

Journal of Trauma and Orthopaedics

Shoulder implant data collection on the National Joint Registry p40 The future of shoulder and elbow surgery p52 Noise-induced hearing loss in orthopaedic surgery: Are we at risk? p24


OrthoFoam Adult Ramp
Indicated for all surgical cases where elevation is necessary without offloading the heel.
Home Recovery
Recover from your surgery in the comfort of your own bed with the HomeFoam version of our Ortholove® Professional Series SRE (Swelling Reduction Elevator).
Reducing postoperative swelling enhances healing and recovery and our beautifully designed HomeFoam is recommended by expert surgeons to keep your foot at the perfect height whilst relieving stresses on your knee, hip and lower back.
Optimal Recovery
Indicated following foot and ankle surgical cases for application in theatre or recovery or even preoperatively for trauma cases to ensure reduction of swelling. The ergonomic design ensures patient comfort, with stable elevation at heart level and without strain on the knee or hip.


Elevator OrthoFoam Foot Holder
Indicated for use in surgery for foot and ankle procedures, from trauma to total ankle replacements.

Journal of Trauma and Orthopaedics
In this issue...
Metastatic bone disease and the development of local specialist networks in the UK
Ashley Scrimshire, Tom Beckingsale, Kenneth S Rankin and Kanishka Ghosh

Seeing the future digitally: Computer vision in trauma and orthopaedics
Ali Ridha and Aditya Vijay
Shoulder implant data collection on the National Joint Registry
National selection to T&O ST3 posts – An update
Lucky Jeyaseelan and Cronan Kerin on behalf of the Selection Design Group
Noise-induced hearing loss in orthopaedic surgery: Are we at risk?
Jerry
Wide awake local anaesthetic no tourniquet (WALANT) hand surgery in a community setting – eight years experience
Ashita Paul, Jagannath Chakravarthy, Martin White and John Harrison


Jaime Candal-Couto, Simon Robinson, David Hawkes, David Miller and Derek Pegg
How trainees can get involved in sustainability in surgery
Oliver Townsend and Karen Chui 48 International:
Establishing an orthopaedic trauma service in rural Ethiopia
Richard Power
The future of shoulder and elbow surgery
Deborah Higgs
53 Subspecialty:
Centralisation of low-volume high complexity orthopaedic surgery: Hub-and-spoke models in the National Health Service
Neal Rupani, Vanessa J Chow, Jonathan L Rees and Steve Drew
56 Subspecialty:
Large language models in upper limb surgery: A narrative review
Catherine Simister, Kyle Lam, Andrew Yiu and James M Kinross
60 Subspecialty:
A tipping point for technology in shoulder surgery?
John McNamara, Matthew Williams and Simon Hurst 64 In Memoriam:
Malcolm Swann














JTO Editorial Team
l Amar Rangan (Executive Editor)
l Paul Banaszkiewicz (Editor)
l Simon Britten (Medico-legal Editor)
l Karen Chui (Trainee Editor)
l Deborah Higgs (Guest Editor)
BOA Executive
l Mark Bowditch (President)
l Simon Hodkinson (Immediate Past President)
l Fergal Monsell (Vice President)
l Amar Rangan (Vice President Elect)
l Hiro Tanaka (Honorary Secretary)
l Ian McNab (Honorary Treasurer)
BOA Elected Trustees
l Mark Bowditch (President)
l Simon Hodkinson (Immediate Past President)
l Fergal Monsell (Vice President)
l Amar Rangan (Vice President Elect)
l Hiro Tanaka (Honorary Secretary)
l Ian McNab (Honorary Treasurer)
l Cheryl Baldwick
l Deepa Bose
l Caroline Hing
l Andrew Price
l Andrew Manktelow
l Andrea Sott
l Paul Banaszkiewicz
l Vikas Khanduja
l Dominic Meek
l Benjamin Ollivere
BOA Staff
Executive Office
Chief Operating Officer - Justine Clarke
Personal Assistant to the Executive - Celia Jones
Policy and Programmes
Head of Policy and Public Affairs
- Gary Robjent
Head of Education and Programmes - Alice Coburn
Programme and Committees Officer
- Eliza Heng
Educational Programmes Assistant - Maimuna May
Communications and Operations
Director of Communications and Operations
- Annette Heninger
Marketing and Communications Officer
- Pujarini Basu Nadaf
Membership and Governance Officer
- Natasha Wainwright
Publications and Web Officer
- Nick Dunwell
Finance
Director of Finance - Liz Fry
Finance Officer - Hayley Ly
Events and Specialist Societies
Head of Events - Charlie Silva
Events Coordinator - Venease Morgan
UKSSB Executive Assistant - Henry Dodds

From the Executive Editor
Amar Rangan
As I take up the reins as Executive Editor, I am reminded of what Benjamin Franklin once said, “Either write something worth reading or do something worth writing.” In many ways, JTO embodies that quote and is helping disseminate important news stories, interesting articles, and key opinion pieces to a wide readership. I would like to start my work in this role by thanking Deborah Eastwood for her stewardship and the editorial team for ensuring the growing popularity of JTO.
This issue does not disappoint. There is something in it for everyone in the T&O community. Did you know that the risk of noise induced hearing loss is nearly 50% in senior T&O surgeons? I wonder how many of us speak louder as we get older! Jerry Sam and Hiro Tanaka present the occupational hazard of noise induced hearing loss affecting orthopaedic surgeons and suggest measures we can take to mitigate that risk (p24). Lucky Jayaseelan and Cronan Kerin provide an update on the current selection process to T&O ST3 posts (p20). Ashley Scrimshire and colleagues propose a hub-and-spoke regional network model to cope with the growing problem of metastatic bone disease (p32). Ali Ridha and Aditya Vijay highlight areas where the all-pervasive AI and Computer Vision have found their place in T&O (p36). Richard Power explains how the fulfilling work by orthopaedic surgeons in Leicester helped the Gondar University Hospital in Ethiopia set up their own trauma theatre and training programme (p48).
Copyright
Copyright© 2024 by the BOA. Unless stated otherwise, copyright rests with the BOA. Published on behalf of the British Orthopaedic Association by: Open Box M&C
Advertising
All advertisements are subject to approval by the BOA Executive Board. If you’d like to advertise in future issues of the JTO, please contact our sales team for more information:
Email: JTOsales@ob-mc.co.uk | Telephone: +44 (0)121 200 7820 Open Box M&C, Premier House, 13 St Paul’s Square, Birmingham B3 1RB
Disclaimer
The articles and advertisements in this publication are the responsibility of the contributor or advertiser concerned. The publishers and editor and their respective employees, officers and agents accept no liability whatsoever for the consequences of any inaccurate or misleading data, opinions or statement or of any action taken as a result of any article in this publication.
BOA contact details
The British Orthopaedic Association, 38-43 Lincoln’s Inn Fields, London WC2A 3PE Telephone: 020 7405 6507
How to contact JTO
Email: jto@boa.ac.uk
Theatres are said to be three- to six-times more carbon intense than the hospital as a whole, which has brought into sharp focus the need for sustainable surgical practices. Patient experience should of course be central in implementing safe and sustainable service improvements. Ashita Paul and her co-authors present their experience in using WALANT in hand surgery, which has now become more established in some centres post-COVID (p28). This is a good example of improved patient experience by avoiding general anaesthesia and a tourniquet, alongside surgical sustainability and benefits to the health economy. Scaling up such initiatives should bring wider benefits. Oliver Townsend and Karen Chui share their thoughts on how trainees can get involved at various levels in driving sustainable practices in surgery (p44).
The subspecialty section is shoulder and elbow with Deborah Higgs as guest editor (p52-62). A major growth in shoulder replacement volumes is anticipated over the next decade. Features in this section include innovation and use of technology in shoulder arthroplasty, initiatives to centralise the provision of low-volume procedures, and the use of large language models to aid clinical practice.
In addition to our upper limb subspecialty section, Jaime Candal-Couto et al. provide highlights of shoulder data analyses from the NJR. In particular, the link between surgeon volumes and outcomes in shoulder arthroplasty provides food for thought (p40).
I hope you enjoy reading this issue. I would like to take this opportunity to extend my very best wishes to you all for the festive season and the New Year. n



Aligning objectives and preventing harm
Mark Bowditch
When you read this, I shall be three months into my presidential year brimming with ideas and focused on tackling the issues raised in our five-year review. In particular, I am committed to demonstrating to you all the value of being a BOA member. You may have read my monthly blog, I’m pleased to have received comments and replies – keep them coming! With the new Government ‘missions’ becoming clearer, the NHS is very much centre stage, and the new investment is welcome. Our role is to ‘Speak up for T&O’ and ensure that we and our patients benefit from new resource. At a recent event, Chris Whitty, CMO, reminded us that alignment to national strategies is the best way to gain traction with our objectives.
There are three facets to the Government’s new health missions.
1. Hospital to community – Right patient, right professional, right place: Patient pathways, estate, workforce, and training are all key to this. We are working closely with stakeholders to ensure that sensible integrated pathways of care with local T&O input are shared.
As I write, I’m delighted to say that tomorrow I do the very first list in a brand new orthopaedic surgical hub named after Dame Clare Marx. It’s a fantastic facility which will hopefully allow us to continue planned essential care without interruption throughout winter for the first time in many years.
We welcome the commitment to surgical hubs, which the BOA has long campaigned for and the early evidence suggests >20% benefit in throughput. Moving to protected hubs may mean that you lose ‘trauma surge capacity’, so if you are doing so, make sure you demonstrate the need for increased trauma lists.
None of us likes inefficiency but we will advocate for safe, high-quality access and care for patients and members. We can achieve little without teamwork, so be kind and supportive to your colleagues as we move sites and try to do more work.
In all this, please do not forget the ‘future surgeons’. If you have extra lists in the NHS – find a trainee and involve them. With over half of routine joint replacements being undertaken in the independent sector (IS), I have been investigating how trainees might follow the work, drawing on the lessons from international colleagues and speaking with the NHS training leads and the IS to identify barriers.
2. Analogue to digital – EPRs seemed to be spreading like wildfire. Change is difficult and at first seems counter-productive but this is something we have to encompass. To help, we are preparing a ‘T&O top tips’ guide to implementing and using the main systems. Data is the new ‘gold’ and AI has much to offer. It won’t replace orthopaedic surgeons but those who embrace it will replace those who don’t.
3. Treatment to Prevention – Prevention is my theme as President. I have classified this into:
Primary: Prevention is better than cure. We’ve more than enough work so can we influence policy or practice to prevent injuries? In my knee world, this might be an ACL injury prevention programme. All sub-specialties will have an example so get your thinking caps on and let us know!
Secondary: When we do intervene with surgery, we must try to prevent harm by the right evidence-based interventions and reduce complications to a minimum. This includes human factors, infection control and learning from the most common T&O litigation themes.
Tertiary: Wellbeing, team-working and preventing toxic cultures. Continuing previous presidential themes of sustainability and workforce – we need to consider how to do this for ourselves and the whole team. After 25 years with largely the same team at Ipswich, I have been reflecting on the importance of this ‘family’ to my work and life balance. We need to support each other, and we will be looking to you all to share good practice and ways to prevent harm.
My new year’s challenge to you all is can you demonstrate and share the multiple ways to prevent harm whilst transforming T&O lives? I would like to thank you all for your commitment to our patients this year and wish you and your families seasonal greetings. Be kind to yourself, laugh lots, recharge and enjoy the festivities. n
BOA Annual Congress 2025Save the Date!
Thank you to everyone for attending the BOA Annual Congress this September, we have received great feedback from our delegates, speaker and exhibitors.
Our next Annual Congress for 2025 is taking place in Liverpool on 16th – 19th September, the programme will be created around the theme of ‘Preventing Harm & Transforming Lives’
Keep an eye out for further information including abstract submissions on the website at www.boa.ac.uk/Congress.
Thank you to all our exhibitors and sponsors for supporting the 2024 Annual Congress. For information regarding exhibiting and sponsorship at the 2025 Annual Congress, contact exhibitions@boa.ac.uk
Obesity Health Alliance
Following on from work by the Orthopaedic Committee and as part of Mark Bowditch’s Presidential year theme of ‘prevention’, the BOA has joined the Obesity Health Alliance (OHA).
The OHA is keen to promote the obesity/MSK agenda, in the same way it has done for obesity/CVD and obesity/cancer.
The OHA is composed of leading national health charities, medical royal colleges, campaign groups and membership bodies with an interest in health and public health. Aligning MSK and obesity issues will provide another channel to raise the MSK/T&O profile.
Further details of the OHA at https://obesityhealthalliance.org.uk
2025 Robert Jones Medal and Association Prize
Applications for the 2025 Robert Jones Medal opens on the 1st January and closes on 31st January 2025. The BOA offers a prize of £500 and a gold medal in memory of Sir Robert Jones through an annual essay competition, in which BOA members can submit an essay of their own choice on an orthopaedic interest.
The essay is to be submitted in the following format:
Typewritten in English, not exceeding 3000 words, (excluding references), do not put your name on the essay –all must be anonymised when reviewed by the President.
Essays should be submitted via e-mail to Celia Jones, PA to President & COO at c.jones@boa.ac.uk

BOA Educational Courses

The BOA runs a wide range of courses under the Education Committee. These courses cater to the educational needs of a wide range of members and non-members at all stages of their careers.
Current courses include:
• SAS Professional Development Programme
• Training Orthopaedic Trainers Course (V-TOTs)
• Law for Orthopaedic Surgeons
Full details of all our courses can be found on the BOA website at www.boa.ac.uk/courses
English Language Support Academy for Medics
Belfast City Council is supporting 11 experienced international doctors to become registered and licenced to practise in the city, through an English Language Support Academy for Medics – the first of its kind in Northern Ireland – as they re-establish their careers in their new home city. The first cohort of medical professionals to receive support from the new programme include an orthopaedic surgeon, emergency medical doctors, gynaecologists, GPs and paediatricians.
Further details are available from www.belfastcity.gov. uk/employability.

BOA ORUK Research Fellowships
Applications for the BOA / ORUK Research Fellowship will open in 2025.
This scheme will award two fellowships of up to £65k for a project in any area of orthopaedics each year, including basic science, diagnosis, treatment, surgical technology.
Applications are open to BOA members who are trainees, post-CCT members, and SAS surgeons. Keep an eye out for information at www.boa.ac.uk/research-fellowships
BOA Ortho Update Course 2025
The BOA Ortho Update Course will take place on Saturday 1st March, in Birmingham
We are excited to announce a newly restructured BOA Orth Update course that has something for everyone. This includes the difficult critical CBDs that delegates often struggle to get signed-off, such as metastatic spinal cord compression and primary/secondary musculoskeletal malignancies. Improve and polish up your clinical examination skills in both a generic and diagnosis-specific manner.
For the first time, we are introducing the hugely popular small group teaching that involves a question-and-answer session on various orthopaedic topics, including the young adult hip, ostomies for the young arthritic knee patient and trauma scenarios. For further information and to register your place, visit www.boa.ac.uk/OrthoUpdate
Get involved in UKITE
More than 800 trainees from across the UK and Ireland are expected to take the UKITE Exam online between the 6th – 13th December 2024.
Since its inception in 2007, UKITE has helped trainees prepare for section 1 of the FRCS Tr and Orth with questions covering the full spectrum of sub-specialties, contributed by our volunteers.


We would like to thank our tireless team of editors, subspecialty leads, and our clinical lead, Mark Sohatee for their tireless work. Our editors make UKITE possible by developing, reviewing and validating questions.
We have vacancies in all sub-specialties for senior trainees, SAS, or new consultants who can contribute an hour or two per month. This is great introduction to question writing and examining, no experience required, we provide all the training. Find out how to join the team at www.boa.ac.uk/UKITE-editorial-role
For any queries, please contact ukite@boa.ac.uk or visit www.boa.ac.uk/UKITE
Medical Student Essay Prize 2025
Medical students are invited to submit an essay on their Quality Improvement Project (QUIP) and how it has equipped them and their department to perform better. The project must have completed at least one round of the Plan Do Study Act (PDSA) cycle and can be on any aspect of T&O.
The competition is open to all medical students in the UK or Republic of Ireland.
Applications will open in 2025 and further news information will be available at www.boa.ac.uk/ medical-student-essay


2024 Medical Student Essay Prize Winner
Congratulations to Andreas Conte, winner of the 2024 Medical student essay prize, for his essay on ‘Improving the suspected Cauda Equina Syndrome pathway’.
Andreas is a final-year medical student studying at King’s College London. His passion for orthopaedic surgery has guided his extra-curricular academic research. He is currently in the process of publishing two textbook chapters in the Oxford Textbook of Trauma and Orthopaedics, has presented work at international conferences, and is currently involved in orthopaedic research.
Essay summary:
The Quality Improvement Project (QIP) focused on addressing delays in obtaining emergency MRI scans for suspected Cauda Equina Syndrome (CES) at Medway Maritime Hospital. CES, characterised by spinal root compression, requires rapid MRI diagnosis and surgical intervention to prevent severe outcomes like paralysis and incontinence. According to national GIRFT guidelines, MRI should be provided within four hours of request, yet audits revealed Medway’s average time to MRI was significantly delayed, averaging ten hours.
Recommendations for improvement involve implementing a standardised CES MRI request form with red flags to minimise unnecessary imaging, ongoing CES-specific audits, and potentially extending MRI operation hours to 10 pm. These changes aim to improve timely MRI access, though broader interdisciplinary collaboration is essential for sustainable progress. Challenges faced included departmental coordination issues and delays from junior doctor strikes during later PDSA cycles, underlining the need for a larger patient sample in future audits to gauge more accurate results.
You can read the winning essay on Orthopaedics Online at www.boa.ac.uk/O2 where we will be featuring the highest ranked essays throughout December. n

BOA Soli Lam Travelling Fellowship
The three-week BOA Soli Lam Travelling Fellowship in August and September 2024 provided invaluable insights into the management of spinal oncology across three leading US institutions: New York University Hospital, North Shore University Hospital, and Memorial Sloan Kettering Cancer Centre. With a focus on primary and metastatic spinal tumours, the fellowship offered a chance to compare approaches in both healthcare systems and clinical management, enhancing knowledge just before beginning my own consultant practice.
At NYU, under Dr Ilya Laufer, I observed a collaborative, multidisciplinary model involving specialists from surgery, oncology, and palliative care, which streamlined patient management and minimised clinic visits. This model demonstrated the potential benefits of incorporating similar practices into the NHS to improve patient outcomes and optimise resources. Dr Laufer’s team also showcased the effective use of allied health professionals, allowing physicians to focus on specialist care – a concept worth exploring within the NHS context.

