How should we introduce new technologies into surgical practice?

A sustainable trauma service – we must make this a priority
Clinical guidelines and the standard of care

Volume 11 | Issue 03 | September 2023 | The Journal of the British Orthopaedic Association | boa.ac.uk Journal
of Trauma and Orthopaedics
p24
p46
p34
OrthoFoam Knee Wedges Nailing, Nailed
Simplify patient positioning for tibial or retrograde femoral nailing procedures with our range of trauma triangles. The knee remains in the correct position throughout the procedure with our durable foam providing the perfect balance of cushioning and stability.
Product Code:
OL.OF.KWS Ortholove Knee Wedge Small
OL.OF.KWM Ortholove Knee Wedge Medium




OL.OF.KWL Ortholove Knee Wedge Large
OrthoFoam Paediatric Ramp Smaller, but Sturdy
Much like the larger Ramp Elevator, this smaller size allows quick and reproducible positioning, with a focus on paediatric and young adult patients, for a variety of lower-limb elective and trauma procedures.
Raises the operative leg away from the table and above the contralateral side, allowing excellent visualisation of anatomy on image-intensifier fluoroscopy.
Product Code: OL.OF.PRE
OrthoFoam Prone Positioning Ramp
Posterior Approach
For cases where the patient is required to be in a prone position, this ramp is angled to support the lower leg, foot and ankle, with a gentle ramp slope providing elevation of the operative limb.
Speak to us about special offers when you buy a full range of Ramp or Trauma Ortholove Professional products.
Product Code: OL.OF.PPR

01480 457222 / info@ortholove.com / www.ortholove.com Distributed in the UK by LEDA Orthopaedics
In this issue...
28 Features:
Sustainability in Orthopaedics – Let’s Share Best Practice

Irrum Afzal, Vipin Asopa and Deiary Kader
30 Features:
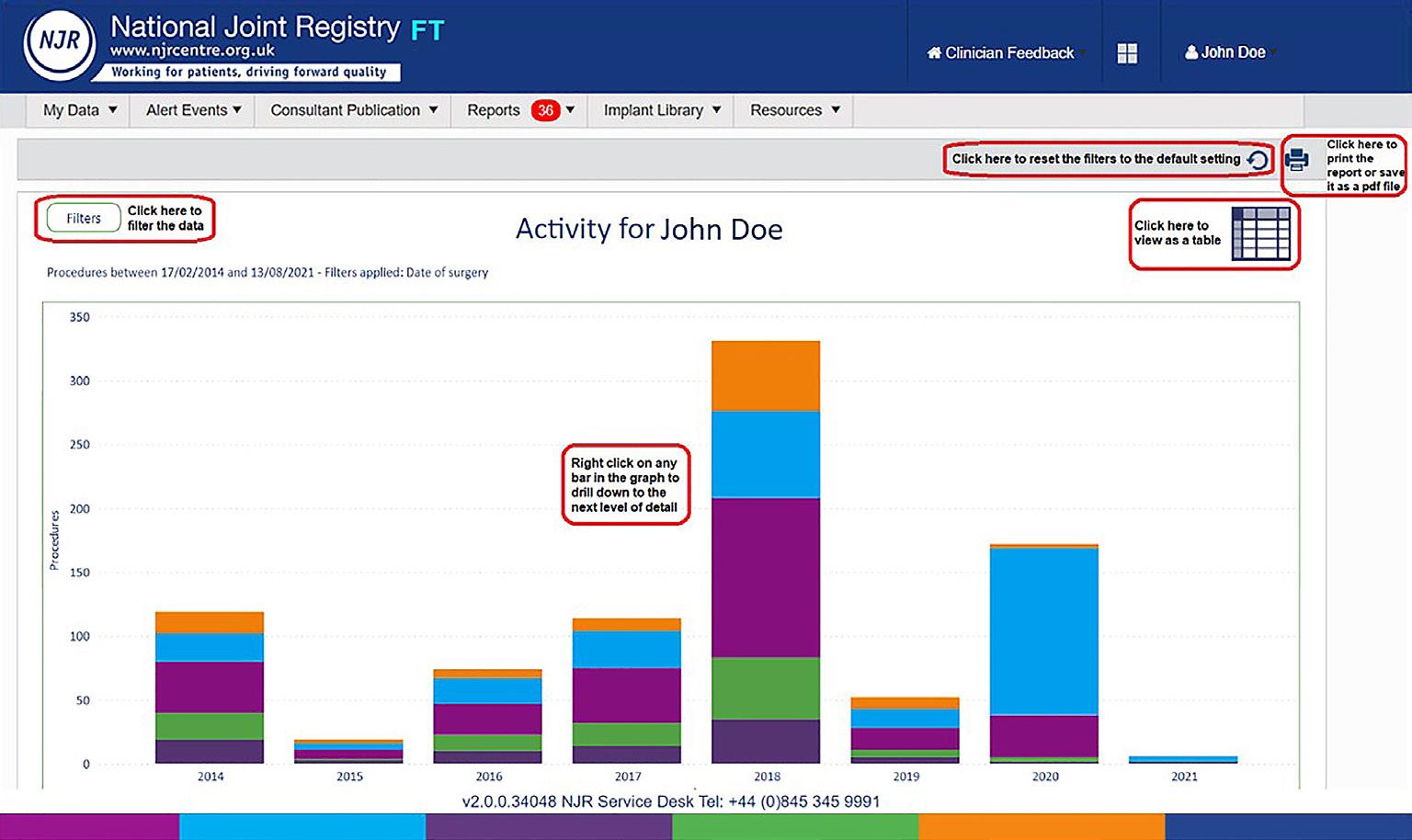
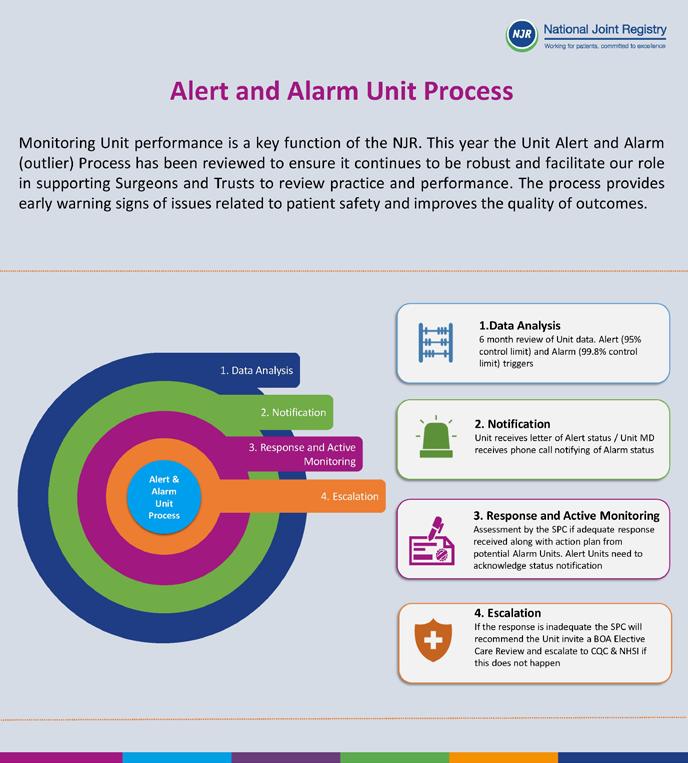
20 Years of the National Joint Registry: who benefits? Part 2: surgeons and implant suppliers


Peter Howard, Tim Wilton, Derek Pegg, Mike Reed and Richard Armstrong
34 Features:
A sustainable trauma service – we must make this a priority

Sharon Scott
50 Subspecialty:
Let’s talk about sustainability

Stephen Bendall and Gareth Chan
22 Features: Another anniversary –the NHS
24 Features: How should we introduce new technologies into surgical practice? Part 1: The challenges of how we innovate now
Chetan Khatri, Steve Gwilym, Keith Tucker, Edward T Davis, Xavier L Griffin, David Beard and Andrew Metcalfe
38 International: Spicing up the Training Programme
Willem Schenk and Sunil Wijayasinghe
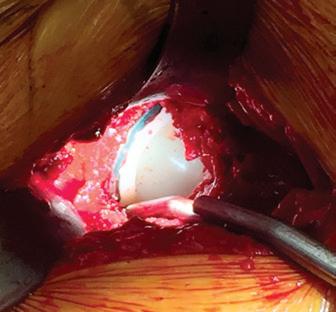
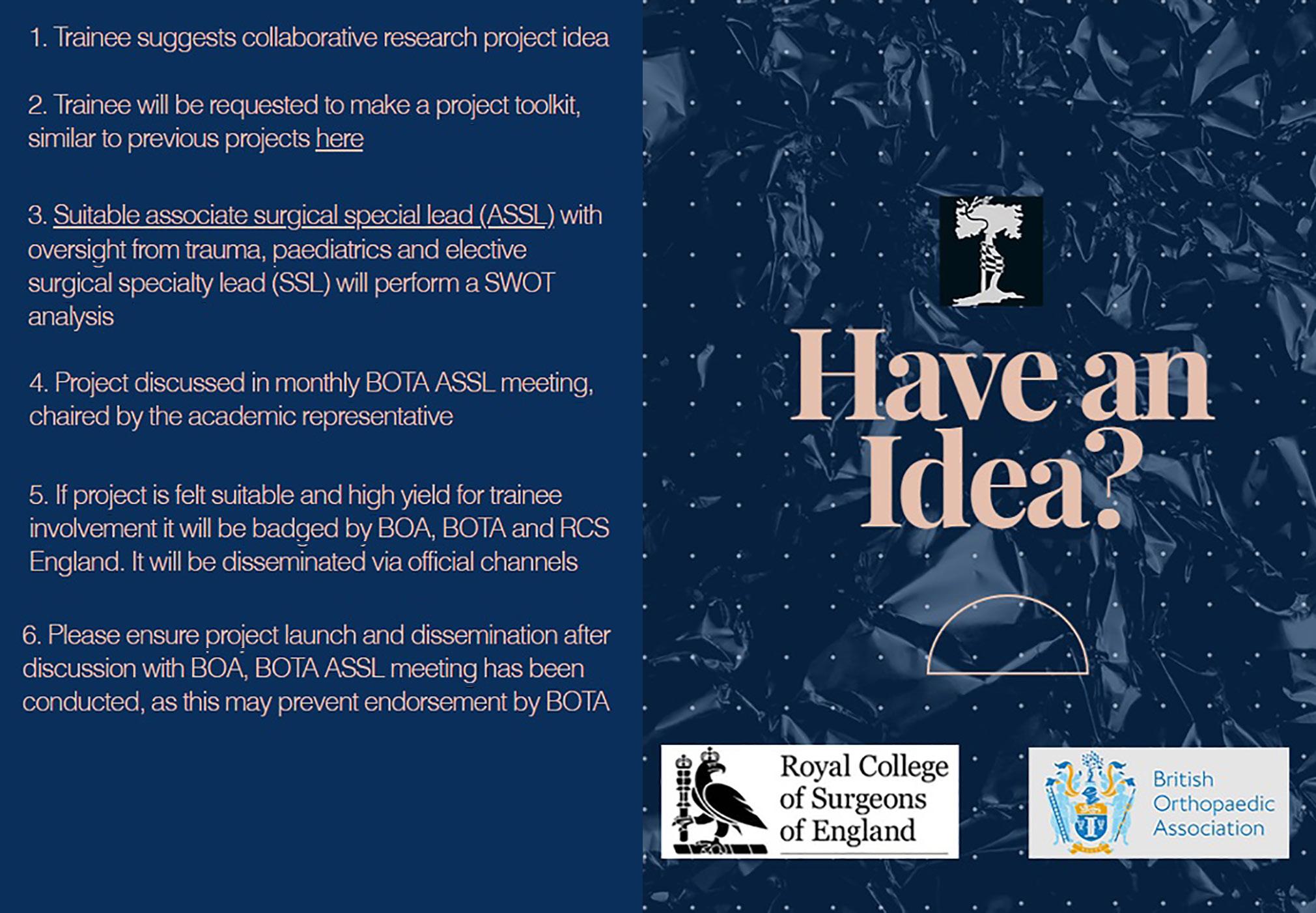
42 Trainee:
The impact of trainee-led collaborative research within UK trauma and orthopaedics

Abhinav Singh, Ignatius Liew, Zaid Hamoodi, Sohail Nisar and Frank Acquaah
46 Medico-legal: Clinical guidelines and the standard of care: Part 2
Simon Britten
Download the App


54 Subspecialty:
Blowing against the wind: the case for shifting the current paradigm on theatre ventilation

Benedict Rogers
56 Subspecialty:

Reusable surgical gowns and drapes. Should we be adopting them?

Hussameldin M Nour, Safeer Javid, Rhodri Gwyn and Riem Johnson
58 In Memoriam:
Rolfe Birch

Kar Hao Teoh
The Journal of Trauma and Orthopaedics (JTO) is the official publication of the British Orthopaedic Association (BOA). It is the only publication that reaches T&O surgeons throughout the UK and every BOA member worldwide. The journal is also now available to everyone around the world via the JTO App. Read the latest issue and past issues on the go, with an advanced search function to enable easy access to all content. Available at the Apple App Store and GooglePlay – search for JTO @ BOA
Did you know that as well as advertising in our Journal publication, we can offer footer banner advertising on the JTO App! For more information please contact Wendy Parker Email: Wendy@ob-mc.co.uk | Telephone: +44 (0)121 200 7820


JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk | 01 3 From the Executive Editor Simon Hodkinson 5 From the President Deborah Eastwood 8-9 BOA Latest News 16 News: Honorary Fellowships 18 BOA Annual Congress 2023
Features: Advancing the MSK health of the nation through research, education and innovation Arash Angadji
20
Mandate Gary Robjent
Contents Amputation the context T OrthopaedicsT Orthopaedics A Surgical Day Begins Volume 08 Issue 02 Volume 08 Issue 01 Volume 08 Issue 04 Journal of the British Orthopaedic Association The Journal of Trauma and Orthopaedics (JTO) has a dedicated news section, a features section containing interesting articles on various themes, a subspeciality section and a medico-legal section. Journal of Trauma
We are committed to sustainable forest management and this publication is printed by Buxton Press who are certified to ISO14001:2015 Standards (Environmental Management System). Buxton prints only with 100% vegetable based inks and uses alcohol free printing solutions, eliminating volatile organic compounds as well as ozone damaging emissions. Open Box Media & Communications are proud to be corporate sponsors of Heart Research UK (Midlands)
and Orthopaedics
46
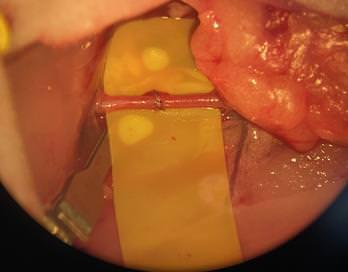
REDUCE RISK FOR INFECTION

Reduction of infection risk* using dual antibiotic-loaded bone cement in high risk patients
in primary hip & knee arthroplasty in fractured neck of femur in aseptic revision TKA
* as reported in study results
11860 UK IMPROVE THE CHANCES Medical
www.heraeus-medical.com
JTO Editorial Team
l Simon Hodkinson (Executive Editor)
l Hiro Tanaka (Editor)
l Simon Britten (Medico-legal Editor)
l Abhinav Singh (Trainee Editor)
l Stephen Bendall (Guest Editor)
BOA Executive
l Deborah Eastwood (President)
l John Skinner (Immediate Past President)
l Simon Hodkinson (Vice President)
l Mark Bowditch (Vice President Elect)
l Fergal Monsell (Honorary Secretary)
l Ian McNab (Honorary Treasurer)
l Bob Handley (Appointed Trustee)

BOA Elected Trustees
l Deborah Eastwood (President)
l John Skinner (Immediate Past President)
l Simon Hodkinson (Vice President)
l Mark Bowditch (Vice President Elect)
l Fergal Monsell (Honorary Secretary)
l Ian McNab (Honorary Treasurer)
l Fares Haddad
l Amar Rangan
l Sarah Stapley
l Hiro Tanaka
l Cheryl Baldwick
l Deepa Bose
l Caroline Hing
l Andrew Price
l Andrew Manktelow
l Andrea Sott
l Paul Banaszkiewicz
l Stephen Eastaugh-Waring
Copyright
BOA Staff
Executive Office
Chief Operating Officer - Justine Clarke
Personal Assistant to the Executive - Celia Jones
Education Advisor - Lisa Hadfield-Law
Policy and Programmes
Head of Policy and Public Affairs - Gary Robjent
Head of Education and Programmes
- Alice Coburn
Programme and Committees Officer
- Eliza Heng
Educational Programmes Assistants
- Mia Gordon
Communications and Operations
Director of Communications and Operations
- Annette Heninger
Marketing and Communications Officer
- Pujarini Nadaf
Membership and Governance Officer
- Natasha Wainwright
Interim Membership and Governance Officer
- Vicky McGuinness
Publications and Web Officer - Nick Dunwell
Interim Publications and Web Officer
- Michael Davis
Finance
Director of Finance - Liz Fry
Finance Assistant - Hayley Ly
Events and Specialist Societies
Head of Events - Charlie Silva
Events Coordinator - Venease Morgan
UKSSB Executive Assistant - Henry Dodds
From the Executive Editor
Simon Hodkinson
Awarm, but currently damp welcome to the September, Congress edition of the JTO.
As I write this editorial, the orthopaedic and national media is reporting the sad loss of one of our young colleagues, cut down in his prime on holiday. A sad reminder of the frailty of human life.
We also mourn the loss of Rolfe Birch, a true giant of our profession. Both are remembered in this edition and our sincere condolences go to the bereaved families.
Turning to this edition, the theme is on sustainability, reflecting the theme for this year’s Congress, ‘Sustainable Systems’.
I would like to start by congratulating the recipients of the BOA’s Honorary Fellowships for this year, listed here with their significant contributions to our profession.
Our first article is about advancing MSK health through research and innovation by Arash Angadji from ORUK. Many of us of a certain generation will remember Ronnie Furlong who was the driving force behind ORUK, and this is an important article at this time of huge waiting lists and an ever increasing workload in our profession, much of it driven by an ageing population and poor health.
Continuing the theme of the ORUK article, Chetan Khatri et al discuss how to introduce new technologies into our practice. This is a very relevant article, given the current issues we face with implant availability in the UK. The authors are all hugely experienced in both research and regulation of the subject.
Moving to the crux of this edition and this year’s Congress theme, there are a series of diverse articles, all with a common theme of sustainability in our profession.
First off is an article from Irrum Afzal et al, about the need to share best practice in sustainability in T&O, pointing out that the NHS is the largest single contributor to greenhouse emissions in the public sector and we in T&O are a big part of that statistic!
Copyright© 2023 by the BOA. Unless stated otherwise, copyright rests with the BOA. Published on behalf of the British Orthopaedic Association by: Open Box M&C
Advertising
All advertisements are subject to approval by the BOA Executive Board. If you’d like to advertise in future issues of the JTO, please contact the following for more information:
Wendy Parker - Media Manager
Email: Wendy@ob-mc.co.uk | Telephone: +44 (0)121 200 7820
Open Box M&C, Premier House, 13 St Paul’s Square, Birmingham B3 1RB
Disclaimer
The articles and advertisements in this publication are the responsibility of the contributor or advertiser concerned. The publishers and editor and their respective employees, officers and agents accept no liability whatsoever for the consequences of any inaccurate or misleading data, opinions or statement or of any action taken as a result of any article in this publication.
BOA contact details
The British Orthopaedic Association, 38-43 Lincoln’s Inn Fields, London WC2A 3PE Telephone: 020 7405 6507
How to contact JTO
Email: jto@boa.ac.uk
Sharon Scott then reviews the real and present issue of sustaining our trauma services against an avalanche of issue familiar to all of us. My generation starting to create a peak in the frail population at the same time as the trough in the younger age group that provide the care occurs. The perfect storm. The article reflects on the need to follow evidence-based practice as best we can, informed and supported by such initiatives as GIRFT in elective care.
We then move on to our invited section of articles on the subject of sustainability in T&O, edited by Steve Bendall in Brighton. These three thought-provoking articles start with a discussion of what sustainability means and what elements are realistic aims in our practice.
Benedict Rogers then covers the issue of ventilation in theatres and what is really required to reduce SSI’s, and whether the time has come to challenge the paradigm that all orthopaedic surgery has to be done in an ultraclean environment.
Finally, Hussameldin Nour et al looks at whether we should do a U-turn in our practice, and return to reusable gowns and drapes.
Three articles that look at what we can realistically do to change our carbon footprint in the practice of Trauma and Orthopaedic surgery.
This is a packed edition and I do hope all recipients find something of interest to themselves in these challenging times.
I look forward to seeing you at this year’s Congress in Liverpool. n
JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk | 03
Credits

Time flies when you are enjoying yourself and certainly this year has flown, and Congress – perhaps a highlight of the BOA year – is just around the corner. Congress provides us with the opportunity to catch up both socially and scientifically, to pick up some exciting new ideas and perhaps identify a few things that are now ‘old hat’ and which should be consigned to the bin of painful lessons learnt.
The Congress theme is Sustainable Systems and if we want to continue to attract and maintain the best talent to work with us in Trauma and Orthopaedics, if we want to train and educate using the best techniques available, if we want to protect our resources while we help our patients, then there is no doubt that the time for change is now. Someone once said that “in order to change we must be sick and tired of being sick and tired”. I hope and believe that we are at that point. This edition of the JTO is full of questions and ideas that challenge us to change the way we think, that give us the power to question what we do, to challenge our attitudes to our work and perhaps the way we live to: ‘why do we work the way we do, should we not change?’
The BOA will be presenting some proposals to you at the AGM: proposals that recommend significant changes to our governance structure, which we believe will improve our diversity in terms of opinion and experience while ensuring high standards of professionalism and behaviour are maintained. The changes will encourage greater engagement with you, our membership. Please do take the time to read the information that will be sent to you and then vote online or come to the AGM to allow your voice to be heard.
Last month, BOTA and BOA hosted a Culture and Diversity Day at the Royal College of Surgeons with Neurodiversity and Disability as its theme. There were a number of stimulating and thought-provoking talks highlighting the differences that make us who we are – the different realities and perceptions that we experience. I know that each and every one of us found at least one aspect of a talk hit home with how we feel from time to time. We left feeling that people had been heard. We left with a better understanding of the breadth of abilities shown by our colleagues and a knowledge that inherently we are perhaps more similar than different. Certainly, aspects of our workplace culture and our attitudes to training and learning must allow all to flourish. As one of the speakers explained: “If a flower does not bloom, don’t blame the flower, look at the environment it’s in and fix that.”
This is my last message to you as BOA President – it has truly been a privilege to represent you and our patients over this year. Together we have faced many challenges and many are ongoing. I thank all of you, the BOA Executive and Council for all your support and hard work. My faith in our profession and my inherent optimism mean that I do believe that next year will be a better year and I know Simon will lead us well.

