






















Welcome
News and Latest Updates
Research News
New Video Support Resources

Meet Some of CRY’s Medical Team
myheartmystory

Looking Back: The history of myheart
myheart Meetings
For more details regarding the events shown on the cover, please turn to the corresponding page references below. Images are listed in rows from the top left:
1. “My heart condition’s 25th anniversary”, by Kerry Shephard. P26.
2. Local mum speaks of shock the moment her son was told he had a potentially fatal heart condition. P5.
3. “My story of being diagnosed with LQT in the midst of a pandemic”, by Ruth Williams. P34.
4. “Volunteering at the CRY Heart of London Bridges Walk”, by Nicole McShane. P6.
5. CRY’s Expert Medical Team: Dr Michael Papadakis. P20.
6. CRY Ambassador Ben Coleman getting tested by CRY. P9.
7. “The Story of my Heart Disease”, by George Ashby. P22.
8. “A Reflection on My Experience Living with a Heart Condition”, by Daniel Redfearn. P32.
Head Office: Unit 1140B


The Axis Centre Cleeve Road
Leatherhead
KT22 7RD
No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means; electronic, mechanical, photocopying, recording or otherwise, without prior permission of Cardiac Risk in the Young (CRY). CRY welcomes all content for the newsletter but reserve the right to edit when necessary and to withhold publication. Any opinion or statement by the author of any article or letter published does not necessarily represent the opinion of Cardiac Risk in the Young (CRY). Articles pertaining to health-related topics are for information only. Readers should obtain advice from their own practitioner before attempting to diagnose or administer any medication. Mention of any products or procedure should not be considered an endorsement for said product or procedure.
I am delighted to present to you the newsletter for 2021 which is a round-up of myheart news and events from 2019 as well as 2020. Whilst 2020 was undoubtedly challenging for everyone, Cardiac Risk in the Young (CRY) and myheart continued to offer support to young people who have been diagnosed with a cardiac condition. We endeavoured to adapt to the ever-changing situation, by moving our support meetings to an online forum and providing information about COVID-19 to our members. We published information about COVID-19 on CRY’s website and our doctors provided regular updates. I feel humbled to say that myheart is now providing personalised support to nearly 600 members. Included in this newsletter is the history of myheart which some of you may find interesting. The group has grown from strength to strength since its inception and has become synonymous with personalised support, expert advice and up-to-date medical information. I would like to extend my thanks to all of you for your continued support, whether it was in terms of fundraising, sharing social media posts, sharing your stories on the website or writing to your MP.
This newsletter includes personal stories shared by some of our members in 2019 and 2020. We have received feedback about how impactful it is to read stories of others who have been diagnosed with a cardiac condition. We are very grateful when any of our members share their stories with us on the myheart website, as peer-to-peer support and shared experiences can help people to feel less alone in their suffering. We also welcome vlogs.
This bumper edition of the newsletter also contains stories, interviews and videos with some of CRY’s expert cardiologists. CRY’s Founder, Alison Cox, has penned the stories of CRY consultant cardiologists, Professor Sanjay Sharma and Dr Michael Papadakis and how they came to be involved with CRY. Dr Sabiha Gati, myheart cardiologist, has kindly provided an interview about her work with young people who have a heart condition, as well as articles answering questions about myocarditis and about her research paper, ‘exercise recommendations in patients with valvular disease’. Professor Sharma and Dr Papadakis also conducted webinars on CRY’s research programme which were very well received. The links to the recorded webinars have also been included in this newsletter. The link to Dr Papadakis’ presentation on ‘exercise in patients with HCM’ can also be found in the newsletter.
Throughout the past year, we were sent quite a few FAQs by individuals with cardiac conditions which were kindly answered by our experts. The links to FAQ pages have also been included in the newsletter for your reference (the identity of the person who asks the question is always kept anonymous). Professor Sharma also very kindly created an article for cardiac patients, answering questions specifically about COVID-19.
As the coordinator of CRY’s support group, it is my responsibility to put this newsletter together and it is my endeavour to get you all the news and event stories relating to members accurately. Please do not hesitate to contact me by emailing me at myheart@c-r-y.org.uk or by calling me at 01737 363222 if you find anything amiss or if you have any views to improve our support network. Thank you for your help!

CRY would like to thank all those that voted for us in the Tesco Bags of Help Centenary Grant initiative. CRY was bidding to bag a massive cash boost from the initiative. To celebrate Tesco’s Centenary, the supermarket teamed up with Groundwork to deliver a special voting round of its community funding scheme which will award grants of £25,000, £15,000 and £10,000 to community projects.
CRY was one of three groups that were shortlisted in 10 different regions across the UK to receive the cash award and we are proud to announce that we will be receiving £165,000 as part of the initiative. Here are the results:
• East Anglia – 1st Place: £25,000
• East Midlands – 1st Place: £25,000
• West Midlands – 1st Place: £25,000
• Greater Manchester –2nd Place: £15,000
• Mid and West Wales –2nd Place: £15,000
• North West – 2nd Place: £15,000
CRY will receive £165,000 to help fund screenings across the UK – all thanks to the support of Tesco shoppers who voted for us with their tokens.
“This will pay for around 3,300 young people from 10 different regions, to be offered free cardiac screening. Research shows that one in every 300 of the young people that CRY tests, will be identified with a potentially lifethreatening condition. Many CRY supporters and families affected by young sudden cardiac death have really got behind this campaign too, spending their spare time in various Tesco stores across the UK, talking to shoppers about the work and services that CRY funds to help prevent these tragedies. So, this initiative has been a wonderful opportunity to raise awareness as well as funds.”
Once again thank you to all of those that voted for us and a big thank you for all of our supporters that held awareness stands in their local Tesco stores.
• South London – 2nd Place: £15,000
• Cornwall – 3rd Place: £10,000
• Highland & Islands/North East Scotland – 3rd Place: £10,000
• South Yorkshire & Lincolnshire – 3rd Place: £10,000
We are sometimes contacted by myheart members who are looking for more information about insurance. Kathryn Knowles, Managing Director of Cura Financial Services, has created a short video to give some more information and guidance about looking for insurance as a young person with a cardiac condition which can be viewed here: www.myheart.org.uk/information-on-insurance-for-a-youngperson-with-a-cardiac-condition-by-kathryn-knowles/
Links for Kathryn’s bio: curainsurance.co.uk/who-we-are/ kathryn-knowles
The link to the ‘find a broker page’ on BIBA is: insurance. biba.org.uk/find-insurance
CRY is unable to recommend any particular insurance organisations or brokers.
Voting was open in all 900 Tesco stores across these areas for the three months between July and September and the £165,000 grant which will go towards cardiac screening for people aged 14-35 in these regional areas. The grants will not only be a fantastic contribution towards CRY’s screening programme, but the awareness of being on the boxes placed in all Tesco stores in these regions is invaluable.
Dr Steven Cox, Chief Executive of CRY comments; “This is fantastic, what an end to this amazing campaign. We were so honoured to have been invited to be a part of this incredible community-based initiative, the Tesco Bags of Help Centenary Grant, and overwhelmed by the news that
Dr Steven Cox responds to the latest (Dec 2019) recommendations from the UK National Screening Committee (NSC) relating to systematic population screening for cardiac conditions associated with young sudden cardiac death (YSCD)
“Just prior to Christmas Day 2019, the UK National Screening Committee published its conclusion to the consultation reconfirming the UK NSC does not recommend systematic population screening for cardiac conditions associated with Sudden Cardiac Death in the young.
“The first point to address is that, as a charity driven by a
mission to prevent young sudden cardiac death through proactive screening and research, we completely disagree with the repeated concerns raised about the accuracy of the ECG (electrocardiogram) test. As CRY has previously highlighted, the 12-lead ECG test is currently recognised by experts worldwide as the ‘gold standard’ test for identifying cardiac abnormalities and signposting a need for further investigations such as echocardiogram scanning, MRI and genetic testing.
“It is a routine, first line test when a doctor is concerned about a patient’s heart. The reality is this is usually only offered to older people. Again, we ask, why should young, apparently fit and healthy young people, who may be harbouring a hidden heart defect, not have access to the same, simple and inexpensive lifesaving test? And, whilst the report goes on to imply that testing in sport – and when symptoms are present is warranted – the NSC has not been explicit about this.
“It goes without saying that CRY believes ALL young people should have the opportunity to be screened, because the majority of young sudden cardiac deaths are not in elite athletes and in 80% of the tragedies there are no signs or symptoms. All too often, the first sign that anything is wrong will be the last sign.
“The conclusion of the NSC also contradicts what is already routine practice within the NHS, as we raised during the consultation. The perception patients have of their symptoms and how this is interpreted by a GP is rarely clear cut. Many people will fall into a grey area where symptoms (e.g. breathlessness, blackouts) are easily dismissed by GPs partly because they are so common, and GPs do not have the resources or training to enable every person with symptoms to be tested. The current position of the NSC to encourage all people experiencing symptoms to go to their GPs for investigation is therefore not viable in practice and it is unreasonable to expect GPs to be able to read ECGs to the same standard as a specialist cardiologist.
“Throughout the consultation, we were frustrated that the NSC was not willing to meet with CRY to discuss the concerns we had raised about the apparent understanding (or, misunderstanding) of the incidence of young sudden cardiac death. Thanks to 10 years of funding of the CRY Centre for Cardiac Pathology (at a cost of £1,000,000) the vast majority of SADS deaths are now investigated at the Centre, giving CRY a unique insight into how many families are affected by young sudden cardiac death. It appears the NSC is underestimating the incidence of young sudden cardiac death by at least 10-fold, and almost 100-fold for high risk groups.
“We believe this fundamental misunderstanding of the epidemiological data of how many people are affected is central to why they are still referring to this as ‘very rare’ and ‘tiny’ when compared to heart attacks in the elderly. Young sudden cardiac death is one of the most common causes of death in young people and the most common cause of death in young athletes. It is unacceptable to continue to frame the issue in this way.
“Whilst we were very disappointed the NSC was not willing to meet during the consultation to discuss the major concerns we had about the way they had misunderstood the incidence, we have been reassured that now the consultation is over they have agreed to meet with us and we will be able to address this issue. We trust they will advise how they would like to present the pathology research data held by CRY to ensure the policy in the UK is informed on a sound scientific basis.
“CRY will continue to engage MPs in our campaign to establish a national strategy to prevent young sudden cardiac deaths. This is important to ensure all policies in the UK are consistent and we hope the key recommendations from the recent review of adult screening programmes (October 2019) will be taken on board to enable this, establishing a single advisor body bringing together the UKNSC and NICE.
“However, the first key issue is for a national strategy to correctly establish the accurate incidence of young sudden cardiac death. As long as this is underestimated the government will underinvest in research, underestimate the impact young sudden cardiac deaths have on communities throughout the UK, and fail to recognise the cost-effective tools we already have that could prevent these tragedies.”
“2020 is CRY’s 25th anniversary year. 25 years ago, CRY was established to prevent young sudden cardiac deaths through screening and research. It is unacceptable for a progressive society to turn its back on 600 young deaths every year and the horrendous impact it has on every family, friend and local community. It is unacceptable to leave it up to the bereaved families to raise the funds to provide the research and resources that are so important to save young lives. CRY will not accept the suggestion that these tragedies are unavoidable. We will continue to screen more young people and invest more than ever before into research to prevent young deaths.
Through research, we will change policy. Through screening, we will save young lives.
It’s every parent’s worst nightmare, being told that your apparently fit, healthy teenager has a heart condition that could potentially kill him and that he may have to give up the sport he loves. That was the news that hit Kerry Preece from Shrewsbury like “being slapped in the face” when her 18-year-old old son, Aron (a talented swimmer who was already competing at national level), was diagnosed with a condition known as Wolff-Parkinson-White syndrome (or WPW) having attended a free heart screening organised by CRY. WPW is a problem with the electrical “connections” in the heart. It causes a very rapid heart rate which in some cases can lead to a dangerous and possibly fatal arrhythmia. However, sufferers will often not be aware of any obvious symptoms.
Following Aron’s successful treatment (and return to swimming!) Mrs Preece wants other young people to understand the importance of booking in for a simple screening test with CRY – and is urging other parents to go to our testmyheart.org.uk website.
Kerry says: “Like most parents who drag their children along to a heart test on a Saturday morning, with both protesting that ‘there’s nothing wrong’, I never imagined the Doctor would call me in to explain he’d found something abnormal on Aron’s ECG and that, until he’d been referred for treatment, he’d have to give up his passion in life –swimming. I admit, I burst into tears and felt completely in shock. But CRY couldn’t have been more supportive, directing us in our treatment journey. We even stayed in touch with the Doctor who identified Aron’s problem on that day back in June 2017.”
Aron was treated 11 days after his diagnosis by the Cardiologist, Dr Adrian Morley-Davies, at University Hospitals of North Midlands, who Kerry describes as “phenomenal”. We know that every week in the UK around 12 young people (under the age of 35) die suddenly from a previously undiagnosed heart condition. 80% of these deaths will occur with no prior symptoms, which highlights, as in Aron’s case, why screening is so vitally important.
Sport itself does not actually cause sudden cardiac death but it can significantly increase a young person’s risk if they have an underlying condition. And, although screening won’t identify all young people at risk, in Italy, where screening is mandatory for all young people engaged in organised sport, they have reduced the incidence of young sudden cardiac death by 89%.
Kerry had taken Aron and his younger sister Anya (aged 14 at the time) to a CRY screening day at Wrekin College funded by the Matthew Dewhirst Memorial Fund. Matthew
(whose parents, Chris and Sue, live in St Martins, Oswestry) tragically died in July 2012 from a previously undiagnosed heart condition. He was aged just 17. Matthew was an incredibly sporty and popular student at Ellesmere College with a passion for rugby and his sudden death, following a training session, sent shockwaves throughout the local community.
Since Matthew’s death, Sue and Chris (with huge support from family and friends) have campaigned tirelessly to raise awareness of young sudden cardiac death and CRY’s work, raising over £150,000 to date which has led to the screening of around 2,300 young people already. Sue has also become a regional Representative for CRY.

