By Bryan Kay
The
NEW STUDY DEMONSTRATES IVC FILTERS ‘SAFE AND EFFECTIVE’ IN TREATING VENOUS THROMBOEMBOLISM
By Clare Tierney, Jocelyn Hudson, Beth Bales and Urmila Kerslake
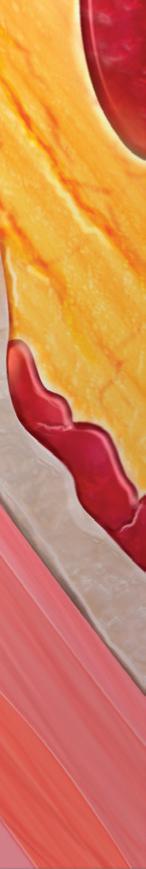
FEW ADVERSE EVENTS ARE connected to the use of inferior vena cava (IVC) filters to help prevent deep vein blood clots from developing into pulmonary embolisms (PEs), according to the findings of the PRESERVE (Predicting the safety and effectiveness of inferior vena cava filters) trial, published jointly in the Journal of Vascular and Interventional Radiology (JVIR) and the Journal of Vascular Surgery Venous and Lymphatic Disorders (JVS-VL). PRESERVE is an FDA-directed
See page 4
COMMENT & ANALYSIS
ABDOMINAL AORTIC ANEURYSM (AAA) DIAGNOSIS
and repair occurs among women almost 10 years later than in men—with similar age-adjusted mortality—the 2023 Society for Clinical Vascular Surgery (SCVS) annual meeting in Miami (March 25–29) is set to be told. The finding is part of a rare U.S. population-based study of AAA trends, spanning nearly 40 years, carried out by researchers at the Mayo Clinic in Rochester, Minnesota, underscoring already established evidence showing that incidence of ruptured AAAs and aortic-related mortality have decreased significantly in the population over time.
The epidemiological analysis was conducted by first-named author Indrani Sen, MBBS, an assistant professor of surgery in the Mayo Clinic Health System, senior researcher Manju Kalra, MBBS, a professor of surgery in Mayo’s division of vascular and endovascular surgery, and colleagues. They used the Rochester Epidemiology Project—which captures population-based data, not merely hospital-based datasets—to track changes over the four-decade-long study period (1980–2017), a stretch of time that includes the coming of the endovascular revolution at the turn of the century, and the institution in 2007 of AAA screening for men at the age of 65 who have ever smoked.
The study included 1,537 patients, 75% of them male and with a median age of 74 years. Diagnosis of AAA was made at pre-
FROM THE SVS PRESIDENT: SUPPORTING ONE ANOTHER
The Society for Vascular Surgery (SVS) has a vision that is unwavering, writes Michael C. Dalsing, MD



We desire quality vascular care for all patients by providing our members with the information and tools they need to provide best care. We believe the goal is the right care, by the right provider, at the right time, and in the right place for each patient.
Over the last few months, there has been much debate amongst members regarding quality and appropriateness of care across various healthcare settings. This stimulated by
See page 6
MARCH 2023 Volume 19 Number 03 In this issue: www.vascularspecialistonline.com THE OFFICIAL NEWSPAPER OF THE Presorted Standard U.S. Postage PAID Permit No. 384 Lebanon Jct. KY ascularV pecialists CHANGE SERVICE REQUESTED 9400 W. Higgins Road, Suite 315 Rosemont, IL 60018
AVF 2023 VS interviews bioprosthetic valve FIH trial investigator
VAM Vascular Annual Meeting registration opens as details of the program are fleshed out
Guest editorial
ABCs for lowerextremity acute DVTs
Comment & analysis
10
17
02
The
07
vascular influencer: Response to February’s editorial on social media
page 4
See
Four decades of AAAs in the US: Rare epidemiological study establishes women are diagnosed and repaired 10 years later than men
SCVS PREVIEW
GUEST EDITORIAL
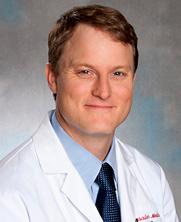
Medical Editor Malachi Sheahan III, MD
Associate Medical Editors
Bernadette Aulivola, MD | O. William
Brown, MD | Elliot L. Chaikof, MD, PhD
| Carlo Dall’Olmo, MD | Alan M. Dietzek
MD, RPVI, FACS | Professor HansHenning Eckstein, MD | John F. Eidt, MD
| Robert Fitridge, MD | Dennis R. Gable, MD | Linda Harris, MD | Krishna Jain, MD | Larry Kraiss, MD | Joann Lohr, MD
| James McKinsey, MD | Joseph Mills, MD | Erica L. Mitchell, MD, MEd, FACS
| Leila Mureebe, MD | Frank Pomposelli, MD | David Rigberg, MD | Clifford Sales, MD | Bhagwan Satiani, MD | Larry Scher, MD | Marc Schermerhorn, MD | Murray
L. Shames, MD | Niten Singh, MD | Frank
J. Veith, MD | Robert Eugene Zierler, MD
Resident/Fellow Editor
Christopher Audu, MD
Executive Director SVS
Kenneth M. Slaw, PhD
Director of Marketing &
Communications Bill Maloney
Managing Editor SVS Beth Bales
Marketing & Social Media Manager
Kristin Crowe
Communications Specialist
Marlén Gomez
Published by BIBA News, which is a subsidiary of BIBA Medical Ltd.
Publisher Roger Greenhalgh
Content Director Urmila Kerslake
Managing Editor Bryan Kay bryan@bibamedical.com
Editorial contribution
Jocelyn Hudson, Will Date, Jamie Bell, Clare Tierney, Eva Malpass and Benjamin Roche
Design Terry Hawes
Advertising Nicole Schmitz nicole@bibamedical.com
Letters to the editor vascularspecialist@vascularsociety.org
BIBA Medical, Europe
526 Fulham Road, London SW6 5NR, United Kingdom
BIBA Medical, North America
155 North Wacker Drive – Suite 4250, Chicago, IL 60606, USA
Vascular Specialist is the official newspaper of the Society for Vascular Surgery and provides the vascular specialist with timely and relevant news and commentary about clinical developments and about the impact of healthcare policy. Content for Vascular Specialist is provided by BIBA News. Content for the news from SVS is provided by the Society for Vascular Surgery. | The ideas and opinions expressed in Vascular Specialist do not necessarily reflect those of the Society or the Publisher. The Society for Vascular Surgery and BIBA News will not assume responsibility for damages, loss, or claims of any kind arising from or related to the information contained in this publication, including any claims related to the products, drugs, or services, or the quality or endorsement of advertised products or services, mentioned herein. The Society for Vascular Surgery headquarters is located at 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. | POSTMASTER: Send changes of address (with old mailing label) to Vascular
Specialist, Subscription Services, 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018.
RECIPIENT: To change your address, e-mail subscriptions@bibamedical.com For missing issue claims, e-mail subscriptions@bibamedical. com. | Vascular Specialist (ISSN 1558-0148) is published monthly for the Society for Vascular Surgery by BIBA News. | Printed by Vomela
Commercial Group | ©Copyright 2023 by the Society for Vascular Surgery
Ashish Gupta, MD, outlines his ABCs for confronting and treating patients with acute deep vein thrombosis (DVT) of the lower extremity, and how he developed his dictums.

A IS FOR “ANTICOAGULATION” FOR NOT MORE than six months of duration. Rationale: At the six-month mark, if the patient is still on anticoagulation, there has to be a reassessment and discussion between patient and healthcare personnel over whether the patient really needs further treatment with anticoagulation. The American Society of Hematology (ASH) guidelines define the treatment period as “initial management” (first five to 21 days), “primary treatment” (first three to six months), and “secondary prevention” (beyond the first three to six months). The guidelines favor shorter courses of anticoagulation (three to six months) associated with a transient risk factor. The guidelines suggest indefinite anticoagulation for most patients with unprovoked DVT associated with a chronic risk factor.
B is for “Be active, Be ambulatory.” Rationale: Many people are told to take it easy, such as limit their walking and stay on bed rest. Both are myths. Both the American College of Chest Physicians and American Physical Therapy Association (APTA) guidelines recommend early ambulation for patients with acute DVT.
C is for “Consider compression stockings or ace wraps.” Rationale: Requirement for compression will be dependent on extent and location of DVT. Per ASH, select patients benefit from compression stockings to help with edema and pain associated with acute DVT.

ABCs background
It is a well-established science that for general treatment of acute DVTs, three to six months of standard anticoagulation, early ambulation, and compression stockings for certain scenarios are recommended.
However, after 17 years of solo private practice in a community setting, I find that these dictums are not being followed the majority of the time.
As vascular surgeons are not the first-line people in treating and diagnosing the majority of DVTs, my personal experience has been that many patients in a wide variety of scenarios are not taken off their anticoagulation (rather they are led to believe that they have to stay on them forever).
Instead of early ambulation, they are told to limit their ambulation post-diagnosis, and only few get their compression stockings prescribed when indicated. Another of my obser vations has been that patients have an inherent feeling of security against DVTs when they are taking blood thinners indefinitely. And when told that you can get off it, they look at you with suspicion and doubt.
Furthermore, I have seen many patients (who have DVT as one of their many diagnoses) admitted in long-term acute care facilities (LTACs) and nursing homes who keep getting their anticoagulation for beyond six months, despite rebounding between hospitals and back to their LTACs and nursing homes. It’s
practically impossible for innumerable rotating physicians, consultants, and emergency room physicians to stop their anticoagulation as they don’t have a total picture of the patient. And their mindset is also: why rock the boat! It is easier to keep the anticoagulation rather than take patients off.
New PCP
Then we also have those patients who move to another city and establish care with a new primary care provider (PCP). And if they have been on anticoagulation with the initial physician, the new PCP continues the same anticoagulation regimen.
On a personal front, I have had several patients over the years who have been on warfarin for several years for a remote DVT (supra- and infrapopliteal), and now they don’t have veins from which to draw blood. When admitted to hospital, they end up getting central lines as they don’t have any peripheral venous access. Also, people with chronic DVT diagnoses found during hospital admissions keep being treated with anticoagulation.
Then there are those several patients who have been on direct oral anticoagulants (DOACs) that don’t require blood testing, but they are paying a lot of money unnecessarily for their medications. They frequently mention that they can’t afford these expensive medications, and ask whether I have samples for them. Finally, how can we forget those patients who get into bleeding complications that are catastrophic. It is obvious that unnecessary anticoagulation is a major risk that patients take while pharmaceutical companies reap their profits.
As March is national DVT Awareness Month, I have been thinking about how to make the treatment algorithm simple for all. This includes patients, their family members, medical students, residents, fellows, practicing doctors (PCPs, hematologists, cardiologists, pulmonologists, internists, vascular surgeons, interventional radiologists), nurse practitioners, physician assistants, and anyone who comes in contact with DVTs. And what better way than using a simple acronym? In the spirit of global awareness and education, I came up with a simple catchy phrase/triad: “Dr. Ashish Gupta’s ABCs for treatment of lower-extremity acute DVTs.”
I strongly believe that implementation of this acronym will help all involved remember easily how to manage DVT
This acronym is by no means discriminating between treatment of supra- and infrapopliteal DVTs, as some do treat infrapopliteal DVTs, on a case-by-case basis, with anticoagulation and/or with follow-up venous duplex for evaluation of propagation. Even if someone is treated for infrapopliteal DVT, their anticoagulation should be stopped by six months at the latest, if not sooner. The hope is to make this acronym a framework for all involved in the treatment of DVTs in order to raise awareness of the ABCs, and not simply over treat.
I strongly believe that implementation of this acronym will help all involved remember easily how to manage DVTs, empower patients and caregivers, and will avoid unnecessary use of anticoagulation, avoid costs, and reduce major complications that can come from diagnosis of DVT. The implications during DVT Awareness Month of this acronym can be exponentially beneficial and fruitful in terms of best practices, where not only healthcare providers, but even patients and their family members can remind themselves at six months whether they need anticoagulants anymore.

Vascular Specialist | March 2023 2
ASHISH GUPTA, MD, is a board certified vascular and endovascular surgeon practicing in Wyandotte, Michigan, as a solo private practitioner since 2005.
ABCs for the treatment of lower-extremity acute DVTs
Advanced Surgical A llograft Products
AMNIOFIX® and AMNIOEFFECT ® are placental-based sheet allografts providing a protective barrier to support the healing cascade and the development of granulation tissue.
AXIOFILL® is an acellular human placental ECM particulate used in the replacement or supplementation of damaged or inadequate integumental tissue.

