 participants experienced at least one serious side-effect.
These findings prompt the researchers to conclude that there is “a strong evidence base” in support of the use of DBS for the treatment of severe, persistent OCD and associated depression. However, they also caution that “while these results are encouraging, it is important to remember that DBS is not without its limitations”.
“First and foremost, it requires chronic implantation of hardware and carries the associated risk of complications,” Sameer Sheth (Baylor College of Medicine, Houston, USA) and colleagues note in JNNP. “Furthermore, although we report a less than 1% incidence of de novo obsessions involving the DBS patient programmer or the device itself, it remains a significant barrier to the effective implementation of DBS for OCD in certain patients.
“Successful application of DBS requires a close therapeutic alliance between patient, neurosurgical and expert psychiatrist teams in centres that specialise in implantation and programming of the device.”
characterisation of neural evoked responses. These experiments generated three key findings, according to Escobar and colleagues:
Evoked-interference DBS was capable of suppressing or amplifying frequency-specific GPi activity, in real time, in the targeted frequency band (16–22Hz)
Stimulation-evoked responses that mediated this modulation resonated in the beta band, within the same frequency range where the peak power of the spontaneous local field potentials (LFPs) was located
Because the evoked responses resided in the beta band, evokedinterference DBS required less stimulation amplitude to modulate beta oscillations than the stimulation needed to modulate neural activity in other frequency bands
“This study provides the rationale for future studies to assess the causal role (direct or indirect) of oscillatory dynamics in Parkinson’s disease using evoked-interference DBS, It also highlights the prospect of developing personalised neuromodulation systems based on interference between stimulation-evoked and spontaneous neural activity,” the authors note.
“[Our results] are also a step towards developing closed-loop DBS systems that control circuit-wide neurophysiological dynamics associated
with brain dysfunction in real time.”
Discussing limitations of their work, the researchers note that the current implementation of evoked-interference DBS employs a constant stimulation level to suppress the mean amplitude of the spontaneous oscillations— an approach that is suboptimal for suppression of neural activity because it does not account for dynamic changes in the amplitude of spontaneous neural oscillations. A second limitation created by the algorithm implemented in their study is suppression of oscillations in the targeted frequency band, resulting in amplification of neural activity in an adjacent band (12–16Hz). “This sideband amplification can be a confounding factor when analysing the effect of suppressing targeted neural activity via evoked-interference DBS on brain function,” they add.
Escobar and colleagues conclude by noting that, to overcome these limitations, future evoked-interference DBS algorithms will require instantaneous changes in stimulation amplitude to precisely suppress spontaneous oscillations in real time. In addition, future iterations of these systems will need to track the oscillations’ frequency and reduce filtering-related phase distortions to minimise side-band amplification during the suppression of neural activity.
David Escobar

24 December 2022 | Issue48
[…] While these results are encouraging, it is important to remember that DBS is not without its limitations.”
Intermittent stimulation of the DRG produces comparable chronic pain results to continuous stimulation
Intermittent dorsal root ganglion stimulation (DRG-S) has been shown to produce comparable results to continuous stimulation across a two-week period, as reported in Neuromodulation: Technology at the Neural Interface by investigators Kenneth Chapman (The Spine and Pain Institute of New York, New York City, USA) and colleagues.


OUTLINING THE RESULTS OF A SINGLEcentre randomised controlled feasibility trial, Chapman et al note that this intermittent delivery approach may extend battery life and facilitate smaller implantable pulse generators moving forward, adding: “The significant improvements in pain, function, and quality of life, utilising very low-frequency stimulation and intermittent dosing with DRG-S have the potential to set a new bar for the meaning of true low-energy neuromodulation.”
The authors initially aver that a spinal cord stimulation (SCS) method with paraesthesia-free waveform used in the dorsal columns, known as burst SCS, has previously demonstrated efficacy in chronic pain treatment through intermittent stimulation— whereby stimulation is cycled on and off for set durations of time. Conventional SCS uses a tonic waveform, they continue, and is a paraesthesia-based therapy that is ineffective at sub-perception levels, as well as when delivered in a cycled manner. On the other hand, DRG-S also uses a tonic waveform, and is
most commonly applied at sub-perception levels.
As such, they embarked on a study, following a prospective, randomised, balanced, double-blinded assessor protocol, with the aim of determining whether the cycling of DRG-S could maintain the approach’s therapeutic efficacy. Chapman et al detail that 20 DRG-S responders (mean age=61 years, nine men) were randomised to a sequence of three programmes for consecutive two-week intervals: continuous stimulation; one minute on/one minute off; or one minute on/two minutes off. The primary outcome of this study was a change in pain ratings with the cycled programmes as compared to continuous stimulation, while secondary outcomes included changes in function and quality-of-life scores, as well as stimulation programme preferences.
Between the three groups, mean scores were similar at the end of each two-week stimulation programme—as per the Numerical Rating Scale for pain (p=0.39), disability (p=0.72) and general health (p=0.95). No clinically significant differences were found from the upper boundaries of the 95% confidence intervals of the mean difference in pain, disability and general health/functional outcomes for either intermittent stimulation programme versus the continuous
programme. According to the researchers, it is also “noteworthy” that outcome measures at the end of each two-week stimulation programme were similar to pre-study DRG-S outcome measures across all three programmes.
And, Chapman et al add, at the end of the study, the continuous stimulation, 1:1 on-off dosing and 1:2 on-off dosing programmes were preferred by a similar number of patients, supporting the notion that there was little perceived difference between continuous and intermittent stimulation dosing.
In addition to demonstrating that delivering DRG-S in an intermittent cycled pattern maintains similar effects on pain relief, disability and functional improvement versus standard, continuous stimulation, the researchers note that this efficacy being sustained at a total charge per second of 0.3μC/s through intermittent dosing “further underscores the potential mechanistic differences between DRG-S and SCS, and highlights the role of DRG-S in the dorsal horn”. Chapman et al go on to state that the typical six-year lifespan of many current DRG-S implantable pulse generators can likely be “extended significantly”— potentially up to 10 years or more—with cycled stimulation.
However, the authors also acknowledge the small number of patients in their feasibility study, and other factors limiting its generalisability across chronic pain patient populations, positing that further research is necessary to address these issues—and to elucidate the maximal stimulationoff durations that can be applied while maintaining efficacy, as well as the long-term sustainability of intermittent stimulation dosing.
25 Issue48 | December 2022
Kenneth Chapman
Gamma sensory stimulation for six months reduces white matter atrophy in Alzheimer’s disease patients
A proprietary gamma sensory stimulation technology (Cognito Therapeutics), delivered at 40Hz over a six-month period, has been shown to reduce white matter atrophy in the brains of patients with Alzheimer’s disease—as per new data presented at the Alzheimer’s Association International Conference (AAIC; 31 July–4 August 2022, San Diego, USA).
ACCORDING TO A PRESS RELEASE FROM Cognito, data presented from the OVERTURE study and the Alzheimer’s Disease Neuroimaging Initiative (ADNI1) database suggest that the company’s 40Hz gamma sensory stimulation therapy may reduce white matter atrophy, protect axons, and possibly prevent myeline and oligodendrocyte damage in Alzheimer’s patients.

