A question from Manj Gohel (Cambridge University Hospitals NHS Foundation Trust, Cambridge, UK) on what the Charing Cross (CX) audience should take back to their multidisciplinary team meetings from the firsttime presentation of the BASIL-2 trial led chief investigator Andrew Bradbury (University of Birmingham, Birmingham, UK) to deliver the stark message: a patient who needs a belowthe-knee revascularisation with or without a femoropopliteal revascularisation is likely to do better if they are treated with a best endovascular-first strategy rather than a vein bypass-first approach.
In the BASIL-2 (Bypass versus angioplasty for severe ischaemia of the leg) trial of 345 patients with chronic limbthreatening ischaemia (CLTI), a best endovascular treatmentfirst revascularisation strategy was associated with better amputation-free survival than a vein bypass-first strategy in those who required an infrapopliteal repair—with or without a more proximal infrainguinal procedure. This result was largely driven by fewer deaths in the best endovascular treatment group. Bradbury presented this key finding at the 2023 CX International Symposium (25–27 April, London, UK). The results were simultaneously published in The Lancet “It all seems to be pointing towards attempting an endovascular procedure first and then if that does not work, doing something else—which could be more endovascular,” Bradbury said in response to Gohel. Alternatively, he added, this could be the point at which the vascular specialist switches over to a bypass approach. BASIL-2, however, “lends quite a lot of weight” to an endovascular-first revascularisation strategy, “with all the caveats that we have to consider”.
Bradbury, delivering the data for the first time during day one
of CX 2023, revealed that 63% of patients randomised to a vein bypass-first strategy of treatment underwent a major amputation or died during follow-up, compared to just 53% of those allotted to a best endovascular-first approach—BASIL-2’s primary outcome measure (adjusted hazard ratio 1.35, 95% confidence interval [CI] 1.02–1.08, p=0.037).

“Essentially this means that, in this cohort, a vein bypass revascularisation strategy resulted in a 35% increased risk of amputation or death during the follow-up compared with a best endovascular-first revascularisation strategy,” Bradbury said.
Median survival for the whole cohort was 3.8 years—3.3 years for the vein bypass group and 4.4 for the endovascular arm, he said. “The significant difference we have observed in favour of best endovascular therapy with amputation-free survival is very largely driven by the fact that there were more deaths in the vein bypass group—53% of vein bypass patients and 45% of best endovascular therapy patients,” Bradbury continued. “There is no significant difference of 30-day mortality but you can see that the median survival of the two groups is quite different.”
CLTI is the “severest manifestation” of peripheral arterial disease (PAD) and presents as ischaemic pain at rest or tissue loss, or both, the authors detail in The Lancet. Against this backdrop, Bradbury and colleagues were comparing
Latest updates

Efforts to move towards routine patch closure or eversion endarterectomy among all carotid surgeons

A NATIONWIDE COHORT study of over 9,000 patients shows that the “controversial” practice of arteriotomy closure for carotid endarterectomy (CEA) is associated with an increased risk of ipsilateral stroke and “should be avoided”. Instead, authors Magnus Jonsson (Karolinska University Hospital, Stockholm, Sweden) and colleagues argue, endarterectomy should be performed with either routine patch closure or using the eversion technique. Despite these findings, the authors underline the fact that primary closure “remains common practice” among some surgeons.
The study—recently published as an Editor’s Choice paper in the European Journal of Vascular and Endovascular Surgery (EJVES)— also shows that the long-term durability of different patch materials is equivalent, and that bovine pericardium and eversion have a lower risk of late infections.

Jonsson et al note in their introduction that current European guidelines recommend both eversion CEA and conventional CEA with routine patch closure, rather than routine primary closure. However, they add, “many surgeons prefer selective patching and there remains much controversy about the relative benefits of the different surgical techniques and patches for CEA”.
The aim of the present study was to evaluate the short- and longterm outcomes after CEA based on surgical technique and patch material.
The investigators detail that there are several available patch types on the market at present. “Dacron, vein and polytetrafluoroethylene (PTFE)



Continued on page 3
Continued on page 2
June 2023 / Issue 98 www.vascularnews.com
“warranted”
16 Profile Rachel Bell
9 Antithrombotic guidelines Key takeaways
14 Bioresorbable stents
The CX audience has its say
Featured in this issue:
25 Transcarotid artery revascularisation
It is very, very crucial that whatever you do first, it does not have to be the last word—” Roger Greenhalgh
First results of BASIL-2 randomised controlled trial revealed at CX 2023
CAROTID
69% of the CX 2023 audience agreed: bioresorbable wins
Hanaa Dakour-Aridi S Keisin Wang
Continued from page 1
effectiveness of a vein bypass-first with a best endovascular treatment-first revascularisation strategy in terms of preventing major amputation and death in patients with CLTI.

“It is important to emphasise that the best way of analysing this trial, which is the way our statistical colleagues have done it, is on the intention-to-treat population; however, for completeness they have done some sensitivity analyses, and this includes a per protocol analysis, which includes only patients who were adherent— that is, they received the allocated intervention they were randomised to,” Bradbury explained at CX. “They also performed an as-treated analysis, which is based upon the first revascularisation that the patient actually received following randomisation, and as you can see here they both trend towards reduced amputation-free survival in the vein bypass-first group.”
The BASIL-2 co-investigators, namely Catherine Moakes, Gareth Bate and Matthew Popplewell (all University of Birmingham, Birmingham, UK) and Lewis Meecham (University Hospital Cardiff, Cardiff, UK) also presented during the session on the journey from BASIL-1 to BASIL-2, a hypothesis-generating prospective cohort study, methodology, study limitations and future work, among other topics.
BASIL-2 was an open-label, pragmatic, multicentre, phase 3, randomised trial performed at 41 vascular surgery units in three countries: the UK (n=39), Sweden (n=1) and Denmark (n=1). The central site was the University of Birmingham. “Eligible patients were those who presented to hospital-based vascular surgery units with [CLTI] due to atherosclerotic disease and who required an infrapopliteal, with or without an additional more proximal infrainguinal, revascularisation procedure to restore limb perfusion,” they state in The Lancet
Bradbury and colleagues randomly assigned participants
1:1 to receive either vein bypass or best endovascular treatment as their first revascularisation procedure through a secure online randomisation system. The Lancet paper details that participants were excluded if they had ischaemic pain or tissue loss considered not to be primarily due to atherosclerotic PAD. Most vein bypasses used the great saphenous vein and originated from the common or superficial femoral arteries, the authors communicate, while most endovascular interventions comprised plain balloon angioplasty with selective use of plain or drug-eluting stents. Patients were followed up for a minimum of two years, Bradbury et al write, with data collected locally at participating centres.
The primary outcome of amputation-free survival was defined as time to first major (above the ankle) amputation or death from any cause measured in the intention-to-treat population. Safety was assessed by monitoring serious adverse events up to 30 days after first revascularisation.
Between 22 July 2014 and 30 November 2020, the trialists enrolled and randomised 345 patients with CLTI— 65 (19%) women and 280 (81%) men with a median age of 72.5 years (62.7–79.3). The patients were randomly assigned to either the vein bypass group (172 [50%]) or the best endovascular treatment group (173 [50%]).
Bradbury detailed at CX that major amputation or death occurred in 108 (63%) of 172 patients in the vein bypass group and 92 (53%) of 173 patients in the best endovascular treatment group. The relevant mortality numbers were 91 (63%) among the vein bypass group and 77 (53%) in the endovascular arm.
In both groups, the authors write, the most common causes of morbidity and death— including that occurring within 30 days of their first revascularisation—were cardiovascular (61 deaths in the vein bypass group and 49 in the best endovascular treatment group) and respiratory events (25 deaths in the vein bypass group and 23 in the best endovascular treatment group). They add that the number of cardiovascular and respiratory deaths were not mutually exclusive.
“A trial of two strategies”
During discussion time, moderator Andrew Holden (Auckland City Hospital, Auckland, New Zealand) asked Bradbury and colleagues whether they had noted a significant change in endovascular practice in the period between BASIL-2 and its eponymous predecessor. Bradbury noted in his interpretation of the data that “there is a much greater willingness now that if you do an endo[vascular], and you are not happy with it, the interventional radiologists will go back and have another go, whereas what we tended to see, I think, in BASIL-1, was that if endo[vascular] did not work, [treatment would] quickly go over to bypass. I think that is the difference.”
Moderator Dittmar Böckler (Heidelberg University Hospital, Heidelberg, Germany) urged the audience to keep in mind the various options that remain open when undertaking an endovascular-first approach. Greenhalgh underscored the point. “It also came out with BEST-CLI that the quality of the vein is important,” he said. “It is very, very crucial that whatever you do first, it does not have to be the last word.” Böckler said vascular specialists “need to learn from this trial which patient deserves which treatment”. It is not a case of surgery versus endovascular therapy, but rather a case of learning from the data, he added. Bradbury concurred. “It is a trial of two strategies,” he said. “That was what BASIL-1 was. It is quite a difficult concept to get across. We are not comparing a vein bypass with an endovascular treatment. We are in a sense—but what we are saying is, ‘What do you do first?’ If you have got equipoise, if you are really on the fence, and you do not know which to do, this trial suggests fairly strongly, I would suggest, that in this subgroup of patients, that you should go endo[vascular] first.”
in brief
latest stories from the vascular world
n PERIPHERAL ARTERIAL DISEASE:
A recent proposal has called for “wholeperson, multidisciplinary interventions” after an interrogation of the interplay between lower extremity peripheral arterial disease (PAD) and mental health impacts. Published in the Journal of the American College of Cardiology, Kim G Smolderen (New Haven, USA) and colleagues have put forward a “biopsychosocial” PAD roadmap, offering solutions to current care “obstacles” to better attend to both behavioural and social health needs throughout vascular treatment. For more on this story go to page 6.
n ANTITHROMBOTIC GUIDELINES: Chris Twine (Bristol, UK) and Stavros Kakkos (Patras, Greece), respectively chair and co-chair of new European Society for Vascular Surgery (ESVS) guidelines on antithrombotic therapy for vascular diseases, outline key points and unanswered questions from the document which they say represents an “important milestone” in the field.
For more on this story go to page 9.
n CAROTID STENTING:
A debate at the 2023 Charing Cross (CX) International Symposium (25–27 April, London, UK) between two prominent carotid interventionists—Peter Schneider (San Francisco, USA) and Domenico Valenti (London, UK)—revealed that the vascular community is currently divided over the benefits of transcarotid artery revascularisation, as compared to percutaneous carotid artery stenting.

For more on this story go to page 24.
Editor-in-chief: Roger Greenhalgh | Publisher: Roger Greenhalgh | Content Director: Urmila Kerslake
Editor: Jocelyn Hudson Jocelyn@bibamedical.com | Editorial contribution: Jamie Bell, Will Date, Bryan Kay, Éva Malpass, Benjamin Roche and Clare Tierney


Design: Terry Hawes, Wes Mitchell and David Reekie
Advertising: Shilpa Suthar shilpa@bibamedical.com
Subscriptions: subscriptions@bibamedical.com
June 2023 | Issue98 2 VascularNews linkedin.com/company/Vascular-news @VascularNews Published by: BIBA News, which is a subsidiary of BIBA Medical Ltd | BIBA Medical, Europe, 526 Fulham Road, Fulham, London, SW6 5NR, United Kingdom Tel: +44 (0) 20 7736 8788 BIBA Medical, North America, 155 North Wacker Drive, Suite 4250, Chicago, IL 60606, United States Tel: +1 708-770-7323 Printed by: Buxton Press Reprint requests and all correspondence regarding the newspaper should be addressed to the editor at the United Kingdom address. © BIBA Medical Ltd, 2023. All rights reserved. If you have comments on this issue or suggestions for upcoming editions write to jocelyn@bibamedical.com
News
The
Randomised Controlled Trial
COVER STORY continued
First results of BASIL-2 randomised controlled trial revealed at CX 2023
Continued from page 1
have been used for a long time,” they state, adding that bovine pericardium has been used in more recent years. “Bovine pericardium may have the advantage of greater resistance to late infections and smaller haematomas than other patch types, but there are few long-term follow-up studies comparing pericardium with other patch materials,” the authors comment.
The researchers conducted a registry-based study on all primary CEAs performed for symptomatic carotid artery stenosis in Sweden from July 2008 to December 2019, which numbered 9,205 in total. This was cross-linked with data from the Swedish stroke registry, Riksstroke, and a chart review for evaluation of any events occurring during followup, they detail. The primary endpoint
was ipsilateral stroke <30 days and secondary endpoints included reoperations due to neck haematoma and <30-day ipsilateral stroke, >30-day ipsilateral stroke, all stroke >30 days and all-cause mortality.
Reporting the results of their study in EJVES, Jonsson and colleagues reveal that 2,495 patients underwent eversion CEA and 6,710 conventional CEA for symptomatic carotid stenosis. They found that the most commonly used patch material was Dacron (n=3,921), followed by PTFE (n=588) and bovine pericardium (n=413).
Furthermore, Jonsson et al relay that a total of 1,788 patients underwent conventional CEA with primary closure, and that 273 patients (3%) had a stroke within 30 days of intervention.
They also share the finding that that primary closure was associated with an increased risk of ipsilateral stroke and stroke or death within 30 days: odds ratio 1.7 (95% confidence interval [CI] 1.2–2.4, p=0.002); and 1.5 (95% CI 1.2–2), respectively. During follow-up, which was a median of 4.2 years, the investigators report that 592 patients had any form of stroke and 1,492 died. “There was no significant difference in long-term risk of ipsilateral stroke, all stroke or death depending on surgical technique or patch material,” the authors communicate.
“There was an increased risk of ipsilateral stroke <30 days in patients operated on with primary closure compared with eversion CEA and patch angioplasty,” Jonsson and colleagues summarise in their conclusion, adding that there was no difference between primary closure, different patch types or eversion after the perioperative phase.
Strengths and weaknesses
In the discussion of their findings, the authors stress that the results of their study “should be interpreted within the context of the strengths and limitations associated with retrospective analysis of prospectively collected registry data”. Focusing first on the latter, they note that “the high validity” of the Swedevasc registry— with its almost 100% coverage for all carotid procedures performed in Sweden—and the possibility for cross-linkage of data based on unique personal identifiers to assess long-term survival and stroke outcome “result in high generalisability and low loss to follow-up in this study”.
On the other hand, given the study assessed carotid procedures performed over a 10-year period, Jonsson and colleagues acknowledge that “changes in practice over time may be a confounder affecting results for factors not captured by the registry”. The
Study finds no correlation between TEVAR timing and uncomplicated type B aortic dissection outcomes
With proper patient selection, short-term outcomes of thoracic endovascular aortic repair (TEVAR) in acute uncomplicated acute type B aortic dissection (uTBAD) are similar irrespective of the timing of treatment after dissection. This is according to a study recently published in the Journal of Vascular Surgery (JVS).
Authors Adam W Beck (University of Alabama at Birmingham, Birmingham, USA) and colleagues write in their introduction that the timing of TEVAR after the onset of uTBAD “remains controversial”. The objective of the present study, against this backdrop of contention, was to evaluate the Society for Vascular Surgery (SVS) Vascular Quality Initiative (VQI) post-approval study (VQI PAS) data for the impact of TEVAR timing for uTBAD on early and late outcomes. These included mortality, procedural complications, and long-term reintervention.