RCT Outcomes with DHACM
DFUs:
2x to 3.8x faster
defect closure vs. SOC1,2*
CONTACT US: Scan the code or visit www.mimedx.com/contact
for the treatment of venous leg ulcers. Int Wound J. 2018;15(1):114-122. 4. Bianchi C, Tettelbach W, Istwan N, et al. Variations in study outcomes relative to intention-to-treat and per-protocol data analysis techniques in the evaluation of efficacy for treatment of venous leg ulcers with dehydrated human amnion/chorion membrane allograft. Int Wound J. 2019;16(3):761-767.
Patents and patents pending see: www.mimedx.com/patents. AMNIOEFFECT, AMNIOFIX, AXIOFILL, PURION, and MIMEDX are trademarks of MIMEDX Group, Inc. ©2023 MIMEDX Group, Inc. All Rights Reserved. www.mimedx.com US-LS-2200045 v1.0

LEARN
MORE
WHEN LIMB DEFECTS HAVE DELAYED HEALING, YOUR PATIENT IS AT RISK OF AN AMPUTATION.1
VLUs:
DHACM = Dehydrated Amnion/Chorion Membrane DFU = Diabetic Foot Ulcer VLU = Venous Leg Ulcer SOC = Standard of Care
* 2x = based on mean time and 3.8x = based on median time, ^ Per Protocol group, † Mean percentage in defect size vs. baseline 1. Zelen CM, Serena TE, Denoziere G, Fetterolf DE. A prospective randomised comparative parallel study of amniotic membrane wound graft in the management of diabetic foot ulcers. Int Wound J. 2013;10(5):502-507. 2. Zelen CM, Gould L, Serena TE, Carter MJ, Keller J, Li WW. A prospective, randomised, controlled, multi-centre comparative effectiveness study of healing using dehydrated human amnion/chorion membrane allograft, bioengineered skin substitute or standard of care for treatment of chronic lower extremity diabetic ulcers. Int Wound J. 2015;12(6):724-732. 3. Bianchi C, Cazzell S, Vayser D, et al. A multicentre randomised controlled trial evaluating the efficacy of dehydrated human amnion/chorion membrane (EPIFIX®) allograft
THINK ASAP
1.6x the defect closure rate vs. SOC at 16 weeks3,4^
NEW! NEW!
NEW STUDY DEMONSTRATES IVC FILTERS ‘SAFE AND EFFECTIVE’ IN TREATING VENOUS THROMBOEMBOLISM
continued from page 1
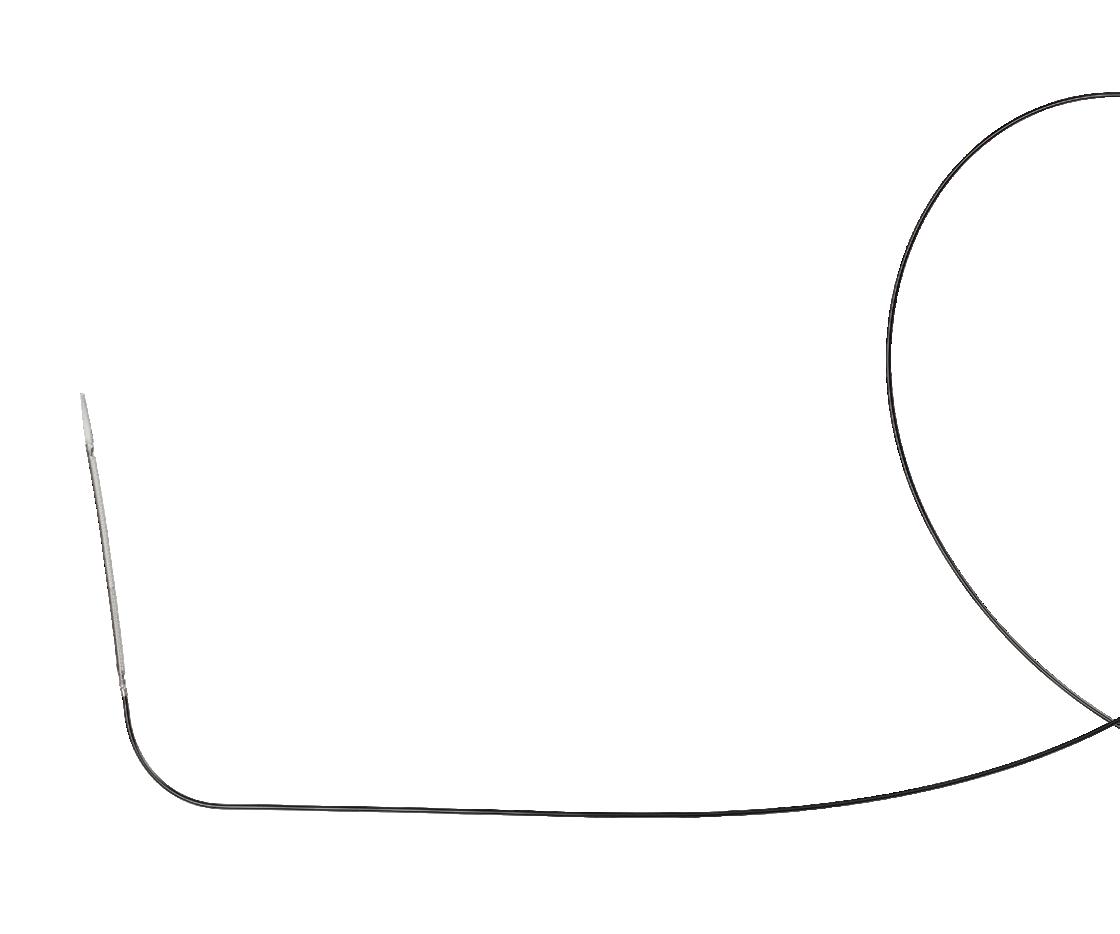
multicenter, prospective, open-label, non-randomized trial that studied the safety and efficacy of IVC filters from six manufacturers. It was a joint effort of the Society of Interventional Radiology (SIR) and the Society for Vascular Surgery (SVS). The study was conducted at 54 sites in the U.S. between Oct. 10, 2015, and March 31, 2019. During that time, filters were implanted in 1,421 patients, of whom 1,019 patients had an existing deep vein thrombosis (DVT) or PE.
Researchers found that IVC filters were effective in helping to prevent PEs in patients experiencing a DVT where anticoagulation medicines failed or were not an option for the patient. Approximately half of the patients in the study had their filters removed within three months of placement without complication or recurrence.
“The question should not be only ‘should we place a filter?’ but ‘how should we offer comprehensive filter-inclusive care of patients with venous blood clots, comprised of a detailed patient evaluation, a plan for retrieval after placement, and frequent follow-up with evaluation for filter removal or replacement,’” said Matthew S. Johnson, MD, an interventional radiologist and professor of radiology and surgery at Indiana University School of Medicine in Indianapolis, and coprincipal investigator on PRESERVE. “PRESERVE showed what questions we should ask as clinicians: ‘Does this person continue to require protection against PE, and, in light of changing clinical status and available therapies, is the current filter needed?’ And then make an informed decision on how to continue care.”
Vascular surgeon David Gillespie, MD, spoke on PRESERVE at the VEITHsymposium 2022. “DVTs and PEs are a significant cause of death worldwide, and understanding fully how tools like IVC filters can be used to prevent the progression of a DVT into a PE allows physicians to safely treat patients at risk of death from venous thromboembolism [VTE],” said
Gillespie, of Beth Israel Deaconess Medical Center in Brockton, Massachusetts, and co-principal investigator on PRESERVE. “Now that the study is complete, we have a roadmap for better filter utilization. We need to solidify a clearer set of practice guidelines for venous thromboembolic disease, based on its symptoms, location and complications. Further studies will focus on how the different manifestations of venous thromboembolic disease may benefit from filter-inclusive care.” Gillespie said that “approximately 10 years ago or so, the clinical management of patients with VTE and the prophylaxis of potential VTE in trauma patients was not well studied with regard to the use of IVC filters.” The result of the PRESERVE trial has been that “essentially, these filters are safe and effective for therapeutic [and prophylactic] use in the patient population [in question],” he continued, and this despite the “challenges” of the COVID-19 pandemic, the “high dropout rate,” and the fact that “a large number of patients” had their filters removed.
To date, PRESERVE is the largest prospective study investigating the real-world patient outcomes of IVC filter use. “Congratulations to Dr. Gillespie, Dr. Johnson, and their many colleagues for shepherding this large collaborative multispecialty, multicenter clinical trial to completion,” said SVS President Michael C. Dalsing, MD. “This highly impactful study provides the realworld evidence needed when recommending IVC filter placement to protect our patients from a potentially lethal disease and when to remove that filter after it has accomplished the desired effect.”
from page 1
sentation with rupture in 95 patients, the research team found—with 75% presenting before and 66% after Medicare established ultrasound screening criteria. “Overall, only 16% AAAs were detected on screening, 23% after 2007, with no significant change per year,” they report. “Patients with incidentally detected AAAs were older, had larger AAAs, more likely female, and to present with rupture, but had similar incidence of progression to and type of repair.”
Overall surviv al in AAA patients was 94%, 72% and 34% at one, five and 15 years—“significantly lower than age and sex-matched controls throughout the study,” Sen et al established.
“Traditionally, it has been believed that based upon single-center series, VQI registry studies, hospital-based data, that outcomes in women are poorer than in men,” says Kalra in an interview with Vascular Specialist ahead of SCVS 2023. “Traditionally, aneurysms have been picked up much less frequently in women than in men. We also know that the actual incidence is lower per 100,000 [patient years], which is what we have confirmed yet again with this population-based study.”


Sen points to the finding around the disparity involving female diagnosis and repair as breaking new ground in this area of AAA. “All the rest of the findings are supportive data for a lot of trends we already see, but nobody has ever actually put it down on paper that aneurysms are diagnosed and repaired in women almost a decade later than men with similar age-adjusted mortality,” she says. “What additionally came to light from this study was that, even though the screening guidelines came in over a decade ago, incidental detection is still the commonest [avenue].”
They now have a new baseline to address these issues, Sen continues. She points to newly initiated research in the UK set to look into AAAs in women. The multinational collaboration of researchers received endorsement from the Global Cardiovascular Research Funders Forum (GCRFF)
Multinational Clinical Trials Initiative for the WARRIORS (Women’s abdominal aortic aneurysm research: repair immediately or routine surveillance) trial. It aims to answer the question: Should women have their aneurysms repaired electively using endovascular aneurysm repair (EVAR) at smaller diameters than men to improve their survival and quality of life? Imperial College London in London, England, is co-ordinating the study, but it will include collaboration with vascular surgeons from Canada, Denmark, The Netherlands, and Sweden, as well as the U.S.
The investigators behind WARRIORS have noted that the rationale and need for this trial, which seeks to recruit nearly 1,200 women, stems from the poor outcomes suffered by women with AAAs. Although women contribute 15–20% of
total AAA burden, and one-third of ruptures, they have been significantly underrepresented in trials which guide current AAA repair, the WARRIORS investigators detailed, adding that women have smaller arteries, a four-fold higher rupture risk, and lose eligibility for EVAR at smaller AAA diameters.
“We have learnt that women worry a lot about their AAA, and modeling has suggested that repair of AAA at 4cm for women might re sult in improved quality of life and reduced overall cost,” the WAR RIORS investigators recently commented.
“These potential benefits as well as reduction in aneurysm-related mortality, would need to be balanced against the operative risk of early repair.” They state that these areas of uncertainty, regarding the optimal strategy for AAA repair in women, are what the trial seeks to answer.
The Mayo epidemiological study provides timely data pointing to the fact that these and similar questions regarding aneurysms in women are relevant, Sen adds. The need for a population-based study to highlight these was great, Sen and Kalra relate.
“We don’t have good natural history data, or epidemiology, of aortic aneurysms in the U.S.,” remarks Sen. “Everything that we use, we take from studies performed in Europe and Australia.
Among the few studies performed in the U.S., one of them was from this same Rochester epidemiology data—which was in the 1980s. Since the 80s, the two major changes that have happened are the introduction of endovascular repair, which has become the commonest way of repairing these AAAs, and the introduction of a screening protocol for men.”
The questions that the research team were looking to answer were: Do advances in screening really work? How comprehensive is the adoption of the program, and who is being screened? “Are we identifying more aneurysms in women as a side effect?” adds Sen. “A lot has changed in clinical practice, and the outcomes of this are being reported using large hospital-based treatment datasets.” The impact of these developments and changes at a population level was not known, Kalra chimes in, nodding toward the questions around potential benefits of early detection of these aneurysms in women, “although data exists that screening for them has been shown not to be cost-effective.” She says the chief finding was actually something of a surprise. “It’s not that women do poorly with AAA repair, it’s because they are nearly a decade older by the time you are fixing them,” adds Kalra.
As they concentrate their efforts on this particular area of the dataset, Sen says future efforts and analysis will be aimed at getting to the bottom of factors that lead to later diagnosis and repair of aneurysms in women.
Vascular Specialist | March 2023 4
“Now that the study is complete, we have a roadmap for better filter utilization”
DAVID L. GILLESPIE
FROM THE COVER: FOUR DECADES OF AAAs IN THE US: RARE EPIDEMIOLOGICAL STUDY ESTABLISHES WOMEN ARE DIAGNOSED AND REPAIRED A DECADE LATER THAN MEN continued
“It’s not that women do poorly—it’s because women are nearly a decade older when you are fixing them”
MANJU KALRA
Indrani Sen
Manju Kalra
“Nobody has ever actually put it down on paper that aneurysms are diagnosed and repaired in women almost a decade later than men”
INDRANI SEN
Click, flush, go
Take charge of CLTI†
HawkOne™ Directional Atherectomy System
Providing versatility and simplicity, streamlining procedural efficiency‡ with a click-in cutter driver and a quick-flush catheter.

