In this issue:
2 From the Editor
The devil we don’t know: The case against private equity in medicine

7 Corner Stitch Grit: The value of a growth mindset and persistence during vascular surgery training
14 Venous stenting Fasting prior to venography and differences in venous stent sizing
19 Dialysis access Data show vascular external support system provides ‘boost’

www.vascularspecialistonline.com

Learning
curve: New data underscore physician experience levels required to derive benefit from transfemoral carotid artery stenting
By Bryan Kay
Data from a new study that maps out the levels at which adverse postoperative events decrease following transfemoral carotid artery stenting (TfCAS) based on depth of physician experience with the procedure represent an “absolute minimum threshold of learning,” the lead author says.
The analysis comes in the wake of the Centers for Medicare & Medicaid Services (CMS) decision to expand carotid stenting coverage, which loosened restrictions on the use of TfCAS.
Findings from an analysis of the Vascular Quality Initiative (VQI), due to be presented at the 2024 Society for Clinical Vascular Surgery (SCVS) annual meeting (March 16–20) in Scottsdale, Arizona, will show that the number of procedures a physician had to
See page 3
NEW ANALYSIS POINTS TO LACK OF VASCULAR SURGICAL VOICES IN NEWS COVERAGE OF VASCULAR DISEASE
By Bryan Kay
A NEW STUDY SET TO BE aired at SCVS 2024 sheds a statistical spotlight on the state of the specialty’s reach into the mainstream consciousness.
A team led by Babak Abai, MD, program director of the vascular surgery fellowship at Thomas Jefferson University in Philadelphia, performed a Google News analysis across both the medical and lay press to detect the scale of representation of vascular surgical voices in news coverage of vascular disease compared to other specialists who treat vascular pathologies.
What they found, Abai told Vascular Specialist ahead of SCVS 2024, demonstrated that
See page 3
NON-PNEUMATIC COMPRESSION DEVICE PERFORMED BETTER THAN ADVANCED PNEUMATIC COMPRESSION FOR LYMPHEDEMA
By Brian McHugh
A new study presented during the 2024 American Venous Forum (AVF) in Tampa, Florida (March 3–6), that compared a novel non-pneumatic compression device with an advanced pneumatic compression modality in the treatment of lower extremity lymphedema demonstrated “statistically significant disruption” in limb volume that favored the former.
The multicenter, randomized, control crossover study’s primary endpoint was change in limb volume from baseline, change in quality of life, and treatment
See page 3
NEWSPAPER
2024 Volume 20 Number 3
THE OFFICIAL
OF THE MARCH
Medical Editor Malachi Sheahan III, MD
Associate Medical Editors
Bernadette Aulivola, MD | O. William
Brown, MD | Elliot L. Chaikof, MD, PhD | Carlo Dall’Olmo, MD | Alan M. Dietzek
MD, RPVI, FACS | Professor HansHenning Eckstein, MD | John F. Eidt, MD | Robert Fitridge, MD | Dennis R. Gable, MD | Linda Harris, MD | Krishna Jain, MD | Larry Kraiss, MD | Joann Lohr, MD | James McKinsey, MD | Joseph Mills, MD | Erica L. Mitchell, MD, MEd, FACS | Leila Mureebe, MD | Frank Pomposelli, MD | David Rigberg, MD | Clifford Sales, MD | Bhagwan Satiani, MD | Larry Scher, MD | Marc Schermerhorn, MD | Murray
L. Shames, MD | Niten Singh, MD | Frank J. Veith, MD | Robert Eugene Zierler, MD
Resident/Fellow Editor
Christopher Audu, MD
Executive Director SVS
Kenneth M. Slaw, PhD
Executive Director SVS Foundation
Rupa Brosseau
Manager of Marketing
Kristin Spencer
Communications Specialist Marlén Gomez
Published by BIBA News, which is a subsidiary of BIBA Medical Ltd.
Publisher Stephen Greenhalgh
Content Director Urmila Kerslake
Global Sales Director Sean Langer
Managing Editor Bryan Kay bryan@bibamedical.com
Editorial contribution Jocelyn Hudson, Will Date, Jamie Bell, Brian McHugh, Éva Malpass and George Barker
Design Terry Hawes
Advertising Nicole Schmitz nicole@bibamedical.com
Letters to the editor vascularspecialist@vascularsociety.org
BIBA Medical, Europe
526 Fulham Road, London SW6 5NR, United Kingdom
BIBA Medical, North America
155 North Wacker Drive – Suite 4250, Chicago, IL 60606, USA
FROM THE EDITOR
The devil we don’t know: The case against private equity in medicine
By Malachi Sheahan III, MD
My household had a longstanding Christmas tradition. In the months leading up to the big day, my wife would craft a gift budget for our three sons. She would then blow said budget on mirth-busters like socks, books and, heaven forbid, educational toys.
Around Dec. 20, I’d look through this impending wreckage of our children’s hopes and dreams and offer up a passive-aggressive comment like, “I never would have thought to buy the New York Times crossword puzzle desk calendar for a four-yearold.” Her standard reply isn’t really printable here, but let’s just say I knew what to do. I understood the secret about boys that eluded my wife. They don’t really want specific things. They just want things. So every year I take what’s left of the budget and it’s go time. Shock and awe.
Pulling up to the Toys R Us on Christmas Eve, I looked much like the other deadbeat dads. But I was different. I had a PLAN. Grabbing two shopping carts, as I strolled down the center aisle my demeanor announced: “Make way fools, amateur hour is OVER. We may all be slackers and procrastinators here, but I am your king.”
There are three general categories of toys that my sons love. Things with teeth, things with wheels, and things that can be used to (hopefully just) simulate maiming your brothers. With Terminator-like efficiency, I quickly process the aisle labels. Jurassic Park Playsets (things with teeth), Matchbox/Monster Trucks (things with wheels), Nerf Missile Launchers (things that maim), Barbie/Disney Princesses (abandon all hope ye who enter here).
Passing this last aisle, I avoid eye contact with all of its desperate residents. Dads (it’s always dads) who clearly have not spent enough time with their daughters and are now trying to make up for it with a grand gesture. They are the Last and the Furious. It’s almost midnight Chad. Which My Little Pony does Sophie have her heart set on? Rainbow Sparkle or Pinkie Pie? Tick tock.
mailing label) to Vascular Specialist, Subscription Services, 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. |
RECIPIENT: To change your address, e-mail subscriptions@bibamedical.com | For missing issue claims, e-mail subscriptions@bibamedical. com. | Vascular Specialist (ISSN 1558-0148) is published monthly for the Society for Vascular Surgery by BIBA News. | Printed by Ironmark | ©Copyright 2024 by the Society for Vascular Surgery
My secret power was that I actually knew my kids. This may not seem like much but compared to my fellow consumers in this rural Louisiana Toys R Us at 10:33 p.m. on Christmas Eve, I was Father of the Frickin’ Year. Our time-honored tradition ended in 2017 with the bankruptcy of Toys R Us. What killed this profitable national chain? Private equity.
And now, as they say, the barbarians are at our gates. Are we ready? First, let’s review private equity FAQ style. Don’t worry, my financial education capped at ECON 101. There will be no mention of Adam Smith or The Wealth of Nations
What is private equity?
Private equity (PE) is best thought of as a financial strategy. The basic goal is to achieve higher returns than are generally possible in the public market. Therefore, PE investments are made in companies or entities that are not publicly traded. If the company is public, the PE firm takes it private after the acquisition.
Why does PE take their companies private?
In response to the rampant corporate fraud that led to the stock market collapse of 1929, Congress passed the Securities Act of 1933 and the Securities Exchange Act of 1934. These laws forced corporations seeking money from the public to disclose a wide array of financial and legal information. All of this information would be regularly reviewed by the Securities and Exchange Commission (SEC). Private companies were limited to only 100 investors. However, following a wave of deregulation in the 1980s, the National Securities Markets Improvement Act of 1996 allowed private funds to raise unlimited money from an unlimited number of investors. Following this Act, the number of private companies skyrocketed as they faced significantly less regulation than public firms.
Why is the strategy so successful?
PE investments usually have a time horizon of four to seven years to yield favorable returns. General strategies revolve around cost-cutting: pay cuts, store closings and layoffs. In addition to Toys R Us, Sports Illustrated, Nabisco, Twitter and even Taylor Swift were all significantly affected by PE investments. However, not all PE interactions have negative outcomes. Dollar General and Michaels survived their buyouts as healthy companies. Under ideal circumstances, PE firms can offer the expertise to turn around poorly performing businesses by eliminating operational inefficiencies and increasing profits.
Most of the money is borrowed, and this debt is immediately transferred to the acquired company

Malachi Sheahan III
How does a PE firm finance its acquisitions?
Most of the money is borrowed, and this debt is immediately transferred to the acquired company. In the case of Toys R Us, the PE firm transferred billions of debt to the corporation. This is referred to as a leveraged buyout. So, at a time when Toys R Us should have been overhauling its infrastructure and strategies to compete with the growing online market, it had to use its revenue to pay off this massive debt. Despite remaining profitable, Toys R Us ultimately had to declare bankruptcy.
What else can PE firms do to ensure profit even if the acquired business eventually fails?
Since the PE firm now owns the acquired business, it can do a lot to harvest cash. A common tactic is the saleleaseback. In this case, the PE firm will instruct the company to sell assets to pay off the debt it has now incurred from the leveraged buyout. Often, a company’s most valuable asset is its real estate. In a sale-leaseback, the PE firm directs the company to sell its land to the firm, and then the firm will lease it back to the company. PE firms can also charge the acquired corporation exorbitant “management” fees. Since the firm owns the business, it doesn’t need to do anything to earn these fees.
One instructive example is the purchase of
continued on page 4
2
Vascular Specialist is the official newspaper of the Society for Vascular Surgery and provides the vascular specialist with timely and relevant news and commentary about clinical developments and about the impact of healthcare policy. Content for Vascular Specialist is provided by BIBA News. Content for the news from SVS is provided by the Society for Vascular Surgery. The ideas and opinions expressed in Vascular Specialist do not necessarily reflect those of the Society or the Publisher. The Society for Vascular Surgery and BIBA News will not assume responsibility for damages, loss, or claims of any kind arising from or related to the information contained in this publication, including any claims related to the products, drugs, or services, or the quality or endorsement of advertised products or services, mentioned herein. | The Society for Vascular Surgery headquarters is located at 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. | POSTMASTER: Send changes of address (with old
FROM THE COVER LEARNING CURVE: NEW DATA UNDERSCORE PHYSICIAN EXPERIENCE LEVELS REQUIRED TO DERIVE BENEFIT FROM TRANSFEMORAL CAROTID ARTERY STENTING
continued from page 1
perform in order to get an in-hospital stroke and death rate below 4% in symptomatic patients was 235.
Similarly, to achieve a stroke and death rate below 2% in asymptomatic patients, the threshold physicians had to reach to derive benefit was 13 procedures. Rates were based on the fact the best available VQI registry data relate to in-hospital stroke and death, not the 30day stroke and death thresholds of 6% and 3% for symptomatic and asymptomatic patients, respectively
Marc Schermerhorn, MD, chief of vascular surgery at Beth Israel Deaconess Medical Center in Boston, the study’s senior author, raised concerns over how the coverage expansion will interplay with data reporting and, ultimately, the tracking of stroke and death rates going forward.
“Now that CMS has done away with all
the regulations and restrictions on who can do [TfCAS] procedures, where, etc., people may not submit data to VQI anymore, unfortunately,” he said.
“There have been a lot of other studies that have shown transfemoral stenting outcomes are not as good as TCAR [transcarotid artery revascularization] and carotid endarterectomy, but I think the concern now is, by opening up the doors for anybody to do carotid stenting, there could be a lot of people who have never done carotid stenting before who now decide to get into the game.

