YEARS IN THE MAKING
By Jocelyn HudsonThe pursuit of a cure for deep venous valvular reflux—long considered to be the “holy grail” of deep venous disease—is underway, with new technologies set to address a longstanding unmet clinical need across the globe.


Chronic venous disease affects nearly 25 million in the USA alone, and among those patients, the deep venous reflux population is close to two million people. Erin Murphy, MD, and Marc Glickman, MD, put forward these figures to set the scene for a deep dive into deep venous valvular reflux during a discussion at the 2023 Charing Cross (CX) Symposium in London, England (Apr. 25–27). They were joined by Ramon Varcoe, MBBS, to outline the scale of the issue, as well as potential solutions in the pipeline.
“The population is large, it is being treated most of the time with conservative therapy, so I think there is a large demand—untreated, unmet and underdiagnosed,” said Glickman in summary of the overarching issue. “This is a large unmet need worldwide.”
Moving beyond the US statistics, he stressed that countries such as India, China and Brazil have even larger patient
populations with deep venous reflux.
Varcoe, a vascular surgeon at Prince of Wales Hospital in Sydney, Australia, concurred that deep venous reflux represents an “enormous global burden,” but not only in terms of healthcare costs, but also in patients’ livelihoods. To this point he described the difficulties associated with living with venous ulcers, and the fact that vascular surgeons “really struggle” with these patients in terms of applying compression therapy and using other conservative measures.
Murphy, director of the venous and lymphatic program at Atrium Health’s Sanger Heart & Vascular Institute in Charlotte, North Carolina, noted that there has been “considerable progress” over the last 10 years in treatment options for patients with reflux in the superficial system, and also in the deep venous obstruction space, with various new stents now available. “Why do you think it is taking so long to establish new
technology in the deep venous valve realm?” she posed to the panel.

“For the last 50 to 60 years, everyone has considered finding a cure for deep venous valvular reflux as the holy grail of deep venous disease,” remarked Glickman, highlighting the importance of, and difficulty associated with finding a solution to, the problem. He put forward two issues at play here—one is
The UIP 2023 World Congress in Miami Beach, Florida (Sept. 17–21) will bring professionals from different countries and regions to share knowledge, exchange ideas, and discuss the latest advances in venous and lymphatic medicine. However, the language barrier can often be a significant obstacle for non-native English speakers to engage effectively. To address this challenge, the American Vein & Lymphatic Society and co-hosts [the American Venous Forum, the Canadian Society of Phlebology, and the Mexican Academy of Phlebology and Lymphology] have decided to use an artificial intelligence (AI) technology called Wordly to provide translation services.
WORDLY IS AN AI-POWERED translation service that can translate speech in real-time in over 25 languages. Attendees can listen to audio translations or read written translations, which are accessible by QR code.
One of the key benefits of using Wordly is that it provides a seamless attendee experience. Attendees can use their smartphones or other devices to access the translation service; nothing needs to be downloaded or installed in advance. Moreover, free WiFi will be provided in session rooms, ensuring attendees can access the translations without incurring additional costs.

All educational sessions will offer translations, making it easier for attendees to follow the presentations and engage in discussions. To use the translation services, attendees must bring a WiFi-enabled mobile device or laptop and headphones. Once they have selected their language, they can listen to audio translations or read written translations in real time.
Virtual attendees will also be able to access the translation services
Continued on page 2
Continued on page 2
Continued on page 4
“I am seeing huge interest in venous disease now and it is a really great time to be involved in the field.”—
RAMON VARCOEDEEP VENOUS VALVES
60 years in the making
the challenging nature of correctly diagnosing of deep venous valvular insufficiency and the other, a lack of standardisation in making that diagnosis, resulting in the severity of the disease being “missed throughout the medical community”. Varcoe also stressed the “huge variability” in how this disease is diagnosed, and mentioned another issue, that surgery in these patients is “next to impossible” due to challenging anatomical conditions.
Glickman noted another challenge in the fact that vascular surgery training tends to focus on arterial disease and less on the venous world, resulting in only “very minor” innovation in the latter.
New technologies “on the horizon”
Glickman expressed his belief that the potential for growth in the deep venous valve market is “enormous”, moving the focus of the conversation towards two new technologies that could improve patient outcomes in this challenging space. On this note, Varcoe expressed his excitement that there are some new technologies “on the horizon” that “might make a huge difference to patients’ lives”.
Glickman is the senior vice president and chief medical officer at Envveno Medical, the company behind the VenoValve, and shared that his training as a vascular surgeon informed him that “most of our endovascular procedures have started out as open procedures that have worked and that have migrated to endovascular,” citing the examples of carotid stenting, ablation and stripping, and the treatment of abdominal aortic aneurysms. In the deep venous reflux space, however, he noted that an open surgical technique is missing.
About seven years ago, Glickman recalled, the VenoValve was developed. He detailed that it is made from a porcine aortic monocusp on a stainless steel frame that is surgically implanted into the femoral vein in the mid-thigh
region. The procedure takes about an hour and 15 minutes.
Glickman noted that three-year data from a first-in-human trial conducted in Colombia, which were recently shared at the 2023 American Venous Forum, showed improvement in reflux time, improvement and consistency of the Venous Clinical Severity Score (VCSS), and a reduction in pain. The team are presently conducting another trial— SAVVE—at 24 sites in the U.S.
He highlighted that the company is now working on a transcatheter version of their VenoValve device, with the plan being to commence a first-inhuman study.
Varcoe, who has been involved in clinical studies on the BlueLeaf (InterVene), shared that this novel device is “completely different” to the VenoValve. “What we do with this device is we make a valve leaflet from the blood vessel wall itself—so we leave nothing behind, we are not transplanting anything, we are literally creating a flap-like valve, which can be either monocuspid or bicuspid and it can be done multiple times in the same vein segment,” he explained. The device is percutaneous, Varcoe added, and is therefore inserted over a guidewire, with the procedure guided by both intravascular ultrasound and fluoroscopy. “It takes around an hour and a half or so to make a series of valves and we hope that over time those valve cusps endothelialise and become part of the native structure of the vein wall,” he said.
In terms of data, Varcoe noted that 41 patients have now been enrolled in a global clinical trial of the technology. The data demonstrate the safety and efficacy of the device in its early stages, Varcoe reported, and that the procedure can be done without creating deep vein thromboses, which was an “initial fear”. He added that the data have shown some “dramatic, remarkable improvement” in VCSS scores. “Patients I have seen who have had ulcers for 20 years have had them healed within six weeks, and that is extremely satisfying,” he shared.
In addition to VenoValve and BlueLeaf, Cook Medical announced
earlier this summer that the first patient has been treated in a clinical study to evaluate a new venous valve designed for treating chronic venous insufficiency (CVI). The patient was treated by principal investigator Mauricio Alviar, MD (Barranquilla, Colombia).
The valve’s safety and efficacy are now being tested in a global, multisite clinical trial. The global principal investigator of the study is Paul Gagne, MD (Darien, Connecticut). “When leg veins function poorly, patients suffer with leg swelling, leg pain, leg ulcers, disability, and possible amputation. Therefore, it is important to restore blood flow out of the leg veins, back to the heart. Part of doing this successfully required restoring the function of the venous valves,” Gagne said in a press release at the time.
What’s next?
While these technologies are in their infancy, both Glickman and Varcoe are cautiously optimistic about the future. Glickman noted that the focus at Envveno Medical will be finishing up the trial for Food and Drug Administration (FDA) approval by the end of this year, after which it will take six months to get the approval. The plan is to conduct a large trial in the U.S. He summarised that the percutaneous device is probably five years out, and VenoValve “probably two years out from being in people’s hands”.
Jorge Ulloa, MD (Bogota, Colombia), one of the key figures behind research of the surgical VenoValve, told Venous News the future looks bright in the venous valve space following 65 years of development. “So far, we are at the pivotal phase of the study [of the surgical version of the valve],” he says, relating how more than 50 cases have now been performed in the U.S. so far. This follows the first-in-human trial carried out at Ulloa’s institution in Bogota. The surgical valve “seems to have a promising future, due to the length and results from the follow-up, that we have presented extensively in the last three years,” the Fundacion Santa Fe-Universidad de los Andes vascular surgeon continues. “There
Publisher: Roger Greenhalgh | Content Director: Urmila Kerslake | Head of Global News: Sean Langer
Editor: Jocelyn Hudson Jocelyn@bibamedical.com | Editorial contribution: Bryan Kay, Éva Malpass, Will Date and Marni Davimes
Design: Terry Hawes and Wes Mitchell
Advertising: Alexis Campbell alexis@bibamedical.com
Subscriptions: subscriptions@bibamedical.com
is another player from Cook Medical, which has already implanted a first device via endovascular deployment, and we are on the way to migrating to [an endovascular device] also.”
Ulloa is similarly involved in the firstin-human trial of the endovascularly delivered version of the valve. In the meantime, continuing study of the surgical valve is showing “a plateau in terms of stabilization in pain, VCSS and reflux time,” he says. “It means that there is no tendency to return to baseline at 36 months of follow-up. That is something that has never happened in previous series, and everything looks like it will continue this way. Of course, only time and follow-up of these cases will show us the path to continue.”
Ulloa believes more new technology will emerge in the venous valve space in the coming years. “I envision a myriad of new devices that will emulate our experience,” he says. “Some will work, some won’t.

So far, there are more than four major companies designing their own concepts, and they will have to run through all the necessary stages in order to prove that they are safe and functional. All of these efforts will only benefit PTS [post-thrombotic syndrome] patients—and that is a good thing.”
Regarding BlueLeaf, Varcoe stated that the team involved is “in a process of innovating and iterating the device”. They are about to launch the fourth generation of the device, which allows for the treatment of larger veins and the creation of more circumferential valve cusps. He added that they are going through the pre-submission process with the FDA about what an investigational device exemption trial might look like, which they hope to be able to start within months. “I see a future where this technology is successful,” he averred, “whichever deep valve technologies do end up being available to us.”
There will undoubtedly be challenges along the way, however. Glickman acknowledged that paradigm shifts in medicine “take time,” emphasising the complexity of the regulatory landscape.
“I have just really enjoyed seeing the focus be put back on venous disease,” Varcoe said in closing. “I am seeing huge interest in venous disease now and it is a really great time to be involved in the field.”








Erasing language barriers at the UIP 2023 World Congress
Continued from page 1
for the live stream. Any attendees who cannot attend in person can still benefit from the translation services and participate in the event remotely.
In addition, Wordly offers a simultaneously written transcription in any of the 25 available languages, including English, for deaf or hard-ofhearing attendees. The goal is for as many attendees as possible to engage with the scientific content presented in Miami Beach.