medtronic.com/takechargeofCLTI
†Treat above and below the knee.
‡Compared to TurboHawk™ directional atherectomy.
Important Information: Indications, contraindications, warnings, and instructions for use can be found in the product labeling supplied with each device. Indications for Use: The HawkOne™ directional atherectomy system is intended for use in atherectomy of the peripheral vasculature. The HawkOne catheter is indicated for use in conjunction with the SpiderFX™ embolic protection device in the treatment of severely calcified lesions. The HawkOne catheter is NOT intended for use in the coronary, carotid, iliac, or renal vasculature. Caution: Federal (USA) law restricts this product for sale by or on the order of a physician.
UC202218083-01 EN ©2022 Medtronic. Medtronic and the Medtronic logo are trademarks of Medtronic. All other brands are trademarks of a Medtronic company. For distribution in the USA only. 11/2022
COMMENT& ANALYSIS
continued from page 1
recent research conducted, published,
recent research conducted, published, and presented by colleagues from Johns Hopkins University, as well as other work published by academic surgeons in the recent past. Before going any further I would like to make two points absolutely clear and unequivocal:
● SVS is 100% supportive, and a champion, for all of its members working hard to provide quality care of patients regardless of site of service. Championing the “right care-right provider-right time-right place” mantra requires the SVS, and all of us, to embrace and continue to improve care for patients wherever it is delivered.
and continue to improve care for patients wherever it is delivered.
values that we follow best science and best evidence
● SVS has always embraced as one of its highest core values, that we follow best science and best evidence to inform and improve our specialty. This means we question, challenge and debate to be sure, but in the interest of strengthening evidence that will help us to take better care of our patients.
It is with these principles in mind that, on Feb. 24, representatives from academic and private practice, along with SVS leadership, had a productive meeting to address the ongoing issues and perceptions that resulted from recent publications and presentations. We openly discussed any misunderstandings and sought to find a constructive path forward.
A primary issue was the discovery of strong correlations within the Medicare database that demonstrated a signal of inappropriate care by extreme outliers. In some cases, these outlier occurrences were found more likely associated with the office-based lab (OBL) setting. Importantly, most outliers were not vascular surgeons
Some members of the vascular surgery community working in the OBL setting interpreted the conclusions and discussions of this correlational data as a general accusation of providing inappropriate care for personal gain.
On our call, it quickly became very clear that everyone wanted the best care possible for our vascular patients. The Medicare database research did point out signals of concern that should worry all of us, that are deserving of more research, and must be addressed through policy, education, and quality improvement. Everyone agreed that the OBL can and does provide an accessible, affordable, patient-friendly setting with vascular surgeons who provide excellent patient care. It was further observed that the other part of the story has been lost in the controversy. The vast majority of vascular surgeons in all practice settings are meeting or exceeding practice guidelines and appropriate use criteria (AUC) recommendations to provide quality care. Other specialty providers seeking to expand their role in vascular interventions and care fall short of this metric much more often. Even so, we need to address any issues within our own community to be “the best we can be for our patients”.
Research from our SVS members provides us with the information we need to consider as potential challenges and opportunities to improve patient care. Some research utilizing “big data” and/or retrospective data highlights “associations” that alert us to potential issues that need to be addressed. These data raise important questions and help inform our discussions around quality care. We discussed that the intentions of the data and its interpretation are not always well aligned, and how open discussion around this is important.
In addition, from the research perspective, what is lacking from the current administrative databases is direct information on the “cause and effect” of clinical questions. During our meeting, there were plans made for our academic vascular surgeon researchers and private practice vascular surgeons to collaborate on pertinent questions that need to be answered—some notably around the cost of care delivery, with research methodologies that are sufficiently robust to conclusively
found more We discussed that the data and its interpretation are not always well aligned, can be overstated, and how open what is lacking from the current administrative databases is direct information on the “cause and effect” of clinical questions. During our meeting, there were plans made for our academic vascular surgeon researchers and private practice surgeons to collaborate on pertinent questions that need to be answered—some around the cost of care delivery, with research methodologies that are sufficiently robust to conclusively answer “cause-and-effect” questions.
answer “cause-and-effect” questions. This most recent debate and dialogue has resulted in improvements in the peer-review process of the Journal of Vascular Surgery Although the editors have previously strived to diversify the reviewer database, there have been few reviewers who were community practice vascular surgeons and/or who worked in OBLs, until now. The editors are grateful for those who have volunteered to review papers, and to write commentaries explaining the nuances of OBL practice and economics.
This most recent debate and dialogue has resulted in improvements in the peer-review process of the Journal of Vascular Surgery. Although the editors have previously strived to diversify the reviewer database, there have been few reviewers who were community practice vascular surgeons and/or who worked in OBLs, until now. The editors are grateful for those who have volunteered to review papers, and to write commentaries explaining the nuances of OBL practice and economics.
From a clinical perspective, we all understand that there is work to be done. There are outliers providing care that deviates from current best or even acceptable practice. The SVS has no direct (legal) knowledge of local vascular care delivery and cannot police these issues
From a clinical perspective, we all understand that there is work to be done. There are outliers providing care that deviates from current best or even acceptable practice. The SVS has no direct (legal) knowledge of local vascular care delivery and cannot police these issues for our members. We can provide the tools to do the
Vascular surgery is a unique specialty with its many sites of service to provide care for our patients. Much of vascular care can be provided outside of a hospital; the OBL setting can provide vascular care in a more accessible, less costly and convenient manner for some of our patients. This relatively new site of service has some unique payment aspects that need clarification. In the Medicare database, Medicare-allowed charges for care are reported. However, these data do not account for all aspects of care, including rent, ancillary service/products (including payment of associate staff), supplies, devices, insurance, and the physician payment so important to consider in the OBL setting. How the cost of care delivery is reimbursed is a question many seem to struggle with if SVSConnect comments are any indication. To add one more way to improve understanding of how this works and to promote an informed readership, a reporting standards document on the cost of care delivery in research publications is in the works.
sites of service to provide care for our patients. Much of vascular care can be provided outside of a hospital; the OBL setting can provide vascular care in a more accessible, less costly and convenient manner for some of our patients. This relatively new site of service has some unique payment aspects that need clarification. In the Medicare database, Medicare-allowed charges for care are reported. However, these data do not account for all aspects of care, including rent, ancillary service/products (including payment of associate staff), supplies, devices, insurance, and the physician payment so important to consider in the OBL setting. How the cost of care delivery is reimbursed is a question many seem to struggle with if SVSConnect comments are any indication. To add one more way to improve understanding of how this works and to promote an informed readership, a reporting standards document on the cost of care delivery in research publications is in the works.
The OBL site of service currently has few requirements in place to ensure patient safety and quality vascular care. Some in the OBL space already have instituted robust measures to provide the oversight and metrics needed for best patient care. The SVS leadership and members working in the OBL site of service believe such oversight and quality improvement measures are important to ensure a safe patient experience that will improve over time. We recommend the use of the ACS-SVS Vascular Quality Program to benchmark care in this new site of service. In addition to patient safety, it is our hope that it provides the infrastructure for quality care improvement and OBL-specific research.
The OBL site of service currently has few requirements in place to ensure patient safety and quality vascular care. Some in the OBL space already have instituted robust measures to provide the oversight and metrics needed for best patient care. The SVS leadership and members working in the OBL site of service believe such oversight and quality improvement measures are important to ensure a safe patient experience that will improve over time. We recommend the use of the ACS-SVS Vascular Quality Program to benchmark care in this new site of service. In addition to patient safety, it is our hope that it provides the infrastructure for quality care improvement and OBL-specific research.
I would be remiss if I did not also make a few comments regarding social media. It is important to stress that every SVS member has the right to post whatever they wish on social media.
for our members. We can provide the tools to do the best job we can for our patients. The SVS leaders, and the members present at this meeting, do stand behind quality vascular care as outlined in our clinical practice guidelines and AUC documents. Clinical vascular care is an art influenced by the science available. Clinical guidelines and AUC documents provide the current best science we have for the art that must be practiced. The SVS provides this information to our members as rapidly as possible.
best job we can for our patients. The SVS leaders, and the members present at this meeting, do stand behind quality vascular care as outlined in our clinical practice guidelines and AUC documents. Clinical vascular care is an art influenced by the science available. Clinical guidelines and AUC documents provide the current best science we have for the art that must be practiced. The SVS provides this information to our members as rapidly as possible.
Perhaps the most important and potentially influential exemplar is the national launch of the new American College of Surgeons (ACS)-SVS Vascular Quality Program (“ACS-VP: A Quality Program with the Society for Vascular Surgery”). If you care about quality and patient safety, I encourage all SVS members to participate in this “vascular center of excellence” program, built around quality improvement.
Perhaps the most important and potentially influential exemplar is the national launch of the new American College of Surgeons (ACS)-SVS Vascular Quality Program (“ACS-VP: A Quality Program with the Society for Vascular Surgery”). If you care about quality and patient safety, I encourage all SVS members to participate in this “vascular center of excellence” program, built around quality improvement.
Vascular surgery is a unique specialty with its many
The SVS’ own guidelines, published by its then-Young Surgeons Committee, now a section, provide important insight and strategy on how to leverage social media for positive gain rather than negative effect.1 All SVS members should refer to these guidelines as a resource in their use of social media. I ask our members to be mindful about respecting their peers on private platforms such as SVSConnect
I would be remiss if I did not also make a few comments regarding social media. It is important to stress that every SVS member has the right to post whatever they wish on social media. The SVS’ own guidelines, published by its then-Young Surgeons Committee, provide important insight and strategy on how to leverage social media for positive gain rather than negative effect.1 All SVS members should refer to these guidelines as a resource in their use of social media. I ask our members to be mindful about respecting their peers on private platforms such as SVSConnect
advance vascular care.
Becoming a vascular surgeon is a unique and impactful choice made by all of us. Our professional compass is aligned in intangible ways—we need to embrace our goals and propel our specialty forward.

Let’s take this opportunity to rededicate ourselves to supporting one another, focusing in a unified manner to address the very real challenges that surround us. Only by working as a team can we hope to rapidly advance vascular care. Becoming a vascular surgeon is a unique and impactful choice made by all of us. Our professional compass is aligned in intangible ways—we need to embrace our common goals and propel our specialty forward.
Reference
Reference
1. Gifford ED, Mouawad NJ, Bowser KE, Bush RL, Chandra V, Coleman DM, et al. Society for Vascular Surgery best practice recommendations for use of social media. J Vasc Surg 2021;74:1783-91.
1. Gifford ED, Mouawad NJ, Bowser KE, Bush RL, Chandra V, Coleman DM, et al. Society for Vascular Surgery best practice recommendations for use of social media. J Vasc Surg 2021;74:1783-91.
MICHAEL C. DALSING, MD, is the current SVS president.
Vascular Specialist | March 2023 6
MICHAEL C. DALSING, MD, is the current SVS president.
FROM THE SVS PRESIDENT: SUPPORTING ONE ANOTHER
“The vast majority of vascular surgeons in all practice settings are meeting or exceeding practice guidelines and AUC recommendations”
The vascular influencer:
Dear editor,
READING “LIKES, DISLIKES AND reposts: The new age of the vascular surgery influencer,” by Drs. Jean Bismuth (@jeanbismuth) and Jonathan Cardella (@yalevascular), they rightly point the spotlight on the trend of some vascular surgeons posting cases on social media for the purposes of self-promotion, virtue signaling, and influencing.
I can agree with their point that many of these posts are made by mediocre practitioners who display only the best and curated images, but I felt uncomfortable with the feeling that I may be one of those people being castigated for over-exposure on social media. They warn the readers of the dangers of misinformation fed to an uninformed public, but overlook the potential of social media for education and community. Being a vascular surgeon who has been on social media for over 15 years, there are reasons why I am here which are not explained by this article.
Be the lede
My journey started with hacking Google searches. My first job out of fellowship was a faculty position at my medical alma mater, Columbia P&S. The PR department asked everyone to compose a blurb for a web page and after searching on Google on how to rise in a Google search, I wrote out a paragraph full of the right verbiage to maximize my relevance on search. It wasn’t very difficult in 2002 to do this. Searching “vascular surgeon in New York” on Google after posting that info page consistently brought me up to the top five links, ahead of whole departments and many big names. I did over 400 cases my first year out, and I really felt if I could make it there, I could make it anywhere.
Bury the lede
Unfortunately, like many vascular surgeons in New York, I got named in a lawsuit, and like many young surgeons with limited means and large loans to pay off, I couldn’t fight it and took the advice of hospital lawyers and settled. After that lawsuit, a Google search would return an article by the law industry PR around 2007, and I was at that point very busy in private practice in Iowa. It was so discouraging seeing that as the only thing speaking for me. I decided that I had to take an active part in shaping the message around me, to not let my Google search profile be defined by that article.
I decided to write and figured a few articles every week over a year would bury
that article behind many better articles. I began to blog about something I am both horrible at but aspire to greatness in –golf (www.golfism.org). Writing about myself and my struggles in golf and being a young father and husband was how I found my voice. It was during this period I found my best pieces were when I gave something of myself.
After finding my author legs, I began writing about vascular surgery, something I’m pretty good at but aspire to greatness in, on a personal blog (docparkblog, on Apple’s defunct cloud service). After a year, the blog got only 30-50 hits a day, at most 100. By internet standards, that’s low, and I kept my day job. After giving a talk at Midwest Vascular to an audience of about 50 mildly interested surgeons, that 30–50 engaged readers on my blog a day felt pretty good. A hundred was amazing. Medscape eventually tapped me for blogging on their site. My blog there, “The Pipes Are Calling,” was rated among the top five most-read medical blogs in the world when I shut it down in 2011.
The influencer
This social media presence generated influence -I was asked to participate in prominent research trials like PIVOTAL, CVRx, and CREST and others despite being in private practice. This is common now, but rare 15 years ago. The blogging did bury the lede. It eventually generated misunderstanding in the hospital administration at that time in 2011 and I was asked to stop blogging, at least until they could figure out what this internet thing was about.
In 2012, I joined the Cleveland Clinic, I huddled with their social media department and came up with ironclad rules:
1. All accounts were to have the header
that posts and articles were my own opinion and not of my employer
2. All patients sign a media release for posting of case histories and images
After launching www.vascsurg.me in 2013, I chose to focus on technique and opinion. I used my LinkedIn and Twitter accounts to promote my articles. I always communicate in my authentic voice, although over the years, I’ve toned down the irony which is frequently misunderstood. In moving to my current hospital, University Hospitals, the first thing I did was arrange for a social media release and confirm what I was doing was okay. In reading the article by Drs. Bismuth and Cardella, in 2023, misunderstanding is still at the core of arguments against the use of social media.

