






myheart Newsletter 2021 In this Newsletter News and Latest Updates myheart Meetings myheartmystory CRY Research News and Events | Research News | myheartmystory Tel: 01737 363222 Email: myheart@c-r-y.org.uk Website: www.myheart.org.uk | 3 | 10 | 11 | 17 @myheart_UK myheartnetwork myheart
The Front Cover
For more details regarding the events shown on the cover, please turn to the corresponding page references below. Images are listed in rows from the top left:
1. “We thought something was wrong with ECG leads or monitor but…” by Jess-Lee Welch. Page 5.
2. CRY transforms its office into new screening centre. Page 4.
3. “I am forever grateful to the GP who saved my life!” by Roxy Ball. Page 11.
4. “Every Cloud.” by Thomas Flanighan. Page 15.
5. “Life with LQTS and LVNC by Abi Edwards.” Page 15.
6. CRY’s 25 Million Metre Challenge. Page 3.
7. “I have a heart condition but it’s not the end of the world!” by Gem O’Reilly. Page 16.
8. myheart meetings. Page 10.
No part of this publication
reproduced,
in
transmitted in any form or by any means; electronic, mechanical, photocopying, recording or otherwise, without prior permission of Cardiac Risk in the Young (CRY). CRY welcomes all content for the newsletter but reserve the right to edit when necessary and to withhold publication. Any opinion or statement by the author of any article or letter published does not necessarily represent the opinion of Cardiac Risk in the Young (CRY). Articles pertaining to health-related topics are for information only. Readers should obtain advice from their own practitioner before attempting to diagnose or administer any medication. Mention of any products or procedure should not be considered an endorsement for said product or procedure.


A note from the myheart Coordinator
We are delighted to present to you the newsletter for 2022 which is a round-up of myheart news and events from 2021. Whilst the last couple of years have undoubtedly been challenging for everyone, Cardiac Risk in the Young (CRY) and myheart continued to offer support to young people who have been diagnosed with a cardiac condition. We continued with online support meetings and shared new videos on CRY’s research made by CRY cardiologists.
myheart is now providing personalised support to nearly 650 members. We would like to extend our thanks to all of you for your continued support, whether it was in terms of fundraising, sharing social media posts, sharing your stories on the website, or writing to your MP. You can read about ways to raise awareness of CRY’s work here: c-r-y.org.uk/awareness
This newsletter includes personal stories shared by some of our members in 2021. We have received feedback about how impactful it is to read stories of others who have been diagnosed with a cardiac condition. We are very grateful when any of our members share their stories with us on the myheart website, as peer-to-peer support and shared experiences can help people to feel less alone in their suffering. We also welcome vlogs.
Dr Sabiha Gati, myheart consultant cardiologist, was interviewed by Sunrise Radio and the interview is included in this newsletter. She has also produced a very useful FAQ blog on the aorta and aortic dissections which, along with her previous article about myocarditis, received much appreciation from those looking for this information.

We regularly receive updates from CredibleMeds, which provides up-to-date information on medicines, and have shared it with our members via our website.

Also contained in this newsletter is information on myheart meetings and how you can volunteer at CRY events.
As the coordinator of CRY’s support group, it is my responsibility to put this newsletter together and it is my endeavour to get you all the news and event stories relating to members accurately.
Please do not hesitate to contact me by emailing me at myheart@c-r-y.org.uk or by calling me at 01737 363222 if you find anything amiss or if you have any views to improve our support network. Thank you for your help!
myheart newsletter 2021 2 myheart Newsletter 2021
5 8 1 2 4 3 7 6 Inside the newsletter 2 3 10 11 17 18 Welcome News and Latest Updates myheart Meetings myheartmystory CRY Research CRY Conference 2021
Head Office: Unit 1140B The Axis Centre Cleeve Road Leatherhead KT22 7RD
may be
stored
a retrieval system or
CRY’s 25 Million Metre Challenge
February 1 - May 2
To help mark CRY’s 25th anniversary, we were thrilled to introduce a new virtual event: the 25 Million Metre Challenge.

The aim of the event was to challenge people to collectively cover the distance of 25 million metres from February 1 (the start of Heart Month) to May 2.
We partnered with CRY supporter and myheart member Tony Eames, who originally created the Million Metre Challenge to raise funds and awareness for the charity. In 1991, when Tony was 12, he was diagnosed with long QT.
“As CRY continues to mark its 25th anniversary, we will be taking the opportunity of celebrating the achievements and milestones of everyone who has been diagnosed with a heart condition at a young age and who is living life to the full,” CRY Chief Executive Dr Steven Cox said as the start of the 25 Million Metre Challenge approached. “As well as helping us to encourage all young people aged 14-35 to get their heart checked.”
Supporters could take part as an individual or create a virtual team of 12 and complete metres by walking, running, cycling, rowing or swimming. 134 people (including some members of CRY’s staff) all around the country took part, covering their distances in various ways to help us towards our lofty target.
The event got off to a fantastic start as participants racked up over 15 million metres in the first month alone! As this momentum continued, we decided to be even more ambitious and double our overall challenge target to 50 million metres.
A combined total amount of 47,369,782.85m was completed!
This is almost double the target we originally set out to accomplish and equates to travelling more than once around the world! It can also be equated to completing 1,122 marathons! A very fitting achievement for our 25th anniversary.
Through this challenge we also raised nearly £4,000 and excellent awareness, as supporters got active in their local communities and shared word of the event on social media.
Thank you so much to everyone who took part in this challenge! It was amazing to see this new event become such a success.
Sunrise Radio 36 hour marathon broadcasting event March 26-27
We have partnered with Sunrise Radio since the start of 2020 as part of CRY’s 25th anniversary to help raise awareness of young sudden cardiac death, the importance of screening, and the work we are doing with on-air advertising and interviews. In March, one of their presenters, Anushka Arora, took on the challenge of hosting a 36-hour broadcast to help raise funds and awareness for CRY.

The broadcast included music, interviews with CRY doctors, families and young people whose lives had been saved by screening, and reminders of why it’s so important to support CRY and raise funds for screening.
“This unique media collaboration will spread awareness as much as it will raise funds for the cause,” Anushka said before starting the event. “We are long past the time when broadcasting was only limited to selling commercials and programming airtime. It has become a means to reach out to the masses and utilize it for the better of the mankind. My heart goes out to those who meet their tragic ends from an undiagnosed heart defect.”
Various guests joined through the broadcast to help push CRY’s key messages. CRY Ambassador and singer songwriter Arjun has been a supporter since the death of his wife Natasha, who died suddenly in 2018 from a previously undiagnosed heart condition when she was just 30 years old. Arjun made an appearance on the broadcast to show his support. Natasha’s sister, Dr Vanessa Sandhu,
www.myheart.org.uk 3
News and Latest Updates
News and Latest Updates
has also become a CRY supporter, and was interviewed about the impact of Natasha’s death. Other guests included doctors such as former CRY Research Fellow Dr Joyee Basu, and athletes like England Women’s cricketer Danielle Wyatt. CRY Chief Executive Dr Steven Cox also joined to see in the end of the broadcast and talk about the charity’s work and the impact of the pandemic.
Sunrise Radio Managing Director Tony Lit MBE said the following about why the network is backing CRY: “Sunrise is now in its 32nd year of broadcasting to the South Asian community and over the years it has become much more than a source for entertainment but is also relied upon for important community messages, news and information. It’s absolutely vital that we do our bit in society and support charitable organisations like CRY. There can be nothing worse than losing a young life needlessly in our country in this day and age.”
This event was a fantastic way to raise awareness and raised £10,000 for CRY through donations from listeners. Dr Steven Cox spoke as the event came to a close:
“I would like to firstly say a huge thank you to Tony Lit. Tony agreed to become a CRY Ambassador after seeing the impact a young sudden death has and for the last 18 months he has done so much to help us raise awareness and funds for CRY as well as putting this idea forward. As well as Tony, I would like to thank everyone at Sunrise, Kay, Paul, Rajit for bringing this together.
“A big thanks to all your guests for supporting this and their kind words about CRY, in particular Arjun for agreeing to come on the show. Also Professor Sanjay Sharma and all the CRY doctors who talked about their work, as well as all the CRY families who shared their stories about the tragedies in their families which so sadly led them to becoming involved with CRY. Thank you to everyone who has donated and supported this campaign.
“But most of all I would like to thank Anushka. You are really quite incredible. I cannot put my hand on heart and say I listened to every minute, but I’ve been listening for more than 24 hours, and in that time my music horizons have
expanded exponentially but I cannot believe you have come to the end of the broadcast with the same energy that you started. You are amazing and I know I speak for everyone out there when I say thank you, Anushka.”
Former CRY Research Fellow and myheart Consultant Cardiologist Dr Sabiha Gati was also invited to speak with them about her research fellowship with CRY and her continuing work with the charity.
To listen to all interviews from this event, you can go to c-r-y.org.uk/sunriseradio

CRY
transforms its office into new screening centre July 10-11
CRY typically provides free heart checks for over 32,000 young people in a normal year. But due to the COVID-19 pandemic and the restrictions and lockdowns in place, we had to put our screenings on hold for around 15 months.