The investigators note that the VQI PAS used for this analysis includes a total of 606 patients. Those patients with uTBAD—who were defined as those without rupture or malperfusion—exclusive of cases categorised as emergency (n=206), were divided into groups defined by the SVS/Society of Thoracic Surgeons reporting guidelines based on the timing of treatment after the onset of dissection. The three groups were: treatment within 24 hours (n=8), between one and 14 days (n=121) and between 15 and 90 days (n=77). The researchers used univariate and multivariable analysis to determine differences
between timing groups for postoperative mortality, inhospital complications and reintervention.
Demographics and comorbid conditions were “very similar” across the three TEVAR timing groups, Beck et al detail. The authors state that there were some “notable differences” between the groups, including higher prevalence of baseline elevated creatinine (>1.8mg/dL)/chronic end-stage renal disease and designation as ‘urgent’ in the <24-hour group, as well as a higher rate of preoperative ß-blocker therapy in the one- to 14-day group.
The authors report that postoperative stroke, congestive heart failure and renal ischaemia were

authors elaborate that this may include changes in medical management of patients prior to surgery—including preoperative thrombolysis or antiplatelet therapy—as well as changes in periprocedural routines, such as use of different techniques for cerebral monitoring during carotid surgery.
In addition, the researchers recognise that the Swedevasc registry did not include data on arteriotomy length, width of internal carotid artery, type of anaesthesia and intracerebral vessel, and as a result, “these variables were not corrected for”.
Primary closure “remains common practice” by some Considering the wider importance of their research, the authors write that their study “underlines the variation in surgical techniques used for CEA in Sweden,” underscoring the fact that up to 20% are operated on with primary closure without patch.
Jonsson et al reiterate in their conclusion that, due to its association with an increased risk of postprocedural stroke, the technique “should not be used”. In addition, they note the current report underlines the fact that selective primary closure “remains common practice” by some surgeons, and stress that “further educational efforts to move towards routine patch closure or eversion endarterectomy among all carotid surgeons are warranted”.
more common in the <24-hour group without an increase in mortality.
Unadjusted 30-day mortality across the groups, they continue, was lowest in the early TEVAR group (0%, 3.3% and 5.2%; p=0.68), as was the one-year mortality (0%, 8.3% and 18.2%; p=0.06). However, they add the caveat that these results were not statistically different at any time point.
Furthermore, Beck and colleagues reveal that reintervention out to three years was not different between the groups, and that multivariable analysis demonstrated the need for a postoperative therapeutic lumbar drain to be the only predictive risk factor for mortality (hazard ratio=7.595, 95% confidence interval: 1.73–33.337, p=0.007).
In the conclusion of their study, Beck et al acknowledge that patients with uTBAD treated within 24 hours were unusual (n=8) and the group was “too small for valid statistical comparison”. They add that these patients “likely represent a high-risk subgroup, which is manifested in a higher risk of complications”.
Although there was a “trend” toward improved survival in the acute (one- to 14-day) phase, the researchers summarise that outcomes did not differ compared with the subacute (15- to 90-day) phase with relation to early mortality, postoperative complications, or one-year survival. They state in closing: “These data suggest that the proper selection of patients for early TEVAR can result in equivalent survival and early outcomes.”
3 Issue98 | June 2023 Journal Highlights
These data suggest that the proper selection of patients for early TEVAR can result in equivalent survival and early outcomes.”
Efforts to move towards routine patch closure or eversion endarterectomy among all carotid surgeons “warranted”
CAROTID
Adam W Beck









*Available for US and EU readers only **Available worldwide A trusted provider of latest news, review of cutting-edge research, congress coverage and opinion from thought leaders A specialised news source in the interventional field Editorially independent Visit interventionalnews.com and click ‘Subscriptions’ for complimentary print subscription* and e-newsletter subscription** Subscribe today Available in print and digital formats and through our social channels
CX juxtarenal aortic session brings new stenting data to light
A series of first-to-podium presentations at the 2023 Charing Cross (CX) International Symposium (25–27 April, London, UK) offered new data on balloon-expandable bridging covered stents and self-expanding grafts, as well as the role of covered stents in the treatment in chronic mesenteric ischaemia (CMI). Before that, however, was a presentation on the Advanta V12 balloon-expandable covered stent (Getinge).
IN A REVIEW OF 20 YEARS OF concerning renal arteries, which were 98.2±0.5% at eight years for fenestrations and 77.3±5.9% at eight years for branches.
Concluding, Verhoeven made clear that despite disparities in the data, Advanta V12 has persisted as an invaluable device, which has provided “excellent” handling and flaring over the course of 20-plus years of use. Placing emphasis on the long-term patency rates that have made the Advanta V12 an invaluable tool within F/BEVAR, Verhoeven finally alluded to its steadfast place within the future of treatment.
Bridging covered stents and self-expanding grafts “similar” on primary patency Konstantinos Spanos (University of Thessaly, Larissa, Greece) presented meta-analysis data of comparative studies evaluating the balloon-expandable bridging covered stent versus the selfexpanding stent graft for BEVAR, also in a first-to-podium presentation
at CX. The findings showed that balloon-expandable stent grafts and self-expandable stent grafts perform “similarly” when compared via primary patency and branch-related endoleak during mid-term follow-up.
Addressing the audience, Spanos explained that currently available stent grafts— bridging covered stents or self-expanding grafts—are not originally designed as bridging stents for complex aortic repair with branched devices. Continuing, he outlined that the aim of the current review was to evaluate the impact of each type of bridging stent graft on target vessel outcomes during the mid-term followup after BEVAR.
In total, Spanos stated, 96% of target vessels remained patent using bridging covered stents and 97% using selfexpanding grafts, and he added the overall pooled primary patency rate did not differ between groups. Concerning revascularisation, Spanos also asserted that no significant differences were found between the two groups, showing 97% for bridging covered stents and 99% for selfexpanding grafts, respectively.
Of note however, Spanos confirmed that the researchers found a lower risk for target vessel instability using self-expanding stent grafts during revascularisation when compared to bridging covered stents, which he defined as any death or rupture related to a side branch complication.
Concluding his presentation, Spanos conveyed that although the performance of bridging covered stents versus self-expanding stent grafts was similar, current data from retrospective
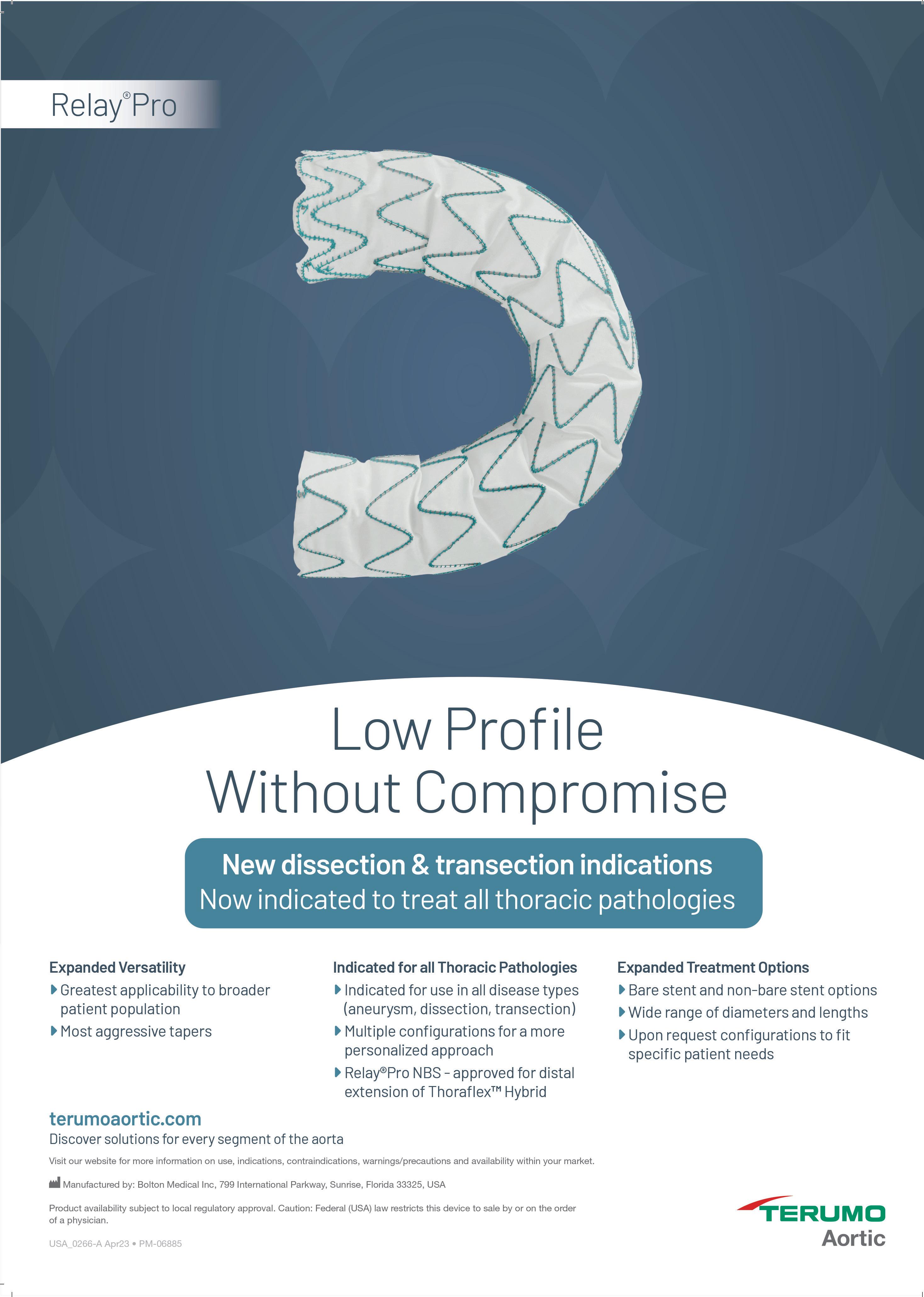
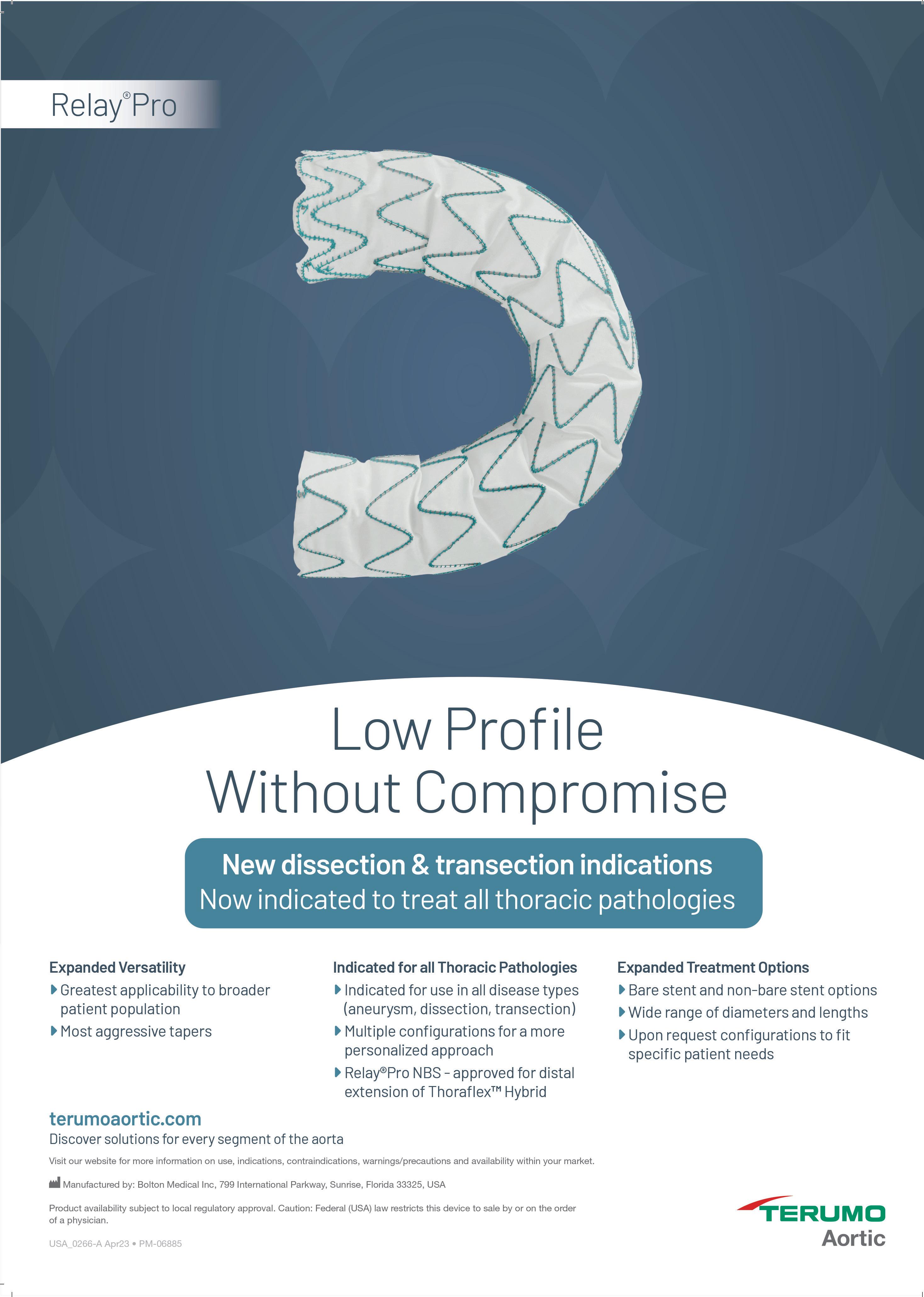
Terumo Aortic announces FDA approval of dissection and transection indication expansion for the RelayPro stent graft



The Pro-D study was a prospective, multicentre pivotal trial conducted in 22 US centres and enrolled 56 patients with acute, complicated type B aortic dissection. Approximately two thirds of the subjects had dissection extension to the iliac arteries. The primary endpoint of all-cause mortality at 30 days was 1.8% and demonstrated a clear early survival benefit. Patients will be followed for five years.
studies suggest that overall target vessel instability and reintervention rates are favourable for self-expanding grafts as bridging stent grafts in BEVAR. Finally, however, Spanos remarked that further research in the form of randomised controlled trials may be needed in this area.
Covered stents “should be preferred” in chronic mesenteric ischaemia
The juxtarenal aortic session on bridging stents offered further salient conclusions to the CX audience, through Luke Terlouw’s (Erasmus MC University Medical Center, Rotterdam, The Netherlands) presentation of longterm results of a randomised controlled trial comparing covered with baremetal stenting of the mesenteric arteries in patients with CMI.
Terlouw described the details of the multicentre patient- and investigator-blinded trial, noting that the study included patients undergoing endovascular treatment of atherosclerotic CMI with a stenosis length of <25mm.
He defined their primary endpoint as 24-month primary patency and specified subsequent patency loss to be luminal surface area reduction ≥75% or performance of a reintervention to maintain patency. Patency was assessed by two interventional radiologists with 15 and 19 years of experience.
Presenting the conclusive findings, Terlouw confirmed that, considering the follow-up data show “significantly” better primary patency and lower reintervention rates, the covered stent should be regarded as the preferred stent when treating patients with atherosclerotic CMI.
study which will be published soon now that approval of this new generation device has been granted; also, it is heartening that our dissection patients will have this additional option.”
The Pro-T study was a prospective, multicentre pivotal study that enrolled 50 patients in 16 US centres. The purpose of the study was to assess the performance of RelayPro for the treatment of transection. The primary endpoint of the trial was allcause mortality at 30 days with follow-up continuing for five years.
for all pathologies of the descending thoracic artery; aneurysm, penetrating atherosclerotic ulcers, transection and dissection. RelayPro offers unparalleled accuracy, proven efficacy and durability as well as the widest range of sizes, tapering and configurations on the market, designed to expand the treatment of thoracic endovascular aortic repair (TEVAR) to patients with smaller access vessels, the release continues.
This approval follows the results from recent studies on RelayPro dissection (RelayPro-D) and RelayPro traumatic injury (RelayPro-T).
National principal investigator of the Pro-D study, Peter Rossi (Medical College of Wisconsin, Milwaukee, USA), said: “The fully covered, non-bare stent (NBS) configuration of RelayPro was most used in the pivotal trial, highlighting the clinical value of this platform, and a full 86% of procedures were percutaneous. I am very encouraged by the one-year outcomes of this pivotal

