






















Welcome
News and Latest Updates

myheartmystory
CRY’s Medical Conference
CRY Upcoming Events and how to get involved
myheart Resources
We are delighted to present to you the newsletter for 2023 which is a round-up of myheart news and events from 2022. Throughout the year myheart continued to offer support to young people who have been diagnosed with a cardiac condition by holding online support meetings and sharing new content by CRY cardiologists and myheart members.
For more details regarding the events shown on the cover, please turn to the corresponding page references below. Images are listed in rows from the top left:
myheart is now providing personalised support to nearly 680 members. We would like to extend our thanks to all of you for your continued support, whether in terms of fundraising, sharing social media posts, sharing your stories on the website, or writing to your MP. Read about ways to raise awareness of CRY’s work here: AwarenessCardiac Risk in the Young (www.c-r-y.org.uk).
This newsletter includes personal stories shared by some of our members in 2022. We have received feedback about how impactful it is to read stories of others who have been diagnosed with a cardiac condition. We are very grateful when any of our members share their stories with us on the myheart website, as peer-to-peer support and shared experiences can help people to feel less alone. We also welcome vlogs.
Also contained in this newsletter is information on myheart meetings and how you can volunteer at CRY events.
As the coordinator of CRY’s support group, it is my responsibility to put this newsletter together and it is my endeavour to get you all the news and event stories relating to members accurately.
Head Office:
Unit 1140B


The Axis Centre
Cleeve Road
Leatherhead
KT22 7RD
No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means; electronic, mechanical, photocopying, recording or otherwise, without prior permission of Cardiac Risk in the Young (CRY). CRY welcomes all content for the newsletter but reserve the right to edit when necessary and to withhold publication. Any opinion or statement by the author of any article or letter published does not necessarily represent the opinion of Cardiac Risk in the Young (CRY). Articles pertaining to health-related topics are for information only. Readers should obtain advice from their own practitioner before attempting to diagnose or administer any medication. Mention of any products or procedure should not be considered an endorsement for said product or procedure.
Please do not hesitate to contact me by emailing me at myheart@c-r-y.org.uk or by calling me at 01737 363222 if you find anything amiss or if you have any views to improve our support network. Thank you for your help!

Cardiovascular disease affects us all. And together we want to make a big impact. Our activity will focus on:
1. AWARENESS – getting CPR and Defibrillator training to as many people as possible so everyone can learn the skills to save a life
2. EXERCISE – getting people moving and understanding the simple changes they can make in their lives to improve their cardiac health
3. SCREENING – preventing young sudden cardiac deaths through additional screenings
4. RESEARCH – raising money for funding innovative treatment, equipment and research into cardiac health
The Heart of West London partnership is a group of organisations working together to change the game for heart health.
The partnership is made up of Brentford FC, Brentford FC Community Sports Trust, Royal Brompton and Harefield Hospitals Charity, Cardiac Risk in the Young (CRY), Resuscitation Council UK, Pablo London and A-K-A Day.

Together the partnership hopes to raise awareness of game-changing research and drive forward our knowledge of cardiovascular disease to discover more effective treatments, and drive education and training within our local communities.
Dr Steven Cox, CRY CEO says, “The launch of the Heart of West London partnership coincides with an important milestone for CRY – the announcement that we have now tested over 250,000 young people in the UK, through our screening programme. As a result, more than 800 young people will have been identified with potentially life-threatening cardiac conditions and will have received treatment, lifestyle advice or corrective surgery which will have dramatically reduced their chance of suffering a cardiac arrest. This partnership will help to raise awareness of the importance of screening and young lives will be saved.
“But we know screening is not perfect and will not identify everyone at risk, and that is why it is essential that every person, young and old, knows how to carry out CPR. Every person should be confident to help when they witness a person suffering a cardiac arrest. Every second is vital and with a bit of knowledge every person has the potential to be a lifesaver.
“We are so pleased to be part of this initiative which is going to raise awareness of screening, raise awareness of how to do CPR and raise vital funds for the crucial research which will save so many lives”.
5. SUPPORT – supporting families affected by cardiac conditions
Former player and manager at Brentford FC, Andy Scott became a Patron of CRY following his own diagnosis with an underlying heart condition, which led to his retirement from the pitch in 2005. Having played for the Club back in the late 90s, Andy returned to the Club on two separate contracts (2007 and again in 2015) as part of its management / talent scout team.
In 2007, Tom Clabburn died of a heart condition aged just 14. Tom was a local schoolboy and Brentford fan and, in June 2009, with the assistance of Andy Scott, his family helped facilitate the final screening in CRY’s pioneering UK-wide ‘testmyheart’ tour at Brentford’s old Griffin Park ground. Since then, the family have continued to campaign tirelessly and to sponsor yearly free CRY heart screenings for young people living in the Brentford / Ealing area.
In November 2018 Rob Rowan tragically died at the age of 28. Rob had been with Brentford FC for many years and had just earlier in the year been promoted to Technical Director. His death had a tremendous impact across football. Since Rob’s death the club have gone to great lengths to help raise awareness of cardiac conditions in young people as well as support his wife Suzanne, Rob’s friends and colleagues to raise funds to screen young people in the local community.
At the end of April 2022, Christian Eriksen and the club’s manager Thomas Frank, attended one of CRY’s screening events which Suzanne had organised in memory of Rob, at Gunnersbury Park Sports Hub. Watch the video here.
We are so grateful to everyone involved with Brentford FC for their incredible support, and all they have done for CRY.
CRY has received a number of updates from CredibleMeds throughout the year. Members with cardiac conditions may like to consider registering with CredibleMeds to be kept up to date with any changes to the QT drugs to avoid list https://crediblemeds.org/everyone/