Given the “crucial role” of white matter connecting expansive brain regions, preventing or reducing its atrophy may diminish Alzheimer’s disease progression, the release adds.
The OVERTURE study treatment group participants received one hour of Cognito’s daily 40Hz simultaneous auditory-visual sensory stimulation at home for a six-month period, with placebo group participants receiving sham stimulation. Analysis between the groups suggested a difference in white matter atrophy favouring the treatment group. To compare the treatment group with a larger control group, the company studied ADNI1 data as well.
The OVERTURE study treatment group participants exhibited 0.38±0.82 percentage increases and ADNI1 study participants exhibited -2.45±0.40 percentage decreases in white matter volume after a six-month period (p<0.004).
Summary results of the OVERTURE clinical trial, also presented at AAIC 2022, demonstrated that gamma sensory stimulation is safe and well tolerated, and efficacy outcomes indicated a beneficial clinical effect, including maintained cognitive and functional abilities, reduced brain atrophy and improved sleep quality.
Why responsive neurostimulation is garnering “wide interest” from the epilepsy field
To date, thalamic responsive neurostimulation (RNS) has shown real potential in the treatment of patients with drug-resistant epilepsy. Mark Richardson (Massachusetts General Hospital, Boston, USA) outlines why it has proven to be such a promising therapy and what the future may hold for this modality—including large-scale trials, alternative brain disorders, and more.