Schermerhorn
“I think that the way things were before, when you had to be an approved center and you had to have credentialing committees that had to collect data, monitor that local data and submit it to Medicare, that prevented a lot of people from doing the procedure. So it concentrated in the people who have the most experience.”
But the respective thresholds for symptomatic and asymptomatic cases represent the basement of learning, continued Schermerhorn.
“You have to remember that transfemoral stenting has been around since the turn of the century—and even before that,” he said. “The VQI didn’t start collecting data on carotid stenting until 2005, and that was only in New England. It wasn’t until 2011 that we started to collect national data. So, most
SCVS 2024: NEW ANALYSIS POINTS TO LACK OF VASCULAR SURGICAL VOICES IN NEWS COVERAGE OF VASCULAR DISEASE
continued from page 1
vascular surgeons are “very underrepresented” in articles focused on both peripheral arterial disease (PAD) and carotid disease. In the case of the former, almost 20% of the articles included in their analysis involved vascular surgical voices, with just 17% of the items focused on carotid disease involving vascular surgeons.
The study comes in the wake of a series of articles appearing in the mainstream press in recent months, some of it controversial and involving coverage of inappropriateness in vascular interventions. More recent popular media reports saw the Society for Vascular Surgery (SVS) join a multispecialty coalition aimed at raising public awareness of PAD, which led to widespread coverage of vascular surgical voices in mainstream outlets.

Since initially performing the analysis on articles related to PAD and carotid disease, Abai and colleagues—including medical student Joshua Chen, BS, who helped develop the study—have probed vascular surgical involvement in news covering aneurysmal disease, arteriovenous fistulas and venous disease. Altogether, the results are “astounding,” he said.
Abai emphasized the need for vascular surgeons to push themselves to the front of vascular disease coverage to help the specialty gain brand awareness.
“The question becomes: how do we become the leaders in the dissemination of data, because we are the experts in these areas,” Abai said. “To us, it was very surprising we had such a low percentage in terms of our representation.”
He continued: “We have a branding issue. We need to go out there, do interviews on news channels, on TV, in newspapers and on the internet—the latter, in fact, might be the best channel for us to disseminate and use to promote vascular surgery as a brand and have much better representation on the disease processes that are key to vascular surgery.”
Addressing some of the more negative coverage that has appeared in the mainstream press in recent times, Abai sees a potential silver lining.
“It’s just like Hollywood,” he said. “Even bad press is not necessarily bad because it can bring visibility to your cause and what you are doing. Ultimately our goals are good. Our goals are to save limbs, our goals are to prevent strokes.
“Although I would hope we could [promote vascular surgery] in a more positive way because we don’t want the population to lose trust in us as physicians and as people who provide care for them.”
people who were in the carotid stent registries in the VQI had experience before they started submitting data, so we actually don’t think this is a full representation of the learning curve.
“We know almost certainly most people had been doing cases prior to entry of data into the VQI, so this is an absolute minimum threshold of learning curve, and the true learning curve is likely larger. I don’t know how much, but it’s higher numbers.”
Schermerhorn said that with the possibility of “a lot more novices” performing TfCAS in the wake of CMS coverage expansion, his team’s latest study clearly demonstrates “results are highly dependent on experience.” Even supposing a lot of TfCAS experience, he added, “the results don’t seem to be as good as with either TCAR or endarterectomy.”
Despite the potential for TfCAS entries into the VQI registry to decrease, Schermerhorn expects monitoring to continue, including via administrative databases, albeit with a lower level of clinical detail available, but expressed hope enough interest would persist in submitting data to the VQI.
“That’s my other concern,” he said, “The people who are interested in submitting data are probably the ones who are more committed to quality improvement and striving toward knowing what their outcomes are— and improving them.”
That raises another dimension of the study set to be presented at SCVS 2024, noted Schermerhorn: the research team also looked at whether those who had bad outcomes when they first started doing procedures were less likely to continue performing TfCAS. They found that this was indeed the case.
“The people who went on to do more than 25 procedures had better outcomes than the people who quit at up to 25 and then didn’t do anymore,” he said.
“We presume that there is some feedback to people and that, if they’re finding that their own results are not that good, then they don’t continue to do the procedure. If people don’t track their outcomes somewhere, then they may not know.
“That’s the problem. When you have a procedure with a low adverse outcome event rate, it’s hard for people to gain personal perspective.”
“The people who are interested in submitting data are probably the ones who are more committed to quality improvement”
MARC SCHERMERHORN
AVF 2024: NON-PNEUMATIC COMPRESSION DEVICE PERFORMED BETTER THAN ADVANCED PNEUMATIC COMPRESSION FOR LOWEREXTREMITY LYMPHEDEMA
continued from page 1
adherence during the study period, presenter Todd Berland, MD, director of outpatient vascular interventions at NYU in New York City, told those gathered.
The patients in the study had an average age of 58, and a majority of them were White women. Of the cohort, there were 11 with primary and 60 with secondary lymphedema, 34 were unilateral and 37 bilateral, and they had an average of eight years since diagnosis.
Berland outlined the non-pneumatic technology at hand: the battery-powered Dayspring (Koya Medical) device, which does not have a foot portion and allows users to walk, featuring components that “stretch and release, and fake or simulate a manual lymphatic massage experience,” Berland said. “Between the static compression that you get with the actual garment, the stretching and elongating phenomenon—and the fact that you can walk with the device, and really activate that calf muscle pump—may account for what we see here in this study, [where] we compare this device to commercially available advanced pneumatic plug-in-the-wall devices.”
The team randomized 99 patients to the non-pneumatic or advanced compression device, which patients then used for three months. “At the end of that three-month period, we checked quality-of-life and limb-volume measurements,” Berland said. “We then had them use nothing for one month, the washout period, to give us a new baseline. We rechecked limb volume and quality-of-life, and then the patients crossed over.”
After cross over, they used the opposite device that they were originally given for another three-month period. Measurements were taken of the patients’ lower extremities. Quality of life was also recorded at the end of three months. Patients were also given a diary to record their thoughts. Results showed a “statistically significant disruption in limb volume favoring the Dayspring device,” Berland said. “[We saw] a 370mm volume reduction in this group compared to an 83mm reduction in advanced pneumatic compression. When we look at the foot, there was actually no statistically significant difference here. Both devices and subgroups trended toward improved diameters and circumference of the foot,” he said.
The quality-of-life questionnaire also favored the Dayspring device, with the function, appearance and symptoms being rated as better than the advanced pneumatic compression device. Even when it came to how committed the patients in the study were, the Dayspring device had an adherence rate of 81% compared to the advanced pneumatic compression rate of 56%, Berland said. Some 78% of patients preferred the Dayspring device compared to 22% for advanced pneumatic compression, he added.
3 www.vascularspecialistonline.com
➽
➽
Marc
Babak Abai
FROM THE EDITOR THE DEVIL WE DON’T KNOW: THE CASE AGAINST PRIVATE EQUITY IN MEDICINE continued
the nursing home chain HCR ManorCare by a PE firm, the Carlyle Group, in 2007. As detailed in the New York Times, Carlyle paid just over $6 billion, most of which was borrowed. It then saddled ManorCare with the debt and recovered its investment by selling ManorCare’s real estate. ManorCare then had to pay rent for the buildings it once owned. Carlyle also charged ManorCare $80 million in transaction and advisory fees. ManorCare began cost-cutting programs and layoffs, resulting in health code violations. Eleven years after the purchase, ManorCare filed for bankruptcy with over $7 billion in debt. Carlyle, however, made millions over its initial investment. Carlyle executives even give talks at industry conferences about structuring investment portfolios to include nursing homes.
What would it look like if you planned a PE takeover of your household?
I’m glad you asked this oddly specific and leading question. I imagine the conversation with my wife would go as follows, “Look, you’re a good earner, but under investments and assets you wrote one word, ‘shoes.’ The nanny seems pretty frugal. I’m making Luisa the CFO. The two older kids are sunk costs at this point. But the youngest’s grammar school is crazy expensive. Also, he says he wants to be an artist. That’s a long road to a return on our investment. We are going to have to lay off Luke. And the dog.”
What makes healthcare attractive to PE firms?
The healthcare industry is often seen as recession proof.
The U.S. spends about $4.5 trillion on healthcare, almost 20% of its gross domestic product, the highest among developed countries. PE firms see this spending as a spigot, unlikely to be turned down.
Over the past decade, almost $1 trillion has been spent by PE in acquiring medical practices. And now that we know the PE playbook, the results are predictable. The goal of purchasing physician practices is the same as for buying companies. Turn a 20–30% profit on investment in four to seven years.
PE acquisitions of physician practices rose from 75 in 2012 to 484 in 2021. In more than one fourth of metropolitan areas, a PE firm has at least a 30% market share in a medical specialty. Studies have shown that prices rise when PE firms achieve this 30% threshold. Nationally, 25–40% of emergency rooms are staffed by PE firms.
A JAMA Internal Medicine study by La Forgia and colleagues showed that prices charged by PE-backed anesthesia groups rose 26% from 2012–2017. The financial burden is passed on to patients through higher outof-pocket fees and rising premiums. The No Surprises Act was a response to unsavory PE billing policies. It is unlikely that physicians see much of the increased revenue, as PE’s goal is to increase profits for its investors. In fact, many PE-owned anesthesia practices replace physicians with nurse anesthetists to save money.
In dermatology practices, physicians have been told to generate profits by increasing elective procedures, ancillary services, and charges. This profit-driven model also threatens health equity. Reimbursements can be maximized by prioritizing commercially insured patients in higher-income communities. Quicker, lower-complexity procedures are also emphasized over delivering complex care.
Scale of PE role in medicine
The true influence of PE in medicine is difficult to measure as their firms have few ownership disclosure requirements. Also, the physicians are routinely required
to sign non-disclosure agreements. Even for doctors getting acquired, it can be impossible to tell who is truly buying their practice. This lack of transparency makes monitoring the actual effects of PE on healthcare nearly impossible. Still, what we do know is damning. In deference to my poorly enforced word count and readers’ attention span, I will not detail all of PE’s plundering and blundering exploits in medicine. But for those not convinced, simply search Envision Healthcare, US Anesthesia Partners, Kool Smiles, or Prospect Medical Holdings.
I believe PE acquisitions are just a symptom of healthcare’s overall problems. Physicians are selling their practices because it is too hard to remain financially solvent on their own. Paperwork, legal requirements,
from page 2
as naming the physicians as practice owners while having a parent company control the actual finances.
In the world of corporate medicine, these are known as “friendly” or “straw” doctors. Often, they will have their name attached to hundreds of practices. Amazon’s One Medical primary care subsidiary and UnitedHealth-owned Optum Health have been accused of this practice. Oregon is currently debating a bill to outlaw this “corporate practice of medicine.” Both Amazon and UnitedHealth Group have retained lobbyists to oppose it.
PE firms also protect themselves politically. Their employees include former cabinet members, secretaries of state, chairmen of the SEC, chairmen of the Federal Trade Commission. speakers of the House, a CIA director,

Much can be done to combat PE’s influence on medicine. Financial and bureaucratic burdens on practicing physicians must be eased
electronic health records and insurance practices have all placed incredible strain on private practitioners. The majority of physicians enter practice with extraordinary educational debt. Hospital system consolidations make it difficult for smaller practices to compete. Many physicians reject the notion of hospital employment but have few options. PE employment offers a potentially lucrative alternative.
The specter of non-compete clauses and loopholes
In addition to raising prices, PE firms strive to generate more income from physician practices by purchasing lower-cost supplies, substituting lowerpaid staff such as medical assistants for nurses, having physicians see more patients, and seeking a better payor mix. The firms also lock the physicians into the practice through non-compete clauses.
The American Academy of Emergency Physicians notes: “The goal of non-compete clauses is to intimidate the emergency physician into unquestioning servitude to business interests. Given physicians’ ethical obligation to patients, many continue to speak out for patient safety; however, knowing that they can be fired at will and then forced to relocate their family to another city or state can have a chilling effect on physicians’ advocacy for patients.”
The legal ability of PE firms and their medical management companies to control medical decisionmaking and clinical care is determined at the state level and varies enormously. Nearly 20 states have no rule prohibiting medical management companies from manipulating clinical practice and medical judgment. Even where regulations exist, PE firms can find loopholes, such
Still, much can be done to combat PE’s influence on medicine. Financial and bureaucratic burdens on practicing physicians must be eased. Indiana, for example, recently passed a tax credit for independent physicians. Other possible financial improvements include Centers for Medicare & Medicaid Services (CMS) payment reforms, reconsidering fee-for-service, and capitated payments for quality care.
Uniting with other specialties to support complete ban
The most direct and achievable method for curbing the undesired aspects of PE influence on physician practices may be to enforce the FTC’s proposed ban on noncompete clauses. If PE firms could not prevent physicians from walking away, it would force them to change their approach to management. Instead of rampant cost-cutting and forcing physicians to do more with less, this could incentivize PE to retain doctors by improving salaries and working conditions.
Even if enacted, the FTC’s proposed non-compete ban will likely face many challenges in court. Most conservative judges, including some on the Supreme Court, have signaled that they don’t favor federal agencies asserting new regulatory authority based on old statutes.
Vascular surgeons should join with other specialties that have already been pillaged by PE to support a complete ban on non-compete clauses for doctors. Only by uniting our physician advocacy efforts do we stand a chance against the private equity-backed lobbyists.
MALACHI SHEAHAN III is the chief medical editor of Vascular Specialist. His opinions do not reflect SVS policy or positions.
4 Vascular Specialist | March 2024







