Attendees welcomed to ‘more inclusive, more innovative, and more educational’ VAM
By Jocelyn Hudson
“Iurge each one of you to seize this unique opportunity to not only enhance your patient care but also elevate your careers,” SVS President Joseph Mills, MD, advised VAM 2024 attendees during yesterday’s Opening Ceremony.
Mills welcomed delegates to the SVS’ home city of Chicago, stressing that VAM “is not just a series of lectures and presentations, but a platform for inspiration, growth and progress.”
SVS Program Committee Chair Andres Schanzer, MD, also took to the podium, underlining some highlights of this year’s agenda, including Karith Foster’s keynote on “Finishing the journey to inclusivity through belonging, intention and respect” (see p. 15).
Both Schanzer and Postgraduate Committee Chair William Robinson, MD, are due to step down from their roles after VAM 2024. Schanzer personally thanked Robinson for his contribution to the annual meeting, remarking: “VAM today does not look or feel like the VAM in past years—it’s more inclusive, it’s more innovative, and it’s more educational—and much of that positive change has been a direct result of Dr Robinson’s vision for continued growth and evolution.”
ENDOVASCULAR CFA TREATMENT ASSOCIATED WITH INCREASED RATE OF LONG-TERM CFA-SPECIFIC REINTERVENTION, STUDY FINDS
By Jocelyn Hudson
02 Carotid disease
How do CEA, TF-CAS and TCAR compare?
04 Aortic disease
One-year AAA device data emerge
09 Vascular nursing SVN conference comes to a close
11 Photo gallery VAM 2024 through the lens
14 WFVS Global PAD burden explored
15 Keynote speaker
Karith Foster delivers DEI pearls of wisdom
www.vascularspecialistonline.com

A RECENT STUDY SUGGESTS THAT endovascular treatment of the common femoral artery (CFA) is associated with an increased rate of long-term CFA-specific reintervention, regardless of indication. Nicholas Wells, MA, a medical student at Yale School of Medicine in New Haven, Connecticut, presented this and other key findings from a tertiary care center analysis of open and endovascular treatment of the CFA during yesterday’s William J. von Liebig Forum.
“The CFA is a common site of disease in patients with peripheral arterial disease,” Wells began. He noted that endarterectomy is seen as the gold standard of treatment, with primary patency rates “often surpassing 95% at five years” and evidence of “excellent long-term durability as far out as eight years.”
The objective of the study, Wells shared,
See page 2
Jumping into day two of VAM 2024, attendees can expect another day of varied science, education and other meeting festivities: award ceremonies, special sessions, the opening of the Exhibit Hall and more.
Among them are the General Surgery Resident/ Medical Student Session: Mock Interviews, which is an opportunity for trainees on the traditional track and students to get a feel for the interviews that will soon be in their headlights. The mock interviews will run from 6:30–8 a.m.
At 9:30 a.m., the John Homan’s Lecture (see story on p. 13) will focus on what can be learned from international variations in vascular care.
Immediately following will be the Awards Ceremony, where the 2024 Lifetime Achievement Award winners along with many others will be honored.
The afternoon will feature the fan favorite “How I Do It” video session, along with two membership sections, including the SVS Community Practice Section session focused on the optimization of clinical practice, and the SVS Section on Outpatient and Office Vascular Care session, which will present findings from grant and award recipients.
Other events will cover topics like a multidisciplinary approach to limb salvage, dialysis creation and more. Join the Opening Reception in the Exhibit Hall at 5 p.m. happening in conjunction with the International Poster Competition and the Interactive Poster Session.—Kristin Spencer

THE OFFICIAL NEWSPAPER OF THE
In this issue: THURSDAY 20 JUNE 2024 | CONFERENCE EDITION 2
DAY TWO HIGHLIGHTS SPOT LIGHT OPENING CEREMONY OPEN/ENDO
#VAM24Turntopage8fordailyplanner
CAROTID DISEASE
TCAR and endarterectomy both ‘reasonable’ but stenting linked to worse outcomes in kidney disease patients
A study examining outcomes between different carotid revascularization procedures has concluded that transcarotid artery revascularization (TCAR) and carotid endarterectomy (CEA) both represent a “reasonable choice” in severe chronic kidney disease (CKD) and hemodialysis patients—but transfemoral carotid artery stenting (TF-CAS) appears more likely to result in worse outcomes.
By Jamie Bell
“AND, ADDITIONALLY, THE MAJORITY OF THESE patients are surviving long enough to benefit from the stroke risk reduction provided by surgery,” said Elisa Caron, MD, research fellow in vascular surgery at Beth Israel Deaconess
FROM THE COVER ENDOVASCULAR CFA TREATMENT ASSOCIATED WITH INCREASED RATE OF LONGTERM CFA-SPECIFIC REINTERVENTION, STUDY FINDS
continued from page 1
was to compare open and endovascular treatment of the CFA with a focus on reinterventions and major adverse limb events.
This was a retrospective study of all revascularizations involving the CFA, including repeated reinterventions, conducted at a single center between 2013 and 2020. “These procedures were performed by various specialists, including vascular surgeons, interventional radiologists and interventional cardiologists,” Wells detailed, adding that the researchers used standard comparative statistics and stratified their analysis by indication— claudication versus chronic limb-threaten-
Medical Center in Boston, Massachusetts. During yesterday’s Plenary Session 2, Caron reported an analysis of Vascular Quality Initiative (VQI) patients with estimated glomerular filtration rate (eGFR) <30ml/min/1.73m2, or on hemodialysis, undergoing TCAR, CEA or TF-CAS between 2016 and 2023.
Presenting on behalf of her co-authors, including senior author Marc L. Schermerhorn, MD, chief of vascular and endovascular surgery at Beth Israel Deaconess Medical Center, Caron relayed data from 13,042 VQI patients with eGFR <30, 2,355 of whom were on hemodialysis.
The majority of outcomes—across both symptomatic and asymptomatic patients—were found to be “fairly similar” between TCAR and CEA, including stroke/death, with both procedures falling within SVS guidelines regarding perioperative stroke and death. However, CEA was linked with a trend towards slightly higher odds of stroke/death/myocardial infarction (MI), as per the analysis’ primary outcome, in addition to higher odds of MI when considered independently. Similar trends continued when the researchers looked specifically at the subgroup of hemodialysis-only patients, according to Caron.
Turning to findings on overall long-term survival, the presenter relayed that CEA and TCAR were once again similar, as survival rates were nearly 80% with both procedures across all asymptomatic patients and only dropped slightly to around 70% in the hemodialysis-only group at five years. She also noted that these trends endured among symptomatic patients, with rates dropping to around 70% across the full eGFR <30 and hemodialysis cohort.
In addition, regarding those who underwent TF-CAS, Caron reported that—prior to statistical weighting—these patients were more likely to be symptomatic, to present with stroke, and to undergo surgery in urgent/emergent settings, compared to TCAR and CEA patients. They also had more baseline comorbidities. But, “even after weighting
ing ischemia (CLTI).
The researchers found that, from their database of 1,954 patients, 23% were treated for the CFA at least once, and 15% of all individual revascularizations involved the CFA.
“Patients with claudication were more likely to be treated initially with endovascular therapy, at 57%, and those with CLTI were more likely to be treated with open surgery, at 60%,” Wells added.
The presenter reported that approximately one-third of the open surgery group underwent extended CFA endarterectomy involving the external iliac arteries, superficial femoral artery, and profunda femoral arteries, and about onethird underwent a concomitant ipsilateral bypass.
He also noted that approximately half of the patients in the endovas cular group underwent concomitant endovascular revascularization of the distal femoropopliteal region.
In the perioperative period, Wells shared that open surgery was associated with an increased rate of bleeding and wound infection, while endovas cular therapy was associ ated with shorter mean length of hospital stay. Perioperative major amputation and mor-
 Elisa Caron
Elisa Caron
for symptom status and comorbidities, TF-CAS still underperformed and did not meet SVS guidelines” she continued, with stroke, death and overall long-term survival being among the areas where TF-CAS produced inferior outcomes versus TCAR and CEA, across both asymptomatic and symptomatic patients. Following Caron’s presentation, session moderator Chelsea Dorsey, MD, associate professor of surgery at UChicago Medicine in Illinois, commented that “these patients are incredibly fragile” and, as such, “the more granular information we have about how to approach them, the better.” Dorsey went on to ask the presenter how she feels these new data may impact people’s clinical practices moving forward.
“I think that patient selection will always play a big role,” Caron responded. “The VQI certainly gives us very granular data but, at the end of the day, it’s not the same as the patient sitting in front of you, and I think that will still have a big impact. That said, I think it’s at least reasonable to consider surgery in these patients [...] But, again, patient selection is still going to be crucial.”
“The VQI certainly gives us very granular data but, at the end of the day, it’s not the same as the patient sitting in front of you, and I think that will still have a big impact”
ELISA CARON
tality were below 1% in both groups.
“For claudication, endovascular therapy led to an increased rate of CFA-specific reintervention in the long term—35% compared to just 21% of those initially treated with open surgery,” Wells revealed.
“Additionally,” he continued, “15% of those who initially received endovascular treatment required eventual conversion to endarterectomy of the CFA, while only 5% of those who were initially treated with open surgery required a redo open CFA with endarterectomy.”
The researchers observed similar outcomes in the CLTI group, where 33% of initial endovascular recipients required eventual CFA reintervention compared to 21% of those initially treated with open surgery. Conversion to endarterectomy was not found to be significant in this subgroup.

