02 Guest editorial Welcome to the new age of vascular surgery influencer

05 Comment & analysis Corner Stitch looks at the trainee’s role in tackling disparities in peripheral arterial disease

SAVS PRESIDENT REVEALS UPCOMING CHANGE TO SOCIETY SEAL
Southern Association for Vascular Surgery (SAVS) President


William D. Jordan Jr., MD, used a portion of his 2023 Presidential Address to outline ways in which SAVS is set to further evolve as a professional body going forward.
Titled “Anatomy and physiology:
2.0,” Jordan’s lecture tackled the structure and function of vascular surgery as a specialty, and SAVS as a surgical society, as he addressed a need for change.
One aspect of SAVS set to evolve, he revealed, is the Society’s signature seal, a depiction of 19th-century pioneering surgeon Rudolph Matas, MD, (1860–1957) who was selected by SAVS founding members to adorn the logo as an embodiment of the qualities they believed a southern vascular surgeon should possess.
Jordan told the SAVS 2023 annual meeting (Jan. 18–21) in Rio Grande, Puerto Rico, that the Society had become aware of concern “that our image among many young surgeons is negatively impacted by having his likeness on our seal.
“Many of us have great respect for the work he has done,” he said, “but some have expressed concern about parts of his academic work that was offensive and not respectful to disadvantaged groups of the day. He wrote about medical conditions of many Black
See page 10
12 BEST-CLI Analysis finds correlation between WIfI stage and reports of poorer mental health
17 VAM 2023
SVS annual meeting all-set to be an exclusively in-person event
www.vascularspecialistonline.com
Prominent venous disease experts discuss venous stenting, appropriate care, and the pursuit of refined data and better education in a space where part of the problem involves practitioners moving “freely from being able to do arterial intervention and suddenly assume they can do a venous intervention.” By

 Jocelyn Hudson and Bryan Kay
Jocelyn Hudson and Bryan Kay
See page 6
THE OFFICIAL NEWSPAPER OF THE Presorted Standard U.S. Postage PAID Permit No. 384 Lebanon Jct. KY ascularV pecialists CHANGE SERVICE REQUESTED 9400 W. Higgins Road, Suite 315 Rosemont, IL 60018 FEBRUARY 2023 Volume 19 Number 02 In this issue:
Have you seen the 8-year sac regression data? See the data on page 3 UC202212257 EN ©2022 Medtronic. All rights reserved. 01/2022
STENTING
VENOUS
Medical Editor Malachi Sheahan III, MD


Associate Medical Editors
Bernadette Aulivola, MD | O. William Brown, MD | Elliot L. Chaikof, MD, PhD
| Carlo Dall’Olmo, MD | Alan M. Dietzek
MD, RPVI, FACS | Professor HansHenning Eckstein, MD | John F. Eidt, MD
| Robert Fitridge, MD | Dennis R. Gable, MD | Linda Harris, MD | Krishna Jain, MD | Larry Kraiss, MD | Joann Lohr, MD
| James McKinsey, MD | Joseph Mills, MD | Erica L. Mitchell, MD, MEd, FACS
| Leila Mureebe, MD | Frank Pomposelli, MD | David Rigberg, MD | Clifford Sales, MD | Bhagwan Satiani, MD | Larry Scher, MD | Marc Schermerhorn, MD | Murray
L. Shames, MD | Niten Singh, MD | Frank
J. Veith, MD | Robert Eugene Zierler, MD
Resident/Fellow Editor
Christopher Audu, MD
Executive Director SVS
Kenneth M. Slaw, PhD
Director of Marketing & Communications Bill Maloney
Managing Editor SVS Beth Bales
Marketing & Social Media Manager
Kristin Crowe
Communications Specialist
Marlén Gomez
Published by BIBA Publishing, which is a subsidiary of BIBA Medical Ltd.
Publisher Roger Greenhalgh
Content Director Urmila Kerslake
Managing Editor Bryan Kay bryan@bibamedical.com
Editorial contribution
Jocelyn Hudson, Will Date, Jamie Bell, Clare Tierney, Eva Malpass and Adam Pearce
Design Terry Hawes
Advertising Nicole Schmitz nicole@bibamedical.com
Letters to the editor vascularspecialist@vascularsociety.org
BIBA Medical, Europe
526 Fulham Road, London SW6 5NR, United Kingdom
BIBA Medical, North America
155 North Wacker Drive – Suite 4250, Chicago, IL 60606, USA
Vascular Specialist is the official newspaper of the Society for Vascular Surgery and provides the vascular specialist with timely and relevant news and commentary about clinical developments and about the impact of healthcare policy. Content for Vascular Specialist is provided by BIBA Publishing.
Content for the News From SVS is provided by the Society for Vascular Surgery. The ideas and opinions expressed in Vascular Specialist do not necessarily reflect those of the Society or the Publisher. The Society for Vascular Surgery and BIBA Publishing will not assume responsibility for damages, loss, or claims of any kind arising from or related to the information contained in this publication, including any claims related to the products, drugs, or services, or the quality or endorsement of advertised products or services, mentioned herein. | The Society for Vascular Surgery headquarters is located at 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. | POSTMASTER: Send changes of address (with old mailing label) to Vascular
Specialist, Subscription Services, 9400 W. Higgins Road, Suite 315, Rosemont, IL 60018. | RECIPIENT: To change your address, e-mail subscriptions@bibamedical.com | For missing issue claims, e-mail subscriptions@bibamedical. com. | Vascular Specialist (ISSN 1558-0148) is published monthly for the Society for Vascular Surgery by BIBA Publishing. | Printed by Vomela Commercial Group | ©Copyright 2023 by the Society for Vascular Surgery
GUEST EDITORIAL
Likes, dislikes and reposts: The new age of the vascular surgery influencer

 By Jean Bismuth, MD, and Jonathan Cardella, MD
By Jean Bismuth, MD, and Jonathan Cardella, MD
The brave new world of social media, with its TikToks and Kardashians, has now invaded our once-sane specialty. No, this is not a veiled reference to controversial swim attire events in our past, but rather a totally new phenomenon. Whether on Twitter, LinkedIn, Instagram, or YouTube, vascular surgeons are posting their “successful” cases like never before. Why the constant need to do this... a cry for validation? Sometimes it appears to be a not-so-subtle show of support for a friendly vendor, as is evidenced by the “clot warriors,” posting dramatic lengths of coagulum in an effort to prove mine is bigger than yours. Could it be that vascular surgeons just don’t feel championed by their own specialty, and they’re in dire need of basic validation, a simple pat on the back? Is there such a void of mentorship in our chosen specialty? Do we need to practice in a stadium full of adoring fans, hanging on to every stitch and stent like the Rolling Stones at Wembley? If I sold tickets to my next tibial bypass, would fans crash the Ticketmaster website like the Swifties?
The psychology of this phenomenon is curious. More than any specialty, vascular surgery is marred by complications. It’s the nature of the patients we treat. We treat very sick patients with difficult problems, and yet only successes are posted. Why not the failures? From our first days in surgery, we discovered that morbidity and mortality (M&M) rounds are where we learn the most valuable lessons. A sensible surgeon will assess and reassess any complication incurred and apply rigor to all outcomes, even those that are viewed as successful. However, despite these lessons learned through our training and practice, there is still a need to “virtue signal” curated images and scenarios on social media and disregard any possible criticism that may be levied.
Virtue signaling is loosely defined as attempting to show you are a good person, or in this case doctor, through the expression of viewpoints (using angiograms, CT scans, etc.), usually on social media. It’s concerning that as physicians, we carefully curate our best cases on social media, like others post luxurious Italian villas or diligently choreographed Cardi B dance moves. The psychology behind the need to have this external validation from the public, many of whom are unknown, is puzzling. One would suspect that good outcomes and happy patients would suffice for many, but it appears this is not the case. There are concerns about this from many angles. What message does this send to the public? Many will view these posts and assume validity based on the detail of the information provided. It is also concerning that this becomes an example for our trainees, many of whom also follow on social media, that this external validation is required as a means of attaining relevance and satisfaction in their careers. Finally, it is not a huge stretch to foresee the HIPAA violations created by the specificity and detail presented in these cases.
Recently on LinkedIn, a vascular surgeon presented an absolute banality of a case—a cephalic arch recanalization and stenting. The waterfall of accolades was simply bewildering! Should it even matter that we all know that this will
fail? When I made a comment to that effect and suggested a surgical alternative, I was sent an old article with a small series of cases where patients were treated successfully with stent-grafts. The surgeon also made a somewhat snide comment that he only believed in randomized controlled trials, and that this was an endovascular forum. This individual evidently failed to see the irony of his comment, but the absurdity naturally did not escape me. Of course, further interaction was futile. So the question begs, why post a case if it is not to engage in an open discussion about pros and cons? Is it really so basic that the person posting is merely petitioning for some emoticons that reinforce their greatness or dispel their insecurities?
A stent-graft deployed in front of an army of fans where none dare to question the decision-making, regardless of the outcome?
It may be somewhat naïve to expect surgeons to be transparent about their motivations for presenting cases. It would be helpful, though, to know the surgeon’s incentives behind their posts—no different than a disclosure slide in a presentation at a conference. Perhaps, before an intervention video on Twitter, a post should warn that DR. SIMPSON IS POSTING THIS AWESOME CASE IN THE HOPES THAT YOU WILL CALL HIM AWESOME. Or maybe: DR. CLARK WOULD LIKE TO DECLARE THAT HE HAS ONLY RECEIVED RUDIMENTARY ENDOVASCULAR TRAINING BUT PLEASE SMASH THAT LIKE BUTTON!!!!
Should we suggest that fact-checkers evaluate cases posted for value and accuracy? In reality, we should be able to police ourselves without resorting to any sort of censuring. Still, one should be concerned about what is posted on social media, a public platform.
In the time preceding social media, these cases would continue in anonymity unless submitted, peerreviewed, and published in a journal
It is also crystal clear that the Federal Trade Commission (FTC) has very explicit guidelines on how to manage disclosures when networking on social media If you have any financial interest with a brand… disclose it! As a surgeon on social media, you are an influencer because posts influence consumers (other physicians, patients). Don’t pretend to hide under the guise of a clinician, particularly when motives are not transparent.
In the time preceding social media, these cases would continue in anonymity unless submitted, peer-reviewed, and published in a journal where they can be consumed by people familiar with the procedures at hand. In the social media era, the very key point of peer review is missing, allowing any charlatan to publish results and claims that may or may not have any academic or physiologic basis. This, again, gets back to motivation and disclosure. Is the incentive to garner social media “likes” in order to further promotion? Job security? Reputation? Financial gains from corporations? By circumventing the peer-review process, this arena has become the Wild Wild West. There are snake oil salespeople everywhere.
The misuse of social media has certainly not gone uncontinued on page 4
Vascular Specialist | February 2023 2
Jean Bismuth
Jonathan Cardella
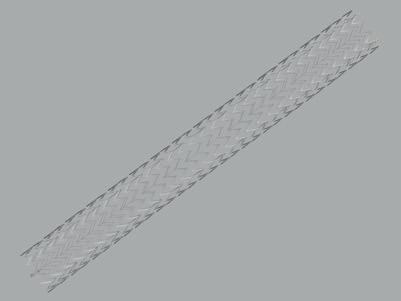
Endurant™ AAA stent graft system

The standard of EVAR durability with 8-year data
66% of patients
demonstrate notable aneurysm sac regression at eight years in the longest-term follow-up of any contemporary, real-world EVAR registry.
Sac regression rates
Results are taken from independent clinical studies for illustration purposes only and are not based on statistical analysis. Results may differ in a head-to-head comparison; multiple factors contribute to clinical study outcomes and need to be considered in making assessments across different studies.
†Sac regression defined as the reduction in maximum diameter by > 5 mm.
‡Sac regression defined as the reduction in maximum diameter by ≥ 5 mm.
1 Teijink J, Power A, van Sterkenburg S, et al. 8-Year Data from the ENGAGE Registry Extension: Insights about the Long-term Performance of a Contemporary EVAR Device. Presented at ESVS 35th Annual Meeting September, 20, 2021.
2 Singh MJ, Fairman R, Anain P, et al. Final Results of the Endurant Stent Graft System in the United States Regulatory Trial. J Vasc Surg. July 2016;64(1):55-62.
3 IFU — GORE™* EXCLUDER™* Conformable U.S. — January 2021.
Excluder™* Conformable EXCeL Registry ENGAGE OUS Registry ‡ N = 166/2511 8-year 66% Not Available 1-year U.S. Endurant IDE (Bifur) † N = 65/1352 Excluder™* Conformable IDE‡ N = 27/733 48% 37%
LIKES, DISLIKES AND REPOSTS; THE NEW AGE OF THE VASCULAR SURGERY INFLUENCER
noticed by the state medical boards in the U.S. Recently, a plastic surgeon in Ohio had her license suspended for exploitation of Snapchat and TikTok by airing live videos of her surgeries. This doctor has a popular TikTok account, which, prior to being suspended and then set to private, had 841,600 followers and 14.6 million likes. Her Instagram account, now also set to private, has 123,000 followers. One of her patients was quoted as saying: “I went to her because, I thought, from all of her social media, that she uplifted women. That she helped women empower themselves. But she didn’t.” Plastic surgery has been plagued by a social media presence that often flirts with unethical standards. This space suffers from a lack of regulation, surveillance, consistent rating scales, user authentication and ethical accountability. People are building entire reputations based on Altmetric Attention Score (#altmetrics), which has, to a great degree, replaced the more traditional academic bibliometrics like h-index. The Altmetric Attention Score is a weighted count of all the online attention for an individual research output. This includes mentions in essentially every public forum, and social network platforms play a particularly important role. With the advent of endovascular techniques, vascular surgery is very analogous to plastics in that the graphics of the procedures make them very “post-” and “like-” worthy.
In 2015, Prestin et al estimated that 70% of adults got their medical information from the internet. Social media, therefore, is an extremely powerful tool. How we engage in that space plays a significant role in defining vascular surgery as a profession and speaks volumes about our character as individuals. Our posting habits and decisions have the power to sway consumers as well as dictate the reputation of our specialty.
JEAN BISMUTH is a vascular surgeon at Katy Heart and Vascular Institute in Houston and an associate professor of surgery at Louisiana State University.
JONATHAN CARDELLA is is an associate professor of surgery at Yale School of Medicine in New Haven, Connecticut, and program director of Yale’s integrated vascular surgery residency.
Sudanese vascular society readies for first-ever conference
The Sudanese Association of Vascular Surgeons (SudAVaS) announced the program behind its first-ever international conference, marking the occasion by celebrating the “first steps in establishing vascular surgery as a standalone surgical specialty” in the northeast African country.

