2 The Crawford Forum Quality in care is this year’s critical issue
4 NCD Data and discussion come at key moment
8 PAD
Toe and flow: The virtues of multidisciplinary care
12 Wellness Radiation safety session aims to address variability
16 IDEs Analysis poised to kickstart conversation on F/BEVAR outcomes

www.vascularspecialistonline.com
DAY ONE HIGHLIGHTS
ANOTHER YEAR IS IN THE books, and another jam-packed VAM schedule beckons. Here is a smattering of meeting highlights featured in the first edition of VS@VAM
First things first, Registration opens at 6 a.m. and remains so through 5 p.m. in the West Building, Level 3, Hall F1 Foyer. The VAM 2024 Opening Ceremony takes place at 8 a.m. in the West Building, Level 3, Skyline Ballroom. It will be followed by the William J. von Liebig Forum. This includes the coveted Resident Research Award presentation, our main cover story.
A full day of educational and scientific sessions awaits. The Vascular Quality Initiative (VQI) Annual Meeting completes its two-day run today in the West Building, Level 4. See story on p. 6.
The Firefighters of the OR: Intraoperative Vascular Emergencies Education session takes place at. 3:15 p.m. in the West Building, Level 1. See story on p. 8.
The Society for Vascular Nursing (SVN), Annual Conference opens today in the West Building, Level 1. For more, see article on p. 11.
RESIDENT RESEARCH AWARD

The Vascular and Endovascular Surgery Society (VESS) also has a slew of scientific sessions from 1:30 p.m. onwards in West Building, Level 1, as part of its summer gathering. See story on p. 13.—Bryan Kay
This year’s James S. T. Yao Resident Research Award winner looks at novel therapeutic target for nonhealing diabetic wounds. Kevin D. Mangum, MD, PhD, speaks to VS@VAM about his paper ahead of presenting the work at the 2024 Vascular Annual Meeting (VAM).
By Jocelyn Hudson
Drilling down on the roots of pathologic inflammation and wound healing challenges in diabetic patients
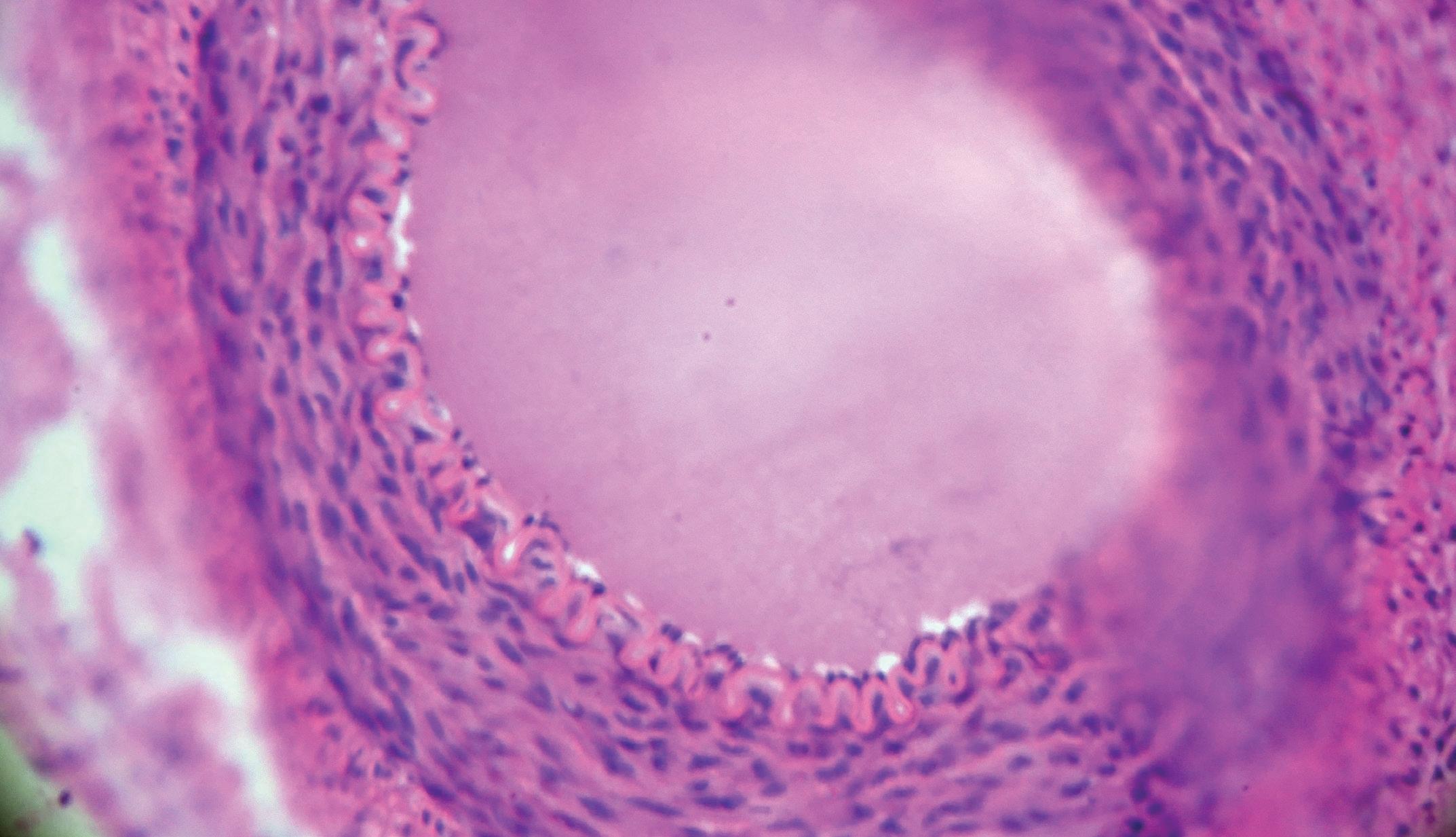
MANGUM, WHO IS A VASCULAR SURGERY
integrated resident at the University of Michigan in Ann Arbor, was announced as the winner of the James S. T. Yao Resident Research Award by the SVS Foundation for his paper ‘The STAT3-SETDB2 axis dictates NFKB-mediated inflammation in macrophages during wound repair.”
This award is designed to support emerging medical professionals exploring vascular disease biology and innovative translational therapies. It recognizes
unpublished, original scientific work in manuscript form that demonstrates publication quality. The recipient will present his research during the William J. von Liebig Forum, which takes place on the morning of Wednesday, June 19, at 8:10 a.m. (West Building, Level 3, Skyline Ballroom).
In the prize-winning paper set to be presented at this year’s Chicago gathering, Mangum sought
See page 2
THE OFFICIAL NEWSPAPER OF THE
In this issue: #VAM24 WelcometoTurntopage10forschedule
LIGHT
SPOT
WEDNESDAY, JUNE 19, 2024 | CONFERENCE EDITION 1
FROM THE COVER DRILLING DOWN ON THE ROOTS OF PATHOLOGIC INFLAMMATION AND WOUND HEALING CHALLENGES IN
to determine the transcription mechanisms regulating SETDB2 expression and activity in wound macrophages. “This is important given the critical and dynamic role that SETDB2 plays in regulating inflammatory gene transcription in wound repair,” he and colleagues at the University of Michigan write in their manuscript.
DIABETIC PATIENTS

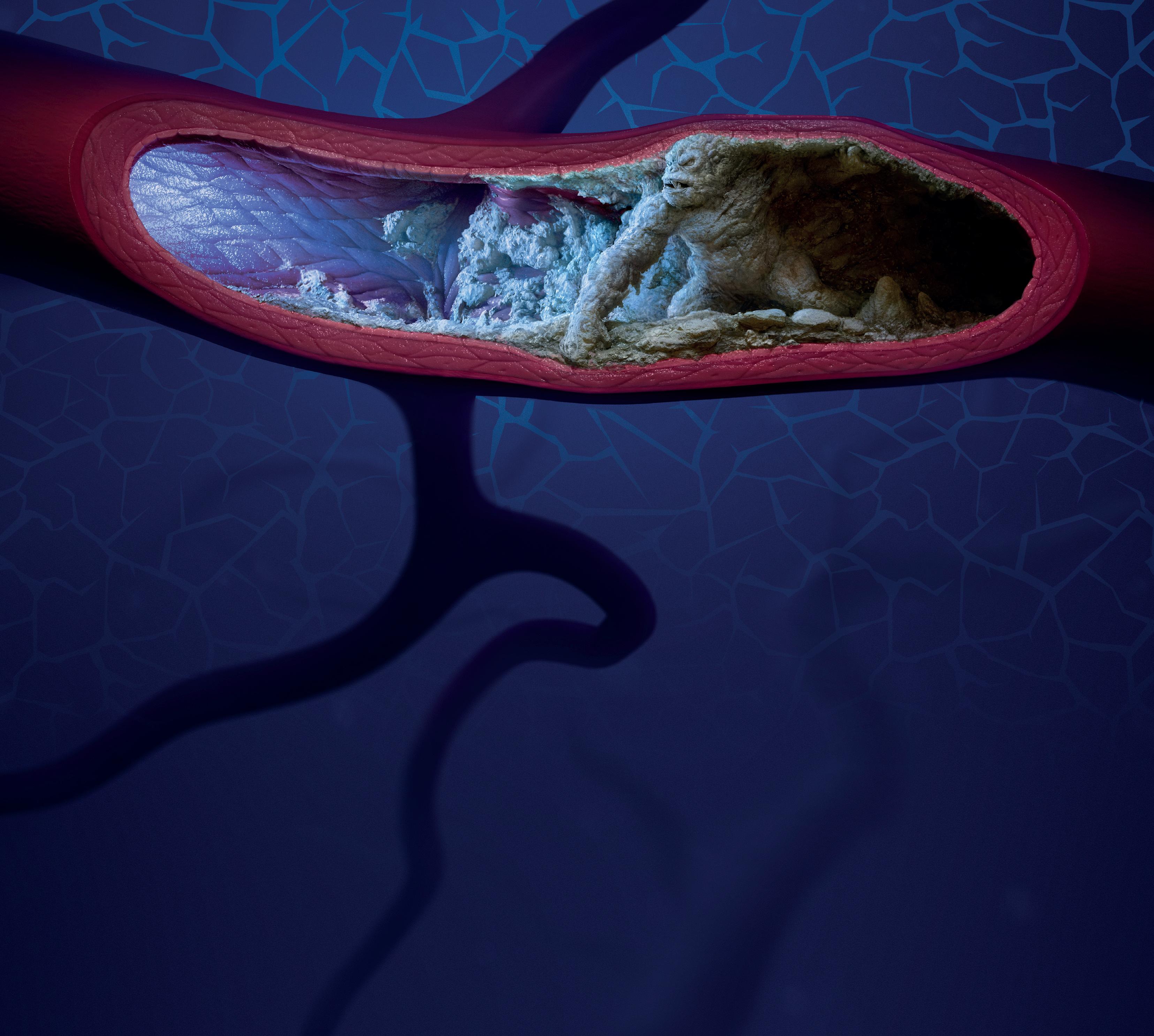
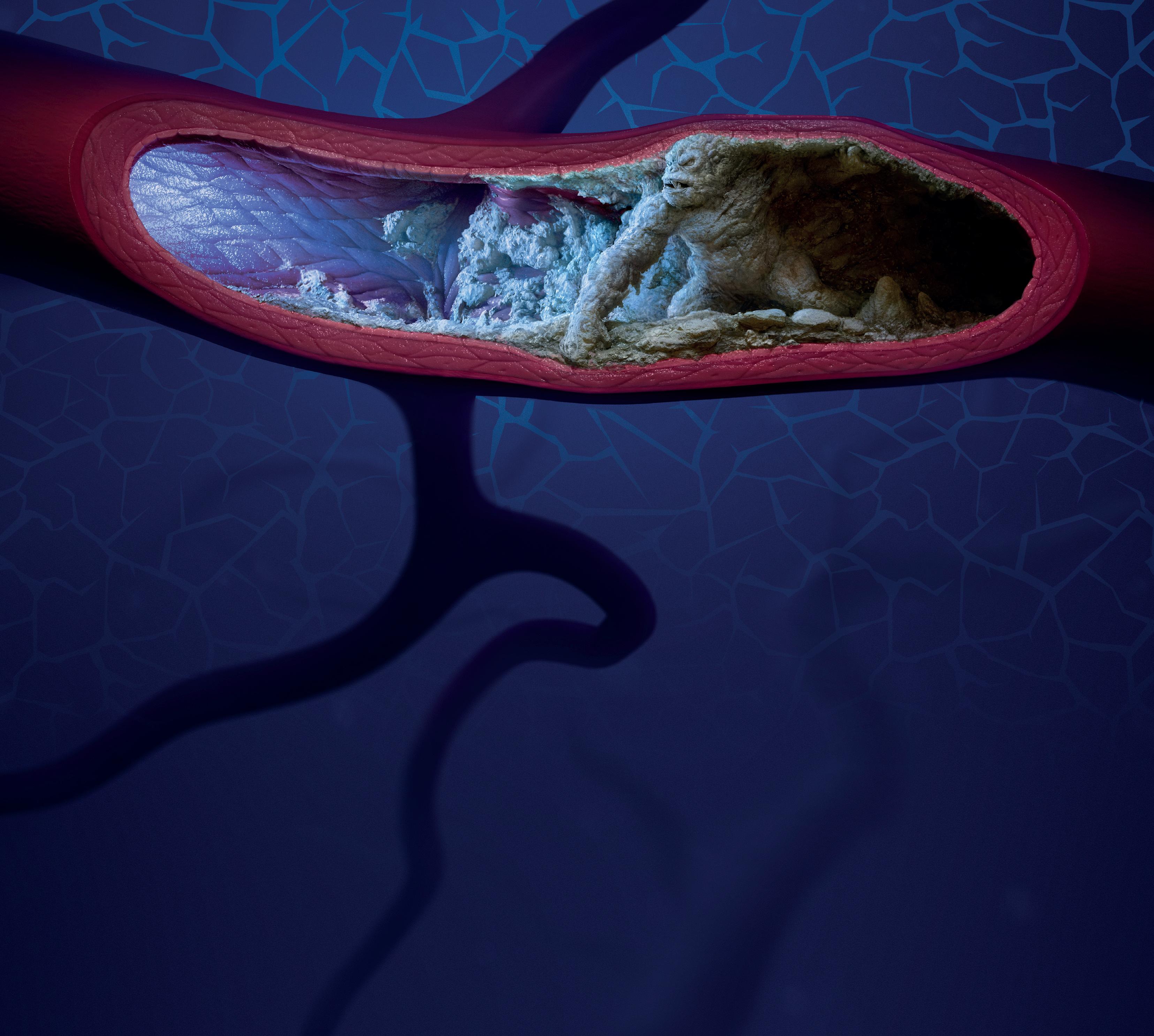
Mangum conducted his research under the mentorship of Katherine Gallagher, MD, vice chair of basic and translational science and professor of surgery in the Section of Vascular Surgery at the University of Michigan. Speaking to VS@VAM ahead of his presentation, Mangum outlined the evolution of his work. “Over the past two years in the Gallagher lab my research has expanded from epigenetic regulation of immune cells in the wound bed to transcriptional alterations in vascular smooth muscle cells in the arterial wall,” he explained. “We’ve been able to dissect specific DNA-protein and protein-protein interactions regulating macrophage phenotype in wound repair and have applied a similar approach to identifying central transcription mechanisms regulating other disease processes like atherosclerosis and hypertension, which will be the central focus of my research investigations after residency.”
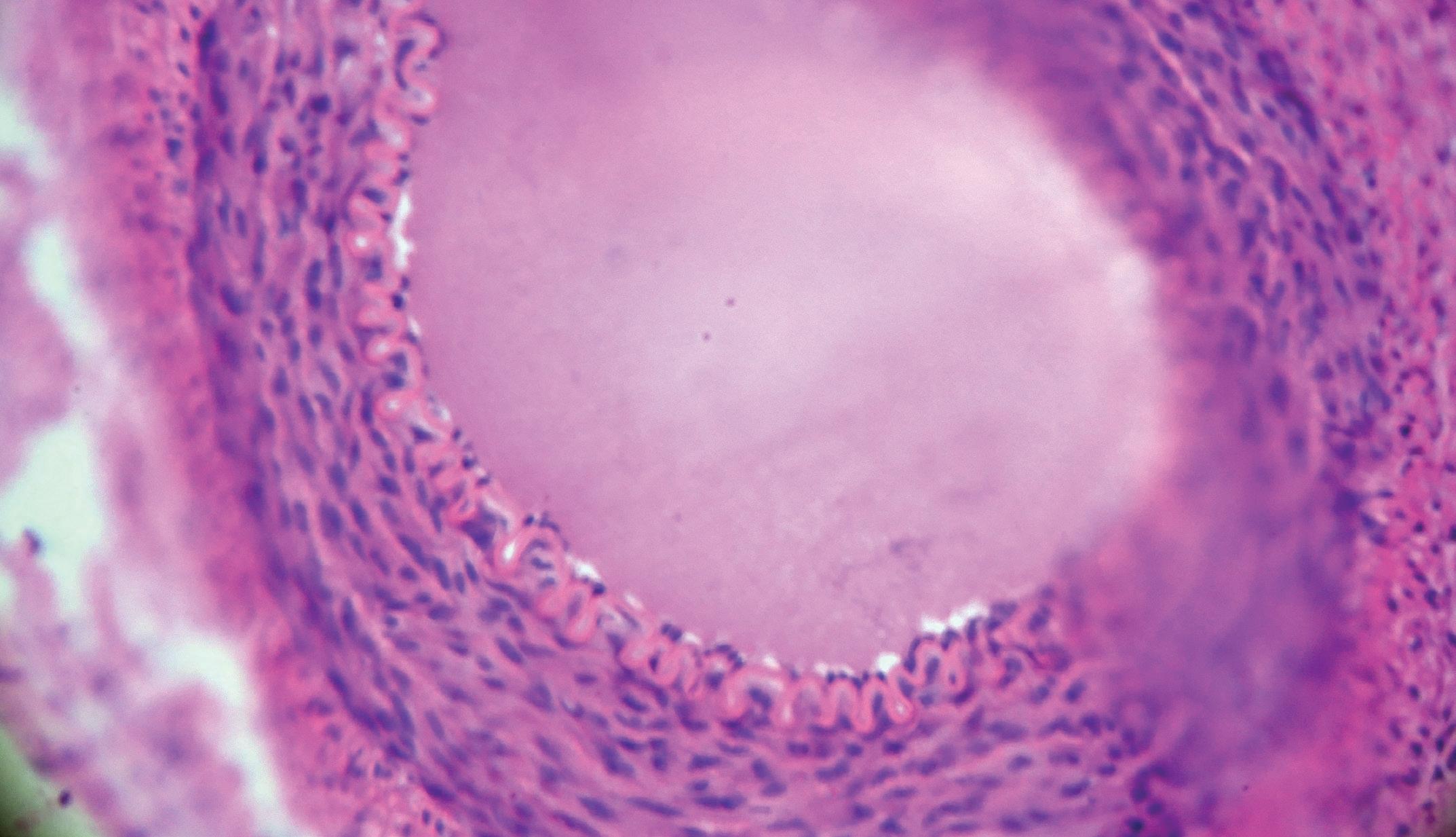
Focusing on the specifics of the paper, Mangum continued: “In our manuscript, we build on prior research studying the histone methyltransferase, SETDB2, which is expressed in macrophages and functions to repress inflammation. We’ve shown that macrophages from diabetic patients actually have lower amounts of SETDB2, which is one mechanism underlying pathologic inflammation and worse rates of wound healing in this population. My research really delves into the exact upstream transcription factors controlling SETDB2 expression, as well as those transcriptional regulators binding to SETDB2 protein to further modulate macrophage phenotype.”
In their research manuscript, Mangum and colleagues give further details about the investigation. “We identified that SETDB2 functions with NFKB to regulate the pro-inflammatory transcriptional repertoire in macrophages during wound healing by targeting NFKB-dependent gene regions,” they write, continuing: “We also demonstrate that the transcription factor, STAT3, regulates
Vascular-VP: ‘The blueprint for what a quality vascular program should look like’
SOME OF THE BENEFITS TO QUALITY care provision ensuing from participation in the American College of Surgeons (ACS) and SVS Vascular Verification Program (Vascular-VP) could be almost immediate.
This is among the insights set to feature during one of the most hotly-anticipated insertions on the VAM schedule.
SVS President-elect Matthew Eagleton, MD, who has made the program the subject of this year’s E. Stanley Crawford Critical Issues Forum on Wednesday, June 19 (11:15 a.m. in the West Building, Level 3, Skyline Ballroom), was speaking to VS@VAM ahead of the six-surgeon Crawford panel’s dissection of the Vascular-VP and discussion of why it matters to the improvement of quality in vascular care under the title, Quality Care Everywhere.
“I think at individual sites, you will even see the effects at the beginning of the process,” Eagleton says. “In the case of those involved in the inpatient program,
continued from page 1
SETDB2 via two pathways. First, in normal wound macrophages, STAT3 increases SETDB2 expression, which decreases inflammation. In contrast, by a separate mechanism, STAT3 also limits SETDB2 activity by physically binding to and preventing it from trafficking to inflammatory genes.” He explains the importance of this, stating: “Our work identifies a completely novel role for a well-known transcription factor, STAT3, in sequestering SETDB2 from NFkB and its associated gene regions. Strikingly, we found STAT3-SETDB2 binding was increased in diabetic macrophages, thereby leading to increased inflammation. This work has larger implications for transcriptional regulation because it identifies previously unknown functions of critical transcription factors in the regulation of downstream gene expression and cell phenotype.”
“By defining a novel STAT3-SETDB- NFKB axis,” they write in their conclusion, “we have identified several potential targets to treat non-healing diabetic wounds in a cell-specific and time-dependent manner.” For example, Mangum and colleagues state that immunomodulators during early wound healing to increase or activate STAT3 in order to increase SETDB2 expression may be useful. In addition, they write that inhibiting STAT3 relatively later in diabetic wound healing “may prove useful to increase SETDB2 localization to active inflammatory gene regions, thereby inhibiting pathologic inflammation and improving tissue repair.”
In terms of what is next for Mangum in the Gallagher lab, the vascular surgery resident commented that he and the team have “several exciting things” in the pipeline. “We’re mapping the specific protein domains mediating the interactions between SETDB2, STAT3 and NFKB in macrophages in hopes of developing a novel small molecular inhibitor of these interactions that can be used to treat diabetic wound healing in a cell-specific manner.” Mangum’s “ultimate goal” after completing residency, he told VS@VAM, is “to really understand how additional chromatin modifiers like SETDB2 are functioning in other cell types, specifically in vascular smooth muscle cells, to regulate vascular disease.”
the minute they start looking at—and questioning—what they are doing at their own organizations, they might see that there are lot of things that we take for granted, that we just assume may be happening, or in place, that many not be. So, with some of the changes that will need to occur at each location in order to meet verification status, there will be an immediate fix. When will we see that trickle down into measurable data changes that we can use for analysis of patient care, patient safety? That will probably take a couple of years until we see something like that.”
Eagleton’s panel includes five colleagues immersed in the conception and birth of the ACSSVS Vascular-VP. The contingent includes Clifford Y. Ko, MD, the director of the Division of Research and Optimal Patient Care at the ACS; Anton N. Sidawy, MD, a former SVS president; R. Clement Darling III, MD, another former SVS president; William P. Shutze, MD, current SVS secretary; and Dennis Gable, MD, from Texas Vascular Associates of Dallas and Plano.
FROM THE EDITOR Welcome to VAM 2024 !
By Malachi Sheahan III, MD
TO HELP US PREVIEW SOME OF the sessions of interest I reached out to the chairs of the SVS Program and Postgraduate Education Committees— Andy Schanzer, Jason Lee, Will Robinson, and Claudie Sheahan. I’ll let you guess which one did not respond to my emails. ANYWAY, here are some anticipated highlights:
● Wednesday at 5 p.m. will feature the first-ever keynote speaker. Karith Foster will present “Finishing the Journey to Inclusivity Through Belonging, Intention and Respect”
● New hands-on opportunities will be offered with Touchpoint and Crossroads
● For long-time VAM attendees like me, the educational programming has undergone a transformative change. This year there will be 26 sessions and there is truly something now for all members, regardless of practice type, clinical focus or academic focus. An emphasis on diverse perspectives means there will be over 200 faculty members this year
● A new audience polling and response system will be in place for Plenary Sessions 3 and 5, along with the My Worst Cases and RPVI sessions. I will be running it for Plenary 5. What could go wrong?
mean? How do they know a location they can go to receive care is considered a quality location? That’s what this forum is about—highlighting a program that was put together in conjunction with the ACS so that we have a verification program that can provide the blueprint for what a quality program should look like within an organization.”