Could you briefly outline thalamic RNS and how it differs from other brain stimulation techniques?
There are two types of implantable brain stimulators—those that do not record brain activity, like standard deep brain stimulation (DBS), and those that do, like the RNS system (NeuroPace). DBS of the thalamus is approved to treat focal epilepsy, and RNS is also approved for focal epilepsy, but RNS of the thalamus is relatively new because the field has recently come to understand that seizures can be detected in the thalamus and that responsive stimulation there can affect wide cortical networks. This is impactful for patients because RNS is tailored to their specific brain activity and their physicians can also use the recorded brain data to evaluate how well a medication is working; side-effects from medication are a huge problem for many people with epilepsy.
How long has this technique been used for epilepsy and to what extent?
RNS has been US Food and Drug Administration (FDA)-approved for focal epilepsy since 2014, and we continue to evolve that use, including as a long-term diagnostic tool and in combination with other minimally invasive surgical therapies like laser ablation. Epilepsy surgery, however,
including neuromodulation, is vastly underutilised. Only 5% of people with drug-resistant epilepsy who would benefit from surgery receive therapy. This represents a public health crisis. Epilepsy is the third most-common serious brain disease after stroke and Alzheimer’s—for what other disease would we accept such a treatment gap? Brain stimulation therapies can reduce seizures by 70%, on average, and contribute to other improvements in quality of life, and the medical field as a whole needs to act more urgently to reduce bias towards people with epilepsy and towards surgery.
Why is thalamic RNS particularly suited to this indication?
Thalamic RNS is particularly well suited to regional, multifocal and generalised epilepsies because of its ability to affect broad cortical regions via thalamocortical connections that are activated by thalamic stimulation. This strategy allows us to overcome limitations of focal surgeries that cannot adequately address seizures that originate from wide networks in the
brain. At the same time, the information recorded on the device provides objective information about the effects of stimulation on these seizure networks, allowing us to personalise the detection and stimulation settings to the individual person’s brain activity.
Have there been any recent breakthroughs that build on existing evidence for this therapy?
One recent breakthrough is the emerging use of thalamic RNS for idiopathic generalised epilepsy (IGE). This group of epilepsies are unique in that the thalamus seems to participate in the origination of seizures, which in other types of epilepsies originate exclusively in the cortex. For this reason, IGE may be uniquely well suited for a therapy that both detects and stimulates in the thalamus. We implanted the first thalamic RNS system in a young lady with IGE in 2017—it worked really well, and we have continued to use this therapy for people with IGE whose seizures do not respond adequately to medication. We recently published the first case series of these patients, other groups are publishing their experiences too, and the use of thalamic RNS for IGE appears to be taking off.
Do you think more research is required and, if so, what direction should these efforts take?
Based on wide interest from the epilepsy field, a nationwide clinical trial sponsored by the company who manufactures the RNS system, NeuroPace, was launched very recently to seek FDA approval for using thalamic RNS to treat IGE in adults and children as young as 12 years old. If the trial is successful, it will open this therapy to more than 300,000 people in the USA
who are suffering from drug-resistant primary generalised epilepsy.
More broadly, what would you say the future holds in this space?
A main advantage to RNS is the ability to use a person’s own brain data to inform therapy and to measure the therapy’s effects directly. Beyond this evolution of personalised medicine, there are huge potential upsides for patients to interact with their own data. Review of the brain recordings, which are accessed through a cloud-based platform, together with their epilepsy doctor is a wonderful way to strengthen the patient-physician relationship. In the future, applications of the technology will evolve to use brain recordings to give patients predictions about which times of the day, week, or month, their seizures are most likely to occur. Imagine how helpful this would be if you constantly spent your time worrying about when your next seizure was going to occur, and whether it would happen in a setting that could lead to anything from social embarrassment to death.
Could thalamic RNS hold major benefits in other conditions too?
RNS of the thalamus, and other areas in the brain that are central hubs in specific behavioural circuits, holds promise for treating many brain disorders— including addiction, depression, posttraumatic stress disorder and Parkinson’s disease. There is massive interest within the translational neuroscience community in studying brain function across these different diseases to understand the best way to employ this technology. It is important to recognise that funding from the US BRAIN Initiative has been fuelling a great deal of work in this field, and continuous support of the BRAIN Initiative by US Congress is critical for long-term success.
DISCLOSURES: Richardson indicated that he has received compensation from NeuroPace for consulting and educational presentations.
26 December 2022 | Issue48
Cognito headset
Mark Richardson
Spinal cord stimulation and other modalities will benefit from greater understanding of gender discrepancies
to relieve pain. Randomised controlled trials demonstrate in several neuropathic pain conditions that SCS is effective at reducing pain and improving healthrelated quality of life, pain-related disability, function and sleep whilst having a good safety profile.
Beatrice Bretherton
Comment & Analysis
Despite their clear significance in pain management, gender differences relating to the ways patients respond to neuromodulation therapies are relatively poorly understood and underpinned by a limited amount of definitive data. Beatrice Bretherton (Leeds, UK) discusses this existing evidence base and the importance of expanding it with future research across multiple fronts.
Based on current epidemiological research, pain is reported more frequently by women than men, and the prevalence of different pain conditions may differ between genders. For instance, neuropathic pain, defined by the International Association for the Study of Pain (IASP) as ‘pain caused by a lesion or disease of the somatosensory nervous system’, is thought to be more prevalent in women compared to men. Similarly, low back pain is higher in females than males, even when accounting for the increase in prevalence with advancing age. In contrast, migraine begins earlier in males than in females. It has a higher prevalence in boys than girls before puberty. Migraine then changes following puberty, whereby the incidence and prevalence increase more rapidly in girls than boys. As well as evidence of these differences between men and women in the prevalence of pain conditions, it is thought that the frequency of pain reporting, the severity of pain and the
degree of pain response to treatments that help with managing pain may also differ between genders.
In the UK, spinal cord stimulation (SCS) is a National Institute for Health Care and Excellence (NICE)-approved treatment for adults who have had chronic pain of neuropathic origin for more than six months with a visual analogue scale score >50mm despite conservative treatment. SCS is a neuromodulation therapy and comprises a surgically implanted battery (called an implantable pulse generator) which provides energy delivered by lead(s) placed in the epidural space to modulate the pain signalling in the spinal cord
Regarding differences between women and men in pain responses with SCS, there is currently only tentative evidence suggesting that gender may influence outcomes. For instance, in a 22-year experience review of SCS for treating several chronic benign pain conditions, more women (81.6%) experienced pain relief than men (76.6%) in the first year of treatment with SCS. However, males had higher success rates in the longer term than females with SCS. In a recently published study, women and men responded equally well to SCS despite ‘average pain’ being significantly lower in males than females before implantation of the therapy.
Intriguingly, there may be differences between men and women in some of the safety aspects of neuromodulation therapies. For instance, with SCS, we found that a more significant percentage of males (5%) than females (1%) had their treatment revised during surgery due to fracturing of the leads that deliver the electrical stimulation. Additionally, more females (13%) than males (6%) had their SCS therapy entirely removed (explanted) due to insufficient pain relief. With further analysis, we found that the female gender—as reported by other research groups—and older age were more likely to have the SCS therapy entirely removed compared to the male gender and younger age.
It is essential to carefully consider potential gender differences when identifying and recommending treatment
options, providing care and treatment, reviewing outcomes and optimising treatments. There is the potential for gender differences to contribute to care disparities between women and men, making neuromodulation treatments more complex. Therefore, awareness and education of possible gender differences are needed in multidisciplinary teams responsible for providing patient care.
Of course, this requires a systematic and reliable evidence base that healthcare guidelines and pathways can use to determine how best to consider gender differences when neuromodulation is a treatment option. Since the research investigating gender differences is discrepant and tentative, and raises ethical and clinical implications, there is a need for a body of research that explores gender differences in the following:
Prevalence of the chronic pain condition being investigated
Pre-treatment pain severity
Pain treatment responses
Safety outcomes
This should include an evaluation of the factors that may modulate gender differences, including psychological, biological and social aspects.
Furthermore, as there are many other forms of neuromodulation in addition to SCS (e.g. peripheral nerve stimulation and [transcutaneous] vagus nerve stimulation), gender differences with these therapies should be studied.
Finally, to develop a holistic account of how neuromodulation may be influenced by differences between women and men, gender differences in other outcomes, such as sleep, quality of life, function, and so on, should also be investigated.
References: References for this article are available online and can be found at neuronewsinternational.com/genderdiscrepancies-scs-other-neuromodulation-modalities.
Beatrice Bretherton is a research fellow at Leeds Teaching Hospitals NHS Trust, and a visiting research fellow in the Faculty of Biological Sciences’ School of Biomedical Sciences at the University of Leeds, in Leeds,

