2 Guest Editorial
Adam Tanious ruminates on how to navigate industry rep exchanges
8 uTBAD
A new randomized trial aimed at improving the lives of aortic dissection patients

2 Guest Editorial
Adam Tanious ruminates on how to navigate industry rep exchanges
8 uTBAD
A new randomized trial aimed at improving the lives of aortic dissection patients
In an official Society response, SVS President Joseph Mills, MD, tackles recent coverage of inappropriateness in vascular care in the mainstream media.


For

11 OBL
Drilling into the detail behind the value of an office-based lab
13 CMS


Proposed reduced conversion factor and reimbursement cuts

www.vascularspecialistonline.com
VAST FIELDS FULL OF MINES HINDER UKRAINE’S FORCES

GRIM PICTURE IN SOUTH
RICHMOND, British Columbia The polls predicted a re-elec- tion victory, maybe even a land- slide. But a couple of weeks before the vote, Kenny Chiu, a member of Canada’s Parliament and a critic of China’s human rights record, was panicking. Something had flipped among the ethnic Chinese voters in his British Columbia dis- trict. “Initially, they were support- ive,” he said. “And all of a sudden, they just vanished, vaporized, dis- appeared.” Longtime supporters originally from mainland China were not re- turning his calls. Volunteers re- ported icy greetings at formerly friendly homes. Chinese-lan- guage news outlets stopped cov- ering him. And he was facing an onslaught of attacks — from un- traceable sources — on the local community’s most popular social networking app, the Chinese- owned WeChat. The sudden collapse of Mr. Chiu’s campaign — in the last fed- eral election, in 2021 — is now drawing renewed scrutiny amid mounting evidence of China’s in- terference in Canadian politics. Mr. Chiu and several other elected officials critical of Beijing were targets of a Chinese state that has increasingly exerted its influence over Chinese diaspora communities worldwide as part of an aggressive campaign to ex- pand its global reach, according to current and former elected offi- cials, Canadian intelligence offi- cials and experts on Chinese state disinformation campaigns. Canada recently expelled a Chi- nese diplomat accused of conspir- ing to intimidate a lawmaker from the Toronto area, Michael Chong, after he successfully led efforts in Parliament to label China’s treat- ment of its Uyghur Muslim com- munity a genocide. Canada’s intel- ligence agency has warned at least a half-dozen current and for- mer elected officials that they have been targeted by Beijing, in- cluding Jenny Kwan, a lawmaker from Vancouver and a critic of Beijing’s policies in Hong Kong. The Chinese government, em- ploying a global playbook, dispro- portionately
Array of Trip Wires and Booby Traps
CounteroffensiveSlows
By ANDREW E. KRAMER
IN A LETTER TO HEALTHCARE providers dated July 11, 2023, the Food and Drug Administration (FDA) declared that the risk of mortality associated with paclitaxelcoated devices to treat peripheral arterial disease (PAD) is no longer supported based on data and analyses.
army is also hindered by a lack of air support and the deep network of defensive struc- tures the Russians have built. But it is the vast array of mines, trip wires, booby traps and impro- vised explosive devices that has Ukrainian forces bogged down only a few miles from where they started. “I couldn’t imagine something like this,” said a Ukrainian private named Serhiy, part of a unit that rescued the soldiers wounded by the explosions. “I thought mines would be lain in lines. But whole fields are filled with them, every- where.” Mines have long been a staple of Russian warfare, used exten- sively in Afghanistan and Chech- nya and earlier phases of the fighting in Ukraine, stretching back to 2014. But the minefields in southern Ukraine are vast and complex, beyond what had been previously known, soldiers who
Continued on Page8
The update signaled a lowering of the red flag raised in a 2019 letter from the FDA— published in response to a meta-analysis that indicated a late mortality signal—warning that treatment of PAD with paclitaxel-coated balloons and paclitaxel-eluting stents was “potentially associated with increased mortality.”
Alongside the letter, the FDA has updated its
See page 7
has renamed the specialty formerly known as “Cardiology & Heart Surgery” to include vascular surgery in its national rankings of the best hospitals
The category will now be called “Cardiology, Heart & Vascular Surgery,” the media company announced ahead of the Aug. 1 publication of its 2023–2024 Best Hospitals rankings and ratings.
See page 3
Vascular surgery added as named specialty to influential national hospital rankingsJoseph Mills
Medical Editor Malachi Sheahan III, MD
Associate Medical Editors
Bernadette Aulivola, MD | O. William
Brown, MD | Elliot L. Chaikof, MD, PhD

| Carlo Dall’Olmo, MD | Alan M. Dietzek
MD, RPVI, FACS | Professor HansHenning Eckstein, MD | John F. Eidt, MD
| Robert Fitridge, MD | Dennis R. Gable, MD | Linda Harris, MD | Krishna Jain, MD | Larry Kraiss, MD | Joann Lohr, MD
| James McKinsey, MD | Joseph Mills, MD | Erica L. Mitchell, MD, MEd, FACS
| Leila Mureebe, MD | Frank Pomposelli, MD | David Rigberg, MD | Clifford Sales, MD | Bhagwan Satiani, MD | Larry Scher, MD | Marc Schermerhorn, MD | Murray
L. Shames, MD | Niten Singh, MD | Frank
J. Veith, MD | Robert Eugene Zierler, MD
Resident/Fellow Editor
Christopher Audu, MD
Executive Director SVS
Kenneth M. Slaw, PhD
Director of Marketing & Communications Bill Maloney
Managing Editor SVS Beth Bales
Marketing & Social Media Manager
Kristin Spencer
Communications Specialist
Marlén Gomez

In the wake of the coverage of inappropriate vascular interventions in the mainstream press, guest editorialist Adam Tanious, MD, tackles the thorny issue of interactions with industry “reps”—particularly among younger surgeons.
Many of us in the surgical community have had an emotional response to the recent New York Times article describing the questionable practices of some of the members of our medical community.1 Against this backdrop, as I look to tackle the subject of interactions with our industry partners as surgeons/ interventionalists, a few disclosures:
I have many positive relationships with my industry representatives.
I have never received any form of payment from any industry partner.
I have just completed my MBA, taking specific courses in sales and marketing.
As a trainee, I did not appreciate at the time how much the way my attendings interacted with their reps influenced the way that I interact with reps as a young attending. This is something not discussed enough from an educational standpoint. We as attendings need to realize that trainees are watching not just how we operate or interact with the operating room (OR) and hospital staff—they are also looking to us for guidance on interacting with our industry partners. As a young intern and junior resident, I remember being incredibly quiet and simply observing the interactions of everybody in the room when reps and attendings were together. Even though I had grown up in a household raised by a rep in the world of finance, seeing this interaction in the field of medicine still did not add up—for profit companies sideby-side with physicians.
Published by BIBA News, which is a subsidiary of BIBA Medical Ltd.
Publisher Roger Greenhalgh
Content Director Urmila Kerslake
Managing Editor Bryan Kay bryan@bibamedical.com
Editorial contribution Jocelyn Hudson, Will Date, Jamie Bell, Éva Malpass, Adam Pearce and Marcus Yau
Design Terry Hawes
Advertising Nicole Schmitz nicole@bibamedical.com
Letters to the editor vascularspecialist@vascularsociety.org
BIBA Medical, Europe
526 Fulham Road, London SW6 5NR, United Kingdom
BIBA Medical, North America
155 North Wacker Drive – Suite 4250, Chicago, IL 60606, USA
Vascular Specialist is the official newspaper of the Society for Vascular Surgery and provides the vascular specialist with timely and relevant news and commentary about clinical developments and about the impact of healthcare policy. Content for Vascular Specialist is provided by BIBA News. Content for the news from SVS is provided by the Society for Vascular Surgery. | The ideas and opinions expressed in Vascular Specialist do not necessarily reflect those of the Society or the Publisher. The Society for Vascular Surgery and BIBA News will not assume responsibility for damages, loss, or claims of any kind arising from or related to the information contained in this publication, including any claims related to the products, drugs, or services, or the quality or endorsement of advertised products or services, mentioned herein. | The Society for Vascular Surgery headquarters is located at 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. POSTMASTER: Send changes of address (with old mailing label) to Vascular Specialist, Subscription Services, 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. | RECIPIENT: To change your address, e-mail subscriptions@bibamedical.com | For missing issue claims, e-mail subscriptions@bibamedical. com. | Vascular Specialist (ISSN 1558-0148) is published monthly for the Society for Vascular Surgery by BIBA News. Printed by Ironmark |
©Copyright 2023 by the Society for Vascular Surgery
Next, I’d like to define our terms. When I say industry, I am referring to both the publicly-traded and privately-held companies that make and manufacture devices that sparked a revolution in minimally invasive surgery we have been enjoying over the past two decades. More specifically, I am referring to the device representatives at the local level who are responsible for knowing their devices and make themselves available to assist surgeons/interventionalists in using these devices correctly to achieve the best outcomes for patients.2,3
For those newer to the world of industry, there are two main people you will work with at the local level as it pertains to industry: your local device representative and your “clinical” representative. A device representative is, by and large, a sales representative. They are required to have expert knowledge of their device and are expected to meet certain sales targets, with one key goal of expanding the sales in their respective territories. A “clinical” is a local representative who carries expert knowledge of the device or product in question, and is immediately available to clinicians to help with proper use and troubleshooting of said device in a clinical setting. They are not held to the same “targets” as their sales representative counterparts. However, based on which company you are discussing, there is likely a mutualistic relationship between a territory’s clinical and sales representatives (collectively referred to here as “reps”).2–4
Let us delve into the relationship our specialty has with industry and how it affects surgeons in their day-to-day practices—with a particular focus on being a young surgeon/interventionalist.
The relationship starts during training. Depending on your training institution, you are exposed to various interactions between your attendings and their industry colleagues. Reps are always excited and engaged when meeting trainees. These interactions usually happen over a much-needed cup of coffee bought by your reps. What proceeds is, hopefully, a very fruitful and positive relationship whereby your rep teaches trainees about the device they represent and its nuances, and appropriate instructions for use. Throughout our course as trainees, we become very familiar with our reps, and often engage them regarding cases where their device is going to be used.
Fast-forward to when trainees are ready to graduate: I recall this time in my life vividly as it is something you’ve been anticipating for the better part of a decade. Once you have decided on where you will go to practice, the inevitable invitations for a “handoff dinner” start to arrive from your local reps who are familiar with those at the location of your future job. These dinners are lovely and really a time to interact with people in a new city where you may have never lived. These dinners offer an opportunity to put a face to the name behind the person you will likely be calling on in the middle of the night during some aortic emergency, when you still have yet to figure out the hospital system, or the inner dynamics of the OR. Additionally, in most job settings you will need to be calling on your reps for a large portion of cases, as you may not have the necessary product available at your hospital to perform your desired procedure.
While these practices may sound questionable to a layperson reading this article, everyone must understand that these interactions go hand-in-hand with our ability as a medical community to provide patients with a “minimally invasive” option for surgery. There are very few patients who, when presented with both an open and minimally invasive surgical option, opt for the maximally invasive option. Our relationship with industry is often necessary to provide the care that patients want.
Additionally, reps have access to resources above and beyond what educators are given to help teach and train the next generation of surgeons and interventionalists. Industry has the power to help fund conferences and educational seminars where experts are allowed to teach their clinical knowledge to a large forum of future practitioners. I can personally attest that these are invaluable teaching and training opportunities that individual training programs just cannot be expected to
Now comes the hard part of being an attending—and the hard part of this article. What happens during the cases where industry representatives are not needed but can help “facilitate” cases? Reps often offer to be present for cases to “support” the case. This typically happens when you are treating a particular category
of disease that has a multitude of treatment options (i.e., peripheral arterial disease). Stated plainly, having a rep present for a case where you have multiple device options to choose from to effectively treat your patient has the strong potential to sway your decision.2–5
My question to everyone reading is this: should we put ourselves in a position to be swayed?
When I have predetermined the need of a particular product for a given case, I will always call upon a trusted rep with many years of experience to be present. Reps see their product used several times a day, every day of the week. It would be wrong of me to assume that level of experience with any device, as our jobs call for us to be experts in many different types of procedures, using an array of different products. As a junior attending, newly managing so many different aspects of the OR environment, why would I not welcome additional expertise that is available to me when I have predetermined a specific tool I plan on using anyway?
What we as practitioners must understand is the strategy to sales. Anyone with a knowledge of sales and marketing should understand that, more often than not, sales reps sell themselves, not just their product.2–6 While I truly believe that it is in the nature of every rep I have worked with to be extremely helpful and engaged in the OR, we must also realize that this is a sales tactic. The more buy-in we are given by reps during a case, the more we are likely to use their product. This extends to the cup of coffee and the meals bought for us before, between, or after cases.3,4,6 Taking it a step further, there will always be more aggressive reps who try to “actively” sell you on their product. It has happened to me personally.
This is not to say that the majority of device reps I have worked with try to actively sell during a procedure. In fact, many of the device reps I work with are the first to pull other competitors’ products during a case if it will serve the patient best. What I am saying is that there is an interaction that occurs that has meaningful outcomes for
all parties involved. More importantly, it may be harder to anticipate these interactions as freshly minted attendings than we give credit to during our training of future surgeons.
As I have grown as an attending, my ability to recognize the nuances of these interactions has evolved rapidly. Additionally, having senior partners who have good relationships with reps has also helped. Moreover, there is an earned confidence that comes with being the primary decision-maker responsible for a patient’s care that cements the relationship between physician and rep.
My goal here is not to provide an answer for young attendings about how to interact with industry. Rather, my aim is to start a conversation. What I think we as practitioners need to be better about is controlling who belongs in the OR. While it is not possible to know every potential problem we will run into during a case, as practitioners we should be better about deciding what tools and devices we anticipate using for specific pathologies, and ensure that, no matter who is present during a case, that our plan for our patient is not swayed by individuals who are ultimately hired to support a particular product.
More importantly, we as attendings should be actively engaged in teaching our trainees about all the tools we use, and be a sounding board for our trainees about the merits and pitfalls of these devices in conjunction with our industry colleagues. We must provide clear guidelines around the interaction between medicine and industry for the younger, more susceptible minds among us.
So, will I continue to have device representatives present for various cases? Yes. Will I plan on the particular device I want to use for each case before deciding on which rep to call? As often as possible, yes. Do I want my trainees to interact with and learn from my reps? Absolutely—with an attending present.
If an industry representative asks whether they can come to my next case “to support me,” will I let them? I can honestly say that, in this regard, I am on the fence.
Thomas K, Silver-Greenberg J, Gebeloff R. They Lost Their Legs. Doctors and Health Care Giants Profited.pdf [Internet]. New York Times. 2023. Chung KC, Kotsis SV, Berger RA, Ummersen GV. The Relationship Between Industry and Surgery. J 2011;36(8):1352–9.
O’Connor B, Pollner F, Fugh-Berman A. Salespeople in the Surgical Suite: Relationships between Surgeons and Medical Device Representatives. PLoS ONE 2016;11(8):e0158510. Lively C. The Dual Role of the Medical Device Representative. Voices in Bioethics 2020.
5. Grundy Q, Hutchison K, Johnson J, et al. Device representatives in hospitals: are commercial imperatives driving clinical decision-making? J Méd Ethics 2018;44(9):589–92.
6. Moed BR, Israel HA. Device Sales Representatives in the Operating Room: Do We Really Need or Want Them? A Survey of Orthopaedic Trauma Surgeons. J Orthop Trauma 2017;31(9):e296–300.
ADAM TANIOUS is an assistant professor of surgery in the Division of Vascular Surgery at Medical University of South Carolina in Charleston.
“The specialty formerly known as Cardiology & Heart Surgery has been renamed Cardiology, Heart & Vascular Surgery, in recognition that vascular specialists take the lead on some cases that have consistently been included in the specialty’s outcome measures,” writes Ben Harder, managing editor, and Min Hee Seo, senior health data scientist. “In certain contexts, U.S. News will use the shorthand Heart & Vascular to refer to Cardiology, Heart & Vascular Surgery.”
Recognition has long been sought for vascular surgery as a separate specialty within the rankings.
In 2020, the question of its inclusion was raised by then incoming SVS President Ronald L. Dalman, MD, and given a
continued from page 1
prominent spot in that year’s E. Stanley Crawford Critical Issues Forum, which took place during SVS ONLINE, the COVID-enforced digital replacement for VAM 2020. Dalman invited Harder to be part of the forum panel.

