More than 200,000 small to medium-sized businesses depend on BenefitMall’s guidance and leadership for employee benefits solutions—and for good reason. BenefitMall leverages innovative technology, backed by our human expertise to provide brokers with the fastest, easiest, and most trusted benefits selling experience.
From quote to enrollment and more, BenefitMall will help you support and retain your clients. Join us and let’s grow business together! Scan to Request to be Broker Partner





August 20 to 22, 2024 at Pechanga Resort Casino, Temecula, CA

e BEST lineup of speakers are scheduled to educate you about growing your medicare business
Stan Morrison will be our Keynote Speaker on August 21, is a renowed basketball coach who has a lot of business savvy to explain how to use the rules of sports in devloping your business to gain more medicare clients.
On August 20, another powerful Keynote Speaker, Michael Fahey III, former Marine who is now the district manager for Colonial Life. His inside knowledge of the industry will enlighten you. Michael will teach you the tricks he has learned to be a successful agent.
is will be a very informative summit. e CEO of NABIP, Jessica Brooks-Woods and the incoming president of CAHIP, Rosamaria Marrujo, will share what some of the new rules will be in a panel discussion for medicare for 2025.
Register today for this important Medicare Summit! A full 3 days of educational certi cations and CE classes, informative panel discussions plus several other guest speakers who are sure to give you all the tools you will need to be a successful Medicare agent. Plus breakout sessions and exhibitors including various insurance carriers, medical groups, and supplemental bene t providers all ready to share their information.



Breakout Sessions, Training Programs, and discussions about the new Medicare Legislation both state and federal for 2025
Visit our website: theseniorsummit.net

8
PUBLISHERS NOTE
Read an introduction to our Medicare Issue which describes our commitments and goals for our readers in this issue.
By Phil Calhoun
17
MEDICARE FMO
The Value of Field Marketing Organizations
Learn about Field Marketing Organizations, referred to as FMOs, which provide benefits to agents, carriers, and consumers with the variety of services they provide.
By Tiffany Stiller
18
MEDICARE BUSINESS DEVELOPMENT
5 Automation Ideas for a More Profitable Medicare AEP
Learn about 5 automations tools that Martin & Associates Insurance Services that brokers have found to be extremely useful, more efficient, and profitable during AEP.
By Elliott Martin
20
MEDICARE BUSINESS DEVELOPMENT
Interview with Steve Kuhtz from Sierra First Insurance Services
Learn about First Sierra Insurance through an interview with Steve Kuhtz and our publisher Phil Calhoun.
By Steve Kuhtz
Cal Broker’s commitment is to be the leading source of news and information for California brokers and agents operating in the health, life, and annuity industry. We are committed to connecting Life and Health insurance professionals to valuable resources and solutions they can provide to their insurance clients.
22
MEDICARE BUSINESS DEVELOPMENT
What Does LOA Stand for in Insurance?
Read everything you need to know about licensed only agents: pros and cons, structuring compensation for LOA agents, structuring LOA contracts, and more.
By John Hockaday
25
MEDICARE BUSINESS DEVELOPMENT
What Does MedPAC Does The Medicare Payment Advisory Commission (MedPAC) advises Congress on a range of issues affecting Medicare, including payments, services, access, and regulations.
26
MEDICARE AND HSA’S
Selling Health Savings Accounts to CPAs and Financial Professionals in California: A Guide for Health Insurance Brokers
Here is a guide on effectively selling HSAs to CPAs and financial professionals in California
By Genna Armanini
28
MEDICARE MARKETING
Embracing the Digital World: A New Era for Independent Life and Health Insurance Agents & The Changing Landscape of Client Interaction
Learn about how to embrace the digital world and seize the vast potential that a borderless market offers.
By Elka Soussana
30
MEDICARE MARKETING
Start Planning Now for AEP 2024
This coming Annual Open Enrollment Period (AEP) is promising to be one of the most challenging and crazy times.
By Maggie Stedt, C.S.A, LPRT
32
MEDICARE MARKETING
Medicare 101: 2025 Drug Coverages for Medicare Part D
The Inflation Reduction Act (IRA) of 2022 has led to many changes to drug coverage, and more are coming in 2025.
By CalBroker Mag
34
MEDICARE MARKETING
Medicare 101: CMS Marketing & Compensation Changes for 2025
In April 2024, the U.S. Centers for Medicare and Medicaid Services (CMS) released the Contract Year 2025 Medicare Advantage and Part D Final Rule.
By CalBroker Mag
MEDICARE MARKETING Planning For Medicare While Still Working Full-Time
Learn how to best guide your clients in planning for Medicare while still working full-time to avoid unnecessary complications such as coverage gaps and enrollment penalties.
By CalBroker Mag
38
MEDICARE & LONG TERM CARE
LTC Insurance Alternatives for Your Medicare Clients That May Surprise You
Explore the insurance alternatives that have emerged to fill the gap as other solutions.
By Marc Glickman
40
MEDICARE REFERRALS
To Get More Medicare Referrals –Think Process Over Products
Find out how it can to achieve more Medicare referrals.
By Bill Cates
41
MEDICARE AND GROUP
New innovative Health plan reduces employer premiums by 30%
Learn about Vitori Health’s self-insured alternative.
By Eric Trost
44
MEDICARE COMMISSIONS
Planning Decisions this Time of Year: Protect, Grow, and Sell Health Commissions
As an Active Broker, learn all about planning and commission protection in this article.
By Phil Calhoun
46
MEDICARE HEALTH TOPICS Vision & Eye Health
Understanding vision conditions, symptoms, and the typical medical care can help you find the best vision insurance for your clients.
By CalBroker Mag
48
MEDICARE HEALTH TOPICS
Bone & Joint Health
Health insurance professionals can promote bone and joint health by educating clients about the importance of preventative services and routine checkups.
By CalBroker Mag
50
MEDICARE HEALTH TOPICS
GLP-1 Transforming Obesity Treatment and Insurance Coverage
Discover the groundbreaking potential of GLP-1 agonists in tackling obesity.
By Misty Baker
52
MEDICARE HEALTH TOPICS Aging Powerfully
Learn three tips for aging with power.
By Megan Wroe MS,RD,CNE,CLEC
54
MEDICARE PATIENT CARE
Top Five California Hospitals for Medicare Patients
Here’s a roundup of the top five hospitals in the state that stand out for their commitment to Medicare.
By Emma Peters
PUBLISHER
Phil Calhoun Health Broker Publishing, LLC publisher@calbrokermag.com
ART DIRECTOR Randy Dunbar Randy@calbrokermag.com
PRODUCTION DIRECTOR
Zulma Mazariegos Zulma@calbrokermag.com
DIGITAL DIRECTOR Carmen Ponce Carmen@calbrokermag.com
PUBLISHER'S ASSISTANT Emma Peters Emma@calbrokermag.com
CIRCULATION
zulma@calbrokermag.com
120,000 subscribers 12,000 monthly website visits
ADVERTISING
Health Broker Publishing 14771 Plaza Drive Suite C Tustin, CA 92780 714-664-0311 publisher@calbrokermag.com
publisher@calbrokermag.com
Subscriptions: U.S. one year: $24. Send change of address notification at least 20 days prior to effective date; include old/new address to:
Health Broker Publishing 14771 Plaza Drive Suite C • Tustin, CA 92780 714-664-0311
California Broker (ISSN #0883-6159) is published monthly. Periodicals Postage Rates Paid at Burbank, CA and additional entry offices (USPS #744-450).
POSTMASTER: Send address changes to California Broker, 14771 Plaza Drive Suite C • Tustin, CA 92780
©2024 by Health Broker Publishing. All rights reserved. No part of this publication should be reproduced without consent of the publisher.
No responsibility will be assumed for unsolicited editorial contributions. Manuscripts or other material to be returned should be accompanied by a self-addressed stamped envelope adequate to return the material. The publishers of this magazine do not assume responsibility for statements made by their advertisers or contributors.
PUBLISHER'S NOTE
BY PHIL CALHOUN
Thank You’s—Thank you to our article contributors as collectively we have put together this Medicare Special issue. We hope you will enjoy the information in our Medicare Special issue covering sales and marketing, compliance and legislation, and valuable and timely tips on ways to be the best client advocate possible.
Let us know what you think — publisher@calbrokermag.com
In this Issue:
With the amount of change proposed and approved by CMS for Medicare in 2025, one thing is clear, the impact will be felt at all levels of the Medicare insurance industry. We have tried to cover as many topics as possible that we feel health insurance professionals will find valuable.
Please stay connected to and learn from insurance carriers, healthcare providers, FMOs, and General Agencies about these changes as the impact is clarified and the industry responds.
Our GOAL:
Our Goal is to help Medicare insurance professionals access news and stories they need to help their clients navigate Medicare changes in 2025. Please contribute your ideas and share tips you feel will help all in the industry to both focus practices during the coming 2025 Annual Election Period.
Our Commitment:
California Broker media is committed to help provide current an to assist health insurance professionals to be the best advocat this issue and always, we source health insurance industry news and local sources. Since 1981 Cal Broker has been the industry have provided information to our subscribers in our weekly and
Our subscribers, currently totaling 110,000 licensed life and health insurance agents and brokers, represent 75% of Medicare beneficiaries in California.
We are proud to state that our subscribers include ALL California licensed life and health insurance professionals.
• 50% of Cal Broker subscribers offer Medicare plans
• 65% of Cal Broker subscribers offer both Group and Medicare plan
At the time of this publication deadline, the most recent Medic included. Our eNewsletters also will have updates as they beco
Please let us know how you enjoy Cal Broker email us.
CMS Increases broker compensation for 2025 MAPD and PDP. Learn More on page 35


Many people with Medicare Part D drug coverage—in particular those who reach the catastrophic coverage phase may experience unexpected costs and significant confusion as their out-of-pocket obligations change throughout the year.
The Inflation Reduction Act (IRA) brings much-needed consumer protections and predictability to these coverage phases, limiting financial exposure for everyone and generating significant savings for those with extreme costs.
As of 2024, Part D enrollees are no longer required to pay 5% coinsurance after they reach catastrophic coverage. This threshold is set at $8,000 in what’s called “true out-of-pocket,” or TrOOP costs. These amounts include what the beneficiary spends on covered prescriptions, what others, like family members, friends or certain charitable organizations spend on their behalf, and any manufacturer discounts during the coverage gap phase. This calculation is different than what’s called “total drug costs,” which includes TrOOP amounts plus the what the Part D plan has paid.
Most people will pay roughly $3,400 of their own money by the time they reach $8,000 in TrOOP costs. After this point, they will pay $0 for covered Part D drugs for the rest of 2024. Exactly how much a person will pay before they reach the TrOOP limit of $8,000 depends on their plan design, and the mix of brand name and generic drugs they take – this is because while the brand-name manufacturer discount in the coverage gap is included in TrOOP, the government-funded generic discount is not. If a person takes only brand-name medications, they will pay around $3,300 before they hit the catastrophic cap, while a person who takes an average amount of brand and generic drugs will pay about $3,400. A person who takes only generic drugs will pay close to the full $8,000 before they reach the catastrophic phase.
Further savings and simplifications are coming. Starting in 2025, beneficiary drug costs will be capped at $2,000, indexed annually for growth in Part D. There will be no change of payment responsibility in the coverage gap, and no differential treatment of the manufacturer discounts for brand and generic drugs. Instead, out-of-pocket expenses will be defined in a way that more closely matches the usual understanding of that term, and once a beneficiary spends $2,000 in the deductible and initial coverage phases, they will pay $0 out-of-pocket for the rest of the year.
To illustrate the impact of these changes, a recent KFF report examined three commonly taken cancer drugs, each priced at well over $100,000 a year. In 2023, Medicare Part D enrollees who used any of these drugs for the entire year faced nearly $12,000 in out-of-pocket costs. In 2024, they will no longer be responsible for $8,000 to $9,000 of that amount. And next year, when the $2,000 cap takes effect, they’ll save even more.
The IRA’s Part D redesign will help millions of current and future enrollees afford needed care. These reforms come on top of the law’s other beneficiary cost saving provisions, many of which have flown under the radar—such as vaccines without cost sharing, reduced insulin costs, expanded access to “Extra Help,” and the drug negotiation program that is already underway and in 2026 will bring down prices for some of the most expensive Part D drugs. Medicare Rights applauds these reforms and urges policymakers to build upon them, to make high quality coverage more available and affordable for more Americans.
By Richard Eisenberg
It may be months before the calendar flips to 2025, but not for Medicare. The Centers for Medicare & Medicaid Services (CMS), which runs the program, just announced two major changes for 2025 you’ll want to know about. Next year, Medicare will also dramatically alter the maximum amount beneficiaries will need to pay out-of-pocket for their covered medications.
Here’s the lowdown on these three ways Medicare will operate differently in 2025 and what they’ll mean for you.
1. A crackdown on agents and brokers who sell three types of Medicare policies
Currently, salespeople sometimes get incentives like exotic vacations and hefty bonuses when they enroll Medicare beneficiaries into private insurers’ Medicare Advantage plans (alternatives to traditional Medicare), or Medigap (Medicare supplemental), or Part D prescription drug plans. CMS hopes to end sales incentives in 2025 for Medicare Advantage and Part D plans. “This announcement is a big win for seniors because it strengthens protections against deceptive and high-pressure marketing practices,” Senate Finance Committee Chairman Ron Wyden (D-Ore.) said in a statement. The new clampdown, in CMS’s 1,327-page final rule for Medicare in 2025, states that it aims to “ensure that agent and broker compensation reflect only the legitimate activities required by agents and brokers” selling those plans. That means the salespeople can no longer be offered incentives to enroll people. In addition, the rule says, Medicare middlemen known as third-party marketing organizations won’t be able to offer incentives that “inhibit an agent or broker’s ability to objectively assess and recommend the plan that is best suited to a potential enrollee’s needs.” Marvin Musick, whose MedicareSchool.com sells Medicare policies, tells Fortune, “I think it’s a really good idea, because the agents should not be incentivized to favor one company or another.” The new rule also says it will stop brokers and agents from receiving “administrative fees” above Medicare’s fixed compensation caps. In most states, that cap has been $611 for new Medicare Advantage signups and $306 for renewals. Part D plans have had lower caps: $100 for initial enrollment and $50 for renewals. In 2025, the government will increase the compensation for initial enrollments in Medicare Advantage and Part D plans by $100—more than three times higher than CMS initially proposed. “It’s much higher than most people in our business were anticipating,” says Musick. Consumer activists at the Center for Medicare Advocacy and the Medicare Rights Center believe that even with the rule changes, brokers and agents will still have a significant incentive to steer people into Medicare Advantage plans.
That’s because the rule will continue letting salespeople earn far more selling those plans than stand-alone Part D prescription drug plans, which some people with traditional Medicare buy along with Medigap policies. “This won’t really address the issue of pushing people toMedicare Advantage,” says David Lipschutz, associate director of the Center for Medicare Advocacy. “What I think it will do is restrict or limit people from being steered toward
one particular plan because that agent or broker is trying to get a particular bonus or other incentive.” Philip Moeller, author of the forthcoming book Get What’s Yours for Medicare, says the new rule “simply reinforces the need for consumers to ask some basic questions when they’re dealing with a broker.” Agents and brokers don’t sell every Medicare Advantage, Part D, or Medigap plan available in a local area, he noted, just a selection of them. Once you know which plans your broker can sell, Moeller advised, “go to Medicare’s Plan Finder tool and look at the available products in your zip code and see what’s missing” from the salesperson’s choices.
2. A new midyear notification to Medicare Advantage policyholders reminding them about their plan’s unused supplemental benefits That’s coming because people in these plans often don’t take advantage of some benefits.
This is somewhat surprising since Medicare Advantage plans often tout the coverage that they provide and traditional Medicare can’t—dental, vision, hearing, and fitness benefits. Most Medicare Advantage plans offer at least one supplemental benefit, and the median number provided is 23, according to CMS.
But a February 2024 Commonwealth Fund study discovered that three in 10 Medicare Advantage members didn’t use any of their supplemental benefits in the past year. And CMS’s statement about its 2025 rule said that “some plans have indicated that enrollee utilization of many supplemental benefits is low.”
The Commonwealth Fund found in 2022 that supplemental benefits were the most common reason people cited for choosing a Medicare Advantage plan over traditional Medicare.
So, starting in 2025, Medicare Advantage plans will be required to send policyholders each July a personalized “Mid-Year Enrollee Notification of Unused Supplemental Benefits.”
READ FULL ARTICLE https://bit.ly/3xEV9Ou