By offering translation services, the UIP 2023 World Congress organisers are demonstrating their commitment to inclusivity and their recognition of the importance of breaking down language barriers to facilitate effective communication and engagement.
Using AI technology like Wordly represents
a significant advancement for medical conferences. Previous translation services relied on a person listening and translating sessions, which was costly and limited the number of languages the Congress offered. AI translation is an ideal solution for large-scale events like the UIP 2023 World Congress, where multiple languages are in attendance, and a high volume of content will be translated.
The UIP 2023 World Congress chose to use AI technology to provide translation services for attendees because it offers a fast and accurate way to communicate across language barriers. By providing real-time translation services of educational sessions, Wordly can help break down language barriers, ensuring
all attendees can better participate in the conference.
At the UIP 2023 World Congress, up to six scientific sessions will run concurrently throughout the day discussing scientific abstracts, superficial and deep venous disease, lymphedema and lipedema, ultrasound and venous imaging, venous nursing, and more. Learn about the UIP 2023 World Congress and venous and lymphatic medicine at www.uip2023.org.
This article was provided by the American Vein & Lymphatic Society.

Study finds similar rates of VTE in both flying and non-flying surgical patients
Uncertainty underlying the magnitude of risk posed by long distance air travel in venous thromboembolism (VTE) patients has created the need for a deeper, systematic dive into the guidelines and resources providers should be turning to when managing their pre-flight VTE patients.

JESSIE SHEA, MD, OF IMPERIAL COLLEGE


London in London, England, took to the stage at the recent European Venous Forum (EVF) in Berlin, Germany (Jun. 22–24) to deliver the findings of a recent systematic review and meta-analysis of VTE risk in surgical patients with recent air travel.
“A number of studies have shown a positive correlation between VTE risk and long-haul air travel, with incidence rates of up to 5% in patients with concurrent risk factors and an estimated 10–30% of patients with VTE dying within 30 days of incidence,” Shea detailed. With surgical tourism on the rise, Shea explained that patients opting to endure long-distance flights to seek surgical intervention could be lacking the resources necessary to guide safe air travel. In 2017 alone, there were an estimated 1.4 million US medical tourists, creating a significant need for perioperative travel guidelines to inform patients of potential risk.
To address the potential risk, Shea et al‘s systematic review and meta-analysis was designed by pulling all
available literature about VTE risk in surgery when flying versus surgery at home. To conduct the analysis, the study design collected reporting of incidence of VTE in patients undergoing surgical intervention who had recently engaged in air travel versus those who had not.
Shea detailed that limiting factors for the study included risk of detection or recall basis, heterogeneity in thromboprophylaxis applied, and variation in flight characteristics and duration.
The presenter concluded that the study found similar rates of VTE in both flying and non-flying surgical patients maintained across subgroup analysis of both preoperative and postoperative air travel, air travel greater than four hours in length and surgery associated with high VTE risk.
“The most important thing is to use a full risk assessment to identify each individual patient’s risk and also take into account the length of surgery,” she said in her closing remarks. “Looking at our study, it would suggest that there is no increase for VTE, but obviously our conclusion is limited by the quality of the evidence.”
n VENOUS THROMBOEMBOLISM:
A study of two risk assessment models (RAMs) for predicting the bleeding risk in patients considered for pharmacologic prophylaxis to prevent venous thromboembolism (VTE) has found that though an increasing risk score correlated with higher bleeding rates, both models had a low predictive ability for major bleeding post-admission. This was the conclusion of Hilary Hayssen, MD, of the University of Maryland School of Medicine in Baltimore, Maryland, who presented the findings of the analysis of more than 1.2 million patients undergoing both surgical and non-surgical interventions at this year’s Society for Vascular Surgery (SVS) Vascular Annual Meeting (VAM) in National Harbor, Maryland (June 14–17).
For more on this story go to page 8.
n ABLATION:
Five-year results of the LAMA randomised controlled trial (RCT) show that both mechanochemical ablation (MOCA) and modern endovenous laser ablation (EVLA) technology are associated with low procedural and postprocedural pain, while clinical outcomes in the short and medium term are worse for MOCA. This led senior author Daniel Carradice, MD, of Hull York Medical School in Hull, England, to conclude that MOCA “may have a role in a small number of selected patients such as those with a fear of needles”.
For more on this story go to page 12.
n SIR POSITION STATEMENT: The Society of Interventional Radiology (SIR) has published a position statement offering recommendations on the management of chronic iliofemoral venous obstruction with endovascular placement of metallic stents.



The statement, published online in the Journal of Vascular and Interventional Radiology, is a companion to the 2022 statement on the treatment of acute iliofemoral deep vein thrombosis.
For more on this story go to page 15.
IN BRIEF THE LATEST STORIES FROM THE VENOUS WORLD
“[Mechanochemical ablation] may have a role in a small number of selected patients.”
“The goal is for as many attendees as possible to engage with the scientific content presented in Miami Beach.”UIP 2023 Congress president Kathleen Gibson The latest advances in venous and lymphatic medicine will be discussed at UIP 2023 in Miami Beach, Florida (Sept. 17–21).
Welcome to the relaunched, rebranded print edition of Venous News. From September 2023, this dedicated news source for venous specialists is back in print with a fresh new look, providing a digest of key developments in the space. The paper, which reaches endovenous and phlebology specialists all over the world with the latest news, opinion editorials, and profiles, is due to restart its publication schedule of five times per year, and will once again be distributed across the U.S. and Europe. The publication schedule has been designed to coincide with key conferences on the venous calendar. In the year ahead, these include:
● International Union of Phlebology (UIP) 2023 World Congress in Miami Beach, Florida (Sept. 17–21)
● The VEINS (Venous Endovascular Interventional Strategies) 2023 (Oct. 29–30) and Vascular Interventional Advances (VIVA) 2023 in Las Vegas, Nevada (Oct. 30–Nov. 2)
● American Venous Forum (AVF) 2024 in Tampa, Florida (Mar. 3–6)
● Charing Cross (CX) Symposium 2024 in London, England (Apr. 23–25)
● International Vein Congress (IVC) 2024 in Miami Beach, Florida (Apr. 27–29)
Study finds no correlation between IVC filter placement position and device complications
Researchers report that inferior vena cava (IVC) filter placement position relative to the level of the most inferior renal vein was not associated with differences in IVC thrombosis in a recent singlecentre cohort study.
ADDITIONAL KEY FINDINGS FROM THE study include a low incidence of other filter-related complications, including migration, fracture, and caval wall penetration, and no occurrence of device-related mortality. These conclusions were recently shared online in the Journal of Vascular Surgery: Venous and Lymphatic Disorders (JVS-VL).
Authors Scott Grubman, BS, of Yale University School of Medicine in New Haven, Connecticut, and colleagues write that indwelling IVC filters can cause complications, including penetration into surrounding structures, migration, and thrombosis of the vena cava. They add that, while computational fluid dynamics suggest juxtarenal placement of IVC filters decreases the risk of thrombosis, this has not been explored clinically.
Against this background, Grubman et al communicate that it was their aim in the present study to examine the effect of filter placement position on long-term device complications with an emphasis on IVC thrombosis. “We hypothesised that IVC filters placed further caudal to the renal veins were more likely to develop long-term thrombosis,” they write.
Venous News aims to cover all areas of the venous space, including the superficial and deep veins, as well as the lymphatic system.
In the September 2023 issue, readers can expect meeting highlights from the first half of 2023—including from CX Symposium, IVC, the European Venous Forum (EVF) and more. Topics covered include thrombectomy updates—notably the latest insights from mechanical thrombectomy trial data—results of the LAMA trial on ablation options, and a risk assessment model for predicting bleeding in patients considered for venous thromboembolism (VTE) pharmacological prophylaxis. In addition, the issue features journal highlights on topics ranging from the effect of inferior vena cava (IVC) filter placement on device complications to venous stenting during pregnancy.