Euan Stirling
A brief visit to North Shore University Hospital, led by Dr Daniel Sciubba and Dr Larry Lo, highlighted advances in surgical navigation, robotics, and pre-operative planning, particularly for complex spinal tumour resections. I also attended a spinal deformity course and gained insights into more aggressive surgical strategies practiced in the US compared to the UK, sparking reflections on surgical risk tolerance and patient management.
Lastly, at Memorial Sloan Kettering, I observed the prioritisation of swift systemic therapy alongside minimised surgical interventions. Techniques like stereotactic radiosurgery (SBRT), intraoperative ultrasound, and postoperative CT myelograms were used to optimise patient outcomes.
The experience underscored the benefits of multidisciplinary and systematised care, alternative therapeutic approaches, and the potential to adapt these learnings within the NHS. I would like to thank both the BOA and the family and estate of Soli Lam for providing me with this opportunity, and the generous financial support accorded to me n
Izuka Cannulated Fracture Awls &
Intramedullary Nail Removal Set
Trocar Set

Trocar Rod #8093-03
Designed to help safely and accurately place standard K-wires up to 0.825” (2,1 mm) with either open or percutaneous techniques, helping to avoid soft tissue injuries that may occur without the use of such devices

Basic Screw Removal System



System designed to help remove an intramedullary nail
INSTRUCTIONS FOR NAIL REMOVAL:
5. Tap on the end of the t-handle tightening assembly with three light taps and re-tighten the t-handle tightening assembly if needed. Using the slaphammer or mallet, start with light taps to remove the nail. Blunt Awl #8093-01 Sharp Awl #8093-02

1. Insert the push rod into the slaphammer rod, leaving the ball end outside of the slaphammer rod. Connect the t-handle tightening assembly over the ball end of the push rod. Screw the t-handle tightening assembly with push rod attached into the slaphammer rod.
2. To determine the correct size of nail extraction spreader, it should be completely inside the nail to be removed. If the extraction spreader wobbles, then it is too small. If threads are exposed, it is too large.
3. The extraction spreader is then completely threaded into the tapered end of the slaphammer rod. It is tightened using the open-end wrench and stabilizing bar.
4. The complete assembly is screwed into the nail by hand tightening.












to help hold a bone/bone plate in position for reduction— the one-side coated jaw helps to protect





Large Bone Clamp with Plate Protection
British Association for Surgery of the Knee (BASK) update
James Murray, BASK Honorary Secretary and Alasdair Santini, BASK President
BASK’s 2024 Annual Congress in May under the Presidency of Leela Biant, was a great success, with both delegates and industry enjoying the excellent facilities at Manchester Central Convention Centre. Before the conference, the Major Revision Knee Networks met to report data for NHSE – whilst this project is still in trial phase, there has been a significant change in practice with excellent uptake of this newer collaborative way of working. Additionally, BASK Executive representatives joined the ‘Power Up To Play’ team for an injury prevention event at Old Trafford (football not cricket!) with one of the Manchester United Academy teams. Please encourage all of your young sports players (patients, friends and family!) to use these resources as 10 minutes twice a week reduces injury rates by approximately 70% –www.poweruptoplay.org


BASK continues to support BOTA as the future of orthopaedics. This year, we hosted a successful ‘Best of the Best’ Top Gun-style training day at the Arthrex Academy in Birmingham. We are also investing in medical students – Kash Akhtar organised an exceptionally popular educational day in London. Thanks to the faculty for their support – stay tuned for more events!
The Lorden Trickey lecture was given by Deepak Goyal who both entertained and informed on the subject of locating the patella into the trochlea groove. A lifetime achievement award was made to Tim Wilton for his services to knee surgery and Presidential medals were awarded to Matts Brittberg, Andy Price, David Beard and Deepak Goyal.
There were novel ‘silent disco’ style industry sessions and feedback indicated these were very popular. These meetings require substantial planning, and we benefited greatly from Clockwork’s expertise and the efforts of the Executive and faculty — thank you. At the same time, our new website went live www.bask.ac.uk, thanks to Steve McDonnell, formerly Web and Media Lead, now Research Lead.
At the BOA Annual Congress, the BASK presidency handover from Leela Biant to Alasdair Santini took place, and Michael Held from Cape Town eloquently delivered the Adrian Henry lecture. BASK strengthened international relations, featuring the newly formed Pakistan Knee Society, with Umer Butt and Zeeshan Khan presenting on ACL and complex primary TKA in two insightful revalidation sessions. Additionally, the BASK Executive welcomed new members: Rahul Bhattacharyya (Web & Media), Abtin Alvand (Education), Rahul Patel (Member at Large for EDI and Administration), Mike McNicholas (Member at Large for International Links and Fellowships), Nick Kalson and Jasion Patel (Early Years). n
Dates for your diary for future BASK Spring Conferences: 2025 – Harrogate – 29th – 30th April 2026 – Glasgow – 14th – 15th April
The British Orthopaedic Research Society (BORS) update
The British Orthopaedic Research Society (BORS) was funded in 1961 and proudly boasts a multidisciplinary membership of surgeons, scientists, engineers and other allied health care professionals, united in the pursuit of collaboration in orthopaedic and musculoskeletal research.
Following last year’s meeting at St John’s College, University of Cambridge, the 2024 BORS Annual Meeting was held with great success at the University of Sheffield on the 9th and 10th September, with over 100 delegates attending. The Presidential Lecture was delivered by Professor Deborah Mason (Cardiff University), while keynote talks were given by Dr Andrew Phillips (Imperial College London), Professor David Pierce (University of Connecticut), Dr Sybille Grad (AO Institute), Professor Ele Zeggini (Helmholtz, Munich), and Professor Martyn Snow (Royal Orthopaedic Hospital). The invited presentations were supported by a Pain
Workshop and free paper sessions on the diverse themes of Clinical Biomechanics, Mechanobiology, Clinical Studies, Biomechanical Modelling, Disease Pathobiology and Therapeutics, in addition to a New Investigator Award session and Rapid Poster presentations.
Pursuant to the Society’s goal of advancing education in orthopaedic research, the next round of BORS/BJR Travelling Fellowship awardees were presented to the membership and we look forward to hearing about their experiences at the Society’s next annual meeting. This will be held at the University of Birmingham, 8th – 9th September 2025.
In other events, Karina Wright (Hon Treasurer) led the BORS revalidation session at the 2024 BOA Annual Congress on the topic of Injectables and Cell Therapies for Cartilage Repair/Osteoarthritis, and Ines Reichert (President Elect) will lead a BORS contingent workshop at the next ICORS meeting in Adelaide, Australia in October 2025.
Readers interested in joining the British Orthopaedic Research Society can apply on the website at www.borsoc.org.uk n
Anthony Herbert, BORS Honorary Secretary
Photographs courtesy of Clockwork Medical
Orthopaedic Trauma Society (OTS) update
Steven Borland, OTS Education Chair and Darren Forward, OTS President
The Orthopaedic Trauma Society proudly celebrated all aspects of trauma at our annual conference, this year hosted in Nottingham. We were honoured to hear from distinguished keynote speakers from our international faculty: Dr Samir Mehta, a Professor at the University of Pennsylvania, and Dr Heather Vallier, a Professor at Case Western Reserve University and Past President of the Orthopaedic Trauma Association (OTA).

Homa Arshad led a powerful session on sexual misconduct in surgery, providing much to reflect on. We heard from our national leaders, including Chris Moran, who led our celebration of 40 years of the Nottingham Fracture Forum, and shared valuable
This year’s conference featured a variety of sessions on topics such as wrist fractures, fracture-related infection, periprosthetic fractures, as well as industry-led and trainee breakout sessions, making it another outstanding event.
The OTS continues to be active with the BOA and delivered another set of successful sessions this year. Special thanks to Jo Round and Beth Pincher for organising excellent revalidation sessions, which included collaborations with BSCOS and the BOA trauma group. We are also honoured to be invited back to the BOTA meeting, this year in Manchester, where Nate Ahearn will lead an esteemed faculty.

Keep an eye out later in the year for the launch of the newly revamped OTS website, which will feature a wealth of information on trauma fellowships, courses, conferences, intriguing case studies, and more. Remember, joining OTS as a full or associate member is still free!
We look forward to welcoming delegates to our 2025 meeting in Sheffield on 5th – 6th June. Look out for top tips on shoulder and hip fractures, medico-legal work, frailty and fragility, as well as a prominent



Photographs courtesy of Clockwork Medical





2024 BOA Congress Review
Hiro Tanaka, Honorary Secretary
The BOA Annual Congress is a special event in the calendar year for three reasons. Firstly, it is the one time where surgeons across all the specialties can professionally network and share their latest research and innovation. Secondly, it brings together the entire trauma and orthopaedic community, which includes the SAS/LED surgeons, residents and medical students. Finally, it is a celebration of the dedication and life-long achievements of our colleagues.
This year’s theme of ‘Recruit, Sustain and Retain’ was both a poignant reminder of the challenges facing the NHS as well as a call to arms to lead the changes necessary to protect the future of our profession and those who serve within it.
Between 17th – 20th September, over 3,000 delegates attended the Congress at the vibrant Birmingham ICC supported by 59 industry partners. The opening address by our President, Simon Hodkinson, set an inspiring, forward-looking tone, focusing upon the need to embrace changes in our professional practice as well as supporting our future colleagues through training and mentorship.
The superb speakers at the plenary sessions were a reminder that we have the support of our partners in the Royal College of Surgeons, Health Education England and the NHS England. The invited carousel presidents shared the opportunities and challenges of their training systems internationally. The

comparison of the US vs UK training systems outlined by the Presidential guest lecturer, Anne van Heist (Past President of the American Orthopaedic Association), leaves us with the question of whether we have the optimal training system for our residents.
The Howard Steel lecturer, John McFall, an orthopaedic surgeon, athlete and astronaut, reminds us that despite adversity, we can all achieve great things by pursuing our passion. The Robert Jones lecturer, Deborah Eastwood (Past President) gave a reflective and personal account of how our profession is changing.
There was a wealth of clinical updates in the revalidation sessions organised by the specialist societies and BOA Committees. As always, we were left with the burden of choice. The quality and number of free paper submissions continues to improve. Congratulations to Richard Holleyman who won Best of the Best, Sharan Sambhwani for E-poster, Kai Nie for the Robert Jones Essay prize and Andreas Conte for the Medical Student prize.
There were excellent opportunities for networking in the well-attended EDI, SAS/LED and leadership sessions. The medical students and BOTA sessions showcased the talents of the next generation and were as energetic as usual.
No one can predict the future but change is certain and there was a healthy
discussion in the ‘Question Time’ session about Physician’s Associates, an update on registries including MDOR/NCIP/PHIN, development of day surgery (BADS) and innovative treatments in cell therapies.
Our Friday sessions once again proved popular and included the Extended Clinical Team (ECT) meeting for the second time. The ECT sessions are catered for a wide variety of health care professionals including ACPs, SCPs and trauma co-ordinators and had an audience of over 90 delegates attending. The programme content was much stronger this year and included breakout sessions in the afternoon. Topics covered included clarifying roles and responsibilities of advanced roles within the ECT, logistics of setting up a new fracture clinic review service and upskilling SCPs and ACPs.
The BOA Congress is a testament to the collaboration of all the specialist and affiliated societies, the exceptional organisational skills of the BOA events team, the community spirit of our membership and the support of our industry partners to whom we are grateful.
Please join us next year in Liverpool and make British orthopaedics great.
Session recordings are available to all Congress registrants via the App or the BOA website (using the below QR code). n

Joint NJR/ORUK/RCS Eng Research Fellowship
Fellowship details
For orthopaedic trainees who wish to contribute to the analysis of data from the National Joint Registry and undertake a period of independent research into joint replacement.
One fellowship is available, worth up to £100,000 per annum, to start in 2025 for a two-year period.
Closing date for applications: 3 February 2025







New BOA Trustees ( 2025 – 2027)

Ajay Malviya
Ajay Malviya is a Consultant Orthopaedic Surgeon based in the North-East of England, working within the Northumbria Trust, where he specialise in hip preservation surgery. In addition to his clinical work, he is an active researcher and an FRCS Examiner. Over the past decade, Ajay has had the honour of serving on the BOA Education and Careers Committee in various roles, including as the UKITE lead and, most recently, as the Vice-Chair. He has been closely involved in the committee’s expansion and its efforts to introduce new initiatives aimed at enhancing education, training, and engagement. Through his commitment, he has seen the significant positive impact of UKITE on many trainees and the success of numerous orthopaedic surgeons across the country. This journey has been fulfilling, allowing Ajay to maintain a harmonious balance between his clinical duties and other pursuits.
Ajay’s advocacy for ensuring surgical quality and measuring outcomes remains steadfast. As the former Chair of the National Arthroplasty Hip Registry (NAHR), he takes great pride in having played a pivotal role in its evolution from a developing registry to a model of excellence at both national and international levels. While he holds traditional values dearly, he remains open to new ideas and suggestions.
As a member of the Council, Ajay would passionately advocate for the modernisation of orthopaedic training to make it a model of excellence that is exemplary to the rest of the world. Additionally, he believes that NHS organisations should support surgeons in improving quality by ensuring there are adequate resources to collect outcome data. Every trust in the UK should have an outcomes team dedicated to measuring surgical quality. n

Deepa Bose
Deepa Bose is a Consultant in Orthopaedic Trauma and Limb Reconstruction at the Queen Elizabeth Hospital Birmingham. Her practice is exclusively in adults, and includes general trauma, major trauma and post-traumatic limb reconstruction.
She is Chair of the Specialist Advisory Committee for Trauma and Orthopaedics in the UK, which advises on the curriculum and other matters pertaining to training.
She is the Past Chairman of World Orthopaedic Concern UK, a specialist society of the British Orthopaedic Association, which focuses on teaching orthopaedics in low resource countries.
She has been on the Emergency Response Team of UK Med, a first response team for international disaster relief, since 2012. She regularly participates in humanitarian projects in Guyana, Gaza and Ukraine.
Deepa decided to run for the BOA Council because she is passionate about safeguarding the future generation of orthopaedic surgeons. She hopes to achieve this by promoting the highest standard of education and training, both in the UK and in low and middle-income countries. She would also like to support UK orthopaedic surgeons who carry out humanitarian work n


Leela Biant
Leela is Academic Head of the department of Trauma and Orthopaedic Surgery at the University of Manchester and Honorary Consultant T&O Surgeon, Manchester University Hospitals. She is Co-Director of the Northwest Joint Preservation Centre, a King James IV Professor, and Immediate Past-President of BASK.
Leela trained in London with fellowships in Sydney and London. Her thesis was entitled ‘Articular Cartilage Injury and Repair in the Young Adult Knee’ and her award winning research focuses on biological regenerative surgery and advanced joint replacement. Leela is on the SAC of ORUK, an ICRS Senior Fellow, and founded the ICRS Global patient registry. She is a Lifetime Honorary Fellow of the UK Biological Knee Society, an ABC Travelling Fellow in 2010 and BASK Travelling Fellow in 2014. Leela has previously been on the Medical Advisory Committee of the NJR.
Leela stood for Council to try to improve the working lives and daily stressors of all colleagues in the NHS, Hybrid, Private and Academic Sectors. This includes the scrutiny of case numbers without clinical context, publishing of unverified data about a surgeons practice that they have no control of, and do not have the time nor the ability to alter, stifling bureaucracy, time-sapping untargeted email and communications so surgeons have ‘been informed’, and rising costs and indemnity cover of a practicing orthopaedic surgeon without parallel rises in remuneration. Our work is joyful and important. Our time is better spent looking after patients, training the next generation and advancing care with meaningful audit and research n
Peter Giannoudis
Professor Peter Giannoudis is the Professor and Chairman of Trauma and Orthopaedic Surgery at the Medical School of the University of Leeds.
He has served in positions of responsibility including, President of the British Trauma Society (2003-2007), President of the European Society of Pelvis and Acetabulum (2007-2012), President of the European Society Tissue Regeneration in Orthopaedics and Traumatology (2018-onwards), Chair of the International Committee of Orthopaedic Trauma Association (USA) (2012-2019), Chair Global Research Commission AO Foundation (2024-onwards), and Editor In Chief of Injury Journal (2010-onwards) and Journal Trauma Case Reports (2014-onwards). He has published over 800 peer review publications and 14 Orthopaedic and Trauma textbooks. His H-index is 131 with 64,745 citations.
Professor Giannoudis is a regular international keynote speaker having delivered over 450 lectures around the globe. He is a visiting professor in 21 Universities worldwide. In 2024, he was included in the King’s New Year’s Honours list and received the Most Excellent Order of the British Empire (MBE) for his services in trauma and orthopaedic surgery in the UK.
Peter is delighted to be elected as a Trustee of the BOA. He feels it is a great honour and is looking forward to contributing to the important challenges facing our profession including maintaining adequate workforce, supporting the training and education of our members, promoting high quality research, strengthening the relationship with the government to improve patient care and to raise the profile of the Association internationally. n
New BOA Trustees ( 2025 – 2027)

Rhidian Morgan-Jones
Rhidian trained in Cardiff at the University of Wales, College of Medicine as it was then, qualifying in 1989. His training rotation was between Oswestry and Stoke-on-Trent and included fellowships in Johannesburg and Sydney.
Rhidian has spent his Consultant career working on orthopaedic infection and revision knee replacements in Cardiff. He recently ‘transferred’ across the border to work in Colchester and help establish the Regional Revision Knee Network.
Rhidian has a strong interest in education at all levels and continues to lecture widely. He has had the pleasure of founding and running national knee infection meetings from which he continues to learn from his peers. A personal philosophy, when possible, has always been to organise cross-speciality meetings, which broadens one’s perspective and heightens respect for colleagues in other medical and non-medical areas.
Now living in Essex, he remains as Welsh as ever but perhaps a little less partisan than before. Professionally and personally, although life continually changes, he could not be happier than at present.
Rhidian is delighted to be re-elected as a BOA Trustee and hopes to contribute and support our profession in any way he can n

Sebastian Dawson-Bowling
Sebastian Dawson-Bowling is a hip and knee surgeon at Barts Health in London, specialising in complex primary and revision arthroplasty. He also undertakes arthroscopy to both joints, and works within the Royal London Hospital major trauma service. Sebastian is a BJ360 Editorial Board member, sits on the NJR Regional Clinical Coordinator and Editorial Committees, and is an FRCS(Tr&Orth) examiner.
Outside clinical practice, his passion within orthopaedics has always been training/mentoring future generations. Whilst BOTA President, Sebastian strongly encouraged medical student attendance and participation at orthopaedic educational events. He subsequently cofounded London Undergraduate Orthopaedic Society, and contributed to establishing BOMSA.
Away from work, Sebastian’s loves in life are his family (wife Emma, a psychiatrist, and children Elspeth and Daniel), opera, food and wine. He is also a qualified rowing umpire.
Sebastian is honoured to be elected to BOA Council. The BOA now has perhaps more influence than at any previous time, which he feels we can use to powerful effect, ensuring the right training and working conditions for members at all career stages – from those caring for young families, or sitting exams (or both!); to consultants fighting to defend standards of care for their patients against increasing management interference; or seeking to undertake leadership or educational roles.
He looks forward to contributing to the Association’s excellent work to guide, support and safeguard trainees; it has been with this foremost in mind that he stood. In doing this, the BOA will continue simultaneously to ensure highest possible standards of patient care for generations to come n
Reduces pain and increases mobility
medi soft OA light knee brace
osteoarthritis off-loading knee brace now available on prescription. 2 0 2 4 B O A A N N U A L










Conference Listing 2025:
BOFAS (British Orthopaedic Foot & Ankle Society) www.bofas.org.uk
29-31 January 2025, Brighton
BHS (British Hip Society) www.britishhipsociety.com 5-6 March 2025, Harrogate
BRITSPINE
www.BritSpine.com 12-14 March 2025, Manchester
BSCOS (British Society for Children’s Orthopaedic Surgery) www.bscos.org.uk 13-14 March 2025, Brighton
BLRS (British Limb Reconstruction Society) www.blrs.org.uk
27-28 March 2025, Newcastle
BSSH (British Society for Surgery of the Hand) www.bssh.ac.uk
23-25 April 2025, Majorca
BASK (British Association for Surgery of the Knee) www.bask.ac.uk
29-30 April 2025, Harrogate







We specialise in casing and packaging solutions for orthopaedic implants, medical equipment and have supplied many of the world’s leading medical organisations.
We specialise in casing and packaging solutions for orthopaedic implants, medical equipment and have supplied many of the world’s leading medical organisations.
Our flight cases are made in our 70,000 sq ft factory in the UK using the highest quality materials to ensure that your vital
Our flight cases are made in our 70,000 sq ft factory in the UK using the highest quality materials to ensure that your vital equipment is fully protected in transit.


Orthopaedic Trauma Society (OTS) www.orthopaedictrauma.org.uk
5-6 June 2025, Sheffield
BAJIS (Bone and Joint Infection Society) https://bajis.org
19-20 June 2025, Coventry
BIOS (British Indian Orthopaedic Society) https://britishindianorthopaedicsociety.org.uk
10-21 June 2025, Grantham
BESS (British Elbow and Shoulder Society) https://bess.ac.uk
25-27 June 2025, Brighton
BORS (The British Orthopaedic Research Society) https://borsoc.org.uk
8-9 September 2025, Birmingham
BOA (British Orthopaedic Association) www.boa.ac.uk
16-19 September 2025, Liverpool
equipment is fully protected in transit. We design and manufacture cases to your exact specification. A range of pull-out drawers, shelves, lift-out trays, doors and shutters can be integrated into the case. With an in-house design team and advanced computer aided design and CNC routing facilities, we can produce custom foam interiors to
house implant samples, instruments and any other equipment.
Trifibre Ltd 17 Boston Rpad
Gorse Hill Industrial Estate Leicester LE4 1AW
We design and manufacture cases to your exact specification. A range of pull-out drawers, shelves, lift-out trays, doors and shutters can be integrated into the case. With an in-house design team and advanced computer aided design and CNC routing facilities, we can produce custom foam interiors to house implant samples, instruments and any other equipment.
Telephone: 0116 232 3166
Email us: info@trifibre.co.uk Web: www.trifibre.co.uk
Trifibre Ltd 17 Boston Rpad
Gorse Hill Industrial Estate Leicester LE4 1AW
Telephone: 0116 232 3166
Email us: info@trifibre.co.uk
Web: www.trifibre.co.uk




Download the App


The Journal of Trauma and Orthopaedics (JTO) is the official publication of the British Orthopaedic Association (BOA). It is the only publication that reaches T&O surgeons throughout the UK and every BOA member worldwide. The journal is also now available to everyone around the world via the JTO App. Read the latest issue and past issues on the go, with an advanced search function to enable easy access to all content. Available at the Apple App Store and Google Play – search for JTO @ BOA
Joint Action Update
Joint Action - The Orthopaedic Research Appeal of the BOA
Research into trauma and orthopaedics has never been more important with one-third of the population being affected by or living with a musculoskeletal condition. If you are looking for an efficient and hassle-free way to support Joint Action, why not consider donating through your payroll! Payroll Giving is a way of giving money to charity without paying tax on it!!
Find out more about donating through your salary at: www.boa.ac.uk/ways-to-donate and more information on Joint Action and the clinical trials we are currently funding is at: www.boa.ac.uk/clinical-trials.
2025 TCS London Marathon
The 2025 TCS London Marathon is being held on


Help us build a stronger clinical research network in trauma and orthopaedics (T&O) across the UK Through our Joint Action Appeal, every donation directly funds essential clinical trials, research fellowships, and training for the next generation of surgeons all to improve patient care
In 2024, we proudly supported the Exeter and Nottingham Trials Units and partnered with ORUK to fund high-quality surgical fellowships With your help, we can do even more.
Donate today to support research that transforms care in T&O surgery.

www.justgiving.com/campaign/jawinterappeal2024

National selection to T&O ST3 posts – An update
Lucky Jeyaseelan and Cronan Kerin on behalf of the Selection Design Group

Lucky Jeyaseelan is a Consultant Trauma & Orthopaedic Foot & Ankle Surgeon at Barts Bone & Joint Health, Barts Health NHS Trust, where he is Clinical Lead for Elective Orthopaedics at the Barts Health Orthopaedic Centre. He is a member of the Selection Design Group for ST3 National Selection and a Liaison Member for the Specialty Advisory Committee (SAC) for Trauma & Orthopaedics.

