Featured in this issue:

Paediatric INR: Challenges and opportunities
page 4
Is it time to re-evaluate mRS as a clinical study endpoint?
page 13

Profile Christophe Cognard
page 16


Featured in this issue:

Paediatric INR: Challenges and opportunities
page 4
Is it time to re-evaluate mRS as a clinical study endpoint?
page 13

Profile Christophe Cognard
page 16

Coil embolisation of smaller intracranial aneurysms—those less than 5mm in size—has been found to be a safe approach, as per data presented for the first time at the 2024 Society of NeuroInterventional Surgery (SNIS) annual meeting (22–26 July, Colorado Springs, USA). Delivering late-breaking results from the COAST study, J Mocco (Mount Sinai Health System, New York, USA) detailed that coiling was associated with low rates of clinically significant stroke or haemorrhage alongside “impressive” adequate occlusion outcomes.
“Is it safe to coil small aneurysms?” Mocco initially queried.
“When I was training, I had a senior neurointerventionist tell me that it is not safe and aneurysms smaller than 5mm are too dangerous because there’s not enough room to fully deploy a coil. But, last year, when we did our polling surveys at SNIS, we asked if it is reasonable to treat small aneurysms [3–6mm], and 95%-plus said that it was generally reasonable to do […] while only 4% or so said we really shouldn’t do this.”
Mocco went on to note that a similar polling question—this time homing in on aneurysms 4–5mm in size—was put to attendees of the 2024 SNIS meeting, indicating once again that the community believes interventional treatment in these cases is “safe”. COAST, which was a prospective, single-arm, multicentre study, sought to provide a more scientific and therefore definitive answer to these questions.
Across 15 centres in the USA and Canada, and over the course of 5.3 years, the study enrolled a total of 300 adult patients (mean age, 56 years; 76% female) with small aneurysms (≤4.9mm)
deemed appropriate for endovascular treatment. Mocco noted that 109 patients (36.3%) had ruptured aneurysms. Enrolled patients were treated using the US Food and Drug Administration (FDA)-cleared Hypersoft family of embolisation coils (Microvention/Terumo), and followed up immediately after occlusion of their aneurysm, as well as at six and/or 12 months post-occlusion.
COAST’s primary safety endpoint was patients’ freedom from new, imaging-confirmed, postprocedural ischaemic stroke and intracranial haemorrhage associated with a four-point worsening on the National Institutes of Health stroke scale (NIHSS) within 48 hours of treatment, or any new aneurysmal subarachnoid haemorrhage secondary to the treated aneurysm. Its primary efficacy endpoint was occlusion with a Raymond-Roy grading scale (RRGS) score of 2 or better on follow-up angiography performed more than 150 days post-embolisation that did not
Continued on page 2
New RCT data elucidate role for tenecteplase in stroke care page 22
THE EUROPEAN SOCIETY OF Minimally Invasive Neurological Therapy (ESMINT) has formalised two agreements in acknowledgement of its shared goals and interests with the national neuroradiology societies in France and Germany.
On 6 June 2024, ESMINT announced it had signed a memorandum of understanding (MOU) with the German Society of Neuroradiology (DGNR) to define joint actions, achieve optimal outcomes and enhance the visibility of both organisations.
The MoU was signed by Zsolt Kulcsár (Zürich, Switzerland) and Ansgar Berlis (Augsburg, Germany)— presidents of ESMINT and DGNR, respectively—and ESMINT treasurer Christian Taschner (Freiburg, Germany).
In addition, on 26 June, ESMINT announced a similar MOU with the French Society of Neuroradiology (SFNR), establishing a formal collaboration to enable “the highest standards of patient care”. The agreement was signed by Kulcsár, Taschner, and SFNR president Hubert Desal (Nantes, France).
These MOUs will provide DGNR and SFNR members with a 20% discount relating to any category of ESMINT membership, and are intended to ensure mutual access to both societies’ scientific and membership platforms.

Continued from page 1

require retreatment, while key secondary endpoints included neurological morbidity/mortality evaluated at >150-day angiographic follow-up, and one-year retreatment rates.
Turning to the study’s results, Mocco reported that 99.3% of patients achieved the primary safety endpoint, with a “very low” rate of periprocedural stroke or haemorrhage that affected the patients’ outcomes being observed. In addition, regarding the primary efficacy endpoint in COAST, Mocco relayed a “quite impressive” 84% rate of adequate occlusion not requiring retreatment—also noting that the “actual” RRGS ≤2 rate, when including patients who did undergo retreatment, was even higher.
Core lab-adjudicated imaging outcomes in the study revealed a 69% rate of initial adequate occlusion, with RRGS ≤2 being observed in 76.1% of ruptured and 64.4% of unruptured aneurysms. And, at six- and/or 12-month followup, these rates rose to 89.8% (ruptured, 81%; unruptured, 94.4%). Mocco commented that these rates are higher than those typically seen across published aneurysm coiling data, perhaps owing to the fact that these were small aneurysms. Lastly, touching on secondary endpoints, the presenter reported that rates of mortality and modified Rankin scale (mRS) 3–5 among unruptured aneurysm patients were both 1.2%, leading to a combined long-term disability-mortality rate of just 2.4%, while 6% of patients in COAST underwent retreatment, with 5.3% being retreated within one year and only two patients (0.7%) requiring a second retreatment.
“It does appear that the coiling of aneurysms that are less than or equal to 4.9mm [in size] carries a very low rate of periprocedural stroke or haemorrhage causing neurological deficit—and I think this is important, because it gets to the heart of that question of if it’s safe to do this,” Mocco concluded, also reemphasising the “excellent” delayed occlusion rates observed in COAST that “stand out” when compared against the existing coiling literature.
Speaking to NeuroNews after his talk, Mocco posited that these data provide evidence that—in those cases where treatment is warranted—coil embolisation remains an “excellent option” for aneurysms that are smaller than 5mm.
“The age-old adage that small aneurysms are too high-risk
to embolise with coils appears to be proven untrue, at least when using modern coil technology,” he added. “Moving forward, patients with small aneurysms, with risk profiles that indicate treatment, can avoid more invasive craniotomies.”
Subsequent to Mocco’s presentation, NeuroNews also caught up with the SNIS’ outgoing and incoming presidents to discuss the significance of COAST and its findings.
“The results of the COAST study are indeed quite impactful for a variety of reasons,” said Mahesh Jayaraman (Brown University, Providence, USA), whose yearlong stint as SNIS president came to an end at the society’s 2024 meeting. “First and foremost, we see that the coiling of aneurysms is indeed safe and effective—even in small aneurysms. As Dr Mocco indicated in his presentation, it was sometimes thought that treating these small aneurysms with coiling may be dangerous, but COAST demonstrated remarkable safety and efficacy. Secondly, it is reassuring to know that, while we have made great strides with newer treatment options including flow-diverting devices and intrasaccular flow disruption, our tried and true method of coiling was very effective in these small aneurysms. Ultimately, it is our patients who benefit from knowing that coiling is a very safe and effective treatment option for small aneurysms. There are certainly many aspects to making a treatment decision in patients with aneurysms and we encourage patients to consult with a neurointerventionist to discuss these options.”
Similar points were conveyed by new SNIS president Johanna Fifi (Mount Sinai Hospital, New York, USA), to whom Jayaraman handed over the baton in July.
“COAST shows that coiling of these aneurysms is safe and should be a primary treatment tool when feasible,” Fifi commented. “However, the decision to treat or not to treat in small, unruptured aneurysms is more nuanced, and conservative management should be carefully weighed and discussed with the patient prior to decision making. In respect to this study’s applicability to general practice, I think we should think along the lines of the relative risk of treatment versus morbidity and mortality from the natural history [of the disease]. COAST has shown that the treatment of small aneurysms can be accomplished by coiling with these coils at a very low complication rate. We know that the biggest divider or risk of the natural history of aneurysms is the rupture status. So, in ruptured aneurysms— which were about a third of the patients in the study—where the risk of rebleeding is quite high, this study demonstrates that treatment by coiling is safe and should, in my opinion, be preferred when feasible to more invasive treatment. For unruptured aneurysms, there is more nuance. We have to carefully weigh the small risk of the patient’s aneurysm causing issues with the comparable small risk of coiling. This should be a tailored approach, best determined after careful discussion of the options and risks with the patient.”
As alluded to by Fifi, some physicians may maintain reservations regarding the coiling of small aneurysms and continue to favour imaging-based follow-up, even in light of COAST’s positive findings, with these low procedural complication rates potentially still outweighing those carried by the condition’s natural history alone.
Editor-in-chief: Prof Philip M Meyers | Publisher: Stephen Greenhalgh
Content director: Urmila Kerslake | Global sales director: Sean Langer
Editor: Jamie Bell jamie@bibamedical.com | Editorial contribution: Jocelyn Hudson
Design: Terry Hawes, Josh Lyon and David Reekie
Advertising: Michael Broughton michael@bibamedical.com
Subscriptions: subscriptions@bibamedical.com
Published by: BIBA News, which is a subsidiary of BIBA Medical Ltd BIBA Medical, Europe, 526 Fulham Road, Fulham, London, SW6 5NR, United Kingdom Tel: +44 (0) 20 7736 8788 BIBA Medical, North America, 155 North Wacker Drive, Suite 4250, Chicago, IL 60606, United States Tel: +1 708-770-7323
Printed by: Buxton Press. Reprint requests and all correspondence regarding the newspaper should be addressed to the editor at the United Kingdom address. © BIBA Medical Ltd, 2024. All rights reserved. neuronews linkedin.com/company/neuronews/ @NN_publishing
n POTENTIAL LINK
FOUND BETWEEN GASTROINTESTINAL SYNDROMES AND BRAIN ANEURYSM RISK:

Data analyses led by Georgios Sioutas and Jan-Karl Burkhardt (both Philadelphia, USA), presented recently at the Society of NeuroInterventional Surgery (SNIS) annual meeting (22-26 July, Colorado Springs, USA), have revealed a potential connection between certain gastrointestinal syndromes, and the formation and rupture of intracranial aneurysms.
For more on this story, go to page 5.
n “HERMES-STYLE COLLABORATIVE” ON THE CARDS FOLLOWING RECENT SUCCESSES FOR MMA EMBOLISATION: The interventional management of chronic subdural haematoma was in the spotlight again at this year’s LINNC Paris meeting (3-5 June, Paris, France), with delegates discussing trial design, anaesthesia approaches, treatment timings and more.

For more on this story, go to page 8.
n NEW DATA PROVIDE “COMPELLING EVIDENCE” ON STENTING VERSUS MEDICAL THERAPY IN INTRACRANIAL ATHEROSCLEROTIC STENOSIS PATIENTS: Among a plethora of new data presented at the 2024 European Stroke Organisation Conference (ESOC; 15-17 May, Basel, Switzerland) was an update given by Peng Gao (Beijing, China) on the CASSISS trial. Gao relayed that, as per seven-year findings from the study, stenting does not appear to confer notable benefits compared to medical therapy in patients with symptomatic, severe intracranial atherosclerotic stenosis. For more on this story, go to page 21.
Subscribe here

If you have comments on this issue or suggestions for upcoming editions write to jamie@bibamedical.com

Arsenal Medical has announced that NeoCast—a first-of-its-kind, shear-responsive liquid embolic material designed for deep distal penetration—met its primary feasibility and safety endpoints in the open-label, multicentre, prospective EMBO-01 clinical trial. These data were presented at the 2024 Society of NeuroInterventional Surgery (SNIS) annual meeting (22–26 July, Colorado Springs, USA).
“NEOCAST HAS THE POTENTIAL TO BE A gamechanger for liquid embolics,” said Lee-Anne Slater (Monash Health, Melbourne, Australia), the principal investigator for the EMBO-01 trial who presented findings at SNIS 2024. “The product was easy to handle and performed consistently and reproducibly during injection while providing excellent visibility during and post-procedure, unlike currently available options. Early results show that NeoCast has the potential to fill a treatment gap with a tool that’s straightforward for clinicians to use and will ultimately benefit patients; I am encouraged by its possibilities in other middle meningeal artery indications.”
An Arsenal press release states that NeoCast “stands alone” in clinically demonstrating predictable and well-
controlled vascular occlusion. The company describes NeoCast as a next-generation, solvent-free, nonadhesive liquid embolic that can enable the significant distal penetration of hypervascular brain tumours.
The late-breaking data presented at the SNIS meeting, according to Arsenal, are further bolstered by an additional presentation highlighting preclinical study results showing that it occluded approximately five times more vessel branches with improved radiopacity, compared to the market-leading liquid embolic, in swine kidneys.
“These emerging preclinical and clinical data are exciting, as they clearly demonstrate the potential for NeoCast to be an optimal liquid embolic agent for the treatment of neurovascular conditions that require

Carmen Parra-Fariñas (Toronto, Canada) discusses key factors that distinguish the growing field of paediatric interventional neuroradiology (INR) from adult neurovascular disease care.
Neurovascular pathologies are a significant cause of brain injury in the paediatric population, resulting in substantial mortality and devastating physical and mental effects on survivors. The emotional and economic costs impose lifelong consequences on patients, families and society as a whole.
Anatomically and physiologically, children differ from adults. Aetiologies, natural histories and treatment strategies are disparate compared to adult homologue diseases. Neuroendovascular surgical interventions in children demand not only a thorough understanding of neurovascular anatomy, pathology and haemodynamics but also manual dexterity—leading to a steep learning curve. The psychological challenges involved in treating children with lifethreatening diseases require approaches to help reduce distress for children and their families as well. These conditions necessitate care in high-volume paediatric
centres by a dedicated neurovascular care team with expertise in diagnosis and management, through the antenatal period, adolescence and early adulthood. Numerous recent advances in our understanding of these disorders, as well as in surgical techniques and devices, have improved outcomes and opened doors to treat conditions previously considered untreatable. Multidisciplinary collaboration and innovative research will further enhance our current understanding of paediatric neurovascular diseases and create new treatment paradigms that will be at the forefront of the discipline.
Paediatric neurointervention encompasses a broad pathological spectrum including age- and physiology-specific conditions at foetal, neonatal, infantile, toddler and school-going ages. Furthermore, the haemodynamic component of these diseases varies greatly. Broadly,
distal penetration of the targeted vasculature,” said EMBO-01 medical monitor Dave Fiorella (Stony Brook University Medical Center, Stony Brook, USA). “Middle meningeal artery embolisation for the treatment of chronic subdural haematoma [cSDH] is the application that immediately comes to mind. The existing clinical data have suggested that distal penetration into the meningeal circulation is associated with faster and more complete cSDH resolution.
“Moreover, this agent has the additional advantage of not incorporating an inflammatory solvent or inducing a thermal reaction upon polymerisation. This characteristic should allow NeoCast embolisation procedures to be carried out under conscious sedation rather than general anaesthesia in many or most patients, as we would expect that the agent would not create any pain or discomfort during the infusion.”
NeoCast has the potential to be a gamechanger for liquid embolics.”
Lee-Anne Slater
paediatric neurovascular diseases can be divided into vaso-occlusive lesions, haemorrhagic lesions, drivers of hydrovenous dysfunction, and drivers of neonatal cardiopulmonary failure. The clinical presentation, diagnosis and treatment of neurovascular disorders in children require a comprehensive understanding of specific neurovascular anatomy, aetiologies, pathomechanisms, and physiology, which differ vastly from those in adults. The psychological challenges of treating children with complex pathologies demand a uniquely tailored support approach. Risk-benefit decisions, ethical considerations and family-oriented care are paramount drivers of care in a paediatric setting. Conversely, persistently encountering intricate cases and observing the resilience of children and families amidst their suffering instils in the healthcare team a profound sense of admiration and gratitude. The optimal and holistic management of these diseases in children therefore requires a multidisciplinary team of paediatric neurovascular experts. Moreover, exposure of neurointerventional operators to paediatric endovascular diseases and procedures is limited outside of large paediatric centres. Treatment planning and technical considerations are key to success. Special considerations for paediatric patients include sedation and anaesthesia, radiation dosage, contrast agents, equipment and device optimisation, and vascular access.
In recent decades, significant advances have greatly improved our understanding and awareness of paediatric neurovascular diseases. There has been substantial progress in neuroimaging, including quantitative magnetic resonance imaging for assessing vascular anatomy and brain blood flow, leading to advanced microsurgical and endovascular techniques to restore flow or repair vascular lesions. Rapid acceleration of device technology
has increased the repertoire of techniques and strategies that can be safely employed in paediatric procedures. Several diseases that previously had dismal outcomes are now treated successfully by dedicated paediatric neurointerventionists with a better understanding of these complex conditions and their many clinical facets. Paediatric neurovascular clinical developments have also been supported by remarkable discoveries in vascular genetics, sparking discussions about previously inconceivable medical treatments. Recent advances in intrauterine endovascular treatment for high-flow vein of Galen malformations, and the potential for medical treatment based on genetic evaluation and vascular anomaly blood samples, represent significant progress and open exciting future possibilities. Additionally, incorporating 3D-printing technology into treatment planning and training offers new opportunities for specialised education in this field—which is difficult to achieve outside high-volume paediatric institutions.
Multidisciplinary collaboration and decision-making for every child, in a prompt fashion, as well as research and education for novel diagnostic and therapeutic strategies to improve disease outcomes and the patient-family experience, are key. Given the necessity of evaluating and treating neurovascular diseases in children—which span a wide diversity of genetic, developmental, inflammatory and traumatic causes— paediatric neurointervention teams have the potential to lead in generating, advancing and translating novel diagnostic and therapeutic techniques for these diseases.
Carmen Parra-Fariñas is an interventional and diagnostic neuroradiologist at The Hospital for Sick Children, and an assistant professor and clinician investigator at the University of Toronto, in Toronto, Canada.
The author declared no relevant disclosures.
Two data analyses presented at the recent Society of NeuroInterventional Surgery (SNIS) annual meeting (22–26 July, Colorado Springs, USA) have revealed new insights on the role of rescue stenting following failed mechanical thrombectomy, with one indicating parity between different stent types and the other suggesting minimal benefits compared to medical management.
DURING A LATE-BREAKING
abstract session at SNIS 2024, Mahmoud Mohammaden (Emory University, Atlanta, USA) presented a post-hoc analysis of the SAINT study—a multicentre collaboration involving prospectively collected databases, which concluded that rescue stenting results in better functional outcomes as well as comparable safety versus procedure termination after failed thrombectomy in both anterior- and posterior-circulation stroke patients.
The analysis delivered by Mohammaden used data from SAINT to specifically compare balloonmounted versus self-expandable stenting approaches, with 329 patients enrolled consecutively across 15 comprehensive stroke centres in the USA meeting its inclusion criteria. Overall, there were 125 patients treated with a balloonmounted stent—including 56.8% with drug-eluting stents and 39.2% with bare-metal stents—and 204 treated with a self-expandable stent, most commonly Enterprise (Cerenovus/J&J), Wingspan or Neuroform Atlas (both Stryker).
“Interestingly, there was no difference in the procedure duration between both
groups,” Mohammaden relayed, “and, also, there was no difference in terms of balloon angioplasty—reflecting the fact that ‘newer’ interventionists tend to use balloon angioplasty for stenting to avoid long-term antiplatelet use.”
Arriving at the analysis’ primary endpoint finding—successful final reperfusion defined as modified thrombolysis in cerebral infarction (mTICI) ≥2b—the presenter noted that balloon-mounted stenting was associated with increased likelihood of achieving a higher degree of reperfusion on the mTICI scale compared to selfexpandable stenting (adjusted common odds ratio [aOR], 2.2; p=0.003), as well as higher rates of mTICI ≥2 reperfusion (aOR, 6.17; p=0.001).
However, these improved technical outcomes did not translate into better clinical results, as 90-day modified Rankin scale (mRS) shift findings, and rates of mRS 0–2 and 0–3, were all statistically similar between the two groups. In parallel, the rates of procedural complications, symptomatic intracranial haemorrhage (sICH) and mortality were ultimately comparable between groups too. The investigators
also determined that there was no treatment-effect modification of stent type on the final reperfusion grade or mRS score shifts across the study’s prespecified subgroups—including age, stroke aetiology and occlusion site.
“In conclusion, in patients who failed mechanical thrombectomy and underwent rescue stenting, our study showed that balloon-mounted stents had higher rates of reperfusion compared to self-expandable stents,” Mohammaden noted. “However, the likelihood of disability, and good and fair outcomes as well as the safety measures, were comparable in both groups.”
A similar topic was the focus of the session’s next talk, with multicentre findings on the safety and efficacy of post-thrombectomy rescue stenting being presented by Kasra Khatibi (University of Southern California, Los Angeles, USA) on behalf of Humain Baharvahdat (Rothschild Foundation Hospital, Paris, France) and colleagues. Via a retrospective cohort study conducted between 2012–2024, investigators compared rescue stenting