The worst
I have seen egregious examples of bad behavior on social media by physicians, as mentioned in the article. On my Twitter stream, I’ve seen people put stents in subclavian veins for thoracic outlet compression and wait for praise, which they get from similarly ill-informed people who don’t realize I see patients like this several times a year with swollen arms and faces. While I was in Abu Dhabi, someone put stents in a patient from the common femoral to popliteal artery, and received accolades for “minimally invasive skills” from all corners of the globe, only for me to remove the stents a month later and perform fasciotomies on the same patient—a middle-aged claudicator! There, I couldn’t post a rebuttal to the original case presentation because of local social media laws. Despite the word getting out, the surgeon only doubled down on his minimally-invasive fantasies. About the same time, I witnessed a relatively famous person self-implode on Twitter while accusing vascular surgeons of butchery (his words) by supporting open surgery over head-to-toe interventions. He got crushed by the general disapproval of his misrepresentation and personal bullying of a vascular surgeon, and then disappeared from social media. Evaporated. Good. We all have to do better.
The best
I have also seen patients with rare diseases such as median arcuate ligament syndrome reach out and connect with each other and with physicians about diseases that aren’t taught in medical school or residency training on social media. There are Facebook groups, Twitter hashtags, and sub-Reddits—rich communities of people who have to make serious decisions about their lives, many with limited access to specialists in their far-flung burgs and precincts. I think the fear is that bad decisions will be made based on bad information, but even in the highest, most rarified medical institutions, patients may get misguidance, have
a complication, a poor outcome, in-person which can be worse than a social media interaction. If we value patient autonomy, access to the best information needs to be available. Social media lowers the barriers to access, for bad or good. Yes, it can do a whole lot of bad, but also an immense amount of good.
Keeping it real
The authors are correct in that people will prefer to promote themselves rather than air complications and bad outcomes. The American surgical M&M process is an amazing and cherished tradition and protected process. It has no place in social media. Most surgeons also take the view that social media presence doesn’t lengthen your CV, it doesn’t bill. The many cheap suits of medical social media, the hawkers, the hucksters, the fragile egos, will always be there on Twitter and LinkedIn.
But other functions such as access and broad dissemination of information, experience, and opinion, are legitimate and critical. Comparatively few people get the message from a closed academic conferences and traditional modes of dissemination are slow. Most of the best social media posts are, as the authors mention, case reports. They fail to mention case reports under “open access” cost about $500 to publish.
The peer review process, which I participate in, results in sometimes glacial turnaround times with papers landing often a year or more after presentation at a conference. I also learned from my time in private practice that these barriers block the voices of many legitimately great surgeons whose remarkable talents are only shared locally. I also learn from my time in academic practice that too many departments are not multiplicities of talents, but shops built around single personalities, who may declare that having never seen something, it cannot exist—to the detriment of those with unseen problems. Social media is the great leveler for patients and surgeons. It brings needed exposure to young surgeons building practices, while connecting people searching for solutions to people who may have a clue. The voices of non-academic surgeons are given a platform to broadly share their experience. If legitimately good people are dissuaded from participating, only the cheap suits will remain. As always, caveat emptor, et primum non nocere
www.vascularspecialistonline.com 7
W. Michael Park, MD University Hospitals, Cleveland
“If legitimately good people are dissuaded from participating, only the cheap suits will remain”
COMMENT& ANALYSIS LETTER TO THE EDITOR
W. Michael Park
COMMENT& ANALYSIS CORNER STITCH
What I wish I had known in vascular training
By J. Aaron Barnes, MD
WELCOME NEWLY MATCHED vascular surgery residents into the fold! I am just over six months into my first attending position after completing my residency training at Dartmouth. While nothing reminds you of how much you don’t know or haven’t seen like being an early career attending, I suppose I am now in a position to reflect back on what I wish I knew or did differently in training. This is certainly not an exhaustive list, but I write this in the hopes that current trainees and those who just matched into vascular surgery are able to find something that resonates with them.
You are a product of your environment
“Gentle, gentle!” This was a phrase that had been said to me—and at me—countless times and at many different volumes throughout my training by a specific attending. I did not fully appreciate the extent to which this phrase was burned into my psyche until I noticed I was often muttering it to myself alone while operating as a new attending
in Alaska. This is just one small example of how we become products of the environment in which we train.
From quirky idioms to highly specific operative techniques, we are shaped by those who train us. Some of the things we learn are obvious—techniques are taught, knowledge is conferred through didactics—while others are subtle. How an attending explains long-term stroke risk in clinic, establishes and maintains a relationship with a referring provider, or speaks with a family after a poor outcome, are not taught but rather observed. I wish I had paid more attention to how my attendings practiced and navigated these crucial yet less obvious aspects of being a vascular surgeon as a trainee.
The things that are ‘mindless’ can be anything but
The night before I performed my first lower-extremity bypass as an attending, I pored over the patient’s chart and history, reviewed the diagnostic studies and pre-operative imaging, studied the anatomy, confirmed we had all necessary equipment available, and made contingency plans in case things went awry. I arrived the morning of surgery feeling ready. This confidence all came crashing down when the circulator asked me what drapes I wanted to use. It took longer than I want to admit to recall the default drape configuration from residency. Fortunately, I was able to pull the information from the
recesses of my mind, and the case was soon underway. This instance, plus a few others that can be described as less than glamorous, made me wish I had paid closer attention to the seemingly mundane things like draping and room setup as a trainee.
Go back to go forward
As in many training programs, I had my pick of cases as a chief resident. My weeks were filled with open aortic cases, complex endovascular aortic aneurysm repairs (EVARs), carotid endarterectomies, transcarotid artery revascularizations, and a smattering of lower-extremity bypasses. Towards the end of my training, though, I was given the opportunity to perform various less complex procedures such as venous ablations, arteriovenous fistula creations, and straightforward peripheral bypasses without the assistance of an attending scrubbed in. These experiences were invaluable. Those “intern-level” cases are part of my current practice and I needed to freshen up on them. I needed to learn to operate alone, as I do many of my cases without an assistant today. While I am thankful for the experiences I did have, I wish I would have made more of an effort to seek out those autonomous experiences with simple cases earlier and more frequently in my training.
VARICOSE VEINS
Dexter reported that 12-month follow-up among 176 patients was completed, with 20% presenting with a PTS Villalta score of greater than 4—and 17 limbs, or 10.5%, with a score greater than 9 (moderate or severe).
There is a method to the madness
The transition from trainee to attending is a little bizarre. Seemingly overnight your role in the surgical hierarchy flips, and you suddenly have more say over your schedule, your cases, and your patients’ care. Now that I am a bit more removed from training, I can look back and see the gradual transition from trainee to attending. I can now appreciate so many aspects of my training program. Case conference forced me to come up with case plans, defend their indications, and have backup plans. Sizing and ordering devices for EVARs in residency prepared me to do so confidently in the middle of the night as an attending for a rupture. Morbidity and mortality conferences taught me to critically examine my complications and identify areas to target to improve outcomes. In the moment and taken individually, these and many other aspects of training, can be seen as mundane. When taken as a whole, these tasks shape us into vascular surgeons. I am not sure it is possible to truly appreciate the entirety of training when you are in the midst of it, but I wish I had known as a trainee that I would eventually understand the method to the madness.
Results from first US trial of Sonovein delivered
THE 2023 ANNUAL MEETING OF THE AMERICAN VENOUS FORUM (AVF) heard the final results from the first U.S. trial of emerging varicose vein treatment, Sonovein echotherapy, with data showing 100% technical feasibility at three months—the principal study objective.

INTERIM ONE-YEAR OUTCOMES from the multicenter, prospective, single-arm CLOUT registry investigating use of the ClotTriever thrombectomy system in all-comer patients with deep vein thrombosis (DVT) demonstrated that 93.5% of limbs had flow present, 97.1% were compressible and 10.5% of patients presented with moderate or severe post-thrombotic syndrome (PTS).
The results were presented by David Dexter, MD, an assistant professor of surgery at Eastern Virginia Medical School in Norfolk, Virginia, at the 2023 annual meeting of the American Venous Forum (AVF) in San Antonio, Texas (Feb. 22–25).



The primary effectiveness endpoint— complete or near-complete (≥75%) clot removal, assessed by an independent core laboratory—was achieved in 91.2% of patients. Nearly two-thirds of patients saw complete thrombus removal. “Patients reported immediate symptom relief and demonstrated sustained improvements in one-year clinical and quality-of-life outcomes,” Dexter told AVF 2023. Rates of PTS “remained low” at the one-year mark, he added.
Dexter concluded: “This one-year interim analysis from the real-world CLOUT registry indicates that the ClotTriever system can effectively remove thrombi with significant and sustained long-term clinical improvements, including PTS, pain, and quality of life. Follow-up with the complete dataset to two years is ongoing.”— Bryan
Kay
Antonios Gasparis, MD, director of the Center for Vein Care at Stony Brook University in Stony Brook, New York, told the AVF gathering in San Antonio, Texas (Feb. 22–25), that the Food and Drug Administration (FDA)-approved trial saw 20 great saphenous veins (GSVs) in 18 patients receive treatment using the high-intensity focused ultrasound (HIFU) proce-dure. Gasparis said no anesthesia was used during the cases and that there was no post-procedure compression.
The study results further revealed that ablation of venous reflux was achieved in 95% of the cases, or 19 of the 20; ablation to flow was recorded at 65%; no complications were reported; and venous clinical severity score (VCSS) improved from 6.9 pre-procedure to 1.1 at three months. Gasparis said the next step is for the HIFU technology to be evaluated in a multicenter trial after FDA approval. “It’s here to stay,” he added.
Meanwhile, separately, Ferdinand Steinbacher, MD, from the Karl Landsteiner Institute for Functional Phlebosurgery in Melk, Austria, delivered the latest data from Europe on the Sonovein S+ and Sonovein HD iterations of the technology
From the end of November 2021 through mid-December 2022, 40 GSVs and anterior accessory saphenous veins were treated, he revealed. Overall efficacy was 88%, Steinbacher said, with the first period of treatment (Nov. 30, 2021, to March 9, 2022) yielding a 71% occlusion rate (12 of 17) when only the Sonovein S+ was used.
During the second period (April 26, 2022, to Dec. 14, 2022), during which both the Sonovein S+ and HD version were utilized, a 100% occlusion rate was achieved among the 23 veins ablated—10 with the S+ and 13 with the HD.—
Bryan Kay
Vascular Specialist | March 2023 8
ONE-YEAR ANALYSIS OF CLOUT REGISTRY REVEALS
DVT
‘SIGNIFICANT AND SUSTAINED’ LONGTERM CLINICAL IMPROVEMENTS
J. AARON BARNES is a vascular surgeon at Alyeska Vascular Surgery, in Anchorage, Alaska.
J. Aaron Barnes
David Dexter
Antonios Gasparis
FASTER
SUSTAINED
for Venous Leg Ulcers
HEALING
Multi-modality Therapy for VLUs

Combining non-contact cyclical compression, supplemental oxygen and humidification, this seamless addition to your care plan can be used in any clinical setting or self-administered by the patient at home over compression dressings, improving compliance and access to care for all.

DELIVERING EXCEPTIONAL OUTCOMES



HIGHER HEALING RATE at 12 weeks LOWER RECURRENCE RATE at 36 months 76% 46% | vs. SOC* 6% 47% | vs. SOC* FASTER TIME TO HEALING MRSA ELIMINATION 57 DAYS 107 DAYS | vs. SOC* 46% 0% | vs. SOC* *Standard of Care (SOC) was Conventional Compression Dressings (CCD)
REFERENCE: 1. Tawfick WA, Sultan, S. Technical and Clinical Outcome of Topical Wound Oxygen in Comparison to Conventional Compression Dressings in the Management of Refractory Nonhealing Venous Ulcers. Vascular and Endovascular Surgery, 2012. Visit www.AOTInc.net for more information MB1083-A
VENOUS REFLUX
BIOPROSTHETIC VENOUS VALVE: ‘WE WANT TO KNOW THAT THIS IS REALLY WORKING’
A key investigator in efforts to tackle chronic venous insufficiency (CVI) with an bioprosthetic venous valve replacement talks about progress being made with surgical and endovascular versions of the device—and surgical community skepticism.
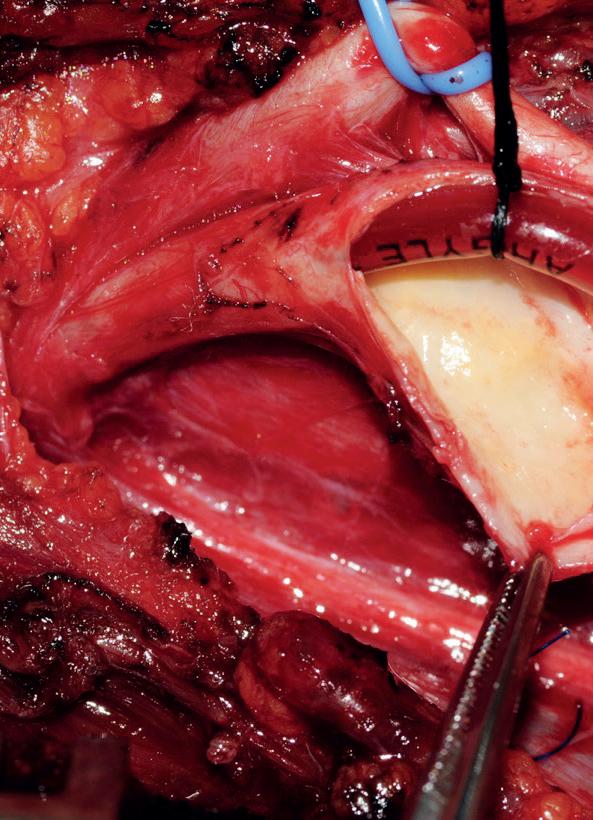
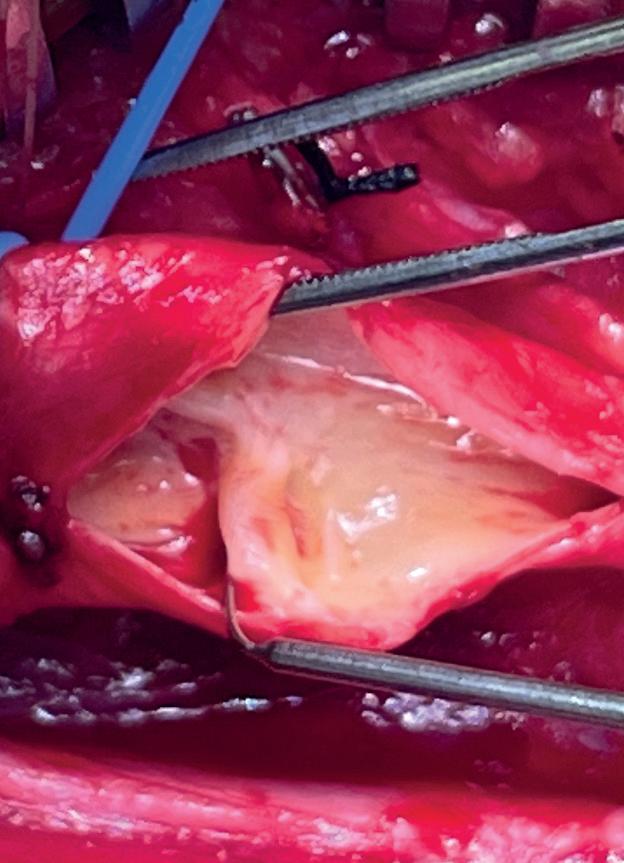
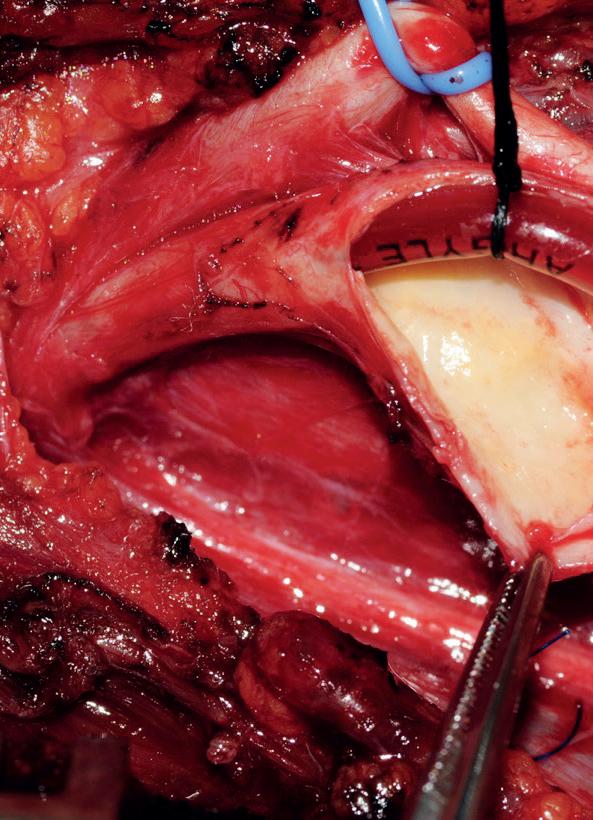
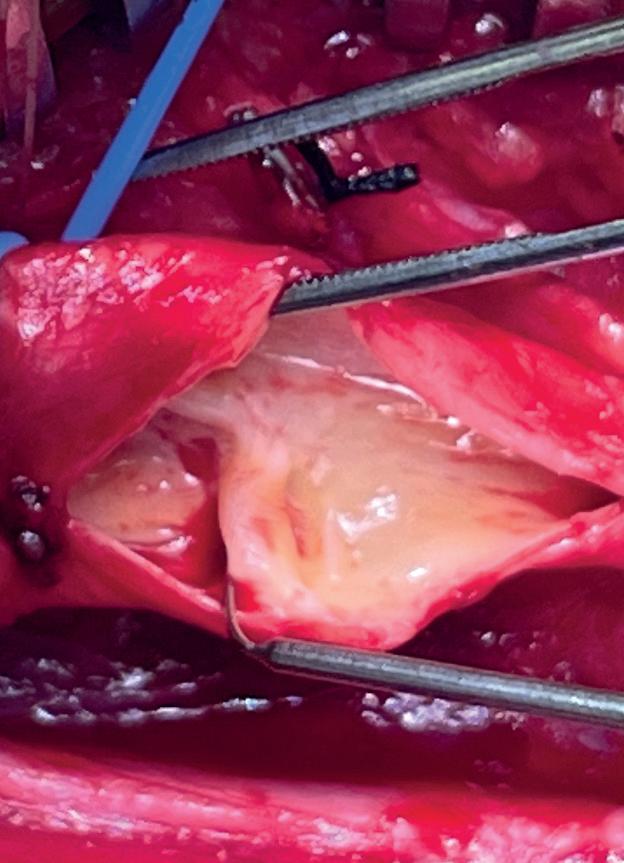
JORGE ULLOA, MD, HAS NOT LONG since produced the latest data from a firstin-human (FIH) trial for emerging stainless-steel frame-based surgical implant, the VenoValve device, intended to treat patients with C5–C6 disease on the CEAP (Clinical-Etiological-Anatomical-Pathophysiological) classification scale.
He is talking on the sidelines of the 2023 annual meeting of the American Venous Forum (AVF) in San Antonio, Texas (Feb. 22–25), where he has just presented the latest update on what the 36-month data from the FIH is showing.