Cronan Kerin is a Consultant Knee and Trauma Surgeon at Liverpool University Hospitals. He is also Chair of the Selection Design Group & National Selection Lead, T&O SAC. He was the Training Programme Director for Trauma & Orthopaedics for the Mersey Deanery from 2018 to 2023.Programme.
Since 2013, trainees in England and Scotland have gained a National Training Number in Trauma and Orthopaedics at ST3 level through a central process. The purpose of this article is to provide an update on this process since the last article published in JTO in June 2021. The Selection Design Group (SDG) is made up of senior consultants, current and previous Training Programme Directors, SAC members and representatives of the British Orthopaedic Trainees Association (BOTA) all of whom are experienced in many aspects of training and education. The collective aim is to ensure the best potential registrars are chosen to enter higher surgical training.
The SDG convenes several times a year to scrutinise the most recent process using data released by Medical & Dental Recruitment and Selection (MDRS) group, a body responsible to the Statutory Education Bodies (SEBs), and to improve the design of the following year’s process. We then implement delivery of the process used to select T&O ST3s in England and Scotland. The last two recruitment cycles have been led by Cronan Kerin, who took over as Chair from Mark Crowther. We continue to build on his hard work and that of his predecessors David Large and James Hunter.
The remit of the SDG is to develop the selection criteria, ensuring that these criteria used to assess candidates align with the skills and qualities needed in T&O. We also review the assessment methods, evaluating the effectiveness and fairness of the assessment, and implementing measures to ensure that the selection process is equitable and that all candidates are assessed in an unbiased and objective manner.
When the COVID-19 pandemic struck in early 2020, Medical and Dental Recruitment and Selection (MDRS) declared that there would be no face-to-face interviews for any medical specialty. Since that point, the
recruitment process has remained an entirely virtual process. MDRS are committed to reinvesting the cost saving into improving the functionality of the Qpercom computer software that is used for the interview process. Since then, we have seen continual development and improvement in both process and assessment modalities.
The recruitment process
The recruitment process begins in November, with all candidates required to submit evidence which covers several domains with their portfolios. This is an online process and covers domains which are validated against this evidence. This evidence is assessed by members of the SDG, Training Programme Directors, and members of the Specialist Advisory Committee (SAC). The top scoring 360 candidates are subsequently shortlisted for interview, which takes place virtually around March/April the following year.
An additional question has been added to the Self-Assessment form for the current 2024/25 cycle, asking candidates to confirm that they will provide the evidence to support their responses to these questions in an organised manner and as specified in the written instructions – an attempt to encourage candidates to submit more clear and structured evidence for the verification process. This has been driven by the complexities of reviewing poorly structured or excessive evidence submission during the validation process.
The use of the ‘N’ number continues, ensuring that core trainees are not disadvantaged in open competition against the cohort of other doctors who have had many years of ‘experience’ and thus more time to develop aspects of their portfolio.
The interview itself is made up of four stations, each assessed independently by two interviewers. These are:
• Commitment to specialty Candidates are interviewed about elements of their career and experience to date. They are assessed in each of the following domains: Career Motivation, Learning and Development; Leadership and Team Involvement; Organisation and Planning; Communication – Information Giving; Academic.
• Clinical
This station is based on clinical scenario. Assessment is in each of the following domains: Technical Knowledge; Problem Solving and Decision Making; Situational Awareness; Communication – Information Gathering; Communication –Information Giving. Anatomy and clinical knowledge is tested through clinical scenarios.
• Prioritisation
This station is an exercise in which the candidate must demonstrate judgement and reasoning in the setting of a scenario requiring prioritisation of care provision. Interviewers score in each of the following domains: Organisation and Planning; Communication – Information Gathering; Communication – Information Giving; Judgement under Pressure; Situational Awareness.
• Communication
This station is based on a scenario involving communication with a patient, with interviewers scoring in each of the following domains: Technical Knowledge; Situational Awareness; Judgement under Pressure; Communication – Information Gathering; Communication – Information Giving.
Each candidate must score a minimum 3:25 to be deemed appointable. To date we have had clear headroom between this minimum appointable level and the number of posts available.
National selection data
Each year of the selection process generates data that is analysed to enable us to understand patterns of application and recruitment through the National Selection process. This data is made generally available shortly after the completion of each recruitment cycle.
Table 1 shows general application information since the 2019/20 process. Application numbers and competition ratios have remained largely static during this time, with the fluctuance in national training numbers offered each year depending on the number of training posts vacated by those trainees achieving CCT. National training numbers by region (excluding Scottish LAT positions) are shown in Table 2.
Gender application numbers and average interview score trends are shown in Figure 1. It should be noted that a significant number of applicants chose not to state gender and as such, this will lead to a degree of bias in interpreting the data. Based on the information we have, female candidates score consistently higher on average than their male counterparts. Figure 2 shows gender trends in those who were successfully appointed to a national training number. After a consistent two years at just below 20% of successful candidates being female, 2023/24 sees a small drop.
Ethnicity data for candidates both applying and appointed in the 2023/24 recruitment process is shown in Table 3. >>

Table 1: Application and recruitment patterns in ST3 T&O National Selection since 2019/20.
Table 2: National Training Numbers (NTNs) by region since 2020/21.
Figure 1: Gender application and average interview score trends since 2020/21.


The future
Despite the underlying desire by many to go back to a face-to-face interviews, the MDRS have expressed their intention for the virtual format to continue for the foreseeable future. As the recruitment process continues to evolve, our role continues in ensuring appropriate format design that reflects the training syllabus and what is expected of those entering higher specialty training. In doing so, we continue to ensure equality of opportunity throughout the process. The full functionality of the Qpercom software used to deliver the virtual interviews, equally evolves. The aim is to use this as a single platform to comprehensively cover the recruitment process from start to finish.



Figure 2: Gender trends and interview scores averages in those who were successfully appointed.
3: Ethnicity data for the 2023/24 recruitment process.
2023/24
2022/23
2021/22
Figure 3: Average Self-Assessment scores of those candidates that were interviewed since 2021/22.


For the future interview cycles, the most notable changes will include increasing the number of neck of femur cases to score full self-assessment marks from 12 to 18 cases, from the 2025/26 recruitment cycle. The Communication station, re-introduced in the 2023/34 cycle, appears to be a solid addition to the interview process and is set to continue.


Information for candidates applying for ST3 National Selection can be found on the Yorkshire & Humber Deanery website (www.yorksandhumberdeanery.nhs.uk/ recruitment/national_recruitment), where the 2024/25 Applicant Handbook is available, as well as scoring guidance information and timelines.
We believe that the current format of the recruitment process is versatile and gives the opportunity for top-level candidates to excel. It works to differentiate candidates well and as such, has proven to be an excellent modality for selecting the very best candidates to commence higher speciality training. n

Figure 5: Total final score ranges achieved by all interviewed candidates in the 2023/24 interview process.
Figure 4: Range of scores achieved at each station of the interview in the 2023/24 recruitment process.
Noise-induced hearing loss in orthopaedic surgery: Are we at risk?
Jerry Sam and Hiro Tanaka

Jerry Sam is an orthopaedic surgeon trained at one of the leading tertiary referral trauma centres in South India. He has significant experience working in low-resource settings, handling trauma cases with innovative approaches. He currently works as a Speciality doctor in Trauma and Orthopaedics at Grange University Hospital, South Wales.

Noise-induced hearing loss (NIHL) is an increasingly recognised occupational health risk across many industries, but its presence in healthcare, specifically in orthopaedic surgery, remains underappreciated. The orthopaedic operating theatre can be a high noise environment with the sound of specific tools and devices reaching levels of 90-140 dB. Prolonged exposure over the course of a career presents a significant risk to surgeons and theatre staff. In this article, we move forward in our series towards creating the safest possible work environment. We will explore the impact of noise on healthcare workers, the Health and Safety Regulations, the various factors contributing to noise levels in orthopaedic surgery, and potential preventive strategies to mitigate risk.
Why is it important?
The National Institute on Deafness and Other Communication Disorders (NIDOCD) estimates that approximately 15% of Americans between the ages of 20 and 69 experience hearing loss that may have been caused by exposure to noise at work or leisure activities. The risk of NIHL among senior orthopaedic surgeons neared 50% in a study conducted by Willetts and appeared to be dose related1
Professional and personal impact of NIHL
1. Impaired communication: One of the most immediate consequences of hearing loss is difficulty in communication. The first symptom of NIHL may be difficulty hearing a conversation against a noisy background. This occurs due to a perceived reduction in volume as well as loss of clarity due to high frequency loss. In the operating room, where clear, precise, and timely communication is essential for patient safety, even minor hearing impairment can lead to misunderstandings or delays in responding to critical situations.
2. Increased stress and fatigue: Noise exposure, even without hearing loss, is associated with increased cognitive load, stress and fatigue. Healthcare professionals working in noisy environments may experience reduced concentration, leading to errors or inefficiencies during surgery.
3. Quality of life: Outside the professional environment, NIHL can significantly affect quality of life due to impaired social interactions leading to feelings of isolation. Tinnitus, for example can lead to difficulty sleeping, anxiety and depression.
Hiro Tanaka is a Consultant Foot & Ankle Surgeon, Aneurin Bevan Local Health Board. He is the BOA Honorary Secretary, a member of the BOA Education and Careers Committee and co-directs the BOA Future Leaders Programme.

Key terminologies
Noise is typically measured on the logarithmic Decibel (dB) scale, which means that a noise level of 100 dB has 10 times as much sound energy as one of 90 dB. A 10 dB increase makes the sound twice as loud. In order to improve the sensitivity of the sound perceived by the human ear, modern measurement devices incorporate an A-weighting dB(A) which decreases sensitivity to low and high frequencies. Typical levels of noise from daily activities can be seen in Table 1. It is important to note that a single loud noise above 120 dB may cause immediate and permanent hearing loss.
The Time Weighted Average (TWA) shows a worker’s daily exposure to occupational noise normalised to an eight-hour day and takes into account the duration and amplitude of sound exposure. It can also be calculated from the dose percentage detected by a dosimeter.
The Occupational Safety and Health Administration (OSHA) states that an eight-hour time-weighted average exposure of 85 dB(A) or a peak exposure of 140 dB represents the threshold for safe exposure.
A 40 year exposure to 85 dB(A) per eighthour working day carries a 35% risk of NIHL amongst exposed workers. This increases to 51% with a 90 dB(A) exposure2
Health and Safety Regulations
The European Commission Directive 2003 on noise at work and the current Control of Noise at Work Regulations 2005 define threshold levels for noise exposure and aims to reduce the risk to staff to as low a level as reasonably practicable3. Action should be taken where noise exposure is likely to be at, or above any of the three action levels given in Table 2.
Should any work, following a risk assessment or noise survey breach the above levels then the following actions should be undertaken:
LEAV: Employees will be notified and advised of the risk from noise.
UEAV: These areas will be designated as Hearing Protection Zones and only authorised staff, equipped with the appropriate hearing protection may work in those areas.
ELV: Immediate action must be undertaken to reduce exposure to noise.
What is the current evidence?
Several studies have demonstrated that a number of orthopaedic instruments would exceed the threshold for sensorineural damage with prolonged exposure. A systemic review of 14 papers by Mistry et al. concluded that 61% of orthopaedic operations and 70% of instruments exceeded the A-weighted noise regulations and 22% of operations exceeded the peak C-weighted acceptable noise levels4 Kwan et al., identified that the highest risk procedure was microdiscectomy followed by hip and knee arthroplasty5 >>

Love et al. demonstrated that average noise levels could exceed 80 dB(A) in hip and knee arthroplasty with peak noise values of 140 dB6. There is significant variation in the noise levels emitted from different instruments with the reciprocating saw producing the highest average and peak levels7
Due to the variation in surgical practice and exposure to instruments, the precise risk to orthopaedic surgeons cannot be determined. However, the evidence is clear that the instruments commonly used in orthopaedic surgery frequently exceed safety levels and potentially poses a risk to health.
Siverdeen et al. recommended that all patients especially the elderly as well as theatre staff should take precautions in procedures involving high-powered tools8
Preventative strategies to reduce NIHL
Given the significant risk of NIHL in the orthopaedic theatre, preventative strategies are essential to protect the hearing of surgeons and staff. These strategies can be divided into engineering controls, administrative controls and personal protective equipment (PPE).
1. Engineering controls
• Noise-reducing tools. Modern electric drills and saws can be engineered with noisedampening features and produce less noise than old-fashioned pneumatic instruments.
• Soundproofing. Soundproofing materials, such as acoustic panels or noise absorbing flooring, can help dampen the reverberation of sound, reducing overall noise level.
2. Administrative controls
• Risk assessment and noise monitoring. Regular monitoring using dosimeters can help identify where and who is at risk. By understanding the noise profile of different operations, targeted interventions can be implemented to reduce noise exposure.
3. Personal protective equipment
• Hearing protection. Although earplugs or earmuffs are an effective way to reduce exposure, they pose problems with communication and are not a practical solution. Custom-fitted earplugs can however, filter out harmful noise frequencies while allowing for speech intelligibility.
• Distance. Willets demonstrated that 95-100 dB(A) from an oscillating saw at 45cm decreases to 88 dB(A) at 3m.
Conclusion and key learning points
• Noise-induced hearing loss is an under-recognised occupational hazard in orthopaedic surgery.
• High frequency hearing loss affects communication, which can affect professional performance and social interactions.
• The impact of hearing loss is cumulative over a career and surgeons should be aware of safe threshold limits.
• A significant proportion of power tools will generate noise levels, which may exceed safe limits depending upon time exposure.
• By taking proactive steps to reduce noise exposure, the healthcare industry can safeguard the hearing of its workers, ensuring a healthier and more sustainable working environment. n
Scan the QR code to take part in our survey and help us reduce hearing loss in orthopaedic surgeons.

References
1. Willett KM. Noise-induced hearing loss in orthopaedic staff. J Bone Joint Surg Br. 1991;73(1):113-5.
2. Gates GA, Cobb JL, Linn RT, et al. Central auditory dysfunction, cognitive dysfunction, and dementia in older people. Arch Otolaryngol Head Neck Surg. 1996;122(2):161-7.
3. The Control of Noise At Work Regulations 2005, Health and Safety Executive UK. Available at: www.legislation.gov.uk/ uksi/2005/1643/pdfs/uksi_20051643_ en.pdf
4. Mistry D, Ahmed U, Aujla R, et al. The relationship between exposure to noise and hearing loss in orthopaedics. Bone Joint J. 2023;105-B(6):602-9.
5. Kwan SA, Lynch JC, DeFrance M, et al. Risk of Noise-Induced Hearing Loss for Orthopaedic Surgeons. J Bone Joint Surg Am. 2022;104(23):2053-8.
6. Love H. Noise exposure in the orthopaedic operating theatre: a significant health hazard. ANZ J Surg. 2003;73(10):836-8.
7. Butt DA, Hadjipavlou M, Walcrak J. A noise at work assessment in the orthopaedic operating theatre. Bulletin of the Royal College of Surgeons of England. 2014;96(1):32-4.
8. S Siverdeen Z, Ali A, Lakdawala AS, McKay C. Exposure to noise in orthopaedic theatres--do we need protection? Int J Clin Pract. 2008;62(11):1720-2.

Rent a CPM from £200 for two weeks
Your patients can now enjoy flexible CPM rental times! With our quick, simple booking and rental extensions, they can simply choose an additional week or two and they’re all set.
CPM machine options: Knee Shoulder Ankle Elbow

Rent a Cryo Pro™ from £150 for two weeks
Our cold compression therapy device, the Cryo Pro™, is available to rent and upgrade to purchase. Included is the unit, a wrap of your choice, next day delivery & collection.

03330 347400 (ext 1) enquiries@kinetecuk.com www.kinetecuk.com


Wide awake local anaesthetic no tourniquet (WALANT) hand surgery in a community setting
eight years experience

Ashita Paul worked as a Junior Clinical Fellow at the Queen Elizabeth Hospital in Gateshead. She is currently working as an Orthopaedic Research Fellow at St George’s Hospital and is aiming to be a specialist trainee in trauma and orthopaedics.

The WALANT (Wide awake local anaesthetic no tourniquet) technique is an alternative to the regular surgical pathways, and bypasses the need for traditional theatre working with high staffing levels, and complex hospital pathways. The technique has been implemented for many distal extremity surgeries including in the hand, carpal tunnel decompression, Dupuytren’s contracture release, trigger finger release, ganglion excision, tendon repair and transfers, and distal radius fracture fixation.
The WALANT technique uses large volume local anaesthetic and local vasoconstrictive agents to attain a good field block and relatively bloodless surgical field. The technique avoids tourniquet pain, long fasting periods, and the need for peri-operative cannulation and monitoring. The patient can continue to be on their regular medicines and continue their day-to-day life without much disruption as the recovery time is often shorter than with traditional anaesthetic techniques. The technique is cost-effective and inexpensive in comparison with traditional surgery with studies suggesting similar outcomes and complication rates1
Inception
The Cumbria Hand Surgery Service was setup in 2016 as a collaboration between the Gateshead Health NHS Trust and Cumbria Medical Services. The aim was to provide a patient centred service outside of a hospital setting. Cumbria has a large geographical area with patients often travelling long distances, and significant pressures on local hospitals with long waiting times for assessment and treatment of hand conditions.
Referrals into the clinic are screened and limited to five conditions: Dupuytren’s contracture, trigger finger release, cubital tunnel syndrome, finger ganglia / swellings, and De Quervain’s tenosynovitis. The WALANT technique has a significant learning curve. We visited Probus Surgical Centre in Cornwall (www.probussurgicalcentre.co.uk ) who at that time were doing WALANT Dupuytren’s surgery. We then practised the technique on elective lists in the hospital setting and once confident started in the community.
The referrals received are from the local MSK service and direct from GPs. A good working relationship with these services, including the provision of education sessions, has meant high quality referrals to the clinic. A healthcare centre setting helps avoid a lot of the logistical issues seen with hospitals such as poor parking provision, confusing signage for departments and having to speak to several different staff as part of each visit who are often not directly part of the patient’s care. The clinic is based in South Carlisle with good access to major roads.
There are three staff (surgeon and two scrub), and patients meet the same team at each visit. We use 1% lignocaine and 1:200000 adrenaline +- 0.084% bicarbonate (1ml per 10mls LA). Antibiotics are not used. Single gloves are worn, with gowns only for more complex Dupuytren’s cases (Figure 1). There are 5-7 cases per list and the majority are Dupuytren’s surgeries.
The afternoon clinic will typically have 10 new patients at 10-minute intervals. Routine investigations such as X-ray and ultrasound imaging, and nerve conduction studies are usually requested as part of the screening
Ashita Paul, Jagannath Chakravarthy, Martin White and John Harrison
Jagannath Chakravarthy is an upper limb surgeon at Queen Elizabeth Hospital, Gateshead, specialising in shoulder surgery with a particular interest in WALANT surgery.

Martin White specialises in walk-in walk-out surgery across a range of specialties including hand surgery, hernia surgery and skin cancer/ plastic surgery. He has developed these services in Cumbria working alongside like-minded colleagues over the last 15 years.

John Harrison specialises in surgery of the hand and wrist, and treatment of elite sportspeople. He is based in the North East of England. He has published extensively, and his interests include biomechanics, WALANT hand surgery and scaphoid non-union.

of referrals, and available for the clinic visit. If a surgery is agreed, they are given a date before leaving the clinic, so they can plan work, etc. The peri-operative management of any anticoagulant medication is arranged, and any allergies confirmed.
More recently, guidelines have been produced by the British Society for Surgery of the Hand (BSSH) for wide-awake surgery2. We generally follow these apart from their recommendations for theatre staffing as our theatre staff admit and
discharge patients. The increased interest in WALANT surgery has been at least partly due to COVID-19.
Present review
The hand surgery clinic currently runs two to three sessions every month with a theatre list in the morning followed by an afternoon clinic session. 1,691 new patients have been seen, and 1,046 operations performed (see Table 1). >>
Figure 1

In 2016, we had a conversion rate of 59.85%, which has now increased to 76.39% in 2023. The service remains efficient with a four week waiting time for the clinic appointment, and four to six-weeks for the surgery. This efficient process was maintained through the COVID-19 period and could be expected to do so in any further events. We have had few complications such as wound healing delay, and incomplete correction of contractures, but no deep infections.
Our cost analysis of 30 consecutive fasciectomy patients in 20203 demonstrated that we were able to save over £900 per Dupuytren’s case when we compared the costs for the same surgery being performed in community vs. hospital (£184.97 vs. £1052.74). It should be noted the main savings highlighted were theatre cost (£722), and staffing (£244.79), and these figures do not include the cost of the anaesthetic consumables. Healthcare generates a huge quantity of landfill waste, and by the use of smaller drapes, no gowns, and no anaesthetic equipment, drugs or monitoring, we generated significantly less waste per case (Figure 2). Patients do not change into a hospital gown and stay in their own clothing during the procedure. We e-consent so no paper consenting forms are generated.
Post-operatively the majority of patients are managed with an advice leaflet and GP practice nurse for suture removal. Physiotherapy is not routinely organised but does occur if it is
felt necessary at the time of surgery or if the patient re-contacts the team with movement difficulties. As a result of the low follow-up appointment rate, we achieve a high new patient to follow-up ratio.
Patient satisfaction has been high agreeing with published studies4. We have received an average of 33 feedback questionnaires annually (range 17-65). These generally demonstrate excellent feedback.
Future plans
We have carried out new patient video clinics using Accurx Software (www.accurx.com). Our patients are often older and have restricted mobility and this decreases the travel time and inconvenience related to traditional hospital consultations. One-stop clinics for carpal tunnel surgery occur in a pathway separate to our clinic, and we aim to achieve a similar pathway for pre-tendinous cord Dupuytren’s patients.
Conclusions
The Cumbria Hand Surgery service has run successfully for eight years and serves a large geographical area. We manage a high volume of work with a small team of three. We have had no serious complications or deep infection. There is a significant cost saving and this model of working may help to reduce waiting times for hand surgery nationally. We have adapted our working to reduce waste with measures
such as no patient gowns, a gownless scrub team, small drape packs, and paper-light with electronic notes and e-consenting.
Embracing new ways of working out of secondary care may lead to more simplified and economical pathways being developed, both to the benefit of patients and to help reduce the strain on valuable healthcare resources. n
References
1. Steiner MM, Calandruccio JH. Use of Wideawake Local Anesthesia No Tourniquet in Hand and Wrist Surgery. Orthop Clin North Am. 2018;49(1):63-8.
2. British Society for Surgery of the Hand (BSSH). Hand surgery: Guidelines for operating outside of main theatres. Available at: www.bssh.ac.uk/_userfiles/pages/files/ professionals/girft/girft-operating_outside_ theatres.pdf
3. Noureddine H, Vejsbjerg K, Harrop JE, White MJ, Chakravarthy J, Harrison JWK. Fasciectomy under local anaesthetic and adrenaline for Dupuytren’s contracture in a community setting in the UK with a cost analysis. Bone Joint J. 2020;102-B(10):1354-8.
4. Tan E, Bamberger HB, Saucedo J. Incorporating Office-Based Surgery Into Your Practice With WALANT. J Hand Surg Am 2020;45(10):977-81.
Figure 2

Metastatic bone disease and the development of local specialist networks in the UK
Ashley Scrimshire, Tom Beckingsale, Kenneth S Rankin and Kanishka Ghosh

Ashley Scrimshire is an ST8 T&O trainee in the North-East of England and a post-doctoral research fellow at the University of York. He has a keen interest in orthopaedic oncology, has previously led on implementing large-scale changes in the NHS and is a co-investigator on the PORTRAIT trial.