Tens of thousands of people missed their heart tests as a result, which would have led to around 150 young people not receiving a diagnosis of a potentially life-threatening condition and the treatment, lifestyle advice or surgery that would reduce their risk of suffering a cardiac arrest.
Our screening services in the community and for both grass roots and elite sports were already scheduled to resume on June 28, but due to the waiting lists caused by the pandemic and the increased awareness and anxiety following the televised collapse of footballer, Christian Eriksen, we worked to increase our testing capacity at the newly established screening centre at CRY’s head office.
Starting on July 10 and 11, CRY’s office in Leatherhead, Surrey was transformed into a specialist screening centre – with regular weekend appointments scheduled for the

myheart newsletter 2021 4
rest of the year and beyond – as part of this innovative new service.
During lockdown we worked really hard to ensure our screening team would be appropriately prepared, with revised protocols in place, in terms of PPE, social distancing and enhanced cleaning, and that we’d be ready “to get back on the road” as soon as it was safe to do so. We felt so relieved and enthused when we had the go-ahead to start screening again – knowing we had a huge waiting list to work through and a ‘duty’ to deliver screening to young, asymptomatic people across the UK.
At CRY we are doing everything we can to identify those at risk, and understand why these collapses and sudden cardiac arrests happen – and that’s also why research is so important. We want every young person between the age of 14-35 to have the opportunity to have their heart tested. For more information about CRY’s screening programme, please go to testmyheart.org.uk

15th anniversary of the CRY Heart of London Bridges Walk June 27

News and Latest Updates
Although it was disappointing that we could not all walk together, it’s amazing how many people took part. Many participants created their own walking routes this year, incorporating local landmarks, rivers, streams, bridges, rural pathways and beaches. It was so lovely to be able to see the beautiful locations that supporters walked through.
Each participant/group took part for their own reason, which was expressed through our digital message wall. 80 beautiful messages were posted on the digital wall as it became the homepage of the CRY website for the day. It was a very emotional and poignant day for everyone involved. Speeches from CRY Patron Kathryn Harries, who walked in her local hometown, and CRY Chief Executive Dr Steven Cox were broadcast live on CRY’s social media channels at 10:50am and were available for everyone to watch together virtually.
“I’ve been a CRY Patron since 2007, and it is an honour and a privilege to be associated with, and support, such a wonderful organisation, doing such fantastic work,” Kathryn said in her speech recorded before the event. “I shall be walking on the 27th of June with you, but here in the Surrey Hills, and I hope with my family, restrictions permitting. I wish you all the very, very best. Thank you all for your support, and I look forward to seeing you again next year.”
“The fact that we have once again been unable to join each other afterwards for a picnic with family and friends in the park doesn’t make today any less important,” Dr Cox said. “I believe I and every person who supports CRY are part of an organisation that celebrates life. The lives which are in our memories and the lives that will be saved, because of what we have all come together to try to achieve... Thank you for joining us today – for everything you do for CRY, for every photo and message you have shared. Thank you for helping to save young lives.”
Sunday 27 June 2021 marked the 15th anniversary of CRY’s flagship event, the CRY Heart of London Bridges Walk. Walking virtually for the second year in a row, we are pleased to say over 315 people from all over the country took part, to connect with each other and remember those they have lost or to support those diagnosed with a cardiac condition. Like last year, the walk was very different from the usual event that is held in Southwark Park, London.
Thank you to everyone who took part in the event. We are so grateful to you all for your continued support. It is amazing to see the map of all the locations where participants walked. It shows how much awareness was raised on the day throughout the UK. There was even one participant in the United States who walked in California which is just incredible.
We will be back in Southwark Park as
A map of all the locations where CRY supporters completed their walks

www.myheart.org.uk 5
News and Latest Updates
normal this year on Sunday 26 June 2022. To register to join the walk, please visit c-r-y.org.uk/bridges-walk-2022
We are only able to hold the event thanks to the incredible support of CRY’s volunteers. If you would be interested in kindly volunteering at this year’s Heart of London Bridges Walk, please register as a volunteer at c-r-y.org.uk/volunteer-registration-form.
Every year, KCL Tennis hosts a tournament with the aim of raising money for a chosen charitable organisation. This year, we chose to raise money for CRY. As a university sports team, we felt this was a good cause to focus on. We hoped that through fundraising for CRY, we would also be able to raise awareness about this important charity, as well as encouraging our members to think about the importance of looking after their cardiac health, particularly in the context of high-intensity sport performance.
Due to ongoing lockdown restrictions, we were unable to host an in-person tennis tournament – this was disappointing as it’s usually one of the highlights of our calendar. Instead, our committee decided on a different way to raise money – we opened up a competition where entrants could send in a video of themselves hitting a tennis ball in the most creative way possible. The most creative entries were to receive a prize, and every entry was included in a video compilation. We were delighted with the response from our club, with a wide array of creative tennis shots featuring in the resulting video. The two top winners were Hassan from our GKT Team, with a very intimidating boxing punch of the tennis ball (perhaps he should consider also joining KCL Boxing), and Amanda’s (one of our Women’s Team Captains) Mum, with a backhand ladle swat to protect her soup broth from the tennis ball. These were worthy winners indeed.

The process of fundraising was enjoyable – we were lucky to have so many people happy to be involved, and we were proud to raise over £300 for CRY. I hope that via our fundraising, we were able to raise the profile of CRY in our club, and I’m grateful to the charity for the work that they do – especially for young athletes.
FAQs about aortic disease answered by Dr Sabiha Gati

