














The American population is older than it used to be, according to new U.S. Census data.
With fewer young children, more baby boomers and even more centenarians, the country's median age is higher — at 38.8 — and the share of people aged 65 and up more substantial, the report showed.
Among the most notable numbers is that the share of people 65 and older grew by more than one-third between the 2010 census and the 2020 census, and that the number of people reaching age 100 grew from more than 53,000 to more than 80,000. Meanwhile, millennials became adults or aged into their 30s, and fewer children were born between 2010 and 2020.
What does that all mean?
“Many more people who have the genetic makeup and environmental exposures that increase one's chances of getting to 100, but who would have otherwise died of what are now readily reversible problems, are able to fulfill their survival destiny,” Thomas Perls, a longevity expert and professor of medicine at Boston University, told the Associated Press.
The share of men living into old age is also larger, which can be attributed to improvements in medical care.
Some of the declines in younger
people are attributed to women having babies later and to birth rates slowing during the 2007 to 2009 Great Recession and not recovering.
“In the short run, the crisis of work-family balance, the lack of affordable child care, stresses associated with health care, housing and employment stability, all put a damper on birth rates by increasing uncertainty and making it harder to decide to have and raise children,” Philip Cohen, a sociologist at the University of Maryland, told the AP.
The 2020 data was delayed by nearly two years as the Census Bureau began a new privacy protection method that obscures respondent identity. The agency also had some trouble gathering information because of the pandemic, the AP reported.

The United States now has 331 million people. Those aged 65 and up comprised 16.8% of the U.S. population in 2020, a share that is still lower than other countries like Japan, Greece and Italy.
White people are the oldest cohort, with a median age of 44.5. Median age for Asian people was 37.2. Black Americans had a median age

of 35.5. The youngest were Hispanic people with a median age of 30. Age also varied by state, with Maine showing a median age of 45.1.
Puerto Rico had a median of 45.2. These facts are attributed to baby boomers aging out of the workforce and people leaving Puerto Rico because of hurricanes and government mismanagement, the AP reported.
It matters that the country is getting older because there will be fewer working-age adults to support older Americans on Social Security and Medicare.
“In the long run, immigration is the only way the United States is going to avoid population decline,” Cohen said.
It’s about more than just weight loss.
It’s about reducing your risk for serious conditions like heart disease and diabetes — and regaining the stamina, mobility and confidence to take on every day.
Crouse’s bariatric surgery program offers a dedicated team of physicians and providers, as well as psychological and nutritional counseling — all with the expertise to support you every step of the way.
Begin the process from home by viewing our online informational video. Then consult with our bariatric team via telemedicine visits to start your journey. It’s time — and now easier than ever.

As specialists in women’s healthcare, we pride ourselves on providing the latest services and procedures - personalized to help you thrive. We deliver high quality healthcare from prenatal to senior health to meet your needs at any age.

WOMEN'S HEALTH & OBSTETRICS & GYNECOLOGY
Call to schedule an Appointment: 315-252-5028
Physicians:
Donald Calzolaio, MD • Amy MacDonald, MD
Tanya Paul, MD • Loren Van Riper, MD
Q: How long have you been chief medical officer of Crouse Hospital now?
A: Chief medical officer? About six weeks.
Q: How do you like it?
A: It’s fantastic. Seth [Kronenberg, CEO] and I are having a really good time.
Q: What are your duties?
A: The chief medical officer is widely seen to be responsible for all things related to the physicians, the PAs, nurse practitioners, the care delivered to patients at the provider level, the quality of that care, what that care looks like. The overall medical care at the institution is my ultimate responsibility.
Q: What got you interested in assuming that position?
A: In truth, it wasn’t something I had been interested in doing. I was
the chief of the department of medicine at Crouse for the last 12 years or so and a practicing ICU physician. I still am. I had been very active in those roles and very happy with the level of administrative involvement I had with the hospital throughout the quality line and clinical line. As Seth moved forward into the CEO position from CMO in March there was a vacancy. We’d formed a pretty solid friendship over the last decade or so, and I saw this as an opportunity to be even further engaged, to work with Seth and to, in many respects, pay forward some loyalty to an institution that had been good to me and my family. And I saw an opportunity where perhaps I had something to offer to give back.
Q: Crouse seems to have had a pattern of physicians in the CEO role. Is that unusual?