The incidence of cancer has increased by approximately 12% since the 1990s, with approximately 385,000 new cases each year in the UK1 Some of the most common types of cancer include breast, lung, prostate and renal. Along with thyroid cancer, these are also the types which commonly metastasise to long bones. Traditionally, once a patient develops symptomatic bone metastases their life expectancy was short, often measured in weeks to months, and functional demands were low. Thus, where surgery was indicated, implants such as intra-medullary nails would usually provide stability for long enough to outlive the patient and their systemic disease. However, treatment options for a wide range of cancers have dramatically improved over recent years. As a result, cancer survival has doubled in the past 40 years and there will be an estimated four million people living with cancer in the UK by 2035.
The presence of metastatic bone disease (MBD) at the time of a cancer diagnosis can be as high as 30%2. In addition, for those without MBD on presentation the cumulative annual incidence is estimated as 4.8% within one year, and 8.4% by ten years3, with a mean time from cancer diagnosis to developing bone metastases of 400 days. However, this varies substantially depending on the tumour type and stage, with prostate cancer being the highest risk (up to 70% at 10 years), followed by lung, renal and breast cancer.
Due to the higher number of cancer survivors and high rates of bony metastases, the overall prevalence of MBD is increasing. In addition, these patients are becoming increasingly complex, with higher functional demands and expectations. Studies have repeatedly shown that quality not just quantity of life is important to oncology patients. Combined, this means that traditional treatments, such as intra-medullary nailing, may no longer be durable enough to
outlast a significant proportion of these patients. Instead, more complex reconstructions, such as cement augmented fixation or endoprosthetic replacement, is often indicated to provide a reconstruction that will outlast the patient (Figure 1). In addition, it is important these cases are identified early as complication rates, length of stay and costs are significantly higher when MBD presents late, with a pathological fracture, compared to earlier prophylactic management4
Guidelines for management
As with any condition presenting to trauma and orthopaedic services the correct assessment, management and follow up of patients with MBD, with impending or complete pathological fracture, is essential. The British Orthopaedic Oncology Society (BOOS) and BOA standards for trauma and orthopaedics (BOAST) on the management of metastatic bone disease, set out the standard of care patients should receive5. Key elements of this guidance include the provision of a MBD lead in each unit, improved multi-disciplinary working, the development of pathways for prompt advice and referral, preoperative investigations and imaging, referral to a recognised tertiary MBD centre for solitary metastases (not always a primary bone sarcoma unit), follow-up and involvement of patients and their family/carers in decision making. Where indicated, surgical interventions should allow immediate weight-bearing and aim to outlast the lifetime of the patient. As outlined above, this means that traditional fixation techniques may require additional supplementation (i.e. with cement), and/or that alternative, more robust approaches to reconstruction may be required. In addition, these patients often have multiple co-morbidities and are frail. Recently published guidance commissioned by the Joint Collegiate Council for Oncology provides a useful benchmark for frailty assessment and holistic care for these patients6
Tom Beckingsale is a Consultant Orthopaedic Oncology Surgeon, Co-Chair North of England Bone and Soft Tissue Tumour Service and Lead for Paediatric Sarcoma Surgery at the Great North Children’s Hospital. He is also Co-Chair of the National Ewing’s Multidisciplinary Team Meeting.

Kenneth Rankin is a Consultant Orthopaedic Surgeon at Newcastle Upon Tyne Hospitals NHS Foundation Trust and Honorary Senior Lecturer at Newcastle University. He is the Chief investigator for the multi-centre NIHR EME funded SarcoSIGHT RCT and co-investigator on the NIHR HTA funded PORTRAIT RCT investigating post-operative radiotherapy following orthopaedic surgery for bone metastases.

Kanishka Ghosh is a Consultant Orthopaedic Oncology and Trauma Surgeon at Newcastle Hospitals NHS Foundation Trust. He is Lead for the North East of England Orthopaedic Oncology Network (NEON).

However, co-ordinating care and setting up pathways for these complex patients is challenging. A wide range of multi-disciplinary teams are often involved in their work up, management and postoperative rehabilitation. This may include oncology, radiology (including interventional radiology where pre-operative embolisation is required), surgical teams and specialist physiotherapists. A recent study that collected data from 84 UK orthopaedic units has shown that UK practice is highly variable and often falls short of the BOAST standards7
MBD networks
The rapid expansion of MBD and the associated complexity is quickly outstripping the capacity of the UK’s primary bone sarcoma units, to whom many of these cases are referred. This has led to the development of regional MBD networks, with a drive
towards regional management, in designated MBD units who have the appropriate MDT capabilities and expertise. The MBD network model follows a hub and spoke type design, with the development of regional MBD units who receive referrals from local Trusts, who are in turn supported by the primary bone sarcoma units for advice, support, or to take over care if appropriate (Figure 2). >>

Figure 1: An example case where a renal metastasis was embolised and nailed. However, the disease progressed around the nail ultimately leading to failure and revision to a total humerus replacement.
Figure 2: An example schematic for a regional metastatic bone disease hub and spoke network.
Features
There are however several barriers which have slowed the development of regional MBD centres in some areas. These include awareness of the issue, developing patient pathways, staff training and experience, funding, system resilience and new MDT working. The British Orthopaedic Oncology Society (BOOS) are actively engaging with surgeons and professional bodies to increase awareness of the burden of MBD and support regions setting up their networks. The past two BOOS conferences have included dedicated sessions, or more recently a whole day, for MBD. It is hoped this article will also go some way to increasing awareness. As for staff training and experience there are increasing numbers of ways this can be achieved, examples include visitations to primary bone sarcoma units, such as part of the Royal Orthopaedic Hospital’s educational offering, or newly developed post-CCT MBD fellowships.
Developing new patient pathways is often difficult and relies on dedication from a few key motivated individuals. However, collaborative working and sharing of ideas with other centres, including those that have successfully developed MBD pathways, networking at events such as the BOOS MBD conference, and working with industry partners can support the development and sustainability of local pathways.
billing teams to ensure appropriate coding and remuneration of multidisciplinary clinics, complex cases, and implant recharging, where appropriate, to limit costs to a department. The ongoing BOOM-C audit is studying the costs associated with MBD management and how these are currently managed.
MBD is also increasingly being recognised by bodies such as the National Joint registry. In collaboration with BOOS new MBD and endoprosthetic data collection forms are under development, to allow monitoring of these implants and outcomes. Alongside this, a new complexity classification system for MBD is also being developed.
and regional MBD networks, is challenging, but will lead to improved care and outcomes. Efforts from colleagues and societies to develop such pathways and networks should be supported by all of us. Our combined efforts here have the potential to make a significant positive impact on the quality of life and experience of our patients and their families, despite the complexity and life limiting nature of their disease. n
References
1. Cancer Research UK. Cancer Statistics for the UK. Available at: www.cancerresearchuk.org/healthprofessional/cancer-statistics-for-the-uk
“Collaborative working and sharing of ideas with other centres, including those that have successfully developed MBD pathways, networking at events such as the BOOS MBD conference, and working with industry partners can support the development and sustainability of local pathways.”
Research
Funding is often a concern when setting up MBD services. They require time for MDT preparation and discussion, theatre time and often expensive implants. One of the first steps to developing a new service and business cases is to understand the scale of the problem locally by collecting data on the incidence of MBD and the surgeries they receive. However, this is often difficult given the complexity of current, non-standardised pathways and variable modes of presentation. Furthermore, centres that have developed a MBD service typically find that once their service is set up the volume of referrals increases rapidly. Once services are developed it is important that time is appropriately job planned and resilience built into the system, so that if the one or two committed individuals can no longer run the service it doesn’t collapse. It is advised units work closely with their management, clinical coding and
In addition to setting out standards and raising awareness based on current literature, there are efforts under way to better understand and improve MBD patient care. This includes high quality research, such as the PORTRAIT randomised controlled trial. This trial will study the effectiveness of post-operative radiotherapy in surgically treated bone metastases8 and is due to start recruiting in 2025.
Summary
In summary, metastatic bone disease is a problem that is increasing in volume and complexity. As a community, we need to address this proactively, not reactively, or patients will suffer. As is the case across the spectrum of orthopaedic care we must strive to ensure these patients receive the most appropriate care and that, if surgery is recommended, we get it right first time. This should be delivered by appropriately experienced, multi-disciplinary teams, working to BOAST standards to ensure the best outcomes. The development of dedicated patient pathways
2. Jiang W, Rixiati Y, Zhao B, et al. Incidence, prevalence, and outcomes of systemic malignancy with bone metastases. J Orthop Surg (Hong Kong). 2020;28(2):2309499020915989.
3. Hernandez RK, Wade SW, Reich A, Pirolli M, Liede A, Lyman GH. Incidence of bone metastases in patients with solid tumors: analysis of oncology electronic medical records in the United States. BMC Cancer. 2018;18(1):44.
4. Mosher ZA, Patel H, Ewing MA, et al. Early Clinical and Economic Outcomes of Prophylactic and Acute Pathologic Fracture Treatment. J Oncol Pract. 2019;15(2):e132-e140.
5. British Orthopaedic Association. Available at: www.boa.ac.uk/resource/boast-managementof-metastatic-bone-disease.html
6. Royal College of Physicians. Implementing frailty assessment and management in oncology services. Available at: www.rcr.ac.uk/media/bwpmjnmz/ implementing-frailty-assessment-andmanagement-in-oncology-services.pdf
7. Archer JE, Chauhan GS, Dewan V, et al. The British Orthopaedic Oncology Management (BOOM) audit. Bone Joint J. 2023;105B(10):1115-22.
8. The National Institute for Health and Care Research (NIHR). The PORTRAIT trial Post-operative radiotherapy in surgically treated bone metastases. Available at: www.dev.fundingawards.nihr.ac.uk/award/ NIHR159676


ċ
ċ

Seeing the future digitally: Computer vision in trauma and orthopaedics
Ali Ridha and Aditya Vijay

Ali Ridha is currently an Orthopaedic research fellow at the South West London Elective Orthopaedic Centre (SWLEOC) where he is involved in projects involving Artificial intelligence in Orthopaedics. He is also an honorary research fellow at the University of Warwick.

Aditya Vijay is currently an orthopaedic research fellow at South West London Elective Orthopaedic Centre (SWLEOC) where he is involved in AI projects in Orthopaedics, focussing mainly on predictive analytics and computer vision.
Artificial intelligence (AI) has significantly advanced since its theoretical roots in the 1940s, evolving from simple shape and pattern recognition to handling complex visual and language tasks1,2
The development of deep learning, especially following a landmark achievement in the 2012 ImageNet competition, propelled AI applications into realms previously dominated by human cognition, such as image recognition and analysis3. This breakthrough fostered the growth of computer vision (CV), a branch of AI that enables machines to interpret and analyse visual data in ways that can support or even exceed human capabilities in specific tasks.
In trauma and orthopaedics, CV is showing promise, but it remains relatively new. Tools like BoneView™ are helping clinicians by identifying fractures on X-rays, while technologies like VERASENSE™ assist in realtime alignment of implants during surgery4 Although these tools highlight what’s possible, CV’s routine use in orthopaedic practice is only just starting to take hold5,6. Interest in CV is growing, fuelled by an ever-increasing volume of healthcare data. Patient imaging, surgical records, and electronic health data all contribute to a rich pool of information that can train and refine these AI models5
As CV becomes more integrated into clinical practice, we must address critical hurdles related to data privacy, availability, and safety to ensure the technology’s safe and effective use. With new draft NICE Guidelines recommending the use of AI for fracture detection in urgent care7, orthopaedics stands at the brink of an AI transformation. The prospect of CV integrated into day-to-day orthopaedic workflows hints at a future where musculoskeletal care becomes more efficient and precise, helping clinicians make faster, data-driven decisions that ultimately improve patient outcomes6,8
Why AI and computer vision?
In orthopaedic surgery, variability in how surgeons interpret fractures is a well-known issue. Human bias contributes to inconsistencies in fracture recognition and classification across trauma cases, affecting injuries from both upper and lower limbs9,10. However, recent advancements in AI, particularly in CV, offer potential to enhance both the speed and reliability of these assessments, providing tools that can standardise diagnostic accuracy and mitigate subjective variability5
CV’s underlying technology—complex neural networks—makes it particularly suited for medical image processing11,12. Unlike conventional machine learning (ML) models like decision trees or support vector machines, CV relies on deep neural networks that use convolutional layers, allowing the model to identify and respond to local spatial and temporal patterns in images11,12 These convolutional layers, particularly in Convolutional Neural Networks (CNNs), perform filtering operations that recognise edges, shapes, and textures, making them ideal for analysing intricate features in radiographs and CT scans5,13. This architecture enables CV models to efficiently process massive volumes of image data while requiring fewer computational resources. Rather than replacing human judgment, CV functions to support surgeons and radiologists by providing consistent, bias-reduced insights and streamlining clinical decision-making5,6,13
Current applications of computer vision
In orthopaedics, CV models have shown promise for fracture detection and classification on radiographs and CT scans, offering enhanced accuracy and efficiency1,2. Other medical fields have seen similar benefits; for instance, clinicians are employing CV for mammogram analysis in early breast cancer detection, fundoscopy for
diagnosing papilledema, and CT imaging to identify intracerebral haemorrhages13. These applications streamline diagnostic workflows, allowing for timely and more accurate interventions.
At the Southwest London Elective Orthopaedic Centre (SWLEOC), an ML model has been designed to screen postoperative arthroplasty X-rays. The model generates heat maps overlaid on the images, visually highlighting areas of interest that it prioritises during analysis. This technique is called saliency mapping and not only aids in identifying potential postoperative issues, but also provides clinicians with a clearer understanding of the model’s interpretive process and supporting informed decision-making.

A wound assessment tool to streamline postoperative wound assessment in total knee arthroplasty (TKA) patients using computer vision is also currently being developed. This initiative aims to develop and validate a deep learning algorithm that categorises wounds. By leveraging labelled wound images and expert input, the algorithm aspires to provide a rapid, accurate assessment tool that aligns with clinical standards. The project’s ultimate goal is to empower patients with an accessible tool, allowing early intervention for wound complications while reducing the follow-up burden on healthcare professionals.
How does computer vision work?
Imagine teaching a child to identify a banana. By showing them bananas of different shapes, sizes, and colours, they eventually recognise a banana by focusing on essential features like its shape, curvature, and colour. Similarly, CV operates by ‘learning’ from numerous labelled images. A CV model is trained on extensive datasets containing annotated images (e.g., ‘fracture’ or ‘no fracture’), learning to identify the unique characteristics that define each category. This training allows CV systems to process visual information and ‘see’ in a way that can augment clinical diagnosis1,13
CV algorithms operate through several key technical stages:
1. Classification: The CV model sorts images into predefined classes, such as identifying an image as depicting a ‘fractured’ or ‘non-fractured’ bone. This process involves the model learning to detect patterns that distinguish between these classes, often relying on thousands to millions of labelled examples.
2. Object Detection: Beyond merely categorising an image, object detection identifies and locates specific objects or areas of interest within the image. For instance, the model may pinpoint the exact location of a fracture line within an X-ray.
3. Segmentation: Segmentation divides an image into multiple distinct segments or regions, enabling the model to isolate specific parts, such as bones or joint spaces in an orthopaedic X-ray.
4. Feature Extraction: This stage involves identifying key characteristics, such as edges, textures, or specific shapes, within an image that are relevant to the diagnosis. This extraction process allows the model to develop a nuanced understanding of the image, supporting clinical tasks like fracture detection or implant alignment.

Following training, the model undergoes a testing phase where its accuracy and generalisability are evaluated using a separate dataset. This testing helps ensure that the model performs reliably in real-world clinical applications13,14 For example, models developed to identify fractures in training images must demonstrate the same accuracy when applied to new images from different institutions or patient populations. This need for rigorous external validation and continuous refinement highlights the complexity of implementing CV in clinical settings. >>
Figure 1: CV model for evaluating post-arthroplasty images.
Features

As CV continues to evolve, so too does its potential to support orthopaedic care, particularly in trauma settings. CV’s ability to consistently and accurately interpret visual data could transform diagnosis, procedural planning, and post-operative monitoring. However, as promising as these tools are, additional clinical trials, regulatory oversight, and improvements in data quality and reporting standards will be necessary to ensure CV models perform reliably and safely across diverse clinical environments.
Future perspectives in orthopaedic computer vision
As computer vision (CV) continues to integrate into orthopaedic practice, its future holds substantial promise but is also met with critical challenges. While tools like BoneView™ and VERASENSE™ illustrate CV’s potential for fracture detection and surgical alignment13, broader applications require scalable data solutions, advanced multi-tasking capabilities, and regulatory advancements to maximise CV’s clinical impact.
Manual video labelling, especially for complex procedures like arthroplasty or fracture reduction, demands significant time and resources, limiting scalability14,15. Interactive and semi-automatic labelling tools are emerging as viable solutions, enabling trained novices to label surgical videos with accuracy comparable to specialists13–15. Applying these methods in orthopaedics could accelerate data generation, supporting more robust model training without overwhelming clinical teams.
accurate, generalisable algorithms, yet most training data is sourced from single institutions. This localism limits the broader applicability of models and raises challenges for external validation, especially given the logistical and privacy constraints associated with sharing sensitive patient data like X-rays across institutions.
Federated learning offers a potential solution to these data limitations. By allowing institutions to collaboratively train a shared model without exchanging raw data, federated learning enables hospitals to maintain patient privacy while contributing to a collective, diversified dataset16,17. For example, hospitals across regions can train a CV model on local orthopaedic X-ray images to identify fractures or assess joint degeneration. Rather than transferring sensitive images, each institution shares only model updates — patterns learned from local data — back to a central server, thereby enhancing accuracy and generalisability without compromising patient confidentiality.
Future CV models will need multi-tasking capabilities to handle various orthopaedic conditions — fractures, joint dislocations, and soft tissue injuries — instead of focusing on isolated tasks. Although CNNs have shown strong performance in fracture detection, challenges remain in identifying subtle or occult fractures, such as scaphoid fractures, where CV models struggle to surpass the accuracy of experienced orthopaedic surgeons18. Prospective trials and multi-centre validation studies are essential to ensure that these models are reliable and generalisable across diverse patient populations and clinical environments.
“Future CV models will need multi-tasking capabilities to handle various orthopaedic conditions — fractures, joint dislocations, and soft tissue injuries — instead of focusing on isolated tasks.”
One of the foremost challenges to CV adoption in orthopaedics is the availability and diversity of large-scale annotated datasets.
Despite these advancements, most CV implementations in orthopaedics remain at the feasibility or proof-of-concept stage. Key hurdles include strict data privacy and security requirements, ethical considerations, and the inherent complexities of integrating CV into existing healthcare IT systems. Effective CV models require diverse datasets to ensure
As CV technology matures, its ability to assist orthopaedic surgeons in diagnostic accuracy and procedural planning will likely expand. By addressing the technical, ethical, and practical barriers of CV integration through innovative approaches like federated learning and improved multi-tasking architectures, CV has the potential to transition from an emerging technology to an integral component of orthopaedic workflows. Ultimately, CV in orthopaedics will complement human expertise — enhancing diagnostic consistency, minimising bias, and enabling surgeons to make data-driven decisions that improve patient outcomes. n
References
References can be found online at www.boa.ac.uk/publications/JTO
Figure 2: Federated model concept.

Shoulder implant data collection on the National Joint Registry
Jaime Candal-Couto, Simon Robinson, David Hawkes, David Miller and Derek Pegg

Jaime Candal-Couto is a Consultant Shoulder and Elbow Orthopaedic Surgeon in Northumbria since 2004 and leads its Upper Limb Unit. Member of the NJR Editorial Board, Data Quality Committee and NJR Shoulder and Elbow Working Group. Past BESS Secretary and Education Committee Chairman, and current Associate Editor of Shoulder and Elbow.