What is aortic disease?
The aorta is the largest tube (artery) that carries blood cells containing oxygen around the body to your vital organs. The blood cells are pumped from the main pumping chamber called the left ventricle in to the aorta.
The aorta can also be affected by disease and can either generally enlarge (dilate) or balloon with localised enlargement (aneurysm) or can also tear or split (dissection) and these effects can have fatal consequences.
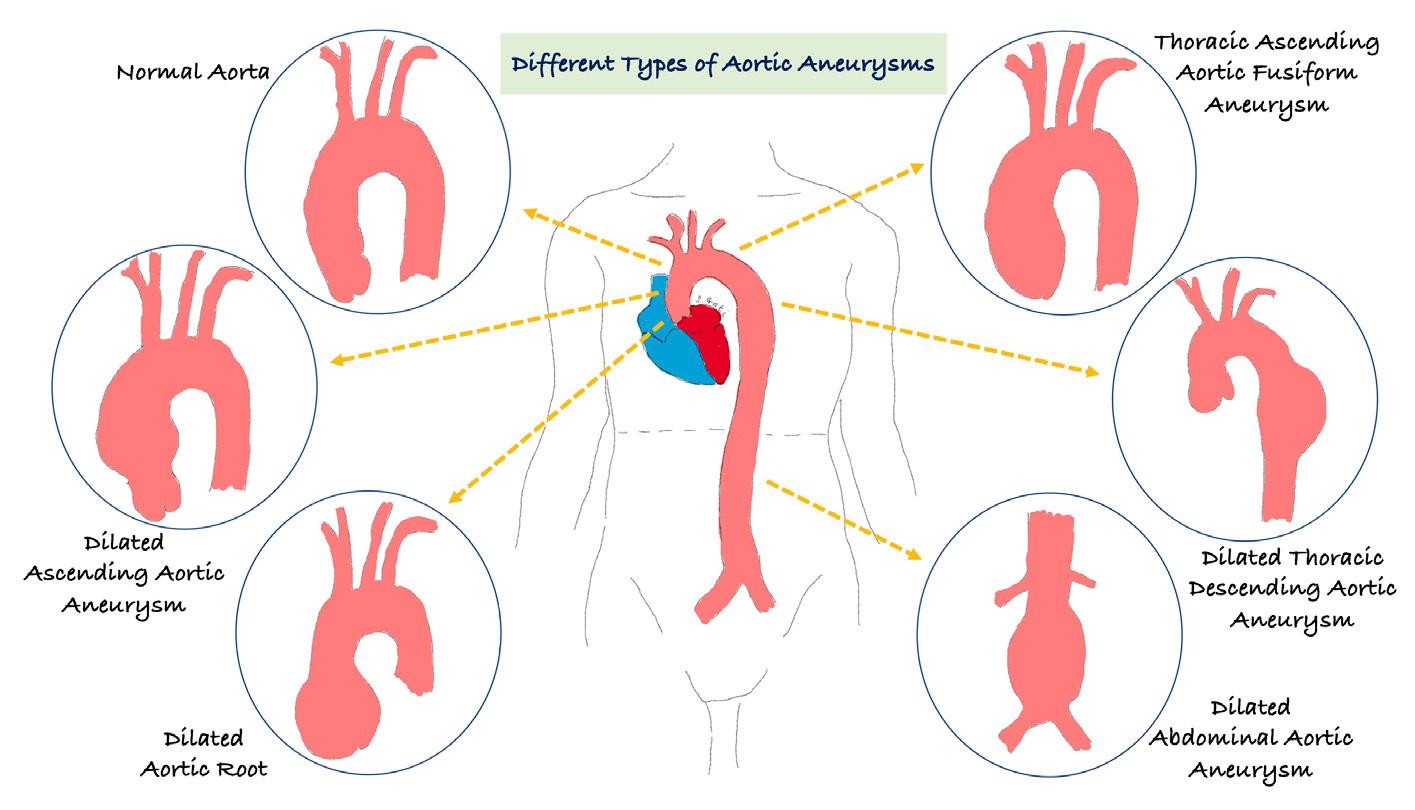
Is there only one type of aortic aneurysm?
The short answer is no, there are three main types of aortic aneurysms. An aneurysm is a weak spot in the wall and cause the aortic tube to bulge like a balloon. The main concern with an aneurysm is that it can rupture and cause severe bleeding which can prove fatal if it is not quickly treated. Aortic aneurysms are classified as:
1. Abdominal (tummy) aortic aneurysms – as the aorta travels through the tummy it can balloon/bulge. These are also sometimes known as triple A (AAA). Older individuals and those who are long-term smokers are at high risk. The type of symptoms these may present with include an extremely sharp and severe pain which may indicate rupture and this requires emergency treatment and must not be ignored. The other symptom includes pain in the back or in the bellybutton region.
2. Thoracic (chest) aneurysms – these occur in the chest; most individuals will not have symptoms but these are usually picked up on imaging such as a Chest X-ray, echocardiogram (ultrasound scan of the heart), CT scan of the chest and/or on an MRI of the heart. If your thoracic aortic aneurysm becomes very large, it can cause discomfort in the chest and even pain between your shoulder blades. If a thoracic aortic aneurysm was found, this would require monitoring on either a 6-monthly or annual basis depending on the size of the aorta. There are many advanced treatments available now when the aorta enlarges significantly, and this includes minimal surgical techniques such as stenting but occasionally you may require complex open-heart surgery to replace the aorta, but this all depends on how complex your disease is. If you want to learn more, please see below.
3. Thoracic abdominal (chest and tummy) aneurysms
myheart newsletter 2021 6
KCL Tennis Rally for CRY by Dan Redfearn, myheart member
What causes damage to the aorta?
There are several medical conditions that may damage the aorta and weaken the aortic wall and these can be acquired (environmental) or genetic (running in the family). If these conditions are not treated and monitored, they can put individuals at risk of sudden death, and these include:
1. Genetic conditions in young people such as Marfan syndrome
2. Connective tissue conditions such as Ehler-Danlos syndrome, Turners syndrome, scleroderma, polychrondritis and polycystic kidney disease
3. Trauma or injury to the chest or abdomen
4. Hypertension (high blood pressure)
5. Atherosclerosis (hardening of the arteries from fatty build up)
What are the treatment options?
Your doctor will initially watch slow growing aortic aneurysms and will advise on lifestyle changes and medications. If the aortic aneurysm is fast-growing it may require surgery and we would advise you are monitored in a specialist clinic.
What is Thoracic aortic aneurysm?
The aorta is the largest tube or vessel in the body and carries the oxygen containing blood round the body. A weakening in the aorta wall can result in an aortic aneurysm (ballooning or bulging) and over time there is a risk it can tear (dissection) or burst (rupture). This would cause life threatening bleeding and place the individual at potential risk of death. Thoracic refers to part of the aorta that runs through your chest.
Once an aortic aneurysm develops it can gradually increase in size and progressively weaken. This would need to be closely monitored in a specialist unit either on a 6-monthly or yearly basis. Treatment for a thoracic aneurysm includes surgery by either repairing it or removing the disease segment and replacing it or a metal mesh coil (stent) can also be inserted if suitable to the diseased aorta and preventing from rupturing.
News and Latest Updates
What causes a thoracic aortic aneurysm?
There are several medical conditions that can cause your thoracic aorta to enlarge or develop an aneurysm and these include:
1. Genetic disorders – Marfan syndrome
2. Family history
3. Diseases of the connective tissue
4. Atherosclerosis (hardening of the arteries with fatty plaques)
5. Degenerative diseases such as hypertension
6. Inflammation of the arteries – your own body develops a heightened immune response to the arteries such as vasculitis
7. Infection but this is rare in the Western world.
What sort of symptoms would I experience with a thoracic aortic aneurysm?
These can be really variable; some individuals may not get any symptoms. However, when symptoms do occur, they must be taken seriously and may relate to the location, size and the speed with which the aortic aneurysm is growing or enlarging. Sudden severe pain in the chest radiating into the back could be serious and should not ignored as it could be a life-threatening emergency.
Symptoms to monitor include:
1. Pain in the chest or back
2. Pain in the neck, jaw, upper back
3. Wheezing, coughing and breathlessness due to the aorta pressing on the windpipe
4. Hoarseness of the voice
5. Difficulty swallowing due to pressure on the gullet pipe.
What tests would
I
need to diagnose an aortic aneurysm?
A comprehensive evaluation includes a detailed clinical and family history and physical examination. The following tests may be considered:
1. Chest X-ray – to check if the cardiac contours on the X-ray image are wide.
2. Computed tomography (CT) – this uses X-rays and can take detailed images of the aorta as well as other
www.myheart.org.uk 7
body structures. Repeats CTs can be associated with accumulated radiation and would not be advised on a 6-monthly basis.
3. Magnetic resonance imaging (MRI) – this uses large magnets and radio-frequencies to acquire images of the heart and aorta. This test does not involve radiation and can be used on a 6-monthly basis if needed. This test may not be available in all hospitals.
4. Echocardiogram (ultrasound scan) – this uses sound waves to image the heart structure and function. This is good to scan the first part of the aorta as it leaves the heart.
5. Aortogram (angiogram) – this is invasive and uses X-rays to assess for aneurysms and narrowing of the blood vessels.
How will my thoracic aortic aneurysm or enlarged aorta be managed?
Once you have been evaluated in a specialist centre, which may include an inherited cardiac condition clinic or an aorta clinic, the initial steps will be baseline tests followed by monitoring with either an MRI or CT. This will allow your doctor to monitor the size and how quickly the aorta is growing. Your clinical surveillance maybe every 6 months or 12 month depending on how complex your condition is. Your doctor will also talk to you about making lifestyle changes including giving up smoking, controlling your blood pressure and blood sugars if you are diabetic. They will also give advice on the exercises you should perform to lose weight if you are overweight but also prevent further aggravation of the aortic size. For some individuals, depending on the cause of the aorta enlargement, your doctor may want you to take some medications called beta-blockers, blood pressure pills and to lower your cholesterol levels. Your doctor may also want to start you on a medication called angiotensin receptor blocker such as losartan or irbesartan.
If you get to the stage where you require surgery, these are the options:
1. Endovascular aneurysm repair (EVAR) – this is minimally invasive and requires a small cut in the groin and through X-ray machines and specially designed instruments, the surgical team would implant a metal coil meshed stent inside the aorta. Unfortunately, not all thoracic aneurysms can be repaired with this technique and it depends on the type, size and location of your aortic aneurysm.
2. Open heart surgery/repair of thoracic aortic aneurysm – if your aneurysm is in the ascending aorta or the arch, you may require an incision/cut through the breastbone. If your aneurysm is also involving damage to the aortic valve, this may also need to be replaced or repaired during your
surgery, but your surgeons will discuss your options in more detail. If your aneurysm is in the descending aspects, the incision may extend from the back around the shoulder blade around the side of your rib cage to underneath the breast tissue.
What size of my aorta requires surgery?
The larger your aortic aneurysm the greater the risk of rupture. It is estimated that once your abdominal aortic aneurysm is >5.5cm, this is likely to rupture within 12 months in 3-6 out of 100 people and therefore, surgery would be indicated.
For thoracic aortic aneurysms, the current European Society of Cardiology (ESC) guidelines suggest surgery when the aneurysm is 5cm or more for individuals with a genetic condition placing them at risk of rupture or dissection such as Marfan syndrome and other connective tissue diseases. In non-Marfan patients and in general, the cut-offs are 5.5cm. However, your doctor may start to plan your work-up for surgery earlier than these cut-offs to ensure there is a medical and surgical plan in place for your future care.
What is familial thoracic aortic aneurysm?
Sometimes, a thoracic aortic aneurysm can run in the family and therefore, has a genetic predisposition. We identify this in around 20% of the general population and many people don’t know they have it plus they may not have any symptoms. When there is a genetic element to your condition, your first-degree relatives which includes, parents, siblings and children should be screened for the condition.
There are many genes involved in aortic aneurysm and here are just a few important ones but there is a very long list which can be found on www.omim.org:
1. Fibrillin -1 – this is associated with Marfan syndrome
2. Elastin (ELN) – this is associated with a narrowing above the aortic valve and ascending aortic aneurysms
3. Collagen 1 alpha-1 or 2 (COL1A1/2) – this can cause osteogenesis imperfecta; Ehlers-Danlos syndrome
4. Collagen 3 alpha-1 (COL3A1) – this causes Ehlers-Danlos type 4 which is frequently associated with artery dissection
5. TGFBR1 and 2 – causes Loeys-Dietz syndrome which is highly penetrating and leads to aortic root and large and medium artery aneurysms
6. SMAD3 (SMAD family member 3) – causes Loeys-Dietz syndrome with osteoarthritis
myheart newsletter 2021 8
News and Latest Updates
7. ACTA2 (alpha-smooth muscle actin) – causes familial aortic aneurysms
8. NOTCH1 (notch1) – associated with bicuspid aortic valve with ascending aortic aneurysm
9. JAG1 (jagged1) – associated with aneurysms of brain arteries, narrowing of the aorta and aortic aneurysms
10. PKD1 or 2 (plycystin-1 or 2) – associated with polycystic kidney disease with aneurysms of brain arteries
What is aortic dissection (tear of the aorta)?
The aortic wall is made of 3 layers of tissue (like a sandwich) and a dissection starts with a tear in the inner layer of the wall of the thoracic aorta. Blood then seeps through the layers separating them and progressively weakening the wall and potentially rupturing/bursting (a bit like a soggy sandwich falling apart). Unfortunately, aortic dissection can be life-threatening, and the most common symptom is constant chest pain radiating through to the back between the shoulder blades. The pain can also move from one position to the next. Depending on the location of the dissection, immediate surgery may be required.
Are there any specific triggers or causes of aortic dissection?
The reason why people develop a tear in their aorta is unclear but there are some risk factors we can certainly manage and try to avoid an aortic dissection, and these include:
1. Ensuring high blood pressure is treated. If your blood pressure is >140/80mmHg please speak to your GP.
2. Genetic conditions such as Marfan syndrome, EhlersDanlos syndrome and Turners syndrome. You may need genetic testing for these conditions.
3. Inflammation of the aorta called aortitis
4. Degenerative disease of the aorta called cystic medial disease
5. Atherosclerosis (hardening of the arteries)
6. Bicuspid aortic valve with 2 flaps to the valve rather than 3 can also cause enlargement of the aorta
7. Trauma/injury
8. Narrowing of the aorta called coarctation of the aorta
9. Polycystic kidney disease which results in fluid filled pockets in the kidneys. This is a genetic disorder.
Can I exercise with aortic disease?
This is a very good question and it depends on the type of aortic disease you have and how dilated the aorta is. However, in general those who are low risk such as individuals with a bicuspid aortic valve with an aortic dimension of <40mm or Turner syndrome without aortic
News and Latest Updates
dilatation can participate in all sports but the preference is endurance rather than power sports.
Individuals who are regarded as intermediate risk such as with Marfan syndrome but without aortic dilatation; people with a bicuspid aortic valve with aorta of 40-45mm or after successful surgery for a bicuspid aortic valve should be advised to avoid high and very high intensity exercise, contact and power sports. Again, the preference for sports should be endurance e.g. running or cycling rather than power sports such as weightlifting.
People who have a moderate aortic dilatation, 40-45mm in Marfan syndrome; 45-50mm in bicuspid aortic valve patients; after surgery for thoracic aorta in Marfan syndromes, the advice is only skilled sports or low-intensity endurance exercise.
Participation in sports as a temporary measure is advised in any individual with a severe aortic dilatation, that is >45mm in Marfan syndrome, >50mm in bicuspid aortic valve or if you have complications after thoracic aortic surgery.
Update from CredibleMeds
CRY has received a number of updates from CredibleMeds throughout the year. Members with cardiac conditions may like to consider registering with CredibleMeds to be kept up to date with any changes to the QT drugs to avoid list crediblemeds.org/everyone
CRY Events
Volunteering at CRY Events
We are so grateful to our supporters who offer up their time. From being an official CRY ‘cheerer’ at a mass participation event, helping to marshal the route at the CRY Heart of London Bridges Walk, holding an awareness stall, sharing our key messages on social media, to volunteering at a UK festival – there are lots of opportunities to get involved by