Intraoperative neuromonitoring may drive a new era in spinal cord stimulation therapies
“We are entering an era where true scientific evidence from IONM [intraoperative neuromonitoring] is guiding technology and our clinical practice.” This was one of the salient messages delivered by Steven Falowski (Argires Marotti Neurosurgical Associates of Lancaster, Lancaster, USA) at the International Neuromodulation Society’s (INS) interim meeting (11–13 November, Mumbai, India).
IN A PRESENTATION ON HIS PERCEPTION of the future of spinal cord stimulation (SCS), and the mechanisms of action involved in this treatment modality, Falowski noted that IONM represents a potential option in ‘asleep patients’ for both safety and confirmation of lead placement, with several studies having demonstrated potential superior results regarding efficacy, safety, adverse events and time savings versus more traditional approaches. In addition, current Neurostimulation Appropriateness Consensus Committee (NACC) guidelines advocate for the use of IONM in an asleep patient.
IONM has now been utilised as a method for recording human nerve activity during SCS therapy, he went on. The majority of work on mechanisms of action, as well as various waveform technologies, has revolved around computer and animal modelling, with IONM recordings having demonstrated a potential mechanism of action for SCS and the multiple industry waveforms on the market today.
Referencing a 2019 Neuromodulation: Technology at the Neural Interface paper, Falowski stated that the BurstDR platform (Abbott) has been associated with the most fundamental differences compared to
traditional tonic stimulation, with charge accumulation, hyperexcitability effects, and penetration to deeper nerve fibres at significantly lower amplitudes.
Subsequent follow-up investigations have also demonstrated that lower frequencies of BurstDR can have the same underlying effects with even more significant energy savings, while multisite BurstDR can activate more areas for broader yet more focal coverage—creating further energy savings—he added.
Other IONM research has looked at the measurements of evoked compound action potentials (ECAPs), as well as measurements of physiologically mapping the spinal cord, lead placement, and patient response to the therapy, which holds the potential to deliver more objective SCS treatments, according to the speaker.
In addition to the benefits that clinical practice with SCS may see moving forward, Falowski also pointed to increased objectivity with IONM could enable quick and easy research, helping to inform future clinical trials, concluding: “The use of IONM for SCS has had a significant scientific progression over the years.”
27 Issue48 | December 2022
UK.
There is the potential for gender differences to contribute to care disparities between women and men, making neuromodulation treatments more complex.”
Optically generated focused ultrasound shows promise for non-invasive brain stimulation
In a new paper published in Light: Science and Applications, a team of scientists and engineers led by Ji-Xin Cheng and Chen Yang (Boston University, Boston, USA) has developed an optically generated focused ultrasound (OFUS) method for non-invasive brain stimulation with ultrahigh precision.

AS A PRESS RELEASE ANNOUNCING THIS publication notes, a neuromodulation tool with ultrahigh precision is needed for mapping subregions of the brain by modulating a small population of the neurons—as less precise brain stimulation modalities usually activate multiple functional regions and cause unintended responses.
Electrical stimulation tools are a ‘gold standard’ for neuromodulation studies and disease treatments, but the current leakage over several millimetres limits how precisely targeting can be controlled. Optogenetics provides an “unrivalled sub-cellular spatial resolution and specificity in targeted cell types”, yet viral transfection has limited applications of these technologies in the human brain to date, the release continues, while transcranial focused ultrasound (tFUS) is stunted by a spatial resolution of 1–5mm despite offering a potentially viable non-invasive neuromodulation technique.
Thus, to date, non-invasive brain stimulation by



focused ultrasound with the optimal spatial resolution of 0.1mm has not been demonstrated; and noninvasive, non-genetic neuromodulation with ultrahigh precision remains a “critical unmet need”.

In their paper, the Boston University researchers outline the fact that OFUS is generated by a soft optoacoustic pad (SOAP) fabricated through embedding candle-soot nanoparticles in a curved polydimethylsiloxane film. Through the ‘optoacoustic effect’, candle-soot nanoparticles absorb the incident laser pulse and convert the energy to thermal expansion and compression—resulting in the generation of an ultrasound pulse.

A transcranial focus with ultrahigh precision of 83µm was achieved by SOAP, which is beyond the reach of the piezo-based low-frequency associated with tFUS. Such a breakthrough benefitted from the high acoustic frequency generated by the mixed layer of candle-soot nanoparticles and polydimethylsiloxane, and was pushed towards the limit through the geometric design with a high numerical aperture.
The team further detail how OFUS enabled direct and transcranial single-cycle stimulation to be performed reliably and safely, verified by calcium
imaging in cultured neurons in vitro. The unique single-cycle modulation of OFUS was found to evoke action potentials with much lower total ultrasound energy input than that of tFUS. The researchers also validated non-invasive transcranial neurostimulation with OFUS in mice by immunofluorescence imaging and electrophysiological recording.
Therefore, they assert that OFUS offers ultrahigh precision non-invasively towards neurological research in subregions of a brain. Notably, according to the release, it shows the “exciting potential” for disease treatment, such as modulating complex brain function and histotripsy. And, to evoke complex functions of the brain, OFUS devices can potentially be scaled up into a large ultrasound array for multisite neuromodulation.


