Global dialysis discussions at VASA 2024 page 03


Global dialysis discussions at VASA 2024 page 03

A bipartisan bill has recently been introduced to the US House of Representatives by representatives Carol Miller, Marilyn Strickland, Earl Blumenauer, and Mariannette Miller-Meeks—with a companion bill expected to be introduced soon in the Senate. The Improving Access to Home Dialysis Act (HR-8075) aims to increase access to care and improve outcomes for patients on dialysis, which has garnered support from the National Kidney Foundation (NKF).
ONE THING THAT THIS COULD DO, the NKF suggests via a press release, is increase access to home dialysis. Whilst the foundation acknowledges that home dialysis is not for everyone, it states that it can provide patients with convenient and flexible alternatives to in-hospital treatment options, which allow them to undergo dialysis in their own homes, without a rigid dialysis schedule set for them.
The NKF adds that this option can be particularly useful to patients in rural or remote areas, by removing the need to travel long distances in order to attend appointments at a dialysis facility. It states that this can “greatly improve the quality of life for patients”, which can lead to patients being more likely to maintain employment and a level of health for long enough to qualify for a kidney transplant.
Despite the benefits of home dialysis, the NKF states that only 14% of patients on dialysis in the USA are using at-home options, despite the availability of evidence that demonstrates that it may be a better option for some patients. The foundation opines that a lack of information is a major barrier, as many patients are not able to educate themselves on the options available to them beyond the traditional in-centre care.
Commenting on the new bill’s introduction to the US House of Representatives, Kevin Longino, chief executive officer (CEO) of the NKF, said: “Patients deserve to know about all options for dialysis so they can make an educated choice for themselves. Too many patients are never told they have options, besides in-centre dialysis, that could improve their quality of life. We are deeply appreciative of representatives Miller, Strickland, Blumenauer, and Mill-
Profile: Debbie BrowerMaier page 10

Long-term cryoablation data for renal carcinoma page 17 International vascular access training page 14

The Vascular Access Controversies Masterclass at this year’s Charing Cross (CX) International Symposium (23–25 April, London, UK) was the setting for a Great Debate titled “EndoAVFs are a failed experiment” which saw four physicians—Tobias Steinke (Schön Klinik Düsseldorf, Düsseldorf, Germany), Robert Shahverdyan (Asklepios Klinik Barmbek, Hamburg, Germany), Shannon Thomas (Prince of Wales Hospital, Sydney, Australia), and Monnie Wasse (Rush University Medical Center, Chicago, USA)—present cases, either for or against the motion. The session highlighted that, not only is there clear division on this controversy amongst the presenters, but also in the wider CX audience. Even after all presentations had been given, when asked via a live poll if they agreed that endovascular arteriovenous fistulas (endoAVFs) are a failed experiment, the audience was split nearly down the middle; 54% disagreed with the motion, with 46% agreeing.
The first to present his argument, which agreed with the motion that they are a failed experiment, Steinke focussed on the number of secondary interventions that are needed for endoAVF maturation and maintenance. At the beginning of his presentation, Steinke stated that he feels the positive reputation that endoAVF has garnered is due to “two warriors” in the field; Shahverdyan and Alexandros Mallios (Hôpital Paris Saint-Joseph, Paris, France). However, he also added that, whilst these two clinicians may see positive results—technical success is quite high for both Ellipsys (Medtronic) and WavelinQ (BD) systems, up to 100% and 97% respectively, he states—this is both from single-centre and single-operator experiences. He opined that, in the “real world”, there is a much higher need for secondary interventions for endoAVFs, when compared to surgically-created fistulas. Looking at patient selection, Steinke argued that the focus on young, male patients led to favourable operating conditions, as this is a patient population that is going to have larger vein and artery diameter. He also argued that, with a larger, more representative patient population, there has been a higher percentage of reinterventions that were needed to mature and maintain endoAVFs.
Summarising his argument, Steinke stated that “the majority of patients undergoing endoAVF procedures will require one or more adjunctive procedures, that might be costly, to create maturation. Ignoring this creates resentment amongst patients and nephrologists, who did not expect further interventions to achieve maturation. And, the need for secondary procedures will be significantly driven by the ability of the dialysis centres to cannulate an appropriate AV [arteriovenous] access.”
argument was that, not only are endoAVFs not a failed experiment, but they have also already become part of the treatment algorithm (at least at his clinic in Hamburg) for several years.
“EndoAVFs are part of my vascular access creation algorithm and it fits this ‘distal to proximal’ strategy,” he said, adding that “we know that we have high satisfaction, maturation, and usability rates.” Further, he argued that, whilst Steinke had shown that there was a lack of evidence supporting the wider use of endoAVF outside of specific centres and practitioners due to a lack of training or experience, the same is true for surgically created AVFs.
“EndoAVFs show comparable high maturation, cannulation and secondary patency rates,” he stated, adding the caveat that this was the case when they are created by


Endovascular AVFs are part of the algorithm The next argument to be presented, this time against the motion, came from Shahverdyan. The main aspect of his


A study recently published in the New England Journal of Medicine (NEJM) has demonstrated that semaglutide (Novo Nordisk) significantly reduces the risk of major kidney disease events, cardiovascular outcomes, and all-cause mortality in patients with type 2 diabetes and chronic kidney disease (CKD). The landmark trial, presented at the 61st European Renal Association (ERA) congress (23–26 May, Stockholm, Sweden), will pave the way for new treatment strategies and offer hope to millions of patients globally, researchers have claimed.
THE FLOW (EVALUATE RENAL FUNCTION with semaglutide once weekly) study is a doubleblind, randomised, placebo-controlled international trial comprising 3,533 patients, with a median follow-up period of 3.4 years. The trial was designed to assess the efficacy and safety of semaglutide, a once-weekly subcutaneous glucagon-like peptide 1 (GLP-1) receptor agonist, in preventing major kidney outcomes—specifically kidney failure, substantial loss of kidney function, and death from kidney or cardiovascular causes—in individuals with type 2 diabetes and CKD. Patients either received semaglutide (1mg) once weekly or placebo.
The study found that participants who received semaglutide had a 24% risk reduction for the composite primary endpoint—which included kidney outcomes and death due to cardiovascular and kidney causes—compared to those who received placebo. This reduction risk was consistent across both kidney-specific and cardiovascular death outcomes.
Secondary endpoints also showed significant improvements with semaglutide. Specifically, the total estimated glomerular filtration rate (eGFR) slope was 1.16ml/min/1.73m2/year slower, the risk of major cardiovascular events was decreased by 18%, and the risk of all-cause mortality was reduced by 20%.
This evidence of efficacy, combined with fewer serious adverse events in the semaglutide group, offers hope to millions of patients globally who face the daunting prospect of CKD and type 2 diabetes, and their related complications.
Vlado Perkovic (Royal North Shore Hospital, Sydney, Australia) presented the results for the first time at the ERA congress, where he said: “The use of semaglutide in people with type 2 diabetes and CKD can lower the risk of major kidney outcomes and reduce the risk of cardiovascular events, cardiovascular death and all-cause death. These benefits signify a profound clinical impact saving kidneys, hearts and lives, for patients with type 2 diabetes
and CKD. Additionally, the reassuring safety findings further support the strong potential value of semaglutide in this population.”
CKD, according to Perkovic et al, affects over 800 million people worldwide and is particularly prevalent among individuals with type 2 diabetes. They stated in a press release promoting the results of the FLOW study that CKD poses a significant risk of kidney failure, cardiovascular events and death, highlighting the critical need for research into its prevention and treatment. They also added that, whilst current therapies have demonstrated kidney protection and reduced cardiovascular risks, many individuals continue to experience declining kidney function and adverse outcomes. This has sparked a growing interest in exploring new treatments, including GLP-1 receptor agonists.
Perkovic further stated: “These findings offer great promise in reshaping treatment strategies for individuals at high risk of diabetes-related complications, offering a new avenue for kidney and cardiovascular protection.”
The FLOW trial was overseen by an academic-led steering committee, in partnership with the study sponsor, Novo Nordisk, which also managed trial operations. For more information on semaglutide from the ERA congress, go to page 17.
“These findings offer great promise in reshaping treatment strategies for individuals at high risk of diabetes-related complications, offering a new avenue for kidney and cardiovascular protection”
Editor-in-Chief: Nicholas Inston | Editorial Board: Ziv Haskal, Stephen Hohmann, Robert Jones
The latest stories from the renal world
PERITONEAL DIALYSIS:

Prior to a debate at UK Kidney Week (UKKW; 11–13 June, Edinburgh, UK) in which she will argue for the use of peritoneal dialysis in elderly and frail patients, president of the International Soceity for Peritoneal Dialysis (ISPD) Edwina Brown (Imperial College Healthcare, London, UK) sits down with Renal Interventions and examines the argument from both sides, whilst highlighting the collaboration between UKKW and the ISPD on this topic and what they hope to achieve from their joint efforts.
● For more on this story, go to page 6

HYPERKALAEMIA GUIDELINES: Discussing the recent updates to the UK Kidney Association (UKKA) hyperkalaemia guidelines, Annette Alfonzo (Victoria Hospital Kirkcaldy, Fife, UK) outlines to Renal Interventions the current state of hyperkalaemia treatment in the UK, what has changed in this latest update, and why the updates are so important.
● For more on this story, go to page 12
THE FUTURE OF KIDNEY DISEASE TREATMENT:
Douglas J Anderson and Jayme E Locke (both Marnix E Heersink School of Medicine, Birmingham, USA) share their thoughts of the field of kidney xenotransplantation in a point of view article that examines what is needed for xenotransplantation to be conducted safely and effectively, some of the obstacles that can be encountered, and the need for clinical trials that closely examine the viability of this new treatment option.


● For more on this story, go to page 15
Publisher: Stephen Greenhalgh | Content Director: Urmila Kerslake | Global Commercial Director: Sean Langer | Editor: George Barker georgeb@bibamedical.com
Editorial contribution: Éva Malpass and Jamie Bell | Design: Terry Hawes, Josh Lyon
Advertising: Rav Pankhania rav@bibamedical.com
Subscriptions: subscriptions@bibamedical.com | News or advertising queries: Tel: +44 (0)20 7736 8788
Published by: BIBA News, which is a subsidiary of BIBA Medical Ltd BIBA Medical, Europe, 526 Fulham Road, Fulham, London, SW6 5NR, United Kingdom Tel: +44 (0) 20 7736 8788 | BIBA Medical, North America, 155 North Wacker Drive, Suite 4250, Chicago, IL 60606, United States Tel: +1 708-770-7323
Printed by: Print Tech Solutions. Reprint requests and all correspondence regarding the newspaper should be addressed to the editor at the United Kingdom address. © BIBA Medical Ltd, 2024. All rights reserved.
If you have comments on this issue or suggestions for upcoming editions, write to georgeb@bibamedical.com
At the recent Vascular Access Society of the Americas (VASA) 2024 Vascular Access for Haemodialysis Symposium (16–18 May, Atlanta, USA), one of the focal points of the programme was the Global Dialysis Access Forum (GDAF). Divided into two sessions that took place during the first afternoon of the meeting, the GDAF looked at dialysis access care and initiatives in the USA, Japan, India, Europe, Asian Pacific nations and Latin America.