The meeting took place in the Sudanese capital of Khartoum from Feb. 7–8, with the scientific program covering the full gamut of the vascular beds, as well as training issues, vascular trauma and the history of vascular surgery in Sudan. SudAVaS President Isam Osman, MBBS, hailed the Sudanese vascular surgical community ahead of the event, writing in an open letter: “… I must pay tribute to the few lonely vascular surgeons in Sudan who have toiled for years on their own, often in very challenging circumstances.”
Osman also expressed thanks to those who had helped craft the program.
“We hope it will inspire our young graduates to consider a career in vascular surgery,” he added.—Bryan Kay
continued from page 2
SVS ANNUAL MEETING INTRODUCES EARLY-BIRD REGISTRATION
THE SVS IS INTRODUCING A THREE-TIERED pricing plan for the 2023 Vascular Annual Meeting (VAM). Early-bird rates start when registration opens March 15. The cost of putting on major conferences and events is skyrocketing in the post-COVID era, requiring medical societies, including the SVS, to plan as early and as accurately as possible for anticipated costs. “There is a premium on getting as much advanced planning data on attendance as we can, to keep costs under control and allocated where they are needed most,” noted SVS Executive Director Kenneth M. Slaw, PhD.
Attendees can take advantage of the early-bird prices until April 5. The advance rate is then in effect from April 6 to June 12. The on-site rate begins June 13, when registration opens at the Gaylord venue in National Harbor, Maryland.
“We have worked through the COVID-19 crisis and now are adapting to a post-COVID world of rising costs and inflation,” said Michael Dalsing, MD, SVS president. “This change to three tiers of registration enables us to better contain rising costs, which in turn allows SVS to keep registration fee increases to a minimum, while continuing to invest in increasing value for VAM attendees. I encourage our members to register as early as possible.” Full pricing across all membership categories and time frames, plus pricing for add-ons, is available at vascular.org/VAM23Registration.—
Beth Bales
Endurant II/Endurant IIs Stent Graft
Indications: The Endurant™ II/Endurant™ IIs bifurcated stent grafts are indicated for the endovascular treatment of infrarenal abdominal aortic or aortoiliac aneurysms. They may be utilized in conjunction with the Heli-FX™ EndoAnchor™ system when augmented radial fixation and/or sealing is required; in particular, in the treatment of abdominal aortic aneurysms with short (≥ 4 mm and < 10 mm) infrarenal necks (see Neck length definition below). The Endurant II stent graft system aorto-uni-iliac (AUI) stent graft is indicated for the endovascular treatment of infrarenal abdominal aortic or aortoiliac aneurysms in patients whose anatomy does not allow the use of a bifurcated stent graft. The Endurant II/IIs stent graft system is indicated for use in patients with the following characteristics: • Adequate iliac or femoral access that is compatible with vascular access techniques, devices, or accessories
• Proximal neck length of • ≥ 10 mm; or • ≥ 4 mm and < 10 mm when used in conjunction with the Heli-FX EndoAnchor system (bifurcated stent graft only)
Note: Neck length is defined as the length over which the aortic diameter remains within 10% of the infrarenal diameter. • Infrarenal neck angulation of ≤ 60° • Aortic neck diameters with a range of 19 to 32 mm • Distal fixation length(s) of ≥ 15 mm • Iliac diameters with a range of 8 to 25 mm • Morphology suitable for aneurysm repair
Contraindications: The Endurant II/Endurant IIs stent graft system is contraindicated in: • patients who have a condition that threatens to infect the graft • patients with known sensitivities or allergies to the device materials. When used with the Heli-FX EndoAnchor system, the Endurant II/IIs stent graft system is also contraindicated in: • patients with known sensitivities to the EndoAnchor implant materials. For contraindications regarding ancillary devices used with the Endurant II/Endurant IIs stent graft system, refer to the Instructions for Use provided with the device.
Warnings and Precautions:
• The long-term safety and effectiveness of the Endurant II/Endurant IIs stent graft system has not been established. All patients should be advised that endovascular treatment requires lifelong, regular follow-up to assess the health and the performance of the implanted endovascular stent graft. Patients with specific clinical findings (e.g., endoleaks, enlarging aneurysms, changes in the structure or position of the endovascular graft), or less than the recommended number of EndoAnchor implants when used in short proximal necks (≥ 4 mm and < 10 mm), should receive enhanced follow-up. Specific follow-up guidelines are described in the Instructions for Use. • Patients experiencing reduced blood flow through the graft limb, aneurysm expansion, and persistent endoleaks may be required to undergo secondary interventions or surgical procedures. • The Endurant II/Endurant IIs stent graft system is not recommended in patients unable to undergo or who will not be compliant with the necessary preoperative and postoperative imaging and implantation procedures as described in the Instructions for Use. • Renal complications may occur: 1) From an excess use of contrast agents. 2) As a result of emboli or a misplaced stent graft. The radiopaque marker along the edge of the stent graft should be aligned immediately below the lower-most renal arterial origin. • Studies indicate that the danger of micro-embolization increases with increased procedure duration. • The safety and effectiveness of the Endurant II/ Endurant IIs stent graft system has not been evaluated in some patient populations. Please refer to the product Instructions for Use for details.
MRI Safety and Compatibility: Non-clinical testing has demonstrated that the Endurant II/Endurant IIs stent graft is MR Conditional. It can be scanned safely in both 1.5T & 3.0T MR systems under certain conditions as described in the product Instructions for Use. For additional MRI safety information, please refer to the product Instructions for Use.
Adverse Events: Potential adverse events include (arranged in alphabetical order): amputation; anesthetic complications and subsequent attendant problems (e.g., aspiration), aneurysm enlargement; aneurysm rupture and death; aortic damage, including perforation, dissection, bleeding, rupture and death; arterial or venous thrombosis and/or pseudoaneurysm; arteriovenous fistula; bleeding, hematoma or coagulopathy; bowel complications (e.g., ileus, transient ischemia, infarction, necrosis); cardiac complications and subsequent attendant problems (e.g., arrhythmia, myocardial infarction, congestive heart failure, hypotension, hypertension); claudication (e.g., buttock, lower limb); death; edema; EndoAnchor system (for infrarenal EVAR procedures using the Heli-FX EndoAnchor system): partial deployment, inaccurate deployment, fracture, dislodgement, embolization, stent graft damage, modelling balloon damage); embolization (micro and macro) with transient or permanent ischemia or infarction; endoleak; fever and localized inflammation; genitourinary complications and subsequent attendant problems (e.g., ischemia, erosion, femoral-femoral artery thrombosis, fistula, incontinence, hematuria, infection); hepatic failure; impotence; infection of the aneurysm, device access site, including abscess formation, transient fever and pain; lymphatic complications and subsequent attendant problems (e.g., lymph fistula); neurologic local or systemic complications and subsequent attendant problems (e.g., confusion, stroke, transient ischemic attack, paraplegia, paraparesis, paralysis); occlusion of device or native vessel; pulmonary complications and subsequent attendant problems; renal complications and subsequent attendant problems (e.g., artery occlusion, contrast toxicity, insufficiency, failure); stent graft: improper component placement; incomplete component deployment; component migration; suture break; occlusion; infection; stent fracture; graft twisting and/ or kinking; insertion and removal difficulties; graft material wear; dilatation; erosion; puncture and perigraft flow; surgical conversion to open repair; vascular access site complications, including infection, pain, hematoma, pseudoaneurysm, arteriovenous fistula, dissection; vascular spasm or vascular trauma (e.g., iliofemoral vessel dissection, bleeding, rupture, death); vessel damage; wound complications and subsequent attendant problems (e.g., dehiscence, infection, hematoma, seroma, cellulitis). Please reference product Instructions for Use for more information regarding indications, warnings, precautions, contraindications and adverse events.
CAUTION: Federal (USA) law restricts this device to sale by or on the order of a physician.
medtronic.com/sacregression
UC202210505d EN ©2022 Medtronic. All rights reserved. Medtronic, Medtronic logo, and Engineering the extraordinary are trademarks of Medtronic. ™*Third-party brands are trademarks of their respective owners. All other brands are trademarks of a Medtronic company. For distribution in the USA only. 12/2022
4 Vascular Specialist | February 2023
EDITORIAL
GUEST
UC202210505d EN PrintAd_8-yearENGAGE_Endurant_US.indd 2 12/19/22 3:40 PM VAM 2023 GLOBAL ➽
& CORNER STITCH
More than a research project: The vascular
role in tackling disparities in peripheral arterial disease
By Chloé Powell, MD
ONE OF MY EARLIEST CLINICAL EXPERIENCES with vascular disease was as a high school student shadowing at a busy urban hospital in Detroit. A Black man with a longstanding history of diabetes developed a foot ulcer that ultimately required an amputation. Though I did not know the exact circumstances that led to his amputation, I would later learn about the cumulative insults that not only impacted his health, but also other members of the community.
The problem at a glance
Disparities in peripheral arterial disease (PAD) care and vascular surgery outcomes persist despite improvements in technology and interventional therapies. Blacks, Hispanics and Native Americans have higher rates of PAD, and undergo amputation at two-to-four times the rate of White patients. They are less likely to undergo revascularization prior to amputation, and have higher rates of morbidity and mortality after amputation and revascularization. Female patients with symptomatic PAD report greater functional impairment and worse outcomes after revascularization compared with male patients. Those patients belonging to lower socioeconomic backgrounds experience a higher burden of disease, higher risk for PAD-related hospitalizations, and higher odds of amputation in the setting of severe PAD. Patients living in rural areas face unique challenges due to physical barriers to access to care, or lack of geographic availability of specialty care. Fortunately, through decades of work we have transitioned from viewing these adverse outcomes as
intrinsic failures of the patient, to considering the barriers across the PAD care continuum.
PAD pipeline
I have conceptualized PAD care—albeit simplified—as starting with patient evaluation, PAD detection and medical management initiation. For those whose disease has progressed, interface with an interventionalist may become necessary. This pathway is the PAD pipeline. However, whether a person reaches this pipeline, and ultimately moves through, it is not equal. It is influenced by structural inequities. As an example, through historical policies, geographic segregation may limit the hospitals to which a person has access, where quality may be lower. Provider biases may serve as gatekeepers limiting access to care. Patient risk factors and comorbidity burden may be influenced by disparities in education and their built environment. As Joshua Beckman, MD, has proclaimed, “PAD is the disparity,” thus mitigating the development of PAD would be most ideal. However, for those that siphon through the pipeline, it should at least be optimized.
Altering the tide
Addressing disparities in PAD care and surgical outcomes will not occur overnight, and will require a movement toward focusing on health equity utilizing a multi-pronged approach. There is no one-size-fits-all intervention. The needs of local and regional communities differ, and thus innovative and successful solutions will take that into consideration. There are several ways we can try to alter the tide:
1. Recognizing the disparities in PAD burden and outcomes are the result of structural inequities. By advocating for and supporting policies that promote equity broadly—but especially those targeted toward improving access to quality healthcare—we are likely to have the greatest impact and break the generational cycle of poor health.
2. At the health system level, we need to develop both intra- and inter-specialty collaboration. Patients with PAD have complex social and medical needs, and, as such, numerous specialists are involved in managing their care. Improved interdisciplinary collaboration paves the way for enhanced risk factor modification, continuity of care and ensures patients receive high-quality care most aligned with their goals. The “toe and flow” model of
care demonstrates the benefits of a collaborative team approach in dealing with patients with chronic limb threatening ischemia (CLTI). Collaboration should also include other health systems. The state of Michigan is rich with collaborative quality initiatives that really seeks to share strategies to improve the quality of care we deliver across the board.
3. Because health is largely shaped by the social determinants of health, developing and fostering intentional and mutually beneficial community partnerships serves to build trust among communities that have faced discrimination and abuse by the medical community. By having a finger on the pulse of the community’s needs, partnerships can help to connect individuals with healthcare providers. For example, Michigan Medicine is developing an initiative called MSHIELD geared toward addressing the social determinants of health.
4. When conducting research, we should generate evidence and examine data through the lens of intersectionality, cultural humility, and acknowledge the research process itself can be biased. We should also actively support efforts to engage, recruit and retain participants from historically excluded and exploited populations. This may require diversifying the research team or partnering with trusted organizations.