“The take-home message here was that endovascular therapy led to higher rates of CFA reintervention in the long term and that for claudicants, conversion to endarterectomy was more common following end-
ovascular therapy than redo endarterectomy,” the presenter told VAM attendees.
After a median follow-up time of three to four years, major amputation, major adverse limb events and mortality were not found to be different. Furthermore, major adverse limb events-free survival—which was defined as time to either reintervention to any artery, major amputation or death—was not found to be significantly different between treatment approaches in either subgroup.
Senior author Cassius Iyad Ochoa Chaar, MD, told VS@VAM that the anatomy of the CFA is “very peculiar,” and that the extent of the disease treated was not accounted for in this analysis.
“Our future work will focus on studying the anatomy of the atherosclerosis affecting the CFA to better understand which lesions are best treated with which strategy of revascularization,” he commented.
“The CFA is a common site of disease in patients with peripheral arterial disease” NICHOLAS WELLS
2 VS@VAM | Thursday, June 20, 2024
Nicholas Wells
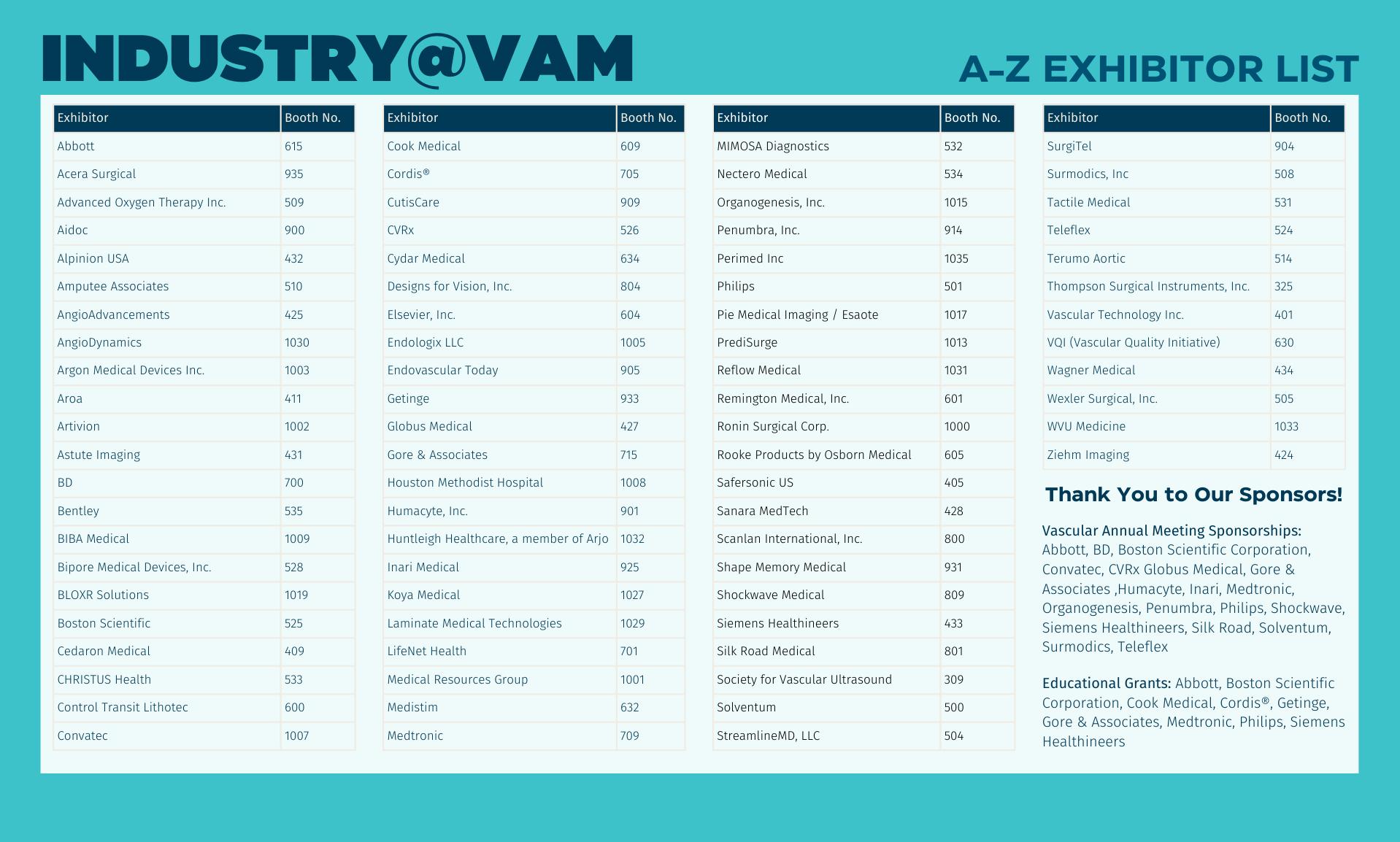
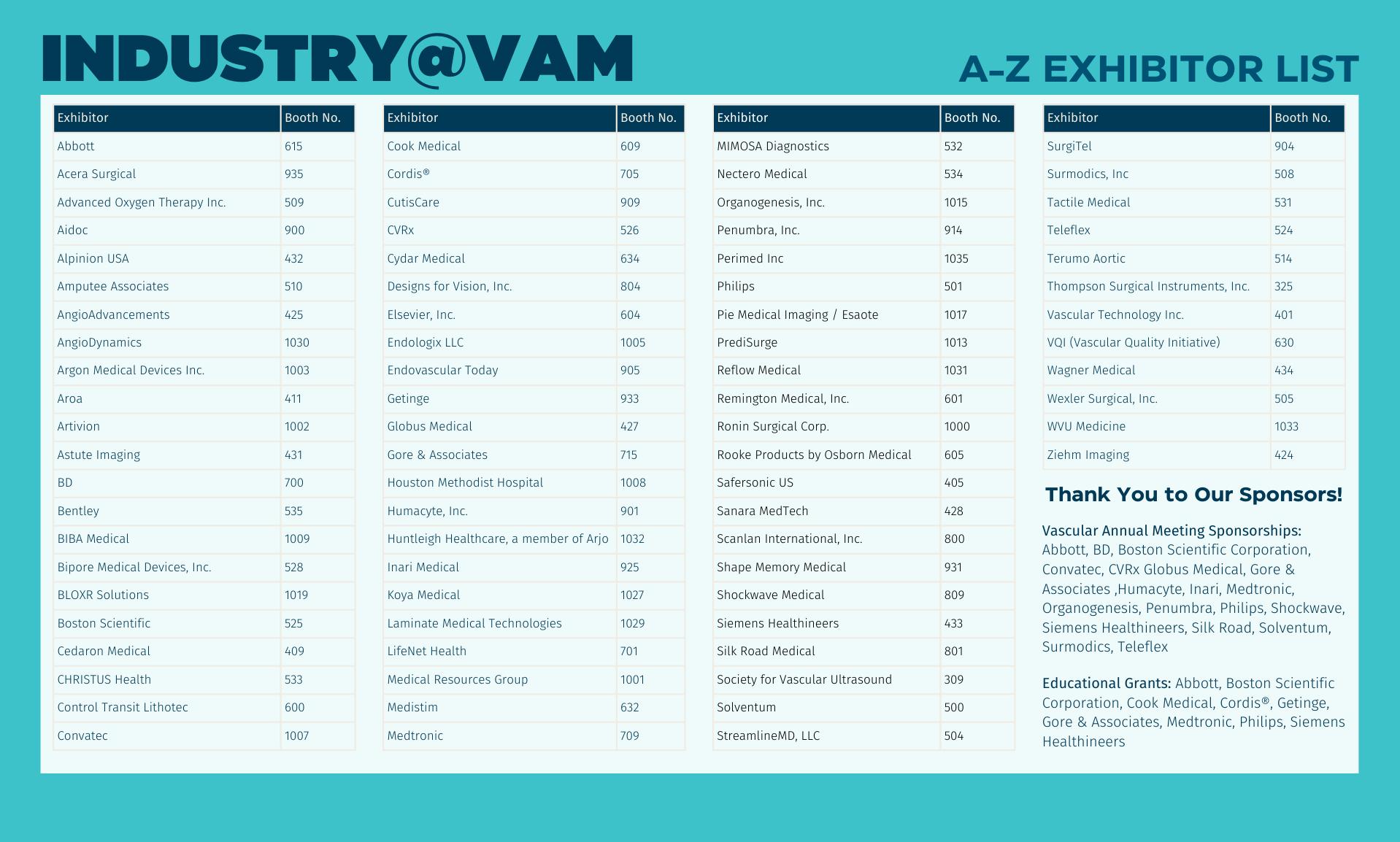
The only one.1
Endurant™ AAA stent graft system
The first and only EVAR system with a decade of global registry outcomes1
94.7% FF aneurysm-related mortality (ARM)†
64.1% Sac regression‡
Visit us in booth 709 as we celebrate over a decade of experience with the Endurant™ AAA stent graft system.
†Data reported through 10-year time frame with full + extended cohort, determined by Clinical Event Committee. ‡Data reported through 10-year time frame with full + extended cohort.
1 Verhagen, et al. The ENGAGE Registry: Ten-Year Outcomes with the Endurant Stent Graft for Endovascular Abdominal Aortic Aneurysm Repair. Presented at: Charing Cross 2023 International Symposium; April 26, 2023; London, UK.