www.myheart.org.uk 9
volunteering!
Events volunteering – Providing your help on-site at any of our events is a great way to get into the action of our fast-paced busy events! Our events include Simplyhealth Great North Run, Virgin Money London Marathon, Heart of London Bridges Walk and more!

Volunteering in your local community – Volunteering in your local community is extremely beneficial in raising awareness of the important work that CRY does.
Raising Awareness – Help promote CRY by distributing CRY general information leaflets/collection pots at your workplace, local school, leisure centre or in theatres, pubs, shops, doctors and pharmacies.
Social media – Follow myheart on Twitter and Facebook. By sharing any of our messages you are helping to raise awareness. Some members also help to raise awareness by sharing their own stories, including #myheartmystory
In-office volunteering – Our CRY in-office volunteers take on a range of practical and administrative tasks. We have limited space but are always grateful for an extra pair of hands in the office!
If you would be interested in volunteering some of your time for CRY, or would like to receive a volunteering information pack, please email volunteering@C-R-Y.org.uk
National myheart meetings
Online myheart meeting: April 24, 2021

A myheart members’ Zoom meeting was held on Saturday April 24, 2021. There was a Q and A session with
cardiologist Dr Sabiha Gati in response to queries and concerns that members had relating to their heart condition and the pandemic.
Online myheart meeting: October 23, 2021
A myheart members’ video meeting was held on Saturday October 23, 2021. There was a Q and A session with cardiologist, Dr Sabiha Gati, giving members the chance to meet with other young people who have been diagnosed with a cardiac condition, as well as an informal space to ask questions of a consultant cardiologist.
Currently myheart holds meetings twice a year for young people, between 18 and 35, who have suddenly been diagnosed with a life-threatening heart condition. Anybody with a cardiac condition between the ages of 18 and 35 can come to the meetings if they:
• Have been offered or already have an ICD
• Have suffered a cardiac arrest
• Have been diagnosed with an inherited or potentially inherited cardiac disease
Given the complexity of some conditions we recognise that there will always be a need to consider some cases on an individual basis.
Meetings are free to attend and give members an opportunity to meet and discuss their experiences in an informal but supportive environment.
Those young people that attend these meetings usually find them very helpful. It does not matter how long ago you first received your diagnosis or whether you are undergoing any sort of treatment at the moment.
For more information about myheart meetings, including upcoming dates, please visit myheart.org.uk/meetings
myheart newsletter 2021 10
Latest
News and
Updates
by Roxy Ball
From being little, I always remember I found running and PE hard. I was good at rounders because I could hit the ball and then race around the posts! But everything else I was bad at. I never had any stamina!
I always got worried about things too, it would just come on. I used to get horrible feelings about things and feel something bad was going to happen. It used to frustrate a lot of my family, because they couldn’t find any triggers for my worries. My friend’s stepdad used to call me Miss Catastrophe!
When I was 13 I contracted tonsillitis which then resulted in a strong positive test for Glandular Fever. The GP told me I needed two weeks off school. It was Christmas and I was devastated, all of my Christmas concerts were happening, and I missed them all. I played saxophone, clarinet, piano, recorder and sang in the school choir. The GP said that the month rest with the two weeks Christmas holidays would hopefully make everything better.
After that month, I didn’t feel any better. I felt tired all the time and achy. I went for my first clarinet lesson and my teacher was so worried that I’d gone pale and shaky, she abandoned the lesson, asked me to sit on a chair and summoned her mum who was upstairs!
I went back to school but was sent home because I looked ill and couldn’t physically move around the school. My year tutor who was also the SENCO Lead intervened and explained I could just go into school for mornings and work in her classroom. They would get teachers to send my work to her classroom.
Although this part of my life was tough, I’ll always be thankful to her. She had a few of us in the classroom, mainly naughty kids! I would quickly finish the work I’d been set, and she started to ask me if I could help the others who found academic work tough. I look back now and think this was the start of my career! In the face of adversity something I love to do, was born.
I became very unwell and could not physically get out of bed. My parents were extremely worried, and the GP visited me at home. I was admitted to hospital with an irregular heartbeat. I spent a week in hospital with medics being baffled. What followed was a lot of avenues being explored such as: arthritis, school phobia, chronic fatigue syndrome
myheartmystory
and post viral syndrome. My parents were amazingly supportive and knew that I loved school – loved doing homework (yeah … I know!) and tried the best they could to try and help me get better.
I spent Y9, Y10 and Y11 in and out of school due to illness, but my year tutor continued to be supportive and I worked in her room a lot. Other teachers such as my English teacher were amazing. When I got my GCSE grades of 2 As, 4 4 Bs and a C I was amazed! I didn’t get entered for some subjects, there was no point as I had missed too much!
I lacked confidence and feared becoming unwell again. My parents supported me to go to a small Beauty and Complimentary Therapy School, which I loved. I achieved an ITEC L3 Beauty Therapy Diploma within a year.
With my newfound confidence and getting a part time weekend job at Debenhams in the cosmetics department, I became the youngest beauty therapist for a prestigious skincare company. I undertook training in London and at 19 became part of their National Sales Team. At 22 I became their National Events Manager. These years were amazing for me working in places such as Harrods, Selfridges, Celtic Manor and The Vale just to name a few.
At 24 I started to feel unwell, I went to see my GP and she asked me to go straight to the hospital to have an ECG. I did and it returned as abnormal. I was continually asked by medics if I had taken any drugs. I hadn’t, but I felt as though I wasn’t believed. I was asked to stay overnight and then told that I could go home but needed further investigations. I had these and then saw a very dismissive trainee Cardiologist. He told me I’d probably got Glandular Fever which is why I felt ill and that my heart was fine. It would be ridiculous to put me through a risky and dangerous Catheter Ablation.

At this point I was in the last year of my Open University degree and decided to change my career. I’d been recommended to make some lifestyle changes. I moved into tutoring English and maths, in a local training provider whilst working towards a PGCE and GradDipEd once I’d achieved my BSc.
Healthwise, the reduction in a physically demanding and national job seemed to help things. However, in 2012 I flew to Australia a couple of days before Christmas on a very full plane from Heathrow. Once we had taken off, I suddenly felt unwell, I don’t remember anything else apart from coming back round to an oxygen mask on my face and an air hostess looking after me. I’d collapsed and lost all control, not what you want on a full long-haul flight! I was then quarantined when I got to Australia and searched. Again, another unpleasant experience due to my strange heart antics!
www.myheart.org.uk 11
I am forever grateful to the GP who saved my life!
myheartmystory
I’ve now worked in education for over 10 years and have always worked with disadvantaged learners. I think this goes back to those school days, there is no better feeling than watching someone achieve more than they think they can! A couple of years ago, I started to fall over at work. I’m quite dippy so I just thought I was tripping up, but I started to fall, regularly resulting in bruises and injuries that I didn’t feel until later. One day I was walking and the next minute I was on the floor. Someone saw this and was insistent I had collapsed, and work asked me to go to see my GP.
I’d recently moved and been very impressed with a GP who had seen me about a skin condition I had had for three years. He had fixed the condition within a month of seeing him and so I requested the appointment with him. I went to see him and he explained he would need to review all of my notes and would run some tests. He reviewed my notes and explained there were some anomalies in what cardiac problems I had. He said as a precautionary measure he would run an ECG but he felt that this was just belt and braces. The ECG was ran by a technician and I could see the look on her face, it was the usual look of surprise. I was then placed in a side room, whilst other people viewed the ECG – again something I’d become quite familiar with! She explained I would need to see a doctor to explain the results.
The GP explained I did have Wolff-Parkinson White Syndrome, something which had been identified as me having and then not having. It was always under question. He said that some ECGs displayed the unusual heart waves and others didn’t. He said he would refer me to a Cardiologist. I saw the cardiologist within a couple of weeks and felt quite shocked. He told me that I either had a Catheter Ablation or I was at risk of cardiac arrest and sudden death. He said I would not get life insurance, be able to re mortgage and wouldn’t be able to get holiday insurance. The cardiologist told me that each time I was falling over, I was collapsing because my heart rate was too high.
I agreed to have the ablation and within four weeks I had the procedure. During the ablation they found not one, but two accessory pathways. I was very fortunate because they took the decision to ablate both of them in the same day, otherwise I would have had to have the procedure all over again to ablate the second accessory pathway they had found. When the cardiologist came to see me after the procedure, he asked me how I felt. I said I couldn’t feel my heart beating, he said he’d asked me if I’d had palpitations and I’d always said no. I realised that you aren’t supposed to feel your heart beating and that’s what a palpitation is! But having always felt my heart beating, I never understood that you shouldn’t feel it beating.
It took me about six months to fully recover from the procedure. It evoked sciatica in me which made walking