There is a potential connection between a diagnosis of certain gastrointestinal (GI) syndromes, and the formation and rupture of intracranial aneurysms, according to research presented at the 2024 Society of NeuroInterventional Surgery (SNIS) annual meeting (22–26 July, Colorado Springs, USA).
IT HAS PREVIOUSLY BEEN QUESTIONED whether GI syndromes may be connected to the formation and rupture of brain aneurysms and, in a study titled “The gut-brain axis: a nationwide database analysis of gastrointestinal syndromes preceding a diagnosis of intracranial aneurysms”, researchers from the University of Pennsylvania (Philadelphia, USA) found that certain digestive symptoms and diagnoses may precede the formation and rupture of these aneurysms.
The team analysed data from 72,545 individuals with ruptured intracranial aneurysms, 46,748 individuals with unruptured aneurysms, and matched controls, looking for patients who had been diagnosed with GI disorders like gastro-oesophageal reflux disease, irritable bowel syndrome (IBS) and diarrhoea before their intracranial aneurysm diagnosis. Then, they validated their findings in a cohort study with a fiveyear timeframe.
The researchers found that GI syndromes and
appendectomy were associated with both ruptured and unruptured intracranial aneurysm cases. Specifically, patients with intracranial aneurysms who had been previously diagnosed with difficulty swallowing (dysphagia), diarrhoea and constipation were more likely to experience both aneurysm formation and rupture—leading to haemorrhagic stroke.
Separately, they found that patients with intracranial aneurysms who had been diagnosed with reflux disease, chronic stomach pain and bloating (known as functional dyspepsia), and IBS without diarrhoea, were more likely to only experience intracranial aneurysm formation without rupture.
“There is evidence from animal studies suggesting a relationship between the gut microbiome and various inflammatory diseases, including the development and rupture of intracranial aneurysms,” said Georgios Sioutas (University of Pennsylvania, Philadelphia, USA), the primary author of the present study.
“Therefore, validating this new potential connection in
to medical management after failed thrombectomy (TICI ≤2a reperfusion). Their primary endpoint was good functional outcome (mRS 0–2) with postprocedural sICH being a key secondary endpoint.
Of 89 patients who underwent a failed thrombectomy throughout the specified timeframe, 30 received rescue therapy with stenting or angioplasty, while the remaining 59 received maximal medical management. Some 37% of these patients subsequently achieved TICI ≥2b reperfusion. The investigators extracted two well-matched, comparable groups from this cohort—one of which included 14 patients who underwent rescue stenting and another that included 14 patients who received medical management—for further analysis.
Baharvahdat and colleagues’ results ultimately revealed statistical parity between these groups, although they did find a trend towards a higher rate of mRS 0–2 at discharge in the medical management group (71.4%) versus the rescue stenting group (42.8%). Mortality rates were identical between groups, with four deaths occurring in each, and occurrence of sICH was also statistically similar (rescue stenting, 35.8% vs medical management, 42.8%). Additionally, they noted a significantly higher rate of decompressive hemicraniectomy procedures in those receiving medical management (42.8%) compared to rescue stenting (0%). They therefore concluded that—while antithrombotic therapies were not found to have led to an increase in bleedingrelated complications—rescue stenting was not associated with a meaningful alteration of post-thrombectomy clinical outcomes, as compared to medical management.
humans has been enlightening.”
“Now that we have found more evidence for a link between intracranial aneurysms and GI disorders, we are eager to explore them further, hoping that early detection of GI syndromes might help identify patients at risk of intracranial aneurysms,” commented Jan-Karl Burkhardt (University of Pennsylvania, Philadelphia, USA), the lead author of the study.
In addition, Sioutas, Burkhardt and colleagues have emphasised the need for further studies to elucidate these associations and explore the intricate interplay among GI syndromes, the gut microbiome, and intracranial aneurysm pathogenesis.
There is evidence from animal studies suggesting a relationship between the gut microbiome and various inflammatory diseases, including the development and rupture of intracranial aneurysms.”
Georgios Sioutas
Ahead of the COATING study’s much-anticipated final analyses, principal investigator Laurent Pierot (Reims University Hospitals, Reims, France) sits down with NeuroNews to outline the “tremendous impact” he feels its results will have on the interventional treatment of intracranial aneurysms.
The use of single antiplatelet therapy (SAPT) alongside a flow diverter in intracranial aneurysm treatment is by no means a totally novel concept. Relying on knowledge and experience alone, some operators already adopt this approach in their practice—but do so in an ‘off-label’ fashion, as flowdiverter treatments are currently only indicated when paired with dual antiplatelet therapy (DAPT).
According to Pierot, however, this could all be about to change. As a prospective, multicentre randomised controlled trial (RCT) directly comparing aneurysm treatments with a surface-modified or ‘coated’ flow diverter plus SAPT versus a ‘bare’ flow diverter plus DAPT, COATING represents a first-ofits-kind study, and is set to provide concrete evidence on the safety of the former of these two approaches.
“Some people—as with stenting—are using SAPT in certain flow-diverter cases,” Pierot says. “But, if you have a complication, you will be in a position that will be a little bit difficult, because it’s not what is written in the IFU [instructions for use].”
He goes on to note that the use of SAPT rather than DAPT alongside coated flow diverters like WallabyPhenox’s p64 MW Hydrophilic Polymer Coating (HPC) device is currently authorised in very specific aneurysm cases, such as those where there appear to be no other viable interventional options. However, a positive finding regarding the company’s HPC surface modification technology in COATING would likely expand today’s indications far beyond this ‘last-resort’ paradigm, enabling surface-modified flow diverters to be deployed with SAPT across a wide array of both ruptured and unruptured aneurysms.
“It’s probably something we will have to do at some point [in the future], if the study is positive—to collect cases of ruptured and unruptured aneurysms with p64 MW HPC, or p48 MW HPC, just to confirm that it is feasible and we have a rate of rebleeding that is in line with other techniques,” Pierot adds.
The COATING RCT involves patients with unruptured or recanalised intracranial aneurysms indicated for endovascular treatment via placement of a flow diverter. Across 25 European centres, patients meeting the study’s inclusion criteria are being enrolled and randomised 1:1 to undergo intervention with either the p64 MW HPC—WallabyPhenox’s surface-modified flow diverter—or the regular, ‘uncoated’ p64 MW device. The former group is receiving SAPT alongside flow-diversion treatment, while the latter is receiving DAPT.
Having begun enrolment in 2021, COATING is now just a handful of patients away from reaching its final target of 170—a goal that was settled on following an interim assessment at the 85-patient mark and safety analyses at the 140-patient milestone. Neither of these evaluations revealed any major safety issues and a data safety monitoring board (DSMB) therefore greenlit continuation of the study. Pierot reports that a total of 156 patients have already been enrolled, stating that he hopes enrolment will be complete by September of this year, with
initial primary-endpoint and safety data anticipated towards the end of 2024 or at the start of 2025.
Relative to many other large-scale RCTs, COATING has been able to enrol, treat and evaluate its patient population “very rapidly”. Pierot attributes the speedy analysis of these patients to the short timeframe forming part of the study’s primary endpoint: the number of diffusion-weighted imaging (DWI) lesions visualised on magnetic resonance imaging within 48 hours of the index procedure.
“Usually, I am not very much in favour of having a primary endpoint that is not clinical,” he concedes. “The goal of surface modification is to reduce thromboembolic complications, but the rate of these complications is not so high—between 5–10%. So, if you want to see a difference between two groups, you need to have a very high number of patients, which is not feasible.”
of the secondary endpoints to analyse and give us a lot of information regarding the use of surface-modified flow diverters,” he comments.
New frontiers
The fundamental motive behind COATING is to enable flow-diverter treatments with SAPT rather than DAPT; the former is associated with fewer bleeding complications and a reduced overall medication burden for the patient. And, as previously stated, while flow diversion with SAPT is utilised in certain cases already, positive findings within the COATING study will allow WallabyPhenox to make p64 MW HPC the most widely indicated surface-modified flow diverter, meaning a far greater array of patients can benefit from SAPT only alongside the device. This milestone may, in turn, convince more physicians of the significant role surface modification can play in aneurysm care too.
“We will no longer be obliged to use DAPT with this flow diverter, which will potentially lead to the [wider] indication of the device,” Pierot explains. “We have to accept one thing: as of now, the most efficacious treatment for intracranial aneurysms is flow diversion. It is the best treatment, at least in terms of efficacy, and you have to use the best treatment as much as you can.”

Here, Pierot touches on an even more vital advantage carried by DWI lesions as an endpoint, stating that these ‘spots’ on imaging—an adjunct for the safety of an endovascular aneurysm treatment—occur far more frequently compared to clinical outcomes like actual procedural complications or patient symptoms. DWI lesions are present in roughly 50% of cases, and COATING’s investigators believe this relatively high prevalence will enable the study to be conducted across a more limited number of patients while still revealing meaningful betweengroup differences.
Pierot goes on to say that COATING represents the first time a study dedicated to intracranial aneurysm treatment has been based around DWI lesions, adding that it is a “very original” endpoint and constitutes a “really new way” to conduct these assessments. As such, COATING will not only provide insights on HPC, and surface modification more generally, but it will also show researchers “how to optimise DWI to evaluate these kinds of populations”.
“The main goal of COATING is safety,” Pierot continues. “We have efficacy already—we are just covering the flow diverter and not changing the mechanical properties of the device, which means the [efficacy-related] results will be the same as with a bare version of the flow diverter. The main question is safety. Can we use a surface-modified flow diverter with a single antiplatelet treatment? It’s a very important question, and this will be the first time we have an answer.”
This primary endpoint is “the most important aspect, but it will not summarise all findings of the study”, Pierot also notes, alluding to COATING’s myriad of secondary safety and efficacy endpoints, which include but are not limited to rates of mortality/ morbidity, neurological stroke or death, intracranial haemorrhage (ICH), technical success, target aneurysm retreatment or recurrence, and in-stent stenosis and/or thrombosis at the target site.
“We are not expecting [to have] a negative primary endpoint finding—but, even if we do, we will have all
Here, Pierot reiterates his belief that COATING could be the catalyst for flow diversion to become a more accepted and widely used treatment for ruptured and unruptured aneurysms alike, and may enable the use of flow diverters in complex cases like bifurcation and ‘blister-like’ aneurysms where existing options are limited as well.
“In the treatment of intracranial aneurysms in the future, I see an increase in the use of flow diversion,” he adds. “If the study is positive, it means we will be able to treat [more] aneurysms with SAPT, so it will be a major change.”
COATING, Pierot states, is not the only research effort currently evaluating HPC in flow diverter treatments. Another RCT with a comparable design is being conducted in Brazil, with final analyses also expected within a similar timeframe, while two single-arm pivotal studies in the USA and China— enrolling 236 and 120 patients, respectively— are seeking to assess the safety and efficacy of WallabyPhenox’s surface modification technology. Pierot feels these studies will all contribute to the overall body of evidence on HPC across a significant collective of patients from around the globe, and help to identify possible factors influencing the occurrence of thromboembolic complications in endovascular aneurysm care.
Closing the conversation, Pierot offers one final message to his peers in the neurointerventional field: “We need more and more evaluation of what we are doing, and of the devices we are using in the treatment of intracranial aneurysms today. WallabyPhenox has designed a proper study to evaluate whether or not we can reduce antiplatelet medication. The only way to answer this question is an RCT, which is a lot more complex than a registry study, and we have to acknowledge the big effort WallabyPhenox has made to do that. We also have to acknowledge participating centres contributing to the recruitment of patients in France, Germany, Israel, Italy, Slovakia, Switzerland and the UK.
“It’s important—not only for the company, not only for the physicians but, most importantly, for the patients. If the study is positive in favour of the flow diverter with SAPT, we will potentially reduce the rate of complications, haemorrhagic or otherwise, and enlarge the indication for efficacious treatment. This will be a great success for the patient.”
“Potentially groundbreaking” research was presented at the 2024 Society of NeuroInterventional Surgery (SNIS) annual meeting (22–26 July, Colorado Springs, USA), with Robert Starke (University of Miami Miller School of Medicine, Miami, USA) introducing a novel outcome metric—‘complete clot ingestion’ (CCI)—that aims to enhance how success is evaluated in stroke thrombectomy procedures.
Starke’s presentation also outlined findings from a recent study assessing the Algo smart pump device (Von Vascular)—equipped with adaptive pulsatile aspiration (APA) mode—in aspiration thrombectomy.
Research led by Starke has suggested that first-pass thrombolysis in cerebral infarction (TICI) 2c–3 reperfusion, despite being the current gold standard for stroke thrombectomy procedures, may be “insufficient” as a singular measure, as it does not account for unvisualised distal emboli that can occur even after TICI 3 is achieved. The CCI metric intends to provide a more comprehensive assessment based on the complete ingestion of a clot into the catheter or pump canister with no external remnants.
“We believe that the introduction of the CCI metric represents a significant advancement in evaluating the success of thrombectomy procedures,” said Starke, who is the lead investigator for the recent study involving the Algo device. “The Algo smart pump, with its APA mode, has shown promise in achieving more complete clot removal, thereby potentially improving patient outcomes. We are excited about the implications of this research and look forward to further clinical validation.”
The study presented by Starke at SNIS 2024 compared two thrombectomy pump devices: the Algo smart pump and the Engine pump (Penumbra). Using an in-vitro synthetic
clot analogue model, these devices were tested in 360 thrombectomies across six catheter systems, focusing on CCI and the presence of distal emboli. In cases where CCI was achieved, there were zero instances of distal emboli, as compared with 7% in cases where CCI was not achieved. Additionally, the APA-equipped Algo device achieved “superior performance”, indicated by higher CCI rates, versus its comparator.
Another late-breaking presentation at the SNIS meeting saw co-principal investigator William Mack (University of Southern California, Los Angeles, USA) deliver results from the Imperative trial—a prospective, multicentre study that evaluated the clinical benefits of the Zoom reperfusion system (Imperative Care), including aspiration with 0.088-inch catheters, for the treatment of ischaemic stroke.
“The observed data showed all three prespecified performance goals were met,” said Mack. “These data suggest a lower rate of rescue therapy than prior thrombectomy trials, and may demonstrate that intracranial positioning of a super-large-bore catheter could influence or reduce the need for stent retrieval rescue therapy as well as decrease costs. Additionally, the very low rate of symptomatic intracranial haemorrhage coupled with high rates of reperfusion are promising. I look forward to the potential implications for my
practice and the patients I treat.”
The Imperative trial evaluated 260 patients treated across 26 US institutions from October 2021 to March 2024. Prespecified performance goals were established in conjunction with the US Food and Drug Administration (FDA) and 254 patients ultimately completed follow-up at 90 days.
Results from the trial demonstrated that the core-lab adjudicated rate of modified TICI (mTICI) ≥2b reperfusion within ≤3 passes—without the use of any additional thrombectomy devices as rescue therapy—was achieved in 82.2% of patients. According to Imperative, this is similar to prior trials used to support US FDA 510(k) clearance for reperfusion indications. In addition, stent retrieval rescue therapy was used to achieve mTICI ≥2b reperfusion in only 5.5% of cases.
Data also showed that the median time from groin puncture to mTICI ≥2b reperfusion using the Zoom reperfusion system was 19 minutes. Additionally, the core-lab adjudicated rate of symptomatic intracranial haemorrhage was 2.3%, which Imperative notes is lower than the 4.7% rate observed in previous trials, and the rate of independently adjudicated dissection and vessel perforation was 1.2%—also comparable to prior trials.
A multicentre analysis representing initial post-market clinical experiences with the Radical catheter (Radical Catheter Technologies)—a recently US FDA 510(k)-cleared device that a company press release describes as “the first significant advance in catheter
technology in more than three decades”— was also presented at SNIS.
“While catheters are the foundation of every neurovascular procedure I perform, current gaps in catheter technology fundamentally limit complex life-saving procedures,” said Christopher Kellner (Mount Sinai Health System, New York, USA), who presented the aforementioned analysis. “The operators in this pilot experience consistently commented on a number of advantages to the Radical catheter, including greater flexibility to access targeted areas, more stability and increased durability. In our initial case series, the Radical catheter consistently reached further territories of the brain than we are accustomed to with conventional catheters. With this dramatically better performance, I expect to be able to more easily address complex procedures.”
The retrospective analysis evaluated a total of 85 neuroendovascular procedures—including treatments for aneurysms and stroke—that were performed by 14 operators across six US hospitals. Radical claims in a press release that the analysis’ findings indicate that its catheter demonstrated “best-in-class performance”, including catheterisation of the target vessel 100% of the time; ability to reach an intracranial position in all anterior circulation treatment procedures; no device failures or device-related adverse events; and elimination of the need for and use of intermediate catheters in the majority of procedures in which one would have typically been used, due to ease of distal access with the Radical catheter.
While catheters are the foundation of every neurovascular procedure I perform, current gaps in catheter technology fundamentally limit complex life-saving procedures.”
Christopher Kellner
Changing standard procedures for evaluating and treating patients with suspected stroke has led to improved access to lifesaving stroke surgery across the US state of Delaware, and should inform triage and treatment nationwide, according to research released at the 2024 Society of NeuroInterventional Surgery’s (SNIS) annual meeting (22–26 July, Colorado Springs, USA).
IN AN ABSTRACT CONCERNING HOW directly bypassing emergent large vessel occlusion patients from the field to a comprehensive stroke centre (CSC) may impact the timeliness and likelihood of thrombectomy, members of the Delaware Stroke System worked with the state’s emergency medical services (EMS) director to change the way that paramedics in Delaware evaluated individuals for suspected large vessel occlusion, increasing the number of patients who were immediately flown to CSCs for thrombectomy. These changes were implemented across the state in 2023.
During the first full year of implementation, 100 patients were flown directly to a CSC—hospitals with certified neurointerventional specialists on staff who can perform thrombectomies—bypassing the local primary stroke centre (PSC). Of those patients confirmed to have a target vessel occlusion on imaging, 79% underwent thrombectomy. In prior years, that figure was just 52% when patients arrived via interfacility transfer. These patients also received thrombectomy an estimated 2–3 hours earlier than if they had presented to the local PSC first.
As outlined in an SNIS press release, many patients
live far from CSCs and, as such, are sent to PSCs— which have fewer stroke resources—first. If these patients are experiencing a severe stroke, they are often then rerouted to a CSC, and this delay in treatment can put patients at risk for long-term disability or death.
“Implementing this new evidence-based screening and routing patients straight to CSCs has saved lives,” said Thinesh Sivapatham (ChristianaCare, Newark, USA). “Every stroke patient deserves access to lifesaving treatment, no matter where they are. We’re thrilled these procedures are allowing more people in Delaware to thrive after stroke and hope further systems across the USA will follow suit.”
Mechanical
52% when patients arrived via interfacility transfer
79% when patients were flown directly to CSCs
Following their initial presentation earlier this year, two randomised controlled trials (RCTs) indicating positive outcomes with middle meningeal artery (MMA) embolisation in chronic subdural haematoma (cSDH) patients were discussed in greater detail at the recent LINNC Paris meeting (3–5 June, Paris, France). Topics including study design, anaesthesia approaches, treatment timings, and the possibility of a future “HERMESstyle collaborative”, were examined by those in attendance.

As co-principal investigator (PI), Adam Arthur (University of Tennessee Health Science Center/ Semmes-Murphey Clinic, Memphis, USA) kicked off proceedings with a summary of the STEM RCT and its findings on the usage of the Squid liquid embolic system (Balt) to treat cSDH. Arthur averred that this is an “incredibly common” disease and frequent cause of in-hospital neurosurgical mortality, with over 60,000 annual cases anticipated in the USA alone by 2030, but one without a body of level-one evidence or clear guidelines on treatment.
“Everyone in this room is dealing with an increase in [stroke] thrombectomies, dealing with an increase in techniques for aneurysm and AVM [arteriovenous malformation], but I’m hopeful that—before we’re done with our careers—neurointervention as a specialty is actually going to be bigger than neurosurgery,” he said. “We’re going to see more diseases that can be approached endovascularly. There are many more of these [cSDH] patients than all of the types of aneurysm patients put together.”
Arthur commended the “major leap of faith” taken by Balt as well as the early efforts of several neurointerventionists as being key drivers of the recent success seen with MMA embolisation in cSDH. He and his co-PI, David Fiorella (Stony Brook Cerebrovascular Center, Stony Brook, USA), began to adopt the approach around 2017 and ultimately devised the STEM trial—with initial results being presented at the 2024 International Stroke Conference (ISC; 7–9 February, Phoenix, USA).
Despite sizeable challenges encountered throughout the study—as Arthur quipped, “we learned that it’s an extremely bad idea to try to run a large, international
RCT on elderly patients during a pandemic”—STEM met its primary endpoint. Treatment with Squid reduced failure rates to 15%, compared to 40% in patients treated without the liquid embolic, which Arthur described as an “extraordinarily significant and extremely powerful” effect. In addition, there were no deaths in the trial’s treatment arm that were attributable to Squid itself.
“We’re working very hard on the data,” Arthur continued. “I’m really looking forward to economic, length-of-stay, patient-reported and neuropsychological data. I should be able to share all of those with you very soon; we just got a major data download in the last 36 hours [speaking on 5 June 2024] that we’ve been working on.
“In summary, this procedure is fast and technically easy. It’s safe—there are risks, but those risks are lowered if you’re very distal—and it’s effective, as already shown in uncontrolled series. And, now, we have evidence from RCTs that have been able to be
I’m hopeful that— before we’re done with our careers— neurointervention as a specialty is actually going to be bigger than neurosurgery.”
Adam Arthur
put together very quickly because it is such a prevalent disease, which is different compared to aneurysms and AVMs.”
Arthur concluded by alluding to the other completed and ongoing RCTs evaluating MMA embolisation for cSDH and, in doing so, provided a fitting introduction for Jason Davies (State University of New York, Buffalo, USA) to recap recent revelations from the EMBOLISE trial. EMBOLISE was also presented for the first time at ISC 2024, by Davies and his co-PI Jared Knopman (Weill Cornell Medical College, New York, USA).
EMBOLISE featured a handful of key differences as compared to STEM, including the exact structure of its treatment and control arms; its primary endpoint, which was concerned solely with haematoma recurrence/progression at 90 days versus STEM’s composite of multiple failure modes at 180 days; and the fact its liquid embolic system of choice was Onyx (Medtronic).
Nevertheless, its overall findings to date are every bit as positive—cSDH patients who underwent surgery plus adjunctive MMA embolisation experienced a “highly significant”, three-fold reduction in haematoma recurrence/progression compared to those who underwent surgery only. Davies also touched on “very strong safety data”, including similar rates of neurologic deterioration, stroke and death between the two arms, low rates of serious adverse events within 30 days, and no adverse events related specifically to Onyx within 90 days.
Prior to concluding, Davies recapped some more granular imaging data from EMBOLISE that were first presented by Jens Fiehler (University Medical Center Hamburg-Eppendorf, Hamburg, Germany) at last month’s European Stroke Organisation Conference (ESOC; 15–17 May, Basel, Switzerland). These data are still to be fully validated but may enable researchers to “parse out which haematomas are more likely to respond, and which patients are apt to be good candidates for [MMA embolisation]”, according to Davies.
Citing Fiehler, the presenter reported a treatment effect that was about 10% greater in patients with more homogenous haematomas; a higher ‘number needed to treat’ in smaller haematomas, suggesting that “the larger the haematoma, the more effective the treatment seems to be”; and a reduced rate of recurrence/ progression in more spherical haematomas with a lower surface-to-volume ratio versus ‘flatter’ ones.
“But, we did see a significant therapeutic effect across all patients,” Davies summarised. “Adjunctive MMA embolisation with Onyx was associated with significantly reduced rates of reoperation and, therefore, MMA embolisation should be considered for surgical patients.”
At the close of these two presentations, Arthur commented that EMBOLISE and STEM, despite their differing designs, produced results that are “very consistent” as well as reproduceable. Davies corroborated this, noting that the raw data are available to make “apples-to-apples” comparisons across both studies—also suggesting that it is likely EMBOLISE would have produced similar findings if it adopted STEM’s endpoints, and vice versa.
Anaesthesia versus sedation
Subsequent discussions saw Davies note that, in EMBOLISE, he and his colleagues advocated conscious sedation—but were ultimately unsuccessful, as roughly 80% of patients received MMA embolisation under general anaesthesia. Davies also admitted he holds a certain ‘Buffalo bias’ here, but added that “this is definitely a procedure that can be done under conscious sedation, with the proper preparation”.
“I find the anatomy variable,” Arthur added. “Some of these cases are very easy and can be done in an older patient even if they are moving around but, in some of
them, the navigation of the MMA can be challenging— and I think getting distal is important. So, either is fine; if you’re going to go without general anaesthesia, I think intra-arterial lidocaine and verapamil prior to treatment with a liquid embolic can be helpful.”
Davies agreed, also commenting that the EMBOLISE investigators observed conscious sedation generally being less optimal when used by physicians who were not accustomed to it and, as such, offered the following advice: “First and foremost, you’ve got to be safe. If you’re not used to a patient moving around, do it under anaesthesia. If you’re comfortable with it, then we can get it done safely [under conscious sedation].”
Next frontiers
Responding to a question from Elisa Francesca Ciceri (Foundation of the Carlo Besta Neurological Institute, Milan, Italy) on whether outcomes may differ when embolising one versus multiple MMA branches, Davies said these data do exist but are yet to be fully analysed.
“The truth of the matter is that we do not yet know what constitutes a minimally adequate embolisation,” he went on. “We believe that getting into the membranes is a significant part of that. We’re using something that involves DMSO [dimethyl sulfoxide]— maybe just hitting the DMSO of the membranes is all you really need, but we don’t know yet.”
On this point, Fiehler stated that the exact requirements for ensuring sufficient cSDH treatment represent “the hundred-thousand-dollar question”, and further analyses may elucidate whether proximal or distal embolisation is more appropriate.
“These analyses are ongoing, and the strength of this moment in time is that we’ve got 1,500 cases between the three trials that have already been presented and there are other trials ongoing,” Davies added. “I think we’re going to have a HERMES-style
collaborative that’s going to be able to answer some of these questions.”
Following this, Zsolt Kulcsár (University Hospital of Zürich, Zürich, Switzerland) commented that SDH is a condition that likely evolves over time—through acute, subacute and chronic phases—and therefore queried when might be the optimal moment to treat these patients.
“In the context of [EMBOLISE], we asked for embolisation to be done within 48 hours of surgery,” Davies responded. “Is that a meaningful time period? I don’t know—in speaking to some of you here, I understand that the constraints of different hospital systems may mean the patient should be discharged and then come back. I think that may work, we don’t have data to support that, but—thinking through the pathophysiology—I don’t think there’s an acute need to embolise right after surgery. You probably have some leniency in terms of the timing.”
Arthur added to this, stating that no definitive data yet support treating asymptomatic cSDH patients nor
Analyses are ongoing, and the strength of this moment in time is that we’ve got 1,500 cases between the three trials that have already been presented and there are other trials ongoing.”
Jason Davies