I also believe that, as my ‘Uncle Clint’ Eastwood suggested, “If you want to see a change for the better, you have to take things into your own hands.” My challenge to you is to do just that.
I look forward to seeing you all in Liverpool! n
From the President
“The power to question is the basis of all human progress.”
– Indira Gandhi
Deborah Eastwood
Simon Hodkinson – Incoming President

As I write this piece, I am acutely aware that soon I will take up the mantle of President of this august association. I am looking forward to the day with excitement, but balanced with a healthy dose of fear and trepidation. I am acutely aware of the challenges that our profession has in front of it and the calibre of the people who have gone before me and, as I know them, will follow me.
Every President has a theme to their year in post and mine is to be you, the Trauma and Orthopaedic workforce in all its forms. My predecessor has focused on sustainable systems in our profession, and I intend to extend this theme to us, the workforce. We have emerged from the pandemic thankfully, but we have a workforce challenged as never before in the NHS and not in the best of health.
We have some of the brightest and best in the world in our profession, yet we are struggling to cope in this post-pandemic world. We need to recruit to our profession, sustain surgeons through these turbulent times and retain what we have for as long, as we can to get back on our feet.
I am well aware that these aims are easy to say, yet anything but easy to achieve. I do not pretend to have the answers, but I intend to make sure that in the recovery to come – and we will recover – you, the workforce in all its forms will remain front and centre in all my dealings in the coming year. I look forward to meeting as many of you as I can in September and working for you all in the coming year. n

06 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk News
“Every President has a theme to their year in post and mine is to be you, the Trauma and Orthopaedic workforce in all its forms.”
Miller’s Orthopaedic Review Course, Oxford*
3–7 January, 2024 at Worcester College University of Oxford, U.K.
• 99% FRCS Examination overall pass rate for past course attendees
• Satisfaction assured! If you complete the course and do not pass your exam, you may repeat the course for FREE‡
• Our esteemed global faculty are all highly respected in their fields and chosen because they are truly great teachers
• Network with colleagues and take in the famous sights and charms at University of Oxford

• Includes complimentary access to JBJS Clinical Classroom plus 65+ hours of recorded sessions from MedShr
• The Royal College of Surgeons of England has awarded 40.5 CPD points for this event
‡Terms and conditions apply.
*Formerly Oxford Comprehensive Orthopaedic Review Course | millerfrcsorthopaedicrevisioncourse.co.uk
Learn more
BOA Educational Courses
The BOA runs a wide range of courses under the Education Committee. These courses cater to the educational needs of a wide range of members (and non-members in some cases) at all stages of their careers.
Early
The COVID-19 pandemic prompted a re-emergence of non-operative management in trauma and orthopaedics to reduce the risk of transmission and reduce the operative and cost burden on healthcare systems. However, there is a wide disparity in clinical practice.

Following the implementation of trust guidelines in accordance with the BOAST recommendations at Gloucestershire Hospitals NHS Foundation Trust, 86% of cases were found to have primary fracture manipulation in the emergency department compared with 32% pre-pandemic, saving approximately 63 hours of trauma theatre time over six-months, reducing waiting times by avoiding unnecessary admissions and bringing some uniformity among the practitioners and departments. Read the full report here: https://pubmed.ncbi.nlm.nih.gov/37405130/

All BOASTs can be found on the BOA website at www.boa.ac.uk/boasts
Training Orthopaedic Educational Supervisors (TOES)
This course is designed to help members prepare for the new curriculum and learn how to supervise trainees to be the very best they can be. For more information or to book, visit www.boa.ac.uk/toes
Training Orthopaedic Trainers Course (TOTs)
This programme aims to improve the standard of teaching for those in T&O training and practice. If T&O trainers understand how people learn and how the T&O curriculum works, by translating that understanding into action, they should improve their teaching. Further information and to book, visit www.boa.ac.uk/tots
Medico-legal Course - ‘Law for Orthopaedic Surgeons – Avoiding Jeopardy’
We have one remaining course date in 2023 on 7th November for this popular course specifically designed to highlight potential pitfalls in practice from the medico-legal perspective and to help steer surgeons away from potential jeopardy. Full details can be found at www.boa.ac.uk/law-for-orthopaedic-surgeons
UK and Ireland In-Training Examination (UKITE)
UKITE 2023 will take place from 8th – 15th December. UKITE is an online mock examination that allows trainees and SAS surgeons to practice for section 1 of the FRCS Tr and Orth.
Registration is now open and is free for members before 30th November (£150 for non-members). All late registrations will attract a £50 fee.
Register now at www.boa.ac.uk/UKITE.
Our Editors make UKITE possible by developing, reviewing and validating questions. Find out how to join the team at www.boa.ac.uk/ukite-editorial-role or e-mail ukite@boa.ac.uk

08 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk Latest News
Management of Paediatric Wrist and Forearm
Fractures – BOAST implementation saves approximately 63 hours of trauma theatre over six months
Registration is now open for the next BOA Ortho Update Course. Designed for orthopaedic trainees at all levels and SAS surgeons, this updated course will give you the opportunity to access new understanding and support your preparation for the FRCS exam. Register now to secure your place!
Date: Saturday, 6th January 2024
Time: 8:30am to 5:00pm
Where: Etc Venues, 11 Portland St, Manchester, M1 3HU
The 2024 course will focus on ‘Exams and Examination’. It is a course of two halves. We are continuing with the popular critical condition CBDs. Along with talks from examiners, eg, ‘How the viva/clinical works’, ‘Taming the examiner’ and much more.
Real FRCS examiners will talk about how the exam is conducted and scored, along with some top tips for preparing and passing. You will hear about some trainee experiences of the exam, along with a chance to quiz the examiner!

Finally, the popular critical condition CBDs will return, which this year will cover diabetic foot and the ‘foot attack’, cauda equina syndrome, and the painful paediatric hip and spine. There will also be a return of the brilliant quick-fire trauma meeting called ‘The Good, the Bad and the Ugly’, which will look at basic science of trauma, biomechanics and complications.
Register now at www.boa.ac.uk/OrthoUpdate
BOA Council Election Results
We are pleased to welcome the newly elected BOA Council members for 2024-2026
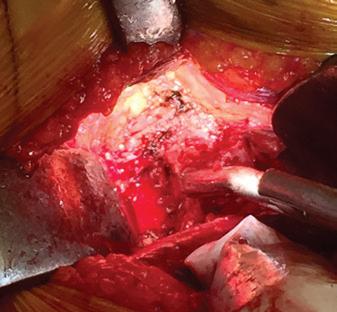
Use of phage therapy to treat joint infection
Use of phage therapy to treat a joint infection has been undertaken for the first time in the UK. Phage therapy is a viral cell-based treatment, which may offer a much needed solution in treating patients with multi-drug resistant infections. This is the first time it has been ever been used in the UK, other than topically. The patient concerned is doing well and their wound has now healed for the first time in seven months. The team from NHS Tayside’s orthopaedic department will publish more detailed results in the upcoming December issue of the JTO.
The BOA has produced a BOAST on Primary Joint Infection, which is available on the BOA website at www.boa.ac.uk/boasts
Final report of Elective Recovery Taskforce
The final report of Elective Recovery Taskforce was published by the Department of Health and Social Care (DHSC) in August. While media headlines concentrated on the continuing rollout of community diagnostic centres, the essence of the implementation plan is to maximise the use of all NHS assets and available independent sector capacity, and to empower patient choice.
Patients will be actively offered a shortlist of a minimum of five providers, where clinically appropriate, and patients are able to see provider quality, waiting time and distance to travel in My Planned Care.
From the end of October 2023, all patients who have waited more than 40 weeks without having had their first outpatient appointment will be able to initiate a request to transfer to another provider. The ‘ambition’ is to expand this solution to further long-wait cohorts in future, depending on the level of uptake and impact on clinical capacity.



Subject to the Parliamentary timetable, revised patient choice legislation will establish the Provider Selection Regime (PSR) to ensure that provider qualification criteria are used more consistently and make clear the circumstances under which NHS England and ICBs must offer a contract to providers that meet the qualification criteria.

Under the PSR, DHSC and NHS England intend to introduce an independent panel, which will review compliance with patient choice and PSR requirements. This panel will, when required, provide advice to commissioners to assist with improving compliance where necessary.
Link to full guidance: https://www.gov.uk/government/ publications/elective-recovery-taskforce-implementationplan/elective-recovery-taskforce-implementation-plan
JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk | 09 Latest News
Amar Rangan
Benjamin Ollivere
Hiro Tanaka Vikas Khanduja
BOA sponsored travelling fellowship to Ganga Hospital, India 2023
Kunal Kulkarni, BM BCh, MA (Oxon), MSc, FRCS (Tr & Orth), FEBHS, Dip Hand Surg (Br) Consultant Trauma and Orthopaedic Surgeon (Hand and Wrist Surgery), University Hospitals of Leicester NHS Trust
Iwas delighted to have been awarded a BOA Travelling Fellowship to Ganga Hospital in Coimbatore, India – an internationally recognised, 650bed private orthoplastic centre of excellence for hand and upper limb surgery, and one of the busiest specialist units in India.

During my visit, I had the opportunity to spend time with their specialist elective and trauma orthopaedic and plastic surgical teams. In a single clinic, I saw a wide variety of upper limb cases, ranging from the simple (carpal tunnel, De Quervain’s) to the complex (birth brachial plexus palsy, open polytrauma).
There is a strong ethos of research and teaching, with residents, fellows and consultants undertaking numerous teaching sessions each week that I was able to attend. I also had the opportunity to complete Ganga’s highly regarded microsurgery course, which takes place over five days in a lab furnished with four Zeiss microscopes.
The course covers a variety of arterial and venous anastomosis on anaesthetised rat femoral vessels (approximately the calibre of adult human digital vessels), allowing repeated practice during the week to build confidence and dexterity. This opportunity allowed me to observe the delivery of complex and life-changing care to a huge number of patients, in a very different clinical and social environment to my usual NHS practice. The expertise of the teams was evident, with many of their senior clinicians wellestablished on the international conference circuit. I had a great experience and would highly recommend a visit. Thank you to the BOA for supporting this experience.
This BOA travelling fellowship took place at Ganga Hospital, Coimbatore, Tamil Nadu, India in February 2023 n
World Orthopaedic Concern (WOC) update

WOC held its annual conference on 3rd June 2023 at the Royal College of Surgeons of England. This is the first hybrid conference we have held, kindly run by MedAll. We were proud and delighted that over 200 attendees joined us virtually from 40 low and middle income countries (LMICs) in addition to those who came in person.
The day was interesting and varied. We heard about a variety of programmes across the world, from Ukraine to South Africa, passing through Guyana, Ethiopia, Kongo, South Sudan, Malawi, Zambia and Zimbabwe.
Audience members –both in person and online – were very engaged, and their questions energised the presenters and the conference in general!
Deepa Bose
The BOTA session saw some strong presentations from the trainees, and this holds bright promise for future collaborations between high and low income countries.


Deborah Eastwood, President of the BOA, gave an update on how the Association is getting more involved in global orthopaedics and Phil McElnay, CEO of MedAll, showed us their vision for accessible health education for all. This has got to be the way forward. Every person in every country has the right to education and if we can do our little bit, we consider it a win.
The talks can be accessed here: https:// app.medall.org/event-listings/world-orthopaedicconcern-conference-2023/content n
10 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk News
WOC 2023 trainees
Ganga Hospital
Microsurgical anastamosis
Microsurgery course laboratory
Deborah Eastwood, BOA President



British Elbow and Shoulder Society (BESS) update
Steve Drew, BESS President
At our annual event this June, I succeeded Jonathan Rees as President of BESS. The event was well-received, and we were grateful to all who made it such a success. At that meeting, the hot topics session highlighted our work over the last year. Central to this was equity, diversity, and inclusion. In the last 18 months we have expanded Council, to better reflect and represent our membership. We are pleased to have formally appointed Nash Siddiqui as our EDI Lead, Aparna Viswanath as Early Career Surgeon and Joanna Winton as Early Career AHP.
These new Council members have already been very busy. Nash has founded an EDI working group and is developing our EDI statement. Aparna, along with Fiona Ashton, Education Committee Trainee, ran successful Early Career Surgeon and Trainee sessions. Joanna has been working to improve how we connect with AHPs and encourage them to join BESS. We have been working to expand our educational portfolio by building our trainee network, BESS-T, for trainee surgeons and AHPs, and developing our BESS Roadshow to provide accessible and affordable learning opportunities to
AHPs. We also plan to raise our profile at other meetings, including ICSES 2023 this September, where we will run a special session in conjunction with the Irish Shoulder & Elbow Society (ISES). Later, in November, we will join ORUK to run our annual Improving Outcomes for the Shoulder & Elbow. We’ll also run our Elbow Updates Symposium in Coventry in March 2024 and our annual meeting will take place in Aberdeen in June 2024.
We continue to strengthen our support of shoulder and elbow research trials across the UK, and focus on updating our management and treatment guidelines for shoulder and elbow conditions, alongside producing new ones. We are pleased to have partnered with the RCS on a Senior Clinical Fellowship for shoulder and elbow. More details are available via the RCS website. All of this, coupled with our transition to charity status, has ensured BESS remains a busy society and I am looking forward to my next two years promoting it. n
British Indian Orthopaedic Society (BIOS) update


Sunil Garg, BIOS President
BIOS continues to work very closely with the BOA, BOTA and the Indian Orthopaedic Association (IOA) in promoting education and training. BIOS annual conference was held in Windsor on 7th and 8th July, organised by Mr Sunil Bajaj from QE Woolwich. Conference-themed innovation and recent advances was a grand success with updates on AI, machine learning and biologics. Dedicated CESR session was applauded, and in attendance were presidents from the BOA and the IOA. Other highlights from the conference were reports from fellowships organised and sponsored by BIOS, a trauma and medico-legal revalidation session and five free paper sessions. The conference ended with its unique Bollywood night of dinner and dance until midnight, when the delegates let their hair down.
BJJ (Bone & Joint Journal) will be the official publication for BIOS as an affiliated specialist society from 2023. The abstracts from BIOS annual meetings have been published in BJJ for the benefit of trainees and education for over 10 years. BIOS has so far sponsored over 50 orthopaedic surgeons from India to UK. BIOS has also pledged to support BOTA and sponsor fellows every year to travel to India at their chosen centre of excellence for trauma or subspecialty interest. BIOS has started a new research wing from 2023 with promised pumping grants to trainees. We will be delivering a ‘How I do it’ session at the BOA Annual Congress in September and at the annual conference at the Indian Orthopaedic Association annual meeting at Lucknow, India on 23rd December. BIOS has also opened a new student wing, and aims to get more medical students and trainees involved in its activities for the silver jubilee of the society at Gateshead on 5th and 6th July 2024, organised by Mr Rajesh Nanda. n

12 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk News
“We have been working to expand our educational portfolio by building our trainee network, BESS-T, for trainee surgeons and AHPs, and developing our BESS Roadshow to provide accessible and affordable learning opportunities to AHPs.”
Missed the Edinburgh Instructional Course & Trauma Symposium 2023?


All lectures available online



For orthopaedic trainees who wish to contribute to the analysis of data from the National Joint Registry (NJR) and undertake a period of independent research into arthroplasty.



One fellowship is available, worth up to £70,000 per annum, to start in 2024 for a two-year period.
Closing date for applications: 5 February 2024

£300 for Instructional Course OR £300 Trauma Symposium access OR £500 combined
visit www.trauma.co.uk

Application form and terms: https://www.njrcentre.org.uk/research/ research-fellowship

For more information
Reduces pain and increases mobility medi. I feel better. www.mediuk.co.uk Tel: 01432 373 500 medi soft OA light knee brace osteoarthritis off-loading knee brace now available on prescription. Intended purpose: medi soft OA light is a knee brace for load relief.
British Orthopaedic Oncology Society (BOOS) update
The British Orthopaedic Oncology Society (BOOS) has had another tremendously successful year, culminating in the annual conference in Burton-on-Trent where our outgoing President, Professor Rob Ashford, handed over to our incoming President, Mr Rob Pollock (Royal National Orthopaedic Hospital). As always, the conference had a wide variety of presentations and the scientific standard of this year’s talks was
probably the highest ever. We received an update on the British Orthopaedic Oncology Management audit led by the Royal Orthopaedic Hospital team, which is leading the way for patients with metastatic disease.
The Birmingham Orthopaedic Network and BOOS have developed a national audit to assess the management of patients with metastatic bone disease against the BOA and BOOS guidelines:
Metastatic Bone Disease: A Guide to Good Practice. The study aims to evaluate whether the recommendations have been adopted into clinical practice and as would be expected, there is significant range across the country. We will continue to promote work in this area and the conference in 2024 in Cardiff will, for the first time, be a two-day event to ensure we have adequate time to cover all these issues. n
Conference Listing 2023:
BTS (British Trauma Society)
www.britishtrauma.com
21-23 November 2023, Cardiff
BSSH (The British Society for Surgery of the Hand) www.bssh.ac.uk
22-24 November 2023, Glasgow
BASS (British Association of Spine Surgeons) www.spinesurgeons.ac.uk
20-22 February 2024, Bournemouth
BOA (British Orthopaedic Association)
www.boa.ac.uk
19-22 September 2023, Liverpool

BORS (British Orthopaedic Research Society) www.borsoc.org.uk
25-26 September 2023, Cambridge
BOSTAA (British Orthopaedic Sports Trauma and Arthroscopy Association)
www.bostaa.ac.uk
09 November 2023, London
BSS (British Scoliosis Society)
www.spinesurgeons.ac.uk/event-5235572
09-10 November, Liverpool
BOFAS (The British Orthopaedic Foot and Ankle Society) www.bofas.org.uk
06-08 March 2024, Belfast
BLRS (British Limb Reconstruction Society) https://blrsmeeting.com/
14-15 March 2024, Glasgow
BASK (British Association for Surgery of the Knee) https://www.baskmeeting.com/
16-17 May 2024, London
British Orthopaedic Oncology Society (BOOS) https://www.boos.org.uk/
27-28 June 2024, Cardiff

14 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk News
“The scientific standard of this year’s talks was probably the highest ever.”
BOA Annual Congress 2023 19th–22nd September, ACC Liverpool
Get involved at the BOA!
We are now recruiting for an exciting variety of Committee roles
Are you interested in improving the landscape of T&O across the UK and want your voice to be heard and represented? If so, you could be the perfect fit for one of our opportunities. This is your chance to use your skills and expertise to influence and input into the work of the BOA, and actively contribute to our vision, mission and values.
We have exciting opportunities for BOA members who are Home Fellows or SAS surgeons to represent, lead and effect change across the trauma and orthopaedic profession.


Committees
Are you passionate about inspiring action and effecting change? Are you keen to be an active advocate and ambassador for an organisation? Are you eager to play a key role in important projects and initiatives? Committees are the engine of the BOA and Committee members are appointed for their passion, dedicated, and innovation.
We are recruiting for posts on the following Committees:
• Orthopaedic
• Research
• Medico-legal
• Trauma
• Education and Careers
Deadline for all applications: Friday 29th September 2023.
Applications are particularly encouraged from currently under-represented groups in the BOA leadership structures including, but not limited to, women, those from minority ethnic backgrounds and LGBTQ+ members.

For more information on all vacancies and how to apply go to www.boa.ac.uk/get-involved
I have enormously enjoyed being part of the Trauma Committee. The COVID-19 pandemic has led to unique strains upon trauma care in the UK. I feel honoured to be able to help in ensuring that patient care is prioritised as we attempt to recover. Membership of the Committee has allowed to me share ideas with, and learn from, experienced orthopaedic surgeons around the country. This, for me, has crystallised into a multidisciplinary project to improve orthoplastic care in the UK. I highly recommend that you consider applying for a role with the BOA. I am confident that you will find it stimulating and fulfilling.
Medico-legal work has formed a substantial part of my orthopaedic practice over the last 20 years. It has shaped my practice and educated me in ways I did not imagine when starting out. Through their career most orthopaedic surgeons will encounter the legal profession from one side or the other. By joining the BOA Medico-legal Committee I have engaged with likeminded individuals keen to pass on their experience and knowledge, and we hope to support and empower orthopaedic surgeons in their interactions with the legal profession.

JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk | 15
Bilal Jamal (BOA Trauma Committee)
‘‘ ‘‘
Stephen Hepple (BOA Medico-legal Committee)
‘‘ ‘‘
News
Honorary Fellowships
The BOA is pleased to announce the recipients of the 2023 Honorary Fellowship, which will be presented at BOA 2023 Congress.
Mr Nigel D Rossiter MB BS FRCSEd (Tr&Orth) FFSTEd FIOTA
Aformer Trauma Orthopaedic surgeon with the British Army, Nigel is a recently retired Consultant Trauma and Orthopaedic Surgeon in Basingstoke, where he was Clinical Director and lead for Trauma.
He is the Chair of Trustees and Medical Director of the Primary Trauma Care Foundation, and founder of his hospital charity. Nigel sits on the board of GACI at the WHO. He is on the Permanent Council of the G4 Alliance and has addressed the UN General Assembly. He is also on the Faculty Advisory Board for the Faculty of Remote Rural and Humanitarian Healthcare at the Royal College of Surgeons of Edinburgh, plus the Oxford University Global Surgery Group.

He is the founding President of the Orthopaedic Trauma Society, a founding Fellow of the International Orthopaedic Trauma Association and an Emeritus International member of the Orthopaedic Trauma Association. He also led the setting up of the South Central Trauma Networks in England.
He is also on the International Consensus panel for VTE prevention and was on the NICE VTE group.
Nigel reviews clinical trials for NIHR and papers for a number of publications: BJJ, Injury, JBJS, Bone & Joint Research, and others. He is also a founder, director, and past Chair, of Incision Medical Indemnity; Chair of the Scientific Advisory Board for Open Medical; medical adviser to Rams Rugby and co-authored many of the BOASTs.
He has been international AO faculty and chaired the AO Advances & Principles Orthopaedic Trauma education in UK and Ireland. Nigel co-authored the original STEP course and has been a Basic Surgical Skills tutor.
He has been named Trainer of the Year for the Wessex area twice, “NHS Shine Awards Inspiring Educator of the year” finalist twice and recipient of a Hippocrates Award for excellence in the field of medicine from Who’s Who – in which he is listed. n
Professor Sarah (Sallie) Lamb
Sallie Lamb is Pro-Vice-Chancellor and Executive Dean of the Faculty of Health and Life Sciences, at the University of Exeter. An internationally recognised scholar in ageing, disability and rehabilitation, she is also an experienced methodologist in the area of clinical trials and high-quality evaluation of health care practice.
Sallie has a strong commitment to improving the lives of older people through excellent research that answers difficult questions, and can inform policy making and commissioning. She works to ensure research is translated into practice, and to drive up the quality of methods and reporting used in medical research. Sallie has mentored and supervised many early career scientists, and is a strong advocate for team working and gender equality in the workplace. n

16 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk News
Tim Wilton MA FRCS



Tim Wilton studied at Oxford and University College Hospital qualifying in 1978. His orthopaedic training was in Cardiff, Nottingham, and Derby where he was appointed Consultant in 1990. He specialised in lower limb arthroplasty immediately. Tim became the first Clinical Director of the orthopaedic unit in Derby in 1993.
Tim was elected Treasurer of the BASK (2000-2005), Hon Secretary (2006-2009) and President (2011-2013). He also was a founder member of the European Knee Society.
Tim was elected to BOA Council (2007-2010) and to the Presidential line in 2013, serving as President of the Association 2015-16. He also was the Robert Jones lecturer in 2016. In addition, he helped establish the process for Elective Care Reviews to address problems with arthroplasty outcomes.
Furthermore, he was Chairman of the Bone and Joint Publishing group having been on the Editorial Board and subsequently the Council of management of the BJJ for most of two decades. He has lectured widely on TKR operative technique, kinematics and balancing the knee, and outcomes of joint replacement from registry data.
Tim was a design consultant to Smith+Nephew for the Journey TKR, gaining considerable insight into the design, development and manufacture of orthopaedic implants.