extremely painful, but that subsided after about three months. It also caused me to have continual visual disturbances, feel constantly nauseous, tired and have a headache for around four months after. I also suffered from low blood pressure and apparently, I was a funny colour for a while!
However, it was all worth it. 18 months on I feel the best I have ever felt in my life. The crippling anxiety I lived with at times, isn’t there anymore. People are disappointed now because I don’t react so much when they tease me! For the first time in my life I have more stamina and I don’t feel tired all the time. I can obtain insurances easily because I’ve had a successful ablation and now, I am not classed as someone with a heart condition. Also, my eyes have improved and I have a weaker prescription, which baffled the optician. They feel the explanation is that my heart must be pumping blood better, which has improved my eyesight!

I will always be truly grateful to the GP who took the time to read through all my notes, examining the detail and the precautionary tests he ran. I’m passionate about young people being able to access screening, the Catheter Ablation has changed my life and my future. I will always be so incredibly thankful to the GP who I believe saved my life.
I was in my final year of uni studying Sport and Exercise Science and we were in the lab doing ECGs on one another. When my lecturer (Dr David Oxborough) came to check on
myheart newsletter 2021 12
We thought something was wrong with ECG leads or monitor but… by Jess-Lee Welch
myheartmystory
mine, he thought something was wrong with the monitor or leads. Long story short, the monitor wasn’t broken. After staying behind and completing an echocardiogram on me, he referred me to Liverpool Heart and Chest Hospital. After 3 years of biannual Exercise Stress Tests, 24-hour monitoring, MRI scans and ECGs, I was diagnosed with Congenital Heart Block and had a pacemaker fitted at the age of 24. They struggled to diagnose me as I had no symptoms and my heart kicked into action when I started to exercise, but with a resting heart rate of 30bpm, I was missing a few beats.
Before diagnosis, I was none the wiser, so I wasn’t affected at all. When I was told they wanted to fit me with a pacemaker, I went along with it and trusted their professional judgement and didn’t think anything of it and I carried on my day-to-day life. I hadn’t told any of my family or friends until after my operation, so I had no conversations that prompted me to think about it. March 2020, I had my pacemaker fitted and I am fortunate to have had a successful and speedy recovery, physically.

I would describe myself as mentally tough and resilient, but this lifestyle change broke me. As a personal trainer, I was extremely active. Playing football, Cross Fit, strength training etc. Now this has completely stopped and turned my life upside down. For the first 6 months, I ignored the experience that I had gone through and didn’t think about it. Once I opened my mind to think about it, anxiety filled my body every minute I was awake. After a gruelling 6-month battle with anxiety and depression, I am now at the stage ready to accept it and open up about my experience to help raise awareness. It has been a tough journey throughout the pandemic, being so isolated, but running has been my life saver. 12 months on and I am hoping to get back into some gentle weight training!
Bang.
Bang.
Bang.
To say it was painful would be a gross understatement. It was a combination of the most painful experience of my life, mixed with the most terrifying. Not only was it the first time I had inappropriate shocks, it was the first time I had multiple shocks in a row.
And the thing is, I didn’t know they were inappropriate at the time (nor am I convinced they were, but I’ll get to that). In my mind, I was dying. As far as I knew, I was going into cardiac arrest again and my ICD was doing its best effort to keep my heart beating. The fact that it shocked me multiple times not only added to the pain I was experiencing — but with each shock it exponentially made it more terrifying. Why wasn’t it working? Why didn’t my heart return to normal after the first shock? Why not after the second? The third? The fourth?
As each shock jolted my shoulder forward, my thoughts quickly entertained the idea that something was even more wrong than “normal”. That this time may be the last time, for good. So why is it not a relief that I wasn’t going into cardiac arrest? I wasn’t dying, it was an “accident”, an unfortunate possible side effect of having an ICD, just a bug in the code that they can’t fix. Why doesn’t that make it feel any better? Well, for one, I’m still not entirely convinced it was inappropriate.
See, I’ve had 9 appropriate cardiac arrests now. I like to consider myself somewhat a “pro” at “dying”. I know the feeling my body goes through, I know the timeframes before my ICD will attempt to treat an arrhythmia, and I know that calming myself down does not prevent me from going into cardiac arrest. The experiences from those 9 cardiac arrests have literally dictated how I live my life, I have avoided that feeling for 4 years by listening to my body (a little too much sometimes). I know what my body “sounds” like before an arrhythmia, I know my heart’s limits, and I stop myself from reaching that limit to avoid potential death. Simple.
 Jamie Poole
Jamie Poole
It’s Scarier Not to Die by
For the first time in 12 years, I experienced my first incident of an inappropriate shock. Not just one, but five, one after the other.
Bang.
Bang.
So with that decade of experience in mind — I was frustrated when the cardiology team paid so little credit to the fact that I felt these exact feelings the minutes before I was shocked “inappropriately”. I’m not a “noob” at this, this is almost a regular Wednesday at this point, and I knew that my heart rate was accelerating and I wasn’t in the driver seat anymore. While it may look like a normal ST rhythm on an ECG, I somehow knew a shock was coming.
After my last cardiac arrest, the nurse responsible for monitoring the ECG summed it up perfectly when she said to another doctor, “It’s weird, he knew it was coming before
www.myheart.org.uk 13
myheartmystory
the ECG picked anything up”. If it was inappropriate, how did I know it was coming?
While the fact is the read-out showed a steady incline that appeared to be ST, I had stopped all activity before it shocked me.
I was literally waiting for it, standing in the doorway to my room. While the cardiology team explain the inappropriateness away as “during mildexercise”, I wasn’t. I wasn’t halfway through making my bed and, “Bang it shocked me”.
No, I felt my heart rate accelerate, I stopped, and stood still for a couple of minutes, as I always do. Again, while it may look like ST on paper — when it did not decelerate when I stopped, warning bells rang in my head.
But what do I know. I don’t know the ins and outs of cardiology and I don’t know exactly how much information my ICD gives doctors post-events. Any reasonable person would have to trust the judgement of cardiologists and electro-physiologists who looked at my case that night. They are the experts at this, and I am obviously not the first patient they’ve had with inappropriate shocks. Which leads to the first of two reasons why it’s scarier not to die.
Reason number 1 why “It’s Scarier Not to Die”
For 12 years, I was gaining quite a lot of confidence in my ability to pick up these changes in my body and stop myself before they escalated into anything serious. I have now gone through my longest period of “not dying”. My last cardiac arrest was in May 2017 and I attribute that to my strict adherence to what I thought my body was telling me. If I was so wrong this time, if despite what I heard my body say it was still only inappropriate, can I trust any of my experiences so far? Are those “warning signs” real, or have I just been correlating mixed feelings to an event that are actually unrelated?
In this respect, I almost wish I did “die”. I wish it was a cardiac arrest, then at least I know that my brain’s defences worked and picked up the feeling before it happened, although I didn’t stop it, I would at least know that my “system” still works. Now I don’t know if it does anymore.
And this has hit me hard. For the last three weeks since the shocks, I have not been able to trust any of my body’s
feelings. I can’t bend over, I can’t pick things up, I can’t brush my teeth, I can’t take the trash out. The moment my body feels different, I have lost all confidence that I am able to determine what is an “okay signal” from my heart versus one that might lead to me getting shocked. My usual way of dealing with the aftermath of a cardiac arrest has been completely thrown out of whack, and I don’t know how to get back to normal.
Reason number 2 why it’s “Scarier Not to Die”
A nurse once told me as she pushed me out of hospital in a wheelchair after one of my cardiac arrests, “you know it’s not going to work every time, right?”. I’ve always known ICD’s aren’t perfect. They fail, they make mistakes, and they can misread the situation. My ICD made that painfully clear.