“One of the challenges for our members in the U.S. at the current time is the U.S. News & World Report rankings do not recognize vascular surgery as a separate specialty,” Dalman told Vascular Specialist at the time. “They have cardiology, cardiac surgery, neurological surgery, general surgery.”

With the recognition now in place, the SVS plans to work with the publication to further improve the rankings. “This move recognizes vascular surgery as an important specialty,” said SVS Executive
Director Kenneth
M. Slaw, PhD.“The SVS worked with U.S. News to enact this change, and as we move forward, we will continue to engage with the publication to offer suggestions to help with continued improvement of the rankings in the newly named domain.”—Bryan
Kay“We will continue to engage with [U.S. News] to offer suggestions to help with continued improvement of the rankings”
KENNETH M. SLAWPast SVS President Ronald L. Dalman
continued from page 1
There have been several recently published articles by respected news media outlets highlighting the deeply concerning issue of the overuse of invasive procedures to treat peripheral arterial disease (PAD). The front-page New York Times article (Sunday, July 16, 2023), first-authored by Katie Thomas, serves as the exclamation point. The SVS appreciates the efforts of the NYT to call attention to the inappropriate use of interventions in an effort to raise patient awareness, promote quality and advocate for safety in the delivery of vascular care.
The SVS has more than a 75-year history of setting the standards of care, quality and safety for patients with PAD. Founded in 1946, and comprising more than 6,000 members, the SVS mission is to advance excellence in vascular healthcare through education, advocacy, research and public awareness. Our mission and code of ethics focus on doing what is best and most appropriate for the care of patients with vascular disease, despite the challenges created by a struggling healthcare delivery system and problematic regulatory/reimbursement policies. We are troubled to see reports of patient harm because of the violation of the fundamental ethos of all physicians and surgeons to “first do no harm.” However, we are also concerned that such articles will cause patients to mistrust the healthcare system and delay seeking appropriate and timely care for limb- and sometimes life-threatening PAD.
It is essential for the public, affected patients and their family members to understand there is one primary specialty in medicine comprehensively educated, trained and tested to provide the full spectrum of evidence-based care to vascular patients. That specialty is vascular surgery. Vascular surgeons are defined and certified by rigorous national standards as the primary specialty trained to provide comprehensive care across the full spectrum of vascular disease states. While vascular care may often be team-based, vascular surgeons are irreplaceable on such teams because of their depth of understanding of the entire spectrum of vascular disease and its wide range of treatment options, including the full range of medical management, minimally invasive endovascular therapy and major surgical reconstructions. The vast majority of SVS members are vascular surgeons, board-certified by the Vascular Surgery Board (VSB) of the American Board of Surgery (ABS), who practice with integrity and are dedicated to appropriate, ethical care. Unfortunately, there are outliers practicing far beyond the pale who stretch ethical boundaries and deviate from the best available science and evidence base. Within the NYT article, regarding the procedure highlighted, it was noted that “from 2017–2021, about half of Medicare’s atherectomy payments—$1.4 billion—have gone to 200 high-volume providers.” It should be noted that none of
the physicians detailed in this NYT story is a board-certified vascular surgeon or SVS member. As the article also documents, after failed attempts at limb salvage by other practitioners, patients end up in the vascular surgeon’s care only as a last resort, sometimes far too late to save a precious limb.
The overwhelming majority of vascular surgeons, and a vast majority of other specialists that receive some training and play a role in the care of vascular patients—including those trained in vascular medicine, interventional cardiology, and interventional radiology—are providing high-quality, evidence-based care with safety and the best patient outcomes in mind. Appropriate and safe vascular care can be delivered in both outpatient and hospital settings.
Unfortunately, as in all professions and trades (albeit, more disturbing in the healthcare arena), there are outliers who overstep the bounds of ethics, appropriateness and quality, perhaps driven by other motivations, including notoriety or financial gain. This is a complex issue that requires the examination not only of the events detailed in this story, in which several patient experiences with the physicians that provided their care were highlighted, but of the underlying healthcare, economic, legal and regulatory policies that created fertile soil for this behavior to germinate and take root.
The issue of overuse in medical care is not a new one. Scientific, peer-reviewed articles written by SVS members and vascular surgeons were among the first to call attention to potential patient harm resulting from the aggressive overuse of interventions for patients with PAD largely brought about by regulatory and reimbursement coverage decisions that financially incentivized such therapy. These studies documented a dramatic increase in atherectomy procedures primarily performed in an outpatient setting, with extremely high-volume users (outliers) more likely to be non-vascular surgeons treating patients early after a diagnosis of claudication. As one example of a highly reimbursed procedure of unproven value, roughly 50% of Medicare reimbursements for atherectomy went to just 200 high-volume providers.
Beijing CanadaTargets Critics From Overseas Meddling With Ottawa
Part of Global Aims
RICHMOND, British Columbia
YDNI ELLEDGE FOR NEW YORK TIMES
Kelly Hanna, whose leg was amputated in 2020, received at least 18 artery-opening procedures on her legs from a Michigan doctor.
This article is by Katie Thomas Jessica Silver-Greenberg and Robert Gebeloff

he performed at least that many artery-opening procedures on Ms. Hanna’s legs, telling her they would improve blood flow and pre- ventTheyamputations. didn’t — for Ms. Hanna or many of his other patients. Sur- geons at nearby hospitals had seen so many of his patients with amputations and other problems that they complained to Michi- gan’s medical board about his con- duct. An insurance company told state authorities that 45 people had lost limbs after treatment at his clinics in the past four years. Dr. Mustapha is no back-alley operator working in the shadows of the medical establishment, an investigation by The New York
The NYT article also alludes to the potential for the development of improper relationships between industry and healthcare practitioners as one factor that may drive inappropriate use or overuse of drugs and devices for financial gain. A detailed discussion of this issue is not possible here, but there is no doubt that the medical industry of drug and device manufacturers is essential to the provision of healthcare and innovation in therapy. Many widely available and highly useful drugs and devices (stents, endovascular grafts, etc.) have been developed by ethical, scientific collaboration between practicing physicians and surgeons and the healthcare technology industry. As do most other medical societies, the SVS has a pol-
Kelly Hanna’s leg was amputat- ed on a summer day in 2020, after a Michigan doctor who called him- self “the leg saver” had damaged her arteries by snaking metal wires through them to clear away plaque. It started with a festering wound on her left foot. Her podia- trist referred Ms. Hanna to Dr. Ji- had Mustapha. Over 18 months,
By SHEERA FRENKEL and STUART A. THOMPSON
For more than 20 years, Kit Loffstadt has written fan fiction exploring alternate universes for “Star Wars” heroes and “Buffy the Vampire Slayer” villains, sharing her stories free online. But in May, Ms. Loffstadt stopped posting her creations af- ter she learned that a data com- pany had copied her stories and fed them into the artificial intelli- gence technology underlying ChatGPT, the viral chatbot. Dis- mayed, she hid her writing behind a locked account. Ms. Loffstadt also helped orga- nize an act of rebellion last month against A.I. systems. Along with dozens of other fan fiction writers, she published a flood of irreverent stories online to overwhelm and confuse the data-collection serv- ices that feed writers’ work into A.I.“Wetechnology. each have to do whatever we can to show them the output of our creativity is not for machines to harvest as they like,” said Ms. Loffstadt, a 42-year-old voice ac- tor from South Yorkshire in Brit- ain. Fan fiction writers are just one group now staging revolts against A.I. systems as a fever over the technology has gripped Silicon Valley and the world. In recent months, social media companies such as Reddit and Twitter, news organizations including The New York Times and NBC News, au-
Times has found. With the finan- cial backing of medical device manufacturers, he has become a leader of a booming cottage indus- try that peddles risky procedures to millions of Americans — enrich- ing doctors and device companies and sometimes costing patients their limbs. The industry targets the roughly 12 million Americans with peripheral artery disease, in
ORIKHIV, Ukraine — I was a grisly scene of bloody limbs and crumpled vehicles as a series of Russian mines exploded across a field in southern Ukraine. One Ukrainian soldier stepped on a mine and tumbled onto the grass in the buffer zone between the two armies. Nearby lay other Ukrainian troops, their legs in tourniquets, waiting for medical evacuation,
of several soldiers involved. Soon, an armored
ar- rived to rescue them.
jumped out to treat the
and knelt on ground he deemed safe — only to trigger
mine with his knee.
weeks into
sive that even
say is off to a
which plaque, a sticky slurry of fat, calcium and other materials, accumulates in the arteries of the legs. For a tiny portion of patients, the plaque can choke off blood flow, leading to amputations or death. But more than a decade of medi- cal research has shown that the vast majority of people with pe- ripheral artery disease have mild or no symptoms and don’t require treatment, aside from getting more exercise and taking medica- tion. Experts said even those who do have severe symptoms, like Ms. Hanna, shouldn’t undergo re- peated procedures in a short peri- od of time.
icy on conflict of interest and conflicts of commitment.
These ethical principles underpin and guide all we do, not only as a medical organization, but also as individual practitioners. The needs of the patient should always come first; no procedure should be recommended or performed in any patient if it is not primarily and solely for the benefit and best interests of that patient.
By J. DAVID GOODMANContinued on Page18
The polls predicted a re-elec- tion victory, maybe even a land- slide. But a couple of weeks before the vote, Kenny Chiu, a member of Canada’s Parliament and a critic of China’s human rights record, was panicking. Something had flipped among the ethnic Chinese voters in his British Columbia dis- trict. “Initially, they were support- ive,” he said. “And all of a sudden, they just vanished, vaporized, dis- appeared.” Longtime supporters originally from mainland China were not re- turning his calls. Volunteers re- ported icy greetings at formerly friendly homes. Chinese-lan- guage news outlets stopped cov- ering him. And he was facing an onslaught of attacks — from un- traceable sources — on the local community’s most popular social networking app, the Chinese- owned WeChat. The sudden collapse of Mr. Chiu’s campaign — in the last fed- eral election, in 2021 — is now drawing renewed scrutiny amid mounting evidence of China’s in- terference in Canadian politics. Mr. Chiu and several other elected officials critical of Beijing were targets of a Chinese state that has increasingly exerted its influence over Chinese diaspora communities worldwide as part of an aggressive campaign to ex- pand its global reach, according to current and former elected offi- cials, Canadian intelligence offi- cials and experts on Chinese state disinformation campaigns. Canada recently expelled a Chi- nese diplomat accused of conspir- ing to intimidate a lawmaker from the Toronto area, Michael Chong, after he successfully led efforts in Parliament to label China’s treat- ment of its Uyghur Muslim com- munity a genocide. Canada’s intel- ligence agency has warned at least a half-dozen current and for- mer elected officials that they have been targeted by Beijing, in- cluding Jenny Kwan, a lawmaker from Vancouver and a critic of Beijing’s policies in Hong Kong. The Chinese government, em- ploying a global playbook, dispro- portionately focused on Chinese Canadian elected officials repre- senting districts in and around Vancouver and Toronto, experts say. It has leveraged large diaspo- ra populations with family and business ties to China and ensur- ing that the levers of power in those communities are on its side, according to elected officials, Ca- nadian intelligence officials and experts on Chinese disinforma- tion. “Under Xi Jinping’s leadership, China has doubled down on this assertive nationalist policy to- ward the diaspora,” said Feng Chongyi, a historian and an asso- ciate professor at the University of Technology Sydney. China’s role in Canada mirrored what has happened in Australia, he added. Chinese state interference and its threat to Canada’s democracy
inter- views with commanders and sol- diers fighting along the front indi- cate the slow progress comes down to one major problem: land mines. The fields Ukrainian forces must cross are littered with doz- ens of types of mines — made of plastic and metal, shaped like tins of chewing tobacco or soda cans, and with colorful names like “the witch” and “the leaf.” Ukraine’s army is also hindered by a lack of air support and the deep network of defensive struc- tures the Russians have built. But it is the vast array of mines, trip wires, booby traps and impro- vised explosive devices that has Ukrainian forces bogged down only a few miles from where they started.
“I couldn’t imagine something like this,” said a Ukrainian private named Serhiy, part of a unit that rescued the soldiers wounded by the explosions. “I thought mines would be lain in lines. But whole fields are filled with them, every- where.” Mines have long been a staple of Russian warfare, used exten- sively in Afghanistan and Chech- nya and earlier phases of the fighting in Ukraine, stretching back to 2014. But the minefields in southern Ukraine are vast and complex, beyond what had been previously known, soldiers who
therapy and control of their risk factors to the extent possible. There are three stages of PAD: asymptomatic, claudication (leg cramping or pain when walking) and chronic limb-threatening ischemia (CLTI, which means non-healing wounds or gangrene).
The SVS has been the leading national
THE COUNTRYPRAIRIE VIEW, Texas — Drive northwest out of Houston, and as cow pastures wrestle back the flat expanse from the city’s sprawl,tentacled there arise along the road, suddenly, improba- bly, many, many cricket fields. Head south to find a small cricket stadium nestled in the
suburbs, or west to find fields sprouting in county parks. The game of cricket — a bat- ball-and-wicket contest of pa- tience and athleticism that was born in Britain and is barely understood by most Americans — has surprisingly taken hold in the land of Friday night football. A surging population of South Asian immigrants around Hous- ton and Dallas imported their favorite sport to their adopted home, where it has grown amid a
Device Makers Finance Cottage Industry for Risky NATIONAL 12-21 Hollywood’s Moment of Angst
Lone Star culture of competition in all things, especially sports. Cricket’s swift rise in Houston has attracted international atten- tion and helped make Texas the launching pad for the sport’s first American professional league, Major League Cricket, whose inaugural season began on Thursday outside Dallas.
“One of the unknown things about Houston is the diversity of the population from many cricket-playing countries,” said
organization in defining quality and safety standards for the provision of comprehensive vascular care, particularly for PAD. There are an estimated 10–12 million people in the U.S. who have PAD, so it is important to educate patients and the public about PAD and how it should be treated. The disease is caused by the build-up of plaque deposits in the walls of arteries due to a combination of risk factors, including diabetes, smoking, hypertension, hyperlipidemia, increased age and genetics. PAD is a broad spectrum of disease; in general, it is a marker for cardiovascular disease, and the most common complication to develop in affected patients is not limb loss, but rather heart attacks and stroke. Thus, all patients with PAD should have best medical
Tim Cork, a deputy consul gen- eral at the British consulate in Houston. “There are Indians, Pakistanis, there’s obviously a huge number of Brits here, Aus- tralian accents wherever you go.” The number of people of Indi- an heritage in Texas has doubled over the last decade to half a million, according to estimates from the Census Bureau’s annual survey, with 73,000 in Harris County, which includes Houston, and 64,000 in suburban Fort
Bend“WhenCounty. I came to this country, the only sport I knew was cricket,” said KP George, the county judge in Fort Bend, who immigrated from India in 1993. When he was elected in 2018, none of the county parks had a cricket field, he said. Now there are seven, and each is reserved for play months in advance. “There’s a huge demand,” he said. “We’re working on a couple
The U.S. envoy John Kerry travels to China as Washington and Beijing re- start talks on global warming. PAGE 10 2 Polluters Meet on Climate LATE EDITION $6.00 Today, showers and thunderstorms, downpours may lead to flooding, high 82. Tonight, thunderstorms, low 72. Tomorrow, humid with sun, high 89. Weather map, Page 20.
Only the latter has a significant risk of limb loss, and even in CLTI patients the risk depends upon the stage of disease. Through the publication of research studies, evidence-based guidelines and appropriate use criteria documents, the SVS has consistently promulgated the principle that the best care for the majority of patients with PAD—particularly those who are asymptomatic—is to promote exercise (walking) and to manage the PAD medically by modifying correctable risk factors such as elevated lipids, diabetes, smoking and hypertension.
Continued on Page21
PAD is common, particularly in older people, but not all leg pain is directly related to PAD—even in those who have the disease. For example, arthritis, gout, musculoskeletal and spinal problems can all cause leg and foot pain. Even for patients who have pain when walking from PAD, the majority are best treated initially with risk-factor control, walking therapy to promote collaterals and muscle adaptation to exercise, and occasionally medicines specific for vascular leg pain brought on by walking (since fewer than 5% of patients with claudication progress to a limb-threatening PAD stage). Vascular surgeons are uniquely trained and positioned to understand the full context and spectrum of PAD and all of the available treatment options. As such, it has been the position of the SVS that a first intervention for PAD patients—even a “minimally invasive procedure”—should be done only when absolutely necessary, as, once completed, it may “accelerate the clock” and speed the progression of vascular disease and its complications.
on page 6“The SVS has been the leading national organization in defining quality and safety standards for the provision of comprehensive vascular care, particularly for PAD”
The first and only EVAR system with a decade of global registry outcomes1
94.7% FF aneurysm-related mortality (ARM)†
64.1% Sac regression‡
Choose the proven one. Choose the one your patients deserve. Choose the standard of EVAR durability.