5. On the clinical front, we need to continue to educate ourselves about the structural inequities and its implication on patient health. We must ensure we are utilizing evidence-based medicine in a culturally sensitive manner to better provide patient centered care.
As a vascular surgery trainee, it is easy to think that vascular surgery is at the end of the PAD pipeline and all the “damage” is done. However, I would argue we have a unique perspective because of the longitudinal care we provide, and we too often bear witness to the devastating effects of progressive PAD. We have insight into problems that arise in routine practice that create gaps between evidence-based care and actual care. By capitalizing on these spheres of influence, vascular surgeons can bridge and accelerate the link between research, community, advocacy, and clinical care in a way that is most relevant and beneficial to patients and vascular surgical practice.
CHLOÉ POWELL is a 5th-year resident in the integrated vascular surgery residency program at the University of Michigan in Ann Arbor.
VRIC: ‘HIGH VALUE PLACED ON SUPPORTING YOUNG RESEARCHERS,’ 2022 TRAINEE AWARDEE SAYS VASCULAR SCIENCE
Warm and inviting. Plenty of engagement at each presentation. A straightforward format that allows everyone to participate at all presentations. Sense of unity. Great support for young researchers. And the ability to talk with prominent scientific leaders (writes Beth Bales).
That’s how Carson Hoffmann, MD, describes his experience as a presenter at the 2022 Vascular Research Initiatives Conference (VRIC). Scientists judged his abstract as one of the four top-scoring submissions, and all four trainees received the SVS Foundation’s Vascular Research Initiatives Conference Vascular Trainee Award and the opportunity to present at the conference.
His presentation was “Modifiable mesenchymal stem cell defects in veterans with diabetes mellitus.” His mentor is Luke Brewster, MD, former chair of the SVS Basic and Translational Research Committee, which oversees VRIC.


This year’s conference, held in conjunction with the
American Heart Association’s Vascular Discovery Scientific Sessions, will be May 10 in Boston. Registration for VRIC—which emphasizes basic and translational vascular science—opened Feb. 1.
After being part of past academic meetings, Hoffmann thought he knew what to expect from VRIC. He was wrong and, in fact, pleasantly surprised.
“Being a newcomer and mostly a stranger, I was received with a warm welcome and invited to participate as if I had attended for many years,” he said.
“I found this to be a very accepting and closeknit group of scientists that sought each other’s opinions and feedback to advance their academic pursuits just as much as they enjoyed the opportunity to gather as friends.”
Besides being an honor, his selection for the VRIC Trainee Award provided “a fantastic introduction with this scientific community,” Hoffmann said, further explaining: “To be recognized in such a big manner for work done in the lab revealed the commitment of this group to fostering scientific research from up-and-coming researchers and wanting to get their efforts acknowledged.
“It was readily apparent that a high value was placed on supporting young researchers by the opportunity to be present for both the VRIC and the Vascular Discovery conference and to interact with highly esteemed and prominent scientific leaders in their respective fields.”
For more on VRIC 2023, visit vascular.org/VRIC23 Read more at vascular.org/VRIC22Report.
www.vascularspecialistonline.com 5
trainee’s
Carson Hoffmann (top) and Luke Brewster
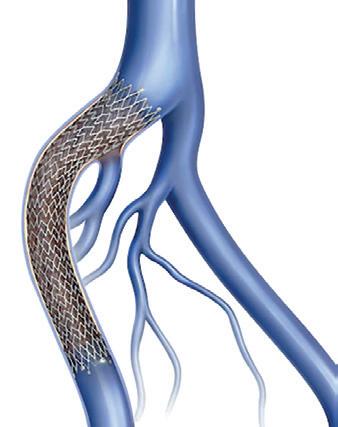
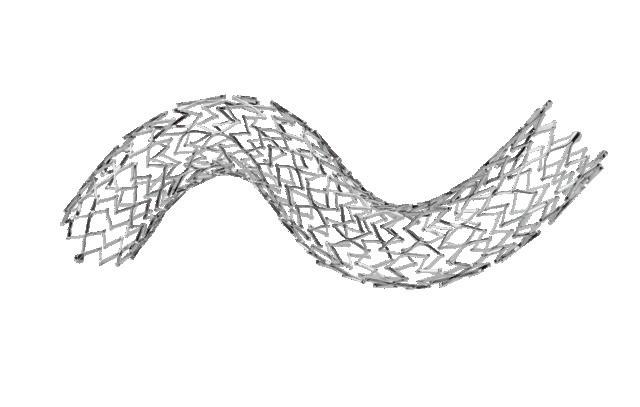
FROM THE COVER: EDUCATE, EDUCATE, AND EDUCATE AGAIN: THE CONTINUING QUEST FOR APPROPRIATE VENOUS CARE
EDUCATION ACROSS THE VENOUS CARE delivery spectrum lies at the heart of efforts to ensure operator judgement is optimal and procedures—like the placement of venous stents—are carried out in the appropriate circumstances.

Or, as Steve Elias, MD, director of the Center for Vein Disease at Englewood Health Network in Englewood, New Jersey, says, “the trend is going to be perhaps that too many stents are going to be placed for a while until we educate people about when this is appropriate, and when it’s not appropriate.”
Elias was speaking ahead of the 2023 American Venous Forum (AVF) where some of the latest data on venous stent usage trends between 2014 and 2021 are to be presented by Karem Harth, MD, director of the Center for Comprehensive Venous Care at UH Harrington Heart & Vascular Institute in Cleveland.
Four dedicated venous stents have been cleared in the U.S.—the Abre, Venovo, Zilver Vena, and Vici devices—with stent migration and overstenting still recurring themes as new research is presented, and surgeons discuss outcomes. Recently, new data from the clinical trial of the Abre dedicated venous stent saw investigator Stephen Black, MD, from Guy’s and St Thomas’ Hospital in London, England—who led the study with Erin Murphy, MD, from Sanger Heart & Vascular Institute, Atrium Health, in Charlotte, North Carolina—declare that, given the study showed no stent fractures through three years, and similarly, no delayed stent migrations, “… stent migration really does seem to be an operator issue rather than a stent issue.”
Elias underscores the point: 99.9% of the time the issue is not one of the stent but of the judgment of the operator, or poor training—“or an issue of considering venous stents are similar to arterial stents,” he tells Vascular Specialist. He emphasizes the role of device makers in education. “Those of us on the leading edge of this are working with all of industry to set up programs to better educate their salesforces, and then also their physician customers, regarding not just stents but also venous disease in general,” he says. “We all realize this is a problem, and the only way to solve it is by all of us working together.”
Data: From IDEs to RCTs
Over the past decade, venous stenting has evolved from a “byword” into a “mainstream and accepted” practice, Black tells Vascular Specialist. In recent times, the on-label, venous-specific devices were made available, along with the first prospective data in the form of investigational device exemption (IDE) trials, and, according to Black, there is now “more enthusiasm for treating patients” among providers in the venous space.
At this juncture, Kush Desai, MD, from Northwestern
University in Chicago, believes the time to embark on “real-world” studies is now, with the aim of “demonstrating the value of treatment of patients across a variety of disease states, from non-thrombotic through post-thrombotic.” He explains that these data will help physicians to “clearly identify which patients benefit and what we can expect for outcomes.”
Black concurs, adding that randomized controlled trials (RCTs) will need to follow, despite the difficulties associated with carrying out such research. The “big problem” here is recruitment—a problem that is affecting various ongoing trials. This recruitment issue is multifactorial, Black notes, specifying that clinicians “feel they do not have equipoise anymore,” and among some there is a “financial conflict bias,” while patients “do not want not to be treated.” The solution? According to Black, clinicians need to work as a group to “overcome our own biases,” in order to ensure randomized evidence ensues.
Desai also points to the importance of data consolidation, referencing in particular the work of the Deep Venous Academic Research Consortium, which he chairs alongside Black. “The goal of this is to improve the rigour and reproducibility of deep venous research,” Desai explains, by way of ensuring that studies are all collecting the same trial data, so that they can be compared. He hopes that this creates “more sound data” for the devices that practitioners are placing, and will thus have a “downstream effect” on impacting clinical practice.
Rabih Chaer, MD, chief of the division of vascular surgery at the University of Pittsburgh in Pennsylvania, notes that “longer-term” data might still be lacking for the individual stents, as well as comparative data between the different stents, that are available for venous placement.
“That becomes important because, at least, the newer-generation venous dedicated stents have shown us that some have performed better in certain locations based on the design of the stent,” he says. “There may be some variability in the performance of each stent, depending on which part of the vein, and for which indication that they are used.”
In parallel to the need for more data, Desai posits there is “quite a long way to go” in terms of refining venous stenting practice. “The devices are very good,” he says, noting that, while there is “certainly room for improvement,” outcomes across studies are “very similar—sort of agnostic to the stent device”.
Both Black and Desai highlight the importance of understanding the specifics of venous disease when it comes to best practice. “Part of the problem with venous is people move very freely from being able to do arterial intervention and suddenly assume they can do a venous intervention,” Black remarks. “It is like playing squash and tennis,” he analogizes. “They are both racket sports
continued from page 1
with a ball, but the rules are not the same.”
According to Desai, the “biggest issues” in terms of practice are with patient selection and disease state recognition. “Simply put, there are far too many stents placed for non-thrombotic disease in the U.S., meaning there is attribution of symptoms that are not likely to significantly improve with placement of a stent.” He states that this can be attributed in part by economic benefits to the operators—which he says “may be a uniquely U.S. thing”—however notes that there are “likely a variety of problems at play.”
Black stresses that “inappropriateness of care” is the key issue, and that one of the main challenges facing venous stenting practice is ensuring “the right patient get the right treatment by people trained who know how to do it properly.”
Non-thrombotic iliac vein lesions (NIVLs) are at particular risk of overtreatment, he says, because “the impetus is to treat anybody with any leg problem on the left-hand side” when there are lots of patients who do not need treatment. In the case of chronic occlusions and post-thrombotic disease, and potentially acute iliofemoral deep vein thrombosis (DVT), he notes there are lots of patients who are not getting treatment who would “probably benefit.”
Education and training
Considering how venous stenting practice can be improved, Desai believes education is key. “I think most providers would be open to the discussion that ‘maybe your stent is not helping patients,’ and would correct their behavior,” he says, while remarking that it is “much more difficult to correct” the practice of providers who are financially driven. “More broadly speaking,” however, he is confident that education remains central “for providers that are willing to listen.” Black points out that a number of educational efforts are in place—from company-run symposia and training to workshops at vascular meetings. He stresses however that training is a “two-way thing.” He explains: “You have to engage in training.”
Looking at the wider picture, Black highlights that, while vascular care “continues to suffer from an unreasonable focus on aortic disease,” there is a “huge opportunity in the treatment of venous disease to make a really big difference to a patient’s quality of life.”
With this in mind, he encourages “all vascular enthusiasts” to commit to collecting the data, partaking in the training, and delivering the appropriate care that should be the hallmarks of venous stenting’s next chapter. Chaer says the venous stenting space has come a long way but looks forward to further improvements to come—“in terms of more data as it pertains to the existing stents, and maybe looking at the hybrid designs, so to speak, to see how these will perform.”
Registry analysis finds women benefit from endovenous ablation with fewer complications
VARICOSE VEINS
AN EVALUATION OF THE VASCULAR QUALITY Initiative’s (VQI) Varicose Vein Registry (VVR) carried out by the Midwestern Vascular Surgical Society (MVSS) found women to benefit similarly from endovenous ablation as men, but that they experience fewer complications post-procedure (writes Eva Malpass)
The MVSS study prospectively collected data from the VVR—a registry included within the Society for Vascular Surgery’s VQI. Uniquely, the VVR includes
both patient-and physician-reported outcomes.
Using these data, Benjamin A. Y. Cher, MD, from the University of Michigan, and colleagues conducted a retrospective cohort evaluation of patients undergoing endovenous ablation procedures on truncal veins with or without treatment of perforated veins between 2015 and 2019.
Cher and colleagues summarized that their findings demonstrate a similar benefit from endovenous
ablation between women and men, with little incidence of post-procedural complications for both. However, considering the study’s procedural registry included almost twice as many women as men, findings which suggest a greater benefit from treatment for women are particularly significant.
The findings were published in the Journal of Vascular Surgery: Venous and Lymphatic Disorders (JVS-VL), November edition
6 Vascular Specialist | February 2023




Partner Driving Change. TOGETHER. REFERENCE: - Technical and Clinical Outcome of Topical Wound Oxygen in Comparison to Conventional Compression Dressings in the Management of Refractory Nonhealing Venous Ulcers. Wael A. Tawfick WA, Sultan S. s. Vascular Endovascular Surgery 2013; 47:30–37 Delivering Exceptional Outcomes Multi-modality Therapy for VLUs. Combining non-contact cyclical compression, oxygen and humidification, this seamless addition to your care plan can be used in any clinical setting or self-administered by the patient at home, improving compliance and access to care for all. Faster, Sustained Healing for Venous Leg Ulcers Visit www.AOTInc.net for more information BE A PART OF THE CHANGE HIGHER HEALING RATE at 12 weeks 46% 76% | vs. SOC* LOWER RECURRENCE RATE at 36 months 47% 6% FASTER TIME TO HEALING 107 DAYS 57 DAYS MRSA ELIMINATION 0% CCD 46% | vs. SOC | vs. SOC | vs. SOC *Standard of Care (SOC) was Conventional Compression Dressings (CCD)
Proud
VENOUS ULCERS
SURGICAL THERAPY
A single-center evaluation of contemporary, multi-modal surgical therapy for venous stasis ulceration (C6 disease) suggests highrisk patients showed similar healing rates at one year, indicating a variety of intervention types should be pursued to achieve “optimal results,” writes Eva Malpass.
PRESENTED AT THE SOUTHERN Association for Vascular Surgery (SAVS) annual meeting (Jan. 18–21), Rachel Reed, MD, a general surgery resident at Emory University in Atlanta, outlined the “significant burden” chronic venous disease (CVD) places on both patients and the U.S. healthcare system.