For many years Tim has focused mainly on patient safety related to medical devices and served on NJR Steering Committee 2003-2007. He was on the Safety of Devices Committee, and currently advises the MHRA and the FDA about arthroplasty devices. He also helped set up ODEP for knees while he was BASK President and remains actively involved in Beyond Compliance.
Tim retired from active clinical work in May 2021 after 43 years in the NHS. He was appointed Medical Director to the NJR in 2019 and maintains ongoing connection with the health service, not only due to his role with the NJR, but also advising the Independent Medical Expert Group of the MoD. n

The iWALK hands-free crutch isn’t just a step forward, it’s a revolutionary leap for anyone dealing with a non-weight bearing, below knee injury. With significant practical and medical benefits over traditional crutches and knee scooters, the iWALK redefines how patients can stay mobile and recover with a newfound freedom and quality of life.

JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk | 17 News
To learn more, read research and testimonials, or to order a patient information pack for your clinic: Visit kneecrutches.co.uk email admin@kneecrutches.co.uk or call 0800 471 4974 GET YOUR LIFE BACK CARRY DRINKS CLIMB STAIRS WITH THE AWARD WINNING
STAND 5 UK KNEE CRUTCHES VISIT US AT THE BOA CONGRESS HANDS-FREE CRUTCH Why struggle with crutches, when you can be hands-free? KC_JTO_September_190x130_Final_AW.indd 1 15/08/2023 13:11
BOA Annual Congress 2023
19th – 22nd September, ACC Liverpool
This year’s flagship Annual Congress is taking place 19th-22nd September, ACC Liverpool under the theme ‘Sustainable Systems’: www.boa.ac.uk/congress

General registration is now open, but late registration begins on Monday 4th September 2023 at 23:59. Please find the registration rates on the Congress https://www.boa.ac.uk/boa-annualcongress-2023/registration.html
Programme Update
The theme of the Annual Congress 2023 is ‘Sustainable Systems’ and we look forward to presenting to you a mix of educational and scientific sessions with a number of high calibre speakers for our plenary and revalidation sessions. This year’s presidential Guest Lecturer will be delivered by Dr Kristy L Weber, MD, Director of the Sarcoma Program, Abramson Cancer Center, USA.

The Howard Steel Lecture will be delivered by Nick Robinson, a British journalist and the current presenter of the BBC’s Today programme. He will be looking at why politics isn’t delivering. Nick Robinson has been reporting and presenting on radio and television for over 30 years. He is the only broadcaster to have been Political Editor for both the BBC and ITV News.

This year’s Robert Jones Lecturer is Professor Andrew Carr, Nuffield Professor of Orthopaedic Surgery at the University of Oxford, whose research has focused on the development and evaluation of surgical implants. His lecturer is titled ‘Innovation, Regulation, and Evaluation in Orthopaedic Surgery’.

Other sessions from the BOA include:
• BOA Diversity and Inclusion Session.
• Congress theme plenary SOS: Sustainable Orthopaedic Systems.
• BOA Trauma Committee – ‘Only do what you need to do – when less is more in orthopaedic trauma’.
• BOA Ortho Committee – ‘More is Less; Sustainable Orthopaedics’.
• BOA Research Committee – Big Studies of 2023.
• BOA Medico-legal Committee – ‘Post pandemic recovery of orthopaedic services’ – update.
• BOA Debate – ‘This House Believes … that Apprentice Training of Doctors represents the Future’. Full details of the programme is available at www.boa.ac.uk/programme
Accommodation & Travel
Make sure to book your accommodation now so you don’t miss out! More information on hotels near to the Congress venue is on the BOA website at www.boa.ac.uk/accommodation which includes a helpful distance map.
Exhibition & Sponsorship
We are delighted to welcome over 80 exhibitors at this year’s BOA Annual Congress – including DePuy Synthes, Smith+Nephew, Biocomposites, Circle Health Group, Ethicon, Let’s Talk Dr, Link Orthopaedics, Orthofix Medical Inc, Stryker, Zimmer Biomet UK and many more! Explore the full list of exhibitors on our website: www.boa.ac.uk/ exhibition-sponsorship #BOAAC23 #orthotwitter
18 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk News
www.boa.ac.uk/congress #BOAAC23
Product Theatre

New for 2023 and in partnership with the ABHI (Association of British HealthTech Industries), we are pleased to launch our first Product Theatre at this year’s exhibition. Join us and discover the latest innovative products and solutions to the market. We have a great line up planned, with sessions from DePuy Synthes, Smith+Nephew and the ABHI, who will discuss how the HealthTech industry is contributing towards the net zero targets and protocols for trusts. Register and join us! Limited spaces available and seats are on a ‘first come first serve’ basis. Visit our website for the full programme of events and discover all the exhibitors featuring inside the theatre. www.boa.ac.uk/product-theatre n


Dates for your Diary
■ BASK Revision Knee
16th & 17th October, Birmingham
■ Sports Knee Surgery
6th & 7th November, Birmingham
■ Uni Knee Meeting
28th November, Bristol
■ Bristol Hip Meeting
30th Nov & 1st Dec, Bristol
■ Basingstoke Knee Osteotomy
14th & 15th December, Basingstoke

JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk | 19 News
Clockwork Medical 2 The Cart House Chestnut Farm Barns Village Street, Sedgebrook Grantham, Lincs NG32 2EW Tel: 01949 843900 www.clockworkmedical.com 21/08/2023 18:28
Advancing the MSK health of the nation through research, education and innovation Arash Angadji
Dr Arash Angadji joined Orthopaedic Research UK in 2008 and was appointed Chief Executive in 2016. Over the years he has been instrumental in the strategic development and rebranding of the organisation, with a focus on improving governance and expanding the research and education programmes within the charity. Arash has a PhD in Medical Engineering, MBA in Management and is a trustee at the British Orthopaedic Research Society (BORS).

Orthopaedic Research UK (ORUK) is a small charity, but with a big ambition to advance orthopaedic and musculoskeletal (MSK) knowledge, and champion the needs of a sector that is all too often starved of investment. We are one of the most significant funders of orthopaedic and MSK research in the UK. Since 2004, we have invested almost £12 million on projects that expand knowledge, improved patient outcomes and pioneered new forms of diagnosis and treatment. Every year we run about 80 educational and training courses. We have also been successful at unlocking funding for research and training from both the public and private sector.
We can only make a significant contribution by working with others. We co-fund fellowship programmes, including two fellowships with the BOA, and collaborate with a wide range of partners, from academic institutions to charities and the private sector. It is only by mobilising the whole MSK community that we can hope to address the poor MSK health of the nation.
In the spirit of our founder Ronald Furlong –who combined a highly successful career as an orthopaedic surgeon with an equally successful career as an entrepreneur – we are the first MSK charity to actively support start-ups and entrepreneurs. With the Ronald Furlong Fund for Start-ups and the recently announced Grand Challenge Award, co-funded by the British Hip Society, our aim is to accelerate the roll-out of innovative ideas. We are also part of the NHS Clinical Entrepreneur Programme.
The sheer scale of the MSK challenges we face as a society has encouraged us to broaden our focus beyond surgery to include education and research into the (non-surgical) management of MSK conditions. Our partnership with ESCAPE-pain – the award-winning group rehabilitation programme for people with chronic joint pain – opens-up new modes of care within a non-healthcare setting such as community and leisure centres.
Over the past 12 months, we have increased our policy work, targeting unmet needs within MSK health. In November, we will be hosting our second AI in Orthopaedics conference. Last year’s event, hosted by the Royal College of Surgeons of England, was the first national conference dedicated to the role of AI and Big Data within orthopaedics. It provided an important opportunity to highlight barriers impeding the application of AI, including access to high-quality data. We have subsequently secured the commitment of Microsoft to fund an AI training programme for surgeons and allied health professions (AHPs), and that of the National Institute for Health and Care Research (NIHR) to highlight the importance of AI research for MSK health in its Invention for Innovation (i4i) programme. Our partnership with Versus Arthritis, focusing on the application of AI to MSK, will start accepting applications imminently. We are also about to launch an MSK health for the workplace programme, in association with the Arthritis and Musculoskeletal Alliance. This will focus on improving the MSK health of the working age population, at a time when more than 2.5 million people are currently unemployed in the UK due to health-related issues, including back and neck pain. The government’s focus on getting people back to work, alongside its long-term aim of increasing the retirement age, demands a serious focus on the MSK health of the working age population. The programme will include research, funding for innovation, policy papers, educational programmes and events.
Poor MSK health is a multi-dimensional, multigenerational problem that has a profound impact on individuals, workplaces and our health system. It is the third-largest area of expenditure for the NHS, and linked to rising levels of obesity, anxiety, isolation and depression. With such a huge societal impact, we must never accept the inevitability of pain, or indeed its cost. We therefore see the purpose of our charity as mobilising the whole MSK community to keep pushing at research boundaries, encouraging innovation and helping to educate the next generation of healthcare professionals. Together we can make a difference.
Features
n
20 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk
Looking to customise your QA4™? We’ve got you covered.

Contact us today to discover our full range of pressure relieving gel supports and other QA4™ accessories.
Thank
sales@aneticaid.com
+44 (0)1943 878647


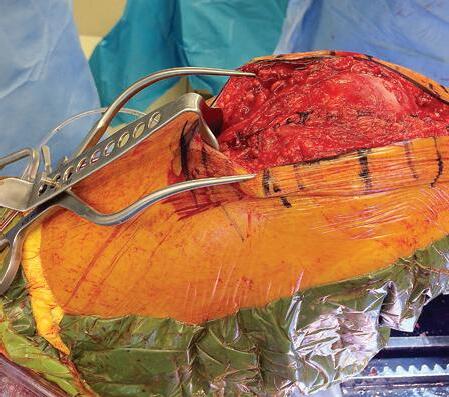
Jig-guided hip revisions


For the first time, Gomina has developed an extraction set that allows a hip revision to be done with minimal bone loss. Thanks to innovative production technologies, it is possible to manufacture dimensionally rigid chisels with different radii. The precision ground, sharp cutting edges of the chisels are the result of Gomina’s many decades of expertise.

The bespoke crafted jigs manufactured by Gomina ensure the application of a precise separation of bone and prosthesis. This innovative pioneering extraction set from Gomina makes surgeon’s work far easier, leading to shorter operating times. Entirely for the patient’s benefit.

To
@dayonetrauma




www.gomina.ch




swiss quality Official Distributor for the UK Judd Medical Unity House, Buntsford Park Road, Bromsgrove, Worcestershire B60 3DX Tel. +44 (0)15 27 55 90 10, sales@judd-medical.co.uk, www. judd-medical.co.uk
you for being there from
aneticaid.com all our supporters at BOA Congress, you’re amazing!
from clinicians and medical companies means fewer people face major trauma alone. We can’t stop now. Help rebuild lives after catastrophic injury. dayonetrauma.org fundraising@dayonetrauma.org
Charity number 1194227
Support
Another anniversary
the NHS Mandate
Gary Robjent
The first NHS Mandate was published 10 years ago, as the NHS celebrated its 65th anniversary. The then Secretary of State for Health (not yet recognising the significance of the close relationship with social care in the title) was Jeremy Hunt – later Chair of the Health and Social Care Committee and now Chancellor of the Exchequer. The Mandate was intended to introduce greater transparency of the government’s objectives and what it legally required* the NHS Commissioning Board (now several iterations later, NHS England) to deliver.
That first Mandate, was structured around five key areas where the government expected the NHS Commissioning Board to make improvements:
• Preventing people from dying prematurely.
• Enhancing quality of life for people with long-term conditions.
• Helping people to recover from episodes of ill health or following injury.
• Ensuring that people have a positive experience of care.
• Treating and caring for people in a safe environment, and protecting them from avoidable harm.
Jump forward 10 years (warming up first to avoid an ACL tear) and the 2023 Mandate is a very different beast. Applicable from 15th June 2023 until a new mandate is published – that will probably be after the General Election – NHS England continues to have a legal duty to seek to achieve the objectives of the government.
In 2023, the foreword from the Secretary of State begins with, ‘The government has promised to cut NHS waiting lists, meaning that people can get the care they need more quickly. That promise is at the very heart of this year’s mandate.’ This sets the tone for a much shorter Mandate than in previous years, with only three priorities. These are:
• Priority 1: cut NHS waiting lists and recover performance
NHS England will lead the NHS in recovering services for patients, in particular, delivering
Gary Robjent is Head of Policy and Public Affairs for the BOA.
more planned hospital activity to tackle the elective backlog. This will be supported by a focus on increasing outpatient productivity and transforming outpatient pathways. Also, by March 2025, 95% of patients needing a diagnostic test should receive it within six weeks with the continued roll out of community diagnostic centres.

Building on the existing patient’s rights to choice, patients should be able to access all providers of NHS healthcare, from a minimum of five providers, where providers meet NHS costs and standards. Patients should be given more information, so they can easily compare providers based on waiting times, distance and quality. From October 2023, for patients already on the waiting list, the longest waiting patients can request to move to a different provider to receive earlier treatment where it is clinically appropriate and should they choose to move.
It is also intended that there will be 5,000 more beds as part of the permanent bed base for next winter.
• Priority 2: support the workforce through training, retention and modernising the way staff work
Working with the Department of Health and Social Care, Integrated Care Boards and other partners, NHS England should lead implementation of the NHS Long Term Workforce Plan (published 30th June), to ensure the NHS has the workforce to meet the changing needs of patients over the next 15 years.
• Priority 3: deliver recovery through the use of data and technology
Within this it is worth noting that by March 2024, all trusts should adopt barcode scanning of high-risk medical devices and submission to the national, mandatory Medical Device Outcome Registry (either directly or via a supporting electronic health record (EHR) or inventory management system that can support registry data submission). The registry will be used to improve patient safety and outcomes in procedures that use high-risk medical devices.
Healthwatch England, a statutory consultee to the NHS Mandate, has raised a growing concern about the rising average waiting time for elective treatment, especially with growing average waits having ‘a much bigger impact on women, ethnic minorities, people with disabilities and those living on lower incomes’.
It also highlighted recent work on referrals showing that thousands of people are on a ‘hidden waiting list’, often waiting weeks or months before their referral is accepted and they join the ‘official’ waiting list for elective care.
Alongside the above objectives, the government expects NHS England to continue the wider work to deliver the key NHS Long Term Plan ambitions, while releasing efficiency savings of at least 2.2% in 2023 to 2024 and that productivity should continue to improve back towards pre-COVID-19 levels, noting that, ‘Ongoing productivity improvement is also an integral part of long-term workforce planning.’
All this must be achieved while NHS Improvement, Health Education England and NHS Digital are integrated into a single NHS England organisation with headcount expected to be reduced in size by 30-40% by April 2024. n
Features
–
22 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk








































































































How should we introduce new technologies into surgical practice?
Part 1: The challenges of how we innovate now

 Chetan Khatri, Steve Gwilym, Keith Tucker, Edward T Davis, Xavier L Griffin, David Beard and Andrew Metcalfe
Chetan Khatri, Steve Gwilym, Keith Tucker, Edward T Davis, Xavier L Griffin, David Beard and Andrew Metcalfe
Some new surgical technologies and procedures continue to revolutionise outcomes for patients, as they have done throughout the history of surgery1. There are many examples of innovations which have led to a vast improvement in the quality and length of peoples’ lives2,3. As a result, innovation and new technology often feels inevitable and desirable, with all new procedures feeling like progress towards better care.
This two-part series sets out the contemporary challenges and opportunities for surgical innovation in the UK. The first part describes the current processes and potential pitfalls of current device regulation, and the limitations in our ability to appraise these innovations. It describes the potential risks this poses to patients and healthcare funders. Furthermore, we discuss why case series and cohort data should not be relied upon by surgeons seeking to introduce new techniques into their practice. The second part (published in the next issue) describes potential solutions to this problem, including a national registries programme, initiatives by the orthopaedic community and the role of randomised trials in this critical and valuable area of orthopaedics.
Innovation has many dangers, and problems often arise that we did not anticipate. There have been well-documented examples of orthopaedic innovations that have caused unexpected harm. By their nature, these events are unpredictable, with new problems potentially representing ‘unknown unknowns’,
albeit that unexpected complications that occur with new procedures may be better recognised as ‘known unknowns’.
We may not feel that we can consent patients for these risks. Consent should include all material risks, whereby it is considered that a new procedure or device has an unknown safety profile. Experience tells us that undertaking new procedures may bring serious yet unanticipated problems, and as surgeons, it would be wise to be transparent about this.
While technological development causing harm is the most commonly cited concern, there is a much greater risk that many simply don’t infer benefit yet cost more. In this context, they represent poor value for money. Scrutiny of value is currently poorly conducted in healthcare generally and at the spearhead of medical innovation specifically. With a fixed budget healthcare system, investing in poor value healthcare in one area necessarily removes finance from another.
While we learn important lessons from each event, we also need to learn wider lessons about innovation in general. Each innovation cycle may bring benefits for patients, but also additional risk. Therefore, it is important that we consider as a community how we can protect patients while continuing to improve the treatments we offer them. The aim of this article is to explore how we currently innovate, how practicing surgeons can innovate safely and in the second part of this series, where we as a community might improve for the future.
Features
Chetan Khatri is a PhD student at Warwick Clinical Trials Unit and a ST3 trainee in the Warwick Orthopaedic Specialist Training Programme.
Steve Gwilym is a Consultant Orthopaedic Surgeon specialising in the management of shoulder disorders and his research interests are focused around optimising outcomes after traumatic injury and upper limb surgery. Professor Gwilym chairs the British Elbow and Shoulder Society Research committee.
24 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk
Professor Xavier Griffin is the Chair of Barts Bone and Joint Health, and leads academic orthopaedics at Queen Mary University of London and Barts Health NHS Trust. Xavier’s vision is for world-class excellence in research and clinical academic training; providing opportunity for the next generation of clinician scientists to realise their aspirations.
What is an innovative procedure?
An innovative procedure has been described as ‘a new or modified surgical procedure that differs from currently accepted local practice, the outcomes of which have not yet been described and which may entail risk to the patient’4. Surgeons are intuitively innovators, constantly seeking ways to improve the care they provide. Sometimes, this might be a stepchange, such as a new implant or procedure. In other cases, innovation involves an iterative adaption or modification of a procedure, where a clear point of change is difficult to pinpoint. For example, we may not appreciate that a software update can represent a major innovation. This grey zone of innovation is difficult to assess, but patients may still be exposed to uncertainties and risk.
The introduction of a new implant or a new instrument are more easily defined and understood. The introduction of the total hip replacement has transformed the lives of those with degeneration of the hip. As such, it has been labelled as the operation of the 20th century 2 Subsequently there were serial modifications of the low friction arthroplasty without simultaneous rigorous evaluation, with disastrous results of high failure rates, such as the 3M capital hip replacement 5. At the time, without a centralised, co-ordinated, monitoring programme, a call to mandate a national joint registry was triggered across the medical profession 6
Keith Tucker was involved in the introduction and development of the NJR. He is chair of ODEP and the Beyond Compliance advisory group and a member of NORE. He is a member of the MHRA metal on metal group. He is a retired orthopaedic surgeon.



Anterior cruciate ligament reconstruction has been shown robustly to improve patient reported functional outcomes, compared with rehabilitation alone7. In the search of the optimum graft, surgeons looked to synthetic options. While early results supported their use in the short to medium term8, further evidence emerged to suggest a higher-than-expected failure rate9. Within foot and ankle surgery, a hemiarthroplasty for the first metatarsal-phalangeal joint was developed to have the biomechanical properties of healthy cartilage. It promised a solution to hallux rigidus. However, its early evidence showed a higher-than-expected failure rate10
These examples describe only a fraction of the increasing problem with device safety11. Between 2006 and 2010, the Medicines and Healthcare products Regulatory Agency (MHRA) issued 2,124 safety notices, representing an 1,220% increase in volume of reports over a five-year period12
How are devices regulated?
The majority of devices and implants are developed within the United States, the UK and the European Union. Within the United States, there are two main routes for approval. The 510(k) process allows devices to be approved if they show equivalence to an existing product. In this scenario, clinical trials are not required. However, the definition of equivalence can be interpreted loosely, although this criterion is likely to change13 . The second, more stringent method, Pre-Market Approval, requires controlled trials. However, of the devices approved, fewer than one-third of devices have undergone randomised trials and only half the trials included a control group14. The obvious brake that randomised trials apply to innovation are the costs associated with running a trial and the timeline to generate a meaningful result. Furthermore, clinical trials that focus on efficacy are also almost always underpowered to detect harm.
Until recently, both the UK and European Union relied upon on the Conformité Européenne (CE) approval and this process has often been regarded as a lighter touch than FDA Pre-Market Approvals, meaning many enterprises would seek CE approval well before costly approvals in the United States. For example, EU approval for a guidewire used in angioplasty required a 22-patient cohort study, while the FDA regulators required an 800-patient multicentre randomised controlled trial15. Carl Heneghan, a professor of evidence-based medicine, exposed a number of weaknesses in the CE marking system by gaining approval for mesh bag used to carry fruit to be implanted in bodies16. The regulatory environment in the EU and UK is in flux; the European Union has just introduced the new Medical Devices Regulations and we in the UK, the Medicines and Medical Devices Act 2021. The details of how these will impact orthopaedics are only just being understood. This may be particularly challenging for smaller enterprises or for devices with low usage (such as for rare diseases) where the costs of meeting the new requirements may outweigh the financial rewards of licencing them.
While regulation is an important step in maintaining safety, it represents a low bar for determining patient safety and can be slow to respond to emerging data and experience. If we are going to effectively prevent harm from new innovations, we need to go beyond this to understand how we can use outcomes and data to protect our patients. >>
Features
Edward Davis is a Consultant Orthopaedic Surgeon in Stourbridge and the West Midlands.
JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk | 25
“Historically, surgeons innovated in using ‘see one, do one, teach one’ principles, with successes or failures reported only as anecdotes or personal experience.”
Interpreting early data

Historically, surgeons innovated in using ‘see one, do one, teach one’ principles, with successes or failures reported only as anecdotes or personal experience. The essential need for data on all patients undergoing innovation is now wellunderstood. The Cumberlege report – written in response to several medical and surgical scandals including the problems of trans-vaginal mesh implants – was clear that we should all be engaging with data collection and reporting of outcomes17 Failing to collect or report data means that problems cannot be identified, and patients are exposed to harm in each new centre that takes on a new technique.
Traditionally, surgeons have reported clinical outcomes of innovative approaches as caseseries. While such papers often provide early data on an intervention, suboptimal outcomes may not be published for fear of personal or department reputation, leading to mistakes being repeated elsewhere. They are also inherently flawed in their ability to determine risks, the effectiveness of procedures and value to the healthcare system.
With many musculoskeletal conditions, patient reported outcome measures (PROMs) improve over time, irrespective of treatment allocated to them. The natural history of PROMs to improve over time is a remarkably common feature of outcomes in orthopaedics, with good evidence that this happens in rotator cuff tears, back pain, meniscal tears and osteoarthritis, a manifestation of the principle of regression to the mean18, 19, 20, 21, 22 . This also leads to false reassurance when assessing case reports, as an improvement in PROMs is almost inevitable and does not necessarily mean that the operation itself was of benefit.
A recent example of how this can mislead is the subacromial spacer balloon, where multiple case reports showed improvements from baseline and were reported as showing evidence that the device was effective. However, such improvements over time are typical for many treatments for rotator cuff disease19. A subsequent randomised trial found worse results when the balloon was used compared to when it was not23. Females had particularly poor results, something that had not been identified in case series. A reliance on early case series data resulted in 30,000 patients across Europe receiving a device which was shown to have no meaningful benefit, and possible harm, in subsequent robust studies.
Case series may have a role in the early stages of a new innovation24, 25 and can be used to describe the refinement of a technique or explore the indications for use of a technique in development centres. They may be considered proof-ofconcept records, describing innovation. Larger case series may provide some understanding of risks, although effective registries are much better for this due to the scale they can achieve. However, the greatest risk to case series data may be that they encourage others to adopt similar practice and provide false reassurance, potentially multiplying harm, with a cessation of the interrogation of the innovation so that it is considered ‘standard practice’.
Reducing our reliance on case series reports is a major challenge to surgeons. However, with increasing sophistication in our methods for collecting data routinely, we can innovate safely. In part two of this article, we will explore how routine and collaborative data collection, registries and trials can all be used to innovate effectively and safely.
Summary
While surgeons are constantly seeking to embrace new technology or devices that may improve the health and function of the people they serve, they should be aware of the potential risks this innovation may also bring. Stifling innovation is undesirable. However, without careful consideration and evaluation of new interventions, the next disaster is a case of when, not if.
Before adopting a new device, clinicians and health funders should be cautious of the regulatory approvals and evidence base behind it. Case-series or cohort data are appealing, but have many hidden limitations. Improvements in PROMs may provide false reassurance that an operation is effective and poor results may not be reliably reported.
We need better systems and studies before routinely adopting new devices and techniques into practice. The second part in this series goes on to describe ways in which surgical communities are developing systems to safely innovate through the appropriate use of registries, routine data collection and randomised trials, and ways we may continue to develop in the future. n

References
References can be found online at www.boa.ac.uk/publications/JTO
Features
Andrew Metcalfe is Professor of Orthopaedics at the Warwick Clinical Trials Unit, and a Consultant Orthopaedic Surgeon at University Hospitals Coventry and Warwickshire where he specialises in knee surgery.
“Each innovation cycle may bring benefits for patients, but also additional risk. Therefore, it is important that we consider as a community how we can protect patients while continuing to improve the treatments we offer them.”
26 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk
David Beard is Professor of Musculoskeletal and Surgical Science and Director of the RCS England Surgical Trials Unit at Oxford University (SITU NDORMS). He has a long-standing interest and expertise in trials for the evaluation of devices and surgical innovation, particularly for surgery and complex healthcare interventions.