National principal investigator of the Pro-T study, Benjamin W Starnes (University of Washington, Seattle, USA), commented: “We are looking forward to having this latest-generation device available for all thoracic indications. A low-profile device will be particularly useful for trauma patients who are typically younger and with smaller access vessels. Eighty per cent of the procedures in this study were percutaneous, highlighting a distinct value of the RelayPro stent graft system.”
The approval of RelayPro-T also introduces a 22mm diameter option. The RelayPro thoracic stent graft received CE mark approval in 2017 and FDA approval in 2021 for the treatment of patients with thoracic aortic aneurysms (TAA) and penetrating atherosclerotic ulcers (PAUs).
5 June 2023 Device Updates
Advanta V12
For the treatment of juxtarenal aortic aneurysms, reinterventions after physician-modified endovascular grafts (PMEGs) are nondetrimental to long-term survival. This is one of the main findings of a recently published study by Ayumi Tachida (University of Washington School of Medicine, Seattle, USA) and colleagues.
THE AUTHORS NOTE IN THEIR Journal of Vascular Surgery (JVS) paper that the frequency and impact of reintervention on mortality after PMEGs in unknown. It was the aim of the present study, therefore, to describe reinterventions after PMEG for the treatment of juxtarenal aneurysms and their effect on survival.
Tachida et al used 11 years’ worth of data (2011–2022) from a prospective investigational device exemption clinical trial in their study. The trial in question—officially titled ‘Physicianmodified endovascular grafts for the treatment of elective, symptomatic or ruptured juxtarenal aortic aneurysm: an investigator-initiated study’—is being led by Benjamin Starnes (University of Washington, Seattle, USA), who is also a co-author of the JVS paper.
The trial aims to enrol 300 participants with an estimated
completion date of January 2035.
On the Clinical Trials webpage for the study, it is mentioned that not all patients presenting with symptomatic or ruptured aortic aneurysms are candidates for endovascular repair, with the reasons for exclusion noted to predominantly involve a lack of a suitable proximal aortic neck.
“Solutions to this problem involve multi-branched or ‘fenestrated’ endografts, which are being assessed in other clinical trials,” the study description continues. However, it is highlighted that grafts in these trials require between six and 12 weeks to manufacture and deliver to the investigational site.
New “biopsychosocial” roadmap set out to address PAD treatment and mental health impacts
A RECENT PROPOSAL HAS CALLED FOR “whole-person, multidisciplinary interventions” after an interrogation of the interplay between lower extremity peripheral arterial disease (PAD) and mental health impacts. Published in the Journal of the American College of Cardiology, Kim G Smolderen, clinical psychologist, and Carlos Mena-Hurtado, interventional cardiologist (Yale University, New Haven, USA) et al have put forward a “biopsychosocial” PAD management roadmap, offering solutions to current care “obstacles” to better attend to both behavioural and social health needs throughout vascular treatment.
The “PAD experience,” including the clinical and financial burden of the comorbid conditions linked with PAD, have received “little consideration,” Smolderen and Mena, who are founders of the Vascular medicine outcomes (VAMOS) lab at Yale, et al opine. This lack is driving the need to “expand the PAD care paradigm” to a biopsychosocial one which acknowledges the contribution of both behaviour and psychosocial factors on disease management and outcomes. Their roadmap identifies four domains that, once addressed, can redesign vascular specialty care services to attend to the behavioural and social health needs of all patients.
Identifying first a “fundamental problem” in the way physical and mental health are divided when providing care, the authors pinpoint the “major advocacy efforts” that are needed across professional organisations
“We seek to evaluate the safety and efficacy of PMEG using a US Food and Drug Administration [FDA]-approved, off-the-shelf device in order to increase the applicability of these technologies to more patients and thus save more lives,” the description reads.
In the study reported in JVS, reinterventions after PMEG were categorised as open or percutaneous and major or minor by Society for Vascular Surgery reporting standards according to high or low magnitude based on physiological impact. The investigators also categorised reinterventions by timing, as well as those interventions which occurred within one week of PMEG. They compared survival between patients who did and did not undergo reintervention and between reintervention subcategories.
Communicating their findings, Tachida and colleagues relay that a total of 170 patients underwent PMEG in the 11-year study time period, 50 (29%) of whom underwent a total of 91 reinterventions (mean reinterventions/ patient, 1.8). They report that freedom from reintervention was 84% at one year and 60% at five years. The authors specify that reinterventions were most often percutaneous (80%), minor (55%) and low magnitude (77%), with the most common reintervention being renal stenting (26%). They also note
that there were 10 early reinterventions within one week of PMEG and that two aortic-related mortalities occurred after reintervention.
There were no differences in survival between patients who underwent reintervention and those who did not, Tachida et al also communicate in the results section of the paper. However, they continue, survival differed based on the timing of reintervention.
Tachida and colleagues further share that, after adjusted analysis, reintervention within one week of PMEG was associated with an increased risk of mortality both compared with late reintervention (hazard ratio [HR], 11.1; 95% confidence interval [CI], 2.7–46.5) and no reintervention (HR, 5.2; 95% CI, 1.6–16.8).
In their conclusion, Tachida et al summarise: “Reinterventions after PMEG were most commonly associated with percutaneous, minor and low magnitude procedures, and [were] non-detrimental to long-term survival.” However, they note that early reinterventions were associated with increased mortality risk.


“These data suggest that a modest frequency of reinterventions should be expected after PMEG, emphasising the critical importance of lifelong surveillance,” the authors state in their closing remarks.
A total of 170 patients underwent PMEG in the 11-year study time period
serving populations of PAD patients. Their recommendations begin at trainee level, defining “core competencies” which reduce stigma and “unawareness” around mental illness and its effects on PAD.
Second, they outline the evolution of highly technological and procedural care which has been “valued disproportionately” over preventative and psychosocial care in the context of reimbursement and code availability—which the authors note are both presently absent from cardiovascular speciality care. To rectify this, they believe payment reform is needed, allowing for “codes and compensation for integrated care models” which should be piloted to integrate quality metrics of care delivery, including mental health screening and treatment tracking in such a manner to affect payment of services.
Thirdly, Smolderen, Mena and colleagues emphasise that despite several evidence-based interventions stemming from high-level randomised controlled trial evidence across cardiovascular populations, there is a prevalent “lack of awareness” among health administrators regarding the “scope of practice” of allied mental and behavioural health physicians in the context of chronic disease. They believe adopting a formal approach to assessing behavioural health could be a solution for this, assigning “routine components of care” and “expanding system capacity to address health disparities and behavioural health conditions”.
As an extension of their solution, they assert that “interprofessional team-based training” that promotes “a climate of mutual respect and shared values, moving away from a hierarchical system of care delivery and delineating roles” be established. Furthermore, Smolderen, Mena et al state that investments in
programme building and co-ordination for vascular patients must be made, as well as the promotion of integrated care for diverse and uninsured populations, to “broaden access” and remove barriers to PAD care. Their fourth and final area of proposed reform concerns integrated behavioural care practice guidelines for PAD management, and the formation of better evidence-based workflows derived from comparative effectiveness and implementation research— which they currently believe to be “lacking”.
“Funding budgets for research,” the authors state, “is needed to generate evidence for implementation models of integrated care delivery, tailored to the PAD context”. Smolderen, Mena et al conclude that research is needed to address “clinical, operational and financial” outcomes— which includes decreased cost of care for comorbid patients—relevant to multiple stakeholders. To this end, they believe quality efforts at a national level will help to “benchmark data” for PAD care, “integrating social determinants of health, and tracking the use of integrated care services for vascular populations”.
6 June 2023 | Issue98 Journal Highlights
The substantial societal cost of healthcare for patients with PAD […] requires a broader perspective of PAD care.”
Reinterventions after physician-modified endovascular grafts
“non-detrimental” to long-term survival
Kim Smolderen Carlos Mena-Hurtado








*Available for US and EU readers only **Available worldwide Visit renalinterventions.net and click ‘Subscriptions’ for complimentary print subscription* and e-newsletter subscription** Subscribe today Available in print and digital formats and through our social channels A trusted provider of latest news, review of cutting-edge research, congress coverage and opinion from thought leaders A specialised news source in the field of renal disease management Editorially independent
Chris Twine Stavros Kakkos
Point of View
Chris Twine and Stavros Kakkos, respectively chair and cochair of new guidelines on antithrombotic therapy for vascular diseases, outline key points and unanswered questions from the document which they say represents an “important milestone” in the field.
The European Society for Vascular Surgery (ESVS) is publishing its first guideline on antithrombotic therapy for people with vascular diseases in the May issue of the European Journal of Vascular and Endovascular Surgery (EJVES).1 The guideline covers many topics and conditions including antithrombotics for patients with acute and chronic arterial and venous diseases and interventions.
Three new studies were performed for the guideline; a risk score for predicting bleeding risk in patients with peripheral arterial disease (PAD; the OAC3-PAD score which needs validating)2 and two systematic reviews; one on platelet function testing (high on treatment platelet reactivity) for patients undergoing endovascular arterial intervention3 and one on antithrombotics for patients with abdominal aortic aneurysm (AAA).4 A Cochrane review was updated to aid recommendations on antithrombotics
for patients with dialysis access.5
Some of the key points of the guideline are updated recommendations based on the publication of new trials. Both COMPASS6 and VOYAGER7 feature heavily in the PAD recommendations. Some of these recommendations were difficult to formulate, for example how do you give clinical recommendations as to when to use clopidogrel or aspirin plus rivaroxaban for patients with chronic symptomatic lower extremity arterial disease (LEAD) when there are no comparative data? A network metaanalysis found no clear difference between the two combinations, but these have to compare very different trial populations so have questionable validity.8 Clopidogrel alone, or aspirin plus rivaroxaban for chronic symptomatic LEAD now have IIa recommendations for use.1

Another difficult question is around the antithrombic choices after endovascular intervention for LEAD. We know aspirin plus clopidogrel are used commonly despite a lack of evidence,9 and now we also have aspirin plus rivaroxaban as a choice. The endovascular subgroup in VOYAGER did not reach significance, but is it fair to consider this unpowered
subgroup separate to the whole trial? In the end the whole trial results were considered, so aspirin plus rivaroxaban has a IIa recommendation. Dual antiplatelet therapy with aspirin plus clopidogrel had to be IIb because of the lack of evidence supporting its use, even if this is clinically widespread.9 We had to update older ESVS guideline recommendations, sometimes with minimal new data so that older recommendations do not clash with the new.
Contemporary treatment of deep vein thrombosis (DVT) with a direct oral anticoagulant (DOAC) agent, as opposed to a vitamin K antagonist, was recommended. However, for patients with unprovoked DVT requiring extended anticoagulation, a reduced dose of apixaban or rivaroxaban was suggested. Both recommendations were based on reduced bleeding rates with DOACs. Patients with cancerassociated venous thromboembolism are recommended to receive low molecular weight heparin (LMWH), but those with a low risk of gastrointestinal or genitourinary bleeding are now recommended to be considered for anticoagulation with a DOAC, preferably apixaban, alternatively rivaroxaban or edoxaban.
Superficial vein thrombosis is mostly treated with prophylactic doses of fondaparinux for 45 days based on the large CALISTO trial, with a LMWH or oral rivaroxaban being an alternative. Anticoagulation following intervention for DVT is given at least as long as standard treatment to prevent recurrent thromboembolic events, while for chronic obstructive lesions, an individualised approach is suggested. The risk of the patient bleeding must always be considered when making decisions on antithrombotic therapy. The challenge for recommendations was that there is no validated way of doing this for populations with arterial disease. Members of the guideline writing committee have started the process of trying to measure this risk for patients with PAD with a new scoring system, but it will be some time before it can be validated.2 Until then we have formulated recommendations to try and help clinicians think about and potentially reduce individual bleeding risk (for example use of proton pump inhibitors for patients at higher
risk of bleeding), especially when using anticoagulants or dual antiplatelet therapy.
There are still many unanswered questions including the role of platelet function testing, antithrombotics following endovascular intervention and for patients with AAA, and antithrombotics for patients with certain presentations of superficial venous thrombosis or undergoing deep venous intervention. We hope the guideline will provide useful day-to-day guidance for clinicians and will be an important milestone in reinforcing the significance of medcial therapy alongside interventions for our patients.
References:
1. Twine CP, Kakkos S, Aboyans V, Baumgartner I, Behrendt CA, Bellmunt-Montoya S, et al. European Society for Vascular Surgery (ESVS) 2023 Clinical Practice Guidelines on Antithrombotic Therapy for Vascular Diseases. Eur J Vasc Endovasc Surg 2023.
2. Behrendt CA, Kreutzburg T, Nordanstig J, Twine CP, Marschall U, Kakkos S, et al. The OAC3-PAD risk score predicts major bleeding events at one year after hospitalisation for peripheral artery disease. Eur J Vasc Endovasc Surg. 2022;63:50310.
3. Zlatanovic P, Wong KHF, Kakkos SK and Twine CP. A Systematic Review and Meta-Analysis on the Impact of High On-Treatment Platelet Reactivity on Clinical Outcomes for Patients Taking ADP Receptor Inhibitors Following Lower Limb Arterial Endovascular Intervention. Eur J Vasc Endovasc Surg. 2022;63:91-101.
4. Wong KHF, Zlatanovic P, Bosanquet DC, Saratzis A, Kakkos S, Aboyans V, et al. Antithrombotic therapy for aortic and peripheral artery aneurysms: a systematic review and meta-analysis. Eur J Vasc Endovasc Surg. 2022;64:544-556.
5. Mohamed I, Kamarizan MFA and Da Silva A. Medical adjuvant treatment to increase patency of arteriovenous fistulae and grafts. Cochrane Database Syst Rev. 2021;7:Cd002786.

6. Anand SS, Bosch J, Eikelboom JW, Connolly SJ, Diaz R, Widimsky P, et al. Rivaroxaban with or without aspirin in patients with stable peripheral or carotid artery disease: an international, randomised, double-blind, placebo-controlled trial. Lancet. 2018;391:219-229.
7. Bonaca MP, Bauersachs RM, Anand SS, Debus ES, Nehler MR, Patel MR, et al. Rivaroxaban in Peripheral Artery Disease after Revascularization. N Engl J Med. 2020;382:1994-2004.
8. Ambler GK, Nordanstig J, Behrendt CA and Twine CP. Network Meta-analysis of the Benefit of Aspirin with Rivaroxaban vs. Clopidogrel for Patients with Stable Symptomatic Lower Extremity Arterial Disease. Eur J Vasc Endovasc Surg. 2021;62:654655.
9. Wong KHF, Bosanquet DC, Ambler GK, Qureshi MI, Hinchliffe RJ and Twine CP. The CLEAR (Considering Leading Experts’ Antithrombotic Regimes around peripheral angioplasty) survey: an international perspective on antiplatelet and anticoagulant practice for peripheral arterial endovascular intervention. CVIR Endovasc 2019;2:37.
Chris Twine is a vascular surgeon at North Bristol NHS Trust in Bristol, UK.

Stavros Kakkos is a professor of vascular surgery at the University of Patras in Patras, Greece.

9 Issue98 | June 2023 Antithrombotic Therapy
New guidelines on antithrombotic therapy for vascular disease represent important milestone
We hope the guideline will provide useful day-today guidance for clinicians and will be an important milestone in reinforcing the significance of medical therapy alongside interventions for our patients.”
National study finds no support for highintensity statin treatment after AAA repair
Statin treatment after aortic repair is associated with improved long-term survival, while dose does not matter. This was the key message from a first-to-podium presentation delivered by Kevin Mani (Uppsala University, Uppsala, Sweden) at the 2023 Charing Cross (CX) International Symposium (25–27 April, London, UK). The CX audience showed their support for this conclusion, with 89% agreeing with the statement ‘Statins save lives’ during discussion time.
Mani began by underlining the fact that abdominal aortic aneurysm (AAA) is a cardiovascular disease that shares risk factors with atherosclerotic cardiovascular disease (ASCVD). According to the American Heart Association (AHA), the presenter detailed, AAA is in fact classified as one of the ASCVDs.
“AAA patients have a higher mortality than the general population due to cardiovascular disease,” Mani noted, adding that statin treatment is associated with improved survival in patients with ASCVD.