By David Garcia, Co-Chair of CAHIP’S Medicare Committee
Here is an easy way to remember how this applies directly below. Medicare –Part B, Does NOT view Cobra (including Cal-Cobra) as Creditable coverage.
Medicare Products – Medicare Supplement, Medicare Advantage and Part D, Does View Cobra (including Cal-Cobra) as Employer Sponsored Coverage
Example 1 – Employer Sponsored coverage ended 12/31/23 – employee has 8 months, through 8/31/24, to enroll in Part B of Medicare without penalty
• The employee will use losing/leaving employer sponsored coverage to enroll in Medicare Part B
• Same employee above enrolled in Cobra because of a younger spouse or dependents
• Reaches out to you, 9/1/24 or later – does not have access to enroll in to Part B of Medicare until Medicare General Enrollment Period 1/1/25-3/31/25
• For a first of the following month effective date
• Why? Because Cobra is not creditable coverage for Part B
Example 2 – An existing Cobra enrolled reaches out to you, however, while on Cobra, they already activated Part B of Medicare
• Can apply for Medicare Supplement and Part D with any carrier when they decide to leave, creditable (for Part D purposes) Cobra/Cal-Cobra or Cobra/Cal-Cobra ends
• Either way doesn’t matter
• Will be guarantee issue with All Medicare Supplement and Part D carriers
• The scenario above will also create a guarantee issue in to ANY carriers Medicare Advantage plan using Leaving/Losing Employer Sponsored coverage SEP
By Lindsey Copeland
While most older adults are automatically enrolled in Medicare Part B because they are receiving Social Security benefits at age 65, a growing number are not. In 2016, only 60% of Medicare-eligible 65-year-olds were taking Social Security, compared to 92% in 2002.
Several factors are responsible for this shift, including the decoupling of the Medicare and Social Security eligibility ages, changing demographics, and evolving employment patterns. For example, more older adults are working later in life and deferring Social Security, though they may not realize that doing so impacts their Medicare enrollment and coverage. Others may choose—appropriately or not—to delay Medicare in reliance on other coverage, such as an employer-based plan.
Unlike those who are automatically
enrolled, when this cohort signs up for Part B they must actively navigate a thicket of complicated Medicare rules and stringent deadlines. Mistakes are common and carry serious consequences, like harsh late enrollment penalties.
The Part B late enrollment penalty (LEP) was designed to encourage individuals to enroll in Medicare when they are first eligible, rather than waiting until they are sick and more costly to insure, and ultimately to guarantee a balanced Medicare risk pool. But because Medicare enrollment rules are so complex, many people end up paying the LEP due to honest error. The impact on these beneficiaries is significant. For as long as they have Medicare, they must pay their monthly Part B premium plus an additional 10% for each year they delayed signing up. In 2021, an estimated 779,400 Medicare beneficiaries were paying the Part B LEP, with the average penalty
increasing their monthly premium by nearly 30%.
A recent issue brief from the AARP Public Policy Institute (PPI) examines these delays, penalties, and opportunities for reform.
Ease Access to Medicare Savings Programs — When an individual is enrolled in a Medicare Savings Program (MSP) that pays their Part B premium, they do not have to pay a Part B penalty. However, the MSPs are chronically under-enrolled, while outdated systems and eligibility rules further hinder access. Streamlining rules and otherwise increasing program uptake would expand participation and protect more people from costly LEPs.
READ FULL ARTICLE
https://bit.ly/3VHVRmq
BY RYLEE WILSON
Across racial and ethnic groups, MA enrollees report broadly similar experiences but wide disparities in outcomes.
CMS published its annual report on disparities in healthcare among Medicare Advantage enrollees May 2. The report reviews patientreported experiences and Healthcare Effectiveness Data and Information Set measures.
The report identified the widest disparities among groups in behavioral healthcare and diabetes care.
Here are 10 numbers to note:
1.In 2023, Asian American and Native Hawaiians and Pacific Islanders, Black, Hispanic, and multiracial people with Medicare were more likely to be enrolled in MA than American Indians and Alaska Native and white people with
Medicare in 2023. Female Medicare beneficiaries were also more likely to enroll in MA than male beneficiaries.
2.Disparities on clinical care outcomes were most significant among American Indian/Alaska Native and Black enrollees. American Indian/Alaska Native enrollees had outcomes below the national average on 10 of 27 measures, and Black enrollees had outcomes below the national average on 18 of 41 measures.
3.American Indian/Alaska Native enrollees had the largest deficits compared to the national average among diabetes care measures.
4.Black enrollees had wide disparities in behavioral care, cardiovascular care, diabetes care and care coordination.
5.Clinical care scores were more mixed among Asian American and Native Hawaiian/Pacific Islander and Hispanic populations. Asian American and Native Hawaiian/ Pacific Islander enrollees had outcomes lower than the national average on 5 of 41 measures, and higher than the national average on 13 measures. Hispanic enrollees had outcomes below the national average on 11 measures and above the national average on 12 measures.
6.For Asian American and Native Hawaiian/Pacific Islander beneficiaries, the largest deficit compared with the national average was treatment for alcohol and drug addiction.
7.Among Hispanic populations, the widest disparities were in alcohol and drug addiction treatment and cardiac rehabilitation.
8.CMS uncovered fewer significant differences across patient experience measures. Black and multiracial enrollees had flu vaccination rates considerably below the national average, according to the report.
9.Asian American and Native Hawaiian/Pacific Islanders reported difficulty getting appointments and care quickly at higher rates than other groups.
10.CMS is targeting policies to improve access to behavioral healthcare and diabetes care, the areas with the widest disparities among racial groups, according to the report.
By David Garcia, Co-Chair of CAHIP’S Medicare Committee
Every now and again you’ll get a request from an active member about an issue they’re having with Medicare. Who should you/they contact when this happens? The info below provides some detail as to who should be contacted and for which circumstance. Medicare and Social Security are inextricably linked. Beneficiaries and agents have long been confused by whom to call for a given situation. Below are a few of the more common Medicare and Social Security questions that arise and whom to call for answers. Medicare (www.Medicare.gov; 1-800-Medicare)
1. What is covered under Medicare Part A and Part B
2. Original Medicare’s deductibles and other costs
3. Information on how to appeal a Medicare claim
4. Authorize another person to oversee your account/talk on your behalf, assist with claims
5. Find doctors and other providers who accept Medicare
6. Research Medicare Part C and D plans on the Plan Finder
7. Find supplement (Medigap) companies in a particular state
8. Find quality-of-care information on nursing homes, hospitals, home health agencies and dialysis centers
9. Download or request the annual “Medicare and You” booklet be mailed
10. Research a library of pamphlets to download or be mailed on Medicare benefits and some Medicare regulations
11. Request a new Medicare card (links you to Social Security)
Social Security (www.ssa.gov; 1-800-772-1213)
1. Enroll in Part A and B of Medicare
2. Find out if eligible for Medicare
3. Find out premiums for Part A, if applicable, and Part B
4. Appeal Income Related Monthly Adjustment
5. Apply for the Extra Help Program (Part D financial assistance based on income)
6. Report a death
7. Search a library of pamphlets to download or be mailed on Social Security topics
8. Set up direct deposit
9. Change name, address, phone and bank
10. Request a new Medicare card
11. Print proof you do not receive benefits
12. Request a replacement Social Security or Medicare number
13. Get personalized retirement benefit estimates for yourself and spouse
14. Information on disability and when eligible for Medicare
Millions of People with Medicare Will Benefit from the New Out-ofPocket Drug Spending Cap Over Time
A KFF analysis shows that a new out-ofpocket spending cap in Medicare Part D could translate into savings for well over 1 million beneficiaries when it takes effect next year, including more than 100,000 people each in California, Florida and Texas, based on analyses of drug
spending in 2021.
The $2,000 cap, part of the Inflation Reduction Act of 2022, will lead to thousands of dollars in savings for Medicare patients who take high-cost drugs for cancer, rheumatoid arthritis, and other serious conditions.
This new limit follows the elimination this year of a longstanding requirement that Part D enrollees pay 5% of their drug costs out-ofpocket after their drug
expenditures reach a certain threshold.
Based on KFF’s review of Part D drug claims data, if the cap been in place in 2021, 1.5 million Medicare beneficiaries would have benefited because their out-of-pocket costs for prescription drugs exceeded $2,000. Of the total 1.5 million, about 200,000 Medicare beneficiaries spent $5,000 or more for their prescriptions that year, while another 300,000 expended
between $3,000 and $5,000. The rest spent between $2,000 and $3,000.

By Juliette Cubanski, Tricia Neuman, and Anthony Damico

In 2025, Medicare beneficiaries will pay no more than $2,000 out of pocket for prescription drugs covered under Part D, Medicare’s outpatient drug benefit. This is due to a provision in the Inflation Reduction Act of 2022, which included several changes to the Medicare Part D program designed to lower patient out-of-pocket costs and reduce what Medicare spends on prescription drugs. This new $2,000 cap (indexed annually to the rate of change in Part D costs) comes on top of the elimination of 5% coinsurance in the catastrophic coverage phase of the Part D benefit, in effect for 2024, which translates to a cap of about $3,300 out of pocket for brand-name drugs. These benefit design changes will save thousands of dollars for people who take highcost drugs for cancer, rheumatoid arthritis, and other serious conditions.
If a $2,000 cap on out-of-pocket drug spending had been in place in 2021, 1.5 million Medicare beneficiaries enrolled in Part D plans would have saved money because they spent $2,000 or more out of pocket on prescription drugs that year. This estimate is based on KFF analysis of Medicare Part D prescription drug claims data for enrollees without Part D low-income subsidies in 2021 (the most recent year available for this analysis). Among these 1.5 million enrollees, most (1.0 million or 68%) spent between $2,000 and $3,000 out of pocket, while 0.3 million (20%) had spending of $3,000 up to $5,000, and 0.2 million (12%) spent $5,000 or more out of pocket.
Over the course of several years, however, far more Part D enrollees will stand to see savings from this new out-of-pocket spending cap than in any single year. A total of 5 million Part D enrollees had out-of-pocket drug costs of $2,000 or more in at least one year during the 10-year period between 2012 and 2021, while 6.8 million Part D enrollees have paid $2,000 or more out of pocket in at least one year since 2007, the first full year of the Part D program (Figure 1).
In most states, tens of thousands, if not hundreds of thousands, of Medicare beneficiaries will feel relief from the new Part D out-of-pocket spending cap (Table 1). In California, Florida, and Texas, more than 100,000 Part D enrollees faced out-of-pocket
costs of $2,000 or more in 2021, and in another 6 states (New York, Pennsylvania, Ohio, Illinois, North Carolina, and New Jersey), between 50,000 and 82,000 did so. As at the national level, more Part D enrollees in each state will benefit over time. For example, in Iowa, Louisiana, and Maryland, 73,000 Part D enrollees faced out-of-pocket costs of $2,000 or more in at least one year between 2012 and 2021. In Michigan, New Jersey, and Georgia, 148,000, 158,000, and 159,000 Part D enrollees, respectively, spent $2,000 or more in at least one year over this same 10-year period. In Texas, 364,000 Part D enrollees did so; in Florida and California, around 400,000 enrollees or more.
Capping out-of-pocket spending will help Part D enrollees with relatively high drug costs, which may include only a relatively small number of Part D enrollees in any given year but, as this analysis shows, a larger number over time. People who will be helped include those who have persistently high drug costs over multiple years and others who have high costs in one year but not over time. While a cap on out-of-pocket costs will help millions of Part D enrollees over time, higher plan costs to provide the Part D benefit could also mean higher plan premiums, a dynamic that the Inflation Reduction Act’s premium stabilization provision was designed to mitigate. Although KFF polling shows that a relatively small share of older adults is aware of the Inflation Reduction Act’s $2,000 cap on out-of-pocket drug costs for Part D enrollees that takes effect in 2025, millions of them will benefit from this cap in the years to come.
By Nancy Ochieng, Jeannie Fuglesten Biniek, Meredith Freed, Anthony Damico, and Tricia Neuman
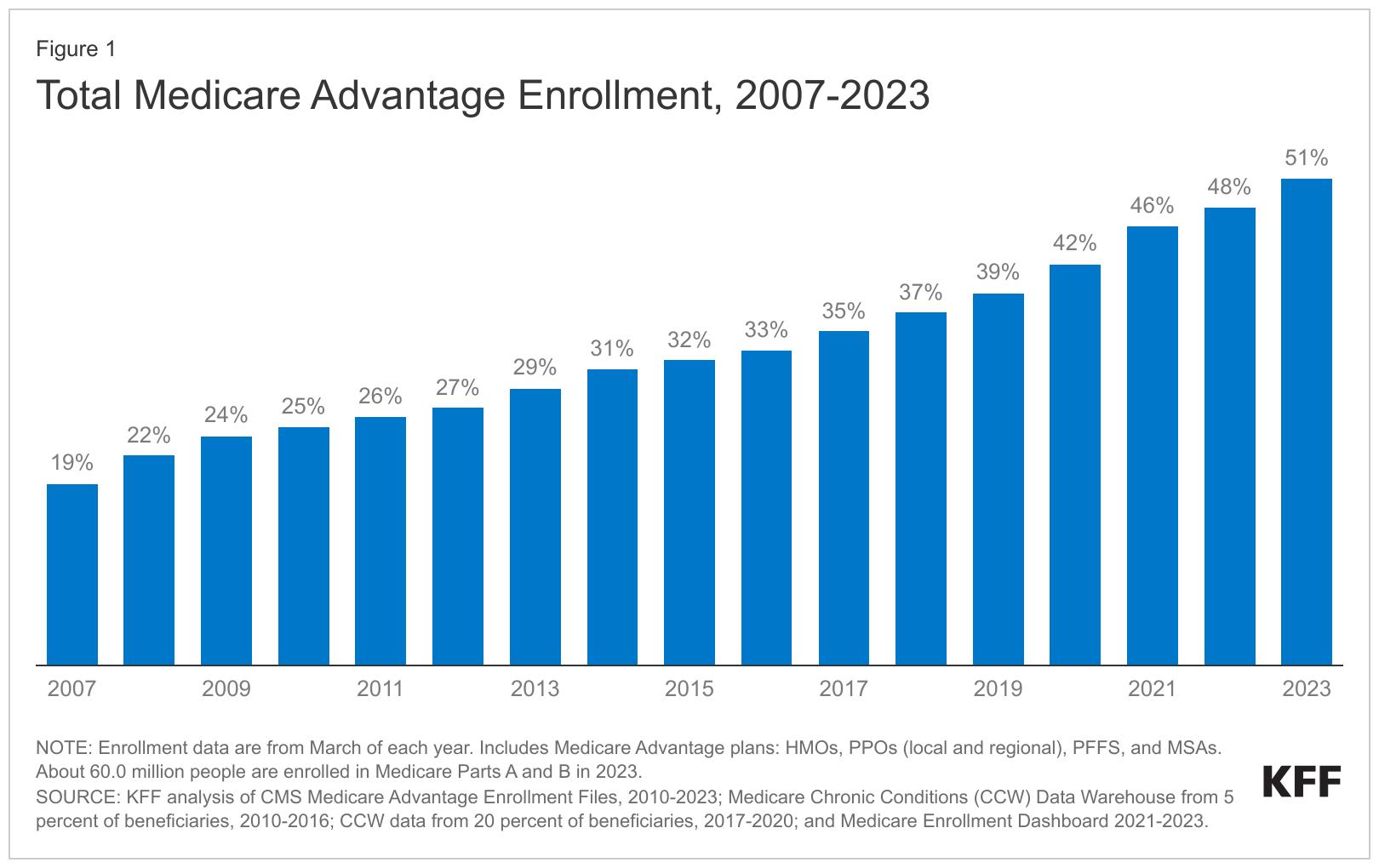
Medicare Advantage enrollment has been on a steady climb for the past two decades following changes in policy designed to encourage a robust role for private plan options in Medicare. After a period of some instability in terms of plan participation and enrollment, The Medicare Modernization Act of 2003 created stronger financial incentives for plans to participate in the program throughout the country and renamed private Medicare plans Medicare Advantage. In 2023, 30.8 million people are enrolled in a Medicare Advantage plan, accounting for more than half, or 51 percent, of the eligible Medicare population, and $454 billion (or 54%) of total federal Medicare spending (net of premiums). The average Medicare beneficiary in 2023 has access to 43 Medicare Advantage plans, the largest number of options ever.
To better understand trends in the growth of the program, this brief provides current information about Medicare Advantage enrollment, by plan type and firm, and shows how enrollment varies by state and county. A second, companion analysis describes Medicare Advantage premiums, out-of-pocket limits, cost sharing, extra benefits offered, prior authorization requirements, and star ratings in 2023.
Key highlights include:
More than half (51%) of eligible Medicare beneficiaries are enrolled in Medicare Advantage in 2023.
The share of Medicare beneficiaries enrolled in Medicare Advantage varies widely across counties. In 2023, nearly one third (31%) of Medicare beneficiaries live in a county where at least 60 percent of all Medicare beneficiaries are enrolled in Medicare Advantage plans, while 10% live in a county where less than one third of all Medicare beneficiaries are enrolled in Medicare Advantage plans. The wide variation in county enrollment rates could reflect several factors, such as differences in firm strategy, urbanicity of the county, Medicare payment rates, number of Medicare beneficiaries, health care use patterns, and historical Medicare Advantage market penetration.
Medicare Advantage enrollment is highly concentrated among a small number of firms. UnitedHealthcare and Humana account for nearly half (47%) of all Medicare Advantage enrollees nationwide, and in nearly a third of counties (32%; or 1,013 counties), these two firms account for at least 75% of Medicare Advantage enrollment.
More than half of eligible Medicare beneficiaries are enrolled in Medicare Advantage in 2023
In 2023, more than half (51%) of eligible Medicare beneficiaries – 30.8 million people out of 60.0 million Medicare beneficiaries with both Medicare Parts A and B – are enrolled in Medicare Advantage plans. Medicare Advantage enrollment as a share of the eligible Medicare population has jumped from 19% in 2007 to 51% in 2023 (Figure 1).
READ FULL ARTICLE
https://bit.ly/4c2Tlhp
By Juliette Cubanski and Tricia Neuman
Changes in 2025 include a new $2,000 out-of-pocket spending cap, elimination of the coverage gap phase, a higher share of drug costs paid by Part D plans in the catastrophic phase, along with a new manufacturer price discount and reduced liability for Medicare in this phase, and changes to plan costs and the manufacturer price discount in the initial coverage phase.
Out-of-pocket drug spending will be capped at $2,000
Beginning in 2025, Part D enrollees’ out-of-pocket drug costs will be capped at $2,000. This amount will be indexed to rise each year after 2025 at the rate of growth in per capita Part D costs. (This cap does not apply to out-of-pocket spending on Part B drugs.)
For Part D enrollees who take only brand-name drugs, annual out-of-pocket costs at the catastrophic threshold will fall from around $3,300 in 2024 to $2,000 in 2025 (Figure 3). In other words, Part D enrollees who take only brands and have drug costs high enough to reach the catastrophic threshold could see savings of about $1,300 in 2025 relative to what they will spend in 2024.
The coverage gap phase will be eliminated
The coverage gap phase, where Part D enrollees had faced 100% of their total drug costs under the original Part D benefit design and currently face 25% of costs for brand and generic drugs, will be eliminated in 2025. This means that Part D enrollees will no longer face a change in their cost sharing for a given drug when they move from the initial coverage phase to the coverage gap phase, which is the case in most Part D plans today, since most plans charge varying cost-sharing amounts, rather than the standard 25% coinsurance, in the initial coverage phase.
Medicare Summits
August 14
@10:00am-5:30pm CAHIP-LA Medicare on the LaLa Land Stage-The Sequel, REGISTER
August 20-22 NABIP Senior Summit @ Pechanga Resort Casino, REGISTER
August 28 @8:00 am-4:00pm, 2024 SAHU Business Medicare Expo, REGISTER JULY
July 11
@2:30-4:30pm:(EPI-OC) Helping Owners Reduce Risk With Business Continuity Planning @Costa Mesa, REGISTER
July 17 @11:00am-1:00pm: (EPI-Conejo Valley) Showdown: Trivia for the Top Guns @Westlake Village, REGISTER
July 17@2:30pm-4:30pm, (EPI –SD) Helping Owners Reduce Risk With Business Continuity Planning @San Diego, REGISTER
July 24 @2:30pm-4:30 pm, (EPI-LA) Aligning Generations: Family Governance in Business and Philanthropy @Los Angeles, REGISTER
July 25 @2:30-4:30pm, (EPI-IE) The Nuts and Bolts of a Family Transaction @Ontario, REGISTER
Virtual Trainings
July 2 @1:00pm-2:00pm EST: (EPI) Quality Earnings and the Exit Planning Process, REGISTER
July 3 @10am, Strategies for Successful Client Retention, Join Live Webinar
July 9 @1:00pm-4:00pm PT: BuddyIns & Amada Senior Care Present: Partnerships for a Winning Team, REGISTER
July 9 @1:00pm-2:00pm EST: (EPI) The Hidden Risks & The Role of Cybersecurity in M&A, REGISTER
July 16 @1:00pm-2:00pm EST: Strategies of the Ultra-Wealthy: How They Increase Net Worth, Maximize Wealth Transfer, and Minimize Estate Taxes, REGISTER
July 17 @3:00pm NABIP Medicare Moments: Compliance and Cyber Security, REGISTER
July 18 @8:00am-9:30am, (CAHIP LA) Breakfast Bytes: Long Term Care, Retirement Planning & Financial Wellness, REGISTER
July 22-25,BBSI Benefits Golden State Brokers Tour, Location: Varies; REGISTER
July 23 @1:00pm-2:00pm, Growing Enterprise Value Through Aligned Executive Compensation Planning, REGISTER
July 25 @11:30am, NAIFA-LA, Q3 – Annuities: Master Annuities and Grow your Sales, REGISTER
October 6-8 NAIFA e3 Conference @ Sonesta Redondo Beach &
By Tiffany Stiller, SVP Carrier Relations and Individual & Senior Division, BenefitMall
Field Marketing Organizations, referred to as FMOs, provide benefits to agents, carriers, and consumers with the variety of services they provide. Bringing together a myriad of products, educational support, and technology tools, FMOs elevate an agent’s ability to offer choice to their clients while streamlining and simplifying the enrollment process. This applies to all products an FMO might represent but is especially relevant when navigating the complexities of the Medicare space.
For carriers, FMOs assist in containing costs by taking on several services such as agent education, marketing, certification and agent contracting support as well as enrollment and issue resolution. They assist the carrier in casting a wider net and exposing more agents and their clients to a carrier’s product offering. FMOs only get paid when a sale is completed and without this variable cost support, carriers would have to increase staffing and support driving up costs.
Agents enjoy the support of sales executives within an FMO that help them identify their target market, direct them to the appropriate carriers to partner with for that segment, and introduce them to new and competitive products that can better support their clients and expand their market reach. End Pullquote. These sales executives can also assist in getting a new agent up and running in the senior space, guiding them through all the steps it takes to get ready to sell and working on a strategy with the agent that will help them to penetrate the market and succeed in the marketplace.
Technology is an essential part of our business, and for many agents the cost of this technology could be a barrier to entry. FMOs provide access to both proprietary and partner tools often shouldering the cost, allowing the agent to invest in other aspects of their business. Quoting, enrollment, contracting/appointment, provider search, and client management are all examples of the electronic capabilities made available to agents by FMOs. Marketing is also an area where an FMO can assist an agent with business costs. Most will provide co-op dollars helping an agent to promote their services and the products they represent, and many will also provide templates for agents that allow them to create their own marketing campaigns.
Information is key in this business and an FMO supports their carrier partners in pushing news out to the agent community and giving agents a single source to keep up to date on the market. This ranges from information about new products, new tools, benefit changes and regulatory updates. Several mediums are utilized including email blasts, newsletters, blogs, social media, and in-person educational events. Many FMOs also provide compliance support, helping to navigate the ever-changing world of benefits and legislative updates. At its best, an FMO is a partnership with its carriers and agents and is only successful when they’re successful, making them top priority. The result is a consumer connected with a large variety of options, allowing them to make the best choice for their unique needs--truly a win for our industry and the customers we serve.