Simon Robinson is a Consultant Orthopaedic Surgeon in Wirral University Teaching Hospital Foundation Trust. He specialises in Upper Limb surgery and has a particular interest in Shoulder Arthroplasty. Currently the Clinical Director, he also has a keen interest in medical education.
The National Joint Registry (NJR) started collecting shoulder implant data in April 2012, nine years after the NJR was established, when it was originally only collecting data on hip and knee implants.
This article looks at and summarises key findings from the 21st NJR Annual Report –shoulder section1, highlights how registry data can inform contemporary shoulder replacement surgery (SRS), and the potential opportunities that future evaluation of NJR data may bring.
Since 2012, the NJR has collected a total of 98,334 shoulder replacement procedures, made up of over 89,172 primary and 9,106 revision procedures (Table 1). This provides a wealth of high-quality data that is complete and mature enough to help guide a surgeon in providing the best outcomes for their patient.
Data quality
Data quality is the foundation on which any conclusions and research are based. Table 2 shows the compliance for shoulders since 2018. The NJR is constantly striving to maximise data capture. Since 2020, the NJR requires hospitals to participate in an ongoing automated data quality audit and as a result captures over 97% of implants across all joints. However, in the early years, shoulder compliance was not as robust. The NJR has identified 15,504 shoulder procedures performed in England between 2012 and 2020 which are recorded in HES (Hospital Episode Statistics) but not in the NJR. A data quality audit is currently being undertaken, involving all affected hospitals and over 4,000 additional shoulder procedures have been added to the NJR so far.
Additionally, the NJR has moved to whole construct validation, ensuring that all relevant elements required to build a construct are present in a procedure. This has led to the definition of unconfirmed constructs, where there are insufficient implants listed to complete a construct or the implants do not match the reported procedure.

David Hawkes is a Consultant Orthopaedic Surgeon in Wirral University Teaching Hospital Foundation Trust with a subspecialist interest is shoulder arthroplasty. He has a longstanding interest in shoulder research and has published widely on normal shoulder function, subacromial pain and rotator cuff tears.

David Miller is a Consultant Trauma and Orthopaedic Surgeon with a specialist interest in Shoulder and Upper limb Surgery, Mid Cheshire Hospitals Foundation Trust, Leighton Hospital, Crewe since 2010. He is Clinical lead in Trauma & Orthopaedics.


Derek Pegg is a Consultant Trauma and Orthopaedic Surgeon in Mid Cheshire Hospitals Foundation Trust, Leighton Hospital, Crewe. He is Chair of both NJR Regional Clinical Coordinators and NJR Data Quality Committees. Figure
Currently, a total of 7,113 (9.6%) shoulder procedures are unconfirmed and the NJR is working on a process of checking and validation of these constructs.
COVID-19 effect still evident
Figure 1 illustrates how elective SRS volumes reduced in 2020 because of the COVID-19 pandemic, but by the end of 2023 had recovered to 2019 volume. However, pre-pandemic there had been a year-on-year increase in volumes recorded. It would therefore suggest that the pandemic deficit continues to impact. The graph also demonstrates that NHS elective SRS activity in NHS hospitals is still noticeably below pre-pandemic levels, while activity in independent hospitals has risen for both independent and NHS-funded surgery.
Primary shoulder replacement
Since 2012, there have been substantial changes in the different indications for SRS as well as the implants used. Currently, the NJR collects data for 12 different indications for surgery, 60% of cases being osteoarthritis, 25% cuff tear arthropathy and 14% acute trauma. Eight main different procedure types are noted, see Figure 2. Data is also acquired as regards fixation with or without cement, patient specific instruments and computer guided surgery. Therefore the data is very heterogenous, indicating it will take time to collect sufficient cases to be meaningful for some particular procedure types. This highlights the importance of on-going reliable and robust data collection.
Traditionally, anatomical constructs (either anatomical total shoulder replacement or hemiarthroplasty) were used to treat conditions such as osteoarthritis, inflammatory arthritis and acute fractures. Reverse polarity total shoulder replacements were initially introduced, very successfully, to treat patients with arthritis and rotator cuff deficiency where the anatomical implants did not perform well. However, the success of reverse shoulder replacements has led to a progressive expansion of its indications across all other different diagnosis including to patients with rotator cuff tears and no arthritis. The NJR has recorded this evolution in shoulder replacement practice since 2012.
Figure 2 demonstrates the progressive decline in the use of anatomical implants, particularly hemiarthroplasties, and how stemmed reverse polarity shoulder replacements have increasingly become by far the commonest shoulder procedure recorded in the NJR. This figure also demonstrates that stemless anatomical replacements are becoming more popular than the traditional stemmed ones, and that high volume surgeons tend to prefer the use of reverse polarity implants while hemiarthroplasties are performed mostly by low-volume surgeons. (Please note the difference in scale of the y-axis between each sub-plot, for both Figures 2 and 3).
Hemiarthroplasty vs reverse total shoulder in trauma
Figure 3 demonstrates how stemmed humeral hemiarthroplasty (HHA) volumes for acute trauma have declined while stemmed reverse total shoulder replacement (RTSR) have steadily risen and are more commonly used by higher volume surgeons.
Revision outcomes in different shoulder constructs in elective surgery
Figure 4 shows KM estimates for cumulative revision rates of the various shoulder constructs, on the NJR, used in elective SRS. The performance of stemmed conventional total shoulder replacement compared to stemmed reverse polarity shoulder replacements is of interest. Reverse polarity total shoulder replacements tend to have an initially higher >>





revision rate which then plateaus, whereas the conventional total shoulder replacements increase more slowly but at a constant rate and therefore exceed the cumulative risk of revision of reverse polarity total replacements and overall is 1.8% higher at 11 years. A failed reverse polarity TSR has historically had limited revision options, and therefore having revision as an end point may under report the true incidence of failure.
The extent to which the different indications for surgery are confounding results is not clear and results should be interpreted cautiously. Caution should be taken when interpreting subgroup outcomes and highlights the importance of comprehensive PROMs data, that would provide a much greater assurance when attempting to differentiate superior outcomes from one type of implant construct to another.
PROMs
From the initial collection of shoulder implant data by the NJR, shoulder surgeons felt it was important to directly collect information on PROMs. This is unique to shoulder implants on the NJR and adds a more sophisticated assessment of success than the current standard outcome analysis for all other implants, where revision and mortality outcomes are used exclusively.
PROMs data are captured and held by NHS England for hip and knees but this has been unavailable to the NJR for over two years. Shoulder PROMs are collected directly by the NJR. While pre-operative PROMs collection for SRS, is excellent for some hospitals, others have struggled. This is obviously a missed opportunity to facilitate a more comprehensive assessment of both implant outcome and hospital services. For the last decade the British Elbow and Shoulder Society (BESS) have consistently advocated the use of shoulder PROMs as essential in the assessment of patient outcomes and surveillance after SRS. We would strongly encourage the collection of pre-operative PROMs. This is mandated by the NHS Standard Contract but many hospitals have generally poor returns, with fewer than 30% of elective patients having their pre-operative PROMs data submitted.
PROMs information is available in the NJR annual report relating to shoulder implants1 It is evident that hemiarthroplasties have a significantly poorer outcome than other constructs but, interestingly, anatomical total shoulder replacements are marginally superior
Figure 2: Frequency of primary shoulder replacements within elective patients stratified by procedure type, bars stacked by volume per consultant per year. HHA - humeral hemiarthroplasty; TSR - total shoulder replacement. RTSR reverse total shoulder replacement. (https://reports.njrcentre.org.uk).
Figure 3: Frequency of primary shoulder replacements within acute trauma patients stratified by procedure type, bars stacked by volume per consultant per year (https://reports.njrcentre.org.uk).

to the commoner reverse polarity implants. However, due to current suboptimal PROMs completeness, there must remain some caution in drawing firm conclusions at this stage.
Minimum volume improves outcome
Research by Valsamis et al.2 suggests that the minimum volume sweet spot for a shoulder replacement surgeon to be able to deliver better outcomes, would appear to be a mean of 10.4 procedures per year. This is illustrated in Figure 5 which presents a multilevel parametric survival model of hazards ratio against mean annual consultant volume, adjusted for key confounding factors. This paper illustrates how analysis of NJR shoulder data can guide surgeons and health systems into achieving the most reliable outcomes for patients.

The current NJR research programme includes evaluating outcomes associated with operationtype in shoulder surgery.
Research and future developments
Ongoing NJR supported research, includes a new prediction model, which incorporates NJR, Hospital Episode Statistics (HES) and Danish Shoulder Arthroplasty Registry (DSR) data. This aims to inform patients of their risks of having shoulder replacement surgery. A recent paper by Valsamis et al.3 suggests that such a model will be a powerful tool for both patients and surgeons in making informed decisions during the consent process for shoulder surgery, on an individual basis.
There are currently five shoulder-specific ongoing research projects that have been approved by the NJR Research Committee. These will evaluate the health and economic outcomes related to the increasing use of reverse shoulder replacement; examine mortality following reverse shoulder replacement; review a stemless prosthesis used in anatomic total and hemiarthroplasty; investigate complication rates and mortality after elective and acute shoulder and elbow replacements; and implement computer adaptive testing for the Oxford Shoulder Score. The NJR encourages the use of the registry dataset to answer research questions that add value to our knowledge about joint replacement practice, clinical performance, cost-effectiveness and patient safety.
More information can be found on the NJR website www.njrcentre.org.uk/research/ research-requests
Annual Clinical Reports (ACR) for hospitals and Consultant Level Reports (CLR)
Finally, the NJR will soon be able to provide shoulder replacement surgeons with a more detailed analysis on the outcomes of the units in which they work. As well as their own personal reports of their surgical outcomes compared to those of their peers, just as hip and knee surgeons currently receive. If the pre-operative PROMs data capture improves the overall analysis of surgical performance it will be a rich source of reference enabling advancement to ultimately improve patient outcomes.
Summary
• The NJR approaches 100,000 shoulder procedures since 2012.
• The COVID-19 pandemic continues to have affected provision of shoulder replacement surgery.
• Observed trends show a greater use of reverse total shoulder replacements.
• Evidence suggests a critical minimum volume for a surgeon, each year, is 11.
• The collection of PROMs data can be crucial in differentiating sustained and successful outcomes from the variety of shoulder replacement constructs currently in use.
Acknowledgement
We are grateful to all patients, surgeons and healthcare staff for sharing data with the NJR. NEC Software Solutions (UK) provide secure data capture for the registry, University of Bristol undertook the analysis that was published in the NJR Annual Report. A full list of authors of the NJR Annual Report is available at https://reports.njrcentre.org.uk. n
References
1. National Joint Registry. NJR 21st Annual Report 2024 – Shoulder Section. Available at: https://reports.njrcentre.org.uk
2. Valsamis EM, Collins GS, Pinedo-Villanueva R, et al. Association between surgeon volume and patient outcomes after elective shoulder replacement surgery using data from the National Joint Registry and Hospital Episode Statistics for England: population based cohort study. BMJ. 2023;381:e075355.
3. Valsamis EM, Jensen ML, Coward G, et al. Risk of serious adverse events after primary shoulder replacement: development and external validation of a prediction model using linked national data from England and Denmark. Lancet Rheumatol 2024;6(9):e607-e614.
Figure 4: KM estimates of cumulative revision for primary elective shoulder replacement by type of shoulder replacement. Blue italics in the numbers at risk table signify that 250 or fewer cases remained at risk at these time points (https://reports.njrcentre.org.uk).
Figure 5: Risk of revision surgery. Association of mean annual consultant volume on risk of revision adjusted for confounding factors in a multilevel parametric survival model (BMJ. 2023 Jun 21;381:e075355)].
How trainees can get involved in sustainability in surgery
Oliver Townsend and Karen Chui

Oliver Townsend is an ST6 in Wessex, and was the Sustainability and Workforce Representative on the BOTA Committee for 2023-24. He organised and ran the 2024 BOTA x ORUK Sustainability Conference and has undertaken several local sustainability audits and projects over the last 18 months.

Karen Chui is a Trauma and Orthopaedic Specialty Registrar in London. As BOTA President, Karen represents Orthopaedic trainees at national meetings, advocating to improve training and education opportunities for trainees. They are passionate about creating cultural change in orthopaedics, building a compassionate profession for the modern surgeon to deliver excellent care to our patients.
When we think about the ever-changing nature of healthcare and transformation of services, it is easy to focus on demographic shifts, clinical breakthroughs and workforce transformation. However, there is another major factor which will change the nature and method of delivery of services in the future: the climate emergency. That the earth is warming up, potentially dangerously and irreversibly so, is widely accepted1. Equally accepted is the role of human activity as the main driver of this, driven by the release of greenhouse gases1,2.
What does this matter for healthcare?
The WHO states that ‘climate change presents a fundamental threat to human health’ and
threatens to undo decades of progress in improving health globally3. The healthcare industry is a major contributor of emissions and needs to actively contribute to the internationally agreed targets to reduce emissions to ‘net zero’4,5. Globally, healthcare contributes more to emissions than aviation (5% vs. 2%)5,6, which gives an important perspective on the scale of the task facing healthcare providers to tackle climate change.
Healthcare leaders and bodies in the UK are increasingly recognising the impact that climate change, and the action required to try to mitigate it, will have on healthcare provision. Government and NHS targets for net zero, in 2050 and 2040-2045 respectively7,8, mean change has to happen. Consequently, work to reduce the environmental impact of healthcare

Figure 1: The Greenhouse Gas Protocol (GHGP) Scopes in the context of the NHS (Source: Delivering
services will only increase in both quantity and visibility. Within healthcare itself, surgery is one of the largest contributors to healthcare system emissions and contributes disproportionately to energy consumption and hospital waste9,10. Reducing theatre resource consumption, waste and carbon gas emissions will be essential, combined with redesigning the provision of services to minimise emissions associated with patient travel and the supply chain7
Why as a trainee?
Environmental changes in the workplace will have a greater impact on our careers than those nearer retirement. As trainees, many of our generation are more climate concerned11, and are therefore well suited to be leaders in driving healthcare sustainability initiatives.
For trainees with an interest in sustainability, getting involved can achieve curriculum requirements for audit, research, and leadership/ management roles12. There are many opportunities to demonstrate experience desirable for consultant roles, such as engagement in change in the theatre environment, or leading a cost- and carbon-saving projects through reducing waste or disposables.
sutures, to reduce the need for clip removal (disposable kit required) or follow-up (patient journeys, clinician appointments), and this could be applied equally to the climate-conscious department14. The Intercollegiate Green Surgery Checklist (Figure 4) is a great starting point for change that can be implemented and audited15
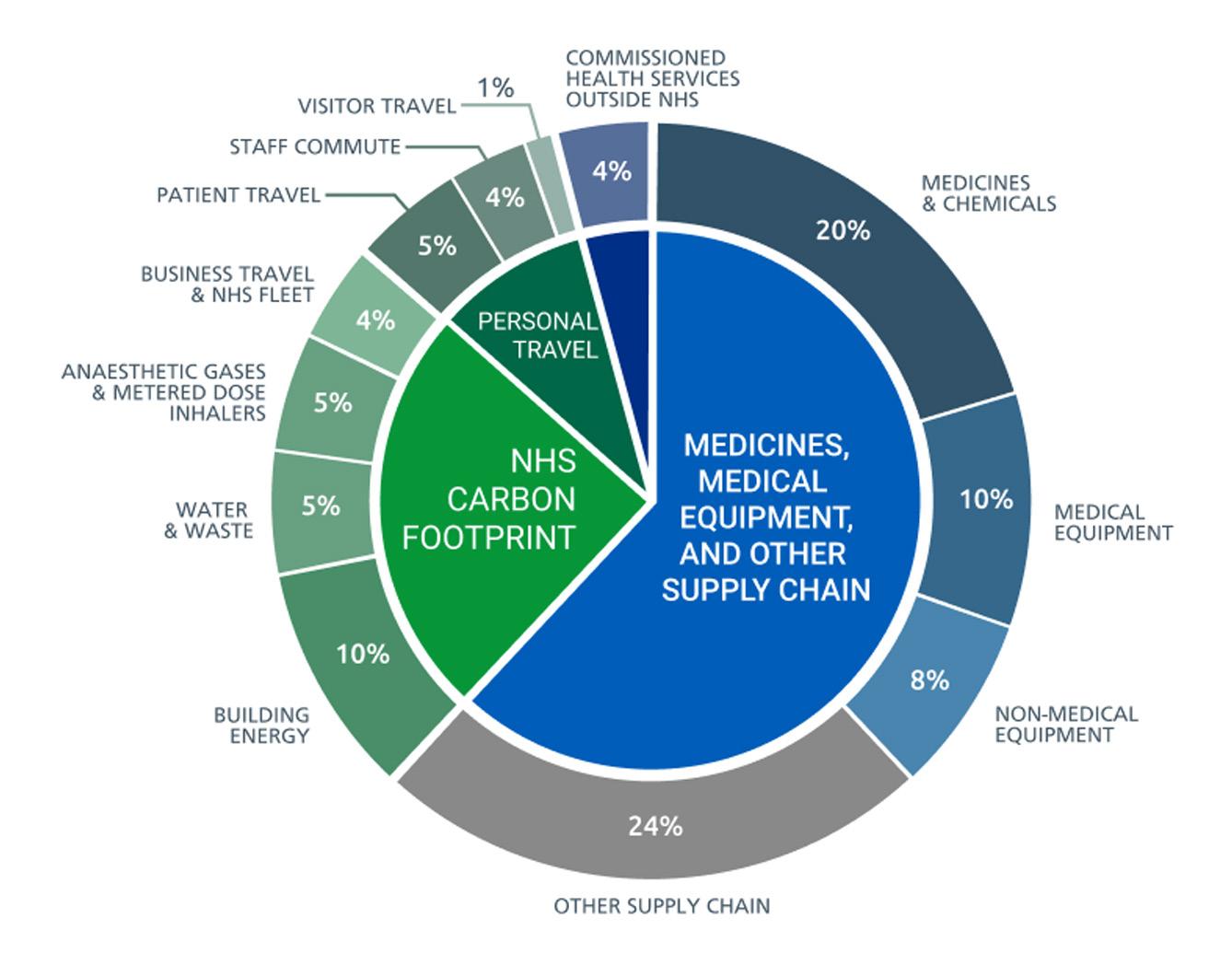
sustainability fellowships, such as the Chief Sustainability Officer’s Clinical Fellowship Scheme with the Faculty of Medical Leadership and Management (FMLM) or the National Joint Registry (NJR) and BOA Sustainability Fellow, which allow trainees to effect organisational change16,17. Finally, there are numerous organisations which offer training and research opportunities, with courses and grants available for sustainability projects. The Centre for Sustainable Healthcare offers a variety of training opportunities18, as well as a network of engaged peers and experts who can offer advice and support with sustainability projects. ORUK and BOA also provide grants and funding for research.
BOTA work
Furthermore, as rotating doctors, we are able to take best practice around with us. Trainees are therefore in a prime position to be leaders in sustainability practice and evoke change. As the consultants and surgical leaders of the future, we can be the change we want to see, and normalise climate consciousness in our everyday practice.
How to get involved
There are many ways trainees can get involved in sustainability in T&O, starting from the individual level through to leading institutional change.
Start with looking at your own, your colleagues’ and your department’s practice, and try to identify where changes are possible. Turning this into local audits can lead to significant change. Examples of this include ‘leaning’ of surgical trays to reduce sterilisation of unnecessary instruments, and substitution of disposable battery pulse lavage systems for rechargeable battery options. Both of these examples were presented at our BOTA x ORUK Sustainability in T&O Surgery Conference this year13, showing the change that trainees are already making (Figure 3). Although pandemic-related, advice during COVID-19 was for absorbable sutures to be used instead of clips or non-absorbable
Starting with easy wins will inspire others that change is possible, and to be more bold with the next project (and there is always a next project).
Beyond this, there is a multitude of more formal roles available. From positions on national committees, such as BOTA (Sustainability and Workforce Representative), to national
Surgical Tray Leaning: Carbon, efficiency and cost-savings in MAKO Robotic-assisted Total Knee Arthroplasty
Surgical Tray Leaning: Carbon, efficiency and cost-savings in MAKO Robotic-assisted Total
Results
Results
Implementing lean methodology has reduced the tray count by one, by removing 36 out of 152 instruments per case. In 5 months, the use of ‘lean trays’ resulted in saving 115 trays being opened, reprocessed and sterilised. This project has resulted in numerous benefits, including a total carbon saving of 220.85 kgCO2e due to reduced use of sterilisation processes (176 kgCO2e)[1] and tray wraps (44.85 kgCO2)[2]. Staff feedback was sought, and satisfaction has been high. Most frequently reported was the ability to count instruments more quickly, increased space in the theatre, and reduced learning curve for new staff. Additionally, an approximate financial saving of £5,750 (115 x £50 per case) was made due to the reduction in the use of sterilisation services.
Implementing lean methodology has reduced the tray count by one, by removing 36 out of 152 instruments per case. In 5 months, the use of ‘lean trays’ resulted in saving 115 trays being opened, reprocessed and sterilised. This project has resulted in numerous benefits, including a total carbon saving of 220.85 kgCO2e due to reduced use of sterilisation processes (176 kgCO2e)[1] and tray wraps (44.85 kgCO2)[2]. Staff feedback was sought, and satisfaction has been high. Most frequently reported was the ability to count instruments more quickly, increased space in the theatre, and reduced learning curve for new staff. Additionally, an approximate financial saving of £5,750 (115 x £50 per case) was made due to the reduction in the use of sterilisation services.
Conclusions
Conclusions
It is imperative that innovative technologies are implemented with sustainability in mind and that the harm to the environment is mitigated wherever possible. In this regard, the implementation of 'lean trays' for orthopaedic and other surgical procedures should be considered by all departments to minimise the impact of such procedures on the environment while also improving efficiency and lowering costs.
It is imperative that innovative technologies are implemented with sustainability in mind and that the harm to the environment is mitigated wherever possible. In this regard, the implementation of 'lean trays' for orthopaedic and other surgical procedures should be considered by all departments to minimise the impact of such procedures on the environment while also improving efficiency and lowering costs.
The great thing is that trainees are already involved. BOTA and ASiT have published Sustainability in Surgery statements and are working towards integrating these fully throughout their organisational activity19. The BOTA Sustainability and Workforce Representative organises the annual ‘Sustainability in T&O Surgery Conference’ which is growing each year13. This year, the conference involved 250 attendees from around the globe, with speakers from RCS England and the BOA, as well as discussions with industry partners Stryker, Johnson & Johnson and Smith & Nephew on green practice in the supply chain. >>
PULSE LAVAGE: AWASH WITH CARBON SAVING OPPORTUNITIES
PULSE LAVAGE: AWASH WITH CARBON SAVING OPPORTUNITIES
Results
Results
37,521 pulse lavage hand pieces were purchased across NHS Scotland in 2022 with an annual spend of £702,644.56. Almost all (99.89%) were single-use battery operated handpieces. The LCA calculations demonstrated that moving from battery operated to AC power would result in a 33.2% reduction in carbon footprint. There was an even greater carbon saving opportunity if moving from battery operated to the power tool driven alternative (ECOpulse ®) which is manufactured in the UK[3] and would provide a 60.9% reduction in associated carbon footprint.
37,521 pulse lavage hand pieces were purchased across NHS Scotland in 2022 with an annual spend of £702,644.56. Almost all (99.89%) were single-use battery operated handpieces. The LCA calculations demonstrated that moving from battery operated to AC power would result in a 33.2% reduction in carbon footprint. There was an even greater carbon saving opportunity if moving from battery operated to the power tool driven alternative (ECOpulse ®) which is manufactured in the UK[3] and would provide a 60.9% reduction in associated carbon footprint.
Conclusion
Conclusion
Alternatives to current practice exist with AC power adaptor options for all battery operated devices currently in use. However, if all pulse lavage in Scotland was power tool driven we could achieve a carbon reduction of 96.5TCO2e per annum. The equivalent of 16 elephants!
The National Green Theatres Programme has now published an ‘Opportunity for change’ to highlight this important carbon saving opportunity and this will be included in board validation and measurement plans moving forward.
Alternatives to current practice exist with AC power adaptor options for all battery operated devices currently in use. However, if all pulse lavage in Scotland was power tool driven we could achieve a carbon reduction of 96.5TCO2e per annum. The equivalent of 16 elephants! The National Green Theatres Programme has now published an ‘Opportunity for change’ to highlight this important carbon saving opportunity and this will be included in board validation and measurement plans moving forward.
Figure 2: Sources of carbon emissions by proportion of NHS Carbon Footprint Plus (Source: Delivering a ‘Net Zero’ NHS)]
Knee Arthroplasty
Figure 3: Extracts from trainee abstracts presented at 2024 BOTA x ORUK Sustainability in T&O Surgery Virtual Conference.
Intercollegiate Green Theatre Checklist
Intercollegiate Green Theatre Checklist
Below are a list of recommendations to reduce the environmental impact of operating theatres. All the relevant guidance and published evidence has been included in the Compendium of evidence, accessed via the QR code:
Below are a list of recommendations to reduce the environmental impact of operating theatres. All the relevant guidance and published evidence has been included in the Compendium of evidence, accessed via the QR code:
Anaesthesia
Anaesthesia
1 Consider local/regional anaesthesia where appropriate (with targeted O2 delivery only if necessary)
1 Consider local/regional anaesthesia where appropriate (with targeted O2 delivery only if necessary)
2 Use TIVA whenever possible with high fresh gas flows (5-6 L) and, if appropriate, a low O2 concentration
2 Use TIVA whenever possible with high fresh gas flows (5-6 L) and, if appropriate, a low O2 concentration
3 Limit Nitrous Oxide (N2O) to specific cases only and if using:
3 Limit Nitrous Oxide (N2O) to specific cases only and if using:
آ check N2O pipes for leaks or consider decommissioning the manifold and switching to cylinders at point of use;
آ check N2O pipes for leaks or consider decommissioning the manifold and switching to cylinders at point of use; introduce N2O crackers for patient-controlled delivery.
آ introduce N2O crackers for patient-controlled delivery.
4 If using inhalational anaesthesia:
4 If using inhalational anaesthesia:
آ use lowest global warming potential (sevoflurane better than isoflurane better than desflurane);
آ consider removing desflurane from formulary;
آ use lowest global warming potential (sevoflurane better than isoflurane better than desflurane);
آ consider removing desflurane from formulary;
آ use low-flow target controlled anaesthetic machines;
آ use low-flow target controlled anaesthetic machines;
آ consider Volatile Capture Technology.
آ consider Volatile Capture Technology.
5 Switch to reusable equipment (e.g. laryngoscopes, underbody heaters, slide sheets, trays)
5 Switch to reusable equipment (e.g. laryngoscopes, underbody heaters, slide sheets, trays)
6 Minimise drug waste (“Don’t open it unless you need it”, pre-empt propofol use)
6 Minimise drug waste (“Don’t open it unless you need it”, pre-empt propofol use)
Preparing for Surgery
Preparing for Surgery
7 Switch to reusable textiles, including theatre hats, sterile gowns, patient drapes, and trolley covers
7 Switch to reusable textiles, including theatre hats, sterile gowns, patient drapes, and trolley covers
8 Reduce water and energy consumption:
8 Reduce water and energy consumption:
آ rub don’t scrub: after first water scrub of day, you can use alcohol rub for subsequent cases;