Following an introductory address from Surendra Shenoy (Washington University School of Medicine, St Louis, USA), the first presentation—which was given by Dirk Hentschel (Brigham and Women’s Hospital, Boston, USA)— examined dialysis access initiatives in the USA. The main message from Hentschel was that, as he said, “there’s still room for improvement”.
Reflecting on recent updates to guidelines for dialysis access, Hentschel used two examples to show how challenging he feels it can be to have a guideline with “implementation tools and concrete advice that is applicable across the USA”. Looking at the Kidney Disease Outcomes Quality Initiative (KDOQI) guidelines, he showed the audience an example of a flow diagram for central venous catheter insertion, specifically looking at the section addressing reduction of complications during catheter insertions.
“What you see there,” he said, “is that it’s recommended to use imaging for central venous tunnel catheter placement. And it gives the option between ultrasound and fluoroscopy. From the setting that I work in—an academic medical centre—there is nobody who would ever dare to place a tunnelled catheter, especially from the left side, without fluoroscopy, just given the complications that have occurred with this.”
Despite this risk associated with not using fluoroscopy for placing tunnelled catheters, Hentschel did concede that, during the COVID19 pandemic, there were many instances where tunnel catheters were placed just with ultrasound in life-saving situations, or situations where the benefits would outweigh the risks. Due to this exception, he stated that these guidelines “now have this asterisk that fluoroscopy is preferred and should be used whenever possible”, which he argues can be both too permissive or too strong a guide, depending on the environment you are in and the resources available to you.
Later in this session, after Hideki Kawanishi (Tsuchiya General Hospital, Hiroshima, Japan)
gave an update on dialysis access care in Japan, Matteo Tozzi (University of Insubria, Varese, Italy) spoke to the VASA audience regarding the state of dialysis access in Europe. When speaking to Renal Interventions, Tozzi said: “My participation in the global session is really an honour. I focused my presentation on three problems in the cohort of haemodialysis patients in Europe; correct timing for vascular access, elderly patients, and the follow-up for vascular access. It’s imperative to be aware of other data from the global perspective—so from the Japanese Society of Dialysis Access [JSDA], the Asian Pacific Society of Dialysis Access [APSDA], and [our VASA colleagues] as well as from South America. I think the outcomes for our patients are based on sharing the experience from global colleagues that perform this type of surgery, allowing us to improve the outcome of our treatment follow-up, and the quality of life of patients.
Following shortly after Tozzi’s presentation, Takashi Sato (Nagoya Kyoritsu Hospital, Nagoya, Japan) updated the audience on organisational challenges in Asia Pacific nations. Carlos Hinojosa (National Institute of Medical Science and Nutrition, Mexico City, Mexico) was then on hand to give the audience an update on dialysis access care in Latin America. The key message from his talk was clear; there are wide disparities in the level of dialysis access care across Latin America, both within nations and across the region as a whole. “In Central America,” he informed the audience, “there is a huge contrast in the management of vascular access. We can see in Costa Rica, they have a universal system and some of the best work, having one of the best health systems, whilst in Mexico, there is an inefficient public system that not everyone has access to, especially in recent years. Panama has a good system, but they face important problems to give or provide these services to the remote or more inaccessible communities.” As well as this, he stated that other countries, such as Brazil, Argentina, and Colombia, not only have dispar-
ities in the level of care available, but also have experienced a rise in the mortality rate.
“The concerning rise in the mortality rates in kidney disease has been noted since 2018 in different regions, and that tells us about the trends in these regions and what healthcare strategies are needed to address that underlying cause and improve the management of chronic renal disease.” Concluding his presentation, Hinojosa stated that “enhancing dialysis access management demands a collaborative and multidisciplinary effort across Latin America”.
When asked by Renal Interventions what he felt the key takeaways were, he said: “We can do much more, we can do better than what we do currently, and we need to communicate better, because there is some fantastic work in different places, but not all the countries have it. We need to carry on this global symposium.”
The final presentation of the session was given by Sanjiv Jasuja (Indraprastha Apollo Hospitals, New Delhi, India), who brought with him some insight into the challenges that accompany the efforts to organise dialysis access in India. Whilst he did say that access to dialysis care is improving in India and South East Asia, he feels that there are still some obstacles to overcome.
“The state economy is very important for us to take on the next level and a lack of time [spent] training hinders the majority of the processes.” It was not all negative, however. “AVATAR [Association of Vascular Access & inTerventionAl Renal Physicians], particularly,” he stated, “has brought a serious change in mindsets, enhanced learning, and supported the implementation of new policies.”
Sharing his thoughts on the value of this GDAF, Jasuja averred that “this is probably one of the finest programmes, because our globe is represented with their thought processes, their achievements, their way of working, and what they are delivering as they are now. For us particularly, coming from South East Asia, this is useful, because we still have a long way to go. It always gives us a challenge, but it also gives us insight, and it gives us kind of an opportunity to interact with our global colleagues and enhance our goals, levels, and our performances. So I think all in all, this is one of the finest programmes at the international level which has a collective approach, that puts everything together.”
“We can do much more, we can do better than what we do currently, and we need to communicate better, because there is some fantastic work in different places, but not all the countries have it”
Carlos Hinojosa
Speaking to Renal Interventions about the session, Shenoy stated: “If you step back and think about it, GDAF is a dream come true because you see so many experts from all over the world—pretty much covering the entire global population—sharing the problems seen with their population and their experience, all in one place. It has a lot of potential for global harmonisation of dialysis access care. There are lots of avenues where it can go to where it can help budding physicians and surgeons and nephrologists who are interested in access. So, it’s a great endeavour and hopefully we will be able to now go full force forward with the future meetings in Japan, in the UK or even VAS in Europe. We will continue to do this. We will continue doing the GDAF meetings and see where we can go.”
“experienced hands”. The key point, he argued, is that “this also applies to the surgical fistulas. Why should we focus on the learning curve for an endoAVF but not for a surgical fistula? Learning curves and experience need to be considered for both [surgical and endoAVFs].”
Shahverdyan also argued that the opinions of patients should be taken into consideration when looking at the success of the endoAVF “experiment”. He stated that one thing that should be considered is the high rate of satisfaction for patients with endoAVFs. Without going into detail, Shahverdyan stated that “although patients who have surgical fistulas are usually satisfied, and patients who have bad fistulas do not care about which kind of fistula they have, mostly, the trend is they are very satisfied with their endoAVFs”.
He also argued that the flexibility granted from the use of endoAVFs show that it is better for patient outcomes. “More disciplines can create [endoAVFs], and if they’re experienced, more patients can get dialysis access early on, avoiding catheter-related complications”. As well as this, he argued that “it is not a replacement for surgical fistulas, it’s an addition, and it is an excellent addition”. Concluding his presentation, Shahverdyan added that “we hope that, with the next generation devices, the problems we have with the first-generation devices might and will be avoided.”
We can have better results with surgical AVFs Next up to the plate, arguing alongside Steinke in support of the motion, was Thomas. He began by stating that this was not going to be an easy argument to make. “These devices aren’t exper-
imental,” he stated, “they’re approved. People are using them, and I think one of the great things is, anyone who’s got a lab, a needle and a wire can make a percutaneous AVF.” However, he continued that endoAVFs are a failed experiment because they’re the wrong approach to the vascular access dilemma that clinicians are facing.
“There’s a tsunami of patients that we’re all facing,” Thomas said, “who are developing dialysis dependency and they need a quick access that’s easy to use, that’s resistant to infection, that doesn’t need a lot of upkeep.” He then stated that he would show the audience, “through some accepted truths”, that endoAVFs are not the solution, nor are they even part of the solution.
The first of the “truths” that he referred to were that there is a rising incidence and prevalence of kidney disease throughout the world, and that, for long-term haemodialysis patients, the matured AVF is the preferred option, as it has got a reduced risk of mortality, thrombosis, a longer usable lifespan, and “there are just many positives to that over other access types”. Whilst he acknowledged that maturation was an issue for surgical AVFs, he argued that better results could be achieved by “upskilling” with surgical AVFs rather than turning to endoAVFs and that early recognition of issues via the use of on-table ultrasound to assess flow rates and the presence of stenoses can be used as a predictor for maturation, allowing for earlier intervention and greater maturation rates.
EndoAVFs need to be in the guidelines
The final presentation of the debate, joining Shahverdyan in defence of endoAVFs, was given by Wasse, who was arguing for the inclusion of endoAVFs in clinical guidelines. Looking at this, she began by stating that it is “important to note what criteria need to be met for that to occur”. The process, she reminded the audience, follows six steps; formulate a question, select outcomes, perform a systematic review, grade this process, evaluate the evidence available, and then recommendations regarding inclusion can be made.
Wasse’s first point was that, when evaluating the data that appear to argue against the use of endoAVFs via the use of the Newcastle-Ottowa
NKF urges passage of new US home dialysis bill
er-Meeks for their introduction of The Improving Access to Home Dialysis Act, which will help more patients learn about and gain access to home dialysis.”
The Improving Access to Home Dialysis Act will, if passed, do the following: mandate that patients get proper education on all of their dialysis options, including making sure that even patients who crash onto dialysis with no preparation can get education on other options once they have stabilised and can make informed decisions about their future; expand the universe of healthcare providers who can provide home dialysis training to remove the burden from the nursing staff and cut down on wait times to get trained, as well as also allowing for the use of group training, telehealth, and off-site training when appropriate; cover the costs of in-home healthcare support staff for patients when they’re beginning their home dialysis journey, which would help patients transition from the facility and support the patient and if available, their care partner, with the goal that they become fully independent over time. Some patients with certain disabilities or other concerns could be eligible for continuing in-home assistance.
The NKF also highlighted patients and advocates who

