02 Guest editorial
Vascular surgeons: The ‘oncologists’ of surgery
11 Comment & Analysis
Bright future predicted for Journal of Vascular Surgery internship program


02 Guest editorial
Vascular surgeons: The ‘oncologists’ of surgery
11 Comment & Analysis
Bright future predicted for Journal of Vascular Surgery internship program

The first results from the BEST-CLI randomized controlled trial (RCT) of 1,830 patients show that surgical bypass with adequate single-segment great saphenous vein (GSV) is a more effective re vascularization strategy for patients with chronic limb-threatening ischemia (CLTI) who are deemed to be suitable for either an open or endovascular approach. Researchers also found that both strategies can be accomplished safely and are effective for treatments for CLTI. Further, the investigators urge that patients with CLTI who are can didates for limb salvage should undergo an evaluation of surgical risk and conduit availability. “Bypass surgery with adequate single-segment saphenous vein should be offered as a first-line treatment option for suitable candidates with CLTI as part of a fully informed shared deci sion-making. Level-one evidence from BEST-CLI does not support an
endovascular-first approach to all patients with CLTI. In patients without a suitable single-segment saphenous vein, both surgical and endovascu lar strategies are effective in treating patients with CLTI, so we believe that there is a complementary role for both revascularization strategies in these patients,” they say, bringing the “quality of vein” back into the center of discussion on revascularization strategy.
The co-principal investigators—Matthew Menard, MD, director of the vascular and endovascular fellowship program at Brigham and Women’s Hospital in Boston; Alik Farber, MD, chief of vascular and endovascular surgery at Boston Medical Center; and Kenneth Rosenfield, MD, section head of vascular medicine and intervention at Massachusetts General Hospital, also in Boston—note that this is the largest RCT comparing revascularization treatment strategies in patients with CLTI and will pro vide important information regarding the management of these patients.

Farber presented the much-anticipated clinical results, and Menard the quality-of-life analysis, from BEST-CLI at the American Heart As sociation (AHA) Scientific Sessions (Nov. 5–7) in Chicago. The results were simultaneously published in the New England Journal of Medicine BEST-CLI (Best endovascular versus best surgical therapy for pa tients with CLTI) randomized patients with CLTI and infrainguinal

15 Drug technology New VQI paclitaxel data shed light on challenging fempop anatomy
16 Presidential address Robert Rhee talks evolution during Eastern Vascular Society address
THE SOCIETY FOR VASCULAR Surgery (SVS) Research Council has updated its top-10 research priorities, originally published in 2011, with patient-centered outcomes and personalized vascular care at their core and a new emphasis on healthcare disparities.
The priorities help the Society target research proposals for its own grants and awards, and provide external organizations with what SVS members regard as important goals, said Edith Tzeng, MD, and Matthew Corriere, MD, of the Research Council.
The updated areas of research focus on aortic, carotid, lower extremity arterial (two priorities each) and venous disease, along with dialysis access, healthcare disparities and medical management of vascular disease (one priority each).
The new priorities add disparities as well as vascular medicine/vascular health as areas of focus, highlighting a shift in emphasis over the past decade. “We can’t focus on everything,” said Corriere. “Part of our discussion was ‘what do we want to call attention to in the updates?’”
The updated priorities “reflect our increasing awareness of the need to understand vascular disease pathogenesis and prevention in the context of a diverse
See page 18–19
Bernadette Aulivola, MD | O. William Brown, MD | Elliot L. Chaikof, MD, PhD
| Carlo Dall’Olmo, MD | Alan M. Dietzek MD, RPVI, FACS | Professor HansHenning Eckstein, MD | John F. Eidt, MD
| Robert Fitridge, MD | Dennis R. Gable, MD | Linda Harris, MD | Krishna Jain, MD | Larry Kraiss, MD | Joann Lohr, MD
| James McKinsey, MD | Joseph Mills, MD | Erica L. Mitchell, MD, MEd, FACS
| Leila Mureebe, MD | Frank Pomposelli, MD | David Rigberg, MD | Clifford Sales, MD | Bhagwan Satiani, MD | Larry Scher, MD | Marc Schermerhorn, MD | Murray L. Shames, MD | Niten Singh, MD | Frank J. Veith, MD | Robert Eugene Zierler, MD
Christopher Audu, MD
Executive Director SVS Kenneth M. Slaw, PhD
Adam Tanious, MD, discusses how he dealt with “end-stage vascular disease” during patient and family consultations and conversations for the first time as an attending vascular surgeon.

supporting personnel capable of handling such complex pathol ogies. Their understanding of their pathology is understandably limited, and they appreciate the gravity of the situation only as it applies to need for their transfer. As a trainee, I’d get fairly excited about this pathology and the opportunity to undertake a major vascular surgery to cure the patient of their infection that could (and most likely would) result in death in the not-too-distant future. When consenting them and their families for their proce dure, we were trained to be as accurate as accountants when it came to risks associated with the specific procedure each patient would need while still being human—talking them through the potential outcomes and try to paint a picture of what life would look like should the patient make it through their procedure.
Directorof Marketing & Communications Bill
Maloney Managing Editor SVS Beth Bales Marketing & Social Media Manager Kristin CrowePublished by BIBA Publishing, which is a subsidiary of BIBA Medical Ltd.
Publisher Roger Greenhalgh
Content Director Urmila Kerslake
Managing Editor Bryan Kay bryan@bibamedical.com

Editorial contribution
Jocelyn Hudson, Will Date, Jamie Bell, Clare Tierney, Anthony Strzalek, Aaron Kudhail and Adam Pearce
Design Terry Hawes Advertising Nicole Schmitz nicole@bibamedical.com
Letters to the editor vascularspecialist@vascularsociety.org
BIBA Medical, Europe 526 Fulham Road, London SW6 5NR, United Kingdom
BIBA Medical, North America 155 North Wacker Drive – Suite 4250, Chicago, IL 60606, USA
Like any good presentation I feel obligated to start with my dis closures: 1) I am married to a woman who decided to pursue a separate fellowship in bioethics, even after a fellowship in pediatric anesthesia. This means that every time I come home and start to discuss a patient’s tough clinical situation, I am invariably met with the question, “Did you discuss all their options with them?” And, 2) I just celebrated my one-year anniversary of being an attending, and, while my confidence slowly grows with each day, I am still always a bit apprehensive when it comes to any major vascular case, from a carotid endarterectomy to a complex bypass—and particularly open aortic surgery.
Allow me to present Patient X, a 70-year-old male who was transferred to our hospital while I was on call. He presented to an outside hospital with obstipation of several days’ duration with associated abdominal pain. His history was notable for an aortic endograft placed for aneurysm four years prior which was explanted and replaced with a rifampin-soaked interposition graft for infection in the last two years. The outside physicians were concerned mostly about his bowel obstruction but thought something was “off” about how the bowel was associated with the graft. Like most centers, we accepted the patient to get them to our hospital and figured we would get the necessary teams involved upon arrival. Upon his arrival to our hospital, we got our gastrointestinal surgery colleagues involved and began working through his history and current status. His initial labs showed a severe leukocytosis and within 24 hours his blood cultures were growing pseudomonas. Additionally, within 24 hours of present ing to our hospital, he began to show signs and symptoms of a colovesicular fistula. A nuclear medicine study was done showing definitive uptake at the site of his aortobifemoral bypass.
Vascular Specialist is the official newspaper of the Society for Vascular Surgery and provides the vascular specialist with timely and relevant news and commentary about clinical developments and about the impact of healthcare policy. Content for Vascular Specialist is provided by BIBA Publishing. Content for the News From SVS is provided by the Society for Vascular Surgery. The ideas and opinions expressed in Vascular Specialist do not necessarily reflect those of the Society or the Publisher. The Society for Vascular Surgery and BIBA Publishing will not assume responsibility for damages, loss, or claims of any kind arising from or related to the information contained in this publication, including any claims related to the products, drugs, or services, or the quality or endorsement of advertised products or services, mentioned herein. | The Society for Vascular Surgery headquarters is located at 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018.
| POSTMASTER: Send changes of address (with old mailing label) to Vascular Specialist, Subscription Services, 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. |
RECIPIENT: To change your address, e-mail subscriptions@bibamedical.com | For missing issue claims, e-mail subscriptions@bibamedical. com. | Vascular Specialist (ISSN 1558-0148) is published monthly for the Society for Vascular Surgery by BIBA Publishing. | Printed by Vomela Commercial Group | ©Copyright 2022 by the Society for Vascular Surgery
To summarize, we have a 70-year-old man with a prior infected endovascular aneurysm repair (EVAR) that was explanted and repaired with a rifampin-soaked Dacron graft which was now also infected and causing a bowel obstruction, leading to sepsis, in addition to a colovesicular fistula.
At this point I’d like to introduce the term “end-stage vascular disease” and, with the readers’ permission, apply it to Patient X. I do not make this statement lightly, nor mean anything offensive by it. My wife and I were discussing patients one evening and she made a comment that really stuck with me. She equated vascular surgery to medical oncology in the sense that in the world of medicine, medical oncology patients often have very tough pathology to treat, “wins” are hard to come by, and any intervention, more often than not, alters the future quality of life for the patient in addition to duration.
Furthermore, there are patients that present with terminal disease who despite all the best efforts and current medicine/technology available, intervention is unlikely to alter the inevitable outcome.
I consider myself more than fortunate to have trained at some of the best institutions in the country where the above story is only all too common. These patients present to our hos pitals as we are usually the only facility in the state/region with the appropriate recourses and
The next few weeks would proceed in a fairly standard fashion including a complex and lengthy surgery with major blood loss; some form of a post-operative complication; prolonged hospital stay; and a transition to inpatient rehabilitation. While the life of a trainee meant that I was usually on a different service/rotation by the time these patients came back for follow-up, my particular interest in these patients infected aortic pathology made me track their outcomes and, not surprisingly, only about 50% of these patients ever made it back for their follow-up once discharged, with about 25% never making it out of the hospital.
So, 13 months into practice, I am presented with Patient X and it is my job to discuss with him our options on how to proceed, knowing that regardless of his decision, I am about to affect the course of not just his life, but the life of all his friends and family. If I’m being honest, I was torn. Here I am talking to a man who just retired and had grand plans to finally enjoy his well-earned retirement with his wife by traveling and experiencing the world. If I steered him towards surgery, we all know what his life would look like for the next year as well as the associated numbers as stated above. But what was my alternative suggestion? What would my peers and partners think? Would they think I was simply scared to tackle this type of procedure? This would be the biggest case I could have done as junior faculty and I know it is the only “life-sustaining” option? We are taught to offer surgery when the benefits outweigh the risks. The risk of not operating in patients with end-stage vascular disease is most often death. This could be an imminent death, a death within a certain amount of time, or eventual death—but death is the conclusion.
I kept thinking about what Patient X’s life would look like and how he would remember his final days should we proceed with surgery. Then I discussed the case with my wife. Physicians,
specifically surgeons, often fall victim to the following sentiment “[doctors] will do everything they can to prolong someone’s life… many medical practitioners are not trained to handle conversa tions that focus on quality of life or relief of pain and suffering, and instead lean toward recommending their own treatments.”
This is a quote from Jeffrey Schnipper, MD, research director for the Division of General Internal Medicine and Primary Care at Brigham and Women’s Hospital, taken from an article about physicians’ lack of understanding regarding end-of-life care. In a study titled “Surgeons’ perceived barriers to
There are patients who present with terminal disease that, despite all the best efforts and current medicine/technology available, intervention is unlikely to alter the inevitable outcomeAdam Tanious




The SVS Foundation has been guided by the three long-term pillars of research and innovation, com munity vascular care and patient education, and disease prevention. Recently, the Foundation added a fourth pillar—for diversity, equity and inclusion (DEI) initiatives. It will emphasize, among other projects, research into healthcare disparities and care delivery solutions, scholarships and career advancement for under-represented minority vascular surgeons, and workforce development.
“DEI is an important cornerstone of the Society for Vascular Surgery itself and we applaud adding diversity, equity and inclusion as a bedrock pillar for the Foundation as well,” said Vincent Rowe, MD, chair of the SVS DEI Committee.
“This helps us support our com munity of vascular surgeons,” said Palma Shaw, MD, co-found

 Rowe
Rowe
er of the SVS Women’s Membership Section. “We are investing into the future of vascular health with programs for our diverse communities and helping the Society more closely resemble the patient population. People want a surgeon who looks like them.”