Headquartered in Dallas, BenefitMall is the largest employee benefits general agency, working with a network of 20,000 brokers to deliver employee benefits to more than 200,000 small and medium-sized businesses. Through its Individual and Senior Division, BenefitMall also provides brokers with access to individual and family life, health and ancillary plans, Medicare Advantage, and Medicare Supplement insurance programs. Founded in 1979, BenefitMall leverages innovative technology backed by human expertise to provide a seamless selling experience for its carriers, brokers, and their clients. BenefitMall is part of CRC Group’s Life, Retirement and Benefits Solutions division, a leading national wholesale distributor of specialty insurance products.

Tiffany Stiller has been with the BenefitMall team since 1999. In her current role as Senior Vice President she oversees Carrier Relations, BenefitMall Individual & Senior Division (ISD), Product, Compliance and the Learning & Development team. As part of BenefitMall’s Executive Leadership her focus is on driving both the growth and culture of the organization.
Prior to joining the BenefitMall team, she spent four years as Vice President of Business Development with Secure Dental, where she was responsible for negotiating General Agency contracts, resolving general agency and broker issues, product advertising and promotion, plan design, and monitoring sales and distribution in 17 states. Previously, Stiller was Marketing Director for a large group of orthopedic surgeons in Southern California and Nevada.
Stiller worked on a bachelor of science degree in Health Science at California State University, Northridge, and earned her bachelor of arts degree from Arizona State University (ASU). She is a member of the National Association of Benefits and Insurance Professionals (NABIP) and The Council. She is Life and Health licensed in all 50 states. Stiller also serves as an advisor for Kappa Kappa Gamma Fraternity. In her free time, she is a competitive equestrian and devoted dog mum.
By Elliott Martin Martin & Associates Insurance Services, Inc.
Have you ever pushed a fax machine so hard to the point where it overheats?
Believe it or not, that was the error message my brother Mo and I were getting while trying to fax in all the Part D applications that had come in the mail that day during AEP not too long ago.
Yes, we were using an actual printer/fax machine!
Our dad, Ray, has been in the insurance industry for over 30 years and has focused on Medicare more specifically for over the last 25+ years. Being in the business for that long means lots of clients to serve during AEP. Eventually we got to the point where our current systems were being pushed to their limits.
We knew there had to be a better way and there was, but we just had to execute on it.
Then the pandemic hit, and we had no choice but to find a better way to keep up with the volume or inquiries coming in. It was time to bring our agency properly into the 21st century and incorporate some of the technological advances within the industry and incorporate automation into our systems.
Since then, we’ve been able to increase our revenue, streamline our processes and toss the fax machine in the dump. In fact, having systems gets you results and the better your systems, the less stress, less labor and faster you get to your goals.
Keep reading, this is VERY important! I’m going to share with you the systems we’ve developed that if you implement them will take you to the next level.
Here they are, the 5 automation tools that we have found extremely useful at making us more efficient and more profitable, especially during AEP:
When it comes to CRMs for Medicare specific agencies, what we’ve discovered (and you may have as well) there’s not really one system that does it all. Some do everything, except the actual enrollments. Some do everything else but can’t track commissions. If you are anything like us, you’ve had to piece together different systems.
The main automation features we’ve been able to find in the CRM we’ve selected include automated emails to clients as their policies are approved, profile creation based on opt-in from landing page forms and appointment requests, commission tracking and automated task creation for internal tasks to be completed by other members of our team. You must have a SMART system to help manage your clients.
You must have systems that organize, automate and replicate results over and over without your labor!
Get in touch with your FMO! They may have tools at their disposal including systems like Lead Advantage Pro, Sunfire and others that allow you to create profiles for your clients, save their prescription lists, send pre-generated emails to clients to update their prescriptions, sending Scope of Appointments and most importantly, sending/submitting electronic enrollments as well as self-service enrollment tools for your clients too. I can’t tell you how much time this has saved us!
If you do not have an online calendar service (Acuity or Calendly come to mind) that syncs with your email service calendar (Outlook, Google) and allows prospects and clients to schedule phone/Zoom/ Teams or even in-person meetings with you, drop everything you are doing now and start working on this.
Talk about time saving! Having a system that allows a prospect (and clients) to select the time on your calendar when you decide to be available is huge. Think about that, you don’t have to talk on the phone (saved 1 phone call) to schedule a meeting with the prospect. They select the meeting time themselves!
One way we’ve been able to capture contact information from prospects interested in our services has been using an automated service that can easily create landing pages. There are services that have user friendly drag and drop options where you can create your own landing page or website. This allows you to easily create a spot online for folks to request information and content from you (think guides, books, tutorials, webinars, articles, etc.) in exchange for their contact information.
We’ve been using landing pages as a great lead generation system and once the prospective person requests the information they want, we capture their information, and they go into our automated pipeline to receive e-mails, invitations and even e-birthday cards. This makes us stand out from the other marketing noise prospects.
The last automation tool that helps piece together a lot of the systems above is a service called Zapier. For example, we use Zapier to relay information from the landing pages and online calendar into our main CRM system so that we DO NOT have to duplicate data entry. Can you say, ‘TIME SAVER’. That’s huge! Zapier is an automated service that glues everything together. Think of it like the electrical system in your car, everything works together once you turn on the juice.
It’s fine to have goals to reach, but goals alone won’t get you the results you want. As many of the most successful business leaders will tell you, systems are the key! You must have systems that organize, automate and replicate results over and over without your labor!
You should start today, seek to implement these systems NOW, before AEP gets here. I promise you it will have a dramatic change to your business and results for this AEP and beyond.
Good luck to you and your team this AEP!
Want to get a complete list of the automation tools we’ve adopted or are looking to adopt for our Medicare business?
www.martinmedicare.lpages.co/automate/

Elliott Martin is an agent at Martin & Associates Insurance Services, Inc. based in Irvine, CA, the company his father Ray Martin founded. He has been insurance licensed and involved in the Medicare space since 2014.
Elliott has helped thousands of individuals with personal Medicare insurance needs and has also helped Martin & Associates develop and improve the agency systems and automations. In his free time Elliott enjoys playing in a men’s slow pitch softball league, pickleball and spending time with his wife Kaycee and daughter Avery.
BY PHIL CALHOUN
Phil: Steve welcome to Cal Broker and special issue for July focused on Medicare.
We want to get to know you and First Sierra. We also want to dive into your thoughts about the upcoming challenges for Agents going into the 2025 Annual Election Period.
Steve: First Sierra Insurance Services provides top level Value Based Services to its independent agents.
Our why story is very simple. We are an agency built by agents for agents. We found a need in the market and we were able to address that need because of our experience being agents in the field.
We have over 300 agents spread out throughout California and Nevada. Over the years we have added additional internal support staff to assist our agents. We have also added tools such as a multi-carrier enrollment and quoting platform and an integrated CRM system all available to our agents.
Phil: What are your biggest challenges and how will you work through them?
Steve: The biggest changes we see coming are from the Carrier challenges with the changes being delivered by CMS. The work through is that everyone will be expected to deliver better service to the Beneficiaries. Efficient use of our agents time will be the key to keeping a stable book of business.
Phil: Well it's unique to have a FMO like your agency that is a fit for all brokers, new to Medicare and also those seasoned brokers with experience and an existing book of business.
Steve: We Provide Services that are focused on the value our brokers need and find helpful and not on simply on the volume of services offered. We find that this provides better outcomes, excellent performance and greater success for our agents.
Phil: As a Value Based Agency what solutions do you provide agents?
Steve: We provide the following:
• Online quoting and enrollment platforms that allow for side by multi carrier comparison for the Agent and Beneficiary. Allowing for the Beneficiary to make the best decision for their needs.
• CRM systems that provide a secure encrypted storage of client PHI.
• Access to a back office to answer questions regarding Marketing Compliance, Contracting, Training, Commissions, general questions, application issues and client service issues
• Updates to the markets as new information hits the streets so agents are informed, and
• Commission Protection Options for agents.
Phil: OK. To learn more about First Sierra our subscribers can go to www.firstsierrainsuranceservices.com
Now let’s turn to your take on 2025 changes in Medicare plans.Tell us about the Part D plan changes---
Steve: The Inflation Reduction Act of 2022 requires several changes to plans in 2025
• Out of pocket cost will be limited to $2,000
• Plans will allow patients to pay deductibles over 12 Months.
• Recommended Vaccines will be required to be available at no cost.
The Part D changes will impact the structure of the plans offered by the carriers. Changes coming in 2025 will affect premiums, formularies and plans offered. Brokers need to be informed by their trusted advisors about the changes and what options clients will have to get the coverage they neeed.
Phil: So brokers need support and assistance to provide what their clients need.
Steve: Yes, we are planning to provide the resources our agents and brokers need as this will be a big challenge to agents with a lot of active PDP’s. To help we have our multi-carrier quoting, and enrollment platform will provide agents the opportunity to quickly and efficiently run prescription drug cost comparison quotes. It will allow them to assist members virtually in a quick and compliant manner. I wish we had a crystal ball to know exactly how broker comp and premiums will change, but in our opinion, we feel that there will be a general increase in plan premiums and some carriers could cease broker comp completely. The good news is that by October 1, or maybe just before we will have a better understanding of what the changes will look like.
Phil: WHAT About MAPD and the drug coverages?
Steve: The CMS Final Rule for 2025 and Inflation Reduction Act of 2022 regarding MAPD Plans is still being digested by carriers.
Other challenges to Carriers will be:
• SSBCI - Also known as Value Added Benefits in plans.
• Carriers will now need to prove the utilization of the benefit in the plan. From what we are hearing the carriers will have to show high utilization of those benefits and then somehow relate that back to improved member health. Possibly showing that cost savings allows them to afford routinely picking up medications and not putting off other health services.
• Carriers will also need to prove the equity of the benefits in the plan. This means does it increase the health and wellbeing of the beneficiaries in the plan.
If the carriers cannot prove the above as adding value they will need to remove the benefit. The impact on brokers will be that benefit plans will change drastically and they will need to either explain why
they beneficiary should remain on this plan or give them a similar alternative.
Phil: WE HEAR Star Ratings are going to be impacted in 2025.
Steve: YES, reductions and methodology changes to the plans will mean plans have received Star Rating reductions and this will drive down plan reimbursement and cause major plan benefit changes from the 2024 to 2025 plan year. Brokers wlll need to prepare as more clients will be shopping plans.
Methodology changes can also affect plan reimbursements again. With plan benefit changes from the 2024 to 2025 plan year, clients will be shopping plans.
Phil: What about the Dual Market changes?
Steve: There will be several including:
Going back to monthly (SEP)changes vs Quarterly changes. Clients can change plans more frequently.
Also, there will be a large push for beneficiaries into the Aligned Dual Plan. This will givee us more opportunities in this market space.
There is currently talk about these changes may end up with individuals being passively enrolled in the aligned Dual Plans. Agents will be bypassed by Medicare auto enrolling beneficiaries. This will leave agents without compensation and beneficiaries without an advocate they have enjoyed in their relationship with their agent.
Another impact expected is how the changes will limit the number of Dual Plans in services areas, by removing the Dual look a like plans. Personally we feel that this is actually is good for Medicare beneficiaries, specifically in counties with aligned plans. It also helps agents with the stability of their book of business, less plan switching by the beneficiaries.
Phil: In the past few changes have impacted the Medicare Supplements. What is new here?
Steve: We expect to see larger than usual rate increases on the Medicare Supplement Plans. Recently multiple large carriers have announced large increases in their premiums. Agents will need to make sure they are up to date on premium increases and will need to be more proactive in running rate checks for their clients and keeping them informed. If rates continue to increase we may see more beneficiaries moving from Med Sup to MAPD especially in counties with large network support, even if the MAPD has a premium.
Phil: Marketing Compliance was a major issue this past year. What is up for 2025?
Steve: Call recording has not changed and remains the same as last year. Best practice is to record all enrollment calls/calls that discuss plan benefits for MA and PDP. Agents are responsible for securely storing that data for 10 years. We provide a call recording feature that also securely stores the data for the required time frame and can be easily accessed. Also, our online enrollment and quoting platform offers call recording and storage. In addition to the tech we also provide in-depth training to all of our agents on all of the compliance updates that directly affect them.
Phil: It can be confusing to determine what is considered Marketing and what is considered communication? we definitely suggest that brokers do their research to look up the definition of both.
Steve: Right we also see the confusion. From the disclaimers that are required to the need to get marketing tools approved. At First Sierra will review any marketing materials our agents plan to use or are using. If it is a marketing piece that needs CMS approval we will inform the agent and assist in getting the CMS approval.
Phil: What about scope of appointments (SOA) and PTC?
Steve: No real changes here, seems to be staying the same as last year.
SOA are good for a year from the date of signature or less if the beneficiary asks them to not reach out. SOAs need to be securely
stored for 10 years. They can be obtained through a paper version and also electronically. Our electronic enrollment platform does offer agent the ability to obtain an electronic SOA and will also store this for the agent for the required 10 years. We do also have approved PDF versions of SOA’s and PTC cards that agents can use. For storage we recommend agents store them securely in either their own CRM system or in the one provided to them through us.
Phil: Protecting private health information (PHI) is anorther concern.
Steve: Seems Blue Shield is one of the few carriers performing broker enrollment audits. We see PHI and brokers this way: There has been a focus on recent audits for agents on how they control and protect PHI. Typically in these situations carriers are asking the agent what steps they are taking to protect the information. We highly recommend the use of a CRM system. We have done many webinar trainings on compliance, making agents aware of what is to be protected and how they should be protecting that information. We also provide tools to our agents such as our multi-carrier online enrollment platform and most recently added CRM system. These are of course optional for agents to use, but do provide the data protection level that is being asked for.
Phil: Thank you Steve... for this insight into 2025 AEP. Sounds like First Sierra provides a wide range of service and support for agents and brokers.We look forward to your input in the coming months as more CMS details are revealed so we can keep our subscribers informed. If a subscriber wants to connect and learn more please go to www.firstsierrainsuranceservices.com
Steve: Thank you for the opportunity to share the services we offer at First Sierra. We are committed to helping more agents and we encourage those interested to contact us. We feel it is important to work with Cal Broker and continue to provide subscribers with up to date and valuable information so they can be a trusted advisor to their clients.