A: As you look around, it’s not. Certainly, we have physicians in
leadership roles both at Upstate and St. Joe’s, so locally it’s not the unusual at all. And if you look around the country, you’ll see a lot of very successful physicians in those administrative roles. What we do as doctors doesn’t always directly translate to the administrative side, but I think a lot of principles we use in trying to care for patients does translate into administrative problem-solving even though these aren’t exactly the same kinds of problems we dealt with in our clinical career. I do think the relationships that physicians develop with each other are incredibly important in getting both the clinical and administrative lines of a hospital aligned. If you want to see a successful hospital you will find that the goals of the physicians and hospital are aligned. And I think it can be easier for a physician, who has lived the life of a physician, to understand a physician’s needs and be able to bridge that gap and align those goals and create longstanding, durable relationships.
Q: What kinds of challenges does Crouse face right now in delivering quality health care?
A: Crouse has the same challenges that all the other hospitals across the country and particularly New York state have. Operating margins are tight. The system is designed to keep them tight. We do a really good job being efficient with our resources to make sure we have a functional organization that can meet its financial responsibilities. Because, ultimately, we’re just stewards of this institution and in this moment there is a group of us in leadership who is ultimately responsible to make sure this hospital continues to serve the people of Central New York. We don’t own it, but we do make sure that it’s here and works. The people of Central New York own it. So we work with those financial challenges. It’s tough, but we’re doing a great job. Under Dr. Kronenberg’s leadership we are moving forward quite well. The other challenge is staffing. Staffing at every level, clinical and non clinical, is a challenge for all institutions. We have many open positions, as do many hospitals, and we’re doing our best to fill those positions. There is some paucity in the workforce.
Q: Is that since COVID-19, or was it a problem even before?
A: That was even before, but in some respects it’s more pronounced now. There are some market pressures that may have not been as pronounced before as they are now. But certainly COVID is part of it.
Q: What are some of those market forces?
A: It’s always been challenging in Central New York. If you live here, you live here, but it’s always been challenging to bring in people from outside. It’s always been hard for us to distinguish ourselves. I’m not native to the area, I’m from downstate, but I’ve been up here 20 years so it’s my home now. But I’ve seen that it’s one of the difficulties. There are some issues with lifestyle and job choices and the way people are choosing to work. There’s a greater desire for remote work. That translates fine for some jobs we have, but doesn’t translate for up-front patient care. There’s no place to be but at the bedside for that. And there are different work paradigms that exist today more prominently, like traveling.
That means you’ll work somewhere distant from your home and likely be paid significantly more money to do so and have all your costs covered. It can be challenging for a geographically, physically constrained job to try to meet the needs of a workforce that has a significant percentage of people who don’t want to work that way.
Q: How can you sweeten the deal for in-person work?
A: For those jobs that could potentially be done outside the hospital but we’d prefer you be present, or for clinical jobs?
Q: Both?
A: For clinical jobs there’s no way around having to be here, but if we can give people the kind of scheduling they prefer, whatever that looks like, we try to be more flexible and work with them to meet their lifestyle needs. With respect to the other group, we’re trying to bridge that gap by bringing as many people back into the hospital as we can. And we’re trying to be flexible with work schedules enough to say, “OK, maybe it’s a hybrid position.” I personally think there’s value in sharing physical space with other people and having tactile interactions that aren’t just visual and electronic. I think having support staff be with us who are providing clinical care can help them understand our jobs better and in turn do a better job in administratively supporting us.
Q: Are you still clinically practicing?
A: Yes, part time. Since I’m a hospital-based physician, it’s easier to maintain my practice than it would have been if I were outpatient. As an ICU physician, I’m in the hospital and have developed relationships throughout the institution. I’m finding that continuing to practice clinically I’m able to get some of the work done that really is chief medical officer-related, since it’s so based on relationship management. It makes me be the best I can be to try to set the best example I can set whenever I’m interacting with a patient.
Q: You’re also a firefighter. Where do you find the time?
A: I’ve been doing it for 30-plus years. I’m on fire calls, EMS calls all the time. It doesn’t pay the bills, but it’s my love.
Name: David Landsberg, M.D.
Position: Chief medical officer at Crouse Hospital

Hometown: Queens
Education: Medical degree: Saba University School of Medicine (Saba, Dutch Caribbean); residency and internship in internal medicine: Mount Sinai Hospital, New York City; fellowship in critical are medicine: Memorial Sloan-Kettering Cancer Institute, New York City
Affiliations: Crouse Hospital; University Hospital, St. Joseph’s, Auburn Community Hospital, Rochester
Regional Organizations: American College of Chest Physicians; American College of Physicians, National Association of EMS Physicians; Society of Critical Care Medicine
Family: Wife (Stacia); son (Solomon); daughter (Graeson)
Hobbies: Firefighting
New chief medical officer oversees all care provided at Crouse Hospital — still sees patients at the ICU and finds time to volunteer as firefighter
David





