those with acute, traumatic SDH, but this is also likely to be explored further over the coming years.
A final topic touched on by the speakers, and the expert panel at LINNC, was the possibility for alternative approaches like particle-based MMA embolisation to also emerge as a viable cSDH therapy. Arthur and Davies noted that they and many others prefer to use liquid embolic agents rather than polyvinyl alcohol (PVA) particles—while the former is more expensive, it offers greater penetration of the pathology and, potentially, fewer risks.
After applauding the STEM and EMBOLISE investigators’ work as “phenomenal”, and noting that they have “opened the door for so many patients who need that help”, Ricardo Hanel (Baptist Neurological Institute, Jacksonville, USA) said the CHESS study—a multicentre RCT comparing standalone MMA embolisation with particles (PVA or embospheres) to surgical drainage in cSDH patients—is “starting soon” and “could help answer this question” of whether particles are as effective as liquid embolics.
“Thank you both for driving this field forward,” said LINNC course director Vitor Mendes Pereira (St Michael’s Hospital, Toronto, Canada), drawing the discussion to an end. “I think, now, we all have to work on improving the workflows, because we have to know how we can get these patients to the angio [suite] as quickly as possible—and that’s coming with the good evidence base that you have created. It’s a good first step, and I’m looking forward to the publications and the subgroup analyses.”
Among other research areas, attention is now likely to turn towards the MEMBRANE RCT, which is evaluating the TruFill n-BCA liquid embolic system (Cerenovus/J&J) alongside surgical and/or medical management in cSDH patients. Enrolment in the trial is approaching completion as of July 2024, with results anticipated in the near future.


The growth of intravenous thrombolysis (IVT) coupled with the advent—and ongoing expansion—of mechanical thrombectomy has seen acute stroke transform from “a diagnosable and hardly treatable condition, to a highly treatable condition”, over the past two decades. However, significant disparities in thrombectomy access exist across the globe, with uptake rates remaining especially low within many developing countries.
That is according to Shashvat Desai (HonorHealth, Scottsdale, USA), who—alongside Ashutosh Jadhav (Barrow Neurological Institute, Phoenix, USA)—recently spoke to NeuroNews to discuss Gravity Medical Technology’s mission to alleviate some of these disparities and ensure more patients have access to these potentially life-saving procedures.
A key building block leading to this mission was the MT-GLASS study, which was initiated back in 2020 as a means for elucidating disparities in thrombectomy care within individual countries, but also between different geographies. Published last year, MT-GLASS ultimately found “extremely low” global access to the procedure; median uptake worldwide sits at 2.79%, with rates dropping below 1% in poorer geographies within Africa and Asia.
“There’s a lot of regional variation,” says Jadhav, Gravity’s chief scientific officer.
“The determinants of that are what you’d expect. One of the big ones is that low- and middle-income countries [LMICs] have much lower access than higher-income countries, so cost and infrastructure are certainly a big part of it.”
Among many contributing factors are the availability of operators and trained healthcare professionals, as well as medical equipment—as Jadhav notes, “some countries don’t even have CT [computed tomography] scanners”. Other barriers relate to matters that are often “taken for granted” in the western world. On this point, Jadhav recalls prior efforts to roll out a stroke awareness campaign in Ethiopia being hampered by the fact that there is no word for ‘stroke’ in the country’s predominant language of Amharic.
people can afford it.
“Every person does their own cost-effectiveness analysis in that situation. This concept is probably well understood by behavioural economists but is yet to be meaningfully translated to healthcare. We study cost effectiveness, but we assume the government will pay for everything from start to finish, and that’s not the case in most parts of the world. Given that the luxury of time is not an option in acute stroke treatment, affordable, cost-flexible devices are most impactful because, up front, the patient or their family is able to pay for it—that changes the game completely.”
Gravity set out to create thrombectomy devices that can be produced at a lower cost and, in turn, made available to developing countries at more flexible price-points. Leading these offerings is its Supernova stent retriever, which progressed through animal testing in 2023, and evaluation in humans for the first time in February 2024, and has since received market approval in South-East Asia.

Shashvat Desai
Preclinical evaluations involving Supernova provided signals that it was equivalent to market-leading stent retrievers from Medtronic and Stryker in strokes caused by ‘softer’, typically easier-to-treat clots, and could potentially be more effective in ‘harder’, more challenging ones. Subsequently, first-in-human findings derived from 10 patients in Pakistan enrolled in the prospective, multicentre, single-arm GRASSROOT study have seen “excellent” performance from the novel device regarding safety and efficacy.
in India and, later, with enrolments in Turkey and Romania, as the company targets European approval further down the line. As Desai puts it, GRASSROOT is set to create a diverse, “first-of-its-kind” dataset thanks to its basis in these developing countries.
The eventual goal for Gravity is to create a stroke thrombectomy ‘kit’ that incorporates its Supernova stent retriever, its Neutron aspiration catheter—for which first-in-human data from Thailand are expected to be presented later this year—and several other devices including microcatheters and guidewires. Jadhav notes that this will effectively mean the company can provide “the whole A through Z” as one bundle of products.
“This is the first time anyone has attempted to produce an affordable [thrombectomy] device kit,” comments Desai. “The example we commonly give is what really brought cardiac stenting procedures to the fore and made them commonplace across the world: the availability of affordable cardiac stents. It took 30–35 years for them to do that. What we are doing right now could shorten that time from three decades to half a decade for acute neurointervention. So, I think we’re trying to address a socioeconomic challenge as much as a healthcare challenge.”
So, how has Gravity attempted to achieve these lower price-points while maintaining the safety and efficacy seen in more established thrombectomy devices? Desai and Jadhav were naturally reticent to give away all of their secrets, but did reveal that utilising novel in-silico simulation techniques alongside European partners has enabled them to “drastically reduce” the costs associated with research and development. In addition, the first-pass effect rates they have observed in preclinical testing appear to be significantly higher than those associated with established devices, meaning fewer individual devices—and, therefore, reduced costs at the hospital level—would theoretically be required per patient to achieve treatment success.
MT-GLASS did show, however, that gross domestic product (GDP) and other determinants of a country’s financial strength are undeniably among the most prominent predictors of thrombectomy access levels, and breaking down these economic barriers in order to “democratise” stroke treatment has become Gravity’s primary goal.
The company’s efforts to “close that gap” began in 2020 and have homed in on one specific yet critical point: the fact that existing devices used in thrombectomy procedures are “cost-prohibitive” for many countries.
“For example,” Jadhav explains, “the cost of a stentretriever device is higher than the [average] annual income of an individual in India—they earn less than the cost of these the currently available devices. That’s just not a sustainable or practical option.”
“Affordability is the question,” adds Desai, chief technology officer for Gravity, highlighting an issue that is almost alien to many in Europe and the USA, but prevalent across much of the rest of the world. “When a patient goes into a private hospital in India, the issue is who’s going to pay the upfront US$4,000–5,000 to buy the hardware to offer thrombectomy. But, if you can bring that down to a more tenable amount of US$2,000, that changes the equation to the extent where an additional two hundred million
Data disclosed at the 2024 World Live Neurovascular Conference (WLNC) and iCure Stroke joint meeting (7–10 May, Istanbul, Turkey) revealed that Supernova achieved modified thrombolysis in cerebral infarction (mTICI) 2b–3 recanalisation within three passes 90% of the time, and at the first pass 60% of the time, without leading to any device-related complications. These results led Dileep Yavagal (University of Miami, Coral Gables, USA), the global principal investigator of the GRASSROOT trial, to conclude that the device has the potential to “substantially advance” first-pass success rates as well as achieving Gravity’s aim of improving thrombectomy access across the world. As of July 2024, more than 70 stroke patients have now been successfully treated using the device across Thailand and Pakistan, and Desai and Jadhav anticipate these numbers growing rapidly in the coming months—initially with the inclusion of patients

Ashutosh Jadhav
Desai also highlights Gravity’s “costconscious” regulatory approach, which involves generating clinical data in countries like Turkey, Thailand and India where levels of stroke expertise are high but clinical stroke research costs are lower, rather than more expensive geographies like the USA or Western Europe.
“We’re trying to do things in efficient ways, and we’ve moved pretty quickly,” Jadhav comments. “If you look at our timeline, we’ve moved from prototyping to flow models, to animal testing, to human testing within about three years. That’s another reason we’ve been able to save costs—by just streamlining our process. If you take 10 years to get to this point, you can imagine that it’d be much more expensive.”
Jadhav goes on to state the testing of devices and drugs alike in the USA has become somewhat restrictive in recent years, owing to how expensive it is to conduct clinical trials. And, “it’s to our detriment, from a commercial standpoint but also a research standpoint”, he adds, alluding to the fact that other regions—Europe and China, for instance—are currently able to conduct large-scale studies in the stroke space more efficiently.
We’re trying to address a socioeconomic challenge as much as a healthcare challenge.”
“Basically, by the time you get to market, as a company, you’ve built up a lot of debt just to get to that point, and then it’s hard to introduce devices at a reasonable price-point,” Jadhav says. “The cost issue is on everyone’s minds and the solutions are difficult. I think we’ve come up with some innovative ways to reduce that cost to get to market and I do suspect that, with time, a lot of these device trials will be conducted in LMICs, as they develop the infrastructure to support that.”
Positive results from the first-in-human CLOT OUT clinical trial—evaluating the safety and performance Clotild smart guidewire system (Sensome) used during mechanical thrombectomy treatments for ischaemic stroke—were presented on the final day of LINNC Paris 2024 (3–5 June, Paris, France) by principal investigator Aymeric Rouchaud (Limoges University Hospital, Limoges, France).
THE RESULTS SHOWED THAT the technology met every primary safety and performance endpoint in the trial. There were no serious adverse events related to use of Clotild, and the device successfully automated the identification of red blood cells (RBCs) and platelets “in close alignment with human experts”, as noted in a Sensome press release.
CLOT OUT is a single-arm, prospective, multicentre, first-inhuman trial being conducted in France and Australia, encompassing 41 patients experiencing acute largevessel ischaemic stroke in whom the Clotild guidewire was used before any thrombectomy pass. As a first-inhuman study, the trial was intended to train the clot-sensing technology to further enhance Clotild’s in-situ clot characterisation performance.
The data presented recently at LINNC Paris showed that, in a blinded-validation dataset, the Clotild
technology’s predictive algorithms successfully identified RBCs and platelets—thereby demonstrating automated processing of thrombus signals acquired in situ by the sensor during the thrombectomy procedure. The technology demonstrated sensitivity of 95% (95% confidence interval [CI], 86–100%) and specificity of 93% (95% CI, 90–96%) for RBCs, and sensitivity of 87% (95% CI, 76–96%) and specificity of 94% (95% CI, 90–96%) for platelets, when compared to analyses by a human expert.
“Understanding the clot is critical to informing the approach we take to clot removal in life-saving stroke treatment, yet today’s imaging provides incomplete information,” Rouchaud said. “This results in 60% of thrombectomy cases requiring two or more passes to remove clot—with each pass reducing patient outcomes—and 10–20% of cases being unsuccessful in removing clot altogether. This first-in-human study showed that
The use of a smartphone-based mobile application may improve medication adherence and risk-factor control among stroke survivors, and appears to be a feasible approach in low- and middle-income countries (LMICs). This is the salient finding of a study performed in South India and published recently in the International Journal of Stroke.
CORRESPONDING AUTHOR P N SYLAJA (professor and head, Department of Neurology, Sree Chitra Tirunal Institute for Medical Sciences and Technology [SCTIMST], Trivandrum, India), Veena Babu (PhD scholar, Department of Neurology, SCTIMST, Trivandrum, India) and their team conducted an unblinded, single-centre, double-arm randomised controlled trial (RCT) with 1:1 allocation, evaluating the smartphone application’s utility among stroke survivors. More specifically, they aimed to
this smart guidewire safely navigated through the brain and successfully characterised common clot components without human analysis. This is an exciting development with the potential to give us a more complete picture of the clot that we are missing today in order to achieve better first-pass success.”
“In addition to the promise of improving our thrombectomy results, we appreciate that this technology integrated well with our current interventional workflow and didn’t require a new technique,” said Andrew Cheung (Liverpool Hospital, Liverpool, Australia), co-coordinating investigator of the CLOT OUT trial. “The Clotild device is ingenious—by simply replacing our existing guidewire with a smart wire, we may be able to gain better information that could help us significantly improve our patients’ chances of a full recovery after stroke.”
The Clotild clot-sensing guidewire integrates the world’s smallest electrical impedance sensor with machine learning, and is being developed to instantly identify clot composition and clot length in real-time, in order to inform treatment approaches during mechanical thrombectomy. Sensome believes it has the potential to be the first device to accurately identify clot length in fully occluded arteries in situ, as well as the first to characterise clots that remain in the body after failed
removal attempts.
In two previous peer-reviewed publications, the company’s microsensor technology has been shown to reliably predict the RBC composition of retrieved clot with good sensitivity and specificity consistent with histologic findings. Data demonstrating the technology’s ability to do the same with platelets is pending publication, according to Sensome.
“Meeting all of the primary endpoints in our first-in-human study is an important milestone for our company and the first step in realising the full potential of our novel microsensor technology across several indications,” said Franz Bozsak, chief executive officer and co-founder of Sensome. “In this first use in stroke treatment, we showed that our technology was able to automate clot component identification with the accuracy of human experts. We look forward to further clinical study of Clotild in larger numbers of patients that will grow its capabilities to ultimately provide recommendations for a personalised treatment approach for each clot and patient.”
Sensome states that the Clotild smart guidewire system has been designated as a Breakthrough Device by the US Food and Drug Administration (FDA), and it is currently an investigational device that is not approved for commercial use in the USA or any other jurisdiction.
Understanding the clot is critical to informing the approach we take to clot removal in life-saving stroke treatment, yet today’s imaging provides incomplete information.” Aymeric Rouchaud
determine whether the application could improve medication adherence and risk-factor control, and provide patients with health education relating to lifestyle and behavioural modifications.
According to the researchers, this study was conducted against the backdrop that “there are little data on the use of smartphone-based applications for medication adherence and risk-factor control for the secondary prevention of stroke in LMICs”. Their primary outcome measure was medication adherence, with co-primary outcomes of lifestyle and behavioural factors, as well as control of vascular risk factors. All of these outcomes were measured at three and six months in the trial. Among a total of 351 stroke survivors who were screened for the trial, 209 were recruited, with 105 ultimately being randomised to the intervention group and 104 to the control group. The mean age across both groups was 60 years.
As per the trial’s primary outcome measure, Sylaja, Babu and colleagues report that mean medication adherence “significantly improved” in the intervention group, as compared to with controls; the researchers observed a between-group difference of 0.735 (95% confidence interval [CI], 0.419–1.050; p<0.001). Investigators also found that—in addition to being in the trial’s intervention group (odds ratio [OR], 4.5; 95% CI, 2.3–8.9)—other factors that turned out to be “significant predictors” of good medication adherence were stroke recurrence (OR, 3.3; 95% CI,
1.9–7.8) and regular physician visits (OR, 2.1; 95% CI, 1–4.4).
Moving on to discuss the co-primary outcomes of their trial, Sylaja, Babu and colleagues relay that—compared to the control group—patients in the intervention group had a greater improvement in self-reported healthy diet intake (p=0.003) and intake of fruits (p=0.005), and were physically more active (p=0.001) as well. At the six-month timepoint, mean fasting blood sugar (p=0.005) and high-density lipoprotein cholesterol (p=0.024) were also higher in the intervention group versus with controls.

According to the investigators, medication adherence and risk-factor control is “very poor” in stroke survivors in LMICs, which leads to a high risk of stroke recurrence. A lack of availability of primary care physicians, and financial barriers, are among key limitations here. Researchers believe that, if an app like the one evaluated in their study can help stroke survivors with medication adherence and monitoring of risk factors, it can reduce the caregiver burden, and has implications for health workers in improving stroke prevention in the community.

The modified Rankin scale as a stroke trial endpoint: Important, but not all-encompassing


