AHEAD NURSING


A
MESSAGE FROM DANIELLE




A

Dear Colleagues,
I proudly present ChristianaCare’s Nursing Report for Fiscal Year 2024 (July 1-June 30). What a year it’s been! This robust report expresses how much our nurses are driven by love—love for our patients, for our community and for our noble profession.
Structured around four Magnet components—Transformational Leadership, Structural Empowerment, Exemplary Professional Practice and New Knowledge, Innovations and Improvements—our report features highlights across acute, ambulatory and primary care and ChristianaCare HomeHealth.
While it’s full of inspiring examples of nursing innovation and excellence, I particularly enjoy sharing how our extraordinary caregivers work together to advance their practice areas and create novel approaches to care delivery. I also love the photos that capture what it’s like to practice nursing at ChristianaCare: We are a collaborative team that celebrates and uplifts each other.
The activities of FY 24 coincided with another significant milestone for ChristianaCare Nursing. We recently applied for the health system’s fourth Magnet® designation for our Christiana and Wilmington hospitals, Ambulatory Services and HomeHealth. It was an all-hands-on-deck effort beautifully guided by our Nursing Excellence Experts and Nursing Excellence Ambassadors.
On the following pages, we’ve included several examples of Magnet principles in action, such as programs designed to reduce harm rates and staff turnover and initiatives that improve caregiver safety and patient experience. There are stories of using technology solutions to provide optimal acute inpatient care, offer acute care services in patients’ homes and support caregiver mentorship systemwide. And we share numerous instances of individual caregivers and caregiving teams leading transformational change at ChristianaCare, whether it’s in our approach to climate change or how we promote nurse-to-nurse collaboration and encourage peer support.
Practicing nursing has always demanded adaptability, creativity, excellence and empathy. These qualities have helped make our field the most trusted for 22 years in a row, according to Gallup, and they define ChristianaCare Nursing.
Our team has met the challenges of the last few years with grace, ingenuity, vision and compassion. In these changing times, they’ve seen opportunities to shape the future of nursing and health care. Each story, accomplishment and innovation included on the following pages reflects the passion that drives ChristianaCare nurses.
I am deeply proud of this brilliant team, and I hope you will be as energized as I am by their contributions to our field.
Sincerely, Danielle
Danielle Weber, DNP, MSM, RN-BC, NEA-BC Chief Nurse Executive Chief Nursing Officer, Wilmington Hospital
MAGNET ® 4.0: LEADING EXCELLENCE AND ADVANCING PRACTICE (LEAP)
ChristianaCare’s Nursing and HomeHealth teams aim to be transformative and intellectual forces improving health through the evolving art and science of nursing. We propel this vision every day in service to our community as we advance the profession with love and excellence, innovation and influence.
Throughout FY 24, the Nursing team has prepared to LEAP into our fourth Magnet designation for our Newark and Wilmington campuses, Ambulatory Services and HomeHealth. For our Magnet application document, we’ve gathered examples of nursing excellence and leadership across the health system. Here, we offer a few highlights from FY 24 and recent years— the tip of the iceberg—of the countless examples of our nurses exemplifying Magnet characteristics.



Reducing the Transitional Medical Unit CAUTI rate
Clinical nurse Briar Dobson, BSN, RN, led the Transitional Medical Unit (TMU) Catheter-Associated Urinary Tract Infection (CAUTI) Comprehensive Unit-based Safety Program (CUSP) team in evaluating patient safety data and implementing interventions to reduce the rate of TMU CAUTIs related to indwelling urinary catheter use. The interventions saw a 100% reduction in the TMU CAUTI rate.
Clinical nurses optimize hypertension management
Clinical nurses Justine Green, BSN, RN, AMB-BC, CPC-A, and Danni Righter, BSN, RN, successfully implemented the Hypertension Medication Management Protocol for Registered Nurses for a patient with a new diagnosis of hypertension. Green and Righter’s autonomy and adherence to the protocol enabled them to enroll the patient in the Hypertension Medication Management Program and help the patient effectively manage hypertension.
Neonatal Intensive Care Unit exceeds targeted certification goal
ChristianaCare’s Neonatal Intensive Care Unit increased its percentage of eligible registered nurses with professional nursing certification by 0.25% annually in 2022 and 2023.
Interprofessional HAPI prevention team receives ChristianaCare Way Value Award for pressure injury prevention initiative
Nurses Susan Mascioli, MS, BSN, RN, NEA-BC, CPHQ, vice president of nursing quality and safety, and Judy Townsley, MSN, RN, CPAN, NEA-BC, FACHE, vice president of Perioperative Services, led an interdisciplinary Hospital-Acquired Pressure Injuries (HAPI) Prevention Team to improve incidents of three and four and unstageable HAPI. Using several evidence-based interventions, including specialized personnel, camera capture technology, prevention products and education and training, the team saw an 88% reduction in stage three or higher HAPI rates and received a ChristianaCare Way Value Award for its approach to reducing HAPI.
6.2 per 1,000 catheter days
Pre-Intervention TMU CAUTI 0.00 per 1,000 catheter days
Post-Intervention TMU CAUTI
2022
31.06%
registered nurses with professional nursing certification
Goal: 25.12% 2023
33.07%
registered nurses with professional nursing certification
Goal: 31.14%
02 MAGNET ® 4.0: LEADING EXCELLENCE AND ADVANCING PRACTICE (LEAP)
Virtual acute care nurse program improves patient experience with implementation of in-room technology
Guided by Nursing leadership, ChristianaCare Nursing caregivers collaborated to create a virtual acute care nurse (VACN) program that launched in September 2022 that promotes optimal patient care and improves both caregiver and patient experiences. Virtual nurses manage responsibilities that can be completed remotely while bedside nurses manage care that can’t be completed virtually. (See page 47.)
42.3%
patient experience score
Pre-intervention
54.3%
patient experience score
Post-intervention


Clinical nurse adoption of technology improves 5A patient experience
Nurses in 5A, a 40-bed intermediate step-down medical unit, leveraged VACN technology to assist with nursing care delivery in the unit and improve patient experience. ChristianaCare’s VACN program provides an innovative care delivery model with nurses using virtual technology to provide any inpatient care that doesn’t require them to be in-person.
52.6% three-month average patient experience score
Pre-intervention
69.2% three-month average patient experience score
Post-intervention
Reducing hospital-onset C. difficile infection rate with nurse manager’s advocacy and influence
Lindsay Sanderson, MSN, BS, RN, NE-BC, PCCN-K, nurse manager, represented Nursing on the multidisciplinary C. difficile Steer Committee, which was reconvened when rates of hospital-onset C. difficile infection rose during the COVID-19 pandemic. Sanderson participated in C. difficile triad case reviews and served as an integral member of the committee, contributing expertise and knowledge as the team identified and deployed interventions that resulted in a 56.5% reduction in cases in the acute care medical and surgical units.

2.3 per 1,000 patient days
Pre-intervention rate
1.0 per 1,000 patient days
Post-intervention rate
Living the ChristianaCare Way through a nursing practice initiative
Ann Painter, MSN, RN, senior vice president, HomeHealth and Community Services, led the development and implementation of a nursing practice initiative to cross-train acute care float and per diem nurses for HomeHealth settings. The innovative strategy utilizes existing nursing to improve patient care and experience and alleviate burdens for HomeHealth staff during staffing shortages.


EXEMPLARY PROFESSIONAL PRACTICE
ChristianaCare’s nursing caregivers provide exceptional, evidencebased, innovative care when and where our neighbors need it most. Our caregivers understand how their vital work profoundly impacts patients, families, our community and colleagues. They understand ChristianaCare is Magnet because our team is extraordinary.
Since its launch in 2021, the ChristianaCare Hospital Care at Home program has become a national model for bringing acute care to the place most familiar to patients — their own homes. The program’s multidisciplinary team, which includes nurse practitioners and registered nurses, provides the highest level of in-home acute care available statewide.

1,000 admissions
December 2021-March 2024

“Having patients at home means people don’t have to find a parking space or walk a million miles just to get to the room. Just to get to a destination for some of our families is a real challenge.”
PAN YEUNG, BSN, RN
03 EXEMPLARY PROFESSIONAL PRACTICE
ChristianaCare offers care when and where it’s most needed for people across the life-span. For school-aged children, we help address their health concerns at school through our school-based health centers, a partnership with the Delaware Department of Health & Social Services, the Delaware Division of Public Health, and several school districts. At each center, a team of medical, mental health and nutrition experts led by an advanced practice registered nurse (APRN) provides a roster of services by appointment during the school day.
“Elementary school-based health centers play a pivotal role in fostering a thriving community by providing accessible, comprehensive health care, ensuring every child has the opportunity to learn, grow and succeed.”
DORRELL GREEN, E d .D. SUPERINTENDENT OF THE RED CLAY CONSOLIDATED SCHOOL DISTRICT
Total number of ChristianaCare school-based centers including
6 elementary schools
3 new elementary school-based centers opened in FY 24
19 high schools

EXEMPLARY PROFESSIONAL PRACTICE
While the majority of hospital-related falls are in acute care settings, a retrospective analysis published in the American Journal of Medical Quality estimates that 20% of falls occur in ambulatory settings. In FY 24, a nurse-led Ambulatory Practices Ambulatory Falls Subcommittee was established to educate ambulatory caregivers on best practices to reduce patient falls in ambulatory settings. The committee’s activities included:
• Sharing weekly Huddle Tips on Falls Best Practices.
• Developing a comprehensive web-ed for all caregivers.
• Disseminating a Falls Best Practice tip sheet to all practices.
• Creating a virtual Best Practice Training step-by-step reference guide.
Number of Falls
2023-012023-022023-032023-042023-052023-062023-072023-082023-092023-102023-112023-122024-012024-022024-032024-04
In FY 24, the nurse-driven effort to prevent ambulatory falls resulted in a 25% decrease in falls through April.
EXEMPLARY PROFESSIONAL PRACTICE
ChristianaCare’s Zero Harm Awards recognize hospital patient care units, HomeHealth teams, Perioperative Services departments and Ambulatory Practices that have maintained zero cases of preventable harm in one of nine harm categories for at least three consecutive months for falls and at least 12 months for other categories. From July 2023 through April 2024, 179 awards were given, including four awards for 10 years (120 months) with zero harm. Since January 2017, 1,173 awards have been earned.