The issue also features interviews with experts in the field, including a profile on Erin Murphy, MD, as well as insights on saphenous vein ablation options with Raghu Kolluri, MD, and on pelvic venous incompetence with Aleksandra JaworuckaKaczorowska, MD. Readers can also expect an opinion piece on the role of vascular surgeons in pulmonary embolism response teams (PERTs) from Nicolas Mouawad, MD. Key industry updates also feature.
In order to investigate their hypothesis, the researchers document that they conducted a retrospective review of the medical records of patients receiving IVC filters at a single tertiary centre between 2008 and 2016. They note that they excluded patients missing follow-up or procedural imaging data.
“The placement procedure venograms were reviewed, and the distance from the filter apex to the more inferior renal vein was measured using reported IVC filter lengths for calibration,” Grubman and colleagues detail in JVS-VL, sharing their study methods. They add that they patients were divided into three groups according to the tip position relative to the more inferior renal vein: group A (at or superior), group B (1–20mm inferior), and group C (>20mm inferior). The researchers then compared patient and procedural characteristics and outcomes between the three groups, with the primary endpoints being IVC thrombosis and device-related mortality.
Grubman et al state in the results section of their paper that, of the 1,497 eligible patients, 267 (17.8%) were excluded from the present study. They write that the most common placement position was group B (64%), and that the mean age was lowest in group C (59.5 years), followed by groups A (64.6 years) and B (62.6 years), with a p-value of 0.003. The team convey that no statistically significant differences were found in the distribution of sex or the measured
The American Vein and Lymphatic Society (AVLS) with the AVF, the Canadian Society of Phlebology, and the Mexican Academy of Phlebology and Lymphology will welcome the venous community at the 2023 International Union of Phlebology (UIP) World Congress and 37th Annual Congress (Sept. 17–21) in Miami Beach, Florida. Pick up a print copy of Venous News at the meeting, and stay tuned for extensive coverage of this global venous congress in our upcoming October issue.
For information on how to subscribe, visit venousnews.com.
comorbidities. The authors continue that group C was the most likely to receive jugular access (group C, 71.7%; group A, 48.3%; group B, 62.4%; p<0.001) and received more first-generation filters (group C, 58.5%; group A, 46.6%l group B, 52.5%; p=0.045).
Sharing their key findings from the study, Grubman and colleagues report: “The short-term (<30-day) and long-term (≥30-day) outcomes, including access site hematoma, deep vein thrombosis, and pulmonary embolism, were uncommon, with no differences between the groups.” They add that cases of symptomatic filter penetration, migration, and fracture were rare (one, one, and three cases, respectively).
The authors further highlight that, although a pattern of increasing thrombosis with more inferior placement was found, the difference between groups was not statistically significant (group A, 1.5%; group B, 1.8%; group C, 2.5%; p=0.638). Grubman et al also relay that no cases of device-related mortality occurred, and that all-cause mortality after a mean follow-up of 2.6±2.3 years was 41.3% and did not vary significantly between the groups (p=0.051). Finally, the authors state that multivariate logistic regression revealed that placement position did not predict for short- or longterm deep vein thrombosis, pulmonary embolism, IVC thrombosis, or all-cause mortality after adjustment for the baseline patient characteristics.
In their conclusion, Grubman and colleagues summarise: “IVC filters have low rates of short- and long-term complications, including IVC thrombosis. The placement position did not affect the occurrence of device complications in this study.”
The authors acknowledge some limitations of their study, including those “common to a retrospective medical record review”, such as inconsistent information entry into the medical records, missing or incomplete records or procedural imaging studies, potential bias from loss to follow-up, and the potential for uncaptured, non-randomised confounding variables.
“Larger studies would be helpful to further elucidate the relationship between filter position and the occurrence of rare adverse events.”
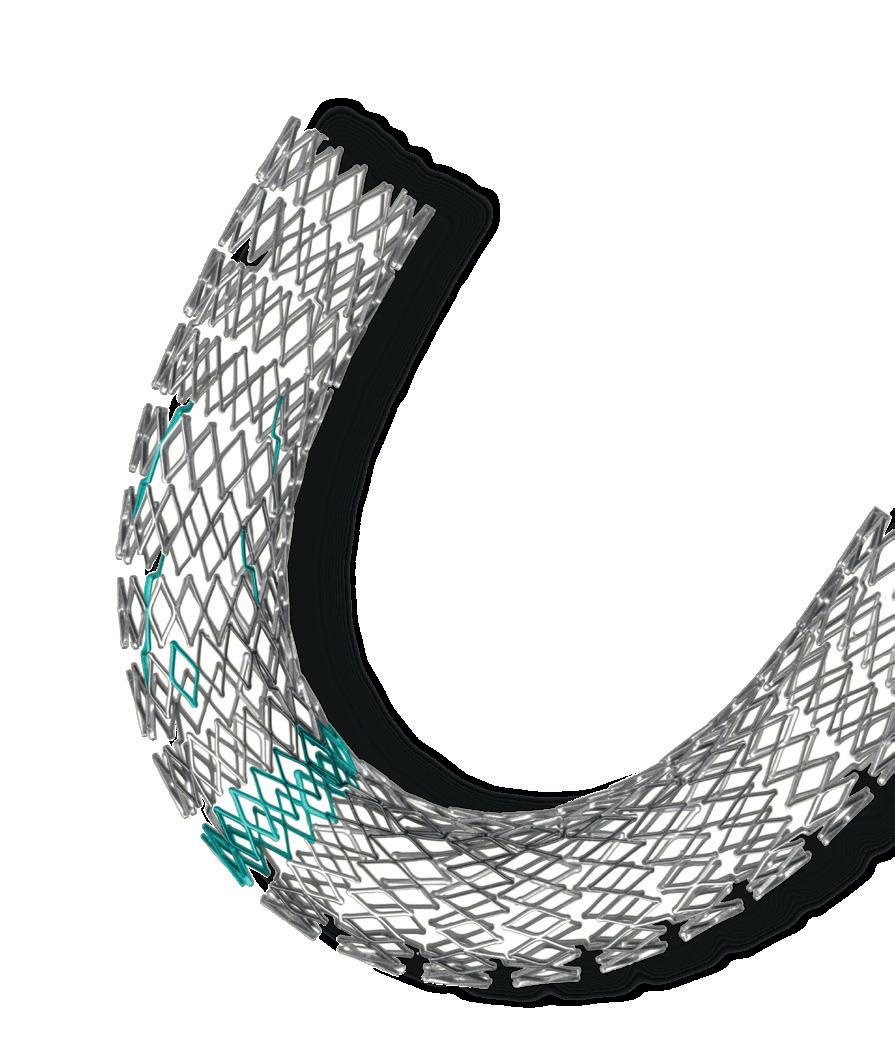
FLAME, FLASH and ongoing PEERLESS trials collect ‘compelling’ data for FlowTriever device
Speaking on the FLAME, FLASH and PEERLESS trials that each collected data on the FlowTriever (Inari Medical) device for the treatment of pulmonary embolism (PE), Ripal Gandhi, MD, of the Miami Cardiac & Vascular Institute & Miami Cancer Institute in Miami, Florida, elaborated on the presiding safety and efficacy that is consistent throughout the research, and how these studies may shape future guidelines to better standardise the PE care pathway for physicians and patients.
IN CONVERSATION WITH VENOUS NEWS about a presentation he gave at the 2023 International Vein Conference (IVC) in Miami, Florida (Apr. 27–29), Gandhi noted that the FLAME trial—which he described as the largest interventional trial done in high-risk PE patients—was intended to enroll more participants but was concluded early after meeting the prespecified interim analysis criterion.
Principal investigator for the FLAME trial James Horowitz, MD, of NYU Grossman School of Medicine in New York City, and his team found that large-bore mechanical thrombectomy with the FlowTriever system in patients with high-risk PE was associated with a significantly lower occurrence of meaningful in-hospital adverse clinical outcomes compared to other contemporary treatments. In the FlowTriever
JETi registry provides ‘remarkable results’ for peripheral thrombectomy system

Presenting “remarkable results” from the JETi registry—a prospective, multicentre, observational study which collected real-world data on the safety, performance and clinical benefits of the Jeti peripheral thrombectomy system (Abbott)—speaker Mahmood K Razavi, MD, of Children’s Health of Orange County in Orange, California, relayed the positive outcomes seen with the “powerful” Jeti device to audience members at IVC 2023.
OF THEIR MAIN OBJECTIVES, the research team set about analysing Jeti outcomes in patients with deep venous thrombosis (DVT), to ultimately determine if iliocaval and iliofemoral DVT in a single session is feasible.
Speaking to Venous News, Razavi explained that “Jeti was one of the earlier devices that came into market that had the capability for single-session treatment of patients—so this was the

arm, a mortality rate of 1.9% was recorded, compared to 29.5% in the context arm.
“It had to be [concluded prematurely]—the study was stopped at 50 patients because the results were so compelling. With the 17% endpoint in the FlowTriever arm versus 63.9% in the context arm, this was lower than the performance goal of 32%—much lower”, said Gandhi, commenting on FLAME’s results.
Turning his attention to the FLASH registry—the “largest interventional study ever done in PE”— Gandhi explained how the analysis drew from an 800-patient, prospective, multicentre, real-world registry. Led by Caitlin Toma, MD, of the University of Pittsburgh School of Medicine in Pittsburgh, Pennsylvania, the researchers’ main objective was to assess the safety and effectiveness of large-bore thrombectomy in an all-comer patient population through to six months.
Their primary endpoint was defined as any composite of major adverse events (MAE) within 48 hours. Their results showed a 1.8% MAE rate, with no device-related deaths. “This was quite remarkable,” Gandhi opined. “However, one of the most important things to look at is all-cause mortality at 30 days in this patient population, which was only 0.8%.”
“[In the FLASH registry] most of the patients did not require an intensive care unit day—as an interventionist the thing that is most gratifying when treating a patient who is very sick is seeing immediate changes in their hemodynamic parameters on the table,” Gandhi described. “In treating patients with large-bore thrombectomy, we see immediate changes in pulmonary artery pressures, improvement in their cardiac index and heart rate, and to see that in real-time is quite remarkable. It is extremely valuable.”
Briefly sketching out the intent for the currently ongoing PEERLESS trial, led by Wissam Jaber, MD,
basis of our intention-to-treat analysis, to evaluate the effectiveness, outcomes and feasibility of the device for this purpose”.
Treating 53 limbs in 47 patients, Razavi stated that around a fifth—21%—had symptoms for longer than 14 days, placing them in the sub-acute category. Their primary efficacy endpoint was acute procedural success defined as the establishment of unobstructed flow from the limb in a single session. Another “critical” secondary endpoint Razavi highlighted was the evaluation of hemoglobinuria due to the Jeti’s differing mechanism of action in comparison to other devices such as the AngioJet (Boston Scientific) device. “People often confuse the [Jeti] mechanism of action with Angiojet. They are different. Jeti can be described as a hydrodynamic thrombectomy device, although this is not a commonly used term,” Razavi explained.
The Jeti system is designed to deliver a stream of high-pressure saline via a pump to the distal tip of the catheter, while aspirating thrombotic material. The saline jet acts to macerate the clot inside the catheter and prevent clogging. Hence, no intravascular clot maceration and no hemoglobinuria.
Razavi, describing their findings, stated that re-establishment of
of Emory University in Atlanta, Georgia, and Carin Gonsalves, MD, of Thomas Jefferson University in Philadelphia, Pennsylvania, Gandhi averred that it is the “first and only” head-to-head randomised clinical trial comparing large-bore thrombectomy— via the FlowTriever system—with catheter-directed thrombolysis in PE patients.
“We happen to be one of the enrolling sites,” Gandhi said. “[PEERLESS] is one of several randomised clinical trials that are being done in this space right now and this is an important one. However, we definitely need more research.”
Amongst the research emerging for the treatment of PE, Gandhi makes clear that better standardised care pathways are the “goal”, although it will not “happen overnight”.
unobstructed flow after a single session was seen in 89% of patients with Jeti alone at a mean procedure time of 90 minutes. Overall, complete flow was reestablished in 94% after Jeti combined with stenting. Iliocaval thrombosis was present in 12 patients included in this cohort, their clot extending into the inferior vena cava (IVC). Furthermore, in nine of these 12 the researchers found the clot to be behind an IVC filter—“this meant that the entire infrarenal IVC was thrombosed and yet we achieved these kind of results—it was somewhat surprising to us.” Breaking their results down further, Razavi stated that in these patients prior to stenting, flow restoration with Jeti alone was seen in 86% of patients with a clotted IVC (100% after stenting), 75% in iliofemoral (92% after stenting) and 100% of the isolated femoropopliteal patients, respectively.
“This is a very different aspiration system, [Jeti] was far more efficacious
than we anticipated,” Razavi opined.
Although their team did not evaluate long-term clinical outcomes, they did assess 30-day Jeti-related efficacy via ultrasound, a measure which Razavi averred has been correlated with longterm patency and the development of post-thrombotic syndrome, as seen in the ATTRACT trial. Referring to the rate of clot absence during ultrasound follow-up, in the common femoral it was 87.2%, and in the femoral vein, 71.7%.
“Not only was this a highly effective treatment in 90 minutes, but the midterm outcomes were also fairly good and comparable to other studies such as the ClotTriever (Inari Medical) outcomes [CLOUT] registry” Razavi continued.
“At the time this system became available there were multiple studies that had been published and none could consistently achieve singlesession thrombectomy in patients with iliofemoral DVT, let alone iliocaval,” said Razavi. “We had made the observation that this is a very efficacious system—but can we successfully treat DVT in a single session? Is Jeti a superior system as compared to devices that were used before? It would be a game-changer if we could treat iliocaval and iliofemoral DVT in a single session with mid-term patency rates similar to thrombolysis.”
Razavi hopes that the team’s experiences throughout this trial will help European and U.S. practitioners alike choose “more carefully as to what works and what does not”.
“This is a very different aspiration system, [Jeti] was far more efficacious than we anticipated.”
“[PEERLESS] is one of several randomised clinical trials that are being done in this space right now and this is an important one. However, we definitely need more research.”Abbotts’s Jeti thrombectomy system







Risk assessment models ‘no better than coin toss’ for predicting bleeding in patients considered for VTE pharmacologic prophylaxis
A study of two risk assessment models (RAMs) for predicting the bleeding risk in patients considered for pharmacologic prophylaxis to prevent venous thromboembolism (VTE) has found that, though an increasing risk score correlated with higher bleeding rates, both models had a low predictive ability for major bleeding post-admission.