Those results, he says, for the investigational device continue to be promising, but the U.S. pivotal trial, the SAVVE study, or Surgical anti-reflux venous valve endoprosthesis, is also approaching a crucial tipping point, he tells Vascular Specialist. “We’re getting into 40-plus patients, more than half of what is required by the Food and Drug Administration [FDA],” he explains. “We’re at 24 sites. The goal is to end up with 75 cases. That data needs to be analyzed in order to know that the experience we had with the small number [of FIH patients] we got in Colombia, which was 13 at the beginning and now eight under the last cut of the follow-up, is replicated. That is the position we are in right now.”
Attention is turning, too, to the early
By Bryan Kay
stages of a catheter-delivered version of the valve, Ulloa says. The Fundacion Santa Fe-Universidad de los Andes, Bogota, Colombia, vascular surgeon has, of course, been at the vanguard of the early research efforts around the surgical valve replacement. He will play a similar role as the FIH trial of the endovascularly delivered bioprosthetic gets underway, also in Colombia.
“This endovascular approach, which is a miniaturization of the valve—the same one that we placed and have been placing in Colombia and the U.S.—in order to accommodate it in a catheter and allow it to be placed, involves a different process in that it goes under nitinol, the material of stents. It will go into a catheter and then be delivered via the popliteal vein, and then deployed at the femoral vein level, in the very same way that we are doing so far with the open and surgical approach.
“The advantages of this are that, of course, delivery is an endovascular process— the morbidity of the surgical approach goes almost toward zero—we don’t make inci sions, we don’t do dissections, we don’t have to deal much with bleeding.”
If all goes to plan, the TAVVE (Transcatheter anti-reflux, venous valve endoprosthesis)
FIH trial will commence within
a couple months, potentially with up to 20, Ulloa adds.
Yet, he is aware of skepticism over results recorded thus far among some within the vascular surgical community. “There have been a series of attempts for the last 60 years or so, with the first report of a prosthetic valve going back to the 1960s,” he says. “The first implantation in the human body was sometime around the late 1980s, early 1990s. The number of cases was very low, and the follow-up was very short and not very promising. Therefore, I understand, we all understand, that there is going to be a whole field of skeptical surgeons.”
Rather, Ulloa argues the medical landscape is more conducive to success now. “Materials are way better than they were 20, 30, 40 years ago,” he continues. “The surgical approaches are better now. We understand physiology way better. We can assess the behavior of a valve right after and during the surgery, and right after the surgery we can check it and can see it; we can measure it, we can get a lot of physiological data out of each and every one of the patients or cases. Also, the numbers we got are a little higher than the historical average, and the follow-up we got [in the FIH VenoValve trial] is the longest we’ve got in history—the longest we had before was six months.”
The valve, Ulloa says, is not going to be perfect, nor cure the underlying problem—“but it will manage the problem, and will improve the quality of life, and the data is supporting all those ideas.” He points to decreased reflux, reduced pain and healed ulcers. “Of course, we have to continue the follow-up to see what is going to happen, and continue to add numbers.”
There might be no more skeptical a group than those investigating the device themselves, Ulloa says. “We want to know that
THREE-YEAR FIRSTIN-HUMAN RESULTS


During the AVF 2023 Ulloa provided attendees with updated data on improvements in venous reflux of 63%, revised venous clinical severity score (rVCSS) of 64%, and visual analog scale (VAS) of 83% compared to presurgery levels.

The VenoValve device has been developed to be surgically implanted in the femoral vein of patients with C5–C6 disease.




Ulloa, principal investigator of the first-in-human trial, said the findings demonstrated the VenoValve “appears to be safe with continued significant benefit.”
The two-year findings, presented at the 2021 Vascular Annual Meeting (VAM) in San Diego, showed 63% improvement in venous reflux time, 60% improvement in VCSS score, and a 93% improvement in recorded pain, or VAS, when compared with preoperative levels.
At AVF 2023 in San Antonio, Ulloa said the remaining eight patients showed “continued and stable improvement” for three years, with no ipsilateral ulcer recurrence. “It appears that long-term anticoagulation may be necessary,” he added.
this really working, we want to see how it is working, we want to assess each and every measurement that we can, and that’s what we have been doing so far with it. Yes, prob ably we are approaching the end of the road, and we are getting into the field of a lifelong problem that has been facing vascular sur geons—really difficult to manage—which is the post-phlebitic syndrome. For the first time, it has real possibility of treatment that will, at least for three years, see a dramatic improvement in symptoms and dramatic increase in quality of life.”
An analysis of venous usage trends in the United States from 2014 through 2021 showed a “significant increase” in stents per day placed over time, despite high-profile recalls of two dedicated venous stents from the market.



Those were among the observations of Karem Harth, MD, associate professor of surgery and director of the Center for Comprehensive Venous Care at University Hospitals in Cleveland, Ohio, who led the study, which looked at the total eight-year period and three distinct timeframes within it: before Food and Drug Administration (FDA) approval of dedicated venous stents, from FDA approval through to the date of the first recall, and the period after the recall. Harth delivered the results at 2023 annual meeting of the American Venous Forum (AVF) held in San Antonio, Texas (Feb. 22–25).
In an interview with Vascular Specialist afterward, she said the increase in usage was not surprising but did highlight a number of areas in need of evaluation. “We found that there was a significant increase in stenting since FDA approval, which is not surprising because this therapy is exciting and
long-awaited,” she explained. “But what we also found was that the top three diagnoses included acute DVT, NIVLs or non-thrombotic iliac vein lesions, as well as mild chronic venous insufficiency [CVI], which came as a surprise to us when we looked at this data, and that trend remained over time.” Analyzing venous stent usage rates both overall and across the three time periods by demographics, indications for stenting and overall mortality, significant differences were identified in gender, race and overall mortality (p<0.05), Harth said. The top four indications for venous stenting were acute deep vein thrombosis (DVT), chronic DVT, NIVL and CVI with no inflammation.
In addition to the increase in stent usage overall (p<0.00001), on multivariate regression analysis Harth and colleagues recorded an increase from the period prior to FDA venous stent approval to the period between that afterward until the first stent recall among more white and female patients (p<0.005), and both acute and chronic DVT patients
(p<0.01). Meanwhile, in the same timeframe trend showed decreased usage in patients with NIVLs, CVI with no inflammation, and CVI with inflammation. From the second time period (FDA approval–first recall) to the third (after the recall), no changes occurred across indications for stenting (p>0.05), Harth told AVF 2023. Risk factors in the first and second periods for overall mortality at more than two years post-stenting included age, male sex and chronic DVT, NIVL, and CVI with ulceration, while African-American race was a risk factor in the period prior to venous stent approval, she added.
Harth concluded her podium presentation by stating that “significant increases in venous stenting occurred after U.S. FDA approval and remained unchanged after FDA recall.” Indications are broad and “may not all be appropriate use of venous stenting,” she said, highlighting the need for further work to understand the venous stent landscape, usage and to minimize unnecessary stenting.—Bryan Kay

Vascular Specialist | March 2023 10
FDA
Jorge Ulloa
Venous stent usage: ‘We need to evaluate use, appropriateness, clinical indication and alignment with criteria’
Karem Harth















































Modifying Beveled Tip 1 Continuous Active Aspiration 3 Rotating Abrading Vortex 2 Refining Atherectomy Please consult package insert for more detailed safety information and instructions for use. BD, the BD logo, and Rotarex are trademarks of Becton, Dickinson and Company or its a liates. © 2023 BD. All Rights Reserved. © 2023 Illustrations by Mike Austin. BD-19798 bd.com BD, Tempe, AZ, USA, 1 800 321 4254
VESS 2023
pMAC score found to be ‘important predictor’ of CLTI revascularization outcomes
By Eva Malpass
HAVING OBSERVED A STRONG RELATIONSHIP between calcification and subsequent limb loss, a research team led by investigators from the University of California San Francisco (UCSF) have conducted a single-center, retrospective follow-up extending an initial study evaluating pedal medial arterial calcification (pMAC) score and major amputation in patients with chronic limb-threatening ischemia (CLTI).
Presented at the 2023 winter annual meeting of the Vascular and Endovascular Surgery Society (VESS) in Whistler, British Columbia, by Shant Vartanian, MD, senior corresponding author and associate professor of vascular surgery at UCSF. Michael S. Conte, MD, professor and chair in the division of vascular and endovascular surgery at UCSF, was also a senior author in this research. Speaking to Vascular Specialist, both Conte and Vartanian discussed the team’s findings.
The data suggest pMAC could become a “robust” marker for hemodynamic response to revascularization and risk of limb loss, and have the potential to better inform healthcare professionals on the most suitable treatment pathway, Conte said.
In their initial study, Vartanian and colleagues found that by measuring the extent of calcium buildup in the foot arteries, a higher incidence of limb-loss risk was noted. However, as Conte admitted, the calcification pattern is not something vascular specialists routinely consider when planning an intervention. This is unless the patient is diabetic or has kidney disease, which vascular surgeons are seeing “more and more,” he said—noting an increasing number of patients are presenting with “distal” and “challenging-to-treat” disease, extending beyond the calf and into the ankle and foot.
Adding to this, Vartanian recalls their initial intention was to study wound healing in correlation with disease severity, but difficulties investigating this retrospectively steered the
investigators to focus on a “clean endpoint”—that being the relative contribution of below-ankle disease and outcomes in CLTI after revascularization.
When conducting a subsequent retrospective review, the team included 306 patients who had a technically successful index infrainguinal revascularization for CLTI between January 2011 and December 2020. They defined technical success as restoration of in-line flow through the target artery pathway into the foot. Furthermore, pMAC scores were blindly calculated by a single reviewer using two-view minimum plain foot radiographs and were subsequently classified using the Society for Vascular Surgery (SVS) WIfI staging system.
The revascularization approach was open bypass in 118 (38%) and endovascular in 188 (62%) patients, their results showed. The pMAC scores were trichotomized (0–1 [125; 41%], 2–4 [116; 38%], 5 [65; 21%]).
In the bypass subgroup, the researchers state WIfI ischemia grade was improved in 35 of 46 (76%) patients—a total of 19 of 118 (16%) receiving major amputation—although data were not associated with pMAC scores. In the endovascular subgroup, WIfI ischemia grade was improved in 43 of 90 (48%), however 37 of 188 (20%) underwent major amputation.
Drawing conclusions from these results, Conte and researchers directed attention to the “selective differences” in the impact of pedal arterial calcification on revascularization outcomes in CLTI. Although pMAC score was “strongly and independently” associated with failure to improve WIfI ischemia grade after infrainguinal angioplasty or stent, the authors identified no factors associated with this outcome in those who underwent bypass.
“[Our results] at very least can help healthcare profession-

als discuss the odds of success with their patients, and rethink how aggressively to push for revascularization, or certainly have in mind that a standard revascularization may not work for a patient with a high pMAC score,” Conte explained. In concurrence, Vartanian noted that it is essential the implications of revascularization be studied prospectively and ultimately be “factored in upfront decision-making” for the management of CLTI and that measuring pMAC scores is a “simple and efficient” way of quantifying the burden of calcification.
Importantly, Conte noted that although the WIfI stage captures the clinical spectrum of CLTI, the pMAC score can describe the underlying pathology and provides useful information that may serve as an “important predictor of revascularization outcomes.” Having been involved in the inception of the WIfI staging system, Conte believes the addition of pMAC scoring would be a “step forward” in stratifying patients with limb-threatening ischemia, delineating who is high risk.
When reflecting on the audience’s reception of their presentation at VESS 2023, Vartanian conceded that “cynicism is healthy”—particularly when confronted with a novel concept, noting: “There’s not a robust body of evidence to support [pMAC scoring] just yet. I think it’s natural to ask difficult questions, and as cases of below-ankle disease increase, healthcare professionals should be having honest conversations with patients, assessing potential risks.” Distilling his thoughts, Vartanian continued, “I believe the take-home message is to reassess adequacy of perfusion, and focus on vigilance short-term, then observation and reintervention sooner rather than later, if a case is not developing on a desirable clinical trajectory.”
Reflecting on the broader relevance of the team’s findings, Conte noted: “Measuring pMAC scores for all comers that are referred for possible limb salvage—rather than looking backwards after receiving a revascularization—could improve assessments and aid in defining treatment strategies for patients with CLTI.” Looking ahead, Conte and Vartanian were clear that further validation is needed from other centers and larger datasets to define the role of pMAC scoring in producing differences in revascularization efficacy and limb salvage in patients with low vs. high burden of pedal calcification. Contemporary research on this topic is on an “exponential curve” upwards. “I think we are going to see an explosion of papers on the subject in the next few years,” Vartanian added, citing chats at VESS with researchers also plowing this trail.
A NEW MEMOIR PENNED BY FORMER Society for Vascular Surgery (SVS) President and vascular surgery leader Frank J. Veith, MD, which touches on a lifetime of service to the specialty and tackles some of its most monumental and controversial moments, was recently published.
The Medical Jungle: A Pioneering Surgeon’s

Battle to Revolutionize Vascular Care and Challenge the Medical Mafia covers the breadth of Veith’s career as a vascular surgeon, from his early steps in the military as a member of the U.S. Army Medical Corps, through innovative work in lung transplantation and, crucially, limb salvage, during his time at Montefiore Medical Center, in the Bronx of New York City.
Veith, in whose name the maiden Frank J. Veith Lecture will take place at the Vascular Annual Meeting (VAM) in June, also recounts his role at the heart of U.S. vascular surgery’s endovascular revolution more than two decades ago. He writes about how this coalesced, in the early 1990s, around his
participation in the first endovascular aortic aneurysm repair (EVAR) in the country alongside technique trailblazer, the Argentinian vascular surgeon, Juan C. Parodi, MD.