It should come as no surprise that OB-GYNs in states with restrictive or confusing abortion laws are considering moving to states that won’t interfere in the care between doctor and patient. The Kaiser Family Foundation published an article about what is happening in Idaho, which just passed a restrictive abortion law. Seventy-five of 117 Idaho OB-GYNs surveyed by the Idaho Coalition for Safe Reproductive Healthcare indicated they were considering leaving the state. Of the 75, 73 said it was because of the newly passed restrictive abortion law. Rural hospitals, typically staffed with minimal OB-GYN physicians, may be forced
The American Medical Association (AMA), the Institute for Healthcare Improvement (IHI) and Race Forward are collaborating as “Rise to Health” to mitigate the barriers that must be overcome to achieve health equity among us all. Barriers such as cost, access, isolation, housing and food security and racism, all impede health equity. The three organizations representing providers, payers, pharma and numerous professional societies and associations are combining their heretofore disparate efforts in the battle against impediments to equity and establish a set of common measurements and goals. Hopefully, Rise to Health will address our fragmented healthcare system which frustrates providers and consumers alike.
to close maternal services, forcing pregnant women to travel hundreds of miles out of state to deliver. OBGYNs provide a lot more health services to women besides maternal care. So, their departure from states with restrictive abortion laws will have a far greater impact on women’s overall healthcare than anticipated. A research paper published in February found 76% (3 of 4) current and future (residents and medical students) OBGYNs won’t even apply to work in states with restrictive abortion laws. The threat of potential fines and even imprisonment was too much of a deterrent.
study by J.D. Powers based on 32,656 interviews, customer satisfaction with commercial insurance plans is declining especially among Gen Y and Gen Z generations. Particularly low scores were given to customer service and communication. Only 17% of those who identified their health status as poor or fair were assigned a case manager. Care fragmentation (multiple providers and several prescriptions) usually leads to high costs, poor outcomes and increased patient frustration. Other scores that declined from previous studies were in coverage and benefits and provider choice. Low scores from new members indicate a need for insurers to do better job of onboarding or how to access benefits and navigate our complicates and fragmented healthcare system. Interestingly, digital health tool usage remained low.
business (private physicians and hospitals), a 70% decrease in urgent care business a 1% decrease in emergency room business. (The decrease in non-emergent visits in ERs is a good decrease.) The pandemic was probably a major cause for the 200% increase at retail clinics as consumers got used to getting vaccines and COVID-19 testing there, so primary care usage at these locations grew by association and convenience. Being associated with a drug chain like CVS or Walgreens further enhanced the convenience, continuity of care and one-stop shopping. Ninety percent of retail health clinics are owned by six huge corporations with CVS being the biggest. Believe it or not, the second largest operator of retail clinics is grocery giant Kroger. So, you can see your doctor, get a vaccination, get tested, get your prescription and grab a dozen eggs all in the same place. Most retail clinics are in the Southwest and Midwest.
The CDC estimates almost half of adults have hypertension. Engineers at UC San Diego have developed a simple clip that works with your smartphone camera and flash. It costs less than $1. It is so cheap it could be handed out by providers to their patients so they can easily monitor their blood pressure at home without the hassle of cuffs and BP monitors. The product is not yet available as the engineers are working on making the clip as user friendly as possible.
ing from the pandemic are struggling to break even.

According to a recently released
Over last five years, retail clinics have experienced a 200% increase in business. Compare that to a 13% decrease in traditional primary care

Ever since Facebook introduced the metaverse (a digital world using virtual and augmented reality headsets) cash-rich CVS has filed for a trademark to sell their products in the metaverse. The pharmacy giant will begin to transition some in-store services like primary care, nutrition and wellness counseling to virtual. As they do so, a lot of people will lose their jobs as they plan to close 900 stores. CVS revenue last year was a staggering $304 billion. Meanwhile, cash-strapped hospitals still recover-
You want to help but your 80-plus-year-old parents are resistant. They are confused or believe you are interfering or they are afraid of losing their independence. Possibly all the above. It is the dilemma confronting most family caregivers. Negotiation and dispute resolution may be the answer. Researchers at Northwest University conclude the very same negotiation and dispute resolution tactics that work for businesses can work for families. 1) Determine the clinical, personal and financial issues.

2) What are your parents’ positions?
3) Lay out what are you willing to do as caregiver. 4) Find common ground. 5) What are your parents’ fears? Both real and perceived. Mitigate everyone’s emotions. 6) Ask questions, don’t present parents with edicts. 7) Agree you are all on the same team. 8) If all fails, seek third party help from social workers, family psychologists or case managers. Above all, don’t let the relationship with your parents devolve into resentment.
The average annual increase in the cost of care since 2021 is 4.8%. According to the Milliman Medial Index, healthcare now costs a family of four just over $31,000 this year. It’s $7,221 for an individual. Healthcare inflation tends to lag six months to a year behind general inflation, so 2024 costs will probably go even higher. Driving costs up are supply chain problems, cost of drugs, labor shortages, ransomware attacks and catching up on the backlog of procedures postponed during the pandemic. Milliman expects employees will bear 60% of the increases. As discussed in an earlier column, commercial insurers are recoding record profits.


George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse. Email him at gwc@gwchapmanconsulting.com.

Monday can be a downer as folks leave weekend play behind. Now, researchers say Monday might also be the most common day for deadly heart attacks.
Doctors at the Belfast Health and Social Care Trust and the Royal College of Surgeons in Ireland determined this by analyzing patient data in Ireland, though they can't determine the reason why.
Past research has suggested it might have to do with circadian rhythm — the body's sleep-wake cycle.
“Someone is admitted to hospital due to a life-threatening heart attack every five minutes in the U.K., so it's vital that research continues to shed light on how and why heart attacks happen,” said Nilesh Samani, medical director at the British Heart Foundation.
“This study adds to evidence around the timing of particularly serious heart attacks, but we now need to unpick what it is about certain days of the week that makes them more likely,” Samani said in a heart foundation news release. “Doing so could help doctors better understand this deadly condition so we can save more lives in future.”