Ko, who oversees quality programs at the ACS, will introduce how such programs have proven successful, says Eagleton. Sidawy, chair of the Vascular-VP Steering Committee, “has been instrumental in shepherding the relationship between the ACS and the SVS” in establishing a “functional program.”
Darling will discuss the inpatient program, on which he has been a leading figure, while Shutze will dissect efforts put in to get the outpatient version off the ground. Gable, meanwhile, will talk about his personal experience implementing the Vascular-VP on his own vascular surgery service line.
● The RPVI content will be a certified course under the APCA for certification and recertification
● The SVSConnect@VAM will be held at Soldier Field in Chicago. We can see the turf where all the legendary Bears quarterbacks played (Trubisky! Cutler! Grossman!!!)
● In addition to long-term partner VESS, the ESVS, AVF and WFVS will all be participating
Remember to pick up your daily copy of VS@VAM for in-depth previews of the many scientific and social options being offered up this year. There are three issues of the newspapers covering the four days of VAM programming. Finally, a reminder that VAM 2025 will be in New Orleans.
Spoiler—you will NOT need to pack a jacket.
“One of the things we always try to achieve in vascular surgery is to provide patients with quality care,” explains Eagleton. “For the public, what does that
“We are using this as an opportunity to educate our members about these programs, why it may be important to them and how can they get involved in utilizing them best in order to improve the quality at their locations.”—Bryan Kay
MALACHI SHEAHAN III is Vascular Specialist medical editor.

2 VS@VAM | Wednesday, June 19, 2024
CRAWFORD FORUM
Kevin D. Mangum
Matthew Eagleton
Malachi Sheahan III
You’re invested. So are we. UC202307996 IE ©2024 Medtronic. All rights reserved. Medtronic and the Medtronic logo are trademarks of Medtronic. All other brands are trademarks of a Medtronic company. 05/2024 Aortic support when and where it matters. Strength in products. Strength in evidence. Technical expertise. 800,000+ Patients treated worldwide Learn more at medtronic.com/aortic
DATA AND DISCUSSION FOREFRONT CAROTID SESSION AT ‘PIVOTAL MOMENT’
By Jocelyn Hudson
CONTEMPORARY MANAGEMENT
of carotid disease after the Centers for Medicare and Medicaid Services (CMS) carotid artery stenting (CAS) decision memo and prior to CREST-2 results will be the focus of an Education Session at VAM 2024.
In October, CMS released its final decision regarding NCD 20.7 covering CAS. The move was made to expand Medicare coverage for CAS to include patients who have symptomatic carotid stenosis of 50% or greater and asymptomatic carotid stenosis of 70% or greater.
The timing of the decision has been a point of contention, having been made
CAROTID
DISEASE
prior to the 2026 expected release date of CREST-2 results. This trial will compare intensive medical management alone to intensive medical management plus revascularization with carotid endarterectomy (CEA) or transfemoral CAS (TF-CAS) in patients with high-grade stenosis.

The VAM 2024 session, set for the afternoon of Friday, June 21, at 1:30 p.m. (West Building, Level 1), will see Pallavi Manvar-Singh, MD, of the Zucker School of Medicine at Hofstra/Northwell Health in Jericho, New York, and Peter Schneider, MD, of the University of California San Francisco in San Francisco, California, moderate eight podium presentations and extensive discussion.
“The management of carotid bifurcation occlusive disease is a core competency for vascular surgeons and vascular surgery continues to be vital to the development of optimized therapy for this disease process,” Manvar-Singh and Schneider told VS@ VAM ahead of the Chicago meeting.
They continued: “Vascular surgeons are experts in the disease process, the longitudinal management of these patients, and different methods of carotid
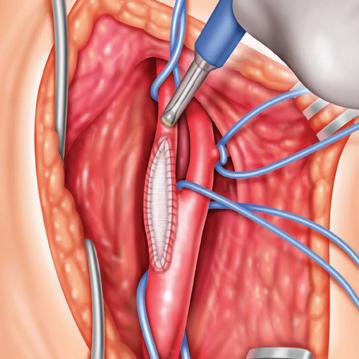
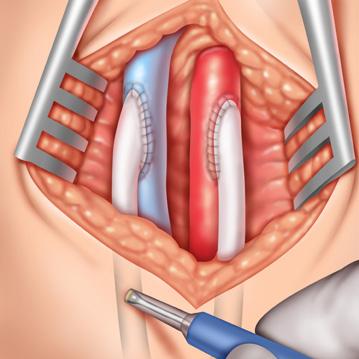
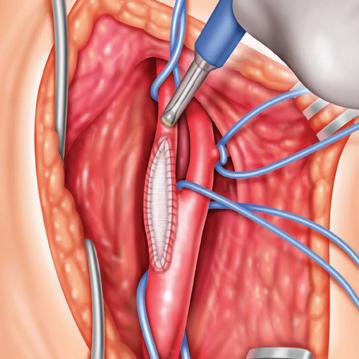
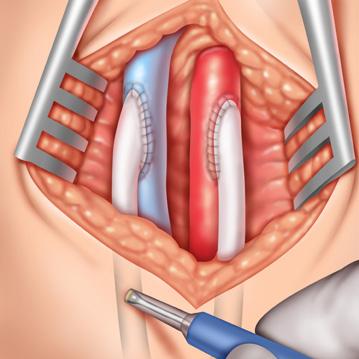
CEA vs TCAR: surgeons should be familiar with both procedures and ‘collaborate as needed’
By Jamie Bell
WHEN IT COMES TO THE ONGOING DEBATE OF carotid endarterectomy (CEA) versus transcarotid artery revascularization (TCAR) in the treatment of carotid artery stenosis, operators should be comfortable and maintain experience with both of these procedures—and “collaborate as needed.” That is the ultimate finding of a registry analysis set to be presented during today’s Plenary Session 1: William J. von Liebig Forum ( 8:10–9:45 a.m. in the West Building, Level 3, Skyline Ballroom).
The analysis in question will be delivered by Andrea Alonso, MD, a research resident at Boston University in Boston, on behalf of lead author Jeffrey J. Siracuse, MD, professor of surgery and radiology at Boston University, and colleagues. “Our study observed an inverse relationship between the proportion of a procedure—either TCAR or CEA—conducted by a surgeon, and the rate of postoperative stroke, with surgeons performing the lowest proportion having the highest stroke rates,” Alonso told VS@VAM. “Our data also suggest that, among surgeons with a more balanced practice, there continues to be a low rate of stroke. To minimize postoperative stroke risk, we conclude that surgeons who offer both types of carotid revascularization procedures maintain a balance. We also suggest collaboration in challeng-
repair when it is indicated, whether by CEA or stent.”