While conventional lead zirconate titanate (PZT)based ultrasound arrays with large cables connected to each element are heavy to wear for patients, the lightweight OFUS device disclosed by the researchers provides the added benefit of improved accessibility and wearability for long-term treatments. In addition, OFUS devices with no metal components further offer improved compatibility with real-time magnetic resonance imaging (MRI) guidance and functional MRI monitoring, enabling real-time functional MRI evaluation of stimulation treatment and providing opportunities for closed-loop treatments in clinical applications..
The researchers summarise their paper by writing: “OFUS offers ultrahigh precision non-invasively towards neurological research in subregions of a brain. Its flexibility in fabrication, high spatiotemporal resolution, and improved electromagnetic compatibility, further enable clinical applications— such as ultrasound surgery, drug delivery and pain management. This work thus underlines the potential for OFUS to be utilised as a valuable technology in neuroscience research and clinical therapies.”
28 December 2022 | Issue48
*Available for US and EU readers only **Available worldwide A trusted provider of latest news, review of cutting-edge research, congress coverage and opinion from thought leaders A specialised news source in the spinal arena Editorially independent Subscribe today Available in print and digital formats and through our social channels Visit spinalnewsinternational.com and click ‘Subscriptions’ for complimentary print subscription* and e-newsletter subscription** This work […] underlines the potential for optically generated focused ultrasound to be utilised as a valuable technology in neuroscience research and clinical therapies.”
Neuro MODULATION NEWS
CVRx launches new version of neuromodulation device intended to treat heart failure CVRx—the developer of the “world’s first” US Food and Drug Administration (FDA)-approved neuromodulation device to treat the symptoms of heart failure— has launched its new Barostim NEO2 implantable pulse generator (IPG).
The second-generation device reduces the size of the IPG by 10% and extends battery life by 20%, reducing the frequency of device replacements for patients and their providers, a CVRx press release notes.
The Barostim NEO2 also offers a streamlined design with a single lead port (compared with two in the priorgeneration device) to further simplify the implant procedure. All Barostim programmer models are compatible with the new IPG model, the release adds.
“The new Barostim NEO2 offers the same clinically proven Barostim therapy, but with a more convenient design for my patients that is smaller and lasts longer,” said Michael Hoosien (Piedmont Atlanta, Atlanta, USA). “We are excited to use this next-generation system to further expand our Barostim programme.”

Theranica announces positive results from placebo-controlled migraine trial of Nerivio device Theranica Bio-electronics has announced positive top-line results in its double-blind, placebo-controlled, multicentre, randomised pivotal clinical trial in the USA. This trial evaluated the efficacy and safety of Nerivio—a wearable remote electrical neuromodulation (REN) device—for the preventive treatment of migraine in both episodic and chronic migraine patients.
The study met its primary endpoint, demonstrating a statistically significant reduction from baseline in monthly (chronic and episodic) migraine days in patients treated with Nerivio, as compared with a placebo device.
Nerivio further demonstrated statistically significant superiority over the placebo in other endpoints, including mean reduction of monthly headache days, and moderate/severe headache days; percentage of patients experiencing a reduction of headache days and moderate/severe headache days; and mean reduction of acute medication days.
Only one device-related adverse event was reported in the study, which occurred in the placebo group, and was categorised as mild and resolved without intervention, a Theranica press release states.
Brian Grosberg (Hartford Healthcare Headache Program, West Hartford, USA), primary investigator of the study, commented: “These data demonstrate Nerivio’s potential to provide a new, non-pharmacological, preventive treatment option for people with migraine. The high efficacy of Nerivio compared to placebo, with favourable safety and tolerability, suggests that REN could be a beneficial non-pharmacological therapy option for both preventive and acute treatment of migraine, subject to FDA [Food and Drug Administration] approval.”
Theranica has submitted this study to the US FDA for an expanded indication to include both preventative and acute migraine treatment, increasing the scope of patients who can be treated with Nerivio.
Abbott announces new CMS telehealth designation extending coverage of NeuroSphere virtual clinic
As part of its Medicare Telehealth Services List, the US Centers for Medicare and Medicaid Services (CMS) will continue to cover the use of Abbott’s NeuroSphere virtual clinic for programming deep brain stimulation (DBS) devices beyond the COVID-19 public health emergency.
Physicians who provide remote care and programming to patients with an Abbott DBS device can now continue to receive reimbursement from Medicare, according to an Abbott media alert.
Having been made official on 1 November 2022, this decision extends Medicare coverage under a telehealth category three designation—which, the alert adds, is reserved for emerging technologies, services and procedures made available during the COVID-19 pandemic.
By extending the availability of these telehealth services for Medicare reimbursement at least through the end of 2023, this designation is intended to create additional time for the collection of data that could support permanent inclusion on the Medicare Telehealth Services List.
NeuroSphere virtual clinic—a connected care neuromodulation technology that was introduced at the start of the COVID-19 pandemic— allows patients with Abbott DBS devices in the USA to communicate with physicians, ensure proper settings and functionality, and receive new treatment settings remotely as needed, the alert notes.
Nevro announces US FDA approval of HFX iQ system to personalise chronic pain treatment
Nevro Corporation has announced that it has received approval from the US Food and Drug Administration (FDA) for the Senza HFX iQ spinal cord stimulation (SCS) system.
The company has initiated a limited release of Senza HFX iQ in the USA, with a broad US market launch planned for early 2023. In addition to this US FDA approval for HFX iQ, Nevro has submitted the technology for approval in Europe too.
Nevro claims that Senza HFX iQ is the “first and only” artificial intelligence (AI)-based SCS system that learns from patients, and was developed to address the variability in pain from patient to patient, as well as helping patients optimise and maintain longterm pain relief and improved quality of life.
hospitalised patients, for patients who present to the emergency room, and with different schedules in clinics.”
The American Journal of Psychiatry published results from a double-blinded randomised controlled trial evaluating SAINT last year, showing that 79% of people in the active treatment arm entered remission from their depression compared to 13% in the sham treatment arm.
The SAINT neuromodulation system, which previously received Breakthrough Device designation from the FDA, is a novel innovation that uses structural and functional magnetic resonance imaging (MRI) to inform a proprietary algorithm that identifies the optimal anatomic target for focused neurostimulation in people with MDD. And, according to a Magnus press release, this new approach is delivered on an accelerated timeline and is precisely tailored to each person’s brain connectivity.
The system is comprised of the HFX iQ implantable pulse generator, HFX trial stimulator, charger and HFX app, and will launch with algorithms specifically for treating chronic back and leg pain, including non-surgical back pain and painful diabetic neuropathy.