Wechsler
The modified Rankin scale (mRS) is something of a default clinical outcome metric in many contemporary stroke studies, but—as Eva Mistry and Paul Wechsler (both Cincinnati, USA) write in this NeuroNews guest article—it represents an imperfect method for measuring success, and the time may therefore be right to reevaluate its usage in stroke research. Mistry and Wechsler initially outline contexts within which the mRS is and is not fully suitable, before going on to discuss potential modifications or alternatives that offer promise.
John Rankin assumingly did not envision his Rankin scale from 19571 forming the basis for measuring success of stroke therapies in clinical trials. After being modified once2, the mRS is able to capture a broad range of an individual’s functional abilities, ranging from 0 (no symptoms) to 6 (death), with scores 1–5 describing increasing levels of global functional disability.
This simplicity and intuitiveness, among other factors, contribute to the mRS being the most common endpoint for therapies that aim to reduce strokerelated disability. Nevertheless, it is often debated what role the mRS should play in future stroke trials.
Selection of a stroke trial endpoint is dependent on the natural history of the disease that a therapy is aiming to modify and the time window in which the therapeutic effect is most likely to be detected.
Hyperacute stroke can cause impairment in several domains, including locomotion, cognition, vision, speech and arm function. These may lead to functional disabilities, such as inability to walk, care for oneself, and engage in social/vocational/ recreational activities (global functional disabilities).
Acute stroke therapies aim to limit this disability. The mRS is thus an ideal endpoint to use in this context, as it effectively measures a patient’s entire spectrum of global functional disability.
Recurrent stroke and chronic motor impairment have quite different natural histories, however. Few patients suffer a recurrent stroke3 and not all recurrent strokes cause measurable, incremental functional disability.4 Similarly, much of motor recovery after stroke does not translate into measurable changes in
and supplement the mRS with endpoints that reflect a wider range of outcomes that are important to patients and that inform clinical practice.
The utility-weighted mRS (UWmRS) converts the mRS into a more patient-centred outcome. In this approach, a ‘utility value’—the desirability of a health state to the patient as measured by patient healthrelated quality of life6—is assigned to each category of the mRS. Rather than clinicians defining a ‘good outcome’ after a stroke treatment as living independently (mRS 0–2)7, the outcome using the UW-mRS is how patients value their functional status.
There are calls for other patientcentred outcomes to be included in trials, such as quality-of-life measures, social functioning measures, and leisure or home time.
Uptake of these more patient-centred outcomes is slow.8 The reasons for this are likely multifactorial, but one legitimate concern is that factors other than biologic effects of treatment— such as cultural and social constructs— highly influence these outcomes.9
that development and implementation of these novel endpoints should not occur without meaningful engagement of stakeholders—such as patients, caregivers and clinicians (physicians, nurses, therapists, and more).
In summary, while the mRS will continue to play a major role in stroke trials given its established validity, importance to patients, and ease of interpretation, its modification and/ or supplementation to capture patientcentrality will allow stroke therapies to demonstrate efficacy in many more meaningful domains than only global disability.
References: 1. Rankin J. Cerebral vascular accidents in patients over the age of 60. II. Prognosis. Scott Med J. 1957; 2: 200–15. doi: 10.1177/003693305700200504.
2. Farrell B, Godwin J, Richards S et al. The United Kingdom transient ischaemic attack (UK-TIA) aspirin trial: final results. J Neurol Neurosurg Psychiatry. 1991; 54: 1044–54. doi: 10.1136/jnnp.54.12.1044.
3. Robinson D J, Stanton R, Sucharew H et al. Racial disparities in stroke recurrence: a population-based study. Neurology. 222; 99: e2464–73. doi: 10.1212/ WNL.0000000000201225.
4. Hobeanu C, Lavallee P C, Charles H et al. Risk of subsequent disabling or fatal stroke in patients with transient ischaemic attack or minor ischaemic stroke: an international, prospective cohort study. Lancet Neurol. 2022; 21: 889–98. doi: 10.1016/S14744422(22)00302-7.
global functional disability.5
Therefore, the mRS is not ideally suited to capture clinically important changes in recurrent stroke and motor impairment that secondary stroke prevention and recovery trials aim to modify over long periods of time.
The mRS captures both broad and narrow treatment effects of stroke therapies.
It is broad in that it describes a wide spectrum of an individual’s functional abilities—from no symptoms (mRS 0), to requiring help with essential tasks despite walking independently (mRS 3), to bedbound (mRS 5). This is advantageous because it provides patients and clinicians with a simple picture of how an individual can move and care for themselves, which are important functional abilities to patients.
Yet, it also paints a narrow picture in that it does not fully describe how
Further research is needed to understand how patient- and societallevel factors influence a patient’s perception of their outcome, to facilitate controlling for these factors in future trials.
Use of domain-specific outcomes that measure explicit stroke-related deficits (motor, visual, cognitive etc.) rather than global functional abilities may prove effective in capturing small but clinically meaningful changes in patient functioning that affect quality of life.10
In addition, the separation of efficacy and tolerability endpoints may contribute to some therapies proven efficacious in trials not being routinely implemented into clinical practice because of side-effects and logistical challenges.
A hypothetical trial may establish efficacy of a repetitive therapy for motor recovery but at the cost of significant patient fatigue and adherence difficulty. Utility functions that mathematically incorporate multiple endpoints into a single
Many opportunities exist to modify and supplement the mRS with endpoints that reflect a wider range of outcomes that are important to patients and that inform clinical practice.”
an individual is functioning in all life domains. A patient may have minor language difficulty that does not prevent them from doing their usual activities (mRS 1). How do these symptoms affect their emotional, cognitive and psychiatric wellbeing? These types of impairments that affect patient quality of life are not reliably captured by the mRS.
Many opportunities exist to modify
measure could make trials more representative of clinical practice by balancing efficacy and tolerability.
The ongoing SISTER clinical trial (NCT05948566) utilises this novel methodology to balance intracerebral haemorrhage (safety) and neurologic improvement (efficacy) outcomes to find the best dose of a novel drug that facilitates thrombus resolution.
Lastly, it is important to keep in mind
5. Erler K S, Wu R, DiCarlo J A et al. Association of modified Rankin scale with recovery phenotypes in patients with upper extremity weakness after stroke. Neurology. 2022; 98: e1877–85. doi: 10.1212/ WNL.0000000000200154.
6. Feeny D. A utility approach to the assessment of health-related quality of life. Med Care. 2000; 38(9 Suppl): II151–4. doi: 10.1097/00005650-20000900200022.
7. Saver J L, Chaisinanunkul N, Campbell B C V et al. Standardized nomenclature for modified Rankin scale global disability outcomes: consensus recommendations from stroke therapy academic industry roundtable XI. Stroke. 2021; 52: 3054–62. doi: 10.1161/STROKEAHA.121.034480.
8. Hostnik J S, Strong B, Reeves M J. Utilization and reporting of patient-reported outcome measures in randomized clinical trials of acute stroke (20102020). Stroke. 2024; 55: 1174–80. doi: 10.1161/ STROKEAHA.123.046209.
9. Lees K R, Khatri P. Stroke treatment academic industry roundtable recommendations for individual data pooling analyses in stroke. Stroke. 2016; 47: 2154–9. doi: 10.1161/STROKEAHA.116.012966.
10. Cramer S C, Lin D J, Finklestein S P. Domainspecific outcome measures in clinical trials of therapies promoting stroke recovery: a suggested blueprint. Stroke. 2023; 54: e86–90. doi: 10.1161/ STROKEAHA.122.042313.
Eva Mistry is an associate professor in the Department of Neurology and Rehabilitation Medicine at the University of Cincinnati (Cincinnati, USA), a board-certified vascular neurologist, and a stroke clinical triallist. She is currently a fellow of the American Heart Association/American Stroke Association (AHA/ASA) and an active member of the American Academy of Neurology (AAN), and serves as a senior associate editor of the journal Stroke. As a researcher, Mistry focuses on novel clinical research methods to ensure efficient translation of innovation to stroke patient care.
Paul Wechsler is a vascular neurology fellow at the University of Cincinnati in the Department of Neurology and Rehabilitation Medicine. He is also receiving clinical research training as a National Institutes of Health (NIH) T32 fellow. His academic interests include acute stroke treatments, novel clinical trial design, and clinical research informatics.
The authors declared no relevant disclosures.
Following the recent publication in Stroke: Vascular and Interventional Neurology of results from HEMERA-1, a prospective, multicentre trial evaluating the safety of novel neuroprotective agent PP-007 (Prolong Pharmaceuticals) alongside mechanical thrombectomy in acute stroke patients, lead investigator Italo Linfante (Miami Neuroscience Institute, Miami, USA) delves deeper into the data and discusses some of the study’s wider implications with NeuroNews.
What is the general background to the HEMERA-1 study, and why did you and your co-investigators decide to initiate it?
Several randomised clinical trials have shown overwhelming superiority of mechanical thrombectomy over medical management for patients with acute stroke secondary to large vessel occlusion (LVO).
In these trials and in large-volume case series post trials, despite high rates of complete recanalisation of the occluded vessel, functional independence at 90 days ranges approximately between 41–71% of patients.
In experimental ischaemia models, middle cerebral artery occlusion (MCAO) induces redistribution of cerebral blood flow (CBF), and activation and engagement of leptomeningeal anastomoses (LMA).
The amount of redistribution and increase of CBF in LMA can significantly influence final infarct volume.
In fact, in experimental ischaemia models and in patients with acute stroke secondary to LVO, increased CBF in LMA reduces the activation of several neurotoxic molecules in penumbral tissue, slows core expansion, and ultimately induces protection from neuronal ischaemic injury. Conversely, poor blood flow in LMA is associated with a faster growth of the ischaemic core.
PEGylated bovine carboxyhaemoglobin, or PP-007, is a carbon monoxide (CO)-releasing and oxygen-transfer molecule with pleotropic neuroprotective effects.
As demonstrated in several experimental ischaemia models, such as temporary rats’ MCAOs, the neuroprotection induced by PP-007 is due to a combination of: increased blood flow in pial collaterals; optimisation of oxygen transport in ischaemic tissue; and plasma expansion effect secondary to the pegylated nature of the compound. Furthermore, since PP-007 also acts as a CO donor and small amounts of CO were found to have anti-inflammatory properties, PP-007 was observed to reduce proinflammatory cytokines.
Dose escalation studies were performed in normal volunteers, patients with sickle cell anaemia and patients with subarachnoid haemorrhage too.
Could you briefly describe the design and methodology of the study?
We aimed to evaluate the safety and feasibility of PP-007 in acute stroke patients undergoing mechanical thrombectomy. HEMERA-1 was a Phase 1, multicentre, prospective randomised controlled clinical trial. Anterior-circulation LVO patients were assigned in a 3:1 ratio to receive either PP-007 (320mg/kg; 30-minute bolus followed by two-hour infusion) plus mechanical thrombectomy or mechanical thrombectomy alone within 24 hours after symptom onset. Comprehensive safety evaluation was performed by an independent data safety monitoring board (DSMB) and an independent imaging core lab.
Could you briefly summarise the nowpublished findings of HEMERA-1?
From 10 January 2021 to 30 June 2022, a total of 17 patients were recruited. Age, baseline National Institutes of Health stroke scale (NIHSS) and Alberta stroke programme early computed tomography score (ASPECTS) were 74.8±12.7 years, 17.3±4.2, and 7.9±1.8, respectively. Twelve patients were randomised PP-007 plus mechanical thrombectomy—one was randomised but not treated— and four patients were randomised to mechanical thrombectomy alone. Recanalisation of the occluded vessel was achieved in all patients.
With this study having been successful, can you shed any light on the randomised controlled trial that will now follow to assess PP-007’s efficacy?
We are currently planning a multicentre, Phase 2b/3 randomised clinical trial for efficacy. Patients with acute stroke secondary to LVO undergoing mechanical thrombectomy will be randomly assigned to receive PP-007 or placebo. The trial will have an adaptive design and a shift analysis of the modified Rankin scale (mRS) at 90 days as its primary endpoint. Secondary endpoints will include NIHSS changes, infarct growth on follow-up imaging etc. We hope to submit the randomised trial design to the US FDA by the end of the year.

Was there anything observed in these results, positive or negative, that surprised you?
No significant safety concerns were identified for the adjunctive use of PP-007 in patients undergoing mechanical thrombectomy after the DSMB reviewed all patients’ data in detail for every organ system, independently from the investigators. A transient systolic blood pressure increase (20–40mmHg) during the bolus was observed in all PP-007 patients without any clinical consequences.
Do you have any concerns at all regarding the transient increase in systolic blood pressure seen in patients treated with PP-007 in the trial?
No, because the increase in blood pressure is consistent with the plasma-expander properties of PP-007. This temporary increase in blood pressure had no safety concerns, as adjudicated by the DSMB and the imaging core lab.
It is noted in the paper that patients treated with intravenous thrombolysis were not eligible for HEMERA-1—do you think it is likely that subsequent studies incorporating thrombolytics can produce even more positive outcomes?
As per US Food and Drug Administration (FDA) request, to avoid drug-drug interaction, we did not enrol patients who received alteplase (tPA) or tenecteplase (TNK) in HEMERA-1. Once the data were analysed and adjudicated to be safe, we then enrolled an additional 14 patients to evaluate safety of the combination of tPA or TNK, and PP-007. The data were reviewed by two additional DSMB meetings and a core imaging lab independent from the investigators. No safety concerns were found, with the data set to be submitted for publication.
How many stroke patients could be positively impacted by this neuroprotective drug if it does continue to progress through trials and into clinical practice—and how much of a difference could it make for them?
Data from the American Heart Association (AHA) report that, every year, more than 750,000 people in the USA have a stroke, and 87% of them are ischaemic. In my humble opinion, if the trial will show efficacy, all ischaemic stroke patients can be potentially treated with PP-007. In addition, if PP-007 is beneficial for ischaemic stroke patients, perhaps this advanced molecule could be used in other organs affected by ischaemic conditions.
There have been some fairly mixed data and findings on neuroprotection over the past few years—what do you think the overall landscape looks like for neuroprotection, and are we getting closer to elucidating its potential role in acute stroke care? Many promising therapeutic agents for neuroprotection have been identified to target the complex pathophysiological events occurring at the level of the neurovascular unit during ischaemia. However, none of these agents have proven to be beneficial in clinical studies to date. It must be considered that most of these studies predated the mechanical thrombectomy era and, most likely, neuroprotection may not be evident without effective recanalisation of the occluded artery. In my opinion—now that we are in the mechanical thrombectomy era, with high recanalisation rates—there will be a tremendous effort to develop pharmacological agents that are able to slow down core expansion and preserve the ischaemic penumbra to improve outcomes in patients with acute stroke secondary to large-artery occlusions.
In my humble opinion, if the trial will show efficacy, all ischaemic stroke patients can be potentially treated with PP-007.”

While the recently presented SEGA trial and many other studies have attempted to establish which of the two prevalent methods for medically inducing a loss of consciousness during a mechanical thrombectomy procedure is best, the neurointerventional community remains divided. Here, Panagiotis Papanagiotou (Athens, Greece/Bremen, Germany) takes a closer look at this debate.
How do you decide between general anaesthesia (GA) and conscious sedation (CS) for stroke thrombectomy? This pivotal choice can significantly impact patient outcomes and procedural efficiency. Both GA and CS have their pros and cons, and the evidence remains mixed.
Pros and cons
GA ensures complete patient immobility and secure airway management—crucial for precision in neurointerventional procedures. It allows better control over physiological variables, such as blood pressure and carbon dioxide levels, reducing intraoperative complications. However, the ideal timing for extubation post-procedure is not well-defined. Prolonged mechanical ventilation can lead to complications like pneumonia or disturbances in cerebral blood flow, while premature extubation might cause agitation, disorientation, sudden bloodpressure fluctuations, and the need for reintubation. CS allows for a faster start to the procedure, and is associated with fewer and less severe blood-pressure fluctuations. Patients under CS are less likely to require intensive care, allowing for more efficient postoperative management. However, ensuring patient immobility can be challenging, and there is less precise control over physiological parameters.
Evidence overview
Recent studies and meta-analyses provide valuable insights, but no definitive answers. A 2023 systematic review and meta-analysis included nine randomised controlled trials (RCTs) with 1,342 patients and found no significant differences in functional outcomes—measured by the modified Rankin scale (mRS)—at three months between GA and CS, although GA was associated with higher successful
more than 90% of thrombectomies— both in the anterior and posterior circulations—are performed under CS. The decision between GA and CS is made just before the intervention, based on the patient’s condition and ability to cooperate. Effective communication and collaboration between the neurointerventionist and the anaesthesiologist are crucial to ensure both professionals are comfortable with the chosen approach. Observations suggest that patients with poor collateral circulation or severe aphasia may not cooperate well with CS, making GA a more suitable option in such cases.
Practical considerations

reperfusion rates. The SIESTA trial reported similar findings, with GA showing higher recanalisation rates but no significant difference in early neurological outcomes. The GOLIATH trial observed higher recanalisation rates and shorter times to reperfusion with GA, but no significant differences in functional outcomes. Additionally, a meta-analysis by Jin et al (2024) involving eight RCTs and 1,352 patients found that GA achieved higher successful reperfusion rates compared to CS but also noted a higher incidence of pulmonary infections with GA. Meyer et al (2024) analysed the effect of anaesthetic strategies on distal stroke thrombectomy, finding similar reperfusion rates between local anaesthesia (LA) with/without CS and GA for distal medium vessel occlusions (DMVOs) in the anterior and posterior cerebral arteries (ACA/PCA). However, GA showed a potential benefit in achieving complete reperfusion in ACA DMVOs
Personal perspective
In our practice, CS is preferred as the first choice, when feasible. This approach offers several benefits, including the ability to observe clinical improvements directly during the procedure. This real-time feedback aids in the decision-making process about when to conclude the intervention based on both angiographic and clinical criteria. Additionally, patients under CS are less likely to require intensive care post-procedure, allowing for more straightforward management and the possibility of transferring the majority to a stroke unit instead. It is also very rewarding to see the enthusiasm of the staff in witnessing direct improvements in the patients’ clinical condition, which serves as a motivating factor to treat these patients. In our centre,
If you are starting to perform thrombectomies, it may be beneficial to begin with GA to ensure better control and stability during the angiographic process. As experience and confidence grow, transitioning to CS could offer the aforementioned benefits. Assessing the patient’s ability to tolerate CS without significant anxiety or movement is crucial. Patients with poor collateral circulation or severe aphasia may not cooperate well, making GA a more suitable option. And, while becoming proficient in one approach is beneficial, maintaining flexibility to switch if the clinical situation warrants is essential for optimising patient outcomes. In our experience, CS is often the preferred choice for thrombectomy, offering immediate clinical feedback and more
The decision between GA and CS should be individualised, considering patient-specific factors and the collaborative input of the medical team.”
efficient postoperative management. However, the decision between GA and CS should be individualised, considering patient-specific factors and the collaborative input of the medical team. Both techniques have their advantages and drawbacks, and ongoing research will continue to refine best practices in this area.
References for this article can be viewed online.
Panagiotis Papanagiotou is a professor of radiology at Aretaieion University Hospital of National & Kapodistrian University (Athens, Greece), and a professor of neuroradiology and head of the Department of Diagnostic and Interventional Neuroradiology at Bremen Hospital (Bremen, Germany).
The author declared no relevant disclosures.
THE EUROPEAN STROKE Organisation (ESO) Executive Committee’s Thrombolysis Taskforce has provided “important updates” regarding the security of supply for Metalyse (tenecteplase) and Actilyse (alteplase) in the context of the European launch of Metalyse 25mg for acute ischaemic stroke treatment.
The European Medicines Agency (EMA) approved the use of Metalyse 25mg earlier this year, on 12 January.
A recent letter from the ESO Thrombolysis Taskforce notes that Boehringer Ingelheim—the company that markets both Metalyse and Actilyse—has adopted a stepwise approach for the launch of Metalyse 25mg. Initially, the thrombolytic drug will be launched in 11 European countries in 2024, aligning with national reimbursement timelines as well as production volumes. The expected schedule for 2024 is as follows:
February: Germany
March: Austria
April: Denmark, Finland, Iceland, Norway, Sweden and The Netherlands
May: Ireland
September: France
October: UK
Further expansion into other European and international markets is planned from 2025 onwards, according to the taskforce.
“We would also like to make you aware that Metalyse 40mg and 50mg are specifically intended for acute myocardial infarction and should not be used for acute ischaemic stroke treatment,” the letter continues. “Use of these dosages are regarded as offlabel use, and would deprive STEMI [ST segment elevation myocardial infarction] patients of essential treatment and risks destabilising the supply chain for Metalyse 25mg.”
In addition, Boehringer Ingelheim is anticipating an end of supply constraints for all Actilyse presentations in the second half of 2024—after the transfer of alteplase drug substance production to an additional Boehringer Ingelheim manufacturing site in Vienna, Austria is completed.
Throughout his life and career, Christophe Cognard (Toulouse, France) has always sought to help advance the interventional neuroradiology (INR) space, and make the management of neurovascular diseases as multidisciplinary and collaborative as possible. Notable examples include his efforts as president of the first-ever congress of the European Society of Minimally Invasive Neurological Therapy (ESMINT) back in 2009, and his contributions to numerous clinical trials that have served to further the treatment of intracranial aneurysms and brain arteriovenous malformations (AVMs). His non-INR interests are both extensive and eclectic too, ranging from medical law and climate change to the origins of the universe itself. Here, Cognard sits down with NeuroNews to discuss all this and more.
How did you first become interested in medicine?
I have never really been interested in medicine. When I was an adolescent, I was intrigued by fundamental physics, brain functioning, and protection of oceans and forests. I finally chose to go to medical school to become a psychiatrist. During my second year of medicine, I was also in my first year of philosophy at Sorbonne University (Paris, France), but I stopped after six months as I was not able to do both simultaneously. I did a fellowship in Paris, taking turns every six months in several psychiatry departments.
How would you say your time doing military service has impacted your medical career?
I did my military service over a period of 16 months in the West Indies, at Centre Hospitalier Universitaire (CHU) de Pointeà-Pitre (Les Abymes, Guadeloupe), as a young psychiatry consultant. This was a very interesting experience as I was personally in charge of patients—often from their emergency arrival at night with an acute delirium, for example, to their long-term follow-up months after in countryside dispensaries. At that time, I came to understand what the real ‘on-the-ground’ psychiatry discipline was. I particularly understood the chronicity of the diseases, and the low impact and efficacy of the therapists. To be a psychiatrist, you must be patient and modest, and accept that you will help patients rather than saving them.
Why did you decide to abandon psychiatry in favour of INR?
I wanted to be at the interface of psychiatry and neurobiology in order to better understand the functioning of the brain, and the causes of mental disorders. But, after three years of practising psychiatry and one year of research work in a department of neurobiology— involving purification and solubilisation of the 5HT1a serotonin receptors of rat hippocampi—I understood that, at that time, we were very far away from filling the gap between mental illness and neurobiology. I should have been more insistent as, today, it is a fascinating field.
Who have been your key mentors and how have they impacted your career?
After years of doubts and hesitations, I found my way when I was resident in Lariboisière Hospital (Paris, France) in the team of Jean
Jacques Merlan. It was a marvellous team full of passion, desires and the will to invent a new field in medicine. Alfredo Casasco was my first mentor. Then, Jacques Moret— with whom I spent three years in Rothschild Hospital (Paris, France)—taught me all of what I know today.
What are the most notable changes you’ve observed in INR practice during your time as a radiology professor?
The development of new devices has deeply changed our practice. Performing long injections of a large volume of liquid embolic, such as Onyx (Medtronic), through detachable catheters has changed the game—even if we still need to master glue injection. Flow diverters have been a revolution, allowing us to treat previously untreatable aneurysms e.g. giant, fusiform, dissecting. The Woven EndoBridge (WEB; Microvention/Terumo) has allowed us to treat very large-neck bifurcation aneurysms much more easily and in a very safe way. And, after years of technological failure, a stent developed to treat unruptured aneurysms (Solitaire [Medtronic]) has finally been used to reopen occluded arteries, and this perfect example of serendipity has revolutionised the treatment of stroke.
How did you come to lead the ESMINT congress in 2009?
The society was created by James Byrne, Daniel Rüfenacht and Jacques Moret, and they asked me to organise the first congress. I was president for two years, then co-president for four years, and then I decided to resign as I thought the congress should not be organised by the same guy for years, but that the presidents should change to represent all of the diversity of European practice. When working for ESMINT, I spend all my time trying to do my best to make it a multidisciplinary society gathering neuroradiologists, neurosurgeons and neurologists together in harmony.
How do you think the society and the congress have evolved in subsequent years?
ESMINT has become like the Society of NeuroInterventional Surgery (SNIS) or European Stroke Organisation (ESO)—one of the most important neurovascular societies in the world. It organises an annual congress, two European courses on INR and ischaemic stroke treatment, diplomas, and training with fellowships and e-fellowships. The most important thing is that ESMINT never
promotes one lobby but is at the interface of all neuroscience disciplines.
Could you outline why you recently became an expert in legal medicine?
Physicians are more and more concerned about legal issues. Eventually, physicians can end up doing bad medical practices because they are too afraid of being prosecuted and ignorant about the law. I wanted to understand both sides of the coin. I spent two years at university learning about law in medicine and, today, I really like to defend patients and families as a legal expert.
What are the most impactful studies you’ve been involved with throughout your career?
CURRENT APPOINTMENTS
2014–present: ESMINT Continuation Committee
2002–present: Chairman, Department of Diagnostic and Therapeutic Neuroradiology, Hospital of Purpan and Hospital of Rangueil
1999–present: Professor of radiology, University of Toulouse
EDUCATION
1989–1992: Fellowship in neuroradiology, Paris
1988–1989: Military service, CHU de Pointe-à-Pitre, Guadeloupe
1985–1989: Fellowship in psychiatry, Paris
1979–1985: Medical school, Sorbonne University
HONOURS (SELECTED)
2012–2014: President, ESMINT
2009: President, inaugural ESMINT congress
2009: President, SFNR congress
2008: Invited professor, University of Montreal, Canada
1985: Ranked 37th among 3,500 candidates in ‘Internat des Hôpitaux de Paris’ competition
ISAT was revolutionary, showing that coiling an aneurysm is better than clipping it. ISUAT was a very low-level study but it had the merit to show that most unruptured aneurysms should not be treated—even though, today, we still treat way too many aneurysms that should only be followed. ARUBA was another very low-level study, but it showed us that embolising unruptured AVMs is dangerous and that surgery, if possible—or abstention—is often better. And, indeed, after 20 years of attempts and failure to treat ischaemic strokes, the five big trials (MR CLEAN, ESCAPE, REVASCAT, SWIFT PRIME and EXTENDIA) produced results that were breathtaking and have changed the world. In addition, trials involving the late window, large cores, posterior circulation and other stroke types have followed. Today, there are also the recent studies on subdural haematomas as well (EMBOLISE, STEM and MAGIC-MT).
How would you assess the current landscape of INR, and how do you envisage the specialty changing over the next 10 years?
INR started as an intimist specialty dealing mainly with cerebral haemorrhagic disease not amenable by surgery in the 1980s. It became the gold-standard approach for aneurysms in the 1990s and has since become the way to treat large-vessel stroke. Today, embolisation is set to also become a treatment of choice not only for subdural haematoma but intracranial hypo/hypertensions and pulsatile tinnitus too.
But, I have some concerns (I sometimes feel like an old, conservative neurointerventionist). Our practice depends on technology, yet technology is somehow becoming more important than the clinical rigour and savviness of a skilled, trained and humble clinician. The fast pace of new devices entering the market sets up a sort of fanatic and less-considered adoption of novel technologies. I observe an escalation of new ‘stuff’—an increasing pressure on clinicians to use the latest, trendy thing and abandon technologies that have shown efficacy through the years, and also have the advantage of keeping the price of the procedure stable or even decreasing it compared to newer devices. The choice of contemporary technologies might be influenced by non-clinical reasons, such as a superficial aim of popularity exacerbated by professional and social network dynamics, or more obscure and as-yet unregulated agreements between clinicians and industry players. Who would have imagined, years ago, that numbers of followers and the ‘like-imperative’ could