Kerry adds: “Everyone involved with Aron’s swimming club at Wrekin College was incredibly supportive – as was our entire swimming community – following his diagnosis and subsequent treatment using a procedure known as ablation. Sue Dewhirst came to meet me and other parents at one of our galas and she gave a very inspiring and emotional speech. I continued to organise fundraising events at Shropshire County Swimming galas, to support further CRY screenings in memory of Matthew. Aron and I were honoured to meet up with Sue again last summer so Aron could personally present a cheque for £1,500.”
We carried out a UK survey among 2,001 adults between 18th - 22nd October 2018 which helped highlight the demand for screening. Around two-thirds of people (62%) are aware that an ECG could detect the majority of conditions which can lead to young sudden cardiac death. And, of the 18-34 age group questioned, over two-thirds (67%) of men and 71% of women said they would like “the opportunity to book in for cardiac screening (with an ECG) before reaching the age of 35”.
CRY Chief Executive Dr Steven Cox says: “Aron’s story is becoming more and more common as we test increasing numbers of young people – with apparently no symptoms, no obvious family history or warning signs. It’s fantastic news that Aron was treated successfully and is now back to swimming at a competitive level and enjoying his first year at university, safe in the knowledge that his heart condition has been treated.
“CRY wants every young person to have the opportunity to
have their heart checked and last year we tested almost 30,000 young people. 1 in 300 people we test will have a potentially life-threatening condition identified and research we published last year showed that of those athletes identified with conditions 75% of them returned to competitive sport after being treated.
“We’d like to thank Kerry for speaking out publicly about their experience and helping to promote the message that a diagnosis of a heart condition during adolescence does not mean the end of your dreams or pursuing your passions. With treatment or even lifestyle changes, you can continue to lead a normal, active life and like Aron, become an advocate of screening and the importance of the ECG test.”
We are so grateful to our supporters who offer up their time. From being an official CRY ‘cheerer at a mass participation event, helping marshal the route at the CRY Heart of London Bridges Walk, holding an awareness stall, sharing our key messages on social media, to volunteering at a UK festival – there are lots of opportunities to get involved!
Events volunteering – Providing your help on-site at any of our events is a great way to get into the action of our fast-paced busy events! Our events include Simplyhealth Great North Run, Virgin Money London Marathon, Heart of London Bridges Walk and more!
Volunteering in your local community – Volunteering in your local community is extremely beneficial in raising awareness of the important work that CRY does.
Raising Awareness – Help promote CRY by distributing CRY general information leaflets/collection pots at your workplace, local school, leisure centre or in theatres, pubs, shops, doctors and pharmacies.
Social media – Follow myheart on Twitter and Facebook. By sharing any of our messages you are helping to raise awareness. Some members also help to raise awareness by sharing their own stories, including #myheartmystory
In-office volunteering – Our CRY in-office volunteers take on a range of practical and administrative tasks. We have limited space but are always grateful for an extra pair of hands in the office!
If you would be interested in volunteering some of your time for CRY, or would like to receive a volunteering information pack, please email volunteering@C-R-Y.org.uk
Many people encounter CRY for the first time as a result of
a sudden death of a young person. Whilst this will always be a tragic loss, the CRY Heart of London Bridges Walk gives hope. Volunteering at the idyllic setting of Tower Bridge was an uplifting experience as all walkers passed by with cheery faces, despite having endured the pain of losing a loved one. Walkers thanked us as volunteers, while we thanked them for participating in the walk.
Whilst sad circumstances likely brought us all to CRY, everyone recognised the importance of fundraising to enable CRY to continue their work in supporting bereaved families, screening young people, carrying out much needed research and ultimately increase awareness of the prevalence of sudden cardiac death. All in all, the day was a pleasant reminder that in the absence of our loved ones, uniting as one, we can work to reduce the #12AWeek figure of young sudden cardiac deaths.
For its 13th year, the CRY Heart of London Bridges Walk found a new home. The event started and finished at Southwark Park, as 1,574 walkers gathered together for the walk and the first CRY Family Picnic.


Walkers collected medals upon their return as they headed into Southwark Park to rest and connect with others. Shortly after most of our walkers had returned, CRY Founder Alison Cox spoke. “Hearing how others manage can provoke a new way forward,” Alison said when sharing how valuable taking part in the walk can be. “Perhaps on your way home you will reflect on your experiences today. We hope that you will feel uplifted with what you have seen and what you have heard. Please do feedback, please do let us know. We are dedicated to reducing your suffering – it matters to CRY.”
In 2019, eight myheart members registered to take part for the walk. Some of them got a chance to meet other members and share each other’s experience. While it was the first time for some members, some have taken part in the Bridges Walk annually for a few years.
Interview with Dr Sabiha Gati about her review paper, ‘Exercise recommendations in patients with valvular disease’
Sabiha started as a CRY Research Fellow in 2010 and is now our myheart cardiologist. She was the first CRY Fellow to complete a PhD, winning several awards and prizes for her research. After completing her PhD and specialist training, Sabiha embarked on a 12 month fellowship training in cardiac MRI at Royal Brompton Hospital and subsequently worked as a Consultant Cardiologist in the unit. Sabiha now works as a Consultant Cardiologist at the Royal Brompton Hospital, London and specialises in sports cardiology, inherited cardiac conditions and Cardiac MRI. She is the Deputy Editor for Education and Training for EHJCase Reports and also a Nucleus members for the EAPC sports cardiology. Sabiha has had publications in a number of leading medical journals and is actively involved in CRY’s screening programme.

Why is valvular heart disease important in the young population?
Valvular heart disease affects approximately 3% of young individuals. Many of whom aspire to partake in competitive sport or high intensity recreational exercises. Research supported by CRY screening program has shown that 1 in 100 individuals have a minor cardiac structural abnormality such as bicuspid valve disease, mitral valve prolapse which requires surveillance throughout life. Therefore, early identification may prevent future heart complications.
Why does valve disease progress with exercise?
Reports on the natural history of valvular heart disease in exercising individuals is limited. However, there is a theoretical possibility that a large blood volume pumped out by the heart during exercise associated vigorous heart contractions may accelerate valve problems and may subsequently cause changes in the heart structure, function, electricity and even lead to sudden death.
How is valvular heart disease managed in exercising individuals?
The management of exercising individuals with valvular heart disease requires a structured approach which incorporates:
1. Assessment of symptoms such as chest pain, breathlessness, dizziness and fluttering in the chest.
2. Assessment of functional capacity.
3. Type and nature of valve disease. Is it a left sided or right sided valve problem and is the valve narrowed or leaky.
4. The impact on the heart structure and function.
Which valve abnormalities are common in young individuals?
Mitral valve prolapse and bicuspid aortic valves are the most common valvular abnormalities in the young exercising individuals. The good news is that the risk of adverse events is low but both valve abnormalities can be associated with important complications that require monitoring with an ultrasound scan of the heart. Young people with minor valve abnormalities can compete in any sport. Those with moderate level of disease with require some further tests including an exercise treadmill test to assess how they do.
What advice would you give to exercising individuals with valve disease?
Exercising individuals with valve abnormalities should undergo yearly to 2 yearly assessment depending on the severity of valve disease they may have and we should inform them about the warning symptoms of progressive deterioration of valve disease.
For more information on CRY’s research please visit: www.c-r-y.org.uk/research
On May 11, we hosted the first CRY Family Research Day, giving some of our supporters a chance to learn more about the massive impact of our research.
CRY myheart cardiologist Dr Michael Papadakis spoke on CRY Research Fellow Dr Joyee Basu’s presentation, looking at exercise in patients with Hypertrophic Cardiomyopathy (HCM). He noted the importance of “the quality of life of those who get diagnosed with a condition” alongside the perspective of cardiologists in studying these conditions. Dr Papadakis talked about the importance of exercise in maintaining good health, but that it can also be a potential trigger for sudden death for individuals with HCM. “The problem that this creates…[is that] HCM patients don’t do any exercise, and about 60% of them fail to meet even the minimum physical activity recommendations.”
Dr Papadakis then discussed Dr Basu’s study in aiming to create a structured, individually tailored, supervised exercise programme for young individuals with HCM.
“We hope that this will inform the exercise prescription in patients with hypertrophic cardiomyopathy,” Dr Papadakis said.
CRY’s research programme has had a huge impact on our understanding of the causes and prevention of young sudden cardiac death as well as the way we treat those at risk.
In this webinar Professor Sharma spoke about how CRY’s research has impacted the way we look after families after a young sudden cardiac death as well as the way it has influenced the way we screen young people.

the following on CRY’s research by Professor Sanjay Sharma:
What has your research taught you about the way to conduct exercise tests?
How has St George’s University helped to take CRY’s research forward?
How has CRY’s research changed the way we understand LQT?
How has CRY’s research changed the way we understand Brugada?
How has CRY’s research changed the way we understand ARVC?
How has CRY’s research changed the way we understand coronary artery anomalies?
To watch all of these videos, please visit myheart.org.uk/ faqs-about-crys-research-by-professor-sanjay-sharma
CRY’s webinar held on the 17 December 2020 was with CRY’s Consultant Cardiologist Dr Michael Papadakis.
Dr Papadakis gave a presentation on how CRY’s research has impacted the investigation and management of people with conditions that can cause sudden cardiac death. After the presentation, there was a Q&A session.
In 2020, a number of new Q&A videos were added to myheart’s YouTube channel throughout the year, including
If you would like to submit a question to be asked next time we film members’ questions with our cardiologists, you can do this at myheart.org.uk/faqs. All questions are asked anonymously.
Some of our members have also shared their own personal vlogs where they discuss how they felt when they were diagnosed, or their experience of having different tests or procedures done.
If you would like to send a short video of your own experience, please could you send this to: myheart@c-r-y.org.uk.
If you’d like to learn more about CRY’s research, please visit: c-r-y.org.uk/research
Information page on CRY’s website to learn more about various conditions and how they are treated.
For more information on other forms of cardiac testing, you can go to c-r-y.org.uk/cardiac-tests
CRY is thrilled to have a growing group of Ambassadors. This position was introduced for people who have achieved recognition in their chosen field, who can raise awareness of CRY and share our key messages and information with their followers.
This includes Ben Coleman, a professional squash player who represents England. Ben turned professional in 2009 and his career started to take off in 2014, as he won his first four titles on the PSA (Professional Squash Association) World Tour. Now, he’s ranked 56th in the world.
Ben joined CRY as an Ambassador in 2018 and has been offering his support since. He came to CRY’s Parliamentary Reception in 2018, and attended a screening event in November 2019 where CRY’s new echocardiogram machine was unveiled.
Most recently, Ben went to St George’s Hospital to be filmed undergoing various cardiac tests with some of CRY’s cardiologists, to demonstrate what is involved. He had an electrocardiogram (ECG), echocardiogram (ECHO), and exercise test, which are all simple, valuable tests that can save young lives.


80% of young sudden cardiac deaths occur without prior symptoms, so the ECG (and further testing if required) is vital in identifying young people at risk.
You can watch these videos to get a better understanding of how these tests are completed, and go to the Medical

In February 2017, CRY launched a dedicated YouTube channel for the myheart network, where videos have been posted from our Consultant Cardiologists Professor Sanjay Sharma, Dr Michael Papadakis and Dr Sabiha Gati, as well as videos from members of the network where they talk about their own personal experiences.
There is also a FAQ page for ICD’s where you can ask questions on ICDs from Former ICD and Pacing Manager, St George’s, Sue Jones.
In 2019, a number of new Q&A videos were added to the channel throughout the year, including the following questions sent in by myheart members and answered by Dr Michael Papadakis:
Can LQT be cured with homeopathy?
What is physiologically happening to the heart when there are palpitations?
What is the difference between heart attack and cardiac arrest?
I have been referred to a cardiologist as I am experiencing symptoms. Should I stop exercising until my appointment?
Do the CRY cardiologists and research team see many people with Brugada syndrome and how many need not have an ICD implanted?
Dr Sabiha Gati, what do you find most interesting about attending myheart meetings for young individuals with cardiac conditions?

myheart sessions are a great forum for young people with (usually inherited) cardiac conditions. These sessions allow the nurses/ physiologists and the cardiologist to spend more time with young people discussing the impact of their condition on their everyday lives and psychological issues relating to coping with disease and its management, such as fears about a shock from an implantable cardiac defibrillator (ICD).
These individuals also worry about relationships and concerns about having affected children in the future. In general the clinic consultations in the NHS do not always allow for very lengthy conversation about psychological issues.
Furthermore, young patients do not always feel comfortable discussing them in such a forum. The myheart meetings allow clinical staff and affected young patients to become more acquainted with each other and permit a more relaxed and reassuring environment. It’s also good to hear from them what they would like more from us as clinicians in our clinics.
My group members get to know me as a person rather than the ‘doctor’ who simply manages their heart condition. I have a mantra, “the purpose of life is to make a difference to the life of others”. After myheart sessions, I feel invigorated and go home feeling I have made a genuine difference.
What new research are you working on? What new research should young individuals with cardiac conditions look forward to in the near future?
The CRY research team are currently working on several very interesting ideas including formulating exercise programmes for individuals with hypertrophic cardiomyopathy. A greater understanding of hypertrophic cardiomyopathy has translated to improved medical care and better survival of affected individuals.
Previously these individuals were considered high risk of sudden cardiac death during exercise and therefore, sedentary lifestyle was often promoted by clinicians. However, the work by Dr Joyee Basu (CRY Research Fellow) suggests that exercise in Hypertrophic Cardiomyopathy
of moderate intensity has a favourable effect on the cardiovascular system and is safe.
I also very much look forward to seeing the results Dr Gemma Parry-Williams projects on the veteran female athlete’s heart. It’s really good to see ‘women in cardiology’ having a significant impact at CRY.
In terms of new research, I’m looking forward to setting up a project at the Royal Brompton Hospital supported by CRY funding. The plan will be to evaluate young individuals with specific changes on their electrocardiogram and to identify whether they harbour subtle structural changes including myocardial scar using cardiovascular magnetic resonance.
Based on our analysis we will be able to create new recommendation on ECG interpretation in young people and athletes. This will have major impact on the cost effectiveness, sensitivity and specificity of our cardiac screening programme.
What advice will you like to give to young individuals with conditions with regards to exercise?
The benefits of regular exercise are irrefutable. All doctors should promote exercise. In young individuals affected by genetic diseases affecting the heart muscle of the electricity of the heart, the aim is to strike a balance between the multiple benefits of exercise such as reducing obesity, high blood pressure, diabetes and the small risk of sudden cardiac death. A moderate amount of exercise is generally safe. The current exercise recommendation for all individuals include at least 150 minutes of moderate intensity exercise per week.
Among individuals affected with heart diseases, I would advise exercising to a point there are no symptoms and generally not above 80% predicted for age (generally 80% of 220-age) or above 70% for those who are treated with beta-blockers. It is also important to tone the muscles and the recommendations are to push no more than 50% of the body weight with the arms and no more than 100% of the body weight with the legs. All individuals should warm up well and cool down.
It is not advisable to exercise in extreme climates without acclimatisation. I would discourage exercise at a temperature above 25oC. Individuals should avoid exercise if they have a fever or diarrhoea. Certain exercises and sports should be avoided with some diseases, for example people with long QT syndrome should not dive into cold water and people with Brugada syndrome should avoid long lasting sports such as marathon running or triathlon where the body temperature may exceed 40oC and promote dangerous cardiac rhythm disturbances.
What are your plans for the future?
doctors to change the natural course of the disease and save young lives.
One of the main differences with working with young people affected by these diseases is that I am dealing with individuals who often believe they are invincible due to lack of symptoms and the inner energy as a result of their youth, hence they do not always appreciate the dangers of the underlying disease. The main challenge is to allow as normal a life as possible and to promote aspirations and goals without increasing the risk of a potentially dangerous heart rhythms.
I am looking forward to starting my new Consultant Post at the Royal Brompton & Harefield NHS Foundation Trust. I will be involved with the inherited cardiac conditions service to support patients with genetic cardiac diseases and cardiac magnetic resonance imaging required for diagnosis at the Hospital. I also have the pleasure of establishing a sports cardiology service dedicated to individuals with cardiovascular conditions who want advice on exercise and sports participation, a project which I’m very excited about and cannot wait to get stuck in!
I am looking forward to supervising my first CRY funded Research Fellow who will be trained in inherited cardiac conditions, cardiovascular magnetic resonance and sports cardiology. The CRY Fellow will be supporting the CRY screening program and will be supervised in the PhD program.
How is it different working with a young population with cardiac conditions?