INDICATIONS The Perclose™ ProStyle™ Suture-Mediated Closure and Repair (SMCR) System is indicated for the percutaneous delivery of suture for closing the common femoral artery and vein access sites of patients who have undergone diagnostic or interventional catheterization procedures. The Perclose™ ProStyle™ SMCR System is used without or, if required, with adjunctive manual compression. For access sites in the common femoral artery using 5F to 21F sheaths. For access sites in the common femoral vein using 5F to 24F sheaths. For arterial and venous sheath sizes greater than 8F, at least two devices and the pre-close technique are required. See Important Safety Information referenced on the next page. Information contained herein for DISTRIBUTION in the U.S. ONLY. www.cardiovascular.abbott ©2023 Abbott. All rights reserved. MAT-2302752 v1.0 Page 1 of 2 Perclose™ ProStyle™ Sutur e - Mediated Closure and Repair S ys tem Early ambulation and early discharge—two big reasons my patients and I like Perclose ProStyle” Dr. Jackson Liang, Electrophysiologist University of Michigan Don’t keep your patients waiting From unrestricted bed mobility to early ambulation and discharge, choose the Perclose ™ ProStyle ™ SMCR System.
Perclose™ ProStyle™ Suture-Mediated Closure and Repair (SMCR) System
INDICATIONS
The Perclose™ ProStyle™ Suture-Mediated Closure and Repair System is indicated for the percutaneous delivery of suture for closing the common femoral artery and vein access sites of patients who have undergone diagnostic or interventional catheterization procedures.
The Perclose™ ProStyle™ SMCR System is indicated for closing the common femoral vein in single or multiple access sites per limb.
The Perclose™ ProStyle™ SMCR System is used without or, if required, with adjunctive manual compression.
For access sites in the common femoral artery using 5F to 21F sheaths. For arterial sheath sizes greater than 8F, at least two devices and the pre-close technique are required.
For access sites in the common femoral vein using 5F to 24F sheaths. For venous sheath sizes greater than 14F, at least two devices and the pre-close technique are required.
CAUTION
Federal law restricts this medical device to sale by or on the order of a physician (or allied healthcare professionals, authorized by, or under the direction of, such physicians) who is trained in diagnostic and / or interventional catheterization procedures and who has been trained by an authorized representative of Abbott.
Prior to use, the operator must review the Instructions for Use and be familiar with the deployment techniques associated with the use of this device.
During closure of access sites using a procedural sheath greater than 8F, it is recommended that a vascular surgeon or a surgeon with vascular training be available in case surgical conversion to control bleeding and to repair the vessel is needed.
CONTRAINDICATIONS
There are no known contraindications to the use of this device.
WARNINGS
Do not use the Perclose™ ProStyle™ SMCR System if the packaging or sterile barrier has been previously opened or damaged or if the components appear to be damaged or defective.
DO NOT RESTERILIZE OR REUSE. The Perclose™ ProStyle™ SMCR System is intended for single use only.
Do not use the Perclose™ ProStyle™ SMCR System if the sterile field has been broken where bacterial contamination of the sheath or surrounding tissues may have occurred, since such a broken sterile field may result in infection.
Do not use the Perclose™ ProStyle™ SMCR System if the puncture site is located above the most inferior border of the inferior epigastric artery (IEA) and / or above the inguinal ligament based upon bony landmarks, since such a puncture site may result in a retroperitoneal hematoma. Perform a femoral angiogram to verify the location of the puncture site. Note: This may require both a right anterior oblique (RAO) and left anterior oblique (LAO) angiogram to adequately visualize where the sheath enters the femoral vessel.
Do not use the Perclose™ ProStyle™ SMCR System in arterial or venous access if the puncture is through the posterior wall or if there are multiple punctures in the same access site, since such punctures may result in a hematoma or retroperitoneal bleed.
Do not use the Perclose™ ProStyle™ SMCR System if the puncture site is located in the superficial femoral artery or the profunda femoris artery, or the bifurcation of these vessels, since such puncture sites may result in a pseudoaneurysm, intimal dissection, or an acute vessel closure (thrombosis of small artery lumen). Perform a femoral angiogram to verify the location of
the puncture site. Note: This may require both a right anterior oblique (RAO) and left anterior oblique (LAO) angiogram to adequately visualize where the sheath enters the vessel.
PRECAUTIONS
1. Prior to use, inspect the Perclose™ ProStyle™ SMCR System to ensure that the sterile packaging has not been damaged during shipment. Examine all components prior to use to verify proper function. Exercise care during device handling to reduce the possibility of accidental device breakage.
2. As with all catheter-based procedures, infection is a possibility. Observe sterile technique at all times when using the Perclose™ ProStyle™ SMCR System. Employ appropriate groin management, as per hospital protocol, post-procedure, and posthospital discharge to prevent infection.
3. Use a single wall puncture technique. Do not puncture the posterior wall of the vessel in arterial and venous access.
4. Do not deploy the Perclose™ ProStyle™ Device at an elevated angle against resistance as this may cause a cuff miss or device breakage.
5. There are no reaccess restrictions if previous arteriotomy / venotomy repairs were achieved with Abbott Medical SMC or SMCR systems.
6. If significant blood flow is present around the Perclose™ ProStyle™ Device, do not deploy needles. Remove the device over a 0.038" (0.97 mm) (or smaller) guide wire and insert an appropriately sized sheath.
7. Prior to depressing the plunger to advance the needles, stabilize the device by the body to ensure the foot is apposed to the vessel wall and the device does not twist during deployment. Twisting (torquing) the device could lead to needle deflection resulting in a cuff miss. Do not use excessive force or repeatedly depress the plunger. Excessive force on the plunger during deployment could potentially cause breakage of the device, which may necessitate intervention and / or surgical removal of the device and vessel repair.
8. Do not apply excessive force to the lever when opening the foot and returning the foot to its original position down to the body of the device. Do not attempt to remove the device without closing the lever. Excessive force on the lever or attempting to remove the device without closing the lever could cause breakage of the device and / or lead to vessel trauma, which may necessitate intervention and / or surgical removal of the device and vessel repair.
9. Do not advance or withdraw the Perclose™ ProStyle™ Device against resistance until the cause of that resistance has been determined. Excessive force used to advance or torque the Perclose™ ProStyle™ Device should be avoided, as this may lead to significant vessel damage and / or breakage of the device, which may necessitate intervention and / or surgical removal of the device and vessel repair.
10. If excessive resistance in advancing the Perclose™ ProStyle™ Device is encountered, withdraw the device over a 0.038" (0.97 mm) (or smaller) guide wire and reinsert the introducer sheath or use manual compression.
11. Remove the Perclose™ ProStyle™ sheath before tightening the suture. Failure to remove the sheath prior to tightening the suture may result in detachment of the tip of the sheath.
12. Care should be taken to avoid damage to the suture from handling. Avoid crushing damage due to application of surgical instruments such as clamps, forceps or needle holders.
13. For catheterization procedures using a 5F – 8F procedural sheath, use manual compression in the event that bleeding from the femoral access site persists after the use of the Perclose™ ProStyle™ SMCR System to obtain hemostasis.
14. For catheterization procedures using a procedural sheath > 8F, use manual compression, compression assisted devices, surgical repair, and / or other appropriate treatment methods in the event that bleeding from the femoral access site persists after the use of the Perclose™ ProStyle™ SMCR System to obtain hemostasis.
15. For catheterization procedures using a procedural sheath > 8F, where the operating physician is not a vascular surgeon, it is recommended that a vascular surgeon or a surgeon with vascular training be available during the procedure to perform any necessary vascular surgical intervention.
16. If the Perclose™ ProStyle™ Device is used to close and repair multiple access sites in the same vessel, space the access sites apart adequately to minimize sheath-device interference.
POTENTIAL ADVERSE EVENTS
Potential adverse events associated with use of vessel closure devices may include, but are not limited to, the following:
• Allergic reaction or hypersensitivity to device components
• Vascular access complications which may require transfusion or vessel repair, including:
• Anemia
• Aneurysm
• Arteriovenous fistula
• Bleeding / hemorrhage / re-bleeding
• Bruising / hematoma
• Embolism
• Inflammation
• Intimal tear / dissection
• Perforation
• Pseudoaneurysm
• Retroperitoneal hematoma / bleeding
• Scar formation
• Wound dehiscence
• Cardiac arrhythmias (including conduction disorders, atrial and ventricular arrhythmias)
• Atrial arrhythmias
• Ventricular arrhythmias
• Femoral artery / venous complications which may require additional intervention, including:
• Arterial / venous stenosis
• Arterial / venous occlusion
• Arteriovenous fistula
• Intimal tear / dissection
• Ischemia distal to closure site
• Nerve injury
• Numbness
• Thrombus formation
• Vascular injury
• Venous thromboembolism (including deep vein thrombosis, pulmonary embolism, postprocedure pulmonary embolism)
• Infection – local or systemic
• Pain
• Hemodynamic instability:
• Hypotension / hypertension
• Vasovagal episode
• Death
• Device complications
• Device failure
• Device malfunction
CAUTION: This product is intended for use by or under the direction of a physician. Prior to use, reference the Instructions for Use, inside the product carton (when available) or at vascular.eifu.abbott or at medical.abbott/manuals for more detailed information on Indications, Contraindications, Warnings, Precautions and Adverse Events. This material is intended for use with healthcare professionals only.
Illustrations are artist’s representations only and should not be considered as engineering drawings or photographs. Photo on file at Abbott.
Information contained herein for DISTRIBUTION in the U.S. ONLY.
Abbott 3200 Lakeside Dr., Santa Clara, CA 95054 USA, Tel: 1.800.227.9902
™ Indicates a trademark of the Abbott Group of Companies.
www.cardiovascular.abbott
©2023 Abbott. All rights reserved. MAT-2302752 v1.0
Page 2 of 2
IMPORTANT SAFETY INFORMATION
ICOMMENT& ANALYSIS
CORNER STITCH
GRIT: THE VALUE OF GROWTH MINDSET AND PERSISTENCE AS A VASCULAR TRAINEE
By Kevin Mangum, MD
ONE OF THE BIGGEST MENTAL SHIFTS I HAD TO make during residency was my view on failure. I literally had to rebrand failure. As a medical student, and like many of my peers, I had been conditioned to automatically feel shame if I didn’t know an answer. Even as an intern, I held the view that if I didn’t know an answer on rounds, in the operating room, or if I made a mistake during my 24-hour call shift overnight, that I was a terrible resident. Fortunately, this view was gradually debunked through perspectives and experiences that highlighted the necessity, importance and inescapable reality of failure.
Often, our views of failure are self-defined, meaning that when we “fail,” it’s because we haven’t met our own standards and expectations for how we think we should have performed. Such a fixed perception of oneself as a “good” or “bad” resident, with zero gray area in between, impedes that of a growth mindset, in which the central driver is “how can I be better than I was before, even in the smallest way possible?” This concept of a growth mindset is not novel. Referred to in the business field as “continuous improvement” or “incremental theory,” growth mindset has been considered a beacon not just at
GOVERNMENT GRAND ROUNDS
the individual level but has been applied to improvement within large corporations as well. A Harvard Business Review article distinguishes those who are motivated, arguably even obsessed with learning and growing after failure, in contrast to individuals who are paralyzed and shut down after failure.
 Kevin Mangum
Kevin Mangum
So can a growth mindset be taught? In particular, can those who respond negatively to failure be taught how to thrive and perhaps even learn to enjoy failure? The education arena is one of the best and most studied examples of this. In fact, a 2019 national study of learning mindsets published in Nature was the largest intervention-based study on the effect of mindset on achievement and found that teaching growth mindset skills could improve grades among lower-achieving students and increase enrollment in advanced mathematics classes.
But can growth mindset be applied to surgical training, especially in vascular surgery? Vascular surgery is a fluid and growing specialty. In a field of rapidly evolving technology and newly published trials that influence how we practice, it’s fundamental to grow with the specialty. As a vascular trainee, one of the aspects I love most is the need to adapt while staying grounded in fundamental skills. With all of this said, however, I acknowledge that mastering the abundance of skillsets in the field amid an ever-growing body of knowledge is intimidating.
So I go back to my initial question: how can growth mindset be incorporated into vascular surgery, to fully embrace all of these developments in which “failure” to some degree is inevitable? As trainees, we have to start
seeing the opportunities for growth in every aspect of our training and patient care. For example, during an operative case, we must be goal-directed and hold ourselves accountable for identifying how we can improve, especially seeking out targeted, specific feedback. Effective strategies can include asking attendings for three areas of improvement at the conclusion of a case, or even going into a case knowing precisely what skills you want to develop. How we receive the feedback is equally as important as getting it; we can’t take it personally, which can be challenging, since so much of our identities as surgeons in training is wrapped up in our performance. We can also detach from our performative view of ourselves, instead leaning into our identity as continuous learners.
With our own recognition of and connection to our identity as seekers of continuous improvement, we can become more resilient and persistent in the face of challenge, since we no longer count ourselves out of the game if we don’t meet our own expectations. In this manner, we can give ourselves some grace, such that in the face of real challenge, we can persevere and insist of ourselves that we keep going—that we keep growing.
So perhaps we can reframe training as a bridge to continuous improvement of our patients and ourselves as practitioners, realizing that the specialty we’ve chosen is naturally and excitingly one that is constantly growing. We have the privilege to grow with it.
KEVIN MANGUM is a PGY5 vascular surgery resident in his second research year at the University of Michigan.
I’m just a bill: An overview of health-related committees on Capitol Hill
By Kelli Summers, MD
n the U.S., the legislative process is complex.
Among the most important in this process are congressional committees, which play a pivotal role in shaping policy concepts, drafting legislative proposals and shepherding them through the path to becoming law. These committees are specialized groups of members with expertise in relevant policy areas. There are key committees known as our “Committees of Jurisdiction,” where legislation relevant to vascular surgery is channeled.
When a bill is introduced in the House of Representatives or the Senate, it typically undergoes a series of committee hearings and markups. Committee members gather valuable information through hearings. During “markups,” committee members critically review and refine the proposed legislation, incorporate amendments and deliberate the proposed legislation. Following these deliberations, the committee votes on whether to advance the bill to the full chamber for consideration. This process allows for thorough examination and refinement of legislation before reaching the broader legislative body.
The Senate Finance Committee,
responsible for matters pertaining to taxation and revenue measures, wields extensive jurisdiction within the Senate. These large and powerful committees are broken down into subcommittees, where legislation is analyzed by subject matter. The Subcommittee on Healthcare has jurisdiction over anything related to healthcare finances, meaning it can have joint or sole jurisdiction over the activities of various agencies and offices. This includes the Department of Health and Human Services (HHS), which oversees the Centers for Medicare & Medicaid Services (CMS). This overarching influence makes this committee powerful regarding any legislation that touches federal revenue streams. Another example is the Senate Appropriations Committee, where subcommittees are tasked with drafting legislation to allocate funds.
Outside of the budgeting process, there are subject matter committees, such as the Committee on Health, Education, Labor, and Pensions, simply known as HELP. The HELP Committee’s jurisdiction includes most federal labor and employment laws, including those that regulate wages and hours of employment. For
vascular surgeons, the HELP Committee holds significant importance due to its jurisdiction over legislation related to healthcare policies and regulations. The committee’s decisions on healthcare reform, medical device regulations, workforce training, and research funding profoundly influence the practice environment, reimbursement structures, and access to innovative treatments. The actions and policies shaped by the Senate HELP Committee have a direct bearing on advancing vascular surgery services and patient care outcomes.
The House of Representatives has a complementary structure, with its own Committee on Appropriations with a Subcommittee on Labor, Health and Human Services, Education and Related Agencies. The House of Representatives and Senate committees individually create budgets and then come to an agreement by the end of each fiscal year to prevent a government shutdown.
In terms of subject matter, two of the most influential committees on health policy in the House are the Committee on Ways and Means and the Committee on Energy and Commerce, both of which
have health subcommittees. The Ways and Means Committee primarily deals with taxation, social welfare programs and trade, whereas the Energy and Commerce Committee addresses energy, healthcare, telecommunications and consumer protection issues. These committees differ from appropriations as they work with the content of the proposed legislation, compared to the Appropriations Committee, which focuses on simply allocating federal funds.
The committees of jurisdiction in both chambers of Congress serve as crucial gatekeepers in the legislative process, overseeing specific policy areas and shaping the trajectory of proposed bills. Their role is pivotal in ensuring that proposed laws undergo rigorous scrutiny and reflect a comprehensive understanding of the issues. By serving as conduits for legislative action, these committees contribute to the effectiveness and integrity of the legislative process, fostering informed decision-making and accountability within Congress.
KELLI SUMMERS is a graduate of the SVS’ Advocacy Leadership Program.
7 www.vascularspecialistonline.com
ClotTriever BOLD®
Catheter
Trusted Performance. Faster Procedures.
The Next Generation ClotTriever BOLD catheter features a ~30% shorter collection bag with HyperClear™ surface technology for improved procedure time and the same trusted performance of ClotTriever.†