Reed and colleagues conducted a retrospective review of patients treated with C6 disease at a single, public academic hospital between 2011–2021, with at least 12-months follow-up. She noted that there are currently “limited data” regarding combined surgical therapy in venous disease, introducing their study as the “only” one performed looking at multiple types of surgical intervention.
Their primary outcome measure was
defined as ulcer-free survival at one year following initial surgical intervention, which included venous ablation, deep venous stenting, and open deep venous valvuloplasty.
Patients were classified using the Clinical, Etiological, Anatomical, and Pathophys iological (CEAP) system, which categorizes C6 disease as its most severe form of venous disease, assessed by a multidisciplinary team.
Reed addressed several comorbidities
characterizing the “high-risk” cohort, such as “diabetes, elevated body mass index [BMI] and active insurance”—specifying that 60% of the included population were classified as obese with a BMI greater than 30, and 35% had a prior history of deep vein thrombosis (DVT).
Producing the results, Reed identified the 80 interventional procedures included in their review, segmenting these into 70% ablation, the most frequent treatment used; 21.3% stenting; and 10% deep venous reconstruction (DVR). Their findings showed 54% of patients were ulcer-free at 12-month follow-up, but no significant demographic disparities were found between patients who healed and those who did not.
“Of note, those with high-risk features, including diabetes and elevated BMI, healed at a similar rate to those without,” Reed told SAVS 2023 attendees.
Overall, 37.7% of patients required more than one type of procedure; 71.7% underwent isolated venous ablation; 13.2% received isolated iliac vein stenting; and 1.8% were treated with isolated valvu-


loplasty. Elucidating the data further still, she emphasized a prevalent “trend” that showed that patients who required multiple types of intervention to obtain durable venous healing were more likely to have ulcer resistance at 12 months—most likely “highlighting the severity of their disease,” Reed determined.
Yet, despite the number or type of procedure that were performed, no “statistically significant difference” was observed in the level of ulcer healing, Reed stated.
When the researchers segmented healing rates of patient limbs by intervention type, she explained, concomitant iliac vein disease appeared to be “associated with reduced ulcer healing at one year,” suggesting iliac vein stenting is associated with poor ulcer healing compared to those individuals who did not require this procedure.
The research team’s findings suggest that high-risk features such as diabetes and increased BMI are “not predictive” of poor ulcer healing, with patients from both cohorts healing at “similar” rates, Reed and colleagues concluded.
However, when considered after multivariable regression, Reed saw that significant demographics appeared to be “increased age and lack of insurance” as indicators of reduced healing at 12 months. “Chronic venous disease remains a challenging disease to treat and in which to obtain durable venous healing,” Reed contended. “Future studies will need to be performed on optimal treatment pathways for these patients.”
Meta-analysis of post-thrombotic syndrome finds one in five at risk of long-term symptoms following isolated distal DVT
Anew meta-analysis is the first to report the pooled risk of post-thrombotic syndrome (PTS) after isolated distal deep vein thrombosis (DVT). Researchers revealed a onein-five risk of long-term PTS after isolated distal DVT, with one in 50 patients progressing to severe PTS, potentially developing to ulceration.


Principal author Benedict Turner, MBChB, from Imperial College London in London, England, and colleagues evaluated The Cochrane Library, Embase, Google Scholar and MEDLINE databases, following PRISMA guidelines to identify eligible prospective cohort studies analyzing the rate of PTS after a first episode of isolated distal DVT.
Published in the European Journal of Vascular and Endovascular Surgery, the study comprised trials held between 2005 and 2021 that included between 52 and 403 participants, with a total of 1,105 included across all seven studies reporting the development of PTS.
Turner et al note that the baseline characteristics of included articles were varied—follow-up periods ranged between one month to four years after the first DVT, and several studies additionally reported which of the distal deep veins were thrombosed and corresponding risk factors.
Interventions used to treat PTS included stockings, though duration, adherence and degree of compression were heterogenous. Other patients also received anticoag-
ulation, although duration of treatment was unspecified. Among patients who were anticoagulated, direct oral anticoagulants, low molecular weight heparin and vitamin K antagonists were used.
The authors report that one in five patients are at risk of long-term PTS after isolated distal DVT, with one in 50 experiencing severe symptoms that may potentially include ulceration.
Going into detail, the authors observed a post-thrombotic rate of 17% ( p<0.01) across the seven studies, 217 cases and 1,105 participants. Three of these studies (302 patients) reported on the severity of PTS symptoms, 78% posited as mild (Villalta score 5–9), 11% as moderate (10–14), and 11% were severe (15 or more).
Even when modulating the follow-up period, the authors did not see a significant change in the risk of developing PTS (p=0.71). This, they write, suggests shorter follow-up periods may be adequate to collect data on symptom development in clinical trials.
The authors note that methods of data collection may have been “confounding” due to recall bias, as most of the included studies only reported rates of PTS at the average follow-up duration, rather than pinpointing the exact time at which PTS was diagnosed.
Overall, Turner and colleagues state that the risk of PTS
after isolated distal DVT appears to be half that in comparison to proximal DVT, although occurring in a similar timeframe. According to the authors, this information is key when considering anticoagulation duration and compression therapy, as “PTS is noted to be the principal moderator of quality-of-life after VTE [for patients].”

When considering preventative measures that can be taken by patients, the authors note that the most recent European Society for Vascular Surgery (ESVS) guidance recommends graduated compression stockings in the proximal context of DVT to prevent the onset of PTS, despite the UK National Institute for Health and Care Excellence and American College of Chest Physicians withdrawing this treatment option since it demonstrated no additional benefit in the SOX trial.
The authors highlight that analysis of stocking use is limited. They detail that trials, including CHAPS, SOX and ATTRACT, have set about evaluating the treatment for preventing PTS. However, they each excluded distal DVT from their eligibility criteria due to assumed lower event rates, although it may constitute up to two thirds of all DVT cases.
The investigators conclude that randomized trials to analyze and support interventions that can effectively prevent PTS are “urgently needed” to improve patient care and subsequent outcomes after isolated distal DVT.—Eva Malpass
8 Vascular Specialist | February 2023
HIGH-RISK CVD PATIENTS WITH VENOUS STASIS ULCERATION SHOW SIMILAR HEALING RATES AFTER MULTI-MODAL
VTE
“Chronic venous disease remains a challenging disease to treat and in which to obtain durable venous healing”
RACHEL REED












NOW WITH 24-MONTH WARRANTY BD reserves the right to terminate this program at any time. Please note, signed Lutonix™ DCB Reintervention Free Warranty Purchase Agreement terms and conditions apply. Please consult product labels and instructions for use for indications, contraindications, hazards, warnings and precautions. BD, the BD logo, and Lutonix are trademarks of Becton, Dickinson and Company or its a liates. © 2023 BD. All Rights Reserved. © 2023 Illustration by Mike Austin. BD-68109v2 bd.com BD, Tempe, AZ, USA, 1 800 321 4254 Go with the DCB Backed by a 24-Month SFA Reintervention-Free Warranty BD is proud to back Lutonix™ DCB with a 24-month SFA reintervention-free warranty. Under the warranty, if you treat a patient with a Lutonix™ DCB, per the IFU, during the contract period, and that patient returns for a reintervention of the original target lesion within 24 months of the initial treatment, then a no-charge replacement code will be sent to your account. Contact your local BD sales representative for more details.
SOUTHERN VASCULAR ROUND-UP
FROM THE COVER: PRESIDENT REVEALS UPCOMING CHANGE TO SOCIETY SEAL
patients without obtaining their consent for medical research. While accepted then, it would be considered inappropriate today. In our efforts to improve our Society, we turn our eyes to the future.”
Jordan said the Society leadership is focused on exploring ways in which SAVS can meet the needs of the current and future generations of vascular surgeons.
“As a sign of this commitment,” he said, “your Executive Council voted to redesign our Society’s seal, create a new seal that will exhibit the standards of our professional society, and remains true to our mission of promoting the art and science of vascular surgery and providing comprehensive vascular care.” SAVS members are being asked to participate in the redesign: “Submit your ideas and be creative,” Jordan added. Bryan Kay
The case for aggressive intervention on symptomatic carotid web
The lead investigator behind new research from a center in Louisiana outlines how his new study— believed to be the largest single-institution analysis of symptomatic carotid web yet reported—shows that carotid duplex is “inadequate” for diagnosis, and medical management is “unacceptable.” The results, he tells Bryan Kay, reveal potential clues to possible genetic risk factors.
THE APPROPRIATE MODALITY USED FOR DIAGNOSIS, treatment method and characterization of symptomatic carotid web could be key to tackling a condition that has been shown to result in high rates of recurrent stroke when managed with medical therapy alone, according to a new study carried out by Clayton Brinster, MD, and colleagues at Ochsner Health in New Orleans.
Because there is no bulky athereosclerotic lesion in the carotid bulb in the case of the shelf-like projection redolent of carotid web, the staff surgeon tells Vascular Specialist , this pathology “is often overlooked as an etiology of acute anterior circulation stroke.”
Brinster recently presented data from a rare 52-patient series from his institution at the 2023 annual meeting (Jan. 18–21) of the Southern Association for Vascular Surgery (SAVS) in Rio Grande, Puerto Rico, that led him to conclude that medical management is “no longer an option” to treat carotid web. Over the six-year study period (2016–2022), the Ochsner researchers identified an average age of 49 years among their cohort of patients—71% of them women, two-thirds African American, and more than a third African-American women under the age of 50. Some 90% presented with stroke, Brinster told SAVS 2023. None were initially diagnosed using carotid duplex, he said. “Definitive treatment consisted of carotid endarterectomy and carotid artery stenting.”
Brinster’s subsequent conclusions were bold. “To our knowledge, this is the largest single-institution analysis of symptomatic carotid web yet reported,” he said. “Our series demonstrates that carotid duplex is inadequate for diagnosis, and that medical

THE SOUTHERN Association for Vascular Surgery (SAVS) announced its 2023–24 slate of officeholders following the conclusion of the 2023 SAVS annual business meeting.
The member-only proceedings marked the conclusion of the 2022–23 presidency of William D. Jordan Jr., MD, chief of the division of vascular surgery and endovascular therapy at Emory University in Atlanta.