be a Patron of CRY. CRY has shaped me so much in what I do now in the charity sector, because in 2010, when I did the London Marathon again, I did it in 26 hours. And for one of those miles I was joined by young ambassadors and families and friends of CRY to raise awareness. It was through that experience that I really started to understand what I wanted to do going forward, with a new life with a disability. It’s an absolute honour to be a Patron of CRY.”
“Thank you very much indeed for inviting me today,” Phil said as he ended his speech. “It really is a joy to be here and I know how special a day it is and I can really feel that, and I have done on the times that I’ve been here before. So thank you very much and have a fantastic walk today.”
Next, CRY Chief Executive Dr Steve Cox gave our final speech of the morning. He began by thanking everyone who helped make the day possible, from volunteers and participants to food vendors, before highlighting the importance of the event, CRY’s screening programme and research.
“We are always humbled to see the incredible lengths you all go to, to raise awareness and fundraise in your local communities. The way in which communities come together is truly amazing, and it’s been what has taken CRY from where we started in 1995 to where we are today,” Dr Cox said.
After the speeches, we held a minute’s silence.
Over the last two years, many CRY events have gone virtual due to the pandemic. This has included the CRY Heart of London Bridges Walk, with supporters completing walks in their local communities around the country rather than all gathering together as normal.

On 26 June 2022, we were so pleased to be able to return to London for the 16th anniversary of this special event.
For the first time in 2019, we moved the Heart of London Bridges Walk to a new starting venue at Southwark Park and returned in 2022. Walkers began arriving in the park from 9am and gathered around the band stand, connected with other participants, and uploaded their messages and photos to our message wall screen. A total of 709 walkers came to take part.
Once walkers had arrived, CRY Patron Phil Packer MBE began our speeches.
“I just wanted to share a little bit of why it’s such an impact for me to be a Patron when my life hasn’t been affected by cardiac risk in the young,” Phil said to open his speech. “In 2009, I did the London Marathon, after I sustained spinal cord injuries, over 14 days, and after that I was asked to
Then at 11am, it was time for the walk to begin. As always, our 5-mile route went past many of London’s iconic landmarks. This included Tower Bridge, the Tower of London, The Gherkin, St Paul’s Cathedral, Shakespeare’s Globe, and The Shard. We also introduced a new quiz to test our walkers along the route with some London trivia.
After making their way through the heart of London, walkers headed back to Southwark Park for the CRY Family Picnic. Back at the park, there was delicious food and drink on offer from 75 Slices, Bratwurst Bros, Chocolate Balloons, and Smokin’ Bean Coffee Truck. As everyone spent time with other walkers, there was also a performance from the Nunhead Community Choir to enjoy.
Meanwhile, many CRY supporters who wanted to take part in their own local areas or could not make it to London completed their own walking routes around the country. 117

We are so grateful to our supporters who offer up their time. From being an official CRY ‘cheerer’ at a mass participation event, helping to marshal the route at the CRY Heart of London Bridges Walk, holding an awareness stall, sharing our key messages on social media, to volunteering at a UK festival – there are lots of opportunities to get involved by volunteering!
Events volunteering – Providing your help on-site at any of our events is a great way to get into the action of our fast-paced busy events! Our events include Simplyhealth Great North Run, Virgin Money London Marathon, Heart of London Bridges Walk and more!

people completed the My Walk for CRY, which is a great way to be involved on the day and raise awareness locally.

The CRY Heart of London Bridges Walk is always an emotional day. It was so special for everyone to gather together, especially after not being able to make it to London for two years due to the pandemic. Thank you to all of our supporters who took part, whether you completed your My Walk For CRY or came to the main event.
Thank you to our fantastic team of volunteers as well. Events like this are only possible because of your help!
CRY’s volunteers were: Krisztina Cserhalmi, Jenny Boag, Rochelle Burrows, Julie and Michael Essex, Caroline and Peter Gard, Rachel Groom, Wendy and Phil Harrington, Sam Helm, Jo and Nick Hudson, Jim and Barbara Holland, Kelvin Holt, Victoria Joy, Jasmine Lambert, Cyril Molony, Tim Munyanyi, Bill and Rosie Taylor, Dai Taylor, Vicky and Aaron Walker, Paul Ward, Toby Ward, Lucy Wasdell-Bowyer, Matt Wilson, India Woodward, Rebecca Zouvani, Ciara Lucas, Lizzie Peers, Ruth Moore and Larissa from Lari Yoga who led a yoga class at park in the afternoon.
And finally, thank you to our sponsors ServiceMaster Clean, Chubb, and Saputo Dairy UK.
Volunteering in your local community – Volunteering in your local community is extremely beneficial in raising awareness of the important work that CRY does.
Raising Awareness – Help promote CRY by distributing CRY general information leaflets/collection pots at your workplace, local school, leisure centre or in theatres, pubs, shops, doctors and pharmacies.
Social media – Follow myheart on Twitter and Facebook. By sharing any of our messages you are helping to raise awareness. Some members also help to raise awareness by sharing their own stories, including #myheartmystory
In-office volunteering – Our CRY in-office volunteers take on a range of practical and administrative tasks. We have limited space but are always grateful for an extra pair of hands in the office!
If you would be interested in volunteering some of your time for CRY, please fill out the from on our website and the fundraising team will be in touch: www.c-r-y.org.uk/ volunteer-registration-form/
Online myheart meeting: March 17, 2022

Given the complexity of some conditions we recognise that there will always be a need to consider some cases on an individual basis.
Meetings are free to attend and give members an opportunity to meet and discuss their experiences in an informal but supportive environment. Those young people that attend these meetings usually find them very helpful. It does not matter how long ago you first received your diagnosis or whether you are undergoing any sort of treatment at the moment.