01827 214773 malcolm.pearson@unitedorthopedic.com uk.unitedorthopedic.com
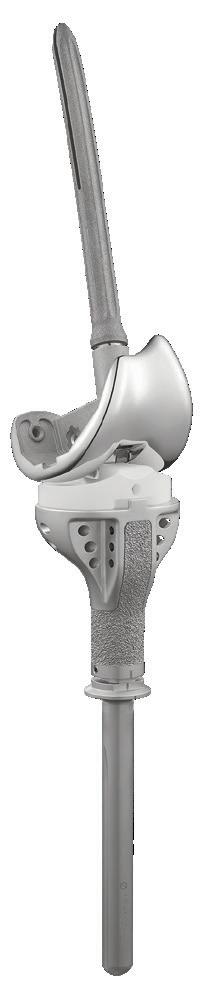
Knee & Limb
Designed for extensive reconstruction of the hip and knee joint and based on over 20 years’ clinical experience of the 1st generation USTAR system. The USTAR II™ system is part of the United Orthopedic family of products designed for difficult primary and revision interventions. Come and see us at BOA Congress on stand 56
USTAR II™ Hinge
Salvage System
Irrum Afzal is the Research and Outcomes Manager at the South West London Elective Orthopaedic Centre.

Irrum is an Imperial College Graduate securing a distinction in Masters of Public Health. She has most recently completed a Postgraduate Diploma in Sustainability Studies and now leads the Sustainability at SWLEOC with her colleagues Professor Kader and Mr Asopa. Irrum is the Co-Director of the London Research Course and is a professional member of the Health Research Authority Research Ethics Committee. Irrum is a member of the BOSTAA trainee committee. She is an active member of the British Orthopaedic Association, National Orthopaedic Alliance, British Hip Society and the British Orthopaedic Sports Trauma and Arthroscopy Association. Outside of clinical research, Irrum plays an active role in the Orthopaedic Research and Education Foundation and the Imperial College London Alumni Service.
Sustainability in Orthopaedics – Let’s Share Best Practice
Irrum Afzal, Vipin Asopa and Deiary Kader: Colleagues from NOA member organisation, the South West London Elective Orthopaedic Centre (SWLEOC)

Sustainability in surgery continues to garner significant attention and support, as global warming and climate change persist as evergrowing issues.
The NHS is the largest single contributor of greenhouse gas emissions in the public sector and NHS England has an annual carbon footprint of 24.9 million tonnes of CO2e.
The carbon footprint of an operating department within a large UK hospital is estimated at 5,000 tonnes CO2e/year and a single operation at 150-250kg CO2e. In light of this, there is a significant challenge ahead to enable surgery to meet net zero carbon by 2045, in line with the Greener NHS strategy. A big part of achieving this will be sharing best practice and continued collaboration between Trusts and healthcare systems.
Features
28 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk
Vipin Asopa PhD FRCS (Tr & Orth) is a consultant hip and knee surgeon based at the South West London Elective Orthopaedic Centre. He has completed a PhD in articular cartilage biology at the Kennedy Institute, before completing his higher orthopaedic surgical training in North West London and fellowship training at Sportsmed SA, Adelaide and The Royal Berkshire Hospitals NHS Foundation Trust. He has recently received Orthopaedic Research UK(ORUK) funding to investigate the optimal conditions for harvesting stem-cells from adipose tissue. Additionally, Mr Asopa is a Python coder and primary investigator for a study titled, ‘The use of machine learning in the early detection of failing total hip replacements’. This is a project that is also being supported by ORUK.
Professor Deiary Kader is a Consultant Trauma and Orthopaedic Surgeon working at the South West London Elective Orthopaedic Centre (SWLEOC). He is the Director of Research of the Academic Surgical Unit, SWLEOC. Professor Kader initiated sustainability at SWLEOC and leads it with his colleagues Mr Asopa and Ms Afzal. He is also Director of the London Research Course. Professor Kader is President of BOSTAA. He is also a visiting professor in the Faculty of Health and Life Sciences in Northumbria University and a director of OASIR Research group (www. oasir.co.uk). Since 2010 Professor Kader has been dedicating a significant amount of his time to humanitarian work with NGMV medical charity (www.ngmvcharity. co.uk) and more recently with the International Committee of the Red Cross (ICRC) and Swisscross Foundation.
At the South West London Elective Orthopaedic Centre (SWLEOC), Professor Deiary Kader initiated a ‘Sustainability in Surgery’ initiative back in 2021. Professor Kader proposed to have ‘Sustainability’ added as an additional pillar to the existing Clinical Governance framework, with regular meetings led by Professor Kader, Vipin Asopa and Irrum Afzal. The overall purpose of this initiative is to improve sustainability, and to provide strategic direction and leadership to ensure there is environmental, financial, and social sustainability. This would be achieved by promoting efficient and cost-effective use of healthcare resources, while reducing variability of care and improving patient outcomes. This initiative was widely accepted by the centre and supported by SWLEOC Medical Director, Vipul Patel and Director, Mary Richardson.


Various teams at SWLEOC undertook a series of audits reviewing environmental, financial, and social sustainability. Dr Kar May Phoon and Amit Sagi shared results from these
audits at the National Orthopaedic Alliance (NOA) Annual Members’ Conference back in 2021 – a thought-provoking session with colleagues from across the country. Work that has been highlighted since then from across the NOA membership has been very promising.
The inaugural NOA Excellence in Orthopaedics Awards in 2022 was one such example of showcasing work being done in orthopaedics to help make the speciality more sustainable. Finalists in the Working Towards Net Zero category included:

• The Robert Jones and Agnes Hunt Orthopaedic Hospital NHSFT – The RJAH Green Plan (winning entry).
• South West London Elective Orthopaedic Centre – Successful implementation of sustainability projects using Com-B Model.
• South West London Elective Orthopaedic Centre – Recycling of Walking Aids.
Scan the following QR code to view project posters for these initiatives.
The Awards are back for 2023 and an awards ceremony will be held in Birmingham to announce the winners on 19th October, following the NOA Annual Members’ Conference. To view the list of 2023 finalists and find out more about the awards, scan the following QR code: n

Features
JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk | 29
20 Years of the National Joint Registry: who benef its?

Part 2: surgeons and implant suppliers
The National Joint Registry (NJR) was founded in 2002 and started collecting data to monitor the performance of hip and knee replacement surgery in England and Wales in 2003. Since then, we have expanded both our scope of joints and territories covered. In this second of a threepart series, we describe the value of the NJR, its data resource and its outputs to clinicians and implant suppliers. These benefits include personalised outcomes reporting, information for clinician annual appraisal, real-time safety checks during surgery, implant usage and information required for regulatory compliance, an international implant classification system and support for the wide adoption of best practice. In part three, we will describe the benefits to service commissioners, regulators

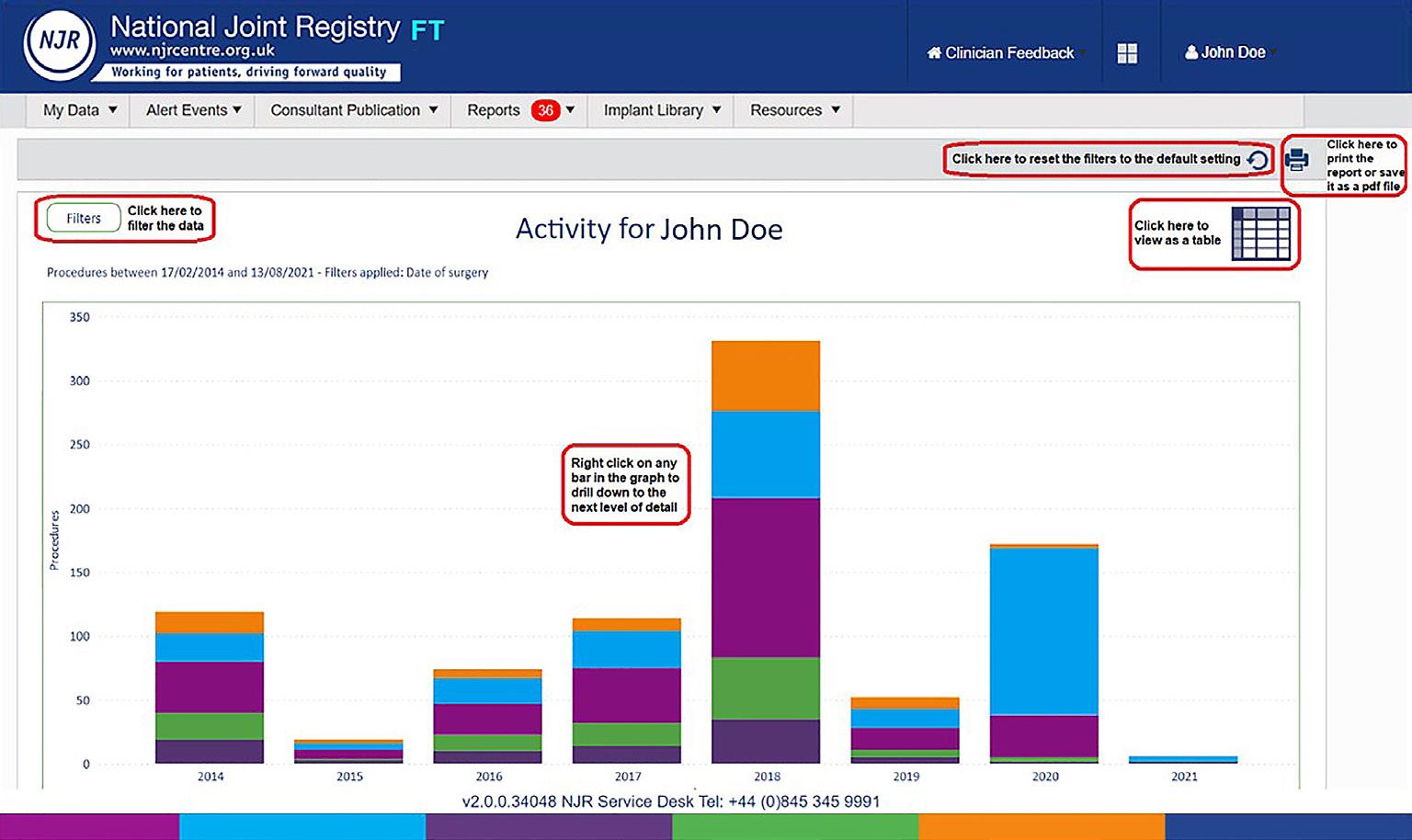

and policymakers and the broader benefits to society (including research and innovation).
Benefits to surgeons
Clinician feedback and annual appraisal
Clinicians are the drivers of the NJR, both as contributing surgeons and through their clinical leadership of the organisation. Surgeons have been prepared to participate in setting the highest standards for themselves, as shown in the publication and review of activity on an annual basis. Through the NJR, clinicians have access to a large repository of clinical data that has been curated over 20 years. The quantity of data available means that analyses are more comprehensive and more accurate, providing surgeons with information upon which they can base decisions about their clinical practice.

Features
Peter Howard, Tim Wilton, Derek Pegg, Mike Reed and Richard Armstrong
Peter Howard is an Orthopaedic Consultant in Derbyshire. He is Past President of the BHS and Chair of Surgical Performance and Implant Scrutiny Committees for the NJR.
Tim Wilton is a Consultant Orthopaedic Surgeon at Department of Orthopaedics, Royal Derby Hospital, Derby, with specialist interests in knee and hip replacement surgery. He is Medical Director of the NJR.
Key to Figure 1. 30 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk
Figure 1: An example of activity report available to NJR-registered surgeons as part of the Clinician Feedback system in NJR Connect - Data Services. Key included (left).
Mike Reed is a Consultant Orthopaedic Surgeon for Northumbria Healthcare NHS Trust. Mike is a member of the NJR Steering Committee, Chair of the NJR’s Editorial Committee and sits on Council of the British Orthopaedic Association.


Richard Armstrong heads the NEC Software Solution’s Registries. Having worked extensively in the field of healthcare informatics, he manages the delivery of national programmes associated with the collection and reporting of clinical and administrative healthcare data.

Through our Clinician Feedback service within the NJR Connect platform, the NJR provides surgeons with a personalised view of their data on total practice and outcomes for their patients, and compares this to national benchmarks. We link patient records across hospitals and notify the surgeon when a patient that they have operated on is subsequently revised, providing them with details of the revising surgeon to facilitate followup review, regardless of which hospital the revision takes place at. We also notify surgeons should their patient die within 90 days of surgery.
Near real-time outcomes information
Through our online platform, NJR Connect, dynamic reporting of clinical activity and outcomes is available. This includes analyses of patient, joint, and prosthesis sub-types that can be customised by the end user to answer specific questions about the patients under their care. Annual Consultant Level Reports also provide detailed and unique summary information that support the clinician in reflecting on the outcomes of their entire practice across the hospitals at which they have worked. This clinical information is essential to support evidence-based implant choices, for annual clinical appraisal, revalidation and for improvement of practice, and is probably the most detailed outcomes report of any medical specialty in the UK.

The NJR Annual Report
Every year the NJR produces an annual report, unveiled at the BOA Annual Congress each September, and includes analysis of all hip, knee, elbow, shoulder and ankle data entered into the registry since 2003. Currently, this includes 3.7 million operations. This analysis shows time trends in implant usage and the survivorship (revision rates) of implant constructs, comparing both class and brands of implants by age and gender. Analysis also includes mortality rates by age and sex of patients undergoing joint replacement. Every year additional bespoke analyses are included, for example comparing the effect of using different bearing types. The annual report is an easy to access comprehensive guide to how implants perform in different groups of people, and thus enables surgeons and healthcare providers to plan evidence-based, individualised care for each patient. The annual report has a direct influence on clinical practice, both nationally and internationally.
Examples include the improvement of patient selection for hip resurfacing and the almost complete cessation of large head metalon-metal hip replacement.
Real-time safety checks during surgery
The NJR also supports the surgical team during prosthesis implantation. Our implant scanning app ensures implant compatibility before the device is taken out of its sterile packaging during surgery. The scanning tool, available as both desktop and mobile applications, scans device barcodes and provides an immediate, intra-operative ‘pass or fail’ compatibility check in respect of implant size and side. This service is also available as an application programming interface to provide the logic rules to existing hospital theatre systems. The development of this tool arose as a response to the Healthcare Safety Information Branch investigation into a case of wrong-sided surgery that recommended surgical teams be supported in establishing the compatibility of implants intra-operatively. At the other end of an implant’s lifetime, if a surgeon needs to revise an implant that is recorded in the registry, but lacks information on the prosthesis specifics to plan the revision, the NJR can also provide these details if the surgeon sends a simple email to request the information to the following address: enquiries@njrcentre.org.uk.
Benefits to implant suppliers
We provide implant suppliers with high-quality, comprehensive data and associated statistical analysis to support their regulatory postmarket surveillance obligations on the usage and outcomes of their devices. Our analyses enable implant suppliers to assess variations in outcomes across patient groups, across different hospitals and across different surgeons. We also provide a comparison to similar types of devices from other manufacturers. Our analyses also enable implant suppliers to identify ‘off-label’/ non-approved use of their products, and we support follow-up actions with hospitals and surgeons to investigate these cases.
Implant performance data for medical device regulations
We provide implant suppliers the opportunity to request additional patient-outcome scores from patients who have received their devices for their ongoing assessment of patient outcomes and to support their submission to the regulatory authorities or notified bodies. This service includes providing access to pseudonymous record level data to support internal analysis, access to routine, high-quality statistical analysis reports on implant catalogues to support post-market surveillance, >>
Features
Derek Pegg is a Consultant Trauma and Orthopaedic Surgeon in Mid Cheshire Hospitals Foundation Trust, Leighton Hospital, Crewe. He is Chair of both NJR Regional Clinical Coordinators Committee and NJR Data Quality Committee.
JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk | 31
Figure 2: Example display of the NJR implant scanning tool.
and the ability to commission bespoke and ad hoc reports, and the collection of bespoke PROMs.
The provision of a robust implant surveillance system allows the relative performance of different prosthesis components to be compared, enabling the development of an early warning system to detect inferior performance. This system enables not only the detection of ‘outlier’ implants for manufacturer and regulators, it also enables the early identification of borderline outliers to allow further examination of performance prior to alarm-level findings. Examples of the value of this system include the following case: In 2014, Finsbury Orthopaedics issued a field safety notice concerning high failure rates of smaller sizes of the Adept Hip Resurfacing. This was based on supplier feedback from the NJR, and followed our 2012 publication demonstrating unacceptably high failure rates in women and with smaller-sized hip resurfacings in men. In another case in 2015, Smith+Nephew issued a field safety notice concerning the Birmingham Hip Resurfacing (BHR) based on NJR data, stating “The use of BHR in female patients is to be contraindicated.” Yet again, in 2022, the NJR provided analysis to the regulator that identified that two variants within the NexGen knee system were associated with worse outcomes than the rest of the NexGen family when used with a specific tibial component.
This resulted in a large-scale field safety notice that the NJR supported by providing lists of affected patients to units.
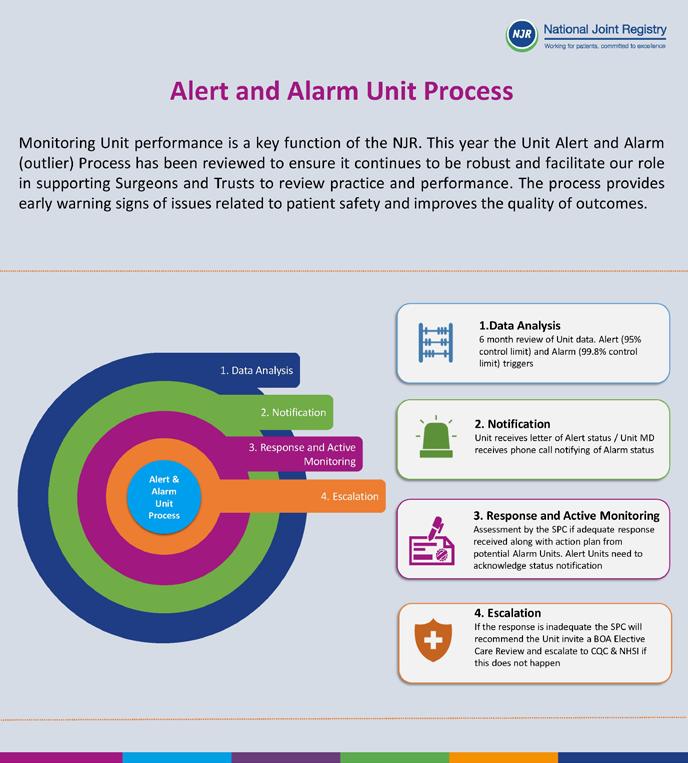
The international implant classification system
One of the NJR’s key achievements in respect of implant surveillance is the development, in collaboration with the German Arthroplasty Registry (EPRD), of a standardised implant classification system that enables all joint replacement registries to use the same unifying set of definitions to describe the characteristics of a hip or knee implant. In 2022, this classification system was adopted by the International Society of Arthroplasty Registries (ISAR) as the global standard. This unifying international standard will further enhance global collaboration in the identification of exceptional and under-performing implant characteristics. Work is now underway to develop equivalent classifications for other joints.