become more important than the H-index, which translates the respect and consideration of our community of scientists and peers?
We’ve gotten used to the idea of being called key opinion leaders (KOLs) or even, imagine, a key online opinion leader (KOOL). I wish we could revise the process that makes us opinion leaders or opinion followers; mainly, I urge my colleagues—young and old—to value and cherish the independence of their opinions, and spend a lot of time and energy on working to critically form their own opinions. It takes study, and exchange, and sometimes discussions and the overcoming of differences and evolution of experiences. Let’s not give industry or anyone else the power to decide who is an opinion leader and who is not.
The risk I see in abandoning coils, balloons and stents for newer technologies is that we might lose skills. Treating an aneurysm with intrasaccular devices or flow diverters makes the procedure easy; the use of 3D-printed models or software to rehearse the procedure in advance makes it easier still. But, the cost
of a procedure escalates and operators lose their skills using devices that can be more dangerous or less efficient—except when used for the specific situations they have been developed for—and much more expensive.
What would your main pieces of advice be to aspiring INRs?
Be human. Spend time with and take care of your patients, and discuss with them. Don’t be too fascinated by novelties, techniques, devices and industry innovation. And, like an Englishman in New York, “be yourself, no matter what they say”.
If you required a neurointerventional procedure, which physician would you want to see leading your treatment?
Anyone—whatever their nationality, religion, colour, sex or specialty (neurologist, neurosurgeon, neuroradiologist etc.)—who is reasonable and properly trained, and who is not inclined to do technical acrobatics but able to manage all techniques and devices, including the old-fashioned ones.
"I observe [...] an increasing pressure on clinicians to use the latest, trendy thing and abandon technologies that have shown efficacy through the years.”
Could you outline any particularly interesting research you’ve seen recently?
Research on understanding the universe: black holes, dark matter, curvature of space-time. What was there five minutes before the big bang? And, artificial intelligence (AI). What will be the robots’ mental illnesses? Specialists are already speaking about ‘AI hallucinations’.
What are your hobbies and interests outside of medicine?
I’m very concerned about carbon dioxide and climate change. I have given several conference talks about this fear for humankind in the short term. I don’t understand the behaviour of humans, and the blindness and obscurantism to be able to destroy their own environment. For me, ‘climate sceptics’ are like flat-earthers, creationists or antivaxxers. I will give a talk at the next European Society of Neuroradiology meeting on the psychology of climato-scepticism. I stopped flying five years ago, and now spend my time on a farm with donkeys, ships and dogs, enjoying a vegetable garden and the beauty of life!







Despite the study very narrowly failing to meet its prespecified primary endpoint, the SWITCH randomised controlled trial has shown a substantial treatment effect with decompressive craniectomy procedures in people with severe, deep supratentorial intracranial haemorrhage (ICH). These findings were presented for the first time at this year’s European Stroke Organisation Conference (ESOC; 15–17 May, Basel, Switzerland) by Urs Fischer (University Hospital of Bern, Bern, Switzerland) and Jürgen Beck (University Hospital Freiburg, Freiburg, Germany).
“I THINK SWITCH INFORMS us about a substantial effect of this treatment in a population with no evidence-based therapy [available to them] so far,” Fischer said, responding to a question from the audience on whether the results indicate equipoise between surgery and medical therapy in this patient population. “The main question you, as a clinician, now have to discuss with the patients and their families is whether a modified Rankin scale [mRS] of 4 is something you would like to achieve, or not. Decompressive craniectomy does not increase the proportion of people who are bedridden or die [mRS 5–6]. I think all the evidence from these large trials should now be translated into clinical practice and, at the end of the day, it remains a personal decision.”
The SWITCH trial was conducted at 42 stroke centres across Europe in an effort to explore the potential benefits of decompressive craniectomy in these particularly severe ICH patients.
While recent, large-scale studies like ENRICH have linked positive outcomes to early, minimally invasive surgical evacuation in selected patients with superficial brain haemorrhages, the SWITCH investigators believe the effective treatment of deep ICH remains a “major unresolved issue”, as surgical evacuation is still yet to demonstrate decreased rates of disability or death.
SWITCH saw researchers attempt to ascertain the long-term outcomes of decompressive craniectomy in patients with deep brain haemorrhages. They enrolled adults aged 18–75 years, with severe, deep ICH affecting critical areas of the brain—including intraventricular haemorrhages—and assigned them to either decompressive craniectomy plus best medical therapy (BMT) or BMT alone.
Despite being halted prematurely due to funding constraints, the trial enrolled a total of 201 patients. Four did not consent, leaving 96 patients to be
allocated to surgery plus BMT (average age, 60 years; 67% male) and 101 to BMT alone (average age, 61 years; 69% male). Ultimately, 95 patients in each of these two groups were included in primary endpoint analyses. Regarding its primary endpoint— the proportion of patients with an mRS score of 5–6 at six months— the SWITCH trial closely missed demonstrating the statistical superiority of decompressive craniectomy plus BMT versus BMT alone, as 56% and 42% of patients, respectively,

achieved mRS 0–4 in the two groups. These figures led to a risk ratio (RR) of 0.77 and risk difference (RD) of −13% (p=0.057), which became significant with an RR of 0.76 and RD of −14% (p=0.042) once the data were imputed. Other key secondary endpoints revealed a statistically significant improvement with surgery versus medical therapy on mRS shift analyses, as 53% of patients in the craniectomy-plus-BMT group achieved mRS 0–4, compared to 40% in the BMT-only group (common odds ratio, 0.57; p=0.039).
Delivering the investigators’ interpretation of these results, Beck stated that decompressive craniectomy plus BMT in severe, deep supratentorial ICH “may be superior” compared to BMT alone, but “the evidence for that is weak”.
TACTICS, a non-randomised intervention trial that aimed to optimise workflow and implement specialised imaging, has shown promise in improving access to endovascular therapy (EVT) for patients in regional and rural areas of Australia.
“WHILE EVT HAS REVOLUTIONISED stroke treatment, access remains a challenge for patients outside major urban centres,” explained Candice Delcourt (Macquarie University, Sydney, Australia), the TACTICS investigator who presented these results at the European Stroke Organisation Conference (ESOC; 15–17 May, Basel, Switzerland).
“The TACTICS trial investigated a multifaceted intervention designed to address this disparity.”
Hospitals included in TACTICS saw the introduction of specialised education via a combination of face-toface, video and virtual reality-based approaches, as well as being fitted with and trained to use multimodal, advanced computed tomography (CT) brain imaging.
These efforts intended to optimise workflow and stroke pathways, improve diagnosis, and aid earlier detection, of EVT candidates within a ‘drip-and-ship’ model.
The trial involved six regional clusters of hospitals in Australia, each with a central hub capable of providing EVT and associated spoke hospitals. These clusters underwent a three-month preintervention period followed by a three-month intervention period, and then a three-month postintervention period.
TACTICS enrolled 1,011 patients across the six clusters and at a total of 34 hospitals. Compared to the preintervention period, the odds of receiving EVT in the pooled intervention and postintervention period increased by 44%. Notably, these improvements were
He also noted that, while there were no safety concerns in the surgical group relative to the medical group in the SWITCH trial, survival was associated with severe disability in both groups. Beck went on to echo Fischer’s point on the possible impact these new, “high-quality” data may have in terms of informing physician and caregiver decision-making regarding the treatment of severe, deep ICH patients. The investigators did also highlight several potential limitations of SWITCH, including the fact the trial was stopped early and may therefore have become underpowered; the trial’s “narrow” inclusion and exclusion criteria; its long recruitment period across more than 40 sites; and the occurrence of crossover from the surgical group to the medical group (1%), and vice versa (8%).
Lastly, they referred to the fact that the trial involved a highly selective group of patients with severe, deep ICH and, as such, its findings may not apply universally across other ICH types, including superficial haemorrhages, and smaller, less severe haemorrhages of deep brain areas.
Despite statistical significance being narrowly missed with regard to the trial’s primary endpoint, the investigators feel that SWITCH highlights a “substantial estimated effect size” compared to previous research as well as a “high degree of certainty of benefit” with decompressive craniectomy.
As such, they added that this intervention constitutes a potential treatment option in severe, deep ICH patients with no other evidence-based treatment options available to them— but, ultimately, SWITCH underscores the “urgent need” for further research into optimising care strategies for these patients.
Alongside Fischer and Beck’s latebreaking presentation at ESOC 2024, these data have also been published in The Lancet
consistent across all individual participating clusters.
“These findings suggest that this intervention has the potential to be a valuable tool for healthcare systems worldwide, particularly those grappling with geographic barriers to stroke care,” said Christopher Levi (University of Newcastle, Newcastle, Australia), lead investigator of TACTICS.
According to the investigators, further research is needed to confirm the long-term sustainability and generalisability of the TACTICS approach.
While EVT has revolutionised stroke treatment, access remains a challenge for patients outside major urban centres.”
Candice Delcourt
New research, presented at the 2024 European Stroke Organisation Conference (ESOC; 15–17 May, Basel, Switzerland), has revealed that high-income individuals have a 32% lower risk of post-stroke mortality. Additionally, those with a higher level of education have a 26% lower risk of death post-stroke, highlighting striking disparities in stroke survival based on key social determinants of health (SDoH).
The registry-based study analysed data from 6,901 stroke patients in Gothenburg, Sweden between November 2014 and December 2019 to examine the impact of SDoH factors on post-stroke mortality risk. The study focused on four SDoH factors: living area, country of birth, education and income.
As well as identifying a significant connection between income, education level and post-stroke mortality risk, the study uncovered a concerning trend regarding the cumulative impact of SDoH factors. Patients with one unfavourable SDoH factor faced an 18% higher risk of mortality compared to patients without any unfavourable SDoH factors. This risk also escalated to 24% for patients with two to four SDoH factors.
“Our findings underscore a stark reality—an individual’s socioeconomic status can be a matter of life or death in the context of stroke, especially when they are confronted with multiple unfavourable SDoH factors,” said lead author Katharina Stibrant Sunnerhagen (University of Gothenburg, Gothenburg, Sweden). “While our study was conducted in Gothenburg, we believe these insights resonate across Europe, where similar healthcare structures and levels of social vulnerability exist, highlighting a pervasive issue throughout the continent.”
The study also found a link between increased mortality risk and additional risk factors like physical inactivity, diabetes, alcohol abuse and atrial fibrillation.
Notably, insights emerged regarding gender disparities and the potential impact of risk factors when examining patient characteristics within the study cohort. The proportion of female patients increased with the number of unfavourable SDoH factors; 41% of the group with no unfavourable SDoH factors were female, whereas 59% of the group with two to four unfavourable SDoH factors comprised females.
‘Time is brain’ in ICH but early detection of stroke type also key
The latest data from the INTERACT trials—a series of studies evaluating intensive blood-pressure (BP) lowering in acute haemorrhagic stroke—point towards the importance of initiating BP reduction as early as possible in patients with intracranial haemorrhage (ICH), but also highlight the potentially harmful effect of these approaches in ischaemic stroke patients.
THE 2024 EUROPEAN STROKE Organisation Conference (ESOC; 15–17 May, Basel, Switzerland) saw Xia Wang (The George Institute for Global Health, Sydney, Australia) deliver findings from a pooled analysis looking specifically at the effect of early BP lowering on haematoma growth in acute ICH patients across all four of the INTERACT randomised controlled trials (RCTs) conducted to date, before Gang Li (Shanghai East Hospital, Shanghai, China) and Lili Song (Fudan University, Shanghai, China) presented first-time data from INTERACT4, which sought to assess the impact of ambulancedelivered BP reduction in patients with suspected acute stroke.
“We have shown that the principle of ‘time is brain’ is also applicable to ICH,” said Wang, a leading author for the former of the two studies. “It is our hope that guidelines will not only strengthen but enforce the importance of time in achieving this level of control.”
In her ESOC 2024 presentation, Wang outlined data from 2,921 ICH patients in the four INTERACT trials, which compared BP lowering to a systolic BP of <180mmHg versus <140mmHg. The four trials, conducted mainly in China, used consistent BP treatment protocols with intravenous agents, as well as standardised imaging assessment and
reading paradigms. Wang et al’s pooled analysis aimed to determine if the timing of initiating BP lowering affected haematoma growth—and their results ultimately showed that the likelihood of mitigating haematoma growth was improved when BP lowering treatment commenced early. Moreover, they produced data suggesting that it is “the earlier, the better” when it comes to BP reduction in acute ICH patients, as starting the treatment sooner was linked to a greater reduction in haematoma growth, up to a ‘cut-off’ of three hours.
“We wanted to determine if very early treatment of BP reduces bleeding in the brain,” Wang stated. “In our patient cohort, the median time from the onset of ICH to randomisation was approximately three hours, and it typically took about one hour to achieve a target BP of less than 140mmHg. Thus, it generally took several hours to achieve BP control after an ICH. In clinical practice though, we can be much quicker, [as] randomisation is not required. Our data show time influences the potential chances of making a recovery from ICH.”
Meanwhile, presentation of INTERACT4 revealed evidence that identifying whether a stroke is haemorrhagic or ischaemic in nature as early as possible could be key to
Additionally, smoking—whether current or within the past year—was more prevalent in the group with two to four unfavourable SDoH factors compared to those with none (19% vs 12%).
Commenting on the actions required to reduce the future stroke burden, Stibrant Sunnerhagen added: “As the number of people affected by stroke in Europe is projected to rise by 27% between 2017 and 2047, the need for effective interventions is more pressing than ever.
“In light of our study’s findings, targeted strategies are essential. Policymakers, for instance, must tailor legislation and approaches to account for the specific circumstances and needs of diverse communities, while clinicians should consider identifying patients with unfavourable SDoH factors to prevent post-stroke mortality.
“By addressing these disparities, we will not only support the principles of health equity, but also have the potential to significantly enhance public health outcomes.”
While our study was conducted in Gothenburg, we believe these insights resonate across Europe.”
harnessing the benefits of very early, in-ambulance BP lowering for patients with suspected acute stroke. The trial— simultaneously published in the New England Journal of Medicine alongside its ESOC presentation—found that intensive BP reduction improved functional outcomes in haemorrhagic stroke patients but worsened outcomes in those with ischaemic strokes.
“Our study highlights the clear benefits of early BP lowering treatment for patients with ICH in the ambulance,” said Craig Anderson—also of The George Institute for Global Health—who was the lead investigator for INTERACT4. “However, it did not alter outcomes for suspected stroke patients overall. In fact, in patients diagnosed with ischaemic stroke, early BP lowering treatment increased death and disability, emphasising the need for a reliable diagnosis at an early stage to harness the benefits of very early BP treatment.”

INTERACT4 was a multicentre, blinded-outcome RCT conducted across dozens of ambulance services in China. It enrolled 2,404 ambulance-assessed patients with suspected acute stroke causing a motor deficit within two hours of onset and elevated systolic BP (≥150mmHg), who were then randomly assigned to immediate, prehospital BP lowering—with a target of 130–140mmHg within 30 minutes—or usual BP management in hospital.
Haemorrhagic stroke patients in the former of these two groups were found to have a lower likelihood of experiencing a poor functional outcome, as compared to haemorrhagic stroke patients who received in-hospital BP
management. Conversely, patients with cerebral ischaemia—those suffering from an ischaemic stroke—had a higher likelihood of experiencing poor functional outcomes in the prehospital BP lowering group versus the in-hospital group. The INTERACT4 investigators also found that, overall, there was balance between the benefits and the harm that early BP reduction may confer, as—across all stroke patients— there was no significant difference in functional outcomes between the two approaches to BP control. The investigators determined that between-group rates of serious adverse events were similar as well.
“All treatments for acute stroke are highly timedependent, as brain cells rapidly deteriorate when deprived of oxygen—but, determining the best treatment approach before identifying the stroke type is difficult without brain imaging,” Anderson explained. “The results do not support in-ambulance administration of BP lowering treatment in patients with suspected acute stroke, that is clear. However, in the last few years, we’ve seen the introduction of mobile stroke ambulances equipped with CT [computed tomography] scanners and diagnostic tools that aim to identify cases of ischaemic stroke for early administration of clot-busting treatment. Additionally, in-ambulance treatment for haemorrhagic stroke is supported by our results. In the meantime, while acute stroke treatment happens in the hospital, quicker diagnosis and swift action upon the patient’s arrival at the emergency department is critical to preserving brain function.”
Intravenous thrombolysis (IVT) prior to mechanical thrombectomy appears to be less effective in ischaemic stroke patients with carotidartery tandem lesions, as compared to those without tandem lesions, as per findings from a MR CLEANNO IV subanalysis presented at the 2024 European Stroke Organisation Conference (ESOC; 15–17 May, Basel, Switzerland).
DELIVERING THESE RESULTS, Fabiano Cavalcante (Amsterdam University Medical Centers, Amsterdam, The Netherlands) was quick to emphasise that the present findings apply to patients presenting directly to a comprehensive stroke centre (CSC) capable of administering thrombectomy treatments. He also reported similar rates of intracranial
haemorrhage (ICH) across patients with and without tandem lesions, effectively refuting the causal pathway investigators had hypothesised for a difference in treatment effect and meaning they “cannot explain” the contrasting functional outcomes between the two groups.
The MR CLEAN-NO IV trial— published in 2021—evaluated thrombectomy with/without prior IVT in European patients, and ultimately found ‘direct thrombectomy’ approaches to be neither superior nor non-inferior to thrombectomy with IVT.
“Perhaps the solution to this problem lies in patient selection,” Cavalcante said. “Patients presenting early appear to benefit from IVT and also, possibly, patients with tandem lesions could [experience] a different effect of IVT. These patients represent about 15% of all those undergoing endovascular treatment and are thus a clinically relevant population.”
be more likely to have large-artery atherosclerosis as an aetiology, better collateral scores, worse functional outcomes on the modified Rankin scale (mRS), and any ICH, compared to nontandem lesion patients.
in the rate of symptomatic ICH, which was our primary hypothesis to explain a difference in treatment effect […] in this population. Thus, the mechanism behind this treatment-effect heterogeneity remains unclear.”