Explore more at: medtronic.com/ENGAGE10year
†Data reported through 10-year time frame with full + extended cohort, determined by Clinical Event Committee. ‡ Data reported through 10-year time frame with full + extended cohort.
1 Verhagen, et al. The ENGAGE Registry: Ten-Year Outcomes with the Endurant Stent Graft for Endovascular Abdominal Aortic Aneurysm Repair. Presented at: Charing Cross 2023 International Symposium; April 26, 2023; London, UK.
continued from page 4
Invasive procedures for claudication may improve function and quality of life but patients should be selected carefully, and the interventions tailored to be both safe and likely to produce meaningful benefit. The SVS practice guidelines have proposed a threshold of at least two years of likely durability for an intervention performed for claudication. There is a disturbing trend of overly aggressive treatment, with recent studies demonstrating nearly 30% of patients are receiving interventions on below-the-knee arteries, despite no evidence they would benefit and mounting evidence it may accelerate their disease. Moreover, the article highlights the growing frequency of multiple, repeated procedures that is emblematic of poor patient selection and inadequate durability of the chosen procedure, leading to a vicious cycle of repetitive interventions that is not only costly, but also dangerous.
There are patients with PAD (perhaps 5–8%) who suffer from, or progress to, the most advanced PAD stage—that of CLTI.
Indications
This condition is more prevalent in people with diabetes. Preventing amputation in such patients hinges on early and accurate diagnosis, followed by an individualized treatment plan targeted to the patient’s risk, goals and stage of disease. Such a plan is best carried out with the involvement of a vascular surgeon, and frequently includes other specialists, such as podiatrists. The SVS spearheaded and published classification systems to assess risk of limb loss, an anatomic staging system, and global guidelines for evidence-based care to save limbs and prevent amputations. Although many CLTI patients require intervention, endovascular therapy is only one option, and a good number of patients fare better with surgical bypass. Vascular surgeons are the only specialists trained to offer both options, when needed. Patients deserve to
The Endurant™ II/Endurant™ IIs bifurcated stent grafts are indicated for the endovascular treatment of infrarenal abdominal aortic or aortoiliac aneurysms. They may be utilized in conjunction with the Heli-FX ™ EndoAnchor™ system when augmented radial fixation and/or sealing is required; in particular, in the treatment of abdominal aortic aneurysms with short (≥ 4 mm and < 10 mm) infrarenal necks (see Neck length definition below). The Endurant II stent graft system aorto-uni-iliac (AUI) stent graft is indicated for the endovascular treatment of infrarenal abdominal aortic or aortoiliac aneurysms in patients whose anatomy does not allow the use of a bifurcated stent graft. The Endurant II/IIs stent graft system is indicated for use in patients with the following characteristics:
• Adequate iliac or femoral access that is compatible with vascular access techniques, devices, or accessories
• Proximal neck length of
• ≥ 10 mm; or
• ≥ 4 mm and < 10 mm when used in conjunction with the Heli-FX EndoAnchor system (bifurcated stent graft only)
Note: Neck length is defined as the length over which the aortic diameter remains within 10% of the infrarenal diameter.
• Infrarenal neck angulation of ≤ 60°
• Aortic neck diameters with a range of 19 to 32 mm
• Distal fixation length(s) of ≥ 15 mm
• Iliac diameters with a range of 8 to 25 mm
• Morphology suitable for aneurysm repair
Contraindications
The Endurant II/Endurant IIs stent graft system is contraindicated in:
• patients who have a condition that threatens to infect the graft
• patients with known sensitivities or allergies to the device materials
When used with the Heli-FX EndoAnchor system, the Endurant II/IIs stent graft system is also contraindicated in:
• patients with known sensitivities to the EndoAnchor implant materials. For contraindications regarding ancillary devices used with the Endurant II/Endurant IIs stent graft system, refer to the Instructions for Use provided with the device.
Warnings and Precautions
• The long-term safety and effectiveness of the Endurant II/Endurant IIs stent graft system has not been established. All patients should be advised that endovascular treatment requires lifelong, regular follow-up to assess the health and the performance of the implanted endovascular stent graft. Patients with specific clinical findings (e.g., endoleaks, enlarging aneurysms, changes in the structure or position of the endovascular graft), or less than the recommended number of EndoAnchor implants when used in short proximal necks (≥ 4 mm and < 10 mm), should receive enhanced follow-up. Specific follow-up guidelines are described in the Instructions for Use
• Patients experiencing reduced blood flow through the graft limb, aneurysm expansion, and persistent endoleaks may be required to undergo secondary interventions or surgical procedures.
• The Endurant II/Endurant IIs stent graft system is not recommended in patients unable to undergo or who will not be compliant with the necessary preoperative and postoperative imaging and implantation procedures as described in the Instructions for Use
• Renal complications may occur: 1) From an excess use of contrast agents. 2) As a result of emboli or a misplaced stent graft. The radiopaque marker along the edge of the stent graft should be aligned immediately below the lower-most renal arterial origin.
• Studies indicate that the danger of micro-embolization increases with increased procedure duration.
be fully informed when making decisions about invasive treatments.
Vascular surgeons have also pioneered tracking patient outcomes. To this end, the SVS established its Patient Safety Organization (PSO) to monitor outcomes of patient care, which now includes 1,007 participating centers, and has collected the outcomes of more than 1 million vascular interventions within its Vascular Quality Initiative (VQI) registries. In addition, in collaboration with the American College of Surgeons (ACS), the SVS recently launched it Vascular Verification Program (Vascular-VP), setting standards of quality across vascular care settings.
Vascular surgeons are actively engaged in and leading the effort to promote shared decision-making and patient education around PAD care, including the message that while an abnormal ankle-brachial index (ABI)—a non-invasive measure of blood flow to the leg/foot—or the symptom of claudication can be important warning signs, the best therapeutic response is most often best medical therapy, not the “quick fix” of an intervention performed unnecessarily or prematurely.
As reported in another recent article by ProPublica, the SVS feels strongly that the public at large and the vascular patient population should be educated and have access

to all the resources they need to make the best choices for their care. This includes being provided with an explanation of the natural history of their condition, the expected outcomes of medical and interventional therapy, and understanding the differences between a variety of types of providers who perform some vascular procedures compared to board-certified vascular surgeons who provide the full spectrum of vascular disease care.
The SVS will continue to actively promote quality and safety for vascular patient care through its published guidelines, appropriate care documents, PSO-VQI registry and initiatives such as the Vascular Verification Program. All practitioners in vascular practice are encouraged to become familiar with and to utilize them. The SVS will continue to develop these resources and make them available.
The SVS encourages patients to check and verify the credentials of their providers before agreeing to a plan of vascular care. We also encourage second opinions. Finally, in their efforts to cover health news, the SVS urges media professionals to be diligent in presenting healthcare and medical information that is fully balanced, as coverage could lead to patient distrust and delays in necessary care with potentially adverse consequences.
JOSEPH MILLS is president of the SVS. He wrote this official Society response on behalf of the SVS Executive Board.
• The safety and effectiveness of the Endurant II/Endurant IIs stent graft system has not been evaluated in some patient populations. Please refer to the product Instructions for Use for details.
MRI Safety and Compatibility: Non-clinical testing has demonstrated that the Endurant II/Endurant IIs stent graft is MR Conditional. It can be scanned safely in both 1.5T & 3.0T MR systems under certain conditions as described in the product Instructions for Use. For additional MRI safety information, please refer to the product Instructions for Use
Adverse Events
Potential adverse events include (arranged in alphabetical order): amputation; anesthetic complications and subsequent attendant problems (e.g., aspiration), aneurysm enlargement; aneurysm rupture and death; aortic damage, including perforation, dissection, bleeding, rupture and death; arterial or venous thrombosis and/or pseudoaneurysm; arteriovenous fistula; bleeding, hematoma or coagulopathy; bowel complications (e.g., ileus, transient ischemia, infarction, necrosis); cardiac complications and subsequent attendant problems (e.g., arrhythmia, myocardial infarction, congestive heart failure, hypotension, hypertension); claudication (e.g., buttock, lower limb); death; edema; EndoAnchor system (for infrarenal EVAR procedures using the Heli-FX EndoAnchor system): partial deployment, inaccurate deployment, fracture, dislodgement, embolization, stent graft damage, modelling balloon damage); embolization (micro and macro) with transient or permanent ischemia or infarction; endoleak; fever and localized inflammation; genitourinary complications and subsequent attendant problems (e.g., ischemia, erosion, femoral-femoral artery thrombosis, fistula, incontinence, hematuria, infection); hepatic failure; impotence; infection of the aneurysm, device access site, including abscess formation, transient fever and pain; lymphatic complications and subsequent attendant problems (e.g., lymph fistula); neurologic local or systemic complications and subsequent attendant problems (e.g., confusion, stroke, transient ischemic attack, paraplegia, paraparesis, paralysis); occlusion of device or native vessel; pulmonary complications and subsequent attendant problems; renal complications and subsequent attendant problems (e.g., artery occlusion, contrast toxicity, insufficiency, failure); stent graft: improper component placement; incomplete component deployment; component migration; suture break; occlusion; infection; stent fracture; graft twisting and/or kinking; insertion and removal difficulties; graft material wear; dilatation; erosion; puncture and perigraft flow; surgical conversion to open repair; vascular access site complications, including infection, pain, hematoma, pseudoaneurysm, arteriovenous fistula, dissection; vascular spasm or vascular trauma (e.g., iliofemoral vessel dissection, bleeding, rupture, death); vessel damage; wound complications and subsequent attendant problems (e.g., dehiscence, infection, hematoma, seroma, cellulitis)
Please reference product Instructions for Use for more information regarding indications, warnings, precautions, contraindications, and adverse events.
Caution: Federal (USA) law restricts this device to sale by or on the order of a physician.
medtronic.com/aortic
continued from page 1
recommendations for healthcare providers regarding the use of paclitaxel-coated balloons and stents for PAD. As well as removing references to the possibility of increased mortality with these devices, the amended guidance softens the language around the monitoring of patients who have been treated with paclitaxel-coated stents and balloons, stating that healthcare providers should continue “routine” rather than “close” monitoring of these patients, as had previously been stated.
The safety of paclitaxel—used in peripheral interventions to prevent restenosis—was called into question by data put forward in 2018 by Konstantinos Katsanos, MD, an interventional radiologist at University of Patras, Patras, Greece, et al that pointed to an increased risk of death at two and five years following the use of paclitaxelcoated balloons and paclitaxel-eluting stents in the femoropopliteal artery.