SVS Foundation Chair Peter Lawrence, MD, said: “The new pillar reaffirms the Society’s commitment to DEI and enables the SVS Foundation to serve as the portal for initiatives of SVS’ many regional societies, such as diversity scholarships or attendance at training courses.”
Early plans for DEI initiatives include targeted scholarships, awards and research grants for diversity candidates, research projects focused on healthcare disparities or bringing programs to under-served areas.
The new pillar highlights, among other tenets, re search into healthcare disparities—one of the updated SVS research priorities.
The new pillar reaffirms the Society’s objectives, sup ported by the DEI Task Force which now has become an ongoing committee as well as a summer DEI sum mit, with outcomes to be announced soon ahead of a second summit planned for January 2023. In addition, the Society’s new research priorities added healthcare disparities as one of seven important topic areas. The focus in that area is evaluating “interventions aimed at improving vascular health in all socioeconomic, racial and ethnic populations.”
Both Rowe and Shaw pointed to how commemora tive months—Black History Month, Women’s History Month, Pride Month and Hispanic Heritage Month, among them—celebrate the diversity of modern life. “We mark these months and others, to celebrate the diverse voices of the vascular community,” said Shaw.
“We will be funding the future of vascular health through a lot of these initiatives,” said Rowe. “We want to grow and nurture these initiatives, while we grow and cultivate our increasingly diverse vascular workforce.”
THE COVID-19 PANDEMIC EXPOSED LINGERING MISTRUST IN the U.S. healthcare system among patients from minority communities as physicians continue to confront the conundrum of healthcare disparities in terms of outcomes alongside a lack of diversity in clinical trials, a roundtable discussion at Vascular Interventional Advances (VIVA) 2022 in Las Vegas (Oct. 31–Nov. 3) heard.
Vincent Rowe, MD, chair of the SVS diversity, equity and inclusion com mittee, told the gathering, entitled, “How to be a trialist,” that despite a National Institutes of Health (NIH) intervention nearly 30 years ago aimed at recruiting more minorities into clinical research, “we haven’t seen much change.”
“We’ve talked a lot about clinical trials, their importance and how they have to be applicable to the full population of patients that we deal with,” he said. “Unfortunately, there are still a lot of disparities in our outcomes, so we’re going to need a diverse cohort to be able to understand the differences.”
Rowe pointed to a study that looked at patients eligible for cardiometabolic trials. The problems that emerged, mostly from the patient side, included lack of awareness, lack of information, mistrust, and a lack of comfort with the process. He highlighted how historical experiences with the healthcare system have led to low levels of trust, especially among the Black community. “And if you think that it is all over and things have gotten better, I think the COVID pandemic was a perfect microcosm of this mistrust that happened,” he said.
Rowe said combating these problems is multifactorial but suggested great er diversity among site investigators and cultural competency as among potential remedies. “You need people in your trials to be applicable to all the patients that you’re seeing,” Rowe said, demonstrating how enrollment for the BEST-CLI trial at his institution among the Hispanic community was bolstered by the involvement of a colleague fluent in both the culture and lan guage. “There needs to be some kind of cultural competency,” but that does not require race concordance, he added. “There just needs to be someone talking to them that’s technically competent and understands the culture.”
The role of referring physicians, too, is key, in order that they receive the support required “to send us patients from a culturally diverse environ ment,” Rowe told the VIVA gathering. “We’re going to need to increase these patients in clinical trials,” he said. “It may be difficult based on the times we are in. People say they are so entrenched in their views, but I think it is possible—and it can only help to improve the care for all of our patients.”
continued from page 2
palliative and end-of-life care” in the Journal of Palliative Care Medi cine from 2018, 76% of surgeon responders cited no formal training or education in palliative care, while more than one-third cited lack of training in how to forgo life-sustaining measures and communica tion regarding these matters.
What if Patient X’s final days involved a few extra medications to treat symptoms but also family dinners and a trip to an ex otic destination he had always wanted? He would ultimately succumb to his infective process, but did that mean not enjoying the time between then and now? Could we offer a picture that focused on enjoying the time he had instead of “fighting” through the proposed surgical course?
I sat down and had a family meeting with Patient X, his wife, his brother and
sister-in-law. I drew pictures, explained the proposed procedure(s), potential complications, and expected hospital and post-operative course. I laid out a timeline. I was blunt. I was not callous, but I was direct. I then offered some alternatives (af ter discussing with our infectious disease, gastrointestinal surgery, and urology col leagues). I offered Patient X the option of antibiotic therapy and pain medication to treat his symptoms. I painted a picture of what his life would look like through this option’s lenses. I then told everyone in the room that Patient X had my support no matter his decision and that we would do everything in our power to ensure the best outcome regardless of his choice. Then I sat there silently.
What felt like an eternity passed. Patient X broke the silence. He started
by thanking me. All parties asked several questions to understand the details that were pertinent to them. They asked me what I would do. The question I feared but prepared for. I told them that the answer to that question depends on what each individual values. I couldn’t decide for Pa tient X what values were most important to him. All I could do is paint as realistic picture as possible and hope that one option would resonate with them. I told them that I know individuals who would happily select either path based on their values and that there is no wrong answer. They thanked me again and asked for some time to decide.
I felt drained. What had I just done? Was I being a coward? My goal is not to talk all of my complex patients out of their complex surgeries. I do feel strongly
that we as a society, and surgical commu nity, need to focus more on these types of conversations and goals when interacting with our patients and our trainees. Quality of life is a metric more recently making into the literature, but why is it not a course that all medical students are taught or a rotation that interventional trainees must spend one month to counsel patients appropriately about all their options?
I was paged not too long after the con versation… Patient X wanted to go home on antibiotics and take a trip to a city he and his wife had been looking forward to visiting for many years.
ADAM TANIOUS is an associate program director for the vascular surgery residency program at the Medical University of South Carolina (MUSC) in Charleston.
“People want a surgeon who looks like them”
PALMA SHAW
‘There needs to be some kind of cultural competency’Vincent Palma Shaw

Only the Ellipsys vascular access system uses a single point of venous access,1 offering the simplest, most minimally invasive option for arteriovenous fistula (AVF) creation.†1,2 It provides an immediate, suture-free, permanently fused anastomosis1 that is clinically proven to improve longevity3-5 and reduce the risk of complications.3,5
medtronic.com/ellipsys

† Compared to surgical arteriovenous fistulas.
THE SOCIETY FOR VASCULAR SURGERY (SVS) WILL ask voting-eligible members to consider three revisions to article X of the SVS bylaws that would take a step toward change on the SVS Nominating Committee.
In the past several years, the membership of the com mittee, which selects candidates for officer consideration, has expanded from the three most recent past presidents to include four more members: a member of the Strategic Board of Directors, an at-large member elected from among the membership, the vice chair of the Community Practice Committee and the chair of what formerly was called the Leadership and Diversity Committee. There also has been an ex-officio, non-voting representative of the Young Surgeons Committee (now Section).
The referendum changes would keep the Nominating Committee membership at seven, while expanding diversity of perspective. The SVS Executive Board has proposed—and the Strategic Board of Directors has approved—putting the following three changes to the membership for a vote:
◆ Reducing the number of past presidents on the Nomi
nating Committee from three to two; the most current past president, who serves on the Executive Board, will join the Nominating Committee one-year removed from this service
◆ Adding the SVS Diversity, Equity and Inclusion (DEI) Committee chair, or vice chair if the chair is unavailable, as a voting member of the Nominating Committee, replacing the chair of the Leadership Committee. The Leader ship Committee chair was added when the committee’s name was the Lead ership and Diversity Committee, but diversity has since been migrated to the DEI Committee
◆ Adding the chair of the Young Sur geons Section, or the vice chair if the
To help the Society for Vascular Surgery chart a path into the future, members— and non-members alike— are asked to complete an ongoing survey by Nov. 22.
The survey is to help SVS better understand members’ and non-members’ perception of top priorities and professional needs and challenges, as well as their experiences with SVS. This feedback is critical to ensure SVS can best support members over the next three-to-five years.
This survey is intended for both current members and non-members eligible for SVS membership. It should take about 20 minutes to complete. Respondents can enter a drawing to win one of three $100 Amazon gift cards.
Avenue M. Group LLC, an independent market research firm and SVS’ partner for the survey, emailed participation invitations in early November. For information, contact Joanna Bronson at JBronson@ vascularsociety .org. Michael C. Dalsing
chair is unavailable, as a voting member of the Nominating Committee. The Young Surgeons Section chair has been serving as a non-voting ex-officio member
These changes have been proposed and approved to further increase the diversi ty of perspective and voice in the Nom inating Committee process. Because the process for nominating SVS officers for 2022–23 begins in January 2023, this spe cial referendum is being called to ensure changes are implemented in time for the 2023 nominating process and elections.
“We feel it is imperative to broaden the perspective of the group that selects our candidates, to hear from the wide range of voices among our members,” said SVS President Michael C. Dalsing, MD.
“The Strategic Board of Directors feels making this change before our next elec tion cycle is so important, in fact, that we’re taking the unusual step of holding an off-cycle referendum election.”
Online voting on the questions will begin in early December. Only Active and Senior members in good standing are eligible
Read the proposed vascular.
org/2023NomComm BylawsChange
References
1Hull JE, Jennings WC, Cooper RI, Waheed U, Schaefer ME, Narayan R. The pivotal multicenter trial of ultrasound-guided percutaneous arteriovenous fistula creation for hemodialysis access. J Vasc Interv Radiol. February 2018;29(2):149-158.e5.
2Shahverdyan R, Beathard G, Mushtaq N, et al. Comparison of Ellipsys percutaneous and proximal forearm gracz-type surgical arteriovenous fistulas. Am J Kidney Dis October 2021;78(4):520-529.e1.
3Hull JE, Jennings WC, Cooper RI, Narayan R, Mawla N, Decker MD. Long-term results from the pivotal multicenter trial of ultrasound-guided percutaneous arteriovenous fistula creation for hemodialysis access. J Vasc Interv Radiol. Published online June 2, 2022.
4Franco G, Mallios A, Bourquelot P, Jennings W, Boura B. Ultrasound evaluation of percutaneously created arteriovenous fistulae between radial artery and perforating vein at the elbow. J Vasc Access. September 2020;21(5):694-700.
5Mallios A, Bourquelot P, Franco G, et al. Midterm results of percutaneous arteriovenous fistula creation with the Ellipsys vascular access system, technical recommendations, and an algorithm for maintenance. J Vasc Surg. December 2020;72(6):2097-2106.
The Ellipsys system is indicated for the creation of a proximal radial artery to perforating vein anastomosis via a retrograde venous access approach in patients with a minimum vessel diameter of 2.0 mm and less than 1.5 mm of separation between the artery and vein at the fistula creation site who have chronic kidney disease requiring dialysis.
The Ellipsys system is contraindicated for use in patients with target vessels that are < 2 mm in diameter. The Ellipsys System is contraindicated for use in patients who have a distance between the target artery and vein > 1.5 mm.
• The Ellipsys system has only been studied for the creation of an AV fistula using the proximal radial artery and the adjacent perforating vein. It has not been studied in subjects who are candidates for surgical fistula creation at other locations, including sites distal to this location.
The Ellipsys™ system is not intended to treat patients with significant vascular disease or calcification in the target vessels.
• The Ellipsys system has only been studied in subjects who had a patent palmar arch and no evidence of ulnar artery insufficiency.
• Use only with the Ellipsys Power Controller, Model No. AMI-1001.
• The Ellipsys Catheter has been designed to be used with the 6 F Terumo Glidesheath Slender *.
If using a different sheath, verify the catheter can be advanced through the sheath without resistance prior to use.
• Use ultrasound imaging to ensure proper placement of the catheter tip in the artery before retracting the sheath, since once the distal tip of the catheter has been advanced into the artery, it cannot be easily removed without creation of the anastomosis. If the distal tip is advanced into the artery at an improper location, complete the procedure and remove the catheter as indicated in the directions for use. It is recommended that a follow-up evaluation of the patient is performed using appropriate clinical standards of care for surgical fistulae to determine if any clinically significant flow develops that require further clinical action.
• This product is sterilized by ethylene oxide gas.
• Additional procedures are expected to be required to increase and direct blood flow into the AVF target outflow vein and to maintain patency of the AVF. Care should be taken to proactively plan for any fistula maturation procedures when using the device.
• In the Ellipsys study, 99% of subjects required balloon dilatation (PTA) to increase flow to the optimal access vessel and 62% of subjects required embolization coil placement in competing veins to direct blood flow to the optimal access vessel. Prior to the procedure, care should be taken to assess the optimal access vessel for maturation, the additional procedures that may be required to successfully achieve maturation, and appropriate patient follow-up. Please refer to the “Arteriovenous Fistula (AVF) Maturation” section of the labeling for guidance about fistula flow, embolization coil placement, and other procedures to assist fistula maturation and maintenance.
• The Ellipsys System is intended to only be used by physicians trained in ultrasound guided percutaneous endovascular interventional techniques using appropriate clinical standards for care for fistula maintenance and maturation including balloon dilatation and coil embolization.
• Precautions to prevent or reduce acute or longer-term clotting potential should be considered. Physician experience and discretion will determine the appropriate anticoagulant/antiplatelet therapy for each patient using appropriate clinical standards of care.
Potential Adverse Events
• Potential complications that may be associated with creation and maintenance of an arteriovenous fistula include, but may not be limited to, the following:
• Total occlusion, partial occlusion or stenosis of the anastomosis or adjacent outflow vein
• Stenosis of the central AVF outflow requiring treatment per the treatment center’s standard of care
• Failure to achieve fistula maturation
• Incomplete vessel ligation when using embolization coil to direct flow
• Steal Syndrome
• Hematoma
• Infection or other complications
• Need for vessel superficialization or other maturation assistance procedures.
CAUTION: Federal (USA) law restricts this device to sale by or on the order of a physician.
Important Information: Indications, contraindications, warnings, and instructions for use can be found in the product labelling supplied with each device.
“The Strategic Board of Directors feels making this change before our next election cycle is so important, in fact, that we’re taking the unusual step of holding an off-cycle referendum election”
MICHAEL C. DALSING
22
Christopher Audu, MD, and colleagues at the University of Michigan lab in Ann Arbor led by Katherine Gallagher, MD, recently saw the latest paper on their tireless work on macrophage-specific inhibition of the histone demethylase JMJD3 published in a recent issue of Cellular & Molecular Immunology. The vascular surgery resident—and Vascular Specialist editor in charge of trainee issues—tells Bryan Kay about how the research team reached this juncture.