I’m not going to pretend I pushed the limits of my ICD’s tolerance of its designated monitor and “shock” zone. It was previously set to shock at 158bpm, and yet I don’t think I ever raised my heart rate over 100bpm (until apparently this night) in the 4 years since my last cardiac arrest. But assuming this was an “inappropriate” shock, this event reminded me that even when everything is apparently going fine, I still might have to experience the pain of acute electrocution again.
Now that I know for sure my device could shock me inappropriately, how am I supposed to let me heart rate accelerate ever again? If I was cautious before, I’m about to become extremely involved in the decision process for every movement I make.
A cardiac arrest is almost a relief in a way — “Hey, it wasn’t your fault. You have hypertrophic cardiomyopathy and you went into an arrhythmia. There’s nothing you could have done to prevent it.” There is solace knowing that even if I try my best, whether or not I go into an arrhythmia is largely out of my control. It’s going to happen whether I want it to or not.
An inappropriate shock is different, it was in my control. It was my “fault” I got shocked. It was my “fault” I just experienced the most painful and terrifying experience in my life. I should have stopped myself. I should have known better. I should have prevented putting myself in a situation that would lead to a shock.
And so, if my ignorance, forgetfulness, or complacency can lead to a shock, how am I ever supposed to play it cool now? That has literally been how I deal emotionally with my cardiac arrests in the past. I ignore it, I do my best to forget it ever happened, and I move on like nothing changed. I can’t do that now. I now need to emotionally deal with this issue. And that’s something I’m not prepared for.
I am in uncharted waters right now. In a lot of ways, I just
myheart newsletter 2021 14
Jamie in hospital
had my “first” shock all over again. I am not prepared mentally or physically to deal with this new “threat.” I don’t know what to do.
As any of you that have known me, or seen me on social media or publicly, my reaction thus far has been to laugh it off, to treat it as a joke, to lock away the memories and feelings in a box down the deepest parts of my brain and throw away the key. It’s a strategy that seems to have worked, and has allowed me to travel, to play, and to experience things otherwise not advised of a heart failure patient. I’ve had a great time dealing with it this way. But I don’t know if I can do that anymore.
Things will need to change, and that’s scary.
Every Cloud by Thomas Flanighan
After serving nine years in the military as a Royal Marines Commando, I needed a new challenge and started striving towards a career as a commercial pilot. The flying medical involved an ECG which showed abnormal results. At the time, I was not concerned as the doctor who performed it was almost certain it was ‘Athletic Heart’. They asked me to attend my GP practice at my convenience. Afterwards, I was referred for an echocardiogram. Once completed they wrote back to the medical centre to inform them that there was a strong suspicion of hypertrophic cardiomyopathy (HCM).
I was referred for a cardiac MRI which would confirm or dispute diagnosis of potential HCM. This was to enable me to fly without restrictions. The cardiac MRI was performed, which later confirmed diagnosis of HCM.
After discussing the condition with my consultant, it was advised I keep my BP and HR low and do not exert myself as this could cause an onset of symptoms (blackouts, palpitations, chest pain). I have been working within these parameters and think this has been helpful for me to remain fit and healthy but to still exercise and stay symptom free.
On the day of my diagnosis, me and my fiancé were driving to our home in Northumberland. This sounds very cliche but there was a huge black cloud over the sky at London

myheartmystory
Heathrow with the most prominent silver lining. At the time, I thought this was the end of a potential career in aviation. I found the news incredibly hard to stomach since I was completely asymptomatic and in the prime of my career. I had invested so much time and money into pursuing a newfound passion for flying.

After extensive cardiology testing, I was assessed fit to train as a pilot. 12 months later, I am in the final stages of my training.
This process has showed me that goal setting is key (no matter how small) and to truly believe in yourself. My diagnosis has shown me that a positive attitude and cheerfulness in adversity can overcome a seemingly negative situation. There is a huge amount of support available from charities for those who need it.
It is incredibly important to me to share my story. Even though my career in HM Armed Forces is understandably ending, this condition does not put a stop to a second professional career. Remember, the black cloud will disperse, and the sun will shine again.

Life with LQTS and LVNC
by Abi Edwards
October 2018, aged 14 and asymptomatic – I was taken to a CRY screening as a precautionary check by my mum at St George’s Hospital. Little did I know that that test would be the beginning of a whole new journey in my life. I was told that they had picked up an abnormality and they thought it would be LQTS, something I had never heard of nor had I expected when I went in for the screening. I was then referred to the Royal Brompton for further tests such as ECGs and echos and it was confirmed that I had LQTS. I was then prescribed Bisoprolol and continuous check-ups at the Brompton.
Following an MRI around a year later, I was found to have
www.myheart.org.uk 15
myheartmystory
Left-Ventricular non-compaction alongside the LQTS. This meant that I was now under two clinics at the Brompton, Cardiology and Cardiomyopathy, both of which were incredibly supportive.
My worries further expanded when I discovered other family members had the LQT gene but it didn’t present itself. While this made me feel more alienated as I felt like it was only me who had these conditions, I was determined not to let it beat me and I continued taking it in my stride and accepting the new journey my life had taken me onto.
Whilst both of these came as a huge shock to me, I understood that this was how things were going to be and I learnt to take it in my stride and make the most of what I can do rather than what my conditions prevent me from doing.
Also, being so young when diagnosed, I was eager to understand more about cardiac conditions, particularly my own, and so I turned to CRY and the myheart network to use the resources they provided to both cope and learn about my conditions.
My life will never be the same as it used to be and I may have extra precautions than the average person. However, this is what makes me me, and I am using my own experiences to help others going through something similar as I know first-hand how daunting it can be.
CRY has saved my life and I could never be more grateful. This is why I took part in the 2019 Heart of London Bridges Walk to fund raise for CRY and see just how many people they have also had an impact on – this in particular made me realise I am not alone.


I am looking forward to a bright future and even further acceptance and understanding of my conditions. For everyone with cardiac conditions, we are not alone.
by
Since being diagnosed with my heart condition at 16 years old, I’ve been trying to understand my body, to understand my limitations and capabilities.
That has stemmed into my life in many ways, particularly when it comes to challenging my body and perceptions of what makes a healthy lifestyle. It has led to me running long distance in a way that is monitored, controlled and measured.
Now for the first time, I’ve been signed off to run long distance competitively. Which is why I’m using this opportunity to raise awareness about undiagnosed heart conditions and talk about my journey.
This process has involved 10 years of training in long distance running, resulting in me having a resting heart rate of around 45 beats per minute, which according to professionals, is an athletic pace.
When I was first diagnosed it felt like my world caved in. My condition has many caveats that I have to be aware of such as the dangers of normal prescription drugs and sports such as swimming and high impact activities. To be told you’re at risk of cardiac arrest is daunting but the thought of not knowing I am at risk is terrifying.
I have an inherited condition called Long QT syndrome which is an electrical fault within my heart. This means that my heart takes longer to recover in between beats, meaning that if my heart contracts before it’s recovered from the previous beat, I could be at risk of collapsing or even sudden death.
Being diagnosed with a heart condition however, is not the end of the world. I feel it allows me to live my life in full knowledge of my potential and my limitations. That knowledge I’ll be forever grateful for, as I know many families who didn’t know and sadly had fatal outcomes from undiagnosed heart conditions.
It should not take a tragedy to realise our vulnerabilities. In knowledge of such weaknesses, we gain strength.
I want others to be confident in their own skin and surpass expectations, while being aware of underlying conditions in sport, whatever sport that may be.
myheart newsletter 2021 16
I have a heart condition but it’s not the end of the world!
Gem O’Reilly
Abi at the 2019 CRY Heart of London Bridges Walk
CRY Research Fellow Dr Raghav Bhatia’s primary research interests include evaluating the role and efficacy of cardiovascular screening in individuals aged 14-35, which incorporates the challenges and opportunities catalysed by the COVID-19 pandemic.