Congratulations to our Cecil County campus’s ICU (left) and PCU (right) for keeping our patients safe. The ICU has been CAUTI-free for five years and CLABSI-free for 12 months, and the PCU has been CAUTI-free for five years.
NEWARK CAMPUS
CLABSI
108 months - 2C
72 months - TSU
48 months - EAD, TNU, 3A
12 months - Hospital at Home, 4E, 3B, 5B, 6MS, 5E
CAUTI
108 months - BMT
60 months - TNU
48 months - CEAD
36 months - WCCU
12 months - 5A, 3C, 5D, 5E, 3A
MRSA
84 months - 4D, TNU
60 months - BMT
48 months - CEAD, 5D
36 months - 6A, 6MS
24 months - 5E
12 months - 7E, TSU, C 5A, 3B, 4E, 5C, CVCC, 6E, SCCC, TMU, 3C
C. difficile
60 months - TNU
48 months - CEAD
24 months - 6MS
12 months - 4B, Hospital at Home, 3A, 7E, TMU, 3C, BMT, 5C, TSU
All Falls
** awarded for 3 consecutive months (and multiples of 3)
96 months - NICU
33 months - OB Triage
18 months - TSU
12 months - TNU, 2M
9 months - BMT, CVCCC, SCCC, P6M, 6MS
6 months - 6M/7M, NCCU, TMU
3 months - 3C, CEAD, 4B, MICU, CSSU, 5E, 7E, LBR
Antenatal Steroids
24 months - OB Triage
WILMINGTON CAMPUS
CLABSI
108 months - 7S
72 months - W3M
48 months - 6W
36 months - WCCU
24 months - 8S
12 months - 4W
CAUTI
120 months - 7S
108 months - 4N/5W
84 months - 6S
60 months - WICU, 6W
36 months - WCCU
24 months - 5N
12 months - 4W, 8S
MRSA
120 months - 7S, 6W
84 months - W3M
36 months - 5N, WCCU
24 months - 7N
12 months - WICU, 4N/5W, 8S
C. difficile
120 months - 7S
84 months - 6W
48 months - 7N
36 months - WCCU
24 months - 5N
12 months - 4N/5W, 4W, 6S
All Falls
** awarded for 3 consecutive months (and multiples of 3)
9 months - WICU
3 months - WCCU, 6S, 7S, W3M, 8S
CECIL CAMPUS
CLABSI
24 months - SSU
12 months - PCU, ICU
CAUTI
60 months - ICU, PCU
24 months - SSU, MSU
MRSA
60 months - SSU
24 months - ICU, MSU
C. difficile
36 months - CDU
All Falls
** awarded for 3 consecutive months (and multiples of 3)
24 months - FBC
6 months - CDU, SSU
3 months - ICU
HOSPITAL AT HOME
CLABSI
12 months
C. difficile
12 months
HOMEHEALTH
CLABSI
72 months - CD Team 3, NC Team 2, NC Team 7
60 months - NC Team 6
12 months - NC Team 8
CAUTI
12 months - NC Team 2
AMBULATORY PRACTICES
Hypertension Admissions (primary care & cardiology practices)
36 monthsPC Woodstown
24 monthsPC Kirkwood
12 months -
PC Kennett, CHF CHR 1070, PC Linden Hill,
EXEMPLARY PROFESSIONAL PRACTICE
PC Concord, PC Limestone, PC at Home
Complications of Diabetes Admissions (primary care & endocrinology)
48 monthsPC Woodstown
36 monthsPC Whitehall
24 months -
PC Smyrna, PC Kirkwood
12 monthsPC Middletown East
PERIOPERATIVE
Perioperative Services
36 monthsGI Lab-Wilmington, PACU-Wilmington
24 monthsOR-Wilmington, Christiana Surgery Center
12 months - HVIS, Endoscopy-Union, Interventional Radiology-Union, Wound Care CenterUnion, PACU-Christiana, OR-Union, Wound Care Center
Nursing Bundles drive Nursing’s evergreen quest to provide patients with the best possible experience. When implemented, bundles improve targeted areas of care. Our Nursing Excellence and Patient Experience teams collaborate systemwide, including with HomeHealth, to introduce, expand and refine bundle adoption.
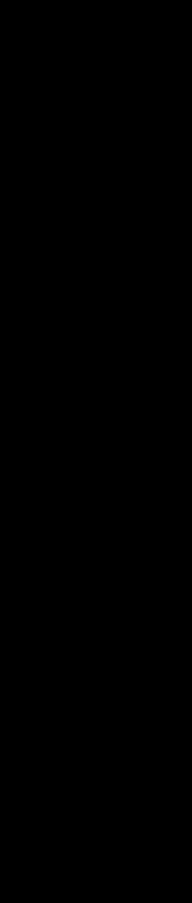
The Ambulatory Bundle for Patient Experience launched in ChristianaCare’s Ambulatory settings in FY 24. The bundle includes the components of AIDET (Acknowledge, Introduce, Duration, Explanation & Thank), HEAT (Hear, Empathize, Apologize and Take Action) and Teach-back.
Since implementing the bundle in our Women’s and Children’s and Cancer service lines in late 2023, the service lines have seen sustained increases in multiple National Research Corporation Survey metrics, including “Staff members courtesy and respect,” “Explain things back,” and “Likelihood to recommend practice.” The remaining service lines launched the bundle components early in calendar year 2024 and continue to collect metrics that examine the bundle’s impact on Patient Experience.


In FY 24, HomeHealth added a third component to its Patient Experience Bundle: Service Recovery. The bundle also includes Nurse Leader Rounding and Teachback. The team continues to track the impact of these best practices through Patient Experience scores and clinical manager co-visits.
W&C SL Percentile Ranks Pre/Post Implementation of Ambulatory Bundle
Metric
The bundle was implemented in August 2023.
Cancer SL Percentile Ranks Pre/Post Implementation of Ambulatory Bundle
The bundle was implemented in October 2023.
The Nursing team values our patients and their families above all else. When a patient or family member has a negative experience under our care, we prioritize restoring their trust and confidence.
In FY 24, a team of ChristianaCare nurses operationalized a Service Recovery approach to trust and alter negative perceptions after a patient expresses negative feedback about care. Through transparent communication and resolution, the program emphasizes personalized care and empathy in addressing concerns and resolving issues. We want to ensure patients and their loved ones feel valued and supported. It's not just about getting it right—it's about doing the right thing.
The incidence of violence against caregivers at ChristianaCare — and nationwide — has increased since the beginning of the COVID-19 pandemic. Systemwide, ChristianaCare’s commitment to caregiver well-being is the foundation for improving workplace civility. Led by nurses, our interdisciplinary workplace civility steering committee helps create an environment safe and free of violence for caregivers and visitors. In FY 24, the committee led the following activities and outcomes:
• Created a Workplace Violence (WPV) Leader Toolkit.
• Implemented a WPV Huddle Response Team activation in response to the escalation of workplace violence concerns during Campus Huddles.
• Increased Center for Worklife Wellbeing follow-up for harm-related Workplace Violence events.
• Implemented Evolv Weapons Detection System to screen for weapons at our Wilmington campus; plans include bringing the tool to our other campuses.
• Launched HomeHealth caregiver education Workplace Violence and De-escalation for Caregivers in Patient Homes and the Community with Review; 289 HomeHealth caregivers (83%) completed the education.
• Trained more than 1,500 caregivers in the Medical Groups on ALICE (Alert, Lockdown, Inform, Counter, Evacuate), an approach to responding to active shootings in ChristianaCare facilities.
• Implemented Dynamic Appraisal of Situational Aggression (DASA), a validated aggression risk assessment, in all adult acute care medical, surgical, step-down and ICU units. The evaluation includes an automatic behavioral health referral and increased rounding for patients with high DASA scores. DASA spread to the ED is being planned.
• Increased the number of staff duress badges used at Wilmington and Christiana Hospitals.

