Featured
24/7 stroke thrombectomy service

Featured
24/7 stroke thrombectomy service
This year’s International Stroke Conference (ISC; 8–10 February, Dallas, USA) saw neuroprotection take another step forward in its ‘renaissance’ as a viable ischaemic stroke treatment option. Phase 2 clinical trials and animal research alike delivered promising findings on novel neuroprotective drug candidates, prompting guarded optimism at a time when data from multiple Phase 3 studies are also expected in the near future.
“What is exciting for me is that we are starting to get a sense that, maybe—and we should be cautious, because we do not have Phase 3 trials yet—but maybe we are on the cusp of some significant breakthroughs in making our patients better,” said Tudor Jovin (Cooper University Health Care, Camden, USA), programme chair for ISC 2023, in a discussion on American Stroke Association (ASA) TV. “[That is] in terms of augmenting the effect of reperfusion, and possibly beyond as well, in patients who receive neuroprotectant therapy without reperfusion.”
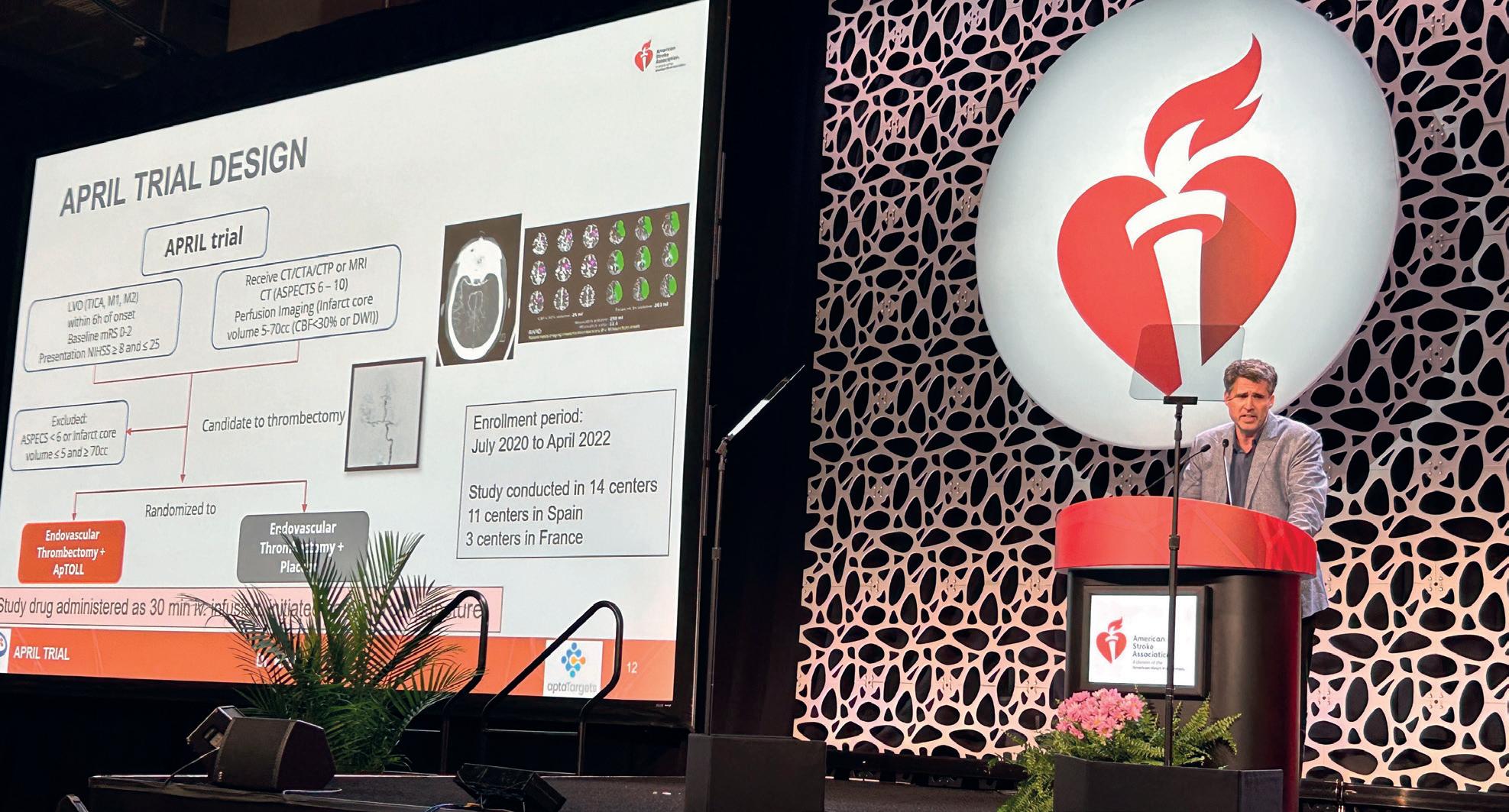
One late-breaking study featured at ISC was the Phase 1b/2a APRIL trial, which assessed the neuroprotective drug ApTOLL—a TOLL-like receptor 4 (TLR4) antagonist developed by Spanish biopharmaceutical firm AptaTargets—

and was delivered by Marc Ribó (Hospital Vall d’Hebron, Barcelona, Spain; pictured above).
This randomised, placebo-controlled, double-blind trial assessed ApTOLL’s safety and efficacy in more than 150 adult acute ischaemic stroke patients treated at 15 hospitals across France and Spain who presented within six hours of symptom onset. When administered alongside mechanical thrombectomy and, if needed, intravenous thrombolysis (IVT) with alteplase, at a dosage of 0.2mg/kg, the drug was associated with a 90-day post-treatment mortality rate (4%) that was more than four times lower than the one observed in a placebo group (18%).
In addition, imaging tests performed 72 hours after treatment showed a 40% reduction in final infarct volumes among patients who received 0.2mg/kg of ApTOLL, while improved 72-hour National Institutes of Health Stroke Scale (NIHSS) scores and 90-day modified Rankin scale (mRS) scores of 0–2 versus placebo were also observed.
“The results are promising because, for the first time, a medicine studied as a neuroprotectant demonstrated not only a biological benefit, by reducing the volume of damaged brain tissue, but also a reduction in long-term disability and risk of death,” said Ribó, the study’s senior author and principal

Continued on page 2
A NEWLY PUBLISHED METAanalysis of individual patient data has found that older patients with symptomatic carotid disease are likely to benefit as much from timely intervention as younger patients. Speaking to NeuroNews in light of this finding, senior author Dominic Howard (Oxford University Hospitals NHS Trust, Oxford, UK) stressed that “vascular surgeons must not turn down symptomatic patients just because of their age”.

Writing in Stroke, Howard et al note previous “uncertainty” around whether elderly patients with symptomatic carotid stenosis have higher rates of adverse events following carotid endarterectomy (CEA). As such, they performed a systematic review and meta-analysis of all studies published between 1 January 1980 and 1 March 2022 reporting post-CEA risk of stroke, myocardial infarction, and death, in symptomatic carotid stenosis patients— particularly in octogenarians.
The investigators included a total of 47 studies—representing 107,587 patients. Within this cohort, the risk of perioperative stroke was 2.04% in octogenarians and 1.85% in nonoctogenarians. In terms of perioperative death, they also report a figure of 1.09% in octogenarians and 0.53% in non-octogenarians.
Howard et al summarise that they found a “modest” increase in perioperative risk with age in symptomatic patients undergoing CEA—but emphasise that stroke risk also increases with age on medical therapy alone and thus say their findings “support selective urgent intervention in symptomatic elderly patients”.
turn to page 20.
Continued from page 1
investigator. “ApTOLL did not show any interactions with the drugs that are administered for ischaemic stroke, meaning that it could be [given] to most patients.”
“Here we have a positive trial—it is a Phase 2, so we have to be careful and cautious—but, still, some very promising results that mirror the basic science and the animal experiments that were done [previously],” Jovin noted. “And, all the results are consistent in that, not only are the clinical results better, but they are also paralleled by lower infarct volumes. It fits very well, it is exciting—of course, we need a Phase 3 to confirm it—but it is so refreshing to see positive signals, even if they may not be definitive.”
The same late-breaking session at ISC saw Lauren Sansing (Yale School of Medicine, New Haven, USA) present findings from an animal-model study that assessed six promising neuroprotective agents. One of these candidates—an intravenous infusion of uric acid (16mg/kg) proposed for testing by a University of Iowa (Iowa City, USA) team—exceeded the study’s prespecified efficacy boundary, and now warrants further investigation to ascertain its utility in stroke care.
Sansing disclosed primary results from the Stroke Preclinical Assessment Network (SPAN), which was devised to address the lack of experimental rigour that currently impedes the translation of promising neuroprotective agents from animal models into clinical trials. SPAN adopted a clinical trial-esque design in which 2,518 rats and mice were randomised to receive a neuroprotective candidate, or placebo, with the animals’ sensory and motor functions being ascertained via a corner test at day 28 post-treatment. Sansing concluded with a nod to SPAN 2.0 whereby up to eight new interventions will be investigated under a similar study protocol.
“This was a remarkable effort, with positive results, and a fruitful exercise [because] we have some directions for where to go in the future—not only identifying a compound that is worthy of testing in humans, in conjunction with reperfusion, but also a roadmap for analysing more neuroprotectant approaches,” Jovin stated.
Another novel neuroprotectant showcased at ISC was butylphthalide, a medication initially compounded from celery seed. Preliminary results from a study involving 1,216 Chinese patients were presented at the conference, indicating that ischaemic stroke patients treated with IVT and/or thrombectomy, in addition to the drug, experienced milder neurological symptoms—as per mRS and NIHSS score measures—as well as improved functionality at three months post-stroke, versus those who received IVT/
thrombectomy plus placebo.
Butylphthalide is licensed for use in ischaemic stroke in China, but has not been approved by the US Food and Drug Administration (FDA). Exactly how the drug works is currently not fully understood and, as such, study co-author Baixue Jia (Capital Medical University, Beijing, China) believes the next step should be to investigate its exact mechanism of action in humans—in addition to confirming the present results via further trials.
“While these are interesting results, this is only one relatively small study on a fairly select population in China,” commented ASA volunteer expert Daniel Lackland (Medical University of South Carolina, Charleston, USA), who was not involved in the study. “Butylphthalide […] is not ready for use in standard stroke treatment; however, these results warrant further study consideration.”
Beyond the data conveyed at ISC, a number of other research endeavours assessing neuroprotective drugs are also currently underway. NoNO, for example, announced in late 2022 that the first patient had been dosed with the company’s novel neuroprotectant NoNO-42 in a Phase 1 clinical trial evaluating its usage in healthy volunteers.

Like NoNO’s first-generation postsynaptic density (PSD)-95 inhibitor, nerinetide, NoNO-42 is intended to offer neuroprotection in ischaemic stroke. Results from ESCAPE-NA1—in which nerinetide administered without thrombolytics exhibited improved functional independence, reduced stroke mortality and less brain damage on imaging—are now undergoing confirmatory testing in the Phase 3 ESCAPE-NEXT study, which completed enrolment in February 2023.
“The stroke neurology community is extremely excited about the prospects of both nerinetide and NoNO-42, and the academic community is eager to follow up ESCAPENEXT with clinical trials to investigate the efficacy of NoNO-42 in stroke patients,” said principal investigator Michael Hill (University of Calgary, Calgary, Canada).


In March this year, Athersys announced that—following a meeting with the US FDA—it plans to alter the primary endpoint of its Phase 3 MASTERS-2 trial to mRS at day 365, from day 90 previously, to “best reflect the full potential benefit” of the company’s neuroprotective MultiStem treatment in acute ischaemic stroke patients. This decision was made based on the MASTERS-1 trial, and results indicating one-year functional improvements and safety outcomes from the TREASURE study in Japan.

The latest stories from the neuro world
n MORE HIGHLIGHTS
FROM ISC 2023:
The 2023 International Stroke Conference (ISC; 8–10 February, Dallas, USA) saw late-breaking data presented on tenecteplase versus alteplase in early-window acute ischaemic stroke; extracranial to intracranial bypass surgery for symptomatic internal or middle carotid artery (ICA/MCA) occlusions; and the benefits of treating large infarctcore volume stroke with mechanical thrombectomy.

For more on this go to page 4.
n “ENORMOUS DISPARITY” FOUND IN THROMBECTOMY ACCESS:

The Society of Vascular and Interventional Neurology (SVIN) has released its first global analysis of access to mechanical thrombectomy for the treatment of large vessel occlusion (LVO) stroke. Findings from MT-GLASS—a study conducted as part of the SVIN Mission Thrombectomy 2020-plus (MT2020+) initiative, which has been published in the journal Circulation—indicated “dismally low” worldwide access to thrombectomy treatments as well as an “enormous disparity” between countries.
For more on this story go to page 7.
n SQUID SAFE AND EFFECTIVE FOR HIGHGRADE DAVF:
The Squid liquid embolic agent (Balt) has been deemed safe and effective in treating high-grade dural arteriovenous fistulas (DAVFs), and serves to expand the armamentarium for neurointerventionists treating DAVFs and other intracranial vascular malformations—as per a recent publication from Markus Möhlenbruch (Heidelberg, Germany) and colleagues in the Journal of NeuroInterventional Surgery
For more on this story go to page 14.
Editor-in-chief: Prof Philip M Meyers | Publisher: Roger Greenhalgh | Content director: Urmila Kerslake
Editor: Jamie Bell jamie@bibamedical.com | Editorial contribution: Jocelyn Hudson
Design: Terry Hawes, Wes Mitchell and David Reekie
Advertising: Michael Broughton michael@bibamedical.com
Subscriptions: subscriptions@bibamedical.com
[…] It is so refreshing to see positive signals, even if they may not be definitive.”
ISC 2023: Latest neuroprotection data provoke cautious excitement inTudor Jovin (top) and Lauren Sansing Shuya Li 2.79% median global thrombectomy access rate
You plan each step with intention. You accept the challenge fearlessly.

Your expertise + our clinically proven2,3 tools will power your journey.
The Solitaire™ device is the most-published stent retriever with over 200 publications demonstrating clinically proven, tried-and-true performance.2,3
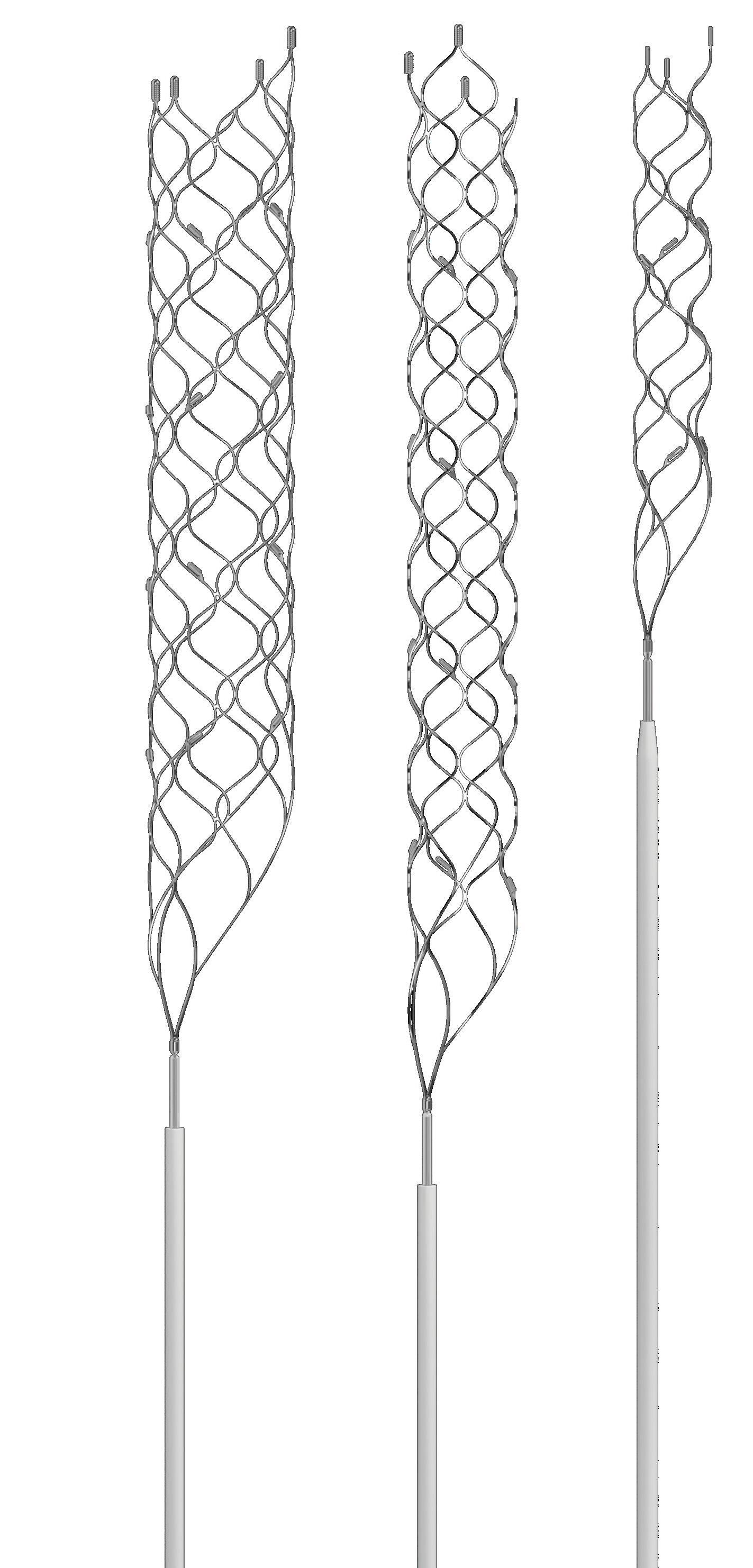
Together, we make one powerful package.
2016;387(10029):1723-1731.
CAUTION: Federal (USA) law restricts these devices to sale distribution and use by or on order of a physician. Indications, contraindications, warnings and instructions for use can be viewed at www.medtronic.com/manuals.
1. The Solitaire X Revascularization Device is indicated for use to restore blood flow in the neuro-vasculature by removing thrombus for the treatment of acute ischemic stroke to reduce disability in patients with a persistent, proximal anterior circulation, large vessel occlusion, and smaller core infarcts who have first received intravenous tissue plasminogen activator (IV t-PA). Endovascular therapy with the device should be started within 6 hours of symptom onset.
2. The Solitaire™ X Revascularization Device is indicated to restore blood flow by removing thrombus from a large intracranial vessel in patients experiencing ischemic stroke within 8 hours of symptom onset. Patients who are ineligible for IV t-PA or who fail IV t-PA therapy are candidates for treatment.
3. The Solitaire™ Revascularization Device is indicated for use to restore blood flow in the neurovasculature by removing thrombus for the treatment of acute ischemic stroke to reduce disability in patients with a persistent, proximal anterior circulation, large vessel occlusion of the internal carotid artery (ICA) or middle cerebral artery (MCA)-M1 segments with smaller core infarcts (<70 cc by CTA or MRA,<25 cc by MR-DWI). Endovascular therapy with the device should start within 6-16 hours of time last seen well in patients who are ineligible for intravenous tissue plasminogen activator (IV t-PA) or who fail IV t-PA therapy.
1. TR-NV15436C, D00272862C, D00344794B, TR-NV15519A, TR-NV15666A 2. Medtronic Data on File. Solitaire Literature Review Aug2022. Includes Solitaire FR, Solitaire 2, Solitaire Platinum, Solitaire X. 3. Goyal M, Menon BK, van Zwam WH, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet.for consistent and confident performance.
NEW DATA ON INTRAVENOUS tenecteplase indicate that it can achieve comparable efficacy and safety to alteplase in treating stroke—and, as such, may be used as an alternative to alteplase for acute ischaemic stroke patients within 4.5 hours of symptom onset.
This was the prevailing message delivered by Shuya Li (Capital Medical University, Beijing, China) in her presentation of the TRACE II trial at the 2023 International Stroke Conference (ISC; 8–10 February, Dallas, USA).

Li began by highlighting previous clinical trials that have indicated 0.25mg/kg of tenecteplase could have comparable effectiveness and safety to 0.9mg/ kg of alteplase in acute ischaemic stroke, including the Phase 2 ATTAST study and, more recently, the Phase 3 AcT study.
In an effort to build on this body of evidence, Li and her colleagues assessed the newer generation intravenous thrombolysis (IVT) drug, tenecteplase, versus alteplase, which is a more well-established and widely used thrombolytic candidate in stroke care.
They did this via a Phase 3, non-inferiority, multicentre, prospective randomised controlled trial—TRACE II—in which acute ischaemic stroke patients received either 0.25mg/kg of tenecteplase (intervention group) or 0.9mg/kg of alteplase (control group) less than 4.5 hours from symptom onset.
Li and colleagues’ primary efficacy endpoint was a score of 0–1 on the modified Rankin Scale (mRS) at 90 days, while secondary outcome measures included
mRS 0–2, ordinal distribution of mRS and quality of life (EQ-5D) scores at 90 days, as well as short-term National Institutes of Health Stroke Scale (NIHSS) scores. Safety endpoints included short- and longterm intracranial haemorrhages (ICHs), and overall mortality and (serious) adverse events within 90 days.
Between 12 June 2021 and 29 May 2022, a total of 1,430 IVT-eligible ischaemic stroke patients were enrolled at 53 clinical sites across China. Following randomisation, 710 were allocated to tenecteplase and 707 were allocated to alteplase for the trial’s modified intention-to-treat (MITT) analysis, while 671 and 642
patients, respectively, were available for the perprotocol analysis.
Reporting efficacy outcomes from TRACE II, Li informed the ISC audience that 62% of patients in the tenecteplase group achieved an mRS score of 0–1 at 90 days, compared to 58% of patients in the alteplase group. As such, the trial met its primary efficacy outcome in the MITT analysis, demonstrating non-inferiority—but not superiority—of tenecteplase versus alteplase.
Li also stated there was no significant difference between the two groups relating to any of the trial’s secondary efficacy outcomes, and an analysis of prespecified subgroups in both the MITT and perprotocol patient populations further supported the non-inferiority of tenecteplase.
Additionally, no significant differences were found regarding the prespecified safety outcomes either, with a low rate (2%) of symptomatic ICH at 36 hours and 90 days in both groups, as well as 46 (7%) and 35 (5%) deaths, and 116 (16%) and 107 (15%) serious adverse events, respectively, in the tenecteplase and alteplase groups.
Owing to the non-inferior efficacy of tenecteplase versus alteplase, and the similar safety profiles between the two drugs in TRACE II, Li concluded that intravenous tenecteplase may be used as an alternative to alteplase in patients who present with acute ischaemic stroke during the early time window (<4.5 hours).
These findings have since been published in The Lancet by Li and the rest of the TRACE II investigators— including lead author Yongjun Wang (Capital Medical University, Beijing, China).
Among Chinese patients with minor, non-disabling stroke presenting <4.5 hours from symptom onset, dual antiplatelet therapy (DAPT) has been found to be non-inferior to intravenous thrombolysis (IVT) with alteplase regarding 90-day functional outcomes.
THANH N NGUYEN (BOSTON University Chobanian and Avedisian School of Medicine, Boston, USA), who presented these preliminary findings on behalf of the ARAMIS trial investigators at the 2023 International Stroke Conference (ISC; 8–10 February, Dallas, USA), noted that—given its ease of administration, low cost, safety profile and association with less intensive monitoring—the present data support DAPT use in these patients. The benefits of IVT in mild strokes (National Institutes of Health Stroke Scale [NIHSS] score ≤5) are not fully understood, Nguyen initially posited, and recent American and Chinese stroke association guidelines advocate treatment with intravenous alteplase in patients who present less than three