The pair further remarked that therapy for both symptomatic and asymptomatic carotid disease “is well studied but remains quite dynamic” and that “updates on important developments will help us predict how the field is evolving.”
“It is a pivotal moment in the evolution of carotid disease management,” they commented. “Any one of these developing issues could substantially shape our future practices. The recent NCD is an endorsement of stent-based therapy by CMS.
“The pressure to reduce treatment and avoid screening for critical asymptomatic stenosis is increasing. The CREST-2 trial is nearly enrolled. TCAR [transcarotid artery revascularization] is nearing 100,000 procedures in the US., and most vascular practices have incorporated it as an option for repair.
“The growth of stroke centers will undoubtedly influence our practices, but we don’t yet know how. For all these reasons, an update on carotid disease management is essential to inform our
ing cases, leveraging the diverse expertise within a practice, to reduce stroke risk.
“We believe that this can be done effectively in the preoperative setting while evaluating challenging cases and with advanced coordination with colleagues to assist in key parts of the operation. This step takes insight from the lead surgeon to recognize the surgical techniques that they may require more assistance with at that stage in their practice, as well as camaraderie within the practice group.”
According to the authors, TCAR adoption among surgeons has been variable—many still perform more traditional CEAs, while others have shifted mostly to TCAR in their practice. Researchers therefore set out to evaluate the association between surgeons’ relative volumes of CEA to TCAR, and
perioperative outcomes, via analyses of the Vascular Quality Initiative (VQI) CEA and carotid artery stenting (CAS) registries from 2021–2023.
Across both registries, participating surgeons were categorized in the following CEA/TCAR volume percentage ratios: 0–25/76–100 (majority TCAR); 26–50/51–75 (more TCAR); 51–75/26–50 (more CEA); and 76–100/1–25 (majority CEA). Primary outcome measures for the analysis consisted of rates
treatment plans.”
Opening the session, Caitlin Hicks, MD, of Johns Hopkins University in Baltimore, Maryland, will deliver a review of the NCD, before Warren J. Gasper, MD, of the University of California San Francisco, shares an update on the CREST-2 trial.
Mark F. Conrad, MD, MS, of Steward Health in Brighton, Massachusetts, is due to speak on asymptomatic disease, after whom Sonya S. Noor, MD, of Gates Vascular Institute in Amherst, New York, will address the question, “Should vascular surgeons be involved in stroke centers?”
After some discussion time, the focus will turn to data. Sean P. Lyden, MD, of the Cleveland Clinic in Cleveland, Ohio, will present new data covering TF-CAS and new technologies since the last NCD, and Gregg S. Landis, MD, of the Zucker School of Medicine at Hofstra/Northwell will outline the totality of data available supporting TCAR.
The final two presentations of the session before another round of discussion will cover technique and training, respectively, from Mazin I. Foteh, MD, of Cardiothoracic and Vascular Surgeons in Dallas, Texas, and Jeffrey Jim, MD, of Minneapolis Heart Institute at Abbott Northwestern Hospital in Minneapolis, Minnesota.
of perioperative ipsilateral stroke, death, cranial nerve injury (CNI) and return to the operating room (RTOR) for bleeding. The researchers found that there were 50,189 patients who underwent primary carotid revascularizations (CEA, 64.3%; TCAR, 35.7%), also noting that—on average—CEA patients were younger (71.1 vs. 73.5 years, p<0.001), with less coronary artery disease and diabetes, fewer symptomatic cases, and lower antiplatelet and statin use (all p<0.001). Meanwhile, they observed that TCAR patients had lower rates of endstage renal disease, smoking and obesity (all p<0.001).
Postoperative stroke after CEA was found to be significantly impacted by relative surgeon volume ratio (p=0.04), with “majority TCAR” surgeons having higher rates of postoperative ipsilateral stroke (odds ratio [OR], 2.12; 95% confidence interval [CI], 1.15–3.9; p=0.02). Alonso, Siracuse and colleagues have also reported that there was a trend indicating a higher stroke rate after TCAR in “majority CEA” surgeons— however, this did not reach statistical significance. In addition, they saw no association between relative volumes and perioperative death, CNI or bleeding-related RTOR for either procedure. It is based upon these findings that the researchers conclude that relative surgeon ratios of CEA versus TCAR do appear to influence perioperative stroke rates when it comes to CEA, emphasizing the need for surgeons to be familiar with both procedures and utilize collaboration.
“Our study observed an inverse relationship between the proportion of a procedure— either TCAR or CEA—conducted by a surgeon, and the rate of postoperative stroke”
ANDREA ALONSO
4 VS@VAM | Wednesday, June 19, 2024
NCD
Pallavi Manvar-Singh
Peter Schneider
Carotid rescularization: CEA and TCAR
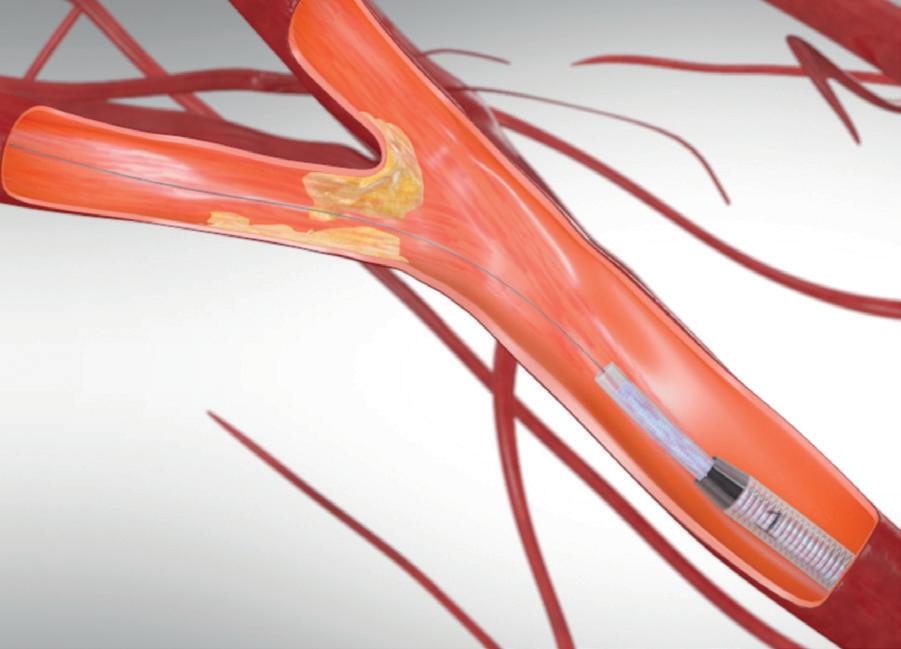
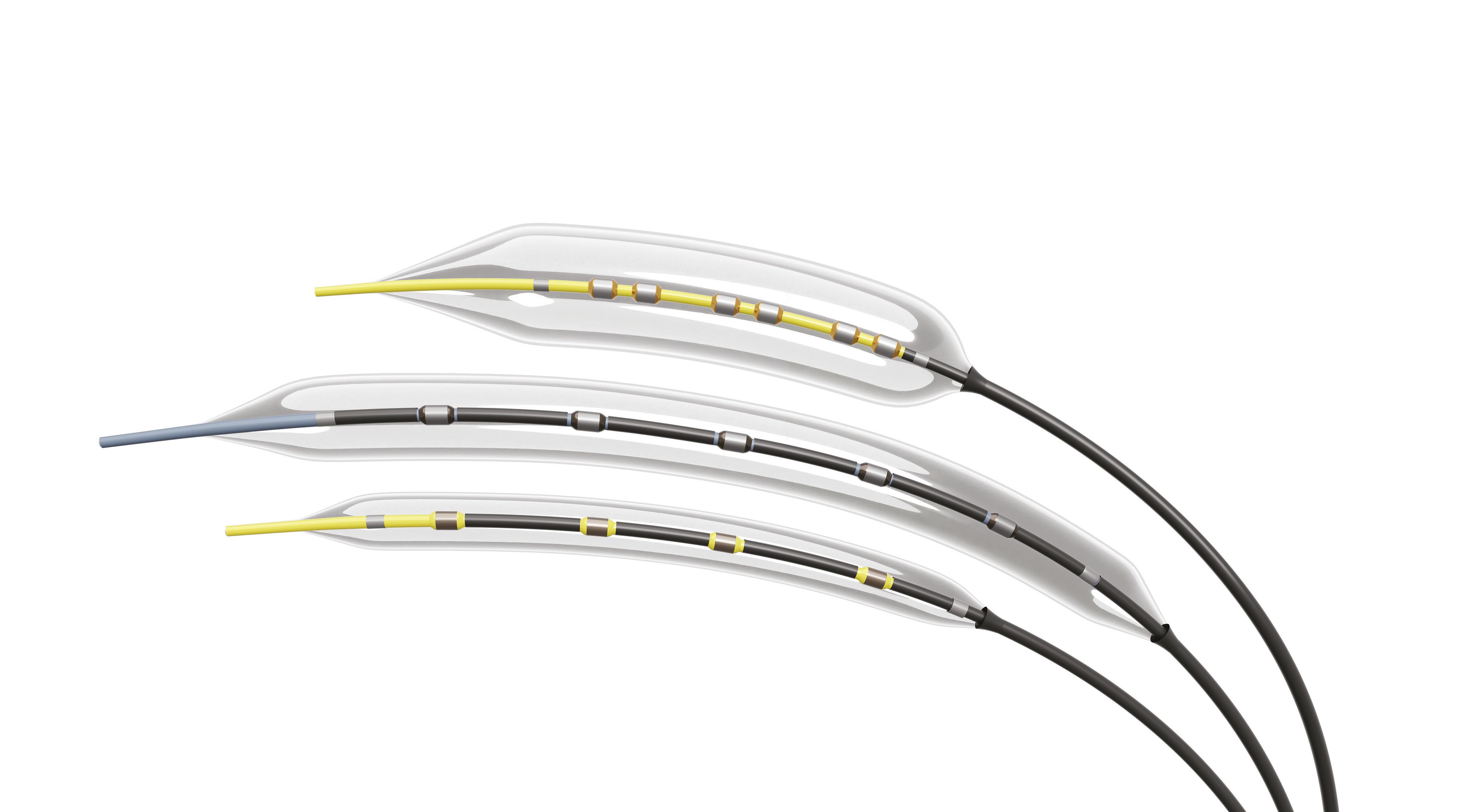
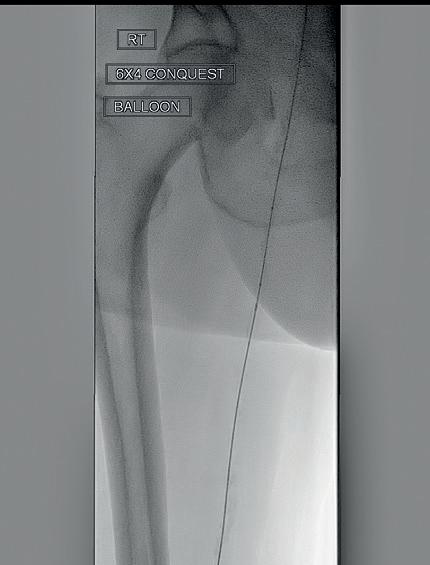
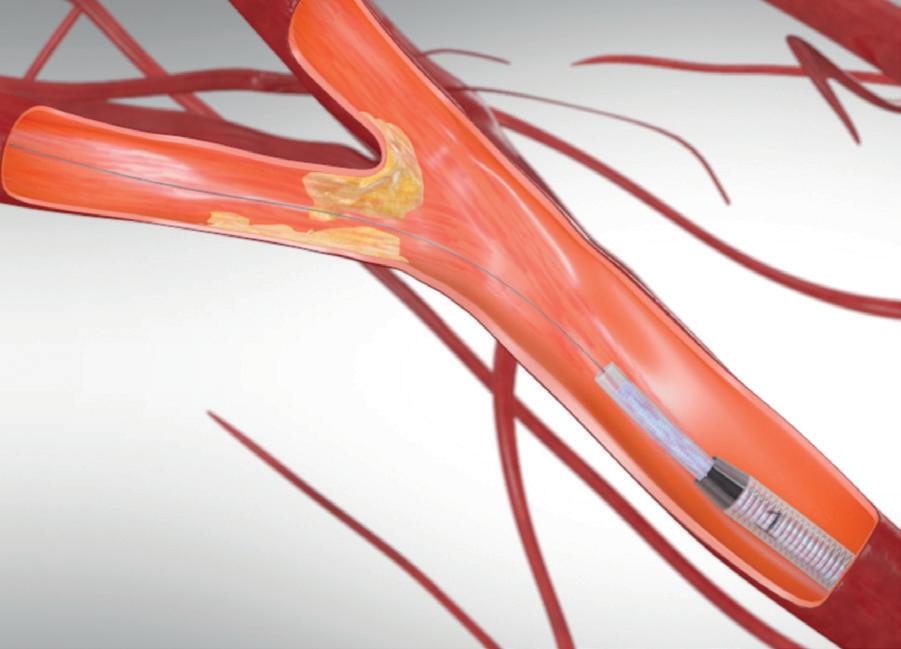
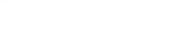
PERIPHERAL IVL
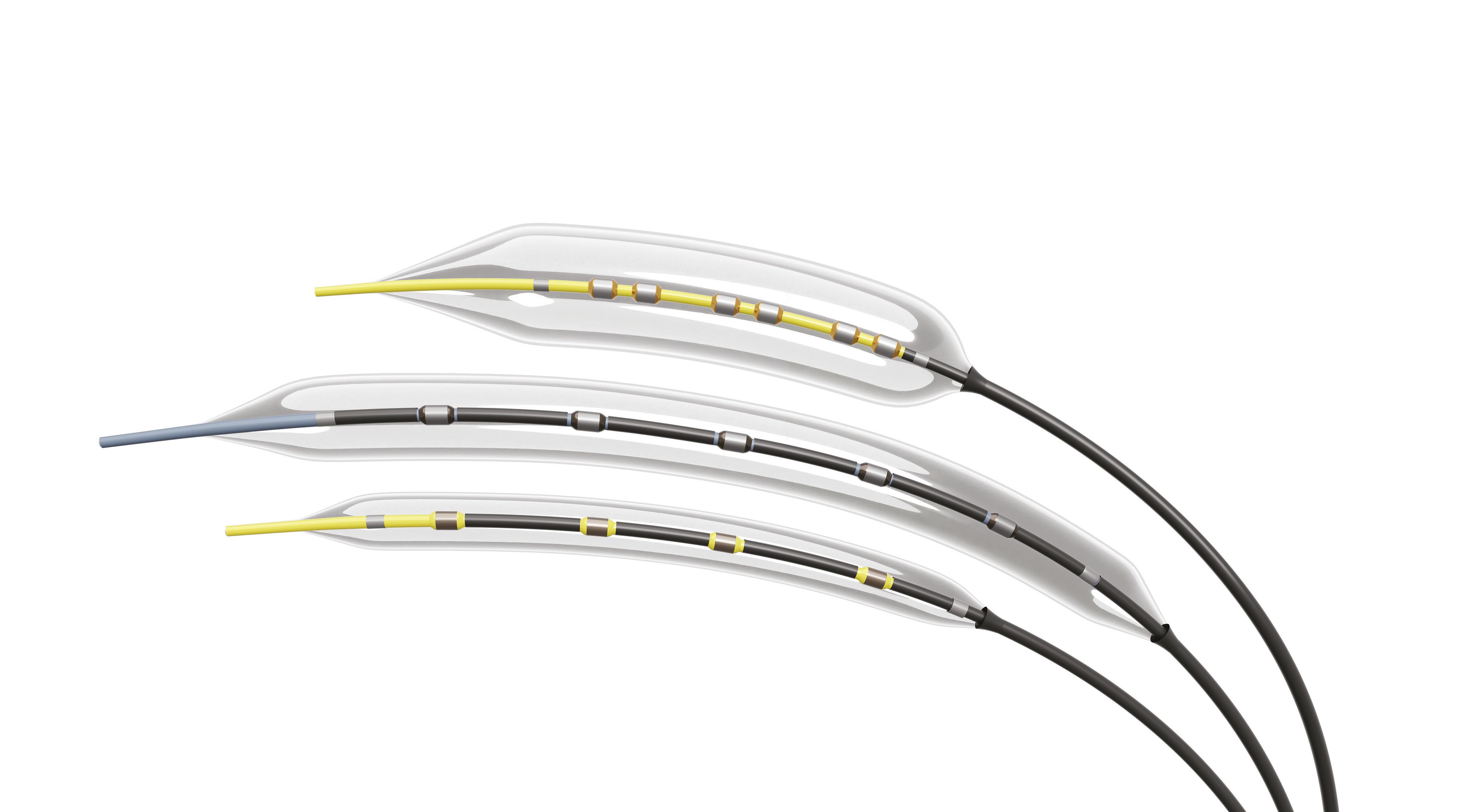