Thank you for making a difference!
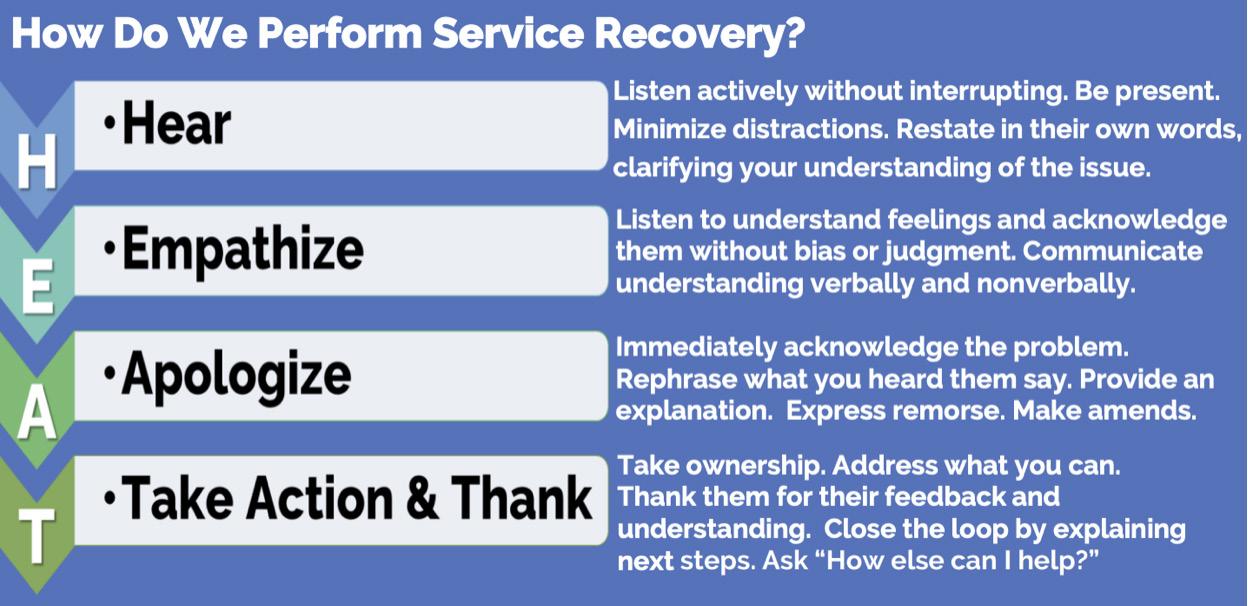
When an accident trapped Janet Belles inside her burning car last fall, ChristianaCare nurse Mark Maitland, RN, rushed from his vehicle to help pull her to safety. Belles and Maitland reencountered each other when he visited her hospital room to place an IV while she was hospitalized for her injuries. They were reunited a third time through ChristianaCare’s Center for WorkLife Wellbeing and Patient Experience Thank You program, which enables patients and their families to express appreciation to caregivers who made a difference during a hospital stay.
“You’re
the finest example of bravery I have ever met. And certainly, you have exemplified the core values of the nursing profession.”
JANET
BELLES to MARK MAITLAND

ChristianaCare's Nursing and HomeHealth leadership nurtures a collaborative working environment that crafts a shared vision for the health system's future and builds the systems and support structures to achieve it. Our emphasis on teamwork empowers caregivers of all tenures and roles to contribute their ideas, talents and innovations to ensure ChristianaCare remains a nursing pioneer.
APRN Council
Chair: Kathleen Salati, MSN, NPc, AGACNP
• Successfully merged physician assistants and advanced practice registered nurses into one APC Council.
• Developed the Advanced Practice Professional Advancement Model.
• Fine-tuned and developed an APC Orientation Day for new advanced practice providers.
Professional Nurse Council
Chair: Maggie Burress, BSN, RN
• Honored 26 ChristianaCare nurses with individual DAISY Awards, awarded one DAISY Team Award per hospital campus and one for HomeHealth/Ambulatory for a total of four DAISY Team Awards and four DAISY Leader Awards. Also initiated a process to recognize one nurse annually with the DAISY Educator Award and honored 16 ChristianaCare Nursing Support Team Members with ROSE Awards.
• Recognized more than 100 ChristianaCare nurses with Excellence in Nursing Awards in May 2024.
• Organized and hosted numerous recognition and celebration activities for nurses in all care settings across the organization for 2024 Nurses’ Month.
Council Highlights contd.
Nursing Research and Evidence-based Practice Council
Chair: Joana Lapinid, MSN, RN, PCCN
• Re-implemented Nursing Grand Round every other month in person and virtually via TEAMS and made recordings available for caregivers.
• Supported evidence-based practice (EBP) fellowship and Nurse Residency programs on EBP projects.
• Educated Practice Councils on the difference between research and EBP.
Technology & Innovations Council
Chair: Alvaro Bedolla-Pantoja, BSN, RN
• Developed and distributed a documentation satisfaction survey to help identify documentation pain points throughout the organization.
• Reviewed changes to PowerChart, including lab results review and a new admission workflow.
• Continued work to find strategies to reduce nursing interruptions and reduce unnecessary printing.
Workforce Connection Council
Chair: Ellen Alvarez, MEd, BSN, RN, CCRN
• Collaborated with the Float Pool Unit Practice Council to increase compliance with bedside shift report on individual units by providing targeted clinical nurse education, access to unit-specific data, and additional resources by unit with a goal to increase National Research Corporation survey responses from baseline by 20% by the end of FY 24 Q3 and to benchmark by the end of FY 24 Q4.
Quality and Safety Council
Chair: Carley Griscom, MSN, RN, CPAN, SCRN
• Partnered with key stakeholders to address barriers to obtaining patient weights, worked with Environmental Services to zero beds with room turnover, and provided monthly education to nursing caregivers regarding patient weights and equipment.
Quality and Safety Council contd.
• Provided feedback and decision-making to improve nursing practice and clinical outcomes for numerous quality and safety initiatives, such as the National Early Warning Score, sepsis, nursing-sensitive indicators and metric lessons learned.
• Collaborated with pharmacy regarding high-alert medication labeling and handling for safe medication practice.
Off-shift Support Council
Chair: Carol Abdill, MSN, RN, CRNI
• Offered advanced cardiac life support and basic life support classes for off-shift caregivers.
• Hosted Paws De-Stress events on all campuses for off-shift caregivers.
• Rounded on all campuses to speak with off-shift caregivers about concerns/needs.
• Collaborated with ChristianaCare’s Community Health team to host a community-based hygiene drive.
Chair: Ingrid Hausner, BSN, RN , CCRN, PCCN
• Presented learning needs assessment topics — including de-escalation techniques; addiction and withdrawal; delegation; and chain of command — at Nursing Assemblies, based on staff feedback for topics.
• Connected Education, Development & Advancement Council with Unit Practice Councils with less than 50% of certified nurses to support increased certification rates.
• Held annual Certified Nurses Day bulletin board contest.
• Collaborated with nurse residency coordinator and Nursing Professional Development Specialists to create a stronger onboarding experience and helped develop an evaluation tool for preceptors.
ChristianaCare Nursing participates in the American Association of Critical Care Nurses Clinical Scene Investigator Academy, a hospital-based, experiential nurse leadership and innovation training program designed to empower direct care nurses as clinician leaders and change agents whose initiatives measurably improve patient, staffing and fiscal outcomes. In FY 24, three ChristianaCare units completed Academy projects focused on nurturing a healthy work environment.

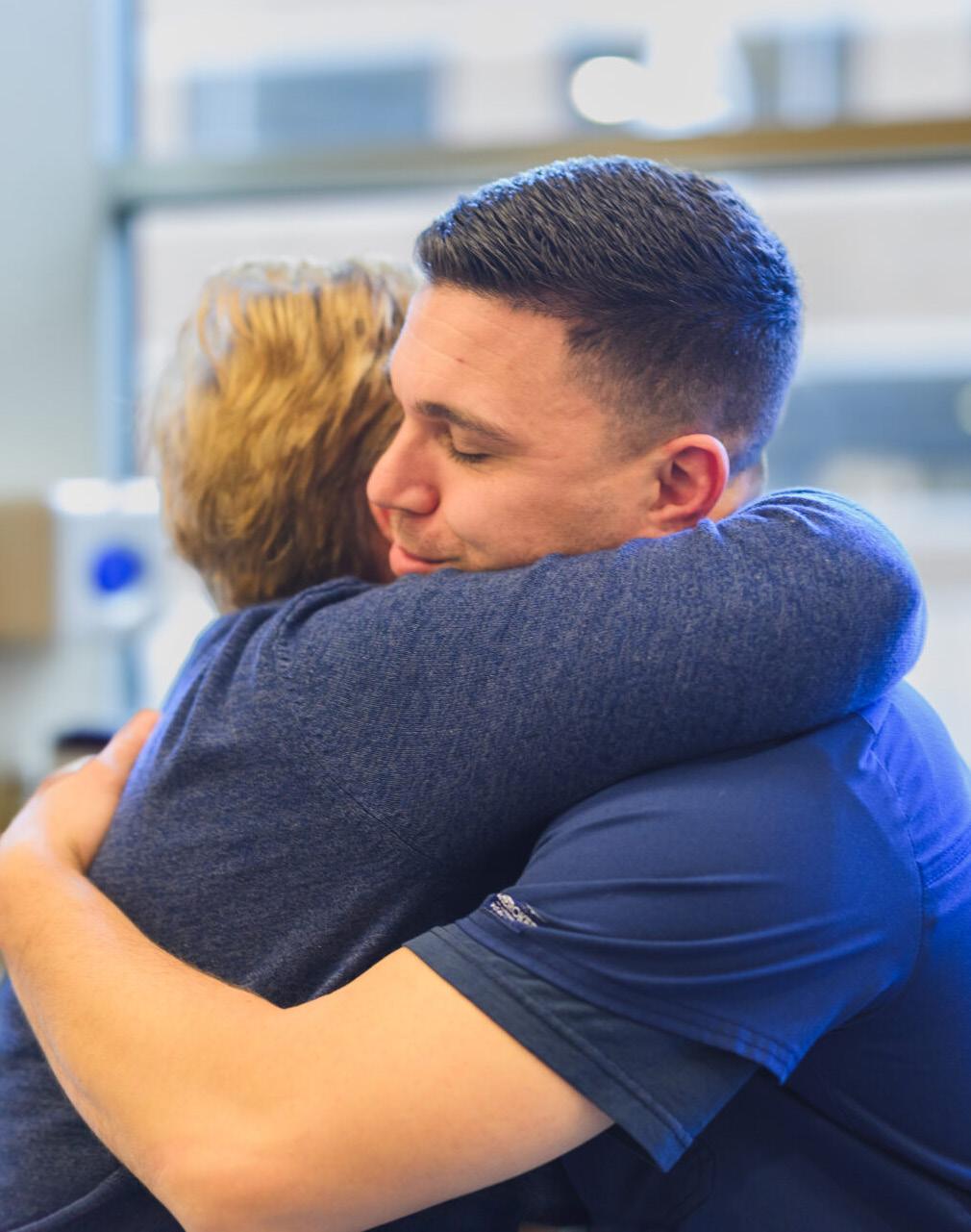
Our Newark Campus’s Medical ICU launched Conversation Is Critical: Let’s Get to the Point! in April. The project aims to provide nurses with tools to give and receive peer feedback, improve skilled communication, promote nurse-to-nurse collaboration and decrease nurse turnover. Nursing team members on the project include Ellen Alvarez, Med, BSN, RN IV, CCRN, WTA-C, Amber Hiltner, BSN, RN, WTA-C, CCRN, Jennifer Papi, MSN, RN, CCRN and Kathleen Luckner, MSN, APRN, ACCNS-AG, CCRN.
Our Wilmington Campus’s Transitional Care Unit and Wilmington Hospital ICU created a Buddy System for their project Oh the Places You Will Go with Your Dynamic Duos. The system is designed to leverage existing teamwork and ensure no team member feels alone or isolated. Buddies assist each another with activities necessary to advance patient care that cannot be done alone. They also cover each other on breaks, provide mentorship as appropriate and are just there, as good buddies are, when needed. The team is Jennifer Sullivan, BSN, RN, CCRN; Colin Durham, ASN, RN; Nallely Zavala, BSN, RN, PCCN; Anne Schu, BSN, RN and Dannette Mitchell, MSN, APRN, ACNS-BC, CCRN, FCNS.