For more information about myheart meetings, including upcoming dates, please visit www.myheart.org.uk/ meetings/.
A myheart members’ Zoom meeting was held on Thursday 17th March, 2022. There was a Q and A session with cardiologist Dr Sabiha Gati in response to queries and concerns that members had relating to their heart condition and the pandemic.
Online myheart meeting: October 1, 2022
The myheart website contains information on cardiac conditions, tests, and treatments. Recently, information on two more cardiac conditions, Right Bundle Branch Block (RBBB) and Patent Foramen Ovale (PFO) have been added to the myheart website. Please read more about these conditions below:
A myheart members’ video meeting was held on Saturday 1st October, 2022. There was a Q and A session with cardiologist, Dr Sabiha Gati, giving members the chance to meet with other young people who have been diagnosed with a cardiac condition, as well as an informal space to ask questions of a consultant cardiologist.
Currently myheart holds meetings twice a year for young people, between 18 and 35, who have suddenly been diagnosed with a life-threatening heart condition. Anybody with a cardiac condition between the ages of 18 and 35 can come to the meetings if they:
•Have been offered or already have an ICD
•Have suffered a cardiac arrest
•Have been diagnosed with an inherited or potentially
Every normal heart is gifted with a natural in-built electrical system. The electrical impulse generated from this system results in beating of the heart. The electrical system divides into 2 branches (called right and left bundle) at the level of the ventricle (bottom chambers of the heart).
The right bundle stimulates the right ventricle into action and the left bundle stimulates the left ventricle. If there is blockage in any of the branches, it results in the delayed activation of the supplied ventricle. This is reflected on the 12-lead ECG (electrical tracing of the heart) and is interpreted as either right or left bundle branch block.
Right bundle branch block (RBBB) is not an uncommon finding in the general population. The prevalence increases with age – i.e. it is more commonly seen in elderly individuals. RBBB is also not an uncommon finding in young people, especially athletes. The prevalence of the condition in young, middle age and elderly individuals is believed to be 0.2%, 0.7% and 11.3% respectively
RBBB is usually an incidental finding on an ECG, which would have been carried out for another reason. However, in the presence of symptoms like chest pain or shortness of breath or syncope, it might signify underlying heart or lung disorders such as:
•Long standing right heart failure
•Myocardial infarction (heart attack)
•Congenital heart conditions (hole in the heart)
•Long standing lung conditions affecting right side of the heart
•Pulmonary embolism (clot in the lung)
RBBB seen in elderly individuals without heart problem could be due to the degenerative changes of the right bundle as a part of normal ageing process.
As mentioned above, RBBB can be an incidental finding. If there are no symptoms associated, there is no need for further investigations and treatment. However, if associated with any of the above-mentioned symptoms, then further evaluation is required in the form of echocardiography (ultrasound scan of the heart).
On the other hand, left bundle branch block (LBBB) on the ECG may suggest underlying heart conditions, meaning that further investigations would be made.
A patent foramen ovale (or PFO for short) is a flap between the top 2 chambers of the heart which has not closed the way it should do at birth. During a baby’s development in the womb, this flap is fully open as a hole called the foramen ovale, and is found in everyone. It is necessary to allow blood containing oxygen from the placenta to get the rest of the body, bypassing the lungs which are not yet working. However when a baby is born, the lungs start working and providing oxygen-rich blood to the heart; pressures inside the heart change; and the foramen ovale (which is now no longer required), usually closes within the first 2 years of life in 70-80% of people.
However in the remainder of people (20-30%), the foramen ovale does not close, and it is then known as a patent foramen ovale (PFO). There is some evidence that genetics may play a role in keeping a foramen ovale open, but
generally PFOs are not thought to be inherited unless they are associated with other heart conditions.
How common is a PFO?
Studies have shown that a PFO is a relatively common finding in adult populations, being present in up to 30% of individuals. However, most people with a PFO do not even know they have it, and it is usually found by chance on investigations for other problems or during cardiac screening.
What symptoms can you get with a PFO?
Most people with a PFO don’t even know that they have it as it causes very few symptoms. Rarely in a child or young person, blue skin may develop, particularly when they strain (e.g. during crying) due to blood without oxygen mixing with oxygen-rich blood from the lungs. However, usually in this scenario, other heart abnormalities are also present. In some cases, a PFO may be associated with stroke or migraine; this is discussed below.
What problems can occur with PFOs? Can PFOs cause sudden arrhythmic death syndrome (SADS)?
In most people, a PFO will not cause any problems and they are not associated with sudden death or SADS. There are some associations, however, with other conditions, and PFOs have been linked with both stroke and migraine.
Although an association of PFO with stroke is well established, there is no conclusive evidence from population-based studies that a PFO alone is associated with an increased risk of a first or recurrent stroke. Therefore no preventive treatment is recommended in individuals with an incidental finding of a PFO. In young people who have had a stroke and found to have a PFO but no other obvious cause (i.e. “cryptogenic” stroke), treatment may be indicated and this is discussed below.
Similarly, despite an association with migraines, evidence for this is conflicting and studies have not shown any benefit in PFO closure for preventing migraine attacks.