The Medical Jungle also sketches out vascular surgery’s evolution as a separate surgical specialty, from its early roots in cardiac surgery through its status today as a comprehensive provider of care throughout the vascular tree outside of the heart and brain.
Finally, Veith charts the development of the world-renowned VEITHsymposium, an annual
global gathering in New York City of vascular specialists that Veith started half a century ago. In the book, he also outlines his philosophy on mentorship and the training of future vascular surgeons.
Additionally, The Medical Jungle also contains an appendix bearing reprints of his presidential addresses as leader of both the SVS (1996) and the Eastern Vascular Society (1994), as well his turn delivering the John Homans Lecture, which took place at VAM in 2016.—Bryan Kay

Vascular Specialist | March 2023 12
NEW BOOK PENNED BY VASCULAR ICON CHARTS CAREER IN SURGERY, REVOLUTIONARY SPIRIT
“I think it’s natural to ask difficult questions and as cases of below-ankle disease increase, healthcare professionals should be having honest conversations with patients, assessing potential risks”
SHANT VARTANIAN
Shant Vartanian (top) and Michael S. Conte
Frank J. Veith
SALVAGE
LIMB
VASCULAR PRACTICE
‘TIME MATTERS’: NEW STUDY FINDS NOVEL EHR WORKFLOW IMPROVES TIMELINESS IN VASCULAR CARE
A NOVEL, ORDER-INITIATED workflow facilitated by the electronic health record (EHR) has been shown to improve timeliness of care for vascular surgery patients, decreasing time to operation and working to standardize and automate the consultation process.
Presented at the 2023 winter annual meeting of the Vascular and Endovascular Surgery Society (VESS) in Whistler, British Columbia (Feb. 23–26), by University of Colorado general surgery resident John Iguidbashian, MD, senior author Jeniann Yi, MD, spoke to Vascular Specialist about why streamlining consultation operations is paramount for the “acute and urgent” cases vascular healthcare professionals often handle.

Implemented at a single institution, the team’s order-initiated workflow automated notifications to providers of consult requests, communication of patient data, patient additions to consultants’ lists, and tracked consult completion. The investiga-
CAROTID DISEASE
tors subsequently compared consultation timelines pre- and post-implementation.
When prompted on their reasoning in evaluating this process, Yi, an assistant professor of surgery at the University of Colorado in Aurora, Colorado, fleshed out the prevalent “issues” they had been encountering with the system, stating that “there was no clear understanding” in the process. She noted a criticism they had encountered which suggested that the system may remove the human element of providing patient information. However, Yi countered this by affirming that, particularly in critically ill patients, if the complete order was initiated and the workflow subsequently expedited, then healthcare professionals are able to trigger those essential, in-person conversations faster. “It removes a lot of steps and mindless work from of the process,” Yi said.
The authors evaluated 278 inpatient and emergency department vascular surgery consultations (158 pre-implementation, 120
post-implementation); 41 and 38 consults required surgery pre- and post-implementation, respectively. Among their results, viewable consult notes were available 31.77 minutes earlier than pre-implementation, while attending attestations outlining final treatment plans were added 205.65 minutes sooner post-implementation.
Yi asserts that by using their novel workflow they were able to more easily track recommendations so that actions could be initiated for patient recommendations sooner, and potentially expedite them to lower levels.
Although their results show positive
evidence to support the EHR as a tool, practitioners expressed “mixed feelings” toward it, Yi explained. When asked about the audiences’ reception of their presentation at VESS, however, Yi stated that discussions centered around how the existing process can be “adapted” to solve “conflicts within existing workflows” as to not pile on additional “[burdensome]” admin.
Emphasizing an area in which their research proves essential, Yi observed that the vascular subspecialty—which frequently includes acute care surgery—is a key area where streamlined workflow processes would benefit most: “Time matters, especially in human intervention—the sooner they receive treatment, the better their outcomes are. To save time is the goal and at the heart of it, it’s about being able to provide prompt treatment for these patients in need of urgent care.”—Eva Malpass
No difference found in TCAR outcomes between academic and community hospitals
New study found no difference in perioperative outcomes and incidence of adverse events at follow-up after transcarotid artery revascularization (TCAR) between academic and non-teaching community institutions. Presented at the 2023 winter annual meeting of the Vascular and Endovascular Surgery Society (VESS) in Whistler, British Columbia (Feb. 23–26), lead authors Samuel Leonard, MD, and Shihuan K. Wang, MD, of UTHealth in Houston, Texas, spoke to Vascular Specialist and situated their research within contemporary vascular practice.
Outlining their two-pronged research aim, Leonard began by elucidating their initial objectives, noting that they wanted to compare patient cohorts between community versus academic hospitals, as well as outcomes in patients who underwent TCAR at these institutions.
Building on this, Wang explained the relatively recent and “[quick]” adoption of TCAR—after the Food and Drug Administration’s (FDA) approval of reverse flow carotid stenting in 2015—which has influenced an “exponential” rise in the volume of TCAR procedures being carried out, he asserted. Due to wider availability, Wang continues, TCAR is no longer limited to academic institutions but is being performed in smaller hospitals, setting the stage for the investigation the authors conducted.
The researchers carried out a retrospective review of prospectively maintained system-wide databases from
UTHealth, Houston, and IU Health, Indianapolis, Indiana, evaluating TCAR procedures performed between 2015–2022.
Patients were stratified based on the setting of surgical intervention, such as academic with trainees or non-teaching community hospital with only staff surgeons. Relevant demographics, medical conditions, anatomical characteristics, intra- and post-operative courses, and adverse events were captured for statistical analysis.
Identifying 729 patients who underwent TCAR, the authors found no significant difference in perioperative stroke at 30-day follow-up, however, they did note disparities in performance metrics between institutions. Procedures carried out at academic hospitals took longer, although Leonard points out that this may be attributable to the complexity level of the cases they receive.
Nonetheless, the “comparable” results for TCAR, regardless of care location, show that you do not necessarily need the “big box of resources” to have desirable outcomes, as Wang phrased it.
“We’re not saying everyone should be getting [TCAR], we certainly don’t have the data for that”—both authors agreed that advocation is not their intent—”the gold standard continues to be carotid endarterectomy (CEA),” Wang clarified.
Additionally, when recalling the questions put to the authors at VESS 2023, Leonard posited that their advocacy for TCAR was tangibly “on the audience’s mind,” reiterating that
the investigators continue to abide by the Society for Vascular Surgery (SVS) guidelines, which continue to recommend CEA for carotid disease.
Quashing any hint of upheaval, the absence of any industry supported trial or study evaluating TCAR data which shows clinical equipoise between TCAR and CEA, meant there “wasn’t too much uproar from the audience,” Leonard explained.
On a sobering note, Wang added: “It’s a new technology, there is limited evidence, and the pendulum is swinging toward TCAR a little too aggressively right now and I do worry about that.” Making clear that CEA still takes precedence, TCAR, he stated, will remain an “alternative” until clinical trials shed more light on its efficacy.
As Wang continued, he stated their results emphasize a broadening of resources, “opening up options” for patients, noting that particularly for elderly or very unwell patients, navigating a large academic hospital may not be feasible, and attending a smaller, local institution may be advantageous. “A lot of these patients prefer, if possible, to get procedures done at a smaller place that’s just as good, and then drive, two, three blocks away to the Big Mega Mart—this data reassures patients a little bit,” he said.
Echoing Wang’s sentiment, Leonard concluded by expressing their continued efforts to build the database to extract “other salient points” in the future.—Eva Malpass
www.vascularspecialistonline.com 13
“Time matters, especially in human intervention—the sooner they receive treatment, the better their outcomes are”
JENIANN YI
John Iguidbashian
ACC 2023: Large bore mechanical thrombectomy reduces adverse outcomes in high-risk PE patients
LARGE BORE MECHANICAL thrombectomy with the FlowTriever system in patients with high-risk pulmonary embolism (PE) was associated with a significantly lower occurrence of meaningful in-hospital adverse clinical outcomes compared to other contemporary treatments, data presented at the American College of Cardiology (ACC) 2023 Scientific Sessions (March 4–6) in New Orleans indicate.
These were among the results of the FLAME study, a prospective, non-randomised study of interventional treatment in high-risk PE, a patient population with a historical mortality rate of 25-50%, which were presented at ACC 2023 by Mitchell Silver, MD, from OhioHealth Heart and Vascular in Mansfield, Ohio.
The study collected data on patients treated with the FlowTriever and on those treated with other therapies in a context arm. The primary endpoint measured a composite of meaningful in-hospital clinical outcomes, including mortality, major bleeding, clinical deterioration, and escalation to an alternate therapy.
Silver reported that FLAME was stopped early after meeting the pre-specified interim analysis criterion at 50 FlowTriever
AVF 2023: REGISTRY SUGGESTS ‘FAVORABLE SAFETY AND EFFECTIVENESS PROFILE’ IN HIGH-RISK PE PATIENTS
patients. Sharing the results of the study, Silver noted that the endpoint was met in the FlowTriever arm, in which a mortality rate of 1.9% was recorded, compared to 29.5% in the context arm. In all, the composite primary endpoint occurred in 17% of patients in the FlowTriever arm, compared to 63.9% in the context arm.
“The remarkably low mortality seen with FlowTriever demonstrates the benefit of rapidly identifying PE patients and getting them to an interventionalist for assessment,” Silver was quoted as saying in a press release issued during ACC 2023. “It is time for our hospital systems to develop standardized care pathways for PE, similar to what has been done in other major cardiovascular diseases such as heart attack and stroke.”
“High-risk PE persists as one of the deadliest cardiovascular diseases,” said James Horowitz, MD, from NYU Grossman School of Medicine in New York City, FLAME national principal investigator.
“Outcomes have remained unchanged for decades. The FLAME data shows that [the] FlowTriever is an important new treatment option that offers a dramatic improvement in survival.”—Will Date
AMONG 61 HIGH-RISK PULMONARY embolism (PE) patients followed through the 30-day visit in the U.S. cohort of the FLASH registry, no mortalities were recorded, while at 48 hours post-treatment with the FlowTriever mechanical embolectomy system, likewise, there were no major adverse events (MAEs), nor serious adverse events (SAEs) reported.
The outcomes emerged during a venous thromboembolism (VTE) session at the 2023 annual meeting of the American Venous Forum held in San Antonio, Texas (Feb. 22–25) in a paper delivered by James Horowitz, MD, from NYU Grossman School of Medicine in New York City.

The sub-analysis was drawn from the 800-patient prospective, multicenter, real-world registry in light of a paucity of data regarding the use of the percutaneous system among high-risk patients, Horowitz noted.

Horowitz reported that, post-embolectomy using the FlowTriever system, hemodynamic improvements were observed, with mean pulmonary artery pressure decreasing from 31.5mmHg to 24.3mmHg, and cardiac index (CI) increasing from 1.5L/min/m2 to 1.9L/min/m2. “Patients demonstrated immediate hemodynamic and vital-sign improvements following the procedure,” he added. “Echocardiographic, dyspnea and quality-of-life outcomes improved through 30 days.”
Horowitz and colleagues highlighted that the large-bore mechanical embolectomy system “has a favorable safety and effectiveness profile” in the high-risk group. They concluded: “In high-risk PE patients, there were no mortalities through 30 days or MAEs after mechanical embolectomy with the FlowTriever system. High-risk patients demonstrated significant improvement of acute hemodynamics and functional outcomes. Results from the FLASH registry suggest mechanical embolectomy is safe and effective for high-risk PE, leading to markedly lower acute mortality compared to previously reported mortality rates for this population.”—Bryan Kay
Vascular Specialist | March 2023 14
FLASH
FLAME
SVS LAUNCHES WEBBASED PERIOPERATIVE CARE GUIDE
By Beth Bales
The Society for Vascular Surgery (SVS) has launched its “Management Guide on the Perioperative Care of Patients with Vascular Disease,” a multidisciplinary resource for care of patients with vascular disease who require an intervention.
The American Society of Anesthesiologists, the Society for Vascular Medicine and the Society for Vascular Nursing all helped develop the guide, supported through an unrestricted educational grant from Janssen Pharmaceuticals, Inc.
The resource provides information on the medical and non-medical management of vascular patients in the perioperative period: 1) 30 to 90 days before intervention, 2) during the intervention, and 3) 30 to 90 days post-intervention.