The presenter detailed that current European Society for Vascular Surgery (ESVS) guidelines on the management of abdominal aortoiliac artery aneurysms, published in 2019, suggest that patients with AAA should have blood pressure control, statins and antiplatelet therapy. “This is a class IIa recommendation with level b evidence,” the presenter specified, which he said indicates that “probably all patients” with AAA should have statin treatment.
The AHA guidelines, Mani highlighted, split statin treatment into high dose and moderate to low dose. “The suggestion is that patients with ASCVD including those with AAA should have high-dose statin treatment,” the presenter shared with the Kensington 1 audience. “However,” he said, “the evidence for what dose should be given to AAA patients is non-existent, and the vascular surgical guidelines do not recommend a specific dose for AAA patients.”
To address this gap in the literature, Mani and
colleagues conducted a national study assessing the potential benefit of statin treatment in AAA patients and whether dose has an effect. The team used four national registries and then cross-matched these to identify all AAA repairs performed in Sweden between the years of 2006 and 2018, the presenter explained. The team then assessed statin treatment by combining patient data and the national prescribed drug registry, looking at outcomes in terms of death, cause of death and rehospitalisation, also using national registries.
Mani detailed that the researchers performed three analyses, the first looking at 90-day mortality for patients who had statin treatment preoperatively, the second assessing statin versus no statin treatment postoperatively, and the final one examining highdose versus low-to-moderate-dose statin treatment postoperatively, considering overall survival, aorticrelated survival and freedom from cardiovascular events. Propensity score matching was used to ensure that the groups were comparable in terms of baseline comorbidities and characteristics.
The presenter revealed that approximately 60% of the 11,000 patients who underwent AAA repair in the national study had statin treatment prior to undergoing repair. Postoperatively, he added, half of the patients had continuous statin treatment 80% of the time after the operation. In both instances, the rates were higher
Endurant stent graft proves efficacious and durable in ENGAGE 10-year data
A first-to-podium presentation at CX 2023 saw Hence Verhagen (Erasmus Medical Center, Rotterdam, The Netherlands) present unique 10-year data from the ENGAGE OUS registry on the Endurant abdominal aortic aneurysm (AAA) stent graft (Medtronic). “Ever since we started doing endovascular aneurysm repair (EVAR) about 30 years ago, there have been concerns about durability,” Verhagen stated at the opening of the talk. “What we have revealed is that the survival between open and endovascular patients is the same in the long term.”
VERHAGEN DIRECTED HIS
audience’s attention to previous randomised controlled trials such as EVAR1 and DREAM, which “raise[d] concern” around durability. The latter in particular showed patients in its EVAR group had “many more secondary interventions after about four years”. He also said that, though there were some other studies with long-term data (≥10 years), many of these
have “strict limitations”, leading to a “paucity of long-term data” with a large stenting sample size. The reason, he said, was the high mortality in such trials— meaning that, after 10 years, “there are not that many patients left […] You need a very large group to start off with to have survival and results after 10 years.”
Verhagen detailed
among men compared to women.
Looking at perioperative mortality, Mani reported that this was the same in the group on statin treatment versus no statin treatment and was equal for the endovascular aneurysms repair (EVAR) and open repair cohorts, with an overall 90-day mortality of just under 3%.
The presenter also shared the finding that patients on statin treatment had an improved survival in the long term, and that overall survival was “significantly improved” in a propensity score-matched group of patients with or without continuous statin treatment after AAA repair. Aortic-related survival was improved with statin treatment, he stated, as was freedom from cardiovascular events, if the patients were on statin treatment.
Finally, the team assessed the highdose statin group versus the low-tomoderate-dose group. “There was no effect of the dose of statins, neither on overall survival nor on aortic-related survival or cardiovascular events,” he communicated. “These were equal, irrespective of dose.”
“In conclusion,” the presenter summarised, “statin treatment is beneficial in AAA patients with improved long-term survival, as well as improved freedom from aortic-related complications and cardiovascular events.” However, he added the caveat that there is no support in the study for high-intensity statin treatment after AAA repair, and that perioperative mortality was not affected by statin treatment.

In subsequent discussion, panellist Janet Powell (Imperial College London, London, UK) asked whether the study results are independent of lowdensity lipoprotein (LDL) cholesterol levels. Mani responded that the team does not have such data. However, he highlighted the fact that the AHA recommendation for high-dose statins for patients with AAA below the age of 75 is irrespective of their LDL levels. “Clearly, this is an area where we need to work more on how we achieve the adequate effect of statins by looking at LDL levels,” he remarked, considering future research in this space.
that the registry included 1,260 patients from 79 sites in 30 countries. The patients initially enrolled only consented to five-year follow-up, however, which required a reconsent process for 10-year follow-up—with only 49 of the initial 79 centres agreeing. This, combined with patient refusals, reduced the total cohort for long-term results to around 390 patients. “Not surprisingly, these patients were a little younger than the original and had generally fewer comorbidities,” Verhagen added.
All-cause mortality up to 10 years was analysed, revealing a survival rate of about 42%. There was no steep decline after five years, something which also held for aneurysm-related
mortality (around 5% of patients). Reinterventions, “the Achilles’ heel of EVAR,” were also not found to accelerate after five years’ follow-up, with around 70% of patients free from secondary interventions. Stratified into groups undergoing reintervention at 0–5 years and at 6–10 years, Verhagen and colleagues found “very, very few” type 3 endoleaks “in the first seven years or so”, he stated, “with a slight increase at 10 years”.
Patients with a type 1a endoleak, Verhagen noted, increased in number by 4.1% at 10 years. Of those, however, 40% “started off with wellknown risk factors”. Clinical events were also examined, with aneurysm rupture—“the ultimate failure”— occurring “very, very little”, increasing at a rate of 1.5% at 10 years.
The take-home message, Verhagen stated, was that these were “probably unique data” up to 10 years, and that they “confirm the long-term efficacy and the durability of the Endurant stent graft with these numbers of aneurysms and mortality”. He added that “lifelong surveillance is critical for EVAR patients”.
10 June 2023 | Issue98 CX 2023
AORTIC
You need a very large group to start off with to have survival and results after 10 years.”
Kevin Mani
Hence Verhagen






Join the CX Vascular platform today to connect and engage with the global vascular community, share expertise and experiences, and stay up-to-date with the latest education and news in the vascular world. Members will also have access to exclusive content including live discussions on the latest advances in the vascular field and interviews with key thought leaders in the space. Register now Education, News, Insights Join the community at https://cxvascular.com
The Aperto® drug-coated balloon: A “first-line” treatment for arteriovenous fistula lesions
In 2023, there are a number of different options available for treating the vascular access complications of thrombosis and stenosis, Matteo Tozzi (University of Insubria, Varese, Italy) tells Vascular News. He highlights that perhaps the most useful option of all—with “fantastic outcomes” for patients—is the Aperto drug-coated balloon (DCB; Cardionovum), and considers this to be a “first-line” treatment for intimal hyperplasia in patients with an arteriovenous fistula (AVF).



THE CE-MARKED APERTO DCB, Cardionovum claims, offers a prolonged dialysis access survival. The company details that the device is a high-pressure DCB intended for the treatment of shunt stenosis. Specifically, Cardionovum notes, it is designed to protect AVFs and shunt grafts from early restenosis and to prevent and successfully dilate intimal hyperplasia.
Tozzi and colleagues in the Vascular Surgery Unit at the University of Insubria recently prepared an analysis of over 600 AVF patients who they have treated with the Aperto DCB in their centre. The analysis includes the team’s experience from 2014 to 2023 with the device. “The outcomes are better [with the Aperto DCB] compared to standard balloon angioplasty,” Tozzi reports, adding that, “for haemodialysis patients with stenosis in their vascular access, I think DCB is the better option for treatment”.




Within the patient cohort included in the analysis, Tozzi highlights that there were a large number of central vein stenosis (CVS) lesions. The associate professor of vascular surgery notes that the central
vein is a very challenging location for treatment of a stenosis and that there are likely many patients suffering with this hard-to-treat complication. In Tozzi’s opinion, the best first approach in these patients is DCB treatment. “In our cohort of patients, we treated more than 100 CVS lesions with the Aperto DCB and the results are better [than with standard balloon angioplasty],” he communicates.
Tozzi continues that around half of the patients he treats with CVS lesions undergo only one procedure within a year, elaborating that it is possible with a DCB alone to prolong the life of a patient’s access circuit and the functionality of their AVF in this period. After two years, however, he states that 40% of these patients go on to receive a stent graft, which he describes as the “second step” in the treatment of a CVS lesion when there are two or three instances of restenosis in the same time period.

He reiterates that the DCB should be viewed as
a “first-line” treatment in CVS lesions, adding the caveat that in cases of “very fast” restenosis it is possible to treat these patients with a stent graft after treatment with a DCB. However, he notes that DCB treatment is often used again in the treatment pathway. Following treatment with a stent graft, he explains, it is sometimes necessary to perform a DCB angioplasty to treat aged stenosis.
Looking ahead, Tozzi believes that in the future the use of DCBs in de novo lesions will become more prevalent. In this type of lesion, he explains, cell replication is higher and so a DCB and the paclitaxel drug “run very well”.
In addition, Tozzi points to the importance of including DCBs in the guidelines for AVF treatment in the near future. This, he believes, would increase the possibility for patients who suffer with a stenosed vascular access to be treated with this “perfect device”.
12 Advertorial June 2023 | Issue98
THIS ADVERTORIAL IS SPONSORED BY CARDIONOVUM® *Available for US and EU readers only **Available worldwide A trusted provider of latest news, review of cutting-edge research, congress coverage and opinion from thought leaders A specialised news source in the vascular arena Editorially independent Subscribe today Available in print and digital formats and through our social channels Visit vascularnews.com and click ‘Subscriptions’ for complimentary print subscription* and e-newsletter subscription**
In our cohort of patients, we treated more than 100 CVS lesions with the Aperto DCB and the results are better [than with standard balloon angioplasty].”
FDA approved
Matteo Tozzi
Not
IN.PACT AV three-year subanalysis trial data show “durable” long-term results
At the 2023 Charing Cross (CX) International Symposium (25–27 April, London, UK), Andrew Holden (Auckland City Hospital, Auckland, New Zealand) presented new data from the IN.PACT AV Access trial of the IN.PACT AV (Medtronic) drug-coated balloon (DCB). Offering three-year subanalysis data, he said that the study is “the only randomised pivotal trial of a device treating dysfunctional arteriovenous fistulas (AVFs) to demonstrate consistent and sustained clinical benefit” up to three years.
Establishing some background to the study, Holden noted that there have been eight published peer-reviewed studies with outcomes reported through to three years, but he said that all of these were single-centre with no adjudication—and that “all except one were single-arm and retrospective”. That means there is, in his words, “a paucity of evidence of long-term outcomes after treatment of stenoses in AV access”.
The IN.PACT AV study was initially planned to extend to 24 months, and a five-year extension meant a shrinking of the pool of participants as a result of death, withdrawal and declined consent to further study. In total, 133 participants completed their threeyear visit out of an original cohort of 330 patients receiving the index procedure. Of that 330, 170 were in the
IN.PACT AV arm, while 160 received percutaneous transluminal angioplasty (PTA). In the IN.PACT AV arm, the mean age was 65.8 years and 112 of 170 were male. The standard PTA arm had a mean age of 65.5 and 101/160 were male.
As presented at CX 2022 (26–28 April, London, UK), at 36 months, the DCB arm yielded a target lesion primary patency (TLPP) rate of 43.1% while the PTA arm had a rate of 28.6%, a statistically significant patency advantage for the DCB. This year, Holden set out for the first time the results of subgroup analyses in patients receiving an AVF in the forearm and upper arm at three years.
Those analyses included one in which the results were stratified by AVF type. In that analysis, the IN.PACT AV arm had a patency rate of 44.5%
PAVE 2 trial to meet need for improved evidence on drugcoated balloons
SPEAKING AT CX 2023, NARAYAN
Karunanithy (Guy’s and St Thomas’ NHS Foundation Trust, London, UK) set out “the need for more evidence” as part of a presentation on the upcoming, National Institute for Health and Care Research (NIHR)-funded, investigator-initiated PAVE 2 trial providing a comparison between multiple drug-coated balloons (DCBs) and plain-balloon angioplasty for the treatment of dysfunctional arteriovenous fistulas (AVFs) in dialysis patients.
In his presentation, Karunanithy noted that, while plain-balloon fistuloplasty continues to be the “mainstay” in dysfunctional AVF treatments, its benefits may only be short-term—with reported sixmonth primary patency rates of 60–70% decreasing to 40–50% at 12 months. Reviewing the published literature on paclitaxel-coated balloon use, the speaker reflected that discrepancies between the findings of multiple studies in this space may have been caused by differences in the choice of balloon device and drug dosage; ethnicity of participants; and proportion of prior-revascularisation patients, in each.


in forearm (radiocephalic) AVFs and 39.9% in upper arm (brachiocephalic and brachiobasilic) AVFs at 36 months, while the same rates with PTA were 33.8% and 21.3%, respectively. The patency advantage for DCB was significant for both forearm and upper arm fistulas.
The authors also stratified results by lesion type, with a DCB rate of TLPP of 50.6% at 36 months for de novo lesions and 40.5% for restenotic lesions. This was statistically superior to TLPP rates for PTA which were 42.2% and 22.7%.
Lesion location
A further subgroup analysis by lesion location focused on peri-anastomotic, cephalic arch and venous outflow lesions. For peri-anastamotic lesions, IN.PACT AV had a TLPP rate of 40.4% while PTA had a rate of 31.1% at 36 months. For cephalic arch lesions, the DCB arm saw a rate of 40.9% and the PTA arm one of 27.9%, while on venous outflow lesions the former had a rate of 45.6% and the latter of 25.5%. While patency was statistically superior at all lesion locations, the most notable effect was seen in peri-anastomotic and
Next, Karunanithy discussed emerging evidence evaluating the role of sirolimus-coated balloons, such as the MATILDA study of the MagicTouch (Concept Medical) device, which has reported target-lesion primary patency (TLPP) rates of 83% at six months and 58% at 12 months, and the ISABELLA study of the Selution DCB (MedAlliance), which found TLPP rates of 72% at six months and 44% at 12 months. Further evidence on the MagicTouch balloon is awaited from the ongoing IMPRESSION randomised controlled trial, he added.
Finally, the speaker announced plans for the upcoming PAVE 2 trial—the primary objective of which will be to evaluate and compare the efficacy of the paclitaxel-based IN.PACT AV DCB (Medtronic), the aforementioned MagicTouch DCB, and plain-balloon angioplasty treatments. According to Karunanithy, this three-arm study aims to recruit 642 patients across approximately 20 high-volume haemodialysis centres in the UK, and is scheduled to commence recruitment in Autumn 2023.
Karunanithy’s presentation was preceded by one from Ounali Jaffer (Barts Health NHS Trust, London, UK), who took the opposing stance of querying: Is there “too much evidence” on DCBs? He called into question the impact patient factors may have had in contrasting trial results to date; emphasised the difference between “efficacy” and “cost-
cephalic arch lesions.
For the first time, the 48-month allcause mortality results were presented which again showed no evidence of a safety concern using a paclitaxeleluting device in the AV access circuit. The mortality at 48 months was actually higher in the PTA arm at 41.8% compared to the DCB arm where mortality was 34.6% although this did not reach statistical significance.
Summarising the findings, Holden stated that they demonstrated “sustained patency benefit for IN.PACT AV DCB compared to PTA in all subgroup analyses”, and he highlighted restenoses, perianastomotic and cephalic arch lesions in particular. Concluding his talk, he said: “Durable long-term data suggest the use of IN.PACT AV DCB as a standard of care for AVF maintenance in patients with end-stage kidney disease.”
effectiveness”, and the need for greater uniformity of trial designs; and noted that artificial intelligence may have a key role to play if global database analyses are embraced in the future.
The CX vascular access programme—directed by Nicholas Inston (Queen Elizabeth Hospital, Birmingham, UK) and Kate Steiner (Lister Hospital, Stevenage, UK)—also hosted a number of workshops intended to provide delegates with handson education, and a chance to hone their practical skills while getting acquainted with many novel technologies. Demonstrators showcased the Ellipsys (Medtronic) and WavelinQ (BD) endovascular AVF (endoAVF) systems along with several other innovations.
Audience polling during the vascular access masterclass revealed differences of opinion on this topic. Following presentations on this subject from Alexandros Mallios (Hôpital Paris Saint-Joseph, Paris, France) and Tobias Steinke (Schoen Klinik Düsseldorf, Düsseldorf, Germany), among others, 59% of attendees voted against the motion that “endovascular AVFs are the way forward”, while 41% voted in favour.
The topic of endoAVFs was also the focus of an edited case delivered by Robert Shahverdyan (Asklepios Klinik Barmbek, Hamburg, Germany) later in the same session.
13 Issue98 | June 2023 CX 2023 VASCULAR ACCESS
Durable long-term data suggest the use of IN.PACT AV DCB as a standard of care for AVF maintenance in patients with end-stage kidney disease.”
Andrew Holden
Narayan Karunanithy
“Excellent” primary success of limb ischaemia thrombectomy study shared as podium first