PFOs have been associated with decompression sickness from scuba diving given the pressure differences that occur in the blood and chest wall with deep sea diving. Therefore for this reason, the only lifestyle advice recommended to people with a PFO is to avoid deep sea diving.
A PFO is generally diagnosed on an ultrasound scan of the heart called an echocardiogram, where a probe with special gel on it is connected to an ultrasound machine and passed along the chest wall. This shows the heart and its
structures using sound waves and can detect blood flow through different parts of the heart. However sometimes, this type of echocardiogram may be suggestive of a PFO but not conclusive.
One of the things a PFO can look like is an atrial septal defect (ASD), which is a hole between the top 2 chambers of the heart. Therefore in order to clarify this and assess the heart further, 2 special types of echocardiogram may be needed:
•Bubble contrast echocardiogram: this is exactly the same as an ordinary echocardiogram, but in addition a small amount of agitated salt water is injected into a vein.
This water forms small micro-bubbles which highlight the chambers of the heart, and can be seen crossing from one chamber to the other if a PFO is present. During the study, you may be asked to strain in order to increase the pressures in the heart and determine whether a potential PFO is present which opens when pressures in your chest increase (e.g. when coughing or sneezing).
•Sometimes, even a bubble contrast echocardiogram may be inconclusive, or may show a PFO which needs further evaluation to determine its size and structure. In this instance, another special echocardiogram called a transoesophageal echocardiogram may be needed.
This uses the same principles as a transthoracic echocardiogram (i.e. sound waves) to visualise the heart, but a special, smaller probe fixed to the end of a tube is passed into the food pipe to visualise the heart from inside the body. This shows the heart in much better detail, allowing the PFO to be assessed better. Given that this test is a little more invasive and can be uncomfortable, it is usually performed with sedation (a medication which makes you feel drowsy and relaxed).
Generally, no specific treatment is required for a PFO if found in isolation. However if found in association with a stroke where no other cause for the stroke has been established, treatment is recommended. In general, 2 options exist: medical treatment with Aspirin, or closure of the PFO with a special device.
Current guidelines do not advocate closure of the PFO over simple medical treatment, although in some centres closure using a device inserted into the heart from the groin (percutaneous closure) may be offered to patients after they are given the pros and cons of each treatment option.
The National Institute of Clinical Excellence (NICE) issued guidance on percutaneous closure of a PFO in December 2013 (see http://guidance.nice.org.uk/IPG472). In this
guidance, they noted that the optimal treatment for patients with PFO who have had a stroke still remains undefined. However percutaneous closure of a PFO is at least as effective as medical therapy for preventing recurrent stroke, and possibly more effective.
Use of the procedure in patients for whom it would be clinically appropriate (for example, those people who cannot have blood thinning medication due to the risk of bleeding) should be strongly influenced by patient choice, taking into the consideration the risks and benefits compared with long-term blood thinning medication or Aspirin.
Closure of a PFO can be associated with serious but infrequent complications, and these must be discussed with the consultant beforehand so patients can make an informed decision.
For a PFO found in isolation, open heart surgery is almost never required.
Is long-term follow-up or screening of other family members needed?
An incidentally detected PFO generally requires no long-term follow-up or monitoring, unless the individual develops symptoms suggestive of a stroke in which case reassessment and treatment as described above may be indicated.
The myheart website contains information on cardiac conditions, tests, and treatments. We have information on the following conditions:
Aortic Disease, Arrhythmogenic right ventricular cardiomyopathy (ARVC), Atrial Fibrillation, Brugada Syndrome, Catecholaminerfic polymorphic ventriculat tachycardia (CPVT), Coronary artery anomolies, Coronary artery disease, Dilated cardiomyopathy (DCM), Hypertrophic cardiomyoparthy (HCM), Long QT syndrome (LQTS), Marfan’s syndrome, Myocarditis, Progressive cardiac conduction defect (PCCD), Short QT syndrome (SQTS) and Wolff-Parkinson-White syndrome (WPW).
If you would like to read more about any of the conditions mentioned, please head over to our website: www.myheart.org.uk/heart-conditions
After years of struggling with heart grumbles, pains and palpitations, I was repeatedly told (by different doctors) that it would just be stress, anxiety and depression. Different medications did nothing to stop the aforementioned issues I experienced. The symptoms also got so much worse after my Mum passed away in 2018 but this was again put down to stress, anxiety and depression.
By pure luck (in a sense) I got tonsillitis which I get often and was given antibiotics by the doctors. I am allergic to penicillin so getting antibiotics that work for me is always tricky and I was actually given some that didn’t agree with me at all. I spent a night in absolute agony unable to sleep with stomach pains, a burning sensation in my spine and more.
In the morning, my dad and sister insisted and dragged me to the hospital (I didn’t want to go at all as I don’t do well with medical things, especially needles and I knew I’d need to give blood to help them find what was wrong with me).
So, against my choice I went to hospital and was immediately admitted, they thought my appendix had burst due to the nature of the pain. I was given a full MOT: multiple scans of everything, CT scans, the works. One of the procedures was an ECG.