With mobile-responsive design and easy, intuitive navigation, it is ideal for on-the-go use by busy members of the entire vascular team, from trainees, to surgeons, anesthesiologists, internists, vascular nurses and allied health members.
It covers the procedures and conditions that encompass the most common vascular disorders. Each section outlines factors for each stage. Pre-operative care for abdominal non-aortic pathology, for example, lists such factors as patient history, including specific elements to assess for certain conditions; physical examination; imaging; medical management and lifestyle changes; risk stratification and risk assessment; preoperative lab tests recommended; and medication adjustments to make prior to intervention.
The guide then provides similarly detailed information and recommended steps for the intraoperative and postoperative phases.
To develop the guide, the SVS brought together experts who represent key members of the perioperative team, including vascular surgeons, anesthesiologists, vascular medicine specialists, vascular nurses and
ADVOCACY
SVS MEMBER DAVID HAN, MD, HAS BEEN re-elected to the American Medical Association (AMA) Relative Values Scale (RVS) Update Committee (RUC). Han’s two-year term runs from March 2023 and ends in February 2025.
physician assistants. “We don’t intend that this new guide replace any of the documents and protocols or local practices,” said Rabih Chaer. MD, chair of the authoring group. Instead, as stated in the guide’s introduction, “It provides guidance that can be used by individual institutions to build their own perioperative management protocols and design educational programming, and complements the Enhanced Recovery After Surgery (ERAS) guidelines that the SVS is developing. The document will help facilities address comorbidities and other risk factors that can affect postoperative outcomes and reduce the use of redundant and/or unnecessary tests.”
Government Grand Rounds: Culture of engagement
By Andrew Kenney
WELCOME
BACK TO GOVERNMENT GRAND ROUNDS,
Rabih Chaer
where the Society for Vascular Surgery Advocacy Council discusses how sustained advocacy engagement is important for all SVS members.
It’s more of a complete 360-degree view of the care of patients who need a vascular intervention, involving all aspects and all team members involved in that care, he said. “The procedure is important, of course,” he said. “But all aspects of perioperative care—from medication compliance to follow-up care—are critical to ensure successful outcomes. This is one of our first official resources that articulates the entire patient experience.”
View the guide, which also includes conclusions, the definitions of approximately 125 terms from abdominal aortic aneurysm to Vitamin-K antagonist, and more than 160 references, at vascular. org/PMG. Users can also download the guide at the site.
While “advocacy” continues to rank high among SVS member priorities, many remain unsure how to support SVS advocacy-related programs, what activities are available and how to measure success along the way. This series aims to answer those questions through the many useful tools of advocacy. Last month, the Council shared the importance of perspective and examined how advocacy can be used as a tool to protect. But how do we use that tool and what are the driving factors behind that tool’s effectiveness? One of the key drivers of success in advocacy is engagement.
Many have probably heard of the term “grassroots” before, but what exactly does that mean in the context of advocacy? Grassroots is often defined as “the basic level of society or of an organization” or something that is “basic, fundamental.” In advocacy, we use this term to describe the efforts that every-day citizens go through to help shape the government, often through sending letters to Congress, protesting in public spaces or organizing their own awareness campaign. These efforts are the bread and butter of what it means to advocate.
The SVS engages in grassroots activities through a few programs, designed to connect SVS members with their lawmakers to create tangible channels for vascular surgeons to personally advocate on issues that significantly impact the specialty. The REACH 535 program establishes a concrete mechanism for the SVS to amplify its advocacy efforts by ensuring we can quickly engage with the 535 decision-makers on Capitol Hill. This engagement with lawmakers is what drives change. (Visit vascular.org/REACH535form to sign up for REACH 535.) To create a strong foundation for grassroots advocacy, the SVS needs to establish a culture of engagement. This culture looks like taking the opportunity to engage with lawmakers via Voter Voice, signing up for REACH 535, and donating to the SVS PAC. When we work together to strengthen our collective voice, we simultaneously expand our impact on Capitol Hill.
These facets of engagement, when done together, help to amplify the entirety of the effort. One letter sent may not change the course of a bill, but organized, collective action from thousands of vascular surgeons could permanently alter the trajectory of a proposed policy or pending piece of legislation. For more information on how to engage with the SVS’ Advocacy programs, visit vascular.org/advocacy or contact svsadvocacy@vascularsociety.org
ANDREW KENNEY is SVS advocacy coordinator.
Medicaid Services (CMS). CMS considers input from the RUC Relative Value Units (RVUs) when making payment decisions.

Han will serve on the committee as one of a handful of members from surgical subspecialities; most seats are held permanently by major national medical specialty societies. The committee provides input to CMS.
RUC. He was named in late 2020 as the AMA alternative representative to the RUC and alternative vice chair. His three-year term began in March 2021.
This is the third time Han will serve in that capacity. He currently is vice chair of the Society for Vascular Surgery (SVS) Coding Committee and will continue as the vice chair of the AMA RUC Practice Expense Subcommittee.
The RUC is the multispecialty committee that makes relative value recommendations for new, revised and potentially misvalued services to the Centers for Medicare &
“Many other specialty societies have permanent seats on the committee. We, as a small subspecialty, do not; instead, our members can be elected on a rotating basis with other small subspecialties,” said Matthew Sideman, MD, chair of the SVS Advocacy Council.
Sideman said Han supports the SVS’ mission of advocacy and payment reform. He is professor of surgery and chief of the division of vascular surgery at SSM Health St. Louis University in St. Louis, Missouri.

Fellow SVS member, and longtime SVS coding expert, Robert Zwolak, MD, serves in a leadership role on the
“Dr. Han will be and has been a valuable asset to the RUC Committee,” said SVS President Michael C. Dalsing, MD. “He understands the complexity, processes, and nuances involved in coding and all the other elements that go into reimbursement rates, which are an integral part of the medical world we live and practice in.”
“I am grateful for working with such a talented team of individuals who work tirelessly on behalf of our specialty to ensure that vascular surgeons are fairly valued for the work we do,” said Han.
“I truly stand on the shoulders of giants with regards to the team as well as those who have come before me. I hope that I can play a similar role in helping the next generation continue to advocate for the highest quality and most sustainable and equitable care.”—Beth Bales
www.vascularspecialistonline.com 15
SVS MEMBER ELECTED TO RUC COMMITTEE AMA
YOUR SVS
The site for the new guide
I’M AMAZED BY THE HIGH-QUALITY MODERATORS AND DISCUSSION. THE DEBATES WERE EDUCATIONAL AND FRANKLY A LOT OF FUN TO WATCH.

CX IS THE BEST OPPORTUNITY TO NETWORK WITH FRIENDS FROM THE INTERNATIONAL VASCULAR COMMUNITY FROM ALL CORNERS OF THE GLOBE.


EXCELLENT MEETING COVERING THE MOST UP-TO-DATE INFORMATION ON THE IMPORTANT ASPECTS OF VASCULAR SURGERY.


INNOVATION EDUCATION EVIDENCE CONTROVERSIES CHALLENGES CONSENSUS OF LOOKING FORWARD CXSYMPOSIUM.COM Consensus Update Vascular & Endovascular 25–27 APRIL 2023 TUESDAY-THURSDAY IN PERSON AND VIRTUAL REGISTER NOW HILTON LONDON METROPOLE, UNITED KINGDOM Peripheral Arterial Consensus Aortic Consensus Acute Stroke Consensus Vascular Trauma Consensus Venous & Lymphatic Consensus Vascular Access Consensus The Hurting Leg Consensus CX 2022 attendee
CX 2022 attendee
CX 2022 attendee
EARLY-BIRD VAM REGISTRATION OPENS
MEETING REGISTRATION AND
hotel reservations opened March 15 for the Society for Vascular Surgery (SVS) 2023 Vascular Annual Meeting (VAM). This year’s premiere educational event for all vascular professionals will be June 14–17 at the National Resort and Convention Center in National Harbor, Maryland, just outside Washington, D.C.

Early-bird registration pricing will be in effect for the first three weeks of registration, through April 5. Advance pricing is then in effect until June 13, when on-site registration opens. On-site pricing remains in effect through the close of the meeting on Saturday, June 17.
This year, participants must register for the meeting itself before making hotel reservations.
SVS members receive a substantial discount on VAM registration. Non-members can apply for membership by May 1 to receive—subject to SVS Executive Board approval—the member discount. Dues must be paid prior to VAM to receive the member registration rate. The rate discount will be refunded after the meeting. See vascular.org/JOIN for more information. Visit vascular.org/VAM and then click the registration information link for admission specifics.
VAM 2023 encompasses four full days of education, networking and learning, and two days of industry exhibits. Topics range from hard science to the vascular surgery workforce, quality care and improvement, planning for retirement, a discussion of clinical trial results, and much more. Each plenary session also will include a video demonstrating a complex surgical procedure.
This year’s VAM includes some new features. The meeting will include SVS’ first annual social event, SVSConnect@VAM: Building Community, which is set for 7–9 p.m. Wednesday. It’s a family-friendly event to bring not only healthcare professionals but also their families together, said Andres Schanzer, MD, chair of the SVS Program Committee, which oversees much of VAM’s education programming. “We want to celebrate our membership and the diversity of our membership.”
The inaugural Frank J. Veith Distinguished Lecture takes the stage from 9:30–10 a.m. Thursday, tackling the topic of the BEST-CLI (Best endovas cular vs. best surgical
therapy in patients with critical limb ischemia), results of which were announced in November 2022. Veith has long had an interest in peripheral arterial disease (PAD) and, in particular, limb salvage, which will be the focus of this named lectureship announced at the close of VAM 2022. The speaker is still to be announced.
A celebration of diversity will be hosted by the Diversity, Equity and Inclusion Committee and the SVS’ Women’s and Young Surgeons sections, from 6:30–7:30 p.m. Thursday.
Of course, educational sessions will cover a wide range of subjects with a mix of clinical and non-clinical topics. Some programs will focus on embolization and aortic dissection, wound care, trauma, hemodialysis access, optimizing vascular reconstruction in oncology, worst cases, clinical learning and the practice environment.
Others will look at planning for retirement and advocating for vascular surgeons in the federal government. After a successful inaugural year in 2022, each SVS membership section will hold a session of interest to their particular members.
Two sessions, one on deep venous thrombosis and the second on deep venous stenting, will be presented in collaboration with the American Venous Forum (AVF).
“Every year we pride ourselves on offering an expansive variety of topics to match the wide-ranging interests of our diverse membership and their practice settings,” said Schanzer. “Every attendee will be able to take home information he or she can put to use immediately, or that will provide food for thought down the road.”
View the VAM Schedule-at-a-Glance (subject to change) at vascular.org/SAG23 to get a jump-start on planning VAM 2023. All times are Eastern Daylight Time.
SATURDAY SCHEDULE ALTERED
BEFORE MAKING TRAVEL arrangements, attendees at this year’s Society for Vascular Surgery (SVS) Vascular Annual Meeting (VAM) may want to note some changes to the traditional Saturday line-up. They include:
● No early-morning educational breakfast sessions
● Breakfast for all at the day’s first plenary session, beginning at 8 a.m.
● The move of the Poster Championship, featuring the top 10 posters, to 9:30 a.m., before the Roy Greenberg Distinguished Lecture at 10:45 a.m. and VAM’s final plenary session at 11:15 a.m.
● The meeting’s conclusion in the early afternoon after the Annual Business Meeting (ABM)

To permit revelers to fully enjoy every
moment of the Friday Evening SVS Foundation “Great Gatsby” Gala, planners have removed the early-morning breakfast sessions from the day’s programming menu. The sessions that were typically held in the morning on Saturday have been moved to Wednesday at lunchtime, and lunch will be provided.
“The Gala is an important event members look forward to. We don’t want people to sacrifice time with their friends and colleagues to make it to a 6:45 a.m. breakfast session,” said Andres Schanzer, MD, chair of the SVS Program Committee. With individual tickets and most tables sold out, attendees will appreciate the later start to the day, he said.
The Poster Championship typically is a highlight of Saturday afternoon. For 2023, the championship round is moving to the morning, with authors of the top 10 posters, as selected in Friday afternoon’s competition, presenting their work from the podium.
HOT TICKET: ‘GREAT GATSBY GALA’ NEARS SELLOUT STATUS
TICKETS AND TABLES FOR THE annual Society for Vascular Surgery Foundation Gala, to be held at the Vascular Annual Meeting (VAM), were nearing sellout at press time. The gala will begin at 6 p.m. EDT on Friday, June 16.

“As a Society, everyone really loves coming together and raising money for a good cause and having a nice evening where we can all enjoy each other’s company,” said Gala Committee CoChair Leigh Ann O’Banion, MD. “I’m excited for the early enthusiasm demonstrated by the ticket sales, and we hope that everyone brings that same enthusiasm to the gala when it comes time to raise money for the Foundation and support our vascular surgeons in their research efforts and community outreach for all our patients.”
This year was a record-breaker for ticket sales that resulted in the Foundation adding additional tables to meet demand. Individual tickets and regular tables sold out in mid-February. A handful of VIP tables remain. For more information contact Catherine Lampi: clampi@vascularsociety.org
Members who still wish to purchase individual tickets can join the wait list by using
the QR code to visit the site. As befits a gala theme set in the Roaring Twenties, guests will be transported to the era of Prohibition at the Surgeon Speakeasy and enjoy an open bar, hors d’oeuvres, Gatsby-inspired performers, photographers and more. The evening includes a three-course plated dinner with wine service, auctions, a DJ and dancing.

Proceeds will benefit the Foundation and its efforts to fund the future of vascular health through its four pillars of research and innovation; community vascular care and patient education; disease prevention; and diversity, equity and inclusion. Those unable to attend in person can still join in on the fun via the Silent Auction. This virtual auction will open in June, prior to VAM, and will run through the event for anyone with an internet connection who wants to participate. Only gala attendees can bid on Live Auction items.
Both auctions will feature international and domestic trips, along with other packages. To contribute items, contact Lampi. Popular items from past auctions have included sports tickets, weekend or weeklong getaways, and medical memorabilia.
TO PROVIDE POTENTIAL attendees with a sneak peek at some of the education that will be presented at VAM, the SVS has launched virtual representations promoting several of its educational sessions.
The visual summaries—prepared by members of the SVS Young Surgeons Sec-
tion—began in February. Visual abstracts, a graphic depiction of some of the scientific research to be presented, began in early March. Summaries will be posted bi-weekly, and visual abstracts weekly, leading up to VAM 2023.
View the educational session promotions at vascular.org/VisualVAM
17
VAM 2023
“Every year we pride ourselves on offering an expansive variety of topics to match the wide-ranging interests of our diverse membership and their practice settings”
ANDRES SCHANZER
VAM INCOMING: FULL SUITE OF EDUCATION STARTS TO TAKE SHAPE
Andres Schanzer speaking at VAM 2022
SOCIETY BRIEFS
Compiled by Beth Bales and Marlén Gomez
ANAHITA DUA NAMED 2023 PRESIDENTIAL LEADERSHIP SCHOLAR
SOCIETY FOR VASCULAR SURGERY (SVS) MEMBER
Anahita Dua, MD, has been named a Presidential Leadership Scholar for 2023.