Indications The Endurant™ II/Endurant™ IIs bifurcated stent grafts are indicated for the endovascular treatment of infrarenal abdominal aortic or aortoiliac aneurysms. They may be utilized in conjunction with the Heli-FX EndoAnchor system when augmented radial fixation and/or sealing is required; in particular, in the treatment of abdominal aortic aneurysms with short (≥ 4 mm and < 10 mm) infrarenal necks (see Neck length definition below). The Endurant II stent graft system aorto-uni-iliac (AUI) stent graft is indicated for the endovascular treatment of infrarenal abdominal aortic or aortoiliac aneurysms in patients whose anatomy does not allow the use of a bifurcated stent graft. The Endurant II/IIs stent graft system is indicated for use in patients with the following characteristics: • Adequate iliac or femoral access that is compatible with vascular access techniques, devices, or accessories • Proximal neck length of ≥ 10 mm; or ≥ 4 mm and < 10 mm when used in conjunction with the Heli-FX EndoAnchor system (bifurcated stent graft only) Note: Neck length is defined as the length over which the aortic diameter remains within 10% of the infrarenal diameter. • Infrarenal neck angulation of ≤ 60° • Aortic neck diameters with a range of 19 to 32 mm • Distal fixation length(s) of ≥ 15 mm • Iliac diameters with a range of 8 to 25 mm • Morphology suitable for aneurysm repair
Contraindications
The Endurant II/Endurant IIs stent graft system is contraindicated in: • patients who have a condition that threatens to infect the graft • patients with known sensitivities or allergies to the device materials. When used with the Heli-FX EndoAnchor system, the Endurant II/IIs stent graft system is also contraindicated in: • patients with known sensitivities to the EndoAnchor implant materials. For contraindications regarding ancillary devices used with the Endurant II/Endurant IIs stent graft system, refer to the Instructions for Use provided with the device.
Warnings and Precautions
• The long-term safety and effectiveness of the Endurant II/Endurant IIs stent graft system has not been established. All patients should be advised that endovascular treatment requires lifelong, regular follow-up to assess the health and the performance of the implanted endovascular stent graft. Patients with specific clinical findings (e.g., endoleaks, enlarging aneurysms, changes in the structure or position of the endovascular graft), or less than the recommended number of EndoAnchor implants when used in short proximal necks (≥ 4 mm and < 10 mm), should receive enhanced follow-up. Specific follow-up guidelines are described in the Instructions for Use.
• Patients experiencing reduced blood flow through the graft limb, aneurysm expansion, and persistent endoleaks may be required to undergo secondary interventions or surgical procedures. • The Endurant II/Endurant IIs stent graft system is not recommended in patients unable to undergo or who will not be compliant with the necessary preoperative and postoperative imaging and implantation procedures as described in the Instructions for Use. • Renal complications may occur: 1) From an excess use of contrast agents. 2) As a result of emboli or a misplaced stent graft. The radiopaque marker along the edge of the stent graft should be aligned immediately below the lower-most renal arterial origin. • Studies indicate that the danger of micro-embolization increases with increased procedure duration. • The safety and effectiveness of the Endurant II/Endurant IIs stent graft system has not been evaluated in some patient populations. Please refer to the product Instructions for Use for details.
MRI Safety and Compatibility: Non-clinical testing has demonstrated that the Endurant II/Endurant IIs stent graft is MR Conditional. It can be scanned safely in both 1.5T & 3.0T MR systems under certain conditions as described in the product Instructions for Use For additional MRI safety information, please refer to the product Instructions for Use
Adverse Events
Potential adverse events include (arranged in alphabetical order): amputation; anesthetic complications and subsequent attendant problems (e.g., aspiration), aneurysm enlargement; aneurysm rupture and death; aortic damage, including perforation, dissection, bleeding, rupture and death; arterial or venous thrombosis and/or pseudoaneurysm; arteriovenous fistula; bleeding, hematoma or coagulopathy; bowel complications (e.g., ileus, transient ischemia, infarction, necrosis); cardiac complications and subsequent attendant problems (e.g., arrhythmia, myocardial infarction, congestive heart failure, hypotension, hypertension); claudication (e.g., buttock, lower limb); death; edema; EndoAnchor system (for infrarenal EVAR procedures using the Heli-FX EndoAnchor system): partial deployment, inaccurate deployment, fracture, dislodgement, embolization, stent graft damage, modelling balloon damage); embolization (micro and macro) with transient or permanent ischemia or infarction; endoleak; fever and localized inflammation; genitourinary complications and subsequent attendant problems (e.g., ischemia, erosion, femoral-femoral artery thrombosis, fistula, incontinence, hematuria, infection); hepatic failure; impotence; infection of the aneurysm, device access site, including abscess formation, transient fever and pain; lymphatic complications and subsequent attendant problems (e.g., lymph fistula); neurologic local or systemic complications and subsequent attendant problems (e.g., confusion, stroke, transient ischemic attack, paraplegia, paraparesis, paralysis); occlusion of device or native vessel; pulmonary complications and subsequent attendant problems; renal complications and subsequent attendant problems (e.g., artery occlusion, contrast toxicity, insufficiency, failure); stent graft: improper component placement; incomplete component deployment; component migration; suture break; occlusion; infection; stent fracture; graft twisting and/or kinking; insertion and removal difficulties; graft material wear; dilatation; erosion; puncture and perigraft flow; surgical conversion to open repair; vascular access site complications, including infection, pain, hematoma, pseudoaneurysm, arteriovenous fistula, dissection; vascular spasm or vascular trauma (e.g., iliofemoral vessel dissection, bleeding, rupture, death); vessel damage; wound complications and subsequent attendant problems (e.g., dehiscence, infection, hematoma, seroma, cellulitis).
Please reference product Instructions for Use for more information regarding indications, warnings, precautions, contraindications, and adverse events.
Caution: Federal (USA) law restricts this device to sale by or on the order of a physician.
UC202500741 EN ©2024 Medtronic. All rights reserved. Medtronic and the Medtronic logo are trademarks of Medtronic. All other brands are trademarks of a Medtronic company. 05/2024
One-year results confirm safety and efficacy results of conformable AAA device in highly angulated necks
Results of a sub-study from the pivotal Investigational Device Exemption (IDE) trial assessing Gore’s Excluder conformable abdominal aortic aneurysm (AAA) endoprosthesis have shown that the device is safe and effective in hostile angulated neck anatomy, with the results maintained out to one-year. By Will Date
MAHMOUD ALMADANI, MD, FROM MAIMONIDES Health in Brooklyn, New York, presented the new data during yesterday’s (Wednesday, June 19) William J. von Liebig Forum.
The analysis involved 95 patients who were enrolled in the IDE trial, a prospective, multicenter clinical trial conducted at 35 U.S. sites between January 2018 and February 2022. To be included in the high neck angulation sub-study, patients had to have an infrarenal aortic neck angulation of >60˚and ≤90˚with an aortic neck length ≥10mm.
Gore’s Excluder conformable AAA device first gained Food and Drug Administration (FDA) approval in late 2020, with an expanded indication for patients with aortic neck angulation ≤90° and a minimum length of 10mm approved last month (May 2024).
The device is comprised of a conformable stent graft with enhanced positioning and optional angulation control. It also includes a mechanism that, after the first stage of deployment, constrains the device to 70% of its full diameter,
which is intended to allow for manipulation and angulation of the proximal end of the stent graft.
“This is the pinnacle of the study, the device was designed for patients with high neck angulation,” Almadani said during his presentation. “Many of you in the audience have experience using this device in a high neck angle situation, and I will present the data to justify its use.”
Patients enrolled in the study had a mean age of 74 years old, were predominantly White and non-Hispanic, and were predominantly male, Almadani detailed, acknowledging this as one of the limitations of the study, but also that this represents the typical distribution of aortic aneurysm disease expected in this type of study.
In terms of the anatomic characteristics, Almadani noted that patients had a mean neck angle of 71˚, with a mean aortic neck length of 21mm. The most common comorbidities included hypertension, hypercholesterolemia and tobacco use.
Technical success—which was defined as a composite of successful access, deployment, removal of delivery catheters, patent and access site closure, and absence of site-reported type I or type III endoleak—was achieved in 97.9% of patients, Almadani reported, with two patients noted to have a type I endoleak at the completion of the procedure, which resolved without intervention by one-month follow-up.
Almadani
97.6% of patients.
The primary effectiveness endpoint—a composite of technical success and freedom from a type I and III endoleak at 12 months, as well as migration of >1cm and sac enlargement >5mm between one and 12 months, AAA rupture and conversion to open repair through 12 months—was recorded in 94.8% of patients for whom data were available at one year.
Sub-group analysis looking at high-risk patients with high neck angles and short necks (10–15mm) showed that in 21 patients analyzed at one year, there were no type I and III endoleaks, no graft migration, sac expansion, or open conversions showing excellent results in high aortic necks.

Freedom from the primary safety endpoint—a composite of procedural blood loss >1,000mL, death, stroke, myocardial infarction, bowel ischemia, paraplegia, respiratory failure, renal failure, and thromboembolic events—was achieved in
“I think this device is ideal in a situation where you have an anatomically high-risk patient, with a highly angulated neck, and you want to try to maintain an infrarenal seal zone”
CAS PATIENT SELECTION MAY EXPLAIN ‘COUNTERINTUITIVE’ RELATIONSHIP BETWEEN CAROTID STENTING VOLUME AND OUTCOMES IN NEW STUDY
By Jamie Bell
HIGH STROKE AND DEATH RATES
relating to carotid stenting in the Pacific Northwest may be driven by the selection of high-risk patients with less than 80% stenosis, and reducing the frequency of stenting in this high-risk group—along with better adherence to guidelinerecommended medical management— could improve regional outcomes. This was among the key concluding messages delivered yesterday by Rahul Ghosh, MS, during one of the VAM 2024 Vascular and Endovascular Surgery Society
(VESS) Scientific Sessions as he presented findings from a retrospective review of asymptomatic carotid stenosis patients in the Pacific Northwest region undergoing transcarotid artery revascularization (TCAR) and transfemoral carotid artery stenting (TF-CAS), within the Vascular Quality Initiative (VQI), from 2016 to 2022. The research was conducted at the University of Washington in Seattle and led by senior author Sara L. Zettervall, MD. “Education and awareness are critical for improving care,” said Ghosh,
“The conformable IDE demonstrates the safety and effectiveness of the Gore Excluder conformable device,” Almadani said in his concluding remarks. “This was also preserved at one year, and we believe this is a new frontier for safely treating high-risk aortic neck patients with an infrarenal sealing AAA device.”
During discussion that followed Almadani’s presentation, he was asked by session co-moderator Andres Schanzer, MD, on the “sweet spot” for the device, given other treatment options, including fenestrated grafts and endoanchors.
“I think this device is ideal in a situation where you have an anatomically high-risk patient, with a highly angulated neck, and you want to try to maintain an infrarenal seal zone without having to extend and manipulate the visceral vessels and place parallel stents or suprarenal stents,” Almadani responded.
Attendees of Thursday morning’s Plenary Session 4 (10:45 a.m.–12 p.m. in the West Building, Level 3, Skyline Ballroom) will hear insights on the use of the Gore Excluder thoracoabdominal branch endoprosthesis (TAMBE) for complex aneurysm repair, with the presentation of 30-day outcomes of the TAMBE pivotal trial, which will be delivered by Mark A. Farber, MD, from University of North Carolina, Chapel Hill, North Carolina. The non-randomized, two-armed prospective study took place across 35 investigative sites, studying the use of the device in the treatment of thoracoabdominal (TAAA) and pararenal aortic aneurysms.
a final-year MD/PhD student at Texas A&M University in Houston, speaking to VS@VAM in light of these findings. “By leveraging registry data to analyze real-world outcomes, surgeons can gain a clearer understanding of how practice patterns affect quality, enabling more informed decisions about when to intervene in asymptomatic patients— particularly those with significant comorbidities.”
Ghosh reported that 1,154 asymptomatic patients across 27 centers underwent carotid stenting in the Pacific Northwest from 2016 to 2022, of which 77% received TCAR and 23% received TFCAS. The overall stroke/death rates were roughly 3% for both TCAR and TF-CAS, with center-specific rates ranging from 0–6% for TCAR and 0–17% for TF-CAS. Researchers also found that centers with higher stroke/death rates generally treated fewer patients with >80% stenosis, as well as more patients with high-risk anatomy or physiology.
Following Ghosh’s presentation, Jordan
R. Stern, MD, associate professor of surgery at Weill Cornell Medical College in New York, commented that another of the study’s findings—that being the fact that all centers with stroke/death rates above 3% ranked among the top half of centers for TCAR and TF-CAS volumes in asymptomatic patients— suggests something of a “counterintuitive relationship” between case volume and stroke risk.
“We know from a myriad of literature […] that higher volume generally leads to better outcomes; what’s your explanation for that?” Stern asked the presenter.
Ghosh conceded that, with this having been an observational study, it is difficult to draw conclusions on any causal relationship, or whether volumes “play into” the high stroke/death rate.
“Of course, patient selection is a big thing,” he added. “The centers with the high stroke and death rates—you could also say they are getting the sicker patients so, maybe, their outcomes are worse [because of that].”

4 VS@VAM | Thursday, June 20, 2024
Mahmoud
COMPLEX AORTIC
PERIPHERAL IVL

Shockwave Peripheral IVL: Reliably safe. Predictably effective. Backed by real-world and level one evidence, Shockwave IVL modifies both superficial and deep calcium. Designed for the iliacs, fem-pop and below-the-knee arteries, these purpose-built devices come in sizes that allow you to treat calcium at any level. So you can count on affecting outcomes for the better.