آ rub don’t scrub: after first water scrub of day, you can use alcohol rub for subsequent cases;
آ install automatic or pedal-controlled water taps.
آ install automatic or pedal-controlled water taps.
9 Avoid clinically unnecessary interventions (e.g. antibiotics, catheterisation, histological examinations)
9 Avoid clinically unnecessary interventions (e.g. antibiotics, catheterisation, histological examinations)
Intraoperative Equipment
Intraoperative Equipment
10 REVIEW & RATIONALISE:
10 REVIEW & RATIONALISE:
آ surgeon preference lists for each operation - separate essential vs. optional items to have ready on side;
آ surgeon preference lists for each operation - separate essential vs. optional items to have ready on side; single-use surgical packs - what can be reusable and added to instrument sets? what is surplus? (request suppliers remove these);
آ single-use surgical packs - what can be reusable and added to instrument sets? what is surplus? (request suppliers remove these);
آ instrument sets - open only what and when needed, integrate supplementary items into sets, and consolidate sets only if it allows smaller/fewer sets (please see guidance).
آ instrument sets - open only what and when needed, integrate supplementary items into sets, and consolidate sets only if it allows smaller/fewer sets (please see guidance).
11 REDUCE: avoid all unnecessary equipment (eg swabs, single-use gloves), “Don’t open it unless you need it”
11 REDUCE: avoid all unnecessary equipment (eg swabs, single-use gloves), “Don’t open it unless you need it”
12 REUSE: opt for reusables, hybrid, or remanufactured equipment instead of single-use (e.g. diathermy, gallipots, kidney-dishes, light handles, quivers, staplers, energy devices)
12 REUSE: opt for reusables, hybrid, or remanufactured equipment instead of single-use (e.g. diathermy, gallipots, kidney-dishes, light handles, quivers, staplers, energy devices)
13 REPLACE: switch to low carbon alternatives (e.g. skin sutures vs. clips, loose prep in gallipots)
13 REPLACE: switch to low carbon alternatives (e.g. skin sutures vs. clips, loose prep in gallipots)
After the Operation
After the Operation
14 RECYCLE or use lowest carbon appropriate waste streams as appropriate:
14 RECYCLE or use lowest carbon appropriate waste streams as appropriate:
آ use domestic or recycling waste streams for all packaging;
آ use domestic or recycling waste streams for all packaging;
آ use non-infectious offensive waste (yellow/black tiger), unless clear risk of infection;
آ ensure only appropriate contents in sharps bins (sharps/drugs);
آ non-infectious offensive waste (yellow/black tiger), unless clear risk of infection; ensure only appropriate contents in sharps bins (sharps/drugs); arrange metals/battery collection where possible.
آ arrange metals/battery collection where possible.
15 REPAIR: ensure damaged reusable equipment is repaired, encourage active maintenance
15 REPAIR: ensure damaged reusable equipment is repaired, encourage active maintenance
16 POWER OFF: lights, computers, ventilation, AGSS, temperature control when theatre empty
16 POWER OFF: lights, computers, ventilation, AGSS, temperature control when theatre empty
DISCLAIMER: These suggestions are based upon current evidence and broadly generisable, however, specific environmental impacts will depend upon local infrastructure and individual Trusts’ implementation strategies.
DISCLAIMER: These suggestions are based upon current evidence and broadly generisable, however, specific environmental impacts will depend upon local infrastructure and individual Trusts’ implementation strategies.
Following this, BOTA has incorporated as many sustainable measures into our Annual Congress in November to reduce our carbon footprint. There is still a lot we can do, but we’ve made a start by making our events more green and influencing organisations we interact with. BOTA represents an important trainee voice and strives to use our involvement with important stakeholders to advocate the sustainability agenda.
Personal life
Climate change work is not the sole responsibility of the government, industry and employers. The impact of any individual’s actions may be limited in the global context, but collectively we can make significant change. Within our personal lives, there are many ways we can be more sustainable and greener. We are not here to preach, and there will certainly be aspects listed here where these authors are not saints! No one is perfect, and change does not have to be immediate or ‘all or nothing’. Individually, it is about trying to make positive changes in habits and practice where possible.
‘Reduce, reuse, recycle’ is far from a new motto, and it is as relevant now as it ever has been. Indeed, it underpins the action needed at organisational level to achieve net zero in much the same way it can be used by individuals. On a personal level, both at work and outside, simple actions like turning off idle devices and lights reduces energy consumption, whilst choosing items or products with less bulky or eco packaging reduces waste for disposal. Reusable shopping bags are now commonplace, whereas using one’s own coffee cup or reusable cutlery is less common but no less impactful. Taking a bottle for refilling with water saves an often-virgin plastic bottle from landfill, with many reusable bottles also having thermal properties. Recycling involves separating the component parts of an individual package into what is recyclable or not and putting the waste in the correct bin. Many items we purchase, or have finished with, can form part of a more circular economy; after all, one man’s trash is another man’s treasure. Sites like Vinted for clothes, and eBay for everything else, allow items to be resold and often saves money (or generates it if you are a seller).
To reduce, reuse and recycle, NHS Green have added ‘Replace’20. This is to guide staff to consider replacing individual car journeys to work with alternative means, such as public transport, walking or cycling, and lift sharing. The cycle to work scheme is an easy and cost- effective way to get a new bike, with bikes paid for in monthly instalments from your payslip taken out of pre-tax income21. Although typically structured over 12 months, which can be tricky for rotating trainees, it is possible through discussion with HR and payroll for this to be done over as little as six months. If considering public transport, combining this with a folding bike, can make door-to-door green travel more flexible and time efficient. Once open to alternative transport, it becomes easier to consider it outside of the commute. Taking time to explore which regular journeys you make by car could instead be made by bus or train often yields surprising results and be cost saving. This, coupled with calculating your private vehicle’s actual cost per mile to run, can make switching from driving to taking the train or bus a no brainer; evening out return train fares are a little-known gem offering cheap day returns for the afternoon and evening, as are capped evening bus fares.
Summary
The time is now to get involved in green and sustainability practice. Start with a few small changes to your own life and to your personal practice, then start with simple audits and changes at your workplace. Consider bigger roles such as the BOTA Sustainability and Workforce Representative role, or national sustainability fellowship roles. There is something for everyone, and we need everyone to do their bit. n
References
References can be found online at www.boa.ac.uk/publications/JTO
Figure 5: How trainees can get involved in sustainability and be greener.
Intercollegiate Green Theatre Scorecard. November 2022.
Intercollegiate Green Theatre Scorecard. November 2022.
Figure 4: Intercollegiate Green Surgery Checklist. Source: The Bulletin of the Royal College of Surgeons of England 2023;105(2):64-7.

Supreme comfort, optimal positioning and optimal access - introducing the QA3™ Treatment Stretcher.
sales@aneticaid.com
+44 (0)1943 878647 www.aneticaid.com


Establishing an orthopaedic trauma service in rural Ethiopia
Richard Power

Richard Power was a Consultant Orthopaedic Surgeon in Leicester 1995-2020 specialising in hip surgery and is winding up his career as a Medical Examiner. He has been involved in the development of orthopaedic care in Gondar, Ethiopia since 2017. Since then he has been one of the leaders of the Leicester Gondar Orthopaedic Partnership and is currently Chair of Health Action Leicester for Ethiopia. He was awarded an MBE in the New Years Honours for his work.
“Give a man a fish and he will eat for a day. Teach a man to fish and you feed him for a lifetime”.
Ancient Chinese Proverb
Much of the surgical support provided in Low and Middle Income Countries (LMICs) by developed countries involves specialised teams providing specialist care not available in the relevant country. This is surgery which can be scheduled and may not even involve local facilities, such as Mercy Ships. However, as the orthopaedic trauma workload is 24/7 and cannot wait for a team to arrive, a sustainable solution has to involve locally trained surgeons working within appropriate facilities.
The original link between Leicester and Gondar in the northwest Amhara region of Ethiopia was established more than 25 years ago. Laurence Wicks, initially as a Medical Student and subsequently as an orthopaedic trainee visited Gondar and recognised the paucity of trauma care. The only operating theatre had been built by the Italians during their brief occupation of Ethiopia in the 1930s which was virtually derelict and the single surgeon only had the skillset or equipment to provide non-operative management. This was for a population estimated at five million, approximately the size of the East Midlands.
Laurence persuaded two Leicester Orthopaedic Consultants (Alwyn Abraham and Christopher Kershaw) to travel to Gondar in 2016 and during that visit they met with senior members of the Gondar University Hospital who indicated a strong desire to establish an orthopaedic trauma service capable of operative intervention. On returning to the UK they approached myself as a colleague and the President Elect of the Rotary Club of Leicester to seek support in raising the necessary funds to provide all the
equipment required for a fully functioning orthopaedic trauma theatre.
After a fact-finding visit to Gondor in early 2017, I, along with the Club, agreed to take on the project. We were successful in our application for a Rotary Foundation Global Grant amounting to a project total of $200,000 with the Club being required to raise approximately two thirds of that amount. The Rotary Club of Gondar Fasiledes were our local International partner (a requirement for a Rotary International grant is involvement of a local Rotary Club in that country). At this point the Leicester Gondor Orthopaedic Partnership was formed.
Medical Aid International, a social enterprise specialising in providing medical/surgical equipment appropriate for LMICs agreed to provide all the equipment, which came from a variety of sources including donations, closing hospitals, ex-demonstration, film sets and new purchase from India. A good

Figure 1: The Orthopaedic Consultant staff at Gondor University Hospital with the first two graduates from the training programme.

example was the ‘Big Bertha’ US Army field steriliser, which simply requires a bucket of water and electricity supply in order to function.
During my presidential year of 2017 and 2018, the Rotary Club raised the necessary funds during which period Gondar Hospital commenced the structural work to the operating theatre. They also appointed Dr Ananya Kassahun, a newly graduated orthopaedic surgeon off the Black Lion Programme. Ananya proved crucial to keeping up the momentum in Gondar and she also visited Leicester to appreciate the important

aspects of theatre management and infection prevention principles. Two theatre nurses were also funded to visit Leicester and spend two weeks in an orthopaedic theatre environment. During this time, my colleagues from various disciplines and I made regular visits to Gondor to maintain the momentum of the project and I was in regular communication with the University of Gondor regarding the building work and staff appointments.
By 2019, all the money had been raised and the equipment procured. It was then shipped to Ethiopia via Djibouti. As the shipping container had been purchased as part of
the consignment, we decided to use it as an additional space alongside the theatre by building an external concrete plinth and cutting an access door in the side. This subsequently housed the autoclave. As the building work had not been completed, the shipping container remained sealed.
By March 2020, the main building works had been completed but as adjacent work was still ongoing with significant dust creation, live surgery wasn’t viable. Despite this, we went to Gondor in early March 2020 and were able to unload the container and assemble all the equipment and conduct some teaching. >>

Figure 3: Tim Beacon from Medical Aid International teaching how to use the Big Bertha.
Figure 2: Operating theatre in Gondor before (left) and after (right).


Everything was then placed in the storeroom adjacent to the theatre with the plan to return in July 2020 to commence live surgery and carry out further teaching. At this point the COVID-19 international lockdown descended preventing any further visit. By July, the Hospital had appointed four surgeons from the Black Lion Programme. We agreed that there was no option other than releasing everything for their use with online support from the team here in Leicester.
To further compound the difficulties, the Tigray conflict started in August 2020. The Amhara Region is adjacent to Tigray and Gondar became one of the main casualty receiving hospitals with up to 150 casualties arriving each day on top of the day-to-day
trauma. Although the Partnership had provided a 12-month supply of trauma implants, this rapidly proved inadequate and had to be augmented by implants provided by the Federal Government military.
The Partnership provided further equipment in the form of proximal femoral nail sets. The four surgeons had online access to advice from the Leicester trauma surgeons and the surgery carried out would have been a credit to any UK Trauma Unit.
The Tigray conflict lasted for two years with an estimated 600,000 lives lost due to injury, disease and starvation. By November 2022, the newly formed University of Gondar Department of Orthopaedics had carried out approximately 4,000 operative procedures.

The Leicester team were finally able to visit in November 2022 to assess progress. Although the operative surgery element had clearly flourished, many challenges remained with basic cleanliness and nursing care. A number of items of equipment had either broken or had not been used because of lack of training. We then planned
further training visits. Sadly at this point, internal conflict started between the Ethiopian federal Government and FANO, (the Amhara militia), with further visits put on hold. I have continued to have regular monthly meetings online with Dr Birlew, the head of Service in Gondor, to provide encouragement and support in developing the department as a cohesive unit.
The department has now expanded to ten trained surgeons and has even commenced its own training programme in conjunction with the regional University Hospital in Bahir Dar. One surgeon was able to take up a six-month spinal fellowship in India and has subsequently been able to carry out surgical intervention without the patient needing to make the long and expensive journey for care to Addis Ababa.
As an allied project, a Rotary-funded Jaipur Limb Centre has recently opened which enables lower limb amputees to receive basic lower limb prosthetics which previously were not available.
I continue to have regular online meetings and am forever hopeful that peace will return to the Amhara region allowing further visits.
In summary, the Gondar University Hospital has gone from having no orthopaedic operative ability in 2019 to having a well-functioning department with ten trained surgeons and its own training programme carrying out 2,000 trauma procedures annually all within five years. This has happened as a result of a multi-agency collaborative approach, giving rise to a longterm sustainable service that hopefully is now ultimately independent of external support. n
Figure 4: An example of the trauma that can now be treated.
Figure 5: Gunshot wound to proximal femur treated with intra-meduallary fixation.
Figure 6: The Leicester Gondor Orthopaedic Partnership.
Arthrosamid® — The first and only synovial scaffold2,3 administered via a single injectable for long-lasting pain relief.4,5

Pioneering Proven1 Pain relief treatment1
For full details about warnings and precautions read the IFU. For more information and the IFU please visit hcp.arthrosamid.com or contact us at enquiries@arthrosamid.com





References: 1. Arthrosamid®, Instructions For Use. Release Date March 2022. 10082-003; 2. Christensen, L., et al. (2016). Histological Appearance of the Synovial Membrane after Treatment of Knee Osteoarthritis with Polyacrylamide Gel Injections: A Case Report. Journal of Arthritis. Vol 5: 217; 3. Christensen, L., et al. (2016). Synovial incorporation of polyacrylamide hydrogel after injection into normal and osteoarthritic animal joints. Osteoarthritis and Cartilage. Vol 24(11):1999-2002. DOI:10.1016/j.joca.2016.07.007; 4. Bliddal, H., et al. (2024) 3 year follow-up from a randomized controlled trial of intra-articular polyacrylamide hydrogel injection in subjects with knee osteoarthritis. Poster LB-31, OARSI 2024 World Congress on Osteoarthritis; 5. Bliddal, H., et al. (2024) A Prospective Study of Polyacrylamide Hydrogel Injection for Knee Osteoarthritis: Results From 4 Years After Treatment. Presented at EORS 2024, Aalborg and Orthopaedic Proceedings of the Bone & Joint Journal.

Statistically significant reduction in pain maintained at 4 years.5 Learn more about our reproducible results here by scanning the code.