VS: Your team has been prolific in this area of research in vascular science. Can you give us some background on this latest publication?
CA: You’re right. This work builds on a decade of work in the Gallagher lab where we have been studying macrophage immunology to figure out why the diabetic wound envi ronment allows for sustained inflammation. What we have found, over the years, is that inflammation is the first step to wound healing, as we all know. However, in diabetes, key enzymes necessary for stopping inflammation and mov ing into the next phase of wound repair are not made. Our group has been trying to answer why this is by looking at the production of DNA gene regulators that, incidentally, are affected by the diabetic environment, i.e., simply hav ing diabetes changes the gene expression of these critical enzymes. This field of study, epigenetics, applied to wound healing is a nascent field.
VS: What are the key takeaway messages from your findings and their implications for future research work and clinical practice?
CA: In this recent paper, we report the dichotomous nature of a gene regulator called JMJD3, which is overproduced in diabetes. Our takeaways are:
◆ JMJD3 regulates inflammation in both diabetic and non-diabetic wound healing
◆ In diabetic wound macrophages, JMJD3 gets turned on late and stays on
cularized tissue, application of a topical (or other formulation) with a JMJD3 inhibitor could lead to improved diabetic wound healing—thus adding to the armamentarium of therapeutics for this population of patients whom we care for as vascular surgeons.
VS: Your research team worked tirelessly to get this work published— what is next for the team?
CA: Yes, it’s been a lot of work to get to this point, especially since most of the work was done during the height of COVID-19 pandemic restrictions. The next items for the team are really developing that last point: bringing this to the clinic. Right now, our wound healing examples are in mice. While we have a firm mechanistic grip on this, we’d like to take this back to the bedside to— hopefully—start helping patients in a meaningful way. Also on the docket is understanding the immunologic interplay of various other cell types in the diabetic wound milieu so that we identify other targets for therapeutic development. Personally, therapeutic development and design in various vascular pathologies is exactly the kind of work I intend to do as an independent surgeon-scientist.
◆ Persistent JMJD3 expression leads to persistent inflam mation in diabetes via key inflammation pathways such as the Stimulator for Interferon Genes (STING) cascade. This is a novel pathway that is implicated in multiple malignancies but has never been directly linked to wound healing before
◆ Inhibiting JMJD3 in diabetic wound macrophages by us ing nanoparticles leads to significant wound healing im provement by limiting multiple inflammatory cascades
◆ The clinical implications of this work are that it provides a new avenue of therapeutic development for wound healing. So, for instance, should we be able to improve in-line arterial flow and debride diabetic wounds to vas
VS: You recently completed your research fellowship and returned to clinical work. How is the transition going?
CA: Coming back has been refreshing. I missed operating and caring for patients! It’s also been challenging as I had to dust the “rust” off and continue learning. Overall, I would say that I’ve come back from the research fellowship ener gized about how I can contribute to the field as a scientist, and ready to continue learning all that I can so that I can be a competent, confident, and compassionate surgeon. Merging the surgeon-scientist model requires different skillsets and right now, my primary goal is to hone my surgical skillset in my final years of training.
CHRISTOPHERTWENTY-NINE PEOPLE HAVE BEEN selected for development as future leaders of the profession and the Society for Vascular Surgery (SVS).
They represent cohort four of the Lead ership Development Program (LDP), ninemonth-long interactive program designed to help them reach their full potential as leaders and positively impact their workplaces, com munities, the vascular surgery specialty and other important areas of their lives.
Content includes the functional day-to-day behaviors and skills that drive success in lead ership, how and where physicians can lead most effectively in complex health delivery systems, the science and physics of leader
ship, personality styles and emotional intel ligence, strategies to strengthen resilience and avoid leader burnout, as well as conflict resolution and negotiation strategies.
“I think more about switching gears be tween how I interact with colleagues in the operating room compared to clinic, the office, etc.,” said Max Wohlauer, MD, a co hort three member. “It was a very positive experience.” Fellow participant Mark Wheat croft, MD, said the experience “taught me the importance of spending time gathering as much information as possible from the right people before acting, and to think deep ly about strategy development. “I also find the LDP toolkit very helpful with analysis.”
The program also provides four $3,000 Mastery Grants to LDP graduates, permit ting them to continue leadership education.
Selected for 2022–23 are: Clayton Brin ster, MD, of Ochsner Health, New Orleans; Joseph Hart, MD, of Medical College of Wisconsin, Milwaukee, Wisconsin; Sharon Kiang, MD, from VA Loma Linda Healthcare System, Loma Linda, California; and Elisa Greco, of the University of Toronto, Toron to, Ontario, Canada. It is co-sponsored by the Society for Clinical Vascular Surgery (SCVS) and the Vascular and Endovascular Surgery Society (VESS).
See Cohort 4 at vascular.org/LDP.
“Right now, our wound healing examples are in mice. While we have a firm mechanistic grip on this, we’d like to take this back to the bedside to—hopefully— start helping patients in a meaningful way”
AUDU
OF WORK
PUBLICATION IN NASCENT FIELD: ‘THIS IS A NOVEL PATHWAY THAT IS IMPLICATED IN MULTIPLE MALIGNANCIES BUT HAS NEVER BEEN DIRECTLY LINKED TO WOUND HEALING BEFORE’
SURGICAL AUGMENTED intelligence in the form of 3D mapping during complex aortic procedures can decrease radiation exposure, fluoroscopy time and contrast use when combined with real-time fluoroscopic images, a new analysis has established

The results were presented during the 2022 Western Vascular Society (WVS) annual meeting in Victoria, Canada (Sept. 17–20) by Rohini Patel, MD, from the University of California San Diego. The researchers aimed to flesh out whether surgical augmented intelligence can be used to decrease radiation exposure in the operating room.
The retrospective chart review, from 2015–2021, looked at 116 patients who underwent a complex aortic repair— with 76 receiving a procedure using augmented intelligence. The majority underwent physician-modified endograft (PMEG) repair.
“Our group that was treated with augmented intelligence had almost half the amount of radiation exposure, with 1,955mGy compared to 3,755mGy in the non-augmented intelligence group,” Patel told WVS.
The former also saw a decrease in fluoroscopy time of around 56 minutes compared to 87 minutes in the latter group of patients, with contrast use significantly decreased to 122cc from 199cc, she added.
Adjusted analysis showed these significant reductions remained, Patel explained.
“Overall, we believe that surgical augmented intelligence is a way to decrease radiation exposure for the entire team and should be further investigated,” she said.—Bryan Kay
“COLLABORATE, INNOVATE, MENTOR, CHAMPION DEI [DIVERSITY, equity, and inclusion] and relish the opportunity to form deep connections with our amazing patients.” This was the key take-home message delivered by Andres Schanzer, MD, chief of vascular surgery at the UMass Memorial Medical Center in Worcester, Massachusetts, during his Presidential Address at the New England Society for Vascular Surgery (NESVS) 49th Annual Meeting in Newport, Rhode Island (Oct. 14–16).
The topic of Schanzer’s address was “creating a bold new future for vascular surgery,” and one of the keys to this—according to the president—is to focus on the patients. “They are the ones who inspire us to get up each morning, and deal with the challenges that we all encounter every single day.” He expressed his belief that the “rich, long-term relationships” with patients that are “unique to vascular surgery” is what will keep the field “thriving.”
He added that, while the cure for burnout is “different for everyone,” for him it is rounding on his patients once in the morning and once before he heads home in the evening. “That is what keeps me going.”
Schanzer also placed a spotlight on DEI as another crucial point of focus. “As providers, we need to build a workforce that looks more like our patients,” he stressed. “This is not about committees and statements and tweets, it is about hiring, promoting, paying, and acknowledging the indisput able fact that diversity makes us better. If you are not bring ing underrepresented groups to the table in whatever leadership capacity you have, then you are the problem.” The president also remarked on the wider importance of championing DEI: “We need to do this not for ourselves, but for our patients, for our trainees, and for our society.”
Schanzer had a specific message for the trainees and young faculty who are the future of the vascular surgical specialty and will “undoubtedly face challenges” in the years to come. “Remember this,” he said: “Try to take yourself a little less seri ously. I know that I need to do this often.”
In closing, Schanzer summarized: “It is not about any one person or any one career, it is certainly not about mine. It is about our field and advancing it by sticking to and leverageing these key anchor values that makes vascular surgery so special. We can create a bold new future for vascular surgery: it’s go time.”—Jocelyn Hudson
PAST JOURNAL OF VASCULAR Surgery (JVS) group editor-in-chief Peter Gloviczki, MD, invoked his hobby of magic to help illustrate what it requires to take the reins of an illustrious peer-riewed publication like JVS during the Eastern Vascular Society (EVS) annual meeting in Philadelphia (Sept. 29–Oct. 1).
Role models and mentors, commitment, the pursuit of competence, compassion and family support are some of the keys to success, he told EVS 2022 attendees in a keynote lecture.
“A journal editor is competent if she or he has an established record of academic excellence and scientific integrity, is a prolific author ... and has leadership qualities since editing a journal is teamwork,” Gloviczki said.
“My life from being a young Hungarian magician to become editor of JVS has been exciting, sometimes difficult, but ultimately joyful and most satisfying.”—Bryan Kay
HOW DOES VASCULAR SURGERY compare to other specialties in the growth of gender diversity in published research? “Are we leaders in the field, or are we trailing?” Those were questions posed by Monica Majumdar, MD, a general surgery resident at Tufts Medical Center in Boston, during the Eastern Vascular Society (EVS) annual meeting in Philadelphia (Sept. 29–Oct. 1) as she presented new data on the topic. “In the Journal of Vascular Surgery there was a statistically evident linear
increase in female-first authorship over time at only 5.3% in 2010 compared to 20% in 2020. And while there appeared to be some gains in the percentage of last authorship and overall proportion of female authors, these trends were not linear or significant over the 10-year study period,” she said. When compared to ophthalmology and neurosurgery, the trend showing “an encouraging increase in the academic footprint of femaledriven research” in vascular surgery “is significantly greater.”—Bryan Kay
A VASCULAR SURGERY-SPECIFIC composite frailty score was not associated with with risk of surgical site infection in patients undergoing lower-extremity revascularization in a review carried out by Andrew Edsall, MD, a general surgery resident in the Gundersen Health System in La Crosse, Wisconsin, and colleagues.
The research team sought to assess an adapted version of the Risk Analysis Index using the Vascular Quality Initiative (VQI), or the VQI-RAI.
Some 1,130 patients treated between 2007 and 2019 were retrospectively analyzed, with an overall rate of observed surgical site infection of 8.05% noted, most of them superficial, Edsall revealed as he delivered the results at the 2022 Midwestern Vascular Surgical Society (MVSS) annual meeting in Grand Rapids, Michigan (Sept. 15–17).—Bryan Kay
New study shows ‘encouraging increase in academic footprint of female-driven research’
Study finds no link between frailty score and surgical site infection
‘We can create a bold new future for vascular surgery: It’s go time’
In the beginning, it took a little convincing for Anil Hingorani, MD, to come around to the idea that cyclical Topical Wound Oxygen Therapy (TWO2) could be the sort of device he would add to his armamen tarium with some degree of confidence. But then he saw the results in some of his most intractable patients, and he started to see value in the multi-modal approach to wound healing. “Remarkable,” was how the clinical professor of vascular surgery in the Department of Surgery at NYU Grossman School of Medicine in New York described the progress in some of the wounds he treat ed with TWO 2
“We tried hyperbaric oxygen for a while and found that to be helpful in certain pa tients, but hyperbaric oxygen was expen sive,” explains Hingorani, also describing issues around insurance company authoriza tion difficulties, transportation convenience and potential systemic complications. Home oxygen therapy, on the other hand, “circum vented a lot of those problems,” he said.
“We started using TWO2 on our patients who were some of the most difficult—the nonhealing on whom we’d tried every thing,” Hingorani continues, describing how the technology was put to use among a demographic of his patients in south Brook lyn who are challenging both economically and in terms of their level of basic medical education.
“Finally, we said, ‘Let’s try this new prod uct.’ We didn’t know if it was going to work, but we had some patients who had had ul cers for years, and other practitioners had tried to take care of these patients. Then we had some positive results. And we started to notice a consistent pattern. That’s why we started using this TWO2 device. Based upon the fact we had some experience with arterial patients, now we’re using this new product with both arterial and venous pa tients—on diabetic foot ulcers [DFUs]—and we’ve had some very good responses.”
TWO 2 combines supplemental oxygen with non-contact cyclical compression and humidification through a single-use extrem ity chamber system, which is accompanied by a controller and oxygen source.
“For me, what really drives TWO2 is that the machine itself is a little bit different from prior generations in that it not only applies some relatively low oxygen, but also the pressure it puts on is fairly low,” observed Hingorani. The extremity chamber, or boot, extends up to and above the knee, he says, and can be placed over all but occlusive dressings.”
A multinational randomized, dou ble-blinded, placebo-controlled trial to evaluate the efficacy of TWO2 in the treat ment of chronic DFUs (known as the TWO2 Study), led by podiatric surgeon Robert G. Frykberg, DPM, and colleagues, showed that the system was six times as likely to heal a DFU wound at 12 weeks compared to opti mal standard of care alone after adjusting for ulcer severity (p=0.004). The data, published in the peer-reviewed journal Diabetes Care, demonstrated that TWO 2 therapy was “safe, without complications, and provided more durable healing for those who had wound closure compared to optimal standard care alone,” the trial investigators concluded. Ad ditionally, they reported, TWO2 can be “ad ministered by the patient at home without the expense and difficulties of daily travel to a specialized center” and can be combined with other advanced wound care modalities.

Hingorani believes such data—allied to upcoming randomized prospective data be ing collected for publication in the vascular surgery literature—might help to trigger more widespread uptake of the device.
“TWO 2 has shown not only positive wound healing at 12 weeks for DFUs, but also sustained wound healing, especially in patients with DFUs,” he says. “The retro spective data from Ireland for venous stasis ulcers has also shown benefit at 12 weeks for

those patients using the product.”
The system “is not meant to replace what you are already doing,” emphasizes Hingo rani. Rather, the cyclical pressure—applied twice per minute with oxygen—”makes a big difference in some of our patients” ow ing to how that component helps combat edema in the wound, which is, “I think, an underappreciated cause for some of our wounds not to heal,” he adds.

Richard Neville, MD, chairman in the De partment of Surgery and associate director of Inova Heart and Vascular Institute in Falls Church, Virginia, recently sat in on a pre sentation on TWO2, leaving with a resolve

baric oxygen chambers, Neville adds, “this seems different. This is more of a focused raising of oxygen tension in the tissue, which theoretically leads to some advan tages that the hyperbaric chamber may not.
Meanwhile, vascular surgery luminary Frank J. Veith, MD, a limb salvage pioneer for more than half a century, says prelimi nary data behind TWO2 suggest it may hold some promise. He highlighted the device’s advantage of oxygen application in combi nation with compression and moisture ver sus hyperbaric oxygen therapy, describing the early findings on the tri-modality ap proach as a potential indicator that it could prove to be an important adjunct to revascu larization. “The data that I’ve seen, although not conclusive indicates that TWO 2 could prove to be an adjunct to help save limbs that might not otherwise be saved,” says the New York University and Cleveland Clinic professor of surgery, and former Society for Vascular Surgery (SVS) president. “The technology is not going to replace revascu larization, but every little bit helps.”
For Hingorani, one other component stands out: the people behind the equipment at Advanced Oxygen Therapy Incorporated (AOTI). “In south Brooklyn, our patients can be quite challenging,” he says. “A lot of them have problems with not only educa tion in general but medical education is very, very poor, and getting the patients to actu ally comply with a lot of their wound care, diabetes care, venous stasis care, coming into the office even—basic stuff you would think would be fairly standard—can be very challenging.
“Having the people behind it, the compa ny behind it, the personnel behind it, who are willing to work with some patients who
to dig deeper on the positive impression the technology made on him. “I was impressed by this particular technology more than some of the other ones I’ve heard, and I’m hoping that we can investigate it and that it has a role in our system,” he says.
A wound care expert colleague, Vickie R. Driver, DPM, is keen to pursue research on its efficacy, Neville explains. “The right peo ple think highly of it, so we’re going to look to either investigate—or start to use—the technology, and then hopefully we’ll be able to make some presentations in the vascular space.”
While his hospital system has four hyper
may not have all of the resources that oth er patients may have in our neighborhood, makes the biggest difference. We have been very fortunate to have some people behind the product who are willing to go the extra mile with some of our challenging patients to really work with them to get them the products they need, some of the wound care and some of the basic education about how to take care of their wound.
“So, it’s not just the machine, not just the product, not just the oxygen; it’s also the people behind it who matter a lot.”
“ We didn’t know if it was going to work, but we had some patients who had had ulcers for years, and other practitioners had tried to take care of these patients. Then we had some positive results”
ANIL HINGORANIClockwise from top left: Anil Hingorani, Richard Neville and Frank J. Veith
FOR MANY OF THOSE INJURED IN COMBAT, THE transition in care from the Military Health System (MHS) to the Veterans Health Administration (VHA) can be a daunting one, fraught with logistical and clerical challenges. The del uge of administrative tasks as one shifts from active military service to civilian life can drown even capable and medically sophisticated individuals. Certainly, great strides have been made over the past two decades. The Department of Defense and Department of Veterans Affairs have made it a priority to ensure that veterans have access to healthcare. But there currently exists a cohort of patients with vein bypass grafts who are not receiving adequate surveillance.
These patients are well-known to the federal healthcare system, the MHS and the VHA, but for some, injury-specific healthcare has not been provided. When we reviewed nearly 100 veterans who had undergone vein bypasses for com bat-related arterial injuries during Operation Iraqi Freedom and Operation Enduring Freedom, we found only 13% had had an imaging study appropriate for bypass surveillance in the last two years. Even fewer had been seen by a vascular specialist. Among these veterans, 88% had a documented visit with a healthcare provider within the previous two years, including 81% who had seen a primary care provider. Sim ilarly, Haney et al, reporting on data from the VA Vascular Injury Study (VAVIS), could only find imaging studies to con firm patency in 30% of a similar cohort of injured patients.
Few would argue that the best care for patients with a vein bypass includes regular surveillance by a vascular specialist, including imaging of their vein grafts. The specialized care necessary to treat an individual’s unique injuries, which may be complex, may be overlooked when one gets referred to the VHA, as may be the case for those veterans who have suffered vascular injuries over the last two decades. The scope of the current problem is neither small and inconsequential, nor grand and insurmountable. And it’s something we’ve faced before. During and after the Vietnam War, long-term patient follow-up was conducted almost single-handedly by Norman Rich, MD, with the Vietnam Vascular Registry.