hours from symptom onset.
As such, the multicentre, randomised, non-inferiority ARAMIS trial was set up to evaluate DAPT (300mg clopidogrel plus 100mg aspirin, then 75mg clopidogrel plus 100mg aspirin for 10–14 days, followed by guidelinebased antiplatelet treatment up to day 90) versus IVT (0.9mg/kg alteplase followed by guideline-based antiplatelet treatment up to day 90) in acute minor stroke patients (NIHSS ≤5) presenting within 4.5 hours of symptom onset and without clearly disabling deficit.
Nguyen relayed that ARAMIS’ primary endpoint was an excellent functional outcome (modified Rankin Scale [mRS] 0–1) at 90 days. The trial’s secondary
endpoints included 90-day favourable functional outcome (mRS 0–2); 90-day ordinal mRS shift; 24-hour NIHSS score change; and 90-day all-cause mortality and symptomatic intracranial haemorrhage (ICH).
Between October 2018 and April 2022, 760 eligible patients were randomised, with a total of 369 patients in the DAPT group (median age=65 years, 69.5% male) and 350 in the alteplase group (median age=64 years, 68.4% male) constituting the trial’s modified intention-to-treat (ITT) population. The two groups were well balanced regarding baseline characteristics too.
Detailing the primary endpoint finding in ARAMIS, Nguyen reported preliminary findings; a 93.8% rate of mRS 0–1 at 90 days with DAPT, compared to 91.4% with alteplase, noting a 2.3% risk difference of having an excellent 90-day functional outcome in the modified ITT population. With the unadjusted lower limit of the one-sided 97.5% confidence interval being -1.5%, the trial therefore met its primary endpoint, exceeding the prespecified noninferiority margin of -4.5%. ARAMIS’ perprotocol and as-treated
analyses also yielded similar results.
In addition, there was overall parity between many of the trial’s secondary endpoints—although early neurological deterioration (≥2 NIHSS point decline) within 24 hours was observed in a higher proportion of patients in the alteplase group (9.1%) than in the DAPT group (4.6%). Regarding safety outcomes, Nguyen informed the ISC audience of symptomatic ICH rates of 0.3% and 0.9% in the DAPT and alteplase groups, respectively, while bleeding events of any kind occurred in 1.6% and 5.4% of patients.
The speaker acknowledged two limitations of the ARAMIS trial; the fact that some US guidelines were updated during the course of the study, establishing DAPT over alteplase as a standard treatment in the target population, and the 20.4% crossover rate between the two groups.
After reiterating support for the use of DAPT in the minor-stroke patient population based on ARAMIS’ findings, Nguyen concluded with a nod to the global TEMPO-2 study—a randomised controlled trial comparing IVT with 0.25mg/kg of tenecteplase versus standard, antiplatelet-based care in transient ischaemic attack (TIA) or minor stroke patients presenting <12 hours from symptom onset.
58%of patients in the tenecteplase group of patients in the alteplase group
90-day mRS 0–1Thanh N Nguyen
The administration of medications to lower systolic blood pressure in acute ischaemic stroke patients who have undergone a successful mechanical thrombectomy procedure—also known as endovascular therapy (EVT)—“should be customised”, owing to possible safety concerns and only marginal benefits associated with their use. That is according to the findings of a Phase 2, late-breaking clinical trial presented at the 2023 International Stroke Conference (ISC; 8–10 February, Dallas, USA).
“HEALTHCARE
should be cautious when lowering blood pressure after endovascular treatment, as there are some signs that blood pressure that is too low may be harmful,” said lead study author Eva Mistry (University of Cincinnati, Cincinnati, USA), who delivered BEST II trial data at ISC. “Individual patients might require lowering of blood pressure due to medical and neurological reasons—however, it should not be done as a blanket practice with all patients. It may benefit some patients and needs to be customised.”
Previous research has indicated that higher systolic blood pressure after EVT is associated with greater disability in people who have had an acute ischaemic stroke, and a systolic blood pressure of 140–160mmHg has been associated with better outcomes following the procedure. But, whether using blood pressure medications to artificially lower systolic blood pressure
to less than 180mmHg is safe and effective has not been demonstrated following clot removal, according to the BEST II researchers.
“There is always the concern if blood pressure is lowered too much in patients who are having an acute ischaemic stroke that it could make the size of their stroke worse by reducing already compromised blood flow in that area,” Mistry explained.
In the prospective, randomised BEST II trial, researchers hypothesised that patients allocated to lowering systolic blood pressure targets might have a higher volume of stroke size at 36 hours and increased disability at 90 days. They enrolled 120 patients (average age of 70 years, 57% female) who had an acute ischaemic stroke and underwent successful EVT across three urban US comprehensive stroke centres. Forty patients were randomly assigned to have their systolic blood pressure lowered to a target of
The initial findings from a recent randomised controlled trial (RCT) do not support the addition of extracranial to intracranial (EC-IC) bypass surgery to the current medical management of patients with symptomatic internal carotid artery (ICA) or middle cerebral artery (MCA) occlusions. Tao Wang (Xuanwu Hospital, Beijing, China) delivered these results at the International Stroke Conference (ISC; 8–10 February 2023, Dallas, USA).
Outlining the backdrop to the CMOSS trial, Wang cited mixed results in previous studies in this space—including COSS, which produced largely negative bypass surgery results and was terminated early for futility, and the Japanese EC-IC Bypass trial, from which the final results were never published in spite of interim analyses indicating potential benefits with bypass surgery.
The CMOSS study, Wang continued, was therefore set up to compare EC-IC bypass surgery plus medical therapy with medical therapy alone in preventing stroke/death in symptomatic stroke patients with ICA
≤180mmHg; 40 patients were assigned to a systolic blood pressure target of <160mmHg; and another 40 patients were targeted to reach a systolic blood pressure of <140mmHg. Patients were treated with an anti-hypertensive medication called nicardipine, administered intravenously, started within one hour after EVT and given for 24 hours if their systolic blood pressure was above their assigned target.
In the ≤180mmHg-, <160mmHg- and <140mmHg-target groups, average systolic blood pressure reached 129mmHg, 130mmHg, and 123mmHg, respectively. In addition, the average 36-hour stroke volumes showed no conclusive evidence of harm, and 90day disability outcomes indicated only a slight indication of harm.
“The main outcomes of the study were the size of stroke at 36 hours and
degree of disability at 90 days,” Mistry said. “Although the study did not find significant evidence of an unequivocal harm of lower blood pressure targets in this population in terms of worsening size of stroke or increasing disability, the trends indicated that there may only be marginal benefit on patients’ long-term disability by lowering blood pressure after endovascular treatment. In fact, there was an indication that lowering the blood pressure after thrombectomy may worsen patients’ long-term disability.
“This study provides an indication that patients’ blood pressure should be allowed to be autoregulated after endovascular treatment, unless about 180mmHg, and clinicians might want to be cautious when they reflexively lower the blood pressure, since there may be some signal of harm. There should be individual patient decision-making, such as if there are other medical reasons for lowering the blood pressure or if there are signs of significant bleeding in the brain.”
BEST II study limitations cited by the researchers include its small number of patients, and the trial being conducted at just three US centres, potentially limiting generalisability of the results.
In her ISC presentation, Mistry posited that “we cannot rule out the potential for harm” with blood pressurelowering medications, advocating an individualised approach to their use after EVT, before concluding that ongoing trials—OPTIMAL BP, CRISIS I and HOPE—will provide additional insight on this topic.
or MCA occlusion, and haemodynamic insufficiency.
The trial—a multicentre, open-label RCT conducted across 13 tertiary care centres in China— also featured refined patient selection and operator experience, Wang noted. Its primary endpoint was a composite of any stroke of death within 30 days, or ischaemic stroke in the territory of a qualifying artery beyond 30 days through two years after randomisation. Secondary endpoints included disabling/fatal stroke, transient ischaemic attack (TIA), and National Institutes of Health Stroke Scale (NIHSS) and modified Rankin Scale (mRS) scores, as well as surgical complications.
After enrolment and 1:1 randomisation to EC-IC bypass surgery plus medical therapy, or medical therapy alone, 161 patients (mean age=52 years, 77.6% male) were included in the surgical group and 163 patients (mean age=53.5 years, 81% male) were included in the medical group for the intention-to-treat analysis.
Regarding CMOSS’ primary outcome measure, Wang reported that 13 patients (8.6%) in the surgical group and 19 patients (12.3%) in the medical group experienced an event, meaning there was no significant difference between the two groups. A posthoc analysis also revealed no significant differences in stroke/death rates within 30 days, although there was a significantly lower rate of ipsilateral ischaemic stroke beyond 30 days in the surgical group.
Wang went on to inform the ISC audience that there were no significant differences observed regarding any of the secondary outcomes. In total, six complications adjudged to have been linked to the procedures (4%) occurred in the surgical group.

The investigators conducted post-hoc subgroup analyses across multiple “important factors”, according to Wang. For example, potential benefits favouring bypass surgery versus medical therapy in MCA occlusions, and in cases of severe haemodynamic insufficiency, were observed— potentially providing directions for future studies.
Another finding highlighted by Wang was the improved overall efficacy in the medical therapy group of CMOSS compared to COSS, as 12.3% of patients reached the former’s main efficacy endpoint, while 21% did so in the latter trial. The speaker attributed this to a younger, lowerrisk patient population in CMOSS, as well as better control of risk factors. Furthermore, the perioperative stroke rate in CMOSS (6.2%) was “substantially lower” than in prior studies—15% in COSS and 12% in EC-IC Bypass. Wang said this was due to CMOSS adopting stricter surgeon certification and perioperative management criteria than COSS.
After referencing its potential limitations— including a lack of sham surgery and “uncertain” generalisability of the results to populations outside of China—Wang concluded that CMOSS’ findings do not support the addition of EC-IC bypass surgery to current medical therapy in symptomatic ICA/ MCA occlusion patients. However, he ended his presentarion by suggesting that the overall efficacy of both bypass surgery and medical therapy in these patients have “improved simultaneously”. One promising direction for the future, he added, may be to assess the benefits of bypass surgery versus medical therapy in more specific patient populations.
Tao Wang
Individual patients might require lowering of blood pressure due to medical and neurological reasons—however, it should not be done as a blanket practice with all patients.”
Two randomised controlled trials (RCTs) presented on the final day of the 2023 International Stroke Conference (ISC; 8–10 February, Dallas, USA) have further bolstered evidence indicating that the addition of mechanical thrombectomy procedures can produce improved clinical outcomes versus standard medical care in acute ischaemic strokes with a large infarct-core volume.
THE FIRST OF THESE RCTS—THE international SELECT2 study—was delivered by global principal investigator Amrou Sarraj (Case Western Reserve University, Cleveland, USA), who reported a “dramatically better recovery” in patients experiencing a larger stroke who received an endovascular thrombectomy plus standard care, as compared to those who only received standard care.
Sarraj initially noted that, while thrombectomy has proven effective in ‘smaller’ strokes, patients with greater core volumes—leading to an increased range of damaged brain tissue seen on computed tomography (CT) or magnetic resonance imaging (MRI)—have previously been considered too highrisk for the procedure.
SELECT2 sought to elucidate this and, as the speaker stated, intended to “challenge the current practice, where patients with large strokes would be precluded from thrombectomy”.
The study involved 31 medical centres in North America, Europe, Australia, and New Zealand, and was halted early because of the successful results and superior outcomes seen in patients who received thrombectomy treatments for their large vessel occlusion (LVO) strokes. While SELECT2 had an initial target of 560 patients with an LVO causing a large stroke, the data and safety monitoring board stopped the trial after the enrolment of 352 patients.
In the trial, patients were randomly assigned to receive thrombectomy plus standard care (n=178) or standard care alone (n=174). Patients who were seen prior to 4.5 hours from the onset of stroke received intravenous thrombolysis (IVT) with alteplase or tenecteplase, if eligible.
“We found that almost 20% of the patients who received a thrombectomy ended up with functional independence, going back to their family, to society, as almost normal or not needing support, compared to 7% for medical treatment only,” Sarraj reported. “We also found that almost 40% of the patients end up ambulating independently. This is a huge improvement in these patients with large strokes who are not being offered [thrombectomy] at this point.”
Sarraj also said he expects the results to change treatment guidelines in the near future—and that “this will give a large number of patients the opportunity for a chance for improvement”.

In his ISC presentation, the speaker further noted that, when considered in conjunction with RESCUEJapan LIMIT trial data—which were presented at last year’s International Stroke Conference (ISC 2022; 9–11 February, New Orleans, USA)—and findings from the ANGEL-ASPECT RCT, also delivered for the first time at ISC 2023, such results “unequivocally demonstrate” the benefits of thrombectomy in patients with a large ischaemic core.
Principal investigator Zhongrong Miao (Capital Medical University, Beijing, China) presented firsttime results from the ANGEL-ASPECT trial at ISC, positing that thrombectomy procedures performed
within 24 hours of symptom onset were found to be more effective than standard medical care in treating ischaemic strokes caused by anterior circulation LVOs with a large infarct core—resulting in improved threemonth functional outcomes. Miao reported that, while the trial met its primary efficacy endpoint, indicating improved outcomes with thrombectomy versus standard care, the procedure was also linked to an increase rate of intracranial haemorrhage (ICH).
At the outset of his presentation, Miao made a similar point to Sarraj, noting that—while thrombectomies have become the standard approach to LVO stroke following positive results in MR CLEAN, ESCAPE, REVASCAT and multiple other prior RCTs— these studies have “almost entirely excluded” patients with a large infarct-core volume.
In ANGEL-ASPECT, which aimed to further assess thrombectomyassociated outcomes in these large-core strokes, patients were included based on their non-contrast computed tomography (CT) Alberta stroke programme early CT score (NCCT-ASPECTS). Some 46 centres ultimately participated in the trial and were spread across 20 Chinese provinces, with enrolment progress starting in October 2020 and being halted early when the efficacy of thrombectomy was detected at the interim analysis in May 2022.
A total of 456 patients had follow-up data available at the 90-day follow-up timepoint in August, Miao reported. After one patient withdrew consent, 230 of these patients (median age=68 years, 58.7% male) were randomised to the trial’s thrombectomy group, with 225 (median age=67, 64% male) being allocated standard care.
In the intention-to-treat (ITT) analysis, findings as per the primary endpoint showed a shift towards better outcomes in the distribution of 90-day modified Rankin Scale (mRS) scores in favour of thrombectomy. The average mRS score at 90 days was 4 in both the thrombectomy group (range 2–5) and the standard care group (range 3–5). However, Miao and colleagues found a treatment effect of 1.37 (generalised odds ratio; p=0.004) with thrombectomy.
Overall, 30% of patients in the thrombectomy group achieved a 90-day mRS score of 0–2, versus 11.6% in the standard care group, with these rates increasing to 47% and 33.3%, respectively, for mRS 0–3. Improved National Institutes of Health Stroke Scale (NIHSS) scores at 36 hours, and reduced infarct core volumes from baseline, were also observed, as per the trial’s secondary efficacy outcomes.
“The efficacy for the primary outcome was similar across predefined subgroups and across all sites, but the trial was underpowered for these analyses,” Miao added. “The primary outcome results of the perprotocol analysis were similar to the ITT analysis.”
Regarding safety outcomes, Miao relayed that 14 symptomatic ICHs (6.1%) and 113 ICHs overall (49.1%) occurred within 48 hours in the thrombectomy group, compared to six (2.7%)
and 39 (17.3%), respectively, in the standard care group. Mortality rates were similar between the two, but more decompressive hemicraniectomy procedures were required during hospitalisation in the thrombectomy group.
Briefly outlining potential limitations of ANGELASPECT, Miao said the proportion of patients receiving IVT was low, to the potential detriment of the standard care group, and the trial being conducted among Chinese patients means the findings may not be generalisable to other populations.

“Verification of our findings is required,” the speaker concluded, highlighting corroborating studies like RESCUE-Japan LIMIT and SELECT2 as well as ongoing research, including TENSION in Europe and TESLA in the USA.
Three’s a crowd
ANGEL-ASPECT data and findings from SELECT2 were recently published in the New England Journal of Medicine (NEJM), just as the RESCUE-Japan LIMIT study was last year. An editorial authored by Pierre Fayad (University of Nebraska Medical Center, Omaha, USA), which appears alongside the publications of ANGEL-ASPECT and SELECT2 in NEJM, notes that—despite differences in design, patient selection, thrombolytic treatment/ dose, geographic location, and imaging criteria—all three RCTs show “remarkably similar results”.
“Together, the trials provide reassuring information from more than a thousand patients with large ischaemic strokes in different medical systems that will probably lead to changes in patterns of care delivery,” Fayad writes.
“It is reasonable to suggest that endovascular thrombectomy be offered to patients with large strokes […] if they arrive in a timely fashion at a centre that is capable of performing the procedure, and if the patients have an ASPECTS value of 3–5 or an ischaemic-core volume of 50ml or greater. Higher rates of ‘good outcomes’ may be anticipated if this treatment is performed, despite increased risks of symptomatic haemorrhage, oedema, neurologic worsening, and hemicraniectomy.”
“One of the biggest concerns patients and their families have about stroke is that they will be bedridden and fully dependent on others for care,” commented Society of NeuroInterventional Surgery (SNIS) president J Mocco (Mount Sinai, New York, USA). “Now, we have an opportunity to improve functional independence for even the most severe stroke patients. These findings further support the notion that every patient should be triaged to the most appropriate care so they are given a chance to survive and thrive.”
Together, the trials provide reassuring information from more than a thousand patients with large ischaemic strokes in different medical systems that will probably lead to changes in patterns of care delivery.”
Pierre FayadAmrou Sarraj (left) and Zhongrong Miao
Point of View
Alongside his colleagues at the Barts Health NHS Trust, Levansri Makalanda (London, UK) was responsible for setting up the second ever 24/7 mechanical thrombectomy service for ischaemic stroke in the UK. He recently spoke to NeuroNews to outline how this service—which is still one of only a handful of 24/7 systems of its kind nationally—was established, and provide his views on the importance of round-the-clock thrombectomy access for patients.
In the UK, there is a significant disparity in access to thrombectomy services—particularly for deprived populations. In order to address this, we set out to establish a 24/7 thrombectomy service at the Royal London Hospital, which serves a particularly deprived part of East London. Our motivations for doing so were to improve access to life-saving treatment for patients in our local area, and to reduce the burden of stroke-related disability and death in our community.
Establishing a 24/7 thrombectomy service required a significant amount of planning and coordination. We worked closely with management, the stroke team, anaesthesia and the wider interventional radiology (IR) team— including nurses and radiographers—to develop a plan for the service. We started by setting up a seven-day service,
and gradually built up the teams and resources needed to expand to a 24/7 service over the course of six months.
One of the main challenges we faced in maintaining the service was the COVID-19 pandemic, which put additional strain on staff. Additionally, within two months of establishing the 24/7 service, we were taking patients from throughout the south-east of England, from Peterborough to Margate. This vastly increased the number of patients we were treating, which required us to hire more staff to prevent burnout. However, finding the right staff was difficult, as all units were competing for these limited resources.
More generally, 24/7 mechanical thrombectomy services are important for a number of reasons. Firstly, they
THE SOCIETY OF VASCULAR AND Interventional Neurology (SVIN) has released its first global analysis of access to mechanical thrombectomy for the treatment of large vessel occlusion (LVO) stroke. Findings from MT-GLASS—a study conducted as part of the SVIN Mission Thrombectomy 2020-plus (MT2020+) initiative—have been published in the journal Circulation
The MT-GLASS study looked at worldwide access to life-saving thrombectomy treatments, and the factors that contribute to this, including income class of the country; proportion of gross domestic product (GDP) spent on healthcare; availability of thrombectomy infrastructure, including operators and centres; availability of reimbursement for thrombectomy; and other relevant stroke systems of care policies.
provide patients with timely access to life-saving treatments. Secondly, they reduce the burden of stroke-related disability and death in the community. This has knock-on financial effects on the National Health Service (NHS), but also for society as a whole.
In our own practice, we have seen the benefits of thrombectomy first hand, with patients making significant improvements in their neurological function after treatment and many being able to return to work. Whilst being the busiest unit to ever exist in the UK, our consultant-delivered service also has some of the best benchmarked outcomes for stroke thrombectomy.
As for the feasibility of a nationwide 24/7 thrombectomy service, it is likely that more services will be set up in the UK in the near future. Collaboration with partners and neighbouring units will be crucial in achieving this goal. Additionally, increasing the numbers of patients who qualify for thrombectomy will require more operators to be appropriately trained and employed. We believe that it is possible to achieve a nationwide service within the next few years—with the right resources and support.
Skilled operators and a robust stroke service are also key for setting up and maintaining a 24/7 offering; the major trials were all done in neuroscience units with trained neurointerventionists. If we fall below these standards, the outcomes are likely to suffer. This creates a number of challenges within a resource-strapped NHS system. While we are in the fortunate position of being able to attract consultants from across the world, given our pedigree in the field, the recruitment of properly trained neurointerventionists will be a problem in some parts of the UK, where there is already a shortage of doctors.
I believe—in order to maintain the great outcomes that we see in
It ultimately found an “extremely low” global rate of mechanical thrombectomy access, with an “enormous disparity” between countries by income level.
“The study findings validate why we founded Mission Thrombectomy in 2016 and our continued mission that has now grown to include 95 countries,” said Dileep Yavagal (University of Miami, Coral Gables, USA), corresponding author and chair of the MT2020+ initiative. “The global access to thrombectomy is dismally low, with the countries’ income level, prehospital protocols to bypass nonthrombectomy centres, and operator and thrombectomy centre availability, all playing critical roles in thrombectomy access in a given region.”

MT-GLASS was conducted throughout 75 countries using the Mission Thrombectomy global network of regions between November 2020 and February 2021, and received 887 responses from across 67 countries.
It found a median global thrombectomy access rate of 2.79% (interquartile range, 0.7–11.74%), and revealed a <1% rate of access in 18 countries and 0% in seven countries. Low-income countries also had an 88% lower rate of access versus highincome countries. The global rate of availability for thrombectomy-capable operators and centres were found to be 16.5% and 20.8%, respectively, of what is considered to be the “optimal” rate.
our service—patients will need to be transported to high-volume neuroscience centres for optimal management before, during and after the procedure. There is a lot more nuance than just pulling out a clot!
We began this service with a view to constant iteration and improvement. We were down on neurointerventionist numbers—having four instead of the required eight—and also had only one room to operate in. These factors are being addressed as we speak. More junior doctors are further required within the stroke team, given the volume of referrals we receive, and we are looking to increase our bed base to help with the extra patients too.
In order to keep at the cutting edge, we are now also involved with a number of registries and trials so that we can contribute to the research and evidence base in the future while keeping at the cutting edge for the patients we currently treat. This has the added effect of allowing our thrombectomy stocks to be continually replenished, which is no mean feat during a worldwide polytetrafluoroethylene (PTFE) crisis.
In conclusion, 24/7 thrombectomy services are a vital component in the treatment of stroke. Our experience has shown that it is possible to establish a 24/7 service. It takes careful planning, coordination and collaboration but— with the right resources and support— a nationwide service can be achieved.
Levansri Makalanda is a consultant interventional and diagnostic neuroradiologist, and clinical lead for Interventional Neuroradiology, at Barts Health NHS Trust in London, UK. He is also a course director for the annual Barts Research and Advanced Interventional Neuroradiology (BRAIN) conference.
“Thrombectomy has proven to be highly effective for mitigating death and disability [...], and it is the largest advancement in stroke treatment in 30 years,” said SVIN president Ameer Hassan (Valley Baptist Neuroscience Institute, Harlingen, USA). “Given the widely distributed global burden of stroke, it is critical to have rapid access to mechanical thrombectomy, worldwide, in an equitable manner. In the USA, stroke is now the number-five killer but, in the rest of the world, it is still number two! The findings highlight distressing results on a global scale, and represent many lives that could have been saved or significantly improved with better access to thrombectomy.”
Given the widely distributed global burden of stroke, it is critical to have rapid access to mechanical thrombectomy, worldwide, in an equitable manner.”
Ameer Hassan
Mechanical thrombectomy appears to be a safe and technically feasible treatment option for ischaemic strokes caused by primary isolated anterior cerebral artery (ACA) occlusions in more distal locations. The procedure—which is more traditionally used in large vessel occlusions (LVOs) of the middle cerebral artery (MCA) and internal carotid artery (ICA)—has also demonstrated similar clinical outcomes to best medical management with or without intravenous thrombolysis (IVT).
These are the key findings of an international registry study published recently in the journal Radiology by Lukas Meyer (University Medical Center Hamburg-Eppendorf, Hamburg, Germany) et al