A typical day’s work involves assessing patients aged between 18 and 25 years old. The vast majority of individuals admitted or investigated in heart clinics are usually in their sixth decade onwards. Most of these individuals have agerelated problems such as high blood pressure, narrowing of the blood vessels supplying the heart, or a weak heart muscle. All of these are extremely important causes of feeling unwell or even dying.
Fortunately, deaths in young people (under the age of 35 years old) are much less common than in the older population, nevertheless, they are associated with a loss of several decades of life. Most deaths are from diseases that run in families and there are several treatments available to
Many young people enjoy participating in competitive sport which may increase the risk of sudden death. We are all aware that the exercise is one of the best therapies known to medicine and one of the challenges is to provide a safe exercise prescription which is sometimes considerably less than the young individual performed.
I often find myself talking to the young about the dangers of substance abuse including alcohol. There is a link between alcohol bingeing and sudden death from Brugada syndrome. Stimulants such as ecstasy or cocaine may provoke sudden death in individuals with long QT syndrome. Young people also frequently delve in activities associated with a surge in adrenaline that can also provoke serious rhythm disturbances in some people with long QT syndrome. In such cases, I find myself trying to provide the best advice about engaging in bungee jumping or going on rollercoaster rides.
I enjoy discussing issues with our young team and learn a lot from them about the apprehensions some of these people have that they may not feel comfortable discussing with their local cardiologists. The questions these individuals pose often leave me thinking about the best approach to managing a situation where the evidence is rather limited compared with cardiac diseases that I encounter in my day to day practice.
I finally confirmed that Sanjay was not your average person when he told me – during a discussion we were having on reminiscing – that he started writing his thoughts and experiences down when he was four. He was a serious, curious child and wanted to know about and remember everything. He already had decided to be a doctor – there seemed to be so many of his relatives getting ill and he was fascinated by the doctors all coming and going and able to make them better – he saw doctors as some sort of miracle people and determined he wanted to be able to do miracles too. From the age of four it never occurred to Sanjay to ever be anything else but a doctor.
His parents had met and married in the U.K. but decided, under pressure from his uncle, to return to Uganda which had just got its independence. Their standard of living rocketed and they enjoyed a beautiful house, servants and nannies. Most of all he thrived on the private education afforded them. He delighted in reading, learning, and discovering challenging new opportunities. At primary school the teacher recognised his ability and put him in the class above to better stimulate his appetite for learning.
The family returned to the U.K. just before General Idi Amin expelled all Asians out of Uganda. Sanjay was about to have his eighth birthday and remembered the stark contrast clearly. Their accommodation became a bedsit above a butcher’s shop in Walthamstow; he struggled to understand the cockney accents of the local junior school children, and they could not resist cruelly taunting him and his two sisters. He missed the security of an extended family close by. It was so rainy and cold. Adjusting was hard work and life took its time to slowly start improving. However – because of Idi Amin’s eviction of Ugandan Asians – his grandparents arrived and he and his siblings greatly benefited from their love and understanding as their parents worked hard to support them.
Both parents had been educated in the U.K. and his father soon settled into a job as an administrator in the NHS whilst his mother became a Citizen Advisor. They were delighted by now to have been able to move to North London where the teachers at Sanjay’s local secondary school were quickly alerted to his academic ability. His aunt and uncle had

both been head teachers at primary schools in Uganda, so education had always been impressed on them as a critical part of their lives, and working hard at junior school was a natural thing to do. By the time he went to secondary school there was an expectation that he would do well. And he did for a while until the third year when he started enjoying the distraction of an attractive social life. He lapsed into lazy indifference and persuaded himself ‘just getting by’ was ok. His wake-up call came just in time when his O Level results proved only marginally good enough to be permitted to sit his choice of A Levels.
He did not have to be reminded that ‘just sitting’ his exams was insufficient. Securing high grades were the only opportunity he would have to enter medical school. His headmaster was confident, however, and Sanjay consequently achieved the correct predictions from his tutors who then encouraged him to enter medical school.
Sanjay’s school did not have a reputation for high grades and his teachers kindly advised him not to be disappointed if he found he had not been able to secure a place in medical school because he would be confronting significant competition from the country’s top universities. As the A Level exams drew closer Sanjay became increasingly aware that the opportunity of doing what he had always dreamed of lay in his hands. That only he could now take it away. Sanjay’s mother had trained as a nurse at Leeds Hospital and spoke fondly of it in his childhood, so he was delighted when he learnt that he had been selected by Leeds medical school! On their first day the students were given a brutal introductory talk by the Dean, informing them that 20% of the intake would be expelled within 12 months for unsatisfactory progress. Sanjay immediately became concerned he might struggle, but in fact found that he loved every aspect of medicine ranging from the basic sciences to the clinical aspects of several sub-specialities. He was greatly relieved to finally learn that he had qualified with three distinctions, as well as obtaining the ambitious BSC degree in biochemistry in relation to medicine which he had included in his studies.
After working as a junior doctor at 3 major hospitals he decided to specialise in cardiology because cardiovascular disease was the biggest killer in the western world and he knew there had been several exciting advances in the management when he was a junior doctor. There were a number of outstanding opportunities produced for him at this crucial time that were unforgettable. His clinical mentor Dr Hackett contacted world expert Professor Bill McKenna when he found Sanjay wanted to specialise in hypertrophic cardiomyopathy, and he subsequently secured a place as a Research Fellow at St George’s Hospital. He had determined athletes would be his particular specialty and again fortune fell in his pathway (and mine!) when his ‘Prof’ introduced us. I had just started CRY with the ambition of creating a screening programme that would
learning of my prospective trip, and courteously requested whether he and his wife could join me as she was very keen to visit Jersey Zoo! And those two days contributed more to how I got to know Sanjay than any other later experience. We were both committed to our ‘day jobs’ but the unusual distraction of a highly publicised orangutan, who Sanjay was requested to examine and coolly accepted as a VIP patient, is what I believe gave me an extra dimension in understanding him and so contributed to developing the friendship that has bound us.
Sanjay’s unique talent is not only to be extraordinarily capable of doing three things at the same time, but most importantly stay loyal to his beginnings, not be seduced by glamour, and be sensitive to the difficulties of others less clever than himself!
initially be limited to young athletes but would expand to all young people between 14 and 35. We fought several (often bloody!) battles together thereafter promoting screening, which soon became an established part of British sport.
Another huge development was when the Medical Director of the London Marathon, Dan Tunstall Pedoe, asked him to be his deputy with a view to Sanjay taking over 3 years later in 2007. Things seemed to happen very quickly after that! Sanjay was promoted to Consultant Cardiologist at Lewisham Hospital, became CRY’s cardiologist for our screening programme, and developed CRY’s research team. This provided the opportunity to not only gain supervision skills, but also crucially achieve multiple high quality publications in major cardiac journals. Sanjay compounded his rapidly developing reputation when, age 44, he became the Professor for Inherited Cardiac Disease and Sports Cardiology at St George’s Hospital. His research, sometimes tackled at midnight when the house was quiet, quickly gained an international reputation and currently is responsible for 20 major publications annually. Perhaps his most revealing quality is exposed in how much he values having developed an established teaching course for the Membership of the Royal Colleges of Physicians of the United Kingdom, which became the largest in the world and during the period of 1994-2017 assisted over 7,000 young people to pass their exam.
As the weather edges away from sunshine and towards its drab, bleak preparations for the winter months ahead, I look back on my 25 years with CRY considering the person who has quietly had the most impact and for the longest time… It was 1996 and Sanjay had just arrived at St George’s. I was looking for an opportunity to get CRY into the news and secured a desperate, but fully funded (!) two day trip to Jersey to raise awareness of Gambor, an orangutan at Jersey Zoo that suffered from hypertrophic cardiomyopathy and was attracting national attention after fathering a precious off-spring due to a newly tried medication.
I did not know Sanjay but he suddenly contacted me after
Professor Sharma is the head of research for the cardiology clinical academic group at St George’s, University of London.
In addition to being the director of the largest sports cardiology unit in the UK and overseeing CRY’s screening programme, he’s served as the Medical Director for the London Marathon since 2007 and the Medical Director for Prudential RideLondon since 2015. In 2012, he was the lead cardiologist for the London Olympics.

He’s been involved in countless pieces of influential research and has over 250 PubMed citations. This includes highlights such as a special piece on cardiac screening in young athletes he wrote for the Journal of the American Medical Association in 2015; the ground-breaking international recommendations for the interpretation of ECGs published in the European Heart Journal and Journal of the American College of Cardiology in 2017, which helped transform the way we carry out screenings; and a paper in the New England Journal of Medicine in 2018, showing that the incidence of sudden cardiac death in footballers is higher than anticipated and ECG screening is essential in detecting underlying conditions.

Michael Papadakis cannot remember a time that he did not want to be a doctor.
His mother, devoted to her husband and children, was a dynamic business woman who proved a tough taskmistress and, from the start of his early days at his primary school in Chania, Crete, emphasised that she expected an 80% pass rate for his schoolwork.
His father, Dr Papadakis, who oversaw Chania Hospital where he was a physician, had sacrificed the opportunity of an academic career in Athens to ensure he could spend time with his family. This was a decision his children did not fully appreciate until they had matured and not only proved of great significance to them, but also hugely benefited the people of Chania, especially after he set up a dialysis clinic at the hospital. Dr Papadakis took a close interest in his children’s education and stressed the importance of always working hard – no matter what it was that you were working at.
Michael enjoyed his primary school and from an early age took his father’s advice seriously. Michael also soon learnt that the best way to make friends was to be in a team. He was especially proud when chosen to play for his school volleyball team, recognising the unique satisfaction of the group celebration if they won.
He found the move to Athens for his A-level education difficult. Life suddenly became more serious. The simplicity of his childhood in Chania seemed a long time ago. He was an ambitious student whose goal was to achieve the A grades in his exams that would secure his place for medical training at one of the big London hospitals. Dr Papadakis had been concerned about the unimpressive medical training that was currently available in Greece which was struggling on every level. He greatly respected what was accessible in the UK and had cautiously discussed with Michael the opportunity to study there.
A deep-thinking, highly motivated young man, Michael planned his career conscientiously and covered potential risks when possible. However, there was one thing that startled him that he had not considered.
He had not realised what a big jump it was to go from school-level English to using English in England, and the shock of suddenly finding that he had not reached the required standard to secure his place to study medicine at a top London hospital came as a jolt. English was a subject that all Greek students had an opportunity to study at school, but improving his English to what was required in England, and fast, was an uncomfortable challenge!
Michael spent his first two years in the UK at Charing Cross Hospital, and then moved on to Imperial to complete his training as a medical student, which he graduated from in 2001. He quickly realised that those who chose to specialise in cardiology were invariably amongst the very best students and that the standard required of them was exacting. Working within his comfort zone to do well was no longer an option.
Having tried and tested himself successfully in England he still found he was always questioning whether he should return home to Greece. A cautious young man, he was pleased to have achieved his long held ambition of the medical training he wanted and needed, but was acutely aware of how much he missed his family and homeland. Besides, he had the necessary commitment of his Greek Military Service to complete. So, at 25, he spent the following year as a Naval medical Officer – a period which gave him more time to think!
An interesting requirement if you were studying medicine that would also permit you to be able to work in Greece was that the student needed to complete a year as a GP in a rural environment. In 2004 Michael chose to do this in the barren setting of the Kampanos Mountains, which proved to be a very different experience from anything he had previously attempted. The “mountain clinic”, with its brutal winter weather, was mostly concerned with elderly citizens in an environment where nature did its worst with impunity. Consequently, their children left home at the earliest opportunity to seek jobs in the city. Parents (and grandparents) were left to manage on the mountain as best they could. As they aged, so did their equipment and facilities.
Michael’s patients proved enormously grateful for any help available, and the extraordinary experience – so different from his own upbringing – served to deeply influence his perspective on life. He learnt to value whatever facilities were available, and, where possible, adapted to fixing (or finding) what was missing. He learnt how to manage difficult situations alone without any support or colleague to consult in a crisis, and how to single-handedly prepare for and deal with emergencies.
As facilities for the clinic deteriorated he learnt where to look for second-hand replacements for the medical items he required, take advantage of all offers from doctor friends, as well as scouring other clinics that might have something he could use in the ‘mountain clinic’ that was no longer required elsewhere. Ultimately, the courage
and dignity with which his elderly patients attempted to manage their health problems inspired him to ask his family to finance four medical centres in the mountains, which included providing the luxury of basic heating and medical equipment, and found considerable satisfaction in knowing that he had been able to make a difference.
By the time he was 30 Michael had met the standard medical requirements for both Greece and England and was quite clear about the direction in which he wanted to go.
his training as a CRY Research Fellow at St George’s Hospital.
We have been lucky indeed that Michael chose to be interested in focusing on inherited cardiac conditions that affect fit and healthy young people. His impact has been significant. Since he joined CRY he has advanced education in the field of sports cardiology by building educational material for the European Society of Cardiology and launching a novel degree in sports cardiology – the first post graduate qualification of its kind.
Then in 2007 – after two years working in the UK as a junior doctor doing his clinical training, followed by training as a registrar helping to set up the Acute Medicine unit at Chelsea and Westminster Hospital – two major things happened.