The acute limb ischaemia programme at 2023 Charing Cross (CX) International Symposium (25–27 April, London, UK) featured a first-to-podium presentation by Sean Lyden (Cleveland Clinic, Cleveland, USA)—primary endpoint results of the STRIDE trial. Designed to report 30-day safety and performance of the Indigo aspiration system (Penumbra), the trial is an international, multicentre, prospective, single-arm, observational study of patients with lower extremity acute limb ischaemia. Lyden informed the audience that the study had successfully met its primary endpoint of target limb salvage at 30 days post-procedure.
STRIDE’s patient cohort numbered 119 patients (of 285 initially screened), across 16 sites in the USA and the European Union. The mean age of patients was 66.3±13.27, and 55/119 were women, the presenter detailed. The highest rates of other medical conditions among patients were hypertension (n=103) and hyperlipidaemia (n=100).
Lyden shared that the inclusion criteria stipulated that patients participating in the trial must have had occlusion of one or more lower limb arteries below the inguinal ligament for up to 14 days, and have a Rutherford category score of I, IIa or IIb. Of
the enrolled patients, 10.9% were ‘viable’, with a Rutherford category I score, 54.6% ‘threatened marginally’ classified as IIa, and 34.5% ‘threatened immediately’ with a IIb score.
Patients with a target vessel size of less than 2mm, amputation in the ipsilateral limb, or with target thrombus in a saphenous vein bypass graft were excluded from the trial, the speaker added.
Eight patients of the 119 enrolled exited the study before the 30-day follow-up point—five died, one was lost to follow-up, and two patients withdrew, Lyden supplemented. A further two patients missed 30-day

follow-up.
In terms of the primary endpoint, target limb salvage at 30 days was achieved in 109 patients, according to the presenter. Multiple secondary endpoints were also measured— efficacy endpoints comprised patency at 30 days, and modified Society for Vascular Surgery (SVS) runoff score immediately postprocedure versus baseline. Lyden elaborated that the results for these measures were 90.3% success and an improvement of SVS runoff score of 6.3±5.49, respectively. Regarding safety-related secondary endpoints, device-related serious adverse events numbered one and major periprocedural bleeding was reported in five patients.
Furthermore, the speaker said, the median time taken to carry out thrombus aspiration with the Indigo system was 22.0 minutes (interquartile range 12.0–47.0).
Lyden concluded that STRIDE study patients treated frontline with the Indigo aspiration system had “excellent” limb salvage rates, a “low” rate of periprocedural complications, and a “high” technical success rate. “Mechanical aspiration thrombectomy provided a safe and effective alternative therapeutic option for lower extremity acute limb ischaemia patients,” were the presenter’s parting words.
In the discussion following Lyden’s presentation, moderator Gunnar Tepe (RoMed Klinikum, Rosenheim, Germany) asked how often during the STRIDE study it was necessary to perform any additional procedures. The presenter responded that there were a “small proportion of patients” who received postoperative thrombolysis after incomplete mechanical aspiration, the data for which will be included in the paper that principal investigator Thomas Maldonado (New York University Langone Health, New York, USA) is currently working on.
Another question probed what is next for the STRIDE study, with Lyden noting that the first thing the study team are planning to do is “get into the dataset” and look at all the cohorts that were included in terms of type of pathology and the vessels that were treated.
Bioresorbable drug-eluting stents swing CX audience vote following peripheral trial update
Following updates from multiple studies assessing bioresorbable drug-eluting stents, the majority (69%) of CX 2023 audience members in the peripheral arterial and chronic limb-threatening ischaemia (CLTI) session voiced support for these technologies, voting in favour of the statement that ‘bioresorbable wins’.
HOWEVER, QUESTIONS WERE RAISED over the length of time it takes for these devices to be resorbed following implantation. Responding to session anchor Roger Greenhalgh’s (Imperial College London, London, UK) question regarding their strength, and their longevity, panellist Ramon Varcoe (University of New South Wales, Sydney, Australia) said one example of these stents—the Esprit below-the-knee (BTK) scaffold (Abbott)—is only slightly less strong than a metallic stent, but how long they last is “up for debate”.
“There is a school of thought out there that these stents should actually dissolve more quickly,” Varcoe stated, also touching on the fact that the Esprit device takes roughly 18–24 months to be resorbed, despite the fact drug-eluting stent treatments in BTK patients may need no longer than six months to be effective.
Delivering an update on the LIFE-BTK randomised trial—which he feels has become “the new gold standard” in BTK studies—Varcoe said the “excellent” long-term patency and freedom from target-lesion revascularisation (TLR) Esprit achieved
in an earlier proof-of-concept study facilitated this larger, multicentre undertaking. He concluded by noting that LIFE-BTK enrolment has now closed, and results are set to be released later this year.
A similarly positive outlook was then delivered by Michel Bosiers (University Hospital Bern, Bern, Switzerland) in his presentation of an update from the MOTIV trial, the results of which showed a 99% rate of technical success in delivery and

revascularisation, as well as 88.3% vessel patency after 12 months, in BTK cases. In this prospective, multicentre study assessing the sirolimus-eluting Motiv bioresorbable scaffold (Reva Medical), Bosier emphasised “excellent” tracking and visibility during implantation; low adverse event rates; and a single, clinically-driven TLR across the entire patient cohort.
During the same session, EFEMORAL I trial results indicating the ability of the Efemoral vascular scaffold system (EVSS; Efemoral Medical) to target a “significant” unmet need in peripheral vascular intervention for femoropopliteal disease were presented by Andrew Holden (Auckland City Hospital, Auckland, New Zealand). In his update on the trial, Holden disclosed encouraging initial results in short lesions.
Despite “no safe and effective formulation of any [bioresorbable] vascular scaffold” being realised to date in the peripheral vascular bed, according to Holden, development of the EVSS specifically for use in this area has provided high radial strength, “unencumbered” movement of the femoropopliteal axis and prolonged sirolimus elution.
With a look to the future, Varcoe acknowledged the relevance of translating these promising findings from proof-of-concept to “real-world disease”, before Holden drew the session to a close by stating that inflammation presents an additional challenge moving forward—quipping that “neointimal hyperplasia has been their Achilles’ heel” in the past.
14 June 2023 | Issue98 CX 2023
PERIPHERAL
Mechanical aspiration thrombectomy provided a safe and effective alternative therapeutic option for lower extremity acute limb ischaemia patients.”
69% of the CX 2023 audience agreed: bioresorbable wins
Sean Lyden

















*Available for US and EU readers only **Available worldwide A trusted provider of latest news, review of cutting-edge research, congress coverage and opinion from thought leaders A specialised news source in the cardiovascular field Editorially independent Visit cardiovascularnews.com and click ‘Subscriptions’ for complimentary print subscription* and e-newsletter subscription** Subscribe today Available in print and digital formats and through our social channels
Rachel Bell
A specialist in complex open aortic surgery, Rachel Bell speaks to Vascular News about her career so far. Raised in Yorkshire, UK, she moved to London for medical school before recently making the move back to the north of England to take up the role of clinical lead for vascular surgery at the Freeman Hospital in Newcastle upon Tyne, UK. She advocates for retaining open surgery skills in an increasingly endovascular world and underlines some of the key challenges facing the specialty in the wake of COVID-19 and against the backdrop of a health service under “massive stress”. Aside from her clinical achievements, she was recently named president of the Vascular Society of Great Britain and Ireland (VSGBI)—making her only the second woman to be elected to the position .“I think we are stronger together,” she says, summarising a key belief behind her main aim in the role of encouraging wider, more inclusive participation within the society.
Why did you decide to pursue a career in medicine and why, in particular, did you choose to specialise in vascular surgery?
I think I pursued a career in medicine because my mum was a nurse and I grew up listening to all the stories from her training and it piqued my interest. She also used reverse psychology as she told me when I was 13 that I might not be clever enough to be a doctor, and so, to prove her wrong I decided I was definitely going to become a doctor. I chose to go to medical school in London because I had lived in Yorkshire for almost all of my childhood and, aged 18, I just needed to experience life outside of Yorkshire. I started at Guy’s and St Thomas’ medical school in 1989 and had pretty much determined by the time I had finished that I was more likely to be a surgeon than a medic. I did not like the medical ward rounds that lasted all day—my attention span is not that long. I did my surgical house jobs at Guy’s and I worked for Professor Lord McColl, who was a general surgeon, but linked to our firm was Professor Peter Taylor, who was inspiring, and he is the main reason I did vascular surgery. He was very inclusive of ‘the firm’ as it was in those days of house officers, senior house officers and registrars— we were all part of his team. I can remember him letting me close an aneurysm sac at the end of an open aneurysm repair and, as a house officer, that was it, I was sold. I think a lot of people would say that I am quite a confident individual and I think he fed into that, because he encouraged the trainees to be involved and speak up, and there was something incredibly powerful about that.
What has been the most important development in vascular surgery over the course of your career so far?
There has been a paradigm shift from open surgery to endovascular treatment and it has really broadened the specialty. You have to be multiskilled and that has changed everything. It has changed how we treat our patients, how we work within the hospital, how we train our juniors and it has changed vascular research. From an endovascular point of view there are questions about durability, but we are now able to offer very complex surgery to a much larger population and that has been the biggest and the best change. However, there is still a role for open surgery. I am a complex open aortic surgeon— because I come from a generation that spanned the ‘old’ open surgery world and the beginning of the endovascular revolution. Nowadays, I see younger vascular surgeons with a total passion for the endovascular side who are a little bit scared of open surgery, particularly in the abdomen. Training has changed now to encompass the endovascular requirements, but the need for open surgeons has not gone away.
What are some of the biggest challenges currently facing vascular surgery?
I think UK hospitals are still struggling to recover after the COVID-19 pandemic. Also, I think vascular surgery suffers a bit because we do not have a cancer. My personal feeling is that cardiovascular disease—and particularly things we treat such as aortic aneurysms, symptomatic carotids and critical limb ischaemia—is our cancer. You are potentially going to die far more quickly from a symptomatic carotid, critical limb ischaemia or even a ruptured aneurysm than from cancer, and yet on a day-to-day basis a critical care bed will often be allocated to a cancer
patient over my open aneurysm repair patient. Vascular surgery is an urgent specialty and we need to learn to tell our story slightly differently. True elective surgery only makes up a small proportion of our workload and as we have set tight targets for the treatment of our patients with urgent conditions it has put a lot of pressure on our hospital systems to ensure patients get seen, imaged and treated in a timely manner. I think during COVID-19 we were ‘lucky’ because we had symptomatic patients with carotid disease and critical limb ischaemia that needed treatment immediately and could not wait until the pandemic was over. Hence, we did not come out of the end of the pandemic with massive waiting lists like other specialities. However the NHS is currently under incredible pressure and the combination of trying to get on top of the waiting lists whilst simultaneously coping with the problems of staff retention and burnout, the financial crisis and industrial action puts the NHS in the most perilous position that I have witnessed in the last 30 years.
What are the aims of the Aortic Dissection Toolkit and how are things progressing with the programme?
The Aortic Dissection Toolkit was launched last March to improve the pathway for patients with acute aortic dissection and ensure good regional governance. We have asked regions to get together and discuss how they can organise an aortic dissection pathway for their area that is sympathetic to their geography
and skill mix. We would like each region to publish a rota for the aortic dissection service so that it is crystal clear who they need to phone when they get an aortic dissection case. The regional team also have responsibility for ensuring there is a safe way of transferring patients to the right hospital and that their imaging can be efficiently electronically transferred so that the receiving clinicians can managed the patient as quickly and effectively as possible. Another responsibility of the regional team is to ensure that we collect data so that we can track our progress and make sure we are making a positive difference. Unfortunately whilst this is incredibly important work the toolkit has no allocated resource. We are essentially asking several specialties—vascular surgery, cardiac surgery, interventional radiology, critical care and emergency medicine—to get together to sort out this problem countrywide for free and I am very grateful to everyone who is participating in this programme. The

16 PROFILE June 2023 | Issue98 Interview
Training has changed now to encompass the endovascular requirements, but the need for open surgeons has not gone away.”
Current appointment:
September 2020–present: Consultant vascular surgeon and clinical lead for vascular surgery, Freeman Hospital, Newcastle upon Tyne, UK
National positions held (selected):
2022–present: President of the VSGBI
2022–present: Member of clinical reference group for vascular
surgery, NHS England (NHSE)
2021–present: National vascular lead for the Aortic Dissection Toolkit, NHS England
2019–2022: Chair of the Circulation Foundation

2018–2021: President of the British Society of Endovascular Therapy (BSET)
Previous appointments (selected):
January 2006–September 2020: Consultant vascular surgeon, Guy’s and St Thomas’ NHS Foundation Trust, London, UK
October 2005–December 2005: Honorary clinical fellow in vascular
trick now is to keep up the momentum to ensure these pathways get embedded into normal clinical practice.
What do you hope to achieve as the president of the VSGBI?
I am only the second woman to be president of the VSGBI, after Professor Averil Mansfield, and I feel honoured and quite humbled to be mentioned in the same sentence as Averil. It never crossed my mind that one day I would follow in the footsteps of some of my vascular surgical heroes and heroine. I would like to make the Vascular Society more inclusive and less elitist. As a society we are aware that many vascular surgeons around the country are not members of the VSGBI and I would like to know why that is and what can be done to change that. I may be a bit biased but the work that the VSGBI Council does behind the scenes is incredible and I would like to encourage others to get involved to shape the society for the future. We are about to send out some engagement questionnaires asking as many non-members that we can contact what things they would like to see that might encourage them to join, because ultimately we are stronger together. We know that there are big problems around pensions and burnout and the society would like to provide some support, or at least be there to listen. I would also like to see younger members on Council and obviously more women, as it would make it more balanced. Alongside all of that I would like to continue the drive to ensure safe national pathways for patients with aortic dissection. That may mean defining specialist centres for complex aortic problems to ensure patients get the best care by the right specialists when they need it.
What are your hobbies and interests outside of medicine?
If I had not been a vascular surgeon, I probably would have been a singer. I sing all the time—to patients, in theatre, and I am a member of a choir—it brings me joy. I have also spent a lifetime following cricket, from county cricket to test match and one day internationals, and I do like a good gin and tonic.
surgery, Edinburgh Royal Infirmary, Edinburgh, UK
April 2005–October 2005: Specialist registrar in general and vascular surgery, Guy’s and St Thomas’ Hospital
Clinical research (selected):
2015–2018: Principal investigator for the ETTAA prospective cohort study
2012–2014: Principal investigator for the IMPROVE randomised controlled trial
17 Issue98 | June 2023 Interview
Study finds correlation between neighbourhood social disadvantage and PAD outcomes
A RECENT STUDY HAS FOUND that, among patients who underwent infrainguinal revascularisation or amputation in the Society for Vascular Surgery (SVS) Vascular Quality Initiative (VQI), those with higher neighbourhood adversity had more advanced peripheral arterial disease (PAD) at presentation and lower rates of revascularisation.
“Studies examining the relationship between socioeconomic disparities and PAD often focus on individual social health determinants and fail to account for the complex interplay between factors that ultimately impact disease severity and outcomes,” authors Lucas Mota (Beth Israel Deaconess Medical Center, Boston, USA) and colleagues write in the Journal of Vascular Surgery (JVS). They claim that area deprivation index (ADI), which they describe as a “validated measure of neighbourhood adversity,” provides a “more comprehensive assessment” of social disadvantage. For this reason, the investigators set out to examine the impact of ADI on PAD severity and its management.
First, the researchers identified all patients who underwent infrainguinal revascularisation—either open or endovascular—or amputation for symptomatic PAD in the VQI registry between 2003 and 2020. They assigned an ADI score of 1–100 to each patient based on their residential ZIP code,
with higher ADI scores corresponding with increasing diversity, and categorised patients by ADI quintiles (Q1–Q5).
Mota et al note that the outcomes of interest included indication for procedure (claudication, rest pain or tissue loss) and rates of revascularisation (versus primary amputation). They used multimodal logistic regression to evaluate an independent association between ADI quintile and these outcomes.
The researchers identified 79,973 patients who met their criteria within the VQI database. Specifically, they communicate in JVS that 9,604 (12%) of these patients were in the lowest ADI quintile (Q1), 14,961 (18.7%) in Q2, 19,800 (24.8%) in Q3, 21,735 (27.2%) in Q4, and 13,873 (17.4%) in Q5. There were “significant trends” toward lower rates of claudication (Q1: 39% vs. Q5: 34%, p<0.001), higher rates of rest pain (Q1: 12.4% vs. Q5: 17.8%, p<0.001) as the indication for intervention, Mota and colleagues report in their JVS paper. They add that they found lower rates of revascularisation (Q1: 80% vs. Q5: 69%, p<0.001) with increasing ADI quintiles.
In adjusted analyses, the investigators relay, there was a “progressively higher likelihood” of presenting with rest pain versus claudication, with patients in Q5 having the highest probability when
Rouleaux Club announces Hurting Leg Competition winners
Vaux Robertson (Leicester Vascular Institute, Leicester, UK) and Natalie Yonan (Newcastle Hospitals, Newcastle, UK) were announced as the winners of the Rouleaux Club’s Hurting Leg Competition designed to create patientfacing infographics and infomercials on ‘the hurting leg’ at the 2023 Charing Cross (CX) International Symposium (25–27 April, London, UK).
YONAN WON THE INFOGRAPHIC category with an entry entitled “RING”, which plays on the theme of rest pain, impaired walking, non-healing ulcers and gangrene. Robertson claimed the prize in the infomercial section with a video called “Arterial disease can affect anyone”. The competition was organised by the UK’s vascular surgery trainee association
compared with those in Q1 (relative risk: 2; 95% confidence interval [CI]: 1.8–2.2; p<0.001). The authors add that patients in Q5, when compared with those in Q1, also had a higher likelihood of presenting with tissue loss versus claudication (relative risk: 1.4; 95% CI: 1.3–1.6; p<0.001). They also reveal that patients in Q2–Q5 had a lower likelihood of undergoing any revascularisation procedure compared with patients in Q1.
“Further work is needed to better understand neighbourhood factors that are contributing to these disparities in order to identify community-level targets for improvement,” the authors write in their concluding remarks.
Healthcare disparities in the spotlight
Senior author Marc Schermerhorn (Beth Israel Deaconess Medical Center) and colleagues have conducted extensive research on the topic of health disparities in vascular care. At the CX Aortic Vienna 2022 Digital Edition (24–26 October), for example, Schermerhorn spoke on the impact of