Interim 2-year outcomes from the CLOUT registry show the long-term clinical benefits of wall-to-wall clot removal with the ClotTriever system.1,2
>90% complete or near-complete clot removal*
†Engineering bench testing. Data on File
93% none or mild PTS symptoms at 2 years
*Effectiveness primary endpoint of ≥75% thrombus removal assessed by independent core laboratory

References:
1. Bisharat, et. al. JSCAI. 2024.
2. Dexter, D. Two-year interim outcomes from the fully enrolled CLOUT registry. AVF 2024.
Indications For Use:
The ClotTriever thrombectomy system is indicated for (1) the non-surgical removal of thrombi and emboli from blood vessels; (2) injection, infusion and/or aspiration of contrast media and other fluids into or from a blood vessel. The ClotTriever thrombectomy system is intended for use in the peripheral vasculature, including deep vein thrombosis (DVT). Refer to IFU for complete Indications for Use, contraindications, warnings, and precautions.
Caution: Federal (USA) law restricts this device to sale by or on the order of a physician
All trademarks are property of their respective owners.
MM-01816_Rev. B_2024-02-26
Next Generation


Tackling DVT head on: Single-session, wall-to-wall thrombus removal with the ClotTriever BOLD
Several years ago, when Nicolas Mouawad, MD, division chief of vascular surgery at McLaren Health in Bay City, Michigan, was confronted with an emergency case of deep vein thrombosis (DVT) in which the patient presented with phlegmasia, he faced a dilemma. With the traditional lytic intervention off the table due to the urgent need for an immediate response, Mouawad turned to a new device he hadn’t used before. For the first time, the ClotTrieverTM System provided Mouawad a DVT intervention procedure with a lytic-free approach in a single-session treatment with wall-to-wall thrombus removal, providing the patient with immediate symptom relief.1
Here, he outlines the current picture of his venous thromboembolism (VTE) practice, how that emergency case helped evolve how he tackles DVTs in appropriate patients, and how he sees the DVT treatment landscape developing going forward.
What does your current venous disease practice look like?
We have a comprehensive venous practice. We manage superficial veins and deep venous disease as well as pulmonary embolism (PE)—the full VTE disease spectrum. We see a significant number of patients who come in with DVT and post-thrombotic syndrome (PTS), as well as with venous leg ulcers, so we feel very comfortable managing the wide array of patients suffering from venous insufficiency and VTE.
Could you expand upon how you go about managing patients with DVT?
Our DVT management is multi-fold. The goal is to, first, relieve the patient’s symptoms, such as significant venous claudication or severe swelling that they find quite bothersome, or pain. Of course, we start with anticoagulation; however, a propor tion of patients presenting with this pa thology we feel benefit from interven tion. Thinking further down the line, we want to avoid patients having significant sequelae of DVT, which, in up to 50% of patients with DVT, means PTS. Presently, these PTS patients are treated using the current stan dard of care, which is anticoag ulation and elastic compression stockings. Even though they’re
undergoing currently recommended treatments, these patients still develop long-term sequelae of PTS, so our goal here is to help mitigate the possibility of them developing these sequelae.
Can you describe how the ClotTriever first made its way into your toolkit?
Like a lot of other vascular specialists, I was using other devices on the market for the management of patients with DVT. I remember very vividly the first patient I treated with the ClotTriever System presented with phlegmasia. Even though I would consider our traditional treatment algorithm which was thrombolytic therapy, that would not be able to deliver an immediate resolution of the problem. What we needed was an immediate treatment for this patient who essentially had a surgical emergency. My hand was forced to try something that was immediate, single session and able to deliver a result without long infusion times. That case was around six years ago, and, frankly, we haven’t looked back since I started doing this type of treatment.
How does the ClotTriever System differ from other modes of intervention for the treatment of DVT?
Multiple variables of the system are beneficial to me. First, the ClotTriever is a single-session device. Bringing the patient back can be challenging, so a single-session device is important to me. Next, I don’t worry about the chronicity of the thrombus. Patients present within one or two days of discomfort, but we all know that the thrombus has probably been there longer. The symptoms may be acute, but the thrombus itself is likely sub-acute and even older. I have been using the ClotTriever BOLD Catheter to eliminate any guesswork on clot chronicity. Lastly, the unique device design allows me to remove wall-adherent thrombus to minimize residual vein obstruction. In terms of residual vein obstruction, creating more than just a channel with other thrombectomy devices is an important consideration regarding long-term outcomes.





Can you outline ways in which the device has evolved your DVT practice?
There is no associated ICU [intensive care unit] stay like there is when using thrombolytic therapy. There are no associated costs for pharmacologic therapy. There is no need for any capital equipment. Those were the benefits early on. To date, more than 50,000 ClotTriever cases have been performed. Additionally, there exists a plethora of data to support the device. Very aggressive efforts have been made to look at the data. The CLOUT registry is the largest study to assess mechanical thrombectomy to date, with interim two-year outcomes that showed 93% of limbs had none or mild PTS.3 Additionally, my experience—and histological analyses of ClotTriever cases— have not identified any cases where there has been venous valve or vessel wall damage.4 I’ve performed more than 200 DVT cases using the ClotTriever System and seen patients back with marked improvement in their discomfort and Villalta scores for PTS. I don’t think that would have been possible if we were ripping out valves or damaging the vein walls.
What do you think the future holds for DVT treatment?
For me, it’s important to be able to work with the groups investing in data. Unfortunately, the guidelines lag well behind what we see in practice. Of course, that is because a lot of data are necessary before guidelines can be created. Those data are forthcoming, however. The DEFIANCE randomized controlled trial (RCT)—currently the only RCT assessing DVT interventions—will be one such source. DEFIANCE, which compares iliofemoral DVT patients treated with the ClotTriever System versus anticoagulation only, should help support what we see day-to-day in our regular practice.