Steve Kuhtz is a Clovis native and holds a Bachelor of Science Degree in Business Administration from California State University, Fresno. He has been in the Insurance and Financial Services industry since 1993.
In 2002, Steve saw a need for a higher standard of client service, so he started a new insurance agency with Robert Diehl. Kuhtz Diehl Insurance has been dedicated to maintaining high standards of service ever since.
In 2009, Steve and Rob started First Sierra Insurance Services, a Medicare General Agency. Offering outstanding agent service and support, First Sierra Insurance has grown to approximately 400 agents throughout California, Nevada, and Oregon. In addition to the home office in Fresno, First Sierra Insurance has offices in Sacramento, Bakersfield, Pasadena, Manhattan Beach, and San Jose.
Outside of work, Steve enjoys sailing, participating in triathlons, snow skiing, water skiing, boating, backpacking, biking, swimming, and travel.
Steve@myseniorsales.com 559-251-0501 Office www.myseniorsales.com 2150 N. Winery Ave. Fresno, CA 93703
There’s no magic to it –it’s up to the agency owner to be fair. And it needs to be crystal clear: what does the agent get, and what value is that agent bringing to the agency?
By John Hockaday
LOA stands for licensed only agent, which is a captive agent – in our case, an agent who sells insurance products – who assigns their commissions to another individual or company.
Note: The acronym LOA also stands for line of authority, or the types of insurance products an agent is licensed to sell. But in this article, we’re referring to licensed only agent.
The individual or company receiving the commissions will keep a certain percentage, called an override. You can think of an override almost like an administrative fee. In exchange, the LOA gets a lot more support, structure, and training than an independent insurance agent doing everything on their own.
For example, an LOA might get office space, a secretary, and a maintained website without having to pay outright for any of that.
It’s probably more common to see people talking about captive agent’s vs independent agents.
A captive insurance agent is the same exact thing as a licensed only agent (LOA). It’s just different terminology.
Another term commonly used in this space is “street level” agents or “sub-street level” agents. This is not the same thing as a licensed only agent.
Every carrier has a street level commission. If you come in at street, it means you don’t need proof of production to get that commission rate. If you have proof of a high level of production, you can sometimes get commission above street level.
However, there’s also a level below street, and that›s sometimes referred to as «sub-street level.»
A sub-street level agent still owns the business he writes, and the carrier pays the commission directly to that agent.
Some agencies prefer to have sub-street level agents instead of licensed-only agents because they don’t have to handle commission payments. Being responsible for all the accounting and tracking commissions is a huge job, and this way, the carrier takes care of it.
However, usually only a very, very small agency would do that. It would also typically only be for a short time; for example, perhaps an agent is helping a new agent get on their feet.
The mentoring agent may put the new agent below street level and take a few commission points as they help that agent get started. When the new agent is ready to go on their own, the mentoring agent would cut them loose and let them get their own contract.
In the world of insurance, things can get complicated as there are several levels between an LOA agent and the actual insurance company.
But here’s the long story short: Insurance Company > FMO > Independent Agent > Agency > LOAs.
Insurance companies have products to sell, but they may not have the distribution – they need agents to sell their stuff! FMOs step in to help market those products, while also providing independent agents with support.
Independent agents may decide they want to grow beyond just themselves, so they may start an agency. And that agency may choose to have licensed only agents, or LOAs.
At the top of this “food chain,” the overrides are very small. Each step down the chain, the override rises as the level of support increases. We’ll get into commission splits and agreements a little later in this article.
Pros of the LOA model:
You can do a lot of production with just 10 captive agents
It’s a natural next step for growth
Bigger impact in your community as you can reach and help more people
Lifelong friendships – we have agents at our local agency that have been with us for decades and are lifelong friends; we don’t think we’ve done something right to warrant that.
Cons, or more so challenges, of the LOA model:
Pressure and responsibility of being an agency owner
Shifting from a sales role to management
Figuring out how to retain agents who become successful and want to leave to become independent
Getting the vesting agreement right
Determining the compensation agreement and how you will structure the commissions
Your own time, money, and effort required to get a brand-new agent up and running
Deciding on what value you have to offer agents in exchange for your override
Figuring out if the book of business will be yours or the LOAs (i.e: will they be able to take that book of business with them if they decide to leave?)
There’s so much to consider before just jumping into the idea of recruiting agents.
I’d start with being honest with yourself: are you prepared for the pressure and responsibility of being an agency owner?
I remember not being able to sleep at night – I’d lay awake thinking about whether my agents were making a living. It’s a lot of pressure, and you feel the responsibility for it.
You also need to ask yourself if you’re cut out to be an agency owner. It takes the right person to be good at this. In my opinion, if you’re a good producer and you enjoy that, that gig is hard to beat.
When you start recruiting agents, you shift from sales to management. I see a lot of producers try it, and they should’ve just stuck with personal production because they ended up hating it.
If you’re a highly successful producer, I’d first consider hiring someone to help you. Keep doing what you do best. People in support roles can help you with the things you don’t like to do.
In sum, you must be management and coaching-inclined to be good at this.
Plus, if you’re a good salesman, you fight the thought that you could be selling everything yourself. You end up being a babysitter, and that may not be what you’re looking for.
So, that’s my word of caution for anyone thinking about starting an agency – seriously think it through first. We took that step and have an agency, but it’s not for everyone.
If you’re ready to start an agency and recruit some agents, one of the first things you need to think about is how to structure the agent compensation agreement.
We’ve tried to be as generous as we can at our agency because we know it’s hard, especially when you’re first starting. So, we give our agents all that we can.
The commission split or structure can really vary, and you can also get creative with it. It could be 60/40 – meaning the LOA gets 60% and the house gets 40%, it could be 70/30, 80/20, or it could be graduated depending on how many years that agent has been with you.
A graduation of commissions can make a lot of sense because a brand-new agent requires a lot more support than an established agent. As they “graduate” and need less help, the agency owner can then give them more commissions, because they’re doing less for them.
I’ve seen agents come up with all kinds of commission splits, but the key is making sure that what you’re doing for the agent is enough to justify your override. Both sides must be fair.
If you provide office space and secretarial administrative help, that agency owner deserves more than the person that just gives a contract and tells you to work out of your home. And yet sometimes, those spreads are the same!
There’s no magic to it – it’s up to the agency owner to be fair. And it needs to be crystal clear: what does the agent get, and what value is that agent bringing to the agency?
The vesting agreement is also an important piece to include in your agreement.
When an independent agent gets appointed, they’re vested Day 1, meaning whatever commissions they earn, they continue to receive until that company’s vesting requirements are satisfied.
As an example, some companies say you’re vested Day 1, and those are your commissions if your commission amount is at least $300/year.
An LOA assigns their commissions up. If that agent leaves after a year, do they take anything with them, or are they just out?
Some agencies will have a vesting period up to 10 years, but around 3 years is the most common.
You really need a vesting period in your agreement, because those first few years require a ton of time, money, and effort. Getting an agent started is an enormous task.
You may even be in the hole, especially in the first year, so is it fair for that agent to get all the training and support from you and then be able to leave once they’re done? You need protection as an owner.
You need a lawyer to put together the initial LOA contract. Then, you’ll have a template you can use for agents moving forward. It’s always best to make sure you don’t leave anything out, especially in today’s world.
A few items to make sure you include:
• Vesting agreement
• Commission split – whether it’s a split or graduation of commissions
• Non-compete based on a radius around your business
• Who owns the block of business – the agent or the agency?
The vesting agreement and commission split are simple – decide what’s fair and include it.
Non-Compete — You can train a person and teach an agent a lot, but if you don’t have a non-compete, they can start a business in an office next door and be your competition.
In your LOA agreement, I’d suggest you have a radius that they cannot do business within so many miles of you.
If I’m looking from the agent’s point of view, I want to know if the customers are mine or the agencies. If I bring in 100 policyholders, do I own that business or not?
That’s a key difference – if I’m the agent, I want that business to be mine.
I personally think the agent should be protected in the business they bring. They should own it and have the right to do with it what they want.
When the agent retires or if they have a change of heart and decide they don’t like it, they have a block of business worth something. There ought to be a buyout agreement.
That’s the way we’ve always done it, and I think it’s fair. It allows agents to grow and not feel like they are stagnant. They are building something of value that’s theirs.
Sometimes, the agent has no idea what they’re signing, and they don’t realize that the agency is taking advantage of them until it’s too late.
Say you want to break away and work somewhere else. Suddenly, they may say you can leave, but you don’t get any of your business. We’d never do that, but a lot of people in this business do, so be aware.
If you’re taking a piece of commission from an agent, you should be offering something of value to earn it.
Here are some examples of things you can provide to agents to make it fair for both sides:
• Office space
• Secretarial support
• Mentorship and professional advice from seasoned pros
• Access to computers, fax machines, copy machines, a phone system
• Postage
• Website
• Leads – often, agency owners will supply leads to new agents, so they have people to call on and go see.
• Software and tools, like MedicareCENTER – if you work with an FMO like us that supplies valuable resources, such as this important tool for quoting and enrollment, that also provides value to your agents.
• Compliance help – training your agents and being a resource in this world of ever–changing compliance is critical.
• Weekly meetings – we have a Monday morning meeting where we go over the production scoreboard, share insurance industry announcements, and connect with everyone to kick off the week.
A person brand new to the business will have trouble making it on their own with no support system, and that’s part of why becoming an LOA is so attractive.
The biggest drawback of the LOA model is that the agents you nurture, and train can eventually leave you. After a while, they feel that if they leave, they can make more by going out on their own.
How are you going to navigate those waters? It’s important to have a game plan upfront before you start. For the agents that make it, how will you keep them and ensure they feel they can continue to grow?
For us, it’s been a mix of providing a lot of value and ensuring our agents own their book of business. It’s an important topic to sit down and really think about before you invest a ton of time and money in new agents.
The key to starting an agency with the Licensed Only Agent (LOA) Model is having a clear understanding of expectations on both sides.
What is the owner bringing to the table, and what is the agent going to bring? What’s the succession plan if the agent wants out?
I never wanted a person to feel like once they came on, they could never grow. If you don’t consider this, I think you’ll end up losing all the agents you bring on.
I hope this was helpful. While we don’t have any cookie-cutter templates and we don’t do consulting on this topic, we’re happy to help however we can.
Good selling!

Hey there, my name is John Hockaday, and I’m the COO & Principal of New Horizons Insurance Marketing and the co-Founder of Sams/Hockaday & Associates. I’ve been business partners with Jeff Sams since 1981.
Back in the 80s, I started out by servicing clients as an agent out in the field.
After a few years, it was clear that Jeff and I needed to expand, so we started an agency and grew it to a staff of 30+ people.
Twelve years later, we started this senior insurance marketing company, New Horizons.
I specialize in the “everyday” flow of the insurance business, spending most of my time talking to senior market agents. Where I help agents, the most is in underwriting. I know what each carrier will and won’t take, so I can help you place those tough cases.
On occasion, I contribute to our blog, and you’ll also find me on our YouTube channel.
Regardless of what level you’re at, I can assure you that I’ve been there and know exactly what you’re dealing with firsthand.
jhockaday@nhmteam.net
217-233-8000 Ext. 106
The Medicare Payment Advisory Commission (MedPAC) is an independent congressional agency established by the Balanced Budget Act of 1997 (P.L. 105-33) to advise the U.S. Congress on issues affecting the Medicare program. In addition to advising the Congress on payments to private health plans participating in Medicare and providers in Medicare’s traditional fee-for-service program, MedPAC provides information on access to care, quality of care, and other issues affecting Medicare.
The Commission’s 17 members bring diverse expertise in the financing and delivery of health care services. Commissioners are appointed to three-year terms (subject to renewal) by the Comptroller General. Appointments are staggered; the terms of five or six Commissioners expire each year. For more information on the commissioner appointment process, please click on ‘Medicare Payment Advisory Commission (MedPAC)’ on this page. The Commission is supported by a career staff who typically have backgrounds in economics, health policy, public health, or medicine.
The Medicare Payment Advisory Commission (MedPAC) is an independent congressional agency established by the Balanced Budget Act of 1997 (P.L. 105-33) to advise the U.S. Congress on issues affecting the Medicare program. In addition to advising the Congress on payments to private health plans participating in Medicare and providers in Medicare’s traditional fee-for-service program, MedPAC provides information on access to care, quality of care, and other issues affecting Medicare.
The Commission’s 17 members bring diverse expertise in the financing and delivery of health care services. Commissioners are appointed to three-year terms (subject to renewal) by the Comptroller General. Appointments are staggered; the terms of five or six Commissioners expire each year. For more information on the commissioner appointment process, please click on ‘Medicare Payment Advisory Commission (MedPAC)’ on this page. The Commission is supported by a career staff who typically have backgrounds in economics, health policy, public health, or medicine.

I just wrote a credit union with CalCPA Health! I thought they only wrote CPAs
financial professionals now too!
By Genna Armanini
Health Savings Accounts (HSAs) are valuable for managing healthcare costs, offering tax advantages and long-term savings opportunities. As a health insurance broker in California, you can leverage HSAs to build relationships with qualified* Certified Public Accountants (CPAs) and financial professionals (wealth management, advisors, financial institutions, etc.) who advise their clients on financial matters. Here is a guide on effectively selling HSAs to CPAs and financial professionals in California.
Just because a CPA or financial professional may have a strong understanding of finances and taxes, does not mean they understand the full benefits of HSAs.
Before you approach these clients, ensure you have a comprehensive understanding of HSAs and the benefits they can provide:
• Tax Advantages: Contributions to HSAs are taxdeductible, grow tax-free, and can be withdrawn tax-free for qualified medical expenses. This means money can be earned (income), invested (investment returns) and used to pay expenses without ever being taxed.
• One way to look at the HSA tax advantage: Example: An HSA subscriber in the 25% tax bracket is enrolled in a $2000 deductible qualified HDHP. Since they pay the deductible with pre-tax dollars, the $2000 deductible would be comparable to a $1500 non-HSA deductible plan. The taxpreferred effect (savings) continues beyond the deductible, all the way up to their out-of-pocket maximum. An $8,000 OOP max would behave like a $6,000 OOP max in a non-HSA plan.
• Cost Savings: HSAs are paired with qualified highdeductible health plans (HDHPs), which typically have lower premiums than comparable non-HSA plans.
• Tax free Investment Returns: HSA funds can be invested, growing into a retirement nest egg, similar to a 401K or IRA, except there are no Required Minimum Distributions and you do not pay tax on the investment earnings when you use the money for qualified health care expenses.
• Flexibility and Ownership: HSA funds are owned by the employee and stay with them throughout their career (from job to job) and into retirement. There are no use-itor-lose-it provisions like FSA’s.
Attract and Retain: HSAs have become a valuable tool in today’s tight labor market for employers to attract and retain talent. With no discrimination tests like 401K plans, employers easily add a valuable employee benefit to their benefits package.
Important Note: The tax effects mentioned above are federal taxes. California is one of only two states that do not recognize HSAs. Given this, the benefit from the federal tax effect is typically good enough to make the HSA math work for most companies and employees.
Identify Key CPA
Target CPAs and Financial Professional firms. You have proven methods to lower the cost of health insurance for employers and the cost of health care for their employees; as well as provide a valuable employee benefit. Their financial acumen should make HSA math more straightforward to understand. Often, the firm benefits administrator may be someone other than a financial professional themselves, and you can assist them with explaining HSAs to their management who would be interested in the financial benefits offered through HSA plans.
3. Develop a Value Proposition for these prospects
CPAs and financial professionals are trusted advisors prioritizing their clients’ financial well-being. Tailor your value proposition to highlight how HSAs can benefit their employees while controlling/reducing employer costs. You are providing a service similar to what they provide to their customers.
• Tax Savings: Emphasize the tax benefits HSAs provide, which can be a significant selling point for tax-focused CPAs and financial professionals.
• Client Satisfaction: HSAs can improve client satisfaction by having a successful, cost-effective enhancement to the employee benefit offering.
• Added Value: Talk their talk by exhibiting a deep understanding of HSAs to CPAs and financial professionals, differentiating yourself from the competition.
Provide your prospective clients with the knowledge and tools they need to implement HSAs to their management and employees confidently:
• Workshops and Webinars: Host informational sessions to educate your clients on the benefits of HSAs, how they work, and how to integrate them into their employee benefit offerings.
• Resource Materials: Create easy-to-understand brochures, whitepapers, and case studies that you can provide prospects and clients. There is an abundance of examples and templates available on the web and from HSA providers/administrators.
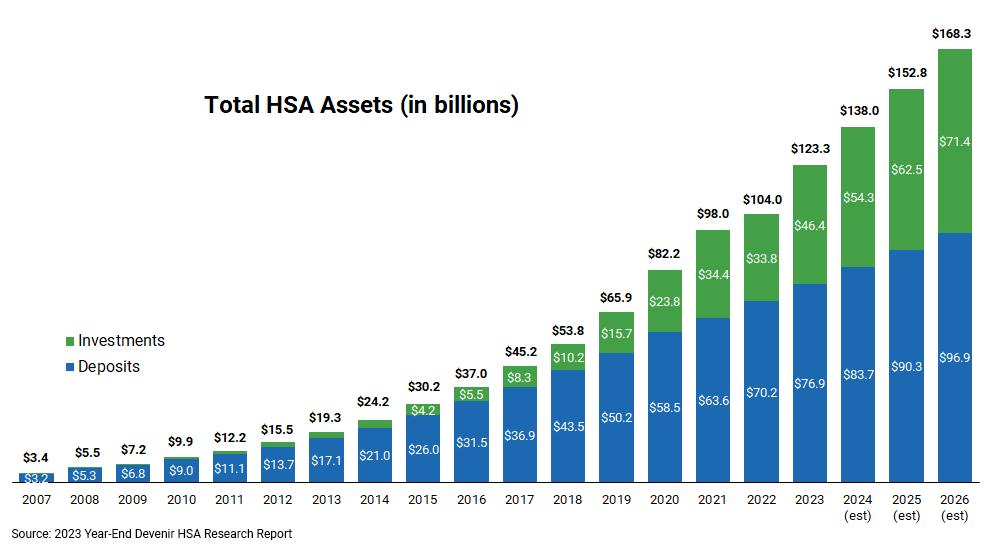
• Personal Consultations: Offer one-on-one consultations to address specific questions and concerns they may have.
Show your prospects/clients this graph below – they will want to be a part of this growing HSA trend!
5. Leverage Professional Networks
Use your professional networks to connect with CPAs and financial professionals and build relationships:
• Join CPA Associations: Become a member of local and state CPA associations, such as the California Society of Certified Public Accountants (CalCPA). Insurance brokers qualify for Financial Professional and Associate membership classes.
• Attend Industry Events: Participate in CPA and banking/ wealth management conferences, seminars, and networking events to meet potential clients.
6. Highlight Compliance and Regulatory Knowledge
California has specific regulations and compliance requirements related to health insurance and HSAs. Demonstrate your expertise in these areas to build trust:
• Stay Informed: Keep current with California state laws and federal regulations affecting HSAs. For example, California requires embedded deductibles for qualified HDHP’s. Know what this means and how it works. Simple examples usually do the trick.
• Provide Updates: Regularly update your clients on any changes in legislation that may impact HSAs –and the effect it may have on their clients.
• Offer Compliance Support: Help ensure they comply with all relevant regulations.
By positioning yourself as a knowledgeable and dependable partner, you can successfully sell HSAs to CPAs and financial professionals in California. You can help them provide valuable financial solutions to their clients while growing your own business.

Genna Armanini is the Marketing Director of CalCPA Health, a California domiciled carrier providing health plans to CPA and financial services firms.
Genna has worked at CalCPA Health for over 23 years, growing brand awareness, helping maintain high retention, and enabling subscribers to become strong advocates for their health and well-being.
To find out more about what CalCPA Health has to offer your clients, please visit us at: www.CalCPAHealth.com/CalBroker info@CalCPAHealth.com 866-954-7406
To contribute to an HSA, you need to be enrolled in an HSA-qualified health plan with a high deductible. You also can’t have any other health coverage. This includes Medicare. Once you’re enrolled in Medicare, you can no longer contribute pretax money to your HSA.
—Use the links below to advise your group clients on how Medicare will impact their HSA:
• HSAs and Medicare: How Does It Work? (healthline.com)
• Medicare | HSAs and Medicare | Fidelity