As Meyer and his co-authors point out in their introduction, despite thrombectomy being a potential therapeutic option in distal occlusion stroke, current evidence supporting its benefits specifically for primary, isolated distal medium vessel occlusions (MeVOs) in the ACA is, to their knowledge, “generally unknown”.
They aimed to elucidate this issue through a case-control study of the TOPMOST registry—an international, retrospective, multicentre, observational registry of patients treated for distal cerebral artery occlusion stroke. Meyer et al analysed the clinical and safety outcomes of thrombectomy for primary, isolated ACA occlusions of the more distal A2–A4 segments, compared to best medical management with or without IVT, in daily clinical practice between January 2013 and October 2021.
In this study, endovascular reperfusion was evaluated using the modified thrombolysis in cerebral infarction (mTICI) scale. The number of reperfusion manoeuvres was counted—including first-pass effect (mTICI 3 after first attempt)—and a final reperfusion result of mTICI 2b–3 was considered a successful thrombectomy, with intervention times and the rate of intervention-related serious adverse events also being detailed.
Regarding clinical measures, early outcome was assessed via the median improvement of National Institutes of Health Stroke Scale (NIHSS) scores at
24 hours, while functional outcomes were defined as favourable (modified Rankin Scale [mRS] score of 0–2) or excellent (mRS 0–1) at 90 days. Safety was assessed by the occurrence of mortality—during hospitalisation and at day 90—as well as symptomatic intracerebral haemorrhages (ICHs).
From a total of 154 patients who met the inclusion criteria, Meyer et al detail that 110 patients (median age=76 years, 50 men) underwent propensity score matching, with 55 having received a thrombectomy and 55 receiving best medical management. Distal MVOs were located in the A2 (53% of patients), A3 (45%) and A4 (2%) segments. Prior to propensity score matching, the authors observed a median time from symptom onset to groin puncture of 195 minutes across 94 patients who received a thrombectomy. The median number of reperfusion attempts was one, and successful thrombectomy (mTICI grade 2b–3) was achieved in 81% of patients. Complete reperfusion (mTICI 3) was achieved in 67% of patients—including a first-pass effect rate in 41%. Symptomatic and asymptomatic bleeding events were observed in 2% and 14% of patients, respectively, before propensity score matching.
The authors report a median 24-hour NIHSS point decrease of 2 in the thrombectomy cohort compared to 1 in the best medical management cohort. In addition, the distribution of mRS scores at 90 days showed “no evidence of a statistically significant difference” between the thrombectomy and non-thrombectomy cohorts regarding mRS scores of 0–1 (38% vs 33%, respectively) and 0–2 (49% in both groups).
“There was no evidence of statistically significant differences when clinical and safety outcomes were
A study intended to examine the impact of different weather conditions and modes of transport on mechanical thrombectomies in stroke patients has found a link between higher temperatures and improved outcomes—whereas daily drizzle was associated with poorer post-thrombectomy outcomes.
Pascal Jabbour (Thomas Jefferson University Hospital, Philadelphia, USA) and colleagues posit that “further studies are needed to modify transfer protocols, especially during cold and rainy days, and potentially improve outcomes”.
Writing in the journal Neurosurgery, Jabbour et al detail how they retrospectively collected data for stroke patients transferred from a ‘spoke’ centre to their ‘hub’ hospital to undergo
a mechanical thrombectomy between 2017 and 2021.
The researchers did this to assess how varying weather conditions may influence stroke risk, as well as patient transfer protocols and outcomes, as the efficient transfer of patients with stroke to a mechanical thrombectomy-capable centre is “essential”.
Jabbour et al included a total of 543 patients with a mean age of 71.7 years in their study. In these patients, they observed an increase in median
stratified by occlusion site,” Meyer et al add. “This finding remained stable if we included the last known mRS scores in patients with missing long-term follow-up.”
Functional outcomes stratified across several subgroups—including age, sex, occlusion site, NIHSS on admission, and whether IVT was given—showed no evidence of a difference in 90-day mRS score distributions between the two cohorts. Ninety-day mortality rates were similar with (22%) and without (31%) thrombectomy too, as were in-hospital mortality rates (11% and 10%, respectively).
“We did not find a treatment effect in favour of one therapy option after propensity matching,” Meyer et al conclude. “These results show the potential efficacy of [best medical management] in the subgroup of ACA distal medium vessel occlusion. Mechanical thrombectomy may be considered a technically feasible treatment option for acute ischaemic stroke due to primary isolated occlusions in the A2 and A3 segments because it can lead to high rates of successful reperfusion associated with favourable long-term outcome and did not result in increased rates of symptomatic bleeding events compared with [best medical management] if patients were treated at tertiary stroke centres.
“Nevertheless, patient selection for treatment allocation requires further investigation to identify patients who will benefit the most from available treatment options.”
And, in spite of their study’s potential limitations— including its retrospective design, small sample size, and absence of some clinical data—the authors assert that these results “reinforce clinical equipoise, and encourage ongoing and upcoming randomised trials investigating treatment options for distal MeVO stroke”.
National Institutes of Health Stroke Scale (NIHSS) score from 14 to 15 after transportation; while the median modified Rankin Scale (mRS) score was 4 at discharge and 90 days, and 3 at the final follow-up (mean time=91.7 days).
“Higher daily temperatures were associated with good outcomes, whereas daily drizzle was associated with poor outcomes,” the authors report. “More patients were transferred by air when visibility was better, and by ground during heavier precipitation, higher humidity, rain, mist, daily drizzle, fog, and thunder.”
However, Jabbour and his colleagues ultimately did not find an association between transportation mode and patient outcomes. And, across the independent predictors of a good outcome, none were determined to be a weather variable. Lower hourly relative humidity (p=0.003) and longer road distance (p<0.001) were independent
predictors of using air transportation, among others, they add.
Speaking to NeuroNews to outline potentially beneficial modifications to transfer protocols, Jabbour said: “It depends on how far [away] the spoke hospital is. Ground versus air transport should be chosen according to which one is faster; above a certain distance, air transport makes more sense. Adverse weather affects all kinds of transport. A traffic map evaluation should be done as soon as a transport team is getting ready to be dispatched— keeping in mind that, sometimes, there is no choice, [as] the weather does not permit air transport.”
And, discussing further studies in this space, Jabbour added: “Future randomisation between different types of transport would help us determine, in a scientific way, which modality to choose, and will help us match the best transport type with each patient according to weather and location.”
There was no evidence of statistically significant differences when clinical and safety outcomes were stratified by occlusion site.”Lukas Meyer
A meta-analysis of recent basilar artery occlusion trials—including ATTENTION and BAOCHE—has further indicated the potential benefits held by endovascular therapy (EVT) in treating posteriorcirculation large vessel occlusion (PC-LVO) stroke.
WRITING IN THE JOURNAL of NeuroInterventional Surgery, authors Jeremy Heit (Stanford University, Stanford, USA), Gautam Adusumilli (Massachusetts General Hospital, Boston, USA) et al note that previous randomised controlled trials (RCTs) and meta-analyses were “underpowered” to demonstrate the superiority of EVT over medical therapy in the treatment of acute ischaemic stroke due to LVO of the posterior circulation.
“We performed an updated systematic review and meta-analysis after the publication of the BAOCHE and ATTENTION trials to determine
whether EVT can benefit patients presenting with PC-LVO,” they add.
Results of the ATTENTION RCT were first presented at the 2022 European Stroke Organisation Conference (ESOC; 4–6 May, Lyon, France) by Raul Nogueira (University of Pittsburgh, Pittsburgh, USA), who stated, “[…] I think we can finally say we have conquered the basilar artery territory”, in his talk. The BAOCHE RCT’s findings were also presented at ESOC 2022 by Tudor Jovin (Cooper University Health Care, Camden, USA) and subsequently published in the New England Journal of Medicine
With these new and more positive data to hand, Heit, Adusumilli and colleagues sought to reassess the benefits of EVT following the negative—or, at the very least, inconclusive—findings from prior RCTs, such as the European BASICS trial and the Chinese BEST trial. Neither of these trials were able to demonstrate significantly improved outcomes with EVT versus standard medical therapy.
Using a research software solution, the authors screened literature for RCTs on EVT in PC-LVO stroke. The primary outcome of their analysis was a 90-day modified Rankin Scale (mRS) score of 0–3, and secondary outcomes included a 90-day mRS score of 0–2, 90-day mortality, and rate of symptomatic intracranial haemorrhage (sICH).

A random-effects model was also used to compute rate ratios (RRs) and their corresponding 95% confidence intervals (CIs).
Four RCTs featuring a total of 988 patients—556 in the EVTplus-medical therapy arm and
432 in the medical therapy-only arm— were included in the meta-analysis.
Outlining their results, Heit, Adusumilli et al report that EVT resulted in “significantly higher rates” of mRS score 0–3 (RR=1.54; 95% CI 1.16–2.04; p=0.002) and functional independence (RR=1.83; 95% CI 1.08–3.08; p=0.024), and lower rates of mortality (RR=0.76; 95% CI 0.65–0.90; p=0.002) at the 90-day follow-up, compared with medical therapy alone.
However, patients treated using EVT also experienced higher rates of sICH (RR=7.48; 95% CI 2.27–24.61; p<0.001), the authors detail.
“EVT conferred significant patient benefit over [medical therapy] alone in the treatment of PC-LVO,” Heit, Adusumilli and colleagues conclude. “Future studies should better define patients for whom EVT is futile and determine factors that contribute to higher rates of sICH.”
Speaking to NeuroNews, Heit stated: “The higher rate of sICH may reflect the high rates of intracranial atherosclerotic disease in the Chinese population that comprised BEST, BAOCHE and ATTENTION. In BAOCHE and ATTENTION, there were high rates of EVT treatment with angioplasty and cerebral artery stent placement that often requires the administration antiplatelet medications. Further study is needed determine if these
intensive treatment targets—in patients with elevated blood pressure after reperfusion with a thrombectomy.
“We conducted an open-label, blinded-endpoint, randomised controlled trial [RCT] at 44 tertiarylevel hospitals in China,” Anderson, Liu and colleagues detail. “Eligible patients (aged ≥18 years) had persistently elevated systolic blood pressure (≥140mmHg for >10 minutes) following successful reperfusion with endovascular thrombectomy for acute ischaemic stroke from any intracranial LVO.”
treatments result in increased rates of sICH.

“BAOCHE and ATTENTION also enrolled patients with a favourable posterior-circulation Alberta stroke programme early CT score (PCASPECTS)—which may have helped to enrich for patients likely to benefit from EVT. Additional research is needed to better define which patient populations respond favourably and unfavourably to EVT. Our ongoing NIH [National Institutes of Health]-funded PRECISE study is designed to help address this question, and we look forward to reporting our findings when the study is complete.”
“Our study is the largest collation of high-level evidence on the effectiveness of EVT compared to medical therapy in basilar stroke, and we were able to demonstrate a significantly greater benefit conferred by EVT in treating these patients,” Adusumilli added. “The number needed to treat was seven for good functional outcome (mRS 0–3) and functional independence (mRS 0–2), and 10 for preventing mortality. We were also able to reaffirm a strong reperfusion success rate (85%) of EVT in basilar stroke.
“However, this does not close the debate on EVT being beneficial in all patients presenting with basilar stroke— the key being ‘all’. Fifty-five percent of patients after EVT ended up with severe disability or died, so there is clear incongruence between reperfusion success and outcomes. As Dr Heit suggests, further work should focus on determining the patients who are not benefitted by EVT, and how we can treat them.”
Anderson, Liu and colleagues write. “The trial was stopped after review of the outcome data on 22 June 2022 due to persistent efficacy and safety concerns.”
A total of 407 participants were assigned to the trial’s more intensive treatment group and 409 to the less intensive treatment group—of whom 404 and 406, respectively, had primary outcome data available.
Recently published data from the ENCHANTED2/MT study have shed new light on the safety and efficacy of more intensive versus less intensive blood pressure lowering after mechanical thrombectomy procedures in large vessel occlusion (LVO) stroke patients.
The key finding from this trial, which is now published in The Lancet, is that “intensive control of systolic blood pressure to lower than 120mmHg should be avoided to prevent compromising the functional recovery of patients who have received endovascular thrombectomy for acute ischaemic stroke due to intracranial LVO”.
Craig Anderson (University of New South Wales, Sydney, Australia), Jianmin Liu (Naval Medical University, Shanghai, China) and the rest of the ENCHANTED/MT investigators begin by asserting that the optimum systolic blood pressure after a thrombectomy procedure for acute ischaemic stroke is currently “uncertain”. As such, they aimed to compare the safety and efficacy of blood pressure-lowering treatments—according to more intensive versus less
In the ENCHANTED2/MT RCT, patients were randomly assigned on a 1:1 basis—via a central, webbased programme with a minimisation algorithm—to more intensive treatments (systolic blood pressure target of <120mmHg) or less intensive treatments (target of 140–180mmHg), which were to be achieved within one hour and sustained for 72 hours.
The study’s primary efficacy outcome was functional recovery, assessed according to the distribution in scores on the modified Rankin Scale (mRS) at 90 days. Analyses were done according to the modified intention-to-treat principle, the authors note. Efficacy analyses included all randomly assigned patients who provided consent and had available data for the primary outcome, while the safety analysis included all randomly assigned patients. The investigators note that treatment effects were expressed as odds ratios (ORs).
“Between 20 July 2020 and 7 March 2022, 821 patients were randomly assigned,”
According to the investigators, the likelihood of poor functional outcome was greater in the more intensive treatment group as compared to the less intensive treatment group (common OR 1.37 [95% confidence interval (CI) 1.07–1.76]). In contrast with the less intensive treatment group, the more intensive treatment group had more early neurological deterioration (common OR 1.53 [95% CI 1.18–1.97]) and major disability at 90 days (OR 2.07 [95% CI 1.47–2.93]), but there were no significant differences in symptomatic intracerebral haemorrhage, nor in serious adverse events or mortality, between the two groups.
These results—which were also presented at last year’s World Stroke Congress (WSC; 26–29 October, Singapore)—lead the authors to conclude by stating that such intensive blood pressure lowering should be avoided. However, speaking at WSC 2022, Anderson said: “While our study has now shown intensive blood pressure control to a systolic target of less than 120mmHg to be harmful, the optimal level of control is yet to be defined.”
Intensive blood pressure lowering “should be avoided” after stroke thrombectomy
Permanent intracranial stenting offers a feasible, safe ‘bailout’ option following a failed mechanical thrombectomy procedure. This was the concluding message delivered recently by Sarah Power (Beaumont Hospital, Dublin, Ireland)—who highlighted stenting’s association with improved successful recanalisation rates (thrombolysis in cerebral infarction [TICI] 2b–3 of 65–100%); positive functional outcome rates (modified Rankin Scale [mRS] 0–2 of 34–49%); and acceptable rates of symptomatic intracranial haemorrhage (sICH; 5–12%), in the current literature.
Speaking at the Barts Research and Advanced Interventional Neuroradiology (BRAIN) conference (5–8 December 2022, London, UK), she posited that the current literature details multiple potential rescue strategies following a failed thrombectomy. These include intra-arterial injection of thrombolytic agents or glycoprotein 2b/3a inhibitors; angioplasty with or without a drug-eluting balloon; and rescue stent insertion, with Power opting to focus on the third of these options.

Drilling down into the existing literature on rescue stenting, the speaker noted that there are no randomised controlled trials (RCTs) assessing this approach, and only a handful of prospective studies, with a preponderance of observational and retrospective research having been conducted to date. However, she continued, there are four systematic reviews and metaanalyses available on this topic.
The most recent of these was published in Interventional Neuroradiology in 2020, and compared rescue stenting with medical care alone in refractory large vessel occlusion (LVO) patients across Europe and Asia. Power reported a “very high” successful recanalisation rate of 65–92% following
stenting in this study, as well as a significantly higher rate of good outcomes and lower mortality rates at 90 days in the stenting group versus the control group.
“There was no significant difference in the rate of sICH,” she added, “but, interestingly, there was a trend towards an increased rate [of sICH] in the control group.”
Here, Power highlighted a trend in this particular study, but also across many others, towards glycoprotein 2b/3a inhibitors being used consistently as a bolus in the intraprocedural phase, later stating that this was the “biggest surprise” she encountered within the existing literature.
The speaker then moved on to two further publications from 2019—a systematic review in World Neurosurgery assessing rescue stenting after failed thrombectomy or high failure risk thrombectomy, and
The utilisation of 3D printing to make drug-eluting stents may currently be in its infancy, but the advantages it carries—such as the ability to develop patient-specific devices and tailored drug-release profiles, and evaluate different materials and designs via computational modelling—offer the potential to overcome some key limitations associated with established manufacturing methods.
THIS WAS THE PREVAILING message delivered by Dennis Douroumis (University of Greenwich, London, UK) at the 2022 Barts Research and Advanced Interventional Neuroradiology (BRAIN) conference
(5–8 December, London, UK), who also highlighted subsequent improvements to the clinical performance of these stents, and to patients’ overall quality of life, that 3D printing may bring.
“We believe that, over the years,
a systematic review and meta-analysis in the Journal of NeuroInterventional Surgery evaluating the safety and efficacy of bailout stenting after failed thrombectomy. Across the global patient populations in both of these studies, high rates of successful recanalisation (79% and 71%, respectively) were observed with stenting, and stenting use corresponded to improved functional outcomes without increasing sICH or mortality rates.
Finally, Power alluded to a 2019 publication in Stroke that specifically looked at LVOs caused by atherosclerotic disease and largely included studies from Asia, noting that patients with underlying intracranial atherosclerosis (ICAS) were significantly more likely to experience intraprocedural re-occlusion (36.9% vs 2.7%), and require rescue balloon angioplasty (9% vs 1.3%) or stenting (37.8% vs 2.6%) after failed thrombectomy, in contrast to the analysis’ non-ICAS group.
Power also briefly outlined data from two registry studies that have been published recently— STAR (Stroke thrombectomy and aneurysm registry) and ReSET (Rescue stenting for failed endovascular thrombectomy). Via comparisons with matched cohorts from the medical arms of multiple stroke thrombectomy RCTs, the former demonstrated improved outcomes with no significant increases in early-timepoint haemorrhagic events when stenting was used, while the latter produced successful recanalisation and favourable outcome rates of nearly 99%, and 66%, respectively, and found that the bailout stent remained patent at follow-up in 82% of cases.
“Is permanent stenting [after] failed thrombectomy feasible?” the speaker queried. “I think, if we look at the literature, the answer to that is yes. We do not have RCT data but what we do have seems to suggest this is something that can help us in failed thrombectomy cases.”
Power went on to note that the literature also indicates that rescue stenting appears to improve successful recanalisation rates as compared to both the medical arms of major stroke RCTs and patients who do not receive stent implantation—and the same can be said for functional outcome rates too.
“Are the risks acceptable?” she continued. “I think that they are, and we also know from the meta-analyses that the rates of sICH are in fact higher in patients who were not treated with stents.”
Power concluded by making an “important point”, which is that—prior to rescue stenting—operators should use an angiographic run to ensure there is flow present through the occluded vessel when the stentriever is deployed, and perform on-table computed tomography (CT) to evaluate for intracranial haemorrhage as well.
improvements to the technological features will render 3D printing as a major manufacturing tool for bioresorbable, drug-eluting stents,” the speaker further asserted.
In a presentation detailing his research involving coronary stents, Douroumis claimed that—while it is thought that bioresorbable stents made from polymers may offer potential benefits compared to their more traditional metal counterparts—the identification of suitable polymers to meet stent specifications and the need for new, optimal drug substances represent two key challenges here.
Outlining the role of 3D printing as a possible solution to this, Douroumis began with a nod to the four key manufacturing methods for bioresorbable, drug-eluting stents— injection moulding, weaving, laser cutting, and 3D printing.
“All of these technologies present some advantages, but most of them have disadvantages [too],” he added. “For example, laser cutting—which is used very often—can cause thermal damage, and create sharp edges on the struts, and it also has high manufacturing costs.”
Even within 3D printing, there are multiple different approaches as well, Douroumis relayed, with the main ones being stereolithography, selective laser sintering, and fused deposition modelling. He went on to state the various advantages associated with these methods, such as the fact that personalised stents can be made to suit an individual patient’s needs and ultimately improve clinical outcomes.
According to Douroumis, other potential benefits of 3D-printed drug-eluting stents include the
Continued over page
Are the risks acceptable?
I think that they are.”
Current literature supports stenting as feasible bailout option after failed thrombectomy
ability to create complex geometries encompassing a range of shapes and sizes; tailored drug-release profiles that allow more than one drug to be administered; the use of bioresorbable and biocompatible materials; and a reduction in wasted materials.
Douroumis also highlighted some of the work done by him and his team using fused deposition modelling to 3D-print and test a wide range of stent designs. However, owing to the high cost of the filaments used to create these devices, and the fact that printing out and evaluating numerous different prototypes would therefore be extremely expensive, he and his colleagues currently use computational modelling to assess how different materials are likely to perform within different stent designs.
“These [simulations] will give us a prediction of the stent’s mechanical properties,” the speaker added. “[The aim of this exercise] was to develop stents with superior radial recoil, longitudinal retraction, foreshortening and max diametral strain.”
Based on how well a given stent concept performs in these assessments, its design, or the formulation of the polymers used, can be adjusted fairly easily, Douroumis noted.
He went on to emphasise the importance of the very high levels of accuracy and precision that can be achieved with 3D printing, as this enables stents with the correct diameter to be created and increases the likelihood of subsequent treatments with the device being successful. However, the speaker also conceded one major
The “renaissance” of neuro- and cerebroprotective paradigms, coupled with “the advent of new ideas”—such as the concept of “transient neuroprotection” to preserve the penumbra—appears to offer promise in interventional stroke care. This was arguably the prevailing message offered by Johannes Boltze (University of Warwick, Coventry, UK) at the Barts Research and Advanced Interventional Neuroradiology (BRAIN) conference (5–8 December 2022, London, UK) in a presentation on neuroprotective therapies “in the recanalisation era”.
BOLTZE INITIALLY OPINED THAT recanalisation has been something of a “gamechanger” in the field recently but that, despite this, stroke interventions are still only beneficial to a minority of patients, with key reasons for this being time lost during the prehospital phase; limited access to capable centres; and certain comorbidities.
Drugs and proteins, the speaker continued, are among leading approaches currently being investigated as a means for minimising cerebral infarction and, thus, improving clinical outcomes following an acute ischaemic stroke.

Improving the supply of oxygen to the brain following a stroke is one neuroprotective mechanism that is believed to offer promise, according to Boltze, who highlighted the role H-NOX proteins—high-affinity nitric oxide sensors—can play here. A recombinant variant of these proteins, named Omniox-Ischemic Stroke (OMX-IS, Omniox), has already been investigated extensively in cardiovascular conditions, and is now being studied in acute ischaemic stroke, with recent data from animal models indicating that OMX-IS can “buy a significant amount of time” for the patient, he added.
Boltze elaborated that, overall, these studies have found “no difference” in infarct size when the protein was administered, but that the time gained in the
limitation of fused deposition modelling technologies.
“These stents are relatively thick—the thickness varies from 300–400μm—so we [are aiming] to make them much thinner,” Douroumis continued. “We had to manipulate and improve the hardware of the printer a lot and, at the moment, the capacity of these particular printers to go down to better resolutions is a bit limited. But, in the next few years, we might see changes there.”
He stated that, because of this, his team has also begun deploying
treated animals was more than two hours—which he reiterated constitutes a “significant” saving.
In addition, reducing oxygen consumption, such as via adenosine A1 and A3 receptors, offers another frontier for mitigating against cerebral infarction, according to Boltze. Firstly, he touched on an A1 receptor agonist that has shown promise in mouse models—reducing overall infarct volume, neurological deficit scores and mortality rates—before highlighting positive preclinical findings with AST004 (Astrocyte) in non-human primates, including total infarct volume reductions that were “on the very edge of statistical significance” and “quite favourable” pharmacokinetic endpoints. The latter has now progressed to a Phase 1 clinical trial, which is ongoing.
“When it comes to the drugs and proteins I [have] introduced to you, we see some promising yet, what I would call, ‘realistic’ results—it is definitely not a golden bullet,” the speaker added. “They may be doing something good on [the surface] but they are not curing stroke as we believed [they could] in the past.”
Boltze further noted that large animal experiments are becoming more important in testing these drugs and proteins, thanks to the “very interesting” parallels they offer versus human stroke patients, and this is reflected in the clinical trials that are now also underway here.
In the second part of his presentation, Boltze discussed the use of cell treatments in neuroprotection, stating: “Clinical trials have been conducted all over the world—mainly using adult cell populations, which are believed to be much safer to employ. And that has indeed [been shown], but the overall outcomes have been rather neutral, and this has made the field a little bit quiet recently.”
He went on to note, however, that this is more pertinent in the western world than in Asia, and some clinical investigations, such as the MASTERS-2 trial assessing the MultiStem stem cell product (Athersys), are underway.
MultiStem progressed to a full clinical trial after being found to be “safe and well tolerated”, and managing to show “very modest benefits”, in a Phase 2 clinical study. Here, Boltze noted a high level of heterogeneity in the Phase 2 study population, and substantial differences between the chosen therapeutic
stereolithography in stent manufacturing as well, owing to its “excellent” print resolution (25μm), and ability to incorporate drugs during the printing process, improve mechanical strength and fabricate ‘shape memory’ stents. Douroumis concluded by stating that assessments of stereolithography-printed stents at his centre have found that they deviate only marginally from initial device designs, and have a “very smooth surface” with “no defects” and a strut thickness of 150–250μm that is “quite consistent”, before adding that there is “more work to do” and clinical trials of some of these 3D-printed stents are hopefully on the horizon.
time window as compared to prior preclinical research.
Nevertheless, the trial did see 14.9% more patients achieve the specified endpoints (modified Rankin Scale [mRS] 0–2 and a minimum reduction of 75% in National Institutes of Health Stroke Scale [NIHSS] score from baseline) in the MultiStem treatment group versus a placebo—which Boltze described as “very modest” yet statistically significant and “clinically meaningful”.
The speaker also highlighted another existing problem in this area—the fact that intravenously transplanted cells reach the brain in “very small numbers”, which may detract from the efficacy of such treatments. Administering them arterially, immediately after recanalisation, is an approach that would not have been technically feasible in the past but may mean a greater number of cells end up in the brain, Boltze continued. However, he conceded that intra-arterial administration “may not always be safe” and optimisation of such procedures is likely still required for some cell populations as well.

Boltze concluded by noting that these experimental therapies offer hope within interventional stroke care, and there is a chance they will translate to improved clinical solutions in acute ischaemic stroke further down the line.
Furthermore, the ‘recanalisation era’ means these therapeutic agents can be applied “wherever and whenever we need them”, in theory, and transient protection of the penumbra offers a new approach in this space.
When it comes to the drugs and proteins I [have] introduced to you, we see some promising yet, what I would call, ‘realistic’ results— it is definitely not a golden bullet.”Johannes Boltze Dennis Douroumis
A recent update on the DISTAL randomised controlled trial (RCT)—which was delivered at the Barts Research and Advanced Interventional Neuroradiology (BRAIN) conference (5–8 December 2022, London, UK)—saw attendees discuss the study’s strengths, and how far it could go towards providing much-needed answers on endovascular therapy (EVT) for medium- and distal-vessel occlusion strokes.