She is one of 60 scholars in this eighth annual class. Dua is an associate professor of surgery at Massachusetts General Hospital and Harvard Medical School in Boston.
‘Voices of Vascular’ series celebrates Women’s History Month

THE CONTRIBUTIONS OF THE Society for Vascular Surgery’s women members take center stage this month as part of the SVS Foundation’s “Voices of Vascular” series.
THE SOCIETY FOR VASCULAR SURGERY will debut “SVS Presents” April 12, a monthly webinar series that provides an evening of educational programming for members.
“Presents” is in response to a key finding from the 2021 Educational Needs Assessment and the 2022 SVS Member Survey, which indicated online education opportunities as a top member priority.
During the COVID-19 pandemic, the SVS produced more than 40 webinars in 2020 alone. Through the educational needs assessment, members stated their interest for the SVS to continue to offer online education, but to condense the offerings to once a month.
“‘SVS Presents’ aims to consolidate the offerings to an identifiable time, hopefully decreasing ‘Zoom meeting fatigue,’” said Education Council Chair Linda Harris, MD. “We are also trying to better engage various committees, councils and membership sections to decrease the work and increase the audience for all presentations.”
The first presentation, on April 12, from 7–8 p.m. (CDT), will focus on the trial results released in late 2022 on the BEST-CLI trial. The second, May 3, will introduce the 2023–24 candidates for Society president and treasurer to SVS members prior to the start of voting. Future topics include advocacy, leadership development, quality practice and guidelines.
“SVS Presents” will take place either the first or second Wednesday evening of every month, excluding January and June due to holidays and preparation for the Vascular Annual Meeting (VAM). Some months will have several hours of programming while others will offer just one hour. This year will be a pilot year to measure interest and increase engagement from all SVS member segments. Planners hope to expand programming and encourage committees to utilize this specific day each month for educational content.
In the effort to standardize SVS educational programming, leaders hope to increase opportunities to participate in the activities. Webinars will be the focus at first, with hopes to offer other educational opportunities, such as releasing video content or micro-learning opportunities, or even hosting the Society’s popular TweetChats.
Presidential Leadership Scholars are “making a difference in the world by applying lessons in leadership learned from the presidential experiences of Presidents George W. Bush, Bill Clinton, George H.W. Bush and Lyndon B. Johnson,” according to program leaders.
“I am honored to be a part of this program that teaches leadership skills utilized by our past presidents of Bush, Clinton and Johnson and their administrations to make the world a better place,” said Dua of her honor.
Her project focuses on decreasing amputations rates among Americans through targeted legislative changes “that would optimize the multidisciplinary team approach to limb salvage, making it both standardized and accessible.”
Her intent is to address limb amputation—one of the most detrimental and costly outcomes of diabetes—and its prevalence amongst minority groups.
The scholars will travel to each participating presidential center to learn from former presidents, key officials of their administrations, business and civic leaders, and leading academics. Dua and the other scholars will study and put into practice varying approaches to leadership and exchange ideas to help strengthen their impact.
SVS, VQI sent letters to CMS
The Society for Vascular Surgery (SVS) and the Vascular Quality Initiative (VQI) have sent letters to the Centers for Medicare & Medicaid Services (CMS) regarding changing the National Coverage Determination for percutaneous transluminal angioplasty of the carotid artery concurrent with stenting.
Read the SVS and VQI letters at vascular.org/ StentingResponseCMS
SPOT LIGHT
In memoriam
See vascular.org/Mackeyobit
Pay SVS dues to receive SVS benefits, including VAM discount
With registration for the 2023 Vascular Annual Meeting (VAM) right around the corner, those people who have not paid their SVS 2023 dues have a good incentive to do so quickly. Members receive a discount on not only VAM but also other SVS educational courses. Other benefits include standing to vote in SVS elections (Active and Senior categories only), access to the Journal of Vascular Surgery, the SVSConnect online community, branding tools and more. Pay dues at vascular.org/Invoices
If non-members apply for membership by May 1, they could receive the membership discount for VAM, which is subject to application approval. Dues must be paid prior to the meeting to receive the member rate; the rate difference will be refunded after the meeting.
The “Voices” series is designed to help celebrate the diversity in the vascular surgery specialty. It debuted in February, Black History Month, and will continue throughout the year. In March, “Voices” will highlight profiles of women, their lives, their road to becoming vascular surgeons and their views of the vascular surgery specialty. The March celebration is in collaboration with the SVS’ Women’s Section.
Audra Duncan, MD, section cochair of the SVS Women’s Steering Committee, explained why such efforts matter.

“More than half of our incoming medical students are women. SVS recognizes this trend and is committed
to recruiting and promoting young surgeons to represent the future of surgery, by embracing diversity and equity, including gender equity,” said Duncan. “Several studies support that patients may have better outcomes when they can be taken care of by physicians of similar gender, race or ethnicity, so it is critical that the face of the SVS reflects the diversity of the populations we care for in order to achieve the best outcomes for our patients.”
In addition, Boston Scientific, the campaign’s presenting sponsor, will match all gifts to the SVS Foundation up to $10,000 through March 31.
That means a gift goes two times as far to support Women in Vascular— past, present and future. Donors can double their impact today by visiting give.classy.org/WHM2023
Patient education is an important part of the campaign, and includes information on how vascular disease impacts women differently and how to inform women about the common signs of vascular disease to promote health and change outcomes.
Vascular Specialist | March 2023 18
‘SVS Presents’ provides enhanced learning opportunities
DAVID WHITTAKER, MD, of Potomac, Maryland, has been named chief medical officer of Alio, Inc., a medical technology company. MILA JU, MD, of Allentown, Pennsylvania, has been named director of quality and patient safety for vascular surgery for the division of vascular surgery at Lehigh Valley Heart and Vascular Institute, with locations in and around Bethlehem and Altoona.
WILLIAM MACKEY, MD, 72, died Jan. 31. He was professor of surgery and former chair and surgeon-in-chief at Tufts Medical Center and Tufts University School of Medicine in Boston. Following medical school and general surgery residency, he completed his vascular surgery fellowship at Tufts Medical School, where he remained for his entire career.
Linda Harris
CAGENT VASCULAR HAS ANNOUNCED the results of a comparative subanalysis of the PRELUDE-below-the-knee (BTK) study versus plain balloon angioplasty.
The study was led by Marianne Brodmann, MD, from the Medical University of Graz in Graz, Austria. This subanalysis compared their PRELUDE-BTK subset to a consecutive plain balloon angioplasty group.
The Serranator-treated lesions had an average final residual stenosis of 17.2±8.2% vs. 33.7±15.7% in the plain balloon angioplasty group. This represents a 49% average improvement in final residual stenosis. In chronic total occlusions (CTO), there was a 62% improvement in final residual stenosis compared to the plain balloon angioplasty group.
The average balloon inflation pressure was 5atm in the Serranator group vs. 9atm in the conventional balloon angioplasty group. Additionally, Serranator-treated arteries demonstrated 2.4 times greater calculated flow improvement versus plain balloon angioplasty. These data, analyzed by the same independent core lab, were recently published in the Journal of Endovascular
Therapy. Brodmann stated: “As an early user of serration angioplasty, it was meaningful to quantify through this subanalysis what we have experienced using the Serranator device.
“William Tang [UC Irvine, Irvine, California] developed a novel model, anchored by Poiseuille’s law, from which we were able to derive the volumetric blood flow from lumen gain achieved with the Serranator compared to conventional balloon angioplasty.
“These results suggest an advantage for serration technology that should allow for superior wound healing and patient outcomes, while minimizing the need for stent placement.”
Raman Sharma, MD, from Mount Sinai Medical Center in New York, who was was an early adopter of serration technology, said: “When it comes to BTK interventions, there simply have not been great options for physicians to treat patients, who are often in jeopardy of limb loss.”
Sharma added: “The results from this subanalysis study support what we have seen in our experience; the Serranator provides greater lumen gain and blood flow versus conventional technology.”

RESCUE trial shows reduction in segmental and main pulmonary artery occlusions
ROBERT A. LOOKSTEIN, MD, FROM THE Icahn School of Medicine at Mount Sinai Hospital in New York City, presented the results of a subanalysis of Thrombolex’s National Heart, Lung and Blood Institute (NHLBI)-sponsored RESCUE trial during the late-breaking trial session at the Society for Interventional Radiology (SIR) annual scientific meeting (March 4–9) in Phoenix.
The core laboratory analysis of this investigational device exemption (IDE) trial demonstrated that pharmacomechanical catheter-directed thrombolysis (PMCDT) therapy using the Bashir endovascular catheter from Thrombolex led to a significant reduction in segmental arterial occlusions (71%; p<0.0001), which correlated with the reduction in right ventricular to left ventricular (RV/LV) ratio (p= 0.0026). There was also a significant reduction in main pulmonary artery (PA) occlusions (61%; p<0.0001) but this did not correlate significantly with the reduction in RV/LV ratio. This reduction in occlusions of not only the main PAs but also the segmental arteries explains why the overall reduction in PA obstruction,

as assessed by the refined Modified Miller Index, is greater with the Bashir endovascular catheter than that which has been reported in contemporary thrombectomy or thrombolysis trials for the treatment of acute pulmonary embolism (PE). RESCUE is a prospective, multicenter trial evaluating the Bashir catheter in 109 patients with intermediate-risk acute PE at 18 sites in the U.S. The Bashir catheter was used to deliver 7mg of recombinant tissue plasminogen activator (r-tPA) into each PA over a five-hour infusion period.
“The RESCUE trial demonstrated rapid resolution of obstruction in the main, and especially segmental, arteries, with less than a 1% major bleeding rate. It is imperative that future PE trials assess the reduction in obstruction in more distal PAs since it has been shown that both the degree of residual PA obstruction and reduction in pulmonary vascular volumes, presumably due to reduced PA inflow, are significant predictors of late PE-related mortality.
This novel approach with the Bashir catheter and low-dose tPA represents a major advance in the treatment of acute PE,” added Lookstein.
DATA FROM A NEW PRESPECIFIED analysis of the phase III VOYAGER
PAD clinical trial show that low-dose rivaroxaban plus aspirin resulted in a 33% reduction in acute limb ischemia (ALI) and a 15% reduction in major adverse limb and cardiovascular events, with or without dual antiplatelet therapy (DAPT).
The data were presented at the American College of Cardiology’s 72nd annual scientific session (ACC.23), hosted in New Orleans, Louisiana (March 4–6).
The new findings reinforce the benefits of the Xarelto (rivaroxaban; Janssen Pharmaceutical Companies of Johnson & Johnson) vascular dose (2.5mg twice daily plus aspirin 100mg once daily) over standard of care (aspirin alone), demonstrating consistent benefit at 30 days, 90 days and up to three years following lower-extremity revascularization in patients with peripheral arterial disease (PAD).
“These data demonstrate an evolution
in the medical therapy of patients undergoing lower extremity revascularization for symptomatic [PAD],” said lead study author of the VOYAGER PAD analysis, Marc P. Bonaca , MD, of the University of Colorado Anschutz Medical Campus in Aurora, Colorado. “We hope these data assist clinicians in understanding how to implement antithrombotic therapy in practice and overall support initiation of rivaroxaban in the first days after revascularization, regardless of whether or not DAPT is utilized.”
Those treated with Xarelto plus aspirin after lower-extremity revascularization saw a 33% reduction in acute limb ischemia, with a trend toward greater benefit observed early (≤30 days hazard ratio [HR]=0.45; 95% confidence interval [CI] 0.24–0.85) vs. late (>90 days HR=0.75; 95% CI 0.60–0.95).
Xarelto plus aspirin was more effective than antiplatelet therapy alone in preventing ALI after lower-extremity revascularization (Kaplan-Meier estimate from 0 to 90 days 1.02% vs. 2.10%, respectively, and 4.3% and 5.7% from 91 days to three years). The hazard ratio for the rate of thrombolysis in myocardial infarction (TIMI) major bleeding at 0 to 90 days was HR 2.01 (range 0.9–4.47) and from days 91 up to three years was HR 1.28 (range 0.82–1.99), neither of which were statistically significant.
Janssen Pharmaceutical Companies of Johnson & Johnson noted in a press release announcing the new results that the Xarelto vascular dose is the first and only approved anticoagulant for PAD.
EU ministers approve changes to MDR transition
stenting
DISTAL EMBOLIC PROTECTION USING a filter has been associated with improved transfemoral carotid artery stenting (tfCAS) outcomes in terms of in-hospital stroke and death risks—underpinning current Society for Vascular Surgery (SVS) guidelines, and supporting the notion that, “if a filter cannot be placed safely, an alternative approach to carotid revascularization should be considered”.
Sophie Wang, MD, Patric Liang, MD, both Harvard Medical School in Boston, and colleagues deliver this message in a recent Journal of Vascular Surgery (JVS) publication in which they detailed a retrospective, propensity score-matched cohort analysis of tfCAS patients in the Vascular Quality Initiative (VQI) across a 16-year period.
“Distal embolic protection confers a benefit in stroke/death rates following tfCAS compared to unprotected stenting,” the authors concluded in their “take-home message” in JVS
THE EUROPEAN UNION’S COUNCIL OF Ministers has adopted a resolution to extend the deadline for the certification of medical devices under the Medical Devices Regulation (MDR).
Producers of medical devices will have until Dec. 31, 2027, for higher-risk devices and until Dec. 31, 2028, for medium- and lowerrisk devices in order to meet the legal requirements.
The extension of the transition period will be granted under certain conditions, ensuring that only devices that are safe and for which manufacturers have already started the certification procedure will benefit from the additional time.
The regulation—which changes the way that medical devices are certified for use in the European market—first came into effect in 2021 with an initial three-year transition period, having been delayed by one year in 2020 due to the onset of the COVID-19 pandemic.
However, challenges in the implementation of the legislation led to concerns about a potential shortfall in the availability of certain medical devices, which prompted a rethink in the timetable for the regulation as proposed by the European Commission in December.
www.vascularspecialistonline.com 19 CLINICAL&
NEWS
DEVICE
Compiled by Jocelyn Hudson, Will Date, Clare Tierney and Jamie Bell
Distal embolic protection linked to significantly better outcomes in carotid
PRELUDE-BTK subanalysis highlights superior lumen gain, greater volumetric blood flow using serration angioplasty
NEW VOYAGER PAD ANALYSIS CONFIRMS CONSISTENT BENEFIT OF LOW-DOSE RIVAROXABAN PLUS ASPIRIN FOLLOWING LOWER-EXTREMITY REVASCULARIZATION