Shockwave Peripheral IVL: Reliably safe. Predictably effective. Backed by real-world and level one evidence, Shockwave IVL modifies both superficial and deep calcium. Designed for the iliacs, fem-pop and below-the-knee arteries, these purpose-built devices come in sizes that allow you to treat calcium at any level. So you can count on affecting outcomes for the better.
Peripheral Important Safety Information
In the United States: Rx only.
Indications for Use—The Shockwave Medical Intravascular Lithotripsy (IVL) System is intended for lithotripsy-enhanced balloon dilatation of lesions, including calcified lesions, in the peripheral vasculature, including the iliac, femoral, ilio-femoral, popliteal, infra-popliteal, and renal arteries. Not for use in the coronary or cerebral vasculature.
Contraindications—Do not use if unable to pass 0.014” (M5, M5+, S4) or 0.018” (L6) guidewire across the lesion-Not intended for treatment of in-stent restenosis or in coronary, carotid, or cerebrovascular arteries.
Warnings—Only to be used by physicians who are familiar with interventional vascular procedures—Physicians must be trained prior to use of the device— Use the generator in accordance with recommended settings as stated in the Operator’s Manual.
Precautions—use only the recommended balloon inflation medium—Appropriate anticoagulant therapy should be administered by the physician—Decision regarding use of distal protection should be made based on physician assessment of treatment lesion morphology.
Adverse effects–Possible adverse effects consistent with standard angioplasty include–Access site complications –Allergy to contrast or blood thinner–Arterial bypass surgery—Bleeding complications—Death—Fracture of guidewire or device—Hypertension/Hypotension—Infection/sepsis—Placement of a stent—renal failure—Shock/pulmonary edema—target vessel stenosis or occlusion—Vascular complications. Risks unique to the device and its use—Allergy to catheter material(s)— Device malfunction or failure—Excess heat at target site. Prior to use, please reference the Instructions for Use for more
contraindications,
©2024 Shockwave Medical Inc. All rights reserved. SPL-70888 Rev A Learn more at ShockwaveMedical.com/Peripheral-IVL COUNT ON IT THE SOUND CALCIUM SOLUTION
information on indications,
warnings, precautions and adverse events. www.shockwavemedical.com/IFU
SVS, AVF BRING THE LATEST INNOVATIONS IN VENOUS DISEASE TREATMENT TO VAM
During the first day of VAM 2024, the Society for Vascular Surgery (SVS) and American Venous Forum (AVF) have co-sponsored a session on the latest innovations in the delivery of venous disease treatment. By
Brian McHugh
MADHAVI MEKA, MD, A CLINICAL associate professor at the University of Arizona School of Medicine and vascular surgeon at the Carl T. Hayden VA Medical Center in Phoenix, Arizona, and Faisal Aziz, MD, chief of vascular surgery at the Penn State Health Hershey Medical Center Heart and Vascular Institute in Hershey, Pennsylvania, are moderating a package of presentations (Wednesday, June 19 at 3:15–4:45 p.m. in the West Building, Level 1) focused on recognizing the various patterns of superficial venous reflux and management options, understanding what the most effective treatment for patients with iliac vein disorders is, and increasing knowledge of venous ulcer care and the influence of health inequities.
“Venous disease is more common than peripheral arterial disease [PAD], affecting nearly 30 million people in the U.S. alone,” Meka told VS@VAM. “Twenty-five percent of the global adult population are afflicted with venous reflux disease or a more serious form of venous disease called chronic venous insufficiency. The spectrum of disease ranges from spider veins, telangiectasia, varicose veins, and venous ulcers.”
The initial section focuses on superficial venous disease. Presenting first will be Glenn Jacobowitz, MD, from NYU Health in New York City, who will be discussing thermal ablation options; Karem Harth, MD, from Case Western Reserve University School of Medicine in Cleveland, is up next and will present
on non-thermal ablation options; Sherry Scovell, MD, from Massachusetts General Hospital in Danvers, Massachusetts, will finish the superficial venous disease section by discussing sclerotherapy techniques.
The second section focuses on iliac venous stenosis. Arjun Jayaraj, MBBS, from the RANE Center for Venous and Lymphatic Diseases at St. Dominic’s in Jackson, Mississippi, will present on intravascular ultrasound (IVUS) and its importance for deep venous interventions. This will be followed by Misaki Kiguchi, MD, from MedStar Heart and Vascular Institute in Washington, D.C., who will discuss stenting below the inguinal ligament.
The final section of the SVS-AVF session covers venous leg ulcerations (VLUs), starting with William A. Marston, MD, from University of North Carolina at Chapel Hill, North Carolina, who will be presenting on whether deep or superficial interventions should be tackled first.
Meanwhile, Anil Hingorani, MD, from NYU Langone in Brooklyn, New York, will present next on the role of perforator veins and interventions in the context of VLUs.
And finally, the last presentation before the panel discussion will be by Leigh Ann O’Banion, MD, from UCSF Fresno in Fresno, California, who will be discussing health disparities in patients with advanced venous disease.
Enhancing vascular care: VQI Annual Meeting set to dig into data and progress
By Marlén Gomez
THE EIGHTH VASCULAR QUALITY INITIATIVE (VQI) Annual Meeting taking place over Tuesday, June 18, and Wednesday, June 19 (8–5 p.m. in the West Building, Level 4) features a series of sessions focused on the SVS Patient Safety Organization (PSO) reporting and analytics, updates to the Fivos pathways systems, progress in data integrity audit programs, and more.
One of Wednesday’s sessions will highlight the latest advancements and findings in vascular care quality and
“Despite advancements in the techniques and procedures, there has been a paucity of literature delineating outcomes, patient satisfaction and improvement in lifestyle,” Meka states.
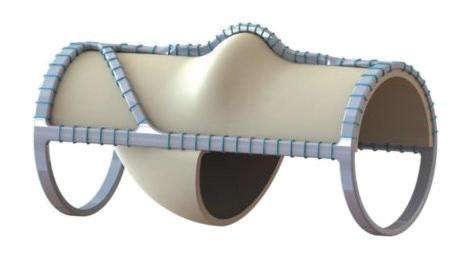
Elsewhere in venous disease developments, on Friday, June 21’s Plenary Session 5 (8–9:30 a.m in the West Building, Level 3, Skyline Ballroom), Cassius Iyad Ochoa Chaar, MD, from Yale School of Medicine in New Haven, Connecticut, on behalf of co-authors Claire L. Griffin, MD, Eric S. Hager, MD, Matthew R. Smeds, MD, and March H. Glickman, MD, will discuss the impact of the VenoValve device (EnVVeno Medical) on venous ulcer healing in patients with deep venous reflux.
The presentation features data from the multicenter Surgical Antireflux Venous Valve Endoprosthesis (SAVVE) trial, which highlights the impact of the VenoValve device after one year of implantation for patients treated for venous ulcers.
of-care therapy. Patient characteristics were recorded and the revised venous clinical severity score (rVCSS), wound surface area, venous ulcer healing, and improvement defined by the reduction of the area was assessed at the preoperative baseline and at three months, six months and one year. During Chaar’s VAM presentation, updated data on all patients who have reached oneyear follow-up will be presented.
The latest results show the trial includes 75 total patients, 41 of whom were treated for venous ulcers and were the focus of the report.
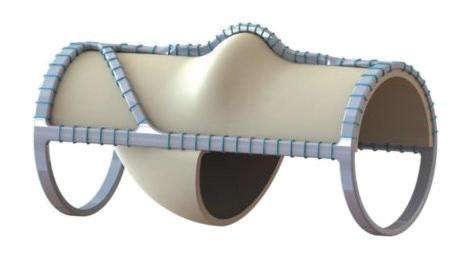
The patient population was majority male (78%) and White (93%), with a mean age of 64.
The SAVVE trial enrolled patients with deep venous reflux and symptomatic advanced venous disease with a clinical, etiological, anatomical, and pathophysiological (CEAP) score of C4b–C6, despite standard-
“Despite advancements in the techniques and procedures, there has been a paucity of literature delineating outcomes, patient satisfaction, and improvement in lifestyle”
MADHAVI MEKA
the significant progress of the VQI. Attendees will gain insights into the initiative’s latest improvements and newly implemented measures aimed at enhancing vascular healthcare.
The VQI, a program dedicated to improving the quality of vascular healthcare by providing a robust data collection and analysis platform, has been instrumental in helping institutions identify best practices and improve patient outcomes. This year’s sessions will cover several critical areas of development within the initiative.
One of the highlights of the VQI Spring 2023 reporting cycle is the introduction of new measures to address smoking among patients undergoing vascular procedures. These measures include tracking preoperative smoking rates and assessing the success of smoking cessation efforts post-procedure. The initiative emphasizes the crucial role of smoking cessation in reducing morbidity and mortality associated with vascular diseases.
During the sessions, faculty will review data on smoking cessation rates before and after the distribution
Most of the venous ulcers (70.7%) had a duration of more than one year, while only five patients (12.2%) had venous ulcers that had a duration of less than one month. The results demonstrate high ulcer healing and reduction of ulcer surface area in a group of challenging patients, the authors will report.
“VenoValve implantation provides sustainable improvement in venous ulcer healing that continues for a year after surgery in patients who have exhausted all current standard-of-care treatments,” the authors will conclude.
Earlier this year at the Charing Cross (CX) International Symposium in London, England, David Dexter, a vascular surgeon at Sentara Vascular Specialists in Norfolk, Virginia, declared: “The surgical challenges of repairing deep venous reflux have been present for more than a generation. It is worth reflecting on the fact that this new technology has made the majority of patients vastly better.” He was speaking as he presented podium-first efficacy results from the SAVVE trial.
“These patients are the most severe of the severe,” Dexter said. He described that the “vast majority—around 60%—of these patients have active ulcers.”
of an infographic for vascular surgeons that details the latest evidence-based strategies for smoking cessation. This evaluation aims to determine the impact of the infographic and other intervention strategies on patient outcomes.
The VQI meeting will also cover the “5 As” approach to smoking cessation: Ask, Advise, Assess, Assist and Arrange follow-up. This method highlights the importance of surgeons providing brief yet effective counseling to encourage smoking cessation among their patients.
Other notable sessions at the meeting include PSO quality updates, Utilizing VQI to Foster Quality Improvement and How to Celebrate Successes, ACS/ SVS Vascular Verification Program: From Application to Site Visit: The Power of Quality Campaign, and the presentation of 3-Star Participation Awards, as well as poster competition winners.
For more information about the VQI and its various projects, visit vascular.org/VQI24


6 VS@VAM | Wednesday, June 19, 2024
QUALITY
INNOVATION
VenoValve
One Laser. Multiple Capabilities.
DUAL IMPACT
Fracture medial arterial calcium while debulking intimal morphologies
BELOW THE KNEE
Proven success in below-the-knee arteries, where calcium tends to be more prevalent2
SAFETY
Safety at the forefront. Treat with confidence by minimizing the risk of embolization and dissection3


Caution: Federal (USA) law restricts the use of the system by or on the order of a physician. Refer to Directions for Use and/or User Manual provided with the product for complete Instructions, Warnings, Precautions, Possible Adverse Effects and Contraindications prior to use of the product. INDICATIONS FOR USE
The Auryon Atherectomy System and Auryon Atherectomy Catheters with aspiration are indicated for use as atherectomy devices for arterial stenoses, including in-stent restenosis (ISR), and to aspirate thrombus adjacent to stenoses in native and stented infra-inguinal arteries.
The Auryon Atherectomy System and Auryon Atherectomy Catheters without aspiration are indicated for use in the treatment, including atherectomy, of infra-inguinal stenoses and occlusions.
1. Rundback et al. Treatment effect of medial arterial calcification in below-knee after Auryon laser atherectomy using micro-CT and histologic evaluation, Cardiovascular Revascularization Medicine, 2023,ISSN 15538389, https://doi.org/10.1016/j.carrev.2023.06.027.
2. Paul D. Bishop, Lindsay E. Feiten, Kenneth Ouriel, Sean P. Nassoiy, Mircea L. Pavkov, Daniel G. Clair, Vikram S. Kashyap, Arterial Calcification Increases in Distal Arteries in Patients with Peripheral Arterial Disease, Annals of Vascular Surgery, Volume 22, Issue 6, 2008, Pages 799-805, ISSN 0890-5096, https://doi.org/10.1016/j.avsg.2008.04.008.
3. Rundback J, Chandra P, Brodmann M, et al. Novel laser-based catheter for peripheral atherectomy: 6-month results from the Eximo Medical B-LaserTM IDE study. Catheter Cardiovasc Interv. 2019;94(7):1010-1017.

RISK
INFORMATION
AngioDynamics, the AngioDynamics logo, Auryon, and the Auryon logo are trademarks and/or registered trademarks of AngioDynamics, Inc., an affiliate or a subsidiary. © 2024 AngioDynamics, Inc. UC/PA/AD/1957 Rev 02 04/2024
The
ATTACKS
severe
below the knee.
Auryon Atherectomy System
and cracks
calcium
1
Read the published study here: Discover the Science and Safety at Auryon-System.com VISIT US AT BOOTH #1030
Toe and flow session aims to break down barriers to multidisciplinary limb salvage teams
By Will Date
“If you had cancer you would go to a cancer center where you would get a multidisciplinary approach,” SVS President Joseph Mills, MD, tells VS@VAM, drawing on this example to highlight the importance of multidisciplinary teams for amputation prevention in patients with diabetes and peripheral arterial disease (PAD)—something, he says, is currently lacking in many centers.
Mills, who is the chief of the Division of Vascular Surgery and Endovascular Therapy at Baylor College of Medicine in Houston, Texas, is one of the architects of the “toe and flow” model of multidisciplinary care that seeks to foster greater alignment between specialties in the field of limb salvage— chiefly podiatry and vascular specialists.
This concept is running through an Education Session taking place on Thursday, June 20 (3:30–5:00 p.m. in the West Building, Level 1), co-moderated by Mills and Lauren Gordon, MD, a vascular surgery resident at the University of Toronto in Toronto, Canada, and seeks to address the fragmented approach to limb salvage in many centers. The session will bring together leaders from multiple specialties
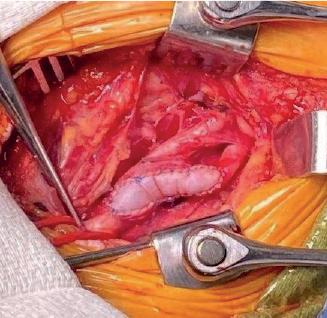
VASCULAR ASSIST Putting out the fires of intraoperative vascular emergencies
AN EDUCATION SESSION TAKING place on Wednesday, June 19 (3:15–4:45 p.m. in the West Building, Level 1) will examine the most common emergency intraoperative vascular surgery consultations, along with trends in intraoperative vascular surgery consultation over time—the subject area that has seen vascular surgeons referred to as the firefighters of the operating room. The aim, through nine presentations given by speakers with broad experience in the field, is for attendees to work together to create a framework for emergency intraoperative consultation, with the assistance of expert viewpoints regarding the best options for vascular intervention for common emergency intraoperative consultation.
Moderated by Maen Aboul Hosn, MD, from University of Iowa in Iowa City, Iowa, and Bryan Dieffenbach, MD, from Scripps Health in San Diego, California,
to highlight algorithms of care, new approaches to assessment, revascularization, wound care and teamwork, in order to look at how to broaden access to limb salvage care to underserved communities.
A cancer patient can be faced with several treatment options, requiring experts from numerous fields to come together to work up a therapeutic plan, says Mills, returning to his analogy to sum up the current state of treatment for chronic limb-threatening ischemia (CLTI) and diabetic foot care. “That does not routinely happen with the diabetic foot. What more often happens is the patient gets admitted to the hospital, somebody swabs the wound, random care ensues, and important things get missed.”
Toe and flow has its roots in Arizona, where, whilst practicing at the University of Arizona, Mills, along with David Armstrong, DPM, now at the University of Southern California, established the Southern Arizona Limb Salvage Alliance—SALSA—to foster a closer relationship between podiatry and vascular surgery clinics, and to harmonize the patient referral,
Joseph Mills
evaluation and treatment pathway.
Outlining how the toe and flow model works in his practice today at STEP (Save The Extremity Program) at Baylor College of Medicine, Mills says it doesn’t matter which specialist sees the patient first—they will be treated according to the same algorithm. “If they get sent to a podiatrist and it turns out they have had three failed angioplasties and their blood flow is poor, they meet a vascular surgeon that same day. If they get sent to the vascular surgeon and it turns out it is not really a blood flow issue [and that] they need better offloading or better shoes, then they see a podiatrist. The idea is to not penalize the patient because our system is disorganized.”