The results came back as just an allergic reaction to the antibiotics. But then I was told privately by a doctor they had detected WPW. I was completely shocked! I thought I was a healthy young lad. At first it didn’t really sink in at all despite a very brief explanation from the doctors that it could be medicated or treated.
I was referred to a specialist and this is when it became more real…
He said that due to it being undetected for so, so long, the stress on my heart will have been so much and therefore medication was no longer an option. And that surgery was the best option as soon as possible or I, and I quote “might not make it to 35”. Obviously, I was talked through the list of risks involved.
I left the specialist’s office and I’m not ashamed to admit
I broke down into tears. And genuinely spent the next two weeks very closed up as a person. Just in shock.
Obviously, I came to terms with it and was determined that I was going to beat it.
It was a long 8 months wait to get a surgery date and when I finally got the letter in January, I was relieved but also scared again, still knowing the risks that accompany the surgery however minimal the statistics.
With around a week or two to go, to the surgery, I went back into my shell a bit again. Really scared about everything that could happen. To the point in a way I was almost making peace with my life, thankful for what I’ve managed to do in my life so far- I’ve backpacked around the world, lived in Spain for two years and kept going after the passing of my mother, so I was proud of myself. (Might sound dramatic but I couldn’t help the way I felt at the time)
My family, friends and colleagues were all amazing and supportive, trying to keep me positive and reassure me.
The day of the surgery arrived and I was obviously incredibly scared. Hugging my Dad before going into the ward wondering if it’s the last.
The doctors, nurses and surgeon (all the staff really) at Wythenshawe Hospital were absolutely amazing! Really, really kind and understanding (especially as it took a shocking amount of time to talk me into getting the cannula in), as I said I really don’t do well around needles.
The surgeon, Dr Brown was incredible, he talked me through everything: kept me calm and discussed options with me such as how much risk they take, i.e. if it looks like it could be more complicated than it seems, does he carry on, or does he stop and then have a few more assessments and plan. He gave me three options to deal with the potential levels of risk and listing the figures relating to said risk i.e. a stroke being caused or a heart puncture. I signed the waiver and simply told Dr Brown “you’re a lot smarter than me, I trust your judgement completely, do what you can to fix me as safely as you can.”
The surgery was supposed to take 2 hours max, and ended up being 4 as Dr Brown found extra pathways which he judged in a safe enough position to ablate, though I do remember him vaguely talking to me when I was awake on the operating table saying he believes it’s a safe call to ablate and tried to check I was happy.
Now, I feel so much better than I ever did. Maybe it’s also a slight pseudo effect as I’m still waiting for my sign-off from Dr Brown. It’s taken longer to heal than I thought because of the extra work that was done to ablate the extra pathway and as boring as 4 weeks bed rest was, I didn’t mind a
small break from work, haha!
I am though feeling a lot better, a lot of the healing symptoms have passed (during healing I still felt palpitations and flutters etc but these are becoming very minimal now).
I’ve felt healthy enough recently to re-join the gym and start regaining full fitness which I intend to keep up to ensure a healthy life. I’m obviously doing this walk* not only as a challenge and to help raise money for CRY, but to raise awareness so hopefully others can catch it earlier and not have to have surgery and the stress and anxiety that comes with it.
I thank all my friends and family and especially all the staff, nurses, doctors and of course Dr Brown so so much for everything they have done. Words can’t actually describe how thankful I am to all of them, they’ve helped give me the chance of happy long life.
*To mark the first anniversary of his initial diagnosis, on Saturday 18th June, Tom was joined by best friends Rochelle Antley and Billy as they kicked off the Heart 2 Heart Fundraising Walk, completing 20 miles from Edgeley Park, to Old Trafford, over to the Etihad, and back to Edgeley Park.
My WPW story by Kathleen Dymond
My journey starts in my early teens when I became aware of my heart pounding in my chest, my heart racing, my throat constricting like hands that had wrapped themselves like a tight vine around my neck. I would feel faint like I would collapse and unable to catch my breath. It felt like I was going to suddenly die.
I was quite sporty, so it was distressing when this would happen unexpectedly when I was playing hockey, running or swimming. It would come on suddenly and it would be very frightening and often it would last for several minutes. When I tried to discuss this with others, it was dismissed as anxiety, it was clearly all in my head.
This continued well into my early twenties when it became far more distressing and longer with each episode. I felt ashamed as anxiety back then was seen as a terrible weakness so I tried to hide it as best as I could and bravely carry on.
Gradually, over the following years, as the episodes occurred more often, more frightening; I would find myself in an ambulance, many times in A&E where I was monitored and then sent home, feeling ashamed with no understanding of what was happening to me. I began to feel like I was broken and damaged. Again, always sent off on my way that everything was fine and that it was anxiety causing these episodes, though in my heart I knew it wasn’t.
Eventually, one year as a student living in Oxford, I found a good GP who started to listen to me. Several conditions were suggested (asthma was one) but no outcome was achieved, though this GP did try to help me for which I am grateful.
I remember one night my sister came to stay and I had an episode that was so frightening, especially to my sister witnessing it, that we called an out of hours GP who told me there was nothing wrong with me and I was a basically an attention seeker and a time waster. It was a very low moment for me.
A few days later, I had several episodes, the worst it had ever been, and I found myself almost crawling back to my home. I remember holding onto a wall along Walton Street in Oxford. I eventually made it to the GP surgery with collapsing where I told the receptionist I was finally experiencing an episode for the GP to witness. There was a flurry of activity, and the GP came out to immediately assess me and within minutes I was in A&E at the John Radcliffe Hospital.
Unfortunately, again once at hospital my heart returned to a normal heart rate. I was assessed for several hours and again, almost discharged until, by a stroke of luck, the Cardiology Professor was leaving to go home, and my case just happened to catch his eye. Within minutes of the Professor consulting me, the ward become a very busy environment and I had to sign a paper to confirm that I was happy to undergo a procedure that may have a positive outcome for myself, but also potentially the opposite.
A drug called Adenosine was administered, which is usually used to slow a fast heart rhythm, but in this case, as my resting heart rate was not very elevated and I was not having any tachycardia, this procedure was for diagnostic purposes. I was told that the drug would be administered through a canula in my arm and would immediately slow any electrical activity in my heart to almost a stop. (Adenosine blocks electrical signals through the atrio-
ventricular (AV) node. This means signals cannot travel from the top to the bottom chambers of the heart for a few seconds, until the drug effects wear off.)
I remember the first round of the drug being given to me and seeing the huge ECG monitor as my heart became a flatter line on the screen.
Another round of Adenosine was given and at this point I felt the full impact of the drug being given and passed out, awakening to sounds akin to a win in a rugby/football match. There were cheers and as the Professor tore off the ECG sheet, slapping of hands on shoulders, whoops of joy and shouts of “We got it!”. Delights from everyone whilst the heart started beating regularly again and I become more conscious. I heard the words that these medical moments are rare and was told that I had something called WPW –Wolff Parkinson White Syndrome.
Finally, after all these years there were people on my side, united in this discovery and the years of research with a good team at the JRH.
I was booked in for an emergency catheter ablation where a wire with a camera is sent up through an artery from the groin into the heart while drugs were administered to monitor the heart’s electrical activity. In addition to finding the hidden accessory pathway in my heart, these Specialists found that I had another arrhythmia occurring in the lower chambers of my heart that also caused my heart to get to the dangerous heart rates I had been experiencing.
I am forever grateful for the team at the JRH especially Dr Yaver Bashir who led the team that day and kept me safe. I also received an unexpected written apology from the GP at my local surgery for missing this. He was very apologetic, as young hearts were not considered to be at risk of issues such as these. There was little knowledge 23 years ago about these matters.
That is why CRY is an essential charity and I would also like to applaud the work that CRY does in helping families and young adults and the wonderful support that they give and the research and education (to medical staff especially) they continue to do. Their efforts are immeasurable. I continue to support this charity as not only is it close to my heart, but it will help many people like myself. Thank you.
why some young people’s hearts stop, and why it seems to affect sportspeople more.
“When your heart suddenly stops pumping blood around your body, the consequences can be life-changing, if not fatal. It’s somehow especially shocking when the cardiac arrest happens to someone who is young and fit”
myheart member Meg Fozzard has written for ‘Welcome Collection’ drawing on her own ex[periences and those of a fellow cardiac-arrest survivior, Tim Butt, as she discusses
“In the 42nd minute of the Denmark versus Finland match, during the delayed Euro 2020 football tournament, Danish player Christian Eriksen suddenly collapsed on the pitch. I was at home, watching the match on television. Alongside viewers from around the world, I saw Eriksen’s teammates huddle around to shield him from the cameras as he received CPR.”
“I had a cardiac arrest in 2019. I, of course, can’t remember what happened, but seeing someone else go through what I experienced was upsetting. I instantly thought of my boyfriend and how time must have stopped for him as he performed CPR on me.”
Read the full article here: www.wellcomecollection.org./ articles/YoeLrBEAACIAXiT-