MARIOS PSYCHOGIOS (University Hospital Basel, Basel, Switzerland), who presented this update and is also the principal investigator (PI) for DISTAL, described it as a “pragmatic trial”, citing the process by which a patient enters the hospital, undergoes imaging and receives best medical therapy (BMT)—meaning there is no delay to the usual standard of care—before being randomised to ‘angio’ or ‘no angio’.
The DISTAL trial is a European, multicentre RCT evaluating the clinical efficacy of EVT in acute ischaemic stroke patients with an isolated medium vessel occlusion (MeVO) or distal vessel occlusion (DVO). Its primary objective is to determine whether these patients experience superior long-term functional outcomes, measured via the modified Rankin Scale (mRS) at 90 days, when treated with EVT plus BMT versus BMT alone. Psychogios also noted that the chosen approach to EVT (aspiration, stent retriever or both) is at the operator’s discretion.
The speaker relayed that—at the time of the BRAIN conference—a total of 74 patients (rising to 93 as of 9 January 2023) had been enrolled across 25 sites but that, with DISTAL initiating new centres “every week”, this number of sites was expected to rise to around 35 by the end of 2022. Psychogios went on to report that the majority of patients have been enrolled in Switzerland, but Germany, Spain, Finland, and Belgium have all contributed, with sites in the UK, Israel and Portugal expected to join as well, with Paul Bhogal (Barts Health NHS Trust, London, UK) to be named as DISTAL’s national PI in the UK.
Highlighting some early results on patient demographics, the speaker also reported an average participant age of 75 years, with the trial mainly enrolling older patients thus far, and a median National Institutes of Health Stroke Scale (NIHSS) score of 5 at admission. The trial has enrolled occlusions spanning a variety of locations, he continued, including non-dominant M2s (40%) and M3s (30%) as well as anterior (6%) and posterior (25%) cerebral artery (ACA/PCA) occlusions.
“In the beginning, we had some gender issues, but this has now been equalised to around 50/50 [male/ female],” Psychogios said. “We tried to
[make it] as easy as possible for you to include patients, and we also did a lot of work on the randomisation tool.”
He also referenced the fact that exact pre-stroke mRS scores are not mandated under the inclusion criteria, and “only three clicks” are required to randomise DISTAL patients in the acute setting.
Following this trial update, Psychogios asserted that, as stroke physicians “climb up the mountain” and go more distally within the neurovasculature, they need more tools—adding that the onus is partly on the companies working in this space to prioritise dedicated devices for treating distal occlusions. After running through a handful of noteworthy cases performed at his centre, the speaker shared his own setup for treating MeVOs and DVOs, and provided the audience with a number of ‘tips and tricks’, such as placing the primary stent retriever distally (two thirds) to the clot—and combining this with a 4Fr or 5Fr aspiration catheter for M2 occlusions, or a 3Fr aspiration catheter for M3 and A2 occlusions.
“I have used most 3mm stent retrievers with a 0.013-inch microcatheter, [which] is available up to a length of 167cm,” Psychogios said. “And, if you use the shorter 3Fr aspiration catheter that is available in Europe [153cm], you do not actually need to do blind mini-pinning.”
Psychogios added that, for thrombectomies in Basel, he and his colleagues prefer a combined approach, and try to create multiple joints to reduce drag and mitigate straightening of the vessels and avulsion of the perforators during the procedure.
“To conclude, mechanical thrombectomy for MeVOs and DVOs is feasible,” he continued. “Of course, we need randomised controlled data, and we are going to get that with the DISTAL trial but also with the other MeVO/DVO trials like ESCAPE-MeVO [in Canada], with DISTALS [in the USA], and with DISCOUNT in France.”
In a subsequent discussion, Tommy Andersson (Karolinska University Hospital, Stockholm, Sweden) commended the DISTAL trial and the “great” pragmatic approach it is
utilising, but also voiced reservations regarding “one small problem”—the inclusion of M2 occlusions in the trial, as they often represent a “regular case” akin to an M1.
Responding to Andersson’s suggestion that this may “blur the results”, or make them better than they would have been without including M2s, Psychogios admitted he used to have a similar mindset—that treating M2 occlusions is a “no-brainer”—until he began working in Basel in 2019, and was challenged regarding the lack of existing randomised data on EVT for M2s.
“It is nice to live in this interventional bubble where we see the world as it is from our side, but we also have to
where no randomised data exist at the moment. He also cited this as one of the reasons why the DISTAL team is looking to join forces with the other groups running DVO trials, potentially providing a larger sample size of patients and paving the way for further subgroup analyses.
Osama Zaidat (Mercy Health St Vincent Medical Center, Toledo, USA) seconded Andersson’s concerns, adding that, despite being a “good” trial, DISTAL may fail to address the true clinical question in this space owing to the enrolment of M2 cases—many of which are “technically easy to do”. Zaidat also pointed out that several prior RCTs have included M2 occlusions too, meaning there is already an abundance of data on ‘good’ M2s. He went on to opine that “everybody is scared” of tackling far more complex “true distal cases”, despite these being the cases for which answers are truly needed.
“But, I think, down the line, the pooled analysis from all the distal trials will give us an answer,” he concluded—a point that Psychogios agreed with.
consider the conservative neurologists’ side at some point, and produce those data,” he added.
“I agree,” Andersson replied, “but, for me, the difference between an LVO [large vessel occlusion] and a MeVO is that LVOs are [all] pretty much the same—regardless of location, you can put them together and you can trust the results. When you talk about distal occlusions, they are so different depending on the area and how distal they are. So, would it not be difficult in the end to analyse the result and get some guidelines based on that?”
While Psychogios conceded that this does pose a challenge, he stated that—by including only co-dominant or non-dominant M2s—DISTAL is excluding the dominant M2s that were included in prior LVO trials and, thus, can concentrate on occlusion locations
Speaking to NeuroNews after the conference, Psychogios clarified once more that not all M2s have been included in the DISTAL trial, and the ‘good’ or ‘easy’ ones that Andersson and Zaidat referenced are subject to the study’s inclusion criteria. DISTAL will only include co-dominant or nondominant M2s, meaning the superior M2 trunk (usually the non-dominant one) is frequently targeted in DISTAL, as opposed to the inferior trunk often included in LVO trials.
He further noted that both the European Stroke Organisation (ESO) and American Heart Association (AHA) guidelines do not give a clear recommendation on whether or not to treat M2 occlusion, due to a “paucity of randomised controlled data”. In addition, as things stand, some 25% of patients in the DISTAL trial are enrolled with a PCA occlusion—a stroke type for which “virtually no” randomised data exist. Thus, Psychogios is “convinced the DISTAL trial will provide answers to an important clinical question”.
DISTAL trial will elucidate non-dominant M2, M3 and PCA occlusions but sparks debate over ‘true clinical question’
When you talk about distal occlusions, they are so different depending on the area and how distal they are.”
Tommy AnderssonMarios Psychogios
Following the recent addition of the EMBOGUARD balloon guide catheter (BGC) to the CERENOVUS STROKE SOLUTIONSi portfolio of devices, Demetrius K Lopes (Chicago, USA) discusses the significance of this latest tool when it comes to treating patients— offering his personal opinions and findings, experiences and perspective, as well as what these developments could mean for the future.
The brain controls our movements, holds our memories, and is the origin of our thoughts, emotions and language. But when an ischaemic stroke occurs, blood supply to part of the brain is interrupted or reduced, preventing brain tissue from getting oxygen and nutrients. Invaluable brain cells die within minutes.
This neurovascular disease is not only harmful but, unfortunately, common. Ischaemic stroke accounts for 85% of all strokes1 and, globally, one in four adults over the age of 25 will have a stroke in their lifetime.2 The impact of stroke can be short or long term, depending on which part of the brain is affected and how quickly it is treated. However, advancements in stroke research over the last decade have led to innovative and effective treatments, like mechanical thrombectomy, which is a minimally invasive procedure3 that offers positive benefits for patients after an ischaemic stroke—if applied in the first few hours after stroke onset.
The overall goal of thrombectomy procedures is to achieve a high first-pass recanalisation rate, which is defined as a complete or nearcomplete recanalisation (restoration of blood flow) with a single thrombectomy attempt.4 First-pass recanalisation is the procedural goal for the treatment of ischaemic stroke, as it helps patients experience the greatest benefits5 and may also be considered as a benchmark to measure the angiographic efficacy for thrombectomy devices.4
As the director of Cerebrovascular Surgery and the Comprehensive Stroke Program surgical director at Advocate Health—a health system that includes five comprehensive stroke centres—I have insight into vast procedural outcomes across the country. Across our system, strokes present within different age groups and patient populations, and with varying sets of difficulties. With so many variables, it is critically important that we choose the right tools to cover the full range of stroke situations—like the CERENOVUS STROKE SOLUTIONS portfolio.
Often, acute stroke is not a problem with a single solution. It can be difficult to predict, and it is important to have tools that are easy to use for every level of training, from the most senior physician to new attending. The CERENOVUS STROKE SOLUTIONS portfolio consists of the EMBOTRAP III revascularisation device, CEREBASE DA guide sheath, CERENOVUS large bore catheter, PROWLER EX microcatheter and, most recently, the EMBOGUARD BGCi to create a comprehensive package of devices.
When you mix and match other devices, there are often discrepancies in compatibility, which can cause lab confusion and treatment challenges that could account for access issues, and even waste valuable time. When devices are comprehensively designed for compatibility and support ease of use, the physician and the lab team may be more comfortable, which can lead to more efficiency in the lab.
My experiences with a comprehensive portfolio of solutions
CERENOVUS STROKE SOLUTIONS has a plugand-play approach to provide comprehensive usage that can address whatever problem I am presented with, especially with the latest addition of the EMBOGUARD BGC.
In the past, BGCs have not been the easiest solution to use or handle, but EMBOGUARD has changed how we are able to approach mechanical thrombectomy procedures.
It has the features and trackability you would expect from a non-balloon guide catheter with the benefits of flow arrest—when inflated, the EMBOGUARD catheter can block blood flow in a controlled manner. BGCs can also result in significantly reduced distal emboli to both affected and previously unaffected territories.6 EMBOGUARD’s excellent balance of trackability and supportii allow me to distally place the device, and keep it there.
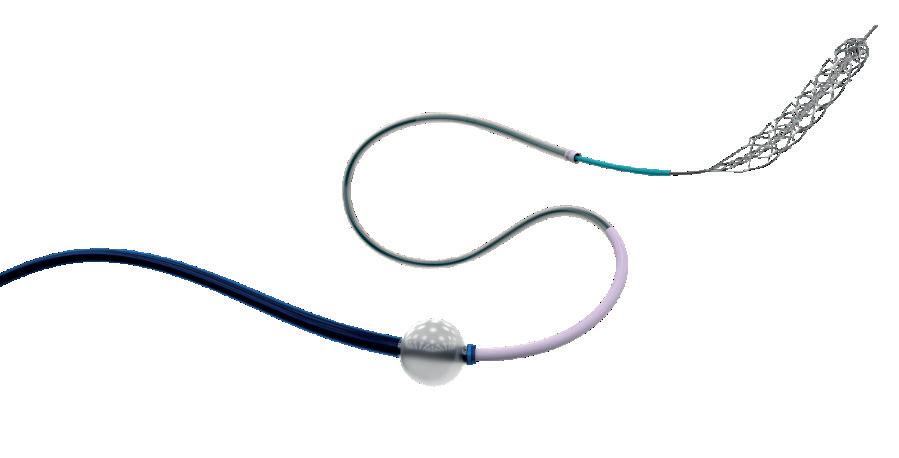
In my experience, its combined features have a positive impact on procedure quality and performance, and allow for variation in the procedure. I am able to perform procedures from thrombectomies, to carotid stenting, to tandem occlusions. Knowing I have the capabilities of a BGC available if needed provides

peace of mind that I can be ready for any ischaemic stroke procedure that requires the use of a BGC.
Clinical evidence has shown that use of a BGC can improve first-pass recanalisation and certain patient outcome measures, including greater odds of a final thrombolysis in cerebral infarction (TICI) score of 3iii (49.1% BGC vs 37.3% non-BGC), better clinical outcomes at 90 daysiv (modified Rankin Scale [mRS] score; 54.5% BGC vs 43.7% non-BGC), shorter procedure time and less adjunctive (supplemental) therapy needed.7,8,9
It is becoming clear that innovative developments, like the EMBOGUARD catheter, that work in tandem with a portfolio of comprehensive and compatible solutionsi will continue to gain traction in the stroke space, as the results speak for themselves. It is particularly important that we dismiss any preconceived notions we may have about BGCs and remain open-minded when it comes to new developments and continued innovation of these next-generation devices. When treating stroke, we want the latest and most effective solutions in order to be successful in caring for our patients. By embracing new innovations in stroke care and partnering with companies like CERENOVUS, who are making important impacts in the stroke space, you will see firsthand how industry is committed to driving strong outcomes for patients, therefore enabling better chances of recovery.
References:
1. “Ischaemic stroke”. Stroke Association. Stroke.org.uk. https://www. stroke.org.uk/what-is-stroke/types-of-stroke/ischaemic-stroke.
2. “Learn About Stroke”. World Stroke Organization. World-stroke.org. https://www.world-stroke.org/world-stroke-day-campaign/why-strokematters/learn-about-stroke.
3. “Mechanical Thrombectomy for Acute Stroke”. The Society of Vascular and Interventional Neurology (SVIN) and Mission Thrombectomy 2020+. 10 October 2020. https://www.svin.org/files/Final_formatted_SVIN_White_ paper_2020_updated_references(1).pdf.
4. Zaidat O O, Ribo M, Mattle H P et al. Health economic impact of first-pass success among patients with acute ischemic stroke treated with mechanical thrombectomy: a United States and European perspective. J Neurointerv Surg. 2021; 13(12): 1117–23. DOI: 10.1136/neurintsurg-2020-016930.
5. Jang K M, Choi H H, Nam T K et al. Clinical outcomes of first-pass effect after mechanical thrombectomy for acute ischemic stroke: A systematic review and meta-analysis. Clin Neurol Neurosurg. 2021; 211: 107030. DOI: 10.1016/j.clineuro.2021.107030.
6. Chueh J Y, Kang D H, Kim B M et al. Role of Balloon Guide Catheter in Modern Endovascular Thrombectomy. J Korean Neurosurg Soc. 2020; 63(1): 14–25. DOI: 10.3340/jkns.2019.0114.
7. Brinjikji W, Starke R M, Murad M H et al. Impact of balloon guide catheter on technical and clinical outcomes: a systematic review and meta-analysis. J Neurointerv Surg. 2018; 10(4): 335–9. DOI: 10.1136/ neurintsurg-2017-013179.
8. Pederson J M, Reierson N L, Hardy N et al. Comparison of Balloon Guide Catheters and Standard Guide Catheters for Acute Ischemic Stroke: A Systematic Review and Meta-Analysis. World Neurosurg. 2021; 154: 144–53. DOI: 10.1016/j.wneu.2021.07.034.
9. Nikoubashman O, Dekeyzer S, Riabikin A et al. True First-Pass Effect. First-Pass Complete Reperfusion Improves Clinical Outcome in Thrombectomy Stroke Patients. Stroke. 2019; 50(8): 2140–6. DOI: 10.1161/STROKEAHA.119.025148.
Demetrius K Lopes is a neurosurgeon at Advocate Health in Chicago, USA, where he is the Comprehensive Stroke Program surgical director, as well as the director of Cerebrovascular Surgery.
CERENOVUS Stroke Solutions featuring EMBOGUARD balloon guide catheter
i. EMBOGUARD balloon guide catheter and CEREBASE DA guide sheat and Vecta 71 catheters in a benchtop study. Better durability than React 68 catheter in a benchtop study. The third-party trademarks used herein are the properties of their respective owners. iii. Total restoration of pre-stroke blood flow. iv. A six-point disability scale to measure outcomes in stroke patients.
The Squid liquid embolic agent (Balt) has been deemed safe and effective in treating high-grade dural arteriovenous fistulas (DAVFs), and serves to expand the armamentarium for neurointerventionists treating DAVFs and other intracranial vascular malformations.
Markus Möhlenbruch (Heidelberg University Hospital, Heidelberg, Germany) and colleagues recently published the results from a prospective, observational multicentre study of this endovascular embolisation treatment in the Journal of NeuroInterventional Surgery.

“Squid is a promising liquid embolic agent for the embolisation of high-grade DAVFs,” they write. “In this prospective, multicentre study, embolisation using Squid was associated with an acceptable complication rate and a high occlusion rate.”
The study’s authors begin their report by noting that endovascular embolisation became established as a feasible treatment option for cranial DAVFs— primarily following the introduction of the Onyx liquid embolic agent (ev3/Medtronic) in the mid-2000s— and that newer agents like the novel, non-adhesive,
precipitating Squid have aimed to overcome existing shortcomings and further improve the success of DAVF embolisation.
“The two major innovations of the new liquid embolic, Squid, in comparison with Onyx, are the size of the tantalum grains, which are admixed to the agent, and the availability of the low-viscosity version, Squid 12,” they write, but note that all other components of the two agents are identical.
As such, Möhlenbruch and colleagues set out to assess the safety, efficacy and short-term outcomes of DAVF treatment with this liquid embolic via the prospective, observational LIQUID study, which was conducted across eight German neurovascular centres. The primary outcome measures were safety—defined as morbidity and mortality—and the occlusion rate 90–180 days after treatment.
A total of 53 patients (mean age=59.8 years, 22.6% female) with high-grade (Cognard type ≥3) DAVFs were treated with the Squid liquid embolic agent across 55 treatment sessions. Of the included DAVFs, 56.6% were Cognard type III, 41.5% were type IV, and 18.9% were ruptured, the authors report. The Squid 18 was used in 83.6% of treatments while the Squid 12 was deployed in 32.7%.
Outlining results from the LIQUID study, Möhlenbruch and colleagues state that the overall rate of intraprocedural or postprocedural adverse events was 18.2%, and procedure-related adverse events resulting in permanent morbidity were observed in 3.6% of cases. One patient (1.8%) died unrelated to the procedure due to pulmonary embolism.
In addition, the immediate complete occlusion rate using Squid only was 92.5%. In one patient, after partial embolisation with Squid, transvenous coiling was performed to achieve complete occlusion, resulting in an overall, immediate complete occlusion rate of
A systematic review and meta-analysis of the “scarce” existing literature has adjudged flow diversion with a coated stent plus single antiplatelet therapy (SAPT) to be “feasible” in the treatment of ruptured intracranial aneurysms, despite thromboembolic complications occurring in a “significant number of patients”— all of which were associated with aspirin-based SAPT.
THESE FINDINGS HAVE BEEN published in World Neurosurgery by Matthias Gawlitza (University Hospital Leipzig, Leipzig, Germany) and colleagues, who also note a low rate of haemorrhagic complications across the patient cohort involved.
At the outset of their report, the authors state that, owing to the increased risk of major bleeding events in patients with ruptured aneurysms who undergo flow diversion alongside dual antiplatelet therapy (DAPT), surfacemodified flow diverters that can be implanted with SAPT would represent “a major step forward” in this setting.
“Flow diverters coated with antithrombogenic substances were recently introduced and have shown encouraging results in the preclinical setting,” Gawlitza et al further note.
“Our aim was to analyse their clinical application in patients with ruptured intracranial aneurysms using SAPT.”
The authors highlight three surfacemodified or ‘coated’ flow diverters designed to reduce thrombogenicity that
have gained CE-mark clearance, and are currently under “intensive clinical and scientific investigation”—the Pipeline Embolisation Device (PED) Shield (Medtronic), and the P48 hydrophilic coating (HPC) and P64 HPC flowmodulation devices (Phenox/Wallaby).
“Hydrophilic polymer and phosphorylcholine coating for flow diverters are major technical advances with encouraging preclinical data proving reduced thrombus formation, both in vitro and in vivo,” they add.
With these devices as their central focus, Gawlitza et al set out to assess the safety and efficacy of flow diverters with antithrombogenic coating in the treatment of ruptured aneurysms under SAPT. To do this, they performed a Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA)-compliant systematic review and meta-analysis covering three major databases up to March 2022.
Random-effects analysis of proportions was used to pool safety outcomes—including haemorrhagic,
94.3%. The final complete occlusion rate at 90–180 days was 93.2%, the authors add, noting that this core laboratory-rated rate of occlusion is slightly higher than previously published occlusion rates on endovascular DAVF embolisation. Regarding functional outcomes, Möhlenbruch and colleagues report that—after a mean follow-up of 5.5 months—the modified Rankin Scale (mRS) score was stable or improved 93% of the time. However, a worsening mRS score was deemed to have been related to the procedure in one patient (1.8%).
“Squid, which features several modifications compared with the established agent, Onyx, expands the armamentarium of liquid embolic agents for the treatment of DAVFs,” they continue.
Despite this, the authors also point out that, even with these potential advantages in mind, impedance of a plug formation; early distal embolisation; and a potentially higher ability to diffuse into collateral meningeal arteries, constitute three major drawbacks associated with embolisation utilising low-viscosity agents. And, while none were directly observed in the LIQUID study, these drawbacks should be known and considered by interventionists using Squid 12.
Möhlenbruch and colleagues go on to briefly acknowledge their study’s limitations, including a relatively low number of patients, the fact that 9.3% of patients did not have data available for follow-up, and the lack of a control group involving other embolic agents. As such, while they claim that this is the largest study reporting on DAVF embolisation using Squid to date—and the first ever prospective study on the endovascular treatment of high-grade DAVFs in “the era of liquid embolic agents”—the scope for comparisons between Squid and other agents is limited.
thromboembolic and overall complications—while studies were also tested for publication bias and heterogeneity, the researchers report.
Five studies including 43 patients with a total of 46 intracranial aneurysms were identified and deemed eligible for inclusion. The authors also note that more than one stent was implanted in 16% of patients, and additional coil embolisation was performed in 53.8%. SAPT with one of several different acetylsalicylic acid regimens was used in 86% of patients, while antiplatelet protocols were variable overall.
The pooled risks of thromboembolic (23.9%), haemorrhagic (9.4%) and overall (28.3%) complications were calculated “in the absence of publication bias, with low-to-moderate study heterogeneity measures”, Gawlitza et al report. All complications occurred in patients under SAPT with acetylsalicylic acid (ASA; also known as aspirin). Adequate aneurysm occlusion was described in 65.5% of patients in the
study, with moderate heterogeneity being observed in few retrospective observational studies, encompassing “a limited number of patients” treated with variable SAPT regimens.
“Flow diversion for ruptured aneurysms under SAPT using stents with hydrophilic polymer and phosphorylcholine coating is feasible, and is associated with low rates of haemorrhagic complications,” Gawlitza et al conclude. “However, thromboembolic complications are frequent and may limit the use of this technique to selected cases.
The literature is scarce, with few heterogeneous studies encompassing a limited number of patients treated with highly variable SAPT regimens. [But], although more and better data are necessary to conclude on the appropriate medication, it should be noted that all reported thromboembolic complications occurred under SAPT with ASA, which therefore should be used with caution as [the] primary SAPT agent.”
A transmural approach for accessing the perivascular tissues of the cervical carotid artery has been deemed safe following initial evaluations in a swine model.
GEOFFREY COLBY, WI JIN KIM and Milan Samarage (all University of California Los Angeles [UCLA], Los Angeles, USA), and colleagues, have published findings from their safety assessment in the Journal of NeuroInterventional Surgery (JNIS) concluding that this endovascular technique “represents a novel approach to various tissues in close proximity to the cervical and cranial vasculature”.
“Recent advances in endovascular devices have allowed access and targeting of perivascular tissues of the peripheral circulation,” the authors state, outlining the backdrop to their research. “The perivascular tissues of the cervical and cranial circulations have many important structures of
clinical significance, yet the feasibility and safety of such an approach has not been demonstrated.”
As such, they set out to evaluate the safety of a novel endovascular transmural approach to target the perivascular tissues of the common carotid artery in swine.
Initially, a micro-infusion device was positioned in the carotid arteries of three Yorkshire swine—across a total of six carotid arteries—with each carotid artery being punctured 10 times in the same location to gain access to the perivascular tissues. Digital subtraction angiography was used to evaluate vessel injury or contrast extravasation, while magnetic resonance imaging (MRI) and MR angiography were
used to evaluate evidence of cerebral ischaemia or vessel injury. Writing in JNIS, the authors further note that post-mortem tissue analysis was performed to assess for extravascular haematoma/intravascular dissection.
“None of the tested carotid arteries showed evidence of vessel injury (dissection or perforation) or intravascular thrombosis,” they state, reporting the results of their study. “MRI performed after repeated puncture was negative for neck haematoma and brain ischaemia. Post-mortem tissue analysis of the carotid arteries showed mild adventitial staining with blood, but without associated haematoma and without vessel dissection.”
This led the researchers to conclude that the endovascular transmural
Physicians in the USA have published details of—to their knowledge—the “first reported use” of the Indigo aspiration system (Penumbra) to treat cerebral venous sinus thrombosis (CVST) via endovascular thrombectomy. The treated patient underwent successful partial recanalisation of the superior sagittal sinus (SSS) and bilateral transverse sinuses (TS), and experienced improved outcomes, they state.