The FDA responded, notifying
healthcare providers in early 2019 about a late mortality signal in patients treated for PAD in the femoropopliteal artery with paclitaxel-coated balloons and paclitaxel-eluting stents. Their most recent update on the topic, prior to that shared on July 11, 2023, was posted in August 2019.

In its new update, the FDA notes that “additional data from the pivotal randomized controlled trials (RCTs) has become available,” and that the Administration has worked with device manufacturers and external stakeholders to develop the protocol and analysis
plan for new data generation.
The FDA referenced the fact that device manufacturers collaborated in an updated meta-analysis, which included “additional studies, more complete vital status information, and longer-term follow-up compared to prior studies.” Patient follow-up in these studies ranged from two to five years, the FDA noted, leading the agency to conclude that the updated RCT meta-analysis “does not indicate that the use of paclitaxel-coated devices is associated with a late mortality signal.”
Furthermore, the FDA stated that it also reviewed additional analyses of the risk for late mortality, including the SWEDEPAD trial interim analysis, the VOYAGER PAD study, the German BARMER Health Insurance study, the Veterans Health Administration study and the Medicare SAFE-PAD study. “None of these studies, with mean or median follow-up ranging from 1.7 to 3.5 years, found a risk for late mortality associated with paclitaxel-coated devices,” the FDA communicated.

 Jocelyn Hudson and Will Date
Jocelyn Hudson and Will Date
● “We are now able to focus back on, not so much safety, but trying to define the most effective type of technology to treat the kind of disease patterns we’re seeing, particularly in our diabetic patients with CLTI [chronic limbthreatening ischemia],” said Michael Conte, MD (San Francisco).
● “Myself, and I think a lot of people in the vascular surgery community, felt strongly that paclitaxel was likely not related to mortality, but a lot of that was based on low-level data, or our own, personal intuition. So it is exciting to see a variety of different data sources upholding these beliefs,” commented Caitlin Hicks, MD, (Baltimore, Maryland).

● “The FDA statement is unambiguous in the sense that they do not see a mortality signal. They urge us to take good care of our patients ... and emphasize the need for concomitant medical therapy” said Peter Schneider, MD (San Francisco).

“None of these studies, with mean or median follow-up ranging from 1.7 to 3.5 years, found a risk for late mortality” FDA
FROM THE COVER: LONG-AWAITED FDA UPDATE FINDS DATA DO NOT SUPPORT EXCESS MORTALITY RISK FOR PACLITAXELCOATED DEVICES
BECAUSE HIGH-QUALITY EVIDENCE from large, prospective multicenter trials on the best treatment of uncomplicated type B aortic dissection (uTBAD) is scarce, SVS members Firas F. Mussa, MD, a professor of vascular surgery at UTHouston in Houston, Texas, and Panos Kougias, MD, chair of the Department of Surgery at SUNY Downstate Health Sciences in New York City, are moving forward with a large randomized trial to address this unmet need. Other principal investigators are Manesh Patel, MD, Seekanth Vemalapalli, MD, and Sean O’Brien, PhD, from Duke Heart Center, Duke University and Duke Clinical Research Institute (DCRI) in Durham, North Carolina, the award recipient institution. Sherene Shalhub, MD, head of vascular surgery at Oregon Health Sciences University in Portland, Oregon, will lead the patient engagement.
This prospective, pragmatic, randomized clinical trial, entitled IMPROVE-AD (Improving outcomes in vascular disease—aortic dissection), will enroll its first patient by the end of the year.
Acute aortic dissection is the most common life-threatening aortic emergency, with 30–40% classified as uTBAD. The current standard-of-care consisting of optimal medical therapy with surveillance is appropriate in the majority of such dissections. However, recent data suggest early thoracic endovascular repair, known as TEVAR, could be beneficial for some patients, said Mussa. In fact, the trial’s primary hypothesis is that the latter therapy will be superior.
The trial will assess clinical outcomes in patients with subacute uTBAD undergoing either upfront TEVAR plus medical therapy vs. medical therapy with surveillance for deterioration.

IMPROVE-AD is funded by the National Heart, Lung and Blood Institute (NHLBI) to enroll and randomize 1,100 patients at 60 sites in North America. It expected to last seven years and generate the sought-after quality evidence to guide daily clinical practice and future SVS guidelines.
Treatment of aortic dissection is a top SVS clinical research priority in aortic disease. Writing a letter of support to Mussa, SVS Immediate Past President Michael Dalsing, MD, said, “… it is our belief that this trial addresses a significant and timely question related to the care of patients with acute type B aortic dissection as there remains clinical equipoise when considering available treatment options
at the time of initial presentation. When completed, your trial will provide strong evidence that will guide clinical practice in a safe and rational manner.”

Mussa has worked on the project for almost a decade, and, over the past several years, with support from other vascular surgeons, has refined the design and organization of the trial. “Until today, I wake up and think of the trial design, endpoint, ancillary studies, enrollment and how to get people engaged,” said Mussa.
Personnel at the 60 sites will collect baseline history, dissection-related data and in-hospital outcomes. Duke Clinical Research Institute will collect medical events.
To be included, uTBAD patients must be more than 21 years old and have no history of aortic intervention. The condition is defined as dissection without involvement of the aorta at, or proximal to, the innominate artery, without rupture and/or malperfusion (renal, mesenteric, or extremity). Patients will be randomized within 48 hours to six weeks, stratified by the presence of one of the high-risk features upon presentation.
Site investigators will determine all subsequent care (including additional testing, medications/procedures), with the exception of aortic interventions. Such interventions will be allowed for: acute complications (rupture and/ or malperfusion, embolization, or aortoesophageal/aortotracheal fistula), aneurysmal degeneration of more than 55cm, significant aortic growth of more than 5mm over a six-month period, or persistent pain and/or hypertension during index admission. All participants will have their blood pressure monitored remotely, with follow-up administered through the use of a centralized call center with physician adjudication of relevant cardiovascular and aortic events.
“In addition to determining the optimal treatment that leads to the best shortand long-term benefit, we also want to address other questions, including the impact of high-risk dissection features on outcomes,”said Kougias. “Also, we should aim to further understand what patients want; what are their priorities? That’s a critical part of what we should be asking.”
The trial’s primary endpoint is the