BY ELKA SOUSSANA
Meet Jane, an independent life and health insurance broker who has built her business one client at a time, sitting across kitchen tables, sipping coffee, and explaining the complexities of insurance in simple terms. For years, Jane’s business flourished through wordof-mouth referrals and participation in local networking events. Her community knew her as the go-to insurance agent, and her personal touch made her a trusted advisor.
But in the wake of the COVID-19 pandemic, Jane faced a new reality. The world of business was shifting rapidly towards digital platforms, and the traditional, face-to-face client meetings were becoming less feasible. Jane realized that to stay relevant and continue growing her business, she needed to adapt to this new digital landscape. The quote from Mark Randolph, co-founder of Netflix, came to mind: “If you are unwilling to disrupt your business, there will always be someone willing to do it for you.” Jane knew it was time to embrace change.
For many independent insurance agents like Jane, the pandemic has underscored an essential truth: opportunities are no longer confined to your local area. With the right tools and strategies, you can now work from anywhere and serve clients across the country. Embracing the digital world isn’t just about keeping up with the times—it’s about seizing the vast potential that a borderless market offers.
Imagine having clients in multiple states, each receiving the same high level of service you’ve always provided. This expansion doesn’t require a significant overhaul of your business, but rather, a shift towards leveraging digital tools that streamline and enhance your workflow. Adaptability is key; those who can pivot and harness new technologies will outpace those who cling to traditional methods.
One of the first steps in transitioning to a digital-first approach is setting up a Google My Business (GMB) page. Even if you’re working from a home office, a GMB page allows you to establish an online presence that clients can easily find. It provides essential details like your services, contact information, and client reviews, making you more accessible to a broader audience. The reviews, in particular, are invaluable for building trust with potential clients who are increasingly looking for social proof before making decisions.
In the digital age, convenience is king. Implementing a digital calendar system, like Calendly or Google Calendar, allows clients to book appointments with you directly online. This not only saves you the hassle of back-and-forth scheduling but also enhances the client experience by offering them the flexibility to choose a time that works best for them. It’s a simple yet powerful tool that can make a big difference in your efficiency and client satisfaction. Adaptability here means shifting from rigid schedules to a client-friendly, flexible booking system.
Using Google links in your email signatures and content for review requests can significantly increase the number of reviews you receive. Positive reviews boost your credibility and visibility in search results, attracting more potential clients. Furthermore, integrating a Customer Relationship Management (CRM) system, like Ease or AgencyBloc, can automate follow-ups and reminders, ensuring that no client or lead slips through the cracks. Mark Randolph’s quote resonates here: automation is a form of disruption that can propel your business forward by making it more efficient and client-focused.
4. AI and Marketing Platforms
AI tools have revolutionized content creation and marketing. Platforms like ChatGPT can assist in generating content, while Canva provides an array of templates for social media posts, flyers, and more. These tools are invaluable for creating professional-looking marketing materials quickly and affordably. Additionally, platforms like Metricool can help you schedule and manage your social media content, ensuring consistent and timely engagement with your audience. In this context, adaptability means embracing AI and other advanced tools to stay competitive and relevant.
5. Video Content and Personal URLs (PURLs)
In today’s digital world, video content is crucial. It’s engaging, easy to consume, and highly effective at conveying complex information. Creating explainer videos for your clients, particularly for those in the Medicare space, can significantly enhance their understanding and trust. This is especially important during the Annual Enrollment Period (AEP), which promises to be tumultuous this year due to changes from the Inflation Reduction Act (IRA) for Part D and shifts in the Medicare Star Rating compensation for MAPD plans. A step-by-step video guide on quoting and enrollment can empower your clients to act while assuring them that you are still their trusted broker. Adapting to video content is not just a trend; it’s a necessity in today’s digital-first approach to client engagement.
6. Building Online Communities and Networks
Another crucial aspect of digital transformation is the ability to build and engage with online communities and networks. Platforms like LinkedIn and Facebook groups offer excellent opportunities for professional networking and connecting with potential clients. Being active in these communities not only helps you stay updated with industry trends but also enhances your visibility and reputation. Adaptability here involves using these platforms to build relationships and expand your influence beyond your immediate geography.
As more business operations move online, ensuring data security and compliance becomes critical. When using digital tools, it’s essential to adhere to best practices for data protection and to comply with regulations such as HIPAA for health information. This means using secure platforms, maintaining strong passwords, and being vigilant about phishing scams and other cyber threats. Adapting to the digital world includes being proactive about safeguarding your clients’ sensitive information.
In the realm of digital marketing, tracking the performance of your campaigns is vital. Utilize analytics tools such as Google Analytics to monitor website traffic, client interactions, and conversion rates. This data can provide insights into what strategies are working and where improvements are needed. By analyzing this information, you can make informed decisions to refine your marketing efforts and achieve better results. Embracing a datadriven approach is a crucial aspect of adaptability in today’s digital landscape.
Actively seeking feedback from clients is an essential part of improving your services and digital tools. Use surveys, feedback forms, or direct outreach to gather client insights. This not only helps you understand their needs better but also shows that you value their opinions. Involving clients in this way can enhance their loyalty and satisfaction, leading to stronger relationships and a more successful business.
For brokers working in Medicare or other insurance fields, partnering with a Field Marketing Organization (FMO) can provide substantial benefits. An FMO can offer tools like a personalized URL (PURL) that consolidates all your contracts in one place, making it easier for clients to access and for you to manage your business. Additionally, FMOs often provide automated marketing solutions that help you maintain consistent communication with your clients without the need for manual effort.
However, not all FMOs are created equal. When choosing an FMO, it’s crucial to ask about their release policy, so that you’re never held hostage, and ensure that you maintain ownership of your book of business. Consider how responsive they are to your needs—not just during the recruitment phase but also when you need support. Speaking with other brokers who work with the FMO can provide insights into their experiences and help you assess whether your values align. Adaptability here involves being flexible and open to new partnerships that can enhance your business operations.
The digital transformation of the insurance industry is not just a trend but a fundamental shift in how business is conducted. For independent brokers, this represents a tremendous opportunity to expand your reach, improve your efficiency, and better serve your clients. Remember Mark Randolph’s words: “If you are unwilling to disrupt your business, there will always be someone willing to do it for you.” Embracing change and adapting to new technologies is not just about survival; it’s about thriving in a competitive landscape.
As you navigate this transition, consider downloading my
Visit simplerhorizons.com/agent-guidebook-2024/ for more insights and tips. It’s available at no cost and can provide valuable guidance as you embrace the digital world.
By leveraging digital tools and platforms, you can position yourself at the forefront of the industry, ready to meet the needs of clients wherever they are. The future is bright for those who are willing to adapt and innovate—embrace it and watch your business thrive.
For more information and resources, visit Simpler Horizons (www.simplerhorizons.com)
With a strategic digital approach, you can ensure your success in the ever-evolving landscape of insurance. Embrace these tools, educate your clients, and continue to be the trusted advisor they rely on, now and in the future. The ability to adapt will not only secure your place in the market but also propel you towards greater heights in your business journey.

Elka Soussana, the driving force behind Simpler Horizons Insurance Solutions, a thriving senior general agency boasting over 100 independent agents. Currently serving as the Vice Chair for the CAHIP-LA Medicare board and as an advisor for the Foundation for Senior Services, Elka is a respected figure in the insurance and senior services sectors. Since making her mark in the Medicare space in 2012, she has skillfully navigated its complexities, ensuring both her agents and the seniors they serve can make informed choices.
BY MAGGIE STEDT C.S.A, LPRT
This coming Annual Open Enrollment Period (AEP) is promising to be one of the most challenging and crazy times. And that’s saying something after the last few we have slogged through!!! Now more than ever independent agents need to plan, budgeting, and learn as much as they can prior to the start of AEP.
There is still much uncertainty as to the support that FMO’s will be able to provide and if there will be a cost for programs and systems and for what financial support the carriers will be providing to the FMOs and the agents. There is still the need for clarity for our commissions that we will be receiving for initial sales and renewals here in California for the Medicare Advantage and the Stand-alone Part D plans.
The biggest impact this year will be for the prescription drug coverage. Under the Inflation Reduction Act of 2024 as of January 1, 2025, there will be an annual limit of $2,000 for prescription drug costs in Part D. In 2026 and beyond the annual limit will be adjusted based on inflation. It is important to note that the $2,000 does not apply to out-of-pocket costs for Medicare Part B drugs. Medicare Part B covers drugs are administered by a doctor, nurse, or other healthcare provider in an outpatient setting such as a doctor’s office.
The Centers for Medicare and Medicaid (CMS) will be providing guidelines for the establishment of the Medicare Prescription Payment Plan which provides for Part D beneficiaries to opt into a monthly payment program. The payment program will be administered by the Part D carriers. More information will be coming from the carriers once they have more guidelines from
CMS. CMS will be developing monthly calculators to help beneficiaries to estimate what their monthly costs will look like, and to determine if enrolling in the Medicare Prescription Payment Plan makes sense for them.
Under the Inflation Reduction Act a greater amount of the costs for prescription drugs has shifted to carriers. This means there is strong potential for a change in the supplement benefits offered under the Medicare Advantage plans. The Stand-Alone Part D plans will greatly impacted due to the cost shift. We expect to see changes in the premiums, plan formularies, what plans will be offered or closed to new enrollees and what plans will be available for agents to enroll their clients in and receive commission payments.
Your first step is to figure out the budget for your fall campaign. You may or may not have marketing dollars available to you. You do have to pay for AHIP or the NABIP certifications as no reimbursement can be provided under the new CMS Marketing Rules. Calculate your mailing costs both for your book of business and if you want to wage a community campaign. If you haven’t purchased a platform like Zoom or GoToMeeting now may be the time. Plus, you will need time to learn to use the system. Look at email campaign systems to help reach more people. Make sure the program has an opt out feature for the recipients.
Be realistic
about your
time and
what
it will take
your current book and to grow it. Is 10% or more targeted growth a good goal and what will it take to get there?
Every client that has Part D coverage (MAPD or Stand-alone Part D plans) will need to review their prescription drug coverage for 2025. Many agents may decide to opt out of assisting their Stand-alone Drug plan clients and send them off to the mercy of Medicare. gov. Many of us prefer to continue to assist our clients. One effective way to meet this challenge is to provide the means for clients to input their own drugs and information into online platforms such as Connecture so that we can then assist them with the selection of a plan. For example, in Connecture you click on your name on the upper right to access Account overview and then in the left-hand corner you can click on copy 2024 link to link to your website. You will need to reset it for 2025 business.
This AEP is most likely to see a greater opportunity for the enrollment into Medicare Supplement Plans on a guaranteed underwritten basis from MAPD plans due to several changes in the Medicare Advantage plans for drug copays, hospital copays, plan premiums and physician copays by 15% or more (reduced benefits or increased costs). This will trigger guarantee issue into any carrier’s Medicare Supplement plan. In addition, if the carrier offers both MAPD and Medicare Supplement plans, and the MAPD plan reduced any of its benefits or increased the amount of cost sharing or premium then the beneficiary may change to their carrier’s Medicare Supplement Plans (under the company’s GI guidelines) without any underwriting.
Make sure to review Medicare Supplement Guaranteed Acceptance Guides for each carrier that you represent. These Guides provide information as to which situation applies, what plans may be offered, what documentation is required with the carrier’s application and the time frame for application submission. Each carrier’s Broker Services or local Broker Representative will be happy to assist you. In a later article this year we will take a deeper dive into Medicare Supplement Guidelines.
Complete your certifications and plan reviews as quickly as possible so you are ready to sell and can plan more effectively for your AEP activities. You need to understand the plan offerings and formularies to be able to confidently assist your clients in finding the plan that
best fits their needs. There may be some delays in the Carrier meetings schedules as many are refiling their plans due to the change in CMS’ calculation of the star ratings.
Start planning your community outreach initiatives. Doctors, community groups, senior centers and so on need to know about the major changes coming. Lunch and learns are a great offering for physicians’ offices. You may want to think about offering carrier specific zoom sales meetings or community meetings. I like to mix clients and prospects and encourage clients to bring their friends. Start thinking outside the box! Make sure to do everything with CMS compliance guidelines. Make sure you are using CMS approved scripts, presentations, and other materials. Your FMO is a great resource for these! Securing Scopes of Appointments and recording calls requirements continuing into this AEP.
With planning, training and realistic expectations you can have a successful AEP this fall. Take care of yourself and don’t overdo! You got this!

MAGGIE STEDT C.S.A, LPRT, is an independent contractor/licensed agent and consultant. She is a certified senior advisor and lifetime member of NAHU’s Leading Producers Roundtable at the Soaring Eagle Level. She has over 40 years of experience in essential areas of the insurance industry including sales and sales management, product development and product management. A dedicated leader, Maggie currently serves on the NAHU Medicare Advisory Committee. Founder of the annual Senior Medicare Summit, attendance grew from 200 in 2010 to close to 1,000 attendees in 2022. She served as past president of CAHIP; NAHU Region 8 Membership Chair 2014 – 2018 and past president of OCAHU, serving two terms.
maggiestedt@gmail.com
By CalBroker Mag
Medicare is an essential insurance option for many. About 66 million Americans have Medicare coverage, and 78.4% have Part D drug coverage. However, the Inflation Reduction Act (IRA) of 2022 has led to many changes to drug coverage, and more are coming in 2025.
Understanding these new chnges will give you insight into deductibles, copays, spending caps, and expanded coverage so you can help your clients choose the best insurance that meets their needs.
The first significant change in Part D coverage is to the program’s general structure. Part D currently has four phases of coverage: deductibles, initial coverage, coverage gap, and catastrophic phase. In 2025, CMS will remove the coverage gap phase and add a separate program, simplifying the phases.
Part D starts with the deductibles phase, as usual. Your clients will pay a monthly premium and 100% of the gross drug costs for covered drugs until they spend $590 — up from $545 in 2024 — and meet the deductible.
Once your client reaches the deductible, they’ll enter the initial coverage phase. In 2025, your client will pay a 25% copay for covered drugs, and the plan sponsor will pay 65% or 75% of all other medicines, depending on the specific medication.
The current Part D structure includes a coverage gap where the plan sponsor temporarily limits drug coverage after the enrollee and the plan spends $5,030 in covered meds.
Once in the gap, your clients are responsible for 100% of drug costs. However, manufacturers discount drugs
at 70% or 75% via the Coverage Gap Discount Program. So, enrollees pay a maximum of 25% of drug costs, and the manufacturer pays 75%, or 70% and 5% for the plan.
In 2025, CMS will eliminate the coverage gap. Enrollees will stay in the initial coverage phase until they reach a new lower out-of-pocket maximum. The Coverage Gap Discount Program will become the Discount Program. In this adjusted phase:
• Enrollees pay a 25% copay for covered drugs
• The plan sponsor pays 65% or 75% of covered drugs
• The manufacturer covers 10% of applicable drugs
• The initial phase now ends once the enrollee meets the new out-of-pocket maximum.
In the current structure, the catastrophic phase starts once enrollees reach $8,000 in out-of-pocket spending. In this phase, copays stop, and enrollees pay nothing for covered drugs for the rest of the year.
In 2025, your clients will still have no copays in the catastrophic phase. However, the out-of-pocket limit is lower. Sponsors pay 60% of covered drugs, the manufacturer pays 20%, and CMS pays a reinsurance subsidy of 20% of applicable meds and 40% of all others.
The IRA established several new requirements and programs to help lower the overall cost of medications for enrollees. These include spending caps, changes to cost-sharing, and inflation rebates.
In 2025, CMS will lower the out-ofpocket spending limits to help reduce overall drug costs for enrollees. The lower limit also simplifies coverage. For 2025, enrollees will now only pay a maximum of $2,000 in out-of-pocket spending.
• Fees that count toward out-ofpocket costs will include:
• Enrollee's out-of-pocket payments for covered drugs
• Payments manufacturers make for enrollee's covered drugs
Enrollees will also have the option to spread out-of-pocket payments over the calendar year instead of paying a large sum all at once.
CMS also changed the cost-sharing structure in the catastrophic phase. Medicare uses a reinsurance subsidy to help pay for drugs in this phase, but the drug type will now determine the calculation method.
In 2025, Medicare’s share of the cost will decrease from 80% to 20% for brand-name drugs and 40% for all other covered generic drugs. Plan sponsors and manufacturers will now be responsible for covering higher portions of the drug costs.
The new Inflation Rebate Program will also offer discounts if the plan sponsor raises drug prices faster than the inflation rate. For Part D drugs, the rebates apply only to certain drugs and biologics. However, manufacturers can ask CMS to lower the amount of rebate available if a drug is on the drug shortage list or part of a severe supply chain disruption.
The Inflation Reduction Act sets limits on insulin costs, improving insulin coverage through Medicare Part D plans. The new limit started in January 2023 and will remain in place for 2025.
Insulin coverage includes:
• A maximum cost of $35 for a one-month supply of insulin through a covered prescription
• No deductibles on insulin
The cap on insulin costs will apply even if enrollees buy more than one month's supply at a time. The plan cannot charge your clients more for bulk buying.
Medicare Part D plans will continue to include more vaccine coverage without extra costs. Enrollees can get any vaccine the Advisory Committee on Immunization Practices recommends without paying a copay or a deductible. These include vaccines for shingles, Ebola, dengue, and others, based on the guidelines for administering.
Finally, CMS will offer Part D plan sponsors more flexibility to substitute drugs without approval from CMS. The goal is to increase access to effective medications, potentially at a lower cost.
In 2025, Part D plan sponsors will now have the ability to update the formulary midyear and substitute biosimilar drugs without needing approval from CMS. Biosimilar drugs are similar in structure to other drugs that are already authorized for use. Before this change, every plan sponsor had to receive explicit approval before making a change. Starting in 2025, CMS will treat these as maintenance changes. However, plan sponsors must give enrollees a 30-day advance notice of the changes.
Plan sponsors will also have the ability to make immediate substitutions for new interchangeable biologicals. This means that plans can instantly swap biological products with new similar products that might not have been on the market when they submitted the original formulary for approval. Plans must give advance notice of the change to enrollees.
The Inflation Reduction Act significantly impacted Medicare Part D coverage. Some changes are already in force, and more are coming for 2025. Staying up-to-date on these changes gives you deeper insights to help you understand how coverage will look and how it will affect your clients.
SOURCES:
Centers for Medicare and Medicaid Services: “Medicare Monthly Enrollment, Final CY 2025 Part D Redesign Program Instructions Fact Sheet.”
Medicare: “Yearly Deductible for Drug Plans, Costs in the Coverage Gap, Catastrophic Coverage, Saving Money With the Prescription Drug Law, Saving Money With the Prescription Drug Law.”
Centers for Medicare and Medicaid Services: “Fact Sheet: Medicare Prescription Drug Inflation Rebate Program Revised Guidance., Contract Year 2025 Medicare Advantage and Part D Final Rule (CMS-4205-F).”