Still, the present need for a solution is urgent, as the conse quences of missed care could be catastrophic. Approximately 52,000 United States services members were wounded in action in Iraq and Afghanistan. In those casualties, the rate of vascular injury was 12–17%. Approximately 80% of these injuries occurred in the extremities and 50% underwent re pair, of which interposition or bypass graft with vein were the most common methods. A conservative estimate would suggest that between 700 and 1,500 veterans underwent a vein graft repair for vascular injury. To have nearly 90% of these veterans miss adequate surveillance and vascular care is a true misfortune, even taking into account that a percentage might have received care outside of the VHA or MHS.
The call to action is before us. We suggest a three-pronged approach to recapturing those veterans who have undergone service-related vein bypasses in the past 20 years. First, the MHS and VHA should attempt to identify as many veterans with vein graft repairs as possible. Second, efforts should be made to contact these veterans either directly or through Veterans Service Organizations (VSOs). Lastly, we must ed ucate primary care and other first line non-vascular providers on the need for ongoing surveillance for vascular injuries.
Certainly, these initiatives will face many fiscal, logistical, administrative and psychological challenges. By aligning

veterans who have undergone arterial repair in the past with current vascular surveillance, we can optimize the vascular care of one of our most deserving patient populations.

1. Unpublished Data. Walter Reed National Military Medical Center IRB #927445. Lauria AL, Kersey AJ, White JM, Rsamussen TE, White PW.
2. Haney LJ, Bae E, Pugh MJV, Copeland LA, Wang CP, MacCarthy DJ, Amuan ME, Shireman PK. Patency of arterial repairs from wartime extremity vascular injuries. Trauma Surg Acute Care Open 2020 Dec 24;5(1):e000616. doi: 10.1136/tsaco-2020-000616. PMID: 33409373;
3. Shireman PK, Rasmussen TE, Jaramillo CA, Pugh MJ. VA Vascular Injury Study (VAVIS): VA-DoD extremity injury outcomes collaboration. BMC Surg. 2015 Feb 3;15(1):13. PMID: 25644593;
4. Zierler RE, Jordan WD, Lal BK, Mussa F, Leers S, Fulton J, Pevec W, Hill A, Murad MH. The Society for Vascular Surgery practice guidelines on follow-up after vascular surgery arterial procedures. J Vasc Surg. 2018 Jul;68(1):256–284 PMID: 29937033.

5. Rich NM, Elster EA, Rasmussen TE. The Vietnam Vascular Registry at 50 years: An historical perspective and continuing legacy. J Trauma Acute Care Surg. 2017 Jul;83(1 Suppl 1):S4-S8. doi: 10.1097/ TA.0000000000001545. PMID: 28452900.
6. White JM, Stannard A, Burkhardt GE, Eastridge BJ, Blackbourne LH, Rasmussen TE. The epidemiology of vascular injury in the wars in Iraq and Afghanistan. Ann Surg. 2011 Jun;253(6):1184-9 PMID: 21217514.
7. Patel JA, White JM, White PW, Rich NM, Rasmussen TE. A contemporary, 7-year analysis of vascular injury from the war in Afghanistan. J Vasc Surg. 2018 Dec;68(6):1872–1879. PMID: 29945835
8. Clouse WD, Rasmussen TE, Peck MA, Eliason JL, Cox MW, Bowser AN, Jenkins DH, Smith DL, Rich NM. In-theater management of vascular injury: 2 years of the Balad Vascular Registry. J Am Coll Surg. 2007 Apr;204(4):625-32. PMID: 17382222.
PAUL W. WHITE and ERIN K. GREENLEAF are members of the SVS VA Vascular Surgeons Committee; ALEXIS LAURIA is an SVS surgical resident member, stationed at Walter Reed National Military Medical Center.
This month on Corner Stitch, Christopher Audu, MD, profiles a new and innovative program offered by the Journal of Vascular Surgery (JVS). It’s called the JVS internship program, and with us this month are Ulka Sachdev-Ost, MD, and Anand Brahmandam, MD. Sachdev is a professor of vascular surgery at the University of Pittsburgh, and the founder of the program, now in its second year, and Brahmandam is the chief integrated vascular surgery resident at Yale and was one of the inaugural JVS interns last year.


VS: What is the JVS internship program? How does it work? How do you apply?
AB: The Journal of Vascular Surgery reviewer internship program is a reviewer training program initiated by the editors of the JVS family of journals and Society for Vascular Surgery (SVS). The goal of this program is to train the next generation of vascular surgeons how to review research papers and be fair, balanced and respectful reviewers in their career. During this year-long internship, trainees are paired with a mentor (senior editor for JVS) and are expected to review around 10–12 manuscripts under the guidance of their mentor. In addition to reviewing papers, there are monthly group sessions and lectures focusing on a variety of topics pertinent to the peer-review and editorial process.
The call for applications is typically through social media, SVS connect and/ or Audible Bleeding, and requires a current CV, a brief statement of interest, and two letters of support (one from a program director, and one from a faculty mentor).
VS: What are you looking for in potential JVS interns?
US: We are looking for an individual who brings a unique perspective based on past experiences and background. We are also looking to create a diverse intern “class” from across the country who have experiences in both urban and rural settings. And of course, we are looking for someone who is interested in contributing to the journal for years to come!
VS: What was the impetus for creating a JVS internship program? It seems pretty neat and unique. Are there similar programs at other journals you’re aware of?
US: There are other journals that have internships but it is definitely not common, particularly in a surgical journal. The impetus to start the program was really to help expand the reviewer pool in a way that has a lasting impact. The program allows the next generation of vascular specialists to get exposure to the role of reviewer in a formalized way so that they can offer unbiased contributions to peer review for our society. It also gives them an exposure to journal leadership which is hugely important. I’d love to see our interns become editors of journals themselves one day!
VS: That’s really neat and a great way to generate a pipeline of qualified reviewers. As an alumnus of the program, Andy, how did the JVS internship help you? Do you review for other journals now because of it?
AB: Excellent question! Prior to this program, I had done some ad hoc reviewing for non-vascular surgical journals. The JVS reviewer internship program gave me formal training in reviewing and the entire editorial process. And who better to learn from than the editors of JVS! Not only did this process help me with reviewing papers, but I think it has helped me formulate stronger clinical research and write better. Moreover, I do review for other vascular surgical journals as well now—thanks to the JVS reviewer internship program!
VS: That’s amazing! Now to your mentor, Dr. Sachdev. How did having an intern shape your style
of reviewing? Did you find that it helped you become a better reviewer?
US: Most definitely. Teaching and mentoring makes one accountable and deliberate in a very specific way. I think the experience was really good for all of the mentors involved.
VS: So, this seems like a winwin situation for everyone! Dr. Sachdev, what advice would you give to a new editor taking on an intern?
US: Excellent question. The mentors have already had experiences helping residents and fellows through the clinical spheres of our profession. Thus, they already have the background to be good mentors. I would encourage them to pick articles that will challenge their mentees. Send them articles that are outstanding as well as those that might need some help or
is certainly very high-yield, there is a time commitment and especially for those trainees in active clinical years, there is some deliberate planning and timemanagement is needed.
VS: You both have been amazing at answering these questions. Last question is for both of you. What do you hope for the future of the program—especially since there’s now a new cohort of JVS interns?
US: I’d love to see the program expand if possible, and I am hoping to put together a publication with the results of its efficacy.
AB: The future of this program is clearly bright! I was so fortunate to be part of a star-studded class from across the country and it was great to finally meet them in person at this past VAM! In the shortterm, I would love to see this program collaborate with other surgical journals and expand the scope of “reviewertraining” to all surgical specialties. For the long-term, I hope to see graduates of this program on the editorial board or as editors of various journals and mentors for future reviewer interns!
are not appropriate for publication. As I told Anand, one of my key criteria for accepting a paper is whether an author did what they said they were going to do. Sometimes the results and conclusions are not congruent with the stated goals of the project. I think each mentor has a similar pearl that they can pass on to their mentees.
VS: That’s sage advice. I’m gonna pocket that one. Dr. Brahmandam, what advice would you give to a new intern?
AB: This process is very much like first year of surgical residency; therefore, it is important to find a workflow system early on. One of the most important tips on reviewing Dr. Sachdev gave me was—are the authors doing what they say they are? And is the methodology appropriate to answer that question? This led me to a very simplified approach of looking at manuscripts. Similarly, I am certain every senior editor/mentor will have their own simplified approach to reviewing. My suggestion to the new interns is to find a simplified system of reviewing—whether it’s from one mentor or multiple mentors—stick to that system, and to make it a habit through repetition. Additionally, while the program
A SESSION AT THE 2022 VEITHsymposium in New York City (Nov. 15–19) focused on new concepts, machine learning, and artificial intelligence (AI) in vascular surgery, with a panel discussion honing in on the cost-effectiveness and wider “value” of emerging technologies in this space.
“What’s the benchmark for success going to be?” moderator Barry Katzen, MD, of the Miami Cardiac & Vascular Institute in Miami questioned.
Katzen made particular reference to the current economic environment in healthcare environments around the world, and was keen to get the experts’ take on how healthcare economics might influence which technologies survive.
Panellist Rachel Clough, PhD, FRCS, of Imperial College Healthcare NHS Trust in London, England, noted that, in her opinion, “the key to this is getting the technology out there for patient benefit in as many healthcare systems as possible.”
Clough added: “I think in many systems around the world, it is all about […] costeffectiveness, about value of the product, and so I think it is about trying to first of all gain regulatory approval and get a decent evidence base, and then get providers to begin to purchase [these technologies].” Jocelyn
Hudson CHRISTOPHER AUDU is a vascular surgery resident at the University of Michigan in Ann Arbor, Michigan, and the Vascular Specialist resident/fellow editor.VEITHSYMPOSIUM
PROBES ‘VALUE’ OF ARTIFICIAL INTELLIGENCE IN VASCULAR SURGERY