Jamie Ayala, DNP, RN, NEA-BC, RN-BC, director of clinical operations, Wilmington Campus
Tammy Brown, MSN, RN, OCN, NEA-BC, manager, Virtual Acute Care Nursing
Cheryl Flowers, MSN, MSM-HCA, RN, CMSRN, nurse manager, 5N
Alyssa Hancock, MSN, APRN, FNP-C, chief APC, Foundational Care
Robin Maguire, MSN, APRN, NNP-BC, chief APC, Pediatrics
Patrice Miller-Ferko, MSN, MBA, RN, director care management & utilization management
Ena Nickens-Chappell, BSN, RN, GERO-BC HV, nurse manager, Vascular Access & Infusion Services
Denny Quinones, MSN, BSN, RN, CNOR, nurse manager, Christiana Hospital operating room
Michelle Stollings, BSN, RN, PMH-BC, nurse manager, Behavioral Health, Union Hospital

STRUCTURAL EMPOWERMENT
ChristianaCare empowers our remarkable, forward-looking caregivers to excel in their professions and embody our mission, vision and values. This culture of empowerment extends beyond our walls. By cultivating strong relationships and partnerships within our community, we collaboratively improve patient outcomes, public health and nursing care delivery.
Supporting caregivers on the path to being exceptional today and even better tomorrow, our four-tiered clinical ladder recognizes and rewards experience, knowledge and clinical expertise. The first of its kind in Delaware, the professional advancement model allows clinical nurses in primary care practices, specialty care practices and ChristianaCare HomeHealth improve their skills and practice at the top of their nursing licenses. Congratulations to our nurses who advanced to RN III and RN IV this year:
RN IV
Carol Abdill
Kiersten Edmondson
Natalie Galinskie
Helen Gehr
Kathleen Heller
Joana Lapinid
Colleen McGhie
Amanda Reese
Megan Sungail
Patricia Szczerba
RN III
Joshua Adams
Aimee Atkinson
Ashley Avallone
Mary Ayers
Elsie Barbosa
Heather Barlow
Kimberly Berl
Stephanie Bingnear
Allison Brander
LaNisa Brooks
Amber Brownley
Katie Burke
Jess Burt
Shon’tiana Butcher
Meghan Byrne
Rebecca Campbell
Rommel Carino
Danielle Carter
Kristen Casey
Taylor Chew
Kerri Coggins
Erin Coulahan
Jennifer Curlett
Olivia Danchik
Jana Dean
Michelle Dorset
Nicolle Dorsey
Tara Eaton
Jennifer Ericson
Ashley Fackler
Meghan Ferguson
Mary Kate Fillingame
Darby Gallo
Marlena Gastunas
Michelle Gent
Ashley Gillespie
continued on next page
RN III contd.
Kellie Glenn
Robin Gray
Dayonna Gunter
Maria Hadzor
Carol Haley
Lauren Harrison
Liann Havis
Amber Hiltner
Lauren Hoffman
Thomas Hoverson
Nikki Imm
Madison Ireland
Kelly Jennings
Jessica Johnson
Cartisha Jones
Sherie Kerr
Nichole Klimoff
Kristin Knorr
Adrienne Krass
Jacqueline Kreydt
Emma Kupis
Christine Lakatosh
Nadia Lazarczyk
Monica Lloyd
Kristen Magaw
Ana Marquis
Lauren Master
Brionna Masterson
Erika Maysonet
Karen Mazei
Amanda McCloud
Mike Mendola
Lauren Mills
Marilou Miranda
Judy Naidoo
Karen Okonowicz
Olasumbo Olateju
Abigail Pantalone
Christine Parks
Beverley-Ann Perera-Anderson
Wendy Pollock
Elise Polloni
Cody Quaglieri
Paola Ramos
Richeille-Anne Ricketts
Melanie Ries
Nathalie Romance
Crystal Rothbart
Erin Saberton
Katelyn Scarff
Nicholas Scarff
Marissa Shendge
Julie Shores
Courtney Slawson
Lewis Smiley
Amanda Smith
Ibelise Smith
Kimberly Smith
Shawn Sprenkle
Ashleigh Steen
Adria Stella
Mariah Swartz
Dawn Todd
Colleen Tontarski
Victoria Torello
Sara Vaile
Kelley VanHorn
Sarah Varnes
Stephanie Walley
Heather Warrell
Kelly Watkins
Christopher Weinacht
Jennifer Wilcox
Wesley White
Amy Woerner
Nallely Zavala
ChristianaCare’s Nursing Strategic Plan, developed annually, is our roadmap for providing a high-quality, exceptional care experience for every patient, every day. In FY 24, more than 80 clinical nurses and nurse leaders came together for a Strategic Planning retreat. Focused on ChristianaCare’s quadruple aim — caregiver experience, patient experience, optimal health, organizational vitality — attendees engaged in dynamic group discussions that resulted in actionable ideas and themes for the FY 24 Nursing Strategic Plan.
During Ambulatory Care Nursing Week in February, we thanked our ambulatory nurse caregivers for the love and excellence they bring to serving our neighbors.




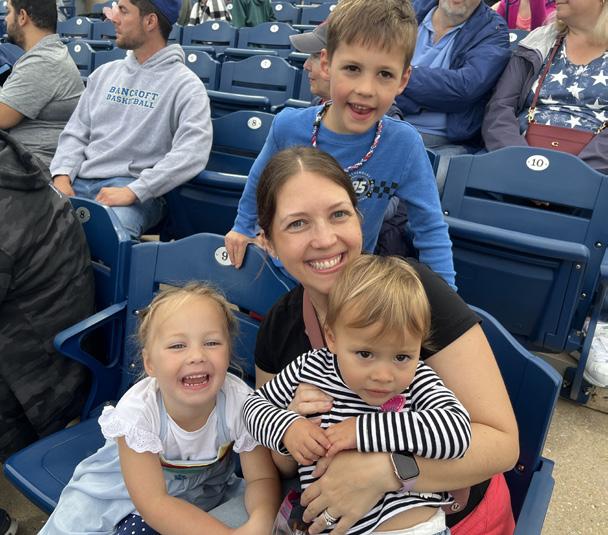
May is all about ChristianaCare’s extraordinary team members. For May 2024, our Professional Nurse Council crafted a calendar of fun, food and wellness activities for our dedicated caregivers across all campuses and HomeHealth. The packed agenda included a Wilmington Blue Rocks game, scavenger hunts, chair massages, a 5K, Share-a-Shift nurse shadowing, blessing of the hands, snack carts and so much more.