have previously utilised home dialysis that are voicing their support. Erich Ditschman, an NKF volunteer from East Lansing, USA, stated: “In 2001, I was fortunate to be offered home haemodialysis soon after I crashed into end-stage kidney disease [ESKD]. Home dialysis gives me the energy and health to be a better husband, father, and friend. Many of the patients on in-centre dialysis may not know home dialysis exists or have not been given the opportunity to use it. Once passed and signed, this legislation will help to make home dialysis much more accessible, especially to rural patients. It will save lives and help many ESKD patients to flourish.”
Speaking in support of the bill, congresswoman Marilyn Strickland from Olympia, USA, averred that “high-quality and affordable kidney care should not be considered a luxury in the USA. We must work together with caregivers and providers to ensure that patients have the resources and training they need to receive dialysis in the comfort
scale of assessment of 17 studies that have, to date, looked at over 2,000 patients who have received endoAVFs using one of the two US Food and Drug Administration (FDA) approved devices, the maximum score that any of them achieved was six out of nine, suggesting that the quality of data is not as good as one may hope it would be.
She highlighted that, whilst much of the currently available data are observational, single arm and retrospective, with a heterogeneous study design and limited follow-up in some cases, there is no doubt that endovascular technical success is high and achievable. As she put it, “there’s good cumulative patency and early cannulation feasibility in select patients. And that is what the data does, in fact, support.”
Similarly to Shahverdyan, Wasse also highlighted the high patient satisfaction with endoAVFs, as well as the fact that “studies to date really do support the idea that [endoAVFs] are non-inferior to surgical fistulas, and that in some ways, there’s a lower incidence of steal, as well as surgical site infection”.
Bringing her presentation to a close, Wasse added that the successful implementation of endoAVFs relies “on proper training, patient selection, and application”. She argued that we should not “do away” with endoAVFs because of issues with cannulation, but we should instead ensure that all team members are sufficiently trained to use these accesses.
“Why should we focus on the learning curve for an endoAVF, but not for a surgical fistula? Learning curves and experience need to be considered for both”
Robert Shahverdyan
of their own homes, and make sure that patients know that in-home care is an option.” Congresswoman Carol Miller from Huntington, USA, also commented on the bill, stating: “Individuals with [ESKD] are often faced with difficult decisions when choosing where to receive dialysis services. In rural areas, some patients must forgo a full-time job or time with their family to travel hours back and forth to dialysis centres to receive the life-sustaining care they need. Home dialysis is a wonderful tool that allows patients to be at the centre of their own care, and Congress should be working to ensure patients that choose this modality receive the training necessary to dialyse safely in their home. The Improving Access to Home Dialysis Act will provide patients the education and support they need to utilise home dialysis if they so choose.”
“Many
of the patients on incentre dialysis may not know home dialysis exists or have not been given the opportunity to use it. Once passed and signed, this legislation will help to make home dialysis much more accessible”
Erich Ditschman
At the 2024 Charing Cross (CX) International Symposium (23–25 April, London, UK), the Vascular Access Masterclass Controversies session delved into the question, ‘We have new technology, but do we need it?’ Among the notable presentations, Ellen Dillavou (WakeMed Heart Center, Raleigh, USA), ignited discourse on whether extravascular support should redefine the standard of care in surgical fistula creation. Advocating for the adoption of the VasQ extravascular nitinol support by Laminate Medical, Dillavou underscored its potential to address numerous prevalent challenges in fistula creation, positioning it as a pivotal innovation in dialysis access.
“Sometimes, it is difficult to see a change in the standard of care as it happens,” Dillavou said as she began her presentation, acknowledging the gradual evolution of medical standards and drawing parallels with the transformative impact of guidelines such as those set forth by the Kidney Disease Outcomes Quality Initiative (KDOQI) in the USA. “We can look back in the USA and see that the KDOQI guidelines emphasising fistula use definitely changed the way we practiced. [They] made more fistulas available for standard use, but it came with costs like increased catheter use, more procedures per useable fistula and a decrease in primary patency results.” Dillavou emphasised the need for enhanced access solutions with fewer interventions, lower infection rates, and faster maturation, highlighting that “the VasQ device can solve a lot of these problems” by mitigating common issues encountered in standard fistulas, such as stenosis and aneurysmal dilation by “keeping the fistula at an optimal angle and offering support to that dissected area of the vein to counteract the shear stress”.
Central to her argument were compelling datasets supporting VasQ’s efficacy. Referencing studies including a randomised controlled trial by Nikolaos Karydis (at time of study publication, at Guy’s and St Thomas’ NHS Foundation Trust, London, UK) and research by Robert Shahverdyan (Asklepios Klinik Barmbek, Hamburg, Germany), Dillavou showcased consistent improvements in maturation rates
and primary patency with VasQ utilisation. Furthermore, she presented findings from an ongoing study comparing VasQ to conventional methods, indicating superior functionality and patency outcomes with the device and pointed to Shahverdyan’s long-term success using the device as standard of care.
“When [Shahverdyan’s] practice shifted to using VasQ as part of his standard of care, he had a drastic reduction in primary failures and an increase in primary patency at six months”. Dillavou also referred to a study that she had contributed to comparing VasQ to historic controls. “In the USA, when we contrasted VasQ fistulas to historic controls, we found increased functionality at three and six months, and increased primary patency at all time-points. When we look at the body of literature in historic unsupported fistulas versus VasQ, we see a clear trend towards enhanced patient outcomes when they are externally supported.”
Beyond immediate postoperative benefits, Dillavou emphasised the long-term advantages of VasQ providing permanent structural support. Drawing from retrospective analyses, she illustrated reduced catheter days, decreased infection-related hospitalisations, and diminished incidences of complications such as steal syndrome and aneurysm formation. “This global view shows that patients have fewer catheter days and have fewer infection-related hospitalisations at one year. We also see that two years after creation with an external support



device, we are seeing fewer instances of steal, and we’re seeing less aneurysmal formation,” said Dillavou.
Addressing concerns regarding costs, Dillavou highlighted substantial cost savings estimated based on the existing clinical data. The potential for significant healthcare expenditure reduction with VasQ integration has been replicated in multiple countries, such as the UK, Italy, Germany and the USA. She also highlighted that VasQ has now reached Asia with Yong Enming and Zhang Li (both Tan Tock Seng Hospital, Singapore), underscoring global interest in exploring both the clinical and economic implications of VasQ adoption.
Following Dillavou’s presentation, audience participation was invited leading to inquiries delving into technical considerations and comparative efficacy, with insights provided by panelists including experienced VasQ users like Shahverdyan and Nicholas Inston (University Hospitals Birmingham, Birmingham, UK).
Speaking to Renal Interventions regarding the role that VasQ has to play in the future of AVFs, Inston, the session’s moderator, said: “The signal coming from multiple global studies consistently shows that VasQ has better outcomes than those in traditional surgical studies. If we strive to improve the outcomes of AVFs, we need to take these data seriously”.
Shahverdyan also shared his thoughts on the device with Renal Interventions, saying: “Looking at our experience of over six years with almost 300 VasQ implants (mostly for radiocephalic AVF creation, which historically have shown to fail more commonly), and the existing evidence throughout the globe on the outcomes of VasQ device, it consistently demonstrates significantly better outcomes in dialysis patients with extremely low safety concerns: we have observed zero cases of infection, steal or juxta-anastomotic aneurysms. Hence, it is
“The signal coming from multiple global studies consistently shows that VasQ has better outcomes than those in traditional surgical studies”
Nicholas Inston
justified to say that we as caregivers should provide our patients with best possible treatment options and consider the application of the VasQ device as standard of care.”
The discourse surrounding VasQ at the CX Symposium underscores a paradigm shift in dialysis access management, with mounting evidence and key experts heralding its potential role as a transformative standard of care. Of course, skepticism still exists based on the bulk of VasQ’s evidence from observational studies, especially compared the numerous randomised-controlled studies for technologies like drug-coated balloons (DCBs). In response to comments regarding the level of evidence for VasQ in comparison to DCBs, Dillavou closed out the discussion by stating “there’s more agreement in the VasQ device than there is for DCBs”. This statement highlights that the strength of the VasQ data has been in the consistent clinical benefit across multiple studies in various countries that is not typically observed for many new technologies.
Learn more about VasQ at laminatemedical.com/
Peritoneal dialysis (PD) is often foreshadowed by the dual spectre of fear of infection and peritonitis. “This happens because many nephrologists only see complications when patients are admitted [into hospital] and not the many fit patients in the community. In fact, PD infection rates are no different to haemodialysis (HD) and are often less consequential,” Edwina Brown, president of the International Society for Peritoneal Dialysis (ISPD) and professor of Renal Medicine, Imperial College London (London, UK), tells Renal Interventions
The ISPD is running a joint session with the UK Kidney Association at the latter organisation’s annual meeting, UK Kidney Week (UKKW; 11–13 June, Edinburgh, UK), on improving the quality of life for older people having dialysis. Brown outlines the “patchy” global usage of PD and takes aim at the multiple forces that are obstacles to improving this modality’s uptake.

What is the vision for the ISPD session at UKKW on improving the quality of life for older people having dialysis?
We aim to increase awareness of the need to think about and offer PD to older people, particularly when they are frail and/or have cognitive impairment. Vitally, we believe that with assistance, older people can have PD at home. Older, frail people find HD exhausting, and transport to the HD unit crushing. One of the most important things that older people are frightened of is the development of dementia; there is a need to discuss the risk of rapid deterioration in cognition on HD, particularly now with hard evidence of drops in cerebral blood flow and brain injury on HD.
Could you provide a succinct snapshot of how home HD therapies are being used in the global setting, particularly PD?
Very simply, the use of PD is patchy. In Europe, this can range anything from <5% in most of Eastern Europe, and even in Germany and France, to more like 25–30% in Scandinavia. Home HD use is even lower.
What are your main arguments that PD is a good option for frail and elderly end-stage kidney disease (ESKD) patients?
When on PD, the person is in their own home, or nursing home, and not dependent on transport. The time to recovery after HD is longer in older and frail people, and the risk of hypotension on HD with associated drops in cerebral blood flow, myocardial stunning, or loss of kidney function well documented. Older people usually start dialysis with residual kidney function so do not need a full dose of dialysis, which corresponds often to only two or three exchanges, five or six days per week. Residual kidney function declines more slowly with increasing age and on PD compared to HD so these people often stay on low dose for their remaining lifespan. Many older people
cannot perform their own dialysis but can be assisted by families and/or by paid assistants. This is still cheaper than in-centre HD when the cost of transport is added in, particularly when complex transport, for instance an ambulance plus a stretcher, is added in. Either automated peritoneal dialysis (APD) or continuous ambulatory peritoneal dialysis (CAPD) can be used, but many older people do not want to be attached to machines because of anxiety and/or wandering at night, particularly if there are cognition issues.
operates beginning with bias against PD (for a variety of reasons) that leads to low use, and therefore there is a lack of expertise that develops and also a lack of knowledge and failure to develop support pathways such as PD catheter placement, surgery, microbiology that all contribute to poor outcomes when a patient is put on PD, and yes, this again then increases the negative bias.
What education is needed in the kidney care community to overcome these barriers?
There is a real need for general education about PD to all members of the renal team, making available knowledge and the choice of PD to all patients starting dialysis. Time in a PD unit, attendance in PD clinics and PD-related courses should be compulsory parts of nephrology training. Management also needs to be aware of the advantages of PD in terms of cost benefits: fewer nurses, better patient satisfaction, lower costs overall, so that care pathways are developed and supported.
What are the main issues that “plague” the idea of PD? Are these backed by evidence and how can outcomes be optimised in different countries and healthcare settings?
PD is haunted by the fear of infection and peritonitis. This happens because many nephrologists only see complications when patients are admitted [to hospital] and not the many fit patients in the community. In fact, PD infection rates are no different to HD and are often less consequential. The other issue is the availability of PD catheter insertion. PD happens more often when nephrologists can insert catheters percutaneously and are therefore not totally dependent on surgeons. A global issue, and fortunately not one in UK, is privatisation of HD with higher reimbursement for nephrologists compared to PD, because they see patients thrice a week on HD but probably only about once a month when they are receiving PD. And in the crossfires of this issue, in some countries nephrologists own HD units or get an incentive or a ‘bribe’ when a patient starts on HD.
Is there any new evidence that the renal care community needs to be aware of?
Front and centre should be an increasing awareness of the global nursing crisis. There is also emerging evidence about sustainability, with PD being environmentally ‘greener’ than HD. Of course, there is the predicted continued growth of the ESKD population which will overwhelm HD centres in many countries and the overarching limitation in healthcare resources and costs in all countries. These are all factors that need to be taken into account.

PD—or any sort of dialysis—is only one part of care for an older person requiring dialysis. People on dialysis have accelerated ageing, and age-related syndromes should be recognised and managed in collaboration with geriatric and palliative care teams. Being on PD enables people to access support systems in
What would you say to patients and the teams that care for them to influence them to look at PD as a worthy approach?
When talking to patients who will need dialysis, I urge physicians and teams to tell each person there are two ways of doing dialysis; the first is coming to a hospital/renal centre three times every week or having a treatment at home. The first response to this from most patients is: ‘at home’. No one wants to go to a hospital three times a week. The next step is to assess feasibility and establish what the barriers are. There are very few absolute barriers against dialysis at home—most can be overcome with a bit of imagination.