For the study, the researchers analyzed data from more than 10,500 patients across Ireland, in both the Republic of Ireland and Northern Ireland, who were admitted to a hospital between 2013 and 2018 with the
most serious type of heart attack.
The ST-segment elevation myocardial infarction (STEMI) happens when a major coronary artery is completely blocked.
The study found a spike in rates of STEMI heart attacks at the start of the working week, with rates highest on a Monday. However, they also found higher-than-expected rates of STEMI on Sunday.
In the United Kingdom, more than 30,000 people are admitted to the hospital with STEMI each year, requiring emergency assessment and treatment to minimize damage to the heart. Typically, this involves an emergency angioplasty, a procedure to reopen the blocked coronary artery.
“We've found a strong statistical correlation between the start of the working week and the incidence of STEMI,” said cardiologist Jack Laffan, who led the research at the Belfast Health and Social Care Trust. “This has been described before but remains a curiosity. The cause is likely multifactorial, however, based on what we know from previous studies, it is reasonable to presume a circadian element.”
The findings were presented in June at the British Cardiovascular Society annual conference. Findings presented at medical meetings should be considered preliminary until published in a peer-reviewed journal.
state, with the federal government. We have some private foundation money. We have a few things that would be considered fee for service. Some childcare; some families pay for the respite services for the seniors, but everything else is either through contract or through insurance billing.
Q: How many clients do you serve?
A: We serve a little more than 30,000 every year. We also do the Christmas bureau for the community. We serve about 9,000 people through the Christmas bureau. All told, we serve somewhere between 31,000 and 35,000 people a year.
Q: Are you seeing an increase in the number of people you serve over the past few years?
Only 13% of American adults understand the purpose of the 988 Suicide and Crisis Lifeline nearly a year after its widely publicized launch, a new survey from the Pew Charitable Trusts shows.

“There is an opportunity and a need for state and local leaders to launch inclusive awareness campaigns in the months ahead,” lead researcher and Pew senior manager Tracy Velázquez said in a statement, CNN reported.
“The federal government's most recent investment into 988 shows a commitment to building a strong crisis care infrastructure in the country — one that is critically important, given the many people experiencing mental health and substance use issues,” Velázquez added.
The 988 line began last year after it was changed from 1-800-273-TALK. It was previously called the National Suicide Prevention Lifeline.
Pew surveyed more than 5,000 adults in April, finding that once people knew about the 988 crisis line, about 7 in 10 said they were somewhat or highly likely to use it.
Respondents also had some concerns about where calling the line might lead them. About 2 in 5 of those surveyed worried that calling 988 would lead to police arriving at their home, being forced to go to the hospital, being charged for services they couldn't afford or having other people learn about the call.
Race played a part in the results: Twice as many white people as Black people were aware of the 988 line. College-educated respondents were more aware of the line than those with a high school degree or less.
Call volume has increased in the past year, with 160,000 more calls, chats and texts in April 2023 than the previous April, which were also answered more quickly than with the previous hotline.
Calls increased 52%, chats increased 90% and texts answered increased 1,022%, CNN reported.
Use of Salvation Army’s food pantry up 25%, demand for other services also high, says the organization’s director for community services
By Mary Beth RoachQ: Can you give us an overview of what the local Salvation Army is and or does?
A: The Salvation Army in Syracuse is a large multi-service agency. We have about 30 different programs. We have five core areas that we work in.
We have early education centers for children ages 0 and 5. We provide full daycare. We have early Head Start services and universal pre-K embedded in that. We also have a drop-in daycare center at the courthouse for families who are using Family Court. Emergency and practical assistance, which is our very large food pantry. Support services related to housing assistance, rental assistance, utility assistance; supports for folks struggling with mental health issues. We have an 84-bed family shelter; a women’s shelter, which is a shelter for women with mental health or substance abuse issues; permanent supportive apartments for that same population. We have a healthcare navigator program, which does enrollment for all the New York State health insurance programs.
We have Booth House, which is the community’s runaway and homeless shelter; Barnabas, which is a shelter for older homeless youth. We have three transitional living programs for youth and young adults — one for older homeless youth, one for young adults who have histories of homelessness and mental health, and the transitional apartments and parenting center for young women who are pregnant and parenting. We also do non residential services and youth services.
We do a lot of preventive child welfare services for Onondaga Coun-