Megan Money, DNP, MBA, RN, PCCN, NE-BC
Nurse Manager, 6S/WICU
Doctor of Nursing Practice, Organization Systems Leadership
Northwestern State University of Louisiana
Danielle Weber, DNP, MSM, RN-BC, NEA-BC
Chief Nurse Executive, ChristianaCare
Chief Nursing Officer, Wilmington Hospital
Doctor of Nursing Practice, Executive Leadership
Drexel College of Nursing and Health Professions
As a Magnet-recognized health system and the largest private employer in Delaware, ChristianaCare promotes a culture where learning opportunities for nurses are plentiful.
Nursing Residency Program
Our Nursing Residency Program is accredited with distinction as a Practice Transition Program by the American Nurses Credentialing Center Practice Transition Accreditation Program® (PTAP). In FY 24, we offered three nurse residency cohorts, serving units across our three campuses, that hire newly graduated RNs with fewer than 12 months of nursing experience:
10 primary curriculum tracks
Critical Care, Emergency, Float Pool, Labor and Delivery, Medical, Neonatal ICU, Perioperative, Postpartum, Progressive Care and Surgical
184 RN residents hired
95% retention rate overall 93.6%
average first-year retention rate across the program (compared to 85.4% for all residencies recognized by the ANCC’s PTAP)
Nursing Residencies and Fellowships contd.
Nursing Fellowships
ChristianaCare Nursing Fellowships are for nurses with more than 12–24 months of experience who are transitioning to new workplace settings. Currently, practice settings that hire Nurse Fellows include Post Anesthesia Care Unit, Heart & Vascular Interventional Services, Interventional Radiology or Cath Lab, Operating Rooms and the Float Pool ICU team.
ChristianaCare’s advanced practice clinicians (APC) Fellowships are for recently graduated APCs seeking to deliver high-quality, exceptional care experiences for our patients.
ChristianaCare shapes the future of nursing through extensive collaborations with premier nursing schools. We provide undergraduate and graduate students with valuable clinical experience alongside leading clinicians. Additionally, we collaborate with nearby middle and high schools to spark and nurture enthusiasm for the field of nursing.
UNDERGRADUATE STUDENT SUPPORT
970 undergraduate students supported 53,915 undergraduate clinical and preceptorship hours with ChristianaCare nurses and patients in FY 24.
GRADUATE STUDENT SUPPORT
90 graduate students supported
90 rotations, 81 were ChristianaCare employees
1,100 hours supported
ChristianaCare supports graduate-level nursing students through our Nursing Advancement Scholarship Program and preceptorships. In FY 24, this support included nurse practitioner and clinical nurse specialist students, neonatal nurse practitioner students, psychiatric mental health nurse practitioner students, nurse midwifery students, and doctor of nursing practice students.
documented graduate-level preceptorships
ChristianaCare partners with MentorLead, a cloud-based app that specializes in facilitating health care mentoring, to offer user-friendly mentorship matching for nurses on the clinical ladder (including nursing students), APCs and caregivers aspiring to or holding leadership roles.
Interested caregivers create a profile — as either a mentor, mentee or both — that includes information about themselves and their professional role and goals for mentorship. The app then matches people based on similar characteristics and goals. This program goes beyond just matching: it offers a dedicated workspace for goal tracking, communicating and collaborating once pairs have matched, ensuring a successful mentoring experience.
Engagement has been robust since the app’s launch in FY 23, especially among Clinical Ladder caregivers.

Carol Abdill, MSN, RN, CRNI, vice president, Delaware Board of Nursing
V. Sheryl Amore, MSN, MSM-HCA, RN, Chi Eta Phi Sorority, Inc., chair, Tau Eta Chapter, Nominating Committee
Lauren Barone, MSN, RN, OCN, LNCC, NPD-BC, president, Oncology Nursing Society, Delaware Diamond Chapter
Gary Bollinger, BSN, RN, CEN, member, Institutional Review Board
Stefanie Bonis, BSN, RN, member, Preventing Child Abuse Delaware Board
Maria Brown, MSN, RN, PCCN, CNL, president-elect, Delaware Organization for Nursing Leadership
William Bryant, DNP, MBA, RN, CNOR, NE-BC, member, Glasgow Medical Board
Michelle Collins, DNP, APRN, CNS, ACNS-BC, NPD-BC, NEA-BC, LSSBB, member, Coalition for Nurse Wellbeing Advisory Board; member, National Nurse Wellbeing Consortium Advisory Board; president, Delaware Organization for Nursing Leadership
Ric Cuming, EdD, RN, NEA-BC, FAAN, member, DAISY Foundation Board of Directors
Beth Dauphin, MSN, RN, OCN, NPD-BC, interim secretary and membership chair, Oncology Nursing Society, Delaware Diamond Chapter
Julia Frawley, MSN, RN, CMSRN, public member-vice president, Delaware Board of Examiners of Nursing Home Administrators
Meghan Hormanski, MSN, RN, OCN, treasurer, Oncology Nursing Society, Delaware Diamond Chapter
Mary Jones-Gant, MSN, FNP-C, RRT, CNS-BC, CM-BC, member, Special Olympics Delaware
Allison Juhl, MSN, RN, MEDSURGBC, CNOR, member, Association of Perioperative Registered Nurses Wilmington Chapter
Paige Kafantaris, BSN, RN, CEN, FNE, founder and president, International Association of Forensic Nurses Delaware Chapter
Denise L. Lyons, DNP, APRN, AGCNS-BC, CPHQ, member, Wilmington University DNP Program Advisory Board
Amy Mackley, MSN-PCNS, RNC-NIC, CCRC, member, Delaware Nurses Association Editorial Advisory Committee
Tabe Mase, MJ, MSN, FNP-C, CHC, COHN-S, president, Choir School of Delaware
continued on next page
contd.
Reina McAndrew, MS, APRN, FNP-BC, SCRN, chairperson, Delaware Stroke System of Care Public Education Committee
Paige Merring, MSN, RN, CCRN, NEA-BC, member, Healthy Nurse Healthy Delaware Advisory Board; secretary, Delaware Organization for Nursing Leadership
Ashley Oncay, MSN, RN, CNOR, NPD-BC, president-elect and secretary, Association of periOperative Registered Nurses Wilmington Chapter
Greg O’Neill, MSN, APRN, AGCNS-BC, NPD-BC, NEA-BC, member, Literacy Delaware, Vice Chair and Advisory Board, Delaware Literacy Alliance
Ann Painter, secretary, Delaware Academy of Medicine — Delaware Public Health Association
Jennifer Painter, DNP, APRN, CNS, NEA-BC, NPD-BC, OCN, AOCNS, LSSBB, immediate past president, Delaware Organization for Nursing Leadership
Laura Rausch, MSN, PCCN, MEDSURG-BC, associate membership growth director, New Castle County, Delaware Nurses Association
Jessi Rhoades, MSN, MBA, RN, RACR, member, Delaware Workforce Development Board
Lindsey Safian, MSN, RN, RNC-OB, EFM member, Cecil County Child Fatality Review Board
Kimberly Schoeffler, MSN, RN, RNC-NIC, treasurer, Delaware Association of Neonatal Nurses
Allison Steuber, MSN, RN, NE-BC, president-elect, American Association of Critical Care Nurses Diamond State Chapter
Kara Streets, MS, BSN, RN, CEN, NE-BC, member, Board of Certification for Emergency Nursing, Exam Construction Review Committee
Michael Szeliga, MSN, APRN, AGCNSBC, CMSRN, CPHQ, director, Academy of Medical-Surgical Nurses
Kelley VanHorn, CNOR, treasurer, Association of periOperative Registered Nurses Wilmington Chapter
ChristianaCare’s Cardiovascular Critical Care Complex earned a gold-level Beacon Award from the American Association of CriticalCare Nurses for the fourth consecutive time, and ChristianaCare’s 4E, a cardiovascular step-down unit at Christiana Hospital in Newark, received a silver-level award.
Of the six Beacon Award-winning patient care units currently in Delaware, all are at ChristianaCare. The others are the Transitional Medical Unit and 3C Intermediate Medical Unit (silver); the Surgical Critical Care Complex (silver); the Transitional Surgical Unit (silver); and the Medical Intensive Care Unit at Christiana Hospital (a recordsetting five-time gold winner).


Nursing Awards and Recognitions contd.
DAISY Awards
Jessica Aliff, BSN, RN MICU, Newark Campus
Regina Beardsley, BSN, RN 5B, Newark Campus
Sandra Baker MSU, Cecil County Campus
Sarah Black, BSN, RN Labor & Delivery, Newark Campus
Cammy Budnavage, RN HomeHealth
Carrie Crabill, BSN, RN SSU, Cecil County Campus
Amanda Crowe, BSN, RN-BC 4N, Wilmington Campus
Maureen Dominelli, BSN, RN
Helen F. Graham Cancer Center & Research Institute
Camille Ferraro, BSN, RN 5B, Newark Campus
Stephanie Fulton, BSN, RN, CCRN 3C, Newark Campus
Casey Geary, LPN Acute Care for the Elderly, Wilmington Campus
Tammi Gorman, RN, C-EFM, RNC-OB Family Birth Center, Cecil County Campus
Ashley Janocha, BSN, RN 5B, Newark Campus
Dawnell Keeler, RN 7E, Newark Campus
Colleen Mahoney, BSN, RNC-MNN 6M/7M, Newark Campus
2024 DAISY Team Awards

Intensive Care Unit Cecil County Campus

Neonatal Intensive Care Unit Newark Campus
Terri-Beth Mimms, RN 4C, Newark Campus
Kristina Pansa, BSN, RN MICU, Newark Campus
Jennifer Peticacis, BSN, RN Labor and Delivery, Newark Campus
Madison Pritt, BSN, RN, ONC 7S, Wilmington Campus
Paige Reynolds, BSN, RN Emergency Department, Cecil County Campus
Michelle Shaffer, RN Emergency Department, Cecil County Campus
Kelin Stanley, BSN, RN, CCRN, GERO-BC MICU, Newark Campus
Lauren Turner, BSN, MEDSURG-BC, CAPA Perioperative Services, Wilmington Campus
Melissa vanNeerden, MSN, APRN, NP-C, AGPCNP-BC Center for Virtual Health
Juliet Westermann, BSN, RN, CCRN WICU, Wilmington Campus
Taylor Wood, BSN, RN 8S, Wilmington Campus


























