10 minute read
Clinical Challenge: Bruising, Bleeding Gums, Nosebleeds in Young College Athlete
CONTENTS
M A R C H / A P R I L 2 0 2 1
12 Erectile dysfunction: early sign of CVD

21 Hepatitis C virus-associated skin lesions

25 Hand, foot, and mouth disease

31 Protection against harassment
FEATURES
5 Clinical Challenge: Bruising, Bleeding Gums,
Nosebleeds in Young College Athlete
Immune thrombocytopenia is a common autoimmune disease.
12 Erectile Dysfunction: Harbinger of Early
Cardiovascular Disease
Comanagement of cardiovascular disease risk factors through exercise and weight loss can improve erectile function.
16 The Impact of Obesity on Knee OA Symptoms and Surgical Outcomes
Weight loss is associated with reduced pain, improved function, and better quality of life in patients with knee OA.
DEPARTMENTS
1 From the Director
Weight Gain in the United States
4 Web Roundup
A summary of our most recent opinion, news, and multimedia content from ClinicalAdvisor.com.
21 Dermatology Clinic
■ Inflammation and Redness of the Fingernail Folds ■ Flat-Topped Papule With Wickham Line
25 Dermatologic Look-Alikes
Blisters on the Hands
31 Legal Advisor
Nurse Sues Over Sexual Harassment
MORE WAYS TO Follow us on Twitter FIND US! @ClinicalAdvisor Like us on Facebook facebook.com/TheClinicalAdvisor Visit us on the web ClinicalAdvisor.com
Download the app ClinicalAdvisor.com/App
EXCLUSIVE TO THE WEB AT THE WEB AT ClinicalAdvisor.com
NEWS
ClinicalAdvisor.com/News
Inappropriate Antibiotic Prescribing Common for Women With UTIs
A considerable proportion of women with uncomplicated urinary tract infections (UTIs) have inappropriate antibiotic prescribing; women living in rural areas also receive longer duration of therapy.
Coffee: A Cup a Day Keeps Heart Failure Away
According to an analysis of 3 large epidemiologic studies, increased co ee intake was linked to a reduced risk of developing heart failure later in life.
Black Infant Mortality Gap Decreases When Black Physicians Provide Care
Excess Black infant mortality rate is halved when Black newborns are cared for by a Black physician vs a White physician.
Fezolinetant showed positive results in phase 3 clinical trials with signi cant reductions found in the frequency and severity of vasomotor symptoms associated with menopause.
COVID-19 Convalescent Plasma Shows Trend Toward Early Survival Bene t
Patients who received convalescent plasma had a longer hospital stay compared with hospitalized patients who received standard therapy but a decreased risk for death at 7 and 14 days.
CLINICAL CHALLENGE
ClinicalAdvisor.com/CaseStudy
Brady Pregerson, MD
Case Study: Is It More Than Just a Migraine?
A 42-year-old woman with a history of chronic migraines presents for evaluation of a new headache that is different from the migraines she typically experiences. The pain onset is more rapid with vomiting occurring earlier in the headache course. The location of the pain is atypical for her: it is both frontal and occipital as opposed to being primarily frontal. See the full case at: ClinicalAdvisor.com/CaseMarch_April21
THE WAITING ROOM
Of cial Blog of The Clinical Advisor
ClinicalAdvisor.com/WaitingRoom
Jim Anderson, MPAS, PA-C, DFAAPA
Why Word Choice Matters
In recent years, there has been a gradual movement away from the word non com pliant in favor of the word non adherent to describe patients who do not listen to medical advice or follow clinicians’ recommendations.

MY PRACTICE
ClinicalAdvisor.com/MyPractice

Kristin Della Volpe
NP and PA Experts Discuss Controversy Over USDA-HHS Dietary Guidelines
Experts debate the USDA-HHS’ decisions on sugar and alcohol intake limits in the updated Dietary Guidelines for Americans, 2020-2025.
Clinical Challenge: Bruising, Bleeding Gums, Nosebleeds in Young College Athlete
Bruising and bleeding can be indicative of many conditions.