Outlier identification
and support Transparency and robust high standards of scrutiny are central drivers of NJR activity. We demonstrate this primarily through the findings and recommendations of the NJR Surgeon Performance Committee and the NJR Implant Scrutiny Committee. The actions brought forward by these committees are implemented in tandem with other stakeholders, including the British Orthopaedic Association. The principles of this activity, outlined in the NJR’s Accountability and Transparency Model, are to survey the outcomes associated with all surgeons, hospitals and implants recorded on the registry. This twice-yearly exercise identifies statistical outliers who are requested to review their performance and where necessary, develop an action plan to improve their outcomes. Alongside the notification of outliers, we also routinely identify and notify surgeons with borderline (alert) level outcomes, so that they may closely examine their performance data to try and avoid tipping over to outlier (alarm) level. A similar exercise takes place for medical devices, with escalation of concerns to the Medicines and Healthcare products Regulatory Agency. Several medical devices have been withdrawn or recalled from the market as a result of this activity, and the NJR is able to respond to these manufacturer field safety notices by rapidly sending lists of affected patients to hospitals to contact for review and follow-up.
Summary
We hope we have given a flavour of some of the benefits the NJR delivers to clinicians and implant suppliers in this second part of our series. A fuller picture of these benefits can be found in the relevant sections of the NJR website (www.njrcentre.org.uk). In the final part of this series, which will be published in March 2024, we will cover the benefits of the NJR to service commissioners, regulators and policymakers, as well as broader society. n
Features
Figure 3: Example NJR Industry Report comparing 15-year outcomes of a sample knee brand to the rest of the market.
Figure 4: Example of part of the international implant classification system for hips and knees.
32 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk
Figure 5: Schematic representation of the NJR Alert and Alarm process.
independent sector · healthcare professionals · doctors · nurses · regulators commissioners · implant suppliers · patients · surgeons · nhs · hospitals
orthopaedic specialist societies · independent sector · healthcare professionals doctors · nurses · regulators · commissioners · implant suppliers · patients surgeons · nhs · hospitals · orthopaedic specialist societies · independent healthcare professionals · doctors · nurses · regulators · commissioners · suppliers · patients · surgeons · nhs · hospitals · orthopaedic specialist societies
independent sector · healthcare professionals · doctors · nurses · regulators commissioners · implant suppliers · patients · surgeons · nhs · hospitals
orthopaedic specialist societies · independent sector · healthcare professionals
doctors · nurses · regulators · commissioners · implant suppliers · patients surgeons · nhs · hospitals · orthopaedic specialist societies · independent healthcare professionals · doctors · nurses · regulators · commissioners · suppliers · patients · surgeons · nhs · hospitals · orthopaedic specialist societies
independent sector · healthcare professionals · doctors · nurses · regulators commissioners · implant suppliers · patients · surgeons · nhs · hospitals
orthopaedic specialist societies · independent sector · healthcare professionals
20 patients · surgeons · nhs · hospitals · orthopaedic specialist societies ·
doctors · nurses · regulators · commissioners · implant suppliers · patients surgeons · nhs · hospitals · orthopaedic specialist societies · independent healthcare professionals · doctors · nurses · regulators · commissioners · suppliers · patients · surgeons · nhs · hospitals · orthopaedic specialist societies
independent sector · healthcare professionals · doctors · nurses · regulators
njrcentre.org.uk
reports.njrcentre.org.uk Visit us at Congress - stand 72
A sustainable trauma service – we must make this a priority

Sharon Scott
With thanks to Mr Bob Handley and Mr Will Eardley
Sharon Scott is an orthopaedic surgeon in Liverpool and specialises in trauma surgery, including pelvic and acetabular fractures. She was integral to the development of the Cheshire and Mersey Major Trauma Network & Centre and spent five years as a clinical member of the Major Trauma and Burns Clinical Reference Group. Her passion is to improve the profile and care provided to trauma patients across the UK.
Asustainable trauma service can be defined as one which has the ability to be maintained and supported continuously over time. To be sustainable, it must be structured to respect its resources; physical, financial and personnel. To be worth sustaining, it must meet the needs of the population it serves. These factors must be considered as the United Kingdom’s National Health Service addresses surgical elective recovery and sustainable trauma care provision.
Orthopaedic trauma care is being lashed by the tail of the pandemic. Staff shortages, resource scarcity and a deconditioned population combine to present a problem never before encountered. Set against the context of an ageing population, these challenges are ever-growing. There are also unwarranted variations of care – both within and between regions – as well as an ineffective use of resources. This has been demonstrated by the recent GIRFT (Getting It Right First Time) deep dives and ORTHOPOD evaluation1, which highlights, in particular, poor provision of day case fracture surgery. Compliance with guidelines on the timing of fracture surgery also varies. Many UK centres operate promptly and within target timelines. Several, however, do not, and there is no current mechanism to match demand and capacity out with individual providers.
Although the evidence base improves, there remain many procedures that the rationale of care and in particular the timing of and location in which surgery is performed in
terms of outcome, is unclear. Data validation, outcome assessment, and both unit and surgeon level performance metrics are absent. Similarly, network level performance assessment and, indeed, networks period are something that do not feature in the delivery of orthopaedic trauma care in 2023.
Much focus is on elective recovery due to huge waiting lists and national agenda. Individual surgeons, anaesthetists and all members of the wider team are reflecting on their work-life balance. This latter factor carries huge and a difficult to quantify impact, as resilience is tested. There are positives, however.
The elective recovery programme is supporting unprecedented collaboration across regions and ‘micromanagement’ on a national level appears to be delivering the virtually impossible. Development of regional teams consisting of both clinical and operational colleagues allows improved communication and visibility of challenges. There is considerable investment in digital solutions to support elective recovery, with development of regional dashboards monitoring theatre performance, for example.
Our trauma service needs to capitalise on and mirror these initiatives, and must have a datadriven approach. Regional fracture networks should be commissioned (potentially on the Major Trauma Network footprint) and digital patient management systems should be seen as mandated practice.
Features
34 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk
“Orthopaedic trauma care is being lashed by the tail of the pandemic. Staff shortages, resource scarcity and a deconditioned population combine to present a problem never before encountered. Set against the context of an ageing population, these challenges are ever-growing.”
The importance of evidence-based medicine and a data-driven approach to trauma have been repeatedly demonstrated in the medical literature: improving the accuracy of diagnosis, treatment decisions and reducing the risk of adverse events. Cloud-based systems facilitate data-driven decision-making and have been shown to allow adaption to changes in demand, delivering safe effective care2. They also provide safer pathway management, both within and between providers, with improved data accuracy which can easily be audited.
Regional dashboards presenting fracture surgery demand and capacity could also be of great benefit, in reducing unwarranted variation and improving access to care. This would be of particular benefit for ‘ambulatory’ trauma patients. It is time to break the dogma of siloed care and enhance a match of patient, capacity and capability. Designated day case fracture surgery lists are required and commissioning of regional hubs should be considered. Fracture surgery undertaken in a timely fashion is easier, quicker, and results in reduced patient morbidity and mortality. The economic argument for doing all we can to get people back to work promptly, is powerful.
The Cheshire and Mersey Reducing Surgical Risk Senate is utilising AI (artificial intelligence) to quantify individual patient risk and modifiable risk factors for patients on elective waiting lists3. There is already evidence that identifying high-risk patients with targeted interventions

can reduce peri-operative complications4, and this technology can and should be used for our trauma patients. This would have the benefit in reducing morbidity and mortality, length of stay and potential dependency on social care.
Virtual fracture clinics (VFC) have demonstrated their effectiveness5, particularly during the pandemic, and should be mandated. The approach of ‘patient initiated follow up’ (PIFU) also garnered support during this period, with the COVID-19 BOAST6 supporting the decision not to follow patients up routinely until radiological union if otherwise progressing as expected. Not to mention the environmental benefit of such practices, they would improve the efficiency and accessibility of fracture clinic appointments for those who need them.
Our existing trauma databases (National Hip Fracture Database and Trauma Audit & Research Network) have been proven to drive improvements in patient care and thought must be given to national oversight of all the remaining non-fragility femur or open fracture trauma patients. This would require investment in data collection systems. Our trauma service will not be data-driven without good quality data, which must include the impact on our patients (PROMS: patient reported outcomes measures).
There are a number of actions which could be undertaken at a local level and which require minimal, if any resource:
• Pathway review. The advent of VFC has proven to be beneficial, but also risks inadvertently incurring delays to surgical care. It has never been easier for patients to be discharged from the emergency department, without being seen by the orthopaedic team and managed through the VFC, which may enable patients to be seen in specialist clinics – but not necessarily promptly. The majority of fracture surgery should be undertaken within seven days and in most cases, sooner than that. Patients with displaced or unstable fractures should not leave the hospital without a decision regarding the need for surgical intervention and ideally be given a date for such. Clearly this means that a senior decision-maker needs to be involved in patient care from the point of presentation, with proof of concept of the benefit demonstrated both during the pandemic and recent industrial action.
• Embrace PIFU, with appropriate patient information and ‘safety-netting’ available.
• Ensure list planning and patient preparation is optimised to enable prompt starts on theatre lists, which is central to overall theatre performance.
The age profile of the population presents a challenge for trauma services and is perhaps a catalyst for change. The population is often said to be ‘ageing’, but it is not that we are >>
Features
JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk | 35
living much longer. The peak in our population timeline as the baby boomers of the 1960’s approach the threshold of frailty is followed by a trough of those of an age to provide the care they need. An opportunity to engage with new technology to support secondary fracture prevention, for example, and probably more importantly educating the population from a younger age, exists. Patients identified at high-risk of falls through AI programming – theoretically in primary care before they have a fracture – could enable appropriate interventions. Future health service provision and ‘planning’ must be predicated on the implications of a changing demographic and more attention focused on the medical care of these patients.
Finance is always a contentious concern and the health service may well be adequately funded. The problem is that money is not spent wisely. Short-term policies with headline grabbing targets are, and possibly already have, destroyed the NHS as originally conceived. Investment in digital solutions and commissioning collaborative projects will prove more economically viable in delivering a sustainable trauma and health service. Investment in data capture and research projects is essential to ensure our interventions are delivering what we expect.
Recruitment and retention need to focus on the needs of the personnel caring for trauma patients; ensuring roles and expertise are valued. Orthopaedic trauma surgeons must be enabled to deliver multi-disciplinary care with ortho-geriatricians – which has been shown to save money and reduce length of stay7. Experience and seniority should be acknowledged and maintained.
As an orthopaedic community, we must agree and lobby for priorities to sustainably
deliver the best care possible to trauma patients, protecting resources and avoiding an adverse impact on elective care. The focus of sustainability is often to protect physical resources, using reusable gowns for example. However, greater gain is often to be had from not doing the ‘unnecessary’ at all, in addition to doing necessary things more efficiently:
1) Where possible, manage injuries in a single visit at first presentation. All units should have agreed protocols for appropriate injuries to be managed in this way.
2) Patients who can be treated surgically as a day case, should be; on designated day case lists, which may be delivered collaboratively on a regional basis.
3) For those whose admission at first presentation is obligatory, they should be admitted to an environment where the correct team can provide care.
4) Our trauma service sustainability must be data-driven on cloud-based systems.
5) VFC and PIFU should become commonplace aspects of patient pathways.
6) Pathways must be managed and coordinated at a local and regional level, embracing digital solutions to deliver safe, effective care which can be monitored and audited.

7) Trauma research should be inclusive of as many trauma patients as possible.
No other element of a large commercial or public sector entity would plan or deliver this without project management and coordination. Administration support is often overlooked. This is where clinician
resilience and its entwined elements are perhaps most strained. Intelligent resource placement includes network management, administration and trauma nurse coordination. This can be written up as a system specification, and must be seen as the first and most important foundation for the change process.
Physical and financial sustainability can be directed with guidelines and protocols, then analysed with spreadsheets and pie charts, but often becomes focused on extrinsic rewards. Extrinsic rewards also play a part in effecting change and motivating a workforce, but people respond more sustainably to intrinsic rewards. They need some satisfaction from their work and most importantly, need to feel valued with a sense of purpose. From the current NHS position, with so many unhappy staff, creating the environment where the rewards are intrinsic would seem to be a challenge, but ‘right patient, right place and right team’ is a good start. n
References
1. Orthopaedic trauma hospital outcomes – Patient operative delays (ORTHOPOD) Study: The management of day-case orthopaedic trauma in the United Kingdom. Wei N, et al. Injury 2023.03.032.
2. Sephton BM, Mahapatra P, Shenouda M, Ferran N, Deierl K, Sinnett T, et al. The effect of COVID-19 on a major trauma network. an analysis of mechanism of injury pattern, referral load and operative case-mix. Injury. 2021;52(3):395–401.
3. Accuracy of a tool to prioritise patients awaiting elective surgery: an implementation report. Sharma V, et al BMJ Health Care Inform. 2023 Jan.
4. Transforming surgical waiting lists into preparation lists. Pritchard-Jones R, et al EBPOM 2023 Poster.
5. Sephton BM, Morley H, Mahapatra P, Shenouda M, Al-Yaseen M, Bernstein DE, et al. The impact of digitisation of a virtual fracture clinic on referral quality, outcomes and assessment times. European Journal of Trauma and Emergency Surgery 2021;48(2):1327–34.
6. Management of patients with urgent orthopaedic conditions and trauma during the coronavirus pandemic. Archived March 2021 boa.ac.uk
7. Multiple hospital organisational factors are associated with adverse patient outcomes post-hip fracture in England and Wales: the REDUCE record-linkage cohort study. Patel R, et al Age and Ageing Vol 51 Issues 8 August 2022.
Features
36 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk



@ConturaLtd Contura-Orthopaedics-Ltd Contura Orthopaedics Ltd w w w arthrosamid .com References: 1 Henriksen, M et al (2023) 3-year results from a prospective study of polyacrylamide hydrogel for knee osteoarthritis Osteoarthritis and Cartilage, Vol 31(5): P682–683 DOI:10 1016/j joca 2023 02 023 2 Bliddal H et al (2021) Polyacrylamide Hydrogel Injection for Knee Osteoarthritis: A 6 Months Prospective Study J Orthop Res Ther Vol 6(2) 1188 ISSN 2575-8241 For full details about warnings and precautions read the IFU. For more information and the IFU please visit https://www.arthrosamid.com or contact us at enquiries@arthrosamid.com Safe and sustained pain relief with a single injection2 See our NEW 3 year data SCAN ME OUS/ARTHRO/JAN2023/016 Visit us Stand 38 at BOA A new class of injectable therapy to treat knee osteoarthritis maintaining pain relief for 3 years1 INTRODUCING
Spicing up the Training Programme
Willem Schenk and Sunil Wijayasinghe
In 2009, during a lovely family holiday in Sri Lanka, we witnessed a road traffic accident. This event called my attention to the trauma burden for local hospitals, considering the hectic, seemingly lawless traffic situation.
Willem Schenk is an orthopaedic surgeon in Bury St Edmunds since 2001, who has a special interest in knee surgery, particularly Oxford knees. He has established registrar training opportunities for Belgian doctors since 2004 and Sri Lankan doctors since 2010, and is one of the Clinical leads for T&O for the International Surgical Training Programme of the Royal College of Surgeons.

The next day, I visited the local hospital and sat down over a cup of tea with the local orthopaedic consultant, Dr Sunil Wijayasinghe. He ran a very busy clinic with seven junior doctors. I enquired about the challenges for T&O in Sri Lanka. He mentioned that there was a demand for senior registrar level training posts abroad, as trainees require two years’ training outside Sri Lanka to become board-certified.
On my return to West Suffolk Hospital, the orthopaedic department was very enthusiastic about the idea of appointing Sri Lankans to
registrar positions. We had already established a successful registrar/fellowship programme with Antwerp, Belgium in 2004 and were keen to do the same with Sri Lanka.

In 2010, Yasas Jayasinghe arrived as a registrar and the first Sri Lankan to obtain a registrar level training position in the UK. He became an outstanding ambassador for the programme, which encouraged us to continue and expand our cooperation, ultimately integrating the training programmes. Beyond this, we have had one or two Sri Lankan registrars join our department each year and have expanded training opportunities to other Trusts in the region.
Members of our department have joined in with the Sri Lankan Orthopaedic Association (SLOA) Annual Meetings, conducted
International
38 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk
Bury St Edmunds on 18 November 2022 at the combined Sri Lankan Orthopaedic Association – East Anglian Orthopaedic Club meeting.
Sunil Wijayasinghe is an orthopaedic surgeon in Sri Lanka since 2000 who has a special interest in paediatric orthopaedics. Currently he works as the senior paediatric orthopaedic surgeon at the Lady Ridgeway Hospital for children, Colombo, which is the main tertiary care referral centre for children in Sri Lanka. He is a past president of the Sri Lanka Orthopaedic Association, member of the Board of Study in Orthopaedic Surgery and co-worker to establish training opportunities for Sri Lankan trainees in UK.

workshops, and have been external examiners for the MD exams in Colombo, participating in clinics, ward rounds and operating lists during our visits. In 2019, we organised the first SLOA regatta in Negombo, with traditional catamarans, crewed by local fishermen.

When the Royal College of Surgeons set up their International Surgical Training Programme, our experience dovetailed perfectly into this and I became one of the clinical leads for T&O for the ISTP. Our Sri Lankan doctors have come through the College portal ever since.
The ISTP has placed Sri Lankan doctors in several Trusts in the UK, including Oxford for specialist training in orthopaedic oncology, Sheffield for paediatric training, and Ipswich and Norwich for spinal surgery. Our current Sri Lankan fellow is specialising in foot and ankle surgery.
Over the years, the Sri Lankan doctors have made a great contribution to our department and have been able to match the standards of their British colleagues, including passing the FRCS exams.
Last November, we organised a combined meeting of the East Anglian Orthopaedic Club and the Sri Lankan Orthopaedic Association. We invited seven Sri Lankan orthopaedic surgeons, as well as BOA leaders and the Dean of Health Education East of England (HEEoE).
The Sri Lankan surgeons, with Dr Sunil Wijayasinghe as chef d’equipe, presented a comprehensive overview of the situation in their country. We heard about the history of the SLOA and the cooperation between our regions. We were informed about the massive
development and enhancement to their orthopaedic training programme, which was only initiated in the last 10 to 15 years, and has been modelled on UK and Australian training programmes.

After basic common trunk surgical training, doctors are selected into the basic orthopaedic training. During this period, they learn and practice orthopaedic principles and attend basic courses, like the AO basic course. They undergo regular appraisals including five RITA assessments, OSCE, OSVE and portfolio assessments to progress to higher orthopaedic training. After successfully completing this, they can apply for the MD Orth exam, which is taken at the PGIM in Colombo and the exam committee is joined by one international external examiner, usually from the UK or Australia. Trainees who are successful in passing this exam are eligible to do two years of final training abroad. The International Surgical Training Programme of the RCS has been a very useful portal to place fellows in UK Trusts.
The Sri Lankan registrars come with a significant theoretical and practical experience. Contrary to many other countries, they have considerate involvement as first surgeon in a large variety of trauma and orthopaedic cases, rather than just having assisted their superiors.
During the presentations, we were shown the enormous trauma and orthopaedic load in Sri Lanka and the very exciting opportunities that exist to be exposed to these. The sheer scale of complex cases, which I have witnessed during my visits to Sri Lanka, is phenomenal. This was confirmed by our first reverse fellow Ady Abdelhaq, who presented his experience of five months in the Lady Ridgeway Children’s Hospital in Colombo, under the guidance of Dr Sunil Wijayasinghe. His report can be found in the Traveling reports 2020 on the BOA website (www.boa.ac.uk ).
The logistical and financial challenges for those wishing to take up a fellowship in Sri Lanka were discussed by Professor Bill Irish, Dean of HEEoE and Mark Bowditch, Chair of the SAC (at that time). These are a major hurdle for many, as leaving home and family without a decent income is daunting. >>
International
JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk | 39
In January 2023, a delegation of the East Anglian Deanery, led by Professor Bill Irish, visited the PGIM in Colombo. There they had a good opportunity to discuss and scrutinise the Sri Lankan training programme. On their return to the UK this group, Mark Bowditch, Ady Abdelhaq and myself, as well as two Sri Lankan consultants, Dr Sunanda Udagedara and Dr Yasas Jayasinghe met on Microsoft Teams. We agreed to start a pilot project to send East Anglian Trainees to Sri Lanka, to do part of their rotation in a major training centre in Colombo or Kandy initially, and Jaffna to follow soon after. The best timing would be one to two years before the FRCS Orth exam and for a period of six months. This would guarantee experienced trainees to become actively involved in the Sri Lankan training programme and provide them maximum exposure to a world of orthopaedics not seen in the East of England. They will be able to join in with courses and workshops, like the advanced AO course. Assuming they return to the UK with a well-filled logbook, the Deanery will then recognise that part of the training in retrospect.
The Sri Lankan supervisors will assess and guide the UK fellows, so they comply fully with UK training requirements. The SLOA has decided to support trainees financially, to the same level as their Sri Lankan counterparts. This will give them sufficient means for housing and costs of daily living. Further grants from various organisations, such as the BOA, EAOC, Deanery and industry will however have to be secured. Professor Deborah Eastwood has given her blessing for this pilot, which will provide our trainees with an incredible opportunity to enrich their training in a completely different environment, but with the same educational support they are used to in the UK. It is almost unnecessary to mention the opportunity to explore the country’s culture, history, natural beauty and amazing cuisine.



We sincerely hope and expect this pilot to become a success and that a training period like this will be an invaluable contribution to a well-rounded T&O education. Similarly, we hope it will enhance the strong networks between the regions.

Once this fellowship model is established, this might be expanded to other parts of the world and other training programmes, which would help to create a global health network of knowledge and skills exchange that will enhance our lives.
I can whole-heartedly recommend this opportunity to my young and enthusiastic colleagues, and I hope they will make this into a sounding success that will continue for decades to come. n
International
“We sincerely hope and expect this pilot to become a success and that a training period like this will be an invaluable contribution to a well-rounded T&O education. Similarly, we hope it will enhance the strong networks between the regions.”
Dr Romesh Gunasekera with Mr Ady Abdelhaq.
Patients waiting to be seen.
40 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk
Willem Schenk with the T&O reverse fellows.
Screw Extractor with Speed Lock




Stainless Steel OrthoVise™ with Slap Hammer





Screw/Pin Removal Locking Pliers



Stulberg Incision Close Gelpi & Blade Set





Lighted Yankaur Suction Device
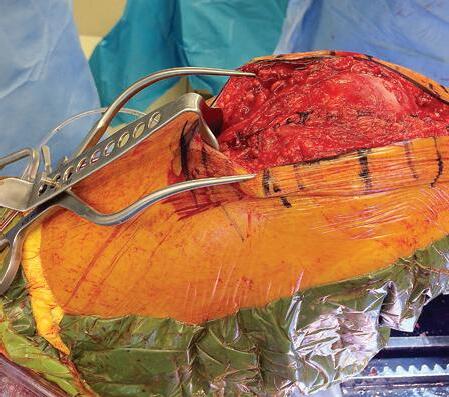

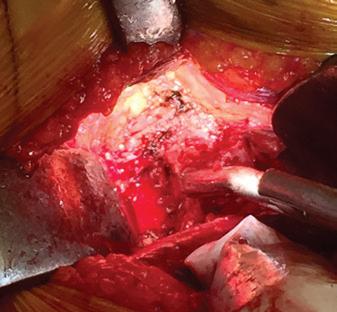
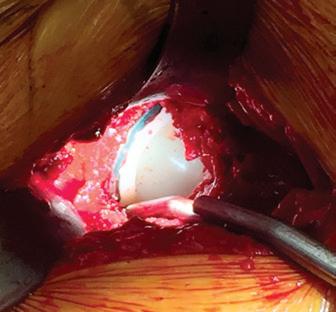
Universal extractor designed to accommodate a large range of screws and screw heads
Designed by Khaled Sarraf, MD & Konstantinos Doudoulakis, MD PRODUCT NO: 2021 Can also be used to help with removal of other devices that may require a twisting universal locking gripper. MADE EXCLUSIVELY FOR INNOMED IN GERMANY U.S. Patent D398,208 PRODUCT NO’S: Standard 3980 Large (10") with Large Slap Hammer 3980-01 Large (10") w/o Slap Hammer, w/Attachments 3981 Large (10”) without Slap Hammer or Attachments 3985 Small (8") without Slap Hammer or Attachements 3985-01 Small (8") with Small Slap Hammer Long Nose 3965 Large (12") with Large Slap Hammer 3965-01 Large (12") w/o Slap Hammer, w/Attachments 3966 Large Bent Jaw w/Slap Hammer 3966-01 Large Bent Jaw w/o Slap Hammer, w/Attachment 3975 Small (9.5") without Slap Hammer or Attachements 3975-01 Small (9.5”) with Small Slap Hammer Standard Long Nose Bent Jaw Long Nose
Unique jaw designed to solidly grip and clamp onto a screw head, broken screw, or pin for removal PRODUCT NO’S: S0142 [Standard] S0142-01 [Small] Standard Small Reduced jaw size for smaller screws, pins and incisions Designed to securely grab pins as small as 1.4 mm (.055") up to 2.4 mm (.095") Designed to securely grab larger pins, screw heads, or broken screws Standard Jaw End & Bite NEW Small Jaw End & Bite PRODUCT NO’S: 2760-00 [Set of 3] 2760-01 [11"] 2760-02 [14"] 2760-03 [16"] Sold Separately – Not In Set: 2760-XS [8.5"] Designed to help provide effective suction with the addition of a light source for enhanced visualization
Designed by Adolph V. Lombardi Jr., MD PRODUCT NO: 8016 -L Fromm Femur & Tibia Triangles Used for femur and tibia positioning Designed by S.E. Fromm, MD Designed to help expose difficult to visualize areas at the end of incisions
Designed by S. David Stulberg, MD PRODUCT NO’S: 4269-00 [Set – 1 Gelpi & 1 Blade] Also available Individually: 4269-01 [Gelpi] 4269-02 [Blade] PRODUCT NO’S: 8009-S [ACMI to Storz Adapter] 8009-W [ACMI to Wolf Adapter] Light Source Cable Adapters FREE TRIAL ON MOST INSTRUMENTS 1.800.548.2362 103 Estus Drive, Savannah, GA 31404 info@innomed.net 912.236.0000 Phone 912.236.7766 Fax Innomed-Europe Tel. +41 41 740 67 74 info@innomed-europe.com © 2023 Innomed, Inc. ISO 13485:2016 www.innomed.net Innomed-Europe Alte Steinhauserstrasse 19 CH-6330 Cham Switzerland Tel: +41 (0) 41 740 67 74 www innomed-europe com UK Distributor: Hospital Innovations Ltd Concept House Talbot Green Business Park Pontyclun UK CF72 9FG Tel: +44 1443 719 555 www hospitalinnovations co uk Can be attached to a fiber optic light cable with ACMI (female) connector. Extra Small size designed by S.E. Fromm, MD & Kenneth Merriman, MD
Abhinav Singh is the current BOTA President. He is a ST5 registrar in the North West Thames Deanery and a NIHR Doctoral Fellow at the University of Oxford. He has previously been a member of BOA’s Research Committee and set up BOTA’s Research Decision Tree.