sex and racial and ethnic factors on abdominal aortic aneurysm (AAA) management and outcome. He concluded that disparities by sex, race and ethnicity “exist at all steps along AAA care,” including AAA detection, clinical trial enrolment and outcomes, among others. Disparities early in the care trajectory likely influence disparities observed later on, he added.
Earlier in the year, at the SVS Vascular Annual Meeting (VAM 2022; 15–18 June, Boston, USA), Aderike Anjorin (Duke University Medical Center, Durham, USA) presented the findings of a study of over 7,000 chronic limb-threatening ischaemia patients under the guidance of senior investigator Schermerhorn. She reported that Black and Hispanic patients had higher three-year amputation and reintervention rates. “Interventions to improve early diagnosis, risk factor modification, and postoperative surveillance in these populations may confer long-term limb salvage benefits,” the speaker told VAM attendees in closing her presentation.
in conjunction with CX and was open to medical students and trainees from across the world.
Rouleaux Club executive committee member Claire Dawkins (Newcastle Upon Tyne Hospitals NHS Foundation Trust, Newcastle, UK) explained why the society created the contest. “Chronic limbthreatening ischaemia [CLTI] and the hurting leg are a major issue,” she told CX 2023. “It is high prevalence, is increasing in incidence and is often, certainly in the UK and, from what I understand, globally there is often a delayed presentation. This has all been exacerbated by COVID, with many difficulties of the patient pathways and pressures on general practice, or family doctors.”
Key are ways to get patients to present as early as possible, said Dawkins. There is little vascular surgery-specific [information] in the public domain in terms of patient awareness and education, she explained. “When I am talking to patients in the UK, they have very little awareness of peripheral arterial disease or CLTI. So, the aim for this is to really get that message out there.”
Rouleaux Club president Leanna Erete (Royal Free Hospital, London, UK) handed over cheques of £500 each to Robertson and Yonan.

“I think there are great things in all of those [entries],” said audience member Jonathon Boyle (Cambridge University Hospitals NHS Trust, Cambridge, UK). “One of the most successful campaigns has been the FAST campaign for stroke, and that is a very simplistic infographic—you have basically got four pictures and four letters pretty much. Take everything away and bring it all together. Have your prize winners today, but then take the best bits from every infographic and try and get one slightly more simplified than the ones you have shown. For the public, they need to be fairly easy to understand.”
Leanna Erete and Vaux Robertson
18 June 2023 | Issue98 Healthcare Disparities PERIPHERAL
Further work is needed to better understand neighbourhood factors that are contributing to these disparities in order to identify communitylevel targets for improvement.”
Marc Schermerhorn








*Available for US and EU readers only **Available worldwide A trusted provider of latest news, review of cutting-edge research, congress coverage and opinion from thought leaders A specialised news source in the neuro interventional arena Editorially independent Visit neuronewsinternational.com and click ‘Subscriptions’ for complimentary print subscription* and e-newsletter subscription** Subscribe today Available in print and digital formats and through our social channels
Handheld ECG device scoops CX 2023 Innovation
Showcase prize
Judges of the CX 2023 Dragon’s Den-style contest—the finale of the 2023 Charing Cross (CX) International Symposium (25–27 April, London, UK) Innovation Showcase programme— described the field of entrants to this year’s edition of the competition as the strongest line-up in its history.
THE JUDGING PANEL OF physician-innovators selected HeartEye, a Netherlandsbased developer of handheld electrocardiogram (ECG) devices, as the overall winner of the innovation prize, which comes with a £1,000 award. Honourable mention was given to four other entrants.

Peter Doevendans (UMC Utrecht, Utrecht, The Netherlands) gave an overview of the HeartEye technology in a short presentation entitled
‘ECG anytime, anywhere in 60 seconds’, describing it as a “digital transformation” for ECG acquisition. HeartEye is a pocket-sized device that can take clinical-standard ECG readings wirelessly, negating the need for a large, stationary ECG unit. The technology, which has been developed with the support of an Innovative Medical Devices Initiative (IMDI) grant from the Netherlands Organisation for Health Research and Development (ZonMw) is patented,
Detecting, predicting and preventing aortic ruptures with computational modelling
IN PHYSICS OF FLUIDS, BY American Institute of Physics (AIP) Publishing, researchers from the Indian Institute of Technology (BHU) Varanasi and Indian Institute of Technology Kanpur made a computational model of the cardiovascular system in order to predict early abdominal aortic aneurysm (AAA) rupture and monitor patients’ blood vessel conditions. The team investigated the effect of realistic, patient-specific AAA shapes on the haemodynamics of pulsatile Newtonian fluids in an aortofemoral artery under normal and diseased conditions.
Predicting the risk of AAA rupture involves a combination of imaging studies, such as ultrasound, computed tomography (CT) scans, magnetic resonance imaging (MRI), and haemodynamics, as well as clinical factors such as age, sex, smoking history, and family history of AAA.
“If an AAA is detected early, treatment options such as surgical repair or endovascular stent grafting are available to prevent rupture,” said the authors. “These treatments are both effective at reducing the risk of rupture and improving survival rates.”
Using image-based computational blood dynamics, the researchers mimicked specific health conditions and investigated various hemodynamic parameters. Their patient-specific geometric models of a human aortofemoral artery were constructed from 3D medical imaging data.
To solve the blood flow governing equations under the pulsating conditions caused by the heart’s beating, they used finite elementbased simulations. The team found that aneurysm size alters the blood flow velocity distribution. In addition, flow separation occurs during systolic deceleration, and the vortex begins to travel in the aneurysm sac. Among other complex dynamics, this may influence the blood circulation of lower extremities.
“In the future, such computational work will help in development of digital twins of the cardiovascular system,” said first author Sumit Kumar (BHU, Varanasi, India). Digital twins are virtual patient representations that receive real-time updates on a variety of data variables, an AIP press release explains.
and could be marketed to healthcare providers or direct to consumers within two years, Doevendans noted.
“We have been doing this for a number of years, and this was the toughest by far,” said judging panellist Robert Mitchell (Park City, USA), before the announcement of HeartEye as the winner of the prize.
Euphrates Vascular, the developer a nano-scale endovascular system to address microvascular occlusion and no reflow, was among those singled out by the judges as being of particular interest. Presenter David Deaton (Medstar Georgetown University Hospital, Washington, DC, USA) told the judges that the Pulse NanoMed device extends the reach of current therapies, and has been given approval to begin a US Food and Drug Administration (FDA) investigational device exemption (IDE) trial in patients with acute ischaemic stroke.
Tilo Kölbel (University of Hamburg, Hamburg, Germany) introduced Mokita Medical, which has developed a technology to address air embolisation during procedures such as thoracic endovascular aneurysm repair (TEVAR) and transcatheter aortic valve implantation (TAVI), a cause of stroke and cognitive decline. The Mokita technology uses a gas-soluble fluid to eliminate air from devices, and is being developed into a disposable device that can be connected to the delivery system for a transcatheter procedure.
The company is planning a first-inman study for 2024, and anticipates commercialisation from 2026 onwards.
Mitchell praised Kölbel’s work in this area as being “really important and impactful”, and said that the entry had been one of the options strongly considered for the prize.
Another technology featured in the session included a non-invasive, wearable monitoring system for arteriovenous fistulas (AVFs), intended to aid early identification of failing AVFs. The innovation, presented by Ali Kordzadeh (Anglia Ruskin University, Braintree, UK) is worn like a wristwatch by patients to monitor venous outflow. Novel device
coating materials were also exhibited, with Tony Simula (Mawson Lakes, Australia) detailing Bioinvisible, a drug-free polymer coating that could replace existing drug coatings in devices such as stents, vascular grafts and heart valves.
Amsterdam UMC leads an AI-powered hunt for high-risk vascular patients
A new study will focus on using artificial intelligence (AI) to predict the worsening of vascular disease in people with an aortic aneurysm or peripheral arterial disease (PAD), a press release reports. VASCUL-AID is a large European study led by Amsterdam UMC, and recently launched thanks to a Horizon grant worth €6.4 million.
KAK KHEE YEUNG (Amsterdam UMC, Amsterdam, The Netherlands) comments: “Our vessels are an important part of the cardiovascular system that keeps people alive. Once you have a vascular disorder such as an aneurysm, we see that the aggravation of these diseases also increases the chance that you will eventually die from another cardiovascular disease. This indicates to us that we also need to investigate how we can stop these conditions that seem to occur outside the heart, but that do affect the functioning of the cardiovascular system. At the moment it is not possible to predict the course of aneurysm or of PAD. People live in uncertainty about how their disease will develop and this results in many hospital visits and treatments. We would like to identify and isolate people with a high risk of their
condition worsening from the large group in order to develop a more specific treatment plan. VASCULAID should make this possible.” The press release states that VASCUL-AID will unite partners across Europe to develop infrastructure in which data from patients with aneurysms and PAD can be monitored. Six clinics across Europe, including Oxford University, will actively collect data from these patients. Using genetic data and imaging studies, as well as looking at protein profiles in blood and medication use. This will then be combined with existing databases and biobanks. Patients will also gather their own data. An app has been developed that will gather data from telephones and wearable device relating to, for example, daily activity and quality of life as well as their heart rate.
21 Issue98 | June 2023 Innovation
We have been doing this for a number of years, and this was the toughest by far—”
Robert Mitchell
CX INNOVATION SHOWCASE 2023
Venous, we have a perception problem
Venous disease care has a problem with optics in the context of growth in the number of venous procedures and the spectre of inappropriate care, the 2023 Charing Cross (CX) International Symposium (25–27 April, London, UK) heard.
The conversation thread emerged in a question from Stephen Black (Guy’s and St Thomas’ Hospital, London, UK), posed to presenter Erin Murphy (Sanger Heart and Vascular Institute, Atrium Health, Charlotte, USA), who had just outlined possible solutions that can be targeted at not only discouraging inappropriate venous care but also encouraging appropriately administered procedures.
Black asked Murphy: “Why is it that it is so easy for people who have never trained in veins just to crack on and treat veins without any consequences?”
Murphy pointed to a problem with misperception— ”that this is an easy patient subset to treat, and I think those of us who are in this room treating these patients know that there is actually very complex decisionmaking [involved] in order to get the right outcomes for our patients,” she said. “We need to change
Multidisciplinary CX faculty address key issues in the pelvic venous disease space
The deep venous consensus update session at CX 2023 covered a range of key topics in the field, including issues associated with pelvic venous lesions.


THE SESSION OPENED WITH A series of presentations on the pelvic veins, starting with one from Kathleen Gibson (Lake Washington Vascular, Bellevue, USA) on optimal work-up before intervention for patients with pelvic venous reflux. “This is going to be one of these talks that is full of my opinions and not data,” she said in opening, explaining that this is an area in which there is, as yet, no consensus.
Among Gibson’s conclusions was the message that patient history and presentation are important in patients with pelvic venous reflux, urging audience members to “treat the patient, not the imaging”. On the
that perception.”
Murphy had outlined several ways she sees of helping to curb the problem, building on a talk Manj Gohel (Cambridge University Hospitals NHS Foundation Trust, Cambridge, UK) gave last year. They included defining appropriate care through research initiatives, consensus statements and guideline data; educating and disseminating such data; holding practices accountable for decisions to carry out inappropriate care; and establishing correct financial incentives.
The biggest of these challenges currently involves educating a sprawling array of providers who treat venous disease patients, Murphy said. Are the right doctors treating the venous disease population? Vascular surgeons, for instance, “have no requirement in their board certification to be treating venous patients,” Murphy said, asking whether they are well-enough trained in the venous area. “Coming out of training, they have done about 40 venous cases
topic of imaging, however, she did note that duplex ultrasound, crosssectional imaging and venography/ intravascular ultrasound “all have important diagnostic roles” and that confirmatory imaging is “very important” to make a definitive diagnosis prior to treatment.
Subsequently, Aleksandra Jaworucka-Kaczorowska (Jaworuccy Center for Surgery and Dentistry, Gorzow Wielkopolski, Poland) outlined three edited cases on ‘bottom-up’ treatment for pelvic origin varicose veins. She explained that, in her experience, ‘top-down’ treatment does not give good results and that very often multiple embolisation sessions are required. The results of ‘bottom-up’ treatment, on the other hand, she has found to be good. This is also a less invasive treatment, she pointed out, adding that it can be repeated if required and is cost-effective.
Moderator Manj Gohel (Cambridge University Hospitals NHS Foundation Trust, Cambridge, UK) noted that the presenter was able to offer a “unique perspective” on this topic due to the fact she is a trained gynaecologist, and, in the discussion following her presentation, Jaworucka-Kaczorowska shared some insights from her practice with an audience of vascular surgeons.
overall.” Similarly, for interventional radiology, the situation is not any better, she reasoned. “Cardiology has no required training. So, what do we do?”
The answer might be dedicated providers who undertake training and fellowship requirements specific to venous disease, as well as specific board certification, and accreditation. “This is in progress,” Murphy pointed out. “This is probably a direction that we need to go.”
In terms of accountability, she queried whether the venous space should be auditing for decisionmaking when people are trained appropriately. “We have seen when we identify practices that are doing things outside the norm,” Murphy explained, drawing attention to examples of practices carrying out more ablations per patient compared to the average practitioner treating venous disease, “when we notified the practice of their outside-the-box numbers, they actually self-corrected to an extent.” The implication here is that they had been educated, she added.
“Underdiagnosis and undertreatment probably affect more patients than overtreatment, particularly over time,” Murphy said. “So, we do not want to disincentivise. But a multimodal effort to address inappropriate care is needed, and, probably, educating providers is our number-one thing.”
De Maeseneer receives CX award for dedication to specialist venous care
Marianne De Maeseneer (Erasmus Medical Centre, Rotterdam, The Netherlands) was at the podium to dispense tips for success and longevity as a venous specialist during the superficial and lymphatic consensus update at CX 2023. For Manj Gohel (Cambridge University Hospitals NHS Foundation Trust, Cambridge, UK), no one is better placed to deliver such advice than De Maeseneer, he told symposium attendees.
DE MAESENEER WAS GIVING
a talk during the superficial venous and lymphatic session, and Gohel, as co-moderator, was welcoming her to the podium. She kicked off her message by recasting the title as ‘How to be a good and happy venous specialist.’ She shortlisted the keys as curiosity, exchange of ideas, commitment to clinical practice, research and scientific societies, work-life balance and passion. “All these elements were important in my career,” De Maeseneer said. “Passion about the patients, passion about the team you are working with, about research, about education— this is all very important to become and stay a happy and good working venous surgeon, and hopefully long-living venous specialist,” she told CX 2023. At the close of her talk, session comoderator Stephen Black (Guy’s and St Thomas’ Hospital, London, UK)
invited De Maeseneer to remain at the podium to receive the CX Lifetime Achievement Award. Presented by Armando Mansilha (University of Porto, Porto, Portugal), she becomes just the second-ever recipient.
“I do not think anyone has put more into defining how we treat our specialty,” said Black. “If any of you can emulate a career in veins, and put veins on the map, Marianne is a great role model to follow.”
22 June 2023 | Issue98 CX 2023
VENOUS
A multimodal effort to address inappropriate care is needed, and, probably, educating providers is our number-one thing.”
Marianne De Maeseneer with the CX venous executive board
Erin Murphy at the CX podium







A trusted provider of latest news, review of cutting-edge research, congress coverage and opinion from thought leaders A specialised news source in the venous arena Editorially independent Visit venousnews.com and click ‘Subscriptions’ for e-newsletter subscription Subscribe today Available in digital format and through our social channels
Vascular community split over “death” of traditional carotid stenting

A debate at the 2023 Charing Cross (CX) International Symposium (25–27 April, London, UK) between two prominent carotid interventionists—Peter Schneider (University of California San Francisco, San Francisco, USA) and Domenico Valenti (King’s College London, London, UK)—revealed that the vascular community is currently divided over the benefits of transcarotid artery revascularisation (TCAR), as compared to percutaneous carotid artery stenting (CAS).
SCHNEIDER KICKED OFF the debate by arguing in favour of TCAR, initially outlining some of the limitations of percutaneous CAS that prior studies have demonstrated—for example, unwanted events relating to manipulation of the aortic arch as well as incomplete particulate capture. He went on to query whether there is a “better way” to treat carotid artery disease, positing that TCAR may offer a solution that overcomes these limitations.