In a press release, the company notes that Senza HFX iQ is digitally enabled and designed to optimise care by collecting patient data and guiding the patient through a customised treatment pathway—providing several key advantages over other SCS systems.
Magnus receives US FDA clearance for SAINT neuromodulation system in severe depression treatment
Magnus Medical has announced receipt of 510(k) clearance from the US Food and Drug Administration (FDA) for its SAINT neuromodulation system for the treatment of major depressive disorder (MDD) in adults who have failed to achieve satisfactory improvement from prior antidepressant medications in the current episode.
“This US FDA clearance of the SAINT neuromodulation system for depression is really exciting news,” said Mark George (Medical University of South Carolina, Charleston, USA). “This is more than just clearance of another device. This clearance expands the way we can use TMS [transcranial magnetic stimulation] to treat depression. The older approaches often took six weeks for depression to respond, while this approach observed remission from depression in just five days. That opens up many new possibilities to use SAINT in
Phagenesis has announced that the US Food and Drug Administration (FDA) has granted a de-novo request for the Phagenyx neurostimulation system, which uses pharyngeal electrical stimulation (PES) to restore swallowing control in patients with severe dysphagia post stroke. The company is now preparing a targeted launch in the USA.
“Dysphagia affects millions of people worldwide and many do not receive the desired outcome with currently available treatments,” said Marta Kazandjian (Stony Brook Southampton Hospital, New York, USA). “Adding an innovative therapy like Phagenyx has the potential to accelerate results and may allow the patient to spend fewer days in the hospital, which would significantly improve quality of care and patient experience.”
The Phagenyx system treats neurogenic dysphagia using PES, targeting the neurological components of swallowing coordination. This therapy has demonstrated best results when delivered at the earliest stages after injury to enhance neurorehabilitation and restore swallowing control, according to a Phagenesis press release.
“There is limited awareness of the significance of dysphagia in the critical care setting following prolonged mechanical ventilation or tracheostomy,” added Wade Smith (University of California San Francisco, San Francisco, USA). “Such patients cannot manage their own saliva, creating a high risk for aspiration and their safety. Phagenyx has the potential to treat patients early in the ICU [intensive care unit], which has been shown to accelerate recovery, reduce hospital length of stay and prevent downstream complications.”
The Phagenyx system is designated as a Breakthrough Device by the US FDA and is commercially available in Europe as well.
29 Issue48 | December 2022
Phagenesis announces US launch of neurostimulation system for post-stroke swallowing control
Barostim NEO2
HFX iQ system
iVascular launches new neurovascular portfolio with four CE-marked devices
Vascular device company iVascular has announced the expansion of its therapeutic areas with the launch of a new neurovascular pipeline, having gained CE-mark approval for four devices in this space: the iNdeep microcatheter, iNedit balloon distal access catheter, iNtercept retriever device, and iNstroke 4Fr and 6Fr aspiration catheter.
The company’s neurovascular portfolio has been designed to provide new tools that can help treat ischaemic stroke patients, as per a press release. It will become commercially available in Europe—and will be released in other regions that recognise the CE mark—in 2023.
The release also notes that this launch was timed with World Stroke Day (29 October 2022), as iVascular aims to raise awareness of high stroke rates, as well as the need and opportunity for improvements in prevention and case management.
With these new products, the company’s overall portfolio expands into a new area of treatment providing opportunities in patient care with devices for endovascular, cardiovascular, and now neurovascular, pathologies.
The company’s recent release also details that a comprehensive training programme and an investment in clinical data to optimise ischaemic stroke outcomes are already in place for this launch.
Medtronic study finds post-stroke protocols “vary significantly” between community hospitals and academic centres
Medtronic has announced the first results from its DiVERT clinical study, which showed that post-stroke workflow protocols and cardiac monitoring vary significantly across community hospitals and academic centres. These data were presented at the 2022 World Stroke Congress (WSC, 26–29 October, Singapore).
According to the company, this “first-of-its kind” multicentre study evaluated more than 7,600 cryptogenic, large-artery and small-vessel stroke patients across 12 US hospitals, and found more than 75% of cryptogenic
stroke patients at large academic centres received some form of cardiac monitoring versus 5% of cryptogenic stroke patients at community hospitals. It also found that community hospitals were half as likely to consult cardiology than academic centres (16% vs 34%).
“Our findings from phase one of DiVERT underscore the need for stronger, standardised care pathways in both academic and community centres to ensure that stroke patients receive guideline-directed therapy,” said David Rose (Tampa General Hospital, Tampa, USA). “We all need to do a better job detecting hidden atrial fibrillation in these patients because treatment will change—starting anticoagulation prevents recurrent stroke. Phase two of the study will address these workflow deficiencies in a standardised poststroke protocol for anyone to use at any stroke-capable hospital. While this protocol may not be the ultimate answer, it is a much-needed first step.”
Other findings from the study included community hospitals being more likely to diagnose cryptogenic stroke (93.2%) than large-artery (5.4%) or small-vessel (1.4%) stroke, while academic centres diagnosed stroke subtypes evenly (32.1%, 37%, and 29.9%, respectively); community hospitals being less likely to order short-term (1%) and/or long-term (4.3%) monitoring in their patients; and patient attrition being higher in academic centres than community hospitals (54.2% vs 45.2%), while the six-month recurrent stroke rate was similar in both groups.
Vesalio announces EU MDR certification of neurovascular product lines
Vesalio has announced EU Medical Device Regulation (MDR) certification of its product lines—achieving this “significantly ahead” of its May 2023 deadline, according to a company press release.
This milestone is the third in a series of recent regulatory approvals of Vesalio’s neurovascular products, following the CE marking of its Neva Net—a neuro-thrombectomy device containing a unique integrated distal filter technology—and the US Food and Drug Administration (FDA) humanitarian device exemption (HDE) approval of Neva VS, which is indicated for the adjunctive treatment of aneurysmal subarachnoid haemorrhage-induced cerebral vasospasm.
In the release, the company asserts that the past few years have seen regulations for medical device manufacturers become progressively complex and demanding. In Europe, the transition from the old Medical Device Directive (MDD) to the
MDR has brought increased quality and regulatory demands, including additional clinical evidence of safety and efficacy, Vesalio claims.
Contego
completes enrolment of
PERFORMANCE II carotid stent trial
Contego Medical has announced that enrolment of the PERFORMANCE II clinical trial has been completed.
PERFORMANCE II is intended to evaluate the safety and effectiveness of the Neuroguard integrated embolic protection (IEP) three-in-one carotid stent and post-dilation balloon system with IEP. The Neuroguard IEP system is designed to treat clinically significant carotid artery stenosis while improving procedural safety through the integration of the stent, balloon and an embolic filter, all in a single device.
“The Neuroguard IEP system combines a truly innovative stent design with a multi-function delivery platform for advanced protection from stroke, while reducing the number of catheter exchanges needed to complete the procedure,” said Christopher Metzger (Holston Valley Medical Center, Kingsport, USA), lead enroller in the trial. “Additionally, it has outstanding conformability for a closed-cell stent, allowing the advantages of this stent system in a wide variety of carotid anatomies.”