THIS WAS THE CONCLUSION OF HILARY Hayssen, MD, of the University of Maryland School of Medicine in Baltimore, Maryland, who presented the findings of the analysis of more than 1.2 million patients undergoing both surgical and non-surgical interventions at the 2023 Society for Vascular Surgery’s Vascular Annual Meeting (VAM) in National Harbor, Maryland (June 14–17). Pharmacologic prophylaxis reduces the incidence of pulmonary embolism (PE) but can cause bleeding, meaning that there is a need to balance the risk of VTE against the risk of bleeding when considering this avenue of treatment, Hayssen told delegates. There are two current risk assessment models to evaluate bleeding risk in those being considered for pharmacologic prophylaxis, the IMPROVE and Consensus models. Hayssen and colleagues assessed
the predictive ability of each model for bleeding within 30, 60 and 90 days post-admission, comparing the performance of the two models in patients admitted at all 1,298 Veterans Health Administration (VHA) facilities nationwide between January 2016 and December 2021.
In total, data were analysed from 1,228,448 patients, 26.5% (n=324,959) of whom underwent surgical procedures, and 73.5% (n=903,489) nonsurgical interventions. To review the two scores, researchers calculated the IMPROVE and Consensus scores using medical record data, which enabled them to assess the predictive ability of the models for bleeding at 90 days in both surgical and non-surgical patients.
A total of 5.6% of patients had major bleeding, as defined by the International Society on Thrombosis and Hemostasis (ISTH), within 90 days postadmission, occurring in 5% of the surgical patients, and 5.8% of non-surgical patients. A total of 68,372 bleeding events occurred within 90 days of admission, and 29% of events occurred between 31 and 90 days, Hayssen reported.
In terms of the performance of the two models, Hayssen reported that higher scores were associated with higher bleeding rates. Results showed that the IMPROVE scores ranged from 0 to 22, while Consensus scores ranged from -5.60 to -1.21.
However, she reported that the ability of either RAM to predict 90-day bleeding, calculated by computing the areas under the respective receiver operating-characteristic curves (AUC) was “no better than a coin toss” (AUCs: IMPROVE 0.61, Consensus 0.59), a finding that was similarly low at 30 and 60 days post-admission. The predictive ability for either score was consistent across both surgical and nonsurgical patients.
“In this validation study evaluating these two bleeding RAMs for patients being considered for pharmacoprophylaxis, we found that increasing scores
Venous stenting and the IVC: ‘Persistent problems’ in the setting of post-thrombotic syndrome
The question of “persistent problems” with venous stenting among post-thrombotic syndrome (PTS) patients emerged as a key talking point during the recent Deep Venous Stenting Summit that took place during VAM 2023.
The issue was raised by venous disease titan Peter Gloviczki, MD, professor and chair emeritus of vascular surgery at the Mayo Clinic in Scottsdale, Arizona, after a talk by Erin Murphy, MD, director of the venous and lymphatic program at Atrium Health’s Sanger Heart & Vascular Institute in Charlotte, North Carolina, drilled into the management of stent complications—pondering whether to recanalize, explant or bypass.
Prior speaker, Mark D Iafrati, MD, a professor of vascular surgery at Vanderbilt University Medical Center in Nashville, Tennessee, had in a prior talk on best medical treatment and surveillance protocols already provided the data behind Gloviczki’s point— published in 2013 in the Journal of Vascular Surgery by Seshadri Raju (Jackson, Mississippi) and colleagues showing 90–100% patency in the setting

of non-thrombotic disease and 74–89% in PTS at three to five years, outcomes which he said hold up today.
“Dr. Raju’s results are excellent, but let’s face it, about one-in-four post-thrombotic patients has problems with stents, and there are persistent problems,” Gloviczki commented at the close of the summit. “One, for instance, is if you have a lesion very close to the IVC [inferior vena cava].
“We really don’t have a beveled stent in this country,” he continued, referring to the CE-marked sinus-Obliquus (Optimed). “Even the dedicated stents extend, at least in part, in these patients into the vena cava. So, I wanted to ask Erin if you still use the technique of combined stenting and have you had problems with the penetration of the wall by the Z-stent?”
Murphy related her early
were associated with increasing bleeding rates, but that the scores actually had low predictive ability for 90-day bleeding in a general hospitalised setting,” Hayssen offered in her concluding remarks.
“The bleeding RAMs possibly are not ready for general implementation in a hospital setting. More validation studies and more evaluation of the components of these models is needed to improve predictive ability to evaluate these models in conjunction with our more commonly used VTE risk assessment models.” In the discussion that followed the presentation, Hayssen was asked by session moderator Michael Dalsing, MD, of Indiana University School of Medicine in Indianapolis, Indiana, what factors could improve the two scores.
“It is a combination of adding risk factors that are not included,” she commented, noting that one of the risk models has 11 risk factors and the other has seven. It could be possible, she said, to include risk factors that are related but also possibly removing risk factors that are not related.
“When we looked at the prevalence of the factors in the bleeding group and the non-bleeding group, there were [factors] that were possibly, in isolation, considered more protective based upon their incidence in the two groups. So, while we have not evaluated which risk factors may be more important, that is definitely an aim of future research that we have.”
experience navigating venous dedicated stents to her intended landing spot.
“With the introduction of more advanced stents, initially, I encountered some challenges in precisely positioning them at the cava and effectively addressing the cranial disease. This predicament led me to consider reverting to the use of combined stenting with Z-stents,” she detailed. “However, over time, I have managed to refine the technique of accurate placement without covering the contralateral vein.”
It is a different story among already stented patients who land in Murphy’s practice, she continued. “I do see patients come into my practice after being stented elsewhere, and many of these stents are extended into the IVC effectively jailing the contralateral iliac vein. While I recognize that our understanding is still evolving, it took us a span of 10 to 15 years of Wallstent [Boston Scientific] use to conclusively identify this as a problem. While there are bigger interstices on the newer generation stents suggesting that jailing may be safer, isolated instances of contralateral deep vein thromboses, hint at the possibility of its eventual prevalence.”
Regarding Z-stent use, Gloviczki
inquired whether Murphy is seeing these stents erode through the caval wall over time. Murphy stated that “proper technique using these stents within a Wallstent, with only a quarter of the stent extending cranially from the Wallstent edge, often prevents this complication. She admits that, “In cases of unsupported Z-stenting, particularly after cutting the cranial Z-stent suture, she has seen this occur in a few patients, albeit without consequences thus far.” Gloviczki further pondered the specter of the external iliac vein. “We never talk about it but most of the time we stent into the external iliac vein, and mostly we do so because some of the common iliac veins are so big, but practically every time we jail the internal iliac vein, and I wonder if in the long run this is not going to be an issue.”
Murphy referred to the use of Wallstents in this setting over the years. “I don’t recall seeing a consequence of that,” she noted. “The internals are so well collateralized, but maybe we’re just not looking.” Fellow panelist Lorena DeMarco-Garcia, MD, chief of vascular surgery at Plainview Hospital, Northwell Health in Syosset, New York, concurred, saying: “The pelvic floor drains contralaterally and that is it. But I’m sure we are probably eventually causing future ostium occlusion, for sure.”
Peter Gloviczki
“We found that increasing scores were associated with increasing bleeding rates, but that the scores actually had low predictive ability for 90-day bleeding in a general hospitalised setting.”
The pulmonary arterial tree— it’s time we branch out
Nicolas J Mouawad, MD, urges vascular surgeons to “get out of their comfort zone” and become more involved in pulmonary embolism (PE) care.
WITH OVER ONE MILLION cases of deep vein thrombosis (DVT) and/or PE diagnosed each year in the U.S. alone,1 the management of patients with venous thromboembolic disease (VTE) is a critical public health concern.2 So much so that in 2008, the U.S. Surgeon General declared a formal call to action against VTE. Despite an initial modest increase in awareness, it has been the recent COVID-19 pandemic that truly erupted a flurry of VTE therapies and catapulted this pathology from the sidelines to center-stage. Although DVT and PE are a continuum of the same disease state, untreated acute PE has a mortality of 30%.3 The severity of impact is primarily based on the embolic burden and the resultant effect on the right ventricle (RV), in addition to underlying comorbid conditions. The vicious cycle commences with acute increases in pulmonary arterial pressure secondary to the embolic obstruction which increases right ventricular afterload, increasing RV myocardial oxygen consumption and impairing RV contractility. This in turn subsequently affects the left side manifest by decreased cardiac output that can eventually lead to cardiogenic shock and death.
Pulmonary embolism response teams (PERTs) have emerged as an effort to battle the crisis of pulmonary emboli. Akin to “doctor-heart” for ST-elevation myocardial infarctions (STEMIs) and code stroke activations, the PERT is a multidisciplinary team focused on early triage, assessment, risk stratification and rapid coordination of an organized response to mobilize resources as necessary for PE care. These traditionally have been composed of interventional medical specialties with surgical counterparts as backup. The role of the vascular surgeon in the management of PEs varies widely and is based on their interest, their comfort (particularly navigating the heart), geography and the institutional politics.
The main issue in my opinion is that it feels outside of our “comfort zone” to be in the thorax. Whether surgically or by endovascular means, the thorax has historically been a black box—a void—for the vascular surgeon. From an interventional perspective, it is a domain of cardiothoracic surgery, interventional cardiology and interventional radiology, among some others. Furthermore, dedicated training paradigms have not
been established for formal education in navigating the heart and the pulmonary vasculature for vascular surgeons. Most of us that are involved in PE care learned it from our interventional colleagues, training courses, or “on the job”. But why do we not take a more active role in this disease process? After all, we are vascular specialists very comfortable in diseases of the arteries, veins and lymphatics, whether medical, minimally invasive or maximally open.
And who gets an intervention? Unfortunately, risk stratification of patients with PE remains in development. The most common system separates them into low risk, intermediate risk, and high risk. An in-depth evaluation of cost, resource utilization, risk and safety profiles as well as clinical efficacy, such as Hi-Peitho, Peerless 2, STORM-PE, PE-TRACTS, among others, are currently underway to help answer many of these questions. For those that qualify for intervention based on currently used criteria, vascular access is obtained in the standard fashion with ultrasound guidance. Caval venography is performed to ensure no anatomic abnormality, thrombosis or clot in transit. The right heart is then catheterized—I’m a fan of the angled pigtail more so than a balloontipped catheter such as the SwanGanz as I feel its shape mirrors the anticipated trajectory. For each one of my PE interventions, a full right heart catheterization is performed. A comfort with waveform analysis traversing right atrium, right ventricle and into the main pulmonary artery is paramount. These are standard displays in a cardiac catheterization laboratory although not usual in the operating suite, so depending on your site of care, it is important to equip your lab with the ability to transmit and display these data. Clearly it will help monitor critical patient vitals and also assist in evaluating the effectiveness of some interventions. The procedure is then completed in the standard fashion.
Just as we have adopted many new disruptive technologies for the management of our patients, the pulmonary vasculature is an extension of the vascular tree we are trained to treat. I submit that it is time we branch out in the pulmonary arterial tree and become comfortable navigating the heart. We are trained for quick
decision making in high-stakes situations. It’s time to dust off our old physiology textbooks and revisit right heart pressures, pulmonary vascular resistance and dynes/sec! A multidisciplinary group is imperative for the management of patients with PE—and for a successful PERT—and vascular surgeons should get out of their comfort zone and play an active role in this patient population and pathology. We have a duty to our trainees to develop training paradigms to tackle all components of vascular
disease and offer a familiarity and applicability of endovascular concepts while addressing barriers to implementation. Through continued awareness, education, and support, we can help cement vascular surgery as an integral component of comprehensive PE care and focus on improving PE patient outcomes.
Nicolas J Mouawad, MD, is chief and medical director of vascular and endovascular surgery at McLaren Health System in Bay City, Michigan.