Peripheral Important Safety Information
In the United States: Rx only.
Indications for Use—The Shockwave Medical Intravascular Lithotripsy (IVL) System is intended for lithotripsy-enhanced balloon dilatation of lesions, including calcified lesions, in the peripheral vasculature, including the iliac, femoral, ilio-femoral, popliteal, infra-popliteal, and renal arteries. Not for use in the coronary or cerebral vasculature.
Contraindications—Do not use if unable to pass 0.014” (M5, M5+, S4) or 0.018” (L6) guidewire across the lesion-Not intended for treatment of in-stent restenosis or in coronary, carotid, or cerebrovascular arteries.
Warnings—Only to be used by physicians who are familiar with interventional vascular procedures—Physicians must be trained prior to use of the device— Use the generator in accordance with recommended settings as stated in the Operator’s Manual.
Precautions—use only the recommended balloon inflation medium—Appropriate anticoagulant therapy should be administered by the physician—Decision regarding use of distal protection should be made based on physician assessment of treatment lesion morphology.
Adverse effects–Possible adverse effects consistent with standard angioplasty include–Access site complications –Allergy to contrast or blood thinner–Arterial bypass surgery—Bleeding complications—Death—Fracture of guidewire or device—Hypertension/Hypotension—Infection/sepsis—Placement of a stent—renal failure—Shock/pulmonary edema—target vessel stenosis or occlusion—Vascular complications. Risks unique to the device and its use—Allergy to catheter material(s)— Device malfunction or failure—Excess heat at target site. Prior to use, please reference the Instructions for Use for more
©2024 Shockwave Medical Inc. All rights reserved. SPL-70888 Rev A Learn more at ShockwaveMedical.com/Peripheral-IVL COUNT ON IT THE SOUND CALCIUM SOLUTION
information on indications, contraindications, warnings, precautions and adverse events. www.shockwavemedical.com/IFU
VASCULAR COMMUNITY HAS A ROLE TO PLAY IN ENSURING SAFETY OF AORTIC DEVICES
PHYSICIAN-SPONSORED
Investigational Device Exemption (IDE) trials have an important role to play in the continued development and refinement of aortic endovascular devices, attendees of a panel session on aortic device regulation heard yesterday.
The session, taking place Wednesday lunchtime, set out the various Food and Drug Administration (FDA)-mandated pathways that a device must follow before it can enter the market, as well as looking at the involvement of vascular surgeons in this process. Speakers from the FDA outlined the agency’s priorities in ensuring the safety of devices that are approved for use, while balancing the need to encourage innovation.
Considerable innovation has resulted
NEW TECHNOLOGY
from physician-sponsored IDEs focused on treating patients with complex aortic aneurysms. “There have been substantive learnings that have really contributed tremendously to the development of future clinical studies, to device design modifications and really have helped the endovascular aortic space move forward for many years,” Ronald Fairman, MD, FDA's Vascular and Endovascular Devices (VEDT) medical officer, and a former SVS president, said during his presentation examining the role of physician-sponsored IDEs.
Fairman outlined the similarities and differences between corporate and physician-initiated IDEs, including the circumstances in which the FDA may recommend the submission of an IDE,
citing the example of the use of physicianmodified devices or where a commercial device is routinely being used for a new indication.
“It is important to acknowledge, the FDA does not regulate the practice of medicine,” said Fairman. “If you are modifying a device to save someone's life, the FDA does not get involved in that. You do not need a investigator-sponsored IDE for that.
“On the other hand, if you are modifying a commercial aortic device or using a commercial device for a new indication and you are doing it routinely, and you are collecting safety and efficacy data to see if it works, we would continue to recommend a sponsored-investigator IDE.”
Gustavo Oderich, MD, professor of surgery and chair of vascular and endovascular surgery at the University of Texas Health Science Center at Houston, shared his considerable experience in physician-sponsored IDEs, and outlined several important developments to have emerged from this setting, in particular in
the development of fenestrated-branched endovascular technologies.
“Physician-sponsored IDEs provide a safe venue for continued access, innovation and refinement of endovascular techniques,” Oderich said, setting out several scenarios in which these trials add value. “These often represent the highest level of data for the specialty, and even after a device is approved new iterations will continue to be needed.”
FDA medical officer Robert Craig, DO, outlined the agency’s approach to postmarket data collection and underscored the importance of vascular surgeons participating in the postmarket clinical studies that FDA requires for aortic endografts as a condition of premarket approval (PMA) application.
To conclude the session, moderator and FDA VEDT medical officer Robert E. Lee, MD, outlined the regulatory requirements for medical device event reporting. He underscored the importance of vascular surgeons voluntarily reporting the adverse medical device events encountered in practice using the FDA MedWatch system.
Artificial intelligence: Breakfast session explores opportunities and risks for vascular surgery
The advent of artificial intelligence (AI) in vascular surgery holds great promise to optimize the delivery of care, with prospective uses including patient selection and procedural planning. Yet, challenges remain. By Will Date.
MANY STILL VIEW AI WITH SUSPICION, AND important ethical and security questions over its use remain. A session taking place Thursday, June 20 at 7:00 a.m. (West Building, Level 1) will explore these issues, and look at current and future uses of AI in the vascular space. Session moderator Judith Lin, MD, MBA, professor and chief of vascular surgery at Michigan State University College of Human Medicine, East Lansing, Michigan and Javairiah Fatima, MD, an associate professor of surgery at Georgetown University, Washington, D.C., spoke to VS@ VAM about opportunities and challenges for AI in vascular, and what attendees can expect from the session.
VS@VAM: What do you see as being the main uses for AI in the vascular field?
JL: AI has the potential to revolutionize healthcare. AI can enhance diagnostic accuracy, improve patient outcomes, and streamline clinical workflows. Specifically in the field of vascular surgery, the main uses of AI include image analysis to identify aneurysms or thrombosis, predictive models of adverse events, decision support to provide evidence-based recommendations, robotic-assisted surgery to enhance precision and dexterity, automated alerts for graft occlusion, natural language processing and large language models to summarize patient history and make recommendations for personalized treatment.
VS@VAM: Is vascular surgery ready for the advent of AI?
JF: AI has been around for a long time in various forms, we are currently enhancing its use in very specific situations to enhance patient care and technological development. So I would say yes, there is acceptance and utilization.

VS@VAM: Are there good examples of how AI is currently used in vascular surgery?
JF: Artificial intelligence is being used to diagnose aortic aneurysms, assist in preoperative planning and in treatment.
Similarly, it has played a role in timely detection of peripheral arterial disease (PAD), pulmonary embolisms, and strokes on imaging done for other indications and routing them to the appropriate personnel for timely intervention.
The ability of AI to analyze large amounts of data, using deep learning analysis to detect patterns, perform risk stratification and draw conclusions surpasses human capacities and has already proven beneficial to patient treatment and outcomes.
“AI is a powerful tool, but it should complement clinical judgement rather than replace it”
JUDITH LIN
VS@VAM: Will AI replace physician judgement?
JL: No. AI will enhance clinical decision-making. AIpowered decision support tools provide evidence-based recommendations to clinicians during diagnosis and treatment planning. AI is a powerful tool, but it should complement clinical judgement rather than replace it. I think physicians who use AI will replace those who don't.
VS@VAM: Can we trust AI?
JF: This is a million-dollar question! I think checks and balance are critical to its ethical and unbiased use. It is incumbent on us to develop algorithms with proper testing and careful and cautious implementation with the highest standards in patient safety.
VS@VAM: How can vascular surgeons prepare themselves for more AI in their daily practice?
JL: Vascular surgeons can prepare themselves for more AI in their daily practice by staying informed about AI developments in medicine and surgery, collaborating with data scientists to develop AI models and algorithms, and investigating relevant existing AI tools and applications.
VS@VAM: What should attendees expect to gain from attending the AI session?
JF: The VAM AI session has an excellent line-up of national leaders in the field who are dedicated to development and implementation of AI to optimize patient care. It’s an excellent opportunity for an interactive discussion on the topic.



6 VS@VAM | Thursday, June 20, 2024 FDA
PREVIEW
Revolutionizing the Treatment of ALI Patients.
The Auryon System’s versatile approach, combining laser and aspiration technology, allows for the treatment of Acute Limb Ischemia (ALI) patients in a single session1-3
Clear all lesion
thrombus to severe calcification, with a single device Advanced
Safety at the forefront. Treat with confidence by minimizing the risk of embolization

RISK INFORMATION
Caution: Federal (USA) law restricts the use of the system by or on the order of a physician.

Refer to Directions for Use and/or User Manual provided with the product for complete Instructions, Warnings, Precautions, Possible Adverse Effects and Contraindications prior to use of the product. INDICATIONS FOR USE
The Auryon Atherectomy System and Auryon Atherectomy Catheters with aspiration are indicated for use as atherectomy devices for arterial stenoses, including in-stent restenosis (ISR), and to aspirate thrombus adjacent to stenoses in native and stented infra-inguinal arteries.
The Auryon Atherectomy System and Auryon Atherectomy Catheters without aspiration are indicated for use in the treatment, including atherectomy, of infra-inguinal stenoses and occlusions.
1. Rundback J, Chandra P, Brodmann M, et al. Novel laser-based catheter for peripheral atherectomy: 6-month results from the Eximo Medical B-LaserTM IDE study. Catheter Cardiovasc Interv. 2019;94(7):1010-1017.
2. Shammas NW, Chandra P, Brodmann M, et al. Acute and 30-day safety and effectiveness evaluation of Eximo Medical’s B-LaserTM, a novel atherectomy device, in subjects affected with infrainguinal peripheral arterial disease: results of the EX-PAD-03 trial. Cardiovas Revasc Med. 2020;21(1):86-92.
3. Auryon. Instructions for use. AngioDynamics; 2020.


AngioDynamics, the AngioDynamics logo, Auryon, and the Auryon logo are trademarks and/or registered trademarks of AngioDynamics, Inc., an affiliate or a subsidiary. © 2023 AngioDynamics, Inc. US/PA/AD/1770 Rev 01 03/2023
laser technology for precise, targeted treatment both, above and below the knee
types, from
Conquer the most severe. Discover the Science and Au ryon-System.com Safety: VISIT US AT BOOTH #1030
VAM 202 4
THURSDAY
SCHEDULE AT-A-GLANCE
Thursday, June 20
6:00 a.m. to 6:00 p.m. Registration West Building, Level 3, Hall F1 Foyer
6:30 a.m. to 8:00 a.m.