By CalBroker Mag
It may feel like 2024 has only just begun, but it’s already time to prepare for upcoming Medicare changes. In April 2024, the U.S. Centers for Medicare and Medicaid Services (CMS) released the Contract Year 2025 Medicare Advantage and Part D Final Rule. This final rule includes a series of new or revised policies that will go into effect in 2025. The Inflation Reduction Act will also change Medicare programs that year.
These regulations are designed to improve Medicare Advantage (MA) and Part D plans. They include new Medicare enrollment restrictions, data privacy protections, and drug plan changes. Many of these policies will directly affect health insurance professionals and Medicare enrollees. Staying informed about these changes will enable you to give your clients accurate advice and help them choose the most suitable plan.
Health insurance professionals are valuable resources for clients who need help understanding and comparing Medicare coverage options. They also assist clients with the enrollment process.
Many private insurers have historically offered sales incentives for agents and brokers who enroll beneficiaries in their MA or Part D plans. However, this practice has raised concerns that health insurance professionals may prioritize their financial interests over client needs. For example, an agent could encourage clients to enroll in a plan that offers lucrative commissions, even if that plan isn’t the best choice for the beneficiaries.
The final rule will safeguard Medicare enrollees by eliminating anti-competitive and anti-consumer steering incentives. The new policy includes these guardrails:
• Agents and brokers will receive a fixed compensation of $100 for every initial enrollment, regardless of the client’s chosen plan.
• MA/Part D sponsors can’t partner with Third-Party Marketing Organizations (TPMOs) to offer incentives that may prevent agents or brokers from objectively evaluating plans for their clients.
The CY 2025 final rule includes new policies to protect Medicare beneficiaries’ personal data.
CMS created these rules in response to complaints about TPMOs selling the personal information of Medicare enrollees. In the final rule fact sheet, the CMS cautions, “Individuals may be unaware that by placing a call or clicking on a genericlooking web link, they are unwittingly agreeing and providing consent for their personal beneficiary data to be collected and sold to other entities for future marketing activities.”
Beneficiaries who unknowingly give their permission report receiving an overwhelming number of unsolicited ads and cold calls from insurance brokers. These aggressive sales pitches can pressure them into choosing an MA or Part D plan that doesn’t cover all their health needs.
The CMS has developed several regulations to address this serious issue. First, TPMOs must ask individuals for express written consent before sharing their data with third parties. This change gives Medicare enrollees more control over their data. Additionally, organizations must get separate written consent for each TPMO receiving enrollee data. For example, a health insurance broker wanting to share a customer’s data with five TPMOs for marketing purposes would need to get the beneficiary’s permission five times before each disclosure. This policy increases transparency and helps beneficiaries understand where their data is going.
In a statement, Senate Finance Committee Chair Ron Wyden highlighted the benefits of this policy, explaining, “This announcement is a big win for seniors because it strengthens protections against deceptive and high-pressure marketing practices that have been plaguing seniors.”
The Biden-Harris Administration has prioritized affordable prescriptions for Medicare patients. They created the Inflation Reduction Act in 2022, but several of its policies didn’t go into effect immediately.
Starting in 2025, this law will cap annual out-of-pocket prescription costs for people with Medicare Part D at $2,000. Once beneficiaries reach this threshold, Medicare will cover the entire cost of their covered medications for the remainder of the year.
This policy aims to make healthcare more accessible and affordable for Medicare beneficiaries. In a press release, CMS Deputy Administrator Meena Seshamani explained that the cap “will provide needed relief for millions of Americans who rely on prescription drugs to stay healthy.”
The CY 2025 final rule will allow healthcare providers to make midyear substitutions of biosimilar products. Clinicians can update their formularies throughout the year without waiting for prior approval from the CMS.
This new policy increases access to affordable healthcare and enables patients to receive cutting-edge care. Providers will be able to make drug plan changes if new treatment options emerge or a prescription changes costs.
For instance, a clinician could prescribe an expensive, brand-name ACE inhibitor to a Medicare patient. Later that year, a more affordable, biosimilar product is released. The clinician can switch their patient to the cheaper option without prior approval, saving money and time.
Medicare Advantage plans offer an average of 23 supplemental benefits. Some plans make these benefits optional, while others provide them for all beneficiaries. These supplemental benefits may include:
• Dental care
• Gym membership
• Hearing aids
• Home air purifier
• Meal delivery
• Transportation for medical or non-medical needs
• Vision care
These benefits can improve Medicare enrollees’ overall health, but many people don’t take advantage of them. The
CY 2025 final rule addresses this lack of usage by requiring Medicare Advantage plans to send beneficiaries a “Mid-Year Enrollee Notification of Unused Supplemental Benefits.” This notice must be issued between June 30 and July 31 each year. The notification will also include additional resources, such as guidelines about accessing each benefit and a hotline to call for help. This rule will improve clients’ understanding of their MA plans and help them maximize their benefits.
Medicare policies can be complex and confusing, even for experienced clients. Keeping updated about Medicare changes for 2025 and beyond will allow you to provide your clients with accurate and informed guidance. You can help them pick the right plan, access supplemental benefits, and more. This knowledge can also help you avoid penalties for non-compliance with compensation caps or misinformation. By staying informed, you can confidently navigate Medicare regulations and advocate for your clients’ best interests.
SOURCES:
CMS.gov: Contract Year 2025 Medicare Advantage and Part D Final Rule (CMS-4205-F), Inflation Reduction Act and Medicare, CMS Releases Proposed Payment Updates for 2025 Medicare Advantage and Part D Programs
WABE.org: "Medicare shoppers often face a barrage of unsolicited calls and aggressive ads."
Senate Committee on Finance: "Wyden Statement on Medicare Advantage and Part D Final Rule."
National Council on Aging: "What Are Medicare Advantage Supplemental Benefits?"
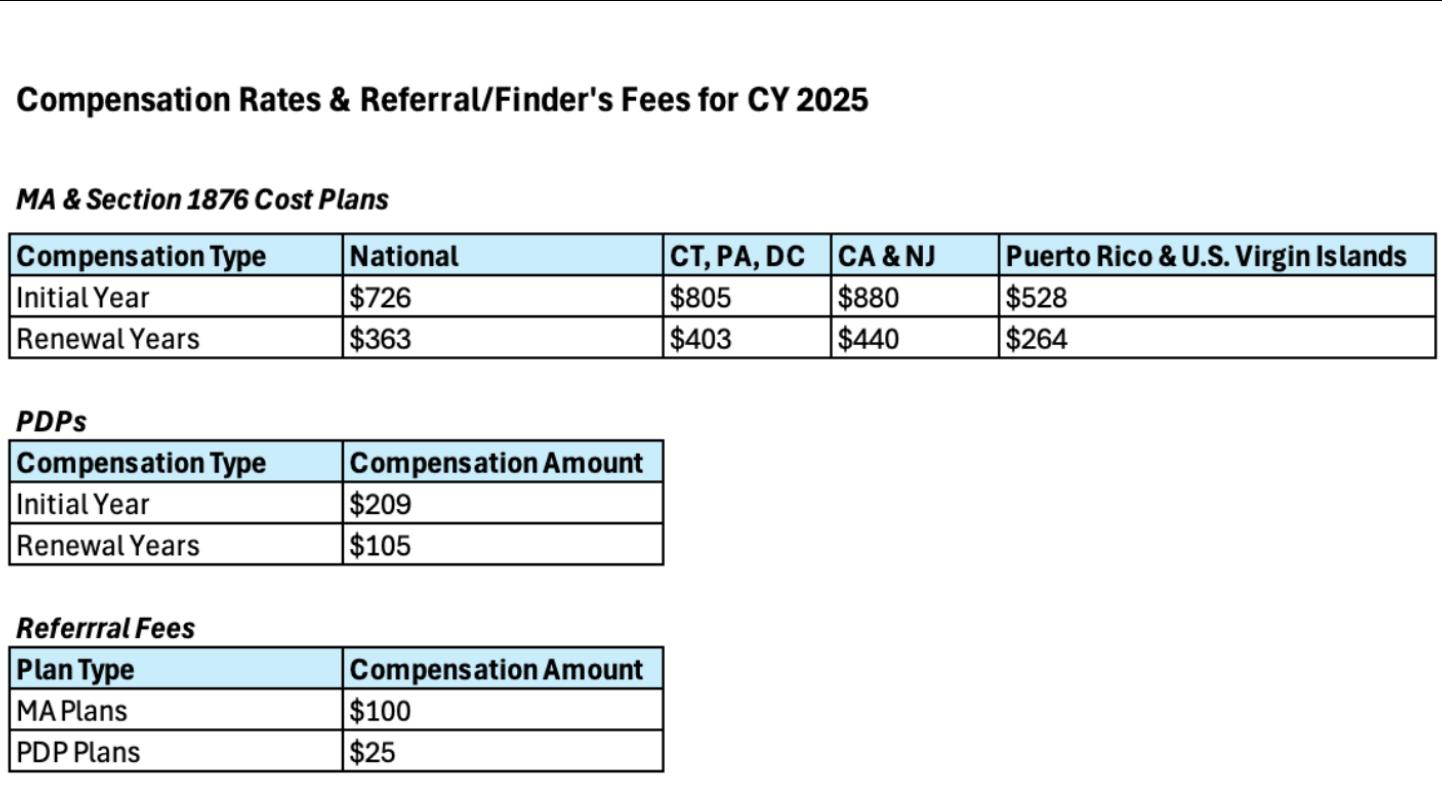

By CalBroker Mag
When an employee reaches 65, they become eligible for Medicare coverage. Medicareeligible employees who work full-time may opt to continue with their current employer's healthcare plan. However, an employer’s health insurance may not cover certain medical service costs if the employee or their spouse can use Medicare benefits instead. As their trusted insurance advisor, you can guide your clients in planning for Medicare while still working full-time to avoid unnecessary complications such as coverage gaps and enrollment penalties.
Employees approaching age 65 who plan to continue working full-time should consider planning their health coverage in advance to avoid complications. If they wait until they become Medicare-eligible, they may face the following problems:
Insurance companies sometimes refuse to pay for services covered by Medicare if they know the patient is eligible for it. They may also reduce the amount they are willing to pay for covered services. This can occur even if the patient has not formally applied for or received Medicare.
Individuals eligible for Medicare may face late penalties if they fail to enroll during the appropriate period. Typically, Medicare charges a penalty of 10% of the premium for each year the employee could have been on Medicare but did not sign up.
This penalty does not typically apply if the employee has health insurance coverage when eligible. However, if the employer coverage is limited, reduced, or eliminated because the employee is Medicare-eligible, they could also face the late enrollment penalty.
If a full-time employee becomes eligible for Medicare but doesn't plan for potential coverage loss, they could face coverage gaps. For example, their employer's health insurance policy may automatically reduce or eliminate coverage once they become eligible for Medicare. If the employee fails to enroll in Medicare coverage within the appropriate enrollment period, they may remain without health coverage until the next enrollment period.
Medicare is divided into four categories with different types of coverage and enrollment requirements:
• Part A, for hospital coverage
• Part B, for healthcare coverage
• Part C, for private Medicare Advantage Plans
• Part D, for prescription coverage
Medicare Part A allows employees to sign up as soon as they meet eligibility requirements and may cover them retroactively. On the other hand, Medicare Parts B, C, and D require enrollment within four months before or three months after the employee turns 65.
The enrollment periods may not apply if the employee is still enrolled in a group plan through their employer. They have the option to sign up for Medicare while they have employer coverage or 8 months after employment or coverage ends, whichever is first.
Other types of coverage that can affect Medicare enrollment periods include:
• Retiree coverage
• Consolidated Omnibus Budget Reconciliation Act (COBRA) coverage
• Veterans Affairs (VA) coverage
• Individual health insurance
• Health Insurance Marketplace coverage
• Union coverage
• Active-duty and retired military coverage through TRICARE
• Federal or state employment coverage
• Medicaid Coverage
Coordination with employer coverage is crucial when planning for Medicare. Employees approaching 65 should contact their employer’s HR department or call the group insurance carrier directly to discuss their options. If they wish to continue with their current employment coverage, the employee may choose to delay their Part B enrollment without a penalty.
Sometimes, employees maintain both Medicare and group health insurance. Medicare has established primary and secondary payer rules to determine which coverage pays first for services.
Generally, Medicare pays first when:
• The employee has retiree health coverage
• When the employee is over 65, and their group health plan is through a current employer with fewer than 20 employees
• When the employee is under 65 and has a disability, and their group insurance coverage is through a current employer with fewer than 100 employees
The employee’s group health insurance pays first if they are over 65 and their group coverage is through a current employer with 20 or more employees. Group insurance also applies before Medicare if the employee is under 65 with a disability and their group insurance is through a current employer with 100 or more employees.
Employees with TRICARE coverage, Medicaid, or endstage renal disease (ESRD) usually operate on different payment schedules.
If an employee has an HSA account with their group insurance plan, they cannot continue to make contributions after their coverage becomes active. Typically, HSA contributions should be discontinued a month before the employee turns 65.
When an employee plans to sign up for Medicare six or more months after they turn 65, they should stop paying into the HSA six months before they apply for Medicare. If the employee makes contributions to their HSA after the required deadlines, they may be charged a tax penalty.
For employed individuals whose spouses are eligible for Medicare, the same general rules apply. Spouses who are eligible for Medicare due to age or disability can opt to keep their spouse’s coverage through a current employer.
The order of coverage for employees who have both Medicare and group insurance depends on the spouse’s age or disability and the number of employees covered by the employer's group insurance plan.
Medicare is an excellent resource for individuals over 65 or those with disabilities. However, employees who wish to continue full-time employment after they become eligible for Medicare may face complications. Planning for Medicare eligibility in advance can ensure full-time employees and their spouses maintain health insurance coverage without coverage gaps or penalties.
Employees should reach out to their employer’s HR department or group insurance carrier to discuss whether coverage will continue if they become eligible for Medicare. They should also explore the transition process from employer coverage to Medicare and the possibility of selecting a multi-payer option. With your expertise in insurance planning, you can help your clients effectively prepare for Medicare while they're still employed full-time.
SOURCES:
U.S. Department of Health and Human Services: "Medicare & You 2024." Medicare.gov: "Working past 65."
By Marc Glickman, FSA, CLTC
I recently attended the annual Medicarians conference to meet with Medicare agencies about long-term care insurance. The conference once again saw record growth with thousands in attendance. A shout out to Jay Weintraub and Sonya Larson for hosting an amazing show and advocating for LTC planning.
There continues to be significant interest in LTC planning for many Medicare clients. Medicare does not cover most LTC services and LTC planning is an essential part of financial planning for most clients who are 65 or older.
Traditional LTC insurance and life hybrids continue to be leading solutions quoted for clients ages 65 and older. However, the value of these solutions may erode for clients purchasing in their retirement years. Nearly half of all applicants are declined for traditional LTCi based on their health at ages 65 and older. Also, because product pricing rapidly increases with age, the insurance leverage may not to be as compelling especially for females.
A couple of LTC insurance alternatives have emerged to fill the gap including:
• Short Term Care insurance for pay-as-you-go funding
• Annuities with LTCi riders for single premium funding
• Let’s explore the solutions growing in popularity in this market segment.
STC is a health product that offers an affordable alternative to traditional LTCi covering care needs typically up to one year, with some products offering both a year of home care and a year of community care. The underwriting process for STC is less stringent, often involving a simple health questionnaire and drug screen, but without requiring medical records or exams. This makes it accessible to more applicants, including those with pre-existing health conditions.
For clients that can’t health qualify or afford traditional LTCi, STC can provide professional care with indemnity benefits and a 0-day elimination period. A one-year plan can provide a huge benefit for a family even if it doesn’t cover most of the risk. Picture buying family time and money once the care event happens instead of reacting to a crisis scenario that creates even more stress.
Short-term care can also be added to complement other LTCi products. For example, many agents use STC as a supplement to products with a 90-day elimination period or to enhance coverage at the beginning of a claim with the indemnity payout if there is proof of loss for each policy.
Be careful with product selection as contract language is not standardized and STC is not available in all states. As a health insurance product, it may be subject to rate increases or decreases in the future.
In states where STC is not available, we have seen one carrier recently launch in all 50 states, a simplified issue traditional LTC insurance coverage with 1 to 2 years of coverage that works similar to STC.
with a Specialist on a ShortTerm
• Client Profile:
• Age: 65
• Health: Moderate, with a few chronic conditions
• Financial: Modest retirement savings and desires an affordable pay-as-you go premium
• Coverage: Medicare Advantage
Process:
1.Needs Assessment: The Medicare specialist assesses the client's health and financial situation.
2.Specialist Consultation: The Medicare specialist can refer the client to an LTC specialist who can shop the market and work as an extension of your team to process the case start to finish. At BuddyIns, we help match Medicare agencies with LTCi specialists. To request help for a client, complete this form: BuddyIns Referrals - BuddyIns
3. Finalizing the Case: Compensation on STC products can be split with other licensed agents. Needs Assessment: The Medicare specialist assesses the client’s health and financial situation.
This sample STC product provides up to $12,000/month for one year of facility care and up to $4,800/month for one year of home health care. The product is unisex priced, so females get especially good value relative to traditional LTCi, which is often priced 50% higher for females.
The benefits are available immediately, but if care is needed at age 85, STC may provide tax-free health insurance benefits at 4.1x the premium paid into the plan as is shown in this example:
app.buddyins.com
You can edit the plan and compare the cost of care once you sign up for a free trial to the Buddy System
STC can be an excellent alternative for clients who are looking for a pay-as-you-go premium who would not otherwise be a good fit for a traditional LTCi solution.
For clients who have more assets, another alternative solution is an annuity + LTCi hybrid. Whereas the pricing of life hybrids can get relatively expensive at ages 65 and older, the pricing of annuity hybrids does not increase as much with age.
The underwriting process for annuities is much less stringent with a page of knockout questions rather than the full underwriting that life hybrids often require.
While there are not as many carriers offering annuity with true LTCi riders, the ones that offer the product are growing quickly in popularity.
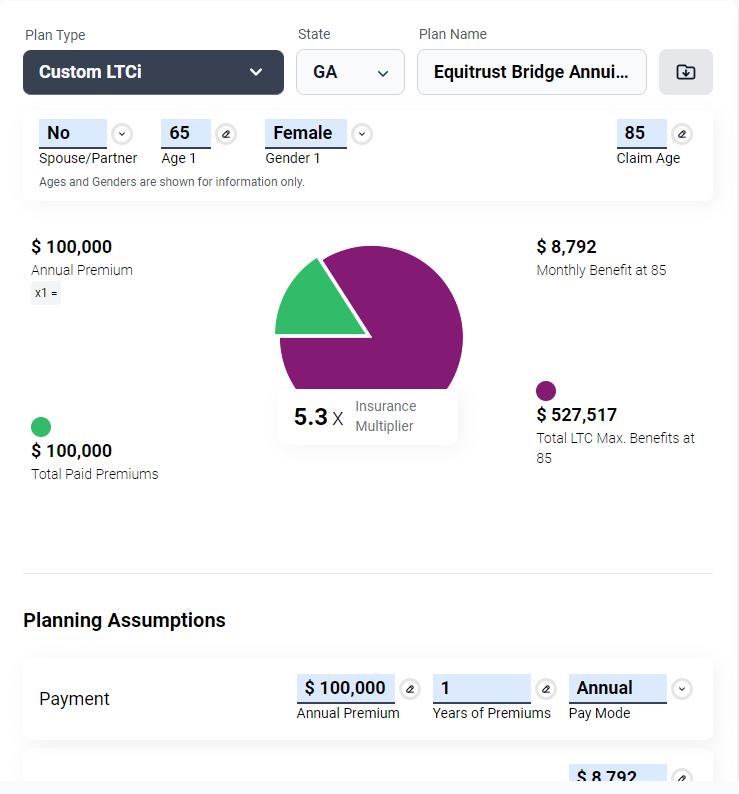



Here are a few reasons why annuity products fit especially well for clients who are 65 and older:
• They often have more readily available assets or cash equivalents that can be used to fund the single premium solution.
• The immediate LTC insurance leverage can be 3x or more of the initial deposit, which compares favorably to traditional LTCi and life insurance hybrids at these ages.
The underwriting is designed for clients at these ages, and there’s even a carrier with a guaranteed issue option should they not qualify for the best health rating.
Clients with an existing non-qualified annuity can tax-free 1035 exchange the cash value into an annuity with LTCi rider. The gains on the existing annuity being exchanged may not be taxed as ordinary income when used on the tax-qualified LTCi rider.
While not true LTCi, there are also fixed indexed annuities with ADL doublers that create additional income if the client meets the 2 out of 6 ADL eligibility trigger. A few of these products have expanded to cover home health care in addition to facility care. Carriers see these features differentiate their FIA offerings. The true LTCi rider products have the added advantage of tax-free benefits.
• Client Profile:
• Age: 65
• Health: Moderate, with a few chronic conditions
• Financial: Significant savings in cash, which can be repositioned for long term care needs
Coverage: Medicare Supplement
This annuity with LTCi rider provides up to $8,792/month for five years of home health, assisted living, or nursing home care paid as an indemnity benefit. It is very competitive to a life-based hybrid policy, but with less strenuous underwriting. This product even has a guaranteed issue alternative should the client not qualify based on health.
PUBLISHER’S NOTE:
California Broker is pleased to have a collaborative relationship with Buddy Insurance, a leading long-term care insurance education, marketing and technology company.
CEO Marc Glickman and his specialists will collaborate with health and life insurance professionals to help design LTCi options. Learn more about LTCi and refer clients — or learn how to write your own LTCi policies using Marc’s system.
LTCi PORTAL HERE:
www.buddyins.com/calbroker
You can edit this plan once you sign up for the Buddy System Bottom Line
LTC insurance and alternatives are a crucial addition to Medicare coverage for many clients, offering protection against the high costs of long-term care. By collaborating with specialists, Medicare brokers can ensure their clients receive an expanded array of solutions. Understanding different solutions, payment options, and the compensation structure for referrals helps brokers provide comprehensive and informed solutions to their clients.