composite of all-cause death or major aortic complications. Secondary endpoints are quality of life, cardiovascular hospitalizations, cardiovascular death and components of the primary endpoint.
The trial is sponsored by UT Health Houston, SUNY Downstate Health Sciences University, and Duke Clinical Research Institute. An IMPROVE-AD informational meeting held during VAM 2023 in June drew a crowd of surgeonscientists and clinicians who wanted to learn more and become involved in the trial.
Meeting attendees had many suggestions and thoughts, including on the “diagnosis-to-intervention” timeframe, with most selecting the six-week mark as the endpoint for intervention to be included in the trial. An attendee suggested the trial should include a parallel patient engagement plan to make sure patient voices are heard.
Many indicated they are willing to enroll their patients. “Every one of you has a patient who would qualify,” Mussa pointed out to those in attendance. “My ‘ask’ of you is to please connect them with us.” He also asked surgeons to participate in the analysis
proposed several ancillary studies pending further funding.
Patrice Desvigne-Nickens, MD, from the NHLBI, stressed the importance of the shared partnership with the institute for the trial. “We really want this to go forward and succeed,” she said.
The trial has several unique features, she explained, including that it is pragmatic. “It will enroll every eligible patient and really answer vital questions for surgeons,” she said. “Medicine is a random distribution of what the physician decides to do.”
Determining systematically what is best in practice is a better way to make decisions, she added, encouraging all the surgeons in attendance to participate, either by enrolling patients or participating in analysis. “Your participation is really key,” Desvigne-Nickens concluded.
The IMPROVE-AD trial will follow these treatment strategies:
● Upfront medical therapy with surveillance for deterioration: Medical therapy will consist of comprehensive secondary prevention with lifestyle and pharmacologic intervention. Site investigators will use SVS guidelines to assess antihypertensive therapy and blood pressure control. Investigators will also be given information regarding societal recommendations for follow-up imaging surveillance.
● Upfront TEVAR plus medical therapy: Medical therapy will be administered similarly to the upfront medical therapy arm. Upfront TEVAR will need to occur within 48 hours to six weeks of the index admission for uTBAD. The Surgical Therapy Committee will be responsible for qualifying site investigators/operators based on TEVAR experience and other criteria. TEVAR with any commercially available
device, as per accepted intervention guidelines, will be allowed, with the Surgical Therapy Committee being responsible for reviewing and ensuring the quality of intervention.
● In both arms, the participants’ care teams will be provided with physician and patient informational resources summarizing current recommendations for medical therapy and blood pressure targets. Optimal medical therapy and adherence to follow-up imaging surveillance will be monitored by the Medical Therapy Committee. Participant follow-up will be performed at 30 days, six months, 12 months and every six months thereafter up to a maximum possible follow-up of 72 months. All studyrelated follow-up will be done via centralized call centers and remote blood pressure monitoring.
“In addition to determining the optimal treatment that leads to the best short- and longterm benefit, we also want to address other questions, including the impact of high-risk dissection featuresPanos Kougias Firas F. Mussa
The Society for Vascular Surgery is proud to welcome the following new members, who joined the SVS in the end of 2022 and first half of 2023.
Matthew Abate, MD; Baton Rouge, LA
Elliot Adams, MD; Charleston, WV
Christopher J Agrusa MD; New York NY
Majid Toseef Aized, MD; Saginaw, MI
Kelechi Akuma, MD; Parkland, FL
Sean Alcantara, MD; Lake Success, NY
Hasan A Aldailami, MD; Scottsdale, AZ
Ioana Antonescu MD MSc; Chapel Hill NC
Cassra Arbabi, MD; Los Angeles, CA
Diego Ayo, MD; Gainesville, FL
Erin Kelly Green Baldwin, MD; Tampa, FL
Melissa Baldwin, MD; Brooklyn, NY
Simpledeep Banipal, MD; Porter Ranch, CA
Michael Barfield, MD; New York, NY
Tushar Barot, MD, MPH; Lakeland, FL
Peter Bartline, MD; Kenmore, WA
Matthew Evans Bennett MD; Seattle WA
Besem Beteck, MD; Oklahoma City, OK
Emelia Noele Bittenbinder, MD; Mechanicsburg, PA
Stuart L Blackwood, MD; Springfield, MA
Jordan Bond; Southlake, TX
Alyssa Bonta MD; Kettering OH
Arash Bornak, MD; Miami, FL
Saideep Bose, MD, MPH; Saint Louis, MO
Michael Bounds, MD; Salisbury, MD
Mina Boutrous, MD; Farmington, CT
Kathryn Elizabeth Bowser, MD; Newark, DE
Estela Brooke, MD; New Orleans, LA
Justin Brown, MD; Savannah, GA
Donald Brown, DO; Dakota Dunes, SD
Michael Buckley MD; Knoxville TN
Rafael Bustamante, MD; Davie, FL
Aurelia Calero, MD; Tampa, FL
Cesar Castillo, MD; Guaynabo, PR
Kirk Charles, MD; Raleigh, NC
Anthony Hung Chau M D ; Orange CA
Steve Chausse, MD; Crestview Hills, KY
Amit Chawla, MD; New Orleans, LA
David Chiapaikeo, MD; Old Bridge, NJ
Johnpaul Chizea, MD; Chester, PA
Carleen Cho MD; Fairview PA
Atish Chopra, MD; Colleyville, TX
Elizabeth Chou, MD; Los Angeles, CA
Warren Bryan Chow, MD; Kirkland, WA
Erica Clark DO; Spartanburg SC
Michol Cooper, MD; Boston, MA
Jonathan Scott Cudnik, MD; Macon, GA
Jason Cumbers, MD; Paducah, KY
Calogero DiMaggio, DO; Hellertown, PA
Danielle Dombrowski MD; Las Vegas NV
Graham Donald, MD; Boise, ID
Garima Dosi, MD; Sharon, MD
Sira Duson, MD; Baltimore, MD
John Dussel, MD; Farmington, CT
Sara Edeiken MD; Houston TX
Justin Eisenberg, MD; Spring Lake, MI
Prince Esiobu, MD; Riverside, CA
Kathryn Fong, MD; Richmond, VA
Brian Freeman, MD; Watkinsville, GA
Daniel Fremed, MD; Livingston, NJ
Justin Galovich, MD; Woodland Hills, CA
Elizabeth Anne Genovese, MD, MS; Philadelphia, PA
Elizabeth Genovese, MD; Charleston, SC
Matthew Gibson MD; Pawleys Island SC
Julia Glaser, MD; Philadelphia, PA
Derrick Green, MD; Minneapolis, MN
Cindy Ha, MD; Tacoma, WA
Heidi Hansen, MD; Lincoln, NE
Spencer Hansen, MD, RPVI, FACS; Fort Collins, CO
Charles Alan Hartranft DO; Grove City OH
Katherine Hekman, MD; Decatur, GA
Anne Henderson, MD; Phoenix, AZ
Brian Hoang, MD; Phoenix, AZ
Jessica Louise Hogan, MD; Shawnee, KS
Samuel Hoh-Yan Hui, MD; Bay City, MI
James Iannuzzi MD MPH; San Francisco CA
Sashi Inkollu, MD; Morgantown, WV
Sina Iranmanesh, MD; Plymouth, MA
Jeremy Irvan, MD; Danville, PA
Arsalla Islam, MD; Fort Worth, TX
Ashish Kumar Jain, MD; Charlotte, NC
Angela Jellison, MD; Woburn, MA
Brandt Jones, MD; Lutz, FL
Benjamin C Jordan, MD; Waunakee, WI
Bruce Tjaden, Jr , MD; Gladwyne, PA
Dejah Judelson, MD, FACS; Worcester, MA
Kalenda Kasangana MD; Little Rock AR
Pamela Sue Kim, MD; Burlington, MA
Alison Kinning, MD; Holly, MI
Jordan P Knepper, MD; South Lyon, MI
Emilia Król, MD; Greenville, SC
Lucy Kupersmith, MD; Annapolis, MD
Mimmie Kwong MD; Sacramento CA
Emily Lagergren, MD; Kennesaw, GA
Anthony Lewis, MD; Lewisburg, PA
Xiaoyi Li, MD; Mesa, AZ
Ruby Lo, MD; Scotts Valley, CA
Kira N Long, MD; Seabeck, WA
Tony Lu MD; Pearland TX
George Makkar, MD; Van Nuys, CA
Rori Mankins, MD; West Des Moines, IA
Neel Mansukhani, MD; Chicago, IL
Chris McAninch, MD; Minneapolis, MN
Graeme E McFarland, MD; Decatur, AL
Sara McKeever DO; Tucson AZ
Spyridon Monastiriotis, MD, MsC; Memphis, TN
Melissa Meghpara, DO; Alexandria, VA
Bernardo Mendes, MD; Rochester, MN
Esther Mihindu, DO; Dallas, TX
Dimitrios Miserlis MD; San Antonio TX
Christopher Mitromaras, MD; Davidson, NC
Abid Mogannam, MD; San Leandro, CA
Jonathan Morrison, MD; Baltimore, MA
Robert Moskowitz, DO; Albuquerque, NM
Zack Nash, MD; San Antonio, TX
Derek Nathan MD; Mercer Island WA
John Chalmers Neill, MD; Tupelo, MS
Daiva Nevidomskyte, MD; Federal Way, WA
Khanh Nguyen, MD; Portland, OR
Tammy Nguyen, MD; Worcseter, MA
Sonya Noor, MD; Amherst, NY
Vincent Noori MD; Finksburg MD
Patrick O'Brien, MD; Missoula, MT
Babatunde Oriowe, MD; Toledo, OH
Niraj Parikh, MD; Gainesville, GA
Rajavi Parikh, DO; Tampa, FL
Jigarkumar Patel, MD; Apex, NC
Hao Duy Pham MD; Richlands VA
David Phang, MD; Clarks Summit, PA
Steven Pike, MD; Lafayette, LA
Grayson Pitcher, MD; Pittsford, NY
Sherazuddin Qureshi, MD, RPVI, FACS; Winfield, IL
Andre R Ramdon, MD; Yeadon, PA
Christopher Ramos, MD; Atlanta, GA
Khurram Rasheed MD; Abu Dhabi United Arab Emirates
Jonathan Ratcliff, MD; Gig Harbor, WA
Nanette Reed, MD; Webster Groves, MO
Thomas Reeve, MD; Carrollton, GA
Margaret Rigamer, MD; Chicago, IL
Anthony Rios, MD, RPVI, FACS; Denton, TX
Elsie Ross MD; Palo Alto CA
Taimur Saleem, MD; Brandon, MS
Karim Salem, MD; Pittsburgh, PA
Joseph Salfity, MD; Cincinnati, OH
Edward Samourjian, MD; Tarzana, CA
Luis Sanchez MD; Saint Louis MO
Vincent Joseph Santo, MD; Portland, OR
Manuela Schuksz, MD PhD; Hampton, VA
Jocelyn Segall, MD; Lake Oswego, OR
Indrani Sen, MBBS; Eau Claire, WI
Michael David Sgroi, MD; Los Altos, CA
Christine Shokrzadeh MD; League City TX
Thomas Shuster, DO; Grand Blanc, MI
Justin Simmons, DO; Coopersville, MI
Allie Sohn, MD; Roca, NE
Kevin Southerland, MD; Durham, NC
Jeffrey Stein, MD, FACS; San Antonio, TX
Samantha Neureuther Stradleigh MD; Roseville CA
Adam Strickland, MD; Charlotte, NC
Luis Suarez, MD; Chestnut Hill, MA
Abhishek Sundaram, MD; Grafton, WI
Hamed Taheri, MD; Long Beach, CA
Mohamed Takki Momin, MD, FACS; Stone Mountain, GA
Tiziano Tallarita MD; Eau Claire WI
Anjan Talukdar, MD; Omaha, NE
Yauhen Alexander Tarbunou, MD; Woodbury, MN
Anan Tawil, MBBS; Salem, OR
Jonathan Robert Thompson, MD; Omaha, NE
Brian Tiu, MD; Temecula, CA
Eric Benjamin Trestman MD; Houston TX
Huong Truong, MD; New Brunswick, NJ
Claudiu Adrian Vlada, MB BCh; Clackamas, OR
Juan Velazquez, MD; Newark, NJ
Aaron Wagner, MD; Davie, FL
Ali Wait MD; Scottsdale AZ
Christopher Washington, MD; Denver, CO
J Devin B Watson, MD; Ocean Springs, MS
Dustin Weiss, MD; Sioux Falls, SD
Chris Werter, MD; Fleetwood, PA
Greg Westin, MD; Indianapolis, IN
Jacob Wood MD; Chapel Hill NC
Halim Yammine, MD; Charlotte, NC
Andrew Yang, MD; Powell, OH
Sung Yang, MD; Cincinnati, OH
Christopher Yi, MD; Irvine, CA
William J Yoon, MD; Cleveland, OH
Dustin Yoon MD; Germantown MD
Shariq Adeel Zaidi, MD; League City, TX
Sara Zettervall, MD; Edmonds, WA
Charlena Alfonsi, MSN, BC-AGACNP, RNFA; Youngtown, OH
Megan Azadian, PA-C; Bedford, NH
Britni Barnes PA-C; Baltimore MD
Lauren Blanchard, PA-C; Toledo, OH
Maria Capitano, PA-C; Scranton, PA
SVS membership is widely recognized in the vascular community as a mark of professional achievement. See vascular.org/join for more information and to apply.


David Conn, PA-C; DuBois, PA
Hgech "Kia" Ear, PA-C; East Norriton, PA
Jeena Fuller, PA-C; Grand Junction, CO
Michelle Gonzalez, PA-C; DuBois, PA
Jill Hinkle ACNP-BC; Loveland CO
Coty Holm, PA-C; Missoula, MO
Megan Holmes-Nusz, PA-C; Lincoln, NE
Colby Horton, PA-C; Hagerstown, MD
Andi Hudson, MPAS, PA-C; Temple, TX
Renee Issacs, PA-C; Pittsfield, MA
Lindsey Jones PA-C; Charlottesville VA
Kimberly Kedenburg, MSPT, DPT; Jamesville, NY
Ga-Young Kelly Suh, PhD; Long Beach, CA
Stephanie Leasure, FNP; Mathews, NC
Tina Mindich, PA-C; Baltimore, MD
Alexa Paley, PA-C; Omaha, NE
Heather Perné NP-C; Toledo OH
Yael Porat, PhD; Netanya, Israel
Bryant Reinking, PA-C; Colorado Springs, CO
Alyse Rettura, PA-C; Greensburg, PA
Danielle Rose, PA-C; Flint, MI
Pauline Salguero, PA-C; Lynwood, CA
Evan Schulz MMS PA-C; Philadelphia PA
Tomas Scoleri, PA-C; Twin Falls, ID
Cheryl Shannon, NP; Corvallis, OR
Rhonda Shulaw, ACNP-BC; Charlottesville, VA
Danielle Vesth, PA-C; Grand Junction, CO
Katherine Wald PA-C RVT RDMS; Columbus OH
Cynthia Washington, DNP, FNP, RN; Richmond, VA
Brittany Williams, PA-C; St Louis, MO
Michael Zugarek, PA-C; Hampton, VA
Larry Horesh MD; Savannah GA
Gaurav Parmar, MPH; East Boston, MA
Yusmila Bouza, MD; Municipio Cerro, La Habana
Daniel Carregal, MD; Divinópolis, Brazil
Hernán Di Tomaso Mesa, MD; Mercedes, Argentine
Andres Dominguez MD; Colombia
Josefina Duque Goicochea, MD; Acapulco, Mexico
Diego Ferreira, MD; Colombia
Shantonu Ghosh, MD; Dhaka, Bangladesh
Rodrigo Lozano-Corona, MD; Mexico City, Mexico
Cesar Medina Suarez, MD; Bogota, OTH
Keisuke Miyake, MD; Ashiya, Japan
German Munive, MD; Colombia
Ricardo Padilla, MD; Ciudad Juárez, Mexico
Hung Phan, MD; Hochiminh,
Nihar Pradhan, MD; Hyderabad, India
Natalia Reinosa MD; Colombia
Lukas Rios, MD; Colombia
Ruben Rodrigez, MD; Zapopan, Mexico
Jorge Ulloa, MD; Bogota, Colombia
Himanshu Verma, MBBS; Gurugram, India
Fausto Julián Virgen Barrón, MD; Tampico, Mexico


The number of office-based facilities has been increasing steadily over the past several years—and more vascular surgeons may be considering becoming involved in operating such centers, reports Beth Bales.
TO HELP VASCULAR SURGEONS CONSIDER THE various details involved, the SVS Subsection on Outpatient and Office Vascular Care (SOOVC) held a special membership section session on The Business of Running an OBL (office-based lab) during VAM 2023 in June.
Among the standout presentations included, Neil Poulsen, MD, from Cardiovascular Care Group in Springfield, New Jersey, delivered a talk entitled “The financial viability of the OBL” during the session.
Top of mind, the number of office-based facilities increased 49% from 2002–2012, he told those gathered. OBLs provide ease and access to care, improved patient satisfaction, and excellent outcomes; they limit hospital exposure; and they increase efficiency, Poulsen pointed out.
In light of recent coverage of overuse of certain procedures, Poulsen said, his presentation assumed “appropriate use by trustworthy/ethical practitioners practicing evidence-based medicine.”
In terms of financial viability, the first step is to identify the three stakeholders: the patients, practitioners and the overall medical system, he continued. “If one is out of balance, the whole system falls apart,” Poulsen said.