References
1. Lutsey PL, Zakai NA. Epidemiology and prevention of venous thromboembolism. Nat Rev Cardiol. 2023 Apr;20(4):248–262. doi: 10.1038/ s41569-022-00787-6. Epub 2022 Oct 18. PMID: 36258120; PMCID: PMC9579604.
2. US Department of Health and Human Services. Surgeon General's call to action to prevent deep vein thrombosis and pulmonary embolism 2008. http://www.surgeongeneral.gov/topics/deepvein.
3. Bĕlohlávek J, Dytrych V, Linhart A. Pulmonary embolism, part I: epidemiology, risk factors and risk stratification, pathophysiology, clinical presentation, diagnosis and non-thrombotic pulmonary embolism. Exp Clin Cardiol. 2013 Spring;18(2):129–38. PMID: 23940438; PMCID: PMC3718593.
“Whether surgically or by endovascular means, the thorax has historically been a black box— a void—for the vascular surgeon.”
ERIN MURPHY
“Occasionally, taking a step in a different direction can pave the way for substantial strides forward,” Erin Murphy, MD, tells Venous News, recalling her discovery of the venous world and a defining moment in her career. In this interview, the director of the venous and lymphatic program at Atrium Health’s Sanger Heart and Vascular Institute in Charlotte, North Carolina, charts her career so far, outlines who have been some key mentors, and highlights some of the most important recent developments in the field.
Why did you decide to pursue a career in medicine then to specialise in vascular and venous surgery?
Interest in the medical field was part of me from an early age from as far back as I can recall. My first formative experience was during high school when an opportunity to set up my own summer internship presented itself through a school program. My friend and I partnered up and I vividly recall the cardiac surgeon’s amused response to our request to shadow him for eight weeks.
Nevertheless, he generously welcomed my friend and I to Buffalo General Hospital the following Monday morning. That summer, I learned to drive while spending my days observing coronary artery bypass surgeries and occasional pacemaker placements. This experience left an indelible mark, solidifying my aspirations and propelling me towards becoming a pre-med student in college.
As I began my journey at Georgetown University Medical School, I found myself gravitating towards the advanced surgical specialties. During my residency, I discovered a passion for fields that demanded both high levels of technical precision and complex thinking. Working alongside Dr. Frank Arko at University of Texas Southwestern Medical Center, I found a passion for vascular surgery, a rapidly evolving field where contributions in both technology and research were instrumental in shaping its current progress. This was around the time of the early endovascular era when endovascular aneurysm repair and percutaneous mechanical thrombectomy for deep venous thrombosis (DVT) were just gaining momentum. The excitement and challenges of vascular diseases captivated me through the remainder of my residency and fellowship, while my fondness for the patients we treated deepened.
Initially I embarked on a more conventional career pathway with emphasis on the treatment of arterial diseases. However, an ill-fitting initial job choice compelled me to question my professional trajectory. Embracing an opportunity within a distinguished venous program, I embarked on a new path with uncertainty but resolute in my conviction that a different direction was necessary.
I swiftly learned a valuable lesson—that occasionally, taking a step in a different direction can pave the way for substantial strides forward. I have since grown appreciative of the year that beckoned me to explore alternative avenues.
I quickly discovered the underdeveloped state of the venous landscape. Patient care in this realm had been marginalized compared with their arterial counterparts. I found that
treating individuals who had long endured limited options was fulfilling and it continues to be meaningful. I was surprised how much was still to be learned and improved on. The immature state of the venous field led to an opportunity to contribute to academic and technological progress in a way that has been unique to the venous field in the past decade.
Who have been your career mentors and what is the best advice they have given?
My earliest mentor was Dr. Frank Arko. In early residency, he met my interest in this field with valuable opportunities for training and research. Through his connections I was able to spend a year working with Christopher Zarins and Tom Fogarty through the Stanford Vascular Division. These physicians’ collective approach to vascular surgery resonated with me, emphasizing a commitment to delivering excellent patient care, staying at the forefront of and contributing to innovation, maintaining high-quality standards, and advocating for our patients. During my fellowship training, other influential mentors included Ed Woo and Ronald Fairman, who offered invaluable guidance, training, and support.
When entering the venous field, I had the privilege of working with Sheshadri Raju at the Rane Center in Jackson, Mississippi. He opened my eyes to the potential impact of venous interventions, the significance of having dedicated interventionalists focused solely on venous disease, and the need for advancements in the field in terms of knowledge and technology.
The environment of continual progress and growth in the venous space has cultured a community of academic leaders in the space that function not only as colleagues but as friends and mentors for each other. I am proud of my professional associations and continue to learn and grow through my collaborations with colleagues such as Stephen Black, Gerry O’Sullivan, Kush Desai, Mark Meissner, Kathy Gibson, Stephen Abramowitz, Ramon Varcoe, Ron Winokur, Kathleen Ozvath, Gloria Salazar and Misaki Kaguchi. Working closely with Peter Schneider, Stephen Black, Manj Gohel, Armado Mansilla, Andrew Holden and Dittmar Böckler for academic program development has been extremely gratifying. Roger Greenhalgh has certainly had a remarkable career and has helped to support mine forward. I have found the career paths of colleagues such as Frank Arko, George Adams, Peter Schneider, Eric Secemsky, and Michael Jaff compelling and forward facing.
Mentorship transcends the boundaries of medicine, as I’ve learned to appreciate individuals in my industry partnership
who embody qualities of professionalism, thoughtfulness, leadership, and grace, providing unique perspectives that have profoundly enriched my personal and professional development. Lynn Oster, Dr. Simona Zanetti, Renata Evertz, Susan Smith, and Jennifer Stryker have modelled career success as women in leadership. David Cole, a prior industry representative, inspires me as I watch the effort, motivation and brass tacks it takes to embark on a different career path. I have no doubt he will succeed in his new endeavours as he utilizes his patient first mentality to create progress.
What has been the most important development in venous surgery during your career so far?
FACT FILE
CURRENT APPOINTMENTS
2023–present: Cochair, Charing Cross (CX) Symposium
2020–present: Venous executive board member, CX Symposium
2017–present: Attenting vascular surgeon, director of Venous and Lymphatic Center, Sanger Heart and Vascular Institute, Atrium Health (Charlotte, North Carolina)
PREVIOUS APPOINTMENTS (SELECTED)
2014–2017: Attending surgeon, Rane Center for Venous and Lymphatic Diseases, St. Dominic's Hospital (Jackson, Mississippi)
SPONSORED CLINICAL TRIALS
(SELECTED)
National principal investigator, site principal investigator, ABRE venous stent investigational device exemption (IDE)
National principal investigator, Venclose postmarket trial
Site principal investigator, Gore Viafort IVC and iliac vein stent trial
Site principal investigator, CLEAR DVT
Site principal investigator, VIVID clinical study
The introduction of dedicated venous stents stands as the most significant advancement in venous surgery since my entry into the field. This technological breakthrough has brought about major gains in the venous space that cannot be overstated, as it extends beyond technological progress. With Food and Drug Administration (FDA) approval, the use of venous stents becomes more widespread and normalized, furthering the field of venous stenting. Moreover, approval opens doors for funding research and supporting education platforms and initiatives.
What are the biggest challenges currently facing the venous world?
The venous field has been facing its challenges head on starting with a foundational perception problem. Venous disease has long been considered less significant, with treatment seen as simpler and less impactful compared to arterial pathologies like peripheral arterial disease and aortic disease. In regards to impact, the reality is that conditions like pulmonary embolism and DVT pose substantial mortality risks. Patients with moderate to severe venous hypertension experience a quality of life comparable to individuals with severe chronic medical conditions including chronic obstructive pulmonary disease, congestive heart failure, and angina. Venous disease remains the leading cause of leg ulcers, placing considerable financial strain on patients and the U.S. healthcare system. Appropriate interventions are crucial and serve to enhance patients’ lives and productivity, reducing economic burdens on the individual and healthcare system.
The perception of simplicity of the judgments and techniques in venous surgery is also false. Given the inherently low pressure in the venous system, even minor errors in technique or judgment can have profound consequences, leading to failures. This issue is especially critical in venous stenting, as rectifying failures after they occur can be exceedingly challenging. The complexity of decision-making in venous is also very high both inside and outside the interventional suite.
The swift technological progress in the venous space has been a major gain in the field; however, this progress has outpaced education. Although efforts are being made to educate on disease processes and long-term success techniques, substantial gaps remain.
Segmentation of venous care is currently common and increases the challenges in closing these knowledge gaps. Physicians are often specializing in only superficial,
deep, or lymphatic treatment options, lacking comprehensive training in all areas of the disease. This issue is exacerbated by limited training options, with only a few venous fellowships available and a lack of comprehensive training in existing interventional fellowships, leaving physicians ill-equipped to handle the complexities of decision-making in this domain. The need to formalize education to the extent and level of importance of aortic and peripheral interventions is paramount to minimize patient risk and maximize patient benefit.
How has Sanger Heart and Vascular Institute’s venous and lymphatic program developed since its inception?