continued from page 1
peripheral arterial disease (PAD) to receive either in frainguinal bypass or endo vascular intervention. The trial consisted of two parallel trials: Cohort 1 included patients with single-segment GSV; Cohort 2 includ ed patients who lacked single-segment GSV and therefore alternative autogenous vein or prosthetic was used in those randomized to the open arm.
According to Farber, the best way to evaluate whether a patient has single-seg ment GSV—one he says needs to be at least 2.5mm in diameter, but ideally above 3mm, and must be free of thrombus—is by using duplex ultrasound. Speaking to Vascular Spe cialist on this topic, Menard notes that while assessment of the vein is common practice for vascular surgeons, it is not for other spe cialties. In the wake of BEST-CLI, he sug gests that evaluation of the GSV—a “very important” part of the assessment for treat ment—should be included in the guidelines.
Farber tells Vascular Specialist: “We are not claiming to bring down the 10 command ments here; all we are saying is that we are introducing some level-one data into a space that has almost no level-one data. […]. Here is another study that says the endovascu lar-first [approach] is a great thing for some people, but [it is not] for everybody. So, if a patient is a candidate for surgery and [..] has a good single-segment saphenous vein, there should be a conversation about surgery, for that individual.”
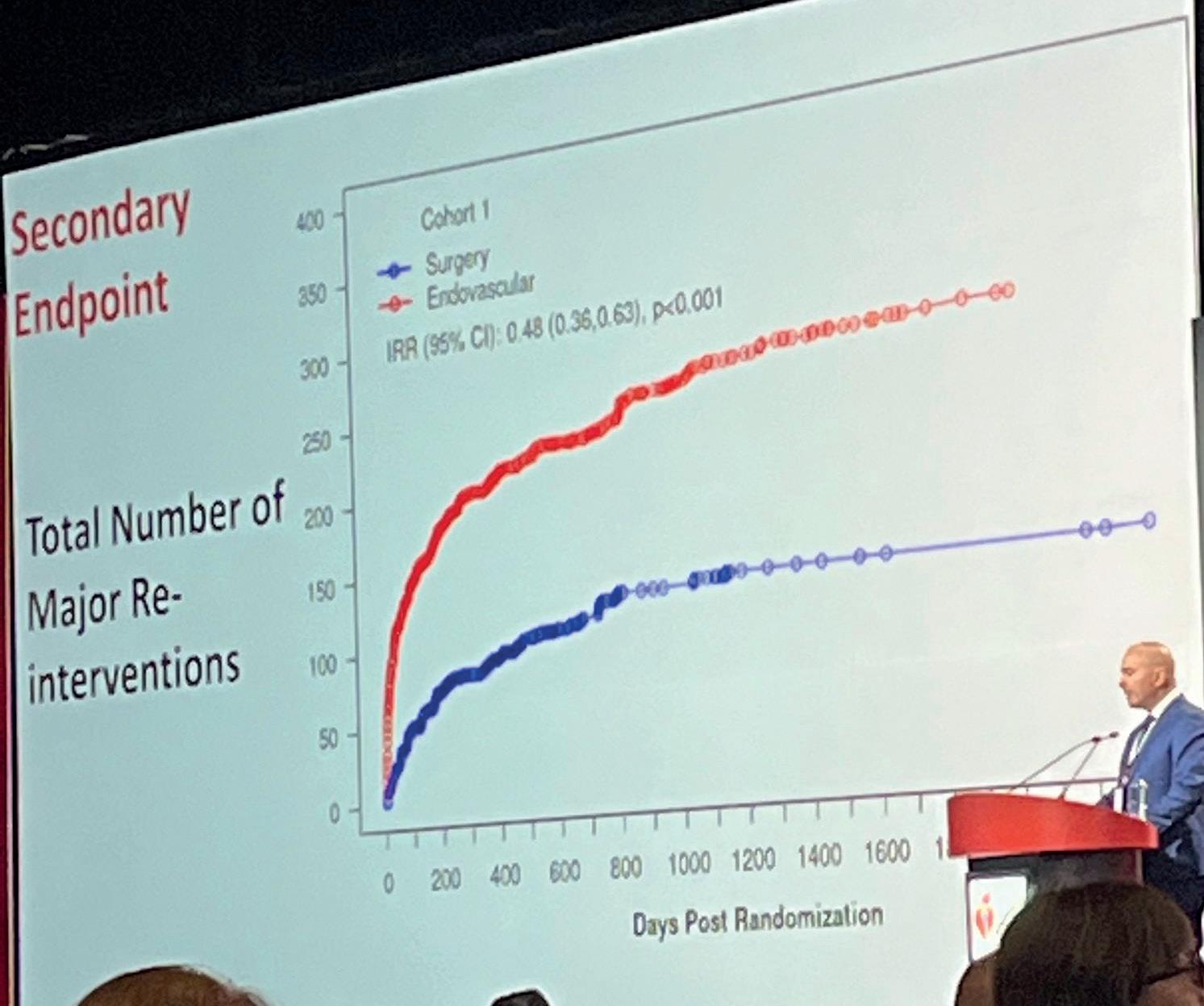
The investigators found that surgery was more effective than endovascular therapy in the Cohort 1 patients. At AHA, Farber re vealed that there was a reduced rate of ma jor adverse limb event (MALE) or all-cause death—the primary endpoint—in patients with good single-segment GSV who under went open surgery, as well as fewer major reinterventions, at median follow-up of 2.7 years. The maximum follow-up time in these patients was seven years.
Going into the details, Farber noted that Cohort 1 included 1,434 patients with sin gle-segment GSV who were randomized 1:1 to either surgical or endovascular treatment. At median follow-up, the rate of MALE or all-cause death was 42.6% in the surgery arm compared to 57.4% in the endovascular arm (hazard ratio [HR], 0.68; 95% confidence in terval [CI], 0.59–0.79; p<0.001). In terms of secondary endpoints, he revealed that 10.4% of patients in the surgery arm underwent above-ankle amputation of the index limb versus 14.9% in the endovascular arm, in ad dition to rates of 9.2% vs. 23.5% for major reintervention on the index limb, and 33% vs. 37.6% for all-cause death for patients in the open and endovascular arms, respectively.
In patients who did not have adequate sa phenous vein, i.e. those in Cohort 2, there were no significant differences in the prima ry endpoint. Farber detailed that this group included 396 patients who were randomized 1:1 to either surgical or endovascular treat
ment. The median follow-up was 1.6 years, with the maximum 5.1 years. Farber report ed that the rate of MALE or all-cause death in this cohort was 42.8% vs. 47.7% in the open and endovascular arms, respectively (HR, 0.79; 95% CI, 0.58–1.06; p=0.12). The corresponding figures for the secondary end points were as follows: 14.9% vs. 14.1% for above-ankle amputation of the index limb; 14.4% vs. 25.6% for major reintervention on the index limb; and 26.3% vs. 24.1% for all-cause death.
Farber added that there were no differences in periopera tive mortality or major adverse cardiovascular events (MACE), and that mortality and MACE were simi lar between treat ment strategies over the course of follow-up.

From the podi um, the presenter concluded that sur gery with adequate sa phenous vein “should be offered as a first-line treatment option for suitable candidates with CLTI, as part of fully in formed, shared decision-mak ing.” He added that level-one evidence from BEST-CLI “does not support an endovascular-first approach to all patients with CLTI,” and instead supports a “complementary role” for both revascularization strategies. He noted that further studies are needed to better elucidate the comparative outcomes in subsets of patients.
While the primary focus of the trial was clinical outcomes in the comparison of open surgery versus endovascular therapy, Menard tells Vascular Specialist that the investigators planned two “very important” ancillary assessments: cost-effectiveness— which the team is yet to con duct—and quality of life. With regards to the latter, he noted that the team used a number of different metrics for this, includ ing the vascular disease-specific VascuQoL, as well as the EQ-5D and the SF-12.


According to Menard, the baseline scores for quality of life speak to the impact of CLTI on patients’ everyday lives: “The quality of life for all patients at baseline on entry into the trial was extremely poor and low, and that is consistent with what is known about the devastating im pact of CLTI on patients’ overall function, the mental status, their physician limitations, and their
high degrees of pain.” Menard—who pre sented quality-of-life data in a separate talk at AHA—reports that both revasculariza tion strategies resulted in “significant gains” across every metric studied, noting also that there was not any significant difference be tween the two treatment arms.
Making the case for the benefits of the endovascular approach, Rosenfield empha sizes: “This is the first trial that really shows that when you compare ‘endo’ to surgery, certainly in the disadvantaged vein group, they both actually had durable outcomes. A lot of us had questions about how durable out comes for the ‘endo’ approach would be. And it should be clear that it is an approach, because sometimes touchups are needed on both sides and those are not considered MALE events. You re ally had to have a major reintervention to reach an endpoint of MALE, or an am putation. But I think that this for the first time shows that, in a head-to-head trial, that both are durable and that, on the ‘endo’ side, once you achieve successful technical outcome, it is compa rable even in the group that had reasonable vein in Cohort 1.”
BEST-CLI meets ‘astronomic’ need for high-quality, practicechanging data
At AHA, Farber noted that data from the Vascular Quality Initia tive (VQI) from centers of excel lence in North America revealed “tremendous” center-specific variability in treatment strategy in the use of bypass versus en dovascular therapy for CLTI pa tients, which BEST-CLI national trial manager Michael Strong tells Vascular Specialist attributes to the lack of evidence-backed guidelines in the space.
Speaking to this newspaper, the investigators express their confidence that the results of BEST-CLI will change practice and impact the Global Vascular Guidelines published in 2019. Menard believes there is “no question” that guidelines will change, partly because current ly they are “riddled with gaps.” He notes that anywhere from 10–15% of current guidelines are based on level-one data—a “miserably low” figure in his opinion. “The need for quality data that the BEST-CLI rep
resents is astronomic,” he says.
Rosenfield remarks that the trial will “defi nitely change practice” as it provides the clear message that “surgery is not dead, in fact it is very much alive and well for the appropriate ly selected patients.” He stated that the data “should be described to patients—simple as that,” and that patients “should have the op tion of deciding, but they should be knowl edgeable that they will do better with surgery [in selected cases], and that is an appropriate response to [these results].”
Farber concurs, noting that there is now level-one evidence to support the role of by pass in certain patients. “It supports a body of literature that is not as strong, and so I think [guidelines] will change,” he comments.
“I think it is nice for us to have all these arrows in our quiver to treat CLTI patients, and that is what this is; it is about saying this arrow does work and it should be used in some situations,” Farber summarizes. “That is a great thing to add because, before BESTCLI, the data were not as strong.”
While the investigators agree that BEST-CLI will be practice changing, they acknowledge that it represents “the first step” in a long tra jectory of future investigations and discus sions in CLTI research.
At AHA, Farber noted some limitations of the trial, including selection and oper ator bias in enrollment and intervention, the fact that equipoise and eligibility were determined locally and were variable, that anatomic complexity is yet to be evaluated, Cohort 2 was likely underpowered, the per centage of female patients was lower than targeted, and the use of paclitaxel balloons or stents was affected by the Katsanos me ta-analysis during enrollment, they outlined.
“We need to dig deeper,” Rosenfield says. He describes the trial as a “game-changer in many respects,” but stresses that “this field is still a moving target” and so BEST-CLI must be seen as “the first foray into developing very solid level-one evidence.” Specifically, he notes that techniques will “continue to improve and get better.” Looking ahead, Ros enfield believes that those who treat CLTI will “learn a lot more over the course of the next couple of years as we peel back the lay ers of the onion.”
According to Menard, the trial stimulates two topics that will take center stage in the “great discussions that are going to be had” in the coming months. “We are all trying to fig ure out exactly how we are going to interpret the results for our own practices, and, in or der to do that, you really need to understand the patients enrolled into the trial, and that is a big focus of the future work—defining what their anatomy was […] and a bit more about overall demographics. You can have selection bias, but you cannot imply or in any way get around the fact that at that institution they were deemed appropriate for both [open and endovascular strategies],” he tells Vascular Specialist
Farber stresses that further investigation
might also elucidate how an operator decides between adopting an open or endovascular approach in certain patients.
“We all know that if it is an easy ‘endo,’ then of course the patient should have an ‘endo,’ there is no equipoise; and then on the other extreme, there are cases where every thing is blocked from the groin to the foot and somebody might say, of course surgery is the way to go, and then there is everything in between,” he says.
What remains, according to Farber, is for the investigators and others in the field to “dig deep” into these data to define appropriate ness for a certain treatment. For now, Rosen field notes that the investigators are “really excited” about analyzing the “treasure trove” of data that BEST-CLI provides and seeing what they can learn. Looking beyond this, Menard expresses the team’s hope that “many more trials will come along and build on what
the BEST-CLI has laid as a foundation.”
Meanwhile, at AHA, audience questions saw the BEST-CLI investigators asked wheth er a competing risk analysis was performed for the MALE endpoint, “specifically taking into account the competing risk of death,” which Farber confirmed had taken place. Far ber also tackled a query over medical therapy use during the trial.
“We delineated expected optimal medical therapy in our manual of operations, and we have an optimal medical therapy committee that oversaw [its] use in the trial, and provid ed dashboards to all the sites,” he said. “So, essentially, in Cohort 1, at 30 days, the use of statins was 75%, and that went up from 70% at baseline. The use of at least one antiplatelet was 83%, up from 72% at baseline. The use of [dual antiplatelet therapy] went from 17.8% to 36.3%, and there was 7.5% use of [direct oral anticoagulants] at three months.”
“ We are all trying to figure out exactly how we are going to interpret the results for our own practices, and in order to do that, you really need to understand the patients enrolled into the trial, and that is a big focus of the future work”
MENARD
The Novo Nordisk Foundation has made a $3.3 million contribution toward the BEST-CLI (Best endovascular versus best surgical therapy in patients with critical limb ischemia) clinical trial, the Denmark-based entity announced. The grant is set to be used by investigators to continue analyzing the wealth of data produced by the nearly eight-year-long study.



ORIGINALLY FUNDED BY THE U.S. NATIONAL INSTITUTES OF HEALTH (NIH), BESTCLI compares the treatment efficacy, functional outcomes, quality of life and cost–effectiveness of surgical bypass and endovascular revascularization for 1,840 patients with CLI across North America, Europe and Asia.
The trial is being led by co-principal investigators Matthew Menard, MD, director of the vascular and endovascular fellowship program at Brigham and Women’s Hospital in Boston; Alik Farber, MD, chief of vascular and endovascular surgery at Boston Medical Center; and Kenneth Rosenfield, MD, section head of vascular medicine and intervention at Massachusetts General Hospital, also in Boston.
The trial started in August 2014 and was completed in March of this year. Patients were followed for at least two years and up to seven years. The fresh funding injection from the Novo Nordisk Foundation will be used by the investigators to continue plumbing the trial data, perform a comprehensive cost–effectiveness analysis, and establish an imaging core laboratory to collate and analyze the radiographic imaging collected.
“BEST-CLI is a landmark trial that has the ambitious goal of establishing the evidence foundation that will help clinicians and caregivers provide the best possible care to patients with critical limb ischemia,” said Menard. “Unprecedented in its effort to bring together all of the specialties that treat CLI, as well as in its global reach, BEST-CLI aims to define a sorely needed standard of care for this particularly vulnerable population of patients. Given the truly alarming rates of diabetes around the world, and the projected rise in the number of patients afflicted with critical limb ischemia, it is of paramount importance that we understand the full impact of our surgical and endovascular interventions.”
In addition to the initial NIH funding, the Society for Vascular Surgery, Vascular Interventional Advances (VIVA), the New England Society for Vascular Surgery, Western Vascular Society, Eastern Vascular Society, Midwestern Vascular Surgical Society, Southern Association for Vascular Surgery, Canadian Society for Vascular Surgery, Society for Clinical Vascular Surgery, Society of Interventional Radiology, Vascular and Endovascular Surgery Society and the Society for Vascular Medicine are among those to have contributed funds toward BEST-CLI.
Industry sources of financial support included Janssen, Gore, BD, Medtronic, Cook Medical, Boston Scientific, Abbott, Cordis and Cardiovascular Systems, Inc.—Bryan Kay
shy of two thirds,” said Menard. The num ber of those still smoking was greater than one third, he continued, with those on at least one lipid-lowering medication “a little better at 72%,” while those on at least one antiplatelet medication was 73%.
He further revealed how just a quarter met all four OMT criteria, with 2% not meeting any of the stated components. Some 38% met three, another quarter two, and 11% just one of the criteria.
A SIGNIFICANT PROPORTION OF patients enrolled in the BEST-CLI trial did not meet optimal medical therapy (OMT) guideline-based recommendations at the time of their entry, co-principal investigator Matthew Menard, MD, told the 2022 New England Society for Vascular Surgery (NES VS) annual meeting in Newport, Rhode Is land (Oct. 14–16).
The investigators were looking to under stand the utilization of OMT at the incep tion point, with baseline data—post-con sent, prior to revascularization—showing that 87% of patients enrolled had hyperten sion, 74% had hyperlipidemia, 69% diabetes, and 36% were active smokers, Menard told attendees. “How did we do?” he pondered. “Not so well. The data show those who had controlled blood pressure was 64%, “so just
Multivariate analysis showed Hispanic ethnicity, prior or existing coronary artery disease, stroke and diabetes were among positive predictors of a higher optimal medical therapy score, while Black race and participation in Cohort 1 were nega tive predictors.
“Patients in this BEST-CLI dataset had utilization rates of defined optimal medical therapy well below recommended at the time of presentation,” Menard said.
“Where do we go from here? The most important work is to turn participation in the trial into improved utilization of optimal medical therapy.”
Changes from baseline utilization of op timal medical therapy over the course of BEST-CLI and associated impacts on clinical outcomes and quality of life are to be fur ther assessed, Menard added.—Bryan Kay
Optimal
therapy adherence ‘well below’ recommended level at baseline