First, through friends, he met Elena Marinaki, a radiologist. Her family background was a complicated one that had been affected by the struggle her mother had wrestled with after the illness and subsequent death of her father at a young age. In spite of her difficult personal circumstances Elena had managed to qualify as a doctor in Italy and then move to specialise as a radiologist in Greece.
For several years, because Michael was in the UK and she was in Greece, they were only able to see each other intermittently and according to the time allowed by their demanding personal schedules. Finally, Michael suggested they should commit to living together and have a six-month trial period which proved a successful decision, resulting in their marriage and becoming the proud parents of three beautiful, energetic children. They had an orderly life, working in their separate hospitals in England and spending holidays with their families in Chania.
Michael’s second “life changing” event was when he met CRY’s Consultant Cardiologist Professor Sanjay Sharma and, in October 2007, was delighted to be invited to start

Michael has transformed CRY’s myheart group since he has taken over, now holding meetings twice a year in a central London location. The myheart group has thrived under his watch, expanding exponentially with 530 young members who have greatly benefited from the 65 videos he has created exclusively for them which cover all the issues they are likely to deal with.
Michael is an enormous asset for CRY and his selfdiscipline, commitment and ability sets the bar high for the fortunate medical recruits that are accepted onto CRY’s training programme and subsequently become a part of the ambitious research into young sudden cardiac death that he and his team aspire to.
Michael is a Reader in Cardiology and Honorary Consultant Cardiologist. His clinical interests are inherited cardiac diseases, sports cardiology, cardiac MRI and echocardiography. His research is focused on inherited cardiac disease, prevention of young sudden cardiac death, sports cardiology, and cardiac imaging. He is accredited with more than 60 publications in peer-reviewed journals.
He is chair of the section of Sports Cardiology of the European Association of Preventative Cardiology (EAPC), Fellow of the European Society of Cardiology, and a Member of the Royal College of Physicians.
My journey with congenital heart disease began on 19th March 2018 when I was 18 years old.
I was at work and had just gone on my lunch break when I had a sudden cardiac arrest. The people around me called for an ambulance and one of the men was then guided through CPR and without any training performed it perfectly. After 6 minutes a first responder arrived and I was defibrillated once before being taken to hospital.
I spent 24 hours in a medically induced coma and initially I was extremely forgetful, which my parents were told was completely normal and wore off within few days. The next stage was working out what was wrong and I had what felt like hundreds of tests. All of the blood tests and regular stomach injections really helped me to get over my fear of needles!
After about a week, I was diagnosed with ALCAPA, which stands for Anomalous Left Coronary Artery arising from the Pulmonary Artery. This means that the left side of my heart was almost completely dependent on the right side to supply it with oxygenated blood. It affects 1 in 300,000 people and has a 90% fatality rate if it isn’t corrected within the first year of life. I am so thankful to have made it to 18 with minimal damage to my heart. There was also a concern that I had Long QT Syndrome, but it is now believed that the longer QT interval was caused by the resuscitation and the fact that my electrolyte levels were severely low, which to this day no one knows why. Due to the uncertainty, I had an ICD fitted as a precaution.
On the day of my open heart surgery I was terrified, but I knew that I was in the best hands possible. The surgery was predicted to take 4-6 hours and it ended up taking 8 because of some complications.
The recovery was a very long process and I had to take over three months off of work. I was in hospital for a week after the surgery and I had to have help to do really basic things, like getting out of bed. The general anaesthetic meant that I was incredibly queasy for a few days, to the point where I was on 3 anti-nausea medications and I couldn’t eat. It also gave me migraines and my consultant considered sending me for a brain scan, but they luckily didn’t need to.
The tough thing was going from being very physically active to struggling to walk for more than about five minutes at a time. I had to go for daily walks where day by day I would try to make it to the next lamppost down the street. I eventually joined a cardiac rehab class, which was harder mentally than physically as I was the youngest there by at least 40 years, but the nurses and personal trainer were lovely and did all they could to make me feel comfortable which made it easier.
Over the course of this past year I have had to get used to all the permanent changes to my body. I was firstly very aware of the physical feeling of my ICD and, later, the anxieties that come along with the fear of being shocked. Despite this, I am so glad that I have it as it has the potential to save my life. As well as the ICD, due to the surgery, lines and blood tests, I have also been left with more scars on my body than I can count. Most of the time I am really comfortable with them and they are a permanent reminder of how lucky I am and how I need to live life to the fullest. As I read – scars are just tattoos with better stories!

Now, a year on, I have been told that my heart has fully healed, I take very little medication and I am already down to yearly appointments, which is amazing. I have had a huge amount of support from my family, friends, colleagues and the wonderful staff at St Thomas’ which has made going through everything so much easier.
George Ashby has made an inspiring video about his experience after being diagnosed with a heart condition.

George’s mother, Amelia Ashby found that George has a heart murmur after a listen to his chest when testing out her new stethoscope, he then went on for further treatment and surgery as shown in his video.
The pair cycled 66 miles round the Isle of Wight to raise awareness and money for CRY.
You can watch George’s video by going to bit.ly/37UILK0

George Ashby had no idea that something could be wrong with his heart. His mum Amelia, a GP, had just got a new stethoscope when, later that same day, George suggested they used it to listen to each other’s hearts. Upon listening to George’s, Amelia realised that he had a serious heart murmur.
“She [Amelia] didn’t tell me at the time obviously, because I would have been terrified to be honest,” George explained during an interview he and Amelia completed on BBC Radio Solent on June 20th. “But it was pretty much by luck and it was quite amazing actually.”
“I heard the murmur and I must admit I was terrified,” Amelia said. “I knew it was going to be quite a significant problem, but like George said, I didn’t tell him at the time and he found out when we had the referral to outpatients. We told him very shortly before we took him in and it turned out he had something called coarctation, where his aorta comes out of his heart and it had actually narrowed to less than 4mm.”
George found the fear he felt hard to explain. “It was something I can’t really describe to be honest. Because normally most people have life-saving heart surgeries when they are older ages. It is quite a scary experience to be honest.”
Heart conditions don’t just affect older generations, though. 12 young people die each week due to undiagnosed heart conditions, and now George wants to raise awareness.
He created a video blog to share his story, and help others realise how common cardiac conditions are in young people and how important screening is for early detection. Because without making the innocent suggestion to his mum to try out a new stethoscope, George may not have had the surgery that saved his life.
Before finishing the interview, George explained why he
feels so motivated to support CRY. “Because I do feel it’s really important,” he said. “Because every week 12 young people die of some kind of undiagnosed heart condition. If the UK introduces screening to the NHS programme, then this has been proved to lead to an 89 percent reduction in deaths, so 9-10 people’s lives could be saved every single week.”
To continue in his support of CRY, George was preparing to complete a 66-mile bike ride in the Isle of Wight with his mum the day after their interview.
My animation consists of 1038 drawings all combined into a video lasting one minute and twenty-six seconds. In this short time I want to help calm the children that visit a cardiac Outpatients ward.
The animation is drawn in a friendly and childlike manner in order for children to immediately relate to the video so they can take in the information being communicated to them, about how they will be tested and potentially treated. The idea behind this animation was that a child would not normally pick up an intimidating leaflet, but there will always be a screen in a waiting room, or, in this day and age, some sort of tablet. This project is based on my own experience in hospitals, especially inspired by my brother, George, who was diagnosed with a heart condition two years ago.
I want the project to raise awareness of the importance of early diagnosis and the importance of getting screened and tested. My brother’s disease was found by chance, but not every child is that lucky. I don’t want cardiac diseases to be a mystery any longer. At least 12 young, healthy people die from undiagnosed heart conditions every week. Some have no symptoms. Don’t let your child be one of them.
Support charities like CRY to get your child screened. Imogen’s animation process and updates can be found on her Instagram: @i.ashby_artwork and her blog: ashbyisblog.wordpress.com
If only Hollie was screened at an early age! by Sarah and Richard Cannon (Hollie’s parents)
I would like to share our story to help raise awareness of fatal Genetic Heart Conditions.
In March 2016, our daughter – Hollie Cannon, then aged 15 years, collapsed suddenly at school having displayed no symptoms of an underlying issue.

She was fit, well and extremely sporty. She participated in most sports her favourites being netball and handball and enjoyed riding her horse most days in all weathers. Hollie was fortunate in the fact that she did manage to regain consciousness after she collapsed. Her initial ECG confirmed multiple ventricular ectopics and bigemeny. She spent several weeks in Glenfield Hospital, Leicestershire where numerous test were carried out including ECGs, ECHOs, 24 hr tapes, exercise tests, MRI scans to try and diagnose the symptoms she was displaying. She was also prescribed medication to try and get things under control and was referred to the Genetics team. Eventually all the testing confirmed a diagnosis of Andersen Tawil Syndrome which in Hollie’s case was causing fatal arrhythmias. This is a very rare Genetic Heart Condition.
When she was initially admitted to Glenfield Hospital the 24 hr tape was showing excessive multifocal ventricular ectopics including excessive episodes of broad complex tachycardia amongst other things. Total ectopic burden was 53.5%.
Without medical intervention another ‘attack’ would have been imminent proving fatal. Hollie is one of the lucky ones. A simple ECG helped to save her life. She will always have to take medication and will remain under the care of the cardiology team at Glenfield Hospital.
She now takes anti arrhythmic medication and has an Implantable Cardiac Device.
She did manage to pass all of her GCSE exams at a very difficult time and went on to study a level 3 extended diploma in Horse management at Nottingham Trent University. She received the ‘top’ student award. She has now moved on to a degree course at the same university studying equine behaviour, health and welfare. She also works 3 days a week at a horse rescue centre. She has remained positive throughout and has not let her condition
hold her back in any way. She has learnt to manage her symptoms. Even when she has felt unwell she has remained positive and determined.
If Hollie had been screened at a younger age her condition would have been diagnosed earlier. The trauma of collapsing, suffering incontinence and feeling very unwell in the school grounds could have been avoided. She could have died. Hollie found this very difficult to deal with at the time.
As a family it has taken until now to feel strong enough to share our story.
Hollie is a true inspiration and her outlook is always positive. She has recently been accepted into the Nottingham Trent University Equestrian team and also been awarded a scholarship. This proves that with determination, a positive outlook and appropriate medical care, goals can be achieved even when you have been diagnosed with a life threatening heart condition.

We hope by sharing her story it will inspire others and show the importance of screening in order to prevent young sudden cardiac deaths.
I was diagnosed with Long QT1 in 2010 when I was 27 years old. A close relative had been having “funny turns” at work with palpitations. Following one of these funny turns my relative went to see our GP, which my relative never does of their own accord. Anyway, following the consultation with the GP he referred my relative to cardiology. My relative actually came home and asked another family member what a cardiologist was which made us very worried.
Through my relative seeing a cardiologist and having a basic ECG it was found that they had a prolonged heart rate, which led to the diagnosis of Long QT. As this is a genetic condition I was asked to have an ECG from which I was also diagnosed with Long QT. Other relatives then had to be tested to see which side of the family it had come down.
As my relative and I were both still under the age of 35 we
were started on Beta Blockers. My relative was then sent for another test to find out what stage of Long QT we had (1-4). This test involved two anaesthetists putting their heart under so much pressure to the point where they were at a dangerous risk of having a heart attack. Following this we were diagnosed with Long QT1 and treatment is lifelong medication. Relatives over the age of 35 were not started on any medication as after this age your risk reduces.
Three days after I was diagnosed and started on medication, I was flying to Fuerteventura for my honeymoon. I was advised not to go into water alone or do any exercise in the water as sudden shock or adrenaline is what can cause our hearts into arrhythmia.
Three years after being diagnosed my husband and I decided we wanted to start a family. We had a discussion about the fact that there was a 50% chance I could pass the gene onto our child, but my husband completely understood and said we would just deal with that if it happened. Unfortunately that did happen and I understood the guilt that my family members feel through passing this on.
While I was pregnant we were given the option of having the blood tested from the umbilical cord or waiting until the baby was slightly older and them having an ECG. We both decided we wanted to know as soon as possible so had the blood tested from the umbilical cord following the delivery.
It was only four weeks later that I got a call from the Queen Elizabeth Hospital to say that my baby had the gene. I remember holding my baby while I was on the phone and being very calm until the call ended and I just broke down. When my baby was six months old they had their first consultation at the Birmingham Children’s Hospital and were started on lifelong medication.
My baby isn’t a baby anymore and is now seven years old. My child is amazing and takes their medication three times a day with no problems whatsoever. My child is fully aware that they have what they call “a poorly heart” and understands that there are some things they are unable to do, like sprinting, being supervised in the swimming pool, etc. The school has been amazing. They give the medication, understand all about the condition, and even alter physical activity so my child can still participate in sports day –they put my child in the
races that do not involve sprinting.
In 2018, I did a fundraiser at work and opened a crowd funding page and raised £1,700 to purchase a defibrillator and case for the school, which is up on the wall of the school and available for the community to use as well. This just gave us as parents a bit of reassurance while my child was at school.

Myself and two of my close relatives also participated in the CRY Heart of London Bridges Walk in June 2019, which was a very emotional experience as we were the only ones there who were not walking in memory of someone but we’re lucky enough to have been diagnosed and be able to continue to live a normal life. We also managed to raise over £300 between the three of us.