PERFORMANCE II is a prospective, multicentre, single-arm, open-label study for the treatment of carotid artery stenosis in subjects at high risk for carotid endarterectomy (CEA). The trial enrolled 305 patients at 32 sites in the USA and Europe. Results of the study will be used to support a US Food and Drug Administration (FDA) premarket approval application.
“The Neuroguard IEP technology may offer significant benefits to patients suffering from severe carotid stenosis, specifically with the potential to lower the embolic burden and overall stroke rates,” said William Gray (Main Line Health, Wynnewood, USA), who is a principal investigator for PERFORMANCE II alongside Ralf Langhoff (Sankt Gertrauden Hospital, Berlin, Germany).
surface modification to the stent results in enhanced safety by significantly reducing thrombogenic complications, a Wallaby/Phenox press release states.
“The benefits offered by surface modification are exceptional and similar to those in flow diverter devices such as the p64 MW HPC [Wallaby/Phenox],” said Markus Holtmannspötter (Klinikum Nuremberg, Nuremberg, Germany).
“HPC enables us to use single antiplatelet therapy in selected cases per IFU [instructions for use] and in turn reduces haemorrhagic complications.”
According to Wallaby/Phenox, the Pegasus HPC stent is the first stent of its kind to introduce coating technology for the treatment of ICAD and aneurysms. Thus, the device addresses multiple indications while providing all the benefits of classic laser-cut, opencell stents and adding increased patient safety.