“The shock of cardiac arrest when you’re young and fit” - Discussion between myheart members, Tim Butt and Meg Fozzard
After a few successful years, the CRY Conference was held online for the third time in 2022. On October 20th and 21st, the conference was held in partnership with CRY and the European Association of Preventative Cardiology (EAPC). We were delighted to welcome leading experts in cardiology from around the world for presentations, discussion of case-based scenarios, and interactive debates for the audience to follow along and engage with.
These “case based scenarios” highlight the basis for the decisions experts make when advising patients with cardiac conditions. The advice the experts provide will be informed by consensus statements, which are informed by the latest research. At the conference the team will typically choose difficult decisions which provide an opportunity to demonstrate the different way in which research is applied, and debated, in the decision making process.
The first item of Day 1 was ‘Debates in Sports Cardiology: Elite Athlete with PKP2 Variant; end of the Road’. This was led by Professor Michael Papadakis of St. George’s, London, and Maria Sanz De Le Garza from Hospital Clinic de Barcelona, Spain, and presented a case asking if an athlete should be cleared for competitive sport.
The athlete in this case is a twenty-three-year-old recreational footballer and runner, asymptomatic with no family history, who was found to have an abnormal ECG at a CRY screening; and was diagnosed with Arrhythmogenic Right Ventricular Cardiomyopathy after further testing. This testing also identified the genetic variant PKP2. Professor Papadakis went on to show the results of the athlete’s family being screened, where it was established that the father and sixteen-year-old brother also had the PKP2 variant, but showed no evidence of underlying cardiomyopathy.
Dr Kristina H Haugaa, Head of Unit for Genetic Cardiac Diseases at Oslo University Hospital joined to argue the case that this athlete should not be cleared for competitive sport; while Andre Le Gerche, a cardiologist and researcher at the Baker Heart and Diabetes Institute in Melbourne, Australia, came in to counter this argument.
The second debate of the day, ‘Athlete post myocarditis and persistent LGE; Let sleeping dogs lie’ was led by Maria Sanz De Le Garza. The athlete in this case is a nineteen year old elite rugby player at an international level, training fourteen hours per week and presenting with sharp chest pains post training.
Blood tests and an ECG showed slight inflammation, and the echocardiogram was completely normal, however taking into consideration the chest pain and inflammation,
a Cardiac MRI was carried out. The initial CMRI confirmed Myocarditis in the acute phase and the athlete was advised to cease training. This test was repeated six months later and showed improvements, but there was scarring of the left ventricular wall still remaining. At this six month point, there were no significant symptoms, normal function and no arrhythmia.
The debate was opened with Alessandro Zorzi from the University of Podova, Italy, arguing that this athlete should be clear for competitive sport again and was followed up with Viviana Maestrini from Sapienza University of Rome, Italy, opposing this argument.
Both debates were followed by Q & A sessions with questions from audience members before the next session of the day began.
These afternoon sessions were introduced by Sabiha Gati from the National Heart and Lung Institute Imperial College and the Royal Brompton, and the discussion panel for the afternoon Jonathan Drezner from the University of Seattle, Antonio Pelliiccia from the Institute of Sport Medicine and Science, Italy, and Maite Tome from St George’s Hospital, London.
There were three cases to be covered, beginning with CRY Research Fellow Saad Fayaz with ‘Devil in the Detail; coronary artery anomaly’. The case looked at a seventeen year old black elite American football player considered the fittest in his academy and completely asymptomatic. The athlete had a cardiac screening through CRY and received abnormal results suggesting Hypertrophic Cardiomyopathy (HCM); they were then referred to St George’s hospital for further testing including echocardiogram and CMRI.
Dr Fayaz went on to discuss the athlete’s heart and normalities that overlap with signs of HCM, family history, and how this can complicate a diagnosis. The athlete’s CMRI also showed a potential coronary artery anomaly which provided some discussion amongst the panel as to what this, combined with the potential HCM, would mean for their future in high impact sports.