As for safety, he cited research showing that among 6,021 procedures in a particular OBL, there were no office-based mortalities, major bleeds, acute limb losses, myocardial infractions, strokes or hospital transfers within 72 hours, and a 0.5% rate of minor complications. “We do
have the evidence that use of OBLs is equal to procedures performed in hospitals,” Poulsen said.
As far as providers, an OBL practice can offset continuing declines in the professional fees for vascular interventions, allow for a more patient-centered practice model, avoid the headaches of dealing with operating room turnovers and access to block time as well as hospital policies, allow for referrals that may have gone to competing practices, and provide a new and increased revenue stream for the vascular practice.
Research from 2020 highlighted 2017 fees for certain procedures, including a balloon angioplasty for which the physician was reimbursed $482. The hospital reimbursement was $4,592, but the provider in the outpatient facility received not only $482 in physician reimbursement but also $2,288 for the facility reimbursement, for a total of $2,770.
compared to $368,897 for the provider reimbursement alone. Of course, revenues must be weighted against the increased responsibility of owning and operating an OBL, he said, with set-up and building costs that could reach $500,000 to $1 million. Other costs involve investors, staffing, supplies and acquiring patients.
The healthcare system as a whole saves money as well. The success of the outpatient practice model is directly related to its ability to provide high-quality patient care while reducing waste spending, and the transition also helps to conserve hospital and inpatient resources, Poulsen said.
Data from his own group showing 1,741 procedures in a single OBL over 12 months showed hospitalbased fees of $2.9 million and OBL fees of nearly $2.5 million. The Medicare system saved $462,443, or 18%, he said. Highlighting code 36902 (fistulagram with percutaneous transluminal angioplasty [PTA]), with 443 performed in a year the medical system saved 38% by having the procedures performed in an OBL.
His group realized increased revenues of $2,453,652, compared to $376,199 for the hospital-based procedures.
from 2002-2012
Other research showed significantly increased revenues in one center, with physician reimbursement for a thrombectomy in an outpatient setting nearly quadruple that performed in a hospital. “In 12 months of procedures in [this] OBL, revenues increased approximately $1.3 million,” he said. Total reimbursements for a group of procedures (with both the provider and facility fees) was nearly $1.7 million,
Jack Cronenwett, MD, announced the recipients of the second-year scholarship that bears his name.
Poulsen concluded by stating that the success or failure of an OBL depends on optimizing outcomes for all stakeholders. OBLs provide a safe, efficient and effective environment for patient care, he continued, and the transition of care from the hospital setting to the OBL is associated with a significant reduction in overall healthcare costs. The financial success of an OBL is driven by the ability to limit expenses while providing highquality, safe and evidence-based patient care, Poulsen added.
“You’ll note I didn’t say anything about improving revenue,” he told attendees. “The revenue is going to come,” Poulsen emphasized. “Don’t go out of your way to improve revenue only. You want to limit your costs and provide appropriate patient care.”
Scholarships are awarded in either the research or quality categories.
THE VASCULAR QUALITY INITIATIVE (VQI) Fellows in Training (FIT) program is a success, say leaders as they provided a oneyear review.
FIT introduces residents and fellows in vascular surgery and medicine to the SVS Patient Safety Organization (PSO). Fellows worked closely with their mentors to participate in VQI regional meetings. They also participated in quality charter development, the quality improvement process and research initiatives using VQI data. FIT is run in collaboration with the Association of Program Directors in Vascular Surgery (APDVS).
Adam Johnson, MD, a vascular surgeon at Duke Health in Durham, North Carolina, briefly reviewed the first year of the program during the recent VQI Annual Meeting in June. During the session, founding VQI Medical Director
Year one included 16 mentors and 16 fellows representing 10 of the VQI’s 18 regions, said Johnson. Over the year, the fellows have submitted projects to research advisory committees, with refinement following review and data analysis. Some of the projects were included in the poster presentations at the annual meeting. Mentors were “very satisfied” with the projects overall, and trainees were “very or somewhat satisfied” with the program, Johnson said.
Leaders added virtual meetings, to which mentors will be added this coming year; formalized the curriculum and made it more readily available; and helped provide local leadership in the aftermath of a few mentor changes. For year two, organizers will promote engagement via presentations by fellows at regional meetings, he said.
The five scholarship winners will continue work with the program, receiving individual funding to continue their research and/or work more closely with VQI staff and committees.
For 2023–24, the FIT fellows and mentors in the quality category are: Hanna Dakour Aridi, MD, from Indiana University Health-Methodist in Indianapolis— mentored by Michael Murphy, MD— who has studied postoperative day-one discharge, which is used as a quality-of-care indicator after carotid revascularization. Her project involved reviewing records of 122,560 elective carotid interventions in the VQI to identify drivers of increased length of stay.
Christine Kariya, MD, from the University of Vermont Medical Center in Burlington, Vermont—mentored by Danny Bertges, MD—is working to incorporate patient-reported outcome measures (PROMs) into the electronic medical record (EMR) and VQI registries.
In the research category, Caronae Howell, MD, from University of Utah Hospital and Clinics/The University of Arizona—who is mentored by Benjamin Brooks, MD—is
studying racial and ethnic disparities in revascularization options for chronic limbthreatening ischemia (CLTI), with a study designed to compare anatomic patterns of disease and limb-salvage outcomes among patients from racial and ethnic groups undergoing first-time revascularization for lower-extremity CLTI.
Brianna Krafcik, MD (mentor Phil Goodney, MD), from Dartmouth Hitchcock Medical Center in Lebanon, New Hampshire, is using the carotid endarterectomy and carotid stenting VQI modules to compare indirect quality-of-life measures such as length of stay, new neurologic events, frailty, and new medications between carotid endarterectomy and transcarotid artery revascularization (TCAR).
Lastly, Ben Li, MD, from Toronto General Hospital in Toronto, Canada— mentored by Graham Roche-Nagle, MD— is developing machine learning algorithms to predict outcomes following major vascular surgery using the VQI database. He used VQI data to develop robust machine-learning models that accurately predict outcomes following carotid endarterectomy.—Beth
BalesVQI FELLOWS IN TRAINING PROGRAM MARKS ONE YEAR
QUALITY
OBL GROWTH OF 49%
AS A VASCULAR SURGERY TRAINEE, there are multiple aspects of vascular surgery that I’ve had the opportunity to learn about. And to be honest, I’m still learning.
To that end, the SVS has put a great deal of effort in providing multiple opportunities to supplement our formal curriculum and cater to various academic and clinical interests through a number of short courses or fellowships. As trainees, I find that these are invaluable to fill gaps in the curriculum that may not exist at individual institutes.
In this issue of Vascular Specialist, the SVS VQI Fellowship-In-Training (FIT) program is highlighted. This program was developed to support the curation of a
cadre of trainees (general surgery, vascular surgery, cardiology, etc.) in the scientific pursuit of analysis of clinical data. I imagine that this pipeline of fellows will be important to shaping future policy in the world of vascular surgery.
Another program supported by the SVS and aimed towards trainees is the Journal of Vascular Surgery (JVS) internship now in its third year. This program is developing a pipeline of conscientious reviewers who will bring a diverse and nuanced approach to journal manuscript reviews to elevate the quality of work published in the JVS journals.
Interested in the business of vascular surgery—including how coding, reimbursements and policy are intertwined? Then the annual SVS Coding
WELCOME BACK TO GOVERNMENT GRAND
Rounds, a campaign aimed at expanding vascular surgeons’ understanding of—and comfort with—the SVS’ many advocacy tools. In the dynamic landscape of healthcare, the promotion of positive change and the advancement of our profession require more than just clinical expertise.
As highlighted throughout this campaign, advocacy plays a critical role in shaping the future of vascular surgery. By focusing on grassroots activations and leveraging the power of our collective voice, we can promote essential initiatives and drive impactful change.
The SVS is currently promoting five pivotal bills. By rallying behind these legislative initiatives, we can pave the way for transformative improvements in patient care and the landscape of vascular care. Together, we can use our power to promote and champion these crucial bills.
● H.R. 3674, the Providing Relief and Stability for Medicare Patients Act
- Legislation to increase the non-facility/office-based practice expense relative value units negatively impacted by the Centers for Medicare & Medicaid Services’ clinical labor policy for the next two years
& Reimbursement Workshop is for you. This 1.5-day course provides an extensive review of coding and critical updates. In addition to becoming savvy in coding and billing for cases/procedures, it helps to shine a light on the importance of policy reforms that affect billing codes and reimbursements for vascular surgery services.
But academic pursuits are not the only domain where the SVS has developed programming. In this issue, there is a highlight on the Complex Peripheral Vascular Intervention (CPVI) Skills Course in which participants will be exposed to didactic and hands-on-training on the innovative aspects of interventions for peripheral arterial disease (PAD), including endovascular, open and hybrid options. This is a course for vascular surgeons, developed by vascular surgeons. It’s a quick two-day course at the SVS office headquarters.
Another course with a similar flavor, although not formally supported by the SVS, is the Advanced Practical Exposures in Vascular Surgery (APEX) held at the St. Louis University hospital every fall. This course provides an invaluable hands-on
● H.R. 2474, the Strengthening Medicare for Patients and Providers Act
- Legislation to provide annual inflationary updates, based on the Medicare Economic Index, for Medicare physician services, similar to updates received by other healthcare providers
● H.R. 1202/S. 704, the Resident Education Deferred Interest (REDI) Act
- Legislation to allow borrowers in medical or dental internships or residency programs to defer student loan payments without interest until the completion of their programs
● H.R. 2389/S. 1302, the Resident Physician Shortage Reduction Act
- Legislation to provide 14,000 new Medicaresupported graduate medical education positions over seven years
● H.R. 731/S. 220, the Workforce Mobility Act
- Legislation to free physicians from non-competes (except in limited circumstances), providing them with an option to work for a competitor and/or more easily transition from one practice type to another
These opportunities serve as catalysts for change and empower vascular surgeons to actively promote their profession.
By leveraging these avenues, SVS members can play a pivotal role in shaping policies, driving awareness, and elevating
experience to less commonly encountered exposures in the neck, chest, abdomen and lower extremities. The highlight of the course is the “How I Do It” didactic sessions prior to the cadaver exercises. And of course, there is the UCLA/SVS course that provides a comprehensive review of vascular surgical techniques. Held every August in Los Angeles, this three-day course is invaluable to the graduating vascular trainee and is often subsidized for trainee attendance.
In addition, there are multiple opportunities to engage in courses offered through the likes of local regional societies and VAM. If there were any course I’d like to see developed, it is one that focuses on vascular trauma. I think that could be helpful to identify best practices for this vulnerable patient population. Nevertheless, as a trainee, I’m glad that these opportunities exist to plug knowledge gaps that exist in every program—and I hope that you too are able to partake in some of these courses.
CHRISTOPHER AUDU is the Vascular Specialist resident/fellow editor. He is an integrated vascular surgery resident at the University of Michigan in Ann Arbor, Michigan.

the vascular specialty. To promote these bills, head to vascular.org/advocacy/grassroots-advocacy and send messages to specific lawmakers. Interested in learning more? Staying informed is of paramount importance in the realm of advocacy, and the SVS’ DC Update newsletter serves as a vital resource for vascular surgeons who are passionate about driving change.
This monthly newsletter provides a comprehensive and timely overview of legislative developments, policy updates, and advocacy opportunities, empowering surgeons to stay at the forefront of the advocacy landscape.

Members who have not received the DC Update newsletter because of preferences they have set in the communications database can send an email to membership@vascularsociety.org for help.
ANDREW KENNEY is a member of the SVS’ Washington, D.C. office.
Empowering vascular surgery to promote five pivotal healthcare bills
By Andrew Kenney
“If there is any course I’d like to see developed, it is one that focuses on vascular trauma”By Megan Marcinko
The Centers for Medicare & Medicaid Services (CMS) in mid-July released two payment-related proposed rules— the highly-anticipated calendar year (CY) 2024 Medicare Physician Fee Schedule Proposed Rule (MPFS) and the Medicare Hospital Outpatient Prospective Payment System (OPPS) and Ambulatory Surgical Center (ASC) Payment System Proposed Rule. The SVS will submit comments for both proposed rules by the Sept. 11 due date.
For CY2024, CMS has proposed a conversion factor—a critical component for calculating Medicare payments—of $32.75, a decrease of approximately 3.4% from the CY2023 conversion factor. Preliminary SVS analysis, in addition to the impact charts provided in the proposed rule by CMS, indicate that vascular surgeons, depending on practice setting, face a 3–4% cut based on current Medicare policies proposed in the MPFS rule.
These cuts result from a reduction in the temporary update to the conversion factor under current law and a negative budget neutrality adjustment, stemming in large part from CMS moving forward with implementation of separate pay-
ment for add-on code G2211 to account for visit complexity associated with certain office/outpatient evaluation and management care. G2211 was initially proposed three years ago, but implementation was delayed as a result of an aggressive advocacy campaign led by the surgical societies, including the SVS.
In addition, payment reductions for many vascular surgeons are compounded by the third year of CMS’ phased-in implementation of its clinical labor pricing update, which was finalized in the CY2022 MPFS Final Rule.
CMS is proposing an update to OPPS for hospitals that meet the quality reporting requirements by 2.8%. The update is based on the projected inpatient hospital market basket percentage increase of 3%, reduced by a 0.2 percentage point for productivity adjustment.
The SVS is aware of the significance of the policies outlined in these rules—particularly the additional Medicare payment reductions vascular surgeons face and the potential impacts on patient care and access.

There is broad agreement thats the Medicare physician payment system is broken and that physicians/surgeons are reeling due to yearly budget neutrality adjustments and the fact that the MPFS is the only fee sched ule lacking an annual inflationary update.
The SVS, in collaboration with medical specialty societies, is continuing to work to mitigate the scheduled cuts and advance policies to stabilize the payment system in the short term and reform the system in the long term.

To that end, the SVS supports legislation to provide an inflationary update for the MPFS (H.R. 2474) and is leading the effort that brought forth the introduction of legislation to provide targeted relief for codes most impacted by the clinical labor update policy (H.R. 3674). The SVS will also seek further delay of the G2211 code implementation via the comment period on the rule, and legislative relief with an additional delay. Visit the SVS Advocacy Center to urge your lawmakers to support these important bills.
The SVS is analyzing both rules and will submit extensive comments to CMS. In addition, the Society will continue to collaborate with other surgical and medical specialty societies to amplify our message on Capitol Hill for Congress to address these cuts before the end of the year.