During this year’s Charing Cross (CX) International Symposium (23–25th April, London, UK), the first day saw two separate sessions titled ‘Real Cases, Real Problems’, split across the Vascular Access Masterclass and Renal Interventions Controversies sessions. Each session looked at an example of a real case and asked the audience to suggest treatment options, exploring how different clinicians would solve issues that occurred in each case, before exploring how the patients were treated at the time.
THE FIRST OF THE SESSIONS, WHICH TOOK place in the morning portion of the Vascular Access Masterclass, was chaired by Nicholas Inston (University Hospitals Birmingham, Birmingham, UK). Kicking off the session, Inston stated that “what we have heard from CX over the years is that people like cases, and people like to discuss them to make things a little more like the real world. So we’ve introduced a bit more of that this year”. The case of the first session regarded a 65-yearold female who had a right brachiocephalic (BC) arteriovenous fistula (AVF) created eight weeks prior to the symposium, but when cannulation was attempted two weeks following initial AVF creation, there was a blow on dialysis, along with extensive bruising over her arm.
When cannulation was attempted again, there was no flow in the fistula and so a venogram was requested.
Displaying the venogram from the case, Inston invited comments, to which there were several suggested courses of action presented by clinicians from around the globe, leading to an international discussion of different treatment options.
The second session, chaired by Kate Steiner (East and North Herts NHS Trust, Stevenage, UK) as part of the afternoon’s Renal Intervention Controversies session, looked at two cases, both of which had more of an “interventional radiology flavour”, as Steiner stated. Rob Jones (Queen Elizabeth Hospital, Birmingham, UK) was the first to present his case—a 64-year-old male with previous failed bilateral brachiobasilic (BB) AVFs, a left axillary graft failure. He had a history of peripheral vascular disease, with a tunnelled catheter in 2021. He presented with head swelling, with blocked right sided central vein.
The last case, presented by Narayan Karunanithy (Guy’s & St Thomas’ NHS Foundation Trust, London, UK) was of a 46-year-old female patient with end stage renal failure secondary to type 1 diabetes mellitus. She had undergone a pre-emptive left BC AVF creation, and later underwent simultaneous kidney-pancreas transplant that was functioning. Three months after transplantation during the inpatient hospital stay, she developed gross
“It’s rare to see a single trial kill something that was greeted with enthusiasm, so the question is why is renal denervation alive again? The answer is new information.”
These were the words of Lindsay Machan (The University of British Columbia, Vancouver, Canada) at the 2024 Charing Cross (CX) International Symposium (23–25 April, London, UK), presenting in a session which discussed developing evidence in support of the retired techniques’ unanticipated return.
SPEAKING FIRST, NEELAN DAS (EAST Kent Hospitals University NHS Foundation Trust, London, UK) detailed the influential trial—SYMPLICITY HTN-3 (Renal denervation in patients with uncontrolled hypertension)— which, in 2014, found no significant difference between renal denervation and sham control groups at six-month follow-up published in The New England Journal of Medicine (NEJM)
“Renal denervation was—up to now—effectively abandoned,” Das said. “Yet, looking at three-year follow-up data from the SYMPLICITY HTN-3 trial published in 2022, the evidence suggested there was merit to renal denervation, and that’s with the first-generation single-electrode technology.”
Since then, the second generation, multi-electrode technology and ultrasound renal denervation techniques have also shown significant reduction in blood pressure compared to sham control groups, Das explained. Exemplifying this, Das quoted the RADIANCE II trial results—the largest trial comparing ultrasound renal denervation to a sham control—and highlighted the statistically significant improvement in blood pressure in patients who were taken off antihypertensive medication for four weeks, with a sustained benefit at night to prevent the deleterious effects of nocturnal hypertension. In November 2023, the Paradise
renal denervation system used in the RADIANCE II trial was approved by the US Food and Drug Administration (FDA), followed closely by the Symplicity Spyral renal denervation system in the same month.
Das went on to detail the current European Society of Hypertension (ESH) and UK National Institute of Clinical Excellence (NICE) guidance which suggests renal denervation should only be used in patients who have resistant hypertension, are intolerant to medications, or have uncontrolled hypertention despite the use of combination anti hypertensive therapy. Das went on to say there may even be a role for denervation in patients who were strongly against taking anti hypertensive medication, but this group must be fully informed of the risks and benefits compared to drug therapy.
Next to present on the topic, Machan lauded the return of renal denervation and why—in the context of 19.2% of global deaths being caused by hypertension—vascular and interventional radiologists “should care”.
“Looking at the historic headlines, everybody here would think this is a dead technology and assume that is shouldn’t resurface—why is it alive again? The answer is new information. We have new information for physicians who treat hypertension—of the 116 million adults in the USA with hypertension, less than half are controlled,
left arm and breast swelling. The computed tomography (CT) venogram had demonstrated likely line related central vein stenosis, focal cephalic arch stenosis and ‘high flow’ in the AVF. The subsequent discussion with multidisciplinary audience participation explored the options of central vein and cephalic arch balloon angioplasty and stenting, flow reduction procedure and other novel solutions. The panel and audience multidisciplinary team came to the consensus that the best course of action was to discuss with the patient and try to “improve life for the day, not for five years’ time,” as Inston framed it, and tie off the fistula to allow for a better quality of life for the patient.

“What we have heard from CX over the years is that people like cases, and people like to discuss them to make things a little more like the real world”Nicholas
Inston
and this rate of control is falling off. Nobody entirely understands why.”
Machan then referenced a 2021 meta-analysis carried out by the Blood Pressure Lowering Treatment Trialists’ Collaboration that found that, in close to 350,000 patients, a reduction of systolic blood pressure by 5mmHg reduced the risk of major cardiovascular events by 10%, irrespective of previous diagnoses of cardiovascular disease and even at high or extremely high blood pressure values.
“There’s a massive clinical need—even if we take 1% of patients affected, this dwarfs any other endovascular procedure out there”
Lindsay Machan
“The average reduction of systolic blood pressure if you add a new medication to a patient already on multiple medications is between 5–8mmHg—these treatments do work to reduce events,” Machan said. This is similar to the blood pressure improvements seen after renal denervation. However, it was newly introduced as a “cure”. “Which it’s not—they didn’t interface with the physicians who treat the disease—man, did they annoy the hypertension specialists. In addition there was poor patient selection and an underestimation of the domain-specific skillset needed to perform renal artery interventions”
Machan concluded by pointing to society consensus statements on renal denervation and the absence of any vascular surgery or interventional radiology society among them. “We need to pay attention to that,” he remarked. “Why should we be interested? There’s a massive clinical need—even if we take 1% of patients affected, this dwarfs any other endovascular procedure out there.” He stated that, today, “with data on the minimal reduction of blood pressure needed to realise clinical benefit, better patient selection, and better physician training, the return of renal denervation is a welcome addition within the present armamentarium”.

At the recent Charing Cross (CX) International Symposium (23–25 April, London, UK), a ground-breaking initiative emerged, focusing on enhancing vascular access anastomosis skills. Through a collaborative effort between BIBA Medical, Laminate Medical Technologies and YourAnastomosis, short workshop sessions were conducted, enabling participants to refine their techniques and understand optimal manoeuvres and devices for vascular access blood flow optimisation under the professional supervision of Nicholas Inston (University Hospitals Birmingham, Birmingham, UK).
UTILISING MACHINE LEARNINGdriven scoring by YourAnastomosis, participants received definitive scores with improvement suggestions, resulting in a mean score of 4.727696 � 1.2469, significantly above the general anastomosis performance median. With a standout score of 6.6954, the winner has been recently announced as Apostolos Chaveles (KAT Attica General Hospital, Athens, Greece). Speaking to Renal Interventions regarding his victory, Chaveles said: “It was a really great experience participating in such a well organised workshop. It helped us gain a deeper understanding in anastomosis technique and gave us the chance to create our own AVFs [arteriovenous fistulas].”
Commenting on Chaveles and his victory, Inston stated: “Not only has he created an anastomosis that looks the best, but YourAnastomosis has analysed this and has shown that it is the best in terms of its technical quality.” Inston also commented on the workshop as a whole: “This was run in conjunction with VasQ [Laminate Medical] for the very first time, and I think that this has been a great demonstration of two technologies, and showed the delegates at CX how all of these things come together to work so well in producing a great workshop.”
During the Vascular Access Masterclass session examining the question ‘We have new technology, but do we need it?’ at this year’s Charing Cross (CX) International Symposium (23–25 April, London, UK), attendees saw a podium first presentation from Andrew Holden (Auckland City Hospital, Auckland, New Zealand) in which he shared new fiveyear follow-up data from the IN.PACT AV access randomised controlled trial (RCT).
Outlining the primary purpose of the RCT, Holden began by asking what we know regarding longterm follow-up for end-stage kidney disease (ESKD) patients. “We do know quite a lot at a population level about these patients,” he averred, “but results in the data are inconsistent. We don’t have any gold standard, for example, on fistula creation or maintenance and the ideal management algorithms.”
To combat this lack of knowledge, researchers conducting the IN.PACT AV RCT have published large amounts of data since 2016, starting with the study set up and primary endpoint results in the New England Journal of Medicine (NEJM), followed by a number of subsequent publications, including some economic analyses that Holden feels “are very helpful in terms of determining the place of DCBs [drug-coated balloons] and in AV [arteriovenous] access interventions”.
Before focusing entirely on the new data from the five-year follow up, Holden first reminded the audience of the primary efficacy results that were published in the NEJM, highlighting that, “for the first time”, a DCB showed a highly significant patency advantage of 81.4% at 210 days compared to 59% for the plain balloon. Holden also pointed out that through various time points, there was not only improved primary patency for the target lesion observed, but also for the entire access circuit. As well as this, he also pointed out that “at 12 months, we saw a primary patency of 63.8%, which was significantly better that the plain balloon arm, which was reported in the Journal of Vascular and Interventional Radiology”.
Holden highlighted the economic benefits of DCBs when compared to plain-balloon angioplasty. Referring to “two important published economic analyses”, he argued that, whilst there is an upfront cost of DCBs at the index procedure, there was a cost saving due to reduced reinterventions at the three-year time point, at the study sites in the USA, Japan and South Korea.
One of the things that researchers began to notice, Holden stated, was a trend in the plain-balloon angioplasty cohort of access circuit thrombosis occurring with a higher incidence, which, at three years, had reached statistical significance. “As you can see, 18.3% versus 8.2%, a statistically significant advantage.” He continued, adding: “Some of the variables in a multivariable analysis impacted on access circuit thrombosis included previous reintervention and a higher pre-procedure diameter stenosis in an upper arm fistula. But the most
powerful impact was the use of a plain balloon rather than a DCB.”
Holden then moved on to the five-year data, stating that the patients in the IN.PACT AV access study were then re-consented to allow a five-year follow-up. “As you can imagine,” he said, “there were withdrawals in both arms of the trial, because the patients had to re-consent, and some patients had passed away.” Despite this, Holden reassured the audience that they still had “good numbers out to five years” to assess vital status. In this analysis, there was no evidence of a mortality risk with DCB AV access, with Holden adding that the survival for patients who received the DCB was a little higher.
One aspect of the trial that Holden did point out was that, in both arms of the trial, the mortality was significantly lower (46.5% for plain-balloon angioplasty and 41% for DCBs) than the estimated mortality (60.4%), based on the United States Renal Data System (USRDS). Holden’s reasoning for this difference was that it was likely a reflection of “patients experiencing optimal medical management in the setting of a clinical trial”.
Another question that Holden asked was why the IN.PACT AV access RCT trial had such positive results compared to other similar trials. “That’s really a long discussion,” according to Holden. “I think we should acknowledge that the trials are different in terms of patient characteristics. There are some differences in trial design and in the procedure, the quality of vessel preparation, but there’s also differences in the device. We’ve seen better patency with IN.PACT than some of the other DCBs not only in AV access, but also in other territories.”
Bringing his presentation to a close, Holden concluded by saying that: “The IN.PACT AV access trial is the only randomised pivotal trial to show consistent benefit out to 36 months. We don’t see any sign of a mortality concern, and I’d propose that the long-term data suggests that we know which device to use; the IN.PACT AV access DCB.”
“The IN.PACT AV access trial is the only randomised pivotal trial to show consistent benefit out to 36 months”