Writing in the journal Interventional Neuroradiology, Tareq Kass-Hout (University of Chicago, Chicago, USA) and colleagues note that CVST is an uncommon cause of stroke that can be difficult to treat and potentially “devastating”. Systemic anticoagulation is generally considered the first-line therapy for CVST, they add, but it may prove “insufficient” in cases of extensive thrombosis.
In these instances, EVT is often utilised to prevent the progression of ischaemic and/or haemorrhagic brain injury. However, according to the authors, while EVT techniques have evolved over time, “high-quality evidence for the efficacy and safety of these techniques for CVST is still lacking”.
“We present a 35-year-old male with ulcerative colitis initially admitted for a flare-up who then presented with altered mental status and was found to have extensive cerebral venous sinus thrombosis on computed tomography [CT] imaging,” Kass-Hout and colleagues write.
Initially, the patient underwent continuous lowdose heparin infusion for three days. However, this yielded “no improvement” and he was later intubated for airway protection. Owing to evidence of complete occlusion of the bilateral TS—and due to “persistently poor exams on systemic anticoagulation with concern for elevated intracranial pressure”—the decision was made to use EVT.
Relaying details of this procedure, the operators state that they gained access through the patient’s right femoral artery. Upon visualising the right internal carotid artery (ICA) view, there was evidence of “extremely slow perfusion”, with no significant
drainage through the dural sinuses, as well as complete occlusion of the distal portion of the SSS and the bilateral TS.
“Here, the decision was made to proceed with mechanical thrombectomy of the venous sinuses,” Kass-Hout and colleagues report.
A follow-up angiographic run revealed “significant thrombosis” of the right internal jugular (IJ) vein with “many completely occlusive thrombi”. Complete occlusion of the bilateral TS was also confirmed at this stage, and the intervention was then initiated, the authors add.
They deployed a 200cm Aristotle guidewire (Scientia Vascular) into a 160cm Zoom 35 catheter (Imperative Care), which was then advanced within the CAT12 large-bore aspiration catheter (Penumbra) and navigated across the occlusion to the SSS. Following multiple aspiration attempts, CAT8 and CAT7 catheters were advanced into the thrombus more anteriorly in the SSS and aspiration attempts were performed in the SSS with a separator device (all Penumbra).
At this stage, “evidence of partial recanalisation of the SSS and full recanalisation with normalised flow in [the] bilateral TS was seen”, Kass-Hout and colleagues note. And, while several additional thrombectomy attempts were made using the EmboTrap stent retriever (Cerenovus) plus aspiration, no further significant recanalisation was observed, and the operators decided to stop the intervention given “significant thrombus removal” had already been achieved.
approach they assessed appears to be safe as a novel way of accessing the carotid artery perivascular tissues.
“The novel endovascular transmural approach represents a means of targeting cervical and cranial perivascular tissues that was not previously possible,” Colby stated, speaking to NeuroNews. “This opens a new realm for minimally invasive delivery of therapeutics for inhibition, activation, or modulation, of numerous important anatomical structures, such as components of the autonomic nervous system. Future clinical applications are broad, but early use may involve conditions with hyperactivity of the sympathetic nervous system, such as cerebral vasospasm that occurs after rupture of a brain aneurysm or traumatic brain injury.”
No thrombolytics were used during the procedure— nor additional heparin—and no procedure-related complications occurred.
The authors report that the patient had a prolonged recovery and a course in the neuro-critical care unit totalling six weeks. Repeat CT venography of the head, performed four weeks after intervention, revealed a decreased SSS burden of thrombus with otherwise patent dural venous sinuses and deep cerebral venous system. The patient was deemed neurologically stable and discharged to a rehabilitation centre. Approximately five months post-discharge, he was reportedly able to track people with his eyes, respond with smiles when shown pictures, and consistently follow commands with his left side, but remains hemiparetic on his right side with no apparent improvement in strength levels.
“This intervention prevented permanent brain injury, providing a better neurological outcome for this patient’s situation,” Kass-Hout and colleagues add.
Discussing the wider implications of this procedure, they also note that several past case reports have demonstrated various methods for treating CVST via EVT—including use of the Penumbra system in combination with urokinase or alteplase infusions; balloon angioplasty; and the Solitaire flowrestoration device (Medtronic).
“However, a single method has not been established as the most effective for CVST,” the authors continue. “The optimal EVT method for CVST treatment is not yet known, and the PIAS [Penumbra Indigo aspiration system] should be considered as a potential candidate, as demonstrated in our case.”
After highlighting the CAT12 catheter’s design, which helped to provide much-needed trackability and torqueability in a patient with tortuous venous vessels, and the Lightning intelligent aspiration technology’s (Penumbra) “extremely useful” ability to prevent significant blood loss, Kass-Hout and colleagues state that the Indigo aspiration system’s applicability in treating CVST “should be further explored”.
Tareq Kass-Hout
The novel endovascular transmural approach represents a means of targeting cervical and cranial perivascular tissues that was not previously possible.”
Geoffrey Colby
in stroke care.
“Only alteplase is licensed for the treatment of ischaemic stroke,” the alert stated. “Stroke teams may also have experience of using tenecteplase from participation in clinical trials, though this would be an unlicensed use. Mechanical thrombectomy is also used to treat some patients with acute ischaemic stroke but should be used

drug “must be reduced by at least 35% nationally, or tenecteplase stock will be exhausted in Australia by the end of 2022”, and advised implementing similar approaches to its European equivalents—including prioritisation of tenecteplase for pre-hospital thrombolysis; increased use of alteplase in metropolitan and larger regional hospitals to conserve tenecteplase; and a 12-month extension to the shelf-life of
In July 2022, the ESO released the first of three letters pertaining to current difficulties, describing what caused them and announcing the establishment of a thrombolysis taskforce. It also noted that the situation “may not be the same in all second letter, dated September were anticipated to last into 2024—but being taken by BI to tackle the issue, Actilyse versus Metalyse (tenecteplase); introducing measures to reduce wasted alteplase while maintaining a consistent total production quantity; working with EU health authorities towards a shelftenecteplase; and establishing a fair and equitable allocation process, worldwide,
As per the results of a small-scale
countries, the ESO also concluded in September that, “overall, the situation is regarded as stable and action plans have been installed in most participating countries”, before conceding that there are still “some countries where there is insufficient communication and supply”.
In early 2023, the ESO published its expedited recommendation on tenecteplase for acute ischaemic stroke in the European Stroke Journal Following the recent emergence of data from four randomised controlled trials comparing IVT with alteplase versus tenecteplase, the ESO sought to update its previous guidelines “in order to reconsider the place of intravenous tenecteplase in patients with acute ischaemic stroke eligible for IVT”. A ‘plain-language summary’ of these recommendations lists five key points regarding tenecteplase for this indication:
1. Tenecteplase at a dose of 0.25mg/kg is equally as safe and effective as alteplase for the treatment of patients presenting with stroke symptoms within 4.5 hours.
2. Tenecteplase should not be used at a higher dose for stroke treatment.
3. Tenecteplase at a dose of 0.25mg/kg may be better than alteplase for patients treated in a specialised ambulance capable of performing brain imaging.
4. Patients with stroke due to a blood clot in a large artery in the brain should be treated with tenecteplase at a dose of 0.25mg/kg, rather than alteplase, prior to receiving a thrombectomy.
5. For patients becoming aware of stroke symptoms on awakening from sleep or those presenting without information on the time of symptom onset, clot-busting medications can only be given if access to special brain imaging is available. In this setting, we do not know whether tenecteplase can be used instead of alteplase. However, the opinion of the experts writing the current document is that tenecteplase at a dose of 0.25mg/kg may be used instead of alteplase in patients becoming aware of stroke symptoms on awakening from sleep, or those presenting without information on the time of symptom onset, provided they meet certain criteria on special brain imaging.
AN INTERNATIONAL STUDY
by Leonard Yeo (National University Hospital, Singapore) and colleagues has found that the presence of atrial fibrillation does not modify the treatment effect of bridging intravenous thrombolysis (IVT) in ischaemic stroke patients undergoing a thrombectomy procedure.

The results of this research are published in the Journal of NeuroInterventional Surgery (JNIS)
Yeo and colleagues initially note that the role of IVT prior to endovascular thrombectomy in acute ischaemic stroke patients remains a matter of debate, and that atrial fibrillation-associated strokes may be associated with a reduced treatment effect from IVT.
As such, they conducted a retrospective, multicentre, international cohort study to compare the effects of bridging IVT in atrial fibrillation versus nonatrial fibrillation patients. More specifically, the cohort included anterior circulation large vessel occlusion (LVO) acute ischaemic stroke patients receiving thrombectomy alone, or bridging IVT plus thrombectomy, within six hours of symptom onset.
According to Yeo and colleagues, the primary
outcome for their study was a good functional outcome defined as modified Rankin Scale (mRS) score of 0–2 at 90 days. Secondary outcomes were successful reperfusion—defined as an expanded thrombolysis in cerebral infarction (eTICI) grading of ≥2b flow—as well as symptomatic intracerebral haemorrhage (sICH) and inhospital mortality.
A total of 705 patients (mean age 68.6 years, 53.9% male) were included in the analysis—314 of whom had atrial fibrillation present and 391 of whom did not.
The odds of a good functional outcome with bridging IVT were higher in the non-atrial fibrillation group (adjusted odds ratio [aOR] 2.28) compared with the atrial fibrillation subgroups (aOR 1.89), the authors detail.
“However, this did not constitute a significant effect
Intravenous thrombolysis (IVT) prior to a mechanical thrombectomy procedure could result in better functional outcomes than thrombectomy alone in stroke patients with M2 occlusions, as per a retrospective analysis derived from the Endovascular Treatment in Ischemic Stroke (ETIS) registry.
Outlining these findings in the Journal of NeuroInterventional Surgery (JNIS), a research team including corresponding author Gaultier Marnat (Centre Hospitalier Universitaire [CHU] de Bordeaux, Bordeaux, France) notes that—alongside the fact that IVT was not associated with an increased rate of haemorrhagic or procedural complications—their results suggest a benefit of IVT in M2 occlusion patients undergoing a thrombectomy procedure.
The authors initially posit that IVT in patients treated with mechanical thrombectomy for proximal occlusions has “recently been questioned” through randomised trials. However, they continue, few patients with M2 segment occlusions—which are somewhat controversial, as their categorisation as ‘proximal’ or ‘distal’ is subject to continued debate—were included in these trials.
As such, Marnat and colleagues set out to investigate the influence of prior IVT for patients presenting with M2 occlusions treated with mechanical thrombectomy, as
compared to thrombectomy alone, via a retrospective analysis of the multicentre, observational ETIS registry. The ETIS registry includes prospective data from 29 of the 38 thrombectomy-capable centres in France, and more than 15,000 realworld stroke patients.
Writing in JNIS, Marnat and colleagues report that data from consecutive patients treated with thrombectomy for M2 occlusions between January 2015 and January 2022 at a total of 26 comprehensive stroke centres were analysed.
The primary endpoint of their analysis was a 90-day modified Rankin Scale (mRS) score of 0–2. Outcomes were compared using propensity score approaches, and sensitivity analyses were performed in relevant patient subgroups, they add.
Among 1,132 patients with M2 occlusions treated with mechanical thrombectomy, 570 received prior IVT—leaving 562 who did not receive prior IVT, with the two groups being comparable after a
modification by the presence of atrial fibrillation on bridging IVT,” Yeo and colleagues continue, noting an interaction aOR of 0.12. “The rates of successful reperfusion, sICH and mortality were similar between bridging IVT and EVT [endovascular therapy] for both atrial fibrillation and non-atrial fibrillation patients.”
Based on this finding, the authors conclude in their JNIS report that the presence of atrial fibrillation did not modify the treatment effect of bridging IVT. However, they add that further individual patient data meta-analyses of randomised trials “may shed light on the comparative efficacy of bridging IVT in atrial fibrillation versus non-atrial fibrillation LVO strokes”.
propensity analysis.
The rate of favourable functional outcome was “significantly higher” in the IVT-plus-thrombectomy group (59.8%) compared with the thrombectomy-alone group (44.7%). In addition, haemorrhagic and procedural complications were similar in both groups.
And, in a sensitivity analysis excluding patients with anticoagulation treatment, favourable recanalisation was more frequent in the IVT-plusthrombectomy group.
Additional sensitivity analyses that focused on ‘mothership’ patients, and patients treated within 4.5 hours from symptom onset, also revealed similar safety and efficacy profiles associated with IVT prior to thrombectomy. Marnat and colleagues therefore conclude that, in cases of M2 occlusions, prior IVT combined with mechanical thrombectomy resulted in better functional outcomes than thrombectomy alone, without increasing the rate of haemorrhagic or procedural complications.
1,132 M2 occlusion patients
570
562 received IVT plus thrombectomy received thrombectomy only
59.8% 44.7%
The rates of successful reperfusion, sICH and mortality were similar between bridging IVT and endovascular therapy for both atrial fibrillation and non-atrial fibrillation patients.”Leonard Yeo
As medical accolades go, performing the world’s first robot-assisted neurointerventional procedure—a feat that Vitor Mendes Pereira and his team achieved back in 2019—is something any physician would be proud of. But, as a professor of Surgery and Medical Imaging at the University of Toronto, director of Endovascular Research and Innovation in the Department of Surgery at St Michael’s Hospital, and co-lead of the RADIS Lab (Toronto, Canada), this is just a snapshot of the pioneering work Pereira has done to help drive the neurointerventional space forward over the past decade. Here, he discusses these efforts with NeuroNews, outlines his vision for the future of stroke care and draws on personal experiences to advise aspiring neurointerventionists.
What initially attracted you to medicine, and neurointervention specifically?
I grew up on an island in the north-east of Brazil called São Luís do Maranhão. As a kid, I was always fascinated by technology and wanted to become an engineer. During my last year of high school, two events changed my life: I started dating Andrea, the love of my life, and my father was diagnosed with prostate cancer. I put my career plans on hold to help take care of my father, run our family’s farm, and stay close to Andrea. Supporting my father through his medical journey made me realise that if he had been managed appropriately, he likely would have survived his cancer. This realisation left me feeling helpless, so I decided to change my career to pursue medicine.
During my time in medical school at the Federal University of Maranhão (São Luís, Brazil), I was fascinated by the brain, and the precision of neurological examinations. I started shadowing a neurosurgeon, Periguari Lucena, and I knew from the first patient I helped treat that I would pursue neurosurgery. I did my neurosurgery residency at São Paulo State University (Botucatu, Brazil) and, during that time, a vascular neurologist, Cesar Raffin, turned my attention to stroke patients—while my preceptor, Marco Zanini, taught me all about brain aneurysms. I also did rotations in neurointervention under the supervision of Guilherme Caldas and his team and, after learning angiography techniques and the principles of intervention, I realised that was what I wanted to do!
In 2005, I started the International Diploma in Neurovascular Diseases—coordinated by Pierre Lasjaunias—which was held in Thailand over two years. Shortly after, Professor Lasjaunias accepted me for a fellowship at the Bicêtre Hospital (Paris, France). He was a thoughtful and caring mentor who inspired me to “be precise”, by mastering neuroangiographic anatomy, and to understand embryology, disease pathomechanisms and genetics. Bicêtre was a great experience and, at the end of the fellowship, Professor Lasjaunias suggested that I continue my training with Jacques Moret—his friend, and one of the most talented neurointerventionists we had seen in our field.
In 2007–2008, I started the second year of my fellowship at the Rothschild Foundation, also in Paris, under the supervision of Professor Moret. He is highly technically skilled but also has a deep knowledge of anatomy. He is always thinking beyond, inspiring me to master procedural techniques and medical device use, and look for perfection from the planning to the execution of a treatment strategy. Working with his dream team—Charbel Mounayer, Laurent Spelle, Michel Piotin and Raphael Blanc—I have shaped my practice, and made friends for life. From time to time, I am still astonished remembering the day that Professor
Lasjaunias called Professor Moret to introduce me for that fellowship position. I am blessed to have been mentored by two brilliant minds that helped to transform our field.
What is your proudest achievement to date in the neurointerventional space?
My greatest achievement is the creation of the RADIS Lab, a translational lab performing cutting-edge research, and applying the latest technological and scientific innovations to treat vascular diseases of the brain. A key strength of our lab is leveraging the close relationship between clinicians and scientists—such as my lab co-lead Nicole Cancelliere, a radiation technologist and master in neurosciences. We are leading the way in areas like robotics, artificial intelligence (AI), procedure simulation and new imaging technologies. Among our most pioneering and successful projects are the world’s first robotic aneurysm treatment; high-frequency optical coherence tomography (HF-OCT) imaging of the intracranial anterior circulation with a dedicated neuroimaging probe; and our lab’s input into the development of new devices, such as the Surpass Evolve flow diverter (Stryker) and the BossStent venous stenosis treatment device (Sonorous).
You recently became a LINNC course director—how did that happen, and what are your goals in this position?
The LINNC conferences, created by Professors Moret and Spelle, are the most comprehensive, continuous educational platforms in neurointervention. These were always my favourite meetings, where I would look for new treatment strategies and tips to better perform complex procedures. I have been part of LINNC Paris since I was a fellow, and—from 2011—have managed a live broadcasting centre from Geneva and, later, Toronto. In 2022, 25 years after the first meeting, they have invited me to become a course director. I am very honoured, but am aware that these are big shoes to fill. I am motivated to maintain LINNC’s innovative format by contributing my research background and experience with digital technologies.
Thanks to advances in mechanical thrombectomy and innovative trial designs, we have been winning every single battle in the treatment of acute stroke—and it should be no different, if we consider that removing a clot in a brain vessel is one of the most powerful treatments in medicine. In the short term, next frontiers will be to conquer distal strokes, and improve outcomes with neuroprotection. The enhancement of cone-beam imaging will also allow ‘direct-toangio’ approaches and workflow improvements. In the long term, I foresee remote robotic treatments being a gamechanger, not only offering access to care for patients in remote communities, but potentially connecting centres and redesigning stroke care models in different geographies as well.
Thanks to advances in mechanical thrombectomy and innovative trial designs, we have been winning every single battle in the treatment of acute stroke.”
Surgeon/scientist and director of Endovascular Research and Innovation, Division of Neurosurgery, Department of Surgery, St Michael’s Hospital, Unity Health Network (Toronto, Canada)
Schroeder Chair in Advanced Neurovascular Interventions and professor in the Division of Neurosurgery, Department of Surgery, University of Toronto

Professor, Department of Medical Imaging, University of Toronto
2006–2008: Clinical fellowship in Interventional Neuroradiology, Department of Interventional Neuroradiology, Bicêtre Hospital/ Rothschild Foundation (Paris, France)
2005–2006: International master in Neurovascular Diseases (professional MSc), Faculté de Médecine de l’Université Paris XI (Paris, France)
2002–2006: Residency programme
Which three novel technologies do you feel will have a significant, lasting impact in neurointerventional surgery?
In the future, I envision us doing neurointerventions like a pilot flies a plane—safe and sound, using technology to improve diagnosis, precision, and human performance. The three technologies I believe will contribute to this future are robotics, AI and neurodedicated intravascular imaging. Alone or combined, they may improve the accuracy of neurovascular disease diagnoses, expand our understanding in different dimensions, and facilitate the execution of procedures with optimised control and automation. And, why should we not also use simulations— like pilots do—to gain or maintain competence in certain surgical procedures? Patient-specific surgical simulation is a dream of mine that will certainly become a reality as other technologies progress.
What advice would you give to people embarking on a career in this space?
They are lucky to be starting in neurointervention these days, as the space has advanced so much and will continue evolving. I advise them to know what they are dealing with; know their imaging systems and tools to deliver care; and ‘balance the consequences’. A strong understanding of neuroangiographic anatomy is key for good decision-making and therapeutic planning. I would recommend starting with anatomy review papers before going to the classic textbooks, as well as the neurorangio.org website. I also recommend utilising the thesmartdevice.com website and making it your ‘open page’ in the angio suite. Treatment strategies require experience as well, and a good way to get it is to attend educational programmes, fellows courses and conferences like LINNC, SLICE and the WLNC. Case discussions in forums can be very informative in many aspects. Recently, I came across a new platform called Global Intervention—a smartphone application enabling case sharing, discussions and a personal case database. We can learn a lot from each other, and from the successes and mistakes of others.
What are your interests outside of the field of medicine?
I like to spend time with my wife Andrea and my three kids: Alice, Pedro and Sarah. We love to travel, and explore the world and nature together. I also love to explore new restaurants with them. We like to cook together and our favourite dishes to prepare as a family are Beef Wellington, wooden-plate grilled salmon, and Brazilian barbecue with special wagyu beef cuts. We like to ski in the winter, and bike and swim during summertime. I am learning to play the cello and starting Mandarin classes with my daughter. Recently, I have been reading the Bible, and Christian books, to understand more about God and his plans for me, my career and my family.
in Neurosurgery, Clinical University Hospital of São Paulo State University (Botucatu, Brazil)
1996–2001: Bachelor in medicine, Medical School, Federal University of Maranhão (São Luís, Brazil)
Honours (selected)
Co-lead and scientist, RADIS Lab
2021: Odette award for Health Systems Innovation, Angels Den
2014: ESNR prize in honour of Rene Dinjian
2012: Peter Huber prize
More than 300 peerreviewed publications

A systematic review and meta-analysis have demonstrated “convincing evidence” that sex differences exist in carotid atherosclerosis, with all types of plaque features— including those relating to size, composition, and morphology—found to be either larger or more common in men than in women.
“Our results highlight that sex is an important variable to include in both study design and clinical decision-making,” the authors, led by Dianne van Dam-Nolen (Erasmus University Medical Center, Rotterdam, The Netherlands), write in the journal Stroke. “Further investigation of sexspecific stroke risks with regard to plaque composition is warranted.”
Over the past few decades, several individual studies on sex differences in carotid atherosclerosis have been performed, covering a wide range of plaque characteristics and including different populations, van Dam-Nolen et al state. In addition to summarising previously reported results on sex differences in this space, the researchers also sought to “present a roadmap explaining next steps needed for implementing this knowledge in clinical practice”. They began by systematically searching PubMed, Embase, Web of Science, Cochrane Central and Google Scholar for eligible studies, including both male and female participants, and reporting the prevalence of imaging characteristics of carotid atherosclerosis. The eligible studies were then meta-analysed. Van Dam-Nolen et al prespecified which imaging modalities had to be used per plaque characteristic and excluded ultrasonography.
Screening of more than 1,000 unique citations, based on the inclusion criteria, led to 42 articles ultimately being included in the final meta-analyses.
Six of these were included in a meta-analysis on the relationship between sex and atherosclerotic plaque size. All three of the characteristics used to measure plaque size—maximum wall thickness (1D size), wall area (2D size), and wall volume (3D size)—were more likely to be larger in men than in women, van Dam-Nolen et al report. However, conversely, the normalised wall index, which accounts for the total vessel size, did not statistically significantly differ between male and female participants, which the researchers describe as “surprising”, and possibly indicative of sex differences in plaque size being driven by contrasting vessel sizes.
In addition, analysing three of the studies further regarding the degree of stenosis, the authors found no statistically significant sex difference for stenosis of 50–69%, although high-grade stenosis of 70–99% was more often seen in men than in women.
Meta-analyses relating to plaque composition examined the presence of calcifications, lipid-rich necrotic core (LRNC), and intraplaque haemorrhage (IPH), and found a higher prevalence in men versus women across all three components. Expounding briefly on their calcification findings, van DamNolen et al report statistically significant differences between men and women for the presence and amount of carotid calcifications, but not in terms of
A prospective study has demonstrated the potential feasibility, applicability and accuracy held by artificial intelligence (AI) in the detection of carotid artery disease on greyscale static duplex ultrasound imaging. This is the conclusion reached by Ali Kordzadeh (Faculty of Science and Engineering, Anglia Ruskin University, Chelmsford, UK) and colleagues in the journal Vascular.
“THIS NETWORK HAS THE potential to be used as a standalone software or to be embedded in any DUS [duplex ultrasound] machine,” they add. “This can enhance carotid artery disease recognition with limited or no vascular experience, or serve as a stratification tool for tertiary referral, further imaging and overall management.”
To evaluate the feasibility, applicability and accuracy of AI in the detection of normal versus carotid artery disease through greyscale static duplex ultrasound images, Kordzadeh et al conducted a prospective image acquisition of individuals undergoing duplex
sonography for suspected carotid artery disease at a single hospital (Broomfield Hospital, Mid and South Essex NHS Foundation Trust, Chelmsford, UK).
A total of 156 images of normal and stenotic carotid arteries—based on North American Symptomatic Carotid Endarterectomy Trial (NASCET) criteria—were evaluated using geometry group network based on convolutional neural network (CNN) architecture. Outcomes were reported based on sensitivity, specificity and accuracy of the AI network for detecting normal versus stenotic carotid arteries, as well as various categories of carotid artery stenosis.
Detailing their results, Kordzadeh et
calcification percentage i.e. the amount of calcification relative to the total plaque volume.
“Furthermore, we found more pronounced sex differences for LRNC in symptomatic as opposed to asymptomatic participants,” they add.
Five studies were also included in the metaanalysis of the relationship between sex and plaque morphology, with the presence of ulceration and the presence of a thin-or-ruptured fibrous cap both being higher in men.
In their report, the authors highlight multiple limitations of their analysis that “deserve comment”, including moderate-to-high heterogeneity among the included studies, as well as the fact it was not possible to adjust for potential confounders on the relationship between sex and carotid atherosclerosis.
“The found sex differences in carotid atherosclerosis are of clinically significant importance, since the composition of plaque affects the risk of (recurrent) stroke,” van Dam-Nolen et al conclude. “Previous studies have shown that especially IPH contributes to a higher stroke risk. Carotid LRNC, calcifications, total plaque size, and plaque ulceration, have also been reported as important risk factors. With regard to sex-specific risk prediction and treatment, it is essential to investigate the effect of these plaque characteristics per sex separately. We hypothesise that the stroke risk as a result of specific plaque compositions varies among men and women.”
The authors further stress the importance of including an adequate number of men and women in clinical trials, as studies on sex-specific risks for (recurrent) stroke risk related to carotid plaque composition are “still lacking”. Men tend to have more “vulnerable” plaques than women, which has implications during stroke workup, for instance, and the role of IPH in carotid atherosclerosis underlines the relevance of using magnetic resonance imaging (MRI)—a modality that can identify IPH more reliably than ultrasonography or computed tomography angiography (CTA).
al state that the overall sensitivity, specificity and accuracy of AI was 91%, 86% and 92%, respectively, in the detection of normal carotid artery stenosis, and 87%, 82% and 90%, respectively, for any carotid artery stenosis.
In addition, subgroup analyses demonstrated that the AI network in question has the ability to detect stenotic carotid artery images (<50%) versus normal carotid artery images with a sensitivity of 92%, a specificity of 87% and an accuracy of 94%. The authors further note that these values (sensitivity, specificity and accuracy) for a subgroup of 50–75% stenosis versus normal were 84%, 80% and 88%, respectively, and—for another subgroup with carotid artery disease with >75% stenosis—were 90%, 83%
and 92%, respectively.
“The biggest advantage of AI is embedded in moving away from qualitative, operator-dependent analysis to a quantitative, data-driven approach in detecting carotid artery stenosis,” said Kordzadeh, speaking to NeuroNews following the publication of these findings. “AI has the potential to reduce human error by a significant margin with [an] ongoing data feed that continues to evolve for better accuracy, even in detection of stable or unstable plaque in addition to carotid artery stenosis. This enhances carotid artery disease recognition in a timely manner, resulting in prompt management, and reductions in mortality and morbidity associated with transient ischaemic attacks or stroke in the carotid artery territory.”
The biggest advantage of AI is embedded in moving away from qualitative, operator-dependent analysis to a quantitative, data-driven approach in detecting carotid artery stenosis.”Dianne van Dam-Nolen
The external validity—in other words, the transferability to realworld clinical practice—of contemporary randomised controlled trials (RCTs) investigating carotid artery stenosis interventions “varies considerably”, as per a recent analysis published in the European Journal of Vascular and Endovascular Surgery (EJVES) by senior author Hans-Henning Eckstein, first author Michael Kallmayer (both Technical University of Munich, Munich, Germany) and colleagues.