ty. We provide intensive in-home services for them. We have the foster visitation center. Children who are in foster care visit with their biological parents at the center and we provide coaching support on parenting, clinical support to help those families get reunified. We have domestic violence counseling services and supervised visitation services. We also have a range of Medicaid-funded services for children with serious emotional and behavioral needs. We have skill-building and some in-home clinical services for them, counseling services and we have children’s care management, which helps families pull together a plan for a child with serious health or mental health issues and get connected with your appropriate resources in our community. We have an adult social day program. We also provide within that center respite care for individuals who might be caring for an older adult and need to go to work. It provides a safe place for them to be during the day. And we have information referral services, some services that can help seniors connect with safe housing.
Q: What’s your coverage area?
A: Onondaga County. Many of our services are located within the city of Syracuse, but we do a lot of home and community-based services so we serve people all over the county.
Q: How’s the Salvation Army funded? How big is your budget?
A: Our budget’s about $18 million, about 200 employees. We have contracts with the city, the county, the
A: For sure. You see it in pockets. For example, right now the food pantry is just swamped. People who are receiving food stamps were getting supplemental COVID benefits. Those ended, so people suddenly had about $90 less per family member. And our housing assistance programs are also really busy now because the cost of rental housing is so high people are really having a difficult time being able to afford safe rental housing. And our children’s mental health services. COVID-19 took a toll on everybody — took a particular toll on children. We have a high demand for services in that area.
Q: What would you consider your biggest challenge?
A: Right now — and I would say this is universal to human services — is staffing. Workforce impacts every sector but has particularly impacted human services. A number of people are still looking for remote options. That’s not human services. The other challenge for us is the food pantry. We served 25% more than we did the same month last year. We’re on track for serving probably well over 250,000 meals out of our pantry. That takes a lot of food.
Q: How can the community help?
A: There are a couple ways. We have a number of people who make cash donations. They can donate through our website (easternusa.salvationarmy.org/empire/syracuse/). Right now, we’re asking corporations, faith communities, if they will do targeted food drives for us. They can call in to our office. We know what the key items are that we need. And we always need volunteer help.
Q: Are there any new initiatives that you’re currently working on or might be coming up?
A: We’re doing an expansion of our early education center. We have created some new space. One of the things that happened with young children during COVID-19 was lags and delays. We serve a lot of children who need speech therapy and physical therapy and occupational therapy. So we’ve created some space for that to occur, while they’re in childcare. We’ve also created a gym space, a space for families to be able to meet with their teachers and educational programs for themselves while they’re here. And one of the really exciting things is we’re adding a STEM room for our 3- and 4-(year-olds.) It’ll be a learning lab for science, technology, math to get our little ones started with that. We’re excited about that.
































Summer has finally arrived. Woo hoo!! Time for barbecues, picnics, festivals and fun!
For many people, the summer months provide welcome relief from the soggy transition from winter to spring. Out of the gloom, summer emerges with longer, brighter and warmer days filled with the promise of travel, socializing, and connecting with friends and family.
So why are you feeling so lonely?
As it turns out, the arrival of summer isn’t embraced by everyone. If you live alone and feel socially isolated, summertime can pose a real challenge. It’s easy to feel like an outsider, looking in on other people’s fun-filled days and activities.
After my divorce, I had bouts of the blues and spent too much time alone. I let my relationships with friends and family drift away and my world became very small and quiet.
Sometimes the loneliness would overwhelm me and I’d lose my oomph for doing much of anything. I became a spectator, rather than a participant, in life.
Feel familiar?
Eventually my phone stopped ringing and the weekends stretched out before me like a long, lonesome highway. Without companionship, a beautiful summer day left me feeling heartbroken.
I knew something had to change.
An attitude adjustment was in order. Specifically, I needed to remind
myself that my life is in my hands — that I’m responsible for how lonely (or not) I am, and that I’m in charge of how large or small my life is.
So what did I do? I picked up the phone, called a girlfriend, and made plans for us to get together. Then I picked up the phone again and left a text message for my sister, asking her to give me a call.
And I didn’t stop there.
The next day, I worked up the nerve, rehearsed a few words, and made a third call to a neighbor who also lives alone. I asked if he wanted to take a walk later that evening. He asked for a rain check, but that was OK. We made plans to take a walk the following week, which gave me something nice to anticipate.
I then shifted to my computer and sent out a few “Hi, it’s been too long!” emails to friends, inviting them over to see (and admire!) my newly installed patio garden. I wanted to share it. And to show it off. Why not, right? It’s rewarding to hear “oohs” and “aahs,” and sometimes we need to create our own opportunities for positive feedback.
I was on a roll, and it was illuminating to see how easily I could change my circumstances by doing just a few small things — by converting my newly adjusted attitude into action.
Within weeks, my phone was ringing again, emails and texts were arriving, and I had entered a few

Spotting ADHD early can ensure children with the condition get the help they need sooner rather than later.
But how can parents know if the behavior they're seeing in their child is a sign of attention deficit hyperactivity disorder or merely the mercurial mood and behavior swings of a toddler?
An expert at the Kennedy Krieger Institute in Baltimore offers some guidance.
"Research shows that children with ADHD have abnormal brain development, meaning that ADHD has a biological basis that often makes it a lifelong condition," Mark Mahone, director of neuropsychology, said on the institute's website. "We want to catch ADHD early because it has such a profound effect on learning and academic development. Chil-
dren whose symptoms begin in early childhood are at the highest risk for academic failure and grade repetition."
The team at Kennedy Krieger was among the first to study preschoolers' brains for signs of ADHD using neuroimaging. The researchers found that children with ADHD have a smaller caudate nucleus, a brain structure associated with thinking skills and motor control.
Up to 40% of children have significant attention problems by age 4. ADHD is the most common mental health disorder among preschoolers. About one in 11 school-aged children have an ADHD diagnosis.
Mahone encourages parents to pay close attention to their toddler's behavior.
Look for these specific signs: Your child dislikes or avoids activi-
social events into my calendar. Life felt better!
Part of what motivates me when I find myself in a slump is a passage I found in a sweet little book called “Living Alone and Lovin’ It,” by Barbara Feldon.
In one particularly helpful chapter on loneliness, she recounts a heart-to-heart she had with an “older and very wise friend” named Leo. She was brooding about being lonely and shared how much she wanted to feel loved and protected again, the way she felt when she was a child.
Leo responded quite bluntly: “But you’re not a child and don’t have a child’s needs. A child is in danger without company because it’s helpless, but an adult has access to any need imaginable: food, medicine, companionship. All an adult has to do is pick up the phone…”
Good friends can be such a help! Especially when they tell it like it is. Barbara was energized by Leo’s no-excuses straight talk, and indirectly so was I. As adults, we can