The impact of trainee-led collaborative research within UK trauma and orthopaedics
Abhinav Singh, Ignatius Liew, Zaid Hamoodi, Sohail Nisar and Frank Acquaah
Ignatius Liew is currently an orthopaedic registrar in East of England, with an interest in joint preservation surgery. He is also the recipient of the Joint Orthopaedic Research Fellowship by the Royal College of Surgeons Edinburgh and ORUK. Ignatius will be starting his MPhil at University of Cambridge and University of Oxford, working with on musculoskeletal Human Cell Atlas. Ignatius is the current BOTA academic representative and past committee of Orthopaedic Research Collaborative East Anglia (ORCA). Through BOTA, his role is to promote and help deliver research through the BOTA/BOA research decision tree, as well as delivering research methodology courses.

In recent times the UK trainee-led collaborative approach to research in orthopaedics has been impressive. Trainee-led research offers the opportunity to run large-scale multi-centre service evaluations, audits and clinical trials by bringing together trainees into one collaborative group. The benefits of this approach are higher patient recruitment in less time and greater generalisability of study findings. For some research questions, such as weight-bearing in ankle fractures, this approach has served as a platform for demonstrating early feasibility and
gaining research funding to proceed toward a randomised control trial1. In other cases, studies like SupraMan2, WiTS3, FFPOM4, and IMPACT5 have all readily provided important epidemiological data, alongside rapid and robust evaluation of current practice.
The BOTA/RCS England/BOA Decision Tree
To further assist trainees with conducting impactful research, in collaboration with the BOA/RCS England Surgical Specialty Leads (SSLs)/Associate SSLs, BOTA created
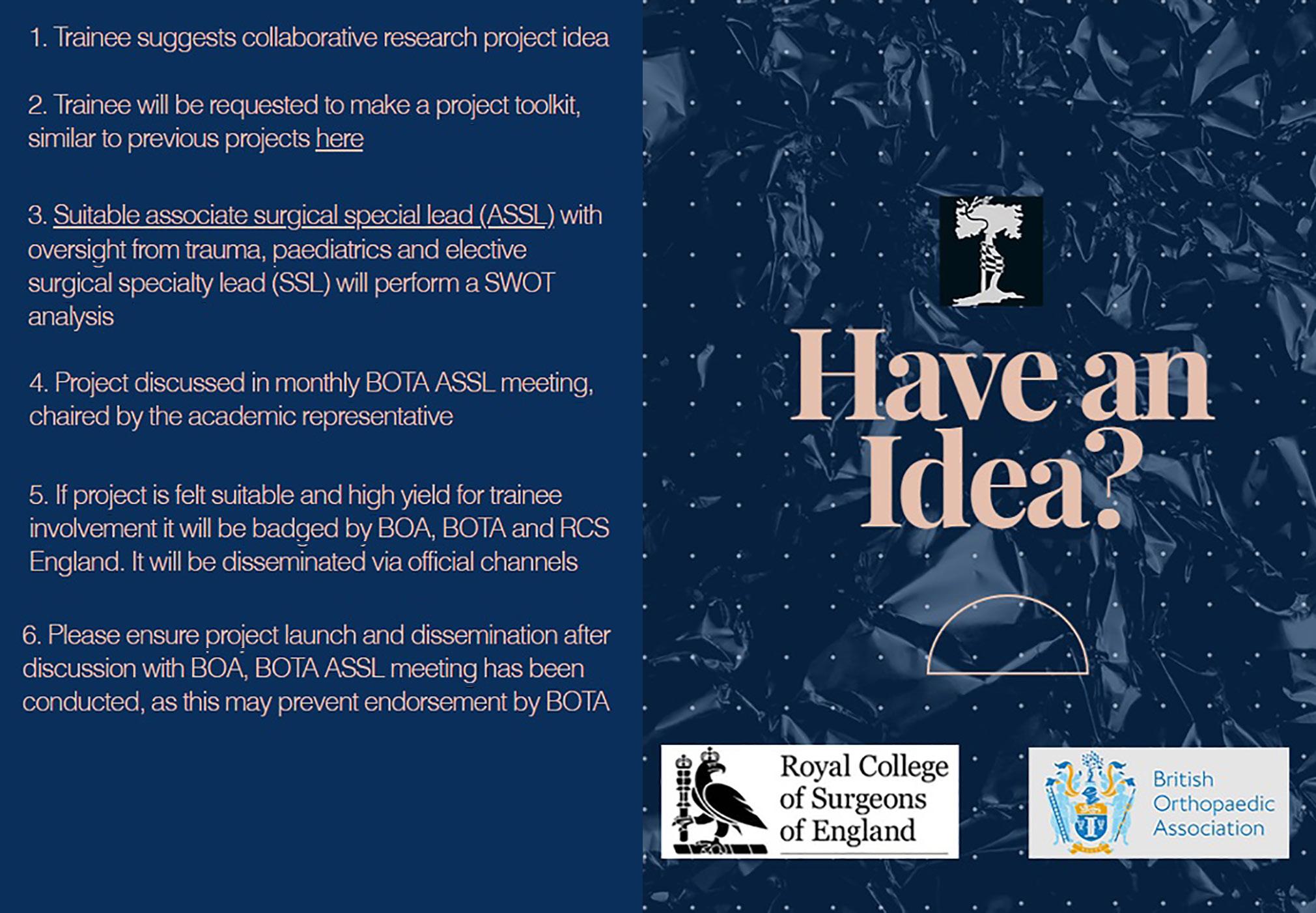
Trainee
42 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk
Figure 1: Decision Tree Process.
Zaid Hamoodi is an ST7 registrar in Mersey. He is the current joint RCSEng/ NJR research fellow at Wrightington, Wigan and Leigh NHS Foundation Trust, and an MD student at the Centre for Epidemiology Versus Arthritis at the University of Manchester.


the transparent Research Decision Tree in September 2021. The overall aim was to prevent research waste and help trainees to collaborate with clinical academics when developing a pertinent clinical question.
Sohail Nisar is an ST8 T&O Registrar in the Yorkshire and Humber Deanery. He is the lead for PPAK which is a cross-speciality collaboration with BOTA and RSTN. The study is in the data collection phase with international collaborators. Sohail is passionate about collaborative research and is the co-founder and chair of the Yorkshire Orthopaedic Research Collaborative.
To gain formal BOTA endorsement, project ideas (pitched by trainees), underwent rigorous assessment by the academic panel above (chaired by the BOTA academic representative). A comprehensive ‘toolkit’ was requested per project to reduce the cross-site burden on trainees to register the project locally. This included a comprehensive study protocol, service evaluation registration proforma, information sharing agreement, terms of engagement (including authorship) and support from a guarantor.
Two-way discussions then focused on 1) the impact of the clinical question; 2) efficient study design; 3) the inclusion of key stakeholder organisations and 4) the scope of future work (feasibility trial, grants). Once approved, the project ‘toolbox’ was then disseminated via BOTA’s official communication channels. Full toolkit available at https://www.bota.org.uk/ getinvolvedinresearch
Frank Acquaah is an ST5 Specialist Registrar training on the Percivall Pott rotation in the North, Central and East London Deanery. He sits on the executive committee of BOTA and the Percivall Pott Club as Secretary. He graduated from King’s College London School of Medicine. He plans to pursue a career centred around the hip and knee.

Successes through the Decision Tree
The expert advice provided by the BOTA/RCS England/BOA Decision Tree has proven to be an effective tool in supporting trainees in the development of successful projects focused on patient care improvements. In its first year, the scheme has already supported over 250 trainees to participate in eight impactful projects and RCS England has since commended this model as a ‘benchmark in promoting trainee-led research’. These studies include:
• The Open-Fracture Patient Evaluation Nationwide (OPEN) Study.
• The National Joint Registry Data Quality Audit of Elbow Arthroplasty (DQA-Elbows).
• The Prophylactic Peri-operative Antibiotics in K-Wire Fixation (PPAK) Study.
• The Prosthetic Hip Dislocations (PhD) Study.
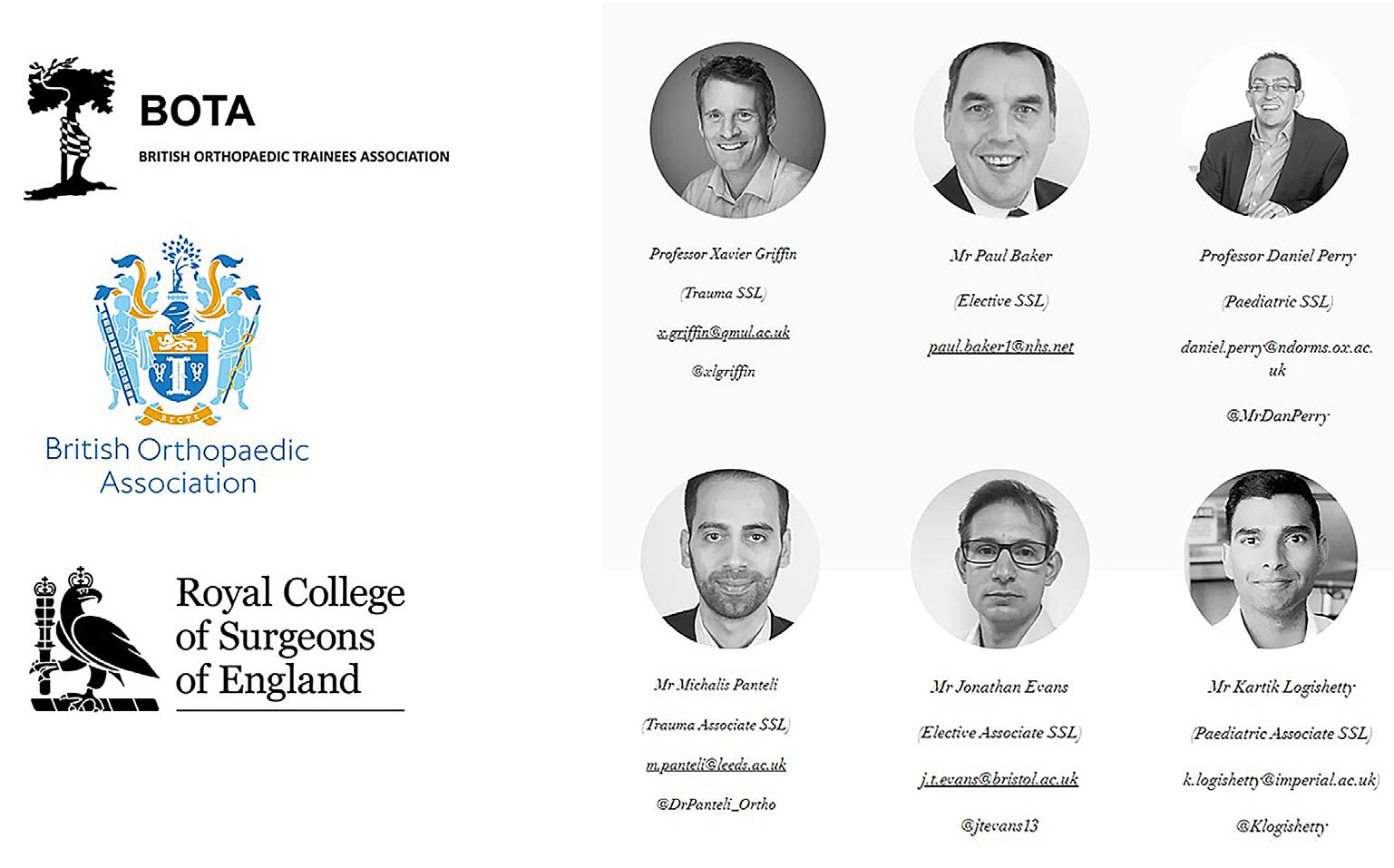
• The KNee Fracture Evaluation in oldEr people (KNEE) Study.
• The Fracture Ankle Implant Review (FAIR) Study.
• The Hip and Femoral Fracture Anticoagulation Surgical Timing Evaluation (HASTE) Study.
• PRosthetic Joint Infections in Shoulder & Elbow: A multicentre service evaluation (PRISE).
The OPEN and the DQA-Elbows studies are notable successes of this process. The OPEN study evaluated the management of open fractures in the UK by analysing 1,175 patients in 52 centres. This study was published in a peer-reviewed journal and presented at international conferences6
The DQA-Elbows was the first national collaborative audit between the NJR and BOTA. This audit assessed and improved the completeness and accuracy of the NJR elbow dataset. The provisional results of 3,157 patients in over 130 centres were presented at British Elbow and Shoulder Society (BESS), BOA, and the BOTA annual meetings, showing an improvement in the completeness of the NJR elbow dataset, from 61% to 85% and accuracy from 93% to 98%7
Trainee recruitment and dissemination strategies
BOTA’s social media platforms and the connection with the regional collaboratives (https://www.bota. org.uk/regional-collaboratives-1) were pivotal to engaging trainees who were then key in the success of these projects. All projects supported >>
Trainee
JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk | 43
Figure 2: Decision Tree Academic Panel. Full profiles of the SSLs and aSSLs- available at https://www.bota.org.uk/pitchanidea//.
by the Decision Tree benefited from official endorsement through BOTA’s social media platforms, newsletters, and a bespoke section on the website (https://www.bota.org.uk/research).
Endorsement consisted of visually attractive posters, which included concise explanations of the study in question, details of why the study was important and how viewers of these posts could be involved in data collection. The posters were typically created by the individual project teams. However, if needed, BOTA was happy to create posters with input from participating project teams. These posts were a powerful tool and had wide engagement for example, the average impressions (total tally of all the times the tweet was seen per post) of four Twitter posts on participating projects was over 1,800.
BOTA Congress Dragons’ Den Initiative

To tackle the well-recognised stumbling block of funding and to further support trainee-led projects, BOTA introduced the Dragons’ Den session at the 2022 Annual Congress in Liverpool. The session certainly lived up to its billing and was very well-attended, with trainees pitching their work to Professors Siobhan Creanor, Caroline Hing, Xavier Griffin and Dan Perry. Innovative presentations and some tough negotiating culminated in a total of £4,000 being awarded to the following trainees: Chris Bretherton, Sarah Abbott, Zaid Hamoodi, Sohail Nisar and Ignatius Liew. The pump-priming funding for new projects was made possible through generous contributions from the BOA/RCS England SSLs and AOUKI.
National Trainee Research Day
Finally, to highlight important research avenues and provide formal teaching, the Orthopaedic Research Collaborative East
Anglia (ORCA) ran its third Clinical Research Methodology Day. The free day, which also fulfilled an important CCT requirement, was a resounding success and was attended by 150 delegates from 12 countries. Speakers from internationally renowned institutions delivered excellent talks about their perspectives on research engagement. These included the National Institute for Health and Care Research (NIHR), National Joint Registry (NJR), Nuffield Department of Orthopaedics, Rheumatology and Musculoskeletal Sciences (NDORMS, Oxford), Barts Bone and Joint Health, and Endo-Klinik, Hamburg.
Trainees also participated in Q&A sessions regarding the NIHR Integrated Academic Training (IAT) pathway, Associate Principal Investigator (PI) scheme, research design service (RDS) and funding streams for higher degrees. The day’s catch-up content is available via MedAll at https://app.medall.org/ event-listings/clinical-research-day-2022by-orthopaedic-research-collaborative-eastanglia-orca
Key learning points
• The research impact of trainee-led collaborations within UK Trauma and Orthopaedics has grown from strength to strength, showcased by several recent impactful publications and presentations.
• The BOTA/RCS England/BOA Research Decision Tree has proven to be an effective tool in highlighting important clinical questions and facilitating multicentre trainee recruitment.
• BOTA continues to work with various stakeholders to ensure that delivered research is of high quality, focuses on patients and enhances the research experience of individual trainees. n
References
1. Gill JR, Lostis E, Bleibleh SS, Hennessy MS, Thondickal F, Gadd RJ, Grupping R, Chikate A, Khor S, Malani S, Nabulyato W. Weight-bearing in ankle fractures: An audit of UK practice. The Foot. 2019 Jun 1;39:28-36.
2. Barrie A, Kent B; Supra Man Collaborative. Supracondylar elbow fracture management (Supra Man) : a national trainee collaborative evaluation of practice. Bone Joint J. 2023;105-B(1):82-87.
3. Raza M, Walters S, Richardson C, Bretherton C, Longhurst K, Trompeter A. Weight-bearing in Trauma Surgery (WiTS) Study: A national survey of UK Trauma & Orthopaedic multidisciplinary health professionals. Injury. 2022;53(2):427-433.
4. Richardson C, Bretherton CP, Raza M, et al. The Fragility Fracture Postoperative Mobilisation multicentre audit : the reality of weightbearing practices following operations for lower limb fragility fractures. Bone Joint J. 2022;104B(8):972-979.
5. Hall AJ, Clement ND; IMPACT-Global Group, et al. IMPACT-Global Hip Fracture Audit: Nosocomial infection, risk prediction and prognostication, minimum reporting standards and global collaborative audit: Lessons from an international multicentre study of 7,090 patients conducted in 14 nations during the COVID-19 pandemic. Surgeon 2022;20(6):e429-e446.
6. Winstanley RJ, Hadfield JN, Walker R, Bretherton CP, Ashwood N, Allison K, Trompeter A, Eardley WG. The OpenFracture Patient Evaluation Nationwide (OPEN) study: the management of open fracture care in the UK. The Bone & Joint Journal. 2022 Sep 1;104(9):1073-80.
7. The National Joint Registry Data Quality Audit of Elbow Arthroplasty: NJR DQA-ELBOWS. BESS 2022 abstracts - Podium. Shoulder Elbow. 2022 Oct;14(2 Suppl):S11-S12. doi: 10.1177/17585732221124843. Epub 2022 Oct 19. PMID: 36275177; PMCID: PMC9583425.
Trainee
Figure 3: Example of a poster created by the project team of the ‘KNEE Study’.
44 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk
Figure 4: National Trainee Research Day.



nsksurgical @NSK_Surgical nsk.surgical Visit nsk-surgery.co.uk or call us on 0800 6341909 Primado2 Designed for efficient, controllable cutting action See the Quad Edge Bur in action FEEL THE DIFFERENCE
Clinical guidelines and the standard of care: Part 2
Simon Britten
Mr Britten is grateful for the assistance of Bob Handley and Chris Moran, who both gave up time to discuss the origins, formulation and ethos of BOAST guidelines.
Simon Britten is is a Consultant Trauma & Orthopaedic Surgeon in Leeds specialising in lower limb reconstruction. He is the President Elect of the British Limb Reconstruction Society and chair of the BOA Medico-legal Committee.

This article is based on the following book chapter: Clinical Guidelines in Trauma and Orthopaedic Surgery. Britten S, in Jo Samanta and Ash Samanta (eds). Clinical Guidelines and the Law of Medical Negligence: Multidisciplinary and International Perspectives (Edward Elgar Publishing, Cheltenham, UK & Northampton, MA, USA, October 2021). All excerpts reproduced with kind permission of the publisher.
In Part 1, I noted that many clinical negligence lawyers have seen some use of clinical guidelines in their cases to assist the court in determining what constitutes reasonable care1
I suggested that when considering the standard of treatment from both the clinical and medico-legal perspectives, the surgeon may wish to take into account the relevant clinical guidelines; consider any circumstances specific to the individual case which may influence treatment options; appreciate that rigid adherence to guidelines may occasionally be unwise and potentially negligent; and recognise that intentional deviation from existing guidelines may be reasonable if there are case-specific factors which warrant departure from the guidelines. That is to say, each individual case should be considered on its own merits.
Part 1 CORRIGENDUM
The fourth paragraph on the last page of Part 1 in the June edition of JTO should have read:
“This wide range of applications of BOAST guidelines, including in day to day clinical practice, as concise revision aids for trainee orthopaedic surgeons, and through to their use as reference tools in the national monitoring and audit of major injury, demonstrates their considerable usefulness and functionality.”
I began to discuss several sources of clinical guidelines of relevance to trauma and orthopaedic practice in the UK, and focused in detail on British Orthopaedic Association Standards in Trauma and Orthopaedics (BOAST) guidelines2, and the BOA/BAPRAS (British Association of Plastic, Aesthetic and Reconstructive Surgeons) clinical guidelines on the orthoplastic management of open fractures3.
I would now like to consider other useful sources of guidelines with which the orthopaedic surgeon should be familiar, both from the clinical and medico-legal perspectives.
Medico-legal
46 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk
National Institute for Health and Care Excellence (NICE)
In the case of Price v Cwm Taf University Health Board4 at trial and on appeal, the court chose to set aside guidance from NICE as to what constituted reasonable treatment, preferring instead to go with the evidence of the expert instructed by the Defendant, Mr Weale. The NICE guidelines for knee arthroscopy in osteoarthritis5 recommended arthroscopy and washout if a clear history of mechanical locking was given, while the Claimant argued that he merely had a sensation of catching within his knee.
Regarding departure from the relevant NICE guideline, at the original trial the judge accepted the expert evidence of Mr Weale, in finding that: “Overall, while [the surgeon] was not in the mainstream view in carrying out a further arthroscopy on the Claimant, bearing in mind the NICE Guidelines, he was within a reasonable body of orthopaedic surgeons who would reasonably have carried out such a procedure6.” At appeal, Birss J found that the original trial judge had been entitled to reach that conclusion, representing a direct application of Bolam test.
At the original trial, there had been consideration of the difference between a clear history of mechanical locking of the knee versus the described symptom of catching within the