A21-year-old woman presents to a college health clinic with complaints of bruising easily. Reporting that the bruising began 3 weeks ago, the patient says she first noticed it on her distal arms after playing volleyball. She reports that the bruising never occurred before, although she played 8 years of volleyball including at college.
A review of systems is positive for bleeding gums, frequent nosebleeds, heavy periods, spotting between menstrual cycles, and a petechial rash on both legs. The patient reports that the rash developed after she was running. She also reports that running has become difficult and complains of a progressive decrease in exercise tolerance.
She denies fever, night sweats, weight loss, headaches, abdominal pain, fainting, dizziness, lightheadedness, chest pain, shortness of breath, blood in her stool or urine, and recent illness. Her last menstrual period was 2 weeks ago, and she denies any chance of pregnancy. She denies use of illicit drugs or any new prescription or over-the-counter medications and has no known drug allergies.
The patient is taking a contraceptive containing norgestimate and ethinyl estradiol. She has a medical history of iron-deficiency anemia but is not taking iron supplements. Her family history is significant for lymphomatoid granulomatosis (a rare lymphoma) in her paternal grandfather and leukemia in a maternal first cousin.
On presentation, the student appears well and is alert and oriented. Vital signs are normal (Table 1). Physical examination reveals ecchymosis on the

FIGURE 1. Ecchymosis on the left wrist. FIGURE 2. Petechiae of the left lower leg.

distal dorsal arms and the proximal medial legs bilaterally (Figure 1). Petechial spotting is noted on both lower extremities, as well as orally along the gum line (Figure 2). Heart sounds show a normal rate and rhythm without murmur, and lungs are clear to auscultation. She has no lymphadenopathy, abdominal tenderness, or palpable hepatosplenomegaly.
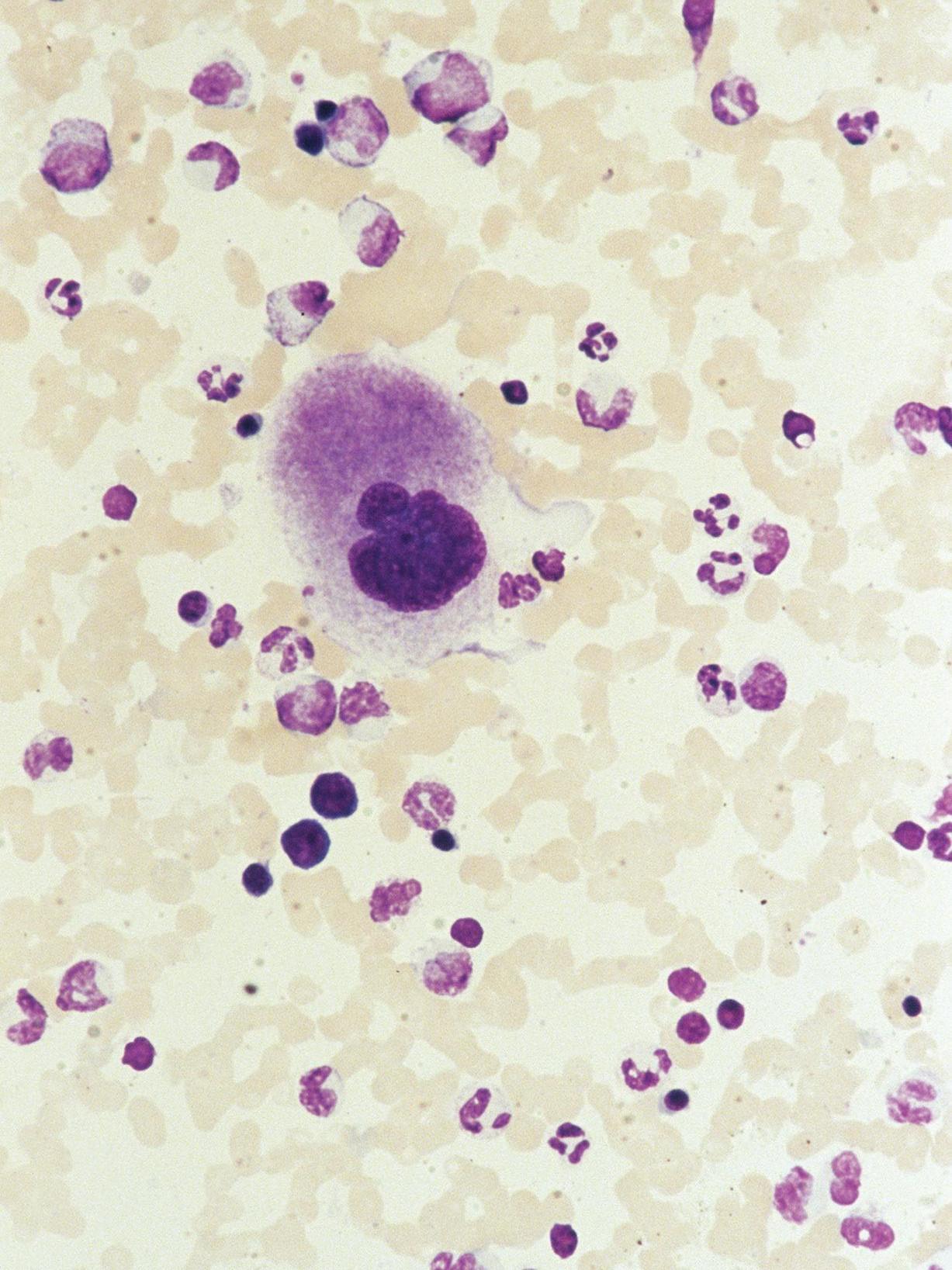
Outpatient laboratory testing is conducted immediately and shows a critically low platelet count and low hemoglobin, hematocrit, mean corpuscular volume, mean corpuscular hemoglobin, and ferritin (Table 2). Trace hemoglobin is detected in the urinalysis. Peripheral blood smear reveals severe thrombocytopenia and mild microcytic anemia, with no morphologic abnormalities.