David L. Cull, MD, professor of surgery at the University of South Carolina in Greenville, became SAVS president for the 2023–24 term, which took place at the end of the 2023 SAVS annual meeting.
Alan Lumsden, MD, the Walter W. Fondren III Presidential Distinguished Chair of the DeBakey Heart & Vascular Center at Houston Methodist, is the new president-elect.—Bryan Kay
FUNDING
Presenting at the 2023 SAVS annual meeting in Rio Grande, Puerto Rico, Amin A. Mirzaie—a pre-medical student at Emory University—offered observations on The National Institutes of Health’s (NIH) “modestly” aligned vascular surgical funding distribution in the context of the current Society for Vascular Surgery (SVS) priorities.
Mirzaie began by remarking on contemporary delegation of NIH funding, referring to a “precipitous and slow decline” in public service funding in the period 2006–2016. Yet, during the same time period, he continued, the NIH received a US$2 million budget increase, spurring Mirzaie and fellow authors to investigate the char-
acteristics of “rare” NIH-funded projects granted to vascular surgeon-scientists. They sought to extract the amounts, types and content areas, and determine their alignment with current SVS research questions—rhetorically setting their research intentions for the audience, Mirzaie asked: “Who is being funded? […] Do funded projects align with SVS priorities?”
Estimating a total of $12 million is awarded to “all active projects,” Mirzaie et al extracted grant research characteristics in instances where a vascular surgeon was a principal investigator (PI). Identifying 53 active NIH awards given to 40 U.S. vascular surgeon-scientists, Mirzaie reiterated that
“only 1%” are receiving these awards. He noted funded vascular surgeon-scientists are an average of 15.9 years out of training, with 37.5% being women—“much higher” than other sub-specialties.
On NIH and SVS research priorities, Mirzaie posed that eight out of 53 active projects given to vascular surgeon-scientists “directly addressed” any SVS primacies. He noted that four SVS priorities included in the most recent 2021 refresh were not “fulfilled by any NIH projects.”
“Moving forward this shows that we need more funded vascular surgeons and better coverage of SVS priorities,” said Mirzaie.—Eva Malpass
10 Vascular Specialist | February 2023
continued from page 1
SAVS UNVEILS LINE-UP OF 2023–24 OFFICEHOLDERS
The catastrophic potential of carotid web
Case of a 39-yearold male, permanently hemiparetic on the dominant side
NIH funding for vascular surgeon-scientists: ‘We need more funded vascular surgeons and better coverage of SVS priorities’
RESEARCH
1 2
Alan Lumsden
management is unacceptable for symptomatic carotid web. Recurrent stroke occurred in all patients managed early in our experience with medical therapy alone. We have since adopted an aggressive interventional approach in cases of symptomatic carotid web, with no postoperative stroke reported over an average follow-up of 26 months.”
The findings offer key insights, Brinster reflects in an interview with Vascular Specialist after the SAVS meeting. For one, when confronted with a patient who has minimal carotid stenosis, especially a younger patient, “and especially a younger African-American woman under 50 years old, which comprised one third of our series—astronomical when you think about it—this pathology must be ruled out,” Brinster explains. “And the most efficient way to rule that out in a stroke patient is with a high-powered CTA, particularly examining the sagittal projections, That is really where carotid web is most readily identified. It is very easy to miss in the axial and the coronal projections in the scan.”
Clayton Brinster
FMD occurs distally in the internal carotid artery—anatomically in a different region. It appears radiographically totally differently than web. Web appears as a shelf-like projection in the carotid bulb, whereas FMD has a very classical string-of-beads appearance in the more distal carotid. Third, the pathologic specimens of carotid web are completely different than pathologic and histologic examination of traditional FMD.” The concerning point, Brinster says, “is that referring to carotid web as simply a form of carotid FMD—which has a well-established treatment paradigm that includes medical management and balloon dilation—I think confuses practitioners.”
This may lead to either undertreatment, or mistreatment, and recurrent stroke in these patients, he argues. “It would be totally inappropriate to balloon angioplasty these lesions,” Brinster adds, with the risk of recurrent stroke “astronomical.”
alluded to a genetic basis ,from Central and West African descent, through the Caribbean.” The historical migration patterns of the American South, particularly through the port of New Orleans, “is no coincidence” in the context of the findings contained in the series presented by the Ochsner group, Brinster points out. He now hopes to join forces with the physicians behind the Caroweb registry, first by creating and leading a national consortium in the U.S.
“The more people who know about it and the more people involved, the more strokes we can prevent,” Brinster says. “I can’t tell you how many people came up to me at the Southern meeting, and said, ‘I have seen this once or twice before and I didn’t know what to do. Now, I will.’ There is a lot more work to be done for these patients.”
Second, carotid web demands its own characterization, Brinster says. In the literature, the condition has traditionally been referred to as a form of carotid fibromuscular dysplasia (FMD), he notes.

“In addition to medical management being totally unacceptable for symptomatic carotid web, carotid web needs to be thought of as an independent pathology from traditional carotid FMD,” Brinster relates. “Traditional carotid
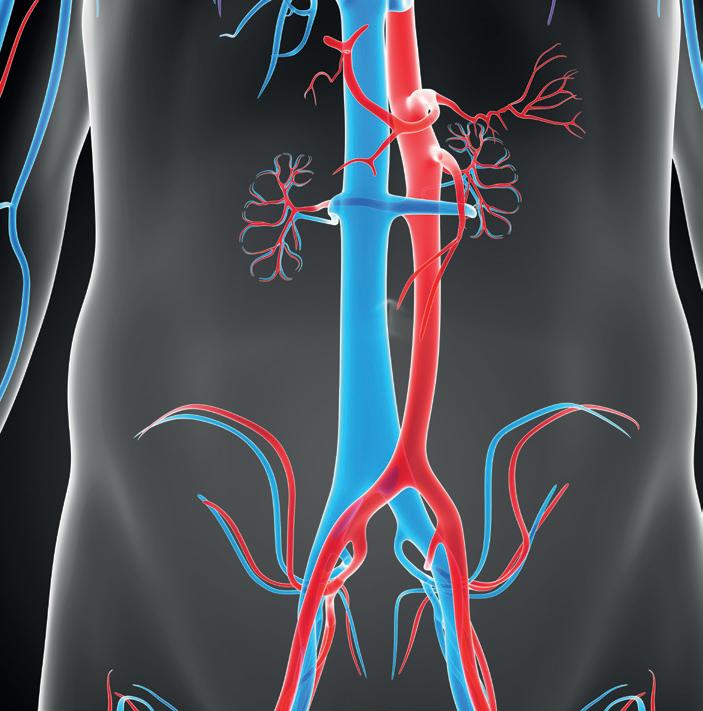
AAA
FIVE-YEAR OUTCOMES OF ESAR IN PATIENTS WITH SHORT NECK
Cohort analysis shows no migrations, a low rate of ruptures, and positive sac regression, researchers say.
FIVE-YEAR OUTCOMES IN PATIENTS
with short neck abdominal aortic aneurysms (AAAs) undergoing endosuture aneurysm repair (ESAR) using Heli-FX EndoAnchors with an Endurant stent-graft in the ANCHOR registry showed a freedom from all-cause mortality of nearly 70%,


Meanwhile, that younger African-American female portion of the cohort is set to form the basis of at least one dimension of further digging. Thus far, Brinster says the group have only performed a pathologic evaluation on the cases they have analyzed. But, he continues, “what we really need to do is a fresh tissue analysis, and a genetic analysis of the tissue,” he reveals. “If this is based on sex and race, then it most certainly must have a genetic component. The larger French registry [of carotid web cases], called Caroweb, has
from aneurysm-related mortality of 90%, from aneurysm rupture of 95.6%, and from any secondary procedures of 77%, lead study author Frank R. Arko, MD— who disclosed a consultancy relationship with and receiving research funds from device maker Medtronic—told SAVS 2023.
The cohort, with a mean age of 72, included 70 patients with an infrarenal neck length greater than 4mm and less than 10mm enrolled from 2012–2015 and fitted with the Heli-FX EndoAnchor system, which was designed to improve the fixation and seal of aortic stent-grafts. At five years, the patient group had clinical and imaging follow up compliance rates of 85% and 70%.
Some 11 patients had a total of 16 secondary procedures. None of the conversions had open repair that were for type Ia
There are hurdles to be crossed, but a potential roadmap appears to be forming. And that could involve a screening dimension.“If we try to prove some sort of genetic disposition, that could lead to more effective screening,” Brinster says. “It may be worth screening family members of those with carotid web to rule out the pathology.” Still, carotid web is a “very tricky thing to screen for without a family member who has been diagnosed, and because ultrasound is not as reliable as CAT scans, and CAT scanning, of course, is expensive and you need contrast,” he adds.

Ultimately, an opportunity beckons, Brinster says. “We have an opportunity with the size of the series, and the fact it was presented at the Southern [annual meeting], to change the way people manage carotid web—and hopefully avoid recurrent strokes in a vulnerable population.”
endoleaks, although there were patients who had this type of endoleak, Arko said. “The type of secondary procedures were endovascular in the majority, and there were three conversions to open repair.”
Through five years, eight had type Ia endoleaks, three of which were resolved by the next follow-up, reported the vascular chief from Sanger Heart & Vascular Institute in Charlotte, North Carolina. There were two type Ib endoleaks, 13 patients who had a type II, and there were no type III endoleaks.
After five years, 68.2% of the registry subjects had sac regression, 13.6% had stable sacs, and 18.2% had increased sac diameter as compared to their one-month measurements, the study authors showed.
“Patients with infrarenal necks of between 4 and 10mm implanted with the Endurant II/IIs in combination with the Heli-FX EndoAnchor system showed durability of treatment through five years,” Arko concluded before the SAVS 2023 gathering in Rio Grande, Puerto Rico. “There is a need for close and lifelong surveillance in these patients with hostile necks due to occurrence of late events that appears to be appearing at around the three-year time period.
“The study is certainly limited by the small sample size and further prospective randomized controlled trials are needed, and these will be performed in the near future.”—Bryan Kay
www.vascularspecialistonline.com 11
Frank R. Arko
A close-up example of thickened carotid web
Removal of thrombus via CEA, or carotid endarterectomy
“ We have adopted an aggressive approach in cases of symptomatic carotid web, with no postoperative stroke reported over followup of 26 months”
3 4
CLAYTON BRINSTER
BEST-CLI: ANALYSIS FINDS CORRELATION BETWEEN WIFI STAGE FOUR AND REPORTS OF POORER MENTAL HEALTH
The BEST-CLI dataset has revealed a correlation between wounds, ischemia and foot infection (WIfI) stage and poorer quality of life due to mental, rather than physical, health for patients with chronic limb threatening ischemia (CLTI), writes Eva Malpass.


Analyzing complete WIfI data from a total of 1,568 enrollees, the prospective randomized BEST-CLI trial compared open and endovascular revascularization strategies for patients with CLTI due to infrainguinal peripheral arterial disease (PAD). The study assessed health-related quality of life (HRQoL), which was the prespecified secondary endpoint of the trial and was used at enrollment and designated follow-up points. This measurement included data from multiple surveys, including the Vascular Quality of Life questionnaire (VascuQoL); 12-item short-form survey (SF-12), including the utility index score (SF6D-R2), mental composite scale (MCS), and physical composite scale (PCS); and EQ-5D. The results were recently published online in the Journal of Vascular Surgery (JVS).
Jeffrey Siracuse, MD, a professor of surgery and radiology at Boston University School of Medicine in Boston, and colleagues sought to establish a correlation between limb severity and health-related quality of life, including details specifically connected to the affected limb and post-intervention changes in preoperative HRQoL scores.

Distribution between WIfI stages was: 35.5% reporting stage four, 29.6% with stage three, 28.6% with stage two, and 6.3% with stage one. Analyzing these groups further, the authors found that patients presenting with WIfI stage four were more often men (74.9% vs 69.6%), current smokers (25.4% vs. 17.6%), had end-stage renal disease (13.3% vs 8.5%), diabetes (83.6% vs 60.2%), were not
independently ambulatory (56.8% vs 38.5%), and had higher median morbidity scores (4 vs 3; p<0.05).
Examining the correlation between WIfI stage and the other assessment modes, the authors found stage four to be associated with worse/lower SF-12 mental component scale scores (estimate, -2.43; 95% confidence interval, -3.73 to -1.13; p<0.001) and SF6D-R2 scores (estimate, -0.02; 95% confidence interval, -0.03 to 0.001; p=0.04).
Siracuse et al state that patients presenting with an advanced WIfI stage had lower HRQoL assessments related to their mental health, however, the remaining assessments (VascuQoL, SF-12 PCS, and EQ-5D), which focused mainly on physical health, did not show a correlation with advanced WIfI stage. The authors note that WIfI stage four had VascuQoL scores that were comparable to groups one to three (-0.12; 95% CI, -0.25 to 0.02; p=0.09), though female sex, current smoking and preoperative opioid use were associated with a lower score. These factors were also associated with lower SF6D (-0.02; 95% CI, -0.03 to 0.001; p=0.04) and SF-12 MCS (-2.43; 95% CI,

-3.73 to -1.13; p<0.001) and PCS (0.04; 95% CI, -0.89 to 0.97; p=0.93) scores. However, they were not found to affect a lower EQ-5D score (-1.85; 95% CI, -4.22 to 0.52; p=0.13).
“The presence of concurrent mental stress is important in patients with CLTI and has most likely been undertreated,” Siracuse et al conclude. Analysis has been previously carried out on the relationship between mental health and CLTI—The Nottingham Health Profile’s study demonstrated a significant correlation between HRQoL in patients with PAD and difficulties in work, family life and hobbies.
The researchers pointed out that, unlike mental health assessments, the physical assessments did not correlate with advanced WIfI stage, however emphasized that this disparity may be due to scores being low across all stages. Development of a “CLTI-specific” instrument to evaluate HRQoL is needed, Siracuse et al determine.
“An improved understanding of HRQoL considerations could better guide care for this complex and vulnerable patient population and enhance patient engagement for joint decision-making.”
12 Vascular Specialist | February 2023 Vascular’s Premier Educational VASCULAR.ORG/VAM June 14 to 17 / Exhibits: June 15 to 16 GAYLORD NATIONAL RESORT & CONVENTION CENTER National Harbor, Md , outside of Washington D C The latest research Practice management tips Industry innovations and presentations Engaging social events, including the ‘Great Gatsby Gala’ Featuring: And much more Registration opens in mid-March Register early to take advantage of our new early-bird pricing
PAD
“The presence of concurrent mental stress is important in patients with CLTI and has most likely been undertreated”
JEFFREY SIRACUSE
Jeffrey Siracuse
Vascular surgery oral boards text seeks to fill certifying void

A new reference textbook for trainees is proving a hit among those readying for the vascular surgery oral board exam, the authors tell Bryan Kay.