knee. As the original trial judge had held that [the surgeon] had been wrong to equate the knee symptom of catching with that of true locking, the claimant’s counsel submitted that essentially [the surgeon] carried out the second arthroscopy as a treatment of osteoarthritis contrary to the relevant NICE guidelines. In considering this point, Birss J noted: “… as the [original trial] judge recognised … the Guidelines also make clear that while they have been arrived at after careful consideration, they do not override the individual responsibility of healthcare professionals to make decisions
on to state the view of NICE itself: “Your responsibility ... This guidance represents the view of NICE, arrived at after careful consideration of the evidence available. When exercising their judgement, healthcare professionals are expected to take this guidance fully into account… The guidance does not override the individual responsibility of healthcare professionals to make decisions appropriate to the circumstances of the individual patient, in consultation with the patient and/or guardian or carer.” Hill concludes by observing that Birss J and NICE are in agreement, noting that all cases are fact-sensitive, so that in some cases clinical guidelines should be observed and/or communicated, while in others not.
Rockwood and Green
Rockwood and Green’s Fractures in Adults9 is a widely accepted and respected text, the scope of which covers the entirety of fracture treatment of the upper and lower limbs, pelvis and spine. While not primarily a source for clinical guidelines per se, each chapter is written by a recognised international expert and includes a review of the relevant peer reviewed literature written on specific injuries. It is useful to treating clinicians and can also add significant weight to an orthopaedic expert’s evidence on the standard of care provided in clinical negligence cases, augmenting the expert’s own clinical experience.
From the author’s own medico-legal experience is another instructional clinical negligence case which demonstrates the use of the relevant chapter in Rockwood and Green’s to back up the expert evidence provided.
appropriate to the circumstances of the original patient. After noting that they do not override the need for appropriate individual decisions, the judge then made the statement which is challenged on appeal: ‘nor is failing to follow the guidelines prima facie evidence of negligence7’.”
In his blog, barrister Mike Hill of Parklane Plowden Chambers ran through a summary of Price, noting that inconsistencies between care given and NICE guidelines are often pleaded as evidence of a breach of duty or vitiation of the consent process, and pointing out that invariably the matter is defended by arguing that they are guidelines only8. Hill went
A ‘reverse oblique’ unstable subtrochanteric femur fracture in a 68-year-old man was fixed using a ‘sliding’ or dynamic hip screw (DHS), rather than with the biomechanically more stable intramedullary nail (IMN). Soon after surgery, the DHS fixation failed and the fracture site collapsed, leading to a symptomatic nonunion of the proximal femur with marked limb shortening and disability. Revision surgery was precluded by the development of an unrelated abdominal problem.
The author was instructed by the Claimant’s solicitors and took the view that it had been unreasonable to use a DHS in this case. This was on the basis that the biomechanics of the DHS are known to be disadvantageous >>
Medico-legal
JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk | 47
“GIRFT (Getting It Right First Time) emphasises the interrelationship between failure to follow clinical guidelines and the potential for litigation as a result.”
to the sound fixation of reverse oblique subtrochanteric fractures and the medical literature does not support the use of a DHS in such fractures; indeed, the literature actively warns against using a DHS in fractures with such geometry – the relevant edition of Rockwood which was in print at the time surgery had been performed stated: “Reverse Obliquity Fractures. A sliding hip screw is not indicated for stabilisation of reverse obliquity fracture patterns … telescoping of the implant can promote fracture separation rather than impaction. This leads to an unacceptably high failure rate when a conventional sliding hip screw is used to treat this fracture pattern. Reverse obliquity intertrochanteric fractures are best stabilised with a cephalomedullary nail10.”
The expert instructed by the Defendant stated that at the time the surgery was performed, in his experience a responsible body of orthopaedic surgeons would have used a DHS to fix such a fracture as a reasonable fixation option. The case settled in the Claimant’s favour before trial for a six-figure sum without admission of liability. There were no obvious case-specific factors to justify using the biomechanically inferior implant contrary to guidance in Rockwood. This case illustrates the potential strength of one’s clinical experience being backed up by a standard text such as Rockwood and Green when acting as an expert witness, provided that the edition quoted is contemporaneous with the case being considered. It also illustrates the importance of not disposing of old editions of standard textbooks, as they may come in handy when casting an eye over retrospective potential negligence cases.
Getting It Right First Time
GIRFT emphasises the interrelationship between failure to follow clinical guidelines and the potential for litigation as a result.
An NHS Resolution and GIRFT working party has produced professional standards guidance for hip and knee arthroplasty documentation11 These clinical guidelines have been produced in collaboration with contributors from the British Hip Society and British Association for Surgery of the Knee, the British Orthopaedic Association, NHS Patient Safety, NHS panel law firms, Claimant law firms, expert witnesses and the medical defence organisations. The documents were produced following analysis of medical negligence cases notified to NHS Resolution by leading orthopaedic medicolegal experts and viewed in light of existing clinical guidelines. GIRFT states the aim of the guidance is as follows: “… to promote good clinical practice based on lessons learnt from previous claims and to ensure that practice is clearly documented so that in the event that a claim was brought against good
clinical practice, there would be sufficient documentation for the NHS to defend it in an efficient and cost-effective manner. In the future other high-volume areas for claims will be reviewed based on the feedback from this guidance12.” The two documents provide detailed guidance as to the extensive operation note required to safely document a total hip or knee arthroplasty in such a way as to minimise the risks of action for clinical negligence.
The two GIRFT clinical guidelines in hip and knee arthroplasty documentation were published in 2019. As yet, there is no reference to them apparent in published case law. On the one hand, the full guidelines provide the orthopaedic surgeon with a cornucopia of opportunities to document the excellence of their arthroplasty practice, but it remains to be seen whether the gold standard level of detail required will prove to be difficult to attain in its entirety and then leave the reasonable surgeon open to censure and on the receiving end of a successful claim for clinical negligence.
Clinical guidelines in the COVID-19 era
From spring 2020 with the worldwide COVID-19 pandemic approaching the United Kingdom, novel clinical guidelines emerged covering two separate areas of potential relevance to orthopaedic surgeons’ jeopardy and clinical negligence.
Guidelines were developed to advise orthopaedic surgeons on how to treat respiratory patients outwith their usual area of expertise, including guidance on oxygen therapy for patients with COVID-19 and escalation of respiratory support for such patients. No examples of orthopaedic surgeons acting as medical registrars during COVID-19 times have yet made it into medical negligence case law. This could be due to the delays to court proceedings introduced by lockdown during the pandemic, the expected time lag from initiating a clinical negligence claim to its conclusion, or alternatively a factor of the innate ability of orthopaedic surgeons to improvise and turn their hand successfully to most things!
An additional genre of guidelines were devised in how to treat a wide range of acute limb injuries non-operatively, without the need for the services of an anaesthetist, bearing in mind that prior to the pandemic many common injuries were treated operatively in order to restore normal anatomy and maximise functional outcomes for injured patients. The BOA produced a set of COVID-19 BOASTs, in anticipation of loss of anaesthetic capacity, the need to protect patients from exposure to disease (including in hospitals with COVID-19 inpatients) and the need to protect the NHS from unnecessary hospital admissions13
It remains to be seen how much litigation will follow, covering such matters as inadequate follow up and rehabilitation, failure to provide the indicated operative treatment leading to poorer outcome, and even ‘unnecessary and avoidable’ early amputation in a potentially salvageable limb. All this will have to be weighed against the very real danger during 2020 of simply being an in-patient in a hospital with many COVID-19-positive patients and the risk of nosocomial hospital-acquired transmission.
Conclusion
In recent years, a burgeoning list of sources for clinical guidelines has emerged covering a range of traumatic and elective conditions in orthopaedic surgery, with NICE and the BOA leading the way. Orthopaedic surgeons need to have a working knowledge of the guidelines relevant to their area of practice to aid sound decision making in their clinical work. If they choose also to engage in medicolegal practice, such working knowledge of the relevant guidelines is even more essential, in conjunction with their clinical experience, to help fashion their expert opinion.
It has to be appreciated by both the orthopaedic expert and the lawyers that there may be some ambiguity as to whether a specific guideline represents the gold standard of care (desirable), the reasonable standard (essential), or the auditable standard (quantifiable). In the author’s experience, orthopaedic experts may occasionally lose sight of the fact that to avoid care provided being deemed negligent, the care provided merely has to be reasonable.
However, guidelines are exactly that – guidelines. The view of NICE is clear, that when making clinical decisions the healthcare professional must take fully into account any available clinical guidelines; but they must also appreciate that all cases are fact-sensitive, and care provided must take into consideration the patient’s individual circumstances of relevance. Accepting that there will be cases in which there are specific individual factors to consider carefully, rigid adherence to clinical guidelines may not protect the orthopaedic surgeon from censure, while intentional deviation from clinical guidelines may be considered entirely reasonable. Depending on the specific circumstances, in some cases guidelines should be observed, while in others not. If the care provided deviates significantly from current clinical guidelines, then both the deviation and the reasoning for the deviation should be communicated with the patient whenever possible. n
References
References can be found online at www.boa.ac.uk/publications/JTO
Medico-legal
48 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk


Stephen Bendall qualified from Charing Cross Hospital and trained on the Charing Cross and the St George’s Orthopaedic Training Programme. He was appointed as consultant at the Princess Royal Hospital in 1997, which has now part of University Hospitals Sussex. He has been involved in training being TPD, in research and was BOFAS President in 2014. He is currently Clinical Director locally and sustainability within T&O is a key issue for the Trust and department.
Let’s talk about sustainability
What does this actually mean? And how realistic is it in practice?
Stephen Bendall and Gareth Chan
Gareth Chan qualified from The Royal Free and UCL in 2014 and is currently an ST7 on the HEKSS Orthopaedic Training Programme. He has an interest in both teaching and research, and is an Honorary Clinical lecturer at Brighton & Sussex Medical School. He has a strong interest is T&O and sustainability, and a track record of publications around this topic.
‘S
ustainability’ is the phrase of our times. In simple terms it means the ability to maintain a process continuously over time and we apply it regularly to our workforce, our training, financially, socially, as well as in regard to global environmental sustainability. It’s on this latter interpretation that we would like to develop in these series of articles.
NHS England published Delivering a Net Zero National Health Service in July last year. It states that the NHS overall accounts for 4% of England’s total carbon footprint, of which orthopaedics is said to account for up to 20%. So there is an onus for us as Trauma & Orthopaedic surgeons to sit up and take note.
The goal of achieving in the NHS a ‘net zero’ NHS by 2040 seems daunting, as it appears to be a complex task with some areas we have remote access to influence as a group of clinicians.

We should approach this as we would any problem we encounter in our clinical practice,
by understanding the problems focusing on what we can change and then monitor the impact of our interventions and allow that to shape future developments accordingly.
So, in coming to the first point about understanding the problem, we need to explore what the conventions and current terminologies are.
When talking about climate change, we tend to focus upon carbon dioxide emissions, but this isn’t the only greenhouse gas involved, which include methane, nitrous oxide, hydrofluorocarbons, perfluorocarbons plus numerous others.
These different gases each have a different range of warming effects – one tonne of methane does not have the same heat absorption impact as one tonne of CO2. So, it has come about that there is an individual warming metric for each of these gases called the global warming potential or GWP. This indicates
Subspecialty
“NHS England published Delivering a Net Zero National Health Service in July last year. It states that the NHS overall accounts for 4% of England’s total carbon footprint, of which orthopaedics is said to account for up to 20%.
50 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk
So there is an onus for us as Trauma & Orthopaedic surgeons to sit up and take note.”
the amount of warming a gas causes over time (by convention a 100 years) and is based upon each gas’s warming effect, and how long it remains in the atmosphere.
In order to make comparisons between the effect of the various greenhouse gases easier, eCO2 (CO2 equivalent) has been adopted to compare gases by converting their effect to the equivalent amount of CO2. Carbon dioxide equivalents are often expressed as million metric tons of carbon dioxide equivalents (MMTCDE), although one can also see it expressed in kilograms too.
CO2 is given a GWP index of 1. Methane causes 25 times more warming than CO2, so 1kg of methane causes 25 times more warming over a hundred years compared to 1kg of CO2. So, using eCO2 as a metric allows us to gather a fuller understanding of the impact of the various emissions.
Thus far, there appears to be no clear direction as to whether we use CO 2 or
eCO 2 as a metric. The aforementioned NHS report is vague on this, but it would seem logical to use eCO 2 in T&O pathways, particularly if we want to pick up on the effect of anaesthetic gases. As an example, Desflurane has an eCO2 of 2,500 and for that reason is banned in Scotland, and to be phased out in England by NHSE by 2024.
or sequester CO 2 – for instance planting trees – which could mean that they have only offset their emissions and not reduced them. Net zero means cutting emissions to as low as possible, which is clearly a different thing, and ‘greenwashing’ is the term applied when you’re duped into believing a company is net zero when it’s actually climate neutral or is making other false claims.
It’s also important to understand the meaning of the terms ‘carbon footprint’, ‘climate neutral’ and ‘net zero’. The carbon footprint is the net impact of a process or company in terms of its CO 2 emissions.
Climate neutral includes any carbon offsetting a company does. Offsetting is where a company funds projects that lower
In coming to what we can change, there will be areas for instance with NHS supply chains and real estate that may be more difficult to realise, but digital solutions to allow remote patient consultations may have a place by reducing patient travel. Remote consultations exploded during the COVID-19 pandemic and we should carry forward the lessons we learnt during this episode of the benefits and disbenefits of this. This leads into the likely impact of machine-based learning (AI) on our practice, which is already making inroads into orthopaedic practice. >>

Subspecialty
JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk | 51
“In coming to what we can change, there will be areas for instance with NHS supply chains and real estate that may be more difficult to realise, but digital solutions to allow remote patient consultations may have a place by reducing patient travel.”
Subspecialty
We also have to look at areas that have become embedded in our day-to-day practice and understand the carbon impact of what we do. Rizan et al. ( J RSM March 2023) gave an insight to cumulative carbon footprints for various surgical procedures, which uniquely encompasses all the products, including disposables used. The top carbon producing procedure was TKR at 85.5kg eCO 2 , noting that 54% of the total carbon footprint of the products used related to the use of single use items. There is also additional significant energy usage from the use of laminar flow too, which accounts for a significant proportion of ‘HVAC’ (heating, ventilation and air conditioning) related emissions.
The BOA, and Brighton and Sussex Medical School recently undertook a survey of orthopaedic surgeons of all grades, aiming to assess the current appetite for a shift towards sustainable surgery, perceived barriers to change and where in their practice change would be most welcomed. The survey was run from March 2023 onwards and remains open for responses.
A total of 132 responses were recorded, with 70.5% being received from Consultant/ Associate Specialist grade surgeons and the remainder from Registrar grade and below. The response rate to the survey represents an approximate return rate of 0.03%, given the BOA’s circa 5,000-strong membership to which the survey was distributed.
There was a near unanimous response (98%) in ‘agreeing’ or ‘strongly agreeing’ that there is
1. I have made significant changes in my personal or professional life to reduce my carbon footprint and/ or other environmental harm.
2. At my place of work I feel I have the knowledge, skills and support to make changes to improve environmental sustainability.
3. There is a need to reduce the environmental impact of Orthopaedic Surgery.
4. I am concerned about the volume of single-use items in Orthopaedic Surgery.
5. I would be happy to operate on a patient using a spinal or regional block alone, whenever clinically appropriate and possible.
6. For any soft tissue and/or arthroplasty operation, I would be happy to use reusable gowns in place of single-use gowns.
7. For any soft tissue and/or arthroplasty operation, I would be happy to use reusable drapes in place of single-use drapes.
8. For any soft tissue and/or arthroplasty operation, I would be happy to use reusable surgical hoods in place of single-use hoods.
9. For any soft tissue and/or arthroplasty operation, I would be happy to operate in a room without laminar flow.
10. In comparison to single-use items, which of the following do you believe to be barriers to adoption of reusable equipment in orthopaedic surgery.
a need to reduce the environmental impact of surgery, 90% of respondents ‘agreed’ or ‘strongly agreed’ that single use items were an issue in orthopaedic surgery. Despite that, only a quarter of respondents stated they would be happy to use reusable drapes and/or gowns for arthroplasty and/or soft tissue procedures.

Regarding laminar flow usage, only 11% would be willing to perform arthroplasty and/ or soft tissue procedures in a non-laminar flow theatre.
So despite there being a clear appetite for a change in practice to support a more sustainable future, the pathway to achieve this appears to be littered with hurdles, with the main one being the lack of a coherent national directive to challenge the status quo and drive changes in practice.
We believe the BOA is ideally placed to play a major role in this by embedding eco-sustainability into UK orthopaedics. This will need support at Council level and could include inserting sustainability in the GMC T&O syllabus and in the FRCS(Orth) examination. It is already supporting research and innovation in this area and should also provide guidance on managing changes in practice driven by the best evidence available.
We’ll start the discussion by challenging the use of laminar flow and paper drapes, and we will discuss these topics in the two articles that follow. n
Table 1: Questions asked on the survey of Orthopaedic Surgeon attitudes to sustainability. Questions 1 to 9 graded on a six-point Likert Scale from Strong Agreement through to Strong Disagreement.
52 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk
Discover the power of collaboration in orthopaedics with the National Orthopaedic Alliance



become an NOA member organisation and unlock a world of possibilities is your organisation not yet a member of the NOA? Attend our webinars or receive our newsletter? it’s time to take the next step!
Consider joining the NOA and gain exclusive access to our extensive network of orthopaedic providers. We are currently offering a free trial period for new organisations that sign up for NOA membership. Interested? Drop us a line on info.noa@nhs.net.
Find out more about the NOA by scanning the Qr code


registration open for the NOA Annual members’ Conference 2023 work for an NOA member organisation and not yet registered to attend this year’s NOA Annual members’ Conference taking place in birmingham on 19 October 2023?



Don’t miss this engaging event designed to foster learning, networking, and collaboration within the orthopaedic community.
For more information and to register, scan the Qr code
www.nationalorthopaedicalliance.co.uk | @NOAOrthopaedics | info.noa@nhs.net
ExplOrE Opp Ortu NitiE s AvA il A blE tO bOth mEmb Er AND NON -mEmb Er Org ANisAti ON s b ElOw
Blowing against the wind: the case for shifting the current paradigm on theatre ventilation
Benedict Rogers
Operating theatre ventilation systems play a role in preventing contamination, but also regulating environmental temperature and humidity.
Deep infection after total joint replacement is a devastating complication. The incidence of recurrent infection is low, but remains a significant complication which may require several procedures at considerable expense1
Professor Benedict Rogers graduated from Oxford and was an orthopaedic trainee on the SW Thames Orthopaedic Training programme. His interest is arthroplasty, sports injuries and trauma. He was appointed to University Hospitals Sussex as a consultant having done Fellowships at Mount Sinai and Sunnybrook. He currently holds the Chair in Orthopaedics at Brighton and Sussex Medical School and is Editor of the Annals of the Royal College of Surgeons of England.

The importance of the operating theatre ventilation system in reducing surgical site infections (SSIs) has been discussed for numerous years. There are two main ventilation systems:
• Turbulent mixed airflow –also called plenum flow.
• Laminar airflow.
The questions that arise are:
• What is the carbon footprint of these systems?
• Do we need to challenge our current paradigm that all T&O surgery is done in an ultraclean setting?
• Can we reduce the carbon footprint of ventilation systems?
Carbon footprint
Laminar flow relies on the use of ventilator systems that use fans to generate a positive air pressure in the roof of the theatre. The fans are connected to high efficiency particulate air (HEPA) filters to remove bacteria and other debris.
To attain laminar flow, there must be a continuous flow of highly filtered ultraclean air (UCA) of <10 colony-forming units per metre cubed (CFU/m3) of bacteria. Once the contaminants are removed, the air is returned to theatre, creating up-to 300 air changes per hour.
The Medical Research Council trial confirmed the value of laminar-flow theatres in the reduction of CFUs3. Plenum ventilation systems rely on filtered but turbulent air currents, which are forced via positive pressure into the theatre suite. These systems create fewer air changes; between 15 and 35 times an hour.
From the point of air changes per hour, laminar flow requires more energy than plenum flow, but there is little in the literature to quantify this.
Shifting the paradigm
Many cite the study by Lidwell et al., using a cohort of over 8,000 patients across the UK and Sweden in a randomised control trial setting4. They followed up all patients undergoing a total hip and knee replacement for between 2-3 years for any evidence of peri-prosthetic joint infection (PJI). A statistically significant reduction in PJI in the laminar flow group (0.6% v 1.5%) was reported, particularly where laminar flow was used as an adjunct to other means of asepsis such as occlusive clothing and exhaust suits. However, this study has been widely criticised for lack of controls of the variables and uncontrolled use of peri-operative prophylactic antibiotics.
It has now become unclear whether laminar flow systems that reduce the overall numbers of potentially contaminating particles within the operative field, translates to a significant effect on the rates of peri-prosthetic joint infection (PJI)5-7. To date, there have been no studies which have shown conclusively that fewer colony-forming units relates to a lower rate of wound contamination and infection. The evidence for the use of laminar flow in reducing infection rates in lower limb arthroplasty is now questioned8-10
Subspecialty
54 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk
Three studies, with increasing evidential value, demonstrate the changing evidence that doubt the benefit of laminar flow in reducing surgical site infection.
1. A simple observational study utilising a new hospital with an old hospital by Van Griethuysen et al. demonstrated that the addition of laminar flow in a new theatre suite resulted in no significant reduction of deep PJI per se11. Similar protocols were followed, after the introduction of laminar flow and while the air quality was improved, this did not correlate with any demonstrable reduction in PJI.

2. A study of 63 surgical departments in Germany evaluated whether laminar flow impacts on surgical site infection for both orthopaedic and abdominal surgery12. Compared to normal (‘turbulent’) ventilation, the risk for severe SSI after hip prosthesis implantation was significantly higher using laminar airflow (1.63 < 1.06; 2.52>). This study, which controlled for many patient and hospital-based confounders, demonstrated that laminar airflow showed no benefit and was even associated with a significantly higher risk for severe SSI after hip prosthesis.
3. The 10-year results of the New Zealand Joint registry investigated the use of laminar flow ventilation in reducing the rate of revision for early deep infection after hip and knee replacement13. A large retrospective study of 83,311 TKR and THR cases the results mirror the study by Brandt et al 12. The rates of revision for PJI were statistically significantly higher in laminar flow theatres (0.148%) versus conventional ventilation theatres (0.061%), with similar results in TKR (0.243% v 0.098%).
In 2017, the effect of laminar flow ventilation on surgical site infection was analysed in a systematic review and meta-analysis14, which includes both the studies from Germany and New Zealand described above. In total, 12 observational studies compared laminar airflow ventilation with turbulent ventilation in orthopaedic, abdominal and vascular surgery were included in systematic review. Eight cohort studies form the basis of the meta-analysis for hip replacements and six studies for knee replacements (see tables 1 and 2).
The outcome of this metaanalysis demonstrate that laminar airflow ventilation does not reduce the risk of deep surgical site infection after hip and knee replacements compared to plenum ventilation, which we need to note.
Actions to reduce the carbon footprint of ventilation systems
These we can divide into short or immediateterm actions and longer-term options.
In the short term, turning the ventilation system off when not in use would seem simple, safe and cost effective and has been put forward23,24
In the longer term, adopting energy capture systems, for instance heat exchangers,26 could be worthwhile and can be retrofitted to existing systems. There are also newer technologies, for example, using temperature-controlled airflow – a variant of laminar flow. This uses a cooled HEPA filtered area above the operating area which, being denser, flows downwards, but uses less energy than laminar flow25
Summary
We need a strategy led by the BOA that looks forward to include revaluating our 40-yearold values around the use of laminar flow and the type of surgery done in these theatres.
There are some easy ‘wins’ to be made with switching laminar flow systems off when not in use, as well as newer technologies that we should be evaluating and promoting. n
References
References can be found online at www.boa.ac.uk/publications/JTO
Subspecialty
Date Study size (n=) Odd ratio Kakwani et al 15 2007 435 0.05 Brandt et al 12 2008 28,623 1.53 Dale et al 16 2009 93,958 1.32 Pedersen et al 17 2010 80,756 0.74 Breier et al 18 2011 41,212 1.84 Hooper et al 13 2011 51,485 2.42 Namba et al 19 2012 30,491 1.10 Song et al 20 2012 3,186 1.2 Total 330,146 1.29
Date Study size (n=) Odd ratio Miner et al 21 2007 8,288 1.57 Brandt et al 12 2008 9,396 1.42 Breier et al 18 2011 20,554 1.09 Hooper et al 13 2011 36,826 1.92 Song et al 20 2012 3,088 0.51 Namba et al 22 2013 56,216 0.83 Total 134,368 1.29
Table 1: Published cohort studies comparing risk of deep surgical site infection after total hip arthroplasty for laminar airflow v conventional ventilation.
Table 2: Published cohort studies comparing risk of deep surgical site infection after total knee arthroplasty for laminar airflow vs conventional ventilation.
“To attain laminar flow there must be a continuous flow of highly filtered ultraclean air (UCA) of <10 colonyforming units per metre cubed (CFU/m3) of bacteria. Once the contaminants are removed, the air is returned to theatre, creating up-to 300 air changes per hour.”
JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk | 55
Figure 1: Laminar airflow ventilation in action.
Hussameldin M Nour graduated from the University of Khartoum in Sudan. He completed core surgical rotations in general surgery, trauma and orthopaedics in Royal Sussex County Hospital, Brighton, and is now an ST3 in general surgery working in the North West.