THE IN.PACT ADMIRAL DRUGcoated balloon (DCB) shows promising results in treating femoropopliteal in-stent restenosis (ISR) in a Society for Vascular Surgery (SVS) Vascular Quality Initiative (VQI) registry-based, postmarket surveil lance study. This is according to Daniel Bertges, MD, a vascular surgeon from the University of Vermont Medical Center in Burlington, Vermont, who presented inter im, 24-month data from the prospective, non-randomized study in a late-breaking clinical trials session at Vascular Interven tional Advances (VIVA) 2022 in Las Vegas (Oct. 31–Nov. 3).
Bertges revealed a freedom from target lesion revascularization (TLR) rate of 89.8% at one year and 72% at two years in the “challenging anatomy” of in-stent rest enosis within the femoropopliteal artery segment as the headline findings.
The presenter informed VIVA 2022 that he and colleagues conducted a multicenter study involving 300 patients at 43 US sites within the SVS VQI. The primary endpoint was TLR within 12 months post-index pro cedure, and secondary endpoints—assessed at 12, 24, and 36 months—included allcause mortality, TLR, target vessel revascu larization, major target limb amputation, and technical success, which was defined as successful deployment of the balloon without resulting in occlusion and having

residual stenosis ≤30% and resting systolic pressure gradient of <10mmHg, if measured.
Bertges noted that patients were in cluded in the study if they were ≥18 years of age, had undergone single-limb and single-treatment during index procedure and received primary treatment of the ISR lesion with an IN.PACT Admiral DCB, and had de novo or recurrent ISR in the superficial femoral and/or popliteal artery and documented ischemia with Rutherford classification 2, 3, or 4. Those patients who had undergone bilateral femoropopliteal artery repair or had a history of tissue loss in the target limb were excluded. Failure to successfully cross the target lesion was another exclusion criterion.


Giving details of the patients included in the IN.PACT SVS ISR registry, Bertges explained that 20% of patients (60/300) had chronic limb-threatening ischemia (CLTI), 56% (168/300) had diabetes, and 53.7% (161/300) had TASC C–D lesions, among other characteristics.
In his conclusion, the presenter re marked that these results “demonstrate the ability of the VQI to conduct postmarket evaluation of peripheral devices in partner ship with industry and federal regulators.”

Speaking to Vascular Specialist follow ing his VIVA 2022 presentation, Bertges commented that one of the main benefits
of registry data is that it is “obtained from everyday practice,” and therefore “in cludes data from a variety of practitioners working to care for a variety of patient populations, as opposed to the sometimes restrictive inclusion and exclusion criteria of clinical trials.”
With reference to a particular benefit of the VQI registry, he stressed that there is “power in numbers,” noting that the VQI includes “several hundred thousand pro cedures recorded over the past decade or more” and that it continues to accrue tens of thousands of patients annually. “That’s a rich repository of information.”

Furthermore, Bertges referenced the multispecialty nature of the VQI registry— which includes vascular surgeons, cardiolo gists, radiologists—as another of its strong points, as well as its “continued efforts towards gathering the best longitudinal data on our procedures for our patients.”
Looking ahead to what is next for the study, Bertges informed Vascular Specialist that the researchers are looking to track their results out to three years. “We expect those findings to be reported back to the


investigators, to the sponsor, and to our FDA [Food and Drug Administration] reg ulators in the early part of the summer of 2023, and so we look forward to bringing those results to the vascular community following that.”
Six-month results from the PROMISE II trial of the Lim Flow deep-vein arterialization system showed an overall amputation-free survival of 66%—“well above” the pri mary endpoint target of 54%, chief investigator Daniel Clair, MD, told the 2022 Vascular Interventional Advances (VIVA) meeting (Oct. 31–Nov. 3) in Las Vegas.

The PROMISE II research team further demonstrated a limb salvage rate of 76% and overall survival rate of 87% in a group of patients that Clair, professor and chair in the Department of Vascular Surgery at Vanderbilt University in Nashville, Tennessee, described as “the sickest group of patients ever enrolled in a lower-extremity pivotal trial.”
PROMISE II was conducted at 20 sites in the U.S. with more than 100 enrollees, all of whom were classed as hav ing Rutherford 5 and 6 levels of peripheral arterial disease (PAD)—commonly referred to as a “no-option” group of end-stage chronic limb-threatening ischemia (CLTI) patients.
Clair reported a technical success rate of 99% across “a wide range of investigators from all different specialties” us ing the LimFlow transcatheter arterialization system among a patient population he described as predominately older,
male, diabetic and who bore the “typical group of comorbidities,” with around 20% on dialysis.
There was a large difference in outcomes for di alysis vs. non-dialysis patients—driven primarily by an increased mortality in the dialysis group, Clair noted. “The primary reason this group did not meet [the target] is really overall survival,” he told VIVA 2022. “This is obviously a very sick group of patients.
DANIEL BERTGESIf you have end-stage renal disease, and in addition, reach the point where your limb is not salvageable, there is probably major changes that we need to do in order to improve their overall survival.”
Six-month results also showed a wound healing rate of 75% , Clair said, rising to almost 80% at the 12-month mark, according to independent core lab evaluation. Pain scores for this patient population, too, continue to decline over time alongside “a signif icant improvement in their quality of life,” he added.
Additionally, Clair reported an improvement in the patient group’s Rutherford classification at the six-month point, telling VIVA that almost 20% were categorized as either Rutherford 0 or 1. Out to a year, he continued, “at least pre liminarily,” nearly 60% were recorded as Rutherford 0.
Concluding, Clair said: “The PROMISE II study met its endpoint with a very reliable amputation-free survival. Tran scatheter arterialization is safe and effective. These results are very much in line with what we saw in the PROMISE I outcomes, and from my viewpoint, now we have to find a new name for this group of patients.”—Bryan Kay
“The data is obtained from everyday practice [and therefore] includes data from a variety of practitioners working to care for a variety of patient populations, as opposed to the sometimes restrictive inclusion and exclusion criteria of clinical trials”Daniel Bertges at VIVA 2022
End-stage CLTI: Deep-vein arterialization procedure demonstrates amputation-free survival rate of 66% at six months LIMB
“These results are very much in line with what we saw in the PROMISE I outcomes, and from my viewpoint, now we have to find a new name for this group of patients”
DANIEL CLAIRDaniel Clair delivers new data Robert Rhee delivers the 2022 Eastern Vascular Soci ety address in Philadelphia
EVOLUTION WAS THE CORE THEME OF THE Presidential Address Robert Rhee, MD, delivered from the Eastern Vascular Society (EVS) annual meeting stage in Philadelphia (Sept. 29–Oct. 1). “Let’s Evolve,” it was en titled. But, Rhee told those gathered, the society lays claim geographically to the Eastern seaboard of the United States and Canada, which is home to “the most incredibly diverse and quantitatively the largest number of training programs” anywhere else in North America. So he had a specific audi ence in mind for his presidential message contained.
“I thought it would be befitting to direct my address to the younger and possibly the greatest generation of vascular surgeons ever, because you are going to take us into that next level of evolution,” said Rhee.
The endovascular aneurysm repair (EVAR) revolution encapsulates the essence of out-of-the-box thinking required to achieve that revolution, he told the audience.
“We, as a pioneering specialty, turned a very maximal ly invasive operation into a minimally invasive one,” Rhee said—with “excellent long-term results 25 years later.”
“It’s not a failed experiment, as some recent editorial in the JVS [Journal of Vascular Surgery] has suggested. It trans formed our specialty overnight to the highest levels, with excellent outcomes, which could not be really compared to any open AAA [abdominal aortic aneurysm] repair at most institutions.”
Rhee turned to the example of Timothy Chuter, MD, a pi oneer in the development of endovascular repair, with whom he worked for a time: “Initially, when he came to us, he was thought to be crazy because the vascular chief at that time ridiculed him constantly at conference. I remember sitting down with him, and him preaching to me how stupid it was to treat a disease of expanding radial force with a device that has constant radial force.
“What would have happened if Timothy Chuter did not forge on and ignore his critics. He was not allowed to do the research involved with EVAR at the main university hospital because they thought he was crazy. So he went to a local, large community hospital, and they said, ‘Do it.’ They ac tually had the insight to allow him to do his EVAR studies.”
Rhee challenged members of the EVS gathering: “To all of you surgeons out there: be a Tim Chuter; don’t be a fol lower. If somebody discourages you, and you have an idea, pursue it.”

Rhee emphasized the need to ensure patients are not being overtreated by raising the figure of the late Roy Greenberg, MD, another vascular pioneer.
“He introduced one key concept that we should all take a second look at in 2022, “ he said. “That is, he advocated, after coming back from Malmo, Sweden, that we should al ways treat to the healthy aorta. It’s a modus operandi that is religiously followed by all these aortic surgeons throughout the world now. But it’s a very dangerous concept in essence, because, by definition, it overtreats patients. Because you’re putting in stents and devices into healthy portions of the aorta.”
Rhee asked the audience whether this level of treatment was truly required in an arena of care where there is no cure, but where vascular specialists are pursuing “endovascular protection.”
“It’s almost heresy to say that, but when you look back, and at the history of vascular surgery and surgical management, you realize if you have a patient with abdominal aortic aneu rysm, the entire aorta is diseased; there is no healthy aorta. So, what are you treating to? I challenge you. I do four-vessel thoracoabdominal [aneurysms] all the time, but I’m saying that we all should take a look at it, and not follow religiously at this point.”
Question everything as new technology emerges, contin ued Rhee. “From the very beginning, vascular surgery had access to a dizzying array of tools, and we embraced that. There are countless examples of tools we have developed for the management of vascular disease; however, there is a dark side to the technology.”
The Food and Drug Administration (FDA) approval pro cess brings countless numbers to the table every year, specif ically through the 510k route, he noted—“about 80% of the devices you all use now.”
This means, Rhee said, “a device company is allowed to sell their devices to you to be used in your patients because the device looks and performs like a similar, already approved device. Many of these devices don’t have any data, and they are still approved and marketed for use in your patients.”
Therefore, “not all of the shiny new toys have the data,” he commented, and it is incumbent upon vascular surgeons to conduct research to establish device safety, raising the concept of what he called “false prophets.”
Rhee urged caution over the ethical conundrums that face the profession. “We have this financial pressure to produce not just volume, but also in clinical research and basic re search. We have to make sure there is an ethical component and accuracy of the research is ever-present throughout our careers.”
When it comes to evolution and revolution in vascular surgery, Rhee honed in on four high-level areas: Understand ing the disease process and the limitations on what can be done. Embracing new technology “but not being blinded by false prophets.” Escaping from the ethical black hole. And embracing diversity to achieve success.
“Vascular surgery is still a relatively new field,” Rhee said, explaining how the specialty developed out of a sense of necessity among cardiac surgeon leaders in those early days. “Let us evolve and not overestimate our abilities by offering solutions that overtreat our patients.”
He was taught, by the vascular elder statesmen like Ken neth Cherry, MD, and Kenneth Ouriel, MD, that “less is bet ter and faster is better for the patient.”
Rhee also addressed diversity, tackling the topic through the prism of his challenge for the specialty to “question everything.” He referred to the experience of a female senior resident who during his own training questioned a leading surgeon who held viewpoints that held that she should not enter vascular surgery because of the fact she was a woman. “Should we cancel him because he said that?” Rhee stated. “He was thinking 1989 beliefs. Yes he was an incredible pi oneer but he had the beliefs of back then. The essence is of evolution is to question everything.” That female resident fought through the pushback and entered vascular practice, Rhee added.
He placed vascular surgery in the guise of “a microcosm of the world’s controversies.” And as vascular surgery evolves to the next level, inclusivity will be key, Rhee said. In that vein, the EVS is poised to extend full membership to all al lied health members and beyond. “Vascular surgeons do not own vascular disease,” Rhee added. “There are blood vessels everywhere ... It doesn’t matter where the controversy is. But my vision is that vascular surgery—because our field encompasses the entire body—we should be the gatekeepers and the quality keepers of vascular disease.”
“To all of you vascular surgeons out there: be a Tim Chuter; don’t be a follower. If somebody discourages you, and you have an idea, pursue it” ROBERT RHEE
2022 BD. All Rights Reserved. © 2022 Illustration by Mike Austin. BD-62443
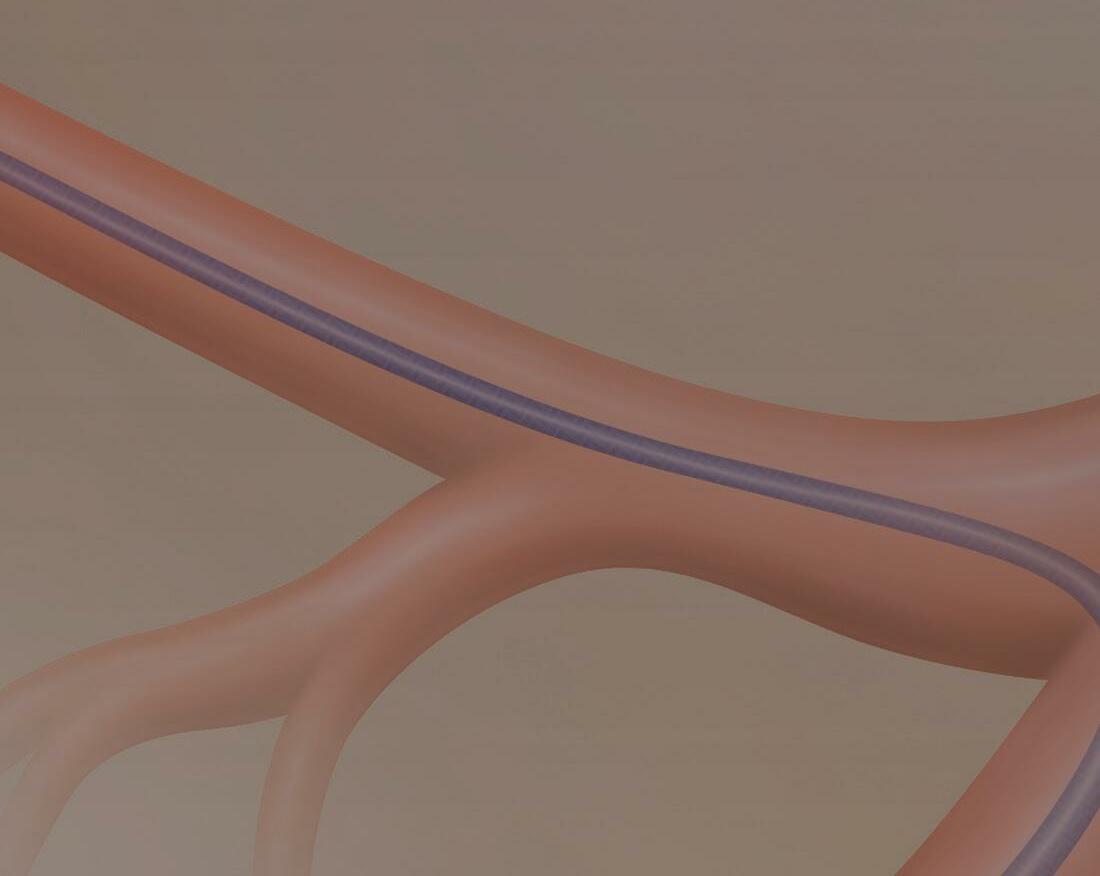



