exercise choices; we can choose to stay in a slump or choose to pick up the phone.
My prediction should you start to reach out? Little by little your world will expand, with one connection spawning another, and another, and yet another.
Before you know it, your feelings of loneliness will lessen and you'll be on your way to banishing the summertime blues!
Gwenn Voelckers is the founder and facilitator of Alone and Content, empowerment workshops for women and author of “Alone and Content,” a collection of inspiring essays for those who live alone. For information about her workshops, to purchase her book, or invite her to speak, visit www. aloneandcontent.com
ties that require paying attention for more than one or two minutes. He or she loses interest and moves on to something else after only a few moments.
Talking a lot more and making more noise than other children of the same age can also be an indicator. So, too, can climbing on things when told not to do that.
Children with ADHD may not be able to hop on one foot by age 4. They are nearly always restless, constantly twisting in a seat or kicking their feet. They insist they must get up after being seated for just a few
minutes.
Kids with ADHD may warm up to strangers too quickly or fearlessly get into dangerous situations. They can be aggressive with playmates or get injured by moving too fast.
"If parents observe these symptoms and have concerns about their child's development, they should consult with their pediatrician or another developmental expert," Mahone said. "There are safe and effective treatments that can help manage symptoms, increase coping skills and change negative behaviors to improve academic and social success."


This month’s column reviews common first aid mistakes to avoid.

This topic was inspired when a recent patient showed up with a poorly executed homemade splint.

The idea was correct: to immobilize a wrist injury that occurred about 36 hours prior to arrival at the urgent care. But the caregiver used a heavy board with no padding, causing significant bruising to the side of the arm touching the splint.

When splinting an injury, use plenty of padding to avoid bruising and skin damage. If an injury is significant enough to require splinting, don’t delay medical evaluation. Since the urgent care is open every day and emergency rooms are open 24/7, this patient’s broken bone could have been seen much sooner than 36 hours after injury.
A segment of a 2x4 board is overkill for a wrist splint. Readily available alternatives include rolled and flattened newspaper, a magazine, a length of cardboard. After fashioning a splint, check regularly to be sure it’s not so tight as to cut off circulation. The ACE wrap, gauze or cloth strips used to secure a splint may need to be loosened when an injury swells. Elevating injured body parts helps minimize swelling.
Applying ice to an injury helps prevent and reduce swelling. That’s another procedure that can be done wrong. Don’t place ice directly on the skin. Protect the skin from cold injury with a washcloth, towel or clothing. Don’t leave the ice on for more than 20 minutes, although it can be reapplied after the giving the skin a
breather to warm up.
Cuts are another injury where first aid errors are common. For heavy bleeding, apply a bandage such as gauze or clean fabric. Then hold direct pressure on the wound. If the cut bleeds through the dressing, add another layer over the soaked dressing and continue to apply pressure. Don’t remove the initial layer.
I won’t go into tourniquets in this article; if bleeding is so severe that a tourniquet is needed you should be calling 911 and following the dispatcher’s instructions!

For wounds without excessive bleeding, the most important first aid is cleaning with soap and running water. You don’t need alcohol or peroxide, which damage tissue. The exception is to use peroxide for initial cleansing if there is a lot of dried blood to remove. Most wounds do not need over-the-counter antibiotic ointments. Ingredients such as neomycin (Neosporin and other brands) are notorious for causing allergic and irritant reactions. You can use plain petrolatum (Vaseline) to keep the wound moist. If you are concerned that a wound needs antibiotics because it is dirty or the victim has an underlying condition such as diabetes, seek medical evaluation and follow the treating provider’s recommendations.
Another common error is to treat skin rashes with any old tube of cream or ointment floating around in the medicine cabinet.
Often people don’t know what the active ingredients are, when it was prescribed and who or what it was treating. This can lead to an in-
appropriate treatment that is useless or harmful. The substance might be old, expired or contaminated. One way to avoid this error is to throw away leftover medications.
The correct way to treat a nosebleed is to pinch the nostrils together and keep pinching for 15 minutes without stopping to check whether the bleeding has stopped. After 15 minutes, if the bleeding recurs you can try again for another 15 minutes. Lean forward to reduce blood flowing down the back of your throat. Don’t lean or tip your head back as this will make you more likely to choke and gag on blood or to swallow blood. Swallowed blood irritates the stomach. If the nosebleed does not stop after the second try, seek emergency care.
Other reasons to head for the emergency room include patients on blood thinners or with bleeding disorders, feeling faint or lightheaded, and facial trauma. Placing an ice pack on the back of your neck will not help nosebleeds. After controlling a nosebleed, reduce the chance of rebleeding by moistening the nostril with saline gel or petroleum jelly.