“To hear what happens to patients and how they perceive their care is really, really important, because often in healthcare we look at outcomes from the standpoint of the system or the doctor, and we forget about the patient” JOSEPH MILLS
the session will begin by looking at common intraoperative emergencies for contemporary vascular surgeons with Andrew J. Soo Hoo, MD, a general surgery resident at Medical College of Georgia in Augusta.
Following on from this and three other presentations given by Rebecca Scully, MD, from Dartmouth-Hitchcock Medical Center in Lebanon, New Hampshire, Gaurav Sharma, MD, from Kaiser Permanente Foundation Hospital in Santa Clara, California, and moderator Aboul Hosn, the next presentation will be given by Manju Kalra, MBBS, from the Mayo Clinic in Rochester, Minnesota, entitled “How I do it: A senior surgeon’s approach to emergency intraoperative consultation.”
The final presentation of the session, “How’re you going to fix It? Case presentation: Emergent endovascular repair of an internal iliac artery injury during an outpatient lumbar discectomy,” will be given by Tara Zielke, MD, from Indiana University Health in Indianapolis, Indiana.
Speaking to VS@VAM about the session, Aboul Hosn said it “will highlight the role of vascular surgeons in managing catastrophic bleeding events and lay out a framework for the approach to emergency intraoperative consultation by utilizing existing multidisciplinary models, available data and expert opinions.”—George Barker
DISPARITIES
Of the session at VAM, Mills tells VS@VAM that the patients’ voice will be heard with involvement from patient representatives, “to bring home how this seemingly simple problem can cause a lot of issues for patients in their lives.”
“Most of the doctors in the audience will probably get this, but to hear what happens to patients and how they perceive their care is really, really important, because often in healthcare we look at outcomes from the standpoint of the system or the doctor, and we forget about the patient,” he comments.
The session also features presentations unpacking some of the recent data underpinning advances in CLTI and diabetic foot care, and discussion of key components of team development. “This is a huge issue for our patients and we need to do better,” says Mills of what he hopes attendees will gain from joining the session. “There are barriers everywhere to setting up this type of system, but they can all be overcome. It is not hard to find a toe partner or a flow partner, and to really make a difference in your local hospital and in your local practice. The barriers that the system sets up can be overcome by clinicians who think this is a problem and want to help patients get better outcomes.”
STUDY UNPACKS ACCESS-TO-CARE CHALLENGES FOR DISADVANTAGED CLTI PATIENTS
RESEARCH PRESENTED DURING THE WILLIAM J. VON LIEBIG FORUM (8:10–9:45 a.m. in the Skyline Ballroom, Level 3) will seek to establish whether care for chronic limb-threatening ischemia (CLTI) within the setting of a multidisciplinary limb preservation program can help to overcome some of the socioeconomic barriers to treatment that may impact outcomes among patients in more deprived communities.
The paper, to be presented by Drayson B. Campbell, BS, a medical student at the Ohio State University College of Medicine in Columbus, Ohio, is a mixed methods study that compares outcomes among patients undergoing treatment within the Ohio State University limb preservation program clinic, which is situated in a minority community, to those treated within the hospital’s traditional clinics. Researchers conducted interviews among patients to understand the barriers to treatment.
Campbell will show that among 882 patients treated between 2014–2023, those treated within the limb preservation program typically have more comorbidities, more distal disease, and fewer live independently. However, despite these being sicker, more disadvantaged patients, their outcomes are similar to those healthier, less deprived patients who were treated outside of the setting of the multidisciplinary limb preservation program. “It is well established that multidisciplinary clinics improve outcomes for limb-threatening ischemia, but the mechanisms by which they improve them are largely unknown,” senior author, Michael R. Go, MD, tells VS@VAM
By interviewing patients, the researchers have sought to unpick some of the underlying reasons behind this difference in outcomes between the two care settings. Emerging themes include transportation, high visit frequency and patient-physician racial discordance. “Intuitively it makes sense to me that it was improvements in access to care that were making a difference, and this abstract is the first foray into trying to establish that,” Go adds.—Will Date
8 VS@VAM | Wednesday, June 19, 2024 PAD
INCENTIVES AND COACHING OFFER PROMISE FOR IMPROVING SUPERVISED EXERCISE THERAPY
COMPLETION IN CLAUDICANTS
Study findings set to be presented during Saturday, June 22’s Plenary Session 7 (8–9:30 a.m. in the West Building, Level 3, Skyline Ballroom) support current vascular guidelines advocating for effective supervised exercise therapy (SET) prior to offering vascular intervention for patients with intermittent claudication. That is the belief of Colin Cleary, PhD, a fourth-year medical student at the University of Connecticut School of Medicine in Farmington, and his co-authors. By Jamie Bell
“CURRENT GUIDELINES BY THE SVS [Society for Vascular Surgery] support the use of effective supervised exercise therapy programming as first-line therapy for all patients with intermittent claudication. These guidelines are supported by primary literature that supports the use of SET before any vascular intervention for symptomatic, flow-limiting arterial disease,” Cleary tells VS@VAM. “However, during this study, we found that patients were motivated much more to complete programming primarily from individualized coaching, and that
patients who completed programming were more likely to delay their vascular interventions.”

effort whereby patients who were diagnosed with intermittent claudication were offered enrollment in a prospective quality improvement protocol for a 12-week SET program at outpatient sites through Hartford HealthCare. Program completion was defined as ≥24 of the 36 offered sessions over 12 weeks.

Published rates of SET program comple tion range from 5% to 55%. Cleary and col leagues note, for example, a historical com pletion rate of 54% at their own institution. As such, they sought to identify if targeted patient-supportive interventions—includ ing financial incentives and individualized coaching—can improve completion rates while still maintaining efficacious SET pro gramming. Cleary


A three-pronged approach was utilized to improve completion during the study, including financial incentives up to $180, scheduled coaching with advanced practitioner staff, and informational materials on the importance of SET programming and lifestyle modification. Patient-reported improve ments in walking symptoms were tracked and analyzed, as were several functional measures of SET programming—including


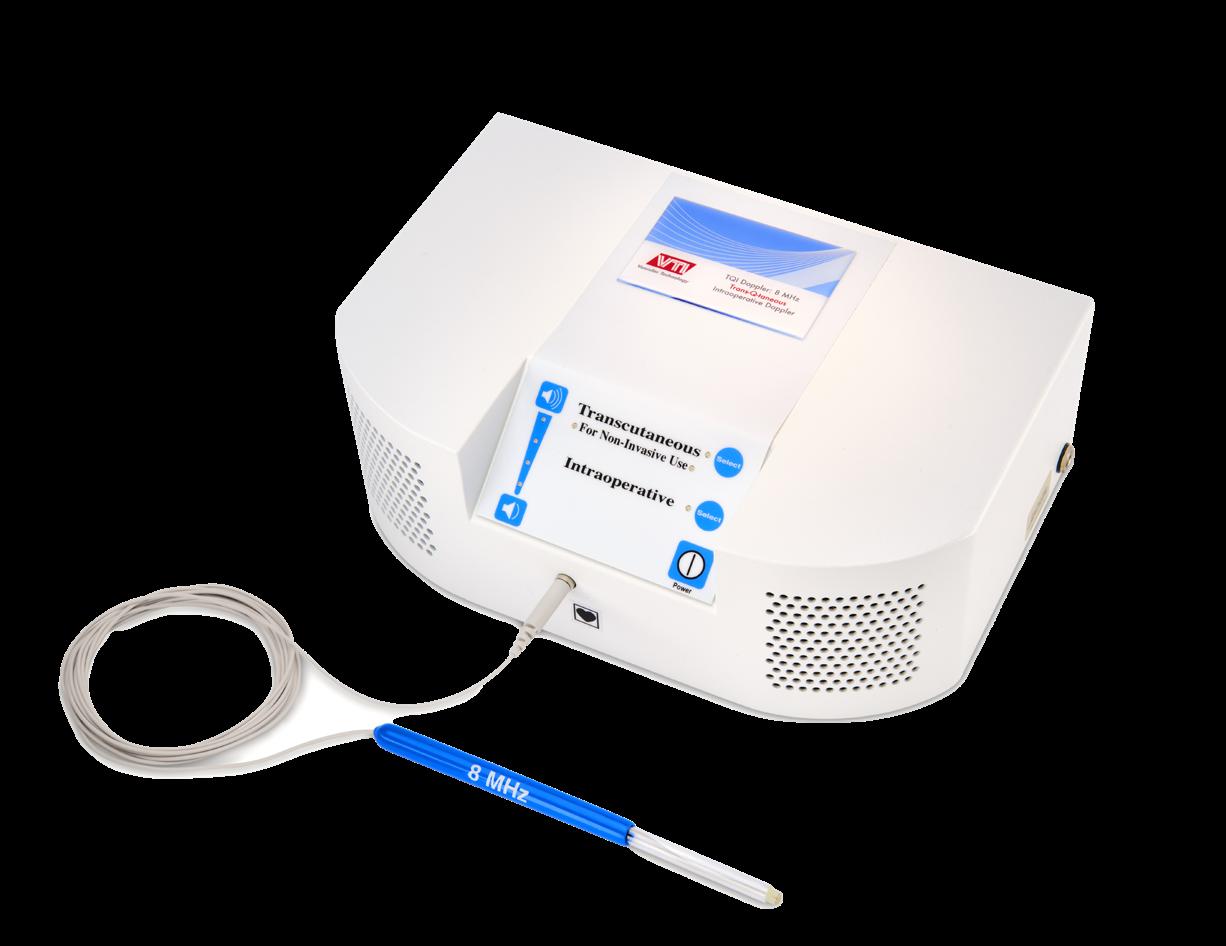
Reach for the Doppler that Works Every Time
The Trans-Q-taneous Intraoperative “TQI” Doppler System is the Doppler you can rely on for all your surgical needs.

RELIABLE
VTI’s single-use surgical Doppler probes provide a high degree of reliability since probe failure due to reprocessing is eliminated.
COST EFFECTIVE
over a two-year study period. Compared to pre-SET baseline, patients who completed SET noted less pain, aching, cramps in calves when walking and less difficulty walking one block. Additionally, patients significantly increased their METs, total walking duration and total walking distance from their preSET baseline. And, while the researchers report participant ABIs remaining unchanged from enrollment to completion, they did find that patients who completed SET programming had delayed vascular intervention compared to those who either did not complete SET or declined participation. Cleary highlights a potentially key factor: patients with public insurance had a median out-ofpocket expense of $0 per visit compared to



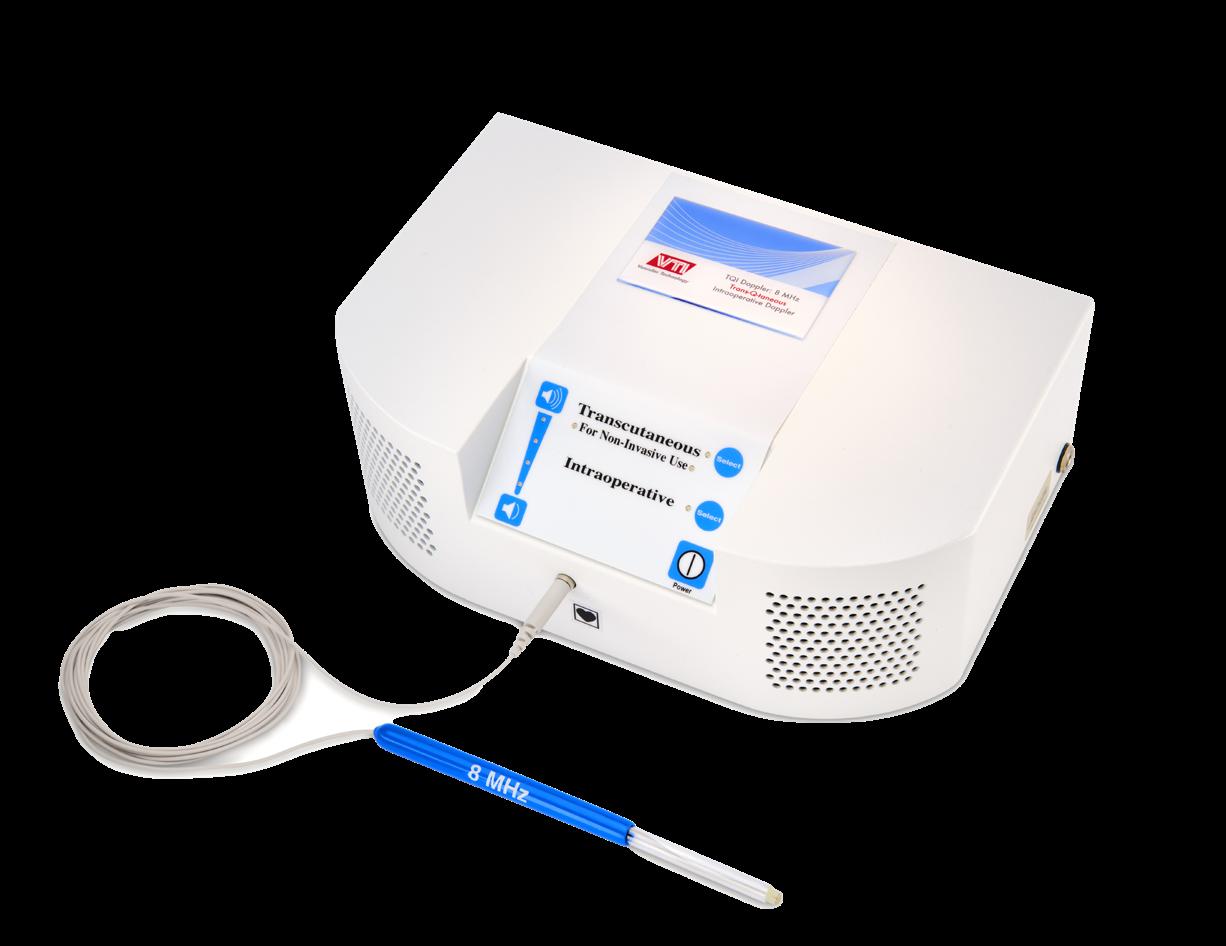
The hidden costs associated with reusable probes, including reprocessing and lost OR time due to probe malfunctions, are eliminated.
MULTI-FUNCTIONAL
Provides real-time intraoperative and transcutaneous evaluation of blood flow, for ALL your surgical needs.









9 www.vascularspecialistonline.com
CLAUDICATION
Colin Cleary
Call 800-550-0856 or visit us at VTI-online.com to learn more about our Doppler. vti-online.com | 603-594-9700 | info@vti-online.com Visit our TQI product page on our website. Be Confident in Your Doppler! atVisitusBoothVAM #401
Welcome to VAM 202 4
TUESDAY/WEDNESDAY SCHEDULE AT-A-GLANCE
Tuesday, June 18
8:00 a.m. to 5:00 p.m. VQI Annual Meeting: Day 1 West Building, Level 4, W470
2:00 p.m. to 5:00 p.m. Registration West Building, Level 3, Hall F1 Foyer
5:00 p.m. to 7:00 p.m. VQI Poster Networking Reception West Building, Level 4, W471
Wednesday, June 19
6:00 a.m. to 5:00 p.m. Registration West Building, Level 3, Hall F1 Foyer
7:00 a.m. to 8:00 a.m. World Federation of Vascular Societies Educational Session West Building, Level 1, W184bc
8:00 a.m. to 8:10 a.m. Opening Ceremony West Building, Level 3, Skyline Ballroom W375ab
8:00 a.m. to 5:00 p.m. Society for Vascular Nursing Conference: Day 1 West Building, Level 1, W187
8:00 a.m. to 5:00 p.m. VQI Annual Meeting: Day 2 West Building, Level 4, W470
8:10 a.m. to 9:45 a.m. Plenary Session 1: William J. Von Liebig Forum West Building, Level 3, Skyline Ballroom W375ab
9:45 a.m. to 10:00 a.m. Coffee Break West Building, Level 3, Skyline Ballroom W375ab Foyer
10:00 a.m. to 11:15 a.m. Plenary Session 2 West Building, Level 3, Skyline Ballroom W375ab
11:15 a.m. to 12:15 p.m. E. Stanely Crawford Critical Issues Forum: Quality Care Everywhere West Building, Level 3, Skyline Ballroom W375ab
12:30 p.m. to 1:30 p.m. Visceral Artery Aneurysms: Modern Insights and Current Dilemmas West Building, Level 1, W183b
12:30 p.m. to 1:30 p.m. APSA-SVS Multidisciplinary Pediatric Vascular Surgery Interest Group West Building, Level 1, W183c