Corindus presents safety and effectiveness results with CorPath GRX robot
Corindus, a Siemens Healthineers company, has announced the presentation of results from a “first-ofits-kind” study demonstrating the safety and effectiveness of robotic-assisted neurovascular aneurysm embolisation using the CorPath GRX system.
The results from this prospective, single-arm, international, multicentre, non-inferiority study, which included 117 patients from 10 clinical sites across six countries, were delivered by principal investigator Michel Piotin (Rothschild Foundation Hospital, Paris, France) at the 2022 European Society of Minimally Invasive Neurological Therapy (ESMINT) congress (7–9 September, Nice, France).
Wallaby/Phenox has officially announced the successful global launch of its novel Pegasus hydrophilic polymer coating (HPC) stent, having first unveiled the device at the 2022 European Society of Minimally Invasive Neurological Therapy (ESMINT) congress (7–9 September, Nice, France).
The introduction of the Pegasus stent enables more patients to benefit from the company’s HPC surface modification in stent-assisted coiling treatments, as well as intracranial atherosclerotic disease (ICAD) and dissections. The application of this
“Neurovascular intervention demands extreme precision to achieve optimal clinical outcomes,” said Piotin. “The results of the study show the CorPath GRX system helps physicians move efficiently within tortuous and unstable vessels. I am honoured to have participated in a groundbreaking study that may lead to an entirely new treatment paradigm in neurovascular care.”
The CorPath GRX system demonstrated a 94% technical success rate and achieved the primary effectiveness goal—which was defined as successful completion of the roboticassisted endovascular procedure absent of any unplanned conversion to a manual procedure.
The system also demonstrated a 95.7% rate of clinical success, and achieved its primary safety goal,
30 December 2022 | Issue48 Market Watch
Industry News
Wallaby/Phenox officially announces global launch of Pegasus HPC stent system
Pegasus stent
iVascular portfolio
Industry News
defined as patients treated without intra- and periprocedural adverse events. Some 64.5% of patients achieved ‘complete obliteration’ of their aneurysm. In addition, 78.2% showed no clinical symptoms postprocedure—achieving a modified Rankin Scale (mRS) score of zero— while the remaining 21.8% had an mRS of 1–2.
Penumbra announces European launch of RED reperfusion catheters for stroke care
Penumbra has announced that its RED reperfusion catheters have secured a CE mark and are now commercially available in Europe. The catheters are part of the company’s Penumbra system, which is a fully integrated mechanical aspiration thrombectomy system designed to restore blood flow in acute ischaemic stroke patients.
“When addressing stroke, our goal is to remove the blood clot as quickly as possible for patients to have the best outcome,” said Saleh Lamin (Queen Elizabeth Hospital, Birmingham,
UK). “With RED catheters, we will be able to get up to the clot quickly and efficiently remove it, most of the time within a single pass. Restoring blood flow promptly is key as it is associated with less damage to the brain and better outcomes.”
The RED family of catheters is engineered with the company’s REDglide technology, which is intended to enhance the trackability of the catheters as they navigate the challenging vessel anatomy of the brain while also maximising aspiration efficiency to remove blood clots— ultimately addressing a wide range of large vessel occlusions via mechanical aspiration thrombectomy.
Earlier this year, Penumbra also announced initial INSIGHT registry data showing that its RED reperfusion catheters were successful in removing all clot types—and, additionally, results of sub-analyses from the company’s COMPLETE study, indicating the Penumbra system’s effectiveness in acute ischaemic stroke patients with tandem lesions, as well as patients who are considered in the late window of treatment.
Calendar of events

5–8 December 2022
Barts Research and Advanced Interventional Neuroradiology (BRAIN) Conference London, UK brainconference.co.uk
6–7 December 2022
LINNC Seminar - Asia Edition Singapore linnc.com/Course-information/ LINNC-Seminar-2022-Asia-Edition
12–16 December 2022
The European Course in Minimally Invasive Neurological Therapy (ECMINT) 4.4 Oxford, UK esmint.eu/ecmint
12–15 January 2023
North American Neuromodulation Society (NANS) Annual Meeting Las Vegas, USA conference.neuromodulation.org
Visionable platform

These findings were presented at the 2022 World Federation of Interventional and Therapeutic Neuroradiology (WFITN) congress (21–25 August, Kyoto, Japan).
Brainomix and Visionable partner to optimise UK stroke care pathway
Brainomix is set to strategically partner with Visionable, a real-time clinical collaboration platform designed to enable virtual healthcare models, in an attempt to transform the delivery of stroke care.
The two tech-enabled health companies will collaborate and comarket two complementary solutions—Visionable’s collaboration platform and Brainomix’s e-Stroke artificial intelligence (AI) software— to enhance the full pathway of stroke care delivery, from pre-acute to intrahospital stages.
Visionable’s patented, next-generation digital healthcare collaboration platform can be used across this care pathway, a press release from the company states—from emergency response, connecting frontline responders and on-scene members of the public to remote specialist clinicians; through to hospital treatment, including virtual consultations, multidisciplinary team meetings and at-home care.

This platform is set to be combined with Brainomix’s e-Stroke software, which constitutes a collection of tools that use state-of-the-art AI algorithms to support doctors by providing realtime interpretation of brain scans, helping guide treatment and transfer decisions for stroke patients, and allowing more patients to be treated in the right place at the right time.
The two complementary technologies are saving time, reducing workload, and supporting improved outcomes, all of which aligns with the UK national strategy to drive integration and efficiency for better care, the Visionable release states.
The benefit of combining e-Stroke with Visionable’s platform has been pioneered by the stroke team at Ipswich Hospital (Ipswich, UK), with patients and staff already reaping positive results through faster delivery of care, superior performance metrics and improved patient outcomes.
8–10 February 2023
International Stroke Conference (ISC) Dallas, USA professional.heart.org/en/meetings/ international-stroke-conference
18–22 February 2023
International Brain Stimulation Conference Lisbon, Portugal elsevier.com/events/conferences/ international-brain-stimulationconference
23–25 March 2023
World Congress on Controversies in Neurology (CONy) Dubrovnik, Croatia cony.comtecmed.com
11–14 April 2023
World Live Neurovascular Conference (WLNC) Rio de Janeiro, Brazil wlnc.org/en/WLNC-2023.html
25–27 April 2023
Charing Cross (CX) Symposium London, UK cxsymposium.com
29 April–3 May 2023
American Society of Neuroradiology (ASNR) Annual Meeting Chicago, USA asnr.org/annualmeeting
NeuroNews is a trusted, independent source of news and opinion in the neurointerventional and neurosurgical world.




31 Issue48 | December 2022 Market Watch
up for a free print subscription* and e-newsletter subscription**
Sign
www.neuronewsinternational.com
*Available for US and EU readers only ** Available worldwide