So, that is my story so far. I never really thought much about having a heart condition until I had my baby and they are the reason why I get more involved with raising awareness, raising the money for the defibrillator, and when my child is older I would like us to do the Heart of London Bridge Walk together.
I have always fainted for as long as I can remember, through assembly at school or if I stood up for long periods of time. My parents kept taking me to the GP who said I had low blood pressure which probably explained the fainting. When I was around 11, I started to develop quite severe chest pain on the left side of my chest. Again I was taken to the GP who suggested it was a strained muscle or panic attack.
The chest pain kept getting worse and so my parents in despair paid for me to see a private paediatric doctor as they were becoming increasingly worried as to what was causing my symptoms. The questions started like they normally did. “How is school?”, “are you worried about anything?”. Even at the age of 11 I remember feeling like I was not being listened to. My parents asked if it could be my heart and were told no, if I had a congenital heart condition this would have been picked up when I was a baby and my
symptoms were most likely anxiety and did not warrant an ECG. Life carried on with fainting, pain, and tiredness.
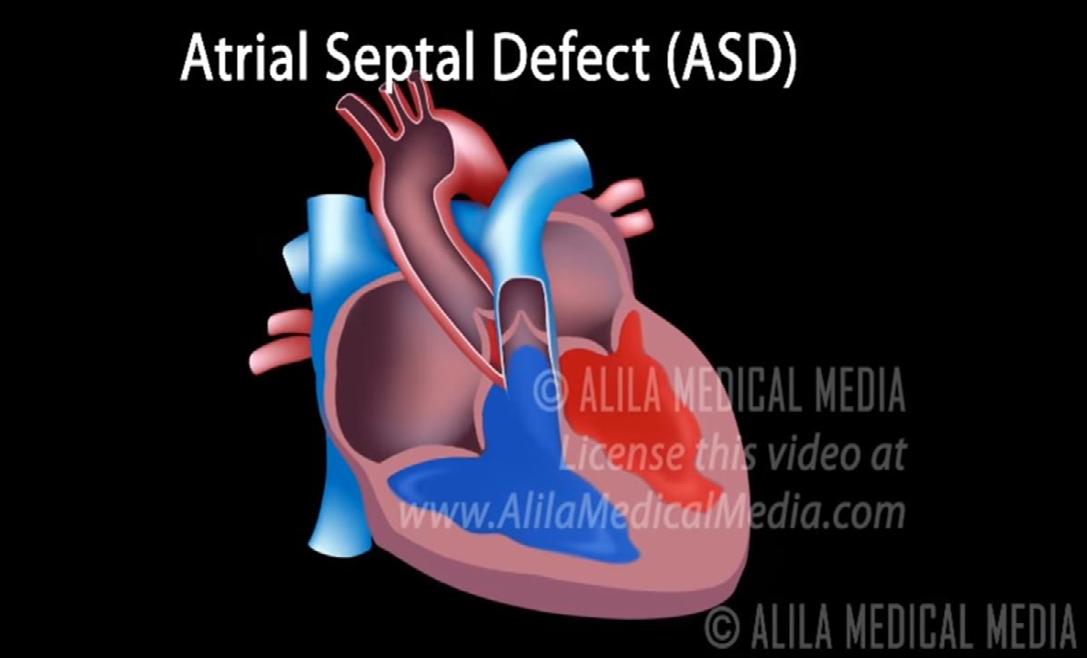
In the summer of 2006, aged 13, I suffered an allergic reaction to ibuprofen and had to undergo an endoscopy under general anaesthetic. During the pre-op the anaesthetist asked my parents what the cause of my heart murmur was, to which they replied they were not aware of any heart murmur. I was booked in for an ECG which came back abnormal and referred to the Royal Brompton Hospital to have an echocardiogram with a cardiologist. My echo showed that I had two holes in my heart the size of two 2p coins known as atrial ventricular septal defect and a leaky mitral and tricuspid valves.
In November 2006, just before my 14th birthday, I underwent open heart surgery to fix my heart. Had I not had that allergic reaction, had I not had that anaesthetist who picked up on my heart murmur, had I not had a consultant who decided to just “check” my heart, my condition would not have been picked up and I would have been another young adult who died of sudden cardiac death. My parents quite understandably were very upset given that they had spent years being told there was nothing wrong with me, however my heart condition is just bad luck, both my brothers have been checked and both have perfect hearts.


My fixed heart let me get on and enjoy a normal life. I went to university, qualified as a solicitor and enjoyed working as a commercial and agricultural solicitor. However unfortunately a few years ago my symptoms of chest pain, palpitations and chronic tiredness begun to reappear. At my annual review we discovered I had super ventricular tachycardia and atrial flutter which are both common in people who have congenital heart disease.
I underwent an ablation which unfortunately
failed – having patches on my heart from my AVSD repair makes an ablation very difficult. My mitral valve is still leaking and may need to be replaced at some point in the future.
I was unable to continue in my job which was very stressful and long hours and putting unnecessary strain on my heart, so I am now following my love of animals and re-training to be a veterinary physiotherapist. My heart condition is something I have to learn to live with, and I am starting to navigate the somewhat confusing and scary world of being an adult with congenital heart disease, things like will I be able to have children, will my body tolerate having a baby, how to deal with side effects of medication and having a full time job etc.
I am incredibly lucky and grateful for that anaesthetist who alongside my cardiologist, my surgeon and the whole team at the Royal Brompton saved my life. I’m getting married next year and looking forward to a long and happy life. I am extremely passionate and supportive of the work that C-R-Y do, I know I was one of the lucky ones, had my heart not been checked I may not have been sat here writing this and been one of the 12 young people who die every week of an undiagnosed heart condition.

My
25th anniversary – by Kerry
ShephardFebruary 2020 marks 25 years since my heart went crazy and hit 268 beats per minute while I was brushing my hair and getting ready for college. 25 years since the doctors battled to save me in resus by stopping my heart twice and rebooting it. 25 years since I was told I was unique and had Wolff Parkinson White Syndrome. 25 years since my parents, sister and other members of my family and friends thought they would lose me forever.
It should be just another anniversary but 25 is a powerful number for me because I was told I was unlikely to live past 25. So I crammed everything I could into those years I thought I had left to make it count – I danced in national comps (I’d been told I was lucky I wasn’t on a dance floor that day my heart lost its rhythm). I travelled for 4 months and knocked off some of the must see & do items on my ‘bucket list’. I made sure I spent time with my loved ones. I found the courage to dream and hope.
Over the years I’ve undergone surgery twice to my heart, I’ve made some incredible lifelong fellow heart buddies and
helped establish the first surgery support group for young people with heart conditions through the amazing charity CRY – which also marks its 25th anniversary later this year.

Personally I’ve achieved so much. From reconnecting with and marrying my soulmate to my two beautiful miracles who I was told I’d never have. It’s not been without its scary moments and knock on illnesses but I’m still here 25 years on. I still have moments my PTSD rears its ugly head, but I’ve learnt how to manage it. To deal with the scary stuff and, in some part, lock it away.

It’s odd to think I’m not classed as a young person with a heart condition anymore, as the cut off is 35. I didn’t know that symptoms I’d suffered during my upper school years was in preparation for the big day 25 years ago today. I was bullied for being different or unable to keep up, both at school and in the workplace, and yet still I find comfort in knowing that there was a reason why I was that way.
I have never seen myself as unique even though I was the first diagnosis in Buckinghamshire at the time. I was an oddity and there was so much interest in me from medical professionals who poked, tested and pushed me to my limits. Yet I trusted them and have so much to thank them for. Being a human guinea pig, I hope, has helped many others after me to get the right treatment.
I’m so thankful that on that day, 3 February 1995, that things fell into place like they did. Nurse Judy, the only medical professional at my doctor’s surgery as all the doctors were on training, who had the foresight when I stumbled with my stepdad through the surgery doors to call ahead to A&E. Dr Samuels, an A&E medic who later in the day called me unique, didn’t waste any time, jumped into action and made the key decisions to stop my heart and restart it to try to reset my internal ‘computer’.
The nurse, whose name I never found out, who held my hand and cradled me, told me to focus on her voice and be prepared for an elephant sitting on my chest, while the doctors working on me shot medicine directly into my heart. None of them knew that day if it was going to work and admitted they had never had to treat a 16 year old with a heart rate as fast as mine. But what they did was nothing short of a miracle.
But one doctor in particular, Dr Kardos, is the one who took over my long term care, promised me he would look after me, believed in me and gave me reason to think I could beat the odds – my own real life guardian angel. Without him, I would never have my children. Without him I simply would not be here. To him, I owe my life.
I am finding today really difficult. Its significance has crept up on me. I naively thought I’d feel the same as every other anniversary but this one has hit me a little harder. To think

I’ll surpass this milestone too is so overwhelming and incredible. I want to celebrate and mark today somehow.
So however you know me, whether it be from before or after my heart episode, give your loved ones an extra hug today. For me. I want today to be a day we hug that bit harder, we hug that bit longer and hug that bit tighter. Cherish each other. Thank you for reading and simply being there.
Last year, on the 28th of August, it was a normal day for me and I was skating down the road like I do every day as I skateboard everywhere. Around 5 pm, when I was skating down the road, my heart just stopped with no warning at all! I remember waking up in hospital thinking, “why am I here, did I fall of my skateboard really badly?”
Later on I got told that my heart stopped for 11 minutes and I was in a coma like state for days fighting for my life. If I died for 15 minutes it would have been fatal and I got told that I will have to be on tablets for the rest of my life.
When I got stable,
they moved me to a normal ward and then discussed with me about having a pacemaker fitted. It was an option but I got an S-ICD fitted and they told me that I can basically live a normal life. I am monitored weekly but it’s a small thing to know that I have a back-up that hopefully I never need.
I skateboard almost every day, just got back from snowboarding in another country and am thankful to everyone that supported me and helped me with everything. They told me I do not need to restrict myself.
Blogs by Joseph TannerOn Monday 16th March, I celebrated my 12th re-birthday. Rebirthday is a term that all cardiac arrest survivors use to celebrate surviving a cardiac arrest.
I didn’t really celebrate it this year, maybe ‘cause of this underlying cloud that was shadowing the world.
This cloud, COVID-19/Coronavirus, we first heard about whilst we were on holiday in Gran Canaria for my birthday. That was the end of January and that already feels like a lifetime ago. Back then we didn’t know what this would become, on the flight back from Gran Canaria there was a couple with face masks. I thought to myself back then they were a little bit overboard, yet now it is common practice.
For a while I think we all joked about it. Memes were shared on social media, I don’t think anyone believed the impact it would have on our lives.
Going back to my Brugada Syndrome, I was diagnosed 12 years ago and the medical world is still learning from people like me and fellow Brugada family. Brugada syndrome is a rare but serious condition that affects the way electrical signals pass through the heart. It can cause the heart to beat dangerously fast.
Symptoms can occur at any time but are sometimes triggered by something such as a high temperature (fever), drinking lots of alcohol, or dehydration. Symptoms typically first appear at around 30-40 years of age, but they can occur at any age. They’re more common in men than women or children.
So on Thursday 19th March when cycling to work my phone
started to ring at 2.20 pm, I had my phone in my hand whilst cycling because I didn’t want to miss a phone call from Daniel. I didn’t recognise the number, I was still cycling whilst I answered the call, the nurse informed that I should self-isolate now for 12 weeks. That I should call emergency services if I even develop a cough, and that she would send me a self-isolation letter to give to my employer.
After I hung up, I continued my cycle to work, in somewhat shock, I could not comprehend what this meant for me for the next 12 weeks. When I arrived at work, Todd was arriving and I joked that I would be going home in a minute, trying to joke about things is my natural defence.
Thoughts were swimming through my head, I knew that this meant statutory sick pay of £94 per week, which did not come close to paying my half of the rent, let alone bills or food to eat. Still, I continued to joke with fellow staff about the situation, Daniel called my workplace, he had been told by his company that he will have his hours reduced by 40%. I had to fob him off. I couldn’t burden him with my news, and I needed to speak to my manager, so I promised him I’d call him back in 20 minutes.
So I chatted with Simon briefly, really not taking in much was said, I knew that all I’d be getting is this measly £94 per week.