Marc Glickman, FSA, CLTC, is CEO and co-founder of BuddyIns, a leading long-term care insurance education, marketing and technology company. Marc is a licensed insurance agent in all 50 states and serves on the Board of Advisors for CLTC. Marc has over 15 years of experience as an actuary including as the chief investment officer and chief sales officer for a major LTC insurance company. Marc earned his degree in economics from Yale University. In 2019, he was named one of the top 20 innovators in the insurance brokerage space.
marc@buddyins.com www.buddyins.com/calbroker 818-264-5464
Helping your clients navigate the decisions related to Medicare is an important mission. You are doing important work!
By
CSP, CPAE President, Referral Coach International
When it comes to guidance with Medicare decisions, folks have a myriad of options. It is your remarkable process that will make you worthy of remark.
In their book The Experience Economy, Joseph Pine and James Gilmore examine what it takes to create word of mouth; what it takes to get your clients telling others about you. And to make their point, they use the metaphor of coffee beans. It goes something like this…

If I were to travel to Brazil and buy fresh picked coffee beans on the wholesale market I would expect to pay about $1.00 per pound. Coffee beans at the source are a commodity. If I went into a grocery store here in the states, coffee beans would cost me about $14.00 per pound depending upon the brand and part of the country (could be a little less or a lot higher). Coffee beans purchased retail are goods. If I purchased a cup of coffee in a diner, I would be paying about $180 per pound of beans. Brewed coffee in a diner is a service. Then there’s Starbucks and all the other high-end coffee shops that have proliferated in our great country. These stores are meant to create an experience.
The premise behind Starbucks was to recreate the Italian Coffee experience. While one could argue that, over time, this experience has been lost, it was the reason for Starbucks initial success story. Commodities are interchangeable. Goods are tangible. Services are intangible. Most financial professionals play on the level of goods and services. You talk about the products you represent and about the service you provide. Nothing wrong with that. Those are important! However, you’re missing opportunities to create word of mouth and become highly referable if you don’t deal on the level of experiences. Experiences are memorable. Memorable experiences are worthy of remark.
Do you have a clearly defined process through which you put most of your new clients? Do you help think big picture? Do you educate them? Do you question their assumptions and
correct their mistaken beliefs? Do you lead them to make the right decisions and stop procrastinating? Do you use the same high-level process virtually every time or do you wing it?
Take a minute to think about the process you put your prospects and clients through from the minute you first contact them, all the way through to when they become a client and beyond. Are you creating “memorable experiences?”
Here are five steps that will ensure you get the most out of your process – to become so referable that you generate unsolicited referrals and if you ask, you are having willing participants.
Have a clearly defined process that is repeatable and naturally gets your prospects and clients wanting to introduce you to others.
Name your process. When you name your process, it becomes yours. No one else has your process. Clients can only get this process from you. This is a way to distinguish yourself in this crowded marketplace.
Illustrate your process with graphic design – on paper and/ or PDF. This brings your process to life. It helps you explain your process to your clients and centers of influence.
Communicate to prospects, clients, and centers of influence why/ how your process is beneficial. Get in the habit of talking about your process on a regular basis.
Bring it to life with stories, anecdotes, and case studies. Stay compliant with your stories and talk about peace of mind and other benefits of your work.
So, your mantra from now on – if you want to become referable quickly in your relationships and remain referable throughout –is process not products.

Bill Cates, CSP, CPAE, is the author of Get More Referrals Now, Beyond Referrals, and Radical Relevance. Bill’s newest book, The Language of Referrals, has just been released and is available as a at Amazon in paperback, Kindle, and Audible. Bill is a highly sought-after coach, consultant, international speaker, and virtual presenter.
CalBroker Readers can get free (and valuable) tools here: www.ReferralCoach.com/resources BillCates@ReferralCoach.com
By Eric Trost
Exhausted by the skyrocketing costs and headaches associated with their fully insured carrier. ACME Inc, an employer with 1700 employees spread across 40 states faced a too familiar challenge, that each year their health insurance premiums would go up. They were paying a fully insured carrier millions of dollars per year-and the carrier planned to increase those annual costs by 18%. Along with facing double digit increases every year they were also struggling to manage plans across multiple states and keep network accessibility.
Tired of costs and headaches associated with fully insured options, ACME, Inc. needed a solution that allowed them to save money while still providing their employees with access to the best provider networks. The company decided to look at Vitori Health’s self-insured alternative to help them:
1. Keep their margins (difference between claims liability and actuarially expected claims), resulting in millions in savings
2. Reduce their pharmacy spend
3. Retain access to the nation’s largest provider networks (open access)
4. Consolidate insurance coverage across all states
This company turned to Vitori Health, which offers an industryleading health plan that help companies save money without losing coverage. Vitori provided them with:
• The ability to only pay for the actual cost of employees’ claims
• Occurrences of balance bills were just 0.2%, 20X less than a traditional carrier
• Eliminated network issues by providing a national open-access architecture
• Flexible plan designs, including Nationwide Surgeons of Excellence program
• Greater price transparency with the most cost-effective and lowest net cost results
• They completed their first year moving from fully insured, to a self-insured plan with millions in Savings, better coverage and an amazing customer service experience.
Take a look at the highlights:
• Saved them $7.97M or 53.7% below cost vs. their prior BUCA carrier
• $2.74M or 28.5% below budgeted expense
• 39.6% / $860K Rx savings - $1.3M vs. $2.17M prior BUCA
• $559,320 preferred surgery savings vs. legacy insurance rates (35 procedures & $15,980 average savings per procedure)
• $243,200 savings with telemedicine use (48% of visits for behavioral health)
• 38% lower stop-loss premium than BUCA self-insured rates
• 5 avoided stop-loss claims that would have occurred under BUCA reimbursement rates that led to a reduced stop-loss renewal
Client Feedback, “Our sales team would need to increase sales by more than $80M to equal the P&L impact of the savings we’ve seen with Vitori Health.”
Learn how we can help you win and retain more business. Vitori Health creates a financially sustainable future for a mid-market broker/consultant running out of options. With rising costs, a looming 4th quarter deadline and a labyrinth of choices, learn how we can become a strategic partner capable of introducing innovative, modern and tangible tools for better control and transparency in managing healthcare costs with an unmatched claims savings guarantee.
Do you have clients that:
• Pay more than $750,000 annually for employee health benefits?
• Have over 150+employees?
• Are fully insured or self-funded?
If so, sign up for our July 23rd Broker Symposium where we will show you how to save your clients 30%.

Eric Trost President, A seasoned employee benefits consultant that has built my career on being employer focused and consumer driven and building strategies that work. My work emphasizes that healthy, productive employees promote healthy business. I have been entrenched in areas such as employee benefit design, PPO network evaluation and other programs that can save self-funded employer groups money without cost shifting to their employees.
As a consultant, I know health insurance is complicated, so I strive to make employee benefits simple, and minimize surprises. My consultative approach helps client partners and employees do more with less. My brand allows employers to reclaim their benefits as an investment vs. an expense.
Benefits Options Insurance Agency
949-922-3920
eric@benefitsoptionsins.com www.benefitsoptionsins.com




Have

Grow,
By Phil Calhoun
The greatest problem with planning is getting started. In 2024, there is still time before you get lost in AEP and open enrollment work. As an Active Broker, you need a Commission Protection Plan to protect your hardearned income and address the fact you will lose your commissions in a life event that prevents you from staying licensed, certified, and capable to handle your client’s service and support. Risks you can plan to deal with include your death or disability. It is common to decide to wait until next year to do this planning work. Another option is to engage in the first step which is to learn more about the process.
This pre-AEP period is a good time to jump on a 15-minute call and get answers about your options to handle risks to your commissions. The most common options for our callers come to resolve are:
#1 Do you want to retire soon and avoid AHIP and carrier certifications, or #2 Will you stay active and work to find a commission protection option.
Planning takes time! The key is to start the process and get your questions answered by a subject matter expert. Your CPA knows tax related issues both personal and corporate. Your lawyer knows personal and corporate legal planning issues. Our commission planning process includes the work we have accomplished with numerous CPAs and estate planning attorneys for 12 years. Through our work with hundreds of brokers we have perfected our role as the expert in health insurance commission planning.
All our planning includes a Purchase Agreement. For plans where the broker stays active, as well as, when the brokers want to sell soon, we use our Purchase Agreement.
Preparing to sell a book of business is a significant undertaking. For most health insurance professionals, the process requires careful planning and consideration. Again, in situations where brokers decide to stay active, they need a plan to protect their commissions. Many of our broker clients have similar concerns. Most often we see the timing when to retire followed by how they want to be paid when they do sell. The solutions we work on for our broker clients are all customized with solutions to fit the broker’s requirements.
Let’s start with the key components that most brokers move through as they start the process to exit the business.
IT/Tech is always important to have your financial statements, tax returns, and any other relevant financial documents organized in an electronic format. Current numbers with details such as revenue by carrier and type of insurance line is the goal.
In some cases, your accountant can help as they normally have a solid heads-up on your business and can efficiently get your financial records accurate and up to date.
When it comes to determining the value of your book of business, Buyers need to see two key items, revenue, and client numbers. From these stats they will see trends. First your financial statements will show the commission income for the current year and the recent two years. In addition to these totals, Buyers want to review trends. Trends lead to the second focus which is a review of client growth and retention. The number of clients you have now and what the client numbers were each of the past two years will be used to complete the trend analysis.
Solid financials lead to higher value and stronger Buyer interest.
Ensure all legal and regulatory requirements are met, including insurance and business licenses, permits, contracts, and agreements.
Resolve any outstanding legal issues or disputes that could affect the sale process. The marketing rules and requirements need to be documented and shared.
Since health insurance sales are mostly only on commissions that are transferred to a Buyer, commissions are the top asset of value to a Buyer. Employees who will stay are also of value to most Buyers. Office equipment and technology may not be needed and certainly are of limited value in many cases.
Streamline your operations and improve efficiencies to make your business more attractive to potential buyers.
Document key processes and procedures that can be scalable and sustainable. Mostly your annual renewal processes are considered both to determine if there is any unique value or take away in your processes, and if so, can these processes be transferred.
Processes lead to consistency and increase the value of your book of business.
Quietly let your trusted colleagues know you are looking for potential partners and buyers. Health plan reps offer a possible lead source. Working with a listing service or business broker is a last resort but may be necessary. Often brokers who have purchased a book recently know of colleagues that may be an option.
Build a strategy to attract potential buyers. If large enough you may include creating a confidential information memorandum (CIM) or teaser document.
Identify and target potential buyers, including strategic acquirers, competitors, investors, and private equity firms.
Develop a best fit list of qualities you look for in a Buyer.
Consider your employees as your Buyer.
Maintain confidentiality throughout the sale process to protect sensitive information and prevent disruption to the business. Use non-disclosure agreements (NDAs) and confidentiality agreements to safeguard proprietary information.
Your CPA or Attorney can be the first place to start. They may know Buyers or be connected to colleagues who have clients in the industry.
Consider hiring a team of professional advisors, including a business broker, investment banker, attorney, and accountant, to guide you through the sale process.
Seek advice from experts who specialize in mergers and acquisitions (M&A) to ensure a successful transaction.
There are local associations and groups to consider such as the Exit Planning Institute. Members often have many connections in the M&A industry.
Anticipate buyer due diligence inquiries by compiling comprehensive documentation on all aspects of the business, including financial, legal, operational, and human resources.
Be prepared to address any potential concerns or questions raised by prospective buyers during the due diligence process.
In most cases, when a Seller wants more of the agreed value paid up front (100% in a short time), the risk increases for a Buyer. Look for a Buyer who can show they have the funds needed and a track record and process to retain clients.
Negotiate favorable terms and conditions of the sales agreement, including price, payment terms, warranties, and representations.
Work with your advisors to finalize the sales transaction and ensure a smooth closing process.
Develop a transition plan to facilitate the handover of the business to the new owner, including training and support during the transition period.
Communicate with employees, customers, suppliers, and other stakeholders to minimize disruption and ensure a seamless transition.
In your planning work, success when staying active is to assure you have 100% commission protection in all life events when you stay active and wait to sell your book of business.
The above information is a fit for all situations. When you plan to stay active or if you want to sell soon, doing this planning work outlined here will help. We know planning for your business can be a complex and time-consuming process. There are many ways planning starts and stops, gets sidetracked, or just is put off for another day. Please know that with careful planning and the right support, you can maximize the value of your business and achieve success. In your planning work, success is staying active with 100% commission protection in all life events or in the sale of your book of business.
Discover how a Commission Protection Plan can help you protect your hard-earned income.


Phil Calhoun is owner and publisher of California Broker Magazine. Phil also is a leader in coaching health insurance professionals. He is an active member of several insurance associations including the California Association of Health Insurance Professionals (CAHIP) and local chapters in Orange County, Los Angeles, San Diego and Inland Empire Health Insurance Professionals. He attends many state and local California chapter meetings. He offers complementary 15-minute coaching sessions. To schedule a phone call “Click Here”
phil@commission.solutions 714-664-0311 www.commission.solutions

ataracts and refractive errors are common conditions. Over half of all Americans aged 80 years and older have cataracts, while 150 million have a refractive error.
Simple treatments can help with these conditions, but people may eventually need advanced cataract treatment. Understanding these conditions, the symptoms, and the typical medical care can help you find the best vision insurance for your clients.
Cataracts and refractive errors are eye conditions that cause vision problems. Refractive errors may be a standalone condition or a symptom of cataracts.
Cataracts are a progressive eye disease that causes the normally clear lens of the eye to cloud over, limiting the passage of light to the retina. There are many types and causes of cataracts. Your clients may develop cataracts:
• At birth, as a side effect of certain infections or the mother’s nutrition
• As part of aging
• As a complication of another disease, such as diabetes
By CalBroker
• From an injury to the eye
• As side effects of some medications
• From chemical injuries or exposure to UV light
• From poor nutrition, smoking, or alcohol use
The lens is made of fibers and is inside a membrane called the lens capsule. These fibers break down for various reasons, and proteins clump inside this capsule, building up and turning the lens from clear to cloudy.
Cataracts usually develop slowly and worsen with time, especially without treatment. This eye disease is more prevalent in women than men and can make daily activities difficult.
Refractive errors are a common condition in which the shape of the eye prevents light from hitting the back of the eye directly, leading to blurriness. These errors may also develop from a thicker or thinner lens, a flatter eye surface, or an eye that’s too short or too long.
• There are several types of refractive errors, including:
• Myopia or nearsightedness, where items far away look blurry
• Hyperopia or farsightedness, where items close up look blurry
• Astigmatism, where objects close or far look blurry or distorted
• Presbyopia, where older people have trouble seeing items up close
Cataracts may lead to refractive errors as the cloudiness affects the lens and changes how light hits the back of the eye. For example, age-related cataracts typically cause nearsightedness, while other forms may also lead to astigmatism.
The main symptoms of refractive errors are blurriness and distorted vision, either with objects far away, up close, or both. They may also cause headaches, squinting, glares or halos around lights, tired or sore eyes, and trouble focusing. Refractive errors may also be a symptom of cataracts.
However, cataracts come with other symptoms, including:
• Sensitivity to glare
• Glare or rainbow halos around lights
• Worsening nearsightedness that may cause frequent changes in prescription glasses
• Double vision
• Blurry or cloudy vision
• Poor night vision
• Colors appear faded
• Cataracts may also lead to blindness without treatment and are one of the most common causes of blindness worldwide.
A healthcare provider can diagnose both conditions based on clinical information. They may take a history of your client’s health and symptoms and perform several eye tests to assess vision and check eye health.
• Typical tests include:
• Pupil dilation, where they apply eye drops to widen the pupil and look at the retina and optic nerve
• Visual acuity, or the eye chart test that measures vision
• Slit-lamp, a microscope with an intense light to check the cornea, iris, and lens
• Tonometry, to check the pressure inside the eye
The healthcare provider may easily see a cloudy or gray lens, though it may also look dark brown, black, or yellow.
The simple treatment for refractive errors is to wear glasses or contact lenses. These temporary lenses bend light so it hits the back of the eye or the retina directly and produces clear vision. Laser surgery is another option, which corrects the eye shape to eliminate or reduce the refractive error.
Treatment in the early stages of cataracts starts with new glasses, other vision aids, and lifestyle adaptations. Eventually, surgery may be necessary as vision worsens.
Simple habits or tools can help patients with cataracts adjust to changing vision, and these vision aids are the most common treatment early in the disease. Vision aids include:
• Bright lights for reading or work
• Magnifying lens to help with reading or other tasks
• Anti-glare sunglasses
• Patients may also need new prescription glasses or contact lenses and may need to change them frequently.
• Surgery
If cataracts progress and cause worsening vision that interferes with daily living, surgery is necessary. Cataract surgery is one of the most common procedures in the U.S. and is safe and effective.
The procedure is simple. A surgeon makes a small cut in the cornea—which is the dome-shaped surface that covers the eye—and removes the cloudy lens. Then, they insert a clear artificial lens to improve vision.
Simple lifestyle changes and habits can help prevent cataracts from developing. Your clients can:
• Quit smoking
• Eat a healthy diet of leafy greens, nuts, whole grains, fruits, and vegetables
• Limit alcohol use
• Wear sunglasses to protect the eyes
• Manage underlying conditions
• Local Resources Several organizations offer education, eye exams, new glasses or contact lenses, or free cataract surgery to patients without insurance, with limited insurance, or who can’t pay. These include:
• EyeCare America: Offers no-cost exams and eye care to people aged 65 and older
• Lions Club SightFirst: Provides gift certificates for exams or frames and lenses for those without insurance or limited insurance
• Mission Cataract USA: Performs free cataract surgeries for individuals who are unable to pay
• Quit Day: A government program aimed at helping people quit smoking, which can help prevent cataracts
• Tang Center: A university clinic offering treatment by medical students and specialty referrals for complex care
• Discussing Vision and Eye Care Insurance With Clients Cataracts and refractive errors require regular exams and health care for monitoring and treatment. In particular, aging clients may need additional coverage to secure the appropriate treatment. Assessing your client’s health and lifestyle patterns can help you understand their needs and find the best plan.
SOURCES:
StatPearls Publishing: “Cataract.”
Johns Hopkins Medicine: “Refractive Errors.”
British Journal of Ophthalmology: “Refractive Error Changes in Cortical, Nuclear, and Posterior Subcapsular Cataracts.”
University of Rochester Medical Center: “Cataracts.”
AGS Health in Aging Foundation: “Cataracts: Diagnosis & Tests.”