With 40 years of experience working in nephrology, a passion for advancing the fields of nephrology and kidney disease, and a love of crafting, vascular access marketing manager at Transonic Systems, Deborah Brouwer-Maier (Lansdale, USA), speaks to Renal Interventions about her career as a dialysis nurse, the importance of training and multidisciplinary teams, and her hopes for the future of dialysis care.
What drew you to your career in haemodialysis vascular access?
I graduated from nursing school and was offered my first job at the same hospital if I would agree to work on the metabolic/renal inpatient ward. At that time, any patient initiated on peritoneal dialysis (PD) or haemodialysis (HD) was admitted to our ward for their first full week of dialysis. We supported their initial education on diet, medications, vascular access or PD catheter care, and the dialysis modality. I quickly became an expert in both continuous ambulatory peritoneal dialysis (CAPD) and cycler dialysis (glass bottles at the time). I was very interested in learning HD as I only observed acute bedside treatments. The dialysis program at the hospital was sold to a dialysis provider, and anyone could apply for a new position, including in their outpatient dialysis centres. I got hired for a new outpatient dialysis centre that was opening much closer to my home. I gained HD experience and then joined a large hospital-based nephrology programme that included all aspects of kidney care, including acute dialysis and transplantation programmes. My interest in vascular access started when I learned to cannulate arteriovenous (AV) accesses. The training consisted of a see-onedo-one training method. I struggled to find references to support my learning of vascular access and cannulation techniques, so I made it my mission to create a proper training programme to support the theory and practical applications of vascular access cannulation. When I joined the hospital-based programme, I gained more resources to create a proper cannulation training process for new staff. I documented the theory in a publication and created a hands-on cannulation camp training model. The cannulation focus then spread to the general vascular access process for care due to the high incidence of access complications.
From the late 1980s to the early 1990s, vascular access care was very limited. Complications were mainly treated surgically as endovascular interventions had not yet progressed to dialysis access. Clinical trials and other research on vascular access care were minimal. Thus, mentors became the main source of new knowl-
worked together on many projects, such as the fistula-first initiative, and professional organisations, such as ASDIN and VASA, until her passing last year.
I am incredibly grateful for the many individuals with kidney disease whose care I have had the privilege of being a a part of or have learned from in my many volunteer activities. My most important role has been, and will always be, to serve as an advocate for individuals with kidney disease.
What, in your view, is the biggest roadblock to further developments in dialysis?
In the USA, the business model focuses on the cost/reimbursement of care and profits for the large dialysis providers. For example, the utilisation of point-of-care ultrasound (POCUS) to support improved cannulation is very limited, due to the added cost of the equipment, staff time for the tasks, and lack of separate reimbursement. With the fragmented care system, cost savings for decreased cannulated-related access complications are not savings for the dialysis providers and thus do not offset the additional costs of POCUS.
Current appointment:
Vascular access marketing manager, Transonic Systems Inc., Ithaca, USA
Education:
1983: Western Pennsylvania Hospital School of Nursing, Pittsburgh, USA
Honours (selected):
1997: National Kidney Foundation – Special Recognition Award for NKF-DOQI Guideline Work Group Member 1997, and KDOQI 2000, 2006 Work Group Member
edge to help me increase my knowledge base and impact changes in the process of care related to all aspects of vascular access. I first encountered Susan Boothe as she was the clinical specialist who was supporting polytetrafluoroethylene (PTFE) grafts for haemodialysis. She connected me with Mitchell Henry, and he visited my hospital to help us gain a better understanding of AV access complications and possible treatments. This led to Henry inviting me to be the first nurse to present the nursing perspective of vascular access at the 1995 Symposium on Dialysis Access IV sponsored by the division of transplantation at The Ohio State University, and the book chapter publication. That was the same year as my first publication, entitled Cannulation Camp: Basic Needle Training for Dialysis Staff. My early publications and presentations on cannulation led to my selection to the first Dialysis Outcomes Quality Initiative (DOQI) Vascular Access Guidelines work group. I was honoured to serve with Gerald Beathard, Jack Work, and Anatole Besarab. I am so grateful for their mentorship over the many years they have helped me understand the complex vascular access issues. I went to serve on the Kidney Disease Outcomes Quality Initiative (KDOQI) 2000 and 2006 work groups, thanks to their support.
The names of the many other devoted professionals who have mentored me are too long to list. I strive to pay it forward with my volunteer work with Vascular Access Society of the Americas (VASA), American Society of Diagnostic and Interventional Nephrology (ASDIN), and American Nephrology Nurses Association (ANNA). My mentors taught me that knowledge shared has the most significant impact on a larger number of patients and that the goal is to improve the care of process for all patients requiring dialysis.
Lesley C Dinwiddie was the reviewer for my Cannulation Camp publication. She then became my mentor as she was the trailblazer for the role of vascular access coordinator. Patt Peterson Ryder worked for the arteriovenous fistula (AVF) needle manufactory, and she helped mentor me for cannulation-related topics and assisted me with the Cannulation Camp hands-on programmes. Janet Holland worked with a large dialysis organisation as a vascular access educator and became a key mentor for me. We
We need to change the mind-set of cost containment and reimbursement as the driving factors leading to fragmented care, and focus on improved outcomes that can reduce overall costs. For example, the implementation of the end stage kidney disease (ESKD) life plan and access plans is blocked by the fragmented process of care in the USA. The utilisation would help focus care on the patient’s lifespan and, more importantly, meet the patient’s goals for their journey with kidney diseases. This would lead to more innovation, such as innovations in dialysis procedures to allow more patient involvement and self-care. Solutions can be simplified dialysis equipment, devices to assist with single-handed cannulation, needle securement, or needle removal. We have heard the patient’s voice via the Kidney Health Initiative ‘s (KHI) work that a needleless vascular access would be their goal. Shifting the focus to the patient’s point of view with their input can help us change innovation to meet their needs, instead of focusing on the business side and the healthcare professional’s needs.
How important is a multidisciplinary team for the care of dialysis patients?
It is the most critical element. All members of the team are needed to support the best overall care. The need starts with CKD diagnosis and continues as the individual progresses into the later stages of CKD, modality selection (regardless of the modality), and continues throughout an individual’s lifetime. The care is interdependent on the entire multidisciplinary team and must include the patient at the team’s centre. All members bring their unique knowledge base and experience to work collaboratively to create the optimal care plan and respond to challenges as they arise.
What changes would you like to see in dialysis access care?
In my 40-plus years of nephrology, limited advances in cannulation have occurred, including limited improvements to the needle designs. The only two innovations that have gained wide adoption in the USA are safety needles and buttonhole needles. My mentor, Patt Peterson Ryder, helped drive both needle design changes. The safety needles were the direct result of US government’s Occupational Safety and Health Administration publication of the Occupational Exposure to Bloodborne Pathogens standard in 1991. The adoption of other needle designs such as buttonhole needles and longer or shorter needle lengths than the standard one
2006: Centers for Medicare & Medicaid Service- Certificate of Award for Leadership with the Fistula First Initiative
2007: Centers for Medicare & Medicaid Service Office of Clinical Standards and Quality, Office Director’s Citation for co-chair of the Practitioner Education & Training subcommittee Fistula First
2007: American Nephrology Nurses Association (ANNA) Nephrology Nurse Educator Award
2010: National Kidney Foundation serving the Alleghenies Gift of Life Samll Hands, Big Heart Award
2023: First recipient of the American Society of Diagnostic and Interventional Nephrology (ASDIN) Associate Recognition Award

inch needles, is limited due to cost per needle differences. A cannula is currently in a clinical study required for US Food and Drug Administration (FDA) clearance, and the same cost concern will impact the commercialisation of plastic cannulas.
POCUS also lags in adoption due to the cost of the devices and related staff time for training and utilisation. I would like to see POCUS become widely available for cannulation mapping to reduce the number of missed cannulations and infiltrations commonly occurring and accepted as just part of the cannulation process when the complications can be avoided with proper implementation of POCUS.
I would also like to see the full implementation of the ESKD life plan and access plans. As a kidney community, we need to improve the education materials and processes for patients in the earlier stages of CKD. No one can make major life choices like a modality choice, including conservative care or kidney transplantation, without proper educational materials geared toward their current level of knowledge and ones that address the emotional and physical aspects. We need to partner with patients to help
“A new dialysis care professional should not be learning cannulation on an actual patient”
create meaningful educational programs for various stages of CKD. We need to urgently engage patients as new therapies gain adoption to help slow the progression of kidney disease.
How would you expand training for those looking to start a career in haemodialysis vascular access?
We need a standardised cannulation training model based on best practices. The model must include theory and skills training prior to actual patient care. We need an easy-to-use, cost-effective cannulation training device. A new dialysis
care professional should not be learning cannulation on an actual patient. We need a simulator for skills training and assessment to ensure the basic cannulation technique is mastered before a needle is inserted into a patient’s vascular access. The patients should not be the test arms for staff learning.
What are your interests outside of medicine?
I love to cook using produce from our garden and from the local farmer’s markets. My son gave me a cookbook as a gift, and we connected via FaceTime to cook recipes together, as he lives too far away to see each other frequently. I enjoy making homemade pasta and sauces.
I also enjoy crafting. I was honoured when my stepdaughter got married, as she allowed me to help design and make the centrepieces as my contribution towards their wedding day.
My gardening time includes both large outside gardens and miniature inside fairy gardens. I design them as gifts to reflect the recipient’s interests.
Homemade gifts are a regular part of my gift-giving as I enjoy making unique things for family and friends.
Following the publication of the updated UK Kidney Association (UKKA) clinical practice guidelines on the treatment of acute hyperkalaemia in adults in 2023, Renal Interventions spoke to Annette Alfonzo (Victoria Hospital Kirkcaldy, Fife, UK) about the current state of hyperkalaemia in the UK, what has been updated in the guidelines, and why these changes are so important.
What is the current state of hyperkalaemia and its treatment in the UK?
So, I would say that, if we rewound the clock about 20 years ago, cases of hyperkalaemia were not nearly as frequent as we are seeing now. This is because we are using drugs that can exacerbate hyperkalaemia more widely to treat many conditions like diabetes, heart failure and proteinuric kidney diseases. Moreover, given the prevalence of chronic kidney disease (CKD), the risk of hyperkalaemia is increased further. Hyperkalaemia limits the management of these conditions and this risk has been shown in many clinical trials. Reducing dose or stopping essential medications due to hyperkalaemia has an impact on disease control and patient outcome. There has been a lot of focus on hyperkalaemia for that reason and specialists are now keen to consider new treatments to avoid down-titration of essential drugs. Hyperkalaemia remains common in the acute setting and affects up to 10% of hospital admissions, so developing a guideline to optimise established treatments (insulin/glucose and intravenous [IV] calcium) and incorporate new treatments (potassium binders) for hyperkalaemia was essential.
What are the key updates to the new guidelines?
Our focus was to ensure that we consider patient safety and to make sure we are giving optimal treatment in the right doses, at the right rate, and to the right patients. That was very important when it came to both IV calcium and insulin. The Medicines and Healthcare products Regulatory Agency (MHRA) has looked into intravenous calcium recently, as they were concerned about several adverse events, including deaths in patients with hyperkalaemia that suggested that patients may not have received an adequate dose of IV calcium. They undertook a period of investigation and fact-finding focusing on the dose and rate of administration of IV calcium and they have advised that the Renal Association guideline should be adopted. Our approach to administer an initial dose of 30ml of 10% calcium gluconate intravenously over 10 minutes protects the heart and avoids delay in initiating potassium-lowering treatments.
When we did the previous guidelines in 2020, we had to consider—should we reduce the dose of insulin to reduce the risk of hypoglycaemia? I would say that this was the part of the guideline that we spent the most time deliberating, because
the risk of hypoglycaemia using the conventional approach (10 units) was up to 20%—nowadays, would you accept a treatment if you had a 20% chance of getting a really significant side effect?
So we worked hard to address this problem and come up with a strategy that reduces hypoglycaemia, yet maintains efficacy. So, our strategy— and it is a big change in practice—is to check the baseline blood sugar before we treat with insulin glucose. From all the studies that have been published, a consistent finding was that the risk of hypoglycaemia was higher in patients with a baseline blood sugar of less than seven. If you treat patients with a follow-on infusion of 10% dextrose for five hours, so it delivers a further 25 grams of glucose, that will reduce the risk of hypoglycaemia over the period that the patients are most at risk of getting hypoglycaemic. I was very reassured that the threshold we chose of less than seven has been supported by several studies
since 2020. That is one of the biggest achievements of the UKKA guidelines and it would be interesting to see if this makes an impact in clinical practice and in future studies.
Why are these updates so important, and what is the ultimate goal with these guidelines?
The ultimate goals are to provide an evidencebased approach to management of hyperkalaemia, to reduce variability in clinical practice and to ensure patient safety. Although the guideline is lengthy, it is the only guideline available that covers the whole scope of how hyperkalaemia can present—community, hospital, and resuscitation. Having a targeted focus and summarising in an algorithm for each subchapter makes ours quite user-friendly. The hospital algorithm can be printed and made as part of your inpatient record—and in my hospital that’s what we do.