Below is the main extract from my doctor letter:
This letter is to confirm that this person who is a patient registered at this practice must self-isolate from coronavirus due to medical risk factors as instructed by the Government and clinical advice from Jane Pavey, Nurse Practitioner, for the next 3 months (advice may alter depending on circumstances).
I printed off the email from the doctor’s surgery and handed it to Simon, then went back down to the office to leave my keys on the table. I joked a little more with my staff, and then got my bike and walked out with Liam. I kept thinking to myself that I might not return. I said my farewell to Liam, and I walked a little further with these thoughts below in my head before I called Daniel at his work.
Earlier in the week I contacted the letting agents to let them know that I may have to self-isolate, they emailed me back to say that the landlord is self-employed and the only income he receives is from the rent of the property, so there will be no reductions.
The previous week Daniel and I signed a new year tenancy, so I was facing the prospect of trying to pay rent and keep my job in these uncertain times. The government did put in place a 3-month ban on evictions, but the tenant and landlord would have to work out a repayment scheme.
With Daniel’s hours being reduced and living in a time of not knowing, what would I be able to repay, when we hardly live now?
When I got through to Daniel I fell back into my natural defence of trying to make light of things, I joked I had good news, I couldn’t follow it through though. I then told him that I am going home because I have to self-isolate for 12 weeks, when Daniel broke down on the phone I crumbled inside. I tried to reassure him that everything will be alright; in all honesty, I didn’t think it would be for a very long time.
When the call was finished, I just kept on walking. I usually love cycling home but this day I was going to savour the outside because I did not know if I’d be able to see much of it for the next few months. I called Francis (Daniel’s Dad). I knew he was home. Francis has one of those reassuring voices and deep down I knew I had to talk with him.
On Sunday 22nd March, Francis was due to have surgery to remove cancer in his bowel. Myself and Daniel were meant to be travelling to Northampton at the weekend, now having to self-isolate I knew that would not be possible for me.
Deep down I still wanted Daniel to go, so he could be with his family. My next job was to convince Daniel to still go. When I finally made it home, I sat in the flat in silence and waited for Daniel to come home from work. Before Daniel came home I received a phone call from Ed, he had heard that I had to self-isolate. Ed knows me well. We lived together for 7 years, he knows I can never spend a day in the house.
Every day I go out, I’m not an inside person, I’m a social person, and this is my life for 12 weeks, and he knew how much that would be eating me up inside like cancer of my own. What scares me the most is if something bad (I mean death) happens to anyone that I love or know and I can’t leave to be with family or friends and be the support network that I am, it would destroy me!
Yes, I’m self-isolating, but this time we needed to hold each other, so when he came through the door we hugged, we cried and we both knew this would be the last time for a long time. We decided one more night of cuddling in bed, we put in place our plan for isolation going forward.
It was decided that Dan would sleep upstairs going forward on the sofa bed. Because he is allowed to leave the house it made sense for him to be by the main exit of the flat. Thursday night whilst in bed, I couldn’t sleep, but I stayed in bed because I didn’t want to leave Daniel, this was my last time for 12 weeks that we could cuddle. I can’t remember the many times I cried whilst in bed, maybe it was the reality that we’re really in a tough position.
Since Thursday, we have kept a social distance of 2m, we’ve
cleaned, we’ve wiped the down sides, we did face masks, we’ve slept apart, we’re hurting but we’re together. I was unable to convince Daniel to go back home and leave me, he was scared that if the country were to go into proper lockdown he wouldn’t be able to get back to me.
One way I guess he is right, and then I would have to depend on friends to get food for me. Talking friends, I have talked to so many people online, on the phone over the last few days, had people offer us money if we come short, we’ve had friends drop stuff over for us. The kindness and love from everyone have been so overwhelming I believe that we will get through this.
On Friday, the government promised to pay 80% of our salary, companies have to apply for this but if this goes through it gives me a little security for the time being. I don’t think my job is safe, this virus has impacted the fitness industry and people will continue to cancel their memberships.
When gyms are allowed to re-open, will people return?? If social distancing does become a thing, then we may have to limit numbers in classes and the gym. Sunday evening French Connection closed their doors so Daniel is home all day with me when they reopen it may be on this reduced contracted hours.
Last night whilst Dan was cooking the extractor fan in the kitchen short-circuited and took all lights out in the flat, it took us some time to find the fuse box to get lights back on in the flat. Unfortunately, the extractor fan is not working, so have contacted the letting agents, which means we will have to allow entry into our flat to an outsider!
The last few days I have completed a couple of online training courses, I’ve cleaned the flat, I have worked out, watched Wrestlemania 35, now starting on Wrestlemania 1… I feel that I have plenty of free time over the next few months.
Dan’s dad did have the surgery and all we know at this point is that it was successful, we will learn more in the coming days. Knowing how close Dan is to his family these last few days must have been torture for him and if I ever doubted his love for me I’d be a fool! We have talked about wedding plans over the last few days, and we wanted a ceremony at Hotel Du Vin, but because we face financial uncertainty we have decided maybe a town hall wedding.
The date we have decided on is Friday 18th June 2021. This day we will have been together for 5 years and this day feels right for us. All we know is that we love each other and it doesn’t matter where we are when we’re married, we just want to be married.
To end this blog, I want to end on a happy note and want to
remind you things will get tough, this is a strange time for everyone, be good to people, stay in contact, stay healthy, stay home!
Being in lockdown, being in isolation, it’s made me reexperience a life I had before and compare the feelings I have now, to that I had back then.
We all live life a little blindly, we all learn from an early age about death, but for many years we’re shielded from it by our parents, then when we do understand it, we don’t talk about it. We accept that death will happen to ourselves one day, but that day won’t come for a long time so why pursue it?
Our first experience of death for some can be the death of a family pet. Some parents may purposely buy a pet with a short life span, for example, a hamster, a rabbit. For the child to grow a bond with the animal full well knowing in a couple of years that pet will get sick and die, then you can introduce your child to death slowly.
You can explain that it happens to all beings, we all die and this pain and sense of loss your feeling will dissipate in time but your memories never die. (That too can be a lie!) We can’t control death, even when we put plans in places it sometimes can bite you in the ass before you can say boo to a goose or bury your cat at the Pet Cemetery.
So I go back to Sunday 16th March 2008, a day where my life would change me forever, in time those changes would dissipate and life would go back to where it was. On this day I would have a cardiac arrest whilst running the Hastings Half Marathon, I did not know that I had a rare heart condition.
I had warning signs, looking back on a blog I posted a day before the Hasting Half Marathon suggested so.
Below is an insert from that blog:
“My training for New York started well but the last couple of weeks I’ve faltered due to a bad cold. Last Sunday I wasn’t still quite right and around the 10-mile mark, I could feel my chest getting tight and found it hard to breathe. So I opted to run with the women and ended up doing 15 and a half miles. The rest of the group did 17 miles.
“This Sunday I’m doing a Hastings half marathon which is only 13.1 miles, so yeah, should be a walk in the park. It’s hard to know what time I’ll do it in cause I’m used to running a longer distance, I have a certain pace but won’t need to leave that extra in the tank…. So erm, yeah, wish me luck!”
We had warning signs with COVID-19. I first heard about this virus when leaving the UK to go on my holiday to Gran Canaria this year. The following month the news was escalating daily, we saw what was happening to Italy and yet so many of us were asleep to what was happening. Maybe we didn’t think it would happen to us in the UK. I didn’t think I would be locked away in my flat from the world.
Knowing I was not well before the Hastings Half Marathon I was asleep to this deadly condition that I have. On that Sunday I caught a lift to Hastings with another runner I met through Brighton Jog Shop run group that was also running that day.
I’d never been to Hastings before, the day was warm but grim with fine rain. I remember chatting to other runners, having to pee on the beach. I sent a group message to people, one that I remember writing and sending, I won’t lie, I wanted attention, I wanted people to know that I was running when I finished the run I wanted to see who responded. The message was the following “Hey everyone, I’m running Hastings half marathon today. It starts at 10.30 I’m feeling nervous. Not good, something not right so wish me luck.”
1 hour and 49 minutes later I collapsed at the finish line, which if you ever run the Hastings Half Marathon is also the finish line. I don’t remember running that day, I don’t remember the crowds, I don’t remember the St John Ambulance doing compressions on my chest, being taken away from the crowds to a tent to be given defibrillation treatment. I don’t remember the blue and twos of the ambulance driving me away to my isolation, I don’t remember yanking out the endotracheal tube, through all this mentally I was asleep.
On Wednesday 19th March, I woke from my induced coma, next to me was Sweep (stuffed toy) and a whole world of confusion. I knew I was in the hospital, with all these wires and beeping monitors that I was attached to, I felt like a puppet on a string. Being attached to machines, this is where my independence was stripped, having to push the nurse call button if I needed anything.
It was easy to get upset, I’d get upset if I needed the toilet and the commode was rolled over to me, especially because nurse Ratchet was happy to unplug me from all these monitors and let me use the toilet on the ward, so why couldn’t nurse Wilkes? Though I guess I should be thankful that I was alive, why do I need to leave my bed, she wasn’t keeping me here against my will.
Needing a pee, a pulp disposable urine bottle was brought over, curtains drawn. Sometimes they would wait for you to finish your business, other times they would leave you and not return which felt like an entirety with your business stewing in your private enclosure. Privacy is a luxury, being
on a ward curtain closed meant a few things, toilet, sponge bath, or the nurse doing their rounds. It was like clockwork, every 4 hours the nurse would come round and take your vitals, sometimes they would take your blood for good measure.
Being on a ward I had to be considerate of others. At 10pm lights went out, being a night owl sleep never came easy. Forget self-relieving, my little friend popped up a couple of times, yet there was nowhere for him to go.
During this time that I felt like I was in isolation, being in Hastings I was too far for many people to visit. My sister would come when she could, my parents went back home after I came out of the coma, so for 3 weeks, I felt truly alone. Yes, I had other bedfellows, being on a cardiac ward these people were all from a different generation. 12 years on these bedfellows have all surely now moved on!
Back then wi-fi in hospitals wasn’t a thing, Debbie did purchase me a dongle so I could go online. I had a bucket load of DVDs brought to me from home that I watched on my laptop.
During this time I had to keep myself busy, as I am doing now. I posted blogs online telling people what had happened to me. I called people, I made an effort to talk to people. I reached out, wanting to be heard. You learn very quickly during this time the people that matter, or at least you thought that mattered.
Currently, my life is my flat. It’s not a holiday for me, boredom sets in. I don’t have an outside space. So being in isolation is nothing new to me, you find your way of coping, staying in contact with friends, doing Skype calls, Zoom parties, watching Netflix until you can watch no more.
Some people may treat this as an extended holiday, using this time to fully recharge their batteries, being able to go for walks and complete those jobs they’ve been putting off for years. Others will find this a struggle, being told not to do something we want to rebel like a 5-year-old child in a supermarket.
The doctors and cardiologist were unable to do any investigations until I recovered from a chest infection, once I recovered it was the Easter Holidays so everything was put on hold. I knew from day one that I would have an ICD (Implantable Cardioverter Defibrillator) implanted in my chest.
I’m an outside person, I never stay home, every day I go out even if it is the betting shop. I hated missing out on things, I had tickets to the X-Factor tour that I had to give up. I missed out on watching Wrestlemania with my friend Nick.
Respite would come, to get to the bottom of why I had
a cardiac arrest. I had a day trip to the Royal Brompton Hospital in London via a private ambulance. On the motorway, nurse Ratchet promised that we would stop by a hot dog stand, so I could have a hotdog.
Uncertainty – there was a lot I didn’t know. I didn’t know how long I’d be in the hospital. I didn’t know if I would be able to work again. I didn’t know how I would pay my rent and bills. Instead of focusing on recovering, I spent a lot of time worrying about not knowing. I can relate to that now.
When the lockdown measures are eased will I be able to return to work? I think that I won’t be able to return to work, currently, the furlough scheme is running until the end of June, I have to hope that gets extended if the shielded are unable to return. Back in 2008, my work promised to pay me until I was able to return to work, kind of like the furlough scheme, still I didn’t know how long this kindness stretched.
Once I got my diagnosis of Brugada Syndrome things started moving rapidly, within days I was transferred to Brighton Sussex County Hospital, and this is where I would have my ICD implanted.
After three weeks of not seeing anyone, I made sure I had many visitors and at one point it became so overwhelming that I threw up. What is happening now in the world, we are all experiencing, some of us are on a different level, but we all can relate.
When I was finally released from the hospital I was told to rest. I was unable to rest. Being able to go out and see people, I felt alive again, walking along the seafront, hearing birds, no longer the beeps of monitors.
I had to learn to adapt to the new me. At first it was unclear if I was able to exercise. I was told not to get drunk, no to drugs, no to sauna’s. The list a mile long.
When the lockdown is eased we’ll have to adapt to a new way of living, social distancing, wearing a face mask, queuing outside supermarkets to get our provisions. There will be people that won’t take this seriously, or it is not in their mental capability to consider others.
This is a virus, anyone can get it, and many people will have minor symptoms but I dislike people that think they are above it. Yes, I have a condition, yes I am high risk, and so being locked in my flat from others is my life for now. This virus has taken healthy people, it’s taken people without underlying conditions, it’s taken young people.
Listen to the advice that is been given by the scientists, the government, your loved ones. At the end of the day you are responsible for yourself, and the people in your household.
My story so far: Left Ventricular

Hello. My name is Phoebe and I’m 22 years old. When I was three years old, I was admitted to Great Ormond Street Hospital to have open heart surgery to repair an Atrial Septal Defect (ASD), otherwise known as a hole in my heart. Since then I was very healthy and finished school and college without many difficulties. For this reason, I never considered myself to be somebody with a heart condition and didn’t particularly ever think much about my previous surgery, apart from for the scar down my chest which today, is barely noticeable.

When I turned 19, I had my final appointment to be signed off the list for cardiac patient care. However, it didn’t end up that way. I had an MRI scan, just to confirm that everything was alright, and was told that this would be a quick, 20-minute procedure.
Instead, I was laying in the MRI scanner for 2 hours and was diagnosed with Left Ventricular Non-Compaction Cardiomyopathy and a dilated aorta. This was a great shock for myself and my family and I had to suspend my university studies for two years due to the fact that my blood pressure kept dropping so low that I was collapsing all the time and I was getting tired very easily.
Flash forward to today and I now have an internal loop recorder fitted and I’m on medication to keep my blood pressure stable. I am also just about to go into my final year at university which has been a long time coming! I’m looking forward to hopefully meeting other people who also have heart conditions and have perhaps had similar experiences to myself!

I had no idea at the end of the summer holidays in 2011 that the following months would be a defining period of my life. I was thirteen years old and soon to start another year of secondary school. At this time, my favourite activity was undoubtedly exercise – I followed many different sports and enjoyed playing them too. At an age where I felt bigger
and stronger every day, learning to challenge myself physically was a great source of satisfaction and reward.
During the first Physical Education lesson of the new academic year, while running a lap around the school field, I remember physically exerting myself harder than ever before. Approaching the end of the run, a deep and heavy pain emerged in my chest. Within seconds it felt as though my legs turned into stone – I collapsed onto the grass and everything went black. Lying in rapidly intensifying discomfort, the feeling of my heartbeat began to encompass the entirety of my thought – it was as though I was willing on every contraction to the point that I was unable to think about anything else.
The following two months consisted of regular journeys in and out of hospitals to meet with cardiologists and undergo further investigations. While at school in January 2012, I received a phone call from my mother telling me that we needed to urgently go to hospital in a nearby city so that I could undergo open heart surgery. This was because the diagnosis of HCM was not entirely accurate, in fact, the issue was that the origin of my left coronary artery was anomalous. This meant that the blood vessel supplying oxygen to the left part of my heart arose from the wrong place, following an erroneous route around my heart.
It is understandable to assume that this information would seem daunting to a 13-year-old, but I think there was an element of naivety that protected me. It was difficult to grasp that every time I played sports I was putting myself in danger.
Aside from gaining the knowledge that my heart’s anatomy was abnormal, nothing else about me had actually changed
– I would look in the mirror and still see exactly the same person in the reflection. I didn’t see someone who was at risk of dying, or somebody who even looked sick for that matter. Compounding this with my lack of understanding that ill health is often out of our control, I still simply didn’t believe that I was any different to anyone else.
I underwent a successful re-implantation of my left coronary artery in late January. Despite the company of my brother and my parents, the first week of recovery felt like one long, never-ending day – daytime and night-time merged into one.
In my own room within the cardiac children’s ward, I would spend the daytime waiting for the nurses and doctors to perform checks, give medication, or to carry out small follow-up procedures. However, as night time approached, I feared having to lie in pain for hours. This was perhaps the most difficult period of the entire process.
My self-perception had changed significantly; I suddenly felt very different from other people my age, and even different from who I was before the operation. Every day I was learning to adapt to and become more comfortable with pain, and how small decisions could manage it.
Some of these small protective actions I still maintain today – for example, I never sleep on my side and I don’t really like anyone pushing against my chest. Adaptations of this nature initially required deliberate thought but I do them subconsciously now.
During my time in hospital, I almost always looked forward to the doctors, nurses, and other allied health professionals spending time with me. I loved learning about the various tests and procedures they performed on me as it helped me to better understand my own condition.
On a couple of occasions, the consultant sat down with me and answered various questions I had about my condition, wider cardiology, and medicine in general. These conversations helped to clarify the process of recovery that I was going through, and it was fascinating to understand how the human heart can go wrong in so many ways.
After returning home, I began the process of returning to school, and within a few months I was attending secondary school full time again, being discharged as a patient completely after
around three years of follow-up.
The time I spent as a patient undoubtedly forms a large part of who I am today. I appreciate being able to run, I appreciate being able to play sports, and I appreciate the feeling of physical freedom. I recognise that good health cannot be taken for granted at any stage in life and I am grateful for every day I can live without fear about my future, or fear of pain itself.
For many of us, the psychological impact of a heart condition can last forever. I will never exercise in the same way again – so much of sport is about reaching your limits and then pushing them, but ever since collapsing aged 13, I can’t do this in the same way. I am now constantly aware of my heartbeat. I fear pushing myself too hard and I’m always mentally making an action plan in the event that something goes wrong. Even before embarking on a long run I always make sure to tell a couple of people my route beforehand… just in case.