FOR THIS STUDY, RESEARCHERS aimed to analyse the exclusion criteria of recent RCTs comparing the two leading carotid revascularisation approaches—carotid endarterectomy (CEA) and carotid artery stenting (CAS)—with the intention of assessing the eligibility of consecutive clinical practice cohorts compared to those RCTs.
An analysis of the clinical and anatomical exclusion criteria of RCTs for asymptomatic carotid artery
stenosis (SPACE-2, ACST-2, CREST-1 and CREST-2) and symptomatic carotid artery stenosis (SPACE-1, CREST-1, ICSS and EVA-3S) was performed, the authors report.
A total of 200 consecutive asymptomatic and 200 consecutive symptomatic patients, treated by CEA or transfemoral/transcarotid artery stenting at a tertiary referral university centre, were assessed for their potential eligibility for each corresponding RCT. Patient data from the selected trials
were pooled and differences from the clinical practice cohort analysed. The authors note that statistics were descriptive and comparative using Fisher’s exact and t tests.
“The number of clinical and anatomical exclusion criteria differed widely between RCTs,” Eckstein, Kallmayer and colleagues write, relaying their results in EJVES

Potential eligibility rates of the clinical practice cohort for RCTs with regard to asymptomatic carotid stenosis were 80.5% (ACST-2), 79.5% (SPACE-2), 47% (CREST-1) and 20% (CREST-2). For RCTs on symptomatic carotid stenosis, the eligibility rates were found to be 89% (ICSS), 86.5% (EVA-3S), 64% (SPACE-1) and 39% (CREST-1).
Distal embolic protection using a filter has been associated with improved transfemoral carotid artery stenting (tfCAS) outcomes in terms of in-hospital stroke and death risks—underpinning current Society for Vascular Surgery (SVS) guidelines recommending routine use of distal embolic protection during carotid stenting, and supporting the notion that, “if a filter cannot be placed safely, an alternative approach to carotid revascularisation should be considered”.
Sophie Wang, Patric Liang (both Harvard Medical School, Boston, USA) and colleagues deliver this message in a recent Journal of Vascular Surgery (JVS) publication detailing a retrospective, propensity score-matched cohort analysis of tfCAS patients in the Vascular Quality Initiative (VQI) across a 16-year period.
“Transfemoral carotid stenting without use of embolic protection is associated with a significant increase in in-hospital stroke/death compared with tfCAS performed with distal filter placement,” the authors write. “Failed attempted filter placement is associated with worse outcomes after tfCAS, but stroke/death rates are no different than those seen in patients in whom a filter was never attempted.
“These findings support the current guideline recommendation for routine use of distal embolic filters during tfCAS. However, the proportion of nonprotected tfCAS performed annually is increasing, and there is significant variability in routine filter usage across physicians and centres in the VQI.”
In an effort to assess in-hospital outcomes in patients undergoing tfCAS with and without embolic protection using a distal filter, Wang, Liang and colleagues identified all patients undergoing this procedure in the VQI from March 2005 to December 2021—excluding those who received proximal embolic balloon protection. As well as creating propensity score-matched cohorts of patients who
underwent tfCAS with and without attempted filter placement, they performed subgroup analyses of patients with ‘failed’ versus ‘successful’ filter placement, and ‘failed’ versus ‘no attempt’ at filter placement.
In-hospital outcomes were assessed using log binomial regression, adjusted for protamine use, the authors detail. Their outcomes of interest were composite stroke/death, stroke, death, myocardial infarction (MI), transient ischaemic attack (TIA), and hyperperfusion syndrome.
Among 29,853 patients who underwent tfCAS, 28,213 (95%) had a filter attempted for distal embolic protection and 1,640 (5%) did not. After propensityscore matching, 6,859 patients were identified.
In comparison to cases in which a filter placement was attempted, no attempted filter was associated with a significantly higher risk of in-hospital stroke/ death (6.4% vs 3.8%)—constituting a more than twofold increase in stroke/death risk, as per the analysis’ key outcome of interest. Similar trends were observed regarding stroke (3.7% vs 2.5%) and mortality (3.5% vs 1.7%) too.
In a secondary analysis of patients who underwent a failed attempt at filter placement—versus successful filter placement—failure was associated with worse outcomes (stroke/death: 5.8% vs 2.7%; stroke: 5.3% vs 1.8%, respectively). However, Wang, Liang and colleagues observed no statistical difference in
Both clinical practice cohorts were older by about three years, and patients were more often male, when compared to the carotid RCT populations, the authors also report.
“Furthermore, a history of smoking (asymptomatic patients), hypertension (symptomatic patients), and atrial fibrillation was diagnosed more often [in the clinical practice cohorts], whereas hypercholesterolaemia and coronary heart disease (asymptomatic patients) were less prevalent,” Eckstein, Kallmayer and colleagues continue. “More clinical practice patients were on antiplatelets, anticoagulants and lipidlowering drugs. Symptomatic clinical practice patients presented more often with retinal ischaemia and less often with minor hemispheric strokes than patients in the RCTs.”
The authors conclude that, as such, patients in routine clinical practice differ from the selected carotid intervention trial populations with respect to age, comorbidities and medication.
“These data are of interest for clinicians and guideline authors, and may be relevant for the design of future comparative trials,” they add.
outcomes in patients with failed versus no attempted filter placement (stroke/death: 5.4% vs 6.2%; stroke: 4.7% vs 3.7%; death: 0.9% vs 3.4%) after adjusted analysis.
“Distal embolic protection confers a benefit in stroke/death rates following tfCAS compared to unprotected stenting,” the authors conclude, putting forward their ‘take-home message’ in JVS. “Failure to place a filter should prompt exploration of alternative carotid revascularisation approaches.”
6.4% with no attempt at filter placement
3.8% with attempted filter placement

The favourable trend toward gender parity that has been seen within neurology faculty over the past decade “has not translated” to the leadership of stroke-related clinical trials, as per a recent analysis published in the journal Stroke
“The results of our study show that gender disparity in the leadership of stroke-related clinical trials has persisted over the last decade with no favourable trend toward parity,” the authors— Sandeep Kumar (Beth Israel Deaconess Medical Center/Harvard Medical School, Boston, USA) and colleagues—write.
“However, the proportion of women leading clinical trials funded by the NIH [National Institutes of Health] or other federal agencies has fared significantly better relative to the overall proportion of women PIs [principal investigators] of clinical trials registered on Clinicaltrials.gov. Our findings merit further investigation into this area and a re-examination of efforts, specifically toward inclusion of women as leaders of clinical trials in the field of stroke research.”
Kumar and colleagues begin by noting that, despite the fact that gender disparities among clinical trial PIs can have implications regarding the areas of investigation, methods, conduct, trial enrolment, and interpretation of results, an estimation of the gender gap in the leadership of stroke-related clinical trials from North America has not been undertaken to date.

To investigate this further, they extracted information about stroke-related clinical trials between 2011 and 2020 from Clinicaltrials.gov and PubMed, and examined gender distribution according to academic
credentials and trial type. Further information was obtained from data resource books on the gender composition of full-time neurology faculty, neurology residents and vascular neurology fellows.
Across 821 trials registered on Clinicaltrials.gov and 110 studies published on PubMed, the authors found that gender disparity among PIs, as well as first and last authors, has persisted over the past decade, “without any significant trend toward parity”.
On examining the gender distribution according to academic credentials, they found that men (78.1%) were “over-represented” in the subgroup of PIs with a medical degree, as compared to women (21.9%). A similar trend was seen regarding trial type, with a significantly greater proportion of acute stroke trials being led by men (86%) versus women (14%).
Discussing their findings, Kumar and colleagues reiterate the favourable trend seen in the proportion of women holding a full-time neurology faculty appointment in the USA over the past decade, and state that, “considering the expected time-lag between starting in a junior role to becoming a Pl, we expected
A study conducted by Michigan Medicine (Ann Arbor, USA) researchers suggests that hospitals without the highest stroke care designation may be missing strokes that occur after transcatheter aortic valve implantation (TAVI)—a common, minimally invasive procedure whereby a patient’s thickened aortic valve is replaced with a manmade device.
THE RESEARCHERS ANALYSED
outcomes of more than 6,200 TAVIs performed across 22 Michigan-based hospitals between 2016 and mid-2019 using data from the Michigan Structural Heart Consortium. The study zeroed in on identification of stroke after TAVI at health systems with and without certification as a comprehensive stroke centre (CSC), the highest certification for acute stroke care.
Published recently in JACC: Cardiovascular Interventions, these findings reveal that CSCs reported significantly greater rates of stroke up to 30 days after TAVI—2.21 times higher than hospitals without the designation. A press release from Michigan Medicine posits that this raises two key questions; are hospitals with stroke centre accreditation finding more strokes because they take care of sicker, more complex patients? Or, are
they not performing TAVI at the level/ rate of those without such status?
But, after adjusting for patient characteristics, such as heart function and lung disease—and comparing other meaningful clinical outcomes after TAVI like mortality and renal failure— investigators found no significant differences in other clinically important outcomes outside of stroke detection.
A possible explanation for this finding is that patients receiving TAVI at high-level stroke centres are not having more strokes but, instead, hospitals with CSC status are better at detecting them—particularly smaller strokes. That is according to senior author Michael Grossman (University of Michigan, Ann Arbor, USA).
“This becomes an issue because stroke has been suggested as a nationally and publicly reported outcome measure for TAVI,” Grossman
to see a trend toward greater gender parity at least over the last five years”.
“Its absence may indicate persistent hurdles women face in leading clinical trials and/or publishing on their trial experience,” they add. “Further, our finding that the proportion of women holding an MD degree has been lower than the overall proportion of women leading clinical trials is suggestive of other systematic barriers that MD degree holders face when it comes to leading a clinical trial.
“These findings reveal some of the inadequacies of the pipeline theory, which postulates that recruiting a greater proportion of women in junior positions would automatically translate to a greater representation of women in leadership roles over time. However, our analysis also reveals that there has been a greater representation of women in leadership roles of NIH and federally funded clinical trials compared [to] all stroke-related clinical trials—regardless of funding status— registered in Clinicaltrials.gov.”
The authors go on to state that, in spite of attempts to close the gender gap, “numerous barriers” remain for women in science, and their findings warrant “a more comprehensive, multifaceted and inclusive effort”. They also highlight the fact that the creation of flexible policies that cater to some of the disproportionate challenges women face—such as access to childcare support, flexibility in promotion tracks, and efforts to retain women in academic leadership roles—may hold value.
“Our findings warrant further investigation into this area and calls for efforts to improve gender diversity in the leadership of clinical trials,” Kumar and colleagues conclude.
said. “Based on these data, stroke is not indicative of a universal quality issue. A death is a death. A transfusion is a transfusion. Stroke detection is inconsistent, and that variability will potentially put high-level stroke centres at a disadvantage in those quality measures.”
CSC status signifies an organisation’s capabilities and resources for integrated acute stroke management and care. Such centres have staff specifically trained in recognising signs of stroke, diagnosing it and activating systems of care to treat those patients, according to the Michigan Medicine release. These high-level centres were also more likely to participate in clinical trials for TAVI, which have reported higher rates of stroke up to 30 days after TAVI—between 3.4% and 6.1%—than
the national average of 2.3% reported in the Society of Thoracic Surgeons (STS)/American College of Cardiology (ACC) Transcatheter Valve Therapy (TVT) Registry.
This is an “extremely important” study, because it shows that TAVI sites with high-level stroke designation have a higher incidence of recognising, diagnosing and accurately reporting stroke to the TVT Registry, said coauthor G Michael Deeb (University of Michigan, Ann Arbor, USA).
“The national TVT Registry uses a composite score, which includes the incidence of stroke to rank the quality of care at all US TAVI sites,” Deeb said. “Those sites with high-level stroke designation are penalised by the composite endpoint, since sites with lower-level stroke designation may be underreporting the incidence of stroke and, thus, have a better composite score and higher TAVI site quality rating.”
Hospitals that participate in TAVI clinical trials adhere to more rigorous protocols for assessing neurologic outcomes, Grossman noted, explaining the higher rates of stroke detection.
“While these stroke rates are low overall, we need to be careful about how we are measuring quality for TAVI outcomes,” he added. “It could both punish sites that strive to mitigate stroke consequences and incentivise sites that are underreporting stroke rates after this procedure.”
While these stroke rates are low overall, we need to be careful about how we are measuring quality for TAVI outcomes.”
Michael GrossmanSandeep Kumar


In the latter stages of 2022, the Society of NeuroInterventional Surgery (SNIS) released a position statement advocating pregnancy and parental leave policies in neurointerventional surgery, stating a belief that physicians “should not have to choose” between a fulfilling family life and their professional career. The statement came off the back of a structured literature review, published in the Journal of NeuroInterventional Surgery (JNIS), that was led by Amanda Baker (San Francisco, USA) and used survey data regarding proposed changes to reduce barriers for women and parents pursuing family life, as well as addressing concerns regarding radiation exposure.
Irecently sat down—remotely—with
Dr Felipe Albuquerque, JNIS editor-inchief, who I was thrilled to hear took an interest in our recently published article on pregnancy and parental leave.1,2 He remarked that some of the barriers that females face in the field of neurointerventional surgery can be subtle.
I was interested in this comment, as it made me give pause and consider: What exactly are the barriers for women interested or currently practising in this field? And, how can we, as women, better communicate to our male colleagues what is and is not contributing to the gender disparity?
I am familiar with being the only woman in a room full of men; my undergraduate studies in nuclear engineering were another example. Nearly two decades later, as a brand new neurointerventionist, I continue to be the only woman—or one of very few women—in a room full of men. At least half of medical school graduates are female3 yet, based on SNIS membership data, women likely represent less than 10% of practising neurointerventionists.4 Gender disparity in neurointerventional surgery has followed from the specialties that comprise it5—neuroradiology, neurosurgery and stroke neurology— with an even smaller percentage of females in these fields interested in pursuing neurointerventional surgery.
I have spent countless hours questioning, reading, thinking: Why are there not more women in the room? Is radiation really the major barrier for women to enter nuclear engineering and, now, neurointerventional surgery?
In 1903, Marie Curie was the first woman to win the Nobel Prize in Physics for her work in radiation.6 Her story reflected the danger of radiation, which likely caused the aplastic anaemia that ultimately took her life. The reality of this is depicted by an infamous radiograph of her hand. The nuclear field has made significant strides in upholding standards for radiation workers in diagnostic and therapeutic medical fields, yet many women remain photon averse, particularly during childbearing years.
Overall, the data suggest that the cumulative dose during pregnancy remains low with the use of appropriate radiation protection equipment.7,8 Personally, this was reflected by my dosimeter during pregnancy in the second year of my neurointerventional fellowship. But what is ‘low dose’— what does this mean in terms of risk, and does that differ with respect to oncologic risk, reproductive risk or perinatal risk?
As a nuclear engineer, the short answer is that we do not know. Health risks related to radiation exposure remain based on atomic bomb survivors, and the data for the lowest doses have been theoretically extrapolated.9,10 More definitive answers have yet to be elucidated due to limitations of cofounding, bias and reverse causation in retrospective and epidemiologic studies; ethical inability to conduct prospective studies; and the gap between the damage/repair cycle in irradiated cells and in vivo reality. For now, we can rest assured that, although this topic
remains controversial, substantially increased risk following low-dose radiation is unproven.11
While we have means to quantify radiation dose by wearing dosimeters, we do not have a way to measure anxiety and the realistic concerns that accompany pregnancy. The best we can do is recognise the difficulty in the unknown (i.e. risk of low doses of ionising radiation to a fetus) and mitigate risk with availability of full protective equipment, as well as allow for continued flexibility in the workplace12—particularly for our pregnant colleagues.
In Interventional Neuroradiology, Power et al demonstrated via a survey of nearly 300 neurointerventionists, the majority of whom were between 35 and 60 years of age, that significantly fewer women were married (63% vs 91%) or had children (42% vs 84%) compared to men.4 We must keep in mind that radiation concerns around childbearing may not be applicable to all women. I would argue other barriers are equally if not more pressing for women choosing this field.
Neurointerventional surgery is inherently a difficult subspecialty, requiring a lot of call, stressful procedures, and inflexible work hours. It is not typically chosen for its ‘quality-of-life’ benefits. These characteristics are unlikely to change and, if anything, may worsen in the wake of the New England Journal of Medicine trials demonstrating efficacy for thrombectomy in patients with largecore infarcts.13-15 The difficulties apply
supporting women is crucial, and I credit the Women in Neurointervention (WINN) group on WhatsApp and Facebook of nearly 400 female neurointerventionists worldwide for doing exactly this.
All this being said, the single most important thing to attract anyone to the field of neurointerventional surgery is to expose everyone—those that are interested will come back. Those interested, and treated well, will keep coming back, and those really interested—who cannot see themselves doing anything else within medicine— will show up in the middle of the night. Neurointerventional surgery is my passion and, as hard as some days have been and will continue to be, I cannot imagine doing anything else.
References:
1. Baker A, Narayanan S, Tsai J P et al. Society of NeuroInterventional Surgery: position statement on pregnancy and parental leave for physicians practicing neurointerventional surgery. J Neurointerv Surg. 2023; 15(1): 5–7.
2. Albuquerque F C, Narayanan S. Pregnancy and parental leave for neurointerventional surgeons. J Neurointerv Surg [internet]. 2023. Podcast. Available from: https://open.spotify.com/episode/6rXWOVRxUrf SHhOLmqwklF?autoplay=true.
3. The Majority of US Medical Students Are Women, New Data Show. Association of American Medical Colleges [press release]. 9 December 2019.
4. Power S, Biondi A, Saatci I et al. Women in neurointervention, a gender gap? Results of a prospective online survey. Interv Neuroradiol. 2022; 28(3): 311–22.
5. Aguwa U T, Menard M, Srikumaran D et al. Sex diversity within US residencies: a cross-sectional study of trends from 2011 to 2019. BMC Med Educ 2022; 22(1): 526.
6. Marie Curie—Biographical. Nobel Prize Outreach. Available from: https://www.nobelprize.org/prizes/ physics/1903/marie-curie/biographical/.
7. Chen S H, Brunet M C. Fetal radiation exposure risk in the pregnant neurointerventionalist. J Neurointerv Surg. 2020; 12(10): 1014–7.
8. Parra-Farinas C. How to Fight the Fear Under the X-Ray Beam: Interventional Neuroradiology Fellow Mom to Be. Stroke. 2020; 51(7): e121–e123.
9. Ali Y F, Cucinotta F A, Liu N A et al. Cancer Risk of Low Dose Ionizing Radiation. Front Phys-Lausanne 2020; 8.
10. Dahal S, Budoff M J. Low-dose ionizing radiation and cancer risk: not so easy to tell. Quant Imaging Med Surg. 2019; 9(12): 2023–6.
11. Cardarelli J J, Ulsh B A. It Is Time to Move Beyond the Linear No-Threshold Theory for Low-Dose Radiation Protection. Dose-Response. 2018; 16(3).
12. Koven S, Haberer J E, Gomez Kwolek D. Pregnancy and Residency—Overdue for Equity. N Engl J Med 2023; 388(11): 966–7.
13. Huo X, Ma G, Tong X et al. Trial of Endovascular Therapy for Acute Ischemic Stroke with Large Infarct. N Engl J Med. 2023.
14. Sarraj A, Hassan A E, Abraham M G et al. Trial of Endovascular Thrombectomy for Large Ischemic Strokes. N Engl J Med. 2023.
15. Yoshimura S, Sakai N, Yamagami H et al Endovascular Therapy for Acute Stroke with a Large Ischemic Region. N Engl J Med. 2022; 386(14): 1303–13.
to men and women alike. However, societal pressures may not be the same, even in 2023—as astutely noted by Dr Dorothea Altschul in a recent interview with LINNC Online for International Women’s Day (8 March), who said that “[...] women are not expected to be in a hard field, whereas men are”.16 It is hard to undo hundreds of years of societal ‘norms’ and expectations.
Beyond that, issues that relate to gender inequity—or being treated differently based on gender—include sexual harassment as well as decreased rates of leadership, research funding, recognition and promotion.4,17 These issues detract time and energy from the meaningful work women could do. In addition, few female neurointerventionists exist to mentor or lead more junior women. Women
16. Altschul D. Pregnancy radiation risk and young women perspectives. LINNC Online 2023. Available from: https://www.youtube.com/ watch?v=9YT4UbCEouE.
17. Javed K, Altschul D, Albuquerque F C et al Assessment of female authorship in Journal of NeuroInterventional Surgery (JNIS) publications in 2016–2020. J Neurointerv Surg. 2022; 14(7): 636–9.
Amanda Baker is a neurointerventional radiology fellow at the University of California San Francisco (UCSF) in San Francisco, USA, and a member of the SNIS. She studied Medicine at Drexel University College of Medicine in Philadelphia, USA and Nuclear Engineering at the Massachusetts Institute of Technology (MIT) in Cambridge, USA.
ACKNOWLEDGEMENTS:
The author thanked those who supported her pregnancy as a neurointerventional radiology fellow at UCSF— specifically, her mentor, Steven Hetts, and ultimate female advocate Christine Glastonbury; SNIS WINN committee chair Sandra Narayanan; and the WINN group, with a special mention to its creator, Thanh N Nguyen.
I have spent countless hours questioning, reading, thinking: Why are there not more women in the room?”

The European Society for Brain Stimulation (ESBS) has said it “strongly opposes” the European Union’s (EU) recent decision to reclassify non-invasive brain stimulation (NIBS) technologies as Class III medical devices.
In what ESBS members describe as a “sudden and unwelcome” regulatory change, which was announced in December 2022, repetitive transcranial magnetic stimulation (rTMS) and low-intensity transcranial electrical stimulation (tES) devices are now set to be considered in the highest-risk category under the EU Medical Device Regulation (MDR).
“Although this new reclassification currently refers only to ‘products without an intended medical purpose’ (a terminology that is, for many researchers and medical doctors, unclear), the evidence adduced about the risks and adverse effects of rTMS and tES—which serves as the justification for this reclassification—is gravely flawed,” Andrea Antal (University Medical Center Göttingen, Göttingen, Germany) et al write in Brain Stimulation
While the authors note their agreement that all NIBS devices must be certified as medical devices—something that was not extensively defined within the previous Medical Device Directive (MDD)—they argue a more moderate-risk Class IIa classification would be more appropriate.
“To reclassify NIBS devices as having the same level of risk as invasive brain stimulation devices that are implanted inside the brain is inappropriate, contradicts 30 years of safety data, and has been decided without consultation of relevant professional stakeholders,” they add.
According to the ESBS, the EU’s assessment that NIBS devices pose a greater risk to patient safety than previously thought is based on “incorrect statements” about rTMS and low-intensity tES, citing claims and assumptions that are
“simply false”—such as TMS/tES inducing atypical brain development and abnormal patterns of brain activity—and concerns around rTMS/tES-related seizure risks that are “no longer supported by scientific evidence”.
The current scientific and clinical evidence suggests both rTMS and low-intensity tES are safe treatment and research interventions, with few and mild adverse effects, making the establishment of this new EU ruling “hard to understand”, in the authors’ view. NIBS products previously listed as Class I or IIa will be allowed to remain on the market—provided they comply with EU transition rules—until the MDR deadline, which was recently extended from May 2024 to December 2027 for higher-risk devices, and December 2028 for medium- and lower-risk devices.
Nevertheless, the ESBS states a belief that this reclassification will “have significant negative consequences for the future of our field”, resulting in higher costs and substantial research and development delays in the short term; and ultimately making NIBS treatments less accessible for European patients in the long run.
“European citizens will be disadvantaged, and there is the risk that other treatment approaches with more serious and established adverse effects will be overused to compensate for the lack of NIBS availability,” Antal and colleagues conclude. “Consequently, we strongly protest this decision, and we urge our colleagues working in our field to do the same, regardless of nationality. We have already sent a protest letter to the EU.”