Pre-procedural venogram shows the extent of thrombus burden (1); postClotTriever venogram (2); thrombus extracted (3); pre-procedural IVUS shows extent of thrombus (4); and post-procedural IVUS demonstrates complete thrombus removal (5)
CASE REPORT
A woman in her early 60s presented with right leg pain and swelling. An ultrasound revealed unilateral right iliofemoral DVT, and the decision to intervene using the ClotTriever BOLD Catheter was made.
Procedural overview
The right popliteal vein was accessed with a micropuncture needle and wire under ultrasound guidance, and exchanged for a microsheath, ultimately upsizing to a short 10F sheath. A venogram demonstrated significant thrombus within the femoropopliteal segment, common femoral vein and extending into the external iliac vein. The lesion was crossed into the inferior vena cava (IVC). Next, pullback intravascular ultrasound (IVUS) from the IVC to the access site was performed to identify the extent of thrombus. A glidewire was advanced up into the right subclavian vein, and a vertebral catheter was advanced over it. Next, the glidewire was exchanged for a guidewire 7cm tip. A 19F dilator was used, followed by insertion of the ClotTriever sheath. The funnel was deployed under fluoroscopic guidance and the ClotTriever BOLD Catheter was advanced into the popliteal vein. The nitinol coring element and mesh collection bag were then deployed at the iliac vein, and the catheter was then retracted, capturing and removing significant acute thrombus. In total, four ClotTriever BOLD passes were completed. Completion IVUS showed complete thrombus removal. Completion venogram demonstrated brisk cephalad flow. Total procedure time was 35 minutes, while total device time was 10 minutes. There was estimated total blood loss of 20ml.
Conclusion
The patient’s pain resolved immediately postprocedure, with the swelling improving greatly. In followup, the swelling was resolved and the patient is doing well.
9 www.vascularspecialistonline.com
ADVERTORIAL | SPONSORED BY INARI MEDICAL
Nicolas Mouawad
1 2 5 4 3
1. Dexter et al JSCAI. 2024. 2. Kahn SR, et al J Thomb Thrombolysis. 2016. 3. Dexter, D. Interim two-year outcomes from the fully enrolled CLOUT registry. AVF. 2024. 4. Silver MJ, et al Catheter Cardiovasc Interv. 2021. The ClotTriever Thrombectomy System is indicated for (1) the non-surgical removal of thrombi and emboli from blood vessels; and (2) injection, infusion and/or aspiration of contrast media and other fluids into or from a blood vessel. The ClotTriever Thrombectomy System is intended for use in the peripheral vasculature, including deep vein thrombosis (DVT). Refer to IFU for complete indications for use, contraindications, warnings and precautions. Caution: Federal (USA) law restricts this device to sale by or on the order of a physician. All trademarks are property of their respective owners.
Vascular surgery resident reflects on Match Day experience
Integrated vascular surgery resident Eric Smith, MD, tells Marlén Gomez how he handled the lead up to Match Day.
FOR MEDICAL STUDENTS HOPING TO SPECIALIZE IN vascular surgery, the eagerly anticipated Match Day (March 15) marks a pivotal career moment. Organized by the National Resident Matching Program (NRMP), it is the culmination of years of hard work, education and clinical experience.
The excitement of imminent professional growth is tinged with the uncertainty of where they will spend the next phase of their medical journey. The days preceding Match Day are a flurry of final preparations, with SVS members revisiting residency programs and seeking advice from mentors to navigate the pivotal decisions ahead.
Eric Smith, a postgraduate year one (PGY-1) integrated vascular surgery resident at the University of California San Francisco and a 2021 SVS Diversity Medical Student Vascular Annual Meeting (VAM) Travel Scholarship winner, shares in sights into the emotional whirlwind leading up to Match Day.
“Once your exams are done, the thing that people should try to remember is to focus on everything that you’ve accomplished to reach this point, so that it keeps you grounded. Medical school goes by so fast, and it’s nice to just sit and take a breather,” said Smith.
Recalling the sleepless nights and stressful dreams preceding the decision, Smith emphasizes the importance of maintaining mental well-be ing during this anxious period. His advice to med ical students is to take control of their situation and time, ensuring a comfortable mental space. He and his partner would engage in activities such as hiking or spending time with family to clear his mind.

“I spent a lot of time travelling—but even though I wanted to be back in the operating room, people had to keep me away for my own good,” said Smith.
Finally, Match Day arrives, and the anticipation peaks. Medical students, alongside their counterparts across the nation, will open their envelopes to discover where they will be completing their vascular surgery residencies. The mixed emotions are evident—joy, relief and perhaps a touch of nostalgia for the programs that brought them to this point.
Smith shared his personal experience, recounting how, by
DIVERSITY MEDICAL STUDENTS ADVOCATE FOR WOMEN’S VASCULAR HEALTH
By Marlén Gomez
In celebration of Women’s History Month, the Society for Vascular Surgery (SVS) Foundation’s “Voices of Vascular” series is underscoring women’s contributions to the specialty. The SVS Foundation initiative champions female accomplishments, emphasizing the pivotal role they play in helping shape vascular surgery, enhancing patient care and contributing to a healthier world.
Three medical students, Nishita Vootukuru, Shannon McDonnell and Kundanika Lakkadi, have shared their insights on why it is imperative to fund the future of medicine, particularly in the context of women’s health.
Vootukuru, a second-year medical student at Rutgers New Jersey Medical School, emphasizes the urgent need to address women’s unique challenges in receiving diagnoses and treatments for vascular disease.
“As a student in the vascular community, the imperative nature of addressing the unique challenges women face in receiving diagnoses and treatments for vascular disease is evident. Through initiatives like Voices of Vascular, we can work towards supporting research tailored to women’s health needs, ultimately improving outcomes for all,” said Vootukuru.
Throughout the month, the SVS Foundation and the SVS Women’s Section
Steering Committee will honor SVS members for their life-saving care and pioneering research in the fight against vascular disease. The Society shared a video from members on its social media channels explaining the importance of giving for Women’s History Month.
McDonnell, currently in her fourth year of medical school at Loyola University in Chicago, credits the mentorship she received from female vascular surgeons as a driving force behind her decision to pursue vascular surgery. She highlights these mentors’ multifaceted roles, serving as researchers, leaders in their field and mothers.
McDonnell emphasizes the importance of representation, stating, “Envisioning myself in similar roles not only served as an enormous inspiration but also underscored the importance of representation as a minority in such an important and ever-growing specialty.
“As the field of vascular surgery continues to evolve, sponsoring women’s research will allow our many female surgeons to improve patient outcomes and recruit more diverse perspectives to the specialty.”
Lakkadi, a fourth-year medical



“Envisioning myself in similar roles not only served as an enormous inspiration but also underscored the importance of representation as a minority in such an important and evergrowing specialty”
SHANNON MCDONNELL






10 TRAINING
Eric Smith
Nishita Vootukuru
Kundanika Lakkadi
Shannon McDonnell
RELIABLE
VTI’s single-use surgical Doppler probes provide a high degree of reliability since probe failure due to reprocessing is eliminated.
COST EFFECTIVE
The hidden costs associated with reusable probes, including reprocessing and lost OR time due to probe malfunctions, are eliminated.
MULTI-FUNCTIONAL
Provides real-time intraoperative and transcutaneous evaluation of blood flow, for ALL your surgical needs.
Call 800-550-0856 or visit us at VTI-online.com to learn more about our Doppler, including a complimentary analysis of your “hidden costs”. Find out why the TQI Doppler provides a high degree of performance reliability and is a more cost-effective solution for ORs.


















Confident in Your Doppler!
Be
Visit
our TQI product page on our website. The Trans-Q-taneous Intraoperative “TQI” Doppler System is the Doppler you can rely on for all your surgical needs.
vti-online.com
info@vti-online.com
Reach for the Doppler that Works Every Time
603-594-9700
ADOPTION OF AI INTO WORKFLOW ASSOCIATED WITH FASTER TIME TO ASSESSMENT OF PE PATIENTS
An abstract presented at the 2024 American Venous Forum (AVF) annual meeting (March 3–6) revealed that, in the treatment of patients with pulmonary embolism (PE), the implementation of artificial intelligence (AI) software has been linked to a shorter time to assessment. By
Jocelyn Hudson
AT THE TAMPA, FLORIDA-HOSTED meeting, Jacob Shapiro, MD, shared this and other key findings from a review of patients diagnosed with PE at a single center over a six-year period.
Shapiro, a resident at TriHealth in Cincinnati, Ohio, and colleagues outlined in their abstract that the serious and potentially life-threatening nature of PE necessitates a “streamlined PE workflow with timely assessment and initiation of treatment” to potentially improve a patient’s chance of survival.
They pointed to the increasing use of AI in healthcare as a means of improving clinical efficiency.
The authors detailed that, in October 2022, TriHealth implemented an AI-powered par-
PRESIDENTIAL ADDRESS
allel workflow tool designed to automatically detect and triage patients with suspected PE. The aim of the study, they shared, was to evaluate the clinical impact of AI software on time to assessment, time to anticoagulation, and patient outcomes at the institution.
Shapiro et al reviewed 150 patients diagnosed with PE between January 2017 and July 2023, retrospectively collecting data on these patients prior to AI implementation and comparing it against those of PE patients following AI implementation.
The researchers looked at scan-to-assessment time, scan-to-alert time—which they noted was used as a surrogate for scan-to-assessment time following AI implementation assuming best practice—time to anticoagulation administration, Pulmonary Embo-
lism Response Team (PERT) activations, and in-hospital mortalities.
Shapiro reported at AVF that scan-to-alert time in the post-AI group of 45 patients was “significantly faster” than scan-to-assessment time in the pre-AI group of 113 pa tients. He added that anticoagulants were administered faster for postAI cases with PERT activation compared to cases without PERT activation, and that in-hospital mortalities decreased from 8.4% (pre-AI) to 2.2% (post-AI), with all mortalities occurring in cases without PERT activation.

bined benefit of AI and PERT activation was highlighted by faster anticoagulation administration and decreased mortality in their sample. “These findings suggest a link between earlier anticoagulation and reduced risk of mortality,” they write.
Speaking to Vascular Specialist ahead of AVF, Shapiro stated that “further research is needed to determine if long-term patient outcomes are impacted by this technology.”
“Adoption of AI into our workflow was associated with faster time to assessment of PE patients,” Shapiro and colleagues concluded. They elaborated that, with an average AI alert time of under six minutes, AI “optimizes standard of care by promoting quicker triage.”
Furthermore, they noted that the com-
“Further research is needed to determine if long-term patient outcomes are impacted by this technology”
JACOB SHAPIRO
On the learning curve with the AI software, Shapiro remarked that it is “very minimal.” He explained: “The interface for reviewing CT [computed tomography] scans is very intuitive, and the chat feature is easy to navigate. The patient’s lab values are also automatically imported and obviously displayed.”
Shapiro commented that over reliance on AI could be a drawback of the technology. However, he emphasized his overall opinion that, as an adjunct to an expert reviewer, there are “no real downsides.” Specifically, he gave the example of the ability to look at scans in views other than axial (i.e. coronal or sagittal) as a benefit for reviewers.
On the wider endorsement of this software, Shapiro noted that it has already been widely adopted by neurosurgeons for strokes and that his institution has been using it for PE for more than 18 months. “We are already seeing it integrated into clinical practice,” he said.
Outgoing president looks at progress made and future direction of American Venous Forum in 2024 turn at the podium
Glenn Jacobowitz, MD, professor of vascular and endovascular surgery at NYU Langone Health in New York City and 2023–24 AVF president, used his turn at the presidential bully pulpit to tackle the future direction of the society—and take a look at where it has come from. By
Brian McHugh and Bryan Kay
Jacobowitz used his outgoing presidential address to outline plans to expand international outreach programs, increase diversity and equity amongst members, and focus on young venous specialists. He also stated that since it has been five years since the previous group retreat where the current AVF five-year plan was outlined, it is time to start looking ahead at what the next five years hold.
Jacobowitz participated in a retreat last year with former AVF President William A. Marston, MD, professor in the Division of Vascular Surgery at the University of North Carolina Hospitals in Chapel Hill, North Carolina, where there was a focus on making sure everyone have access to prevention and treatment options, improving on the current inequalities of venous care, and increasing access to and understanding of venous disease prevention and treatment.
Jacobowitz peered back into AVF history for help determining what its future should look like. “The AVF went through a brief time of financial stress and lower membership,” he told those gathered for the AVF 2024 address. “But our leaders identified a need to redefine our mission goals and align these goals in a way to expand our membership and diversify, and also restructure our management team and our strategic plan.
“We can’t have a myopic view of the world,” Jacobowitz told the audience. The AVF has partnered with 35 interna-

tional societies “to increase collaboration and improve management of venous disease globally, leading to information exchange and joint project proposals, including guideline summaries, collaborative research, and education,” he added.
The AVF now has educational offerings around the world, including early training programs, webinars, and planned symposia in South America, Europe, Egypt and China. There are also international webinars, the first of which was viewed in over 60 countries and had more than 1,000 registrants. The plan is to hold them every three months, Jacobowitz said.
Jacobowitz also mentioned that the AVF recently estab lished around $200,000 in annual grants. Those include the AVF-Jobst Clinical Research Grant ($85,000), AVF-BSCI Translational Research Grant ($85,000), AVF-NIH/ NHLBI Grant ($25,000), AVF Basic Science Research Grant ($15,000), and the AVF Janssen Fellowship ($50,000).
In the new year, there will be “increased fo cus on young venous specialists,” Jacobowitz stated. “We have a record number this year.” He continued by mentioning the importance of advanced practice providers (APP) and the need to engage more with them to “help mitigate the equities of care.”
Jacobowitz issued a call to action on equity of
care. “It’s a complex problem, a large problem, but it involves the disease process … we need to develop programs over hurdles, understanding this and the geographically and economically underserved,” he said.
He concluded by saying the AVF will “lead the way in venous care in the U.S. and abroad through our own initiatives and through collaborative work with our global partners and industry. All the while we’ll maintain focus on research, mentorship, education and advocacy.”