Resuscitation practice has shown that algorithms are quite helpful and they’re good aide mémoires and teaching tools.
I think hyperkalaemia management is different depending on the clinical setting. In the very first guideline in 2014, we didn’t really have a dedicated section for community management. A fair number of cases happen outside of a hospital setting, so it was quite important to make sure that we included management in the community—this means anyone not in an acute hospital bed. So, it could be a GP surgery, outpatient clinic, community hospital, or hospital at home.
So I think when you ask what is the importance of the new guideline, it’s really to make sure that we are using the most current evidence, translating that in a way that people can use it at a bedside, and ensuring that we take steps to reduce avoidable harm like hypoglycaemia.
Is there anything else that needs to be highlighted about these new guidelines or hyperkalaemia in general?
I think that hyperkalaemia is not just a renal problem. It can happen to any acutely unwell patient, as well as patients in a stable, well condition. It can be life-threatening, so vigilance is important. We wanted to create a guideline that makes it easy for the first responder to act. This may be a foundation year one and two trainees, treating a patient in the middle of the night. They need to know the initial steps, when to call for help and ultimately, how to monitor the patient, because it’s not only about monitoring the potassium, it is also about monitoring the heart and the blood sugar level.
I would also add that the UKKA guideline follows a five-step approach; whereas historically, most other reports stop after the first three. We’ve extended to five-stages to embed two further critical steps in every patient’s management—“monitoring” and “prevention”.
“Hyperkalaemia is not just a renal problem. It can happen to any acutely unwell patient, as well as patients in a stable, well condition. It can be life threatening, so vigilance is important”







Prior to the recent Vascular Access Society of the Americas (VASA) Vascular Access for Hemodialysis Symposium (16–18 May, Atlanta, USA), Renal Interventions spoke to William Jennings (OU Health-University of Oklahoma Medical Center, Tulsa, USA) about being chosen as this year’s speaker for the Henry Lecture. During his lecture, Jennings planned to draw attention to his work with Bridge of Life’s (BOL) medical missions, which are focused on chronic kidney disease (CKD) treatment and prevention in developing countries.
Could you outline the premise of the Henry Lecture and also your work with BOL and its vascular access missions?
VASA, much like the European Vascular Access Society (VAS), was founded to combine all the different specialties that are involved in vascular access. Outcomes are clearly much better when you have association with the different specialties and cooperation between them. Mitchell L Henry (The Ohio State University Wexler Medical Center, Columbus, USA) was one of the founders of VASA. He was the third president of the organisation and has been very active in kidney disease, transplantation and vascular access throughout his career. The Henry Lecture was started to honour him for his decades of patient care, teaching and research in the field. Previous examples of past Henry Lectures have featured nephrologists, interventional nephrologists, basic scientists, allied healthcare personnel and surgeons, so it’s a broad range of individuals invited to give this lecture.
I’ve been involved with BOL vascular access surgical efforts since the original vascular access surgical mission in 2012. BOL is a not-for-profit organisation with over 220 missions since its inception in 2006. The surgical missions started in Jamaica, and we’ve now completed over 1,000 vascular access operations in several localities. We have also had many missions for paediatric vascular access in Guatemala City, and it has been particularly rewarding to be involved with all those kids.
We published our experience with children in Guatemala a few years ago, which looked at our first three years of data and we are now preparing our eightyear data to look at teaching with surgical graded responsibility among a group of paediatric surgeons in Guatemala City. We’ve also had missions in other areas of Guatemala for adults, and we’re starting a new mission programme in Guatemala City for adults. There is a lot going on with BOL and we have had good results in Jamaica with a markedly improved fistula rate. Several local surgeons have become skilled vascular access surgeons with good results.
What do you think has been the main thing you have taken back to your own practice from these missions?
I have been involved with teaching surgery and research efforts for 45 years now at the University of Oklahoma in Tulsa with my own practice and with residents and fellows, so we extend that
educational experience into our missions. The surgeons who go with us on these mission trips are all educators, they’re all experienced in teaching vascular access surgery, they’re all competent and very skilled in ultrasound, preoperative diagnosis and postoperative care. We also have didactic teaching at these centres besides hands-on graded responsibility and surgical learning. We have been invited to go to each location by the nephrology and surgery groups that recognise the need for something other than catheter dialysis access. We have pre-mission conferences and consultation with them to understand where they stand and how we can best help them.
What do you think are obstacles for vascular access that are more prevalent on a global level?

The places we visit on these missions have very different challenges; some have more resources, some have less. As an example, when we were first invited to work in Guatemala with children, they had very skilled paediatric surgeons and a peritoneal dialysis programme. They also had a functioning transplant department. They just had no experience in vascular access creation. All their dialysis catheters were placed in the subclavian position without ultrasound. We were able to help them get an ultrasound machine—facilitated with Alexandros Mallios (Hôpital Paris Saint-Joseph, Paris, France)—and teach them how to use that for placing catheters via the internal jugular vein and for vessel mapping to plan vascular access operations. Then, over two or three of the first missions, we advanced their surgeons from being assistants to the primary surgeon. So it’s a process, rather than a single visit. That also reflects our experience in Jamaica. We have now been going there for 14 years, to different localities and different hospitals—including the University Hospital of the West Indies— and we’ve watched individual surgeons who were just out of residency move into becoming attending physicians and they have become skilled in vascular access.

That’s our primary goal; to establish those local surgeons where they have the skills and the abilities to create the best access, deal with any complication that might arise and understand how to fix a dysfunctional fistula.
Looking forward, what is one goal that you have for the future of these missions?
The University Hospital in Kingston, Jamaica, has established a specific surgical vascular access clinic with two experienced surgeons and resident physicians. There is a surgeon we have trained in access in Mandeville with reliable arteriovenous fistula (AVF) skills, and on the western side of Jamaica, we worked many years with a very skilled surgeon, but their main hospital has been closed for several years and they have a large AVF backlog. Our upcoming mission will be to work with him again and help with the large number of patients who need access in the Montego Bay region of the island. In Guatemala, we’re initiating a mission programme for a new adult access programme. The catheter rate is very high in the adult group and we’re going to extend our children’s AVF effort into these adult patients in Guate-
“One thing that VASA attendees will see in my lecture is the huge numbers of untreated and underserviced individuals throughout the world; its a giant area that cries out for help”

mala City. We are also starting a visiting surgeon programme with the first surgeon from Honduras—who will spend a week with us in Guatemala City doing paediatric access. Those are some examples of where we’re headed.
What is it that you’re hoping the audience at VASA will take away from this lecture?
I think the main thing I hope will come from this lecture is that other people will start individual programmes in other areas. One of our colleagues who was a fellow here in Tulsa, Alexandros Mallios, has started vascular access procedures in some of the French islands off Eastern Africa, expanding more efforts for new access training. One thing that VASA attendees will see in my lecture is the huge numbers of untreated and underserviced individuals throughout the world; it’s a giant area that cries out for help.


Douglas J Anderson and Jayme E Locke (both Marnix E Heersink School of Medicine, Birmingham, USA) write about genetically edited pig kidney xenotransplantation, the promising results that have been seen from previous studies, and their hopes for the future of this new treatment option for end-stage kidney disease (ESKD).
Kidney transplantation remains the best available treatment for ESKD. Sadly, most patients will not realise the benefits of kidney transplant due to the shortage of donor organs; many patients die waiting for a transplant and many more are never listed. Xenotransplantation, using an animal as the donor, offers the opportunity to end this shortage.
Decades of effort placed into exploring the immunobiology of cross-species transplantation yielded increased understanding of the barriers to xenotransplantation. Pigs emerged as the preferred donor due to rapid growth, early and frequent reproduction with large litters, and relative ease of husbandry.1 However, preformed antibodies lead to rapid hyper-acute rejection of untreated pig xeno grafts. Genetic modification of the donor animal offered a solu tion to this issue, and furthermore allows for introduction of human regulatory genes to further ameliorate the human anti-pig response. However, introducing multiple genetic modifications into a large mammal remained a significant challenge until the advent of CRISPR-Cas9 technology. Now, we have produced donor animals with up to 69 genetic edits.2
accelerating factor, and a human tumour necrosis factor regulator.2,3 Genetic manipulation can also address practical concerns, such as knockout of the growth hormone receptor to reduce post-transplant organ growth or deletion of all copies of the porcine endogenous retrovirus (PERV) genome as a safety measure. 2,4 What combination of genetic edits is optimal, and which could alternatively be managed pharmacologically, or by careful husbandry and screening in the case of the PERV genome, remains to be seen.