A randomised, triple-blinded clinical trial involving 35 women has found that active transcranial direct current stimulation (tDCS)—delivered at an intensity of 2mA and across a total of 10 sessions—may be an effective treatment option for patients with fibromyalgia.
This finding has been published in Neuromodulation: Technology at the Neural Interface by Eduardo Henrique Loreti (Centro Universitário da Grande Dourados, Dourados, Brazil) and colleagues.
The authors report improvements regarding pain, fatigue and quality of life in their study’s treatment arm.
Loreti and colleagues state that the aim of their study was to analyse the effects of 10 sessions of active tDCS (2mA) via a conventional tDCS device, with the anodal stimulation target being the left primary motor cortex (M1) region of the brain.
“To the best of our knowledge, this is the first article that uses this protocol in patients with fibromyalgia,” the authors note. “The main hypothesis is that the protocol would be effective in decreasing pain and that the results would last for up to 90 days.”
The primary outcome was a change in the visual analogue scale (VAS) and the survey of pain attitudes (SOPA) pain score at the end of treatment, after 30 days, and 90 days after the end of treatment. Secondary outcomes included changes in fibromyalgia impact, depression, anxiety, quality of life and fatigue.
Thirty-five women with fibromyalgia were divided into two groups in the trial—an active tDCS group and a sham tDCS group.
Loreti and colleagues report that the active tDCS group showed improvements in pain after 10 sessions (p<0.001). Improvements were also seen after 30 days (p<0.01), and after 90 days (p<0.001), as compared with sham tDCS.
“In addition, improvement in quality of life and fatigue was observed in the active tDCS group,” the authors add.
As such, they conclude their report by stating that the specific active tDCS treatment protocol used here proved to be an effective therapy for patients with fibromyalgia.
To reclassify NIBS devices as having the same level of risk as invasive brain stimulation devices that are implanted inside the brain is inappropriate, contradicts 30 years of safety data, and has been decided without consultation of relevant professional stakeholders.”
Spinal cord stimulation (SCS) therapy has been shown to trigger instant improvements in arm and hand mobility, enabling people affected by moderate-to-severe stroke to perform daily activities more easily, as reported in Nature Medicine by researchers from the University of Pittsburgh and Carnegie Mellon University in Pittsburgh, USA.


“WE DISCOVERED THAT electrical stimulation of specific spinal cord regions enables patients to move their arm in ways that they are not able to do without the stimulation,” said corresponding and co-senior author Marco Capogrosso (University of Pittsburgh, Pittsburgh, USA). “Perhaps even more interesting; we found that, after a few weeks of use, some of these improvements endure when the stimulation is switched off, indicating exciting avenues for the future of stroke therapies. Thanks to years of preclinical research building up to this point, we have developed a practical, easy-to-use stimulation protocol adapting existing FDA [Food and Drug Administration]approved clinical technologies that could be easily translated to the hospital and quickly moved from the lab to the clinic.”
According to the researchers, this new technology has the potential to offer
hope for stroke survivors living with impairments that would otherwise be considered permanent.
“Creating effective neurorehabilitation solutions for people affected by movement impairment after stroke is becoming ever more urgent,” said co-senior author Elvira Pirondini (University of Pittsburgh, Pittsburgh, USA). “Even mild deficits resulting from a stroke can isolate people from social and professional lives, and become very debilitating, with motor impairments in the arm and hand being especially taxing and impeding simple daily activities, such as writing, eating and getting dressed.”
While SCS therapies have been used widely to treat high-grade, persistent pain, and multiple research groups have shown it can be deployed in restoring leg movement after a spinal cord injury, the researchers state that the “unique dexterity of the human

hand”—combined with the wide range of motion of the arm at the shoulder, and the complexity of the neural signals controlling the arm and hand—create a significantly greater set of challenges.


However, following years of extensive preclinical studies involving computer modelling, and animal testing in macaque monkeys with partial arm paralysis, the researchers were cleared to test this optimised therapy in humans.
“The sensory nerves from the arm and hand send signals to motor neurons in the spinal cord that control the muscles of the limb,” said co-senior author Douglas Weber (Carnegie Mellon University, Pittsburgh, USA). “By stimulating these sensory nerves, we can amplify the activity of muscles that have been weakened by stroke. Importantly, the patient retains full control of their
movements; the stimulation is assistive and strengthens muscle activation only when patients are trying to move.”
In a series of tests adapted to individual patients, stimulation enabled participants to perform tasks of different complexity, from moving a hollow metal cylinder to grasping common household objects, such as a can of soup, and opening a lock. Clinical assessments showed that stimulation targeting cervical nerve roots immediately improves strength, range of movement, and function of the arm and hand, the researchers have reported.
Unexpectedly, the effects of stimulation seem to be longer-lasting than scientists originally thought and persisted even after the device was removed, suggesting it could be used both as an assistive and a restorative method for upper limb recovery. The researchers believe the immediate effects of the stimulation enable administration of intense physical training that, in turn, could lead to even stronger long-term improvements in the absence of the stimulation.
Moving forward, they will continue to enrol additional trial participants to understand which stroke patients can benefit most from this therapy— and how to optimise stimulation protocols for different severity levels. Additionally, the two universities involved are working with startup firm Reach Neuro to translate this therapy into clinical use.

Creating effective neurorehabilitation solutions for people affected by movement impairment after stroke is becoming ever more urgent.”
Elvira Pirondini
High-frequency spinal cord stimulation (HF-SCS) for treating chronic refractory low back pain (CRLBP) may be associated with a significant decrease in total healthcare costs, offsetting device acquisition costs within 27 months, according to a recent analysis published in Neuromodulation: Technology at the Neural Interface.
Shivanand Lad (Duke University Medical Center, Durham, USA) and colleagues, who conducted this analysis based around large claims data on the cost of HF-SCS, also note that “as advances in neuromodulation expand therapy options for patients, it will be important to understand their financial implications”.
At the outset of their report, Lad and colleagues posit that—while HF-SCS is a new advance in neuromodulation that may be effective in treating CRLBP patients—the cost burden of this therapy is “yet undetermined”.
Using IBM MarketScan databases, the researchers retrospectively identified patients who had undergone HF-SCS implantation between 2016 and 2019 in the USA. Those with low back pain diagnosis, but without history of surgery, were included in the cohort. Cost data, including inpatient and outpatient service, medication, and out-of-pocket costs, were collected at six months before HF-SCS implantation, and at one, three and six months after implantation. The explant rate within those six months was also evaluated.
A total of 119 patients met the analysis’ inclusion
criteria, Lad and colleagues detail. The majority (73.1%) were female and owned commercial insurance (83.2%), and the median age across the final CRLBP cohort was 54 years. Common comorbidities included inflammatory arthritis (22.7%), depression (26.1%), hypertension (44.5%) and obesity (26.1%).
In the six months before HF-SCS implantation, patients incurred median total costs of US$15,766, whereas the post-implant median total cost excluding device acquisition was US$398 at one month, US$2,569 at three months, and US$5,840 at six months.
The authors report that, therefore, the average reduction in total cost was US$6,914 (95% confidence interval [CI]: US$588–US$12,458, p<0.001). The median total acquisition cost was US$43,586, with most of this coming from outpatient services. And, of 88 patients with six-month continuous enrolment, two (2.3%) underwent a device explant.
This study was hindered by the inherent limitations of conducting retrospective studies using large commercial databases, Lad and colleagues concede, as well as its relatively small sample size and lack of
Spinal cord stimulation (SCS) therapies targeting the dorsal column “may be considered” within the multimodal treatment plans typically required by cancer patients, but it is “unclear” which types of cancer-related pain are likely to respond to these therapies. That is according to Sandy Christiansen (Oregon Health and Science University, Portland, USA), who also noted in a presentation at the North American Neuromodulation Society (NANS) annual meeting (12–15 January 2023, Las Vegas, USA) that the current research is limited to certain types of treatmentinduced neuropathy across case reports with a “very low grade for certainty of evidence”.
CHRISTIANSEN BEGAN WITH
a brief outline of the numerous causes of cancer-related pain—ranging from the primary or metastatic disease itself, to treatments like surgery or chemotherapy, as well as immobility, infection and cytokine-created inflammation. She further noted the criticality of treating these patients, citing a prevalence as high as 85% in certain cancer types, and the psychological distress and disrupted quality of life many patients experience.
Proposed SCS mechanisms of action to treat cancer-related pain have come under three main categories: nociceptive, neuropathic and nociplastic. However, according to Christiansen, no randomised control trials have been conducted in this space to date, with small case reports
and series—in addition to some larger retrospective reviews—constituting the bulk of the existing evidence here.
The speaker did discuss one such report, a 2019 Cochrane systematic review published in the Journal of Pain Research by Jonathan Hagedorn (Mayo Clinic, Rochester, USA) et al, which found significant reductions in pain severity and decreased opioid usage, but also determined a high risk of bias across all of the included studies and, thus, concluded that the evidence was “insufficient”. A retrospective review published in Neuromodulation: Technology at the Neural Interface last year by Amitabh Gulati (Memorial Sloan Kettering Cancer Center, New York, USA) et al did, however, assert that “SCS can be considered as a treatment modality for patients with
generalisability outside of the US healthcare system. They go on to note that, owing to costs not being included for control groups—such as CRLBP patients who did not receive SCS—future trials involving HF-SCS for CRLBP should include a more specific focus on CRLBP-related costs, in order to corroborate their results and address comparisons in costs more definitively.
“Furthermore, combination of cost data with qualityof-life data in such studies may shed light on the costeffectiveness of HF-SCS,” they state.
“HF-SCS is associated with a statistically significant decrease in total healthcare costs and with reductions in out-of-pocket costs for patients. As the USA struggles with exorbitant healthcare spending, HF-SCS is potentially a treatment option that may reduce costs in patients with CRLBP.”
cancer whose pain is not adequately controlled with medical therapy or by less invasive interventions”, based on data from a cohort of 73 patients.
Moving on to outline key considerations for implanting and trialling SCS systems in cancer patients, Christiansen stated that the “bottom line” is that standard procedural risks are amplified. For example, bleeding risks are exacerbated in cancer patients due to disordered coagulation; infection risks are heightened by immunosuppression, which can be caused by the cancer directly, or may occur secondarily to treatments like radiation or immunotherapy; and impaired wound healing, which can also be a result of the patient being malnourished, or sideeffects of their cancer treatments.
Naturally, Christiansen opined, all of these factors demand additional consideration when it comes to implanting an SCS system into a patient—as does the fact that previous reports have indicated stimulators may experience battery drain and electrical failure when they are directly within radiation fields. With these elements in mind, clinicians should pre-emptively anticipate complications or possible reasons for treatment failure that are specific
to cancer patients.
“Stick with what you know” was another key message delivered by the speaker, who pointed out that there is Level 1 evidence suggesting a benefit of dorsal column stimulation for chronic neuropathic pain in non-cancer patients. As such, neuropathic cancerrelated pain may be an appropriate starting point for the use of SCS therapies.
She also provided the NANS audience with several pieces of advice pertaining to cancer patients, including focusing on the timing of the SCS implantation—or any other interventional pain procedure—relative to chemotherapy, radiation and any other planned treatments, and having a “thorough understanding” of the patient’s prognosis, current state and past treatments.
“Given the time-intensive nature of cancer pain care, a cancer care coordinator can be critical to your success,” Christiansen added.
Prior to concluding, she further highlighted that, in the future, the dorsal column could be targeted in order to reduce centrally sensitised neurons in the spinal cord and supraspinal centres— an approach that could offer benefits in cancer patients who fail sympathetic neurolytic blocks.

SCS therapies can play a role in cancer-related pain treatment despite
As the USA struggles with exorbitant healthcare spending, high-frequency spinal cord stimulation is potentially a treatment option that may reduce costs in patients with chronic refractory low back pain.”Sandy Christiansen
Abbott presented new data across more than 30 presentations and posters at this year’s North American Neuromodulation Society (NANS) annual meeting (12–15 January 2023, Las Vegas, USA), including results from its REALITY sub-study, which were delivered by Denis Patterson (Nevada Advanced Pain Specialists, Reno, USA).
As per a company press release, the findings from this sub-study reinforce the value of wearable technology in monitoring patient responses to spinal cord stimulation (SCS) therapy. It assessed the use of wearable sensors in finding biomarkers associated with pain during SCS treatment, and identified several objective features from the wearable pre- versus post-SCS therapy— including heart rate, step count and stand time.
Responses to SCS therapy are usually evaluated in the clinical setting via patient-reported outcomes (PROs), the release notes, and objective measures collected from wearable sensors may complement these PROs to provide a better understanding of patients’ chronic pain. According to Abbott, these results “set up a foundation for using objective measures for predicting response to SCS therapy in the future”.
Another NANS presentation intended to highlight how neuromodulation can help people suffering from chronic pain and movement disorders, including in potentially new indications, was given by Frank Huygen (Erasmus University Medical Center, Rotterdam, The Netherlands), whose discussion of the international REALITY study underscored the potential of streamlined sets of patient-reported measures in SCS recipients.
While frequent data collection can inform patient progress and success, traditionally,
this tracking utilises long-form questionnaires, which can be burdensome for both patients and clinicians, the release from Abbott states. As such, the goal for this study was to investigate the feasibility of using a limited set of outcome questions from multiple validated, patientrecorded outcomes to increase patient engagement, based on data from the prospective, multicentre REALITY study. Insights from this trial highlight the value of transitioning from a more subjective numerical rating scale to a digital platform, which may include only the most important questions to increase engagement, Abbott claims.
A third presentation highlighted by the company referred to late-breaking one-year data from the DISTINCT randomised controlled trial (RCT), demonstrating the superiority of the BurstDR SCS system as compared to conventional medical management.
Findings from this 12-month, post-implant study demonstrated “dramatic improvements” in pain, function and pain-related emotional suffering when using Abbott’s BurstDR SCS system in patients suffering from chronic low back pain that cannot be addressed through corrective surgery.
These findings were presented by Timothy Deer (West Virginia University, Charleston, USA), who also received the inaugural Presidential Merit Award at NANS’ annual meeting.
Saluda Medical has announced that first-time data from the “landmark” EVOKE clinical trial were presented at the North American Neuromodulation Society (NANS) annual meeting (12–15 January 2023, Las Vegas, USA)—constituting what the company claims is “the longest follow-up evidence from a US investigational device exemption (IDE) trial in spinal cord stimulation (SCS) history”.
THE INTENTION-TO-TREAT (ITT) AND crossover analysis of 134 randomised patients across 13 US sites in this 36-month, double-blind, randomised controlled trial (RCT) was presented by Nagy Mekhail (Cleveland Clinic, Cleveland, USA) during the latebreaking clinical abstracts session.
The long-term dataset demonstrated that patients in the treatment arm receiving closed-loop Evoke SmartSCS system therapy experienced clinical outcomes “never before reported in SCS”—according to Saluda—including:
Sustained superiority over open loop in treating overall back and leg pain
Seventy-eight percent of ITT (83% of implanted closedloop patients) achieved >50% pain reduction
Forty-nine percent of ITT (59% of implanted closedloop patients) achieved >80% pain reduction
Zero explants due to loss of efficacy after 36 months of closed-loop therapy
High patient satisfaction; 90% very satisfied or satisfied
While blinded to whether they were receiving closedloop or open-loop therapy, patients were able to cross over to the other treatment arm at 24 months and then decide which arm they preferred. The majority of patients who crossed over from open-loop to closed-loop therapy chose to cross over in search of better pain relief.
In addition to experiencing significant and durable pain relief, patients who crossed over to closed loop experienced improvements in quality of life, functional ability, mood and sleep at 36 months, achieving a similar treatment benefit as patients who stayed in closed-loop therapy throughout.
“The Evoke system is the only SCS therapy capable of continuously listening to the spinal cord and optimising neural activation with precise, prescriptive closed-loop dosing based upon an individual patient’s unique neural signature,” said Mekhail.
“This is one of the most important innovations in the field of neuromodulation since Norman Shealy implanted the first stimulator lead in 1967.”
Combination spinal cord stimulation (SCS) therapy with Boston Scientific’s WaveWriter system has demonstrated superior outcomes to conventional medical management (CMM) in chronic pain patients with no prior back surgery, as per randomised controlled trial (RCT) data presented at the North American Neuromodulation Society (NANS) annual meeting (12–15 January 2023, Las Vegas, USA).
DURING NANS 2023, BOSTON Scientific showcased some 40 abstracts relaying randomised controlled data and real-world evidence pertaining to the company’s therapies for patients with chronic pain and neurological disorders.
One such abstract was presented by James North (Carolinas Pain Institute and Center for Clinical Research, WinstonSalem, USA), who delivered three-month data from the SOLIS RCT—a multicentre, prospective, parallel-group study evaluating WaveWriter SCS with multiple modalities versus CMM. The trial involved patients with chronic low back pain and/or leg pain who had not undergone spinal surgery, often referred to as non-surgical back pain (NSBP). A total of 60 patients were enrolled and became available for the trial’s three-month primary endpoint analysis.
In SOLIS’ experimental treatment arm— which saw multiple mechanisms of action engaged under a single SCS combination therapy—NSBP patients experienced higher responder rates (88% vs 8%) without an increase in opioids, as well as a significant improvement in disability and higher satisfaction rates, at three months. As such, the trial was determined to have met its primary endpoint, which was the proportion of subjects with a ≥50% reduction in average, overall pain with no increase in baseline opioid medications in the experimental (SCS plus CMM) arm versus the control (CMM only) arm.
With the SOLIS trial also meeting its prespecified secondary endpoints across a 60-patient cohort—improvement in disability and patient satisfaction rates— the investigators concluded that SCS with multiple modalities is effective in treating chronic pain, demonstrating superior outcomes to CMM alone in patients with no prior back surgery. In addition, North reported that these SOLIS RCT outcomes are consistent with long-term, real-world NSBP data from the global, prospective RELIEF registry, which are now published in Pain Management, and two-year results from the COMBO RCT.
This is one of the most important innovations in the field of neuromodulation since Norman Shealy implanted the first stimulator lead in 1967.”
Neuromod Devices has announced that the US Food and Drug Administration (FDA) has granted denovo approval to Lenire—the first bimodal neuromodulation device of its kind to be approved by the FDA for the treatment of tinnitus, according to a company press release.

“FDA approval of the Lenire tinnitus treatment system is a quantum leap forward in the caring of patients with bothersome tinnitus,” said Steven Cheung (University of California San Francisco [UCSF], San Francisco, USA). “The otolaryngologist now has access to innovative Lenire technology and can prescribe it to patients who are at least moderately impacted by their tinnitus. The majority of these tinnitus patients are either inadequately relieved or are opting not to pursue existing options, such as hearing aids. These patients can now move forward with this impressive treatment system.”
The FDA’s de-novo approval of Lenire—which was based on the technology’s success in the large-scale TENT-A3 trial comparing six weeks of bimodal neuromodulation to six weeks of sound therapy alone—is significant in that it establishes a new regulatory category for medical devices in the USA, the release also notes.
Axonics has announced that the US Food and Drug Administration (FDA) has approved the company’s fourth-generation rechargeable sacral neuromodulation (SNM) system—a technology intended to provide patients suffering from overactive bladder and/ or faecal incontinence with long-lived, easy to use, safe and effective therapy.
The newly approved Axonics R20 neurostimulator is labelled for a functional life in the body of at least 20 years and reduces how frequently a patient needs to recharge their implanted device to just once every 6–10 months for only one hour, as per a company press release. This compares
to the third-generation’s recharge interval of once per month for one hour.
The Axonics R20 neurostimulator utilises the same small, 5cc form factor as the Axonics R15, and is paired with the same tined lead and intuitive patient remote control. Axonics plans to commercially launch the product in the USA in March.
Cognito Therapeutics has announced the first patient enrolment in its US pivotal study, HOPE, which is designed to demonstrate the safety and efficacy of the company’s proprietary, non-invasive stimulation device—CogTx-001—in patients with Alzheimer’s disease.
The HOPE study for Alzheimer’s disease is evaluating a novel wearable device that has the potential to slow the progression of Alzheimer’s disease, without the safety concerns associated with medications or highly invasive procedures, according to a Cognito press release. In the blinded, shamcontrolled study, 400 patients with Alzheimer’s will use the company’s non-invasive wearable device at home, on a daily basis, for 12 months.
HOPE is intended to build on the success of the OVERTURE study, in which patients using CogTx-001 reported reductions in disease progression of 83% (mini-mental state exam [MMSE]) and 78% (Alzheimer’s disease cooperative study-activities of daily living [ADCS-ADL]). In addition to its primary endpoint of slowing disease progression, the HOPE study will also assess the slowing of brain atrophy on magnetic resonance imaging (MRI) and changes in clinical dementia ratings from baseline.
“The HOPE study offers a rare opportunity for patients with mildto-moderate Alzheimer’s disease to participate in a research study utilising technology as an intervention,” said Michelle Papka (Cognitive and Research Center of New Jersey, Springfield, USA). “Patients and their family members have expressed great interest in enrolling in this study because it is non-invasive, and represents a novel and safe approach to potentially slowing the progression of Alzheimer’s disease.”
Nevro Corporation announced that it has now initiated the full US market launch of its HFX iQ spinal cord stimulation (SCS) system, following the completion of a successful limited market release.
“This is an exciting time in spinal
cord stimulation—better waveforms, more conditions we can treat, and a massive treasure trove of patient data,” said Usman Latif (University of Kansas Medical Center, Kansas City, USA). “The way forward in this field is precision medicine powered by big data and artificial intelligence [AI].”
HFX iQ starts patients on the programme most likely to provide pain relief, based on Nevro’s HFX algorithm. It combines clinical inputs, such as pain relief and pain score, with quality-of-life inputs like pain medication and activity level changes to provide an individualised programme setting for each patient.
According to a Nevro press release, the system offers both low frequency and the company’s proprietary highfrequency 10kHz therapy, which represents “the widest range of frequencies of any SCS system on the market”.
Having received US Food and Drug Administration (FDA) approval for its Senza HFX iQ SCS system last year, Nevro has now also submitted for approval in Europe and Australia.
Mainstay Medical has announced the publication of a paper in the journal Neurosurgery containing a review of patients from the pivotal ReActiv8-B study, and the effect of ReActiv8 restorative neurostimulation on known drivers of direct and indirect long-term healthcare costs.
The present results show that patients “overwhelmingly converted” from a ‘high-impact’ pain state to a ‘low-impact’ pain state after two years of ReActiv8 therapy. In a completer analysis of patients available at two years and having work data, 103 (70.5%) were high-impact pain patients at baseline. After two years, 15 (10.3%) patients remained in the high-impact pain state, while 124 patients (85%) were in the low-impact pain category.
Regarding indirect drivers of economic impact, the study found that, at baseline, approximately 50% of patients experienced significant restrictions on work participation, while fewer than 50% reported no work problems. After two years, more than 80% of patients reported no/minor impact on their work participation due to low back pain, and 88% of patients were not missing any workdays due to low back pain.
“It is incredibly impressive to see a novel therapy that is able to successfully treat chronic mechanical low back pain, not only clinically, but also in a way that has a positive economic impact on the healthcare system and the employers of these patients,” said Chris Shaffrey (Duke University, Durham, USA). “Physicians across multiple specialties should strongly consider providing ReActiv8 for their patients earlier in their care continuum based on these results.”
LivaNova has announced the launch of SenTiva DUO—an implantable pulse generator (IPG) with a dual-pin header intended to provide vagus nerve stimulation (VNS) therapy for patients with drug-resistant epilepsy.