The Sanger Heart and Vascular Institute is renowned for its exceptional clinical cardiovascular care, as well as its commitment to cutting-edge research and innovation. Recognizing the increasing treatment options available for venous and lymphatic conditions over the past decade, the institute naturally sought to establish the Venous and Lymphatic
Center. This endeavour aimed to extend its world-class expertise to patients who had previously faced limited options.
Initially integrated into the vascular clinics, the center steadily evolved into an independent clinic within the vascular division, attracting referrals from local, national, and international sources. Demonstrating a dedication to pioneering research, the center has become a pivotal site for numerous international trials and has been involved in the initial use of groundbreaking medical devices in patients.
Given the rapid advancements in this field, the focus on research and innovation is of paramount importance to me. It enables us to stay at the forefront of developments and provide our patients with the most advanced treatment choices available.
Equally crucial is our center’s capacity to offer comprehensive care for venous patients. Venous diseases often exhibit interrelated complexities, and our ability to thoroughly assess and address all aspects is indispensable. Presently, our range of treatments covers acute DVT, non-thrombotic and post-thrombotic
chronic venous obstruction, superficial venous insufficiency, and pelvic venous disorders.
I am committed to continuing the center’s growth. Our dedication to patient care, research and innovation fit well within Sanger and I seek to help the center to maintain a leading position in the ever-evolving landscape of venous and lymphatic disease, offering our patients the highest standards of medical excellence and access to cuttingedge treatment options, all while seeking improved outcomes for our patients and the venolymphatic field as a whole.
What are your hobbies and interests outside of medicine?
I love adventure, being out in nature, and the thrill of travel. I enjoy connecting with friends and family. As a devoted mom to three vibrant young boys, they are my regular adventurous sidekicks. They have met many of my gracious colleagues at academic meetings! We are most often hitting the trails, exploring creek beds, enjoying lake life, playing football, heading to the beach, or exploring a new park or city.
"I found that treating individuals who had long endured limited options was fulfilling and it continues to be meaningful.”
LAMA trial: MOCA ‘may have a role in a small number of selected patients’
Five-year results of the LAMA randomized controlled trial (RCT) show that both mechanochemical ablation (MOCA) and modern endovenous laser ablation (EVLA) technology are associated with low procedural and post-procedural pain, while clinical outcomes in the short and medium term are worse for MOCA. This led senior author Daniel Carradice, MD, of Hull York Medical School in Hull, England, to conclude that MOCA “may have a role in a small number of selected patients such as those with a fear of needles”.

FIRST AUTHOR ARTHUR LIM, MD, also of Hull York Medical School, presented the five-year results at the recent European Venous Forum (EVF) in Berlin, Germany (June 22–24). He began by stating that MOCA offers a non-thermal, non-tumescent alternative to endovenous thermal ablation (EVTA)—the current first-line treatment for superficial venous incompetence (SVI)—and detailed that it combines mechanical and chemical damage to achieve vein occlusion. He stressed that the longer-term outcomes of MOCA are little known.
LAMA is a single-centre RCT that included adult patients with single-axis unilateral symptomatic SVI who were treated with either MOCA, using the ClariVein device (Merit Medical) with or without phlebectomy, or EVLA—a type of thermal ablation—using the VenaCure laser (AngioDynamics) with
or without phlebectomy.
At the one-year follow-up point, Lim recapped that both groups (each comprising 69 patients at this stage) had similar procedural pain scores. However, he added, MOCA had “significantly lower” anatomical occlusion compared to laser. In addition, both groups had similar Venous clinical severity scores (VCSS). “Our results are similar to other RCTs of MOCA,” he said.
After sharing these early results, Lim then underlined the goal for longer-term follow-up in the LAMA trial, which was to determine how reduced anatomical occlusion rates impacted venous health and quality of life.
Lim revealed that 52 patients in the laser group and 57 in the MOCA group completed follow-up out to five years. He reported that, for anatomical occlusion, initial success was achieved in all but two patients in the laser
group and all bar one in the MOCA group. Five years after treatment, however, it was observed that EVLA had a “significantly higher” anatomical occlusion rate compared to MOCA.
Regarding total reinterventions, the presenter continued, MOCA had a “significantly higher” number compared to laser—specifically, 16 for MOCA and six for laser.

Lim also communicated clinical outcome scores, first sharing that VCSS scores for both groups were similar at one year and also at five years after treatment. “The improvement in VCSS is maintained from baseline after one year and five years for both groups,” the presenter stated. For disease-specific quality of life, Lim added that both groups had similar scores at one year and five years after treatment, with the improvement maintained at both one and five years for both groups.
Results were similar for generic quality of life, with both groups showing similar scores at one and five years.
“To conclude, MOCA has significantly lower anatomical occlusion at five years,” Lim said, adding that this treatment option saw a higher reintervention for symptomatic clinical recurrence. The presenter also reiterated that the investigators were unable to detect any difference in clinical outcomes between laser and MOCA at five-year follow-up.
Speaking to Venous News, Carradice summarizes that LAMA supports the case that the likely disadvantage of MOCA is reduced anatomical occlusion over time, and that this reduced anatomical occlusion is clinically relevant as it is linked to much higher reintervention. He continues that while there is no significant difference at five years in clinical severity or quality of life between the two treatment methods, this should be interpreted with caution, as it is only after a high rate of reintervention, and the smaller numbers in the subgroup analysis are susceptible to type 2 statistical error.

“LAMA supports the case that the likely disadvantage of MOCA is reduced anatomical occlusion over time.”
DANIEL CARRADICE
Data in the pipeline for ‘toolbox’ of saphenous vein ablation options
In an interview with Venous News at this year’s Leipzig Interventional Course (LINC) in Leipzig, Germany (June 6–9), Raghu Kolluri, MD, of OhioHealth in Columbus, Ohio, outlined the “vast list” of options that are now available for the treatment of patients who require saphenous vein ablation.

FROM RADIOFREQUENCY, WHICH FIRST gained approval over a quarter of a century ago, to surgical, laser and non-thermal ablation options, the treatment landscape for these patients has evolved over time, Kolluri began. “All these are tools in the toolbox to take care of our patients’ pathology depending on their anatomy and presentation,” he explained, inspiring hope for the field as advancements continue. Turing his attention to data, Kolluri referenced SPECTRUM as the most important trial in the superficial venous space in the near future. “I cannot think of a larger trial or more important trial in this space because (a) it is the largest post-market study in the space of superficial venous intervention and (b) it is going to assess the role of closure of the great saphenous vein in the treatment of venous ulcers,” he opined. In terms of what is missing from the literature, Kolluri did stress that there is no head-to-head comparison of the available treatments to assess which
has the fewest complications.
The system medical director of Vascular Medicine at OhioHealth, Kolluri also touched on the importance of multispecialty treatment, stressing that “holistic care” is crucial in the venous space. “If [you are] unable to offer the full spectrum of venous treatments, [you have] got to collaborate,” he said, highlighting the importance of his vascular surgery, interventional cardiology and interventional radiology colleagues in his day-today practice.
“There are large venous aneurysms that I send routinely to my vascular surgery colleagues who are my partners in my practice,” Kolluri continued. “And on the other hand, the vascular surgeons will send their complicated thrombotic patients with reflux to me because I deal with hypercoagulable states and venous interventions.” Kolluri also made note that he advises colleagues to “jump in with both feet” rather than making venous intervention a side operation to the main procedure the patient is undergoing.
Finally, Kolluri listed some unmet needs in the saphenous vein ablation space, including which procedure to tackle first in postthrombotic patients, and whether to treat reflux or obstruction first in venous ulcer patients. He remarked that while there have been great advancements, there is still room for growth within the field.
“You have data from the EVRA trial, which tell us that for small
Review urges development of protocols to reduce hypersensitivity reactions after cyanoacrylate varicose vein treatment
Despite being considered “generally safe”, cyanoacrylate can cause local reactions in up to 25% of patients, disproportionately affecting women, Asian race and thin patients with a body mass index of <22. This was the conclusion drawn by Eduardo Silva, MD, of Coimbra Hospital and University Centre in Coimbra, Portugal, in his presentation at EVF 2023.
CYANOACRYLATE, THE speaker first noted, has gained popularity in recent years for the treatment of varicose veins, due to its “minimally invasive” procedural nature and its ability to be performed in an outpatient setting. However, concern has grown in parallel to cyanoacrylate’s uptake, since increasing reports of “phlebitis-like reactions” have led some to question its safety.
These kinds of reactions have been later associated with type IV hypersensitivity, Silva explained, observing that symptoms can range from local itching, erythema, pain and swelling—typically resolving within a few days—although “severe” reactions have been reported.
Elaborating further on the typical presentation of this kind of hypersensitivity, Silva emphasised that type IV hypersensitivity often has a delayed onset, developing days to months after exposure to cyanoacrylate. Warning against expecting an immediate reaction, he made clear that “most of
these will be between two to three days after the treatment”. Silva explained that these reactions occur in response to antigens produced by the subject to foreign substances that he has previously been exposed to, which, upon new exposure, triggers an “inflammatory cascade mediated by T cells”.
Using this information as the foundation of their study, Silva et al conducted a literature review using Embase and PubMed databases,
wounds, you probably do not need to treat the deep system. But for the larger wounds, we all believe that we need to treat the deep system first before treating the superficial system,” Kolluri noted, while acknowledging that there is currently no science to support this approach.
Additionally, Kolluri highlighted that the venous field is still lacking data comparing thermal ablation for saphenous reflux to physiciancompound foam, which he noted was used in approximately 50% of patients in the EVRA trial.
When it comes to venous research over the next five to ten years, Kolluri’s stance is that the need to assess whether “the deep is responsible for the ulcers or the superficial is” should be at the forefront of future study. Secondly, he expressed the importance of understanding what a “true hemodynamically significant lesion” should be defined as.
He also touched on the need for a research trial to understand the success rates of physician-compounded foam in the treatment of axial reflux and how the intervention compares to thermal and non-thermal treatments. Lastly, he spoke on the need for data regarding sub-ulcer plexus treatment.
“All of us who take care of these ulcers, we use sub-ulcer sclerotherapy under ultrasoundguidance, but there is no data to support it, and so I am looking forward to that trial being done as well.”
evaluating the incidence and symptoms of suspected hypersensitivity reactions and their relation with phlebitis-like adverse events following cyanoacrylate varicose vein treatment.
Identifying 17 studies which reported severe complications, they highlighted 1,208 patients that had undergone cyanoacrylate varicose vein treatment, amounting to 1,631 treated veins. In total, 13 veins had to be excised in nine patients. Among these patients, the majority were female (65.8%), with a mean age of 52 years.
Looking closely at less severe reactions to cyanoacrylate treatment, Silva and his team noted 250 patients who had developed some form of adverse reaction after administration, the most common reaction being thrombophlebitis or phlebitis-like reactions (4–25.4%); however, he asserted that “most complications were mild and self-limited”.
Building a portfolio of risk factors, the speaker noted that the presence of suprafascial saphenous vein location (<1cm underneath the skin), as well as larger veins (>8mm), were associated with adverse reactions to cyanoacrylate. Although Silva concluded that population characteristics and procedural factors “did not seem to influence the risk of developing hypersensitivity”.
After critically reviewing the literature, Silva concluded his presentation by asking the question: “Who should we test?” He asked if it should it be everyone? Patients with a known acrylate allergy? Or patients
at risk of previous exposure? First, he considered patch testing all patients preprocedure, stating that this “can be very useful to identify patients that might be at risk of developing hypersensitivity,” though he warned that “exposing everyone to [patch testing] may actually be causing first exposure and sensitising the patient”.
Secondly, revealing a trick question, Silva eliminated patients with a known acrylate allergy completely, stating that these patients “should not be treated [with cyanoacrylate] at all”. Looking at his third option, he concluded that patients at risk of previous exposure should be considered for testing, although “many patients do not know they have been previously exposed,” posing difficulties for healthcare providers.
Providing a clear overview of their findings, Silva conveyed that cyanoacrylate is “a safe treatment,” but discussion needs to address the differences between phlebitislike reactions and “classic” thrombophlebitis. Finally, he emphasised the importance of “developing protocols to identify and reduce hypersensitivity reactions,” and urged physicians to consider referral to clinical allergists “when in doubt.”