Other miscellaneous first aid errors:




Burns — don’t smear with butter or similar fatty substances. You can run cool water over the area and gently pat dry.
Syrup of ipecac to induce vomiting. This is seldom if ever useful. If someone ingests possible poison or other toxic substances, call poison
control 800-222-1222 and follow their instructions.
Snakebites — don’t apply a tourniquet, don’t make cuts, don’t attempt to suck out the poison. Do keep the patient calm, keep the injured body part still, and remove tight clothing or jewelry that could constrict the limb if it swells. Then seek medical care. Fortunately, venomous snakes are rare in Central New York.
Fever — don’t apply rubbing alcohol or immerse the patient in cool water. Although this cools the skin, the body responds by constricting surface blood vessels and channeling more blood — and therefore more heat — to the body’s core. Do use appropriate doses of ibuprofen or acetaminophen. Fever is common in children. The height of the fever is less important than how the child is acting and other symptoms.
Summer outdoor activities are a risk factor for injury and illness. Get out there and play, but review this list of first aid tips to be prepared.
Men’s health encompasses everything from physical, mental and social aspects. Health challenges can include chronic conditions to acute illnesses. Men are also at risk of suffering from heart disease, cancer, diabetes, depression and anxiety. These risks range from lifestyle choices such as poor diet, stress and lack of exercise to biological and genetic factors.
“Traditionally men have been much more likely to neglect their health when compared to women,” said Andrew Rogall, a primary care physician at Oswego Health’s Fulton PrimeCare. “This is one factor that contributes to men having a much higher rate of overall disease and illness in their lifetime, as well as a life expectancy that is five years shorter than the average American woman.” Rogall added.

One of the most overall common myths that patients tell their physician is that they feel healthy so there is no need to see a doctor. However, there is a clear distinction between feeling well and being healthy.
”Heart disease is the leading cause of death in men each year. Two major risk factors for heart attack are high blood pressure and high
cholesterol which for most are completely asymptomatic,” said Rogall. “Simply feeling well does not mean these things are not happening in the background until they suddenly present with chest pain and a heart attack. These are also great examples of things that are easy to diagnose and treat when we see people in the office regularly.”
Men are assailed by diseases that can affect anyone — heart disease, stroke, diabetes, cancer, depression. But they also have unique issues.
”Well, there is the obvious elephant in the room and that is prostate cancer, which happens exclusively in men,” said Rogall. “Additionally, heart disease, smoking, alcoholism, high blood pressure and cancers are some of the many conditions that are more commonly seen in men.”
Several risk factors increase the chances of developing health problems. Twelve percent of men age 18 and older are in fair or poor health, according to the Centers for Disease Control and Prevention. In addition, more than 50% of men older than 20 have hypertension.
“Fortunately, many of these
As with many aspects of life during the COVID-19 pandemic, physical therapy shifted to a virtual model. However, some physical therapy offices are keeping virtual PT as an option for patients.
For Robert Berkley, doctor of physical therapy and owner of Robert Berkley Physical Therapy in Oswego, advantages include the safe, familiar environment of virtual physical therapy.
“The patient feels comfortable in their home,” Berkley said. “They can know they can do their home exercise program because they’re already at home. It’s easy to instruct the patient and not as time consuming as when they come into the office.”
Traveling to and from therapy may be physically difficult for patients already in pain and experiencing deconditioning and limited movement. It’s also tough for patients who lack transportation or whose health makes them unable to drive.
“For a more complex diagnosis, we’d need to see the patient in person, but once they’ve seen a provider with a diagnosis of back pain or weakness, we can treat them virtual-
ly,” Berkley said.
Among the drawbacks is the lack of equipment, although creative therapists can usually find ways patients can perform movements with items they have around their homes.
“Sometimes, it’s difficult to instruct patients,” Berkley said. “You can’t put your hands on them to touch and feel.”
Despite this, he believes that virtual physical therapy would be more widely used if more people knew about it.
“Many people aren’t aware it’s available,” he said. “The platform is simple and easy to use.”
Virtual physical therapy can help more people enter and complete physical therapy.
“It’s all about access, like for people without transportation, who have socioeconomic restraints or who live in rural areas,” said Bryan Guzski, doctor of physical therapy and strength and conditioning specialist with Motive Physical Therapy in Brighton, a Rochester suburb. “Virtual services allow us to overcome a lot of those barriers.”
Patients do not need to be in person to discuss their health his-
diseases are preventable with regular office visits and routine screening,” he said.
All men should have a yearly wellness visit to screen for potential health problems. Bloodwork to check cholesterol levels and screen for diabetes is important.
“In smokers, it may be beneficial to screen for lung cancer and aneurysms, which is something we only do in men that have smoked,” he said. “We will discuss screening for prostate cancer which we may or may not do based on the individual.”
Rogall sees a combination of reasons why men hesitate booking regular visits. Some deal with the ego of manhood where seeing a physician is shown as a sign of weakness.
“Men are still much less likely to talk about their health and much more likely to downplay their symptoms,” he said. “They prioritize work and essentially anything else over
self-care. Unless we have a cold, then you’re not going to hear about it.”
Early detection is one of the greatest tools we have to prevent severe illness and death. By screening regularly, physicians can decrease the extent and severity of heart disease, high blood pressure, diabetes and cancers.
“In many cases, we may detect some of these early enough to reverse the course or prevent them from happening in the first place. It’s easier to blow out a candle than it is to put out a house fire,” Rogall said.
Health experts from the U.S. Preventive Services Task Force have made recommendations, based on scientific evidence about various ailments. Talk to your doctor about prostate health, obesity, high cholesterol, high blood pressure, colorectal cancer, diabetes, depression, sexually transmitted diseases and other screenings.
tory and offer an opportunity for a provider to observe their movement. As they squat, lunge, raise their arms and perform other movements — depending on their case — the provider “can get a pretty good picture as to how that person moves and functions,” Guzski said. “There’s an expectation that you need to be right by their side, but a lot of that coaching can be done with visual and verbal feedback from the provider and patient. There’s a lot of value and ways we can help patients.”
Virtual visits also permit providers the chance to see patients’ home environment. They can see how patients move and function in the place where they spend more time than anywhere else. Providers can also observe any obstacles to their ac-