ChristianaCare’s FY 24 Magnet Nurse of the Year is Clinical Nurse Specialist Brittany Anderson, MSN, APRN, AGCNS-BC, CCRN, CEN, an exemplary, inspirational nurse and colleague. Anderson cares for critical patients, many with complex issues or social needs. She holds a particular interest in helping people living with disabilities navigate care. As co-chair of the DiverseABILITIES Employee Resource Group, she has improved the process for bringing people with disabilities into care. A data-driven leader, Anderson has helped reduce OR-attributed HAPI rates by 88% from 2020 to 2022. Her contribution to post-operative acute kidney injury rates has been significant. As co-lead of the Acute Kidney Injury Workgroup, she has structured monthly stakeholder meetings to improve these rates. From January 2023 to March 2024, the post-operative acute kidney injury rate decreased from 10% to 6%.
Delaware Today’s list of Top Nurses for 2024 included more than 115 ChristianaCare nurses, representing all care areas and levels of the nursing practice. Congratulations to our honorees!
Scan the QR code to view the full list of awardees.
ChristianaCare nurses were named in Delaware Today's list of Top Nurses in 2024
The annual ChristianaCare Way Awards recognize multidisciplinary teams of caregivers as innovators in their areas of specialty or interest. There were 46 entries for this year’s awards, and of the 23 winning projects all but one were nurse-led, co-led, or included nurses on the team.
President's Award
Clean Catheter, Happy Bladder: A CAUTI Prevention and Foley Vacation Project
Transformation Award
Mastering the Mortality Matrix
Value Award
Maximizing Value of Type and Screen Testing for Obstetrical Patients
Strengthen the Core: Safety Gold Award Don’t Wait! A Smart Zone Alert Prevents HospitalOnset C. difficile
Strengthen the Core: Safety Silver Award
Suicide Prevention Pathway
Strengthen the Core: Quality Gold Award
Protecting the Preemie Brain:
Preventing Intraventricular Hemorrhage in Tiny Babies
Strengthen the Core: Quality Silver Award An Aspiration to Eliminate Aspiration: Implementing a Post-extubation Swallow Screen
Strengthen the Core: Quality Bronze Award Achieving Inpatients Daily Mobility Goal
Strengthen the Core: Flow Gold Award Streamlining Success: Enhancing Efficiency in Express Admissions
Strengthen the Core: Flow Silver Award The Newborn Hospital
Stay: Maximizing Value Without Sacrificing Patient Experience
Strengthen the Core: Flow Bronze Award Let’s Get Me
End Disparities Award Expansion of HighLevel Imaging on the Wilmington Campus: A Multi-Modality Approach
Radically Simplify Access Gold Award
Increasing Wilmington OR Ophthalmology Surgery
First Case On-Time Starts
continued on next page
ChristianaCare Way Awards contd.
Radically Simplify Access Silver Award and Peoples Choice Award
Access Made Easy: Improving WAM Follow-up Appointments
Enable Every Caregiver to Thrive Award
Daring to De-escalate: Increasing Caregiver Access to Workplace Violence Education
Accelerate Growth: Environmental Sustainability Award
Using an Electronic Tool for MRSA Surgical Status Documentation
Magnet Transformational Leadership Award
Innovating Nursing Practice: Virtual Care Nurse Model Delivers Outcome Improvements
Magnet Exemplary Professional Practice Award
Fall Reduction in the Clinical Decision Unit-A Standardized Approach
Magnet Structural Empowerment Award
Reduce Inpatient HAPI rate by 30% in FY 23 ChristianaCare, Union Hospital
Magnet New Knowledge, Innovations & Improvement Gold Award Harry, Not All Wizards Are Good! Obliviating the Medication
Administration Wizard
Magnet New Knowledge, Innovations & Improvement
Silver Award
To Using the Ipsilateral Arm in Breast Cancer Patients: A Practice Change
Zero Hero Award Whitney Lane
The annual Dot Fowler Award honors an exemplary RN III or RN IV caregiver for his or her passion for the nursing profession and exemplary teaching, mentoring, leadership and service. Congratulations to our FY 24 awardee, Jessica Johnson (center), BSN, RN, CCRN, pictured here with (left to right) Bridget Bieber, MSN, RN, CCRN, BC-NPD, Robyn M. Dougherty, MBA, MSN, RN, CCRN, Amanda E. Latina, MBA, MSN, RN, TCRN, and Caitlin E. Draper, BSN, RN-BC.

Every May, during Nurses Month, ChristianaCare’s Excellence in Nursing Awards shine a spotlight on exceptional nurses. In FY 24, we celebrated the awards with recipients on all our campuses. In total, 135 nurses received awards.
Scan the QR code to view the full list of awardees.
ChristianaCare nurses received Excellence in Nursing Awards FY 24
Tabe Mase, MJ, MSN, FNP-C, CHC, COHN-S, director of caregiver health services, was honored by the African Diaspora Advisory Board of Prince George’s County with the board’s 2023 Phenomenal Woman Award.
Mase, who vaccinated President Biden and the nation’s First Lady in 2020, received the award for her role in programming that helped health care workers affected by and recovering from COVID-19 return to work.
Rosemary C. Polomano, Ph.D., RN, FAAN, nurse scientist, Department of Nursing Research and Evidencebased Practice, was selected to serve on the Pacific Northwest Evidencebased Practice Center, Oregon
Health & Science University, National Guideline Development Group and Technical Expert Panel.
ChristianaCare HomeHealth’s Camden Branch received a SHPBest™ TOP 20% Superior Performer Award for HOME HEALTH Patient Satisfaction for 2022. SHP is the vendor HomeHealth uses to monitor and improve performance for patient outcomes and patient satisfaction. The SHPBest™ program acknowledges home health agencies that consistently provide high-quality service to their patients.
continued on next page
National and regional nursing awards contd.

ChristianaCare’s Wilmington Hospital Emergency Department was one of 53 emergency departments worldwide to receive the Emergency Nurses Association Lantern Award for 2023. The award recognizes the excellence of its caregivers in incorporating evidence-based practice and innovation.
Michelle Collins, DNP, APRN, CNS, ACNS-BC, NPD-BC, NEA-BC, LSSBB, vice president of Nursing Professional Excellence, received a Distinguished Alumni Award from Wilmington University.
Paige Kafantaris, BSN, RN, CEN, FNE, forensic nurse, Newark Campus Emergency Department, was
International Association of Forensic Nurses’ member of the month for February 2024.
Danielle Weber, DNP, MSM, RN-BC, NEA-BC, chief nurse executive, and Michelle Collins, were named fellows in the 2024-25 cohort of the Johnson & Johnson Nurse Innovation Fellowship Program.

ChristianaCare was named by U.S. News & World Report to its 20232024 Best Hospitals as a High Performing Hospital for 11 conditions and two procedures. This is the highest distinction a hospital can earn for U.S. News’ Best Hospitals Procedures & Conditions ratings.
The Junior Board of ChristianaCare made two gifts, totaling $62,000, to our highly acclaimed and highly valued Forensic Nurse Examiners program.
Our specially trained forensic nurses are part of our Emergency Department teams and provide compassionate physical and emotional care to the victims of crimes while also carefully collecting and preserving evidence.

In May, Delaware Gov. John Carney awarded our full-time team of 25 forensic nurses the Compassionate Champion Award in health care for their innovative, dedicated approach to care. The recognition is awarded by the Family Services Cabinet Council, Trauma Matters Delaware and the Governor’s Office and is the latest acknowledgment for this one-of-a-kind team in the region.
In FY 24, the Junior Board also gave $40,000 to support nursing scholarships at ChristianaCare. The gift helps offset the cost of tuition and textbooks for students pursuing their dreams of a nursing career.

ChristianaCare Nursing never rests with the status quo. Systemwide, our caregivers exemplify creativity, innovation and excellence. They contribute new knowledge, create new technologies and drive evidence-based care that advances the art and science of the nursing profession itself.
ChristianaCare’s Center for Nursing Innovation is a collaboration across four areas — Nursing Excellence, Nursing Quality and Safety/Research and EBP, Clinical Informatics and Professional Development. It not only drives innovation across the Nursing team, the center defines it — the team recently worked with the Technology and Innovation Council to establish a definition of nursing innovation at ChristianaCare:
ChristianaCare empowers all nursing caregivers in the exploration, development, implementation and evolution of innovation. The contributions of every nursing caregiver in creating and introducing new ideas, methods and solutions are celebrated to promote a culture of innovation.
This definition is our North Star for Nursing innovation systemwide. As such, it guided the creation of Nursing’s first-ever Nurses' Month Innovation Speaker Series, a learning opportunity for all caregivers to connect with colleagues, enhance skills and accelerate innovation that shapes the future of health care.
NurseHack4Health teams work to solve vexing health care challenges
ChristianaCare’s Center for Nursing Innovation led Nursing caregivers in the national NurseHack4Health “hackathon.” Sponsored by Microsoft, Johnson & Johnson, and SONSIEL, the annual NurseHack4Health allows nurses and other innovators to collaborate in real time to develop tech-based products that can help address today’s most pressing health care challenges.
32 countries
100 teams
3 of 10 finalists from ChristianaCare
ChristianaCare’s four hackathon projects:
• Expanding Virtual Acute Care Delivery at ChristianaCare — Michelle Collins, DNP, APRN, CNS, ACNS-BC, NPD-BC, NEA-BC, LSSBB, with Maria Brown, MSN, RN, CNL, PCCN; Shelby Durgin, MSN, RN-BC; Paige Merring, MSN, RN, CCRN, NEA-BC; Dannette Mitchell, MSN, APRN, ACNS-BC, CCRN, FCNS; Melanie Ries, BSN, RN-BC, and Rochelle Williams, BSN, RN. (Finalist)
• Helping Engage, Attract, Retain & Train — Jennifer Painter DNP, APRN, AOCNS, NEA-BC, NPD-BC, OCN, LSSBB, with Meghan Blomquist, MSN, RN, CEN, NPDBC; Beth Dauphin, MSN, RN, OCN, NPD-BC, CUA; Bridget Remel, MSN, APRN, NEA-BC, AGCNS-BC, NPD-BC, CCRN-K, and Amy Sutor, MSN, RN, CCRN, NPDBC. (Finalist)
• Building a Disability Support Network: An Innovative Approach to Providing Equitable and Effective Care — Kate Shady, PH.D., RN, OCN, with Brittany Anderson, MSN, APRN, AGCNS-BC, CCRN, CEN; Madalene Zale, MPH, and Jacqueline Ortiz, M. Phil. (Finalist)
• “Safety Sidekick” Application — Susan Mascioli, MS, BSN, RN, NEA-BC, CPHQ, LSSBB, CPPS, with Nathalie Romance, MSN, RN, CEN, and Tara Woodside, DNP, RN, CALA.
ChristianaCare is in the vanguard of care delivery with our virtual acute care nursing (VACN) program, launched in 2022. Offering a critical extra set of eyes and connection to patients, our virtual nurses are helping to alleviate staffing shortages and improve patient experience. The VACN program provides an innovative care delivery model with nurses using virtual technology to provide any inpatient care that doesn’t require in-person at-the-bedside care. Most importantly, patients are pleased: 78% of patients who used virtual nursing during their hospital stay liked it.