General Surgery Resident/ Medical Student Session: Mock Interviews West Building, Level 1, W185bcd
6:30 a.m. to 8:00 a.m. International Chapter Forum Educational Session West Building, Level 1, W184bc
7:00 a.m. to 8:00 a.m. The Past, Present and Future of Radiation Safety West Building, Level 1, W183a
7:00 a.m. to 8:00 a.m. New Technology in Vascular Surgery – Leading Artificial Intelligence in Vascular Care West Building, Level 1, W183c
7:00 a.m. to 12:00 p.m. Society for Vascular Nursing Annual Conference: Day 2 West Building, Level 1, W187
8:00 a.m. to 9:30 a.m. Plenary Session 3 West Building, Level 3, Skyline Ballroom W375ab
9:30 a.m. to 10:00 a.m. John Homans Lecture West Building, Level 3, Skyline Ballroom W375ab
10:00 a.m. to 10:15 a.m. Awards Ceremony West Building, Level 3, Skyline Ballroom W375ab
10:15 a.m. to 10:45 a.m. Coffee Break in the Exhibit Hall West Building, Level 3, Hall F1
10:20 a.m. to 10:45 a.m. Vascular Live Presentation: Large Bore Arterial Closure in EVAR and TEVAR, Sponsored by Teleflex West Building, Level 3, Hall F1
10:45 a.m. to 12:00 p.m. Plenary Session 4 West Building, Level 3, Skyline Ballroom W375ab
12:00 p.m. to 1:30 p.m. Lunch with the Exhibitors West Building, Level 3, Hall F1
12:15 p.m. to 12:40 p.m. Vascular Live Presentation: Is ‘Leave Nothing Behind’ A Realistic Goal in All SFA Lesions, Sponsored by Boston Scientific West Building, Level 3, Hall F1
12:15 p.m. to 4:30 p.m. Society for Vascular Nursing/ Physician Assistant Section West Building, Level 1, W187
Key: ES: Educational Session
12:30 p.m. to 1:30 p.m. Industry Symposia: Solventum Presents: Reducing Surgical Site Complications: Innovative Techniques and Technologies West Building, Level 1, W184d
1:00 p.m. to 1:25 p.m.
Vascular Live Presentation: Shockwave E8 Experience, Sponsored by Shockwave West Building, Level 3, Hall F1
1:30 p.m. to 3:00 p.m. “How I Do It” Video Session West Building, Level 1, W183b
1:30 p.m. to 3:00 p.m.
1:30 p.m. to 3:00 p.m.
1:30 p.m. to 3:00 p.m.
3:00 p.m. to 3:25 p.m.
3:00 p.m. to 3:30 p.m.
Dialysis Creation and Percutaneous Challenges West Building, Level 1, W183c
Contemporary Issues in the Management of Ruptured Aortic Aneurysms
Community Practice Section: Optimizing and Protecting your Clinical Practice
Vascular Live Presentation: Seeing Clearly: Unlocking the Potential of IVUS in Venous Stenting, Sponsored by Philips
West Building, Level 1, 183a
West Building, Level 1, W184bc
West Building, Level 3, Hall F1
Coffee Break in the Exhibit Hall West Building, Level 3, Hall F1
3:30 p.m. to 5:00 p.m. A Multidisciplinary Approach to Limb Salvage: Creating and Expanding the Toe and Flow Model
3:30 p.m. to 5:00 p.m.
3:30 p.m. to 5:00 p.m.
3:30 p.m. to 5:00 p.m.
5:00 p.m. to 6:30 p.m.
5:00 p.m. to 6:30 p.m.
5:00 p.m. to 6:30 p.m.
5:15 p.m. to 5:40 p.m.
Decision-Making and Endovascular Techniques in Challenging Aortic Aneurysms
Entrustable Professional Activities: A Disruptive I nnovation in Surgical Training and Certification
West Building, Level 1, W183b
West Building, Level 1, W183a
West Building, Level 1, W183c
Section on Outpatient and Office Vascular Care West Building, Level 1, W184bc
Interactive Poster Session West Building, Level 3, Hall F1
International Poster Competition West Building, Level 3, Hall F1
Opening Reception in the Exhibit Hall West Building, Level 3, Hall F1
Vascular Live Presentation: Innovating with Clinical Evidence: Proof of EVAR Durability and New Insights Through the RCTs, Sponsored by Medtronic
5:30 p.m. to 7:00 p.m. Alumni and Affiliate Receptions
5:50 p.m. to 6:15 p.m.
7:00 p.m. to 9:30 p.m.
Vascular Live Presentation: Breaking New Ground in Chronic Venous Disease with RevCore and VenaCore, Sponsored by Inari
West Building, Level 3, Hall F1
West Building, Level 3, Hall F1
Women’s Leadership Dinner Marriott Marquis
8 VS@VAM | Thursday, June 20, 2024
Hope For The Day Back for Year Two at VAM
THE SVS WELCOMES BACK HOPE
For the Day to this year’s VAM. Hope For The Day is a non-profit movement empowering the conversation on proactive suicide prevention and mental health education.
Over 130 suicides take place each day, according to Hope for the Day’s website, and the organization strives to provide resources and silence the stigma around mental health and suicide.
The SVS is hoping to provide more accessible resources to those dealing with mental health crises, including burnout, for VAM attendees.
One of Hope For The Day’s main concepts is the impact of having a solid self-care routine to help bring individuals back to their baseline and preparing a “self-care toolbox,” or list of physical or mental activities that one can do to heal and manage their mental health. Taking care of oneself is as essential to wellness as tending to patients.
Cast those ballots! Voting for SVS vice president ends this afternoon
TIME IS ALMOST UP SENIOR, Active and Early Active Society for Vascular Surgery (SVS) Members are strongly encouraged to submit their votes for SVS vice president by today’s 2 p.m. deadline.
The candidates for this year’s election are Linds Harris, MD, DFSVS, and Palma Shaw, MD, DFSVS. QR codes are scattered throughout McCormick Place to provide ease of voting. Members should sign in and use their SVS credentials.
Eligible members can visit vascular. org/VOTE2024 to cast their vote.
Remember to claim CME credits
VASCULAR QUALITY INITIATIVE, VAM and Society for Vascular Nursing annual conference attendees must claim continuing medical education (CME) credits and contact hours o later than July 22.
The American Board of Surgery (ABS) recently made changes to its claiming processes.
Max Credit Available: VAM 2024: 26.75 credit; VQI 2024: 15.25; SVN 2024: 13 contact hours.
To claim, visit vascular.org/VAM24CME.
SVN WRAPS CONFERENCE WITH JOINT PA SECTION PROGRAMMING

THE SOCIETY FOR VASCULAR NURSING (SVN) IS IN THE MIDST OF ITS 42nd Annual Conference at McCormick Place, West. The conference kicked off Wednesday morning with the Presidential Welcome from Kristen Alix, MS, ANPBC, AGACNP, CVN, and was followed by the keynote address, “Disrupting DEI in a disruptive environment,” delivered by Katie Boston Leary, PhD, MBA, MHA, RN, NEA-BC.
The conference’s education sessions continue to follow four different tracks: Breaking News in Vascular Care and Thoracic Aneurysms; Thinning it Out: Perioperative Considerations and Wound Care Basics, Stroke and Reaching your Vascular Summit; and Upgrades in PAD and Limb Salvage Care.
Alix stated that the education for this year’s program is “unmatched,” with a clinically diverse faculty from all over the U.S. and Canada.
“The conference has grown so much since I became a member and being more involved this year as SVN president has been a true highlight. I can’t wait to see what education and opportunities are brought forth in the years to come,” said Alix. The official SVN meeting program will wrap up today with a closing ceremony that includes “Best Of” awards.
The available education for SVN attendees won’t end after the four tracks are covered. The SVN conference takes place alongside the VAM 2024. The two meetings have collaborated to offer an immersive program that will merge SVN with the SVS Physician Assistant’s (PA) Section.
The program, built for Advanced Practice Providers (APPs), kicked off on Wednesday evening with the return of Vascular Jeopardy, which first debuted at VAM 2023 in National Harbor, Maryland. The game involved vascular nurses, APPs and PAs facing off in a jeopardy-style format answering questions about different cases and treatment of vascular patients.
The immersive program will resume this afternoon with a lunch coinciding with Vascular Team Talks that will be moderated by Suzanna Fitzpatrick, DNP, ACNP-BC, FNP-BC, immediately followed by an hour-long diagnostics session with Kate Carrato, from Advent Health. The remaining time will consist of a hands-on simulation program covering wound care and compressions, closures, vascular ultrasound and sclerotherapy. The last half hour of education will be spent covering Organizational Change by APP Impact, led by Alix, Matthew Smeds, MD, and Holly Grunebach, PA-C, MSPH. The evening will wrap up with a happy hour for all attendees.
The idea of the immersive APP program was generated for VAM 2023. “We realized that if we are working together on cases, it only makes sense for us to learn together at our annual meetings,” said SVS PA Section Chair Holly Grunebach, PA-C, MSPH. “Learning together helps us to develop skills as a team which then translates to more fluidity when it comes to patient care, which is something we all want.”
Visit vascular.org/VAM24Planner.
Brand new at VAM 2024
There are exciting new industry initiatives happening at VAM 2024.
New Look for Vascular Live! Enjoy education from SVS industry partners in the new Vascular Live! theater. Relax and take in the industry-led sessions while on a sofa or lounge seat or enjoy your lunch at one of the cabaret tables.
Industry Night: Enjoy one of three industry events during the new SVS Industry Night at VAM—tonight—June 20. Each event will offer attendees the opportunity to network with colleagues and industry representatives.
Crossroads@VAM: This initiative offers VAM 2024 attendees the unique opportunity to connect with two SVS industry partner companies over refreshments. Crossroads@ VAM kicked off on Wednesday and will resume today and tomorrow from 8 a.m. to 5 p.m.
How to succeed as a vascular fellowship applicant
On Friday morning, a special breakfast session for general surgery residents will be held to walk through succeeding as a vascular fellowship applicant.
The session is being put on by the SVS Resident Student Outreach Committee and will take place at 6:30 a.m. in the West Building, Level 1, W183a.
Gala tickets are still available
A LIMITED NUMBER OF TICKETS TO the SVS Foundation’s Gala, A Night at the Museum—a Celebration of Science, are available for purchase at VAM 2024. The blacktie event will occur on Friday at Chicago’s Museum of Science and Industry. At 5:45 p.m., a complimentary transportation service will take attendees from the Marriott Marquis to the museum with beverages available to all on board. At the venue, attendees will enjoy an open bar, threecourse meal, late-night snacks, DJ, dancing and more. Transportation back to the Marriott Marquis will begin running at 9:30 p.m. Gala proceeds benefit the Foundation’s mission to optimize the vascular health and well-being of patients and the public through support of research, as well as education and programs, to prevent and treat circulatory disease.
To purchase tickets, visit the SVS Foundation at the SVS Central booth outside the Exhibit Hall.
9 www.vascularspecialistonline.com
Compiled by Kristin Spencer
A hands-on session from VAM 2023
COMMENT& ANALYSIS
CORNER STITCH
Corner Stitch welcomes new editor for trainees!
 Saranya Sundaram
Saranya Sundaram
Vascular Specialist has a new resident/ fellow editor in time for VAM 2024: Saranya Sundaram, MD, is an integrated vascular surgery resident in PGY-3 at the Medical University of South Carolina in Charleston. She replaces Christopher Audu, MD, a graduating vascular surgery resident at Michigan Medicine in Ann Arbor. Here, Sundaram breaks down some of her highyield highlights from day 1—and what she is looking out for across the rest of the week.
CONGRATULATIONS TO THE MEDICAL students and residents who made it to the Vascular Annual Meeting this year, and even more praise to those who will be standing at the podium to present their research! VAM can be both a wondrous and overwhelming experience to those joining for their first time. But it is also the chance to get involved in some of the newest projects in vascular surgery and, not to mention, make major headway in the
networking arena. VAM opening day yesterday produced a rich vein of high-yield sessions for medical students and resident. Starting with the Opening Ceremony, things quickly picked up pace with the first two plenary sessions, including the William J. von Liebig Forum.
Other sessions of note were APSA (American Pediatric Surgical Association)-SVS Multidisciplinary Pediatric Vascular Surgery Interest Groups; Vascular Fellows: Preparing for Practice; and the SVS-Vascular and Endovascular Surgery Society (VESS) Scientific Sessions@ VAM.
Across the next three days of VAM 2024, here are some more of the sessions that could be worth prioritizing:
Thursday, June 20
General Surgery Resident/Medical Student Session: Mock Interviews (6 a.m.) ◆
Practice Essentials of Thoracic Outlet Syndrome (7a.m.) ◆
New Technology in Vascular Surgery—Leading Artificial Intelligence in Vascular Care (7 a.m.) ★
Plenary Session 3 (8 a.m.) ●
John Homans (Presidential) Lecture (9:30 a.m.) ●
Plenary Session 4 (10:45 a.m.) ●
Lunch with Exhibitors (12 p.m.) ■
“How I Do It” Video Session (1:30 p.m.) ★
Dialysis Creation and Percutaneous Challenges (1:30 p.m.) ★
Contemporary Issues in the Management of Ruptured Aortic Aneurysms (1:30 p.m.) ★
“Entrustable Professional Activities: A Disruptive Innovation in Surgical Training and Certification” (3:30 p.m.) ★
Opening Reception (5 p.m.) ■ Women’s Leadership Dinner (7 p.m.) ■
Friday, June 21
General Surgery Resident Session: How to Succeed as a Vascular Surgery Fellowship Applicant (6:30 a.m.) ◆
Medical Students: Introduction to Vascular Surgery (6:30 a.m.) ◆
Plenary Session 5 (8 a.m.) ● Plenary Session 6 (10 a.m.) ● Presidential Introduction and Address (11 a.m.) ● Career Fair (12 p.m.) ■ Residency Fair (1:30 p.m.) ■
Infra-inguinal Bypass—How to do it Successfully and Efficiently (1:30 p.m.) ★
Young Surgeons Section: “Well, Here We Are, But Right Now I Wish I Wasn’t”—Early Career Errors (1:30 p.m.) ★ International Young Surgeon’s Competition (3:30 p.m.) ● Poster Competition (3:30 p.m.) ● Women’s Section: Vascular Trauma—What I Need to Know in the Middle of the Night (3:30 p.m.) ★ SVS Foundation Pre-Gala Reception (6:15 p.m.) ■
Saturday, June 21
Plenary Session 7 (8 a.m.) ● Poster Championship (9:30 a.m.) ● Frank J. Veith Distinguished lecture (10:45 a.m.) ● Plenary Session 8 (10 a.m.) ●
10 VS@VAM | Thursday, June 20, 2024
KEY:
only at VAM ■ networking/career session ◆ trainee-focused session ★ unique/trainee-relevant educational session
●
VAM THROUGH THE LENS »
A visual snapshot of opening day at VAM 2024, when delegates gathered from across the globe for a series of program highlights, incuding the Opening Ceremony, the William J. von Liebig Forum, and the Crawford Forum, among many others.