“If [you are] unable to offer the full spectrum of venous treatments, [you have] got to collaborate.”Raghu Kolluri Eduardo Silva
“Many patients do not know they have been previously exposed.”










SIR position statement outlines appropriate use of endovascular management for chronic iliofemoral venous occlusions
The Society of Interventional Radiology (SIR) has published a position statement offering recommendations on the management of chronic iliofemoral venous obstruction with endovascular placement of metallic stents. The statement, published online in the Journal of Vascular and Interventional Radiology, is a companion to the 2022 statement on the treatment of acute iliofemoral deep vein thrombosis.
In the new statement, a multidisciplinary group of experts from interventional radiology (IR), vascular medicine, and vascular surgery indicated that among patients with chronic venous disease and iliofemoral venous obstruction, those who are experiencing life-disrupting symptoms or disability, and who have anatomic features that favour longterm patency, may be more likely to benefit from stenting as an adjunct to conservative management. Most other patients with chronic iliofemoral venous occlusions would be better served with conservative management alone, such as use of medical therapy and compression garments, and re-evaluated over time.
“There is strong consensus on the panel that excellent clinical decisionmaking around venous stent placement will be most likely when the treating physician has strong familiarity with key clinical considerations around optimal diagnosis and evaluation of iliac vein obstruction, as well as assessment of its clinical severity and life impact,” said

Suresh Vedantham, MD, of Washington University School of Medicine in St Louis, Missouri, who is the lead author of the statement. “The statement provides a framework against which IR physicians can review their practices, address knowledge gaps, deliver treatment effectively, and ensure that patients selected for stent placement are likely to benefit from it.”
The statement authors note that additional research is needed to better guide the use of stents in this patient population. If completed, two ongoing multicentre randomised controlled trials—C-TRACT and BEST— can enable a strong and unbiased understanding of the treatment effects associated with the addition of venous stent placement to standard care, Vedantham said.
“For both studies, success will depend on whether providers make it a priority to refer patients to study sites,” he said.
“It is hoped that physicians will promote the welfare of future venous disease patients by actively choosing now to
enrol eligible patients in ongoing clinical trials that are designed to generate high-quality evidence on the benefits, risks, and best practices around venous stent placement.”
While this research proceeds, SIR believes that adherence to the statement’s recommendations will enable judicious use of endovascular therapy in a manner that optimises benefit and minimises harm.
“The new statement provides the best assessment of the current evidence we have to date, and SIR is grateful to the authors for their time and energy in ensuring that we have evidence-based guidance for the treatment of chronic venous occlusions,” said SIR President Alda L Tam, MD, of the University of Texas MD Anderson Cancer Center in Houston, Texas.
“SIR remains committed to supporting ongoing and future research in this area to ensure that physicians have the information they need to optimize patient care now and in the future.”
Primary patency after venous stenting best in NIVL patients, study finds
A recent study concludes that non-thrombotic iliac vein lesion (NIVL) patients have better primary patency after venous stenting than patients with venous thrombotic disorders. Olivier Espitia, MD, of CHU de Nantes in Nantes, France, and colleagues report this main finding from a multicentre cohort study in the European Journal of Vascular and Endovascular Surgery (EJVES).
THE AUTHORS DETAIL THAT IT WAS THEIR aim to assess primary stent patency predictive factors in three groups of patients with history of lower limb vein thrombosis: NIVL, acute deep vein thrombosis (aDVT) and post-thrombotic syndrome (PTS).
The investigators included consecutive patients from January 2014 to December 2020 with history of lower leg vein stenting from seven hospitals in the study. They note that all patients received an iliac
or common femoral venous stent and had at least a six-month follow-up available with stent imaging.
The team reported the anticoagulant and antiplatelet therapy strategies employed after venous stenting and compared these between the three patient groups.
In their results section, Espitia et al state that the study included 377 patients in total, comprising 134 in the NIVL group, 55 in the aDVT group and 188 PTS patients, and that median follow-up was 28.2
months (interquartile range 16, 47). The authors report in EJVES that primary patency was statistically significantly higher in the NIVL group (99.3%) compared with the PTS group (68.6%; p<0.001) and the aDVT group (83.6%; p=0.002).
In addition, the researchers note that PTS patients received a statistically significantly greater number of stents (p<0.001) and had more stents below the inguinal ligament (p<0.001).



Finally, Espitia and colleagues relay the findings that discontinuation of antiplatelet therapy at the last assessment was 83.6% for NIVL, 100% for aDVT, and 95.7% for the PTS group (p<0.001). Discontinuation of anticoagulation therapy at the last assessment, they add, was 93.2% for NIVL, 25% for aDVT, and 70.3% for the PTS group (p<0.001). “The only predictor of worse primary patency in the aDVT group was long-term anticoagulation before stenting,” the authors highlight.

“For both studies, success will depend on whether providers make it a priority to refer patients to study sites.”
Child-bearing age ‘should not be a contraindication to venous stenting’
In a recently published study, dedicated venous stents performed well through pregnancy and postpartum, and a protocol including the use of low-dose antiplatelets in combination with anticoagulation at either a prophylactic or therapeutic dose depending on the patient’s risk profile appeared safe and effective.
WRITING IN THE JOURNAL OF VASCULAR Surgery: Venous and Lymphatic Disorders (JVSVL), authors Laurencia Villalba, MD, of the Vascular Care Centre in Wollongong, Australia, and Theresa A Larkin, PhD, of the University of Wollongong in Wollongong, Australia, share that the aim of their study was to assess the performance of dedicated iliac venous stents during subsequent pregnancy and postpartum, including stent patency and stent integrity, as well as incidence of venous thromboembolism (VTE) and bleeding complications.
The investigators outline in their introduction that, while venous stenting has become the preferred method of treatment for non-thrombotic iliac vein lesions, postthrombotic lesions, and lesions found after thrombus removal in the setting of an acute iliofemoral deep vein thrombosis, “concern remains about stenting women of child-bearing age”. They explain that this is because pregnancy is a hypercoagulable state, and the gravid uterus can potentially compress the stent and/ or the inflow vessels and thus compromise patency.
Villalba and Larkin add that the current literature on the performance of venous stenting during pregnancy comprises only six studies to date, including 66 patients and 74 pregnancies, with most stents assessed being Wallstents (Boston Scientific).
This was a single-site, prospective cohort study.
Villalba and Larkin detail that women of childbearing age who had received dedicated iliac venous stents were included in a surveillance program and then, for any subsequent pregnancies, followed the same pregnancy care protocol. They explain that this included an antithrombotic regimen of 100mg aspirin
Pelvic venous incompetence:
‘Do not treat images, treat symptoms’
“EVERYTHING DEPENDS ON THE symptoms,” Aleksandra JaworuckaKaczorowska, MD, of the Center of Phlebology and Aesthetic Medicine and the Center of Surgery, Gynecology and Obstretics in Gorzów Wielkopolski, Poland, stresses in an interview on pelvic venous incompetence with Venous News