The SVS is also working in earnest to identify long-term solutions that will provide stability and equity across the Medicare physician payment system. SVS members should be prepared to engage in these ongoing advocacy efforts through the remainder of the year.
MEGAN MARCINKO is SVS director of advocacy.CMS: Proposed reduced conversion factor would cut vascular surgeon reimbursements
“ There is broad agreement that the Medicare physician payment system is broken and physicians are reeling due to yearly budget neutrality adjustments”

recanalization, angioplasty, atherectomy and other treatment options for extensive atherosclerosis, McDevitt and Kashyap explained.
Due to limited space, the faculty advise early registration to guarantee participation. McDevitt noted that the faculty encourages close interaction between participants and instructors and that they had received positive feedback from last year’s inaugural course.
This model will be repeated, allowing participants to acquire and demonstrate new skills through simulation-based learning.
used. This is important because it benefits the patients who can be treated with less invasive approaches.”
The skills course will offer up to eight AMA PRA Category 1 Credit(s). Times are 7:30 a.m.–5:30 p.m. Oct. 1, and from 7:30 a.m.–4 p.m. Oct. 2.
Kashyap is excited about the upcoming course. “Not only is this course intended to showcase our capabilities, but also to guide us on what we should do, not just what we can do. The experienced faculty will highlight the appropriate techniques for specific patient presentations, making it a valuable learning experience.”
enhance their skills in complex peripheral vascular interventions (CPVI) can register for an upcoming in-person course offered by the SVS in order to better equip themselves for the changing landscape of endovascular treatment. The CPVI Skills Course will take place Oct. 1–2 at the OLC Education and Conference Center at SVS headquarters, 9400 W. Higgins Road, Rosemont, Illinois.
At its heart, the course aims to teach vascular specialists the latest innovations in new devices and techniques in the field of peripheral vascular surgery and intervention. Participants will have the opportunity to engage in a combination of didactic and case-based presentations that will enable them to delve into the intricacies of the field, said course co-directors Daniel McDevitt, MD, and Vikram Kashyap, MD.
Attendees will gain hands-on experience using cadavers and benchtop models during small-group simulations. This practical component will allow participants to apply novel and advanced endovascular technologies for long-segment
The second edition of a popular trainee-created textbook primarily aimed at trainees taking the Vascular Surgery In-Training Exam (VSITE) has hit the shelves.
The Vascular Surgery Review Book, authored by Thomas Creeden, DO, a resident from the University of Massachusetts in Worcester, Massachusetts, was first released a year ago and quickly saw soaring sales.
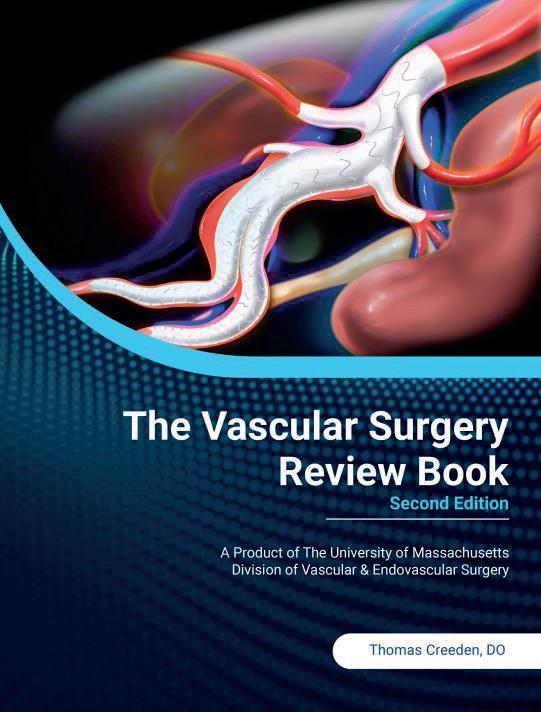
The latest edition features updates on technical steps for the majority of routine vascular surgery procedures—including bailout techniques—as well as detailed descriptions and explanations of sizing/designing of custom fenestrated and branched aortic grafts.
Also new are summaries of high-yield societal guidelines, new chapters covering areas such as ascending aortic management and distal lower-extremity bypass, and a section on the recently published results from landmark chronic limb-threatening ischemia (CLTI) trials, BEST-CLI and BASIL-2.
Late last year, as sales soared, Creeden told of how the textbook had also reached many medical students, vascular surgery interest groups (VSIGs), and even those
“Usually, because these courses are relatively intimate, the course size is limited so that everybody has a chance to speak with the faculty, and the faculty can speak to the attendees,” said McDevitt. “After the course, if people have questions or comments, they can email the faculty and create long-term connections to establish more than just a casual relationship,” he said.
Key objectives of the course include a comprehensive review of recent innovative treatments for peripheral arterial disease (PAD). According to Kashyap, because of the swiftness with which advancements ensue in the field, medical professionals must keep themselves updated with the latest techniques and technologies.

“We can’t stop learning at the end of our train ing,” said Kashyap. “Continued education and re finement of practice are true for every field, and I am proud to say it has been a hallmark of vascular surgery.
By Marlén Gomez Vikram KashyapFor more information and to register, visit vascular.org/CPVI23

“We’ve had a revolution, going from only an open surgical practice to one where both open and endovascular techniques are
The Journal of Vascular Surgery (JVS) and JVS-Vascular and Lymphatic Disorders (JVS-VL) editors have identified the free-access articles from each publication for the month of September issues, reports Beth Bales.
best surgical therapy in patients with CLI] trial,” vascular.org/JVS0923MedManagementinBESTCLI
4. “Prevalence of intracranial aneurysms in Marfan syndrome,” vascular.org/ JVS0923-MarfanSyndrome (continuing medical education [CME])
From JVS-VL:
1. “Race, gender and socioeconomic disparities affect the clinical stage of patients presenting for treatment of superficial venous disease,” vascular. org/JVSVL0923-DisparitiesAffectClinicalStage
operating in the device industry. By December, the title had registered as one of the top-selling books on Amazon within the vascular and thoracic surgery category, with copies selling in 14 countries, he detailed.
Creeden’s original driving force was to create a high-yield reference text that would be fundamentally easier and quicker to work through than traditional vascular surgery textbooks—which can run thousands of pages long—when preparing for the VSITE, along with exams such as the vascular boards.— Bryan Kay
From JVS:
1. “Impact of Medicaid expansion on outcomes after abdominal aortic aneurysm repair,” vascular.org/ JVS0923-MedicaidExpansionAAA (This paper features on the Audible Bleeding podcast, an SVS media outlet)
2. “Low-volume surgeons can have better outcomes at certain hospital settings for open abdominal aortic repairs,” vascular. org/JVS0923-openAAAOutcomes (Editor’s Choice)
3. “Baseline modern medical management in the BEST-CLI [Best endovascular vs.
2. “Black or African American patients undergo great saphenous vein ablation procedures for advanced venous disease and have the least improvement in their symptoms after these procedures,” vascular.org/JVSVL0923-VeinAblation (CME)
3. “Comparison of outcomes following polidocanol microfoam and radiofrequency ablation of incompetent thigh great and accessory saphenous veins,” vascular. org/JVSVL0923-OutcomesComparison
4. “Surgical and endovascular treatment of pelvic venous disorder: Results of a multicenter retrospective cohort study,” vascular.org/JVSVL0923-PelvicVenousDisorder (Editor’s Choice)
“We’ve had a revolution going from only an open surgical practice to one where both open and endovascular techniques are used. This is important because it benefits the patients who can be treated in with less invasive approaches”
VIKRAM KASHYAP
The SVS will host the SVS Coding and Reimbursement Workshop this fall, providing a comprehensive program designed to equip vascular surgeons and their support staff with essential knowledge and competence in appropriate billing and coding procedures.
Over the course of the workshop, scheduled for Oct. 16–17, attendees will receive a review of coding practices, recent changes to the current procedural terminology (CPT) and Medicare, the proper application of modifiers for streamlined reimbursement, and the impact of Medicare’s Global Surgical Package on billing and reimbursement.
Workshop director Sean Roddy, MD, provided an overview of what attendees can anticipate during the workshop, which includes an optional half-day workshop on evaluation and management (E&M) codes. The workshop will address the
intricate and distinctive aspects of vascular sur gery coding that distinguish it from other medical specialties.
“Vascular surgery has some nuances that are different from other specialties, and it is important to get the vascular lab coding correct for the ultrasounds and procedures. Endovascular procedures can be confusing on what codes you bill, so we try to clarify that with examples,” said Roddy.
Sean RoddyParticipants can expect to receive the most up-to-date information di rectly from vascular surgeons who are deeply involved in the creation and valuation of codes, ensuring the most accurate and reliable recommendations. Roddy emphasized the significance of this educational event, highlighting the direct impact Medicare has on the specialty.

“We have decreasing revenue from Medicare, which uniquely impacts vascular surgeons since up to 70% of our patient population has Medicare. Accurate coding and good

documentation are crucial to optimizing our revenue for all payers, reducing denials, optimizing accounts receivable, and increasing our revenue,” said Roddy. The workshop demonstrates SVS’ commitment to empowering medical professionals with the tools they need to provide the highest quality of care possible, according to Roddy.
Medical professionals interested in attending the educational course are encouraged to register early.
It will be held at the OLC Education and Conference Center at SVS headquarters, 9400 W. Higgins Road in Rosemont, Illinois.
It is designed for vascular surgeons and their office staff, including practice managers, nurse practitioners, physician assistants, nurses, surgery schedulers, coders, and others who seek to improve and expand their knowledge of accurate coding and reimbursement for vascular surgery.
Course leaders point out the event is ideal for vascular trainees and surgeons as the level of the content is intermediate to advanced.
Attendees can earn a maximum of 3.75 AMA PRA Category 1 Credit(s) for the optional evaluation and management (E&M) coding workshop and 10.00 AMA PRA Category 1 Credit(s) for the Coding and Reimbursement Workshop.
The optional workshop will be held from 8 a.m.–12 p.m. Oct. 16, while the main workshop sessions will follow from 1–5 p.m. the same day and from 7:30 a.m.–4:30 p.m. on Oct. 17.
More information about the courses and the preliminary agenda vascular.org/coding23.




“Accurate coding and good documentation are crucial to optimizing our revenue for all payers, reducing denials, optimizing accounts receivable, and increasing our revenue”
SEPTEMBER’S VASCULAR HEALTH STEP
Challenge is fast-approaching, and SVS members are preparing to step up to meet it.
The challenge benefits the SVS Foundation, which asks people to walk 60 miles—representing the 60,000 miles of blood vessels in the human body—throughout September. Funds raised will help the Foundation amplify the importance of vascular health while also promoting healthy vascular health habits throughout the country.
Participants all receive a Step Challenge T-shirt and can walk individually or as part of a team. Those who register by Aug. 5 will receive their T-shirts by Sept. 1, the start of the campaign.
September is National Peripheral Arterial Disease (PAD) Awareness Month, making it the perfect time to highlight the benefits of walking and overall vascular health. Walking is a front-line therapy for PAD, a chronic disease in which plaque builds up in the arteries to the legs. Vascular surgeons deal with PAD routinely and, thus, are the perfect advocates for walking, said SVS Foundation
Their parents are heroes, say the children of Ali AbuRahma, MD, Bernadette Aulivola, MD, Matthew Eagleton, MD, Jason T. Lee, MD, and Palma Shaw, MD. “The next generation of women in vascular surgery are my heroes,” said Shaw. “The SVS Foundation has done so much to help fund women like me people as we pave the way for the future of vascular surgery.”
Vivian Ho, MD, is a hero to her parents and extended family, including her grandparents who left South Vietnam in search of a better future for their children. When Ho realized her dream of becoming a vascular surgeon, her father said, “They recognized all their sacrifices had been vindicated.”
These contributions featured as part of one of the most heart-warming moments of the SVS Foundation Great Gatsby Gala in June: the airing of the Vascular Heroes video, where loved ones delivered messages to the vascular heroes in their lives. “She saves people’s lives,” said Shaw’s children.
Chair Michael Dalsing, MD. And, as vascular surgeons are, by nature, highly competitive, they’re typically up for such a challenge.
For example, in asking several of 2022’s top fundraisers why they put their shoes to pavement last year, answers included the importance of walking—and beating another surgeon.

Adam Beck, MD, walked and donated for two reasons, he said: “To support the SVS and to try to encourage others to walk as well through competition and to beat Dr. [Leigh Ann] O’Banion.” He noted, “(I lost, no surprise).”
O’Banion, who walked as part of “Team FAB,” laughed at his response, saying her two reasons were: “I am committed to advancing the care of patients with PAD in disadvantaged and rural patient populations, and I am the most competitive person ever and was so proud to be part of a FABulous group of surgeons who kicked some butt!”
O’Banion’s 27-member team raised the most funds, a healthy $12,970.
Said Jesus Matos, MD: “I walked and donated because I wanted to be a role model to all of our patients. Exercise is the most powerful medicine for all chronic illnesses and the best predictor of longevity,” he said, adding, “Walk with me, 2023.”
Laurel Hastings, MD, was also part of “Team FAB.” “I walked to support programs that fund community outreach, bringing awareness to PAD, and to give Leigh Ann O’Banion a formidable competitor,” she said, adding with a smile emoji, “See fundraising results please.” (Let
AbuRahma’s son, Zachary AbuRahma, MD, himself now a vascular surgeon, remembers his dad’s dedication, the hard work that went into every day. Ali AbuRahma is his hero, said Zachary.
“You’re all heroes to me,” declared Eagleton, SVS president-elect. “The difference you make is immeasurable and I truly cannot thank you enough for being a part of the SVS Family. The SVS Foundation arms heroes like you with the resources you need to continue to save and enrich and save lives. Your generosity makes a difference. Join us and together we can truly fund the future.”
The video is available at vascular. org/HeroVideo. The end includes a blooper reel, including siblings asking each other questions such as, “What is it that Dad actually does?”—Beth Bales

the record show she was the top individual fund-raiser, beating O’Banion by $60.)
Surgeons are undoubtedly planning their competitions for this year.
The Vascular Step Health Challenge entry fee is $60. New this year is a “pay -it-forward” registration to help cover the participation fee for low-income vascular patients.