The day prior to the start of the annual gathering, the AVF staged an inaugural “Day of Service,” in which leadership and members headed out into the Tampa area community to promote awareness of venous disease. Organized by the AVF Task Force on Venous Health Inequities and hosted in partnership with the University of South Florida, the AVF aimed to reach out to underserved communities who have little or no access to skilled venous care.
The AVF plans to make the Day of Service an annual event in the cities where the annual meeting takes place.
12 Vascular Specialist | March 2024
VTE
Jacob Shapiro
Glenn Jacobowitz


BRACE YOURSELF...
for an SCVS-Exclusive Data Release

Comparative U.S. Data
Vascular External Support Reduced Intervention Rate and Time to Achieve Two-needle Arteriovenous Fistula
Cannulation in a Multicenter US Study
Dr. Alik Farber, MD, MBA
Interim Chief of Surgery
Chief of Vascular and Endovascular Surgery
Boston Medical Center
Scientific Session V: Dialysis
Monday, 12pm

Scan to learn more about
NEW!
Longer fasting before venography appears to impact stent size selection, new study finds
By Brian McHugh
DURING THE 2024 AMERICAN VENOUS FORUM (AVF) annual meeting in Tampa, Florida (March 3–6), Kurt S. Schultz, MD, a general surgery resident at the Yale University School of Medicine in New Haven, Connecticut, presented findings from a study exploring how fasting duration prior to venography is associated with stent sizing in patients with iliac vein compression, finding that a longer fasting duration was associated with a smaller iliac vein stent size.
He stated that, while iliac vein stenting is a viable treatment option, “inappropriate sizing of venous stents can have catastrophic complications, and there’s been an increased rise in
PULMONARY EMBOLISM
reports of stent migration to the heart and lungs. Iliac vein size, as we know, depends on several factors, like BMI [body mass index] and whether the patient is prone or supine.”
Schultz and colleagues divided patients into two groups— those who received their procedures before 11 a.m. (early group) and those who received their procedures after 11 a.m. (late group).
The number of patients in the study was 64, with 30 being in the early group and 34 in the late group. Of the 64 patients, the mean age was 52 years old and 48 of the 64 were female.
Since these patients are typically fasting starting at midnight the day of their surgeries, “patients who are having elective procedures later in the day are likely to be more dehydrated,” Schultz told the audience.
“So, our hypothesis was patients undergoing iliac vein stenting later in the day would have smaller stents placed compared to those who had stents placed earlier in the day.”
The clinical outcomes supported the hypothesis, with the left common iliac vein and external iliac vein being larger in terms of surface area in the early group when compared with the late group. However, Schultz explained, “this didn’t reach statistical significance.”
The study found that, while delayed start times were associated with a smaller stent size, patients who were prone were also more likely to have a smaller stent size. The dif-
LARGE ADMINISTRATIVE DATABASES ENTER CROSSHAIRS AS COMPARATIVE ANALYSIS SHOWS PERCUTANEOUS MECHANICAL THROMBECTOMY AS SUPERIOR TO CDT FOR ACUTE PE
By Bryan Kay
The pitfalls of large administrative databases came to the fore during the presentation of a propensity-match scoring analysis demonstrating that percutaneous mechanical thrombectomy (MT) was superior to catheter-directed thrombolysis (CDT) in patients diagnosed with acute pulmonary embolism (PE).
Junji Taukagoshi, MD, a vascular surgery resident at the University of Texas Medical Branch (UTMB) at Galveston, Texas, presented the results from the retrospective analysis of patients drawn from the multi-institutional TriNetX network during the 2024 Southern Association for Vascular Surgery (SAVS) annual meeting (Jan. 24–27) in Scottsdale, Arizona.
Taukagoshi and colleagues—including senior author Mitchell Cox, MD, the vascular surgery program director at UTMB— showed that MT was associated with fewer 30-day perioperative complications, improved long-term pulmonary hypertension and right heart failure, and significantly fewer emergency room (ER) visits.
They performed the 1:1 propensity-match analysis with around 1,100 patients in each group who underwent the respective interventions within three days of a PE diagnosis from January 2017 to August 2023.
But the question of whether large administrative databases like TriNetX are equipped to produce the granularity of data can en-
able robust enough analysis quickly emerged when the study came under post-presentation scrutiny, with one questioner suggesting the research team perform a sensitivity analysis to “potentially tease out these patients a little bit more precisely to make sure you don’t have a melting pot of individuals.”
Taukagoshi and Cox both acknowledged this limitation, with the latter describing both its benefits—large size, breadth and ease of use—along with the chief drawback that means “you can only get certain data from it.”
Taukagoshi detailed 30-day results showing comparable mortality and number of blood transfusions. “However, MT was clearly superior when it comes to gastrointestinal bleed and intracranial hemorrhage. It is interesting that it was also superior with both lower rates of myocardial infarction and immediate post-procedural pulmonary hypertension. So, it looks like MT is a clear winner in the acute phase.”
Long term, MT continued to have better outcomes out to five years, Taukagoshi con tinued. “While mortality is not that much differ ent, the incidence of chronic pulmonary hypertension and right heart failure are much improved in patients

ference in fasting times for the two groups was significant, with a mean of eight hours and 45 minutes for the early group and 13 hours and 33 minutes for the late group.
“In conclusion, based on our linear regression we found that a nine-hour fasting duration was associated with an approximately 2mm decrease in stent size,” Schultz stated. “So, the longer fasting duration was associated with smaller iliac vein stent size.”
During the question-and-answer portion of the presentation, Schultz was asked about whether there were any complications in patients due to the size of the stents. He explained that, while he and his team have these data, they have yet to analyze it.
When asked about whether the patients had chronic pain associated with the oversized stents, as there is a larger issue with chronic pain as compared to catastrophic complications such as a stent migration, Schultz responded by saying that his team has the data to look at those complications, adding, “I think that’s an appropriate next step.”
Schultz explained that the study group will now look to develop a pre-procedural hydration protocol.
who had MT. They also had significantly less ER visits.”
Commenting further, he said 30-day data clearly showed MT as associated with “significantly fewer bleeding complications compared to CDT, which can be explained by thrombolytics,” alongside the lower incidence of MI and immediate post-operative pulmonary hypertension.
“Why is that?” he asked. “We would speculate that more rapid clot clearance with MT might result in less myocardial strain and more rapid improvement in pulmonary hemodynamics.”
At five years, MT was also shown to be
“We would speculate that more rapid clot clearance with MT might result in less myocardial strain and more rapid improvement in pulmonary hemodynamics”
JUNJI TAUKAGOSHI
better, Taukagoshi added. “However, the overall incidence of chronic pulmonary hypertension is certainly higher than in previous studies. Clearly, our patient cohort had a high percentage of very significant high-risk PE events.”
So, is MT truly better? Taukagoshi asked, as he pointed to the limitations inherent in large databases. He further revealed that such data had persuaded his institution to shift away from thrombolysis toward MT in the majority of cases where interventions are required for massive or sub-massive PE. “In the future, we would like to see if these results can be replicated with other large multi-institutional series or large datasets.”
Designated discussant Jean Panneton, MD, a professor of surgery at Eastern Virginia Medical School in Norfolk, Virginia, led the queries of the paper. He pointed to a lack of PE risk stratification information. “How do you believe that this may have impacted your results—[with] a propensity match that only matched for regular comorbidities, but nothing specific to the actual PE?”
In light of the administrative database source of the data and attendant Current Procedural Terminology (CPT) codes, Panneton questioned if it was possible to know whether all of the interventions for suction thrombectomy or CDT were indeed “actually done for PE.” “Could they have been possibly done for ischemic legs or for the 43% of patients with acute deep vein thrombosis [DVT] in that database?”
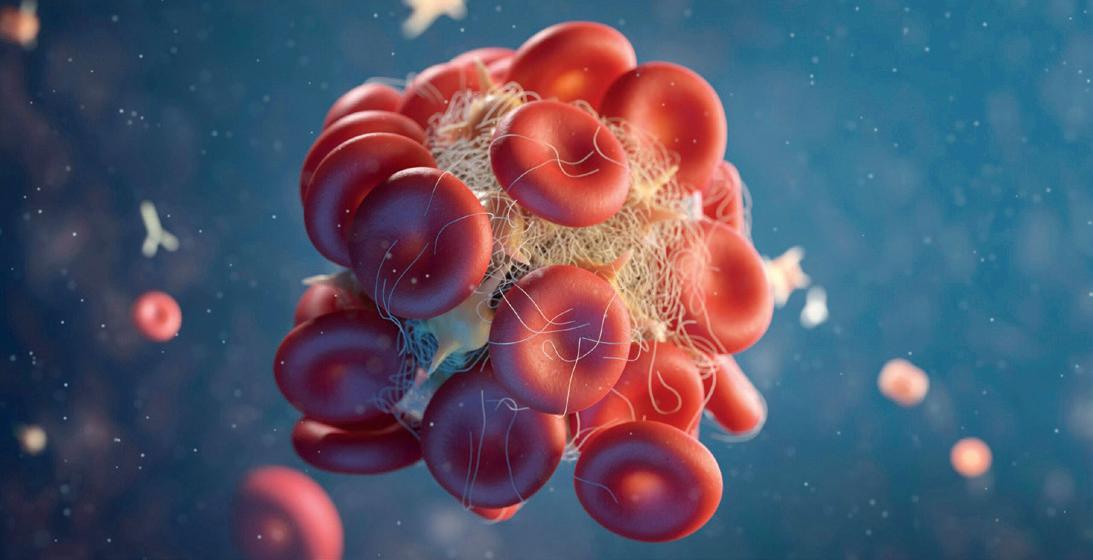
Jason Chin, MD, a vascular surgeon at MedStar Health in Baltimore, Maryland, pointed out the different CDT regimens available and how that might have impacted results. “It doesn’t seem like this database can parse that out. I’m not sure if there is a code for ultrasound-assisted thrombolysis versus no-ultrasound assisted thrombolysis.”
14 Vascular Specialist | March 2024 VENOUS STENTING
Kurt S. Schultz
PE study draws scrutiny on utility of administrative databases
SCIENCE
VRIC 2024 TO HEAR FROM LEADING LIGHT ON ROLE OF IMMUNITY AND INFLAMMATION IN ATHEROSCLEROSIS
By Marlén Gomez
FILIP SWIRSKI, PHD, A LEADING figure in cardiovascular immunology research, will deliver this year’s Alexander W. Clowes Distinguished Lecture at the 2024 Vascular Research InitSiatives Conference (VRIC).
Swirski, currently the director of the Cardiovascular Research Institute at the Icahn School of Medicine at Mount Sinai in New York City, has made groundbreaking discoveries on the role of immunity and inflammation in atherosclerosis.
His latest work, published in Nature, opens avenues for potential therapeutic interventions against Alzheimer’s disease, showcasing the interdisciplinary nature of modern vascular research.
VRIC organizers are gearing up for another round of surgeon-scientist-student com-
VESS 2024
munity engagement aimed at translating basic science more efficiently and effectively to positively impact vascular patients.
The Alexander W. Clowes Distinguished Lecture—named after the late Alexander Clowes, a luminary in vascular research—is a key part of VRIC. The lecture pays tribute to Clowes’ significant contributions and symbolizes the intersecting realms of surgery and science.
This year’s theme, “Immune and Structural Cells in Cardiovascular Disease,” promises to unravel the complex interplay between immunity, inflammation and cardiovascular health.
“We have the most up-to-date research in this area focused on immune cells, structural cells and cardiovascular diseases,” said Katherine Gallagher, MD, chair of the Society for Vascular Surgery (SVS) Basic and Translational Research Committee.
“We’ll be looking at multiple disease processes, including aneurysms, atherosclerosis, intimal hyperplasia, carotid disease and other themes that are relevant to surgeon-scientists and others in the cardiovascular arena.”
“We were looking for an internationally known speaker who has transformed the field of cardiovascular therapy and is very cutting-edge at translating basic science into clinical applications,” said Gallagher. “Our speaker certainly fits the bill for all of
that and has been published in the highest journals available.”
Scheduled to take place on May 15 at the Hilton Chicago, VRIC is held concurrently with the American Heart Association’s Vascular Discovery: From Genes to Medicine Scientific Sessions, held May 15–18 in the same location. The event will provide attendees with an exploration of the latest developments in vascular research.
A translational panel will feature figures such as Kathryn J. Moore, PhD, the Jean and David Blechman professor of cardiology and director of the New York University Cardiovascular Research Center, and Dianna M. Milewicz, MD, PhD, President George H. W. Bush chair of Cardiovascular Medicine, with insights anticipated to elevate the discourse and foster collaborative initiatives.
Gallagher emphasized VRIC’s intimate
“We have the most upto-date research in this area focused on immune cells, structural cells and cardiovascular diseases”
KATHARINE GALLAGHER
Conrad: Determining success in vascular surgery PAD
OUTGOING VASCULAR & ENDOVASCULAR
Surgery Society (VESS) President Mark Conrad, MD, used the 2024 VESS presidential address to illustrate how he got into vascular surgery, what determines success for different generations, what does and does not factor into building a career, and how he would advise those now entering the profession.
“It actually started at Henry Ford Hospital with Alex Shepard,” the chief of vascular surgery at St. Elizabeth’s Medical Center in Brighton, Massachusetts, told those gathered in Sun Valley, Idaho, for VESS’ annual winter meeting (Jan. 18–21). “My first two months as an intern were on vascular; it was the most horrible experience I can ever describe. Every time my pager went off, I got a shot of adrenaline that made me want to throw up, because it meant someone was dying, someone needed to be intubated, someone needed something else.”
their successes for the changes they helped create in the medical world.”
Conrad then looked ahead to the future of medicine, as Generation X doctors slowly give way to millennials. He mentioned how he and other Gen X doctors have tended to try to teach millennials to network the way they had been taught, but found that, “you see there are certain students that take over, they lead it, they pass it on, and it’s just this organic thing that happens. Maybe we need to step back and let the millennials do it their own way,” he told VESS 2024.