p.m. to
p.m.
12:30 p.m. to 1:30 p.m. Endovascular Aortic Devices: From Regulatory Approval to Post-Market Oversight West Building, Level 1, W183a 12:30 p.m. to 1:30 p.m. Vascular Fellows: Preparing for Practice – Presented by Gore
W184d
3, Skyline Ballroom W375ab
p.m. to 4:45 p.m. Registered Physician Vascular Interpretation (RPVI) Exam Review and Refresher Course: Ultrasound Physics and Vascular Test Interpretation West Building, Level 3, Skyline Ballroom W184a
2:22 p.m. to 3:02 p.m. SVS-VESS Scientific Session @ VAM: Session 1b
3:15 p.m. to 4:06 p.m. SVS-VESS Scientific Session @ VAM: Session 2a West Building, Level 1, W184bc
3:15 p.m. to 4:45 p.m. The Firefighters of the OR: Intraoperative
10 VS@VAM | Wednesday, June 19, 2024
West
1:30
West
West Building, Level 1,
1:30
2:21
SVS-VESS Scientific Session @ VAM: Session 1a
Building, Level 1, W184d
p.m. to 3:00 p.m. My Worst Cases
Building, Level
1:30
West
Building, Level 1, W184bc 3:00 p.m. to 3:15 p.m. Coffee Break West Building, Level 3, Skyline Ballroom W375ab Foyer
Vascular Emergencies West Building, Level 1, 183b 3:15 p.m. to 4:45 p.m. SVS-AVF: Latest Innovations in the Treatment of Venous Disease West Building, Level 1, W183a 3:15 p.m. to 4:45 p.m. Clinical Guidelines Discrepancies Between the Society for Vascular Surgery and European Society for Vascular Surgery West Building, Level 1, W183c 4:07 p.m. to 4:47 p.m. SVS-VESS Scientific Session @ VAM: Session 2b West Building, Level 1, W184bc 5:00 p.m. to 5:45 p.m. SVS Keynote Speaker Series: Finishing the Journey to Inclusivity Through Belonging, Intention and Respect West Building, Level 3, Skyline Ballroom W375ab 6:30 p.m. to 8:30 p.m. SVS Connect@VAM: Building Community Soldier Field Sears Tower, also known as Willis Tower, in the heart of Chicago
Around town
WELCOME TO CHICAGO, VAM 2024’s host city brimming with attractions and activities to enhance your visit. Here are some recommendations for making the most of the trip:
The Art Institute of Chicago is a hub for art enthusiasts situated in Grant Park. The museum’s extensive collection includes renowned Impressionist and Post-Impressionist works.
The Field Museum is a place where attendees can dive into the wonders of natural history.
Experience Chicago’s architecture from the water with a river cruise—a unique perspective on the city’s skyscrapers, including the Willis Tower (also knows as Sears Tower, opposite, left) and John Hancock Center
Millennium Park offers an urban oasis perfect for a stroll.
For a mix of entertainment and relaxation, head to Navy Pier. The Chicago Riverwalk is another scenic stroll opportunity. With an array of cafes, public art installations and boat rental options, it’s a great place to relax and enjoy the city’s vibrant atmosphere.
Take in Women’s Leadership Dinner
SCHEDULE TO TAKE PART IN the Women’s Leadership Dinner on Thursday, June 20, from 7–9:30 p.m. in the Marriott Marquis. The dinner offers attendees the opportunity to engage in meaningful discussions, network with industry leaders and support the advancement of women in vascular surgery. A highlight will be a keynote address from Donna Mendes, MD.
Attendees who didn’t sign up during their VAM 2024 registration can still purchase the add-on ticket through their registration login.
Join SVS Connect@VAM: Building Community tonight at Soldier Field!
VAM, THE VASCULAR QUALITY Initiative (VQI), Society for Vascular Ultrasound (SVU) and Society for Vascular Nursing (SVN) annual meeting attendees are invited to attend the 2nd annual SVS Connect@VAM: Building Community event taking place tonight, June 19, at 6:30 p.m. at Soldier Field. Families are welcome.
An SVS Connect@VAM shuttle service will depart from the Marriott Marquis located across from McComick Place beginning at 6:20 p.m. The event is sponsored by Philips.

SVS RAISES ALARM OVER HEALTHCARE CONSOLIDATION IN COMMENTS TO
FTC, DOJ, HHS
THE SOCIETY FOR VASCULAR SURGERY (SVS) HAS SUBMITTED comments to the Federal Trade Commission (FTC), the Department of Justice (DOJ) and the Department of Health and Human Services (HHS) in response to a Request for Information (RFI) concerning the consolidation of healthcare markets.
In its comments, the SVS highlights how the consolidation trend in healthcare exacerbates barriers to patient access, especially for those with vascular diseases. The comments stress that mergers and acquisitions within hospital systems often lead to increased prices and reduced service availability, impacting patient care.
SVS Advocacy Council Chair Margaret Tracci, MD, JD, emphasized the urgency of these concerns, stating, “Our primary concern is ensuring that patients have access to high-quality care. The consolidation in healthcare markets creates significant challenges, particularly for vulnerable populations, by driving up costs and reducing service availability.”
The comments outline several critical concerns regarding the impact of healthcare consolidation. The SVS argues that consolidation often results in higher costs for patients and payors, which can limit access to necessary medical services, particularly for older patients with vascular diseases who are frailer and more reliant on Medicare or Medicaid.
Consolidation threatens the viability of independent or private practices, where many innovative, minimally invasive vascular disease treatments occur in more accessible and cost-effective outpatient settings such as ambulatory surgery centers (ASCs) or office-based labs (OBLs). Tracci pointed out, “The reduction of these accessible and cost-effective service sites due to consolidation is a step backward for patient care.”
The SVS also highlights the role of private equity in driving consolidation. Tracci noted that the influence of private equity in healthcare tends to prioritize financial returns over patient outcomes, thereby compromising the quality and accessibility of care.
The comments note that large healthcare systems may reduce the range of clinical services at various locations based on profitability. The SVS calls for careful consideration of these issues in the administration’s policy development and enforcement actions, and urges any actions to address the negative impacts of consolidation on patients and providers.
The SVS will now await the relevant agencies—including the FTC, DOJ and HHS—to review the feedback and inform their policymaking process. The agencies may use these insights to draft proposals, typically publishing them to solicit further public comments.
“We look forward to collaborating with the FTC, DOJ and HHS to ensure policies that support high-quality care and accessible healthcare services for all patients,” said Tracci.
SVS members and VAM 2024 attendees with inquiries regarding the SVS’s comments should contact advocacy@vascularsociety.org
APP united: Society for Vascular Nursing and SVS PA Section to host immersive program
THE SOCIETY FOR VASCULAR NURSING (SVN) is again hosting its 42nd Annual Conference June 19–20 at McCormick Place alongside VAM 2024. This year’s meeting offers attendees a diverse offering, including an immersive program that will merge with the SVS Physician Assistants (PA) Section. The program will kick off on Wednesday evening with the return of Vascular Jeopardy, which debuted at VAM 2023. The educational game will involve vascular nurses, PAs and other APPs facing off in a jeopardy-style format answering questions about different cases and treatment of vascular patients.
The SVN program has been approved for 13.1 contact hours.
Step on it for PAD!
DON’T LET EVERY EXTRA STEP TAKEN at VAM 2024 go to waste. All attendees are eligible to register for the SVS Foundation’s Vascular Health Step Challenge at VAM. C hallenge registrants will compete to be VAM’s top walker. It kicks off on Wednesday, June 19, at 6:20 p.m., with a walk from VAM to SVS Connect@VAM at Soldier Field and concludes at 5 p.m. on Friday, June 21. The person with the highest step count will receive a $100 gift card. Visit vascular.org/STEP2024
Remember to cast your vote for SVS vice president
EARLY ACTIVE, ACTIVE AND SENIOR SVS members should submit their vote for SVS vice president by this Thursday, June 20, at 2 p.m. The candidates for this year’s election are Linda Harris, MD, and Palma Shaw, MD.
This election will be the first one that welcomes Early Active SVS members to vote. This change was made due to the 2023 SVS bylaws referendum that passed in November 2023. All eligible members are strongly encouraged to take advantage of this membership benefit and help SVS leaders reach a goal of 1,000 total votes.


Votes can be cast at vascular.org/ Vote2024. QR codes are scattered throughout McCormick Place. Members should sign in with their SVS credentials. Email governance@ vascularsociety.org with any difficulties.
Learn more at vascular. org/2024Candidates

11 www.vascularspecialistonline.com
Compiled by Kristin Spencer and Marlén Gomez
Margaret Tracci
Radiation safety session seeks to address variability and improve access to education
“Variability is a source of inferior quality, poor outcomes and harm,” says Anil Hingorani, MD, vascular surgeon at New York University (NYU) Langone in Brooklyn, speaking to VS@VAM ahead of Thursday morning’s VAM 2024 session on the past, present and future of radiation safety. By Jamie Bell
THE SESSION—WHICH INTENDS TO IMPROVE access and address variability within radiation safety education—will feature talks on special concerns for staff, women and pediatric patients, and even new technologies that may enable vascular surgery to “move away” from radiation. It takes place from 7–8 a.m. (the West Building, Level 1)
Hingorani, who will moderate alongside Gale Tang, MD, associate professor and chief of vascular surgery at the University of Washington (UW) in Seattle, continues: “Radiation safety has been relegated to the purvey of each hospital—some have vigorous annual certification and exams;
at some others they are practically non-existent.
“After looking over to see what some of our colleagues in other fields have established for education and certification in radiation safety for national standards, and examined the variability at our institution, I would suggest we need to establish minimum standards for the sake of our patients, our staff and ourselves. This course focuses on a key set of skills that all vascular practitioners should own.”
The session kicks off with a presentation on the relevance of radiation safety for the practicing vascular surgeon from Fernando L. Joglar, MD, associate professor of surgery at the University of Puerto Rico School of Medicine in San Juan. Subsequent talks include “Maximizing protection from radiation,” given by Melissa L. Kirkwood, MD, professor and chief of the Division of Vascular and Endovascular Surgery at the University of Texas Southwestern Medical Center in Dallas.
wear in order to minimize radiation exposure—something that, in her view, is “extremely practical for every trainee and practicing vascular surgeon to learn.”
Special concerns for women patients, staff and pediatric patients regarding radiation safety are next on the agenda, and will be outlined by Agelilki G. Vouyouka, MD, professor of surgery and radiology at Icahn School of Medicine at Mount Sinai in New York. Following this, a presentation from Peter A. Schneider, MD, professor of surgery in the Division of Vascular and Endovascular Surgery at the University of California San Francisco, will center around the As Low As Reasonably Achievable (ALARA) principle, and methods for “maximizing imaging while reducing radiation exposure.”
Discussing Kirkwood’s talk, Tang notes that the presentation will cover dose-sparing strategies and also review evidence around various pieces of protective gear that operators
“Every couple of weeks, a new technology is being added to our armamentarium, often using fluoroscopy. Similarly to all technology, it is very useful but has to be used properly”
ANIL HINGORANI
Fittingly, the final presentation will nudge audiences to consider the future outlook of radiation safety and education, with Andres Schanzer, MD, professor of surgery in the Division of Vascular and Endovascular Surgery at the University of Massachusetts Memorial Medical Center in Worcester, discussing the latest technologies in this space, and a possible “move away” from radiation further down the line.
“Vascular surgery is still undergoing the endovascular revolution,” says Hingorani. “Every couple of weeks, a new technology is being added to our armamentarium, often using fluoroscopy. Similarly to all technology, it is very useful but has to be used properly. This session focuses on using radiation safely to optimize outcomes and imaging.
“It will cover not only the present technology but also developing technology. These upcoming technologies have the potential to reduce radiation exposure, especially in complex cases. In addition, our future is our trainees. To make change, we need to focus on how to train the trainees in these important concepts.”
12 VS@VAM | Wednesday, June 19, 2024
WELLNESS
VESS
Unmet
needs and paradigm shifts: VESS scientific sessions set to plumb the vasculature for advances in
practice
By Éva Malpass
SELECTED RESEARCH TO BE PRESENTED DURING the Wednesday afternoon, June 19, series of Vascular and Endovascular Surgery Society (VESS) Scientific Sessions (from 1:30 p.m. onward in the West Building, Level 1) will highlight areas of unmet need and offer paradigm-shifting analyses concerning thrombectomy for pulmonary embolism (PE), carotid endarterectomy (CEA) and endovascular aneurysm repair (EVAR), among other key domains.
Presenting in this afternoon’s first session, Jin Hyun Joh, MD, from University Hospital at Gangdong in Seoul, South Korea, will deliver a comparison of outcomes between percutaneous atherectomy versus balloon angioplasty and/or stenting in the treatment of femoropopliteal disease based on the Korean Society for Vascular Surgery’s (KSVS) DAMOEUM registry. The nationwide prospective multicenter repository assessed primary patency rate and postprocedural ankle-brachial index (ABI).
“There have been many studies that have reported on interventional treatments of peripheral arterial disease [PAD]; however, most of these are single-arm or company-sponsored studies, and so are not reflective of real-world practice,” Hyun Joh tells VS@VAM. Theirs, he states, will offer “meaningful real-world data,” suggestive of lower rates of occlusion recurrence post-atherectomy, but places emphasis on “careful” patient selection.
Later in this session, resident Tiffany R. Bellomo, MD, from Massachusetts General Hospital in Boston, is set to present multi-institutional retrospective registry data on the clinical and anatomic characteristics of popliteal artery aneurysms (PAAs) associated with limb-threatening and thromboembolic events. As senior author Anahita Dua, MD, also from Massachusetts General Hospital states, this research identifies a “new variable”—thrombus burden—to more accurately identify which patients will have complications, so lesions can be treated before causing an acute event.
“Through this research, we have identified thrombus bur-
VASCULAR PRACTICE
den has the biggest impact in terms of predictive value and we have quantified this through ultrasound,” Dua states. “We hope our research will allow for a new paradigm by which popliteal aneurysms can be evaluated to identify threatened patients and save limbs.”
In the following session, among several abstract presentations, resident Paul Rothenberg, MD, from West Virginia University in Morgantown, West Virginia, will deliver data on abdominal aortic aneurysm (AAA) care, discussing the impact of rural residence on the presentation of AAA and the likelihood of being lost to follow-up after endovascular repair.

Speaking to VS@VAM, Rothenberg emphasizes how deadly AAA ruptures are and how preventable they can be with appropriate screening: “Rural populations are often medically underserved and are particularly vulnerable as a result. At our institution, which is located in a highly rural state in Appalachia, our endovascular repair rate for symptomatic and ruptured AAA is nearly double the national rate reported by the VQI [29.2% vs. 15% for symptomatic AAA; 11% vs. 6.1% for ruptured AAA]. Not only are rural patients presenting with ruptured or symptomatic aneurysms, we also found these patients are lost to follow-up. We know that losing EVAR and TEVAR patients to follow-up brings worse outcomes over time, so we want to highlight these results to emphasize that these patients are not being seen over time, which represents a problem that affects rural patients more. That is why we undertook this research.”
In presenting these data, which highlight the need for access to AAA screening and surveillance in rural areas, Rothenberg and his team of researchers hope to increase resources for rural provider education, ultimately to decrease the number of patients that present with a symptomatic or ruptured AAA.
Rounding off this session with a report on long-term
COMMUNITY AFFAIRS: OPTIMIZING, PROTECTING AND ENHANCING CLINICAL PRACTICE
T
he SVS Community Practice Section (CPS) has put together an extensive 90-minute program for Thursday afternoon at VAM.
The session, entitled Community Practice Section: Optimizing and Protecting your Clinical Practice, will take place on Thursday, June 20, from 1:30 to 3:00 p.m. (West Building, Level 1). CPS Chair Robert Molnar, MD, and the VAM Postgraduate Education Committee Chair William Robinson III, MD, will moderate. It will consist of six talks from a variety of speakers across community practice in vascular surgery.
The session will cover a wide breadth of relevant topics, including supplemental income opportunities for practices, malpractice protection, retirement and signing a contract. The education portion will wrap with a 25-minute panel discussion where questions will be taken from the audience.
“The CPS session at VAM 2024 was developed to provide actionable opportunities to optimize, protect and enhance your clinical practice. Every vascular surgeon, regardless of practice type, recognizes how difficult it has become to successfully manage the practice while providing expert vascular care to their community.
The Community Practice Section has created a robust session to assist in ensuring continued success,” said Molnar.
outcomes and adaptive changes in collateral visceral circulation following intentional celiac artery embolization (CAE) during complex EVAR/TEVAR, resident Arash Fereydooni, MD, from Stanford University in Stanford, California, outlines how this research has shown that CAE is a “useful adjunct” to extend proximal or distal seal during EVAR/ TEVAR; however, mesenteric complications occur in 10–15% of patients over a 90-day postoperative period. He notes that, although CAE may have “less utility to treat complex aortic pathology in the future,” it will nevertheless “remain a technique in the toolbox of the vascular surgeon in emergency circumstances or when new-generation endografts are not readily available.”
Continuing discussion of CAE, medical student Leana Dogbe, from Penn State Hershey College of Medicine in Hershey, Pennsylvania, will later deliver data on African American women’s more frequent presentation with more severe forms of carotid disease, and the effect of their “inadequate care” on clinical outcomes. She tells VS@VAM that representation of this patient population is “lacking” in landmark trials to date, and with the U.S. population’s increasing diversity, these insights must spark “action” to mitigate poor post-surgical outcomes.
Later today, there will feature an analysis of factors which influence general surgery residents to specialize in vascular surgery. Presenting author, resident Christina Cui, MD, from Duke University in Durham, North Carolina, comments that, in the context of the projected shortage of vascular surgeons, their research highlights how “boosting pipelines is crucial to avoid impacts on patient care.”
“We hope our research will allow for a new paradigm by which popliteal aneurysms can be evaluated to identify threatened patients and save limbs”
ANAHITA DUA
decided facilities would no longer require approval by the Centers for Medicare and Medicaid Services (CMS) to perform TF-CAS procedures and that TF-CAS would furthermore be reimbursed for standard indications.
The NCD suggests that there should be oversight at the hospital level, but there are no enforcement criteria required to ensure these procedures are being performed appropriately by adequately trained interventionalists.