“The science of vascular surgery knows no borders, and the more collaborative we are, the stronger we are”
JOSEPH MILLS
11 www.vascularspecialistonline.com
24
The current and next SVS president are pictured the day prior to VAM opening, while family members of the late Jimmy Yao attended the inaugural Resident Research Award renamed in his honor. Elsewhere, early plenaries and educational sessions, as well as the Crawford Forum, captured the attention of attendees at McCormick Place in Chicago
Pediatric vascular trauma:
‘Collaboration really matters in this space’
By Jocelyn Hudson
THE FOCUS OF YESTERDAY LUNCHTIME’S
American Pediatric Surgical Association (APSA)-SVS task force’s spring quarterly interest group meeting was the “incredibly crucial” topic of pediatric trauma, as described by co-moderator John White, MD. Various speakers shared a series of predominantly case-based talks, with the importance of collaboration emerging as a key take-home message.
White, who is chair of surgery at Advocate Lutheran General Hospital in Park Ridge, Illinois, outlined the gravity of the topic at hand. “We lose 20,000 young lives each year from trauma,” he said, adding that trauma is the leading cause of death of all children over the age of one and exceeds the combined total of all other causes.
Furthermore, he noted that for every death, 40 children require hospitalization for major injuries and thousands of others are treated in emergency rooms. These factors, he remarked, make this “an extremely important topic.”
The session featured presentations from co-moderator Dawn Coleman, MD, division chief of vascular and endovas-
cular surgery at Duke University in Durham, North Carolina, J. Westley Ohman, MD, associate professor at Washington University in Saint Louis, Missouri, Luigi Pascarella, MD, associate professor at University of North Carolina at Chapel Hill, and Jayer Chung, MD, MS, associate professor at Baylor College of Medicine in Houston, Texas.
Delivering the final presentation of the session was Regan Williams, MD, medical director of trauma services at the Le Bonheur Children’s Hospital in Memphis, Tennessee, who delivered a presentation titled “Expanded support of the pediatric vascular trauma patient—the importance of care processes and resources.”
“I think the previous speakers have shown that we have an increased number of pediatric vascular trauma patients, mostly related to the increased number of penetrating injuries that are affecting our children, and the vascular surgeons and pediatric surgeons have really been working well collaboratively together to save these children’s lives,” Williams began. “But what happens after you’ve repaired them, how do we get them back to normal life, how do we help them to be functional children and to live a very long, happy life after
“But what happens after you’ve repaired them, how do we get them back to normal life, how do we help them to be functional children and to live a very long, happy life after they’ve had these drastic injuries?”
REGAN WILLIAMS

they’ve had these drastic injuries?”
Part of Williams’ talk focused on child life services, which the presenter noted is a relatively new field. “Child life uses play and developmentally appropriate communication to help inform hospitalized children and their families,” she explained.
“I think the best collaborative model for pediatric vascular injuries is an adult vascular surgeon that has tons of experience in the technical aspects, but really partnering with a pediatric surgeon and a pediatric hospital so we can support the other parts of the child—they’re really important for their long-term outcomes,” Williams said in her conclusion. Closing out the session, Coleman summarized: “I’m taking away from this whole session that collaboration really matters in this space.”
White and Coleman co-moderated the session alongside Claudie Sheahan, MD, professor of clinical surgery at LSU Health in New Orleans, Louisiana.

12 VS@VAM | Thursday 20 June 2024
VASCULAR TRAUMA
Special session on pediatric vascular surgery
OVERCOMING BARRIERS AND FINDING SOLUTIONS FOR DIABETES-RELATED AMPUTATIONS
AMONG UNDERSERVED
POPULATIONS
By Marlén Gomez
DIABETES-RELATED LOWER extremity amputations (LEA) disproportionately impact racial minorities and low-income groups. The Vascular Volunteers in Service to All (VISTA) assessment tool identified significant barriers to effective care from a patient's perspective, including financial constraints, systemic issues, time and access limitations, knowledge gaps, and cultural and provider-related factors.
The Plenary Three paper—"VISTA: Targeting diabetes-related lower extremity amputations among underrepresented communities through a patient-centered multidisciplinary approach"—will see presenting author Paulette Torres Ruiz, MD, a clinical researcher at Baylor College of Medicine in Houston, deliver recent findings and future directions of the VISTA project. It is being held today (8:53–9:04 a.m. in the West Building, Level 3, Skyline Ballroom).
The paper will provide insights into designing a community-based awareness campaign to improve outpatient care accessibility and implement an internal systemic
CLINICAL PRACTICE
algorithm to promote limb salvage.
"Diabetes-related lower extremity amputations (LEAs) remain a devastating consequence for many individuals, particularly those from racial minorities and low-income backgrounds," said Torres Ruiz. "Our study aimed to understand the factors contributing to these outcomes and how the VISTA assessment tool could help mitigate this issue."
The paper will take an in-depth look at the VISTA assessment tool's impact on non-traumatic amputations in a regional, urban and underserved community. Over the course of a year, 101 consecutive patients with diabetic foot ulceration or infection were enrolled in the study. The results were sobering: 63 LEAs were recorded, including 34 minor amputations, eight transmetatarsal amputations (TMA) and 21 below-the-knee amputations (BKA). Notably, 45 LEAs occurred at baseline admission, and 18 occurred during extended follow-up after discharge.
Torres Ruiz highlighted the primary barriers identified through the VISTA assessment tool, including financial constraints, sys-
Navigating clinical guidelines discrepancies between SVS, ESVS patients
CLINICAL GUIDELINES FROM THE SOCIETY FOR Vascular Surgery (SVS) and the European Society for Vascular Surgery (ESVS) are pivotal in directing practitioners' management of complex vascular conditions.
However, the development and release of these guidelines have not been synchronized, resulting in differences and gaps in recommendations. VAM 2024 attendees were presented with this sentiment during a Wednesday postgraduate session focused on the discrepancies between the clinical guidelines of two societies.
Ronald L. Dalman, MD, from Stanford University in Stanford, California, and Jonathon R. Boyle, MBChB, from the University of Cambridge, England, introduced the session, which examined the real-world implications of these discrepancies
Dalman remarked, "Understanding why these disparities exist is crucial for improving patient outcomes. This initiative aims to ensure that vascular specialists worldwide can deliver care based on a comprehensive understanding of global recommendations, ultimately promoting better patient care."
Key topics included the management of aortic graft infection, asymptomatic carotid stenosis, intermittent claudication and incompetent perforators in venous disease.
Contributions from specialists highlighted how scientific evidence, cultural nuances, societal variations and potential personal biases among guideline authors contribute to these differences.—Marlén Gomez
temic issues, time and access limitations, knowledge gaps and cultural and provider-related fac tors. "Our patients reported 83% dissatisfaction with diabetic foot care," she noted. "Over half were uninsured, and a mere 50.5% had been treated at a wound care special ty clinic."
Joseph Mills

The study's findings un derscored the necessity of a multidisciplinary approach, dubbed the Toe and Flow model, to reducing lower limb amputations due to diabetic foot ulcers or infections in marginalized and low-income minority groups. "By addressing these barriers and enhancing patient education, we can significantly improve limb salvage rates," said Torres Ruiz.
limb salvage is also crucial."
A significant increase in major amputations, particularly below the knee, was observed during the three-month follow-up period.
High Wound ischemia foot infection (WIfI) scores were predictive of increased risk of limb loss during the study.
“We need to focus on creating awareness campaigns to improve outpatient care accessibility”
JOSEPH MILLS
SVS President Joseph Mills, MD, senior author, highlighted the importance of community-based interventions. "We need to focus on creating awareness campaigns to improve outpatient care accessibility," said Mills. "Implementing an internal systemic algorithm to promote
"Our goal is to implement these findings into practical solutions that can be replicated in other underserved communities. The community-based awareness campaign is just the beginning," said Mills. The findings from the VISTA assessment tool and the proposed Toe and Flow model are intended to reduce the burden of diabetic lower extremity amputations in underserved communities.
"We have the data and the strategies," said Torres Ruiz. "Now it's time to act and make a tangible difference in the lives of those most affected by this condition."
PREVIEW
HOMANS LECTURE
‘REMARKABLE’ VARIATION IN INTERNATIONAL VASCULAR CARE CALLS FOR BETTER ADHERENCE TO EVIDENCE-BASED PRACTICE
“ALL VASCULAR SURGEONS HAVE ACCESS TO the same randomized trials and guidelines, which should harmonize international treatment patterns, but this is not always the case,” says Maarit Venermo, MD, PhD, University Hospital and University of Helsinki, Finland, giving VS@VAM a sneak peek of her upcoming John Homans Lecture this morning (Thursday, June 20, 9:30–10:00 a.m. in the West Building, Level 3, Skyline Ballroom).
At present, Venermo shares, there is “remarkable” international variation in vascular surgery services which are seen through indications for treatment, patient demographics, sex distribution and treatment profiles.
“For example, the proportion of asymptomatic patients in carotid surgery varies between 0–80%, and the proportion of women from 12–40%. In abdominal aortic aneurysm surgery, the proportion of small aneurysms [<55mm aneurysms] vary from less than 10% to almost 30%.”
The reasons for these geographical differences are many, she says, due to prevalence of vascular diseases, risk factors and life expectancy.
However, in following evidence-based practice, vascular care “should” be harmonized internationally.