Next, Eleni Nakou from St George’s University Hospital, London, looked at a case of a sixteen-year-old, Nigerian club football player who attended a pre-participation screening event. The athlete was asymptomatic, with no family history but his ECG showed abnormal results, suggesting Hypertrophic Cardiomyopathy.

Dr Nakou goes on to speak about the results shown, including T-Wave inversions and explains the clinical significance of lateral T-Wave inversions in black athletes. After further testingthe diagnosis was still not clear, with the panel discussing the possibility of ‘Athlete’s Heart’ or mild HCM. Dr Nakou continued with discussion over management of the potential condition long-term and whether the athlete could continue participating in competitive sport.
The first sessions of day two ‘Updates in Sports Cardiology; the CRY experience’ were chaired by Dr Aneil Malhotra from Wythenshawe Hospital & Manchester Royal Infirmary, alongside Professor Meagan Wafsy from Massachusetts General Hospital.
The first speaker was Professor Michael Papadakis, who began by talking about his experience screening young individuals and working with the CRY screening programme. Michael then went on to discuss the methodology and results of a study aiming to determine: the diagnostic yield of a nationwide screening programme; report the frequency of false-negative results; and show the incidence of sudden cardiac arrest and sudden cardiac death.
The second item of the morning was presented by Professor Sanjay Sharma from St George’s University Hospital; ‘The veteran athlete’s heart; does sex matter?’. Professor Sharma discusses differences in heart tissue, the cardiovascular system, genetics, aging and cardiovascular risk-factors in men and women, concluding that indeed, sex does matter when it comes to cardiovascular adaptation to sport among veteran athletes.
The final speaker of the morning was introduced, Professor Domenico Corrado from the University of Padova, Italy, presenting ‘’Low QRS voltages in athletes; What do they mean?’. Professor Carrado discussed low QRS voltages in athletes, and the prevalence of this ECG pattern in familial cases and those with cardiomyopathies.
Audience members were encouraged throughout the session to send in their questions, and these presentations were followed by a Q&A session led by Dr Malhotra.
The interactive afternoon sessions were introduced

by Professor Michael Papadakis and co-chair Dr Silvia Castaletti from Istituto Auxologico Italiano, Milan, and welcomed the expert panel Dr Jonathan Kim from Emery Healthcare, USA, and Professor Sanjay Sharma to begin the presentation of the first case.
The first talk of the afternoon was ‘Cases in Sport Cardiology; Athlete with chest pain post COVID-19 vaccine’, presented by Dr Raghav Bhatia from St George’s University, covering the case of a thirty-nine year old, white professional runner with no history of cardiac conditions, who had two doses of the COVID 19 vaccine. The athlete presented to A&E after experiencing chest pain during exercise, and there received an abnormal ECG result and was recommended for further testing. The panel then discussed the next steps in terms of testing and treatment for the athlete, and debated how they would make a diagnosis in this case.
The second debate of the afternoon ‘Athlete with dilated ventricle’ was presented by CRY Research Fellow, Dr Saran Marwaha from St George’s University, London. The patient in this case is a cyclist, completing roughly 20km per week and presented to clinic with an Athlete’s Heart diagnosis from ten years ago in Australia. Upon new tests being completed, the results showed improvements and a possible different diagnosis. The panel then discussed treatment and management of the condition.
The final presentation of the day ‘Athlete with Ventricular Arrythmia’ was presented by Dr Emmanouil Androulakis from the Royal Brompton, London. This case was a referred patient; a 70 year old, veteran endurance athlete. The panel discussed which further investigations might be the most useful in this case followed by what possible diagnosis could be made. The panel discussion was followed by a Q & A session and the day was concluded with the Great Imaging Quiz.
We are grateful to the panel of experts who gave their time and knowledge over the two-day conference. We would also like to thank our sponsors as well as Wondr Medical, our digital partner who streamed the event.