Mark Conrad
Shepard wasn’t the only one to have a lasting impact on Conrad and his career. Former VESS President Emerick Szilagyi, MD, the Hungarian vascular pioneerwho also served as SVS president, taught at Henry Ford in Detroit after working as a medical director at a rubber plantation in Brazil for the Ford Motor Company.
Szilagyi’s skepticism of technology around how its advancement could lead to a lack of fulfillment for surgeons in their jobs led Conrad to ponder technology’s role: does it lead to a lack of fulfillment and a lack of success? “It made me question, what determines success? Certainly, most of us think of success by outside factors … I think you’re judged based on your timeline, and I think that’s important,” Conrad stated. “Success based on a person’s timeline is an interesting concept, but it makes sense: we don’t look back at the failures of doctors such as Szilagyi, we look at
Closing, Conrad reflected again on one of those people who got him into vascular surgery—Szilagyi—and called upon his words. “The art of surgery is not yet perfect and advances now unimaginable are still to come. May you have the wisdom to live with them with grace and humanity,” Conrad recited to the crowd. He finished with a quote of his own: “We can’t imagine what’s going to occur in vascular surgery by 2074. As you progress through your career, don’t be derailed by outside influence. Be true to yourself.” Brian McHugh
“We can’t imagine what’s going to occur in vascular surgery by 2074. As you progress through your career, don’t be derailed by outside influence. Be true to yourself”
MARK CONRAD
nature. “Because it is a smaller meeting and a closer-knit group, there’s a lot more collaborations that take place and active discussion that can’t necessarily happen in some of the big meetings” she said.
“People that are there are very focused on this particular theme, making it a breeding ground for partnerships and relationships that extend beyond the conference.”
The early-bird rate for the conference is available until March 18. For more information, visit vascular.org/VRIC24

IVUS USE FOR CLAUDICANTS NOT ASSOCIATED WITH IMPROVED OUTCOMES, CLAIMS DATA SHOW
THE USE OF INTRAVASCULAR ULTRASOUND (IVUS) for the treatment of claudication doubled over a four-year period but there was “no clear relationship between IVUS use and improved patient outcomes,” a recently presented retrospective analysis of claims data showed.
Researchers found the rate of use of the diagnostic tool in peripheral vascular interventions went from 15.5% in 2018 to 29.2% in 2022 among Medicare beneficiaries undergoing index femoropopliteal interventions for claudication.
Use across all procedure types also increased over the time period, with the steepest rate of increase in cases treated using atherectomy.
Looking at site of service, the study showed that IVUS use in hospital settings nearly doubled (4.8% to 8.8%), while in ambulatory surgery centers (ASCs) and office-based labs (OBLs) IVUS was being used in 48.5% of all femoropopliteal interventions performed for claudication by 2022—up from 30.6% in 2018.
The data were delivered during the VESS 2024 winter annual meeting.
Statistical analysis showed that the cumulative incidence of repeat interventions was “significantly greater when IVUS was used during the index femoropopliteal [procedure] than when it was not,” Sanuja Bose, MD, a postdoctoral research fellow in the Division of Vascular Surgery and Endovascular Therapy at Johns Hopkins University in Baltimore, Maryland, told VESS 2024.
“Overall, IVUS was associated with greater conversion to chronic limb-threatening ischemia after adjusting for the baseline patient characteristics and clustering by physician.”
Bryan Kay
15 www.vascularspecialistonline.com
VASCULAR
Filip Swirski
Multi-society PAD Pulse Alliance
aims to highlight importance of patient education
By Marlén Gomez
SOCIETY FOR VASCULAR SURGERY
(SVS) EXPERTS are spearheading initiatives as part of the multispecialty PAD Pulse Alliance and its Get a Pulse on PAD public awareness campaign aimed at educating and raising awareness of the risk factors and potential symptoms of peripheral arterial disease (PAD) among Americans. As the campaign gathers steam, the SVS is focused on closing the health equity gap with the aim of equipping patients with essential tools for early detection and treatment.
The collaborative effort with the Association of Black Cardiologists, Society for Cardiovascular Angiography & Interventions (SCAI) and Society of Interventional Radiology (SIR) has already seen SVS members take a central role as the campaign rolls out.
“This particular disease process, even though it’s an epidemic, is understudied, and the public does not have great awareness about the disease process and unfortunately tend to only find out about it when they’re in dire straits,” said
General Hospital in Boston, one of the spokespeople for the alliance.
“PAD is unique in that it has multiple providers that are involved in caring for these patients. The whole point of the campaign is to show solidarity for our patients and to simultaneously build public awareness about the disease process.”
The Get a Pulse on PAD campaign, launched Feb. 8, includes a survey, media materials, a new website and a comprehensive media strategy to promote disease awareness. Dua has completed dozens of media interviews across TV and radio, with the campaign yielding nearly 200 million impressions across various social media platforms.
Additional SVS members will assist with local market media opportunities in the coming weeks and months. The campaign is the first step in a broader branding campaign to be launched by the SVS in the next few months.
The alliance conducted three distinct surveys, covering the general, Black and Hispanic populations, aiming to gain a nuanced understanding of perceptions of PAD.
The surveys demonstrated that 70% of Americans are unaware of PAD and that there is a disconnect between perceived and actual risk, especially among Black and Hispanic populations.
William Shutze, MD, a vascular surgeon at Texas
“We’re going to have to roll up our sleeves and talk about how to sustain this momentum and keep it going”
WILLIAM SHUTZE
Vascular Associates and one of the initiative’s chairs, expressed his initial astonishment at the survey results, emphasizing the role of raising awareness as the primary step in addressing the severity of PAD.
To maximize the campaign’s impact, initial media efforts were strategically directed toward regions with higher amputation rates. The campaign features not only digital content but also includes video and media interviews in Spanish, aiming to break down cultural and language barriers.
Dua explained how societies can utilize the information provided by the alliance to shape discussions with patients. “In this particular case, the doctors are unable to do their job for patients unless the patients themselves are aware of the disease process,” she said.
“Societies like the SVS that have a lot of power, reach and credibility can do things like this Get a Pulse on PAD awareness campaign where they join forces with other providers to put one message out there that says we care about you, our patients, and this is the way in which we want to provide you with the best care. There’s no point in having all these fancy tools in the hospital if the patient gets to you when it’s too late.”

A reassessment of the campaign is scheduled for October when the societies involved will collaborate to determine the next steps forward. Shutze emphasized the persistent nature of the problem, stating, “It’s not going to go away with one campaign. We’re going to have to roll up our sleeves and talk about how to sustain this momentum and keep it going.”




16 Vascular Specialist | March 2024
AMPUTATION
R E G I S T E R T O D A Y A T The Women’s Vascular Summit is an annual meeting for medical professionals who treat vascular disease in women. It designed to present and discuss what we know and do not know about how vascular disease presents differently in women. M A Y 3 - 4 , 2 0 2 4 | T H E H Y A T T R O S E M O N T 6 3 5 0 N . R I V E R R O A D , R O S E M O N T , I L womensvascular org/registration For sponsorship inquiries please contact: Jennifer Cheetham at jennifer@wellassembled com | 503-545-2662
Anahita Dua
SOCIETY BRIEFS
Compiled by Kristin Spencer, Marlén Gomez and Bryan Kay
SVS invites new compensation study participation, former participants to update information
IN 2023, THE SVS COLLABORATED with Phairify to launch a compensation study to provide vascular surgeons with tailored insights into compensation, practice and productivity data relevant to their specialty and practice in a bid to help them make informed career decisions. The SVS continues to encourage members to complete the survey and is now asking former participants to log back in to update their data for 2024. The compensation study is an SVS member benefit.
Any SVS member willing to participate can engage in a 15-minute survey to unlock enhanced power-searching capabilities with comparative functionality and an expanded career reach that allows access to a new range of opportunities.
At the end of 2023, 22% of SVS members had participated in the survey, which is two percent over the intended goal. Now all members who previously participated are encouraged to update their information to continue providing the most accurate data to those making career changes. “It is only necessary to update the information if anything has changed,” noted Keith Calligaro, MD, a senior author of the study.
To participate and/or update information, visit vascular.org/CompensationStudy2024
GAIN DISCOUNT ON PREMIER VASCULAR REVIEW RESOURCES
THE SOCIETY FOR VASCULAR Surgery (SVS) is encouraging members to prepurchase the sixth edition of the Vascular Education and Self-Assessment Program (VESAP6), a premier digital resource for those preparing for qualifying, certification and recertification examinations. Presales will end on March 26. The presale period provides a 10% discount on the individual license price. Those who participate in the presale will be entered into a lottery to win a complimentary registration for the 2024 Vascular Annual Meeting (VAM 2024) exclusive. This opportunity is open only to SVS members, making membership a valuable investment for those in the field.
VESAP6 is designed to aid professionals in their examination preparation and ongoing education, with more than 600 questions covering more than 10 content areas, and serves as a comprehensive review resource. The product offers up to 102 continuing medical education (CME) credits, with 39.25 eligible for Registered Physician in Vascular Interpretation (re)certification credits. Visit vascular.org/VESAP6