OUS/ARTHRO/NOV2024/276

The future of shoulder and elbow surgery
Deborah Higgs

Deborah Higgs is a Consultant Shoulder and Elbow Surgeon at the Royal National Orthopaedic Hospital, Stanmore, and has a special interest in complex surgery of the Shoulder and Elbow with a tertiary referral practice that reflects this. She lectures on the Elbow and Shoulder nationally and Internationally.
A previous member of the BESS Education Committee, she is the current BESS Instructional Course Sub-Committee Elbow Surgeon Member and was appointed the NCIP (National Consultant Information Programme) Clinical Lead for Orthopaedics in 2022.
Istill remember my first mobile phone, a NOKIA that simply allowed me to ring someone and send a text, with emojis limited to colons, semi-colons and brackets. The year was 1998. Whilst I now have a smart phone, that allows me to be connected 24/7, it is an iPhone 7, which tells you everything you need to know about technology and me. Having said this, I recognise the transformative role that technology is playing in the evolving world of shoulder and elbow surgery, with artificial intelligence and machine learning having the potential to enhance diagnostic accuracy, optimise surgical planning, enable robotic-assisted interventions, and personalise postoperative care. In my own practice, I have already embraced technology in my surgical planning. I was therefore delighted to be asked to guest edit this specialist section on shoulder and elbow surgery where we have two articles that explore this further.
“I
recognise the transformative role that technology is playing in the evolving world of shoulder and elbow surgery, with artificial intelligence and machine learning having the potential to enhance diagnostic accuracy, optimise surgical planning, enable robotic-assisted interventions, and personalise postoperative care.”
In Catherine Simister’s article on Large Language Models (LLMs), she writes about the role they may play in education, academia and clinical efficiency, writing how LLMs are capable of passing the Member of the Royal College of Surgeons (MRCS) exam, scoring more than 85%. She highlights that as the potential of LLMs are realised that regulation must ensure data quality, and a ‘clear definition of the scope of LLMs within medical practice’.
In the second article ‘A tipping point for technology in shoulder surgery?’, Simon Hurst writes about technology’s second coming and explores the role of robotics and mixed reality in shoulder surgery. He describes how industry is investing in technologies that support existing implant systems with refinement in planning, navigation and robotic platforms, and how this time around they may become more embedded in our everyday practice.
Both articles describe the role technology can play in the future but emphasise that with these new technologies comes responsibility to ensure that they are regulated and deliver genuine improvement in care. This aligns with NICE’s position statement from August 2024, “When AI methods are used, the transparency, rigour and trust in our guidance production is maintained. Therefore, any use of AI should be done judiciously, leveraging the strengths of AI to support and enhance decision making only when it is suitable and when it adds value”.
The final article written by the current president and immediate past president of the British Elbow and Shoulder Society (BESS) discusses Hub and Spoke Models of care in the delivery of low volume/ high complexity orthopaedic surgery. They discuss the rationale and challenges in centralising care concluding that “changes in the provision of services based on guidelines alone seem to be ineffective until coupled with new NHS network funding models”.
These are interesting times in shoulder and elbow surgery, and all three articles provide food for thought, with a common theme of improving patient outcomes. I hope you enjoy reading them. n
Centralisation of low-volume high complexity orthopaedic surgery: Hub-and-spoke models in the National Health Service

Neal Rupani has just completed his Shoulder and Elbow Fellowship at University Hospital of Coventry and Warwickshire NHS Trust. He completed his specialist training within the Health Education Thames Valley Deanery, and will soon be commencing a consultant position with a special interest in Shoulder and Elbow Surgery.

Neal Rupani, Vanessa J Chow, Jonathan L Rees and Steve Drew
A2015 national review by Getting It Right First Time (GIRFT) identified unwarranted variation in patient care delivery and outcomes within orthopaedic surgery and recommended the hub and spoke model for low-volume high complexity surgery within the National Health Service (NHS)1. It is argued that the hub-and-spoke model would optimise operational efficiency, resource allocation and patient outcomes amidst national economic constraints and an ever-aging population.
Originating within the aviation and transportation industry, the hub and spoke model streamlines and centralises resource-intensive and
infrequently performed procedures into a few specialist centres (hubs) whilst maintaining access to routine common surgery in community-based hospitals (spokes)2 Hubs are usually larger tertiary care hospitals or specialised centres equipped with multidisciplinary teams, advanced diagnostic and treatment capabilities, making them ideally suited for managing low-volume high complexity cases. Conversely, spokes are smaller hospitals that deliver high-volume low-complexity procedures and also serve as satellites to hubs in referring complex cases and supporting pre-operative investigation and post-operative care. This ensures comprehensive and coordinated patient care throughout the network or region. >>

Vanessa Jane Chow is an aspiring orthopaedic surgeon and graduate of St George’s University. She has completed her foundation years in the Thames Valley Deanery and is currently pursuing an MSc in Advanced Surgical Practice.

Jonathan Rees is Professor of Orthopaedic Surgery and Musculoskeletal Science, Botnar Institute Director and Head of Department (NDORMS) at the University of Oxford. He is an NIHR Senior Investigator and Past President of the British Elbow and Shoulder Society (BESS).

Steve Drew is a Consultant Shoulder and Elbow Surgeon at University Hospitals Coventry and Warwickshire and the current President of the British Elbow and Shoulder Society (BESS).
Volume-outcome relationship
The rationale for centralising low-volume high complexity surgeries in higher volume hubs is primarily grounded in the evidence supporting a positive volume-outcome relationship, i.e. higher surgical volumes drive improved patient outcomes3-5. It is theorised that performing procedures more frequently improves technical proficiency, which leads to better outcomes6
This association has predominantly been demonstrated in high-volume lower limb surgery, such as total knee replacements (TKRs) and total hip replacements (THRs), where higher centre or surgeon volumes are associated with reduced rates of surgical site infection7, revision4,8,9, post-operative dislocation5 and mortality4,8-12. For revision lower limb replacement surgery, lower mortality rates and improved lengths of stay were found in high-volume centres13. Highervolume centres in total ankle replacement (TAR) have also shown fewer complications, shorter hospital stays, and reduced costs14
This relationship has been studied less in upper limb joint replacement. For total elbow replacement (TER), higher volume centres have achieved improved implant survival15 and lower revision risks with registry data suggesting a 1.5 times risk reduction16,17. Similarly, for shoulder replacements, increased surgical volumes results in lower revision rates3,18, fewer adverse events, shorter hospital stays and shorter operating times18,19. Recent peer-reviewed research indicates a career annual surgeon average of 10.4 primary shoulder replacement procedures results in lower revision rates18
However, the isolated use of a volumeoutcome relationship has been criticised for:
• Selective referral. Better outcomes naturally attract more referrals and therefore drive higher surgical volumes, as opposed to the other way round6
• Variable definitions. There is variability in methodologies, data types and a lack of standardisation in how volume thresholds are calculated for different procedures.
• Configurations. High-volume centres may be made up of many low-volume surgeons, creating a fallacy for the gains in technical proficiency hypothesis.
• Confounders. Available evidence fails to consider individual hospital variables such as clinical guidelines, use of multi-disciplinary teams, surgeon expertise based on training, and variable case mixes10,20
A context-specific understanding of the volume-outcome relationship is desirable but challenging to achieve.
Current practice for joint replacement
Low-volume high complexity surgery was common in 2015, with 58.2% of revision TKRs and 45.9% of revision THRs performed by surgeons with an annual volume of five or fewer1 Despite this, data from the 2023 UK National Joint Registry report demonstrates the shift to a hub and spoke model to reduce the distribution of low-volume high complexity surgery has gained minimal traction21, and is discussed below.
Hip and Knee Replacement. Both primary THRs and primary TKRs are considered highvolume procedures and conducted across most orthopaedic units with the annual number of replacements performed nearing 100,000 each. The numbers drop for revision replacements with 6,258 revision THRs and 5,464 revision TKRs performed in 2022, of which 1,196 and 889 were re-revision replacements respectively. The British Orthopaedic Association (BOA) and British Association for Surgery of the Knee (BASK) have recommended that complex or re-revisions TKRs are undertaken at hubs, with primary revisions being suitable in spokes which perform medium to high volume revisions22. Revision knee networks have been set up and piloted. Re-assessment of the new volume distribution and outcomes would help assess the clinical and healthcare cost impact of this change.
Shoulder Replacement. While primary shoulder replacements take place at lower volumes compared to THR and TKR, the numbers continue to increase. In 2022, 6,780 replacements were performed with a median surgeon volume of 10 across 370 hospitals. Although primary shoulder replacement is not considered a low volume procedure, it is worth noting that primary reverse total shoulder replacement (RTSR) is now a common treatment for proximal humeral fractures and over 25% of trauma RTSRs were performed by surgeons performing six or fewer annually. Revision shoulder replacement is a lower volume procedure with only 662 cases performed in 2022. Discussions are now taking place between NHSE, GIRFT and the British Elbow and Shoulder Society (BESS) on the topic of revision networks for revision shoulder replacement surgery.
Ankle Replacement. TARs performed have increased in total and per unit over the last decade but remain a low-volume high complexity procedure with 880 primary replacements performed in 161 units in 2022. Currently a third of TARs are performed by surgeons performing six or less annually and only seven units perform over 20 per year. GIRFT and British Orthopaedic Foot and Ankle Society (BOFAS) expect surgeon involvement in at least six TARs annually, along with the consideration of clinician passports and dual operating to support regional services and bolster surgeon experience23
Stakeholders Advantages
Patient
Surgeon
• Access to centralised hubs with concentrated expertise and coordinated multidisciplinary care which enhances outcomes for complex conditions2
• Routine care managed locally at spokes reduces travel for less complex needs, enhancing accessibility.
• Surgeons at high-volume hubs benefit from frequent exposure to complex procedures enhancing surgical outcomes.
• Hubs provide robust opportunities for continuous professional development, including structured mentorship and specialised training programs, essential for maintaining high standards30
Provider • Centralisation in high-volume hubs promotes economies of scale thereby reducing operational costs and avoiding resource duplication.
• Streamlined care pathways in hubs allow for efficient management of high-complexity cases.
• Higher case volumes increase the ease of audit and research, particularly for infrequently performed procedures.
• Shared regional governance meetings can allow good ideas and practice to be transmitted.
Elbow Replacement. Only 281 TERs were performed in 2022, making it the lowest volume large-joint replacement and the major orthopaedic focus for introducing the hub and spoke model. GIRFT and BESS produced recommendations in 2017 for best practice and the provision of TERs, and strongly advocated for 1-2 regional hubs to be nominated to undertake this surgery24. Adoption of these recommendations and shifting to centralisation has been variable and limited. 99 surgeons across 92 units currently perform only 281 primary TERs (median number per consultant = 3, median number per unit = 2). The proportion of TERs being performed by high-volume (greater than 12) surgeons has increased but the proportion of surgeons performing four or less TERs has remained unchanged. Much of the delay in any full transition to elbow hub and spoke networks relates to NHS funding changes and adequate tariff for complex revision work. This funding has been approved in 2024 and the full transition to elbow replacement networks is now expected.
Other applications of the hub-and-spoke model
The perceived advantages and disadvantages of the hub and spoke model can be seen in Table 1. The benefits can be seen in real life examples, as centralisation in trauma and orthopaedics is not new or unique to joint replacement surgery. Nationally, high-severity
Disadvantages
• Increased travel distances to specialised hubs can be inconvenient, expensive and lead to a lack of compliance and exacerbating healthcare inequities34
• Transfer delay, particularly in emergencies, leading to worse outcomes.
• Potential delays in treatment due to inappropriate referrals to hubs.
• Surgeons at spoke centres may experience professional stagnation and diminished skill development due to limited opportunities to perform complex surgeries, leading to decreased job satisfaction and reduced morale.
• Resistance from surgeons reluctant to give up ‘hard-won’ skills and experience at spoke centres, especially those with proven high-quality outcomes despite low procedural volumes20
• Potential loss of high-quality training opportunities and training surgeons if complex cases are entirely centralised at hubs, affecting skill diversity and development.
• Unsupported staff managing outpatient care of complex patients.
• Reimbursement models favouring high-volume, low-complexity procedures may undermine the financial viability of hubs, particularly for managing resource-intensive complex surgeries that are not appropriately compensated.
• Increased patient volumes at hubs can strain bed capacity, operating theatres capacity , administrative workload and parking capacity, all potentially leading to longer wait times.
• Ambiguity in defining specialised or complex surgery and arbitrary thresholds for minimum surgical volumes lead to inconsistencies in care delivery10,20
• Ineffective communication and coordination between hubs and spokes, due to underutilisation of digital tools and regional governance meetings, can fragment care delivery.
• Diluted responsibility and accountability can hinder integrated care delivery.
trauma has been centralised to major trauma centres (MTCs). Since then, quality-of-care indicators and the rate of ‘good recovery’ outcomes have improved25,26. Patient volumes at MTCs also increased by 200%. Sarcoma services are also nationally centralised, with improved survival rates and disease-free intervals from this model being seen both within the UK and internationally27-29
More recently, a region centralised treatment for complex congenital talipes equinovarus30, where primary correction rates were similar across both hub and spokes. Hub-treated patients required significantly fewer casts applications, had fewer complications, and were able to correct complications referred from spoke sites.
Examples have also highlighted key challenges to be considered prior to implementation. Delays in care arising from prolonged transfer times has been one of those key concerns. Definitive treatment for peri-prosthetic fractures was delayed by seven days when centralised31 Outside of orthopaedics, patients suffering from acute ischaemic stroke were unable to get thrombectomy treatment owing to this32. Robust communication and clear transfer protocols are essential to ensure effective patient management and minimise delays. Another key challenge was ensuring careful network planning and ‘outreach work’ to provide specialist support to spoke sites33. These examples illustrate the value and difficulties surrounding the hub and spoke model.
Summary
The hub-and-spoke model presents a recommended framework for enhancing orthopaedic care for low-volume procedures by centralising expertise, increasing operational efficiency and improving patient outcomes. However, challenges such as ensuring equitable and easy access for patients, along with ensuring engagement from the surgical community, NHS Trusts and commissioners need to be carefully considered. While the centralisation of low-volume, high complexity procedures is a persuasive argument some of the examples discussed highlight that any changes in the provision of services based on guidelines alone seem to be ineffective until coupled with new NHS network funding models. It is the opinion of the authors that until such funding models are in place, including levelling up of any disparity in tariffs paid to trusts for some of these resource-intensive procedures, then effective hub and spoke changes for low-volume procedures will not take place. There also remains scope for further monitoring and high-quality research of the clinical and cost effectiveness of these models. n
References
References can be found online at www.boa.ac.uk/publications/JTO
Table 1: Advantages and disadvantages of the hub-and-spoke model from the perspectives of patients, surgeons, and healthcare providers.
Large language models in upper limb surgery: A narrative review
Catherine Simister, Kyle Lam, Andrew Yiu and James M Kinross

Catherine Simister is a final year medical student at Imperial College London with an interest in surgery.

Adoption of large language models (LLMs) has grown exponentially throughout society, and the most well-known of these is ChatGPT (OpenAI, San Francisco, CA, USA). Since in its launch in 2022, it now averages 100 million weekly users1,2. LLMs represent a form of artificial intelligence (AI) that are capable of understanding and generating human-like text3,4.
While the workings of LLMs are more complex than this description, in its simplest form, these models work by predicting the next word in a phrase. If a human is asked to complete the sentence, ‘Humpty Dumpty sat on a’, they would most likely say ‘wall’ and LLMs perform a similar task in reading the input text and predicting what word is most likely to follow it. The input or ‘prompt’ (Table 1) to a LLM can similarly turn this next-word prediction mechanism into a question answering machine, for example, ‘The nerve innervating the biceps brachii muscle is…’.
Kyle Lam is a NIHR Academic Clinical Fellow and Registrar in General Surgery at Imperial College London. He completed a PhD in AI for surgical performance assessment. He has wide ranging research interests within surgical AI including computer vision, large language models, and challenges in clinical implementation. Term Definition
Artificial Intelligence
Machine Learning
Large Language Model (LLM)
Generative AI
Parameter
Supervised learning
Unsupervised learning
Semi-supervised learning
Fine-tuning
When confronted by this, the LLM must predict what word would come next through the generation of probabilities for possible next words based on patterns from the data it was trained on and the selection of the highest probability word. Here, the model might output a probability of 95% for musculocutaneous, 2% for radial, and 1% for median and therefore select musculocutaneous.
The power of these models lies in the fact that LLMs learn this next word prediction through the recognition of patterns in enormous quantities of textual data. Commonly available LLMs on the market (Table 2) are likely to have been trained across the majority of textual data available on the internet including internet forum discussions and Wikipedia via a process called self-supervised learning. Differing from supervised learning, where the model would learn that a picture was that of a cat because it had been annotated by a human as a cat, in self-supervised learning
The science and engineering of making intelligent machines.
The field of study that gives computers the ability to learn without explicitly being programmed.
AI systems capable of understanding and generating human language by processing vast amounts of text data.
A type of artificial intelligence that can create new content ranging from text, images, or video based on data it has learnt from.
A variable learnt from the data during the training process of an AI model which is subsequently used to make predictions on new data.
A model that is trained on labelled inputs to classify data or predict outcomes.
A model that learns patterns exclusively from unlabelled data.
A model that learns from a small portion of labelled data and lots of unlabelled data to train a predictive model.
The process of taking an AI model and further training it on a smaller targeted dataset. The aims are for the model to keep the original capabilities of the initial model while adapting it to more specialised use cases.
Prompt In the context of a LLM, this is the input or set of instructions given to the LLM. Table 1: Definitions of common terms.

Andrew Yiu is a General Surgery Registrar in Surrey and Honorary Research Fellow at Imperial College London. He has an interest in digital surgery with a focus on improving patient outcomes using operative data, particularly surgical video.

James Kinross is a Reader in Colorectal Surgery and a Consultant Surgeon at Imperial College London. His clinical interest is in robotic surgery and minimally invasive surgery for colorectal cancer. He performs translational research in the fields of early colorectal cancer detection and prevention and in surgical technology transfer.
the model would guess ‘Dumpty’ if ‘Humpty’ was inputted and then compare this prediction with the actual word contained within the training data. If correct, the model then updates the variables within the model or ‘parameters’ so that it is more likely to predict this the next time. The model subsequently looks at ‘Humpty Dumpty’ and tries to predict the third word in the sentence by repeating the same process.
The speed of societal AI adoption has been driven in part by the increase in computing power for the training of generative AI based models, which is climbing fourfold each year, and by novel developments in AI architectures. AI capable of creating original content, such as these models, are termed ‘generative AI’ and can output text, images, video, and audio, from minimal input data5,6 Generative AI has seen rapid uptake across multiple industries including the financial sector for report writing and within retail for online chatbot services7 and this has been reflected within its growth within the market having been estimated to be worth over $1 trillion by 2032. It is therefore little surprise that healthcare has also been a proposed target for LLMs8,9. This review sets out prospective uses and benefits of LLMs within healthcare, with a focus on upper limb surgery, describes envisaged challenges to clinical translation, and future targets for research.
LLMs encode clinical knowledge
LLMs have been found to encode significant clinical knowledge, with ChatGPT 3.5 either meeting or achieving close to the pass mark in all three steps of the US Medical Licensing Exam (USMLE)10-12. Within postgraduate examinations, LLMs have also passed the Member of the Royal College of Surgeons (MRCS) exam, scoring more than 85%12. LLMs, such as MedPaLM and PubMedGPT, which have been specifically fine-tuned on medical datasets may enhance the trustworthiness of ‘out-of-the-box’ models and may demonstrate further promise for the use of LLMs within clinical practice13,14
One proposed clinical application for LLMs within the literature are for LLMs to act as co-pilots for diagnosis and management. Within upper limb surgery, Google’s Gemini correctly classified 70% of hand injuries from a series of textbook vignettes15 and Daher et al found ChatGPT 3.5 correctly diagnosed 93% of shoulder and elbow complaints, but relied heavily on MRI reports16. ChatGPT’s diagnostic success was, however, not replicated when presented with more complex cases, such as patients with comorbidities or uncommon injuries16,17. For example, ChatGPT 3.5 was unable to diagnose an atypical radial nerve injury where the sensory impairment differed from the conventional pattern17. Whilst models themselves are limited by the data they are trained upon, they are also limited by the input or ‘prompt’ they are given. Limitations of these models will likely be improved upon with future technological iterations which will likely see an exponential growth in model size.
LLMs for improved clinical efficiency
LLMs have also been proposed to improve clinical efficiency allowing time to be more effectively dedicated to direct patient care18. One potential application is within triage, where LLMs could facilitate clinical decisionmaking and automatically streamline patients to the correct services at presentation19-20. Newer iterations of LLMs, which allow processing of multimodal input, such as radiographic images, open significant avenues for their wider use, especially within orthopaedic surgery21,22.
Beyond direct clinical use, the capability of LLMs to automatically generate text often indistinguishable from that authored by humans could see them alleviating the high administrative burden of clerical work for junior doctors, who are estimated to spend approximately 50% of their time completing these tasks23, (Figure 1). >>
2)