Think of it as the omega of the vascular surgical textbook literature, quips Andrew M. Wishy, DO. As a training resource, it fits neatly on the trainee bookshelf on one side— the end to a partner title, The Vascular Surgery Review Book, the alpha, or the beginning, on the other.
He is referring to Vascular Surgery Oral Board Review: Behind The Knife Premium, a textbook aimed at vascular surgery trainees taking the Vascular Surgery Board (VSB) Certifying Exam (CE), a work he helped craft and publish last year alongside colleagues Ravi N. Ambani, MD, and Kevin R. Kniery, MD, the latter known as a founder of popular surgical podcasts, Behind the Knife and Audible Bleeding
Like the author of The Vascular Surgery Review Book, Wishy, Ambani and Kniery produced their title to provide a training resource and help fill a void they identified as they made their way through their own training. The idea germinated as they studied together to take the VSB CE, realizing there was a lack of available material with which to prepare.
“Both Ravi and Kevin were general surgeons first and had
CAROTID DISEASE
been through the oral board before in the general surgery realm,” explains Wishy, who, in contrast, completed his training under the integrated vascular surgery residency pathway. “We always practiced and tried to simulate these kinds of things for the integrated resident like me in our training institution: How is this really going to go? How is the back and forth going to be between the examiner and examinee? What kind of information are they going to want me to know? What’s too much? What’s not enough?”
As the CE preparation process was new to Wishy, that made him the perfect foil as the trio fine-tuned exactly what the textbook required. The ensuing text is comprehensive, he says.
“From cover to cover, you’re probably going to hit every high-yield topic there is [in vascular surgery], with every most-common procedure performed, and I would say the most common complications that I’ve ever ran into in practice, in the textbooks or heard from other people,” Wishy continues. “It’s not an all-inclusive resource by any means, but I think it’s a very good starting point, and covers the whole breadth of all the major and minor topics.”
The book has already proven a success among trainees since it was published last year, explains Ambani. “The three
it was best to get the cases and material we used down on paper, and get it published,” he says. “After this last round of oral boards, a bunch of people messaged to say that this was the only thing they used, and that they were successful and passed.”
Ambani reckons the two reference titles— their Vascular Surgery Oral Board Review: Behind The Knife Premium and Creeden’s The Vascular Surgery Review Book—meet vascular surgery at a crucial juncture. “Vascular surgery as a group is growing,” he says. “It’s becoming one of the most competitive specialties to match into after general surgery and after medical school, so the volume of trainees keeps going up and the interest keeps peaking. We have our own boards, so it’s time for us to develop resources to help people study for those specialty boards. The resources that exist currently are aimed at general surgery as a whole.”
Top:
of us were able to pass our boards on the first attempt, and once we had the proof of concept that we did well, and now that we’re all Board-certified vascular surgeons, we thought
SEX FOUND TO BE ‘IMPORTANT VARIABLE’ IN STUDY AND TREATMENT OF CAROTID ATHEROSCLEROSIS
A systematic review and meta-analysis have demonstrated “convincing evidence” that sex differences exist in carotid atherosclerosis, with all types of plaque features—including those relating to size, composition, and morphology—found to be either larger or more common in men than in women, reports Jamie Bell.
“OUR RESULTS HIGHLIGHT THAT sex is an important variable to include in both study design and clinical decision-making,” the authors, led by Dianne van Dam-Nolen, MD from the Department of Radiology and Nuclear Medicine at Erasmus University Medical Center, in Rotterdam, The Netherlands, write in the journal Stroke. “Further investigation of sex-specific stroke risks with regard to plaque composition is warranted.”
Over the past few decades, several individual studies on sex differences in carotid atherosclerosis have been performed, covering a wide range of plaque characteristics and including different populations, van
Dam-Nolen et al state. Their study began by systematically searching PubMed, Embase, Web of Science, Cochrane Central and Google Scholar for eligible studies, including both male and female participants, and reporting the prevalence of imaging characteristics of carotid atherosclerosis. The eligible studies were then meta-analyzed. Van Dam-Nolen et al prespecified which imaging modalities had to be used per plaque characteristic and excluded ultrasonography.
After identifying more than 1,000 unique citations, screening whittled this number down to 60 articles, with 42 being included in the final meta-analyses.
Six of these studies were included in a meta-analysis on the relationship between sex and atherosclerotic plaque size. All three of the characteristics used to measure plaque size—maximum wall thickness (1D size), wall area (2D size), and wall volume (3D size)—were more likely to be larger in men than in women, van Dam-Nolen et al report.
However, conversely, the normalized wall index, which accounts for the total vessel size, did not show a statistically significant difference between male and female participants, which the researchers describe as “surprising,” and possibly indicative of sex differences in plaque size being driven by contrasting vessel sizes.
In addition, analyzing three of the studies further regarding the degree of stenosis, the authors found no statistically significant sex difference for stenosis of 50–69%, although high-grade stenosis of 70–99% was more often seen in men than in women.
Meta-analyses relating to plaque composition examined the presence of calcifications, lipid-rich necrotic core (LRNC), and intraplaque hemorrhage (IPH), and found a higher prevalence in men versus women across all three components.
Expounding briefly on their calcification findings, van Dam-Nolen et al report statistically significant differences between men
The textbook tandem is “like a one-two punch,” Ambani adds. The Vascular Surgery Review Book plugs a hole for those the preparing for the Vascular Surgery In-Training Exam (VSITE) and the VSB Qualifying Exam, while Vascular Surgery Oral Board Review: Behind The Knife Premium slots into the oral boards, or CE, realm. “Together, they are synergistic. They both came out a couple of months apart. These both are super useful in different ways, and together relatively low-cost resources for trainees that get them through their entire training—and hopefully through their boards.”
and women for the presence and amount of carotid calcifications, but not in terms of calcification percentage i.e. the amount of calcification relative to the total plaque volume.
“Furthermore, we found more pronounced sex differences for LRNC in symptomatic as opposed to asymptomatic participants,” they add.
Five studies were also included in the meta-analysis of the relationship between sex and plaque morphology, with the presence of ulceration and the presence of a thin-or-ruptured fibrous cap both being higher in men.
“The found sex differences in carotid atherosclerosis are of clinically significant importance, since the composition of plaque affects the risk of (recurrent) stroke,” van Dam-Nolen et al conclude.
“Previous studies have shown that especially IPH contributes to a higher stroke risk. Carotid LRNC, calcifications, total plaque size, and plaque ulceration, have also been reported as important risk factors. With regard to sex-specific risk prediction and treatment, it is essential to investigate the effect of these plaque characteristics per sex separately. We hypothesize that the stroke risk as a result of specific plaque compositions varies among men and women.”
www.vascularspecialistonline.com 13
“From cover to cover, you’re probably going to hit every high-yield topic there is”
VSB
ANDREW M. WISHY
Andrew M. Wishy, left: Ravi N. Ambani, right: Kevin R. Kniery
Innovations and Exploration in Venous Interventions





April 27-29, 2023 | Miami Beach, FL


COURSE DIRECTORS

21st ANNUAL
Jose I. Almeida MD, FACS, RPVI, RVT
Edward G. Mackay MD, FACS, RPVI, RVT
Lowell S. Kabnick MD, RPhS, FACS, FACPh
REGISTER TODAY AT ivcmiami.com MANAGED AND ACCREDITED BY
New Government Grand Rounds series highlights how perspective matters in advocacy
Matthew Sideman, MD, and Megan Marcinko, MPS, unveil new advocacy column aimed at drilling into the actions of Congress, and how they impact vascular surgery. The first in the series looks at advocacy as a tool to “protect.”
Welcome to “Government Grand Rounds,” where we will examine and discuss how the actions of Congress and regulatory agencies affect vascular surgeons and the patients they serve, and importantly, how sustained advocacy engagement is important for all SVS members.
“Advocacy” continues to rank high among SVS member priorities, and yet many remain unsure how to support SVS advocacy-related programs, what activities are available and how to measure success along the way.
Foundational in this series is the notion that perspective matters. Like all aspects of life, the importance of any given activity, goal or initiative is measured via the eye of the beholder. Advocacy is no different, with everyone engaging, or not engaging, based on their interests, level of understanding and sense of urgency related to the issue at hand.
To enhance our perspectives on advocacy, this series will highlight some of the most important tools that advocacy provides us. This month we will examine advocacy as a tool to protect. How does “protect” relate to advocacy? As you
YOUR SVS
STRATEGIC PLANNING SESSION OUTLINES SVS PRIORITIES FOR COMING YEAR
By Marlén Gomez
KEY LEADERS FROM THE SOCIETY for Vascular Surgery (SVS) gathered in mid-January for a two-day Strategic Board of Directors (SBOD) meeting to work through the Society’s six strategic domains.

SVS Executive Director Kenneth M. Slaw, PhD, noted, “The SBOD provides a global and diverse perspective on SVS priorities; members selected from the major vascular societies represent the full spectrum of demographics and practice settings and keep the overarching needs of the entire specialty in mind as they work to set SVS priorities.”

The strategic domains focus on advocacy, education, clinical practice, quality, research and the overall health of the SVS.
“Through discussions of each domain, our Strategic Board of Directors provides the overarching strategy and directional objectives for the Society’s work over the next year but, more importantly, with an eye to a three-to-five-year horizon,” said SVS President Michael Dalsing, MD.
Slaw emphasized the importance of positioning vascular surgeons to provide optimal care for their patients while working to
may have guessed, it depends on your perspective and what you believe your role in the healthcare delivery system to be. Consider the following: as a vascular surgeon, is it “part of the job” to do the following and, if so, how?
◆ Protect patient access to care
◆ Protect the physician-patient relationship
◆ Protect the future of private/community practice
◆ Protect the autonomy of physician decision-making
◆ Protect the value of quality vascular care
Lawmakers and regulators are constantly considering health policy-related changes that will impact the practice of medicine. Stakeholder engagement is among the few tangible mechanisms for policy-makers to learn and, hopefully better understand, the real-time impact of their decisions.
Absent sustained engagement from those within the healthcare delivery system, lawmakers lack the perspective relating to what a suggested policy (which may look good on paper) would mean in a practical or operational sense. In other words, becoming involved in advocacy is a tangible action to protect against bad policy becoming law and help to reinforce and/or shape the system in which you are providing care for your patients.
While this might seem like a simplistic perspective, it is actually a realistic assessment relating to the value of advocacy. If the SVS, as a whole and via its individual members, fails to engage in the policy-making process, we are ceding the collective expertise of our members and the importance of this experience regarding how policy translates to practice.
You may have heard the saying, “If you’re not at the table, you’re on the menu.” Let’s work together to engage policy-makers to the greatest extent possible. By doing so, we can not only secure our seat at the table, but also play a role in determining what is served.
For more information about how the SVS’ Advocacy programs help protect vascular surgeons and the patients you serve, visit vascular.org/advocacy
ensure they have a fulfilling, rewarding and valued career.
Advocacy
Members across SVS worry about the survival of vascular surgery within the current health policy and delivery system. Megan Tracci, MD, vice chair of the SVS Advocacy Council, and Megan Marcinko, SVS director of advocacy, led the conversation on the pressing issues regarding the vascular surgery payment policy.
“It is obvious that we need to continue to work within the system to represent our members on the Hill but more is needed, and lively discussions regarding proactive options were entertained,” said Dalsing.
“It was good to see the enthusiasm and brainstorming that took place and suggests that a second payment summit needs to be convened. Vascular surgeons need to sculpt and map out a new future for vascular health delivery.”
Education
Plans for the coming year include building an enhanced online education platform to provide members with both formal education and “micro-learning” opportunities. “SVS Presents,” a monthly webinar series, is scheduled to begin in April, and will provide an evening of programming members can access at any time. The next version of the Vascular Education and Self-Assessment Program (VESAP), the online learning assessment and self-study tool, is in the works for later this year. In
addition, education leaders plan a Vascular Annual Meeting Education Retreat for the fall to prepare for VAM for the next three to five years. Education Council Chair Linda Harris, MD, and Lisa Cohen, SVS director of education, presented the information.
Clinical practice
Clinical Practice Council Chair Dan McDevitt, MD, and Reva Bhushan, SVS director of clinical guidelines and quality practice, presented the domain findings concerning clinical practice issues. The top priorities are the need to develop a Society position report on optimizing vascular surgery service, the role of vascular surgeons and the need for an optimized vascular team. This year will see the launch of the first phase of a national compensation study. The data will provide a vascular-specific, in-depth understanding of the different components of a vascular surgeon’s compensation and puts this in SVS members’ hands.
Quality
Quality Council Chair Thomas Forbes, MD, presented priorities in this domain. This included the necessity of appropriateness of care and the next steps to launch SVS’ second appropriate use criteria (AUC) project, focused on carotid disease. Also discussed was the “Vascular Verification Program: A quality program with the Society of Vascular Surgery,” in collaboration with the American College of Surgeons (ACS).
This program is designed to ensure
quality, as well as quality improvement in vascular care, in both the inpatient and outpatient settings. The inpatient component is launching this winter, with the outpatient program expected to begin in the spring.
Research
Of particular note in the research area is the finalization and publication of the updated research priorities, which will shape the focus and funding for vascular surgery research in the coming decade. The research council plans to focus on developing new scholarships and awards for translational research development. Research Council Chair Raul Guzman, MD, presented the priorities for this domain.
SVS health and vitality
Slaw, presenting alongside SVS Secretary William Shutze, MD, highlighted the importance of building member value and improving membership retention, specifically among early-career members. The necessity of branding the specialty to its different audiences also is deemed critical, as is investing in the SVS communications platform and infrastructure to reach audiences across different media channels and in different formats. The SVS will also press forward on its diversity, equity and inclusion (DEI) initiatives.
The meeting adjourned Jan. 14 with the near-finalization of the 2023 strategic objectives and budget discussion for fiscal year 2024. The SBOD will meet next on March 21.
www.vascularspecialistonline.com 15
MATTHEW SIDEMAN is chair of the SVS Advocacy Council. MEGAN MARCINKO is SVS advocacy director.
ADVOCACY
Becoming involved in advocacy is a tangible action to protect against bad policy becoming law
SYMPOSIUM CHAIRMEN:
Anthony Estrera, MD