The patient’s white blood cell count, comprehensive metabolic panel, erythrocyte sedimentation rate, C-reactive protein level, tickborne disease panel, prothrombin time/international normalized ratio, antinuclear antibody test, human chorionic gonadotropin test, and vitamin D, vitamin B12, and folate levels are normal.
Conditions considered in the differential diagnosis include trauma, anemia, infections such as mononucleosis or meningitis, Henoch-Schönlein purpura, drug-induced thrombocytopenia, immune thrombocytopenia (ITP), vasculitis, coagulopathies, myelodysplastic syndromes, and leukemia.
Discussion
The patient’s medical history, examination findings, and test results suggest a diagnosis of ITP (previously known as idiopathic thrombocytopenic purpura), which is a common autoimmune disease characterized by low platelet count (<100×109/L) and an increased risk for bleeding.1,2 It may present as an isolated thrombocytopenia or occur in the setting of additional autoimmune cytopenias (Evans syndrome), as a manifestation of a primary immunodeficiency, or secondary to an autoimmune condition or infection.2
Although the pathophysiology of ITP is unclear, several mechanisms have been proposed such as autoantibodies and
TABLE 1. Patient’s Vital Signs
Temperature, °F 97.6
Heart rate, bpm 72
Blood pressure, mm Hg 128/78
Respiratory rate per minute 16
Pulse oximetry, %
bpm, beats per minute 99 (on room air)
TABLE 2. Laboratory Results
Test Result Normal Reference Range in Womena
Ferritin, ng/mL 5 6-137
Hemoglobin, g/dL 11 12-16
Hematocrit, % 34.4 36-46
Mean corpuscular hemoglobin, pg/cell 24.9 26-34
Mean corpuscular volume, fL 77.8 80-100
Platelet count/L 1×109 140-440×109
a Normal reference ranges are based on laboratory used by author
cytotoxic T cells that target platelets and/or megakaryocytes.1 Immune thrombocytopenia affects people of both sexes and all ages, with a peak in childhood and a second and third peak in young adults and the elderly.3 In the United States, the incidence of ITP is approximately 2 to 5 per 100,000 patients per year.2
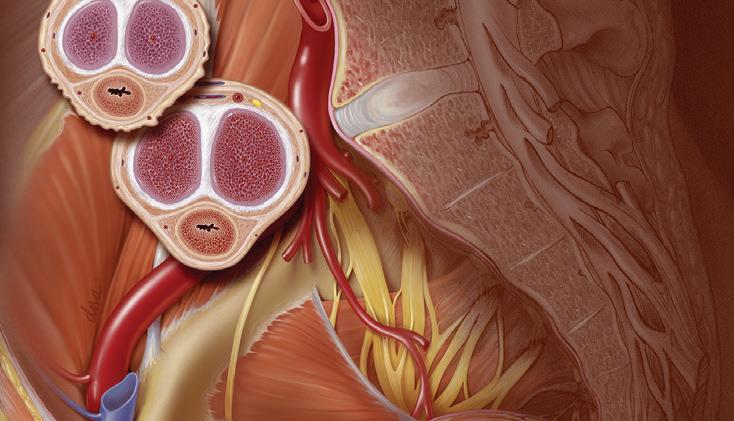
Platelets are critical to the maintenance of vascular integrity; thus, patients with ITP are at increased risk for bruising and spontaneous bleeding events.1 Patients with a platelet count of <30×109/L are at increased risk for severe bleeding (eg, intracranial hemorrhage, mucocutaneous bleeding, lower gastrointestinal bleeding, other internal bleeding, and menorrhagia).4 Patients with a platelet count of <10×109/L are at risk for life-threatening bleeding.
