PERIODONTAL CASE STUDY
CATHERINE CHUNG
CCBC DENTAL HYGIENE PROGRAM
DNHY 221- DENTAL HYGIENE CLINIC
INSTRUCTOR: MS. AMANDA WALBRECHER, RDH. MAY 9, 2024

CCBC DENTAL HYGIENE PROGRAM
DNHY 221- DENTAL HYGIENE CLINIC
INSTRUCTOR: MS. AMANDA WALBRECHER, RDH. MAY 9, 2024
63 years old European male
Diabetes Type II - HbA1c: 6
5 coronary bypasses: 1 year ago
Allergy: Omnipaque (iodine contains)
Medications : Forxiga, Atorvastatine, Esomeprasole, Resitune, Bisoprolol
Symptoms: Dysgeusia, xerostomia
Chief complaint: limited opening, halitosis and stain on his teeth.
Last dental cleaning: 7 months ago
BP: 123/69 mmHg and Pulse: 55 /min
ASA III - Patientwith severe systemic disease (American Society of Anesthesiology, 2020).

• No significant findings
• Normal variants - bilateral lina alba, mandibular tori, and exostosis
HTC
• Severe crowding and attrition
• Bridge with 8-9 being the abutments teeth – mesiodens removed
Periodontal exam
• PD :1-7mm
• CAL: 1-4mm
• Bleeding onprobing
• Inflammation
Radiographic findings
• No suspicious areas
• Calculus
• Generalized 15-30% boneloss
• Localized vertical boneloss
• Thinning ofthe lamina dura
Periocondition :
Stage III - severe active periodontitis and Grade Bmoderate rate progression.
Patient is an excellent candidate for the periodontal case study as he is presenting with active periodontitis according to the assessments


Treatment
• Nonsurgical periodontal therapy - SRP with local anesthetic
Goal
• Removal of calculus and stop the progressionof the active periodontitis with a reduction of pocket depth and gain of clinical attachment.
Prognosis
• Success of treatment and positive expectations
Special consideration:
• Patient might not be able to have access to same level of care as in United Stated and periodontitis may return if personal hygiene is neglected.
• Poor outcome withuncontrolled diabetes
1st appointment
• Assessments
• Treatmentplan
• Patient education: bacteria formation, oralsystemic link, recommendation andeducate on the use ofelectric toothbrushandfloss.
• Informconsentfor case study
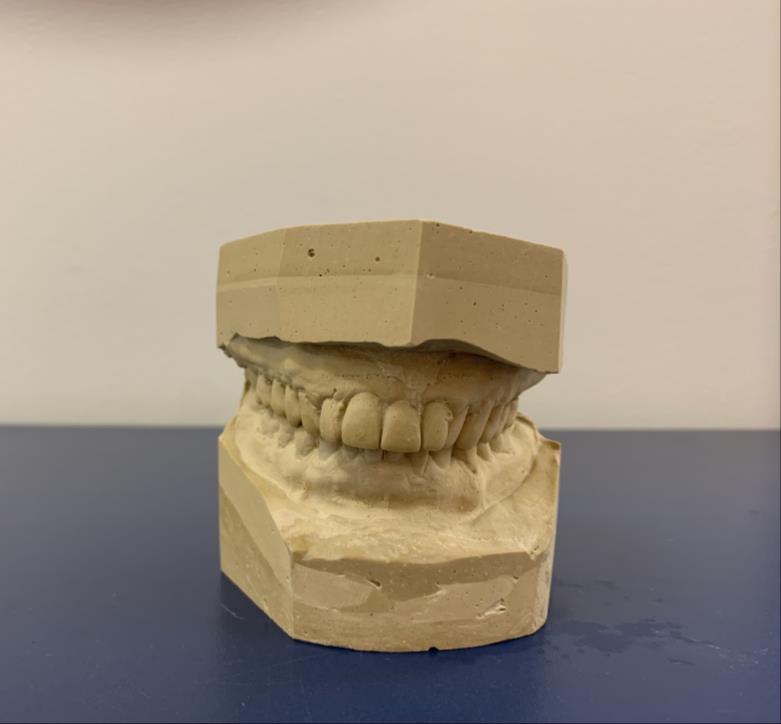
• Impression
2nd / 3rd appointment
• PFI
• Topical Benzocaine
• Local anesthetic – 3% mepivacainewithout epinephrine
• SRPLeft (2ndappt)/ Right (3rdappt)
• Oral irrigation with 0.12% Clorhexidine
• Post-operation instructions
4th appointment
• Fullmouthprobing
• Fine handscale
• Polish
• Fluoridevarnish
Obstacles / reactions
• Limited openings
• Gagging during anesthesia
• Patient requestedto notbeing in supine position
Positive outcomes post treatment
Presence of 7mm pocket depth
Some reduction of probing depth
No bleeding during probing
Reduction of gingival tissue
PFI improvement 76% to 83%
Negative point - presence of build-up on lower anterior after one week.
Medical condition and persistence of 6-7mm pocket depth, need referral to periodontist.
3MRC
Weaknesses – lack of product recommendations and calculus tenacity removal
Strength – communication to patient about oral link systemic
Staging and grading periodontitis.AmericanAcademy of Periodontology.(2017).
https://www.perio.org/wp-content/uploads/2019/08/Staging-and-Grading-Periodontitis.pdf
Statementon asa physicalstatusclassificationsystem.American SocietyofAnesthesiologists . (2020.).https://www.asahq.org/standards-and-practice-parameters/statement-on-asa-physicalstatus-classification-system.
Wynn, R. L., Wynn, R. L., Meiller,T. F., & Crossley, H. L. (2023). Drug informationhandbook for dentistry: Includingoral medicine for medically compromised patients& specific oral conditions. Lexicomp.