The genetic modifications of the donor pig both reduce the burden of preformed antibodies, but also make the pig xenograft more “humanlike” in the view of the recipient immune system. Various genetic modifications have been introduced. Virtually all constructs utilise knockout of the Gal antigen, which accounts for the majority of preformed antibodies. Other modifications that have been employed include knockout of two other carbohydrate xenoantigens and introduction of a variety of human transgenes: thrombomodulin, endothelial cell protein C receptor, CD47, haem oxygenase-1 (HO-1), CD46, decay
Preclinical work using genetically modified pig kidneys has yielded promising results. Xenokidneys have provided life-sustaining renal function in non-human primates for over two 2 In the Parsons model, using a brain-dead human recipient, renal function with clearance of creatinine and maintenance of physiologic homeostasis has been demonstrated, and this can be accomplished with standard, clinically available immunosuppression. 3,5,6 While hyperacute rejection is relatively easily avoided at this point, thorough investigation of the human immune response to the pig xenograft has yielded mixed results, likely owing to differences in the exact genetic construct used and differing immunosuppressive protocols.7,8 Transmission of PERVs and other porcine viruses, such as porcine cytomegalovirus (CMV) can be avoided with careful screening of the donor herd. 3 Two living patients have now been the recipients of porcine kidneys, reportedly with initial graft function.9,10
The promising results of these translational studies suggest we have reached the point where xenotransplantation should be studied in a systematic clinical trial to address remaining knowledge gaps. The longevity of a xenotransplant remains a significant unanswered ques -
tion: is this destination therapy or merely a bridge to allotransplantation? What is the optimal combination of genetic modifications and immunosuppressive protocols? Will zoonotic infection remain a concern over longer periods of time? These are all questions that will need to be addressed in a systematic way, and in larger numbers than individual case reports or even small series. The time for a clinical trial is now, in hopes that we can end the organ shortage. Collaboration between medical teams, engineers and patients is crucial for advancing such technologies in haemodialysis access. Collaboration with patients and caregivers, meanwhile, is equally vital, and involving them in the design and testing process ensures that the solutions developed truly meet the needs and preferences of those who will use them. Patient feedback is invaluable when refining wearable devices and algorithms so that they are user-friendly, reliable, and well-integrated into patients’ daily lives.
Disclosures: Anderson and Locke have received research support/grants from United Therapeutics and its subsidiaries, Revivicor and Lung Biotechnologies.
References:
1. Sachs DH. The pig as a potential xenograft donor. Vet Immunol Immunopathol. 1994 Oct;43(1–3):185–91.
2. Anand RP, Layer JV, Heja D, et al. Design and testing of a humanized porcine donor for xenotransplantation. Nature. 2023 Oct 12;622(7982):393–401.
3. Porrett PM, Orandi BJ, Kumar V, et al. First clinical-grade porcine kidney xenotransplant using a human decedent model. Am J Transplant Off J Am Soc Transplant Am Soc Transpl Surg. 2022 Apr;22(4):1037–53.
4. Hansen-Estruch C, Iwase H, Jagdale A, et al. Initial Experience with Growth Hormone Receptor Knockout in Pig-to-Baboon Kidney Transplantation: Effect on Ureteric Viability and Kidney Growth [abstract]. Am J Transplant [Internet]. 2021. Available from: https:// atcmeetingabstracts.com/abstract/ initial-experience-with-growth-hormone-receptor-knockout-in-pig-to-baboon-kidney-transplantation-effect-on-ureteric-viability-and-kidney-growth/
5. Locke JE, Kumar V, Anderson D, et al. Normal Graft Function After Pig-to-Human Kidney Xenotransplant. JAMA Surg. 2023 Oct 1;158(10):1106.
6. Jones-Carr ME, Fatima H, Kumar V, et al. C5 inhibition with eculizumab prevents thrombotic microangiopathy in a case series of pig-to-human kidney xenotransplantation. J Clin Invest. 2024 Jan 25;134(5):e175996.
7. Loupy A, Goutaudier V, Giarraputo A, et al. Immune response after pig-to-human kidney xenotransplantation: a multimodal phenotyping study. The Lancet. 2023 Sep;402(10408):1158–69.
8. Cheung MD. Spatiotemporal immune atlas of a clinical-grade gene-edited pig-to-human kidney xenotransplant. Nat Commun. 2024;15:3140.
9. Chase B. World’s First Genetically-Edited Pig Kidney Transplant into Living Recipient Performed at Massachusetts General Hospital [Internet]. 2024. Available from: https://www.massgeneral.org/news/ press-release/ worlds-first-genetically-edited-pig-kidney-transplant-into-living-recipient
10. DeVries C. First-Ever Combined Heart Pump & Gene-Edited Pig Kidney Transplant Gives New Hope to Patient with Terminal Illness [Internet]. 2024 [cited 2024 Apr 25]. Available from: https://nyulangone.org/ news/first-ever-combined-heart-pump-gene-editedpig-kidney-transplant-gives-new-hope-patient-terminal-illness
“The
promising results of these translational studies suggest we have reached the point where xenotransplantation should be studied in a systematic clinical trial to address remaining knowledge gaps”



The role of the EVA
and what we are trying to accomplish
Dimitrios Karnabatidis, Konstantinos Katsanos, and Panos Kitrou (University of Patras, Patras, Greece), the directors of the Endo Vascular Access (EVA) meeting, together write about their upcoming meeting (14–15 June, Patras, Greece), discussing what they hope to accomplish through the meeting, what attendees can expect at this year’s event, and the importance of collaboration between societies.
“Paideia” is the Greek term, since ancient times, defining education. A process not limited to learning but expanding to the deep understanding of things and the holistic approach of acquiring knowledge. This has been the goal of the EVA meeting since it was first introduced in 2019 with an aim to improve the quality of care provided to end-stage kidney disease (ESKD) patients. What do we need to know about vascular access? What is new and interesting? What are we still missing? These are some of the questions we try to answer during the EVA meeting which takes place this year on 14–15 June in Patras, Greece. We try to do this by inviting a multinational, but most importantly, a multidisciplinary faculty. Interventional radiologists, transplant surgeons, vascular surgeons, nephrologists and interventional nephrologists are invited to provide their perspective on important topics in this demanding field.
During the EVA meeting the main trial updates will be discussed. Additionally, the characteristics of the upcoming guidelines will be presented. New European Society of Vascular Surgery (ESVS) vascular access guidelines, a standards of practice document on vascular access from the Cardiovascular and Interventional Radiological Society of Europe (CIRSE), and the upcoming Spanish vascular access guidelines, together with the new Brazilian vascular access guidelines will be on podium. Like every year, the meeting dedicates “The Way Ahead” session to new technologies and advancements in therapy and innovations. This is where all future projects are presented. Artificial intelligence, machine learning and
augmented reality are already part of medical training, diagnosis and decision making and during the EVA meeting, their role in vascular access will be discussed. Endovascular arteriovenous fistulas (endoAVFs)—the ability to create non-surgical AVFs—is a fundamental part of the meeting’s discussions.
This year, the directors put the “balloon-assisted maturation” concept under “the spotlight”. A procedure widely known, but possibly with evidence missing, will be discussed by a faculty of experts aiming for consensus rather than controversy. Ultrasound use in vascular access surveillance, as well as an intraprocedural decision-making tool, was a hot topic during the last EVA meeting and a Delphi initiative was taken. To that end, another session is also part of this year’s meeting. Since “endo” is a cornerstone of EVA, two sessions on endovascular procedures, one regarding interesting
(“amazing”) and another one regarding difficult (“morbidity & mortality”) are part of the programme, giving the opportunity for a case-based discussion. However, as in everyday practice, vascular access treatment is not only endovascular, but also surgical, which is why we
“It is the EVA meeting’s principle to create collaborations and alliances with societies and congresses which dedicate part, or all of their programme, to vascular access”
Panos Kitrou
also have a session focused on the surgical procedures improving vascular access outcomes.
EVA will be celebrating its 7th collaboration with the Vascular Access Society of Britain and Ireland (VASBI) this year. It is the EVA meeting’s principle to create collaborations and alliances with societies and congresses which dedicate part, or all of their programme, to vascular access. So far, Controversies in Dialysis Access (CiDA), Dialysis Access Synergy (DASy), Spanish Multidisciplinary Vascular Access Group (GEMAV), Pan Arab Interventional Radiology Society (PAIRS), Saudi Interventional Radiology Society (SIRS), and Symposium on Vascular and Endovascular Access in Nephrology (SAVE) have already been invited and presented their perspective. We look forward to further collaborating and increasing awareness for vascular access with all our present and future partners.
The EVA meeting directors would like to express their gratitude to the faculty supporting the meeting over the years, some of whom have been present from the inaugural event back in 2019, but also the new members taking part this year. We would also like to thank our sponsors for understanding the importance of a meeting dedicated to vascular access and seeing the benefit provided to the physicians but most importantly to patients, the improved quality of care and life of whom is the goal of what we do.

A single-centre, retrospective review has reported 13-year data confirming cryoablation as a “highly effective” treatment modality for solitary T1a renal cell carcinoma (RCC) with low complication and recurrence rates.
INTERVENTIONAL RADIOLOGY FELLOW
Ahmed Awad (The University of Texas MD Anderson Cancer Center, Houston, USA) presented these data at the recent Global Embolisation Oncology Symposium Technologies (GEST; 16–19 May, New York, USA).
Cryoablation has emerged as an “attractive treatment option” for small renal masses, Awad stated, due to “favourable” intermediate- and long-term outcomes and its subsequent inclusion in the National Comprehensive Cancer Network (NCCN) guidelines alongside thermal ablation techniques.
Investigating the long-term experiences of their centre, Awad described their review, which regarded adult patients with a confirmed histopathology of solitary RCC with tumours of less than 4cm who received percutaneous cryoablation between January 2008 and December 2021. Exclusion criteria included patients with a prior history of RCC, patients with RCC metastases at the time of ablation or patients found to have multiple renal metastases at the time of the procedure.
Awad noted that overall survival, local recurrence-free survival, disease-free survival, metastases-free survival, and cancer-specific-free
survival were each measured in this cohort. Of the 86 patients included in their cohort, 57 were male and 29 were female. The median age in this population was 69 years and the median size of RCCs treated was reported as 2.7cm. The most common subtype of RCC was clear cell carcinoma, making up 63% of patients, and 4.6% of patients had a grade 3 or higher complication rate, which Awad defined as the requirement of any kind of intervention.
The median overall survival rate following cryoablation was 10.3 years. At five-year follow-up, overall survival was 69%; “this stems from the fact that 60% of our population has another primary malignancy which confounded their overall survival”, Award reported. Local recurrence-free survival was 93.5%, five and 10 years disease-free survival was 91% and 84% at follow-up, respectively, and median disease-free
“Cryoablation provides us the ability to visualise the ablation zone and the opportunity for a more controlled and confident approach both when planning and executing the procedure”
survival was 7.8 years. Additionally, both metastases-free and cancer-specific-free survival were 100% at 10 years.
“Our results show that cryoablation is highly effective in treating T1a RCC. Our continued collection of long-term follow-up data will favour additional quality and survival outcomes,” Awad said. “Cryoablation provides us the ability to visualise the ablation zone and the opportunity for a more controlled and confident approach both when planning and executing the procedure.”
Following the presentation, session moderator Bradford Wood (National Institutes of Health [NIH] Center for Interventional Oncology, Bethesda, USA) commended Awad and his team at MD Anderson for their research efforts, stating that theirs is one of the “greatest experiences” of the use of cryoablation for T1a RCC to date. He added that “caveats” in the most recent NCCN guidelines “keep [interventional radiologists] out of the mix and keep patients from hearing that [cryoablation] is an option”, and he then congratulated Awad on the addition of their data to the growing body of evidence which supports the use of cryoablation in this pathology.

The SELECT (Semaglutide effects on heart disease and stroke in patients with overweight or obesity) trial has revealed the potential of semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist, in combating kidney function decline among overweight or obese individuals with established cardiovascular disease but without diabetes.
UNVEILING THE RESULTS AT THE 61ST EUROPEAN Renal Association (ERA) congress (23–26 May, Stockholm, Sweden), researchers presented the secondary analysis from the SELECT trial, a randomised trial comprising a participant pool of 17,604 individuals.
They stated that experts believe the study’s results offer hope for those affected by obesity, a condition known to exacerbate the risk of kidney function decline and macroalbuminuria (abnormal amounts of the albumin protein in urine).
The study had an average follow-up of approximately 3.5 years and looked at patients who received a onceweekly subcutaneous injection of semaglutide (2.4mg). According to the authors, adverse kidney-related events were experienced by 22% fewer persons (1.8%) compared to those receiving placebo (2.2%). These events included death from kidney causes, initiation of chronic kidney replacement therapy, significant (≥50%) decline in kidney
function, or onset of persistent macroalbuminuria. The researchers highlighted semaglutide’s ability to prevent the onset of macroalbuminuria as a key factor in reducing the likelihood of kidney-related complications.
The study also assessed the impact of semaglutide on estimated glomerular filtration rate (eGFR). The findings indicated a significantly reduced decline in eGFR among semaglutide recipients compared to the placebo group, with the effect being more pronounced in participants with baseline eGFR below 60mL/ min/1.73m².
These results indicate the potential for semaglutide to particularly protect kidney function in individuals with a pre-existing kidney impairment, a press release says.
An important aspect of the study that was highlighted was that it found no increased risk of acute kidney injury (AKI) associated with semaglutide treatment, irrespective of baseline kidney function.
According to the researchers, over one billion people worldwide are affected by obesity and rates of obesity are rising significantly, having doubled among adult women (8.8–18.5%) and nearly tripled in adult men (4.8–14%) between 1990 and 2022. The total number of children affected by obesity in 2022 was nearly 160 million, compared to 31 million in 1990.