Earlier on in the pandemic, Dr Bhatia led on consensus recommendations, aimed at providing practical answers to pertinent questions being posed by the sporting community around safe participation in exercise.
The recommendations were endorsed by the European Association of Preventive Cardiology (EAPC) and widely adopted and utilised by sporting bodies which included the Rugby Football Union (RFU), English Institute of Sport (EIS), and the English Football Association (FA). A twinned review (“The Impact of COVID-19 on the Continuity of Cardiovascular Care.” Bhatia RT, Gati S, Papadakis M, Sharma S. Eur Heart J. 2021) provided an overview of the challenges posed by the pandemic on cardiovascular services, whilst suggesting potential solutions based on current models of care.
With the above in mind, Dr Bhatia joined us in conversation to discuss all things COVID-19 related.
What are the main ways COVID-19 has impacted people with cardiovascular conditions?
Whilst COVID-19 can be contracted by all individuals, multiple studies have demonstrated that individuals with established cardiovascular disease, and those with risk factors such as diabetes mellitus, hypertension and obesity, are associated with an increased morbidity and mortality. Case fatality is also higher in older age groups, with the highest mortality in those aged ≥80 years in whom mortality is six times higher than in younger patients. Furthermore, patients with heart failure have significantly poorer outcomes including in-hospital complications.
What are your current research interests, specifically around COVID-19?
Firstly, in my capacity as a Research Fellow I am grateful to the families and supporters who fund our screening events and research. It is with this support that I am currently working on two large scale projects which 1) address the impact of COVID-19 infection in young individuals aged 14-35, who attend our screening events and 2) outcomes of cardiac screening in athletes following
COVID-19 infection. Overall, we aim to address current knowledge gaps around the epidemiological aspects of the disease and impact on individuals who engage in regular physical activity, as well as enhance our understanding around the optimal screening strategies.
How much do you think the increased use of remote technology during the pandemic can help us moving forward with new remote care for people with cardiovascular conditions?
Largely due to necessity, aspects of e-health, which includes utilising information technology and communication technology to aid patient care, have been broadly adopted by healthcare systems. Telemedicine has been responsible for the buoyancy in maintaining outpatient services through virtual consultations.
Meanwhile, mobile applications and wearable technologies continue to empower patients in their management. For example, cardiac rehabilitation services, which have traditionally been delivered in a hospital setting, saw an effective shift towards home-based cardiac rehabilitation.
Whilst the pandemic has accelerated the utilisation of remote technologies, it has emphasised the importance of 1) risk stratifying patient groups in whom more traditional models of care with face-to-face encounters would provide safer and more effective care; 2) comparing clinical outcomes in specific patient groups using different models of care; 3) evaluating patient experiences where remote care has been delivered; and 4) ensuring adequate infrastructure, training, and investment.
Specifically, with reference to our CRY screening programme, we are evaluating the potential incorporation of remote technologies in tandem to our nationwide mobile screening units. This takes into account potential logistical issues such as connectivity, evaluation of licensed platforms, technologies for ECG acquisition, and most importantly governance.
Online meetings and conferences have been used more than ever through the pandemic as well. How could this continue and help us with education in the future?
The online shift in medical education has been positively received by colleagues. However, we do miss the interaction and networking opportunities from in person meetings!
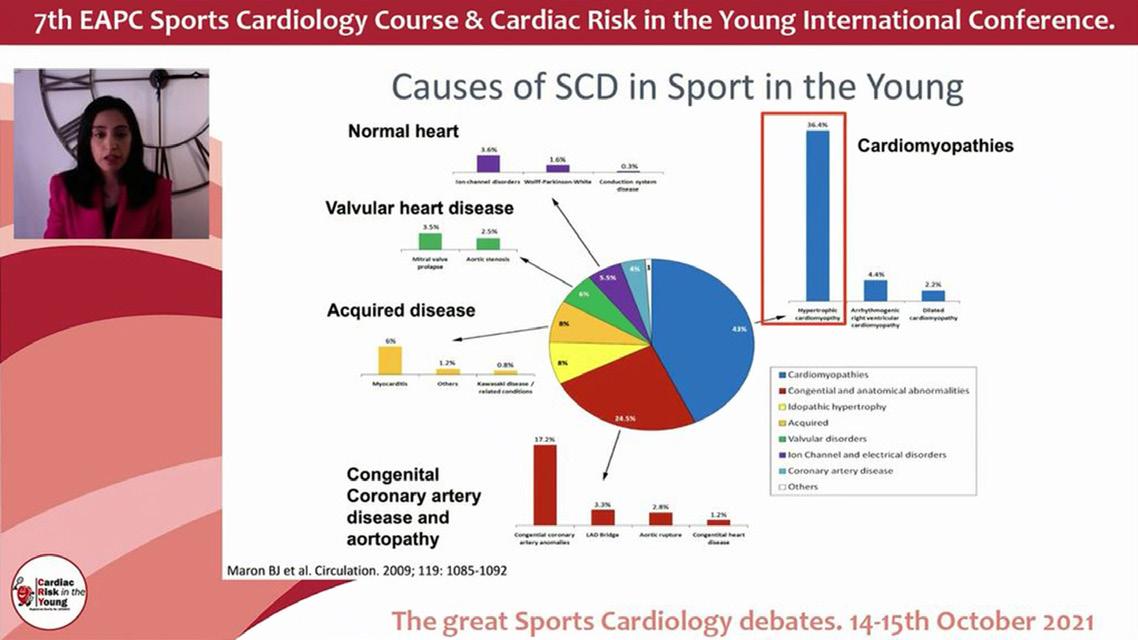
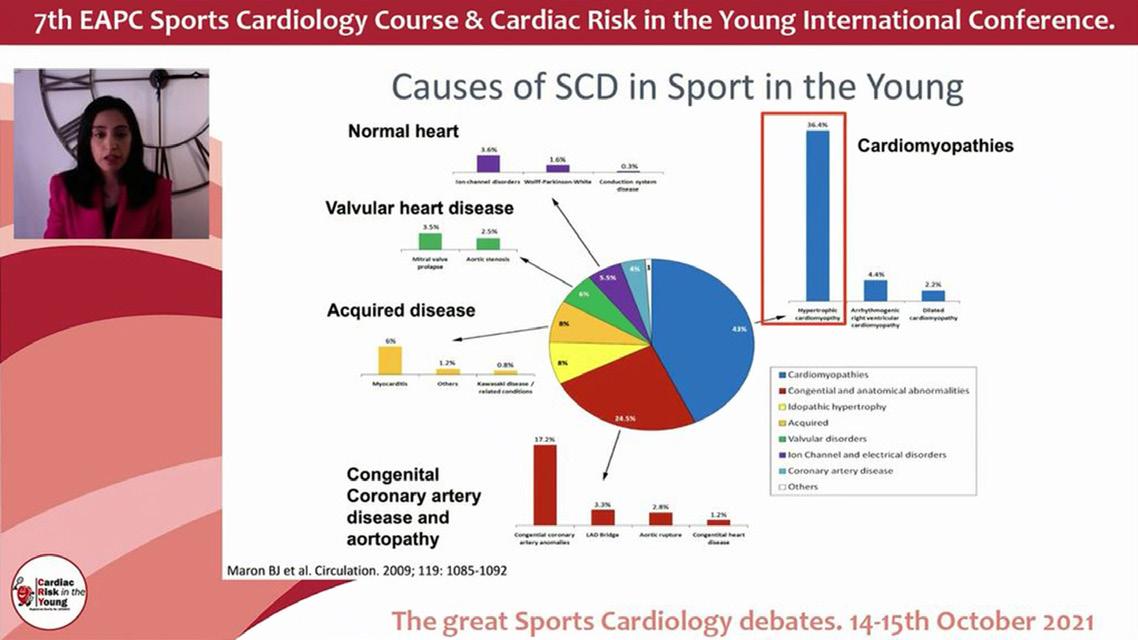
We recently held the 7th EAPC Sports Cardiology Course & CRY International Conference virtually in liaison with Wondr Medical, over two afternoon sessions. 242 delegates joined us from over 30 countries, with attendees spanning a broad range of medical specialities.
www.myheart.org.uk 17
CRY Research
CRY Research
Due to the ongoing COVID-19 pandemic, the CRY Conference was moved online again for 2021. On October 14 and 15, the conference was hosted in partnership by CRY and the European Association of Preventive Cardiology (EAPC). We were thrilled to welcome leading experts in cardiology from around the globe for presentations, discussion of case-based scenarios, and interactive debates for the audience to follow and engage with online.
The first debate of Day 1 was “Athlete with an ICD; No way back to competition?” This was led by Andre La Gerche, a cardiologist and researcher at the Baker Heart and Diabetes Institute in Melbourne, Australia, who presented a case of whether an athlete should be allowed to return to competition. The athlete in this case was an elite 26-year old Australian Rules Footballer, who had previously been well with no family history of any medical problems. He collapsed during a match and after getting up was immediately taken to hospital. In the presentation, Professor La Gerche went on to show some of the tests the athlete went through. It was established that the athlete had no other symptoms before or after the incident, and he went on to have a subcutaneous implantable cardiac defibrillator.

Professor Rachel Lampert from Yale Medical Center joined to argue the case against the athlete returning to sport, while CRY Consultant Cardiologist Professor Sharma presented the case that the athlete could resume competing.
Silvia Castelletti from the Cardiomyopathy Unit and Center for Cardiac Arrhythmias of Genetic Origin, Milan, Italy followed to present the case against the athlete returning to competitive sport. Dr Castelletti presented more data and outlined some of the arguments against, such as how participating in sport can lead to a further prolonged QT which can correlate with the increased risk of a cardiac event occurring.
After a Q&A session with questions from audience members, the second session of the day got underway. This session included three different cases. Firstly, Dr Harald T. Jørstad began with “Veteran athlete with atrial fibrillation; pit stop or steady on?” The case looked at a 39-year-old man who is a former professional football player with atrial fibrillation. The former footballer contacted a clinic one morning to say that he had atrial fibrillation the night before and took his medication (flecainide). Now that he was feeling fine, he asked if it would be safe for him to play in a football match later that day. Dr Jørstad went on to discuss atrial fibrillation in more detail and how this case could be dealt with.
The second debate of the day was entitled “Athlete with LQTS and prolonged QT interval; Treat and release.” This case looked at an 18-year-old competitive swimmer with long QT, who had a syncope spell two years ago and whose mother had a syncope spell while skiing, meaning there was family history to consider. The swimmer underwent a variety of tests. After 83% of the audience voted to say the athlete should not return to competitive sport, the debate began.