patient population.
Importantly, patientcentered outcomes and personalized vascular care are at the core of these updated priorities,” said members of the SVS Research Council writing about the priorities in the November issue of Journal of Vascular Surgery (JVS). Tzeng, the former council chair, is first author.
“With our greater social awareness, it is paramount that we address these disparities and understand their impact on patient health and outcomes of treatment,” said Tzeng.
Currently, there is a big emphasis on medical optimization, said Corriere, “That aligns with paying attention to healthy living and disease prevention.”
“We think disparities and patient-centered care are extremely important aspects of what we can do to improve health in the broader community,” said Raul Guzman, MD, current chair of the Research Council. “We’re very aware of the issues related to providing care for a diverse patient population and, by doing research in this area, we hope to improve care for all of our patients.”
Healthcare assessment is also moving from technical outcomes to more patient-centered outcomes, said Guzman. And research in coming years will focus on what patients consider to be the most important aspects of their care.
The 10 priorities were selected through a lengthy process (see adjacent article), which began with 106 selected surgeon-scientists asked to submit “the two most important questions in vascular research that need to be answered for the care of our patients.”
The new priorities create a ”framework for vascular surgeons to engage in research in ways that the wider community thinks are significant and will improve patient care,” said Guzman.
“We hope to help our young investigators focus on problems that our Society’s membership feels are important in terms of our daily practices. If we can encourage our members to become enthusiastic
about these particular topics, that would be a big accomplishment,” he said.
Researchers hope the updated priorities will serve as a starting point for aligning research efforts within the SVS and among vascular surgeons and scientists, and that they will help drive larger investigations that lead to improved patient care.
This occurred with the 2011 priorities; four of the nine priorities have been explored in national multicenter studies “that directed the questions we posed,” said Tzeng. “By listing priorities and putting them down on paper, it helps us as a Society and helps other researchers develop trials to look into these topics.”
Priorities from 2011 remain important to the vascular research community said all three doctors, emphasizing that the new priorities listed are not the only areas of research that are important. “At this moment, these are areas that membership believe should be a higher priority,” said Corriere.
Corriere, Guzman and Tzeng also pointed out that for this update, the group overall intentionally refers to the updated priorities as simply “research priorities,” removing the word “clinical.”
“Although these priorities are clinically oriented, the answers to these important questions may lie in investigations that focus on basic, translational or clinical research,” said the article. “These priorities are intended to be as inclusive as possible, encouraging research approaches that may use genomic data to identify disease-specific mutations, cell-based therapies, computational modeling, novel imaging technology, implementation science, clinical trials and so on.”
What’s the future for the priorities? Guzman foresees a shorter time interval between updates, “because treatments and care are evolving so rapidly,” he said, with treatments common today that simply were not available in 2011. “There are things just now being discovered that in five years will make the cut,” said Guzman.
After all, it was partly such advances that spurred the review. “There are so many new technologies and medications that appear and make us review an old question,” said “Corriere. “We wanted to get fresh eyes on the priorities (from 2011) in light of new evidence and treatments.”
All three surgeons hope people read the JVS article and review the priorities. “It shows what our members think are important topics and demonstrates the success of the prior priorities,” said Tzeng. “It says, ‘here are our updated research priorities. Look at how much we have achieved since the original set of priorities.’“
For SVS and SVS Foundation awards, the stated priorities help the organizations determine what kind of studies should be considered.
External organizations—such as the National Institutes of Health, the Veterans Administration and other organizations—also will know what SVS is looking to as important goals,” said the SVS Research Council’s Matthew Corriere, MD, who proposed updating the 2011 priorities.
Four of 2011’s nine priorities have been explored in national multicenter trials “that addressed the questions we posed,” said Edith Tzeng, MD, former chair of the SVS Research Council who orchestrated the current process to update the priorities. “Those original priorities provided some momentum in setting up trials. That helps drive the important message that, by listing priorities and putting them down on paper, it helps us as a Society and helps other researchers develop related trials. That’s our hope again—that’s the purpose of doing this,” she said of the update.
The four trials based on the initial research priorities are:
◆ Carotid Revascularization Endarterectomy versus Stenting-2 (CREST 2), seeking to define optimal management of asymptomatic carotid disease
◆ Best Endovascular versus Best Surgical Therapy in patients with critical limbischemia (BEST-CLI) evaluating the effective of open versus endovascular treatment of CLI. This was ranked third in 2011 and results of the trial were just announced


◆ Non-Invasive Treatment of Abdominal Aortic Aneurysm Clinical Trial (N-TA3CT), to identify medical therapies for the prevention of the growth of abdominal aortic aneurysms (AAAs), specifically testing the ability of doxycycline to prevent AAA growth. Identifying and evaluating medical therapy to prevent AAA growth was ranked eighth in 2011. No clear benefit was demonstrated but “this trial represented the culmination of bench-to-bedside efforts of a number of SVS members
a. Develop personalized medicine and shared decision-making processes in the care of patients with aortic disease
b. Determine best medical and surgical treatment algorithms for uncomplicated type B aortic dissections with the goal of improving survival and reducing complications
a. Develop diagnostic tools, imaging techniques and selection strategies aimed at identifying patients who would benefit from treatment of asymptomatic carotid stenosis b. Compare carotid interventions (CEA, TCAR, TF-CAS—carotid endarterectomy, transcarotid revascularization, and transfemoral carotid artery stenting, respectively) with medical therapy for treatment of asymptomatic patients with carotid artery stenosis
EDITH TZENGRead the article in JVS at vascular. org/ResearchPriorities.
As was the case with the 2011 set, researchers hope the updated priorities will serve as a starting point to align research efforts within SVS and among vascular surgeons and scientists. This, in turn, will help drive larger investigations that lead to improved patient care, writes Beth Bales.
“ With our greater social awareness, it is paramount that we address these disparities and understand their impact on patient health and outcomes of treatment”
working together to identify a medical therapy for AAA disease,” said the article
◆
Finally, studies showed that ultrasound examination works for surveillance following endovascular AAA repair. That has been incorporated into recent SVS practice guidelines, and ultrasound surveillance has supplanted computed tomography angiography. Follow-up was the ninth priority in 2011


“Our signature topics include aortic, carotid, and lower extremity vascular diseases,” Raul Guzman, MD, current chair of the Research Council, said. “Clinical trials would be very valuable in answering the big questions. We can invigorate and support research along the lines of our priorities now that we’ve stated what they are.” The aim is stated in the Journal of Vascular Surgery. “It is our hope that, with the support of our partners in the National Institutes of Health, the American Heart Association, the Patient-Centered Outcomes Research Institute, the Veterans Administration, and other non-profit organizations such as Vascular Cures, we will continue to develop large-scale clinical trials and translational research efforts aimed at addressing many of these priorities. It is also our hope that these efforts will exceed the success of the inaugural set of research priorities, all for the betterment of our specialty and for the health of our patients.”
The process of updating the nine Society
for Vascular Surgery 2011 research priorities began in 2020, jump-started by SVS Clinical Research Committee Chair Matthew
Corriere, MD, who noted that, after nine years, an update might be in order.
A total of 106 people involved in research were invited to answer an open-ended question: what are the “two most important questions that need to be answered in vascular research for the care of our patients?”
Those selected included the 2011 participants, SVS leadership, members of SVS Research Committees from 2019 to 2021 and members involved in vascular research.
Sixty-six people responded with 134 questions, which were collected into topic areas. Lower extremity arterial disease was the focus of nearly 40 questions, followed by research methodologies, approximately 23; aortic disease, nearly 20; and carotid disease, approximately 17.
The council then identified 28 unique research priorities “of significant contemporary interest to the SVS membership,” including: ◆ Five for carotid disease ◆ Five, aortic disease ◆ Six, lower extremity arterial disease ◆ Four, venous disease ◆ Three, dialysis access ◆ Two, health care disparities ◆ Three, medical management of vascular disease
Participants convened for a virtual meeting in May 2021, where subject matter experts presented summaries of their topic areas, and focused on key knowledge gaps.
Attendees reviewed and discussed the topics
and identified additional holes, creating a final list of 36 research questions to score.
The list was distributed to the 28 stakeholders for voting, with 26 people—93%—responding and SVS administration tallying the results.
In the larger topic areas of carotid, aortic and lower extremity arterial disease, the top two priorities were selected. The top-scoring question in venous disease, dialysis access, health care disparities and medical management of venous disease made the list.
The Research Council reviewed and approved the final 10 research priorities.

The majority of those who responded to the request for research priorities were in the 40–49 and 50–59 age ranges, but the larger group did include both younger and older members. Most of the respondents were male, with 20% female representation.

This breakdown is similar to the demographics of the overall SVS membership, said Tzeng, former chair of the Research Council, and lead author of the article on the priorities in the Journal of Vascular Surgery
The full breakdown by age and sex of respondents and SVS membership can be found online in the article at vascular.org/ ResearchPriorities . The council hopes to further diversify respondents for the next update on priorities, Tzeng added.
The Research Council recognized the SVS Executive Committee and SVS staff, particularly Sarah Murphy, senior director for research and education, who participated in the 2011 process and coordinated the updating effort, said Tzeng, Corriere and Guzman.
From the SVS Research Council: Adam Beck, Luke Brewster, Matthew Corriere, John Curci, Matthew Eagleton, Katherine Gallagher, Raul Guzman (then vice chair, now chair), Peter Henke, Brian Rubin, Andres Schanzer, Sherene Shalhub, Edith Tzeng (then-chair), Gilbert Upchurch and Grace Wang.
Invited guests: SVS thenPresident Ronald Dalman, plus Ellen Dillavou, Patrick Geraghty, Philip Goodney, Thomas Huber, Marc Passman, Salvatore Scali, Cynthia Shortell and Wei Zhou.
Several SVS members served as subject matter experts, presenting the state of each topic area, focusing on current clinical trials and research efforts plus the areas of greatest need.
These were: Brajesh Lal, carotid disease; Sherene Shalhub, aortic disease; Michael Conte, lower extremity arterial disease; Peter Henke, venous disease; Karen Woo, dialysis access; Shipra Arya, health care disparities; and Naomi Hamburg, medical management of vascular disease.

WITH THE END OF THE YEAR COME dues invoices for the year ahead. Existing members have already received at least one invoice, one via email in early October and, if dues were still outstanding, a mailed invoice in early November.
Paying dues by year’s end will prevent a lapse in membership benefits, which include access to the Journal of Vascular Surgery pub lications at reduced or no cost; the custom izable SVS Branding Toolkit, discounts on education programs, networking, practice management resources and more.
For 2023, the Society for Vascular Surgery (SVS) will debut a new member classifica tion—Early Active—specifically for those vascular surgeons completing or having re cently completed their training.

Knowing that early-career vascular sur geons are spending much of their time be coming established professionally, SVS has simplified the membership process for those transitioning from training. Dues also are lower—just $275 for the year, instead of the $695 fee for Active members—to help these new members transition from trainee to ac tive working life.

The new membership classification debuts Jan. 1, 2023, and requires no application or letters of recommendation. A total of 575 members who have finished training with in the past three years have been notified that they have automatically become Early Active members.
“Members early in their careers told us the application process, and finding of surgeons to write letters of recommendation, was burdensome,” said Afshin M. Molkara, MD, chair of the Membership Committee. “We wanted to simplify the process and make it easy for our members to maintain their im portant SVS membership as they transition from Trainee to Active status.”
Once members have become certified in vascular surgery by the American Board of Surgery, they are eligible to become full Ac tive members. As is the case with the new Early Active category, applications are no longer required. Active members may use the Fellow of the SVS Designation, be includ ed in the “Find a Specialist” referral tool and can vote in SVS elections.