The authors stated that the reduction in urinary albumin-to-creatinine ratio (UACR) further substantiated the beneficial effect of semaglutide on kidney health, with a significant decrease observed in semaglutide-treated individuals compared to placebo. With semaglutide, there was a net 8.1% decrease in UACR in those with normal albumin levels at baseline, a 27.2% decrease in those with microalbuminuria (slightly raised albumin) at baseline, and a 31.4% decrease in those with macroalbuminuria at baseline relative, to placebo.
Helen M Colhoun (Institute of Genetics and Cancer, University of Edinburgh, Edinburgh, UK), lead study author, stated: “By addressing key markers of kidney health, semaglutide 2.4mg weekly may contribute to a significant reduction in the risk of kidney-related complications, including chronic kidney disease and end-stage renal disease. This could lead to improved management of comorbidities and, ultimately, enhance the quality of life for individuals with obesity.”
Continuing, she added that “the observed benefits in eGFR and UACR are particularly encouraging, suggesting potential for the enhanced management of kidney complications in the overweight and obese patients without diabetes. The findings also underscore the importance of continued research into the possible renal benefits of semaglutide and highlight its role as a promising therapeutic option in the multifaceted management of cardiovascular and renal health in this high-risk population.”

Outset Medical and US Renal Care announce collaboration aimed to grow home haemodialysis across USA
Outset Medical and US Renal Care have announced via press release a multiyear agreement to help accelerate home haemodialysis in the USA.
According to their announcement, studies have shown that patients with end-stage kidney disease (ESKD) are healthier both mentally and physically when completing dialysis at home. They also state that they are more likely to be employed and maintain more control of their daily activities.
Despite this, the press release states that only 3% of the US ESKD population currently performs home haemodialysis, in large part, they claim, due to historically complicated systems that made it “too difficult to undertake or sustain”. Under their multi-year agreement, US Renal Care can utilise Outset’s Tablo haemodialysis system as a home dialysis option throughout the 33 states in which it provides care. Patients dialysing with Tablo report that the system is easy to learn and operate in their home, according to Outset and US Renal Care. The companies hope that by expanding treatment options in the communities served by US Renal Care, they will be able to aid in meeting the growing demand of dialysis patients seeking treatment at home.
Tablo, which is indicated for use in both a hospital setting and at home, represents a significant technological advancement that transforms the dialysis experience for patients and operationally simplifies it for providers, according to the press release. The system requires access to tap water and a standard electrical outlet and can serve as a single enterprise solution that can be utilised “across the continuum of care”, as Outset frame it, allowing dialysis to be delivered anytime, anywhere and by anyone.
Commenting on the announcement, Leslie Trigg, chair and chief executive officer (CEO) of Outset Medical, stated: “Our collaboration with US Renal Care is an important step forward in providing dialysis patients with options for where, when and how they want to dialyse. Tablo was specifically designed to reduce the complexity of dialysis and help restore the identity and agency of patients who must dialyse to survive. We are pleased to partner with US Renal Care to advance this mission.”
Adding his thoughts, co-CEO at US Renal Care, Steve Nottingham, said: “We strive to provide patients with new and innovative solutions that deliver the best outcomes possible. We have seen success using the Tablo system in
our home haemodialysis programme, and with our multi-year agreement with Outset, can continue providing our patients and caregivers access to lifesaving dialysis treatment in an easyto-operate system, all in the comfort of their own homes.”
Healionics awarded US$1.25 million NIH grant to support commercialisation of novel vascular graft Healionics Corporation has announced via press release that it has been awarded a US$1.25 million Small Business Innovation Research grant by the National Heart, Lung, and Blood Institute (NHLBI), in order to support the commercialisation of its STARgraft vascular graft. This grant was awarded under the National Institutes of Health (NIH) Commercialisation Readiness Pilot Program, which provides additional technical assistance and late-stage research and development support that is not typically covered within small business awards to help products get to market.
According to Healionics, over 550,000 people in the USA suffer from kidney failure and require frequent dialysis. Its press release stated that the current methods of creating and maintaining regular bloodstream access for dialysis “are risky, unreliable and costly, driving a significant portion of the US$50 billion the USA spends each year to treat kidney failure”. A vascular graft, they add, is often implanted to create an access site with sufficient flow rate for dialysis, but existing grafts frequently fail due to occlusion and/or infection. Healionics’ STARgraft vascular graft, which it has based on proprietary synthetic biomaterial technology, is, the company adds, designed to resist both problems.
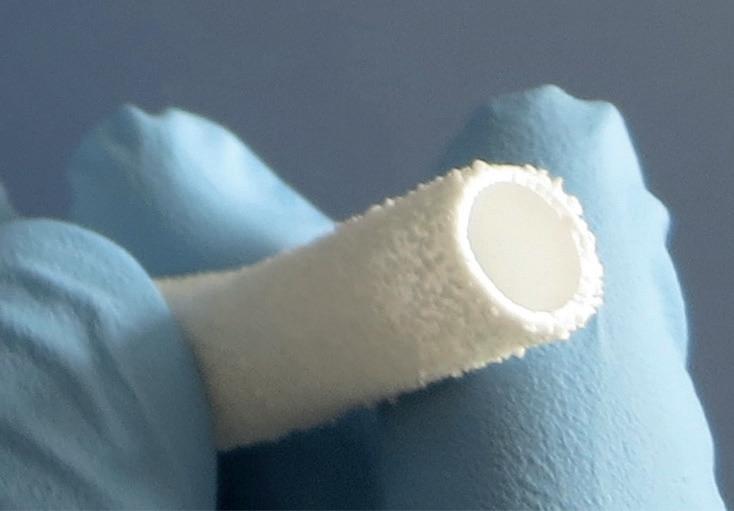
Commenting on this recent grant, Mike Connolly, Healionics’ chief executive officer (CEO) stated: “We appreciate NHLBI’s recognition of STARgraft’s potential to provide more reliable vascular access for dialysis patients. These funds will help us complete testing, pursue regulatory clearance, and prepare for market launch.”
First-ever combined heart pump and pig kidney transplant performed in USA NYU Langone Health has announced via press release that a team of surgeons have performed the first-ever combined mechanical heart pump and gene-edited pig kidney transplant surgery in a 54-year-old woman with heart and kidney failure—an
advancement that NYU Langone Health states “showcases the possibility and hope of modern medicine”.
The transplants were performed by the team in two stages: first, they surgically implanted the heart pump days before embarking on the geneedited pig kidney transplant, which also included the pig’s thymus gland to aid against rejection. Before undergoing the procedure, the patient, Lisa Pisano, faced both heart failure and end-stage kidney disease (ESKD) that required routine dialysis. She was not a candidate for heart and kidney transplants due to having multiple chronic medical conditions that reduced the likelihood of a positive outcome. Another contributing factor was the lack of suitable transplant organs for those who require them.
In the press release, NYU Langone Health states that nearly 104,000 people are on the waiting list for a transplant, with 89,360 of those waiting for a kidney. It also added that nearly 808,000 people in the USA have endstage kidney disease, but only about 27,000 were able to receive a transplant in 2023.

The hospital states that, to date, there have been no documented instances of anyone with a mechanical heart pump receiving an organ transplant of any kind, and that this is only the second known transplant of a geneedited pig kidney into a living person. It is also, they aver, the first instance of a genetically edited pig kidney being transplanted with the thymus combined.
Commenting on the success of the procedure, Pisano said: “All I want is the opportunity to have a better life. After I was ruled out for a human transplant, I learned I didn’t have a lot of time left. My doctors thought there may be a chance I could be approved to receive a gene-edited pig kidney, so I discussed it with my family and my husband. He has been by my side throughout this ordeal and wants me to be better.”
Sharing his thoughts on the combined operations, the lead transplant surgeon for this procedure Robert Montgomery (NYU Langone Transplant Institute, New York, USA) stated: “It is incredible to consider the scientific achievements that have led to our ability to save Lisa’s life, and what we are endeavouring to do as a society for everyone in need of a life-saving organ. This could not have been done without the dedication and skill of the many talented physicians, researchers, nurses, health administrators, and perioperative care teams at NYU Langone Health, and the numerous pioneers who came before us.”
New technique detects novel biomarkers for kidney diseases with nephrotic syndrome
A novel study, presented at the 61st European Renal Association (ERA)
congress (23–26 May, Stockholm, Sweden) and recently published in the New England Journal of Medicine (NEJM), has uncovered what researchers refer to as a “significant breakthrough” in the diagnosis and monitoring of kidney diseases associated with nephrotic syndrome, which is linked to kidney diseases such as minimal change disease (MCD), primary focal segmental glomerulosclerosis (FSGS), and membranous nephropathy (MN).

Using a hybrid technique, researchers identified anti nephrin autoantibodies as a reliable biomarker for tracking disease progression, opening new avenues for personalised treatment approaches. The study took place across Europe and the USA and, according to Tobias B Huber (University Medical Center HamburgEppendorf, Hamburg, Germany) et al, introduced a “novel approach combining immunoprecipitation with enzyme-linked immunosorbent assay (ELISA) to reliably detect anti-nephrin autoantibodies”.
Huber et al’s findings revealed that anti nephrin autoantibodies were prevalent in 69% of adults with MCD, and 90% of children with idiopathic nephrotic syndrome (INS) who had not been treated with immunosuppressive drugs. The authors of the study also highlight that the levels of these autoantibodies correlated with disease activity, suggesting potential as a biomarker for monitoring disease progression.
Researchers administered laboratorymade nephrin protein to mice, creating a condition akin to MCD in the mice, so as to further investigate the impact of nephrin immunisation on kidney function and disease. They found that this led to the phosphorylation of nephrin, as well as notable alterations in cell structure, which they state indicates the involvement of antibodies targeting nephrin in podocyte malfunction and nephrotic syndrome. Unlike other models necessitating multiple immunisations, the researchers found that this model induced swift disease manifestation with a single immunisation, even at low antibody concentrations.
Diagnosing these conditions has previously posed a challenge, due mainly to overlapping histological features and hesitancy to conduct invasive kidney biopsies, particularly in children. While anti nephrin autoantibodies have been observed in patients with MCD and FSGS, their precise role in the advancement of these diseases is, according to the study, not fully understood.
Commenting on the recenty published data, Huber, lead author of the study, said: “By providing insights into underlying mechanisms, these findings lay the groundwork for personalised interventions and pave the way for a new era of precision medicine for these complex conditions.
31 May–05 June
American Transplant Congress (ATC) 2024 Philadelphia, USA atcmeeting.org/
10–11 June
International Conference on Renal Medicine and Dialysis (ICRMD) Barcelona, Spain waset.org/renal-medicine-and-dialysisconference-in-june-2024-in-barcelona
11–13 June
UK Kidney Week 2024 Edinburgh, UK ukkw.org/
14–15 June
Endo Vascular Access (EVA) Meeting Patras, Greece evameeting.org/
19–22 June
Society for Vascular Surgery (SVS) Vascular Annual Meeting (VAM24) Chicago, USA vascular.org/vam-2024
14–18 September
Cardiovascular and Interventional Radiological Society of Europe (CIRSE) Annual Congress Lisbon, Portugal cirsecongress.cirse.org/


21–24 September
52nd EDTNA/ERCA International Conference Athens, Greece edtnaerca.org/conferences/conferencesathens-2024
26–27 September
Vascular Access Society of Britain & Ireland (VASBI) Annual Scientific Meeting 2024 Cardiff, UK vasbi.org.uk/annual-scientific-meeting-2024/
26–29 September
International Society for Peritoneal Dialysis (ISPD) Congress Dubai, United Arab Emirates ispd.org/dubai2024/






*Available for US and EU readers only **Available worldwide