Yet, as Venermo makes clear, this is not always the case.
“Despite the 10-year results from the Asymptomatic Carotid Surgery Trial 1 [ACST1] showing that patients with a life expectancy less than five years do not benefit from carotid surgery—and younger patients with tight stenosis do—the treatment of asymptomatic stenosis has remained the same in a majority of the countries before and after the publication.”
However, if data have not largely influenced vascular care, Venermo explains, reimbursement has been “a force” for change. “In countries that have a fee-for-service reimbursement system, the proportion of asymptomatic carotid patients and patients with small aneurysms who undergo surgery is higher, compared to countries with a public health system,” she says.
“Ultimately, all of the current evidence has been evaluated carefully in the guidelines, and the recommendations have been built on the basis of evidence.”—Éva Malpass
13 www.vascularspecialistonline.com
DIABETES
PREVIEW
Maarit Venermo
Medical Editor Malachi Sheahan III, MD
Associate Medical Editors
Bernadette Aulivola, MD | O. William Brown, MD | Elliot L. Chaikof, MD, PhD
| Carlo Dall’Olmo, MD | Alan M. Dietzek
MD, RPVI, FACS | John F. Eidt, MD | Robert Fitridge, MD | Dennis R. Gable, MD | Linda Harris, MD | Krishna Jain, MD | Larry Kraiss, MD | Joann Lohr, MD
| James McKinsey, MD | Joseph Mills, MD | Erica L. Mitchell, MD, MEd, FACS | Leila Mureebe, MD | Frank Pomposelli, MD | David Rigberg, MD | Clifford Sales, MD | Bhagwan Satiani, MD | Larry Scher, MD | Marc Schermerhorn, MD | Murray
L. Shames, MD | Niten Singh, MD | Frank J. Veith, MD | Robert Eugene Zierler, MD
Resident/Fellow Editor
Christopher Audu, MD
Executive Director SVS
Kenneth M. Slaw, PhD
Senior Director for Public Affairs and Advocacy
Megan Marcinko, MPS
Manager of Marketing
Kristin Spencer
Communications Specialist
Marlén Gomez
Published by BIBA News, which is a subsidiary of BIBA Medical Ltd.
Publisher Stephen Greenhalgh
Content Director Urmila Kerslake
Global Commercial Director
Sean Langer
Managing Editor Bryan Kay bryan@bibamedical.com
Editorial contribution Jocelyn Hudson, Will Date, Jamie Bell, Brian McHugh, Éva Malpass and George Barker
Design Terry Hawes
Advertising Nicole Schmitz nicole@bibamedical.com
Letters to the editor vascularspecialist@vascularsociety.org
BIBA Medical, Europe
526 Fulham Road, London SW6 5NR, United Kingdom BIBA Medical, North America 155 North Wacker Drive – Suite 4250, Chicago, IL 60606, USA
Twin global burdens of growing PAD prevalence and vascular workforce shortfall
demand action, WFVS session hears
A GROWING PREVALENCE OF PERIPHERAL ARTERIAL disease (PAD) across the world parallels a deteriorating PAD landscape in the U.S., underscoring a need for more vascular surgeons and risk-factor reduction globally, according to a leading expert in the field.
Vincent Rowe

Vincent Rowe, MD, chief of vascular surgery at the University of California, Los Angeles (UCLA), was speaking during the VAM 2024 World Federation of Vascular Societies (WFVS) Educational Session yesterday morning (Wednesday, June 19), telling the audience, “It is pretty apparent, that in both the U.S. and globally, we are heading down this dark road to the complications that occur with PAD: if we don’t do something soon it could be an issue, not only for the United States, but also globally.”
Risk factors in the U.S. include tobacco use and glucose and blood pressure control, Rowe explained. Across the world, it is a similar picture, he said, adding low physical activity and diet to the list.
He raised the twin specter of diabetes, with “a tsunami” expected across the U.S. in the next 20 to 30 years, especially among some minority patients, running alongside the global PAD burden. “If we look at diabetes globally, you can see it is increasing, both in terms of prevalence and in terms of incidence, and also deaths.”
Rowe referenced a recent publication that laid out the scope: a 72% increase in global prevalence of PAD, with mortality also continuing to rise.
“The authors stated that this pattern represents a major public health challenge that warrants a coordinated and targeted response from governmental and private medical institutions to try to combat this disease, and especially slow the progression medically,” he said.
The global picture of increasing PAD and associated risk factors— body mass index and food consumption levels among them—plays out across gender and among children, Rowe pointed out.
The bottom line is, according to Rowe, “in the U.S., with all these increases in risk factors, that we predict we’re going to need more vascular surgeons. “The current estimate is a 31% shortfall in the
EDUCATION
Vascular Specialist is the official newspaper of the Society for Vascular Surgery and provides the vascular specialist with timely and relevant news and commentary about clinical developments and about the impact of healthcare policy. Content for Vascular Specialist is provided by BIBA News. Content for the news from SVS is provided by the Society for Vascular Surgery. The ideas and opinions expressed in Vascular Specialist do not necessarily reflect those of the Society or the Publisher. The Society for Vascular Surgery and BIBA News will not assume responsibility for damages, loss, or claims of any kind arising from or related to the information contained in this publication, including any claims related to the products, drugs, or services, or the quality or endorsement of advertised products or services, mentioned herein. | The Society for Vascular Surgery headquarters is located at 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. | POSTMASTER: Send changes of address (with old mailing label) to Vascular Specialist, Subscription Services, 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. | RECIPIENT: To change your address, e-mail subscriptions@bibamedical.com | For missing issue claims, e-mail subscriptions@bibamedical. com. | Vascular Specialist (ISSN 1558-0148) is published monthly for the Society for Vascular Surgery by BIBA News. | Printed by Ironmark |
©Copyright 2024 by the Society for Vascular Surgery
next couple of years, he noted, “and unfortunately we’re not very well distributed across the country.” Currently, some 2,600 counties in the U.S. have no vascular surgery representation, Rowe said. And they’re not all rural: “Almost half of them are considered urban counties,” he added. “If we look at the world, we can see that the population is going to continue to increase, and our distribution of vascular surgeons across the world in certain countries is not very good at all.”
Rowe offered some potential remedies aimed at starting to tackle the increasing disease burden and workforce shortfall. “We can try to increase the number of vascular surgeons, but that is going to be a tall order. But we’re going to really need to, especially globally,” he said.
He also raised the idea of international rotations. “Perhaps if we were allowed to take our fellows and residents internationally, that would increase their interest in going back and serving in those countries,” he elaborated, also suggesting paid service programs as another possible avenue.
“Also, maybe loan forgiveness: we forgive loans for people who go and practice in underserved areas—maybe they should forgive them if someone goes and practices for two to three years internationally as well.”
Rowe added one more remedy from his own circle. “One of my friends is from Nigeria, and he does global grand rounds—not to educate the vascular surgeons but to educate all the other practitioners about vascular disease to help them take care of these patients medically.”
“Perhaps if we were allowed to take our fellows and residents internationally, that would increase their interest in going back and serving in those countries”
VINCENT ROWE
VASCULAR COMMUNITY EMBRACES LEARNING FROM PAST OPERATING ROOM EXPERIENCES IN 'MY WORST CASES'
Transparency was at the forefront of a My Worst Cases session at VAM yesterday afternoon. Moderator William Robinson, MD, professor and chief in the Division of Vascular Surgery at Southern Illinois University School of Medicine in Springfield, Illinois, set the tone for the session, emphasizing the importance of shared learning experiences.. By Marlén Gomez
"THE AUDIENCE WANTS AN opportunity to engage, ask questions, make comments and we're going to provide that today," remarked Robinson in his opening remarks.
Afterward, VS@VAM caught up with medical student attendees of various backgrounds who shared their reflections on what they heard from the panel of vascular surgeons.
"A lot of cases presented were fantastic because they showed that even in situations where a procedure didn't go as planned, you
know, the surgeons that were presenting were professionally composed and, in many cases, admitted to their faults of being too aggressive with treatment and how they always try to work in the best intention and protection of the patient," said Alan Nagarajan, from the Baylor College of Medicine, Houston, Texas.
"Much of this is technically their worst cases, as in their worst moments. I think coming up there and showing that bravery of just showing all of the steps and what went wrong, and thinking about the steps where
they could have done something different, and leaving it up to the audience to discuss some other options. I think it showed how innovative this field can be," said Nikitah Gidh from Baylor College of Medicine.
"This is my first time at VAM, and to see experienced doctors humbly admit their difficult cases, it reassures us because, when you're stepping out, it gives you confidence that things can go bad. It's bound to happen to anyone," said Benjamin George, Pushpagiri Insitute of Medical Science, Pathanamthitta, India.
14 VS@VAM | Thursday, June 20, 2024 WFVS
KARITH FOSTER PRESENTS VISION ON HOW TO TRANSFORM DIVERSITY AT VAM 2024
By Marlén Gomez
“ TRUE DIVERSITY IS A GOOD AND powerful thing that should be celebrated. It's not mandatory quotas; it's intentional inclusion," said Karith Foster, chief executive of Inversity Solutions, as she addressed the audience at the inaugural Keynote Speaker Series at VAM 2024.
Foster aims to create an effort that enrolls people, not repels them. In her talk,“Finishing the Journey to Inclusivity Through Belonging, Intention and Respect," she challenged conventional approaches to diversity, equity, and inclusion (DEI) initiatives. She advocated for a paradigm shift towards true inclusivity through belonging, intention, and respect.
Foster's keynote captivated attendees with her candid reflections on the shortcomings of current DEI strategies. She emphasized that many efforts are reactive rather than proactive, failing to achieve sustainable impact beyond initial training sessions.
“Burnout, confusion, overwhelm, exhaustion is real," Foster acknowledged. "People are exhausted by how we've been addressing diversity. Whether you're painted as the victim or villain, it's robbing all of us of our agency and defeating the purpose of unity."
Foster's message was central to the need for organizations to move beyond token-
CLI
ism and surface-level diversity metrics. She critiqued the prevalent approach in which diversity efforts, though well-intentioned, often result in short-lived benefits that fail to foster genuine change.
“When DEI is overwhelming, it can do more harm than good," Foster cautioned, drawing attention to instances where flawed implementation led to legal and reputational repercussions for companies like Starbucks and FedEx.
Foster's career trajectory, including her role as a national media figure addressing race relations, provided a backdrop for her deep dive into the complexities of achieving true inclusivity. She stressed the importance of acknowledging imperfections and fostering environments where individuals feel safe learning and growing.
“We're not perfect. We will misspeak. We will put our foot in our mouths. We may freeze up when something makes us uncomfortable or over-explain, making things worse. We're not all psychic all the time. We are all doing the best we can with the tools we have. But that doesn't mean we become lackadaisical, or we stop trying. It means we make an effort to do and be better."
Addressing the audience's skepticism towards DEI discussions, Foster referenced
Sex-based analysis finds BESTCLI data generalizable to female patients
A NEW SECONDARY ANALYSIS OF SEX DISPARITIES IN THE BEST endovascular versus best surgical therapy in patients with critical limb ischemia (BESTCLI) trial data has found that improved major adverse limb event (MALE)-free survival via open surgical bypass with single segment greater saphenous vein (SSGSV) available, is generalizable to female patients.
Ahead of delivering the analysis during today’s Plenary Session 3 (Thursday, June 20, 8–9:30 a.m., in the West Building, Level 3, Skyline Ballroom), Katharine L. McGinigle, MD, associate professor at the University of North Carolina at Chapel Hill, North Carolina, tells VS@VAM of the sex-based, biologic differences in atherosclerosis development which have led to variances in revascularization procedures offered to females.
“In retrospective studies, females have inferior short- and long-term outcomes after intralingual revascularization compared to males. Few randomized controlled trials report sex-stratified results, but this is important to do in order to understand what results can actually be expected in females,” McGinigle explains.
“Despite clear biologic differences, the efficacy of new medications, endovascular devices and other outcomes are rarely tested in females specifically.
“This is much like the common but flawed assumption that non-Hispanic White males are the default standard and that results are generalizable to other populations,” McGingle added.
Looking at the BEST-CLI data, McGinigle and colleagues identify that, regardless of revascularization modality, females had better amputation-free survival at one year when compared to male patients.
However, improved MALE-free survival with surgical bypass in female patients suggests a surgery-first approach should be considered primarily, regardless of conduit availability, she adds. Éva Malpass
studies that show widespread disillusionment despite substantial investments. She challenged the audience to redefine diversity beyond quotas and superficial differences, advocating for an inclusive culture that values diverse perspectives and encourages open dialogue.