Professor Elijah Behr had the task of convincing the audience otherwise, making the case that the athlete could be treated and return to sport. After discussing various data, Professor Behr concluded with a few key points, including that athletes have longer QT intervals, many with QT prolongation do not have long QT syndrome, and there is no evidence of higher risk attributable to the additional QT prolongation of athletes. In fact, most patients are low risk, Professor Behr added. Dr
Next, Dr Michael Papadakis from St George’s University, London, looked at a case of an athlete with pre-excitation. In this instance, a 16-year-old sportswoman who attended a CRY screening. Her exercise regimen involves 13 hours of training per week, including competing in swimming and netball at county level. She reported some shortness of breath from exertion which had been attributed to hay fever, and she had no family history of concern. Dr Papadakis then looked at the ECG of the athlete to ask the audience what it showed, and discussed what tests could be done next.
For the third and final case of Day One, Dr Alessandro Zorzi from the Department of Cardiac, Thoracic and Vascular Sciences and Public Health at the University of Padova, Italy joined to give a presentation, entitled “Athlete with ventricular ectopy: it is a family thing.” Dr Zorzi looked at four members of a family who were referred to his cardiac clinic for evaluation. He explained their various symptoms, looked

myheart newsletter 2021 18
at their ECG results, and discussed what further testing or treatment they may need. To bring Day One to a close, Dr Papadakis hosted The Great ECG Quiz.
The first session of Day Two got started with a talk from Professor Martin Halle, examining the case of a 52-year-old male who suffered a non-ST-elevation myocardial infarction. In the three months since, the man underwent cardiac rehabilitation with moderate intensity exercise three to four times per week and had no symptoms. Before his acute myocardial infarction, though, he was more active – he went jogging for 45-60 minutes five times a week and took part in several half marathons and marathons, and wanted to return to a similar level of physical activity. So, Professor Halle discussed some of the testing the patient had and asked the question whether participation in high-volume sports, such as a marathon, could be recommended.
Dr Meagan M. Wasfy from the Cardiovascular Performance Program at the Massachusetts General Hospital in Boston, USA argued the case for the runner to return to this kind of sport. Dr Wasfy did say that personally she would not recommend training for a marathon, but did look at why cases need to be individualised and consider the goals of the patient. To counter, Professor Mats Börjesson argued why the runner should not return to such significant levels of sport.
The next case, presented by Professor Antonio Pelliccia, looked at a 43-year-old male football player with no symptoms or family history. The only finding with the footballer was abnormalities on his ECG, including markedly increased voltages. After Professor Pelliccia explained the footballer’s test results and low risk score, former CRY Research Fellow Dr Sabiha Gati from the Royal Brompton Hospital argued the case for a return to sport. Dr Gati closed with a few key arguments, such as how moderate exercise reduces cardiac risk factors and improves fitness, and how a sedentary lifestyle can have detrimental effects on people including those with hypertrophic cardiomyopathy.
To conclude, Dr Jonathan Drezner gave his presentation to make the argument against the footballer returning to play. Dr Drezner looked at a few key points, such as how exercise can be safer for older patients with HCM but not necessarily younger patients, and that restricting participation in sports can reduce the risk of SCD. The session finished with a Q&A and discussion amongst the panel of experts.
The second and final session of Day Two began with a case presented by Dr Guido Claessen, “Athlete with dilated LV and reduced/borderline LVEF.” The athlete in this case was
a 23-year-old elite runner who had reported some atypical chest pain when in a resting state. His clinical examination was normal, he had no personal medical history and takes no medication. There was some family history, though, as his father was a runner who was diagnosed with dilated cardiomyopathy at 44 years old. Dr Claessen discussed the testing the runner underwent and the panel of experts weighed in on the findings.
The next case of the session was presented by Dr Elena Cavarretta from Sapienza University of Rome, Italy on “An athlete with mitral valve prolapse.” Dr Cavarretta looked at the case of a 40-year-old competitive triathlete diagnosed with mitral valve prolapse, and discussed his condition and to what degree he should be able to participate in sports. The final presentation of the conference was given by CRY Research Fellow Dr Raghav Bhatia. Dr Bhatia’s case looked at a 20-year-old semi-professional cricketer after being infected with COVID-19. The cricketer was typically fit and well but went to his local Accident and Emergency department after having a two-day history of chest pains and a few other symptoms. The athlete had received two doses of the PfizerBioNTech vaccine and had mild illness with COVID a week after his first dose. Dr Bhatia looked at how to diagnose the athlete and how long they may need to wait before returning to sport, along with discussion from the expert panel.
The 2021 CRY Conference featured so many brilliant presentations and we are grateful to all the experts who took part. We would also like to thank all of our sponsors for the conference, as well as Wondr Medical, our digital partner who streamed the event.

It is important that anyone with a cardiac condition speaks with their own cardiologist for individualised advice about an exercise plan.

www.myheart.org.uk 19
CRY Research
Have you been diagnosed with a heart condition when you thought you were fit and healthy?
We understand that being young and suddenly finding that you need to be treated for a heart condition is not easy. CRY’s myheart network provides personalised help, support and information to individuals who have been diagnosed with a life–threatening cardiac condition.
myheart is a support system for individuals to help develop effective coping strategies and reduce social isolation. The network was developed in response to feedback from young people who found that support groups available were not effective in helping them deal with issues such as fitting of ICDs and pacemakers, and undergoing ablation surgery.
myheart offers:
• Medical information about different cardiac conditions, tests and treatments.
• Personal stories/videos from other young people who have been diagnosed with a cardiac condition.
• Videos from our cardiologists answering frequently asked questions.

• A private area of the website for members aged 16–35 which features a members’ blogging area.
• Meetings for people aged 18–35 who have had a cardiac arrest; have been diagnosed with an inherited cardiac condition; have an ICD; or have been offered an ICD.
• A private Facebook group for anyone over the age of 18 who has been diagnosed with an inherited cardiac condition.


How to get involved
This
How to join myheart
Email: myheart@c-r-y.org.uk Online: www.myheart.org.uk Telephone: 01737 363222
(Please ask for the myheart coordinator) Post: FAO myheart Cardiac Risk in the Young Unit 1140B The Axis Centre Cleeve Road Leatherhead KT22 7RD
Young, fit and suddenly diagnosed with a life-threatening heart condition
This booklet – with an introduction from double Olympic gold medallist Tom James MBE, who was diagnosed with a heart condition known as atrial fibrillation in the run up to the London 2012 games – features 10 personal essays from young men and women who recount and talk through their own experience of suddenly being diagnosed with a heart condition. The booklet is for and by the growing number of young people who –thanks to greater awareness and early diagnosis – are learning to live with a diagnosis of a potentially life-threatening heart condition.
Tel: 01737 363222 Email: myheart@c-r-y.org.uk
Website: www.myheart.org.uk
is your newsletter – we would like to include your stories and photos. If you have been diagnosed with a cardiac condition and would like to share your story, thoughts and experiences with others, please send in your stories to myheart@c-r-y.org.uk.
@myheart_UK myheartnetwork myheart


























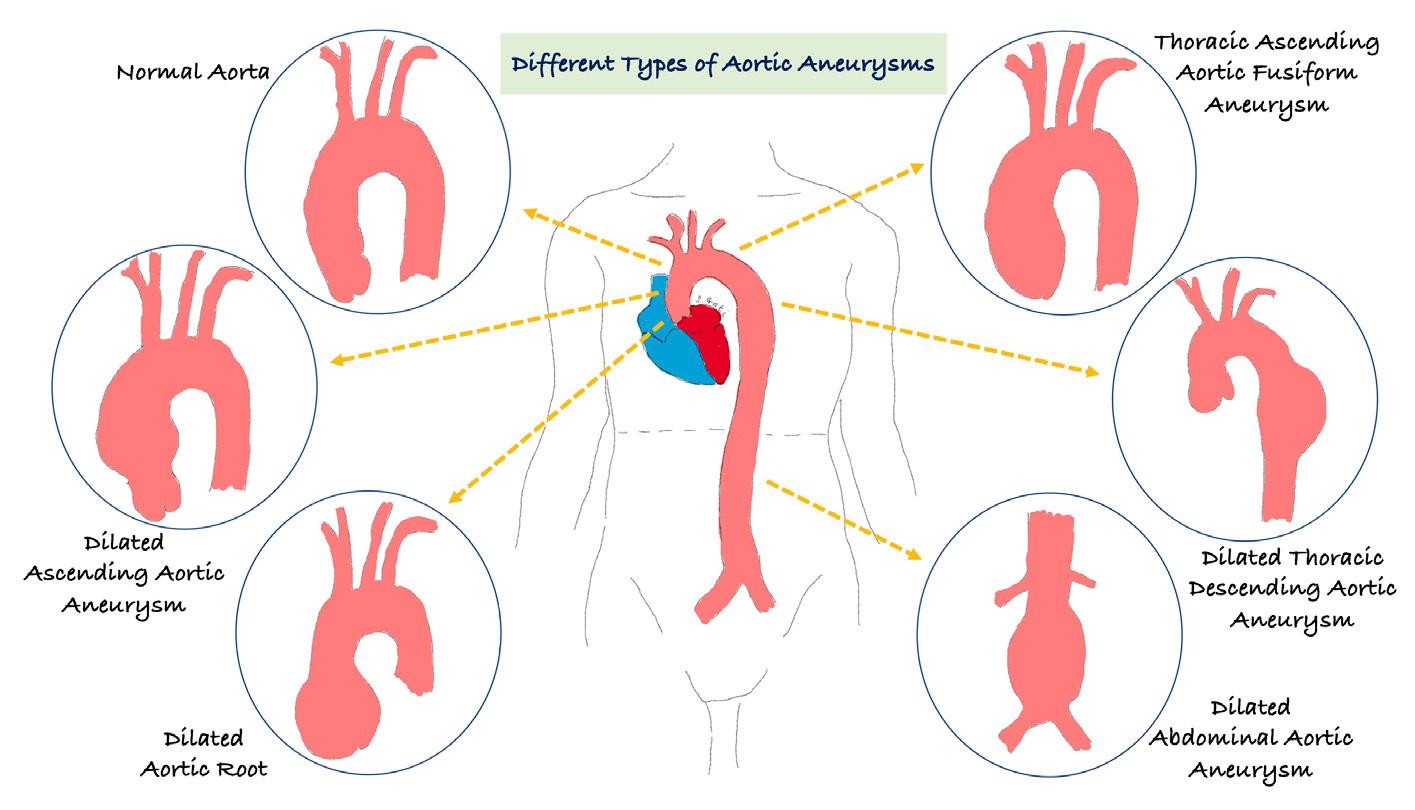







 Jamie Poole
Jamie Poole