Once again referring to the current literature in this space, he noted that TCAR can enable greater neuroprotective capabilities; improved safety in symptomatic patients and octogenarians; and carries a


more efficient learning curve, versus percutaneous stenting.


After reiterating the “unresolved challenges” CAS faces, including those relating to the aortic arch and particulate capture, Schneider concluded that prospective TCAR studies and his own experiences have shown both safety and efficacy with the procedure, demonstrating outcomes that are “competitive” with carotid endarterectomy (CEA) and “substantially better” than percutaneous stenting.
Offering a riposte to these assertions, Valenti stated that TCAR—in essence, at least— has been around for many years, and is therefore not the


“disruptive technology” within carotid interventions it is sometimes presented as, also claiming that his opponent and other TCAR advocates have been “mesmerised” by the existing data. Homing in on said data, Valenti challenged positive conclusions drawn from the results of the ROADSTER 2 trial, noting its non-randomised nature, low proportion of symptomatic patients and, “more importantly”, lack of stratified data on delay to treatment. Additionally, he told attendees that findings from the Society for Vascular Surgery’s (SVS) Vascular Quality Initiative (VQI) are also limited by selection biases, gaps in the data, and the fact they come from a nonrandomised trial.

Finally, Valenti noted that CAS has been subject to far more “intense scrutiny” than TCAR to date—for example, in the CREST, ICSS and SPACE randomised controlled trials (RCTs).
And, while he commented that TCAR may yet prove useful in certain patients, they are yet to be identified, and the lack of RCT-derived evidence supporting it means the “death” of percutaneous stenting is not imminent.
An audience poll produced a close result, but ultimately saw more CX attendees concur with Valenti’s closing gambit that “TCAR is not about to send CAS to oblivion”, as 52% voted against the statement that ‘TCAR is better than percutaneous carotid stenting’.


24 June 2023 | Issue98 CX 2023
CAROTID *Available for US and EU readers only **Available worldwide Subscribe today Available in print and digital formats and through our social channels Visit vascularspecialistonline.com and click ‘Subscriptions’ for complimentary print subscription* and e-newsletter subscription** An official publication of the Society for Vascular Surgery (SVS) A trusted provider of latest news, review of cutting-edge research, congress coverage and opinion from thought leaders Editorially independent Voted
52%
against the statement that ‘TCAR is better than percutaneous carotid stenting’
Left to right: Peter Schneider, Maarit Venermo, Alexander Zimmermann and Domenico Valenti
Dual antiplatelet therapy linked to better post-TCAR outcomes versus other drug regimens
Dual antiplatelet therapy (DAPT) has demonstrated improved clinical outcomes, including reduced in-hospital stroke and mortality risks, compared to other medication regimens in carotid artery disease patients who undergo stent placement via a transcarotid artery revascularisation (TCAR) procedure.
This is the key concluding message put forward by Hanaa Dakour-Aridi (Indiana University School of Medicine, Indianapolis, USA), S Keisin Wang (McGovern Medical School at UTHealth, Houston, USA) and colleagues in a recent Journal of Vascular Surgery (JVS) publication.
The authors queried all patients who underwent TCAR within the Vascular Quality Initiative (VQI) from September 2016 to June 2022 to determine the association between antiplatelet choices and outcomes. They did this against the backdrop of DAPT being the preferred medication regimen in post-TCAR patients, “despite a dearth of quality data”, in an effort to define the risks carried by different antiplatelet approaches.
“Patients maintained on DAPT were compared with those receiving alternative regimens consisting of single antiplatelet [therapy], anticoagulation, or a combination of the two,” Dakour-Aridi, Wang and colleagues note. “A 1:1 propensity-score match was performed with respect to baseline comorbidities, functional status, anatomic/physiologic risk, medications and intraoperative characteristics. In-hospital and one-year outcomes were compared
Initial
cases
indicate
between the groups.”
The authors report that a total of 29,802 procedures were included in their study population, with 82.7% receiving DAPT and 17.3% receiving an alternative antiplatelet regimen. Propensity-score matching generated 4,876 unique pairs across which they performed their analysis.
Compared with patients on DAPT, in-hospital ipsilateral stroke rates were “significantly higher” among those receiving other types of antiplatelet therapy (1.1% vs. 1.7%, respectively). And, while there was no statistically significant difference between the two groups regarding mortality—0.5% with DAPT and 0.6% without—a composite of stroke/death was more likely in patients receiving an alternative regimen (2.4%) rather than DAPT.
Furthermore, Dakour-Aridi, Wang and colleagues found that immediate stent thrombosis was more common in the ‘alternative’ group of patients, and a non-significant trend towards increased rates of returning to the operating room was observed as well.
lithotripsy
can help TCAR expand into high-risk patients
Lithotripsy may hold the key to enabling more carotid artery disease patients who require calcification treatment to undergo stent placement via a transcarotid artery revascularisation (TCAR) procedure, as per single-centre experiences presented at the recent Society for Clinical Vascular Surgery (SCVS) annual symposium (25–29 March 2023, Miami, USA) by Kathryn DiLosa with principal investigator Misty Humphries (both University of California Davis, Sacramento, USA).
IN CASES OF CIRCUMFERENTIAL or eccentric calcification, TCAR is precluded and carotid endarterectomy (CEA) often becomes the preferred approach—however, in patients considered ‘high risk’ due to their anatomy, for example, “another alternative exists”, the speaker averred. Detailing the use of intravascular lithotripsy (IVL; Shockwave Medical) prior to a TCAR procedure, DiLosa noted that predilation angioplasty may be required to allow passage of a lithotripsy balloon, and the balloon “should be sized to fully oppose the vessel wall, but not extend past the intended coverage area”.
She further stated that lithotripsy technologies have been used in the treatment of kidney stones previously. The speaker also reported a 100% rate of technical success with this approach at her institution, across a total of seven patients, with comparable procedural

“Conversely, the incidence of perioperative myocardial infarction was lower in the alternative regimen group [than with DAPT],” the authors posit, highlighting rates of 0.4% and 0.7%, respectively. “At one year after the procedure, we observed an increased risk of mortality but not stroke in patients treated with an alternative medication regimen.”
Dakour-Aridi, Wang and colleagues ultimately convey that their propensity score-matched analysis found an increased risk of both in-hospital stroke and one-year mortality in TCAR recipients who were treated with an alternative approach to DAPT. And, although patients on triple therapy experienced the same rate of major adverse cardiovascular events (MACE) as DAPT, bleeding events were not available in the VQI, the authors also note.

“Further studies are needed to elucidate the drivers of DAPT failure in patients undergoing TCAR to improve outcomes for carotid stenting patients,” they conclude.
trials
“THE TIME HAS DEFINITELY COME TO LOOK AT THE evidence, and redo these studies,” posited Alun Davies (Imperial College London, London, UK), putting forward his argument that the NASCET and ECST clinical trials “need to be reconducted” at this year’s Charing Cross (CX) International Symposium (25–27 April, London, UK).
and flow-reversal times to standard TCAR, and no observed complications within 30 days of the procedure.
“However, a larger cohort [of patients] is still needed to confirm safety,” DiLosa said.
Briefly touching on the available literature regarding pre-TCAR lithotripsy, she stated that case studies—but no significant case series—are available at this point, although she and her colleagues are currently compiling a multiinstitutional cohort including more than 50 patients.

“This is definitely for a specific patient population—those who cannot tolerate endarterectomy, but that would need the benefit of calcification [treatment],” DiLosa concluded.
Much of Davies’ argument centred around the fact that best medical therapy—the comparator arm against which carotid endarterectomy (CEA) was assessed, and found to produce clinical benefits in carotid artery stenosis patients, in both of these studies—is “significantly better than it was”.
After briefly outlining discrepancies between the North American NASCET and European ECST trials regarding how internal carotid artery stenosis was defined—with ECST having a higher threshold for severity—Davies also reminded the audience that NASCET observed a 3.3% stroke/death rate at one month in its medical therapy arm, compared to roughly 5–6% with CEA.
He then alluded to a 2003 paper by Ross Naylor (University of Leicester, Leicester, UK) et al that concluded, based on primary and secondary analyses of both trials, hat not all patients with symptomatic stenosis >70% will benefit from CEA.
Furthermore, he continued, recent research has shown that targeting and lowering a patient’s cholesterol, and initiating best medical therapy more quickly, can reduce adverse event rates by up to 80% early on. Applying this reduction to the rate of 3.3% seen in NASCET, he theorised that stroke/death incidence could now be as low as 0.7% with today’s best medical therapy.
This, coupled with uncertainties surrounding if—and in which cases—CEA is a cost-effective procedure, led Davies to reiterate that more randomised controlled trial data are now needed to re-evaluate the benefits of surgery versus medical therapy.
At the close of his presentation, the speaker highlighted the COMeT study—a proposed randomised trial comparing carotid intervention and best medical therapy that he and his colleagues are currently preparing to submit to the UK National Institute for Health Research (NIHR) for the second time, and for which they intend to enrol more than 2,500 patients.
25 Issue98 | June 2023 Carotid Updates
Medical therapy improvements mean “the time has come” to reconduct prior endarterectomy
Further studies are needed to elucidate the drivers of DAPT failure in patients undergoing TCAR to improve outcomes for carotid stenting patients.”
Hanaa Dakour-Aridi
S Keisin Wang
Kathryn DiLosa
CLASSICAL OPEN AND ENDOVASCULAR SOLUTIONS



CARDIAC, VASCULAR AND ENDOVASCULAR AORTIC ADVANCES

HOLD THE DATES
MONDAY–WEDNESDAY

2–4 OCTOBER 2023
IN PERSON AND VIRTUAL ANDAZ VIENNA AM BELVEDERE, VIENNA, AUSTRIA









AORTIC VIENNA cxaortic.com
cohort than the rate of 31.6% seen with the comparator devices
Clinical News
related outcomes between patients randomised to the AFX endograft system, with anatomical fixation, and commercially available endografts with proximal fixation.
Cook Medical treats first patient in first-in-human clinical trial for venous valve

Cook Medical recently announced that the first patient has been treated in a clinical study to evaluate a new venous valve designed for treating chronic venous insufficiency (CVI). The patient was treated by principal investigator Mauricio Alviar (Clinica de la Costa, Barranquilla, Colombia).
The valve’s safety and efficacy are now being tested in a global, multisite clinical trial. The global principal investigator of the study is Paul Gagne (Vascular Care Connecticut, Darien, USA). In addition to being a practicing surgeon and interventionist, a press release notes that Gagne brings significant experience in performing clinical trials of minimally invasive vascular medical devices.

“When leg veins function poorly, patients suffer with leg swelling, leg pain, leg ulcers, disability, and possible amputation. Therefore, it is important to restore blood flow out of the leg veins, back to the heart. Part of doing this successfully requires restoring the function of the venous valves,” said Gagne.
Cook Medical states that CVI affects around 1 in 20 adults. To address this need, the company and Cook Advanced Technologies developed a valve that functions similar to the way the veins naturally work. The artificial valve is a novel proprietary design that mimics native venous valves.
“After extensive ultrasonic and venographic evaluation of venous anatomy, we placed the Cook Medical venous valve in the leg vein. The deployment took a few minutes and the patient had local anaesthesia. It was a team effort to manage this complex case, resulting in the first clinical use of this venous valve,” said Alviar.
The clinical trial will continue to evaluate safety, efficacy, wound healing, leg pain, and disability levels over the next five years.
Five-year results of the LEOPARD trial published in the Journal of Vascular Surgery
Endologix has announced the online publication of the final five-year results of the LEOPARD trial in the Journal of Vascular Surgery (JVS). The study’s findings showed that there was no significant difference in aneurysm-


“The publication of these final five-year results in JVS reinforces the performance of our AFX2 endovascular AAA [abdominal aortic aneurysm] system in the treatment of patients with [AAAs],” said Matt Thompson, president and CEO of Endologix. “We are proud to have conducted the first randomised controlled trial comparing commercially available endografts, and we remain committed to providing the highest quality clinical evidence that underpins our life-changing vascular therapies. Importantly, the comparable performance results from the LEOPARD study between AFX/AFX2 and other endografts align with a recent publication that was authored on behalf of the Society for Vascular Surgery’s Patient Safety Organization and used
linked registry claims data.”