VAM ABSTRACT SUBMISSIONS HIT NEAR-HISTORIC HIGH
A NEARLY RECORD-BREAKING 794 ABSTRACTS WERE SUBMITTED for the SVS 2024 Vascular Annual Meeting (VAM 2024). The abstracts were scored by the VAM Program Committee in early February 2024 and notice letters were sent out later that month. VAM 2024 is taking place June 19–22 in Chicago.
Several types of abstracts can be submitted each year for VAM, such as plenary, “How I Do It,” the Vascular and Endovascular Surgery Society (VESS) session, International Forum and posters. The abstracts are submitted topic areas like aortic, practice management, wound care and more. Once the submission period closes, the Program Committee breaks into small groups when the abstracts are blindly reviewed, given a score and then presented to the full Program Committee. Of the 756 submitted abstracts, 407 were accepted and added to the meeting’s program, which is consistent with the levels in previous years.
“I’m really excited about the diversity of content. This year proved to be one of the most difficult when it came to abstract scoring,” said VAM Program Committee Chair Andres Schanzer, MD. “Every submission was great, but we can’t choose them all. I’m confident that the meeting will have pieces of content that will resonate with vascular surgeons at all career levels.”
VAM 2024 will be the third and final year of Schanzer’s tenure as the chair of the VAM Program Committee. The full VAM 2024 program will be available later this month. To learn more, visit vascular.org/VAM Registration will launch March 20 with an early-bird rate that will be in place through April 10, after which prices will increase to the advance registration rate, which will last through June 17. An increased, on-site registration fee will be available to anyone who cannot register for VAM 2024 in advance.
In addition to the early-bird registration discounted prices, SVS members will see an additional discount on their rates when compared to those of non-members. Any non-member wanting to take advantage of the member discount can apply for SVS membership by May 1 to receive the refunded difference, pending application approval.
To register for the premier educational event in the vascular surgery field, visit vascular.org/ VAM on March 20.
Purchase tickets for SVS Foundation Gala’s ‘Night at the Museum’
TICKET INFORMATION IS available for the SVS Foundation’s “Night at the Museum—A Celebration of Science” Gala during the 2024 Vascular Annual Meeting (VAM 2024) on June 21. Ticket sales are expected to launch in coordination with VAM registration on March 20.
The Gala promises an unforgettable evening filled with elegance, entertainment and philanthropy at Chicago’s world-famous Museum of Science and Industry.
Attendees can choose from various ticket and table options, each offering an array of benefits. The options include: Gold table ($12,000) with $8,500 of the total tax-deductible; silver table
SVS seeks nominations for vice president
THE SVS HAS OPENED THE nomination period for the position of SVS vice president, with the deadline set for March 15. Anyone can nominate/self-nominate for vice president, but only Active and Senior SVS members in good standing are eligible for the position. Following the deadline, the SVS Nominating Committee will review the nominations and select two-to-four candidates to run for office.
Previously, only two candidates were selected to run for open positions on the SVS Board of Directors. During the 2023 bylaws referendum, SVS members approved an increase in the number of candidates to between two and four, allowing members to have a broader choice when casting their votes for SVS leaders.
The Nominating Committee seeks qualified, eligible members from all aspects of gender, sexual orientation, age, ethnicity, geographic location and practice environment as nominees for the open position.
“The change to the number of potential candidates is exciting,” said SVS Nominating Committee Chair Ronald Dalman, MD. “Being the chair of this committee in a year of such monumental change is an honor, and I look forward to seeing which members will be nominated.”
Once the candidates are selected, eligible voting members can cast their votes through an online portal in June, with the results being announced at the SVS Annual Business Meeting on June 22 at the end of the 2024 Vascular Annual Meeting (VAM 2024) in Chicago.
Anyone looking to submit a nomination for themselves or another eligible candidate can visit vascular.org/2024VP.
($8,500), $5,000 tax-deductible; bronze table ($6,500), $3,000 tax-deductible; and individual ticket sales ($600), $250 taxdeductible.
All tickets to the 2024 Gala will include complimentary round-trip transportation from the Marriott Marquis to the Museum of Science and Industry, featuring champagne and non-alcoholic beverages, admission to the Museum of Science and Industry, an open bar, a three-course dinner and snacks, live entertainment and more.
Gala organizers promise this year’s celebration to be a VAM highlight that brings together leaders in the vascular surgery community for a noble cause. For more, visit vascular.org/Gala2024
Ruth Bush takes over as AVF president in Tampa
 Ruth Bush
Ruth Bush
RUTH BUSH, MD, associate dean in the Office of Educational Affairs at John Sealy School of Medicine, the University of Texas Medical Branch (UTMB), in Galveston, Texas, took over as American Venous Forum (AVF) president in Tampa, Florida, at the close of the society’s meeting (March 3–6), succeeding Glenn Jacobowitz, MD.
17 www.vascularspecialistonline.com

CLINICAL&DEVICENEWS
Vascular external support system use found to boost key functional outcomes for surgical arteriovenous fistula creation
By Urmila Kerslake
ALIK FARBER, MD, PROFESSOR OF SURGERY AND radiology at Boston University, is set to present the results of a multicenter U.S. study at the 2024 Society for Clinical Vascular Surgery (SCVS) annual meeting (March 16–20) in Scottsdale, Arizona, that will show creating arteriovenous fistulas with a vascular external support system, VasQ, decreases the median time to achieve two-needle cannulation by reducing the need to perform maturation procedures.
The study set out to assess the functional outcomes of fistulas created with an external vascular support device as compared with rigorously matched controls of unsupported fistulas for end-stage kidney disease (ESKD) patients by the same surgeons.
Farber focuses on the unreliable trajectory of unsupported fistula functional success that surgeons grapple with: “Arteriovenous fistulas (AVF), when they work, are much more durable and much better for patients [than central venous catheters or arteriovenous grafts],” he said. “But to work, they require maturation, which means that the vein that is plugged into the artery needs to grow in diameter and thickness. We are asking the body to do this, but the problem is, this doesn’t work all the time. Sometimes the vein may grow in diameter but not in thickness, or it may not grow
BRIEFS
U.S. study highlights racial and ethnic disparities in the placement of ‘overused’
IVC filters
A nationwide U.S. study, recently published in the Journal of Vascular Surgery: Venous and Lymphatic Disorders (JVS-VL), showed that Black patients had the highest inferior vena cava (IVC) filter placement rate per 100,000 persons compared with White and Latino patients from 2016 to 2019.
“Given the known long-term complications and uncertain benefits of IVC filters, coupled with the 2010 Food and Drug Administration [FDA] safety warning regarding adverse patient events for these devices, proactive measures should be taken to address this disparity among the Black patient population to promote health equity,” authors Jordan J. Juarez, MS, from Lewis Katz School of Medicine at Temple University, Philadelphia, et al remark.
in diameter and simply grow in thickness. So, the corollary to that is many surgically created fistulas do not mature; some fistulas require procedures to help with maturation, and these may or may not be successful.
“In the ideal world, the best thing for the ESKD patient is the creation of a fistula that, after a certain period of time, say six weeks, is usable 100% of the time without any other interventions. That’s the predictable ideal, but doesn’t happen very often. So, anything that improves outcomes to get us closer to that ideal is going to be a very good thing for our patients,” he added bluntly.

Alik Farber
One approach to overcoming this quandary is the concept of external support during surgical fistula creation. The VasQ device is a nitinol-based permanent vascular reinforcement implanted around the artery-vein connection. The device is designed to reduce both hemodynamic and mechanical stress to create more functional fistulas. The device, implanted during the surgical creation of either upper arm or forearm fistulas, guides the remodelling in the juxta-anastomotic region to promote outward wall thickening by maintaining the optimal angle, reducing wall tension and facilitating a more stable, laminar flow profile.
“It appears that externally supporting the fistula and making the fistula take an improved angle has promise in increasing functional patency and decreasing the number of interventions to get to maturation,” Farber told Vascular Specialist
Six U.S. sites that participated in the VasQ U.S. pivotal study and enrolled more than six patients were eligible to participate in a retrospective chart review of unsupported AVFs to compare them to fistulas that had VasQ support. The cohort for this analysis included 104 ESKD patients with 52 in the unsupported group and 52 in the VasQ group. Both groups were well-matched with no significant differences in baseline parameters, including vessel diameter. The researchers evaluated the functional outcomes of time and intervention rate prior to first use, as well as functional success, which was defined as the proportion of fistulas used
FORS-powered LumiGuide 3D imaging technology is rolled out at specialized centers in U.S. and Europe

Philips’ LumiGuide “human GPS” technology— which uses light reflected along an optical fiber inside a guidewire to generate three-dimensional (3D), high-resolution, color images of devices inside a patient’s body in real-time powered by Fiber Optic RealShape (FORS)—is now available to specialized hospitals in Europe and the U.S., the company has announced.
The LumiGuide system enables doctors to navigate through blood vessels during
for hemodialysis at three and six months after AVF creation.
Farber is expected to present the results showing a nearly 30-day reduction in median time to first use driven by a significantly lower need for maturation procedures in the VasQ group as compared to the unsupported cohort. Additionally, significantly more fistulas in the VasQ cohort achieved functional success by the three-month timepoint. The VasQ cohort also showed a trend toward higher functional success rate at six months, but that finding did not reach statistical significance.
“We’re going to present that the immediate days to first use is typically shorter with VasQ fistulas. The ratio of interventions to first use is also significantly less in the VasQ-supported fistulas and the functional success is higher in this group,” commented Farber, adding that the device is relatively easy to place and doesn’t add significant time to the procedure.
Commenting on the results, he said: “The study offers encouraging evidence for the efficacy of an external vascular support of fistulas, especially in lowering intervention rates and shortening the time to achieving functional success.
“I think it’s exciting that there is new clinical science in this space. There’s a huge opportunity that we have with these patients because the maturation rates are currently 50 to 60%, at best. And that’s a pretty small number. So, there’s a considerable need to improve the maturation rates and I applaud Laminate Medical and other companies that are trying to develop ways to address this issue.”
“ We’re going to present that the immediate days to first use is typically shorter with VasQ fistulas”
ALIK FARBER
endovascular procedures using light, instead of X-ray, and was first used to treat patients in late 2023 at Maastricht University Medical Center in Maastricht, The Netherlands, closely followed by the University of Alabama at Birmingham.
Endologix initiates postmarket study of the Detour system
Endologix has announced the initiation of the Percutaneous transmural arterial bypass (PTAB) 1 postmarket study, the beginning of a comprehensive evaluation of the real-world performance of the Detour system in patients undergoing treatment for long complex superficial femoral artery (SFA) disease.
Organization (PSO), a company press release noted.
Frank J. Veith joins ViTAA Medical Solutions’ board of directors
ViTAA Medical Solutions has announced the appointment of vascular pioneer Frank J. Veith, MD, professor of surgery at the Cleveland Clinic Lerner College of Medicine of Case Western Reserve University in Cleveland, Ohio, and New York University Medical Center in New York City, to its board of directors.

The study will leverage the Vascular Quality Initiative (VQI) registry infrastructure developed and supported by the Society for Vascular Surgery (SVS) Patient Safety
ViTAA is developing technology aimed at providing precision, personalized medicine to non-invasively map the strength and weakness of abdominal aortic aneurysms (AAA).
19 www.vascularspecialistonline.com
















 Kevin Mangum
Kevin Mangum




























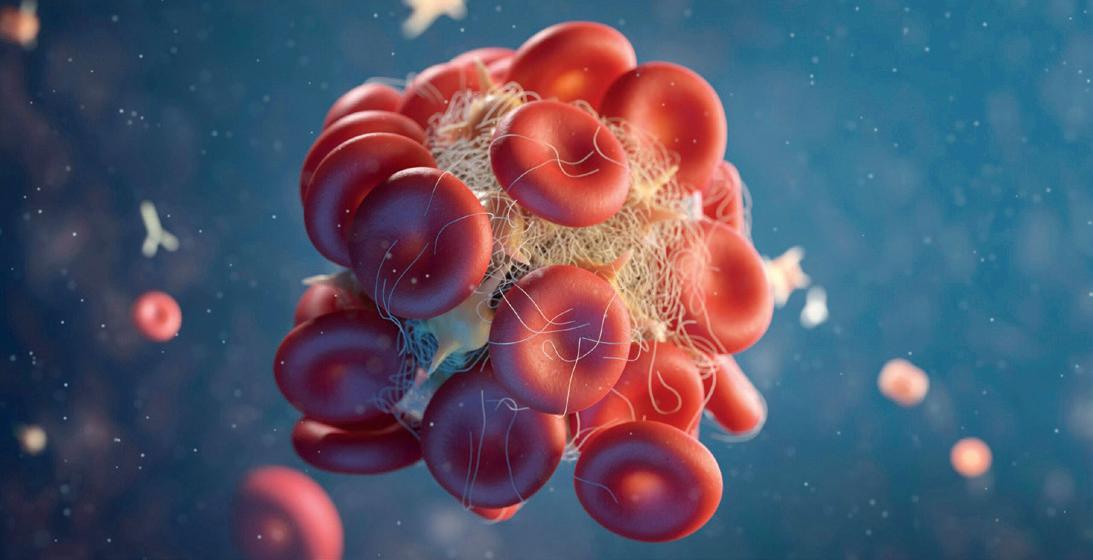








 Ruth Bush
Ruth Bush