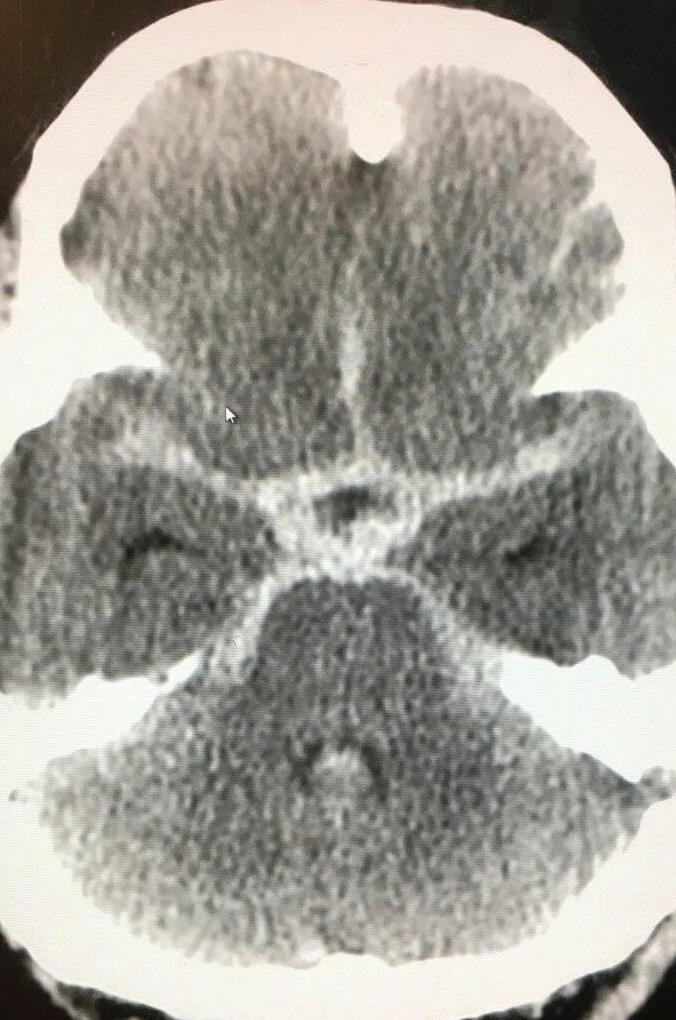
Deaths associated with ITP are rare and associated most frequently with spontaneous or trauma-induced intracranial hemorrhage.4 Intracranial hemorrhage reportedly occurs in 1.4% of adults and 0.4% of children with ITP, most of whom have chronic ITP.5 If severe bleeding occurs, rapid intervention with platelet transfusions in conjunction with continuous infusion of intravenous immunoglobulin G (IgG) therapy or emergent splenectomy may be lifesaving.6
The signs and symptoms of ITP are highly variable, and onequarter of patients are asymptomatic and diagnosed through routine blood tests.4 Symptoms primarily are related to bleeding in the skin or mucous membranes presenting as petechiae or purpura.6 Patients with platelet counts of ≥30×109/L usually do not require any treatment and can be managed with observation (Table 3).2 If adult patients require intervention, American Society of Hematology (ASH) guidelines recommend treatment with corticosteroids, which prevent the destruction of platelets by macrophages within the spleen.2 The ASH guidelines also include treatment recommendations for children.2
The prognosis of ITP is variable and appears to depend on age, with 1-year spontaneous remission rates in pediatric patients ranging from 74% in children younger than 1 year to 62% in patients aged 10 to 20 years.2 Spontaneous remission rates in adults range from 20% to 45% at 6 months.2
Conclusion
The patient in this case study was referred to the emergency department in response to her critical low platelet count. There the patient received a blood transfusion and high-dose steroids and was admitted to the hospital. The platelet count responded to therapy and began to rise. She was discharged with a platelet count of 38×109/L and diagnosed with ITP. She was sent home on oral steroids and advised to follow up with hematology. At her follow-up appointment with the hematologist, repeat laboratory studies revealed a decline in the platelet count to 3×109/L. This resulted in a second admission to the hospital. She received IgG therapy and, subsequently, the platelet count rose to 93×109/L. She received a total of 2 IgG treatments with good response, and there were no future treatments planned at that time. She moved back home, and no further updates were made. ■