The dual-pin header distinguishes this latest IPG from the original SenTiva device, which is only available in a single-pin format. Now, with SenTiva DUO, patients described by LivaNova as “the pioneers of VNS therapy”, who were originally implanted with a dual-pin lead and IPG, can receive the benefits of the company’s latest VNS technology.
“This new offering enables those VNS therapy patients with legacy dual-pin systems to have the option to replace their device with SenTiva DUO, delivering the most advanced VNS therapy treatment without the need for lead revision,” said James Wheless (Le Bonheur Children’s Hospital, Memphis, USA). “Having access to SenTiva DUO offers patients therapy that can be customised and delivered automatically, providing
optimal seizure control and enabling maximum adherence to treatment.”
The US Food and Drug Administration (FDA)-cleared SenTiva DUO offers the same therapeutic benefits as SenTiva, providing stimulation in response to rapid heartrate increases; allowing day-night programming; offering scheduled programming; and logging low heartrate and prone position events.
Abbott has announced that the US Food and Drug Administration (FDA) has approved its Proclaim XR spinal cord stimulation (SCS) system to treat painful diabetic peripheral neuropathy (DPN).
The Proclaim XR SCS system can provide relief to DPN patients in need of alternatives to traditional treatment approaches, such as oral medication, according to an Abbott press release. People who receive therapy from the Proclaim XR SCS system will also be able to use the company’s connected care app, the NeuroSphere virtual clinic.
Proclaim XR SCS provides “hasslefree” pain relief with a battery that lasts up to 10 years at low-dose settings, Abbott also claims.
EndoStream Medical has announced that the first patient has been enrolled in the TORNADO-US clinical study in the USA, which will evaluate the Nautilus intrasaccular system in the treatment of cerebral aneurysms. The patient was treated at Mount Sinai Hospital in New York, USA by Icahn Mount Sinai surgeon Tomoyoshi Shigematsu.
“I was impressed by the ease of use and the versatility of the device,” Shigematsu said. “The procedure went smoothly and the patient is recovering well.”
ESTEEMED NEUROLOGIST
Ralph Sacco (pictured) passed away at the age of 65 earlier this year, and a number of prominent neurology and stroke societies subsequently paid tribute to him and his achievements in the field.
Sacco’s obituary in the journal Neurology details that he was the only physician to have served as both the president of the American Heart Association (AHA), from 2010–2011, and the American Academy of Neurology (AAN), from 2017–2019, and the first ever neurologist to serve as president of the AHA as well.
Among those to have paid tribute to Sacco are AAN president Orly Avitzur, who said: “Dr Sacco’s achievements belied his humility—a trait equally appreciated by friends, associates, trainees and patients whose lives and careers he indelibly touched over the years.”
AHA CEO Nancy Brown stated that “Ralph’s death leaves a void in the lives of all who knew him and the organisations he so faithfully served”, while European Stroke Organisation (ESO) president Peter Kelly noted that “he will be remembered as an outstanding clinician-scientist, a role model, a leader, and a friend to many in the field of stroke medicine”.
During his time as a professor of Neurology, and chief of the
Stroke and Critical Care Division, at Columbia University (New York City, USA), Sacco established the Power to End Stroke initiative with the AHA, focusing on stroke prevention in African-American communities, and was the founding principal investigator of the multiethnic Northern Manhattan study (NOMAS), helping to clarify the role of modifiable stroke risk factors across ethnic groups in the USA.
In 2007, he moved to the University of Miami’s Leonard M Miller School of Medicine (Miami, USA), becoming a professor of Neurology and Olemberg Family chair in Neurological Disorders, and chief of the neurology service at Jackson Memorial Hospital, as well as continuing his distinguished work researching stroke epidemiology and health disparities.
Sacco published more than 1,000 peer-reviewed articles across many areas and, in 2019, was made editor-in-chief of the journal Stroke He received numerous honours throughout his career—such as the inaugural Edgar J Kenton III Lecture Award from the American Stroke Association (ASA).
Sacco passed away due to a brain tumour on 17 January 2023. Tributes have noted that he died peacefully at his New York home in the company of family, including his husband Scott Dutcher.
“The enrolment of the first patient in the TORNADO-US clinical study is a major milestone for the treatment of cerebral aneurysms,” added Chris Kellner (Mount Sinai, New York, USA), principal investigator of the TORNADO-US clinical study. “We are excited to be at the forefront of this innovation.”
The Nautilus intrasaccular system is a self-conforming, intrasaccular flow diverter, designed to maximise neck coverage and enhance coil stability, optimising intrasaccular thrombosis and enabling progressive occlusion of the aneurysm. The device is CE-marked and cleared for sale in Europe, but is yet to be approved for sale or distribution in the USA, and is limited by US law to investigational use.
Viz.ai announces realworld study demonstrating clinically relevant time saving with AI platform Viz.ai and TeleSpecialists have announced new data presented at the 2023 International Stroke Conference (ISC; 8–10 February, Dallas, USA) from the VALIDATE study, which demonstrated that hospital utilisation of Viz’s artificial intelligence (AI)powered care coordination platform was associated with a 39.5-minute reduction in patient arrival to time of first contact with a neurointerventionist for potential emergency endovascular treatment.
“The VALIDATE results demonstrate a time improvement in emergency stroke workflow between Viz-enabled and non-Viz-enabled centres that was statistically significant, and highly clinically important,” said Thomas Devlin (University of Tennessee Health Science Center, Memphis, USA), co-author of the study. “The study design allowed for very careful and rigorous insight into exactly how powerful the Viz platform is at expediting treatment for one of the most time-sensitive conditions in all of medicine.”
In the independent VALIDATE study— which analysed data extracted from acute stroke consultations with more than 14,000 patients across 17 US states—the statistically significant improvement in median door-to-neurointerventionist
notification time with AI at Viz-enabled centres occurred regardless of whether the centre in question did, or did not, have thrombectomy capability.
Viz.ai also recently announced a collaboration with the BIOS Clinical Trials Coordinating Center at Johns Hopkins University (Baltimore, USA) to expedite patient enrolment for the BEACH study, which is assessing a novel treatment for intracerebral haemorrhage, and will provide research teams with access to the company’s Viz RECRUIT software for accelerating and improving clinical trial enrolment.
Vesalio announces successful initial use of Neva VS device in USA
Vesalio has announced the successful initial use of its Neva VS device in the USA for the treatment of postaneurysmal subarachnoid haemorrhage (aSAH) cerebral vasospasm.
“We are excited to be the first centre to use the Neva VS device in the USA,” said Rishi Gupta (WellStar Health System, Atlanta, USA). “We have used the device in four patients thus far and have not had to return any of them to the cath lab for further treatment. The Neva VS device is a valuable tool for the management of postaSAH vasospasm.”
As per a press release from the company, Neva VS is the only US Food and Drug Administration (FDA)-approved device for this indication and the only device on the market specifically designed to treat vasospasm.
The Neva VS device is tailored to post-aSAH vasospasm treatment owing to its “smooth and continuous architecture, operator-friendly deliverability of a stent retriever, and an enhanced outward radial force to dilate critically narrowed vessels”, Vesalio’s press release notes. The device has also been determined safe by the recently published VITAL trial, which reported that 93.2% of treated vessels required no retreatment.
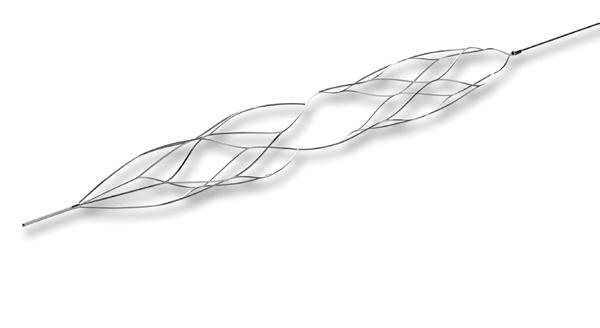
A team from the University of Oklahoma (Norman, USA) has embarked on a five-year research project with the intention of designing a device that can be customised to better treat intracranial aneurysms.
For the project—funded by a US$3.25 million grant from the National Institutes of Health (NIH)—researchers are set to
Dr Sacco’s achievements belied his humility—a trait equally appreciated by friends, associates, trainees and patients whose lives and careers he indelibly touched over the years.”Neva VS device
use advanced biomedical 3D printing to design and create unique devices that can be tailored to the specific geometrical shape, size and location of a specific aneurysm.
Under the direction of Chung-Hao Lee (University of Oklahoma, Norman, USA), the team will target subarachnoid haemorrhages in an effort to improve on current treatment approaches like surgical clip ligation and endovascular coil embolisation.
“The driving problem is, even with this technique [coiling], due to the complexity of the shape, size or geometry of the aneurysm, there is a heightened risk of recurrence,” Lee said. “It is possible that, five or six years after initial embolisation, 20–25% of patients will develop the same issue again. So, it is increasing the corresponding healthcare burden, and may also lead to poor prognosis and even mortality for the patient.
“The overall clinical and translational benefits of our project will be to prevent aneurysm rupture and its induced strokes, which accounts for roughly 15% of new strokes every year, and to decrease the 20% rate of failed cases from the current gold standard. This is an extremely promising area to drive the clinical field forward.”
Phenox, a Wallaby Medical company, has announced the presentation of the primary results of the PROST trial at the International Stroke Conference (ISC; 8–10 February 2023, Dallas, USA).
This randomised trial was conducted to evaluate the safety and efficacy of Phenox’s Preset thrombectomy device, which recently received 510(k) clearance from the US Food and Drug Administration (FDA) for use in the USA. The trial design saw patients randomised to be treated with either the Preset thrombectomy device or the Solitaire revascularisation device (Medtronic).
The PROST primary and secondary endpoints were successfully achieved, and these results led to the FDA’s decision to clear the device for use in the USA—granting it an indication to reduce disability in stroke patients with a persistent, proximal, anterior-circulation large vessel occlusion (LVO), and smaller-core infarcts, who have first received thrombolytic therapy.
“PROST is the first randomised clinical trial comparing a novel versus an established stent-retriever technology, establishing a new scientific benchmark for stroke device trials,” said co-principal investigator of the trial Raul Nogueira (University of Pittsburgh Medical Center Stroke Institute, Pittsburgh, USA). “Our study confirms the overall safety and
efficacy of Preset in treating LVO acute ischaemic stroke patients.”
IRRAS has announced the publication of the first comparative study detailing the use of its novel IRRAflow system, which concludes that the IRRAflow system resulted in favourable clinical outcomes versus passive drainage in the treatment of chronic subdural haematomas (SDHs).
This clinical study was conducted under the guidance of Adnan Siddiqui (University of Buffalo, New York, USA) and colleagues, and has since been published in the journal Operative Neurosurgery
Siddiqui et al also found low complication and revision rates, faster clearance of collected blood, and a statistically significant reduction in rates of catheter infections, across 21 patients treated with IRRAflow as compared to 34 patients treated with passive drainage using an external ventricular drain (EVD).
Additionally, in a subgroup analysis that looked at procedures performed using a burr hole alone, treatment IRRAflow treatments resulted in significantly lower haematoma expansion at discharge and significantly improved brain expansion. Non-significant reductions in duration of catheter placement, total length of hospital stay, and rate of seizure activity, were also observed.
Hyperfine has announced the presentation of new stroke patient follow-up data regarding the use of the Swoop system— which it claims is the world’s first US Food and Drug Administration (FDA)-cleared portable magnetic resonance imaging (MRI) system—at the 2023 International Stroke Conference (ISC; 8–10 February, Dallas, USA).
“We believe these observations set the stage for using portable MRI in the dynamic environment of acute stroke intervention, where patients are at high risk for ongoing injury,” said Kevin Sheth (Yale School of Medicine, New Haven, USA), one of the study’s leading investigators.
In this single-centre study, conducted between December 2021 and August 2022, researchers performed bedside, portable MRI exams in a standard, non-magnetically shielded interventional radiology suite following mechanical thrombectomy procedures, with clinical and research staff present. They found that
ultra-low-field portable MRI can facilitate a post-treatment baseline for stroke patients who undergo a thrombectomy, evaluating the impact of potential changes in blood pressure and heart rate on ongoing brain injury.
According to the company, these findings are significant because brain imaging is not routinely available, particularly with conventional MRI, following mechanical thrombectomy— potentially precluding accurate infarction assessments.
[Equipo de Neurocirugía Endovascular y Radiología Intervencionista], Buenos Aires, Argentina).
JMIR Publications has announced the expansion of its journal portfolio with JMIR Neurotechnology (JNT)—an open-access, peer-reviewed journal focused on the intersection between clinical neuroscience and technology to prevent, diagnose, and treat neurological disorders.
Neurosurgeon Pieter Kubben (Maastricht University Medical Center, Maastricht, The Netherlands), the editorin-chief for this new journal, said: “JNT aims to be a platform where applied human research can connect patients, caregivers and information engineers active in any neurological domain where patient benefit is clear for all involved. JNT is not interested in fundamental neuroscience nor in animal research.”

Gentuity has announced the first human use of the Vis-M high-frequency optical coherence tomography (HF-OCT) imaging system and probe. As per a company press release, this represents a “significant technological advance for the field of neurointervention”, making highresolution intravascular imaging in the brain possible.
The procedures were performed in the neuroangiography suite, with a minimally invasive, endovascular approach, at St Michael’s Hospital (Toronto, Canada) by Vitor Mendes Pereira. These first-in-world experiences were also presented at the ABC WIN Seminar (15–20 January, Val d’Isère, France).

“This is an incredibly exciting milestone,” said Pereira. “The direct visualisation technology we evaluated here offers unprecedented potential in the diagnosis and treatment of aneurysms, stroke, intracranial atherosclerotic disease (ICAD) and other neurological pathologies. The system and imaging probes performed very well, integrating with our workflow seamlessly, and provided us with important information that we cannot obtain with any other technology—very impressive.”
Gentuity’s Vis-M neuro-intravascular imaging probe has been designed to specifically address the challenges of navigating through the tortuous and delicate blood vessels of the brain. This enables in vivo, micron-level resolution at 250 frames per second, providing highresolution images of the arterial wall and interventional therapies, and beyond the vessel wall too.
“Because of neuro HF-OCT, we will now be able—for the first time—to analyse and better understand different pathologies, and the results of our neurointerventional therapies. It is a real gamechanger in the cerebrovascular field,” said Pedro Lylyk (ENERI
As per a press release, JNT pragmatically defines neurotechnology as the use of information technology to diagnose or treat chronic neurological disease—and its hope is to foster the explicit linking of these two domains into a merged domain and a single, coherent neurotechnology community.
JMIR claims it wants to connect these typically separate domains and intends to do so, in part, by including a short, author-written statement referred to as a ‘handshake box’ with every article that concisely articulates either the technical or clinical implications of their findings.
MedRhythms’ novel digital intervention meets primary endpoint in stroke trial MedRhythms has announced that the company’s pivotal trial for MR-001, a novel digital intervention being developed to treat gait deficits in chronic stroke, has been successfully completed and met its primary endpoint of gait-speed improvements.
The multicentre randomised controlled trial was conducted at eight of the top rehabilitation hospitals and research institutions in the USA, according to a MedRhythms press release. It included adult chronic stroke survivors who participated in 30-minute sessions, three times per week, over a five-week intervention period. The study participants either used MR-001 or were part of an active control group.
MedRhythms intends to submit these “important clinical data” for peer review in a scientific journal, and to present the data at a major conference later this year, the release also notes.
MR-001—which is in development to treat chronic stroke gait deficits—is anticipated to be the first product the company brings to market. Other investigational digital therapeutics MedRhythms is currently working on to target gait deficits include MR-004 for multiple sclerosis; MR-005 for Parkinson’s disease; and MR-010 for postacute stroke.
Scientia receives US FDA clearance for Aristotle Colossus macrowire Scientia Vascular has announced the US Food and Drug Administration (FDA) 510(k) clearance of the Aristotle Colossus microwire, which the company claims is the only 0.035inch macrowire currently indicated for neurovascular intracranial use.
Like its predecessors—the Aristotle 18 and Aristotle 24—Aristotle Colossus utilises “breakthrough microfabrication design technology”. According to a Scientia press release, this advancement in manufacturing allows for a soft, atraumatic tip and is designed to support the tracking of large bore catheters to the treatment site, and drive superior navigability of distal, tortuous anatomies, in both ischaemic and haemorrhagic stroke care, the release notes.
“We are grateful to be one of the first labs in the world to evaluate the Aristotle Colossus’ performance,” said David Fiorella (Stony Brook Cerebrovascular Center, Stony Brook, USA). “Colossus could be a real gamechanger for stroke catheter navigation. In my initial experience, the Colossus navigated challenging neurovascular anatomy with precise torque control and provided solid support, allowing us to seamlessly and safely track aspiration catheters into both proximal and distal vessels. I anticipate that Colossus will be our wire of choice for most thrombectomy procedures going forward.”
Scientia states that, despite the large diameter of its microfabricated nitinol tube, the Aristotle Colossus can safely navigate the neurovascular anatomies—similarly to a much smaller guidewire—and offers support to facilitate the tracking of catheters with a ≥0.038-inch inner diameter, in an effort to eliminate the use of an additional intermediate catheter.
Stryker launches “state-ofthe-art” neurovascular lab to accelerate stroke care innovation
Stryker recently opened its Neurovascular (NV) lab—a “stateof-the-art” laboratory designed to accelerate stroke-related innovation in the Asia-Pacific region.
Located within the Stryker Global Technology Center (SGTC) at International Park in Gurgaon, India, the Keystone Suite will enable collaboration between customers, product development engineers, cross-functional teams, and other key stakeholders, according to a company press release.
The release further notes that Stryker’s NV lab intends to offer an “ideal environment” for medical education, research and development,
and customer engagement activities for improving patient outcomes.
The lab has three main components: a neurovascular catheterisation laboratory designed to mimic the hospital treatment experience, with the latest imaging and communication equipment; a performance lab with hands-on stations outfitted with flow models, neurovascular simulators and 3D-model-printing capabilities; and planned space for physician interaction.
The CELLO II balloon guide catheter (Fuji Systems Corporation) has received 510(k) premarket approval from the US Food and Drug Administration (FDA), and can now be marketed in the USA and other FDAregulated territories for peripheral and neurovascular indications.
Having been deemed “substantially equivalent” to a legally marketed predicate product—
Fuji’s FDA-approved CELLO balloon guide catheter—the device was cleared as a Class II percutaneous catheter on 9 December 2022.
The CELLO II balloon guide catheter is indicated for use in facilitating the insertion and guidance of intravascular catheters into a selected blood vessel in the peripheral and neurovasculature systems. The balloon provides temporary vascular occlusion during these and other angiographic procedures.
In its 510(k)-approval notification, the FDA details that “no clinical testing was deemed necessary to support this premarket notification” owing to the design similarities between CELLO II and the predicate device—as well as the fact that the indications for use, and intended patient population and anatomical sites, are all the same between the two products.
While CELLO is a trademark of and is manufactured by Japan-based company Fuji Systems Corporation, it is distributed in Europe and the USA by Medtronic.
Methinks has announced receipt of a CE mark for its artificial intelligence (AI)-based medical imaging software, Methinks Stroke Suite, following a milestone year of development progress enabling commercialisation in Europe and assisting in emergency settings for the benefit of acute stroke patients.
Methinks Stroke Suite is the first CE-
marked medical device that assists in finding large vessel occlusions (LVOs), both hyperdense and not, a company press release claims.
Working in parallel with hospitals’ existing clinical workflows, this radiological, computer-aided triage and notification system uses AI algorithms to identify suspected LVO on non-contrast computed tomography (NCCT) and computed tomography angiography (CTA) images. The software also has the ability to detect intracerebral haemorrhages on NCCT images.
“Early detection and diagnosis are crucial to improving a patient’s outcomes,” said Tudor Jovin (Cooper University Health Care, Camden, USA). “This disruptive technology is capable of detecting LVO from NCCT images and will undoubtedly have an impact on our clinical practice due to the potential of significantly shortening the time from stroke onset to reperfusion in a large number of patients with LVO stroke. As an interventional neurologist, I look forward to having the product available in the USA soon.”
The Methinks Stroke Suite has been validated across 3,800 cases from three different stroke reference hospitals in Europe, demonstrating high sensitivity and specificity capabilities, and an average time to notification of 87 seconds.
Perfuze announces US FDA clearance and first US clinical use of Millipede 088 access catheter
Perfuze has secured its first product clearance from the US Food and Drug Administration (FDA) for the company’s Millipede 088 access catheter. The first US clinical procedures with Millipede 088 were also successfully performed by physicians at Stony Brook University Hospital in New York, USA and the University of Pittsburgh Medical Center Stroke Institute in Pittsburgh, USA.
The Millipede 088 access catheter is designed to facilitate the safe insertion and guidance of microcatheters for neurointerventional or diagnostic procedures.

With a physician-led approach to device innovation, Perfuze is working to advance all aspects of stroke treatment from vessel access through to thrombectomy, as per a company press release. This 510(k) clearance is “a major milestone for the company and a testament to its commitment to advancing the field of neurovascular care”, the release states.
In 2023, Perfuze plans to move towards initiating a US pivotal study of its Millipede system for the revascularisation of patients with acute ischaemic stroke.
Brainomix receives US FDA clearance for flagship stroke AI imaging software

Brainomix has announced that its 360 e-ASPECTS tool for stroke has received US Food and Drug Administration (FDA) clearance, enabling the company to introduce its cutting-edge artificial intelligence (AI) imaging platform to stroke centres in the USA.
With deployments across more than 30 countries, Brainomix’s AI stroke software has been studied and validated in over 60 publications, a press release notes. The Brainomix 360 stroke platform is a collection of tools that use advanced AI algorithms to support doctors by providing real-time interpretation of brain scans, helping to guide treatment and transfer decisions for stroke patients, and allowing patients to be treated in the right place at the right time.
Powered by explainable AI, the 360 e-ASPECTS tool assesses non-contrast computed tomography (CT) scans to automatically generate an Alberta stroke programme early CT (ASPECT) score and features a unique overlaid heatmap to visually assist clinicians in assessing the output.
Recent studies having seen the implementation of Brainomix’s software validated by faster treatments (reduced door-in-door-out times) and improved outcomes (greater number of patients achieving functional independence after stroke). The company has an established US field team that will introduce the platform to stroke centres across the country and provide dedicated ongoing support, the release also details.
Corindus has been rebranded to Siemens Healthineers Endovascular Robotics and will sit as a dedicated business within the Advanced Therapies area of Siemens Healthineers, the company has announced.
This brand unification is the final step of the company integration process that commenced in 2019 with the acquisition of Corindus by Siemens Healthineers, according to a press release. The aim of the Endovascular Robotics business is to advance interventions with robotics, and change the way that care is delivered through innovations that enhance physician technique and bring precision to
interventional procedures. Siemens Healthineers Endovascular Robotics says it will continue to offer the CorPath GRX system to support endovascular procedures while working to “revolutionise” the treatment of emergent conditions by developing technologies to provide specialised and timely medical care to more patients around the world.
Infinity Neuro announced recently that its Inspira aspiration catheters have received CE-mark approval as a Class III medical device and are now commercially available in Europe.This is the first offering from Infinity—a company that plans to launch a full range of products for the treatment of ischaemic and haemorrhagic stroke throughout 2023, and beyond, a press release states.
The Inspira aspiration catheters are “physician-inspired” to deliver next-level navigation and aspiration performance; designed to access targeted vessels easily, restore cerebral
6–7 April
Stroke Live Course (SLICE) Next Frontiers
Virtual masterandfellow.com/slice/nf

11–14 April
World Live Neurovascular Conference (WLNC) Rio de Janeiro, Brazil wlnc.org/en/WLNC-2023.html
blood flow quickly, and retrieve clots in patients experiencing acute ischaemic stroke due to a large vessel occlusion.
The catheters are indicated for injection of intravascular fluids; introduction of interventional devices into the peripheral and neuro vasculature; and removal/aspiration of soft emboli and thrombi from the arterial system, including the peripheral and neuro vasculature.
Infinity claims that this constitutes the first neurovascular device approved under the new and more rigorous CE-certification process under the European Medical Device Regulation (MDR) as an original submission. The European commercial launch of these devices is now underway.

Imperative Care has announced that the US Food and Drug Administration (FDA) has finalised 510(k) clearance of its Zoom RDL radial access system— the company’s latest innovation in elevating stroke care and the “first
21–24 April
American Association of Neurological Surgeons (AANS) Annual Scientific Meeting
Los Angeles, USA aans.org/meetings
22–27 April
American Academy of Neurology (AAN) Annual Meeting
Boston, USA aan.com/events/annual-meeting
radial access platform developed specifically for ischaemic stroke treatment”, as per a press release.
In addition to this new component of Imperative’s Zoom stroke solution, the company has also announced the successful completion of the first inhuman case using Zoom RDL. The case in question was performed by Justin Singer (Corewell Health, Grand Rapids, USA).
Zoom RDL was used during treatment of an acute stroke for a patient with a complex anatomy that would have made femoral access challenging. It provided 0.088inch intracranial access from the radial artery, allowing the physician to remove the clot using a Zoom aspiration catheter and achieve complete revascularisation in less than 20 minutes.
“As we continue to advance how we care for our stroke patients and see the overwhelming benefit of performing radial interventions, it is remarkable to have a company like Imperative Care respond with much-needed tools for a radial approach,” said Singer. “I am impressed with the performance of the Zoom RDL in my initial experience and look forward to continuing a patientfirst approach in my stroke practice. The addition of this new technology will allow me the first capability to choose the best access approach for
each patient without limitations.”
Zoom RDL features an extended hydrophilic coating and the longest optimised vessel dilator on the market—the company claims— providing a smooth introduction into the radial artery. The device’s engineered support profile is also intended to give physicians more control over thrombectomy procedures.

The European Union’s (EU) Council of Ministers has resolved to extend the deadline for product certification under the Medical Device Regulation (MDR). Device producers will now have until 31 December 2027 for higherrisk devices, and 31 December 2028 for medium- and lower-risk devices to meet the legal requirements.

Having been passed on 7 March, this extension of the transition period will enter into force on the day of its publication in the Official Journal of the European Union
25–27 April
Charing Cross (CX) Symposium London, UK cxsymposium.com
29 April–3 May
American Society of Neuroradiology (ASNR) Annual Meeting Chicago, USA asnr.org/annualmeeting
24–26 May
European Stroke Organisation Conference (ESOC) Munich, Germany eso-stroke.org
5–7 June

LINNC Paris 2023 Paris, France linnc.com/Course-information/ LINNC-Paris-2023
19–23 June
The European Course in Minimally Invasive Neurological Therapy (ECMINT) 5.1 Oxford, UK esmint.eu/ecmint
1–4 July
Congress of the European Academy of Neurology (EAN) Budapest, Hungary ean.org/meet/congresses/ future-congresses