Throughout her keynote, Foster emphasized the role of leadership in fostering environments conducive to inclusivity. She highlighted the significance of psychological safety, where individuals feel empowered to speak up without fear of retribution, fostering a culture of trust and mutual respect.
“Inversity is about never forgetting the statistics I shared earlier about how close we
“When DEI is overwhelming, it can do more harm than good”
are genetically to one another," Foster said of her vision of inclusivity that transcends visible differences. She called for a collective shift in consciousness, where biases are acknowledged and addressed to pave the way for healthier relationships and more equitable workplaces.
Foster's call for "incremental Inversity“1%" urged small but meaningful steps towards a more inclusive future. Her blend of personal anecdotes and empirical insights
left a lasting impression, challenging attendees to reconsider their roles in shaping inclusive organizational cultures.
During the forum, Foster emphasized leadership's critical role in addressing workplace bias. She asserted, "Leadership must help empower employees, and employees must be empowered to address an issue when it comes up immediately rather than letting it sit and fester." Foster underscored the pervasive nature of unconscious bias, stating, "Unconscious bias is real; it'spervasive and not going anywhere any time soon. So, we have to learn to deal."
She outlined a proactive approach to managing these biases by "identifying and recognizing to minimize, mitigate and move forward with as little disruption as possible."
Highlighting the issue's complexity, Foster noted that "over 100+ unconscious and implicit biases have been identified," making it clear that addressing them requires continuous effort and attention.
As Foster concluded her address, she left attendees with a call to action, encouraging them to integrate the principles of INVERSITY into their daily practices. Her message of empathy, humility and continuous learning echoed through the conference halls, sparking conversations on how to transform diversity initiatives from compliance-driven tasks into catalysts for genuine cultural change. As organizations navigate the complexities of a globalized workforce, Foster's insights offer a roadmap toward a more equitable future.
GORE® EXCLUDER® Thoracoabdominal Branch Endoprosthesis
INDICATIONS FOR USE IN THE U.S.: The GORE® EXCLUDER® Thoracoabdominal Branch Endoprosthesis is indicated for endovascular repair in patients with thoracoabdominal aortic aneurysms and high-surgical risk patients with pararenal aortic aneurysms who have appropriate anatomy as described below: Adequate iliac/femoral access and brachial/axillary access; proximal (supraceliac) aortic neck treatment diameter range over 2 cm seal zone of 22-34 mm for aneurysms extending up to 6.5 cm or less above the origin of the most proximal branch vessel; aortic neck angle ≤ 60° at the Aortic Component proximal seal zone; iliac artery treatment diameter range of 8-25 mm and iliac artery seal zone length of at least 10 mm; renal artery seal zone diameters between 4.0-10.0 mm; celiac and superior mesenteric artery seal zone diameters between 5.0-12.0 mm; ≥ 15 mm seal zone length in renal arteries, superior mesenteric artery and celiac artery; and visceral segment of aorta (3 cm proximal through 9.5 cm distal to the most proximal visceral artery) must be ≥ 20 mm in diameter.
CONTRAINDICATIONS: The GORE® EXCLUDER® Thoracoabdominal Branch
Endoprosthesis is contraindicated in: Patients with known sensitivities or allergies to the TAMBE materials including ePTFE, FEP, nickel titanium alloy (Nitinol), stainless steel and gold. Patients who have a condition that threatens to infect the graft. Patients with known hypersensitivity to heparin, including patients who have had a previous incident of Heparin-Induced Thrombocytopenia (HIT) type II and cannot receive the GORE® VIABAHN® VBX Balloon Expandable Endoprosthesis. Refer to Instructions for Use at eifu.goremedical.com for a complete description of all applicable indications, warnings, precautions and contraindications for the markets where this product is available.
Products listed may not be available in all markets.
GORE, Together, improving life, EXCLUDER, VBX, VIABAHN and designs are trademarks of W. L. Gore & Associates. © 2024 W. L. Gore & Associates, Inc. 24AR1031-EN01 MAY 2024
15 www.vascularspecialistonline.com
KEYNOTE PREVIEW
Karith Foster
GORE® EXCLUDER®
Thoracoabdominal Branch
Endoprosthesis

THE BRIDGE BETWEEN THORACIC AND ABDOMINAL CARE
Extend your treatment options with the GORE® EXCLUDER® Thoracoabdominal Branch Endoprosthesis (TAMBE), the first and only FDA-approved device for endovascular repair.
Breakthrough solutions
A leader in developing products that are the first of their kind, Gore offers solutions to treat a range of aortic diseases including complex aneurysmal disease.
Off-the-shelf device
TAMBE incorporates a newly designed aortic component with other commercially available Gore devices to create a modular solution for minimally invasive branched endovascular repair.
W. L. Gore & Associates, Inc. Flagstaff, Arizona 86004 goremedical.com
Please see accompanying prescribing information in this journal.
Products listed may not be available in all markets.
GORE, Together, improving life, EXCLUDER and designs are trademarks of W. L. Gore & Associates.
© 2024 W. L. Gore & Associates, Inc. 24AR1054-EN01 MAY 2024
Versatility by design
TAMBE was created to provide procedural versatility all within 1 device system.
Learn more during the Vascular Insights & Practice (VIP) event at VAM24



 Elisa Caron
Elisa Caron





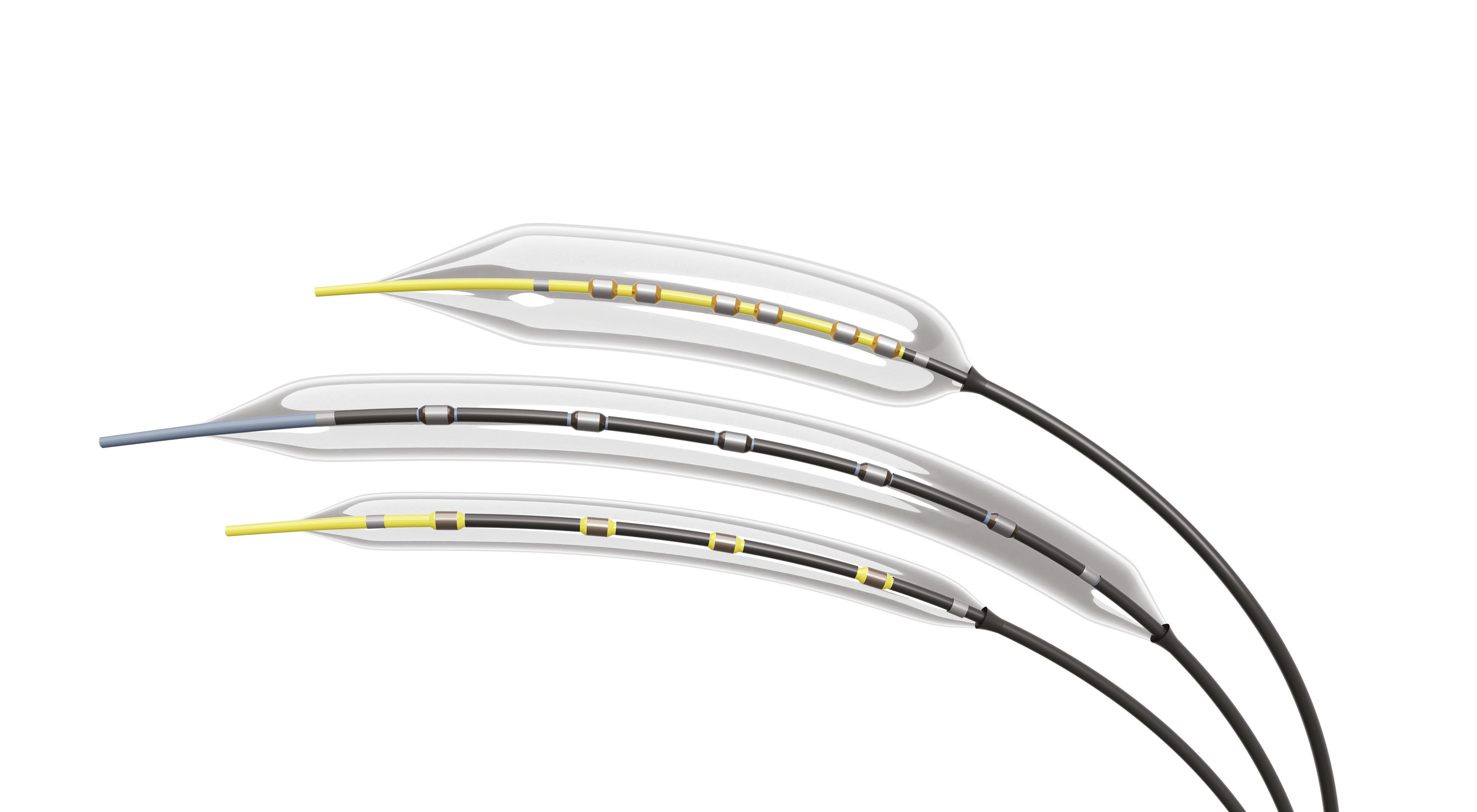








 Saranya Sundaram
Saranya Sundaram