TABLE 3. Selected American Society of Hematology Guidelines on Immune Thrombocytopenia in Adults2
Variable Recommendation
Adults with newly diagnosed ITP and a platelet count of ≥30×109/L who are asymptomatic or have minor mucocutaneous bleeding
Adults with newly diagnosed ITP and a platelet count of <30×109/L who are asymptomatic or have minor mucocutaneous bleeding
Adults with newly diagnosed ITP and a platelet count of <20×109/L who are asymptomatic or have minor mucocutaneous bleeding • Manage with observation • Corticosteroid treatment typically is not recommended
• Corticosteroid treatment is recommended over observation: —Prednisone (0.5-2.0 mg/kg/d for ≤6 weeks) —Dexamethasone (40 mg/d for 4 days) —If rapid response is important, dexamethasone may be preferred over prednisone —Monitor for side effects
• Admit to the hospital
Elizabeth Houser, CRNP, is a nurse practitioner at Indiana University of Pennsylvania, in Indiana, PA. She holds a MS in Nursing from Carlow University. Houser has been practicing in college health for 8 years and has an additional 5 years of emergency nursing experience.
References
1. Arnold DM. Bleeding complications in immune thrombocytopenia. Hematology. 2015:237-242. doi:10.1182/asheducation-2015.1.237 2. Neunert C, Terrell DR, Arnold DM, et al. American Society of Hematology 2019 guidelines for immune thrombocytopenia. Blood Adv. 2019;3(23): 3829-3866. doi:10.1182/bloodadvances.2019000966 3. Lambert MP, Gernsheimer TB. Clinical updates in adult immune thrombocytopenia. Blood. 2017;129(21):2829-2835. doi:10.1182/blood-2017-03-754119 4. European Group for Blood and Marrow Transplantation. Immune thrombocytopenia: a practical guide for nurses and other allied healthcare professionals. 2011. Accessed March 22, 2021. https://www.ebmt.org/ practical-guides-immune-thrombocytopenia. 5. Neunert C, Noroozi N, Norman G, et al. Severe bleeding events in adults and children with primary immune thrombocytopenia: a systematic review. J Thromb Haemost. 2015;13(3):457-464. doi:10.1111/jth.12813 6. Neunert C, Lim W, Crowther M, et al. The American Society of Hematology 2011 evidence-based practice guidelines for thrombocytopenia. Blood. 2011;117 (16): 4190-4207. doi:10.1182/blood-2010-08-302984