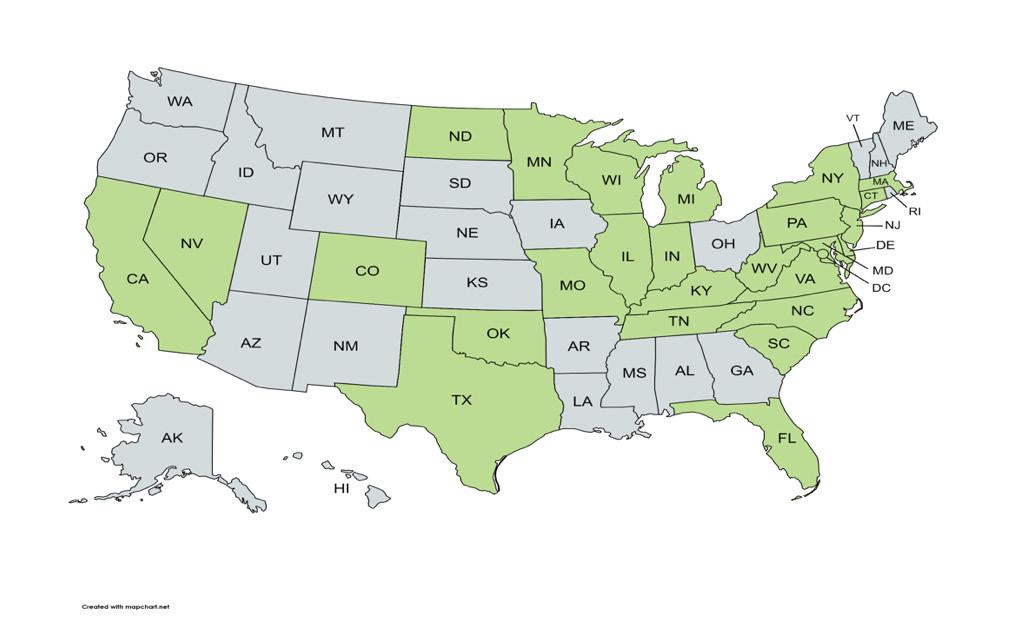
Nurse innovation leaders are also taking VACN on the road, speaking nationwide on the program’s impact, vision and scalability.
549 acute care beds
72,825 calls initiated by virtual nurses
27,839 calls initiated by patients/caregivers
26,730 patients participated in VACN program
As of May 2024
Virtual Acute Care Nursing Impact
Meetings/presentations given to organizations for VACN
The Evidence-based Practice (EBP) Fellowship is designed to provide nurses with foundational knowledge, skills and specific competencies in EBP. Nurses selected for the 12-month fellowship receive structured training and mentoring. Nurse leaders, nurse educators, nurse scientists and clinical experts also serve as internal consultants, supporting the training of fellows and helping them in EBP activities.
In FY 24, there are five fellows and three mentors working with them. Fellows Jordan Prieto, MSN, BA, RN-BC, CWOCN; Samantha Stafford, MSN, RN, RN-BC and Ibelise Smith, BSN, RN, are focused on HAPI prevention; fellows Ingrid Hausner, BSN, RN, PCCN, and Joana D. Lapinid, MSN, RN, PCCN, are focused on mobility in heart failure patients and compassion fatigue among surgical nurses, respectively.
Our Nursing team is determined to achieve Zero Harm across all patient safety indicators. In FY 24, a multidisciplinary, systemwide Fall Prevention & Mobility team redesigned several protocols and implemented new tools to help preempt acute care falls with major injury, including:
• Updating ChristianaCare’s electronic medical record (EMR) system to send nurses’ orders for mandatory interventions when a patient is at high risk for falls
• Redesigning orthostatic vital sign documentation in the EMR to make it more user-friendly for staff.
Acute Care Fall Rate (Newark, Wilmington and Cecil campuses)
• Familiarizing staff with built-in bed exit alarms by adding a QR code to the foot of all beds with links to educational resources about the bed.
Acute Care Fall Rate Newark, Wilmington and Cecil County campuses Fall Rate Falls Acute Care includes W&C units. Excludes inpatient BH and Rehab units.
















































• Revising and updating the Fall Perfect Care bundle questions based on staff feedback.
• Partnering with ChristianaCare’s Health & Technology Innovation Center on a fall Ideation workshop and several fall prevention prototypes.
• Developing a new Fall Care Management Guideline for procedural areas.
• Standardizing weekly fall reviews on our three campuses and sharing lessons learned through a new monthly newsletter called The Metric for all inpatient Nursing caregivers, which highlights key details, lessons learned and paths forward for our most common Nursing Sensitive Indicators in acute care.
Denise Lyons, DNP, APRN, AGCNS-BC, CPHQ, Patricia Curtin, MD, FACP, CMD, co-lead this work for Nursing. And Mike Knorr, MSN, RN, NEA-BC, and Kristen Foulk, MSN, MS, RN, PCCN-K, NEA-BC, formed a Fall Standardization and Accountability team to standardize fall prevention strategies across all inpatient units on all three campuses.
Since Moxi first rolled the floors of Christiana Hospital in 2022, the “cobot” — or collaborative robot — has become a unique “colleague” and delight for patients as it assists caregivers on our Newark campus. Moxi performs lower-level tasks, freeing up caregivers to focus on more important work caring for patients. Moxi is now at the next level of innovation with a new pilot of electronic health record integration: The cobot will automatically deliver certain supplies without a nurse’s request.
ChristianaCare was the first health system in the Philadelphia region to pilot the cobot, and we continue to learn about the value it brings to the health care system and hospital workforce. A team of ChristianaCare nurse researchers and others have completed their first study after the implementation of Moxi.
“Integrating Collaborative Robots into a Complex Hospital Setting: A Qualitative Descriptive Study,” by Susan Birkhoff Ph.D., RN; Paige Merring, MSN, RN, CCRN, NEA-BC; Amanda Spence, BSN, RN-BC;, and Wendy Bassett and Stephanie Roth, MLIS, concluded that cobots have the potential to augment hospital workflows that were once exclusively performed by hospital staff and clinicians. To integrate cobots seamlessly and effectively into hospital workflows, in-person human assistance will be required until the cobots can transition to a model of increased autonomy.
20,804 deliveries, most from pharmacy to nursing units
13,479 active hours
70+ units using Moxi

According to The Commonwealth Fund, a nonprofit that supports independent research on health care issues, the health care industry is responsible for 8.5 % of total greenhouse gas emissions in the United States. ChristianaCare takes our obligation seriously to be stewards of the environment, reduce greenhouse gas emissions and lead in sustainability efforts.
The health system’s nurse-inspired and -led Environmental Sustainability Caregiver Committee engages caregivers in identifying sustainability initiatives and driving systemwide environmental goals.
In FY 24, during Earth Month, the committee hosted its first daylong climate-focused conference for caregivers. The virtual and in-person Climate and Health Conference explored the link between our health and the environment and how caregivers can promote health through climate change education, policy and practice.
Pictured below: Clinical Nurse Specialist Greg O’Neill, MSN, APRN, AGCNS-BC, NPD-BC, NEA-BC, and Nurse Practitioner Deanna Benner, MSN, APRN, WHNP, co-chairs of ChristianaCare’s Environmental Sustainability Caregiver Committee, helped organize the health system’s Climate and Health Conference.
90 caregivers in attendance 10 speakers on topics related to excessive heat and weather, population health, sustainable diets, mental health and more