Cavalcante et al therefore conducted a subanalysis of MR CLEAN-NO IV including patients with tandem lesions in their carotid arteries—a population that accounted for 17% of the 539 patients enrolled in the original trial.
Regarding baseline differences, patients with tandem lesions were found to
Intention-to-treat analyses of the study’s primary endpoint—90-day ordinal shift in mRS scores—revealed that stroke patients without tandem lesions who were treated with IVT prior to thrombectomy experienced “slightly better functional outcomes” compared to those who did not receive IVT; an observation “in line” with the effect of IVT in the overall population of MR CLEANNO IV. However, tandemlesion patients experienced worse functional outcomes when treated with IVT versus without, and a statistically significant difference was observed here (p=0.02).
“We see similar results when we analyse the rate of patients with excellent functional outcomes [mRS 0–1], and the rate of patients with good functional outcomes [mRS 0–2] as well,” Cavalcante reported.
“And, we see a similar trend in the opposite direction when we assess the rate of patients having a poor functional outcome or mortality—but, importantly, we do not see an increase
data provide “compelling evidence” that intracranial stenting does not confer
Seven-year data from the Chinese CASSISS trial have, in the investigators’ view, provided “compelling evidence” that percutaneous transluminal angioplasty and stenting (PTAS) plus medical therapy does not confer additional benefits over medical therapy alone in patients with symptomatic, severe intracranial atherosclerotic stenosis. Peng Gao (Capital Medical University, Beijing, China) presented these findings at the 2024 European Stroke Organisation Conference (ESOC; 15–17 May, Basel, Switzerland), informing audiences that “these results underscore the importance of medical therapy as the cornerstone of long-term stroke prevention in this patient population”.
GAO BEGAN BY NOTING THAT PRIOR randomised trials, including SAMMPRIS and VISSIT—as well as initial follow-up data from CASSISS itself, published in 2022—have indicated no benefit when adding PTAS to medical therapy in symptomatic, severe intracranial atherosclerotic stenosis patients. However, he added that it “remains uncertain” whether PTAS can enable improved outcomes at five years or more. With three-year results having already been published, Gao and colleagues’ present analysis of CASSISS sought to shed further light on stenting versus medical therapy in these patients at an even longer follow-up timepoint.
CASSISS was a multicentre, open-label, randomised controlled trial conducted at eight centres across China, enrolling patients experiencing a transient ischaemic attack or ischaemic stroke with a modified Rankin scale (mRS) score of 0–2 attributed to severe intracranial atherosclerotic stenosis—meaning stenoses of 70–99%. These patients were then randomised 1:1 to either PTAS with the Wingspan stent (Stryker Neurovascular) plus medical therapy involving three months of dual antiplatelet therapy followed
by single antiplatelet therapy thereafter, or medical therapy alone.
The trial’s primary endpoint was a composite outcome including stroke and death within 30 days post-enrolment, or stroke in the territory of the qualifying artery beyond 30 days. Between March 2014 and November 2016, a total of 380 patients were enrolled, with 188 being randomised to the PTAS group and 192 randomised to the medical therapy group. Some 358 patients were confirmed as eligible for final analyses and, of these, 237 (66.2%) completed the study’s seven-year follow-up.
Regarding CASSISS’ primary endpoint, Gao reported no difference between the two study groups across the seven-year follow-up period (hazard ratio, 1.02; p=0.97), as 14.8% of 176 patients in the PTAS group and 14.3% of 182 patients in the medical therapy group experienced stroke/death within 30 days or qualifying-artery stroke beyond 30 days. The presenter also relayed no major differences between the PTAS and medical therapy groups concerning a number of secondary outcomes, including ipsilateral ischaemic stroke (14.8% vs 14.3%), disabling stroke or death
Before wrapping up, Cavalcante disclosed several limitations, including the ‘secondary’ nature of the analysis and the fact that data from three trials also investigating thrombectomy with/ without IVT in tandem lesions have not replicated these findings.
“For patients who present directly to centres capable of providing endovascular treatment, IVT before [thrombectomy] was less effective in patients with tandem lesions, and more effective in patients without tandem lesions,” Cavalcante concluded. “This interaction and [treatment]-effect modification has limited credibility, so we believe that should be taken into consideration [and the results] should be interpreted carefully.”
The mechanism behind this treatment-effect heterogeneity remains unclear.”
(16.5% vs 14.3%), and death (9.1% vs 7.1%), after enrolment. Additional safety-related endpoints, such as rates of disabling ischaemic stroke, symptomatic intracranial haemorrhage, and both stroke-related and non-stroke-related death, were statistically similar between groups as well.
Intention-to-treat analyses of the two components of the primary endpoint revealed a trend towards a lower risk of stroke specifically in the territory of the qualifying artery post-30 days within the PTAS group (9.7%), compared to the medical therapy group (12.1%), but this observation did not reach statistical significance. This also contrasted with a slightly higher—but still statistically insignificant—rate of 30day stroke/death in the PTAS group (5.1%) versus the medical therapy group (2.2%).
Gao noted some “inherent limitations” of the trial, including the fact it was conducted solely in Han Chinese patients and, as such, has “uncertain” generalisability to other populations. Also, CASSISS did not evaluate angioplasty alone—or other devices like drug-coated balloons and drug-eluting stents that are currently used off-label to treat intracranial atherosclerotic stenosis. Finally, Gao conceded that the trial may not fully reflect present-day clinical practice, as patients were treated in line with the 2014 American Stroke Association (ASA) guidelines, and many changes in stroke management are likely to have occurred in the years since then.
“Medical and interventional management have been improving in equal strides since the 2014 ASA guidelines,” Adam A Dmytriw (Massachusetts General Hospital, Boston, USA), one of the authors for the original publication of CASSISS in the Journal of the American Medical Association (JAMA) two years ago, told NeuroNews. “It remains to be seen whether there is a select population of intracranial atherosclerotic stenosis patients who might benefit from stenting, and what tools we might need to make that selection.”
This year’s European Stroke Organisation Conference (ESOC; 15–17 May, Basel, Switzerland) saw a plethora of data on intravenous tenecteplase—from studies spanning Australia, Canada, China, Europe, and beyond—presented for the first time. Fresh findings from the ATTENTION-IA, ORIGINAL, TASTE, TEMPO-2 and TRACE III randomised controlled trials (RCTs) were disclosed, as were a combined analysis of data from the SWIFT DIRECT and EXTEND-IA TNK studies, and a meta-analysis of a total of nine already-published RCTs in this space.
“DURING ESOC 2024, SEVERAL TRIALS were presented in which tenecteplase was evaluated versus alteplase,” Robin Lemmens (KU Leuven, Leuven, Belgium), chair of the ESOC 2024 Conference Planning Committee, told NeuroNews. “Data from trials like TASTE and ORIGINAL were again illustrations of the benefit of tenecteplase, which will likely result in the replacement of alteplase for the treatment of acute stroke. Furthermore, the use of tenecteplase was explored in patients presenting in the later time window and for an additional effect after endovascular treatment. Although not all these results showed improved outcomes in patients treated with tenecteplase, these trials highlighted the shift [in recent] years towards tenecteplase in studying extra indications for thrombolysis. TEMPO-2 provided important evidence that, although thrombolysis is an important treatment option for acute stroke patients with clear functional impairment, it should not be the first treatment for patients with minor stroke. In short, the future of thrombolysis for acute stroke will involve tenecteplase, but not for each clinical scenario, and indications may shift with evidence from trials to come.”
First to be presented was the international, phase-three TASTE trial, with principal investigator Mark Parsons (University of Newcastle, Callaghan, Australia) reporting that tenecteplase narrowly failed to demonstrate noninferiority to alteplase—the traditional gold standard for intravenous thrombolysis (IVT)—in intention-to-treat (ITT) analyses. TASTE, which specifically included acute ischaemic stroke patients presenting within 4.5 hours of symptom onset and selected via perfusion imaging, did, however, find tenecteplase non-inferior to alteplase in its per-protocol analysis.
“TASTE is the largest clinical trial ever in stroke to use modern brain perfusion imaging selection in all patients,” Parsons said, also noting that the trial exclusively included patients with a proven tissue target for reperfusion treatment. “Thus, the TASTE results increase confidence that tenecteplase is actually a superior agent [to alteplase] for stroke thrombolysis.”
TASTE was a non-inferiority trial conducted in 35 hospitals across eight countries, with all patients undergoing measurement of salvageable tissue— known as ‘target mismatch’—on brain perfusion imaging, before being randomly assigned to either tenecteplase or alteplase. Its primary endpoint was the proportion of patients without disability (modified Rankin scale [mRS] 0–1) at 90 days. The trial was stopped early in light of positive results from previous tenecteplase trials, with a total of 680 patients having been randomised.
In ITT analysis, the primary endpoint occurred in a numerically higher proportion of patients allocated to tenecteplase (57%) versus alteplase (55.3%), translating into a standardised risk difference of 0.03 and marginally missing the predefined non-inferiority criteria of a lower boundary of −0.03. However, noninferiority was demonstrated via per-protocol analyses,




and the trial also found that safety outcomes including all-cause mortality and symptomatic intracranial haemorrhage (sICH) were comparable between groups. TASTE’s investigators have stated that their results are in line with those from previous tenecteplase trials for acute ischaemic stroke and indicate the drug’s superiority over alteplase—regarding ‘excellent’ threemonth recovery—shown in meta-analyses alongside other studies.
Another study featured at ESOC 2024 was the ORIGINAL trial, delivered by Shuya Li (Capital Medical University, Beijing, China), which ultimately deemed tenecteplase statistically non-inferior—but not superior—to alteplase in terms of 90-day mRS 0–1.
Some 72.7% of 732 patients treated with tenecteplase and 70.3% of 733 treated with alteplase in the study achieved this outcome, resulting in a non-inferiority risk-ratio (RR) margin of 0.937. Ninety-day mRS score distribution was found to be statistically similar between groups as well.
Also assessing acute ischaemic stroke patients presenting within 4.5 hours of symptom onset, but doing so across 55 sites in China, the trial’s primary endpoint finding of 90-day mRS 0–1 being comparable between the two drugs remained consistent across multiple prespecified subgroups, including age, gender, comorbidities, baseline National Institutes of Health stroke scale (NIHSS) score, time to administration, and whether or not mechanical thrombectomy was performed. In addition, several secondary efficacy endpoints, such as rates of 24-hour major neurological improvement (48% vs 45%) and 90-day mRS 0–2 (80.9% vs 79.9%) were statistically similar between tenecteplase and alteplase, as were safety endpoints including rates of adjudicated sICH events (5.2% vs 5.3%), all-cause mortality (4.6% vs 5.8%), and 90-day mRS 5–6 (6.8% vs 7.8%).
Li’s concluding message on behalf of the ORIGINAL investigators was that these results are
consistent with those seen in prior investigator-initiated tenecteplase trials, supporting use of the drug as a “promising alternative” to alteplase as the standard of care in acute ischaemic stroke.
Findings from TRACE III—another trial in China evaluating tenecteplase, this time when administered in a later time window of 4.5–24 hours post-stroke—were presented on the same day by Yunyun Xiong (Capital Medical University, Beijing, China). Xiong reported that tenecteplase improved functional outcomes in large vessel occlusion (LVO) stroke patients with salvageable tissue on perfusion imaging and without access to thrombectomy, providing evidence of the benefits the drug can enable in settings where patients do not have immediate access to endovascular treatment.
Conducted across a number of centres in China, TRACE III randomised 516 eligible patients to receive either tenecteplase in the intervention group or standard medical therapy involving aspirin and/or clopidogrel in the control group. Tenecteplase was associated with a higher rate of patients achieving 90-day mRS 0–1, as compared to medical therapy (33% vs 24.2%), leading to a relative RR of 1.37. Mortality at 90 days was comparable between the intervention and control groups, and, while there was a numerically higher rate of sICH observed with tenecteplase (3% vs 0.8%), this did not reach statistical significance.
“The trial demonstrates a clear benefit of intravenous tenecteplase in patients with LVO and tissue at risk of infarction up to 24 hours after symptom onset,” Xiong stated. “These results are important for patients arriving in the late or unknown time window who require interhospital transfer, and in whom there is no guarantee they will remain eligible for endovascular thrombectomy on arrival.”
Positivity surrounding tenecteplase was dampened slightly the following day—initially by a further study from China, ATTENTION-IA, which found no significant differences in terms of functional outcomes, mortality or ICH, when comparing the drug to standard medical therapy. There were, however, multiple design discrepancies between ATTENTION-IA and some of the other RCTs presented at ESOC, including the fact it exclusively enrolled patients with posterior-circulation stroke—TRACE III, for example, only included anterior-circulation patients—and also its focus on the effects of tenecteplase after a thrombectomy procedure specifically. Nevertheless, investigators for the ATTENTION-IA study have noted that their results are “contrary to expectations” and a “surprising revelation”, and that they “challenge assumptions, emphasising the need for continued research in stroke management”.
The trial was conducted at 31 centres across China and sought to determine the efficacy of tenecteplase following successful endovascular recanalisation— defined as a thrombolysis in cerebral infarction
The future of thrombolysis for acute stroke will involve tenecteplase, but not for each clinical scenario, and indications may shift with evidence from trials to come.”
Robin Lemmens
(TICI) score of 2b50 or higher—in patients whose acute stroke was caused by a posterior-circulation occlusion. Investigators enrolled 208 patients and randomised them 1:1 to receive tenecteplase or medical therapy post-thrombectomy. At 90 days, as per ATTENTION-IA’s primary endpoint, 34.6% of tenecteplase patients and 26% of medical-therapy patients achieved mRS 0–1; a difference that did not reach statistical significance. The trial was therefore unable to demonstrate tenecteplase’s superiority over the existing standard of care in posterior-circulation stroke and, while a comparable mortality rate between groups was observed, Wei Hu (University of Science and Technology of China, Hefei, China)—who presented these findings at ESOC—concluded that tenecteplase after thrombectomy does not provide any added benefit and may, potentially, increase sICH risks. Investigators have also suggested that their results highlight “the need for further exploration and refinement of treatment protocols in this challenging clinical scenario”.
The fifth and final large-scale tenecteplase RCT presented was TEMPO-2. Shelagh Coutts (University of Calgary, Calgary, Canada) delivered first-time findings from the trial, which aimed to improve the current understanding of tenecteplase’s impact on clinical outcomes—as compared to antiplatelet therapy—in non-disabling minor ischaemic strokes caused by confirmed intracranial occlusion. A prospective study conducted at various global sites, TEMPO-2 set out to establish tenecteplase’s superiority over the current standard of care—but was halted prematurely due to futility, and ultimately revealed no significant benefit, as well as higher mortality and sICH rates, with tenecteplase.
A total of 886 patients were enrolled in the trial and randomised to either tenecteplase or a control group involving standard medical therapy with antiplatelet medications. TEMPO-2’s primary efficacy endpoint—a return to baseline functioning on mRS at 90 days—was not notably different between groups, being achieved by 72% of 432 patients on tenecteplase and 75% of 452 on antiplatelets. In addition, eight patients in the tenecteplase group (2%) experienced sICHs, while only two such cases were observed with controls (<1%).
Investigators have described this as an “expected finding” that was low in incidence and similar in both groups—but also one to which the lack of benefit with tenecteplase in the trial cannot be attributed, as sICH rates were not statistically significantly different between groups. Finally, a higher 90-day mortality rate was observed with tenecteplase (5%) versus controls (1%), due to “what appears to be a series of late deaths biologically unrelated to the drug”.
Ultimately, TEMPO-2 investigators feel that, while tenecteplase failing to show benefit in their study
is a divergence from prior meta-analysis evidence, this finding is “entirely concordant” with the recent PRISMS and ARAMIS trials. They have suggested that their results may yet “pave the way to treatment tailoring and optimisation”, but conclude that—for now—antiplatelet therapy should be favoured over IVT for the majority of minor ischaemic stroke patients.
Audiences witnessed additional first-time data presentations at ESOC, with one such presentation coming from Valerian Altersberger (University Hospital Basel, Basel, Switzerland). Altersberger delivered findings from a combined analysis of two previously published trials, SWIFT DIRECT and EXTEND-IA TNK, revealing that tenecteplase prior to thrombectomy was not associated with improved functional independence at 90 days, as compared to thrombectomy alone, but was linked to a higher proportion of nondisabling functional outcomes.
Using a ‘target trial emulation’ design, researchers from Australia and Switzerland combined observational data from 187 patients in the thrombectomy-only group of SWIFT DIRECT, and 240 patients treated with tenecteplase followed by thrombectomy in parts one and two of EXTEND-IA TNK. Based on the analysis’ primary endpoint, tenecteplase did not lead to a significant increase in patients achieving 90-day functional independence, as 58.3% of patients treated with the drug pre-thrombectomy achieved mRS 0–2, compared to 56.2% of patients who underwent ‘direct’ thrombectomy without prior tenecteplase. However, across the full range of mRS scores, investigators found an association between pretreatment with tenecteplase and better functional outcomes—signified by a greater mRS reduction—with an adjusted odds ratio of 1.5. The rate of freedom from disability (mRS 0–1) was higher with tenecteplase (47.9%) versus without (38%) too, while mortality and sICH rates did not differ significantly between groups. Further analyses also suggested that tenecteplase-related improvements in outcomes appeared most evident in patients treated early after symptom onset.
“Our results may reflect a potential benefit of ‘bridging’ with tenecteplase prior to thrombectomy,” Altersberger said. “As the two arms in this target trial emulation originate from different trials conducted within different settings, results should be validated in an RCT.”
At ESOC, another presentation of fresh data on tenecteplase in acute stroke care saw Lina Palaiodimou (National and Kapodistrian University of Athens, Athens, Greece) outline findings from a systematic review and meta-analysis of a total of nine RCTs evaluating tenecteplase’s usage in the early time window (<4.5 hours) as compared to alteplase. Results spanning thousands of patients included in the AcT, ATTEST, ATTEST-2, EXTEND-IA TNK, TAAIS,
TASTE-A, TNK-S2B, TRACE and TRACE II trials ultimately suggested tenecteplase was associated with improved rates of excellent functional outcomes (mRS 0–1) at 90 days, and was reasonably safe in terms of all-cause mortality and sICH, versus alteplase. Further assessments of seven of the nine aforementioned studies also indicated that tenecteplase was superior to alteplase in terms of reducing disability, with mRS shift analyses favouring the former of the two drugs.
“While there are nuances and differences between the trials comparing tenecteplase with standard of care—be that thrombolysis with alteplase or antiplatelets—a clear picture is emerging,” ESO treasurer Jesse Dawson (University of Glasgow, Glasgow, UK) told NeuroNews “The evidence is accumulating that, where thrombolysis is indicated, tenecteplase is at least as good, as safe, and maybe better, than treatment with alteplase.”
“These recent studies provide further evidence to substantiate the case that tenecteplase can be the standard-of-care thrombolytic agent in patients with acute ischaemic stroke,” added Bijoy Menon (University of Calgary, Calgary, Canada), programme vice chair for next year’s International Stroke Conference and a leading investigator for the AcT trial. “Studies such as TEMPO-2, TRACE III and ATTENTION-IA help to better clarify the border zones of thrombolysis efficacy and safety. With this transition to tenecteplase in our practice worldwide, we also have a unique opportunity to generate more randomised evidence on how best to give tenecteplase—when and at what dose—in different patient risk groups, including the elderly; those with cognitive impairment, large infarcts or small clots; those on newer anticoagulant or antithrombotic agents; those with comorbidities such as renal failure; those who are candidates for emergent endovascular therapy, or those who present late after stroke onset. Such randomised evidence will help increase the confidence we as physicians have in treating our diverse patient population with this life-saving medication.”
“The enormous number of tenecteplase studies presented at ESOC demonstrate the tremendous international enthusiasm for this agent,” stated Gregory Albers (Stanford Medicine, Stanford, USA), principal investigator for the TIMELESS trial—which was published in full in February 2024, and found that tenecteplase initiated 4.5–24 hours after stroke onset was safe in terms of mortality and sICH but did not substantially improve clinical outcomes versus placebo. “The results presented solidify the following conclusions: tenecteplase should replace alteplase for treatment of disabling strokes within 4.5 hours of onset; tenecteplase can be administered safely up to 24 hours in stroke patients with imaging evidence of penumbral tissue and an infarct core less than 70ml; and neither tenecteplase nor alteplase is appropriate for very minor, non-disabling strokes.”
CEA versus TCAR: surgeons should be familiar with both procedures and ‘collaborate as needed’
When it comes to the ongoing debate of carotid endarterectomy (CEA) versus transcarotid artery revascularisation (TCAR) in the treatment of carotid artery stenosis, operators should be comfortable and maintain experience with both of these procedures—and “collaborate as needed”. That is the ultimate finding of a registry analysis presented for the first time at the 2024 Vascular Annual Meeting (VAM; 19–22 June, Chicago, USA).
The analysis in question was delivered by Andrea Alonso (Boston University, Boston, USA) on behalf of lead author Jeffrey J Siracuse (Boston University, Boston, USA) and colleagues.
“Our study observed an inverse relationship between the proportion of a procedure—either TCAR or CEA—conducted by a surgeon, and the rate of postoperative stroke, with surgeons performing the lowest proportion having the highest stroke rates,” Alonso told NeuroNews “Our data also suggest that, among surgeons with a more balanced practice, there
continues to be a low rate of stroke. To minimise postoperative stroke risk, we conclude that surgeons who offer both types of carotid revascularisation procedures maintain a balance. We also suggest collaboration in challenging cases, leveraging the diverse expertise within a practice, to reduce stroke risk.
“We believe that this can be done effectively in the preoperative setting while evaluating challenging cases and with advanced coordination with colleagues to assist in key parts of the operation. This step takes insight from the lead surgeon to recognise the surgical techniques that they may require more assistance with at that stage in their practice, as well as camaraderie within the practice group.”

According to the authors, TCAR adoption among surgeons has been variable—many still perform more traditional CEAs, while others have shifted mostly to TCAR in their practice. Researchers therefore set out to evaluate the association between surgeons’ relative volumes of CEA to TCAR, and perioperative outcomes, via analyses of the Vascular Quality Initiative (VQI) CEA and carotid artery stenting (CAS) registries from 2021–2023.
Across both registries, participating surgeons were categorised in the following CEA/TCAR volume percentage ratios: 0–25/76–100 (majority TCAR); 26–50/51–75 (more TCAR); 51–75/26–50 (more CEA); and 76–100/1–25 (majority CEA). Primary outcome measures for the analysis consisted of rates of perioperative ipsilateral stroke, death, cranial nerve injury (CNI) and return to the operating room (RTOR) for bleeding.
The researchers found that there were 50,189 patients who underwent primary carotid
New data presented at the 2024 Vascular Annual Meeting (VAM; 19–22 June, Chicago, USA) have revealed poor overall rates of medical therapy adherence in moderate asymptomatic carotid stenosis patients—with smoking cessation representing a “ripe target” for improvement moving forward.
“THE OBJECTIVES OF THIS study were to examine adherence to three common tenets of medical therapy among a cohort of patients treated with medical therapy alone, and then to identify shortfalls in therapy to serve as opportunities for improvement,” said Randall Bloch (St Elizabeth’s Medical Center, Boston, USA), presenting these data on behalf of senior author Mark Conrad (St Elizabeth’s Medical Center, Boston, USA) and colleagues.
Bloch et al’s single-centre, retrospective study reviewed consecutive carotid duplex ultrasound scans from 2019–2020. Patients with moderate (50–69%) asymptomatic carotid stenosis— based on Society for Vascular Surgery (SVS) guidelines—were included, while those who underwent upfront surgery “for any reason” were excluded, as were those without available follow-up data. Patients were assessed for their adherence to optimal medical therapy at
the time of the index duplex scan, the first follow-up visit, and at each subsequent follow-up visit until the end of the study, ultimately leading to a median follow-up period of 2.7 years. In the study, optimal medical therapy was defined via three key tenets: abstinence from smoking; use of aspirin or other antiplatelets; and use of statins or other lipid-lowering therapies.
The study, now also published in the Journal of Vascular Surgery, identified a total of 323 duplex ultrasound examinations with moderate asymptomatic carotid stenosis across 255 patients. Bloch reported that 56.1% of these patients were already on all three of the aforementioned aspects of medical therapy at the time of the index duplex, with this rate improving to 68.6% by the end of follow-up.
“However,” Bloch continued, “when looking specifically at the 112 patients that were not already on medical therapy, 38.4% were able to achieve adherence to
revascularisations (CEA, 64.3%; TCAR, 35.7%), also noting that—on average—CEA patients were younger (71.1 vs. 73.5 years, p<0.001), with less coronary artery disease and diabetes, fewer symptomatic cases, and lower antiplatelet and statin use (all p<0.001). Meanwhile, they observed that TCAR patients had lower rates of end-stage renal disease, smoking and obesity (all p<0.001).