Reusable surgical gowns and drapes. Should we be adopting them?
Surgical site infection (SSI) is a major complication in orthopaedic surgery, as introducing micro-organisms into the operating field can lead to periprosthetic infections (PPI), which can have a devastating outcome for patients as well as wider healthcare systems1
Safeer Javid is a dedicated medical professional who graduated from Muhammad Medical College, Mirpurkhas, Pakistan in 2016. In 2021, he joined the NHS, and currently is serving as a clinical fellow specialising in trauma and orthopaedics. His passion for this field has led him to set his sights on obtaining a training number in trauma and orthopaedics, with the goal of achieving this milestone in 2024. He is committed to providing high-quality healthcare and making a positive impact in the lives of patients in need of orthopaedic care.

Gowns and drapes are universally used to reduce the risk of SSIs, as well as protecting healthcare providers as part of maintaining the sterile surgical field2
Single use or reuseable?
Gowns and drapes can be either single use or reusable. There is an acceptance that reusable drapes could be better for the environment, yet there are concerns regarding increased surgical site infection, as well as user comfort and safety3
Early reusable surgical gowns were made from woven cotton fabrics, which are not resistant to liquid penetration5 and failed to protect the wearer, as well as the patient from microbial transmission.
Single-use gowns and drapes were therefore introduced and this led to a parallel introduction of single use equipment.
The latter gained popularity in the 1990s after the discovery of variant Creutzfeld-Jakob Disease (vCJD) for infection control purposes, when sterilisation techniques at that time were not as efficient as they are now4
More recently, these older woven cotton fabrics have been replaced by cotton/polyester (PET) blended fabrics and full PET fabrics5
However, despite the almost universal use of disposable gowns in T&O, there is no data to suggest that disposable gowns and drapes are superior to reusable ones in reducing SSI6,7
There is some work looking at physical properties. The Association for the Advancement of Medical Instrumentation (AAMI) defines four levels of protection for all types of gowns which are:
• Level 1: Minimal level of fluid barrier protection.
• Level 2: Low level of fluid barrier protection.
• Level 3: Moderate level of fluid barrier protection.
• Level 4: Highest level of fluid and viral barrier protection8
McQuerry 9 studied single-use gowns using the American Association of Textile Chemists and Colourists test method. This study suggested that level I and II disposable gowns did not satisfy AAMI standards for impact penetration water resistance.
All levels of disposable gowns did not fulfil the American Society for Testing and Materials performance prerequisites for breaking strength in the crosswise direction, but reusable gowns had superior protection in comparison to disposable gowns.
There are currently no studies comparing disposable gowns and drapes in surgery, which requires a high level of protection such as arthroplasty.
The aforementioned study would suggest that although reusable gowns have superior physical properties than disposable gowns and drapes, that does not mean that there is protection from developing infection and SSI.
Subspecialty
Hussameldin M Nour, Safeer Javid, Rhodri Gwyn and Riem Johnson
56 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk
Riem Johnson qualified from Leicester and undertook basic surgical training on the NE England Training Programme. She did her MD at the University of Newcastle and completed her CCT. Her subspecialty interest is Hand Surgery and did her fellowship at the Chelsea and Westminster Hospital, as well as working as a locum consultant at the Pulvertaft Unit in Derby. She was subsequently appointed as consultant at University Hospitals Sussex working in the UHS Hand Unit. She is the current sustainability lead in the department.

Ecological impact
The biggest issue threatening human health and health care systems in the world is the climate crisis14, yet our health systems are contributing to this crisis.
Healthcare contributes to 4.4% of the global greenhouse gas emissions10. In the UK, the National Health Service (NHS) produces 22.8 million tons of carbon dioxide (CO2) per year11 and 10% of the NHS carbon footprint in England is caused by medical equipment12
Rizan13 reported that operating theatres are 3-6 times more energy-intensive than the rest of the hospital and are a major contributor of waste with an estimate footprint of 6-814kg carbon dioxide equivalents per a single operation.
A study done in Canada, the United States and the United Kingdom estimated that emission contributions from the annual operation of surgical suites were found to range from 3,200,000 to 5,200,000 kg of carbon dioxide equivalent, which is equivalent to the annual carbon footprint of 2 million passenger vehicles15,16
Single-use items account for a large proportion of the carbon footprint of procedures. In carpal tunnel decompression for example, drapes account for 32% and single-use PPE for 23% of the overall carbon footprint17 It has been shown that selecting reusable gowns, rather than single use items, reduces natural resource energy consumption by 64%, greenhouse gas emissions by 66%, blue water consumption, defined as any water that is removed from and not returned to the water supply, by 83% and solid waste generation by 84%.
Recent studies have shown that 1,000 grams of disposable surgical gowns consumes 26,286 megajoules (MJ) of natural resource energy, in comparison to only 2,366 MJ in reusable gowns. Moreover, 1,000 grams of reusable gowns releases 557kg of CO2 equivalent in comparison to 1,636kg with single-use gowns. The figures above were calculated in relation to gown manufacturing and supply chain, packaging manufacturing, sterilisation, phase transport and end of life18
Financial cost
Health systems consume a huge share of a country’s budget. In the UK, it is estimated that £153 billion was spent on the NHS in 2022/2319. In the USA, 4.2 trillion US dollars
was spent on healthcare in 202120. Health care demand is expected to increase over time. By 2030, the global demand for primary total hip arthroplasties is estimated to expected grow by 174% to 572,000. Likewise, the global demand for primary total knee arthroplasties is projected to grow by 673% to 3.48 million procedures21 and this will cause a further financial burden to health systems.
Surgical equipment and gowns play a role in this financial impact, and there is a debate about the cost effectiveness of reusable gowns and drapes versus disposable ones.
Baykasoglu et al’s study22 showed that the cost of reusable gowns was approximately 25% of the cost of disposable gown costs.
Wedmore et al23 suggested that reusable clothing and draperies may result in cost savings through requiring less waste output and landfill use. The initial investment barrier being addressed by implementing costeffective methods of laundering.
Conclusion
Therefore, reusable gowns and drapes have a smaller carbon footprint. As well as being cheaper, they should tick the sustainability boxes not only on the environmental, but also on the financial front.
In returning to the question posed in the title, the answer is yes. We believe that more sustainable and environment friendly solutions such as reusable textiles should be adopted for these reasons.
How that is brought about will require leadership by the BOA and other stakeholders as well as grass roots commitment. We as a group have access to NHS data, along with the orthopaedic registries and most recently the Medical Outcome Devices Registry. If we were to record what type of gowns and drapes were used in the insertion of an implant, we would then be able to allay our concerns about SSI and reusable drapes. This could be supported by BOA-led guidelines on the adoption of reusable materials for gowns and drapes. n

References
References can be found online at www.boa.ac.uk/publications/JTO
Subspecialty
Rhodri Gwyn is a Post CCT fellow in Hand Surgery. University Hospitals Sussex NHS Foundation Trust. Trained in Wales.
JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk | 57
“Reusable gowns and drapes have a smaller carbon footprint. As well as being cheaper, they should tick the sustainability boxes not only on the environmental, but also on the financial front.”
Rolfe Birch
18th February 1944 – 22nd May 2023
Obituary by Michael Stewart
Professor Rolfe Birch was one of the most remarkable surgeons and clinical scientists of his generation, who determined the modern principles of surgical treatment of Brachial Plexus and complex peripheral nerve injury, and by whose outstanding leadership in a unique specialty established two world-class Peripheral Nerve Injury Units – one Civilian and one Military.
‘RB’ was born in London, and educated at Cambridge University and St George’s Hospital. He developed an interest in nerves at Cambridge studying for the Natural Sciences Tripos. In 1979, he was appointed Consultant in Neurological Orthopaedics to St Mary’s Hospital, Paddington and to the Royal National Orthopaedic Hospital, Stanmore.
At St Mary’s, he joined George Bonney, a pioneer of Surgery of the Brachial Plexus. In 1991, the Unit at St Mary’s was transferred to Stanmore where RB established an outstanding multidisciplinary team in research, based on clinical and investigative assessment of Brachial Plexus Injury. He advocated among other things a new policy of urgent surgical exploration in blunt trauma, where clinical evidence pointed to major disruption of the plexus and he established that surgical reinnervation of the limb relieved pain. His relationship with his patients demonstrated the depth of his dedication and his capability to inspire confidence. He said of them, “One of the great joys is to work with these young men and women. Many of them live on the edge, they are risk takers, they take chances, which is perhaps one reason I get on with them so well.”
He believed in unfaltering commitment to the patient’s wellbeing, and duty to teach and train young surgeons. He expected the best from you – not by way of imposition, but rather an invitation to strive to do whatever you were doing, as well as you could. As the expert in his field, he was asked to teach up and down the country. His presence, analytical style, and a vocabulary richly laced with reference to the Classics dazzled his audiences. He established many regional units nationwide and visited regularly. Ever supportive, never critical and always ready to share the burden in those cases, which did not proceed as intended, he became friend, mentor and an inspiration to a generation of young surgeons.
For over 30 years, he served with distinction as Honorary Consultant Advisor to all three of the Defence Medical Services (DMS). In 2003, he was appointed Consultant in Charge, War Nerve Injuries Clinic, DMS Rehabilitation Unit, Headley Court where, again, he established a world-class team. This collaboration represented a high point in British Surgery and Science and from it flowed the current concepts of management of War Nerve Injuries. Rod Dunn, Consultant Plastic and Reconstructive Surgeon, recalls, “Because of the extraordinary advances made by the DMS over the period, patients were surviving dreadful injuries that would have been fatal even in the recent past. His empathy, affinity, and respect for these young service men and women conveyed an inestimable sense of being valued and cared for.” As it was at Stanmore, he was revered by his patients, and colleagues alike.
RB’s research and published work altered the attitude of clinicians worldwide; his contributions were recognised in this country and overseas with many Honorary clinical appointments. He delivered several prestigious eponymous lectures, including the Robert Jones Lecture, ‘The Transition Zone’ in 2000, and the James IV Lecture, ‘Power and Pain’ in 2009. In 2011, he completed his magnum opus, ‘Surgical Disorders of the Peripheral Nerves’.
In his leisure time, he climbed, and fell ran. In his retirement, he enjoyed reading and writing, sea swimming and creating a fragment of English woodland in his garden at Stanmore. He bore his illness with stoical dignity. He died on 22 May 2023. He is survived by his dear partner Margaret Taggart with whom he worked at St Mary’s in her capacity as Sister in Charge of the Orthopaedic Department, and at Stanmore, where she was Coordinator of the Peripheral Nerve Injury Unit. He was divorced, and leaves a son and daughter from that marriage.
Surgeon, scientist, leader, teacher, author, mentor. It is given to few in medicine to be more than one of these. Rolfe Birch was an exception. His range was truly remarkable and in every one of his vocations, he excelled. n
In Memoriam 58 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk
“Rolfe Birch was one of the most remarkable surgeons and clinical scientists of his generation, who determined the modern principles of surgical treatment of Brachial Plexus and complex peripheral nerve injury, and by whose outstanding leadership in a unique specialty established two world-class Peripheral Nerve Injury Units – one Civilian and one Military.”
Kar Hao Teoh
22nd January 1983 – 3rd August 2023
It is with profound sorrow that we mourn the untimely passing of Mr Kar Hao Teoh, who left us on August 3, 2023, aged 40.

After completing surgical training in Wales (2017), he undertook multiple international fellowships (EFAS, BOA, BOFAS, AO, SICOT, EFORT/APOA, IBRA), before Consultant appointment (foot and ankle) at The Princess Alexandra Hospital, Harlow (2018).

Kar Hao developed a tertiary practice for total ankle replacements, pioneering the UK use of the ‘Vantage’ system. As Clinical Lead for Major Trauma, he was instrumental in improving patient outcomes. Additional roles emphasised his dedication to training and education, including regional Specialty Professional Advisor (Trauma & Orthopaedics, East of England), interim Associate Dean for Undergraduate Education (Queen Mary University of London) and Clinical Subdean (Anglia Ruskin University).
He excelled in research with multiple publications and won the EFAS Presidential Prize for best project (2022).
Kar Hao was a dedicated and devoted husband, doting father, and a loving son to his mother. He was a loyal friend and well-loved colleague. As well as being a keen traveller with a personal goal to visit every country in the world, he enjoyed learning history and experiencing other cultures. He was a foodie and an excellent cook.
Kar Hao was a trailblazer, an unstoppable force, fiercely determined, curious minded and analytical. He was also selfless, steadfast, generous, witty and a maverick.
He is survived by his mother Ai Nah, wife Sara and 2-yearold son Hugo.
May he rest in eternal peace, leaving behind a legacy that will forever inspire. n
JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk | 59
In Memoriam
Products, Courses and Events
We specialise in casing and packaging solutions for orthopaedic implants, medical equipment and have supplied many of the world’s leading medical organisations.
We specialise in casing and packaging solutions for orthopaedic implants, medical equipment and have supplied many of the world’s leading medical organisations.
Our flight cases are made in our 70,000 sq ft factory in the UK using the highest quality materials to ensure that your vital
Our flight cases are made in our 70,000 sq ft factory in the UK using the highest quality materials to ensure that your vital equipment is fully protected in transit.

equipment is fully protected in transit. We design and manufacture cases to your exact specification. A range of pull-out drawers, shelves, lift-out trays, doors and shutters can be integrated into the case. With an in-house design team and advanced computer aided design and CNC routing facilities, we can produce custom foam interiors to




16th Trauma & Orthopaedics Update
Val d’Isere, 22-25 January 2024
www.doctorsupdates.com info@doctorsupdates.com
+44 (0) 208 7151924
Doctorsupdates 2024, in their 35th year will feature 16th Trauma and Orthopaedics Update. This meeting is unique as it provides interaction between a number of

house implant samples, instruments and any other equipment.
Web: https://uk.unitedorthopedic.com

Email: uk.service@unitedorthopedic.com
Telephone: +44 (0) 1827 214773

Trifibre Ltd
17 Boston Rpad Gorse Hill Industrial Estate Leicester LE4 1AW
Telephone: 0116 232 3166
Email us: info@trifibre.co.uk
Web: www.trifibre.co.uk
We design and manufacture cases to your exact specification. A range of pull-out drawers, shelves, lift-out trays, doors and shutters can be integrated into the case. With an in-house design team and advanced computer aided design and CNC routing facilities, we can produce custom foam interiors to house implant samples, instruments and any other equipment.

different specialities: orthopaedics, anaesthetics, critical care and pain, emergency medicine, radiology, plastic surgery, dermatology and general practice. We also invite speakers from other specialties like haematology, neurology, rheumatology to contribute to our education.
The programme is suitable for consultants and senior trainees. The format is informal and sessions
Trifibre Ltd
17 Boston Rpad
Gorse Hill Industrial Estate
Leicester LE4 1AW
Telephone: 0116 232 3166
Email us: info@trifibre.co.uk

Web: www.trifibre.co.uk
include trauma and elective surgery, multidisciplinary sessions and a free paper competition for trainees.
Each day concludes with a lecture of general interest by an eminent guest speaker.
We have an excellent orthopaedic faculty lined up and the programme, when confirmed, will be available at www.doctorsupdates.com

For over 25 years, United Orthopedic has been a leading international designer, manufacturer, and distributor of versatile orthopaedic solutions that deliver world-class orthopaedic joint replacement implants which have made life better for hundreds of thousands of patients needing hip and knee replacements.

Find out more about our USTAR II Primary and & Revision Hinge Knee and Limb Salvage System which is part of the United Orthopedic portfolio of arthroplasty and limb salvage products.

• Platform-based approach - consistent design philosophy allows a platformbased approach to provide surgeons flexibility for a wide range of procedures
• Demand-matching - includes a wide range of product options for demandmatching to optimise solutions based on patient needs

• Advanced surgical technologies - builds on proven design philosophies with advanced surgical technologies to help deliver reproducible clinical outcomes and a streamlined procedure

Surviving
We provide national support and can help with:
• Legal advice
• Financial support
• Peer support
• 24hr counselling
• Benefits and welfare advice
Download the App


We’re here for you and your patients:
Visit dayonetrauma.org/supporting-you

Call 0300 303 5648
Email dayone@dayonetrauma.org
Follow @dayonetrauma
Together, we will provide #MoreTraumaSupport
Charity number 1194227
The Journal of Trauma and Orthopaedics (JTO) is the official publication of the British Orthopaedic Association (BOA). It is the only publication that reaches T&O surgeons throughout the UK and every BOA member worldwide. The journal is also now available to everyone around the world via the JTO App. Read the latest issue and past issues on the go, with an advanced search function to enable easy access to all content. Available at the Apple App Store and Google Play – search for JTO @ BOA

60 | JTO | Volume 11 | Issue 03 | September 2023 | boa.ac.uk
trauma is just the start No one should be left to rebuild their life on their own
Ant ibiot ic-Loaded Bone Cement in Hemiarthroplasty Following FNOF – New Insights
Fractured neck of femur (FNOF) often leads to disability and is associated with high morbidity and mortality.1
Hemiarthroplasty is considered a good treatment option, particularly in the elderly population. However, despite improvements in theatre standards and treatment standards, periprosthetic joint infection (PJI) remains one of the most relevant complications in hemiarthroplasty.2,3 The findings of the prospective WHiTE 8 trial, published on June, 21 2023 in Lancet, now add valuable insights into the management of cemented hemiarthroplasty and infection prevention in FNOF patients.4
Adding antibiotics effectively prevents PJI
The WHiTE 8 study included 4,936 patients aged 60 years or older from 26 hospitals in the United Kingdom (UK). In this study, fixation of hip prostheses with highdose dual antibiotic-loaded bone cement was associated with a PJI rate in the “intention to treat analysis” at 90 days post randomization of 1.2% vs. 1.7% when using single antibioticloaded bone cement (p = 0.16). In the “as treated analysis” with 1.1% vs. 1.8% respectively results were very close to demonstrating a significant effect (p = 0.077). The overall very low PJI rates in this study support the benefit of using antibiotic-loaded


bone cement in hemiarthroplasty presented in previous studies18, 19. The low PJI level in the WHiTE 8 high-dose dual antibiotic-loaded bone cement group is in line with previous studies which demonstrated almost identical infection rates for high-dose dual antibioticloaded bone cement between 1.1% and 1.2% for hemiarthroplasty and significant relative risk reductions of up to 69% with highdose dual vs. single antibiotic-loaded bone cement.5-7, 18 Of note, it has to be taken into account that these studies covered longer observation periods of 12 months compared to 90 days in the WHiTE 8 study.8, A
Variable risk of infection
Theatre standards, perioperative prophylaxis, as well as patient-related risk factors contribute to the occurrence of PJI.9 The prevalence of infection varies according to location and type of hip arthroplasty, reaching up to 2% in primary surgery and 4% after revision.10 Epidemiological studies point to considerable variations in PJI rates and standards of care for infection control across different settings and health services worldwide.11 The UK always has been a lighthouse in applying high standards of care for the management of hip fracture such as the guideline produced by the National Institute for Health and Care Excellence (NICE).12
A In a comment on the WHiTE 8 trial results Tarabichi and Parvizi emphasise that WHiTE 8 is the largest randomised controlled trial in a large number of sites on the efficacy of prophylactic antibiotics in patients undergoing hemiarthroplasty.8 They discuss, however, that at least 1 year of follow- up would be necessary in order to truly determine the efficacy of DALBC in preventing the development of deep surgical site infection.
PJI reduction – the common goal
In addition to patient-related factors perioperative variables such as operating room traffic, timing of surgery, selection of prophylactic antibiotics and surgical site preparation should be evaluated and optimized prior to surgery to decrease rates of PJI13 Even stricter infection prevention measures implemented during the COVID pandemic may additionally have favorably influenced PJI rates with infections becoming an exception.
Experts agree that rapid access to surgery and coordinated care are essential in order to help patients recover faster and regain mobility.14,15 All efforts should be made to lower the burden of PJI, in particular in a multimorbid high-risk population such as hip hemiarthroplasty patients. In fact, there is evidence that improvements in infection control translate into decreased risk of reoperation due to surgical site infection such as seen in a large Danish cohort study.16
Increasing clinical experience with combined local antibiotics
To this end, a whole range of actions must be taken into consideration. Among others, antibioticloaded bone cement constitutes one significant aspect of local infection prevention. Indeed, experienced surgeons worldwide have increasingly adapted standard procedures to using antibioticloaded bone cement, including dual antibioticloaded bone cement, when providing hip hemiarthroplasty in patients with FNOF.
Due to the growing number of arthroplasties, the number of patients with PJI is expected to further increase. There is an urgent need to lower the burden of PJI faced by practicing clinicians, institutions, and patients as well as a need for infectionrelated revision surgery.17 n
References available at Heraeus Medical www.herae.us/boa-advertorial

“The overall very low PJI rates in this study support the benefit of using antibiotic-loaded bone cement in hemiarthroplasty presented in previous studies.”
SPONSORED CONTENT www.heraeus-medical.com

What would you do if...? Did you know? The Medical Protection Society Limited (“MPS”) is a company limited by guarantee registered in England with company number 00036142 at Level 19, The Shard, 32 London Bridge Street, London, SE1 9SG. MPS is not an insurance company. All the benefits of membership of MPS are discretionary as set out in the Memorandum and Articles of Association. MPS® and Medical Protection® are registered trademarks. medicalprotection.org/nhs £549 Get protected from just * 2304244967:06/23 *Cost shown is the annual membership price for a UK Medical Consultant working exclusively in the NHS. Subject to protection requirements and underwriting approval. 1 in 4 of our consultant members have received a complaint.† If a patient complains about you, it’s important to have the support of an expert medicolegal team by your side. †Source: MPS January 2023. The likelihood of a consultant non-claims member experiencing a complaint. You received a complaint from a patient Your personal conduct was called into question You received a letter from the GMC You were called upon as part of an inquest You needed to provide a formal report



































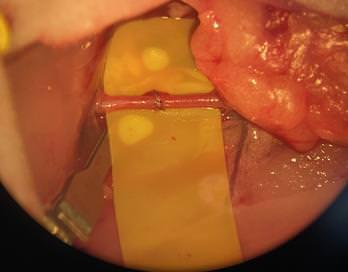
















































































































































 Chetan Khatri, Steve Gwilym, Keith Tucker, Edward T Davis, Xavier L Griffin, David Beard and Andrew Metcalfe
Chetan Khatri, Steve Gwilym, Keith Tucker, Edward T Davis, Xavier L Griffin, David Beard and Andrew Metcalfe