By CalBroker
Osteoporosis and arthritis affect millions of Americans, especially older adults. Healthcare professionals have developed numerous treatments and preventative methods to treat these conditions. However, many medical plan members don’t know about these available options — or even, in some cases, that they may be at risk for osteoporosis and arthritis.
Health insurance professionals can promote bone and joint health by educating clients about the importance of preventative services and routine checkups. Learning about the symptoms, diagnosis methods, and treatments for osteoporosis and arthritis will also help you advocate for your clients more effectively.
People often use the terms osteoporosis and arthritis interchangeably. However, they’re distinct conditions that affect different parts of the body.
• Osteoporosis
• Osteoporosis occurs when the bones lose mass and mineral density faster than they grow. These changes cause the bones to weaken and become fragile, which can lead to breaks.3
Arthritis is a broad term for joint disease or pain. Researchers have identified over 100 types of arthritis with varying causes and symptoms.
Osteoarthritis is the most prevalent type of arthritis. This condition develops when weakening bones damage the connective tissue in the joints and cause painful inflammation. Other common types of arthritis include autoimmune inflammatory arthritis, gout, and infectious arthritis.
An estimated 10 million Americans aged 50 and older live with osteoporosis. Another 43 million people have low bone mass, which may eventually progress into osteoporosis.1 Plan members with this condition can benefit from early screening and management techniques.
People with osteoporosis often don’t notice symptoms, especially during the early phases. This condition typically only becomes evident when a bone breaks.
The most common osteoporosis-related fractures affect the hips, spinal vertebrae, and wrists. These fractures can occur when an individual falls or performs everyday activities. For example, they might break vertebrae while bending over to tie their shoes or fracture a wrist while carrying groceries. Fractures may also happen spontaneously.
Women are more likely to develop osteoporosis than men because they have thinner bones. Advancing age can also lead to osteoporosis as bones lose density and weaken over time.
Other factors that increase the risk of developing osteoporosis include
• Having a slender frame and small bones
• Low levels of estrogen or testosterone
• A family history of osteoporosis or hip fractures
• Dietary deficiencies in calcium and vitamin D
• Low protein intake
• Sedentary lifestyle with infrequent exercise
• Smoking Prolonged use of certain medications, including glucocorticoids, proton pump inhibitors, and selective serotonin reuptake inhibitors (SSRIs)
Healthcare professionals typically use a bone mineral density (BMD) test to diagnose osteoporosis. This painless method uses dual-energy X-ray absorptiometry (DXA) to detect bone loss.
Healthy people have a hip BMD T-score of -1 and higher. People with low bone mass score between -1 and -2.5, while those with osteoporosis score -2.5 or lower.
The International Osteoporosis Foundation recommends BMD testing for everyone aged 65 and older to screen for osteoporosis.
Researchers haven’t developed a cure for osteoporosis yet. However, the Food and Drug Administration (FDA) has approved several medications to manage or prevent this condition, including:
• Bisphosphonates
• Calcitonin
• Estrogen and hormone therapy
• Parathyroid hormone analog
• RANK ligand inhibitor
• Sclerostin inhibitor
• Understanding Arthritis
According to the Arthritis Foundation, this condition affects almost 60 million Americans, or 25% of adults. Recognizing the symptoms and causes of arthritis can help clients receive prompt treatment.
Arthritis can affect every joint, including the elbows, fingers, hands, hips, knees, and shoulders.
Here are the hallmark symptoms of this condition:
• Persistent joint pain lasting for three days or longer
• Joint swelling that occurs three or more days monthly
• Redness and warmth surrounding the joint
• Stiffness or inability to move the joint
The arthritis effects can also include non-joint-related symptoms. For example, people with these conditions may experience fatigue, fever, rashes, scaly skin, and weight loss.
Causes
There are many arthritis causes, such as:
• Autoimmune disorders
• Bacterial, fungal, or viral infections
• High uric acid levels
• Nutritional deficiencies
• Occupational damage
• Sedentary lifestyle
Diagnosis
Clinicians can diagnose arthritis with X-rays, MRI, or ultrasound. These tests can reveal the presence of joint erosion and inflammation. They may also perform blood or joint fluid tests to diagnose inflammatory arthritis and other conditions.
Arthritis specialists (rheumatologists) and other healthcare providers may prescribe these treatments for arthritis pain:
• Non-steroidal anti-inflammatory drugs (NSAIDs)
• Zostrix cream
• Corticosteroid injections
• Preventative Measures for Osteoporosis and Arthritis
There’s no guaranteed way to prevent osteoporosis and arthritis. However, there are many ways to improve and maintain joint and bone health.
Exercise is one of the most effective ways to reduce the risk of arthritis and osteoporosis. Older adults should participate in moderate exercise regularly to build muscle and improve flexibility. Physical activity will help keep bones strong and joints mobile.
Diet can also affect the bones and joints. A nutritious diet with adequate vitamins and nutrients can maintain bone density. Men and women over 70 should consume 800 IU of vitamin D daily. Additionally, men over 70 and postmenopausal women of all ages should get 1,200 mg of calcium daily.
Glucosamine and chondroitin sulfate supplements support healthy cartilage and may reduce joint pain. These natural remedies are available over the counter.
You can support clients with osteoporosis or arthritis by connecting them with these resources in California:
Arthritis Foundation California: This branch of the Arthritis Foundation hosts regular events and webinars to support and educate California residents with arthritis.
Bone Health and Osteoporosis Foundation: This organization hosts osteoporosis support groups in San Diego and Torrance, CA.
Free DXA scans: The University of California San Diego School of Bone Densitometry offers free DXA scans for San Diego residents.
Osteoporosis and arthritis are common conditions that can significantly impact your clients’ quality of life. Fortunately, most health plans cover bone density screenings for postmenopausal women and all women over 65. Men may also qualify for preventative screening for osteoporosis.
You can also encourage clients to schedule appointments with their physician if they experience joint pain and other arthritis symptoms. Routine care will help plan members protect their health and stay mobile.
SOURCES:
CDC: Osteoporosis or Low Bone Mass in Older Adults: United States, 2017–2018, Arthritis Related Statistics
National Institute of Arthritis and Musculoskeletal and Skin Diseases: Osteoporosis
Arthritis Foundation: What Is Arthritis?
International Osteoporosis Foundation: DIAGNOSIS
National Institute of Arthritis and Musculoskeletal and Skin Diseases: Osteoporosis: Diagnosis, Treatment, and Steps to Take Arthritis Foundation: “About Arthritis, Recognizing the Symptoms of Arthritis, Diagnosing Arthritis
MedlinePlus: Medicines, injections, and supplements for arthritis, Aging changes in the bones - muscles - joints, Arthritis Foundation California
Bone Health and Osteoporosis Foundation: “BHOF Support Groups.”
UCSD School of Bone Densitometry: “Free Scans.”
HealthCare.gov: “Preventive care benefits for women.”
Discover the groundbreaking potential of GLP-1 agonists in tackling obesity. From reshaping insurance coverage to revolutionizing workplace wellness, explore how these medications are transforming the fight against excess weight and its associated health risks.
By Misty Baker
New weapons are emerging in the battle against obesity, and among the most promising are Glucagon-like peptide-1 agonists, or GLP1s. These medications, developed initially to manage type 2 diabetes, are now gaining significant attention with their gamechanging potential to impact and assist with weight loss. As their effectiveness becomes increasingly evident, health insurance companies and employers are starting to take notice and are swiftly adapting their strategies to embrace this groundbreaking approach.
GLP-1's belong to a class of drugs that mimic the action of glucagon-like peptide-1, a hormone that regulates blood sugar levels and appetite. Initially introduced as treatments for type 2 diabetes due to their ability to stimulate insulin secretion, GLP-1 agonists have demonstrated an unexpected side effect – weight loss.
The emergence of GLP-1's as a weight loss agent is more than just a TikTok trend; it marks a significant shift in obesity treatment. Unlike conventional methods that primarily focus on diet and exercise, GLP-1's can offer a unique option that targets the underlying and root causes of obesity and potentially provides a more comprehensive and sustainable solution.
How does it work? Research has shown that GLP-1's slow down gastric emptying, reducing food intake and increasing feelings of satiety. These effects make them highly effective in promoting weight loss, even in individuals without diabetes. Furthermore, GLP-1's have shown promise in addressing other obesity-related factors, such as improving blood pressure, cholesterol, heart disease, and lipid profiles.
Employers are recognizing the potential benefits of GLP-1's for weight loss, too, both in terms of employee health and productivity, and are responding by incorporating them into their workplace wellness programs and benefits. These initiatives promote healthy lifestyles and encourage weight management, often including educational programs, fitness incentives, and access to nutritional counseling, all of which complement the pharmacological approach of GLP-1's.
Obesity not only contributes to increased healthcare costs but can also lead to higher rates of absenteeism, reduced productivity, and lower morale among employees. By proactively addressing
obesity through interventions, employers can potentially reduce their healthcare expenditures over time and create a healthier, more resilient workforce.
Initially, insurance carriers were reluctant to cover GLP1s as weight-loss medications, a stance shared by both commercial carriers and Medicare and Medicaid, with Medicare even prohibiting them. However, the landscape is beginning to shift, offering a glimmer of hope for GLP1 for weight loss advocates.
In November 2023, the American Medical Association (AMA) passed a resolution “urging all payers to ensure coverage parity for evidence-based treatment of obesity, including FDA-approved medications, without exclusions or additional carve-outs” 3. U.S. Congress has also released the Treat and Reduce Obesity Act of 2023 (H.R. 4818 and S. 2407) in an effort to prompt Medicare to cover weight-loss medications. Additionally, the Congressional Budget Office has been working to provide information to Congress on the potential for preventative medical care, including obesity treatment, to save money. Research shows that preventative obesity care could prevent heart disease and Type 2 diabetes 4.
As clinical evidence demonstrating the efficacy of GLP-1's in weight loss grows, health insurance companies are beginning to take notice, though full coverage isn't widespread yet. Acknowledging the potential of these medications to reduce healthcare costs linked to obesity-related comorbidities, insurers are becoming more open to covering GLP-1 therapies.
Coverage, however, is not always clear-cut. Some GLP-1 drugs are explicitly FDA-approved for obesity management, while others are FDA-approved only for Type 2 diabetes management. Some providers have prescribed GLP-1 agonists approved for diabetes off-label, but pharmaceutical companies are increasingly pursuing approval of the drugs specifically for weight loss.
Plans covering GLP-1 medications for weight loss typically mandate that participants meet three main criteria:
• Being obese according to BMI measurements
• Having at least one related health condition
• Committing to lifestyle changes alongside drug treatment, often including participation in a structured weight management program, including coaching and/or counseling
These requirements aim to ensure that treatment is reserved for those likely to benefit, striking a balance between cost and access via the pre-authorization process.
The decision to cover GLP-1's is a testament to the insurance industry's evolving approach, shifting towards preventive care and value-based healthcare models. By investing in interventions that tackle obesity at its early stages, insurers are aiming to reduce the occurrence of costly complications such as cardiovascular disease, diabetes, and certain cancers, a shift that all should welcome.
Insurers also recognize that the health benefits of covering GLP-1's for weight loss can lead to significant long-term cost savings. Studies have demonstrated that even modest weight loss can lead to substantial health improvements and a reduced need for costly medical interventions.6 By endorsing the use of GLP-1's for weight loss, insurers are promoting better health and securing cost savings for themselves and their policyholders.
Despite the promising potential of GLP-1's for weight loss, they do not come without their own challenges. One significant barrier is the cost of these medications, which can be prohibitively expensive for some patients, particularly those without adequate insurance coverage.
As with any medication, GLP-1 drugs have potential side effects and safety concerns. Nausea, vomiting, and headaches are common side effects of treatment. Some studies have raised questions regarding the possible long-term effects of the drugs on pancreatic and thyroid function.
Another consideration is the need for a multidisciplinary approach to combat obesity and its side effects. While GLP1's offer a valuable tool in the treatment arsenal, they should be used in conjunction with lifestyle modifications, light to moderate exercise, and dietary changes to achieve sustainable weight loss outcomes. An informed evaluation of the risks and benefits associated with GLP-1 drugs is essential, especially when alternative options are available.
So, when, if ever, might these weight loss drugs be covered by insurance? Unfortunately, there's no clear, universal answer. The experts stress that it's really in the hands of insurance companies right now—and levels of coverage vary based on carrier, plan, and how state mandates will evolve over the coming months and years. Large and small employers should also be taking note and weighing projected costs against employee satisfaction, health, and well-being. Reach out to your BenefitMall Compliance Team or your BenefitMall Sales Team to ensure you are up to date with the latest news and information on this evolving topic.
SOURCES:
FDA News Release FDA Approves First Treatment to Reduce Risk of Serious Heart Problems Specifically in Adults with Obesity or Overweight March 2024
Accolade GLP-1 Coverage in Employer Plans Could Nearly Double in 2024
October 2023
American Medical Association AMA urges insurance coverage parity for emerging obesity treatment options November 2023
American Diabetes Association - Standards of Care in Diabetes—2024
USC Shaffer White Paper April 2023
Agronauti Cosmetics Improving Liver Health through Obesity, NAFLD,and Weight Loss April 2023
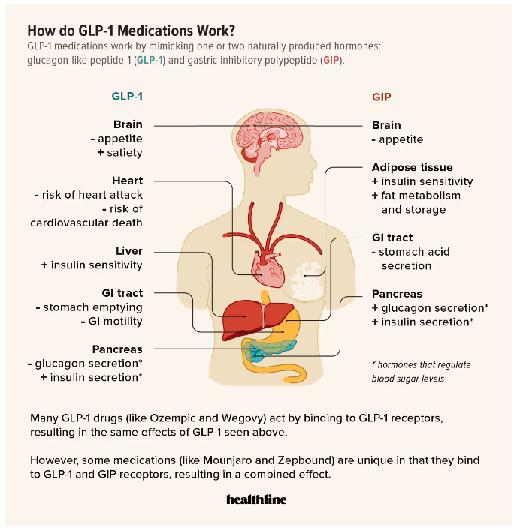



Misty Baker, director of compliance and government affairs at BenefitMall, is an Affordable Care Act compliance and agent advocate, specializing in ACA, ERISA, FMLA, COBRA, and legislative advocacy for over 20 years. She was a registered lobbyist in Texas for four years and is a strategic leader focused on compliance, agent knowledge, legislative advocacy, and ultimate client understanding of how to be successful in the changing world of compliance.
Her passions include agent education, insurance advocacy inside and outside of the Capitol, and compliance.
By Megan Wroe MS, RD, CNE, CLE
hen you think about ‘aging gracefully,’ what images come to mind? For many of us, this concept brings thoughts of minimizing pain, slowing cognitive decline and remaining as independent as possible. When I googled this phrase, all that came up were links about minimizing wrinkles. I recently listened to a podcast where the fitness expert being interviewed discussed the consequences of our current societal beliefs about aging and this really got me thinking. What if instead of thinking about minimizing the effects of aging, we focused on maximizing our health and fitness as we age? What if instead of aging gracefully, we age powerfully? This simple shift of mindset can be incredibly potent so that possibilities in the areas of movement, nutrition and mental health remain open and endless even in our era of retirement, of possible grandchildren and of course, of Medicare. Here are my top 3 tips for aging with power:
Stop thinking that all you can or should do is go on walks. Walking is beneficial no doubt, but powerful bursts of movement keep those fast twitch muscles working effectively.
Think Powerfully. Challenge your brain every single day as often as possible by truly going outside of your comfort zone. This can mean walking in a completely new route, reading a new type of book or article (maybe nonfiction instead of a novel), rotate through puzzles and games, or join new social learning groups to practice new skills with new people, from hiking and book clubs, to sewing or archery classes. Challenges in any form create new synapses that allow our mind be sharp and focused. Similar to our movement mantra, the more you think, the more you think.
Health and fitness expert JJ Virgin is known for prompting her audience with, “what if you could be your healthiest, most fit self at age 60?” Isn’t that empowering? What can you do today to be healthier and more fit than you were yesterday?
Move with Power. Stop thinking that all you can or should do is go on walks. Walking is beneficial no doubt, but powerful bursts of movement keep those fast twitch muscles working effectively. So add in some resistance training 2-3 days per week and in between sets, do some power moves like jumps, rapid squats, high knees or going up stairs quickly. What counts as powerful moves will vary per individual so work with a trainer to do so safely, but remember that the more you move, the more you move.
Eat Power Foods. Aka protein. Most adults do not meet their protein needs and as we age we want to make sure we have enough muscle mass on board, which can only be created through adequate protein intake. A protein calculation of 1.2 grams protein per kilogram body weight is a good place to start. If you know your lean body mass you can also calculate protein needs with 1 gram protein per pound lean mass. (Calculate a 150 pound and 200 pound persons)

Megan Wroe manages St. Jude Wellness Center, an integrative wellness department of St. Jude Medical Center. St. Jude Wellness Center is located in Brea, CA and offers a variety of nutrition, fitness and restorative programs and services for population health.
Visit their website for blog content, recipes and more information: www.stjudewellnesscenter.org


California, known for its diverse healthcare landscape, boasts several hospitals renowned for their excellence in Medicare patient care and rehabilitation services. Here’s a roundup of the top five hospitals in the state that stand out for their commitment to Medicare
Every year U.S. News and World Report ranks hospitals in 15 specialties and utilizes objective data (such as data from Medicare) in 12 specialties, including cancer, heart surgery, and obstetrics and gynecology to develop the ranking results. The Best Hospitals rankings are broken into two subcomponents — specialty rankings, and procedure and condition ratings. We looked at the ratings for Medicare patients and those in need of rehabilitation services from 2023 and compiled from the report the top five hospitals in California for brokers to recommend to your clients based on their specific needs.
As Trusted Advisors, Brokers can share with their Medicare clients this top hospital information
By Emma Peters
We used the geriatrics ratings from U.S News and World Report to put together the geriatrics rating is based on analysis of various data categories, including the number of high-risk patients aged 75 and older, patient outcomes, key programs, services and staff, and professional recognition of the hospital. We have also linked the insurance plans and medical groups accepted by each hospital. It must be noted that contracts between insurance and medical groups are subject to change, so your clients should check with the hospital and their provider before proceeding with a specific hospital.
These hospitals represent the pinnacle of Medicare patient care and rehabilitation in California, each offering unique strengths and specialties that cater to the diverse needs of their patients. Whether through cutting-edge medical technology, research-driven practices, or compassionate care, they continue to set benchmarks in healthcare excellence. Take these hospitals into consideration as you offer your Medicare clients advice and support!
The UCLA Medical Center is ranked No. #3 on a national level for their geriatric services. It provides personalized care plans that cater to the unique needs of Medicare patients. Use this link to survey the Medicare Plan options that are available for patients at this hospital.
2:
UCSF Medical Center is a leader in geriatric care and ranks as No. #4 in the nation for this type of medical care, It integrates research, education, and patient care to deliver top-tier outcomes for Medicare patients. Use this link to survey the Medicare Plan options that are available for patients at this hospital.
3: 5:
Cedars-Sinai consistently ranks high for its comprehensive Medicare services and ranks as No. #8 in the nation for geriatric care. It offers specialized care across various medical disciplines, ensuring holistic treatment for patients. Use this link to survey the Medicare plan options that are available for patients at this hospital.
UCSD Health offers comprehensive Medicare services with a focus on patientcentered rehabilitation. It’s recognized for its compassionate approach and excellent clinical outcomes. It ranks as No. #17 in the nation for geriatric care. Use this link to survey the Medicare plan options available for patients at this hospital.
4:
Located in the heart of Silicon Valley, Stanford Health Care excels in Medicare services with cutting-edge technology and innovative therapies. It’s known for its research-driven approach to patient care and ranks as No. #10 in the nation for geriatric care. Use this link to survey the Medicare plan options available for patients at this hospital.
These hospitals represent the pinnacle of Medicare patient care and rehabilitation in California, each offering unique strengths and specialties that cater to the diverse needs of their patients. Whether through cutting-edge medical technology, research-driven practices, or compassionate care, they continue to set benchmarks in healthcare excellence. Take these hospitals into consideration as you offer your Medicare clients advice and support!

Emma Peters is a media intern at California Broker Magazine. She recently graduated from Point Loma Nazarene University summa cum laude, with a Bachelor of Arts in Literature and a minor in Humanities.