Postoperative stroke after CEA was found to be significantly impacted by relative surgeon volume ratio (p=0.04), with “majority TCAR” surgeons having higher rates of postoperative ipsilateral stroke (odds ratio [OR], 2.12; 95% confidence interval [CI], 1.15–3.9; p=0.02). Alonso also reported that there was a trend indicating a higher stroke rate after TCAR in “majority CEA” surgeons—however, this did not reach statistical significance. In addition, they saw no association between relative volumes and perioperative death, CNI or bleeding-related RTOR for either procedure.
It is based upon these findings that the researchers conclude that relative surgeon ratios of CEA versus TCAR do appear to influence perioperative stroke rates when it comes to CEA, emphasising the need for surgeons to be familiar with both procedures and work cohesively.
“There are multiple positive impacts that can arise from these kinds of collaboration,” Alonso added. “Principally, one is a reduction in patient stroke rate, particularly for patients with challenging disease. Other positive impacts include continued teamwork and mentorship within a practice, as well as the exchange of perspectives, practice techniques and ideas among surgeons from different training backgrounds.”
all three tenets of medical therapy by the end of follow-up—and abstinence from smoking was the aspect [...] that was least commonly achieved.”
The presenter went on to highlight the fact that patients with hypertension and those who were not smoking at the outset of the study demonstrated the highest rates of medical therapy adherence.
According to Bloch, non-smokers achieving generally better adherence rates was able to be attributed to a rapid, initial uptake in adherence, likely due to “the relative ease of adding additional medications to the regimen, as opposed to the relative difficulty of smoking cessation”. In addition, multivariable analysis revealed that smoking at the time of index duplex correlated with lower odds of achieving optimal medical therapy adherence.
“In conclusion, adherence to best medical therapy is suboptimal—less than 40% of patients who were not previously on therapy were able to achieve
Smoking cessation should be a leading priority in the care of these patients.”
Randall Bloch
adherence to best medical therapy by the end of follow-up,” Bloch stated. “And, so—despite rapidly evolving medical therapies for cardiovascular risk reduction—smoking cessation remains a ripe target for interventions aimed at adherence to medical therapy.”
Subsequent to Bloch’s presentation, session moderator Wei Zhou (University of Arizona, Tucson, USA) described this as a “really important study”, and suggested that it may have wider implications in other medical areas beyond carotid disease where medication adherence is also poor.
Further discussion led Kakra Hughes (Howard University, Washington DC, USA) to note reservations regarding Bloch et al’s conclusion, highlighting the fact that the study indicated a “pretty good” adherence rate of roughly 80% when best medical therapy was defined without smoking cessation.
Bloch agreed with Hughes to some degree but asserted that smoking cessation was part of the study’s prespecified regimen and is also recommended by multiple societal guidelines. And, speaking to NeuroNews after VAM 2024, Bloch added: “Given that smoking cessation is such an integral aspect of best medical therapy, my concern is that separating it from the [...] regimen may lead to a false sense of success when it comes to stroke and cardiovascular risk reduction. As such, smoking cessation should be a leading priority in the care of these patients.”

TCAR and endarterectomy both deemed ‘reasonable’ but transfemoral stenting linked to worse outcomes in kidney disease patients
A STUDY EXAMINING outcomes between different carotid revascularisation procedures has concluded that transcarotid artery revascularisation (TCAR) and carotid endarterectomy (CEA) both represent a “reasonable choice” in severe chronic kidney disease (CKD) and haemodialysis patients— but transfemoral carotid artery stenting (TF-CAS) appears more likely to result in worse outcomes.
“And, additionally, the majority of these patients are surviving long enough to benefit from the stroke risk
reduction provided by [intervention],” said Elisa Caron (Beth Israel Deaconess Medical Center, Boston, USA). During a plenary session at the 2024 Vascular Annual Meeting (VAM; 19–22 June, Chicago, USA), Caron reported an analysis of Vascular Quality Initiative (VQI) patients with estimated glomerular filtration rate (eGFR) <30ml/min/1.73m2, or on haemodialysis, undergoing TCAR, CEA or TF-CAS between 2016 and 2023.
Presenting on behalf of her coauthors, including senior author Marc
data represent lowest event rates in published trials of CAS, TCAR and CEA
New data from the C-GUARDIANS pivotal investigational device exemption (IDE) trial support consideration of carotid artery stenting (CAS) with the CGuard embolic prevention system (EPS; InspireMD) as a “frontline therapeutic option for appropriate patients being considered for carotid revascularisation”. This is according to lead investigator Chris Metzger (OhioHealth, Columbus, USA), who presented one-year results from the trial at the 2024 Leipzig Interventional Course (LINC; 28–31 May, Leipzig, Germany).
L Schermerhorn—also of Beth Israel Deaconess Medical Center—Caron relayed data from 13,042 VQI patients with eGFR <30ml/min/1.73m2, 2,355 of whom were on haemodialysis.
The majority of outcomes—across both symptomatic and asymptomatic patients—were found to be “fairly similar” between TCAR and CEA, including stroke/death, with both procedures falling within Society for Vascular Surgery (SVS) guidelines regarding perioperative stroke and death. However, CEA was linked with a trend towards slightly higher odds of stroke/death/myocardial infarction (MI), as per the analysis’ primary outcome, in addition to higher odds of MI when considered independently. Similar trends continued when the researchers looked specifically at the subgroup of haemodialysis-only patients, according to Caron.
Turning to findings on overall long-term survival, the presenter relayed that TCAR and CEA were once again similar, as survival rates were nearly 80% with both procedures across all asymptomatic patients and only dropped slightly to around 70% in the haemodialysis-only group at five years. She also noted that these trends endured among symptomatic patients, with rates dropping to around 70% across the full eGFR <30ml/ min/1.73m2 and haemodialysis cohort.
In addition, regarding those who underwent TF-CAS, Caron reported that—prior to statistical weighting— these patients were more likely to be symptomatic, to present with stroke, and to undergo intervention in urgent/ emergent settings, compared to TCAR and CEA patients. They also had more baseline comorbidities. But, “even after weighting for symptom status and comorbidities, TF-CAS still underperformed and did not meet SVS guidelines” she continued, with
IN HIS PRESENTATION, METZGER
detailed that this was a prospective, multicentre, international, single-arm clinical trial comparing the primary endpoint—a composite of incidence of major adverse events including all-cause death, any stroke or myocardial infarction (DSMI) through 30 days post-index procedure, or ipsilateral stroke from day 31 to day 365 post-procedure—to a performance goal derived from existing literature.
The objective was to evaluate the safety and efficacy of the CGuard device for the treatment of carotid artery stenosis in symptomatic and asymptomatic patients at high risk for carotid endarterectomy (CEA) undergoing CAS. From July 2021 to June 2023, 316 patients were prospectively enrolled in the study at 24 sites across the USA and Europe.
Metzger revealed at LINC 2024 that stenting with the CGuard device in patients with carotid artery stenosis and at high risk for CEA led to
stroke, death and overall long-term survival being among the areas where TF-CAS produced inferior outcomes versus TCAR and CEA, across both asymptomatic and symptomatic patients.
Following Caron’s presentation, session moderator Chelsea Dorsey (UChicago Medicine, Chicago, USA) commented that “these patients are incredibly fragile” and, as such, “the more granular information we have about how to approach them, the better”. Dorsey went on to ask the presenter how she feels these new data may impact people’s clinical practices moving forward.
“I think that patient selection will always play a big role,” Caron responded. “The VQI certainly gives us very granular data but, at the end of the day, it’s not the same as the patient sitting in front of you, and I think that will still have a big impact. That said, I think it’s at least reasonable to consider [intervention] in these patients—I know some people are hesitant to do so, so this at least provides evidence to support the decision of whether to intervene. But, again, patient selection is still going to be crucial.”
The majority of these patients are surviving long enough to benefit from the stroke risk reduction provided by [intervention].”
Elisa Caron
an event rate—as per the C-GUARDIANS primary endpoint—of 1.95%, from procedure through oneyear follow-up.
In addition, he commented that data from this trial are consistent with previously published European findings.
1.95% One-year event rate=
“We are very excited that the one-year, carefully adjudicated C-GUARDIANS data confirm the extremely low rates of stoke, death, myocardial infarction, and target-vessel revascularisation, in this prospective trial of high-CEA-risk patients with obstructive carotid disease, including 25% who were symptomatic,” Metzger stated in an InspireMD press release announcing the results. “These data confirm the potential ‘neuroprotective properties’ of this unique MicroNet technology, offering an outstanding frontline option to consider for each patient with obstructive carotid artery disease.”



A UK clinical trial evaluating deep brain stimulation (DBS) in children with epilepsy recently got underway—and a teenager who was the patient to take part in the study has seen his daytime seizures reduced by 80%.
In October 2023, 12-year-old Oran, who had been having severe epileptic seizures for eight years and often needed resuscitation, was the first child in the country to have a DBS device implanted at Great Ormond Street Hospital (GOSH; London, UK).
Eight months later, his seizures had dramatically reduced in frequency and severity as a result of the DBS treatment he received.
The CADET pilot study is said to be the first UK-based clinical trial measuring this type of neuromodulation therapy in children with epilepsy. The study is now set to recruit three additional patients before 22 patients take part in the full trial. It has been funded by the UK Royal Academy of Engineering, GOSH Charity and LifeArc, and sponsored by University College London (UCL; London, UK), with other notable collaborators including King’s College London (London, UK), the University of Oxford (Oxford, UK) and UK-based company Amber Therapeutics.
“Every single day, we see the life-threatening and
life-limiting impacts of uncontrollable epilepsy. It can make school, hobbies or even just watching a favourite TV show utterly impossible,” said Martin Tisdall (GOSH/UCL, London, UK).
“For Oran and his family, epilepsy completely changed their lives and, so, to see him riding a horse and getting his independence back is absolutely astounding. We couldn’t be happier to be part of their journey. Deep brain stimulation brings us closer than ever before to stopping epileptic seizures for patients who have very limited effective treatment options. We are excited to build the evidence base to demonstrate the ability of deep brain stimulation to treat paediatric epilepsy and hope in years to come it will be a standard treatment we can offer.”
Among the purported benefits of the specific DBS technology being used in this trial are the fact that— unlike other devices, which are mounted on the chest— it is mounted on the patient’s skull, meaning the leads are less likely to break or erode as the child grows. The present device is also rechargeable via wearable
Boston Scientific has announced the presentation of positive five-year pooled results for the Intracept intraosseous nerve ablation system, measuring outcomes across three clinical trials in the treatment of vertebrogenic low back pain. The data were presented at the 2024 American Society of Pain and Neuroscience (ASPN) conference (11–14 July, Miami, USA).
A BOSTON PRESS RELEASE
details that more than 30,000 patients have now been treated with the Intracept system, which utilises the only US Food and Drug Administration (FDA)-cleared device for the treatment of vertebrogenic low back pain. Five-year outcomes with the Intracept system from three long-term follow-up studies utilised the patient-reported Oswestry Disability Index (ODI) and visual analogue scale (VAS), comparing these scores to baseline across 249 patients.
The study produced clinically and statistically significant improvements in pain (measured by VAS on a 0–10 scale) and function (measured by ODI on a 0–100 scale) from baseline to five years. In addition, 83% of patients reported a ≥2-point reduction in VAS from baseline (p<0.0001) and 78% of patients had a ≥15-point reduction in ODI from baseline (p<0.0001). Nearly 66% of patients had a 50% or more reduction in pain relief (p<0.0001), while nearly onethird of patients reported being 100% pain free after five years (p<0.0001).
In total, ASPN 2024 saw 15 abstracts and posters presented that featured Boston’s clinical data.
An additional data highlight came from a US multicentre, observational, real-world study of patients being treated with Fast-Acting Sub-perception Therapy (FAST) via the company’s WaveWriter Alpha spinal cord stimulation (SCS) system. In the study, patients who preferred the use of FAST therapy achieved durable and robust pain relief out to 12 months of followup (n=89), while outcomes among 289 patients assessed at mean final followup included a 5.5-point reduction in numeric rating scale (NRS) pain score, from 7.8 to 2.3 (p<0.0001), as well as 91% of patients reporting a ≥50% reduction in pain and 61% of patients reporting an NRS pain score of ≤2.

headphones, meaning it can be used while watching a video or interacting with a tablet, and does not require surgery to replace it every three-to-five years.
“Our mission is to design pioneering research systems for exploring the treatment of intractable health conditions, such as paediatric epilepsy,” said Tim Denison (University of Oxford, Oxford, UK).
“Oran is the first child in the world to receive this device and we are extremely pleased that it has had such a positive benefit for him and his family.”
The device in question targets the thalamus, which is a hub for electrical signals in the brain. It is hoped that the device will block electrical pathways and consequently stop seizures from spreading. The device also has settings for optimisation towards seizure patterns, which—although not utilised in this trial— could be used in the future for patients with LennoxGastaut syndrome (LGS).
Deep brain stimulation brings us closer than ever before to stopping epileptic seizures for patients who have very limited effective treatment options.”
Martin Tisdall
Saluda Medical has announced the recent presentation of two abstracts analysing biomarker-based spinal cord stimulation (SCS) data at the 2024 American Society of Pain and Neuroscience (ASPN) annual conference (11–14 July, Miami, USA).
THE ABSTRACTS—WHICH WERE among 10 total abstracts featuring Saluda’s clinical data at ASPN 2024— centred on evidence from patients treated with the Evoke system in clinical studies. According to a company press release, key takeaways from these two abstracts demonstrate the significance of objective neurophysiological measurements in SCS with evoked compound action potential (ECAP) dose-controlled closed-loop therapy.
The first of these abstracts, titled “Maximal analgesic effect attained by the use of objective neurophysiological measurements with ECAP dosecontrolled closed-loop SCS” and presented by Robert Levy (Marcus Neuroscience Institute, Boca Raton, USA), was based on a paper recently accepted for publication that ultimately received the “Top Abstract” award at ASPN 2024.
It sought to characterise the biomarker-based dose-response relationship that produced a patient’s maximal analgesic effect. The analysis showed a statistically significant relationship between usage over ECAP threshold, ECAP dose and pain relief across the patient population. In addition, the analysis demonstrated
that the clinical benefit observed in the trial period was reproduced following permanent implantation when the neurophysiological metrics remained consistent.
The second abstract highlighted in Saluda’s recent press release, titled “Identifying SCS trial responders immediately after postoperative programming with ECAP dosecontrolled closed-loop therapy”, was presented by Jason Pope (Evolve Restorative Center, Santa Rosa, USA) and based on a recently published paper. Its purpose was to analyse the benefits of closed-loop, dose-controlled SCS as it relates to trial outcomes, and the predictability of long-term success. The analysis compared neurophysiological and certain patient-reported metrics between the day of the trial procedure, or day zero, and the end of the trial. Success criteria included confirmation of neural activation and dose-controlled closed-loop therapy, patient reported pain relief and functional improvement. The analysis measured patients who passed all success criteria on day zero and demonstrated that these success criteria had a 98% positive predictive value for being responsive to therapy at the end of the trial period.
Microvention announces publication of one-year results from CLEVER study
Microvention, a wholly owned subsidiary of Terumo Corporation, has announced the recent publication in the Journal of NeuroInterventional Surgery (JNIS) of one-year results from CLEVER—a study that sought to provide a clinical evaluation with the Woven EndoBridge (WEB) 17 device in treating ruptured and unruptured aneurysms.
The CLEVER study was a multicentre, prospective study assessing the WEB 17 system in ruptured and unruptured aneurysms to understand the safety and effectiveness of the newest and smallest WEB system.
The study comprised of 163 patients across 17 European centres, with results concluding that WEB 17 is just as safe and effective as previous WEB generations with a low complication rate, and no rebleeds at 30 days and one year. The adequate occlusion rate was 86.5% for ruptured aneurysms (73.1% complete occlusion) and 82.4% for unruptured aneurysms (57.1% complete occlusion) at one-year follow-up.
The results of CLEVER demonstrate that the WEB 17 system maintains the same efficacy as previous generations of WEB, a company press release reiterates.
“One-year angiographic results of CLEVER show excellent complete occlusion rates at one year in the population of wide-neck bifurcation aneurysms treated with WEB 17,” said Laurent Spelle (Bicêtre Hospital, Le Kremlin-Bicêtre, France), a leading author for the recent publication of CLEVER in JNIS
“WEB has changed my practice and set a new standard for safety in the treatment of cerebral aneurysms,” added Adam Arthur (University of Tennessee Health Science Center, Memphis, USA), principal investigator for the WEB-IT Trial—which was the investigational device exemption (IDE) study supporting WEB’s post-market approval (PMA) in the USA.
Microvention is also currently celebrating the five-year anniversary of WEB in the USA, having featured this product and its entire line of medical device products at the recent Society of NeuroInterventional Surgery (SNIS) annual meeting (22–26 July, Colorado Springs, USA).
Ceretrieve announces successful results in FIH study of stroke aspiration catheter Ceretrieve has announced the successful results of the company’s multicentre, single-arm study, showcasing the capabilities of its “state-of-the-art” aspiration catheter in stroke treatment.
The study—conducted across two centres—included 20 patients
suffering from acute ischaemic stroke due to intracranial large vessel occlusion (LVO) who were eligible for thrombectomy within 24 hours of symptom onset. The aim of the study was to assess the safety and initial performance of the Ceretrieve device.
“The ‘first-pass effect’ has been shown to improve patient outcomes,” said Shady Jahshan (Galilee Medical Center, Nahariya, Israel), who performed the first neurothrombectomy procedure with the Ceretrieve device.
“Our experience in FIH [first-inhuman] trials demonstrated that the Ceretrieve device quickly enables complete clot ingestion in first pass— even for the most challenging clots and anatomies. This has the potential to dramatically improve patient clinical outcomes.”
Ceretrieve says that, as shown in the present FIH study, its aspiration catheter not only excelled in performance but also ensured the highest safety standards by reducing the risk of releasing clot fragments further into the brain. In the study, an 80% rate of complete/near-complete perfusion was achieved.

The study included two generations of the device, and the results with the improved, second-generation device are “highly impressive”: a 100% rate of complete/near-complete perfusion was achieved in all treated patients, in addition to an 83% rate of first-pass complete perfusion (modified thrombolysis in cerebral infarction [mTICI] 3) that far exceeds the 30–40% rate of current goldstandard devices.
“The term ‘everything comes with a price’ is not valid for the Ceretrieve device,” said Serdar Geyik (Florya Medical Park, Istanbul, Turkey).
“Ceretrieve’s device aspirates the clot with a giant bore tip—double the largest catheters in the market—for maximal vacuum effect without paying the price in trackability. In addition, it provides local flow restriction in the middle cerebral artery, reducing distal emboli. It is the only device that includes all the features for successful thrombectomy and first-pass effect in one single device.”
Anaconda Biomed receives IDE approval to initiate enrolment in ATHENA study
Anaconda Biomed has announced that it has received conditional investigational device exemption
(IDE) approval from the US Food and Drug Administration (FDA) to begin the ATHENA study of its Ana funnel catheter. This prospective, randomised, dual-arm, multicentre study will assess the safety and effectiveness of mechanical thrombectomy using the catheter device in combination with a stent retriever.
“The neurointerventional community is eager to assess this innovative technology, which is designed to enhance the efficiency of mechanical thrombectomy,” said Adnan Siddiqui (Jacobs Institute/University at Buffalo, Buffalo, USA), coordinating investigator of the ATHENA study.
“Even a small difference in the revascularisation success after one pass can have a profound impact on the clinical outcomes of people with ischaemic stroke.”
Studies have shown that flow arrest during mechanical thrombectomy can improve revascularisation rates and clinical outcomes at three months, according to a recent Anaconda press release. However, the release continues, the approach has been underutilised to date due to the limitations of current devices. Anaconda’s Ana funnel catheter is uniquely designed to facilitate flow arrest during clot retrieval.
Upon institutional review board (IRB) approval, the ATHENA study of the Ana funnel catheter will be conducted at up to 40 US and international centres enrolling patients experiencing acute ischaemic stroke and treated within 24 hours of symptom onset.
The study will report acute reperfusion success after a single thrombectomy pass with three of the most commonly used stent retrievers, and on procedural safety between study arms.
Rapid Medical completes initial neurovascular cases with recently US FDA-cleared Drivewire 24
Rapid Medical has announced the first procedures in the USA with the breakthrough deflectable access platform Drivewire 24, doing so at the 2024 Society of NeuroInterventional Surgery (SNIS) annual meeting (22–26 July, Colorado Springs, USA). This milestone follows the US Food and Drug Administration (FDA) clearance of the device.
Rapid claims that, with active technology, Drivewire articulates a wide range of catheters for direct access to endovascular locations.
“Drivewire addresses a major unmet need in the endovascular space,” said Shahram Majidi (Mount Sinai Health System, New York, USA). “It transforms access across a range of procedures, from aneurysms to strokes and more. We’re always looking for devices to make procedures faster, safer [and] less expensive. My first experience with Drivewire suggests it could do all of these.”
In two cases completed by Majidi,
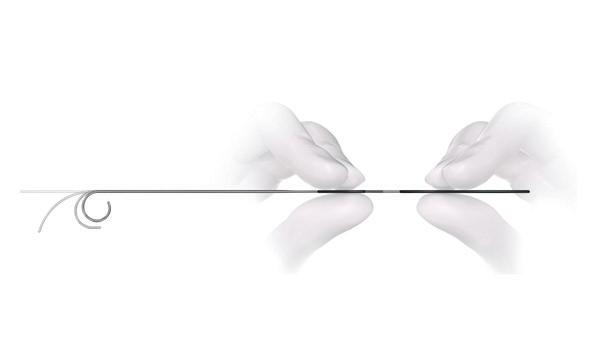
Drivewire 24
Drivewire 24 navigated an aspiration catheter directly to an M2 arterial occlusion for excellent reperfusion at the first pass. In the second case, Drivewire navigated complex turns to place two flow diverters in a large, multilobed intracranial aneurysm.
Drivewire provides highperformance intravascular steering, according to a recent press release from Rapid, as physicians control the direction and shape of the guidewire tip in real time—eliminating the need to remove the wire to reshape it.
The device also features variable support to articulate a wide range of micro and intermediate catheters without advanced forerun, or additional support devices. This results in precise navigation via the most direct route through the neuro and peripheral vasculatures, the release adds.
Evasc announces first case with latest Eclips device alongside European approval Evasc Neurovascular has announced the successful use of the Eclips Short Landing Zone device in treating all anterior communicating artery (ACOM) and middle cerebral artery (MCA) bifurcation aneurysms.
The first successful case using this pioneering device was performed by Jonas Jensen at Aarhus University Hospital in Aarhus, Denmark.
Alongside this clinical milestone, Evasc has also announced that the Eclips Short Landing Zone device has received CE-mark/Medical Device Regulation (MDR) approval. A company press release notes that this approval underscores the device’s safety and efficacy for use across the European Union.
Jensen performed the “groundbreaking” first procedure with Eclips, achieving “excellent results” and setting “a new standard” in the treatment of complex intracranial aneurysms, the release continues.
The Eclips Short Landing Zone device—designed for stable aligning and orientation of the spine—offers a “paramount solution” for addressing bifurcation aneurysms in both ACOM and MCA regions. Its innovative design allows for enhanced navigation and deployment, thus ensuring optimal outcomes for patients, as per the release.
Evasc representative Wieger Kaptein commented that, with this new technology, the company now has an Eclips device “for every bifurcation aneurysm”, including those at the basilar tip (BT), carotid terminus (CT), ACOM and MCA.
NeuroOne completes first-inhuman ablations with OneRF system
NeuroOne Medical Technologies Corporation has announced that the OneRF ablation system was recently used at a prestigious hospital located in Jacksonville, USA to successfully complete five ablations in one patient. According to a company press release, the patient was suffering from multifocal epilepsy—a condition whereby seizures are triggered from multiple areas of the brain.
In this procedure, 10 Evo stereoelectroencephalography (sEEG) electrodes were placed in various locations of the patient’s brain. Four electrodes identified problematic areas of the brain that were triggering seizures. Ablations were performed at the targeted areas using the temperature control safety feature, and two of these ablations occurred at different contacts on one electrode. Using the same electrodes, the successful ablations were confirmed by post-ablation sEEG recordings demonstrating lack of brain activity at the point of tissue ablation. The procedure was performed at the patient’s bedside, saving both the time and cost of having to conduct the procedure in an operating room.
The OneRF ablation system is NeuroOne’s first device with a therapeutic indication and its third US Food and Drug Administration (FDA) 510(k)-cleared device. The company announced a limited commercial launch of the device in March 2024 and was granted an International Classification of Diseases (ICD)-10 procedure code by the US Centers for Medicare and Medicaid Services (CMS) in June.
Brainomix presents US data validating AI technology in stroke Brainomix has announced new data from studies presented at the Society of NeuroInterventional Surgery (SNIS) annual meeting (22–26 July, Colorado Springs, USA), relating to research conducted in collaboration with the Mayo Clinic (Rochester, USA), West Virginia University (Morgantown, USA), and Boston Medical Center (Boston, USA).
According to a Brainomix press release, the research highlighted the latest artificial intelligence (AI)enabled technology that the company has developed within its pipeline for the US Food and Drug Administration (FDA)-cleared Brainomix 360 Stroke platform, representing “groundbreaking capabilities” that will allow physicians to extract maximal value from universally available non-contrast computed tomography (NCCT) scans across stroke networks.
Key studies that were presented at SNIS 2024 and are highlighted in Brainomix’s recent release included a research collaboration in which baseline NCCT scans from patients
with large vessel occlusion (LVO) were analysed using Brainomix 360 e-ASPECTS to identify hyperdense clots and quantify their length. Results showed that clot biomarkers from NCCT are predictors of successful recanalisation and could facilitate the planning of mechanical thrombectomy procedures. Another presentation pertained to a collaboration attempting to validate Triage Stroke as a reliable tool for LVO detection, from which the authors concluded that—when coupled with clinical information like National Institutes of Health stroke scale (NIHSS) scores—the tool may help centres to identify thrombectomy candidates, especially those with constrained resources and basic imaging. A further collaboration saw researchers quantify ischaemic core volume and depth of hypoattenuation using net water uptake (NWU) from baseline CT scans using Brainomix 360 e-ASPECTS, with results showing that NWU extracted automatically from routine imaging may help identify patients at risk of futile recanalisation, especially those with large cores.
pathology. Revolutions in imaging technology—from the discovery of X-rays over 120 years ago to threedimensional imaging in the angiography suite more than 20 years ago—occur roughly once in a generation.”
The procedures, performed by Vitor Mendes Pereira (St Michael’s Hospital, Toronto, Canada) and Pedro Lylyk (Clínica la Sagrada Familia, Buenos Aires, Argentina), demonstrated successful navigation and imaging with the nOCT probe in 32 patients undergoing routine investigation or treatment for cerebrovascular disease.