“Your decision should be based on the pelvic symptoms, not the images,” Jaworucka-Kaczorowska elaborates, sharing her advice on how best to determine the most effective treatment plan for a patient with pelvic venous incompetence.
She notes that the varying nature of symptoms for pelvic venous incompetence makes this strategy necessary, noting for example that pelvic-origin varicose veins can be present without pelvic symptoms. In addition, Jaworucka-Kaczorowska highlights that in many cases patients
daily until gestation week 36, and subcutaneous enoxaparin at a dose dependent on risk of thrombosis. Going into more detail, Villalba and Larkin specify that low-risk patients, those stented for non-thrombotic iliac vein lesions, received a prophylactic dose of 40mg/day from the third trimester, while high-risk patients, those stented for thrombotic indication, received a therapeutic dose of 1.5mg/kg/day from the first trimester. All women underwent follow-up with duplex ultrasound assessment of stent patency during pregnancy and six weeks postpartum, the authors note.
The authors report that, among 10 women who had received dedicated iliac venous stents for either a nonthrombotic or thrombotic indication, and 13 post-stent pregnancies—during which a dedicated protocol for stent thrombosis prevention was followed—there was a 100% patency rate, no bleeding complications, and no VTE during pregnancy or puerperium. Only one stent was permanently deformed/compressed by the gravid uterus, but it was a Vici stent (Boston Scientific) that had been “balloon fenestrated” at the time of insertion due to concerns of contralateral caging, so it had lost its structural integrity.
In the discussion of their findings, the investigators write that the main limitation of their study is its small sample size. They also acknowledge that it is still unknown whether multiple pregnancies could affect stent structure over time.Villalba and Larkin also highlight the study’s key strengths, including the fact that patients were followed up prospectively, and that the investigators followed a protocol including serial imaging, multidisciplinary
are asymptomatic, and do not require any pelvic diagnosis or treatment at all.
In the patients who do experience pelvic symptoms due to pelvic venous incompetence, Jaworucka-Kaczorowska explains, the best option is to embolise, citing “very good” results for this treatment option. She mentions in particular one systematic review that showed 70–100% of patients reported some degree of symptom improvement with embolization, and another in which 75% of patients said that embolization relieved their pelvic symptoms.
In other situations, however, such as when a patients has varicose veins of pelvic origin without pelvic symptoms, Jaworucka-Kaczorowska points out that embolization would not be the treatment of choice. Instead, the best option would be to treat from below, she says, for example with sclerotherapy of pelvic escape points and related varicose veins.
Jaworucka-Kaczorowska notes that new guidelines on the management of varicose veins from the European Society for Vascular Surgery, published in March of last year, recommend that patients with varicose veins of pelvic origin and without pelvic symptoms should be considered for treatment from below. “We should not do embolization [in these patients],” she stressed. “Of course, when a patient has pelvic symptoms, you do the embolization to
input and a tailored antithrombotic regime.
“Dedicated iliac venous stents perform well during subsequent pregnancy with no stent occlusion or fracture,” Villalba and Larkin conclude. They state in closing that child-bearing age “should not be a contraindication to venous stenting”.
The current literature on the performance of venous stenting during pregnancy comprises only six studies to date, including 66 patients and 74 pregnancies
reduce such symptoms,” JaworuckaKaczorowska reiterates. On this note, however, she stresses that the data indicate only about 10% of patients with varicose veins of pelvic origin has pelvic symptoms. For this reason, she explains, treatment from below is done more frequently and also done better. Summarising her key message, Jaworucka-Kaczorowska highlights that “the most important thing” in pelvic venous incompetence patients is to “not treat images, treat symptoms” for good outcomes. Here she cites her clinical experience as a gynecologist, noting that she sees many patients with varicose veins around the uterus that develop
around the time of a first pregnancy. Around 10% of the general population will have varicose veins, she states, while the incidence increases to roughly 30% of women after once pregnancy and the figure increasing up to 60% by the fourth pregnancy. These statistics do not mean that all these patients need to be coiled, however, JaworuckaKaczorowska says.
Finally, she stresses that the possibility for complications after coil embolisation, such as migration, need to be considered. “We have to choose wisely when we are selecting patients and do the proper diagnostic,” Jaworucka-Kaczorowska asserts.

“We have to choose wisely when we are selecting patients and do the proper diagnostic.”—
ALEKSANDRA JAWORUCKA-KACZOROWSKA
pregnancies
patients








Clinical News
VeinWay reports second human compassionate use of Traversa for venous recanalisation
In a second compassionate use case, interventional vascular surgeon Stefan Stalhoff, MD, of Klinikum Hochsauerland in Arnsberg, Germany, used VeinWay‘s Traversa for venous recanalization to save a patient’s arm, with supervision by VeinWay scientific advisory board member Michael Lichtenberg. The patient had been in so much pain, that she could not hold her young children.
This news follows the firstin-human compassionate use case announced in March, where interventional radiologists David M Williams, MD, and Minhaj S Khaja, MD, both of the University of Michigan Health in Ann Arbor, Michigan, used VeinWay’s Traversa for venous recanalisation to save a patient’s leg that was close to being amputated.
Details of both compassionate use cases were presented at this year’s Leipzig Interventional Course (LINC) in Leipzig, Germany (June 6–9) by Michael Lichtenberg, MD, of Klinikum Hochsauerland in Arnsberg, Germany.
VeinWay CEO Jordan Pollack said, “VeinWay’s Traversa helped the doctors in Germany to successfully cross a previously uncrossable blockage in the patient’s vein and restore blood flow. The patient experienced immediate relief of symptoms. I only wish we could have captured the joy on her face, as she can hold her children again pain-free.”
Stalhoff said, “By using the Traversa we saved hours of procedure time and were able to achieve a goal previously unreachable, with comparable ease. This makes two successful clinical outcomes using the Traversa thus far.”
Gore announces first US enrolment for the Viafort vascular stent iliofemoral study
Gore has announced that the first US patient has been enrolled in a prospective, non-randomized, multicenter, single-arm study with five-year follow-up to evaluate the investigational Gore Viafort vascular stent for the treatment of symptomatic

Conference calendar
Sept. 9–13
Cardiovascular and Interventional Radiological Society of Europe (CIRSE)
Annual Congress 2023
Copenhagen, Denmark cirsecongress.cirse.org/about/ welcometocirse2023
iliofemoral venous obstruction.
The first US patient was enrolled by David J Dexter II, MD, at Sentara Vascular Specialists, Norfolk, Virginia. “With several US Food and Drug Administration [FDA]-approved stents on the market, there was a concern that enrolment in another iliac vein stent trial would be difficult. Designed with the unique qualities for flexibility and radial force, the Viafort device is compelling to use in a clinical trial,” he said.
A company press release notes that the Gore Viafort vascular stent utilises the Gore expanded polytetrafluoroethylene (ePTFE) technology in conjunction with a single wire, sinusoidalwound nitinol frame. The Gore Viafort vascular stent iliofemoral study is evaluating the device in a treatment range of 10 to 20mm diameter for iliofemoral veins. The study is being conducted in the USA under an approved investigational device exemption (IDE).
Akura Medical announces successful first-in-human use of its mechanical thrombectomy platform
Akura Medical announced it has initiated its first-in-human clinical study of the Akura mechanical thrombectomy platform. A press release notes that the Akura platform is a low-profile solution designed to easily access and efficiently remove largevolume, mixed-morphology clots, and eliminate the guesswork around the procedure. The initial five cases were performed in Georgia and marked the first use of mechanical thrombectomy for pulmonary embolism (PE) in the country. Ehrin Armstrong, MD, of the Advanced Heart and Vascular Institute in St Helena, California, and S Jay Mathews, MD, of Bradenton Cardiology Center in Bradenton, Florida, proctored the first procedures in Georgia. A prospective, single-arm, multicenter study will evaluate the safety and performance of the Akura mechanical thrombectomy platform for venous thromboembolism (VTE), the company reveals.
Sept. 17–21
UIP 2023 World Congress
Miami Beach, Florida myavls.org/annual-congress-2023. html
Oct. 29–30
The VEINS (Venous Endovascular Interventional Strategies) 2023
Las Vegas, Nevada viva-foundation.org/future-meetings
Product News
Biolitec announces two new devices in the ELVeS radial portfolio
Biolitec recently announced that it has extended its ELVeS Radial laser system for the minimally invasive laser treatment of insufficient veins by two further new developments.
The ELVeS Radial 2ring Pro laser fibre is capable of removing even highly tortuous veins thanks to its additional channel for saline solution. The saline solution can be inserted directly to the front of the fiber tip via a rear Luer Lock connection. This stretches the vein before the laser light is emitted.
Also new to the ELVeS Radial family, is the single wavelength Leonardo 1940 laser. The laser with this special wavelength enables more efficient absorption of water components in the vein wall. This significantly reduces the occurrence of bruising, shortens convalescence and gives excellent esthetic results.
Biolitec has also released an updated on the “first” empirical experience with off-label use of the ELVeS Radial 2ring Pro laser fibre in the treatment of varices. By combining distal endovenous laser ablation (EVLA) and proximal foam sclerotherapy, varices can also be sclerosed in a single step. This reduces the risk of recurrence or neovascularization caused by untreated varices. A retrospective single-center cohort study from Switzerland published in March 2023, showed persistent complete occlusion of treated truncal veins and neovascularization’s even after 52 weeks, with no clinically relevant complications observed.
The researchers note that this means there are “no longer any limits” to minimally invasive varicose vein laser therapy, large truncal veins, side branches and perforating veins, veins with a large diameter, strongly tortuous veins and smaller varicose veins, which
can all be effectively and sustainably removed with Biolitec’s laser system.
Inari Medical announces commercial launch of RevCore and Triever16 Curve for venous stent thrombosis and VTE

Inari Medical has announced the launch of two new purpose-built products, the RevCore thrombectomy catheter, and the Triever16 Curve catheter.
According to a company press release, RevCore is the first mechanical thrombectomy device designed to address venous in-stent thrombosis, an increasingly common occurrence impacting more patients every year. The device includes a diametercontrolled coring element designed to engage thrombus within stents.
With RevCore, Inari has developed a solution for an entirely new patient population not currently addressed by the ClotTriever or FlowTriever platforms, the press release reports.
“Until now, physicians have had limited options to treat patients suffering from symptoms of venous stent failure and some patients are relegated to repeated suboptimal interventions,” said Steven Abramowitz, MD, of MedStar Health in Washington, D.C. “RevCore is a game changer as it physically removes in-stent thrombus, restores flow, and could potentially reduce the need for additional reintervention. There are a lot of patients out there that may benefit from the RevCore procedure.”
The Triever16 Curve catheter, the latest addition to the FlowTriever platform, is purpose-built to be versatile for both pulmonary embolism and peripheral thrombectomy. The trackable catheter features a pre-shaped curve for targeted aspiration. Inari claims that Triever16 Curve offers unique advantages over 16Fr continuous aspiration catheters, including compatibility with the FlowSaver blood return system and simple access to larger, more powerful 20Fr or 24Fr catheters within the company’s price-per-procedure model.
“Triever16 Curve is an important addition to the already comprehensive Inari venous thromboembolism [VTE] toolkit,” said Angelo Marino, DO, of Yale School of Medicine in New Haven, Connecticut.
2024 Jan. 22–25
International Symposium on Endovascular Therapy (ISET)

2024 Miami Beach, Florida hmpglobalevents.com/iset
Mar. 3–5
27th European Vascular Course (EVC)
Maastricht, The Netherlands vascular-course.com
Mar. 3–6
American Venous Forum (AVF)
2024 Tampa, Florida venousforum.org
Apr. 23–25
Charing Cross (CX) Symposium 2024 London, England cxsymposium.com