Ali Azizzadeh, MD
PROGRAM DIRECTORS:
Gustavo S. Oderich, MD
Danny Ramzy, MD, PhD
HONORARY CHAIRMEN:
Hazim J. Safi, MD
David D. McPherson, MD
March 16, 17 & 18, 2023
www.promedicacme.com • www.houstonaorticsymposium.com • Rebecca Law, Rlaw@promedicacme.com Join us March 16-18, 2023 in Houston, Texas to discuss diagnosis and treatment paradigms for aortic and structural heart diseases, including medical, endovascular, surgical, and hybrid options! The Houston Aortic Symposium Frontiers in Cardiovascular Diseases
FIFTEENTH IN THE SERIES
Westin Oaks Hotel, Houston, Texas 5th Annual Houston Aortic Nursing Symposium Wednesday, March 15, 2023 • 12:00 – 5:00 pm Additional CME opportunity for nurses! Register & Submit Abstracts at www.houstonaorticsymposium.com
THE
The
ANNUAL MEETING SET TO TAKE PLACE AS EXCLUSIVELY IN-PERSON EVENT
By Beth Bales
A BLOCK PARTY ON OPENING DAY, session recordings available daily and—of course—the educational and scientific sessions for which the Society for Vascular Surgery’s Vascular Annual Meeting (VAM) is known: all this and much more will be part of VAM 2023.

The premiere educational event of the vascular world will be June 14 to 17 at the Gaylord National Resort & Convention Center in National Harbor, Maryland, just outside Washington, D.C.
Educational sessions and abstract-based plenaries will take place across all four days, ending at 12:30 p.m. Saturday. The Annual Business Meeting will follow, from 12:30 to 1:45 p.m. and will mark the official close of the meeting.
products and services industry has to offer, will be open June 15 and 16. And people who love a party should be sure to purchase tickets soon for the SVS Foundation’s premier event, the “Great Gatsby Gala,” set for the evening of Friday, June 16.
ic research but also educational sessions with topics for all career stages, from tips for young

surgeons to financial planning for surgeons preparing to retire. With receptions and dinners—not to mention chance meetings in the hallways and hotel—there will be plenty of opportunities to converse with friends and colleagues old and new.
People will need to be on site to experience it all. With substantial winding down of COVID-19 and the availability of vaccines, no live-streaming (with the exception of the Vascular Quality Initiative’s VQI@VAM) will be offered this year. However, all sessions will be recorded and available to registrants during the week of VAM. These recordings will be available for three years post-meeting, so attendees have plenty of time to catch any sessions they may have missed on-site or give a presentation additional review.
resources for nursing mothers, also are in the works.
As in years past, both the SVS Patient Safety Organization Vascular Quality Initiative (VQI) and the Society for Vascular Nursing (SVN) annual meetings will convene in collaboration with VAM.
VQI@VAM will be held the afternoon of Tuesday, June 13, followed by an early-evening reception and poster presentation, and all day Wednesday, June 14. This meeting will be live-streamed for those who cannot attend in person and recorded for registrants.
The SVN’s 41st Annual Conference will be held on Wednesday and Thursday, with its Presidential Luncheon, including awards presentations on Wednesday and a Welcome
week of the meeting for up to three years post-meeting.
To take advantage of National Harbor’s proximity to the country’s seat of government, a trip to Capitol Hill is planned, as are two sessions on the importance of advocacy and how advocacy impacts vascular surgeons’ lives and livelihoods.
In the wake of the completion of the BESTCLI (Best endovascular versus best surgical therapy for patients with CLTI) clinical trial, the Planning Committee has slated a session on outcomes and what comes next.

The United Kingdom’s BASIL-2 clinical trial—which is investigating outcomes of bypass versus angioplasty in severe ischemia of the leg—will be discussed at the same 90-minute session. Trial investigators will summarize key findings of each. The presentation also will include a debate on appropriate therapies plus discussion of implementing recommendations from both trials.

The SVS introduces the new Frank J. Veith Distinguished Lecture, announced at VAM 2022, this year. It, too, will cover BEST-CLI.

Learn more about VAM at the VAM web-



www.vascularspecialistonline.com 17
VAM 2023
R E G I S T R A T I O N N O W O P E N ! 2 0 2 3 V A S C U L A R R E S E A R C H I N I T I A T I V E S C O N F E R E N C E ‘ S T R U C T U R A L A N D I M M U N E C E L L S I N V A S C U L A R D I S E A S E ’ Stimulating discussion between presenters and attendees Abstract and poster presentations Translational panel The Alexander W. Clowes Distinguished Lecture Featuring: Wednesday, May 10 Marriott Copley Place, Boston, Mass. VRIC 2023 VRIC 2023 Highlighting emerging vascular science and biology
Michael Dalsing Andres Schanzer
SOCIETY BRIEFS
Deadline is March 1 for several awards
APPLICATIONS AND NOMINATIONS
Compiled by Beth Bales and Bryan Kay
MARCH’S FREEACCESS ARTICLES IN JVS, JVS-VL
are due March 1 for a number of Society for Vascular Surgery (SVS) and SVS Foundation awards.
The SVS Lifetime Achievement Award: This award, presented at the Vascular Annual Meeting, recognizes an individual’s outstanding and sustained contributions to the professions and SVS, and their exemplary professional practice and leadership.
The SVS Medal for Innovation in Vascular Surgery: The medal is given to an individual whose contribution has had a transformative impact on the practice or science of vascular surgery.
The SVS Foundation Clinical Research Seed Grants: These provide $25,000 in direct support for pilot clinical projects that could potentially become larger studies funded by industry or government sources. A patientoriented topic is encouraged.
Beginning this year, SVS has added service to the Society as an important component of its SVS Distinguished Fellow process.
Nominations and applications also are due March 1 for this honor, which goes to Active, International or Senior vascular surgeon members who have made substantial contributions in two of the three categories of research, service and education.
For award information visit vascular. org/SVSAwards or vascular.org/ SVSFoundationAwards. Visit vascular.org/ DistinguishedFellows for more information.
SVS DEI COMMITTEE LAUNCHES ‘VOICES OF VASCULAR’ SERIES
TO HELP CELEBRATE THE DIVERSITY in the vascular surgery specialty, the Society for Vascular Surgery Diversity, Equity and Inclusion Committee has launched “Voices of Vascular,” a series highlighting the contributions of surgeons from a wide variety of backgrounds.
“Voices” debuts this month, during the celebration of Black History Month. The initiative will highlight the stories of SVS members while also emphasizing patient education and awareness and sharing healthrelated facts and information pertinent to the community. The series will continue throughout the year.
SVS members from all backgrounds are invited to share their stories (or nominate someone else) by filling out the form available at vascular.org/VoicesForm. The SVS Foundation added a new fourth pillar for DEI in 2022. The “Voices of Vascular” series is aimed at helping to raise awareness as the Foundation works to raise funds to support DEI initiatives. The first profiles will be available at vascular.org/VoicesOfVascular
EMORY TRAINEE COLLECTS SAVS FOUNDERS AWARD
Emory University, Atlanta, vascular fellow Emma Rooney, is flanked by Southern Association for Vascular Surgery (SAVS) annual meeting moderators Adam Beck, MD, left, and Salvatore Scali, MD.

Get ‘Gatsby’ Gala tickets today
TICKETS—BOTH INDIVIDUAL AND for tables—are selling faster than a Gin Rickey during Prohibition for the Society for Vascular Surgery Foundation’s “Great Gatsby Gala,” to be held at the 2023 Vascular Annual Meeting (VAM).
From Feb. 3 to 18, individual tickets are $550. Starting Feb. 19, ticket prices will increase to $600 each. Standard price tables have sold out. Limited VIP tables ($7,500), Gold “champion” tables ($12,000) and Platinum tables ($20,000) remain. The evening will include the Surgeon Speakeasy Cocktail Reception, including cocktails (A Bee’s Knees or Hemingway Daiquiri, anyone?) and passed hors d’oeuvres, Gatsby-inspired performers and more; three-course dinner with wine service; live and silent auctions
and dancing. All proceeds will benefit the SVS Foundation and its efforts to fund the future of vascular health through its four pillars of research and innovation; community vascular care and patient education; disease prevention; and diversity, equity and inclusion.
Besides general tickets and table sales, SVS has sponsorship opportunities and table ticket levels available, including Young Surgeons/Fellows Table Sponsor, Dinner, Wine and Entertainment Sponsor, and Surgeon Speakeasy Sponsor. To learn more about these opportunities, contact Scott Behm at sbehm@vascularsociety.org
For more information and to purchase tickets, scan the QR code or visit vascular. org/2023gala