“The Spryte nOCT technology is an imaging probe, sized like a guidewire, that navigates seamlessly through the brain vessels using our usual neurointerventional techniques,” Pereira explained. “The system and imaging probes performed well, integrating with our workflow, and provided us with incredible images and critical information that we cannot obtain with any other technology.”
In addition to this publication, Spryte recently announced receipt of Breakthrough Device designation from the US Food and Drug Administration (FDA) for its nOCT technology, as well as being included in the FDA’s new Total Product Life Cycle Advisory Program (TAP).
and take minutes off my stroke thrombectomy times, allowing me to get the clot out faster.”
InspireMD congratulates CREST-2 investigators on completion of trial enrolment
InspireMD recently congratulated leading investigators on the completion of enrolment in the CREST-2 clinical trials, which are seeking to evaluate and compare endarterectomy, stenting and medical management in patients with asymptomatic, high-grade carotid stenosis.
The CGuard embolic prevention stent system (EPS), utilising InspireMD’s MicroNet mesh, was included as a device option for stenting in the CREST-2 trials following US Food and Drug Administration (FDA) approval of the company’s investigational device exemption (IDE) supplement application in February 2022. In a press release dated 5 August 2024, InspireMD notes that CREST-2 included 23 cases in which patients were implanted with CGuard.
Marvin Slosman, chief executive officer of InspireMD, offered thanks to Brajesh Lal (University of Maryland School of Medicine, Baltimore, USA) and the other investigators for executing this “landmark trial”— describing it as a “remarkable achievement” in the field of carotid revascularisation and stroke prevention.
“The studies presented […] at SNIS highlight the clinical value of the Brainomix 360 Stroke platform, particularly relating to the e-ASPECTS and Triage Stroke algorithms that assess non-contrast CT scans, which are universally available to all stroke centres across the USA,” said Ansaar Rai (West Virginia University, Morgantown, USA). “The results indicate that these algorithms generate clinically relevant results for frontline stroke physicians that could help them to better manage stroke patients eligible for mechanical thrombectomy across all centres within a network.”
Spryte publishes clinical study on novel intravascular brain imaging
Spryte Medical has announced the publication of a first-in-human study of its neuro optical coherence tomography (nOCT) technology in the peer-reviewed journal Science Translational Medicine. The study— hailed as a “significant milestone” by researchers—is the first to demonstrate the ability to bring intravascular imaging to the brain, helping clinicians to better see the pathology associated with neurovascular disease, as per a Spryte press release.
“This is an incredibly exciting milestone for the field of neurointervention,” said Matthew Gounis (UMass Chan Medical School, Worcester, USA). “Direct imaging of the pathology and its relationship to devices will transform treatment decisions, and the fundamental understanding of cerebrovascular
Imperative announces initial cases with “first” stroke-specific insert catheters
Imperative Care has announced the successful completion of the first case with its Zoom 6Fr insert catheters, which was performed by Dana Tomalty at Huntsville Hospital in Huntsville, USA. The company claims that these catheters, which recently gained US Food and Drug Administration (FDA) 510(k) clearance, are the first insert catheters developed specifically for ischaemic stroke procedures.
In the first case performed by Tomalty, the Zoom SIM insert catheter was used to quickly select the target vessel and provide 0.088-inch intracranial access from the femoral artery with Zoom 88 in a patient with a challenging anatomy and distal left M2 occlusion. The Zoom SIM provided added stability to navigate Zoom 88 far into the brain and access the clot more quickly. Tomalty then used both Zoom 71 and Zoom 35 to aspirate and remove the clot in only 10 minutes from puncture to reperfusion, resulting in a complete thrombolysis in cerebral infarction (TICI) 3 revascularisation.
“In my experience, navigating the aortic arch can pose a significant challenge in patients with more tortuous anatomy,” Tomalty said. “Due to the unique design and capabilities of the Zoom 6Fr insert catheters, I believe the use of these technologies will help mitigate this challenge
“There continue to be significant advancements in the field of carotid revascularisation and stroke prevention, and information from this study will help determine the optimal treatment for carotid stenosis patients without stroke symptoms,” commented Lal, who is a CREST-2 co-principal investigator. “This trial, when complete, will ensure that we remain current with state-of-the-art innovation to achieve the best possible short- and long-term patient outcomes. Along with my fellow investigators, we eagerly await topline results from this important study.”

Across two independent, multicentre randomised controlled trials, CREST-2 will ultimately attempt to establish which of the three key methods of stroke prevention in asymptomatic patients with high-grade carotid disease—carotid endarterectomy (CEA), carotid artery stenting (CAS) and intensive medical management— offers the safest and most effective solution. In July, the studies surpassed their prespecified enrolment goal of 2,480 participants, with patients having been enrolled at 142 centres across the USA, Canada, Spain and Israel.
Route 92 Medical announces commercial launch of FreeClimb 88 catheter system
Route 92 Medical has announced the commercial launch of the FreeClimb 88 catheter system comprising the FreeClimb 88 catheter and the Tenzing 8 delivery catheter—all designed to work with the Base Camp sheath.
The US Food and Drug Administration (FDA) 510(k)cleared FreeClimb 88 catheter system offers reliable navigation through tortuous anatomy in the neurovasculature, and is available in 125cm and 132cm lengths to provide clinicians with the flexibility they need to reach their targeted locations, as stated in a Route 92 press release.
“Having a broader set of tools gives clinicians greater flexibility when treating difficult cases,” said Ajit Puri (University of Massachusetts Medical Center, Boston, USA). “The 0.088-inch catheter systems will make procedures easier by minimising setup complexity, providing vessel size matching leading to distal flow control during the delivery of therapeutic devices, and leveraging the strengths of the Tenzing product design to improve navigation.”
The tapered tip of the patented Tenzing 8 delivery catheter significantly reduces ‘ledge effect’ and allows the FreeClimb 88 catheter to consistently navigate past the ophthalmic artery and predictably reach the M1 segment of the middle cerebral artery (MCA), Route 92 claims. Tenzing’s soft, tapered tip provides atraumatic tracking in the neurovasculature, and was designed to reach the targeted locations without the use of a microcatheter, the recent release adds.
Route 92’s family of FreeClimb and HiPoint products simplify endovascular thrombectomy procedures by allowing clinicians to select the optimal length and size of access or aspiration catheter for every case, according to the company. Its FreeClimb and HiPoint products are powered by custom-sized Tenzing delivery catheters, allowing for rapid and predictable delivery to the targeted location.
The FreeClimb 88 system joins the company’s growing 88 portfolio, including the Monopoint system, powered by the HiPoint 88 and Tenzing 8 catheters, and Base Camp sheath.
Vesalio introduces NeVa NET 4mm for LVO acute ischaemic stroke
Vesalio has launched a NeVa NET 4mm device to treat acute ischaemic stroke due to large vessel occlusion (LVO), a press release reports.
The company states that this introduction builds on the success of NeVa NET 5.5mm in international markets, and follows promising findings from studies published in the Journal of Vascular and
Interventional Neurology and the Journal of NeuroInterventional Surgery
Vesalio notes that both the 5.5mm and the newly launched 4mm sizes incorporate NeVa NET’s integrated micro-filter—a patented feature aimed at preventing the escape of clot particles into new or distal territories. Patented distal net filtration complements the NeVa device’s allclots capability, the company adds.
“We are excited to be among the first centres using NeVa NET,” said Paul Bhogal (NHS Royal London, London, UK). “Our team has been eagerly anticipating the release of the 4mm size. Our experience with NeVa has been excellent and, in our cases, we are seeing very high first-pass effect (eTICI [expanded thrombolysis in cerebral infarction] ≥2c). The new NeVa NET holds much promise and the fact the 4mm version can be used with 0.021inch microcatheters is wonderful.
“I believe that this new device will, in conjunction with other technologies such as large-bore aspiration catheters and BGCs [balloon guide catheters], offer the best chances of complete recanalisation on first pass and better reperfusion for the brain. My initial experience has indeed been very good, and this is effectively my go-to device for M1 and ICA [internal carotid artery] occlusions.”
Vesalio advises that NeVa and NeVa NET are CE-marked but not cleared in the USA.
Medtronic unveils nextgeneration Artisse intrasaccular device alongside new data Medtronic has announced the European launch of Artisse—a new intrasaccular device designed to treat intracranial aneurysms by conforming to the shape of the aneurysm. The launch coincides with interim data examining the safety, efficacy and performance of the device being presented for the first time at LINNC Paris 2024 (3–5 June, Paris, France).
Artisse was designed to address the needs of complex wide-neck bifurcation aneurysms that have traditionally been managed by stentassisted coiling, coil adjunctive neckbridging devices and other intrasaccular basket devices. The former two methods require multiple steps and multiple devices, with stent-assisted coiling requiring dual antiplatelet therapy, which can present challenges in ruptured aneurysms, according to a Medtronic press release.
The company claims that—owing to its combination of conformability and optimum outward radial force—Artisse offers a simple, one-step technique in treating complex and simpler aneurysms alike. Alongside the device, Medtronic is also offering expert clinical support, including access to simulation software intended to further
support sizing selection.
“Artisse behaves differently to other intrasaccular devices because I can control the optimal positioning of the device in the aneurysm,” said Riitta Rautio (Turku University Hospital, Turku, Finland). “Due to its conformability and softness, I can reach the optimal position of Artisse in the aneurysm with partial re-sheathing of the device and slight movement of the microcatheter.”
Early-experience analysis presented at LINNC Paris 2024, from a study involving 35 patients enrolled into the multicentre, core lab-adjudicated European INSPIRE-A registry, has shown that 80% of patients treated with Artisse achieved complete occlusion by a six-month angiographic assessment, indicating successful aneurysm occlusion with no residual filling.
“Artisse is a promising device that appears to be a step in the right direction for intrasaccular technology,” said Tufail Patankar (Leeds General Infirmary, Leeds, UK). “Its softness and conformability allows you to manipulate the device within the aneurysm. Complex wide-neck angled aneurysms that were previously difficult to treat with other intrasaccular devices now seem to be treatable with Artisse.”
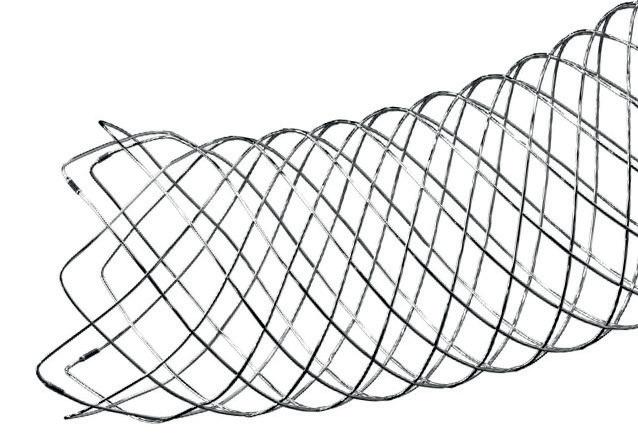
Microvention announces US availability of LVIS EVO intraluminal support device Microvention, a wholly owned subsidiary of Terumo Corporation, has announced that the LVIS EVO intraluminal support device is now commercially available for the treatment of wide-neck intracranial aneurysms in the USA.
“I’ve really enjoyed getting to use and know EVO,” said Charles Matouk (Yale University, New Haven, USA). “With improved visibility and the ability to shelf the stent across the aneurysm neck, it’s become my tool of choice for stent-assisted coiling.”
A company press release describes LVIS EVO as the “next evolution” in stent innovation, and notes that the device has been available in Europe since 2019 with more than 12,000 units having been sold.
LVIS EVO is the first fully visible coil-assist intracranial stent available in the US market, delivering enhanced visualisation, optimised opening and precise placement with drawn filled tube (DFT) wire construction, and advanced braid design, the release adds.
With enhanced visualisation, the device provides wall apposition
confirmation, as the entire body of the stent is fully visible under fluoroscopy. Its optimised braid angle allows for improved device opening along the entire length of the device. And, with precise placement, LVIS EVO offers controlled delivery and development, as well as the ability to resheath it up to 80% of the device length.
According to Microvention, the entire LVIS EVO portfolio is compatible with the company’s Headway 17 advanced microcatheter, and Scepter C and Scepter XC occlusion balloons.
Penumbra launches BMX81 and BMX96 neuro access offerings in Europe
Penumbra has announced the CE mark and European launch of BMX81 and BMX96—devices designed for the neurovascular management of ischaemic and haemorrhagic stroke. A company press release also notes that these technologies constitute Penumbra’s most advanced neuro access offerings.
This announcement further expands the company’s neuro portfolio in Europe following the launch of three new RED reperfusion catheters—RED 43, RED 72 with SENDit technology, and RED 78—back in May 2024.
“I need to be able to trust that my access catheters can provide the stability that I need. The new BMX catheters promise excellent support. With their expanded inner diameters, I will be able to increase therapeutic options for my patients, especially when going radial,” said Markus Holtmannspötter (Klinikum Nürnberg, Nürnberg, Germany).
Unlike traditional access catheters, Penumbra’s BMX81 and BMX96 are made using laser-cut stainless steel hypotube technology, offering stability and trackability, the company’s recent release notes, adding that they are designed to allow physicians to easily navigate the brain’s complex anatomy via either a femoral or radial access approach. The stainless steel hypotube also allows for a larger inner diameter while maintaining a lower outer diameter without compromising support, expanding intraprocedural options in both ischaemic and haemorrhagic stroke.

Penumbra claims that, centred on 20 years of experience optimising science-based aspiration thrombectomy (S-BAT), its catheters are engineered with the latest technology in trackability and aspiration. BMX81 and BMX96
Q’Apel Medical appoints Jodie Fam as new CEO
Q’Apel Medical has announced the appointment of Jodie Fam as its new chief executive officer (CEO). Fam succeeds R King Nelson, who retires after leading the company for the past five years and will continue to serve on Q’Apel’s board of directors.
With more than two decades in the medical device sector, Fam has held executive leadership positions at multiple medical device firms, including public and several venturebacked startups, “building a solid track record of experience in execution and commercial expansion” during her industry tenure, as noted in a Q’Apel press release.
Most recently, Fam served as

4–6 September
16th Congress of the European Society of Minimally Invasive Neurological Therapy (ESMINT) Marseille, France esmint.eu/esmint-congress
18–22 September
European Society of Neuroradiology (ESNR) Annual Meeting Paris, France esnr.org/en/scientific/annual-meetings/18-092024-47th-esnr-annual-meeting
Q’Apel’s chief marketing officer and general manager for the company’s international business. Prior to joining Q’Apel, she served as the CEO of AblaCare (now May Health), and held senior management positions at Route 92 Medical, Medina Medical (acquired by Medtronic), CardioKinetix and Concentric Medical (acquired by Stryker).
“The attractive thing about the neurovascular space is that it continues to evolve—even in short periods of time,” Fam told NeuroNews. “We’ve seen it in stroke in a matter of five or less years, and I think it will continue. There are new procedures, techniques and devices that are being developed and tested by many companies today. I think we’ll see a host of new procedures available for our physicians to treat more patients with new disease states, and that’s incredibly exciting.”
Following her appointment, Fam spoke to NeuroNews at the recent Society of NeuroInterventional Surgery (SNIS) annual meeting (22–26 July, Colorado Springs, USA) to discuss the current landscape of the neurovascular industry. This video interview can be seen online at neuronewsinternational.com.
Boston Scientific announces agreement to acquire Silk Road Medical
Boston Scientific has announced that it has entered into a definitive agreement to acquire Silk Road Medical, a medical device company involved in producing products to be deployed during transcarotid artery revascularisation (TCAR).
The purchase price is US$27.50 per share, reflecting an enterprise value of approximately US$1.16 billion, a Boston press release details.
“The TCAR platform developed by Silk Road Medical is a notable advancement in the field of vascular medicine, which has revolutionised stroke prevention and the treatment of carotid artery disease,” said Cat Jennings, president of vascular and peripheral interventions at Boston.
“We believe the addition of this clinically differentiated technology to our vascular portfolio demonstrates our continued commitment to provide meaningful innovation for physicians who care for patients with peripheral vascular disease.”
The TCAR system gained US Food and Drug Administration (FDA) approval in 2015 and is supported by several clinical studies demonstrating a reduced risk of stroke and other complications associated with open surgery, the release adds.
Siemens-WSO partnership to tackle stroke’s “disastrous disease trajectory”
Siemens Healthineers and the World Stroke Organization (WSO) have announced a two-year partnership to develop the acute stroke workforce, and improve treatment and care for stroke.
“Stroke treatments exist that we know deliver better outcomes for patients, and we have evidence that these can be delivered cost-effectively in low-, middle- and high-income countries,” said WSO president Sheila Martins (Federal University of Rio Grande do Sul, Porto Alegre, Brazil).
“Supporting healthcare providers and clinicians to deliver the best possible standard of care is at the core of the WSO mission, and we need all parts of the care system to pull together to alter this disastrous disease trajectory.”
The Siemens-WSO partnership will have a new global scope, building on a successful programme of handson workshops to deliver education and training programmes aimed at strengthening clinical capacity and driving access to mechanical thrombectomy. WSO programmes will attempt to address this system change through stroke centre certification, clinical education, and public awareness campaigns, while Siemens attempts to provide holistic solutions along the entire stroke care pathway.
28 September–2 October Congress of Neurological Surgeons (CNS) Annual Meeting Houston, USA cns.org/2024
3–4 October
British Society of Neuroradiologists (BSNR) Annual Scientific Meeting Bristol, UK bsnr.org.uk/annual-meeting
6–10 October 17th Congress of World Federation of Interventional and Therapeutic Neuroradiology (WFITN) New York, USA wfitn2024.org/en
13–17 October
The European Association of Neurosurgical Societies (EANS) Congress Sofia, Bulgaria eans.org/page/EANS_Congress
23–26 October 16th World Stroke Congress (WSC) Abu Dhabi, UAE wsc2024.kenes.com
20–24 November Society of Vascular and Interventional Neurology (SVIN) Annual Meeting San Diego, USA svin.org/i4a/pages/index.cfm?pageid=3645









a. Tests performed and data on file at Penumbra, Inc. Testing performed evaluated 2 variables: 1. Device unpackaging and preparation time and 2. Aspiration catheter tracking time. Bench results may not be indicative of clinical performance. Physicians’ treatment and technique decisions will vary based on their medical judgment. Individual results may vary depending on patient-specific attributes and other factors. The aspiration system includes the respective manufacturer’s commercially available guide catheter, delivery or intermediate catheter, and large-bore aspiration catheter. Systems tested include the Stryker ® AXS Vecta ® Aspiration System, Imperative Care™ Zoom™ Aspiration System, and the Penumbra RED 72 with SENDit Aspiration System.
Photograph taken by and on file at Penumbra, Inc. Caution: Federal (USA) law restricts these devices to sale by or on the order of a physician. Prior to use, please refer to the Instructions for Use (IFU) for complete product indications, contraindications, warnings, precautions, potential adverse events, and detailed instructions for use. For the complete Penumbra IFU Summary Statements, please visit: peninc.info/risk. Please contact your local Penumbra representative for more information. Copyright ©2023 Penumbra, Inc. All rights reserved. The Penumbra P logo, RED, and SENDit are registered trademarks or trademarks of Penumbra, Inc. in the USA and other countries. All other trademarks are the property of their respective owners. 28370, Rev. A 10/23 USA
learn more
(Including Penumbra IFU Summary Statements)