LEOPARD was a prospective, randomised, multicentre trial that enrolled 455 patients across 56 US centres. Two-hundred and thirty-five patients were included in the AFX/ AFX2 arm and 220 patients in the comparator arm.
The primary endpoint was freedom from aneurysm-related complications (ARC), a composite endpoint consisting of perioperative death, aneurysm rupture, conversion to open surgical repair, postoperative endoleaks, endograft migration, aneurysm enlargement, endograft limb occlusion, and device- or aneurysmrelated reintervention.
The results presented included:
A rate of freedom from ARC at five years that was:
– 63.8% in AFX/ AFX2 device cohort
– 55.5% in comparator endografts
There was no clinically significant difference in aneurysm-related mortality, all-cause mortality, rupture, secondary interventions, and type 1 and type 3 endoleaks between the two cohorts
– The type 3 endoleak rate for the AFX/AFX2 device cohort was 1.5% at five years and was not statistically different from the comparator devices
– The type 2 endoleak rate reached a statistically significant lower rate at 21.2% at five years for the AFX2
First patient
enrolled in PROWL registry study using Pounce thrombectomy system
Surmodics has announced enrolment of the first patient in PROWL, the Pounce thrombectomy system retrospective registry. PROWL is an open-label, retrospective, multicentre US registry of the Pounce system for the nonsurgical removal of emboli and thrombi in the peripheral arterial vasculature.
The registry will collect real-world efficacy and safety outcomes data for endovascular interventions using the Pounce system for up to 500 patients at up to 30 sites. Sean Lyden, chairman of the Department of Vascular Surgery, Cleveland Clinic (Cleveland, USA) and Joseph Campbell, interventional cardiologist, OhioHealth (Columbus, USA) are national co-principal investigators. The first site to enrol a patient in the registry study was Baton Rouge General Medical Center (Baton Rouge, USA).
“We are delighted to be the first site to enrol a patient in the PROWL registry,” said Joseph Griffin, vascular surgeon at the Vascular Specialty Center and Baton Rouge General Medical Center.
“In our experience, the Pounce system promptly removes peripheral arterial clot in a single treatment session while reducing the need for thrombolytic drugs and subsequent intensive care unit stays. We are eager to help track outcomes in this important study.”
“We have long needed better tools to help us resolve acute limb ischaemia in a simple and effective manner, without the use of multiple adjunctive treatments,” he added. “In this respect, our experience with the Pounce system has been quite positive.”
PROWL’s primary efficacy endpoint is procedural success, while the primary safety endpoint is the incidence of device-related major adverse events in the 30 days post-procedure.
“Acute limb ischaemia from arteries blocked by thrombus or embolus is an urgent threat to both limb and life,” said Gary Maharaj, president and CEO of Surmodics. “With hospitals increasingly short on staff and beds, physicians need a simple and effective tool that lets them restore arterial flow right on the table without resorting to time-consuming and costly adjunctive treatments. We are confident the PROWL registry will demonstrate these exceptional attributes of the Pounce system in real-world clinical practice.”
Results from PROMISE II pivotal trial suggest “transformational value” of deep vein arterialisation in no-option CLTI patients
Results from the PROMISE II pivotal trial investigating transcatheter arterialisation of the deep veins using
the LimFlow system in so-called no-option chronic limb-threatening ischaemia (CLTI) patients were recently published in the New England Journal of Medicine (NEJM).
The publication confirmed an amputation-free survival rate of 66% at six months, which exceeded the trial’s primary endpoint target of 54%, as reported by co-principal investigator Daniel Clair (Vanderbilt University, Nashville, USA) at the 2022 Vascular Interventional Advances (VIVA) meeting (31 October–3 November, Las Vegas, USA).
PROMISE II—multicentre, prospective and single-arm—included 105 patients with CLTI. The pool bore a median age of 70, 33 (31.4%) were women and 45 (42.8%) were Black, Hispanic, or Latino.
Transcatheter arterialisation of the deep veins was performed successfully in 104 patients (99.0%), the researchers report in NEJM. At six months, 66.1% of the patients had amputation-free survival. “Limb salvage (avoidance of above-ankle amputation) was attained in 67 patients (76.0% by Kaplan-Meier analysis),” they write. “Wounds were completely healed in 16 of 63 patients (25%) and were in the process of healing in 32 of 63 patients (51%). No unanticipated device-related adverse events were reported.”
Patients enrolled in PROMISE II “were representative of real-world patients,” including those with dialysisdependent chronic kidney disease (CKD) and Rutherford class 5 or 6 wounds—groups “routinely excluded” from vascular device studies, the trialists noted in the discussion section of their paper.
Prespecified subgroup analyses indicated a difference between the 19 patients with dialysis-dependent CKD—who had amputation-free survival of 36.8%—and the 86 patients who did not (72.7%), the authors report. Similarly, the mortality rates among these groups of patients were 36.2% (dialysis dependent) and 8.6%, they show.
“Results of a prespecified subgroup analysis were aligned with those of previously published outcomes indicating an increased risk of death after peripheral arterial revascularisation procedures among patients who were undergoing dialysis,” they write.
“Although the incidence of limb salvage was similar between patients who had dialysis-dependent CKD and those who did not, mortality appeared to be greater in the population with dialysis-dependent disease.
27 Market Watch Issue98 | June 2023
AFX2 system
Paul Gagne
Vein becoming artery with LimFlow crossing stent
Product News


arteriovenous (AV) access in haemodialysis.
Penumbra launches new Red 43 reperfusion catheter for mechanical thrombectomy
Penumbra recently announced the launch of the latest addition to its Red family of catheter devices for mechanical thrombectomy, the Red 43 reperfusion catheter.
According to the company, this device is intended to take distal aspiration “to the next level” with optimised lumen occupation as well as a soft distal design that allows for enhanced and compliant delivery in tortuosity.
With a 0.043-inch lumen, Red 43 provides powerful distal aspiration alongside the Penumbra Engine and features Redglide technology as part of its advanced hydrophilic coating for smooth trackability.
As per the company’s website, additional features of this newly launched device include:

A 1.52mm (0.060-inch) outer dimension: low profile and atraumatic design for distal deliverability
Precision tip: articulating marker band with short polymer tip design for optimal visualisation and placement
Full-length polytetrafluoroethylene (PTFE) liner: designed for durability and lumen integrity under powerful aspiration

Proximal hybrid stainless steel and nitinol coil wind: engineered to provide optimal support and softer profile atraumatic navigation
Humacyte’s

HAV receives
US FDA’s Regenerative Medicine Advanced Therapy designation for urgent arterial repair

Humacyte has been recently granted the US Food and Drug Administration’s (FDA) Regenerative Medicine Advanced Therapy (RMAT) designation for its Human Acellular Vessel (HAV) for urgent arterial repair following extremity vascular trauma.
The US FDA’s RMAT designation is for breakthrough therapy of regenerative medicine. The designation allows for more interactions with the US FDA and expedited development and review of regenerative medicine products within the USA, including the potential for a priority review process for a Biologics License Application (BLA). This is the second RMAT designation granted by the US FDA for Humacyte’s HAV, in addition to a previous RMAT granted for
“We are delighted to receive our second RMAT designation from the [US FDA],” said Cindy Cao, chief regulatory officer at Humacyte. “The RMAT designation for the HAV in our lead indication of vascular trauma is an important milestone. This designation will further enhance our communication with the US FDA and will provide us with a higher likelihood for an expedited review of our planned upcoming BLA filing.”
Humacyte’s HAV is designed to be a universally implantable vascular conduit for use in vascular repair. Importantly, the HAV has shown a low rate of infection in clinical trials, making it well-suited for use in settings such as vascular trauma where wounds may be contaminated with foreign material. The HAV is designed to be available off the shelf and ready whenever surgeons need it, potentially saving valuable time and potentially improving patient outcomes in cases requiring urgent vascular repair, for both civilians and military personnel.
Humacyte is nearing the completion of enrolment in its Phase 2/3 V005 clinical trial of the HAV in the repair of civilian vascular trauma, a study that is being conducted at level 1 trauma centers in the USA and Israel. Currently, a total of 66 patients have received the HAV in the V005 trial, including 49 patients belonging to the primary endpoint population. Humacyte plans to file a BLA with the US FDA later in 2023.
The HAV is an investigational product and has not been approved for sale by the FDA or any other regulatory agency, Humacyte advises.
(University Hospital Innsbruck, Innsbruck, Austria). Terumo Aortic details that Moore was able to access the device through the Health Canada Special Access programme.
The lead centre in Europe for this hybrid procedure, the company states, is the University Heart Center in Hamburg, Germany, under the direction of Sebastian Debus.
Moore commented: “This unique hybrid graft was designed through Terumo Aortic’s custom device programme, specifically for the patient we were treating. With no other device with similar technology currently available globally for thoracoabdominal aortic repair, the Thoracoflo graft is designed to reduce the risk of complications associated with thoracotomy and extracorporeal circulation. This is the first time the device has been implanted in North America; it was easy to implant, and the procedure was uneventful and straightforward. The patient is recovering well with no complications postoperatively.”

John Canning, chief technology and marketing officer at Terumo Aortic said: “This expansion into North America represents a significant commitment to developing patient-specific solutions to treat a wider group of patients as part of our comprehensive surgical, endovascular and hybrid portfolio.”
Terumo Aortic relays that Thoracoflo incorporates a combination of Terumo Aortic’s Gelweave woven polyester grafts and ring-stent technology to fit the patient’s specific anatomy.
Surmodics announces successful first patient use of Sublime radial access microcatheter
Surmodics has announced that Ankur Lodha (Cardiovascular Institute of the South, Lafayette, USA) and Pradeep Nair (Cardiovascular Institute of the South, Houma, USA) were the first physicians to use the company’s Sublime radial access microcatheter.
The Sublime microcatheter is in limited market evaluation, a press release notes. The full suite of Sublime microcatheters will be launched in 2024. The Sublime portfolio will include the industry’s first suite of 0.014”, 0.018”, and 0.035” highperformance peripheral microcatheters.
200cm and compatible with 0.014”, 0.018”, and 0.035” guidewires, the press release details that the Sublime microcatheter is made with Surmodics’ Pristyne hydrophilic coating for lubricity to optimise device trackability through vessel tortuosity. The device’s dual stainless steel, locked-braid layers work in unison to optimise torque control, and to push transmission, and deliverability to distal target lesions, the company adds. The microcatheters are available in straight or angled tip configurations. The Sublime 0.014” and 0.018” microcatheters can be telescoped through the 0.035” Sublime microcatheter to provide additional back-up support when navigating extreme tortuosity or heavily stenosed lesions, the press release continues.
“This successful first use of our Sublime microcatheters is a major milestone, not only for Surmodics, but for the countless patients who stand to benefit from peripheral arterial treatment,” said Gary Maharaj, president and CEO of Surmodics. “For years, torqueable microcatheters have enabled coronary operators to overcome the most extreme challenges presented by complex arterial disease. We are pleased to bring this industry-first capability to peripheral interventions.”
Getinge receives US FDA premarket approval for the iCast covered stent system

Getinge’s iCast covered stent system has received premarket approval from the US Food and Drug Administration (FDA) for the treatment of patients with iliac arterial occlusive disease.
Iliac arterial occlusive disease is a type of peripheral arterial disease (PAD), which affects 8 million people in the USA. As the world population ages and rates of diabetes and obesity rise, it is estimated that more people will be affected with iliac artery disease.
Terumo Aortic announces first implant of custom-made thoracoabdominal hybrid device in North America
Terumo Aortic recently announced the first North American implant of a custom-made hybrid device, Thoracoflo. A press release notes that the device is used to treat patients with thoracoabdominal aortic disease using a less invasive surgical technique than traditional open surgical repair.
This thoracoabdominal repair procedure using Thoracoflo was carried out by Randy Moore (University of Calgary, Calgary, Canada). Moore and the team at University of Calgary were supported by Sabine Wipper
“For peripheral as well as coronary interventions, radial access is safer than femoral access and much preferred by patients,” said Lodha. “I am pleased to report that the Sublime microcatheter performed exceptionally well during our first uses of the device in treating peripheral arterial disease.”




“The lack of long-length, highperformance catheters for peripheral procedures has slowed adoption of radial access for treatment of lower extremity artery disease,” added Nair. “Sublime microcatheters will fill a major gap in the peripheral intervention toolkit, including for procedures from access sites other than the wrist.”
Available in five lengths from 65 to
“We are pleased that the iCast stent system is approved in the USA for use in iliac arteries to benefit an even greater number of patients,” says Elin Frostehav, president of acute care therapies at Getinge. “The global market for covered stents is growing at an annual rate of 5%. Getinge will continue to ramp up capacity throughout the year in order to meet the demand.”
The iCast covered stent system, which is sold outside the USA under the brand name Advanta V12, has been used by clinicians for 20 years and is the most clinically evaluated balloon expandable polytetrafluoroethylene (ePTFE)-covered stent in the world, with clinical data published in more than 550 articles.
Thoracoflo
Red 43
iCast
REGISTER BY JULY 17 TO SECURE EARLY TUITION RATES
VIVA-FOUNDATION.ORG/REGISTER









VASCULAR INTERVENTIONAL ADVANCES



October 30 - November 2, 2023
Wynn Las Vegas
VENOUS ENDOVASCULAR INTERVENTIONAL STRATEGIES
October 28 - 30, 2023
Wynn Las Vegas
THE GLOBAL EDUCATION COURSES FOR VASCULAR MEDICINE AND INTERVENTION
Presented by The VIVA Foundation
Industry News

Bentley buys key suppliers and engages employees in planned IPO
Bentley has bought its main supplier, the Switzerland-based Qmedics, Bentley has recently announced in a press release. It also announced its plan of initial public offering (IPO), which is planned for autumn/winter 2023/2024, depending on market conditions.
Qmedics manufactures approximately 80% of all balloon catheters used in conjunction with Bentley’s covered stents. Bentley, in turn, is responsible for about 70% of the Swiss company’s sales.
The acquisition, which was signed on 21 April and will come into effect on 3 July, will enable Bentley to secure the central supply chain for balloon catheters in the long term. In addition to balloon catheters, Qmedics has a complete portfolio of self-expanding stents for peripheral endovascular procedures. The acquisition of Qmedics thus represents an opportunity for Bentley to accelerate its expansion into the field of interventional radiology (IR).
Anita Patteet, CEO of Qmedics,
Conference calendar
6–9 June
Leipzig Interventional Course (LINC) 2023
Leipzig, Germany leipzig-interventional-course.com
14–17 June
Society for Vascular Surgery (SVS) Vascular Annual Meeting 2023 National Harbor, USA vascular.org/vam-2023
22–24 June

23rd European Venous Forum (EVF) Annual Meeting Berlin, Germany europeanvenousforum.org/index.php/meetings
said—“I am very pleased that the future of Qmedics is in good hands with Bentley. Together, we will certainly be able to celebrate further market successes.”
Sebastian Büchert, CEO at Bentley, said—“With the acquisition of Qmedics, we not only ensure the availability of one of our most important components, but at the same time complete our newly created product portfolio for [IR].”
Bentley’s planned IPO intends to be completed on the Swedish stock exchange, a part of Nasdaq Nordic, an offshoot of the US technology exchange Nasdaq. A Swedish holding company was set up for the upcoming IPO, which is temporarily called BeThundered AB. This holding company becomes 100% owner of Bentley Innomed GmbH from Hechingen and Qmedics AG, which thus operates as Bentley’s sister company. The pre-IPO, the first step in an IPO, is scheduled for the summer 2023. The actual IPO is planned for the autumn/winter 2023/2024, depending on market conditions.
Bentley is also launching a
29–30 June
British Society of Endovascular Therapy (BSET) Annual Meeting 2023 Wotton-under-Edge, UK bset.co.uk/meetings/bset-annualmeeting-2023
9–13 September
Cardiovascular and Interventional Radiological Society of Europe (CIRSE) Annual Congress 2023 Copenhagen, Denmark cirsecongress.cirse.org/about/ theannualcongress
€15million employee programme to make all of its employees shareholders. Every employee has received a promise to receive shares worth around 400€ (±100€) per month of their affiliation with the company at the time of the IPO. Büchert explained—“Bentley’s management is very pleased that the previous shareholders have agreed to give the Bentley staff this share gift. Our employees really deserve this for their great work over the past few years.”
AVS’ pulsatile IVL technology attracts an additional US$8.8 million to close US$28.8 million Series B round

AVS has announced that it closed an additional US$8.8 million in new financing, bringing its Series B round to US$28.8 million total.
A press release reports that the funding will continue to support clinical trials for the company’s device for pulsatile intravascular lithotripsy (PIVL) in peripheral cases, while advancing preclinical work for an expanded indication in coronary cases.



“We are pleased to see the investor excitement around this technology,” said Mark Toland, chairman of the board for AVS.
“Intravascular lithotripsy represents an emerging therapy that demands new solutions for patients with severely

calcified arterial disease. With the support of our partners, we can continue our work toward US approval for both peripheral and coronary applications.”
AVS notes that it successfully enrolled, treated and collected positive 30-day follow-up with patients in a first-in-human study, the POWER PAD I clinical trial, in September 2022.

The prospective, single-arm, multicentre feasibility study is evaluating the technical and clinical success of the Pulse IVL system for treating patients with calcific femoropopliteal arteries.
The Pulse IVL system is a novel, balloon-based platform that expands calcified lesions by gently shattering calcium with pressure waves in frequent bursts, all through a single device, a press release details.
17–21 September
UIP 2023 World Congress Miami Beach, USA myavls.org/annual-congress-2023.html
26–29 September
European Society for Vascular Surgery (ESVS) Annual Meeting 2023 Belfast, UK esvs.org/events/annual-meeting/annualmeeting-2023

2–4 October

CX Aortic Vienna Vienna, Austria cxaortic.com
29 October–2 November

The VEINS (Venous Endovascular Interventional Strategies) and VIVA (Vascular Interventional Advances) 2023
Las Vegas, USA viva-foundation.org/future-meetings
8–10 November
Paris Vascular Insights (PVI) Paris, France paris-vascular-insights.com

14–18 November
VEITHsymposium 2023 New York, USA veithsymposium.org/index.php
June 2023 | Issue98 30 Market Watch Vascular News is a trusted, independent source of news and opinion in the vascular and endovascular world. Sign up for a free print subscription* and e-newsletter subscription** www.vascularnews.com *Available for US and EU readers only ** Available worldwide
AVS console

CONTROVERSIES CHALLENGES CONSENSUS INNOVATION EDUCATION EVIDENCE Controversies Update Vascular & Endovascular HOLD THE DATE CXSYMPOSIUM.COM 23–26 APRIL 2024 TUESDAY-FRIDAY NEW VENUE, E xCeL LONDON, UNITED KINGDOM Peripheral Arterial Controversies Aortic Controversies Acute Stroke Controversies Vascular Trauma Controversies Venous & Lymphatic Controversies Vascular Access Controversies The Hurting Leg Controversies