There will also be a clinical element to the session. Molnar’s talk will be the first of the six and is entitled, “Transfemoral carotid artery stenting (TF-CAS)—is your practice prepared?” His talk will delve into the detail of the November 2023 National Coverage Decision (NCD) on carotid angioplasty and stenting that
Robert Molnar
“There is no registry requirement to follow patient outcomes. In addition, the NCD requires a shared decision-making process, but there has not been a verified tool developed to provide for said process,” said Molnar.
“In short, the guardrails that had been in place to ensure TF-CAS was being performed appropriately in the past have been removed and this potentially places our patients with carotid occlusive disease at risk.”
Molnar’s talk will highlight how community practices can be better prepared for
TF-CAS procedures as they relate to the ruling—and so patients receive the best possible care.
The last 15 minutes of the session will be spent highlighting the 2024 Excellence in Community Practice Award recipients. Formerly known as the Excellence in Community Service Award, it is an honor the SVS bestows on members who have exhibited outstanding leadership within his or her community as a practicing vascular surgeon. Selection for this award recognizes an individual’s sustained contributions to patients and their community, as well as exemplary professional practice and leadership.
“It is important that community practice vascular surgeons know that they are an integral part of vascular care across the country,” said Molnar, who himself received the award in 2022.
Molnar will be presenting the awards as chair of the CPS to the 2024 recipients: Enrico Ascher, MD; Sachinder Hans, MD; Chistopher LeSar, MD; and Manish Mehta, MD. – Kristin Spencer
13 www.vascularspecialistonline.com
VESS President Misty Humphries
VAM THROUGH THE LENS » 23
Take a look back at some of the highlights and goings-on at VAM 2023 in National Harbor, Maryland. The landmark meeting (last June 14–17) drew nearly 1,400 vascular professionals, moving the needle with program innovations, a slew of new science and a jam-packed agenda. With more content presented than ever before, a family-friendly Wednesday night gathering, the inaugural Frank J. Veith Distinguished Lecture, and a hugely successful Gala, VAM 2023 set a benchmark for VAM 2024 in Chicago to follow.








“The quality and impact of the science was really high. It was diverse across the whole array of vascular surgery”
ANDRES SCHANZER

14 VS@VAM | Wednesday, June 19, 2024
Clockwise from middle left: Past President Ronald Dalman attends the Gala with his daughter; a scene from the Exhibit Hall; then SVS President Michael Dalsing with his family; a Plenary presenter; BEST-CLI and BASIL investigators come together; an SVS PA Section session; and an attendee visits a VQI poster. Inset (middle): a special session on pediatric vascular surgery (top); and Leigh-Ann O’Banion conducts Gala festivities
Dedicated session offers insight on ebbs and flows of SVS, ESVS guidelines
By Jocelyn Hudson
AN EDUCATION SESSION SET TO TAKE PLACE IN the afternoon of Wednesday, June 19 (3:15–4:45 p.m. in the West Building, Level 1), will examine discrepancies between Society for Vascular Surgery (SVS) and European Society for Vascular Surgery (ESVS) clinical practice guidelines.
The session centers around the fact that, with the exception of the 2019 Global Vascular Guidelines on the management of chronic limb-threatening ischemia (CLTI), the production and release of clinical practice guidelines by the respective journals of the SVS and ESVS are not coordinated or managed between these societies. Furthermore, recommendations between societal guidelines often differ, leave gaps or content areas unaddressed, or unilaterally define new content areas unique to a specific society.
Against this backdrop, the VAM 2024 session has four key aims: to highlight differences between the SVS and ESVS guidelines and how they play out in day-to-day clinical practice; to examine the scientific, cultural, societal and personal reason(s) behind these respective differences; to gain insight into the guideline development processes between the SVS and ESVS; and to consider future publication upgrades between the respective societies to harmonize recommendations or contextualize differences when apparent, in order to enhance understanding and adaptation when appropriate.
Moderating the session will be Firas Mussa, MD, of the University of Texas Health Science Center at Houston, Texas; Ronald Dalman, MD, of Stanford University in Stanford, California; Ian Loftus, MD, of St. George’s University Hospitals NHS Foundation Trust in London, England; and Thomas Forbes, MD, of the University of Toronto, Canada.
Speaking to VS@VAM, Mussa underscores what attend-
ees can expect. “The session is meant to highlight where the SVS and ESVS might agree or disagree on clinical practice patterns. […] Furthermore, it is meant to touch on the drivers of patient care in the U.S. as compared to Europe,” he says.

Dalman notes that “there are a few important differences in guideline recommendations between those outlined by the SVS and the ESVS” and that SVS members and VAM attendees “will be interested to learn the rationale and evidence behind these differences—and make up their own minds regarding how to manage patients with these challenging conditions based on the explanations provided.”
Dalman anticipates the debate-format session will be “lively and highly engaging” and is one VAM attendees “won’t want to miss.”
Loftus remarks that international clinical guidelines are “important tools to guide patient pathways and decision-making for individual patients,” and that each set of guidelines from the SVS and the ESVS “take many months of intense collaboration between key opinion leaders in
FULL SMORGASBORD OF VASCULAR SURGERY TO BE SHOWCASED DURING FRIDAY’S INTERNATIONAL FAST TALK SESSION GLOBAL EDUCATION
On Friday morning, June 21 (6:30–7:15 a.m. in the West Building, Level 1), VAM 2024 attendees will have the chance to take in an International Fast Talk scientific session featuring updates on the latest devices, studies and procedural techniques from all over the globe, and across the full gamut of vascular surgery—including venous stenting, aortic remodeling, dialysis access creation, carotid aneurysm management, and much more. By Jamie Bell
“The abstracts highlighted in this international session are extremely diverse, including multicentered clinical trials, original research and innovative techniques from around the world,” said Wei Zhou, MD, professor of Surgery at the University of Arizona in Tucson, who is among the session’s moderators.
The session will kick off with a presentation on the safety and effectiveness of the single Prostyle (Abbott) vascular pre-close technique in patients undergoing endovascular procedures. Presenting author Rocco Cangiano, MD, vascular
surgery resident at the Sapienza University of Rome in Italy, will deliver findings from a single-center, prospective study that indicate the technique’s efficacy and safety in selected vascular accesses.
Additional European perspectives will be highlighted during the session, as Jerome Albertin, vascular surgeon at Polytechnic Notre Dame in Draguignan, France, presents positive 12-month ELLIPSE study results regarding the treatment of femoropopliteal lesions using the Jetstream atherectomy device and Ranger drugcoated balloon (both Boston Scientific).
the field.” He continues, “While [society guidelines] undoubtedly advance the care of patients with vascular disease, there are often differences between individual recommendations made either side of the Atlantic, which stimulate debate and occasional controversy. It is important that guidelines reflect different healthcare systems, disease patterns and expectations of clinicians and patients alike.
“In this exciting session, we will highlight and debate some of the key differences in our important guidelines, and how they have influenced decision-making with real case examples,” Loftus says.
Forbes notes that the editors of the Journal of Vascular Surgery and the European Journal of Vascular and Endovascular Surgery have brought together an international panel to discuss the guidelines. “We’re looking forward to this session and what should be a robust discussion around these clinically relevant practice recommendations, as well as to explore opportunities to harmonize these efforts in the future,” he tells VS@VAM
“In this exciting session, we will highlight and debate some of the key differences in our important guidelines, and how they have influenced decision-making with real case examples”
IAN LOFTUS
The session will cover four guideline topics, namely the management of aortic graft infection, asymptomatic carotid stenosis, intermittent claudication and the management of incompetent perforators in venous disease. Due to speak on the latter, Maarit Venermo, MD, PhD, of Helsinki University Hospital in Helsinki, Finland, highlights that the recommendations on invasive treatment of perforator veins are very different between SVS and ESVS, with the key variance being that the ESVS “is much more conservative when it comes to the invasive treatment of perforators.” These differences will be discussed in this session around a patient case, with Venermo noting that patient cases will feature throughout the session.
And, later, maintaining the thread of endovascular topics, Pasqualino Sirignano, MD, associate professor of vascular surgery at the Sapienza University of Rome, will present insights from SAFEEVAR—a Delphi questionnaire-based study that sought to elucidate the attitude of Italian vascular surgeons towards the use of standard endovascular aneurysm repair (EVAR) to treat infrarenal abdominal aortic aneurysms (AAAs) outside the current instructions for use (IFU).
Venous stenting is also on the agenda, with Mahmood Razavi, MD, director of the Clinical Trials and Research Center at St. Joseph Vascular Institute in Orange, California, set to present the VIVID clinical trial and discuss outcomes with the Duo (Vesper Medical/Philips) stent system.
Lixin Wang, MD, deputy director of Zhongshan Hospital affiliated with Fudan University in Shanghai, China, will outline a study that aimed to compare aortic remodeling of the distal aorta after traditional thoracic EVAR (TEVAR) against repair with the Fabulous (Hangzhou Endonom Medtech) stent—a new, two-stage stent system based on the PETTICOAT technique—in type B aortic
dissection (TBAD) patients. The session will also see International Achievement Award recipient Chun Che Shih, MD, deputy superintendent of Taipei Wanfang Hospital in Taipei, Taiwan, provide insights from his lifelong work on aortic dissection. Later in the session, TBAD will come into focus again, as Besher Tolaymat, MD, integrated vascular surgery resident at Cooper University Hospital in Camden, New Jersey, delivers findings from a systematic review assessing the available literature on the variability of impulse control management in these cases.
Elsewhere, a potential innovation in hemodialysis access is set to be presented.
Hsuan Yu Chen, from China Medical University Hospital in Taichung, Taiwan, will describe the creation of an “artificial aneurysm” over the brachial artery as an alternative to traditional “shuntless” access approaches.
The carotid territory will also feature—initially, with insights from the prospective, multicenter, international Carotid Aneurysm Registry (CAR) on the conservative management of extracranial carotid artery aneurysms by Saskia I. Willemsen, a PhD student at UMC Utrecht in The Netherlands.
15 www.vascularspecialistonline.com
CLINICAL PRACTICE
Analysis will kickstart conversation on F/BEVAR outcomes
By Will Date
NEW DATA PRESENTED DURING FRIDAY’S PLENARY
Session 6 (10–11 a.m. in the West Building, Skyline Ballroom) will shed light on trends in the adoption of fenestrated and branched endovascular aortic repair (F/BEVAR) outside of Food and Drug Administration (FDA) Investigational Device Exemption (IDE) trials, and probe whether there are differences in mortality rates among patients treated inside and outside of the trial setting.
Presenting author Sara Zettervall, MD, an assistant professor of surgery at University of Washington in Seattle, tells VS@VAM that the results of the analysis should kickstart an important conversation about protocols for the use of F/ BEVAR, an approach that is “increasing dramatically” across the country.
Zettervall and colleagues have used Medicare claims data to identify patients undergoing endovascular treatment of the visceral aorta incorporating two or more visceral artery endoprostheses between 2014–2022, identifying cases performed at both IDE and non-IDE sites. The research -
ers compared the 30-day and three-year mortality rates between procedures performed within both the trial and non-trial locations. Through the analysis, the researchers have sought to quantify the use of F/BEVAR in the United States and to evaluate any association with case volume and mortality at IDE and non-IDE sites.
“We all suspect that physician-modified endografts are happening all over the place, but because published data are limited just from IDE sites, what is really going on in actual practice has not been widely studied,” Zettervall comments, looking ahead to her presentation of the analysis during Friday’s session, in which she will reveal the findings of the study for the first time. “There needs to be a starting point to know how much this is happening and how are these patients doing, because we really don’t have a marker outside of IDE sites at all,” she says.
Turning to the results, Zettervall explains that the analysis points to the fact that most of the sites at which these procedures are being performed are non-IDE centers, albeit that these sites are performing a much lower volume of procedures than those participating in the IDE trials.

“We all suspect that physician-modified endografts are happening all over the place”
SARA ZETTERVALL
“What we see is that there are a lot of these cases being done outside of IDE sites, in fact the majority of them, and it is increasing,” says Zettervall. “I think the most shocking thing is that the majority of folks who are doing this are doing
WFVS RUTHERFORD LECTURE AT WORLD FEDERATION SESSION SET TO FEATURE VASCULAR LOW FREQUENCY DISEASE CONSORTIUM DIRECTOR
By Bryan Kay
The director of the Vascular Low Frequency Disease Consortium (VLFDC) is set to be among the headline presenters at this year’s World Federation of Vascular Societies (WFVS) Educational Session on Wednesday, June 19 (7–8 a.m. in the West Building, Level 1). Peter F. Lawrence, MD, also a former SVS president, will deliver the Rutherford Lecture, covering how the WFVS can play a role in helping the VLFDC widen its research efforts.
The WFVS session will feature seven of the member societies from across the globe that make up the federation, and be co-moderated by Palma Shaw, MD, WFVS secretary-general, and Prem Gupta, the current WFVS president.
“The WFVS continues to have consistent representation at VAM, with the European Society for Vascular Surgery [ESVS], the Society for Vascular Surgery [SVS], the Vascular Society of India [VSI], the Japanese Society for Vascular Surgery
[JSVS], Vascular Society of Southern Africa [VASSA], the Latin American Association for Vascular Surgery [ALCVA] and the Australian and New Zealand Society for Vascular Surgery [ANZSVS] all taking part this year,” says Shaw
Lawrence’s lecture will crown the series of presentations covering a number of vascular disease beds and issues facing vascular surgery on a global scale.
With the VLFDC, the WFVS intends to form ties in order to foster “more intense collaboration” going forward, Shaw tells VS@VAM ahead of the VAM 2024 event.
“The VLFDC already reaches out to different parts of the world, but the WFVS makes it more strategic, and in this way we can have representation from all over the federation membership, expanding the opportunities for collaboration and research.”
The WFVS continues to expand its own reach since recalibrating in 2021
one or two per year per hospital, which is super low volume.”
Through their research, Zettervall and colleagues have identified 7,977 patients treated with F/BEVAR at 551 hospitals during the eight-year period under the focus of the study. Of these, 25% of procedures were performed at 20 hospitals with an IDE.
The researchers have found that the median annual case volume per hospital was significantly higher at IDE sites, while their research also points towards differences in the 30-day and three-year mortality between patients treated inside or outside of IDE sites.
“When we look at the data, what we can see is that the folks who are doing it outside of [an] IDE are having worse perioperative survival, and I think we will need to do more research to understand the drivers of that,” Zettervall tells VS@VAM , adding that this will become increasingly important as devices such as the Gore Excluder thoracoabdominal branch endoprosthesis (TAMBE)—the first off-the-shelf endovascular device for the treatment of complex aneurysmal disease involving the visceral aorta to receive FDA approval—gain wider usage.
“This is really the starting point,” says Zettervall of the research, as her team will be looking to release more data from their study in the coming months.

and taking on new administrative headquarters at the SVS offices in Chicago. The Federation recently staged a session that placed a focus on leadership challenges at the Charing Cross (CX) International Symposium in London, England, while another WFVS run will take place later this year at the 2024 VEITHsymposium in New York City.
The WFVS’ own annual meeting, slated to be hosted by the serving president’s home society, the VSI, in Jaipur, India, in October, will feature two dedicated WFVS sessions. The VSI-WFVS tandem will play host to the recently established inaugural Roger M. Greenhalgh Lectureship, which will be given by Alan Lumsden, MD, the Walter W Fondren III presidential distinguished chair at Houston Methodist’s DeBakey Heart
& Vascular Center in Houston, Texas, and president-elect of the Southern Association for Vascular Surgery (SAVS). Greenhalgh, who passed away in October last year was chairman and founder of the CX Symposium and a world renowned vascular surgeon.
“Overall, we are seeking to bring more consistent representation, more of an international presence to VAM,” Shaw continues. “This allows for more interaction between the member societies around the world, and now allowing for expansion into more research efforts.”
One such WFVS research outreach involves collaboration on rare diseases. The effort is geared toward establishing global guidelines. “This collaboration to develop guidelines for rare diseases is already underway, and, of course, separately, in a similar vein, we are collaborating with the VLFDC.”
Among the other highlights at the WFVS session at VAM, meanwhile, is a presentation from SVS member Vincent L. Rowe, MD, chief of vascular surgery at University of California, Los Angeles (UCLA), in which he will pose the question: “Peripheral arterial disease on the global scale: Are we winning or losing the battle?”
Elsewhere on the program, Syed Mohammed Ali Ahmed, MBBS, from the VSI, will deliver a talk on “Management of lymphedema nostrus verrucosa.”
16 VS@VAM | Wednesday, June 19, 2024
PMEGs
Peter F. Lawrence
TRAINING SVS RESIDENT AND STUDENT PROGRAM BOOSTS INTEREST IN VASCULAR SURGERY AMID WORKFORCE CRISIS
By Jocelyn Hudson
Against the backdrop of a national shortage in the vascular surgery workforce, a recent study has found that the Society for Vascular Surgery (SVS) VAM General Surgery and Medical Student Program “has a positive impact on interest in vascular surgery,” with more than 50% of scholarship recipients matching into the field.
Paula Pinto Rodriguez, MD, a postdoctoral research fellow at the Yale School of Medicine in New Haven, Connecticut, is set to present this finding during the William J. von Liebig Forum (Wednesday, June 19, 8:10–9:45 a.m. in the West Building, Level 3, Skyline Ballroom). Rodriguez will add that the quality of the program and the number of scholarships correlate with vascular surgery Match rates and thus advise that additional investment in similar programs “could help close the gap in the workforce.”
The overarching aim of the study, led by senior author Cassius Iyad Ochoa Chaar, MD, associate professor in surgery at Yale School of Medicine and chair of the SVS Resident and
Student Outreach Committee (RSOC), was to increase interest in the vascular surgery specialty. The SVS RSOC developed a dedicated program for general surgery residents and medical students at VAM and invested in a scholarship program to support attendee expenses, with the study’s main objective being to assess the program’s effectiveness, correlating recipient feedback with likelihood of matching into a vascular surgery training program.