In 2016, I began studying Medicine at King’s College London with the aspiration to one day become a cardiologist myself – I continue to hold this dream today. I recognise that I am fortunate to be on this path and one day hope to be able to work for young people with heart conditions.
I was told about Cardiac Risk in the Young (CRY) last year while completing an intercalated degree in Cardiovascular Sciences at Imperial College London. As someone who nearly
lost their life while playing sport, I greatly appreciate the work that CRY does, and was encouraged to share my story on this platform.
I’m primarily writing this post for other young people living with a heart condition. In the days following my operation, meeting other children recovering from heart surgery was a true source of solace. It was comforting to know that there were others who understood what I was going through. Despite the many challenges that a heart condition can present to us, we can find strength in the knowledge that we are not alone.
It is often impossible to predict what challenges life will present – a part of these challenges involves acceptance of the circumstances you find yourself in, as well as learning how to forge a positive outcome from something so seemingly difficult. Life is a fine balance between good and bad, but the hardest periods often shape us the most; adversity gives us the benefit of perspective, as well as the chance to reflect on and appreciate what we do have.
To those reading this who are afflicted by a heart condition and worry for their health, I hope better days lie ahead, and that you are able to find strength to persevere.
Thank you for reading my story.
In April of this year, I was diagnosed with Long QT Syndrome (LQTS). In the midst of a pandemic, this was the most unwelcome conclusion to my ongoing investigations!
In 2001, my sister Ellie died very suddenly whilst on a telephone call with me one morning. I found her body later that day with the phone still in her hand. In utter shock from her sudden passing, we were left even more distraught as the inquest could not find a cause of death. I developed a love for running as a way of coping with the grief, and in 2011 I received a ballot place for the London Marathon. Sadly, I did not accept this place as they cautioned against taking part if there was a history of sudden death in the family.

I underwent low level screening locally, however I still had many unanswered questions, and so my search for reassurance led me to CRY and Professor Sharma’s clinic at St George’s Hospital in 2012. I was met by Dr Abbas Zaidi who was a research fellow at St George’s, and I underwent extensive investigations including an ajmaline challenge searching for signs of an inherited cardiac disease.
The results were all clear and I was advised that I could safely participate in endurance sports. Dr Zaidi also explained that Ellie’s cause of death was in fact Sudden
Arrhythmic Death Syndrome, SADS. This was personally quite emotive and pivotal in accepting her loss.
Shortly afterwards, I was running my first marathon with one of my closest friends Fiona. My family, including three children, were all at the finish line cheering loudly as I completed the course in disbelief! Many marathons and ultra-marathons later, I was about to embark on a winter endurance event. I asked another dear friend of mine Nia, who is a GP on the island of Anglesey where I live, if she could take an ECG for me before I committed to competing.
Nia found that I had a slightly prolonged QT interval and suggested that I contact Dr Zaidi again for some advice. 7 years after first meeting him as a research fellow, I went to his clinic at Cardiff University Hospital where he is now a Consultant Cardiologist. Repeated ECG recordings found that I did now have a prolonged QT interval.
My diagnosis was complicated by the fact that in some female athletes the heart undergoes normal physiological changes demonstrated on an ECG recording and these features are in fact very similar to that of certain inherited cardiac diseases. These ECG changes revert in athletes after a period of detraining, so I significantly reduced my participation is sports over a 12 month period, and it then became clear that I still had an abnormal ECG. Genetic testing was performed and a group of specialists including world experts in LQTS, finally concluded that I do indeed have Long QT Syndrome.
I consider myself extremely fortunate to have a mild form of the disease. My family and friends have offered tremendous support over the years, as has Dr Zaidi who has been diligent with his care throughout. I have immense gratitude to CRY and everyone involved with its operation. From the research they do, the specialist training they offer doctors, to the screening that they perform, these are all vitally important components in the prevention future young sudden cardiac deaths.
–
Myocarditis is an inflammatory process involving the heart muscle. It can present acutely (suddenly), sub-acutely (of recent onset) or as a chronic disease (weeks or months later). It may present with focal involvement (at a specific location) or diffuse involvement (over a widespread area) of the heart muscle. When individuals have symptoms, these can be highly variable from generalised tiredness, malaise (a general feeling of discomfort), chest pain, breathlessness, electrical abnormalities of the heart and even a cardiac arrest. Viral infections are the most common cause of myocarditis in the developed world.
How common is viral myocarditis?
The incidence i.e. the number of new cases of myocarditis is approximately 1.5 million worldwide per year and estimated at 10 to 20 cases per 100,000 persons. The exact incidence or prevalence of viral myocarditis is unknown as many cases are subclinical (not severe enough to present definite or readily observable symptoms) and follow a benign course (not serious). According to some estimates, 1-5% of patients with a sudden onset viral infection may involve the heart muscle. So, a small number. The majority of patients are young and healthy. Individuals who are predisposed include children, pregnant women and those who are immunocompromised (when your immune system’s defences are low).
Does exercise make it more likely you will develop viral myocarditis?
Myocarditis accounts for 5-10% of sudden cardiac deaths (SCD) in athletes and up to 20% of SCD in military recruits, suggesting that exercise may be a trigger for sudden death in this condition. Clinical data linking intensive physical activity to expressions of myocarditis have not been assessed in humans, but clinical observations do suggest it, given that we do identify a higher prevalence in athletes particularly as they are more likely exposed to germs than the general population. There may be an increased risk of infection with contact sports or team sports with a higher potential for droplet infections. We know from animal studies, specifically in the Coxsackie virus B3, that there is a reduction in our immune defences induced by intensive exercise that predisposes us to upper lung airway viral infection and possible involvement of the heart muscle.
How many days after a viral illness should you wait before exercising again?
Exercising individuals should be careful when they experience symptoms of coughing, sore throat, running nose or diarrhoea. Viral infection not only affects the heart muscle, but can also cause muscle soreness, joint pains and generalised body fatigue/aches. If an athlete has
these symptoms that may or may not be accompanied by a raised temperature, they should refrain from any strenuous exercise as this may further impair the immune system defences and increase the potential for general viral spread and involvement of the heart muscle. Also, with exercise you increase the chances of the virus transitioning from the respiratory/lung-airway system to the circulatory (blood vessels) and may also impair and disrupt the gastrointestinal tract (digestive tract). Therefore, athletes with a viral infection should refrain completely from exercise during the acute phase (sudden onset) of the infection. Symptoms to watch for include systemic tiredness (extreme fatigue which doesn’t go away with rest) and increase in body temperature. Once these general symptoms of a cold have completely resolved, one should wait between 3-5 days without symptoms before moderate intensity exercise can be commenced. In severe cases this may be 7-10 days.
In acute (sudden onset) severe myocarditis that results in hospital admission, a reduction in the heart function is seen in around 25% and exercise is strongly not recommended during this acute phase. The European Society of Cardiology (ESC) guidelines in sports cardiology recommend that athletes with myocarditis can start regular training, including resistance exercise after complete resolution, after a 3-6 month period. The rest period depends on the severity and development of the disease and may depend on the heart function, electrical abnormalities and the presence of fluid around the heart. 50% of athletes may demonstrate mild forms of myocarditis which does not require hospital admission and resolves within 4-6 weeks. However, strenuous endurance exercise is not recommended for at least 3 months. Exercise training should be gradually increased with rest days in between.
Are there any long-term effects of myocarditis?
Myocarditis begins with the direct invasion (spread) of the infection and its replication either within or near the heart muscle. This results in destruction of the cardiac tissue. Later, the human immune defence system is activated, resulting in an inflammatory response to the infection.
Acute stage of the disease – direct viral cytotoxicity (quality of being toxic to cells) and focal or diffuse necrosis (death of body tissue/cells) or destruction of the heart muscle.
Subacute – Human immune activation mediated injury creating autoantibodies (an antibody produced by the immune system that is directed against the body’s proteins) that react to the heart muscle with inflammatory proteins.
Chronic phase – Diffuse heart muscle scarring and reduction of heart function which may lead to a dilated
cardiomyopathy (heart muscle condition with reduced contraction). Therefore, the long-term effects include heart failure, dangerous electrical abnormalities and an abnormal baseline electrical trace.
At what point should I seek medical attention if I am developing symptoms similar to myocarditis? What are the symptoms of myocarditis?
Patients typically present within 7-14 days of a flu-like illness that includes fever, generalised body and muscle ache, vomiting, diarrhoea, chest pain worse on breathing in, breathlessness, and palpitations (fluttering in the chest). Your vital signs may be abnormal, including a high temperature, increasing heart rate, and breathing rate and sometimes dizziness from a low blood pressure. If an individual has any of the symptoms described above, they should seek advice from a medical professional.
If you had myocarditis once, are you more susceptible to have it again?
Yes, myocarditis can recur and there is no known way to prevent recurrence of myocarditis. However, the risk of recurrence is low (probably about 10-15%). However, I recommend to my patients that they get an intermittent echocardiogram, especially if they think they are having recurrent symptoms. Your cardiologist will suggest frequency of follow up.
If a family member has had myocarditis, does that make me/my genetics more predisposed to developing myocarditis? Should first degree family members be referred for screening after a young SCD where the cause has been recorded as myocarditis?
Myocarditis is not inherited (i.e, it is not running in the family); it is an acquired condition. There are no known genes associated with human myocarditis. When multiple family members are affected, the cause is usually due to common infection or environmental exposure, but the chances of this occurring are very low. There are no known genes associated with human myocarditis. However, arrhythmogenic cardiomyopathy (familial heart muscle condition associated with electrical abnormalties, fatty deposits and inflammation) causes a form of myocarditis in the course of the disease process. Therefore, following the post-mortem assessment if there are no other associated features of arrhythmogenic cardiomyopathy (which also includes fatty replacement of heart tissue) and the pathology is purely associated with inflammation process of myocarditis, then first-degree relatives do not need to be referred for further screening evaluation. However, if there is any doubt or family members are anxious, you can always undergo a cardiac screening via charities like CRY.
Myocarditis during pregnancy is rare. Its clinical presentation varies from being completely free of symptoms, having mild generalised symptoms, to serious heart failure and life-threatening electrical abnormalities. Diagnosis is based on a combination of clinical features, the electrical trace, blood tests and imaging that would include echocardiography and cardiac MRI.
Athletes may be taking medications, such as tricyclic antidepressants, or drugs such as cocaine which can cause a toxic myocarditis. The precise mechanism remains unclear but does result in an inflammation of the heart muscle. Toxic myocarditis, even if recognised early in its course, may not be reversible. However, withdrawal of the offending drug and continued follow-up is essential for effective management.
I have seen that myocarditis is most commonly caused by Enteroviruses. If I have developed myocarditis from one of the Enteroviruses, how long will I be contagious for after getting the virus and after starting symptoms? Is COVID-19 in the family of Enteroviruses and can it cause myocarditis?
The contagious period for an enterovirus infection starts 3 days after infection and remains for about 10 days after symptoms develop. Infectious individuals can shed the virus without having symptoms. Enteroviruses are members of the picornavirus family and include Coxsackie A, Coxsackie B virus and Echovirus. SARS – coronavirus – 2 disease (COVID-19) is an infectious disease caused by a newly discovered family of viruses known as coronaviruses. Other coronaviruses are capable of causing illnesses ranging from the common cold to more severe diseases such as Middle East respiratory syndrome (MERS). COVID-19 can cause myocarditis and the prevalence is around 7%.
How can systemic lupus erythematosus and other autoimmune diseases cause myocarditis? I have an autoimmune disease, should I be worried? What can I look out for?
The disease most strongly associated with the development of myocarditis is systemic lupus erythematosus, but it might also occur in association with Sjogren’s syndrome, vasculitis and Polymyositis. These conditions can cause inflammation of the body as well as the heart muscle through mounting an autoimmune response. Additionally, because these autoimmune conditions create an added risk for developing infection especially if you are taking immunosuppressive drugs places you at increased risk for developing infectious myocarditis. If you have an autoimmune condition, you should seek advice from your rheumatologist, especially if you are taking medications that may potentially suppress your immune system.
Since CRY was first launched in 1995, there’s always been a huge focus on supporting families and individuals through the aftermath of a young sudden cardiac death – as well as funding research and screening to help prevent these devastating tragedies. That focus has never wavered in CRY’s 25-year history and has been at the forefront of our work and vision – but, it’s still important to emphasise (particularly as we look back over our past) that’s not all we do…
From very early on in our journey and development as a charity, it became clear that there was an unmet need to support those young people who had been diagnosed with – and treated for – a serious cardiac condition, providing them with information, education and most importantly opportunities to meet up with others in a similar situation, as they learnt to navigate to their ‘new normal’ and readjust to daily life and activities.
As with many of CRY’s early milestones and developments, the initiative was very much pioneered by CRY’s founder, Alison Cox MBE, who has always remained a passionate supporter, advocate and champion of this inspiring group of young people.
“Our first meeting was very relaxed and we asked questions on issues that we wouldn’t normally ask our cardiologists. It was so good to talk to others who have been through similar experiences as myself. We – the founder members of CRY’s SS Club – all agreed that there needs to be more done to raise awareness about ‘sudden death syndromes’ and more support for young people and families affected by them.
“I wish I could have talked to someone before I had my implantation. You have so many things you want to ask but you don’t want to ask your parents as they are as uptight about it as you, and you don’t want to ask the doctors as they may think that you are being silly. This club should help solve these problems, because it’s young people talking to other young people.”
From there, CRY’s (and possibly, the UK’s) first ever support group for young people, following the diagnosis of a hidden heart condition was born and the mission statement devised then, was much the same then as it is now;
“… to provide personalised help, support, and information to individuals who have been diagnosed with a potentially life-threatening inherited or congenital cardiac condition… a support system for individuals to help develop effective coping strategies and reduce social isolation.”
Over the years as awareness of CRY grew, so did interest and membership of the Surgery Supporters Club. Meetings were held twice a year, originally at the CRY office, then branching out to meeting rooms at a hotel in neighbouring Reigate, followed by venues in Central London.
We also began to notice a clear link to the growth of CRY’s nationwide screening programme – in simple terms, as more young people were screened, more young people were identified, diagnosed and treated and therefore, more young people were coming forward seeking support and advice from their peers.
Launched in October 2002, the group we now know as myheart was initially called The Surgery Supporters Club, reaching out to young people who had been diagnosed with an inherited or congenital heart condition and had undergone treatment (whether surgery or long-term medication). And, what became clear from the very outset was that everyone who came along found the personalised help, support and individual information invaluable (and simply not available anywhere else).