THE MARCH ISSUES OF THE Journal of Vascular Surgery (JVS) and JVS: Venous and Lymphatic Disorders (JVS-VL) include eight articles that will be available via free-access by Feb. 21 (JVS-VL) and Feb. 23 (JVS). The fully accessible peer-review papers are as follows:
JVS
1. “Early peripheral vascular interventions for claudication are associated with higher rates of late interventions and progression to CLTI,” Editor’s Choice, with a visual abstract. Visit vascular. org/JVS-ClaudicationCTLIMarch23
2. “Females are less likely to receive best medical therapy for stroke prevention before and after carotid revascularization than males,” with a visual abstract and continuing medical education (CME) credit possible. This paper is set to be featured on an episode of the popular Audible Bleeding podcast. Visit vascular.org/JVS-Gende redMedicalManagementMarch23
3. “Comparison of upper extremity and transfemoral access for fenestratedbranched endovascular aortic repair,” with a visual abstract. Visit vascular. org/JVS-F-BEVARMarch23
4. “Mortality analysis of endovascular aneurysm sealing versus endovascular aneurysm repair,” with a visual abstract. Visit vascular.org/JVSMoralityAnalysisMarch23
JVS-VL
In memoriam
SPOT LIGHT
GREGORY DOMER, MD, has been named chair of vascular surgery for the Deborah Heart and Lung Center in Browns Mills, New Jersey. He also will serve as director of the center’s vascular surgery fellowship program. He previously was director of the fellowship program and an attending vascular surgeon at St. Luke’s University Health Network in Bethlehem, Pennsylvania, as well as medical director of vascular surgery at AtlantiCare Regional Medical Center in Atlantic City, New Jersey. Meanwhile, members JOHN C. LANTISII, MD, and MATTHEW G. GAROUFALIS, DPM, have been named to the newly formed Medical Advisory Board for Arch Therapeutics, Inc., which is a developer of wound care and biosurgical products.
Former SVS President WILLIAM ABBOTT MD, 86, of Weston, Massachusetts, Jan. 9. He was the first chief of vascular surgery at Massachusetts General Hospital and became a professor of surgery at Harvard Medical School, Harvard University. Abbott served as SVS president in 1998. Fellow SVS member Richard Cambria, MD, was a vascular fellow with Abbot and was hired by him to the vascular surgery staff. “Bill’s leadership brought the vascular division at MGH to national prominence,” said Cambria.
U.S. Navy Capt. DONALD D. BELL, MD, 84, of Norfolk, Nebraska, on Jan. 9. He practiced in California from 1974 to 1994, before relocating to Norfolk. He served two tours of duty as a medical officer in the Navy. His family said, “His legacy will continue, forever reminding us that life is about taking action and that a life full of meaningful acts of love and service to yourself and others is not only possible, but worth emulating.”
1. “Clinical tolerance of untreated reflux after iliac vein stent placement.” Visit vascular.org/JVSVLLilacVeinStentMarch23
2. “Percutaneous superior vena cava puncture for hemodialysis catheter placement.” Visit vascular.org/JVSVLSuperiorVenaCavaPunctureMarch23
3. “Venous stent patency is independent of total stented length in nonthrombotic iliac vein and postthrombotic venous stenoses,” Editor’s Choice and CME credit possible. Visit vascular.org/JVSVL-StentMarch23
4. “A practice audit of short-term outcomes of Wallstent versus Venovo stents for the treatment of non-thrombotic iliac vein outflow stenoses.” Visit vascular.org/JVSVLIliacVeinOutflowMarch23
18
Vascular Specialist | February 2023
MID-TERM RESULTS FROM A PHASE II study of surgical bypass using the Human Acellular Vessel (HAV) demonstrated an overall secondary patency rate at 72 months of 60% measured by Kaplan Meier. There was no evidence of graft rejection or infection, the authors reported.
Humacyte, the biotechnology platform company behind the product, said the publication describes the long-term analysis of the clinical trial as it evaluates the bioengineered HAV as a conduit in patients with symptomatic peripheral artery disease (PAD).
The research team, led by first-named author Piotr Gutowski, MD, from the Department of Vascular Surgery at Pomeranian Medical University of Szczecin in Szczecin, Poland, concluded that “the infection-resistant, offthe-shelf human acellular vessel could provide a durable alternative conduit in the arterial circuit setting, to restore lower extremity blood supply in patients with peripheral artery
disease.” The results were recently published in the Journal of Vascular Surgery-Vascular Science (JVS-VS).
No patients underwent amputation of the affected limb out to six years, they found, and none reported pain at rest or ischemic ulcers on the affected legs. Gutowski et al reported that “these data have demonstrated the durability of the HAV and suggest the occurrence of cellular remodeling by the host.”
Gutowski commented: “Synthetic grafts can be limited due to poorly matched mechanical compliance, risk of infection, and variable patency rates. Furthermore, cryopreserved allogenic grafts are limited due to poor durability, thrombosis, and mechanical degradation. The HAV is designed to be consistent in size, durable in high-pressure circulation, show no clinical immunological response, and remodel with the patient’s own cells.”
The HAV has been evaluated in eight clinical studies in the U.S., Europe and Israel, including an ongoing phase II/III clinical trial in vascular trauma and an ongoing phase III trial as a dialysis access graft in end-stage kidney disease. The HAV is an investigational product and has not been approved for sale by the Food and Drug Administration (FDA).
SURMODICS PROVIDES REGULATORY UPDATE RELATED TO FDA PREMARKET APPROVAL APPLICATION FOR DCB
SURMODICS RECENTLY ANNOUNCED IT HAS RECEIVED A LETTER from the Food and Drug Administration (FDA) related to its premarket approval (PMA) application for the SurVeil drug-coated balloon (DCB).
In the letter, the FDA indicated that the application is not currently approvable, while providing specific guidance as to a path forward. The letter stated that certain information within two general categories—biocompatibility and labelling— must be added by an amendment to the company’s PMA application to place it in approvable form. Although the information identified by the FDA to put the PMA application in approvable form would require additional testing and analysis, the letter did not question the human clinical data submitted nor request any further human clinical data.
“We are disappointed by the FDA’s response to our PMA application and continue to have confidence in our SurVeil DCB including its compelling performance in the TRANSCEND clinical study,” said Gary Maharaj, chief executive officer of Surmodics.
“We are evaluating the issues raised in the FDA’s letter and plan to meet with Agency representatives regarding its contents. Based on our discussion with the Agency, our team and external advisors will determine the appropriate path forward. Concurrently, we will be evaluating options to reduce our use of cash given this development. We expect to address these topics further in connection with our upcoming first quarter fiscal 2023 earnings call.”
Surmodics notes in a press release that the SurVeil DCB is a next-generation device for the treatment of peripheral arterial disease and includes a proprietary drugexcipient formulation using an innovative process to improve coating uniformity. The company advises that, in the U.S., the SurVeil DCB is an investigational device, limited by Federal law to investigational use.
GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface*
GERMANY-BASED
endovascular device company Bentley announced the launch of the BeBack crossing catheter— formerly known as the GoBack— designed for the treatment of heavily calcified lesions above and below the knee.

Bentley acquired the catheter in September 2022 from Upstream Peripheral Technologies, of Caesarea, Israel. The now-rebranded BeBack crossing catheter is available in an 80cm and 120cm catheter in both 2.9F and 4F sizes. The device makes use of a steerable and in-length adjustable nitinol needle, which can be used for crossing and targeted re-entry purposes. “A radiopaque marker indicates the direction in which the curved needle protrudes from the tip of the catheter. Multiple treatment options like antegrade, retrograde and crossover are possible with the BeBack catheter for intraluminal and subintimal approaches of stenotic or occluded lesions.”

The BeBack is CE marked and Food and Drug Administration (FDA) cleared.
VIZ.AI HAS ANNOUNCED THE LAUNCH OF Viz Vascular Suite—artificial intelligence (AI)-powered software enabling vascular care teams to automatically detect and triage care for suspected pulmonary embolism, right heart strain, aortic dissection, and abdominal aortic aneurysm (AAA).
The company submitted a new 510(k) application to the Food and Drug Administration (FDA) for the AAA algorithm, a press release notes.
“Recognizing the symptoms of serious vascular conditions, such as aortic dissections, is hugely important because any delay in treatment can have a direct impact on patient outcomes,” said Philip Batista, MD, Cooper University Health Care, Camden, New Jersey. “When Viz identifies an abnormal scan, it quickly notifies the appropriate specialists regardless of their location, facilitating seamless communication via mobile application. We have been using the Viz software for the last several months and have seen improvements in patient care across our institution.”
Viz.ai says that the Viz Vascular Suite uses AI to automatically analyze an array of imaging modalities, including computerized tomography (CT), electrocardiogram (ECG), and more for suspected vascular diseases. If a suspected pathology is found, the app automatically alerts and displays high-fidelity patient scans on providers’ mobile devices. Clinicians can use Viz Vascular Suite to remotely coordinate vascular pathology care within a hospital system’s hub and spoke network and enable synchronous, HIPAA-compliant communication among specialists. The platform is enhanced by AI for immediate team activation and facilitates informed, efficient treatment decisions.
INDICATIONS FOR USE IN THE U.S.: The GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface is indicated for improving blood flow in patients with symptomatic peripheral arterial disease in superficial femoral artery de novo and restenotic lesions up to 270 mm in length with reference vessel diameters ranging from 4.0 – 7.5 mm. The GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface is indicated for improving blood flow in patients with symptomatic peripheral arterial disease in superficial femoral artery in-stent restenotic lesions up to 270 mm in length with reference vessel diameters ranging from 4.0 – 6.5 mm. The GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface is indicated for improving blood flow in patients with symptomatic peripheral arterial disease in iliac artery lesions up to 80 mm in length with reference vessel diameters ranging from 4.0 – 12 mm. The GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface is also indicated for the treatment of stenosis or thrombotic occlusion at the venous anastomosis of synthetic arteriovenous (AV) access grafts. CONTRAINDICATIONS: The GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface is contraindicated for non-compliant lesions where full expansion of an angioplasty balloon catheter was not achieved during pre-dilatation, or where lesions cannot be dilated sufficiently to allow passage of the delivery system. Do not use the GORE® VIABAHN® Endoprosthesis with Heparin Bioactive Surface in patients with known hypersensitivity to heparin, including those patients who have had a previous incident of Heparin-Induced Thrombocytopenia (HIT) type II. Refer to Instructions for Use at eifu.goremedical.com for a complete description of all applicable indications, warnings, precautions and contraindications for the markets where this product is available.
*As used by Gore, Heparin Bioactive Surface refers to Gore’s proprietary CBAS Heparin Surface. Products listed may not be available in all markets.
www.vascularspecialistonline.com 19 & NEWS
Compiled by Jocelyn Hudson and Bryan Kay
Bentley
launches rebranded crossing catheter Viz.ai launches AI-powered Viz Vascular Suite
Human-tissue engineered blood vessels remain durable at six years in PAD patients, study results show
Consult Instructions for Use eifu.goremedical.com
©
W. L.
01: 4.5” x 5.625” 21373436-EN-VSX-Indications-Ad.indd 1 12/8/21 11:10 AM BeBack Bentley
GORE, Together, improving life, VIABAHN and designs are trademarks of W. L. Gore & Associates.
2021
Gore & Associates, Inc. 21373436-EN DECEMBER 2021
Human Acellular Vessel
SAFE AND EFFECTIVE TREATMENT OF SFA ISR




The Gore RELINE MAX Clinical Study demonstrated safe and effective treatment of real-world superficial femoral artery (SFA) in-stent restenosis (ISR) through three years with the VIABAHN® Device.1








65% 100% freedom from major amputations and VIABAHN® Device stent fractures *

freedom from target lesion revascularization

Occluded bare metal stent Post VIABAHN® Device placement Images courtesy of Peter Soukas, M.D. Used with permission.

GORE® VIABAHN® Endoprosthesis
Heparin
W. L. Gore & Associates, Inc. Flagstaff, Arizona 86004 goremedical.com Please see accompanying prescribing information in this journal. Products listed may not be available in all markets. GORE, Together, improving life, VIABAHN and designs are trademarks of W. L. Gore & Associates. © 2023 W. L. Gore & Associates, Inc. 22820057-EN JANUARY 2023
with
Bioactive Surface*
Gore, Heparin Bioactive Surface
Gore’s proprietary CBAS ® Heparin Surface. 1. Soukas P. Three-year
GORE® VIABAHN® stent-graft in the superficial femoral artery for in-stent restenosis. Presented at VEINS (Venous Endovascular INterventional
and VIVA (Vascular InterVentional Advances)
Conference; October 31, 2022- November 2, 2022; Las Vegas, NV. See the data
As used by
refers to
results of the
Strategies)
Annual





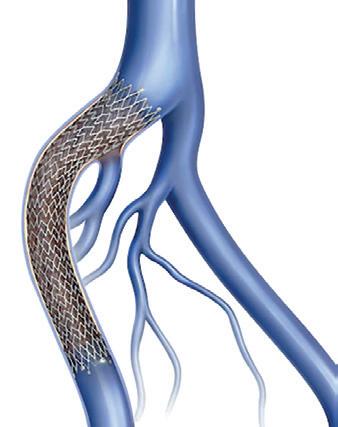
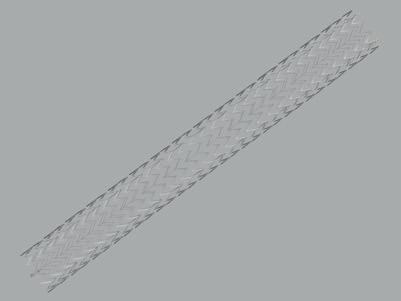
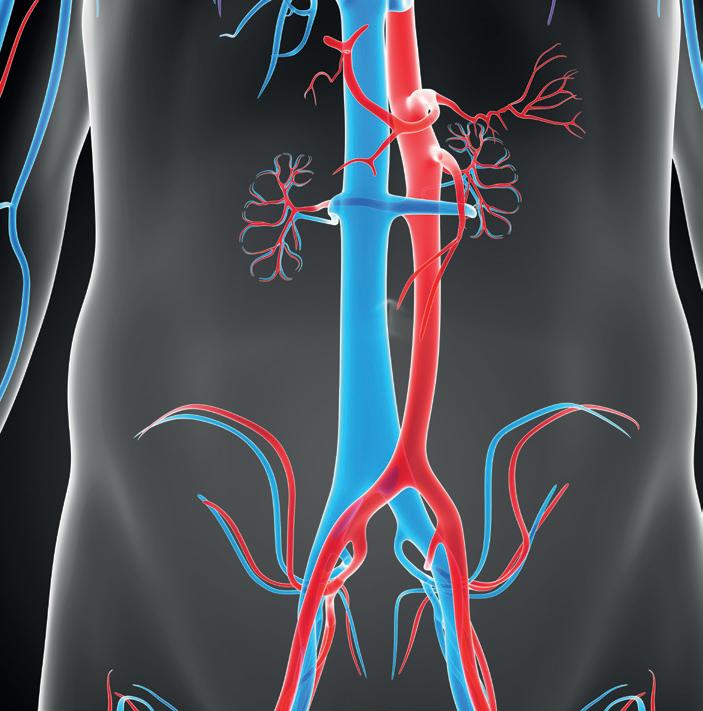
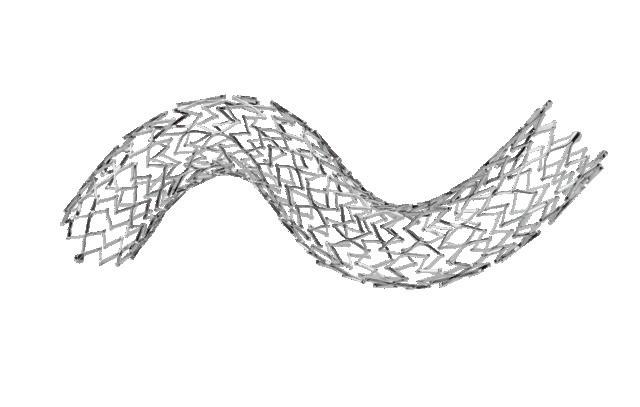 Jocelyn Hudson and Bryan Kay
Jocelyn Hudson and Bryan Kay




 By Jean Bismuth, MD, and Jonathan Cardella, MD
By Jean Bismuth, MD, and Jonathan Cardella, MD