Publications and Presentations
Publications
• Hailey Bowser. (2024). “The Best Decision.” Nursing for Women’s Health. https://doi.org/10.1016/j.nwh.2024.04.001
• Michelle Collins. (2023). “The Tech Behind: How ChristianaCare Uses Tech to Maintain Patient Care Despite the Nursing Shortage.” Technical.ly, October 2023.
• Michelle Collins and Stephanie McClellan. (2023). “Innovation Leadership: Cultivating a Spirit of Inquiry and Innovation for Nurses.” Delaware Nurses Association Reporter, 48(4),10-11.
• Michelle Collins and Maria Brown. (2023). “Virtual Acute Care Nurses: Implementing Successful Change.” Delaware Nurses Association Reporter,48(2),10.
• Jillian Crane. (2023). “Worth the Extra Time.” Nursing 2023, 53(9), 51-52. https://doi.org/10.1097/01.nurse.0000946772.63444.88
• Gina Davis and Richard Choi. (2023). “Experiencing the Spectrum of Care: From Patient to Nurse in the NeuroICU.” Neurocritical Care Society Stories of Hope. https://currents.neurocriticalcare.org/Stories-of-Hope/Article/experiencingthe-spectrum-of-care-from-patient-to-nurse-in-the-neuroicu
• Colleen Fischer. (2023). “Valuable Support after My First Adverse Event.” Nursing for Women's Health, 27(4), 317-318. https://doi.org/10.1016/j.nwh.2022.11.007
• Lija Gireesh, Tabe Mase, and Marci Drees. (2024). “Implementing a Successful Influenza and Updated COVID-19 Vaccination Campaign Among Healthcare Workers in a Delaware Healthcare Facility.” Delaware Journal of Public Health, 10(1), 102-104. https://doi.org/10.32481/djph.2024.03.13
• Amanda Hafker. (2024). “Compassionate Care at End-of-Life.” Nursing 2024, 54(4), 48-49. https://doi.org/10.1097/01.nurse.0001007660.43768.22
• Mary Ellen Hendrickson. (2024). “He Wasn't Alone.” Nursing 2024, 54(3), 41-42. https://doi.org/10.1097/01.nurse.0001006308.10457.e1
• Jason Keller. (2023). “A Sense of Belonging.” Nursing 2023, 53(9), 49-50. https://doi.org/10.1097/01.nurse.0000946796.40872.45
• Kathleen Luckner and Maureen Seckel. (2024). “Understanding the Evolving Pathophysiology of Coronavirus Disease 2019 and Adult Nursing Management.” Critical Care Nursing Clinics of North America. https://doi.org/10.1016/j.cnc.2024.01.002
continued on next page Bolded names are ChristianaCare nurses
Publications contd.
• Reina McAndrew and Mary Ciechanowski. (2023). “Nursing Care of Delaware's Stroke Patients.” Delaware Journal of Public Health, 9(3), 34-37. https://issuu.com/dam-dpha/docs/djph_-_neurological_impairment_and_ stroke?fr=xKAE9_zU1NQ
• Paige Merring, Michelle Collins, Maria Brown, and Julie McCulloh Nair. (2024). “Nurses' Evaluation of a Professional Practice Model.” Nursing 2024, 54(1), 42-48. https://doi.org/10.1097/01.nurse.0000995612.43818.f2
• Julia Pala. (2024). “Making a Difference.” Nursing 2024, 54(1), 34. https://doi.org/10.1097/01.nurse.0000995600.46681.db
• Marisa Schilling. (2023). “Let's Talk.” Nursing 2023, 53(9), 47-48. https://doi.org/10.1097/01.nurse.0000946800.93430.99
• Catherine Shull Fernald and Tamekia Chisholm. (2023). “The Power of Mentorship to Prepare the Next Generation of Nurse Leaders.” Delaware Nurses Association DNA Reporter. 48(4).
• Susan Birkhoff. (2024, April). Technology Focused Research in Academia and in Clinical Practice. Villanova University School of Nursing.
• Susan Birkhoff. (2024, April). Empowering Nursing Innovation & Implications for Population Health. University of Delaware School of Nursing.
• Susan Birkhoff. (2024, March). Creating Virtual Reality Storytelling Experiences for Oncology Family Caregivers. Junior Investigators Network.
• Susan Birkhoff. (2024, February). Implementing Collaborative Robots (Cobots) into a Complex Acute Care Hospital Setting. Junior Investigators Network.
• Susan Birkhoff. (2023, November). Innovation in Nursing. Invited keynote speaker, Annual Nursing Research Conference hosted by ChristianaCare, virtual.
• Susan Birkhoff. (2023, November). Innovations in Healthcare Led by Nurse Scientists. Veterans Affairs Nurse Scientist Retreat, virtual.
• Susan Birkhoff & Gregg Springan. (2023, October). Evaluating Robots in Nursing. ANCC Magnet Conference, Chicago, IL.
• Maria Brown and Michelle Collins. (2023, November). Virtual Acute Care Nursing: Impacting Care Delivery and Outcomes with One Click. Podium presentation at 18th Annual Nursing Research Conference, virtual.
• Michelle Collins. (2024, May). Virtual Nursing Care Model. Institute for Healthcare Improvement, virtual.
• Michelle Collins. (2024, May). Magnet® Designation: Leading Excellence and Advancing Practice. Lee Health, virtual.
• Michelle Collins. (2024, May). Virtual Nursing: Leading the Future of Care in the Digital Age. National Healthcare Chief Nursing Officer Summit. Dallas, TX.
• Michelle Collins and Maria Brown. (2024, April). From 50 to 500 patients daily: Successfully Scaling Virtual Care. Podium presentation at Memorial Hermann Nursing and Clinical Innovation Summit in Houston, TX.
• Laura Dechant. (2024, March). Reducing Length of Stay: CNS Implementation of IV Sotalol Program. Podium presentation at National Association of Clinical Nurse Specialists Annual Conference in New Orleans, LA.
• Kiersten Edmondson and Joseph Fiorelli. (2023, November). Project War Games. Poster presentation at 18th Annual Nursing Research Conference, virtual.
• Shannon Guzman and Tiffani Lee. (2023, August). Every Patient, Every Time: Reducing Preventable Falls on an Acute Stroke Treatment Unit. Poster presentation at AANN Stroke Conference in Louisville, KY.
• Anna Hewitt. (2023, September). Communication, Care and the Community. Lecture at MidAtlantic AETC, virtual.
• Reina McAndrew. (2023, August). Panelist for Jefferson College of Nursing Professional Practice Panel.
• Paige Merring and Amanda Spence. (2023, November). Not Your Typical Robot: Use of Robotics in Nursing Practice. Podium presentation at 18th Annual Nursing Research Conference, virtual.
• Paige Merring and Amanda Spence. (2024, March). Not Your Typical Robot: Use of Robotics in Nursing Practice. Poster presentation at Penn Medicine Nursing Research Conference, virtual.
• Paige Merring and Amanda Spence. (2023, November). Not Your Typical Robot: Use of Robotics in Nursing Practice. Podium presentation at Memorial Hermann Clinical Innovation Summit in Houston, TX.
continued on next page
Presentations contd.
• Paige Merring and Amanda Spence. (2023, October). Not Your Typical Robot: Use of Robotics in Nursing Practice. Poster presentation at ANCC Magnet Conference in Chicago, IL.
• Paige Merring and Maria Brown. (2024, March). Empowering Nurses as Leaders through a Governance Bootcamp. Podium presentation at Creative Healthcare Management International Governance Summit, virtual.
• Paige Merring and Maria Brown. (2024, June). Empowering Nurses as Leaders through a Governance Bootcamp. Podium presentation at AONL Professional Governance Leadership Conference in Chicago, IL.
• Paige Merring and Michelle Collins. (2024, June). Aligning Governance and a Nursing Strategic Plan to Drive Outcomes. Poster presentation at AONL Professional Governance Leadership Conference in Chicago, IL.
• Evalyne Mwangi. (2023, August). Development and Implementation of a Nurse Practitioner-driven Discharge Bundle Process Among Hypertensive Patients in an Acute Care Setting. Poster presentation at Graduate Nursing Student Academy in Washington, DC.
• Stacy Noel. (2023, November). Self-care in Healthcare. Podium presentation at Mid-Atlantic Education and Training Center Program in Smyrna, DE.
• Stacy Noel. (2023, October). Self-care in Healthcare. Podium presentation at Delaware Diamond Oncology Nursing Society Conference in Newark, DE.
• Stacy Noel. (2023, October). Healing Touch and Tree Meditation. Podium presentation at ANCC Magnet Conference in Chicago, IL.
• Stacy Noel and Michelle Collins. (June 2024). Effects of Healing Touch Training on Nurses Stress Levels. Poster presentation at American Holistic Nurses Association in Rochester, MN.
• Melanie Ries and Michelle Collins. (2023, October). Hybrid presentation at ANCC Magnet Conference in Chicago, IL.
• Michelle Ritona, Mathew Cohen, Alyssa Lanzi, Anna Saylor, Aaron Boulton, Jennifer Rittereiser, and James Ellison. (2023, November). Older Adults Who Screen Positive for Cognitive Impairment: Predictors of Follow-Up. Poster presentation at The Gerontological Society of America 2023 Annual Scientific Meeting in Tampa, FL.
• Kate Shady. Using the Ipsilateral Arm in Breast Cancer Patients – An EvidenceBased Practice Project. Podium presentation at Oncology Nursing Society Congress in Washington DC (2024, April). and 18th Annual Nursing Research Conference, virtual (2023, November).
• Kate Shady. (2024, February). A Multiple Methods Assessment of Factors Affecting In- Hospital Provider Communication with Adults with Communication Difficulties. Poster presentation at Penn Medicine Nursing Research Conference, virtual.
• Leslie Verucci. (2023, October). Providing Care to Prevent ED/Hospital Admissions and Delay in Treatment. Lecture at Vizient Clinical Workforce Conference in New Orleans, LA.
ChristianaCare nurse-led conferences
18th Annual Nursing Research Conference
In partnership with other Delaware health systems and universities, ChristianaCare held its 18th Annual Nursing Research Conference, The Power of Innovation in Nursing. The convening brought together professional nurses and students seeking to use research and evidence-based practices to improve patient outcomes and enhance the practice environment.










We serve our neighbors as respectful, expert, caring partners in their health. We do this by creating innovative, effective, affordable and equitable systems of care that our neighbors value.
We Serve Together Guided by Our Values of Excellence & Love
We anticipate the needs of others and help with compassion and generosity.
We embrace diversity and show respect to everyone.
We listen actively, seek to understand and assume good intentions.
We tell the truth with courage and empathy.
We accept responsibility for our attitudes and actions.
We commit to being exceptional today and even better tomorrow.
We seek new knowledge, ask for feedback and are open to change.
We use resources wisely and effectively.
We are curious and continuously look for ways to innovate.
We are true to our word and follow through on our commitments.