If you would like to watch the presentations from the event please visit our YouTube channel: www.youtube.com/ cardiacriskintheyoung



The myheart network provides personalised help, support and information to individuals who have been diagnosed with a life-threatening inherited or congenital cardiac condition. We have a range of resources that you might find helpful, from literature, to website and video content, to our social media platforms and meetings.


This booklet provides medical information for young people who have been diagnosed with a cardiac condition or have been referred to a cardiologist for further tests, as well as their family and relatives. You can read the booklet online at bit.ly/3t2cSsJ

Enewsletters
We send out regular enewsletters to members and update them about the latest myheart developments. You can subscribe to our enews here: www.myheart.org.uk/services
Meetings
myheart typically holds two meetings a year in a central location for young people, between 18 and 35 years old, who have suddenly been diagnosed with a potentially life-threatening heart condition. Anybody between the ages of 18 and 35 can come to the meeting if they have been offered or already have an ICD, have suffered a cardiac arrest, or were diagnosed with an inherited cardiac disease. Members can gain support through meetings by talking to others in a similar situation.
Facebook Group

myheart has a Facebook group where members (aged 18 and over) can connect with other people who have been diagnosed with a cardiac condition often ‘out of the blue’. So many people who contact CRY/myheart want to talk to others who are in similar circumstances to themselves. The group is a private community for members of the myheart network to share their feelings and experiences with others who have suffered a cardiac arrest, inherited a cardiac condition, have a congenital condition, or found out that they have a cardiac condition after a sudden cardiac death in the family and want to be part of a support network for one another.
To join the myheart network and find out more about the private Facebook group, please visit www.myheart.org.uk/joinmyheart. If you are already a member of the myheart network and would like to join the Facebook group, please email myheart@c-r-y.org.uk

As well as videos sent in by members to help others – sharing their experiences of being diagnosed or undergoing certain tests and procedures – the myheart YouTube channel features a number of frequently asked questions which have been sent in by members and answered by Dr Michael Papadakis. You can visit the YouTube channel at bit.ly/3DzdPxj @myheart_UK

We understand that being young and suddenly finding that you need to be treated for a heart condition is not easy. CRY’s myheart Network provides personalised help, support and information to individuals who have been diagnosed with a life–threatening cardiac condition.
myheart is a support system for individuals to help develop effective coping strategies and reduce social isolation. The network was developed in response to feedback from young people who found that support groups available were not effective in helping them deal with issues such as fitting of ICDs and pacemakers, and undergoing ablation surgery.
myheart offers:
• Medical information about different cardiac conditions, tests and treatments.
• Personal stories/videos from other young people who have been diagnosed with a cardiac condition.
• Videos from our cardiologists answering frequently asked questions.
• Meetings for people aged 18–35 who have had a cardiac arrest; have been diagnosed with an inherited cardiac condition; have an ICD; or have been offered an ICD.
• A private Facebook group for anyone over the age of 18 who has been diagnosed with an inherited cardiac condition.


Email: myheart@c-r-y.org.uk
Online: www.myheart.org.uk
Telephone: 01737 363222
(Please ask for the myheart coordinator)
Post: FAO myheart
Cardiac Risk in the Young Unit 1140B The Axis Centre Cleeve Road
Leatherhead KT22 7RD
This is your newsletter - we would like to include your stories and photos. If you have been diagnosed with a cardiac condition and would like to share your story, thoughts and experiences with others, please send in your stories to myheart@c-r-y.org.uk.
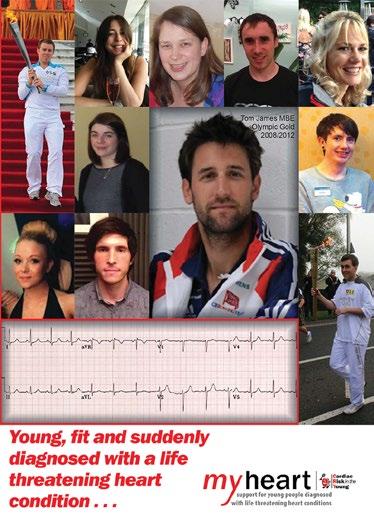
This booklet – with an introduction from double Olympic gold medallist Tom James MBE, who was diagnosed with a heart condition known as atrial fibrillation in the run up to the London 2012 games – features 10 personal essays from young men and women who recount and talk through their own experience of suddenly being diagnosed with a heart condition. The booklet is for and by the growing number of young people who –thanks to greater awareness and early diagnosis – are learning to live with a diagnosis of a potentially life-threatening heart condition.
Tel: 01737 363222
Email: myheart@c-r-y.org.uk
Websites: www.myheart.org.uk