There were just 6 young people at that first meeting, held at CRY’s previous head office in Tadworth, Surrey. Speaking at the time, one 16-year-old boy (who had been diagnosed with Brugada syndrome and fitted with an ICD following a near fatal cardiac arrest, 12 months before) said:
From day one, all those associated with CRY’s SS Club were thirsty for knowledge and keen to share their experiences. A regular programme of informal Q&A sessions was
arranged, led by Professor Sanjay Sharma, with expert input from other cardiologists. There have also been special sessions held during meetings on issues such as ICDs, with opportunities to send in questions, answered by former ICD and Pacing manager at St George’s NHS Hospital Trust, Sue Jones.
In 2013, CRY’s Surgery Supporters Club rebranded as myheart. At a high-profile Parliamentary Reception, a new resource was unveiled, featuring 10 personal ‘essays’ from young men and women, recounting their own story of suddenly being diagnosed with a heart condition. The booklet also included an inspiring introduction from double Olympic gold medallist, Tom James, who himself had been diagnosed with a heart condition known as Atrial Fibrillation in the run up to the London 2012 Games.

unexpected diagnosis of a potentially fatal heart condition.
One year on, a new-look website was launched. It was not only engaging and ‘youthful’ but also quickly became an invaluable information portal, packed full of bespoke medical information, expert advice, newsletters, a members’ area, FAQs and further video content (including many recorded by Professor Sharma about a range of conditions and recent research – a topic which is always of great interest to those diagnosed with a cardiac condition). Now, the ‘hub’ also provides a space for testimonials and blog content about personal experiences and the journey from diagnosis to resuming daily life.
In 2017, the group’s social media presence was further amplified with the launch of its own YouTube channel which continues to be populated with important and current content. This was soon followed by a Facebook forum for members’, too.
Alison Cox told guests and MPs: “It can be mind-blowing for a young person when first diagnosed. And, many of those who come to us for advice often do so after the sudden and unexpected death of a parent, sibling or other relative which has possibly been the only indication that any form of genetic abnormality existed in their family.

“Feelings are running high – fear, anger, insecurity. They desperately need the reassurance that their lives are not over – in fact, in some cases, following successful treatment, they are only just beginning. But often, the only person who can do that convincingly is someone else who is going through the same experience as themselves.”
In 2015, the group officially came under the supervision of Dr Michael Papadakis, one of the key doctors in Professor Sharma’s team based at St George’s, University of London.
Thanks to his dedication and commitment, combined with the obvious ease and rapport he has with the young people within the group, it really grew from strength to strength – with Michael also having overseen the development of more than 65 videos created exclusively to cover many of the issued faced by young people, following the sudden and
Our myheart members have continued to be regular guests at CRY’s annual Parliamentary Reception in Westminster, not only enjoying another opportunity to come together and to meet up with CRY’s team, but also serving as a really positive reminder that a diagnosis of a cardiac condition does not mean a future of ill health, inactivity and missed opportunities.
Far from it!
So many of the young people associated with myheart have reached amazing goals, and it’s always wonderful when we hear updates about their achievements, whether academic, professional, sporting and personal, to name just a few aspects!
Over the years, myheart members have spoken in Parliament, met celebs such as David Walliams, Pixie Lott and gold medallists, carried the Olympic torch, and even been asked to ‘toss the coin’ at the start of the Wimbledon men’s final!
Many have also become involved with national and regional media opportunities, always willing to speak to journalists about their own personal stories, the importance of cardiac
screening and ‘life after diagnosis’.
One myheart member has recently played a pivotal role in helping to facilitate a major research project funded by CRY looking at “safety and outcomes of a structured exercise programme in young patients with hypertrophic cardiomyopathy”.
And another – one of the CRY SS Club’s founding members (now aged 40 and with three young children) has developed the hugely successful fitness platform, “Million Metre Challenge” which, next month, will be rolled out even further as part of a new virtual fundraising collaboration with CRY.
Watch this space for further details…!
Recently, myheart has come under the supervision of Dr
National myheart meeting
March 23th, 2019
A myheart members’ meeting was held on Saturday 23rd March 2019 at Friends House, Euston. The meeting was introduced by cardiac nurse, Polly Castello followed by a session with ICD specialist, Sue Jones.
After lunch, there was a Q&A session with cardiologist, Dr Sabiha Gati. In this session, the eight registered members asked questions they had about their condition, the exercise(s) they can do and any other concerns they had.
National myheart meeting
November 16th, 2019
A myheart members’ meeting was held on Saturday 16th November, 2019 at Friends House, Euston. The meeting was introduced by cardiac nurses, Katie Frampton and Polly Castello followed by a session with ICD specialist, Sue Jones.
After lunch, there was a Q&A session with cardiologist, Dr Sabiha Gati. In this session, the 10 registered members had to the opportunity to ask questions or raise any concerns that they had about their condition.
Online myheart meeting
April 14th, 2020
A myheart members’ Zoom meeting was held on Saturday 4th April, 2020. There was a Q and A session with cardiologist, Dr Sabiha Gati in response to queries and concerns that members had relating to their heart condition and the pandemic.
Sabiha Gati (formerly a CRY-funded Research Fellow and now Consultant at the Royal Brompton & Harefield NHS Foundation Trust).
As part of an interview for the CRY website, Dr Gati explained; “The myheart meetings allow clinical staff and affected young patients to become more acquainted with each other and permit a more relaxed and reassuring environment. It’s also good to hear from them what they would like more from us as clinicians in our clinics.
“My group members get to know me as a person rather than the ‘doctor’ who simply manages their heart condition. I have a mantra, ‘the purpose of life is to make a difference to the life of others.’ After myheart sessions, I feel invigorated and go home feeling I have made a genuine difference.”
October 17th, 2020
A myheart members’ video meeting was held on Saturday 17th October, 2020. There was a Q and A session with cardiologist, Dr Sabiha Gati, giving members the chance to meet with other young people who have been diagnosed with a cardiac condition, as well as an informal space to ask questions of a consultant cardiologist.
Currently myheart holds meetings twice a year in a central location for young people, between 18 and 35, who have suddenly been diagnosed with a life threatening heart condition. Anybody with a cardiac condition between the ages of 18 and 35 can come to the meetings if they:
• Have been offered or already have an ICD
• Have suffered a cardiac arrest
• Have been diagnosed with an inherited or potentially inherited cardiac disease
Given the complexity of some conditions we recognise that there will always be a need to consider some cases on an individual basis.
Meetings are free to attend and give members an opportunity to meet and discuss their experiences in an informal but supportive environment. Those young people that attend these meetings usually find them very helpful.
It does not matter how long ago you were diagnosed or whether you are undergoing any sort of treatment at the moment.
For more information about myheart meetings, including upcoming dates, please visit myheart.org.uk/meetings
Save the date: 20th - 28th November
CRY’s annual Raising Awareness Week has always been an essential part of our year. It’s a time for us to place even more emphasis on raising awareness of cardiac conditions and how CRY is working to save young lives using any means we can – from social media messages, to various campaigns, to a mixture of events.
In 2021, Raising Awareness Week will be held between November 20th and 28th. Please help support CRY by organising your own fundraising event, information stand, displaying or distributing posters and leaflets, sharing social media posts and CRY’s YouTube videos, or taking part in the CRY Great Cake Bake.

For more information on CRY’s upcoming fundraising events, go to www.c-r-y.org.uk/fundraising
Friday 26th November
Saving
For more info visit: www.c-r-y.org.uk/great-cake-bake-2021
The myheart network provides personalised help, support and information to individuals who have been diagnosed with a life-threatening inherited or congenital cardiac condition. We have a range of resources that you might find helpful, from literature, to website and video content, to our social media platforms and meetings.

This booklet provides medical information for young people who have been diagnosed with a cardiac condition or have been referred to a cardiologist for further tests, as well as their family and relatives. You can read the booklet online at bit.ly/3t2cSsJ
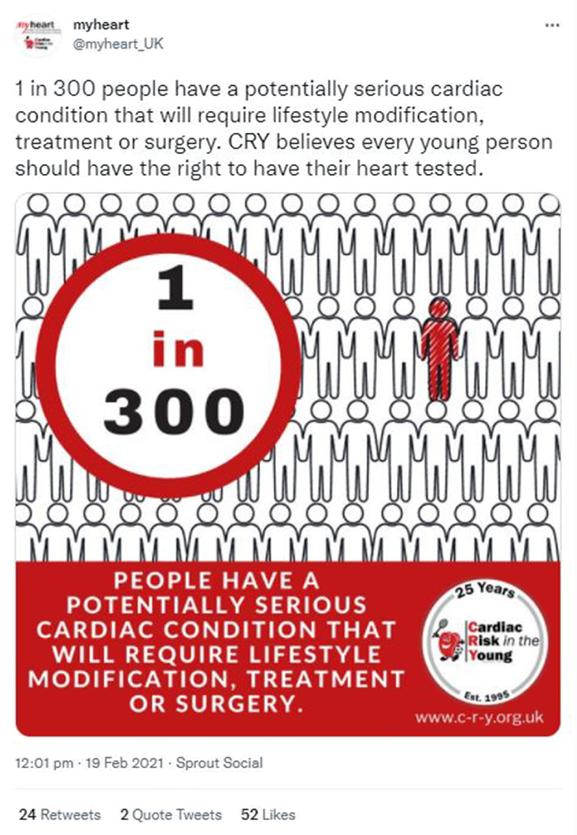

We send out regular enewsletters to members and update them about the latest myheart developments. You can subscribe to our enews here: www.myheart.org.uk/services
The website is accessible to all, however the members’ area is exclusively reserved for myheart members who are between the ages of 16 and 35 and living with a life-threatening cardiac condition (parental consent is needed for 16-year-olds). This area includes an activity area where the members can safely share their thoughts, feelings and experiences. Members can also ask each other questions.
There is also the facility in the members’ area for members to create their own blog posts. This is a great way for members to talk about any tests or treatments they have had. Some examples of experiences shared by members include living with a cardiac condition, how they felt when they found out, or when they had to give up sports.
As well as videos sent in by members to help others – sharing their experiences of being diagnosed or undergoing certain tests and procedures – the myheart YouTube channel features a number of frequently asked questions which have been sent in by members and answered by Dr Michael Papadakis. You can visit the YouTube channel at bit.ly/3DzdPxj
myheart typically holds two meetings a year in a central location for young people, between 18 and 35 years old, who have suddenly been diagnosed with a potentially life-threatening heart condition. Anybody between the ages of 18 and 35 can come to the meeting if they have been offered or already have an ICD, have suffered a cardiac arrest, or were diagnosed with an inherited cardiac disease. Members can gain support through meetings by talking to others in a similar situation.
myheart has a Facebook group where members (aged 18 and over) can connect with other people who have been diagnosed with a cardiac condition often ‘out of the blue’. So many people who contact CRY/myheart want to talk to others who are in similar circumstances to themselves. The group is a private community for members of the myheart network to share their feelings and experiences with others who have suffered a cardiac arrest, inherited a cardiac condition, have a congenital condition, or found out that they have a cardiac condition after a sudden cardiac death in the family and want to be part of a support network for one another.
To join the myheart network and find out more about the private Facebook group, please visit www.myheart.org.uk/joinmyheart. If you are already a member of the myheart network and would like to join the Facebook group, please email myheart@c-r-y.org.uk
You can follow myheart for updates and a wide variety of content on social media at:

We understand that being young and suddenly finding that you need to be treated for a heart condition is not easy. CRY’s myheart Network provides personalised help, support and information to individuals who have been diagnosed with a life–threatening cardiac condition.
myheart is a support system for individuals to help develop effective coping strategies and reduce social isolation. The network was developed in response to feedback from young people who found that support groups available were not effective in helping them deal with issues such as fitting of ICDs and pacemakers, and undergoing ablation surgery.
myheart offers:
• Medical information about different cardiac conditions, tests and treatments.
• Personal stories/videos from other young people who have been diagnosed with a cardiac condition.
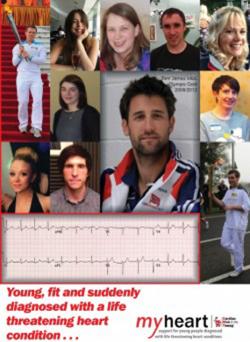
• Videos from our cardiologists answering frequently asked questions.
• A private area of the website for members aged 16–35 which features a members’ blogging area.
• Meetings for people aged 18–35 who have had a cardiac arrest; have been diagnosed with an inherited cardiac condition; have an ICD; or have been offered an ICD.
• A private Facebook group for anyone over the age of 18 who has been diagnosed with an inherited cardiac condition.

Email: myheart@c-r-y.org.uk
Online: www.myheart.org.uk
Telephone: 01737 363222
(Please ask for the myheart coordinator)
Post: FAO myheart
Cardiac Risk in the Young Unit 1140B The Axis Centre Cleeve Road
Leatherhead KT22 7RD
This is your newsletter - we would like to include your stories and photos. If you have been diagnosed with a cardiac condition and would like to share your story, thoughts and experiences with others, please send in your stories to myheart@c-r-y.org.uk.

This booklet – with an introduction from double Olympic gold medallist Tom James MBE, who was diagnosed with a heart condition known as atrial fibrillation in the run up to the London 2012 games – features 10 personal essays from young men and women who recount and talk through their own experience of suddenly being diagnosed with a heart condition. The booklet is for and by the growing number of young people who –thanks to greater awareness and early diagnosis – are learning to live with a diagnosis of a potentially life-threatening heart condition.
Tel: 01737 363222
Email: myheart@c-r-y.org.uk
Websites: www.myheart.org.uk