The board certification process already includes vetting by other surgeons; because SVS members trust the thoroughness of that work, members of the Membership Com mittee and the Strategic Board of Directors members felt letters of recommendation are no longer needed, said Molkara. Members are automatically transitioned to full Active status after achieving their vascular board certification and a minimum of two years of Early Active membership.
To learn more about the new classification, visit vascular.org/Join. Pay invoices at vascular.org/invoices.
DURING NOVEMBER—NOV. 11, specifically—the United States salutes and honors all those who have served this coun try in its Armed Forces.
This November, the Society for Vascular Surgery highlights the Korean War, where vascular surgeons typically served in Mobile Army Surgery Hospitals. The idea of moving care closer to the battlefield was born during World War II and the first MASH Unit was organized in 1948.
This past September marks the 50th an niversary of launch of the television show M*A*S*H, which ran for 11 seasons on CBS. Two episodes during those 11 years included advances in vascular surgery. Ahead of that occasion, in August, the Society’s Audible Bleeding podcast aired “MASH-Part 1,” on how the young surgeons working near the battlefield in MASH units during the Korean War pioneered vascular wartime repair.
The “MASH” episode is part of Audible Bleeding’s “Vascular Origin Stories,” which explore “the fun and engaging stories that shaped vascular surgery.” See vascular.org/ AudibleBleedingMASH1
In addition, “Korea, MASH and the acci
dental pioneers of vascular sur gery” appeared in the Journal of Vascular Surgery ( JVS ) in 2017, outlining the use of the army hospitals, the youthfulness of the surgeons, arterial repair and the book that led to the television show.
“Despite their limited training and prepa ration, the horrific working conditions, the ongoing threats of court martial for attempt ing to save rather than sacrifice limbs, and the endless cataracts of broken and maimed young soldiers requiring desperate treat ment, the MASH surgeons in Korea cared for their patients with extraordinary dedi cation and perseverance. As a result, a new surgical specialty was born, concludes Steven G. Friedman, MD, author of the JVS article.
“We salute not only their service but their quick thinking and innovations that led to many advances in the specialty. War truly was the catalyst for many advances in vascu lar surgery we take somewhat for granted today,” said SVS President Michael C. Dals ing, MD.—Beth Bales
(
They are:
● “Factors associated with lower preoperative quality of life in patients with chronic limb-threatening ischemia in the BEST-CLI trial,” (Editor’s Choice); visit vsweb.org/JVS-BESTtrialQofLife
Authors include principal investigators
Alik Farber, MD, and Matthew Menard, MD. A history of smoking, impaired ambulation, opioid use and female sex predicted lower healthrelated quality of life scores in chronic limb-threatening ischemia (CLTI)—or critical limb ischemia (CLI)—patients, using multiple HRQOL measurement tools
● “Rates of progression of carotid instent stenosis and clinical outcome,” (Continuing Medical Education [CME] credit available). Visit vsweb.org/JVSStenosisProgression
● “Decreasing trends in reintervention and readmission after endovascular aneurysm repair in a multiregional implant registry.” Visit vsweb.org/ JVS-EVARreintervention
● “Use of an app-based exercise therapy program including cognitive behavioral techniques for the management of intermittent claudication,” in print and also discussed in an Audible Bleeding podcast. Visit vsweb.org/ JVS-AppExerciseTherapy
“Members early in their careers told us the application process, and finding of surgeons to write letters of recommendation, was burdensome”
AFSHIN M. MOLKARA
“War truly was the catalyst for many advances in vascular surgery we take somewhat for granted today” MICHAEL C. DALSING
SUBMISSIONS ALREADY ARE OPEN for 2023 Vascular Research Initiatives Conference (VRIC), which will be May 10, 2023, in Boston. The conference includes abstract sessions, a translational panel, posters and the Alexander W. Clowes Distinguished Lecture.
VRIC is held in the same location and in conjunction with as the American Heart Association’s “Vascular Discovery: From Genes to Medicine” meeting on May 10–13, 2023.
The AHA’s cost for submission is $49. VRIC submissions will close Jan. 11, 2023. Visit vascular.org/VRICabstracts23
Abstract submissions for the 2023 Vascular Annual Meeting (VAM) opened Nov. 16. New this year is a requirement for abstract authors to include with their submission one self-assessment question for post-presentation evaluation
“This is an opportunity for SVS members to present their research on all aspects of vascular diseases—causes, pathology, prevention, diagnosis and care,” said Andres Schanzer, MD, who chairs the SVS Program Committee.
Compiled by Beth BalesTHE SOCIETY FOR VASCULAR SURGERY HOSTS A NUMBER OF TOWN HALLS, roundtables and webinars for the benefit of its members.
In the past few months, members were able to participate in a webinar on how best to use electronic medical records as well as a three-part series of virtual webinars on putting the Global Vascular Guidelines on chronic limb-threatening ischemia (CLTI) into daily clinical practice.
For those who missed the sessions or who want a refresher, recordings of all four are now available for members to access.
“Hacking the EMR: How to Make the EMR Work for You” covered how to manage records to benefit daily practice needs; using EMRs in small independent practices, in cluding outpatient-based (OBL) facilities; and how to manage the burnout so many physi cians and surgeons feel as a result of dealing with electronic records. It was sponsored jointly by the Society for Vascular Surgery’s Community Practice Section and the Health Information Technology and Wellness committees.
Visit vascular.org/EMRrecording to go directly to the recording or visit vascular.org/ VascularTools to see other available practice tools. Once there, click on the recording link within the “Hacking the EMR” description.
The roundtables, held in August, September and October, covered “Translating Guidelines into Practice: Global Vascular Guideline on the Management of Patients with CLTI.”
Session One focused on overall medical care of CLTI patients, including the current state of optimal medical management; recent developments in anti-thrombotic, anti-hy pertensive and lipid-lowering management; and best ways to help patients quit smoking.
Session Two covered Wound, Ischemia and Foot Infection (WIfI) staging and the use of the WIfI stage calculator; a review of contemporary data on the relationship between WIfI staging and important clinical outcomes in CLTI patients; current approaches and limitations to hemodynamic assessment and perfusion measurement in the foot and how they are employed in both pre- and post-revascularization; and how WIfI staging drives triaging of care.
Session Three discussed every-day clinical decision-making around revascularization options and the Global Limb Anatomic Staging System (GLASS). It covered the system, its current limitations, the growing impact of pedal artery disease in clinical practice and the latest data on the risks and benefits of drug elution in the CLTI population.
Visit vascular.org/CLTIrecordings to access all three sessions.
“We’re interested in any and all research that moves the ball forward in terms of taking care of our patients, from peripheral arterial disease, thoracic outlet syndrome, dealing with complications, preventing amputations, even artificial intelligence,” he said. “All have a place in helping improve the care for our patients. We are also especially interested in championing and spotlighting research that deals with disparities, diversity, equity and inclusion.”
Abstract submissions will close at 3 p.m. CST Jan. 11, 2023. Read more at vascular.org/ VAM23AbstractProcess
Katherine Gallagher, MD, of the University of Michigan, has been elected to the National Academy of Medicine for her “innovative translational research on epigenetic regulation of immune cells during normal and pathologic tissue repair and other cardiovascular disease processes.”
Gallagher chairs the Society for Vascular Surgery (SVS) Basic and Translational Research Committee and is a member of the Research Council.
Donald Baril, MD, has been named director of the Vascular Surgery Fellowship Program in the Smidt Heart Institute at Cedars-Sinai in Los Angeles. Baril joined Cedars-Sinai in 2020.
Two SVS members, Daniel Clair, MD, and Michael Dake, MD, have been honored with awards from the VIVA Foundation. Clair, from Vanderbilt University Medical Center, received the Leader In EndoVascular Education (LIVE). Dake, senior vice president of Health Sciences at the University of Arizona Health Sciences, received the ATLAS (A Teacher, Leader And Scholar) Award.
YOUNG VASCULAR SURGEONS from outside the United States and Canada have until Dec. 31 to apply for scholarships to attend the 2023 Vascular Annual Meeting (VAM). VAM will be held June 14 to 17, 2023, in National Harbor, Maryland, just outside Washington, D.C.
Working with a mentor, recipients— who cannot be older than 40 in the year they submit their application—will not only attend VAM but also will visit clinical, teaching and research programs before or after the meeting.
Recipients will receive free VAM registration plus a $5,000 stipend to defray travel. Required materials include a personal statement, three letters of recommendation, three publication reprints, curriculum vitae of no more than 10 pages and a headshot or photograph. Learn more and download the application form at vascular.org/ InternationalScholars
Attendees at the 2023 SVS Foundation Gala will be taking a trip 100 years back in time—to the Roaring Twenties and Prohibition.
The “Great Gatsby Gala” is set for Friday, June 16, during the Society for Vascular Surgery’s Vascular Annual Meeting. The “Surgeons’ Speakeasy” will be open for special Prohibitionstyle cocktails, with flappers and their elegantly clad escorts recreating F. Scott Fitzgerald’s tale of mysteriously wealthy Jay Gatsby and Daisy Buchanan on Long Island in the madcap, music-filled era of the 1920s. This year, the SVS Foundation will offer special early-bird tickets for the “Gatsby Gala,” which will go on sale soon.
Meanwhile, SVS members can turn festive season shopping at www.smile. amazon.com into a donation for the SVS Foundation. For those who have designated the Foundation as their “smile” organization, the retail giant donates 0.5% of every eligible purchase to it.
These donations aren’t restricted to the end of the year. Every purchase that starts on “smile,” garners contributions to the SVS Foundation.
November is Diabetes Awareness Month. To help members help their patients, the Society for Vascular Surgery offers a number of resources, including patient education fliers.
SVS offers not only fliers on diabetes itself, but also on physical activity, which reduces the risk for Type 2 diabetes, and an overall educational flier on vascular disease. In addition, surgeons can point their patients to information on diabetes, treatments and complications contained on the SVS website.
The website also includes material and a link to a supplement published in the Journal of Vascular Surgery called “Management of Diabetic Foot,” with clinical practice guidelines developed by the SVS in collaboration with the American Podiatric Medical Association and the Society for Vascular Medicine.
To view the supplement, visit vascular. org/JVS-DiabeticFootSupplement.
Members also can take advantage of the members-only SVS Branding Toolkit to promote the valuable care they provide their patients with diabetes.
Visit vascular.org/Branding for more information.
For Gala, prepare to return to theRONALD M. WEBB, MD, 75, of Lafayette, California, Oct. 17, 2021, after a battle with Parkinson’s disease.
“We are also especially interested in championing and spotlighting research that deals with disparities, diversity, equity and inclusion”
ANDRES SCHANZER SPOT LIGHT
Apatient-level, propensity-adjusted comparison of three-year results from a quartet of prospective, multicenter trials sup port the primary use of drug-coated balloons (DCBs) versus bare metal stents (BMSs) in moderately complex femoropopliteal lesions, new data show.
Lead researcher Mehdi Shishehbor, DO, revealed adjusted Kaplan-Meier estimates showing a 12-month primary patency of 90.4% for DCB vs. 80.9% for BMS (p=0.007); freedom from 36-month clinically driven target lesion revascularization of 85.6% for DCB vs. 73.7% for BMS (p=0.001); and cumulative 36-month major adverse events of 25.3% for DCB vs. 38.8% for BMS (p<0.001).
The results show “superior effectiveness” in favor of DCB use and no differences in mortality, amputation, or thrombosis, Shishehbor, from University Hospitals Health System,
Compiled by Bryan KayHarrington Heart & Vascular Institute, Cleveland, Ohio, and colleagues report.
Shishehbor delivered the data during the 2022 Vascular Interventional Advances (VIVA) meeting (Oct. 31–Nov. 3) in Las Vegas, with the results published in the Journal of the American College of Cardiology (JACC).

Patient-level data were pooled from the DCB arms of the IN.PACT SFA I/II and IN.PACT SFA Japan randomized controlled trials, and the prospective, multicenter, singlearm COMPLETE SE and DURABILITY II BMS studies. DCBs and BMSs were compared using the inverse probability of treatment weight method with weighted log-rank p values.
“The question for us was comparing the safety and efficacy of DCB versus bare metal stents in patients with femoropopliteal disease who have Rutherford class 2–4,” Shishehbor told VIVA 2022.
A total of 771 patients (288 DCB; 483 BMS) were included in the primary analysis. Demographic, baseline lesion and procedural characteristics were matched between treatment groups after adjustment.
“In this prospective, patient-level pooled analysis with advanced statistical methods comparing the safety and efficacy of DCB vs. bare metal stent in prospectively conducted studies with core lab adjudication, we showed that DCBs had a superior primary patency at 12 months on duplex ultrasound and superior freedom from clinically driven [target lesion revascularization] at 36 months compared to BMS,” Shishehbor concluded at VIVA. “There were no significant differences at 36 months for all-cause mortality amongst the three arms. This analysis supports the use of DCB vs. bare metal stenting in moderately complex femoropopliteal lesions, which are amenable to both treatments.”
Venous stenting: Abre data show ‘struggle to maintain patency’ among post-thrombotic syndrome patients
THE ABRE VENOUS STENT DEMONSTRATED THREE-YEAR PRIMARY PATENCY rates of 97.1%, 76.5% and 70.4% respectively for non-thrombotic iliac vein lesion (NIVL), acute deep vein thrombosis (DVT), and post-thrombotic syndrome (PTS) patient populations within the ABRE clinical study, a late-breaking session at The VEINS (Venous Endovascular Interventional Strategies) 2022 conference (Oct. 30–31) in Las Vegas heard.
Presenter Stephen Black, MD, from Guy’s and St Thomas’ Hospital in London, England, delivered the breakdown of clinical outcomes from the trial based on initial clinical presentation two weeks after revealing an overall effectiveness rate through 36 months of 81.6% and a freedom from clinically driven target lesion revascularization (CD-TLR) rate of 89.3% at the American Vein and Lymphatic Society (AVLS) 2022 annual meeting (Oct. 13–16) in New Orleans. The data show that the “struggle to maintain patency” largely rests in the PTS patient population, Black noted. In terms of secondary endpoints, Black revealed that the study showed no stent fractures through three years, and similarly, no delayed stent migrations. “This speaks to the topic we’ve been continuing to discuss: that stent migration really does seem to be an operator issue rather than a stent issue,” Black told The VEINS 2022 attendees.
Quality-of-life assessments showed a “steep increase” in the first six months, which “was maintained through all the follow-up time points of 12, 24 and 36 months for all the population subgroups, acute DVT, PTS and NIVL,” he said. The same was true for functional assessments of the venous system, Black added. “This was a challenging and complex patient population, with a significant number of patients with PTS with stent extension into the common femoral vein below the inguinal ligament,” he concluded. “[We saw] a sustained primary patency out to 36 months, with the NIVL group in particular performing well. There have been no issues with stent integrity in terms of fracture or delayed stent migration through 36 months. And, most importantly, [we saw] improved quality of life in all presenting subgroups maintained throughout the follow-up period, with similar in venous function.”
W. L. GORE ANNOUNCED THE FIRST implants of its investigational Gore Viafort vascular stent as part of a recently initiated pivotal clinical study for the treatment of inferior vena cava (IVC) occlusive disease with or without iliofemoral vein involvement.

The first patient procedures were completed at the Auckland City Hospital in Auckland, New Zealand, by interventional radiologist Andrew Holden, MD.
“Right now, there are limited device options indicated for both IVC and iliofemoral venous disease,” said Holden. “Implanting the Gore Viafort vascular stent in patients represents a significant step forward in research.”
The stent, which has received Breakthrough Device designation from the Food and Drug Administration (FDA), utilizes expanded polytetrafluoroethylene (ePTFE) technology in conjunction with a singlewound nitinol frame. The Investigational Device Exemption (IDE) study is evaluating the device in a treatment range of 10–28mm diameter for iliofemoral veins and the IVC.
New analysis: Four multicenter trials support primary use of drug-coated balloons over bare metal stents in femoropopliteal lesionsVena cava Stephen Black at the podium