The program takes place on the Charity Footprints platform. During registration, participants can link their fitness tracker to the platform to automatically log steps throughout the month of September. Eligible trackers are Apple Watch, Fitbit, Garmin, Google Fit, Misfit and Strava. Those people who don’t have eligible trackers can enter their steps manually, or connect via their smartphone.
Pay-it-forward participants, as of July 20, are: James Persky, Edward Gifford, Bethany Slater, Yong Daniel, Kate Shuman, Rhuseet Patel, Kimberly Thomas, William Shutze, Kathryn Bowser, Dejah Judelson, Simpledeep Banipal and Bill Maloney.
ORGANIZERS OF VAM 2024 WANT MEMBERS TO CONSIDER WHAT THE MODERN-DAY vascular surgeon needs to know for optimal patient care and professional success. What’s the latest in the venous disease space? What are helpful tips and tricks in open surgery and endovascular intervention? How about new information on in the world of peripheral arterial disease (PAD)? What are the optimal practice management strategies?
The SVS Postgraduate Education Committee (PGEC) is requesting proposals for Educational Sessions for VAM 2024. All proposals for the 2024 meeting are welcome and must be submitted by Aug. 23. Those whose proposals are selected for inclusion in the VAM program will be expected to collaborate with the PGEC on the development and delivery of the proposed sessions, and then co-moderate the session at VAM 2024, which takes place June 19–22, 2024, in Chicago, with educational sessions spread over all four days.
“Each and every year, we want VAM to deliver the most cutting-edge, innovative, high-impact information to address the patient care and professional needs of those who care for vascular disease,” said PGEC Chair William Robinson, MD.
“To do this, we need to mobilize the considerable enthusiasm and expertise of all of our members. So, we ask all interested members to submit proposals on the most important and current information and issues they believe impact vascular surgeons today.
“The majority of the educational sessions come from these proposals, so it’s a great way to get involved and contribute to the impact of the Vascular Annual Meeting.”
Educational Sessions are aimed at covering a breadth of subjects—both clinical and non-clinical— deemed important and timely to the ongoing education of SVS members and other attendees.
These segments of the VAM agenda—which makes up close to 50% of programming each day of the meeting—occur in varying size, meet the educational needs of different age groups and practice settings, and take on formats such as small-group interactive lectures, case-based courses, and handson and innovative/non-didactic approaches.

PGEC members judge proposals blindly through an online platform, followed by an unblinded selection meeting. Proposals scoring above a certain threshold are typically considered for inclusion in the VAM program, sometimes with suggestions for further development based on the overall content needs and related requirements.
To see the formal call for submissions as well as to find the link to the submission guidelines, visit vascular.org/VAM24CallForProposals. Meanwhile, to view recordings of the sessions from VAM 2023, which took place in National Harbor, Maryland, in June, visit the VAM Online Planner at vascular.org/OnlinePlanner23.—Beth Bales
“Exercise is the most powerful medicine for all chronic illnesses and the best predictor of longevity”
JESUS MATOSStephanie
Vasquez
VAM 2023 included a number of “firsts,” including the opening evening celebration, the inaugural Frank J. Veith Distinguished Lecture, and a Celebration of Diversity reception.
The SVS Subsection on Outpatient and Office Vas cular Care (SOOVC) had some firsts of its own, including naming and honoring the subsection’s new Presentation Award and Research Seed Grant. The Presentation Award recipients all gave talks on their topics during the SOOVC special section at VAM in June.


The subsection introduced the awards in the fall of 2022.
“We do a lot of really good work in the OBL [office-based lab] space, and there’s really very little written about that space,” said SOOVC Chair Anil Hingorani, MD. “We set up these presentation awards to encourage people to publish their information, present their information, and support the research projects they have done in an OBL or ASC [ambulatory surgery center] setting.”
The SOOVC Presentation Award recipients are:
● Michael A. Curi, MD, Newark, New Jersey, “Arteriovenous fistula creation and care in a dedicated office-based practice is superior to hospital-based care”
● Keerthi Harish, MD, of New York City, “Prior authorization processes in the office-based laboratory setting are administratively inefficient and threaten timeliness of care”
THE SVS HISTORY DIGITAL Archives Task Force is creating a historical digital archive and asking members to share any items they have that might be of significance in preserving the history of vascular surgery and the SVS.
Examples of items may be old photos, correspondence or video clips of pioneering procedures. Members are encouraged to share a description of items and information on their significance. Questions can be sent to Jerry Goldstone, MD, (jgoldst77@gmail. com) and Craig Miller, MD (drcraigamiller@gmail.com).
● Pavel Kibrik, MD, Brooklyn, New York, “Success rate and factors predictive of redo endothermal ablation of small saphenous veins”
The SOOVC Research Seed Grant recipients are:
● Michael Curi, MD, Newark, New Jersey, for the same arteriovenous fistula creation study above
● Robert Molnar, MD, Flint, Michigan, “Assessing the currently accepted indications for outpatient fistulogram performance and developing a quality improvement plan to establish a treatment algorithm for patients with hemodialysis dysfunction”
● Heather Waldrop, MD, and Christina Cui, MD, Raleigh, North Carolina, “Potential cost savings by moving appropriate cases to an officebased angiography suite”
These grants provide vascular surgeons with funds (grants are $10,000 each) to analyze research data for actionable insights, quality improvement and patient care. In announcing the recipients, Hingorani said, “We want to encourage people and support different teams to do the research that is so badly needed.” He hopes next year’s VAM will include presentations by the three recipients. The section looks forward to additional submissions for 2024.
More information on the subsection and the awards is available at vascular. org/SOOVC or by emailing SOOVC@vascularsociety.org.
SOCIETY FOR VASCULAR SURGERY
members can access the July 12 webinar recording on “SVS Presents: Leadership Challenges” for free as a member benefit. The webinar, the first installment of a twopart series, featured insights from disaster preparedness experts Deborah A. Kuhls, MD, and Susan Miller Briggs, MD.
They shared their experiences from the Boston Marathon bombing and the Las Vegas MGM mass shooting.
The webinar covered institutional preparation, lessons learned, dealing with post-traumatic stress disorder (PTSD) and engaging trainees in preparedness efforts. Members can save the date for part two in the series, set for Wednesday, Oct. 4.
SESSION RECORDINGS FROM THIS year’s VAM are now available for viewing online through the Online Planner platform. VAM attendees have access to these recordings for three years. Individuals must log in to the Online Planner, navigate to the “Full Schedule” section, choose the specific session of interest, and click on the corresponding popup message.
Attendees can access and rewatch the session by clicking on the “Video Recording” button next to the moderator’s name in the pop-up window, allowing them to revisit key points and reabsorb crucial information.
SPOT LIGHT
Former SVS President JULIE
, MD, has been named chair-elect of the Association of American Medical Colleges 2023–24 Board of Directors. Her term begins Nov. 7 and will end in November 2024. Freischlag, chief academic officer and executive vice president of Advocate Health, chief executive officer of Atrium Health Wake Forest Baptist, and executive vice president for health affairs of Wake Forest University, received the SVS’ highest honor, the Lifetime Achievement Award, at VAM 2023.
TIME IS RUNNING OUT TO PLAN ATTENDANCE AT THE ANNUAL COURSE, A Comprehensive Review and Update of What’s New in Vascular and Endovascular Surgery, to be held from Aug. 23–26 at the Beverly Hilton, in Beverly Hills, California.
The course is a joint effort of the Division of Vascular and Endovascular Surgery at the University of California, Los Angeles (UCLA) and the SVS. Besides an in-depth review of the specialty, it also provides basic didactic education for vascular residents and fellows in training. Many attendees find it offers a good review before the Vascular Surgery Board (VSB) exams.
The course recognizes four major pillars of vascular surgery practice: conventional open operations, catheter-based interventions (endovascular surgery), medical management and diagnostic imaging and noninvasive testing.
For more information, including the schedule, visit vascular.org/UCLAReviewCourse23
Registrants to the Vascular Quality Initiative (VQI) Annual Meeting and the Society for Vascular Nursing Annual Conference can also view the recordings for those meetings.
Visit vascular.org/OnlinePlanner23 to view recordings.
THE SVS HAS BEEN REACCREDITED AS a provider of continuing medical education (CME) by the Accreditation Council for Continuing Medical Education (ACCME).
ACCME is the gold standard for CME for physicians. ACCME providers certify that educational activities have been planned for physicians and include category 1 credit of the American Medical Association’s Physician’s Recognition Award.
Such credits are utilized by state licensing boards and boards of medical specialties to re-license physicians and re-certify them in their areas of specialty, and is recognized around the world.
Data from the Vascular Quality Initiative (VQI) have indicated that younger patients (aged ≤55 years) who undergo a carotid endarterectomy (CEA) procedure face an increased likelihood of carotid disease recurrence and late neurological events, as compared to their older counterparts. These findings have been published in the Journal of Vascular Surgery (JVS) by senior author Caron Rockman, MD, vascular surgery program director at New York University Langone Medical Center in New York City, and colleagues.
By Jamie Bell“THESE DATA SUGGEST THAT YOUNGER CEA patients may require more diligent follow-up, as well as a continued aggressive approach to medical management of atherosclerosis to prevent future events related to the op-
erated artery, given the particularly aggressive nature of premature atherosclerosis,” the authors write. The data were originally presented at the 2022 Eastern Vascular Society annual meeting held in Philadelphia last September.
The researchers posit that there are “few data” regarding outcomes of patients with premature cerebrovascular disease who undergo CEA, and this led them to conduct a study analyzing the demographics, presentation, and perioperative and later outcomes of younger patients receiving this treatment.
Querying the SVS VQI for CEA cases between 2012 and 2022, and stratifying patients based on age, Rockman and colleagues found that 7,009 of the 120,549 patients undergoing CEA (5.5%) were ≤55 years old. Their analysis revealed that younger patients were more likely to be African American (7.7% vs 4.5%), female (45.2% vs 38.9%), and active smokers (57.3% vs 24.1%).
As per their prespecified primary endpoints, the authors note similar rates of perioperative stroke/death (2% in both groups) and postoperative neurological events (1.9% vs. 1.8%) across younger and older patients. Reintervention rates did not significantly differ either.
However, younger patients were also found to have lower rates of overall postoperative complications (3.7% vs. 4.7%)—as well as being “significantly more likely” to experience late failure, defined as significant restenosis (≥80%) or complete occlusion of the
THE CHARACTERIZATION OF AORTIC tissue by means of three key biomechanicsbased biomarkers bundled into a compound Regional Areas of Weakness (RAW) Map showed “very good performance” in an artificial intelligence (AI)-based prediction of faster than average growth for a population of abdominal aortic aneurysm (AAA) patients under serial monitoring, according to a new study published in the Journal of Vascular Surgery-Vascular Science (JVS-VS).
The retrospective study was conducted among 36 AAA patients undergoing surveillance by electrocardiographically (ECG)-gated computed tomography angiography (CTA) at the University of Calgary in Alberta, Canada, by a team of researchers led by vascular surgeon Randy Moore, MD, and Elena Di Martino, PhD, a professor of biomedical engineering, using the emerging ViTAA Medical Solutions technology, which aims to provide an algorithm-driven route to precision care.

The RAW Mapping assessment of aortic weakness incorporates timeaveraged wall-shear stress, in-vivo principal strain, and intraluminal thrombus thickness, with the research team concluding
from the published analysis that “the use of features based on the functional and local characterization of the aortic tissue resulted in a superior performance in terms of faster than average growth prediction when compared to models mostly based on geometrical assessments.”

The technology deploys an AI model to predict accelerated aneurysmal growth, with the current study looking at RAW Mapping’s ability to predict growth and AAA evolution within a year. Future work will focus on expanding the investigation and growth prediction over a longer surveillance period, the investigators reported. Further research will also aim to broaden the applicability of the methodology to different imaging modalities and protocols used to monitor AAAs. “The ability to access functional information related to tissue weakening and disease progression at baseline for individual aortas has the potential to benefit patient monitoring, risk stratification and treatment selection, and optimize precisionbased aortic care,” the researchers added.—Bryan Kay
operated artery (2.4% vs. 1.5%). Furthermore, younger patients were observed as being more likely to experience a neurological event of any kind (3.1% vs. 2.3%).
“After controlling for covariates using a logistic regression model, [being aged] 55 years or younger was independently associated with increased odds of late restenosis or occlusion […] as well as late neurological events […],” Rockman et al add. They conclude that younger patients are more likely to experience carotid occlusion or restenosis and subsequent neurological events “during a relatively short follow-up period”—despite similar perioperative outcomes between the two groups.
INDICATIONS FOR USE IN THE U.S.: The GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface is indicated for improving blood flow in patients with symptomatic peripheral arterial disease in superficial femoral artery de novo and restenotic lesions up to 270 mm in length with reference vessel diameters ranging from 4.0 – 7.5 mm. The GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface is indicated for improving blood flow in patients with symptomatic peripheral arterial disease in superficial femoral artery in-stent restenotic lesions up to 270 mm in length with reference vessel diameters ranging from 4.0 – 6.5 mm. The GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface is indicated for improving blood flow in patients with symptomatic peripheral arterial disease in iliac artery lesions up to 80 mm in length with reference vessel diameters ranging from 4.0 – 12 mm. The GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface is also indicated for the treatment of stenosis or thrombotic occlusion at the venous anastomosis of synthetic arteriovenous (AV) access grafts. CONTRAINDICATIONS: The GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface is contraindicated for non-compliant lesions where full expansion of an angioplasty balloon catheter was not achieved during pre-dilatation, or where lesions cannot be dilated sufficiently to allow passage of the delivery system. Do not use the GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface in patients with known hypersensitivity to heparin, including those patients who have had a previous incident of Heparin-Induced Thrombocytopenia (HIT) type II. Refer to Instructions for Use at eifu.goremedical.com for a complete description of all applicable indications, warnings, precautions and contraindications for the markets where this product is available.
*As used by Gore, Heparin Bioactive Surface refers to Gore’s proprietary CBAS Heparin Surface. Products listed may not be available in all markets.
Young endarterectomy patients more likely to experience restenosis and late neurological events
“ These data suggest that younger CEA patients may require more diligent follow-up, as well as a continued aggressive approach to medical management of atherosclerosis to prevent future events related to the operated artery, given the particularly aggressive nature of premature atherosclerosis”
CARON ROCKMAN ET AL





The Gore RELINE MAX Clinical Study demonstrated safe and effective treatment of real-world superficial femoral artery (SFA) in-stent restenosis (ISR) through three years with the VIABAHN® Device.1








65% 100% freedom from major amputations and VIABAHN® Device stent fractures

freedom from target lesion revascularization

Occluded bare metal stent Post VIABAHN® Device placement Images courtesy of Peter Soukas, M.D. Used with permission.