Rodriguez, Chaar and colleagues detail in their abstract that records related to the VAM initiative from 2013–2023 were reviewed, focusing on evaluations of the program. They note that the program included a simulation session from 2013–2019.
Going into the specifics of the study methods, the researchers outline that the average Match rate into vascular surgery was used to divide the data into below-average and above-average groups.
Furthermore, they write that survey responses were based on a five-point Likert scale and allowed for comments, with responses divided into high value, strongly favoring the activity, and low value. The data from years of above- and below-average Match rate were compared.
“Our study demonstrates the positive impact that the program has on trainees’ interest in vascular surgery and highlights the return on investment to our society” CASSIUS IYAD OCHOA CHAAR
The study revealed that the SVS awarded general surgery residents and medical students 1,040 travel scholarships over 10 years.
Rodriguez, Chaar et al found that, overall, applicants had a 43% success rate in receiving a scholarship, with the annual number of applicants increasing, while the number of scholarships and Match success rates significantly decreased over time.
In addition, the research team established that the average Match rate into vascular surgery among scholarship recipients was 50.2%, decreasing over time.
Rodriguez, Chaar and colleagues further detail that the survey response rate was 33%. Results from the survey showed that, during above-average Match rate years, evaluations for simulation allotted time and lectures were significantly more likely to be high value compared to below-average years.
In addition, they reveal that simulation content and residency fair consistently had the most favorable evaluations, and that, overall, the program had a consistently positive impact on recipients’ interest in vascular surgery.
Additional findings include the fact that trainees in the above-average group were significantly more likely to provide positive comments, and that several recipients commented on the need for a dedicated space to interact with faculty and mentors, and highlighted simulation as the standout aspect of the program.
“Our study demonstrates the positive impact that the program has on trainees’ interest in vascular surgery and highlights the return on investment to our society. Expanding this program and developing similar ones in other vascular surgery societies is crucial to keep attracting the brightest trainees to our specialty,” Chaar told VS@VAM ahead of the presentation.
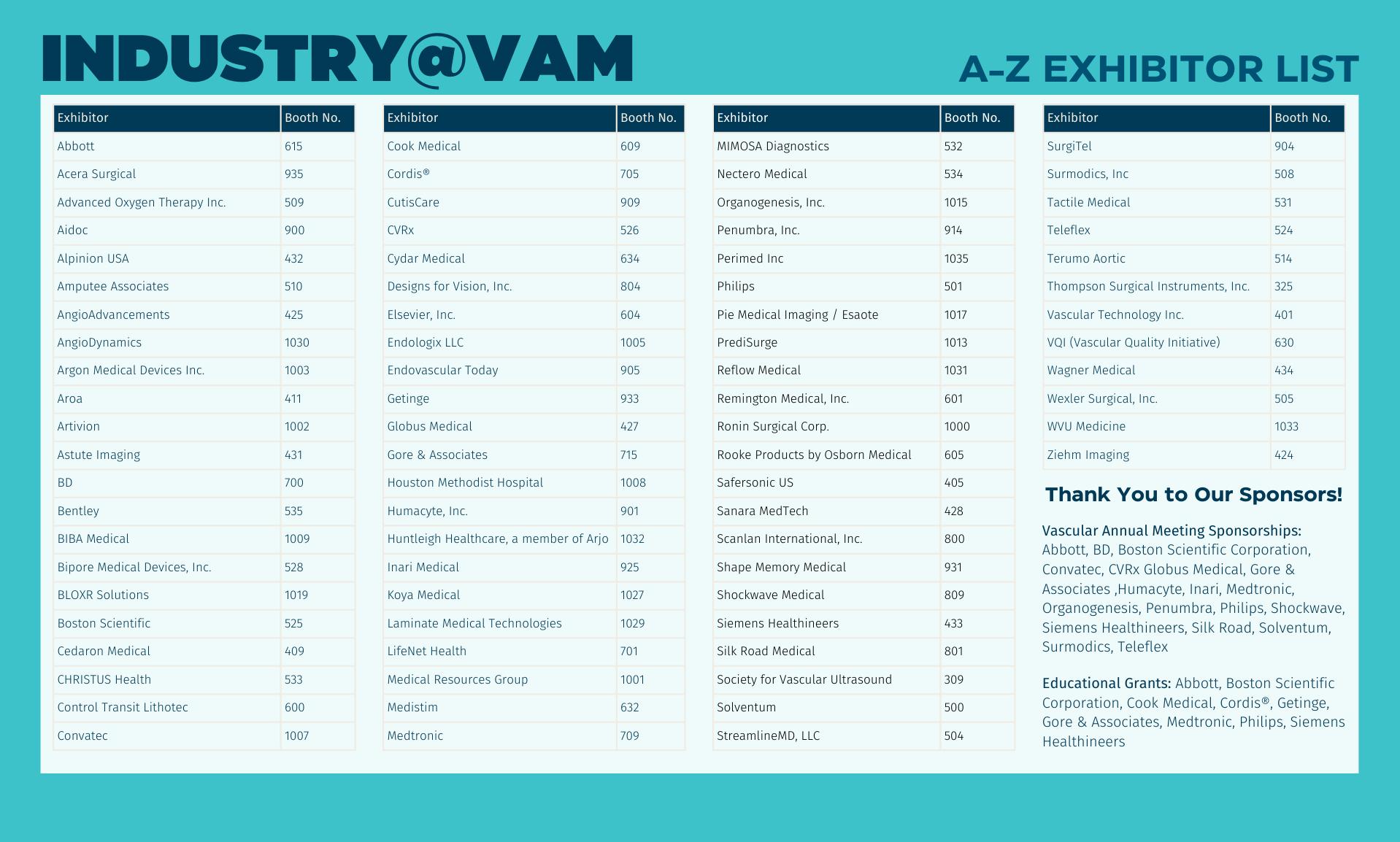
18 VS@VAM | Wednesday, June 19, 2024
Ochao
Cassius Iyad
Chaar
Medical Editor Malachi Sheahan III, MD
Associate Medical Editors
Bernadette Aulivola, MD | O. William Brown, MD | Elliot L. Chaikof, MD, PhD
| Carlo Dall’Olmo, MD | Alan M. Dietzek MD, RPVI, FACS | John F. Eidt, MD | Robert Fitridge, MD | Dennis R. Gable, MD | Linda Harris, MD | Krishna Jain, MD | Larry Kraiss, MD | Joann Lohr, MD
| James McKinsey, MD | Joseph Mills, MD | Erica L. Mitchell, MD, MEd, FACS | Leila Mureebe, MD | Frank Pomposelli, MD | David Rigberg, MD | Clifford Sales, MD | Bhagwan Satiani, MD | Larry Scher, MD | Marc Schermerhorn, MD | Murray L. Shames, MD | Niten Singh, MD | Frank J. Veith, MD | Robert Eugene Zierler, MD
Resident/Fellow Editor
Christopher Audu, MD
Executive Director SVS
Kenneth M. Slaw, PhD
Senior Director for Public Affairs and Advocacy
Megan Marcinko, MPS
Manager of Marketing
Kristin Spencer
Communications Specialist
Marlén Gomez
Published by BIBA News, which is a subsidiary of BIBA Medical Ltd.
Publisher Stephen Greenhalgh
Content Director Urmila Kerslake
Global Commercial Director
Sean Langer
Managing Editor Bryan Kay bryan@bibamedical.com
Editorial contribution Jocelyn Hudson, Will Date, Jamie Bell, Brian McHugh, Éva Malpass and George Barker
Design Terry Hawes
Advertising Nicole Schmitz nicole@bibamedical.com
Letters to the editor vascularspecialist@vascularsociety.org
BIBA Medical, Europe
526 Fulham Road, London SW6 5NR, United Kingdom
BIBA Medical, North America
155 North Wacker Drive – Suite 4250, Chicago, IL 60606, USA
Vascular Specialist is the official newspaper of the Society for Vascular Surgery and provides the vascular specialist with timely and relevant news and commentary about clinical developments and about the impact of healthcare policy. Content for Vascular Specialist is provided by BIBA News. Content for the news from SVS is provided by the Society for Vascular Surgery. | The ideas and opinions expressed in Vascular Specialist do not necessarily reflect those of the Society or the Publisher. The Society for Vascular Surgery and BIBA News will not assume responsibility for damages, loss, or claims of any kind arising from or related to the information contained in this publication, including any claims related to the products, drugs, or services, or the quality or endorsement of advertised products or services, mentioned herein. | The Society for Vascular Surgery headquarters is located at 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. POSTMASTER: Send changes of address (with old mailing label) to Vascular Specialist, Subscription Services, 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. | RECIPIENT: To change your address, e-mail subscriptions@bibamedical.com | For missing issue claims, e-mail subscriptions@bibamedical. com. | Vascular Specialist (ISSN 1558-0148) is published monthly for the Society for Vascular Surgery by BIBA News. Printed by Ironmark | ©Copyright 2024 by the Society for Vascular Surgery
Vascular surgery trainees face the future armed similarly with both open and endovascular skills
The BEST-CLI trial underscores the importance of ensuring trainee competence in open peripheral revascularization as well as endovascular treatment. Indeed, the trial results have called for a reshift in focus to ensure trainees have muchneeded open skills. By Urmila Kerslake
THAT’S BECAUSE, FOR SELECTED PATIENTS, “BYPASSES are actually very relevant.” So says new, multi-institutional data to be showcased on Friday in Plenary Session 5 (8–9:30 a.m. in the West Building, Level 3, Skyline Ballroom), which reveals that trainees do face the future with parity in their graduating operative autonomy and competency in both approaches. Erin Buchanan, MD, a vascular and endovascular fellow at the University of Virginia, Charlottesville, and presenting author of the study, and Libby Weaver, MD, assistant professor of surgery and assistant program director at the same institution, and senior author, spoke to VS@VAM about why these data matter.
“The utilization of endovascular procedures for peripheral arterial disease [PAD] treatment has significantly increased over the years, but open procedures still have a really important impact in vascular care—bypasses are really very relevant. We’re trying to ensure that all vascular trainees, whether they are integrated, or follow the traditional pathway of general surgery training and vascular fellowship, are appropriately achieving competence both in endovascular and open procedures to achieve the right balance in training and patient care,” Buchanan said.
Their study’s conclusion shows just that. “There is no difference in the graduating level of autonomy and competence of endovascular compared to open peripheral revascularization procedures for vascular surgery trainees.”
Buchanan says: “These data are reassuring because vascular surgeons want to confirm that we’re creating safe surgeons who can capably use all the tools in their toolbox and use the wide breadth of their knowledge to take appropriate care of patients. In the setting of appropriate complexity cases, this dataset supports that trainees are ready to care for those patients, no matter what approach they need to use.”
Weaver pivots to those more complex PAD procedures. “When we looked at the most complex procedures, there was a slightly lower level of predicted competence achieved. In those situations, about 70% of the time we expect graduating residents and fellows to be able to competently perform complex procedures, whether they are open or endovascular, which just means that we should expect that with complex cases; even in independent practice, there’s a degree of ongoing mentorship needed.” Buchanan adds: “It’s also not unexpected that in situations where trainees are going out into practice and doing complex cases, they may need assistance from their senior partners.”
Weaver explains that these data follow hot on the heels of a recently presented dataset of nearly 5,000 assessments of open and endovascular procedures for fellows and residents at the Society for Clinical Vascular Surgery (SCVS) annual meeting in March that also show “in general, across the board, our residents and fellows, while they follow two unique pathways, seem to be equally prepared to do open and endovascular procedures.”


Erin Buchanan (top) and Libby Weaver
The big picture takeaway results and specific numbers that are striking, says Weaver, are “assuming average-case complexity and a typical resident, rater and program; the predicted probability of a graduating resident or fellow being rated as autonomous was 96% for endovascular cases and 97% for open procedures. The predicted probability of a graduating resident or fellow being rated as competent was also similar for these cases at 88% for endovascular and 86% for open procedures. In other words, there’s no difference in predicted autonomy or competence upon graduation between open or endovascular cases when trainees perform average complexity peripheral vascular revascularization.”
STUDENTS
MOCK INTERVIEWS AND EXPERT INSIGHTS HIGHLIGHT MEDICAL STUDENT SESSION
BRIGHT AND EARLY THURSDAY morning, June 20 (6:30–8 a.m. in the West Building, Level 1) medical students and general surgery residents can dive into an immersive session designed to introduce them to vascular surgery. It offers a comprehensive overview of the specialty, including hands-on mock interviews and tips for facing residency applications. Students and residents will be greeted by SVS
Outlining the need to capture more nuanced information on true competence rather than just case volume, which Buchanan suggests is merely a surrogate marker of competence, the researchers used the operative performance and autonomy ratings for infrainguinal endovascular and open revascularizations from the Society for Improving Professional Learning (SIMPL) application database for all vascular surgery participating institutions from 2018–2023.
The Vascular Surgery Board (VSB) is supporting the use of this app, which will help implement Entrustable Professional Activities (EPA) for all trainees. While the use of the app is not a requirement, Weaver notes that it will likely be used widely, with required EPA implementation anticipated in early Fall. This dataset, along with a pilot study already underway, is, therefore “a preview of the type of information we can get for our trainees and the way that we can give our trainees good assessments and feedback to help them improve their technical skills and measure pre- and post-operative management of patients as well,” she says.
“There’s no difference in predicted autonomy or competence upon graduation between open or endovascular cases when trainees perform average complexity [procedures]”
LIBBY WEAVER
President Joseph L. Mills, MD, as he gives a welcome with introductory remarks at 6:30 a.m. His introduction will emphasize the importance of preparing for a career in vascular surgery and mastering interview skills.
Following Mills’ welcome, Cassius Iyad Ochoa Chaar, MD, from Yale School of Medicine’s Division of Vascular and Endovascular Surgery, will provide an overview of vascular surgery as a specialty. His focus will center on key aspects of the field.
Earlier this year, Match Day (March 15) yielded data by the National Resident Matching Program that listed 100 open positions for vascular surgery, with 99 positions being filled.
During the mock interview segment, participants can engage in simulated interviews

designed to mimic real-life scenarios, helping students and general surgery residents refine their responses and build their confidence.
The session will conclude with a panel discussion and question-and-answer section, during which attendees will have the chance to seek advice from top-level vascular surgeons.
Marlén Gomez
19 www.vascularspecialistonline.com
PAD
Student breakfast at VAM 2022

PLEASE JOIN US FOR VASCULAR LIVE












VAM Exhibit Hall
McCormick Place West
Chicago, Illinois
Friday, June 21
1:00–1:25 p.m.
Delivering results: Achieving good outcomes in patients with up to 90˚ aortic neck angulation
Gregory Magee, M.D.
Los Angeles, California









Learn more during the Vascular Insights & Practice (VIP) event at VAM24
W. L. Gore & Associates, Inc. Flagstaff, Arizona 86004 goremedical.com
To comply with the AdvaMed Code of Ethics, Gore policies and applicable laws, only participants with a bona fide purpose for attending this Gore event may participate – spouses, family members, other guests or office staff who do not have a legitimate business purpose themselves to participate should not attend Gore events or meals.
Products listed may not be available in all markets.
GORE, Together, improving life and designs are trademarks of W. L. Gore & Associates. © 2024 W. L. Gore & Associates, Inc. 24VS1166-EN01 MAY 2024