Patel and Lam found that ChatGPT was able to produce a discharge summary when provided with a short clinical vignette, suggesting LLMs may be useful in reducing the time taken to complete these tasks24. However, such applications must be balanced with the need to maintain patient confidentiality, which can limit the capability of LLMs both within the training and inference process25.
LLMs for education
There are significant challenges ahead of translation of LLMs for direct clinical applications, including quality assurance, trustworthiness, and security. Education, however, is a potentially low-risk, high-reward setting for the use of LLMs, which could breach the gap prior to their wider clinical use. For example, LLMs could assist with simulating patient-doctor scenarios, creating study plans, exploring concepts, and providing multiple choice question response explanations, (Figure 2), with few consequences in the case of algorithmic failure26. As previously discussed, LLMs can encode clinical knowledge, but within orthopaedic education, performance of LLMs has been variable. Lum et al., concluded that ChatGPT could perform at a second-year resident’s level in the Orthopaedic In-Training Examination (OITE), although another study
found that ChatGPT was able to achieve a score above that of residents at any level27.28 When tested on exclusively upper limb questions, however, ChatGPT only achieved 45%, well below the expected standard29. This study, however, demonstrated the need for effective prompt engineering as the model was likely limited by the use of manual descriptions of images within the prompt rather than the input of the raw images themselves29
LLMs for academia
Academia also stands to benefit from the skills of LLMs, which could assist in multiple stages of research30. LLMs may assist in the brainstorming phase, as well as providing elaboration on existing ideas31. LLMs could shorten the notoriously time-consuming tasks of grant and manuscript writing, plus offer grammar checking for final drafts. Their ability to summarise text could be useful in writing abstracts, and the use of LLMs for this purpose has already been demonstrated, with Bisi et al., finding the highest rates of AI-generated text within abstracts30-32. Yet the use of LLMs to generate academic text is controversial, raising questions over academic integrity33,34. Whilst guidelines are not standardised, most leading medical publishers do not accept LLMs as an author on scientific papers and require disclosure if LLMs
have been used beyond grammar and spellchecking purposes. However, the challenge of identifying AI generated text remains35 The need to create methods to detect AI generated text and standardised guidelines between journals is therefore urgent.
LLMs for patients
Patients are also increasingly likely to utilise LLMs and there are several possible ways in which LLMs could alter the way patients interact with healthcare providers. The Topol Review, which explored future roles of digital technology in healthcare, cited telemedicine as a major advancement36. LLMs are likely to play a significant role in telemedicine. The now-extinct Babylon Health was used to assist in the initial triage, diagnosis and management of patients, but failed due to cost inefficiency and limited usefulness of its chatbot service37. There is significant potential for LLMs or ‘chatbots’ to assume a triage role, facilitating direction towards the most appropriate service or management.
It is not uncommon for patients to consult ‘Dr Google’ and with the ease of access, many may look to LLMs to answer questions about their health. ChatGPT’s ability to answer common questions relating to
Figure 1.


upper limb conditions has been explored extensively38-40. One study looking at questions relating to rotator cuff injuries, found that whilst answers were generally correct and written at a suitable reading level, they rarely cited references41. The concern here is that LLMs can produce plausible but incorrect information or ‘hallucinations’ which may not be obvious to non-expert readers, and may lead to misdiagnosis, excessive investigation, or adverse patient outcomes. If specialist LLMs are to be deployed for patient-facing use, methods for dealing with errors must be determined first.
Barriers to the deployment of LLMs
Regulation is struggling to keep up with the pace of LLM development – both the UK and EU AI acts have been through multiple iterations, demonstrating the challenges of regulating a dynamic field42-44. With general purpose LLMs, like ChatGPT, there is limited knowledge on the quality of the data that has been used in training, making their use in clinical practice particularly high risk45 Using LLMs in clinical decision-making also necessitates discussion regarding liability46. If a patient were to come to harm following LLM input in their care, there would need to be clear policy on who is held accountable for the decision. For example, if a chatbot consulted with undifferentiated patients, it is easy to see how LLMs could misinterpret
a prompt with potentially life-threatening implications. Equally, patients must be aware of LLM use within their care, and it is uncertain whether this would actually increase patient concern. LLMs are also at risk of bias due to their dependence on their training data, which likely comes from high-income, Western countries47. It is therefore essential that models are trained and evaluated on diverse datasets prior to deployment.
A roadmap to LLM translation
Despite these issues, technologists continue to seek solutions to improve performance of LLMs. The risk of hallucination can be reduced through ‘reinforcement learning with human feedback (RLHF),’ where humans are directly involved in the training process48, (for example, if the LLM outputs ‘Humpty Dumpty sat on a fence’, a human can correct the model to ‘wall’ and the LLM can adjust based on this feedback and improve on future iterations). Fine-tuning can also be used, which involves further training existing models on targeted datasets to enhance their capabilities carrying out specific tasks. LLMs are also intrinsically dependent on their training data. As clinical practice evolves with rapidly changing guidelines, technical solutions such as retrieval augmented generation (RAG) (a method which allows LLMs to search data outside its training set, for example clinical guidelines or patient datasets) could enhance trustworthiness of these models49
Technological limitations are likely to be resolved as newer iterations of models emerge, but regulatory issues must be solved if clinical translation of LLMs is to become a reality. Regulatory bodies must negotiate data quality assurance, model evaluation, and monitoring, and a clear definition of the scope of LLMs within medical practice4,45. This will likely require a multi-stakeholder approach including patients, healthcare professionals, software engineers, and policymakers.
Conclusion
LLMs are being adopted at a rapid pace and its use in healthcare is likely to expand in the coming years. Whilst its use may be reasonable in low-risk settings, it is critical that regulations are in place to ensure they are accurate and contributing meaningfully to the healthcare field. Barriers to deployment will likely be beyond technological barriers alone and include trustworthiness, confidentiality, and liability. This will likely require a multi-stakeholder approach including patients, healthcare professionals, software engineers and policymakers to establish codes of conduct, guidelines and standards for the use of LLMs within orthopaedic surgery. n
References
References can be found online at www.boa.ac.uk/publications/JTO
Figure 2.

John McNamara graduated from the University of Birmingham in 2018. He is a Specialist Registrar in the Oxford Deanery with a research interest in Enhanced Recovery after Surgery.

Matthew Williams graduated from St Catherine’s College, University of Oxford in 2020 and is a Trauma and Orthopaedic Registrar in the Thames Valley Deanery. He has a research interest around innovation in orthopaedic surgery.

Simon Hurst is a consultant trauma and orthopaedic surgeon in Oxford at the John Radcliffe Hospital and Nuffield Orthopaedic Centre. He is evaluating and developing roles for wearable devices and mixed reality headsets in shoulder & elbow surgery and major trauma. Previously he was a Chef de Clinique at AP-Hôpitaux de Paris, and Université Sorbonne Paris Nord in France.
A tipping point for technology in shoulder surgery?
John McNamara, Matthew Williams and Simon Hurst
In 2009 at Harvard’s annual arthroplasty meeting, industry was showcasing its latest product offerings, amongst them Brainlab™ showing early iterations of navigation. The possibilities appeared unlimited with a broad range of uses demonstrated from navigating a distal locking screw in a tibial nail to aiding acetabular component positioning in hip resurfacing. One of the authors was there and spent some time lining up various cross hairs at the stand, it felt like the future had arrived. There was nothing yet for the shoulder, but it was surely only a matter of time.
Big bang theory
15 years ago, technology in orthopaedics was enjoying its ‘first coming’. Commercial spaces were filling with navigation systems allowing for more precise positioning of cutting blocks, guide pins, entry points and screws. The very concept of navigation itself implies that one has a destination in mind - or the correct position – and so it also came in lockstep with planning software.
The overriding principle was to reduce outliers, surgeons with lower annual numbers of a procedure type, those in training, or for use in procedures which might be considered to have a narrower window of tolerance for malposition.
Robotic systems such as Justin Cobb’s (Imperial College, London, UK) novel Acrobot™ arrived onto the scene1. Technology in this form didn’t compete with existing portfolios, because if you wanted to use their technology for navigation you usually had to use the company’s respective implant. With implants placed more accurately there was also the prospect of lower revision rates and improved registry data.
Mako™ went one step further and designed a totally new implant to work with their robotic system for uni-compartmental knee replacement. In this setting it was easy to see and imagine the
future. Arthroplasties would all be planned with subsequent execution of the plan using either a navigation or robotic platform. Except it really didn’t quite work out that way. Yet…
Hype and suspicion
As surgeons, we strive to be evidence-based and outcome orientated. This rightly creates natural suspicion and resistance to any deviation from habitual techniques and established technology. After all, it took some 45 years, and significant criticism, for Palmer’s initial laparoscopic techniques in the 1940s, to culminate in the first laparoscopic cholecystectomy in 1985. A technique which paved the way for similar methods, including shoulder arthroscopy within our own specialty.
Perhaps stronger than this is an innate resistance to change something that appears to all intents and purposes to be working. The navigation and robotic systems of that period arrived and in some instances were wrecking balls, disrupting flows, and forcing surgeons to amend techniques long perfected. As a result, cases took considerably longer, and there was sometimes abandonment to traditional techniques midcase. This accompanied by the need to insert navigation pins, alongside time consuming registration procedures and occasional equipment malfunctions led people to persist for a few cases but many then simply gave up.
A strength of industry is often to inspire us to do something new. But with the associated hype comes a risk of over promising and under delivering. Many will try something, but will they become adopters? After they have tried and failed to adopt, a window is then shut for a period. This is usually until that individual decides that something fundamental has changed and is as a result willing to try it anew. In this way, technology’s ‘first coming’ ended up being predominantly left to the enthusiasts.
A paradigm shift in commercial models and technology’s second coming
The recent Cumberlege enquiry, GIRFT movement, and increased regulation and costs associated with new implant development have shifted the balance away from implant innovation in favour of doing what we know works well, better.
This has led to a paradigm shift away from developing new implants, towards increasing the yield from current implant portfolios. In this environment, we see money being directed towards investment in technologies to support the use of existing implants.
This has led to substantial refinement in planning, navigation and robotic platforms and the emergence of several new domains: mixed reality (MR) headsets, 3D printed guides, and wearable devices amongst many others.
Many trainees have had exposure to these technologies during their training and will be looking to incorporate them into their practice. For those who tried the initial inceptions of navigation and robotics and didn’t become adopters it is likely that enough time has passed for many to be open to re-visiting latest iterations. This combined with a natural awareness and acceptance of technology into our lives outside of the workplace makes fertile ground for a ‘second coming’ of technology into the orthopaedic space.
Watch this space
Mixed reality
Mixed reality (MR) technology (a slightly more immersive version of augmented reality) allows for a digital image in 3D holographic form to be both superimposed and controlled by the user on top of their normal visual field. In surgery, it is easy to see the potential in projecting visual information in this way without compromising sterility.
As a result, there has been significant investment towards developing software for these devices. Microsoft’s Hololens™ arrived in 2016 and a year later, a first shoulder replacement was performed by Thomas Gregory at Avicenne Hospital, APHP, Paris, France using visual holographic aids2. Zimmer Biomet has since adapted the later version of the headset, the Hololens™ 2 for surgery with their Optivu™ system including an inbuilt camera tilt amongst other features for surgery.
At present most of the large manufacturers have their own MR packages. Almost all use the Microsoft Hololens™ 2 platform, itself launched in 2019 and already five-years old with focus to date being predominantly within domains of planning, MR adjuncts to traditional navigation, and remote assistance.

As with navigation and robotics in the late noughties, this hasn’t quite taken off yet, which likely comes down to the concept of genuine utility. Many products launched to date have made for interesting and visually compelling demonstrations during surgery but have objectively added little. They improve conceptualisation and allow for others to view remotely, but only like any other head mounted camera, furthermore MR headsets can even remove acuity from the visual field akin to wearing sunglasses.
Despite these challenges, we believe that MR will have an enormous role to play. Some hurdles in providing a smoothly functioning MR navigation system have been overcome by Stryker’s Blueprint™ software (Figure 1)3
An emergence of newer MR devices such as Apple’s Vision Pro™, and Google Glass™ provides an opportunity to develop software, taking advantage of their enhanced capabilities.
A key domain for focus should be in remote surgical assistance. The ultimate goal being to develop technology around accurate holographic representation of another surgeon’s hand in the visual field of another operating remotely. The possibilities of being able to accurately point and gesticulate to another remotely being easy to comprehend.
To maximise the likelihood of surgeons becoming adopters, functionality in this domain must be shown to have genuine surgical utility. New users must be properly trained and logistics (including the banalities of charge times, internet bandwidth, and DICOM data management) must be seamless.
Novel robotic platforms
The core concepts of robotic platforms around supporting the precise execution of surgical plans are well established as a navigation adjunct with a robotic arm aiding guide wire position or the preparing of a bony surface in preparation for an implant. Custom guides provide an alternative but can take weeks to manufacture with 3D printing not yet providing a robust solution when the negative effects of autoclave sterilisation are considered.
In shoulder arthroplasty, De Soutter’s CelitoTM robotics platform represents a way of rapidly manufacturing guides using a robotic platform. A truly novel technique whereby a mould is taken by the surgeon of the glenoid surface using a special cartridge. The mould cartridge then sets and the robot which is within the sterile field uses an optical scanner to scan the mould taken and map to cross sectional imaging of the patient. It then drills a hole corresponding to the planned guide wire position, (Figure 2), allowing for an angular accuracy of 1.9 degrees version and 1.2 degrees inclination with a positional accuracy of 1.1mm when compared to the preoperative plan4. As upper extremities often represent a smaller market share, they usually end up with technology extrapolated from the hip and knee world. The rapid on table manufacture of guides using this robotic technique, is an example of innovation in the other direction and one could imagine its use outside of the shoulder.
Wearable devices
Wearable technology is the use of sensors attached to a patient, which can detect and record movement, or other variables. This technology in society is common, existing in devices such as smart phones or accelerometers and its use is increasing. >>
Figure 1.

This has created a natural opportunity to monitor patients and observe progress following injury, therapy or surgery. A global poll of AO Trauma members found that 21% of respondents use wearable technology in clinical treatment, the largest proportion of these were used in the upper limb.
Researchers have already started to track return of movement following shoulder surgery and are even able to monitor sleep quality as a marker of pain following arthroplasty. Many groups are showing an increase in patient recovery from injury and surgery with the addition of a wearable5. The data types that can be obtained is both novel and compelling with the ability to be used alongside PROMS and other data to provide a more complete picture (Figure 3) in the outcomes of surgery6
Has the low hanging fruit from RCTs already been harvested? If so we may see less impact from them over the coming years as conducting them at a global scale becomes more time consuming, logistically complicated and expensive7
As technology reaches a tipping point in shoulder surgery this should provide space and impetus for both its further development and assessment; a premise that technology must never be used for its sake alone. n
References
1. Cobb J, Henckel J, Gomes P, Harris S, Jakopec M, Rodriguez F, et al. Handson robotic unicompartmental knee replacement: a prospective, randomised controlled study of the acrobot system. J Bone Joint Surg Br. 2006;88(2):188-97.

Wearables will offer real time updates to the surgeon, therapist and patient for range of movement, recovery and discomfort. This will allow detailed remote monitoring and early identification of outliers. In the non-elective setting, data collected from a wearable provides opportunity to show when patient function returns following fracture. This in turn, providing feedback to clinicians to initiate progress to load bearing such as for clavicle or proximal humerus fractures. With wearable technology becoming ubiquitous in modern society, the clinical implications of this are unlimited.
Conclusions
A favourable financial climate for technology more generally is being created by the predicted force of artificial intelligence (AI) being introduced across our health systems. With this second coming of technology will come a responsibility of all of us to conduct rigorous examination of these technologies and decide whether they provide genuine utility for our patients. The UK has a proud tradition being a world leader in orthopaedic research with a particular focus on high quality RCTs which have shaped contemporary practice.
2. Gregory TM, Gregory J, Sledge J, Allard R, Mir O. Surgery guided by mixed reality: presentation of a proof of concept. Acta Orthop. 2018;89(5):480-3.
3. Fleet CT, Gao R, Johnson JA, Athwal GS. An in vitro comparison of mixed-reality navigation to traditional freehand and patient-specific instrumentation techniques for glenoid guide pin insertion during shoulder arthroplasty. J Shoulder Elbow Surg. 2024;33(11):2482-92.
4. Darwood A, Hurst SA, Villatte G, Tatti F, El Daou H, Reilly P, et al. Novel robotic technology for the rapid intraoperative manufacture of patient-specific instrumentation allowing for improved glenoid component accuracy in shoulder arthroplasty: a cadaveric study. J Shoulder Elbow Surg. 2022;31(3):561-70.
5. Small SR, Khalid S, Price AJ, Doherty A. Device-Measured Physical Activity in 3506 Individuals with Knee or Hip Arthroplasty. Med Sci Sports Exerc. 2024;56(5):805-12.
6. Van de Kleut ML, Bloomfield RA, Teeter MG, Athwal GS. Monitoring daily shoulder activity before and after reverse total shoulder arthroplasty using inertial measurement units. J Shoulder Elbow Surg. 2021;30(5):1078-87.
7. Costa ML, Brealey SD, Perry DC. International orthopaedic trials. Bone Joint J. 2023;105-B(7):719-22.
Figure 2.
Figure 3.

Designed for the extensive reconstruction of the hip and knee joint and based on over 20 years of clinical experience of the 1st generation USTAR system. The USTAR II™ system is part of the United Orthopedic family of products designed for difficult primary and revision interventions.
Lorem ipsum
Malcolm Swann
7th August 1931 – 31st October 2024
Obituary by Robin Allum and Michael Thomas
Malcolm Swann was born in 1931 in West London and trained at the Westminster Hospital Medical School.
He spent four years abroad during his surgical training, two years on secondment to a hospital in Nigeria whilst working as a registrar at the Royal National Orthopaedic Hospital and two years spent doing National Service with the Royal Army Medical Corps in Malaya.
He was appointed as consultant to the Windsor Group of Hospitals in 1967, which included the newly built Wexham Park Hospital Slough, Heatherwood Hospital Ascot, King Edward VII Hospital Windsor, St. Mark’s Hospital Maidenhead and the Canadian Red Cross Hospital Taplow.
As well as a running a busy general orthopaedic practice at Heatherwood and Wexham, Malcolm worked alongside the late Dr Barbara Ansell CBE, Consultant Rheumatologist at the Canadian Red Cross Hospital specialising in treating juvenile idiopathic arthritis where both built an international reputation in the management of this disease. Medical management was not nearly as successful as it is now and this was immensely challenging work carrying out soft tissue surgery and joint replacement in children and young adults with stunted growth and severe joint deformity.
He served as Honorary Secretary of the BOA from 1984 to 1985.
After fully retiring from the NHS at 70, he continued to work as a volunteer abroad for over 20 years. He initially worked with World Orthopaedic Concern (WOC) and Mercy Ships UK, then joined Richard Brueton and Chris Lavy in Blantyre, Malawi at the Beit Cure Hospital (an American Christian Charity).

After the two other surgeons had returned to the UK, he ran the hospital before spending a short time working in Ethiopia. He then moved to Zambia to oversee the completion and equipping of the Beit Cure International Hospital in Lusaka, becoming its Medical Director. He finally stopped operating at 80 but continued to manage a hospital and teach medicine in Lusaka until he was over 90!
His work in Africa was rightly recognised with an MBE in 2010.
An amazing medical legacy and wonderful colleague. n


The Cost of Periprosthetic Joint Infection: Prevention is better than cure
Periprosthetic joint infection (PJI) is a common and serious complication following total joint arthroplasty. In addition to its clinical impact, the financial and psychological costs of PJI are a major burden for both, the individual and society. Preventive strategies to reduce the risk of infection and thus the costs are mandatory.
PJI is an important public health issue. The incidence of PJI has been estimated to reach up to 2% in primary surgery and 4% after revision.1 Several factors contribute to the occurrence of PJI, including poor adherence to operating theatre standards, inadequate perioperative prophylaxis and patient-related risk factors.
The burden and costs of PJI
Implant infections can result in significant morbidity and mortality, as well as immense socio-economic costs. It is not only associated with direct medical costs such as hospitalisation and staffing. There are also indirect costs associated with PJI, such as the negative impact on the patients’ quality of life and psychological well-being. And, not to be forgotten, in addition to the emotional burden on affected patients, PJI also has a profound effect on their families as well as on doctors, nurses and other healthcare workers.2
Where do the costs of PJI originate from?3
Looking to the future, the financial and emotional costs of PJI are expected to further increase as the population ages and the incidence of fractures increases. In fact, in Germany, a 23.3% increase of femoral neck fractures was observed within a decade, making it the most frequently surgically treated fracture.3
Reducing the Risk of PJI – The Value of Preventive Local Antibiotics
An integrated and effective preventive approach is essential to reduce the risk of infection in arthroplasty patients. Individually tailored infection prevention measures may include optimisation of surgical procedures, preoperative optimisation of patient risk factors and comorbidities, as well as consistent systemic and local antibiotic prophylaxis.
The use of dual antibiotic-loaded bone cement has been shown to be an effective measure to prevent surgical site infection
(SSI).4 This is illustrated by the results of a quasi-randomised study of 848 patients with femoral neck fractures showing that the addition of two antibiotics to bone cement, rather than just one, reduced the infection rate by 2.4% points one year after hip replacement surgery (p=0.041).4
For more information visit our clinical evidence overview for the use of COPAL® G+C, a high-dose dual antibioticloaded bone cement, for prosthesis fixation after femoral neck fracture: www.herae.us/ clinical-evidence-fnof n

References
1. Izakovicova P et al. Periprosthetic joint infection: current concepts and outlook. EFORT Open Rev 2019; 4: 482-494.
2. Zardi EM, Franceschi F. Prosthetic joint infection. A relevant public health issue. J Infect Public Health 2020; 13: 1888-1891.
3. Szymski D et al. The prophylactic effect of single vs. dual antibiotic-loaded bone cement against periprosthetic joint infection following hip arthroplasty for femoral neck fracture: an analysis of the German Arthroplasty Registry. Antibiotics 2023; 12.
4. Berberich et al. Patients at a high risk of PJI: Can we reduce the incidence of infection using dual antibiotic-loaded bone cement?. Arthroplasty 2022; 4: 41
I’m an ophthalmologist and my dad is a retired consultant. We’d been out for lunch and a few drinks when we came across a badly injured motorcyclist. Despite us doing everything we could, he died.
Months later, we received coroner’s letters, asking us to give evidence at the inquest. I went cold. What would this mean for my career?
From the moment I called Medical Protection, they took away a huge burden. They assigned us a case manager who helped us prepare for the legal process. They say they’re always there for you, and they really are. They know exactly what to do and they just get on with doing it.
In the end, I received no criticism in court. The relief was indescribable. I am incredibly thankful to have had Medical Protection by my side.






