tivities of daily living, such as a chair that’s hard for them to use and offer suggestions that can help.
“There’s definitely no substitute for getting your hands on the patient, feeling the tissue and joint,” Guzski said. “You can have the patient palpitate, but the feedback is different. The detail and accuracy are different from a trained provider.”
He does see many advantages such as reducing the burden on primary care providers, especially urgent care and emergency rooms, since insured patients can seek physical therapy without a referral in New York and receive treatment for 30 days without a prescription. Most insurance covers virtual physical therapy just as it would in-person physical therapy.
We’ve already had some sizzling days, and there will be many more this summer. Not everyone responds to the heat in the same way, and for some people, a stretch of high temperatures can be deadly.
Heat-related illness, known as hyperthermia, results from exposure to extreme heat, with the body unable to properly cool. Prompt treatment with fluids and cooling the core body temperature are critical to reducing illness and preventing death.


“The elderly are prone to heat
exhaustion since, as we age, our bodies don’t regulate heat as well as they did when we were younger,” says physician Lorna Fitzpatrick, vice president for medical affairs and senior medical director at Excellus BlueCross BlueShield. “Often, seniors aren’t aware of the impact of high temperatures on their bodies until it’s too late,”

In addition to the elderly, the Centers for Disease Control and Prevention says people at greatest risk for heat-related illness include those who are overweight or have existing medical conditions, such as diabetes
and heart disease.
Among the symptoms of heat exhaustion are headache, nausea, dizziness, weakness, irritability, thirst, heavy sweating (or no sweating), elevated body temperature, muscle cramping, and decreased urine output. If untreated, heat exhaustion may progress to heat stroke, a life-threatening condition that can damage the brain or other vital organs and, in severe cases, cause multiple organ system failure. Fitzpatrick offers the following tips to prevent heat-related illness:
• Check on those at risk. During a heat wave, frequently check on people at risk, such as the elderly, disabled, or homebound. Check on them at least twice a day.
• Ask your health care provider if you or someone you care for is vulnerable to excessive heat. Some conditions or medications can impair the body’s ability to regulate temperature, inhibit perspiration, or restrict how much fluid can be consumed.
• Wear light clothing. On extremely hot days, dress in lightweight, light-colored, and loose-fitting clothes.
• Drink liquids. In hot weather, make sure you, or the person you care for, consume an appropriate amount of nonalcoholic fluids. Stay away from beverages high in sugar or caffeine, as they cause the body to lose more fluid.
• Don’t wait until you feel thirsty to have a beverage. By the time you recognize the thirst, you are already in need of fluids.
• Take a cool shower or bath. Taking a shower or bath with room-temperature water will allow your body to cool.
exhaustion includes immediate medical attention from an urgent care center or hospital emergency room. If medical care isn’t available, call 911 and stay with the individual until help arrives. Remove unnecessary clothing, including shoes and socks. Encourage frequent sips of cool water, and apply cold compresses to the head, neck, and face.
First aid for someone with heat
When did you last see your doctor? It might be time. Routine preventive care is key to staying healthy. Most screenings and immunizations are no cost when you visit a participating plan provider.* Common preventive services include:
• Annual routine checkup
• Well-woman visit
• Well-child visit
• Immunizations
• Mammography screening
Submitted by Excellus BlueCross BlueShield Learn
Every once in a while, I come across information about a certain food that takes me by complete surprise. I read it and whisper, “Who knew?” I consider friends and family who might benefit from this goldmine of information. And then, I can’t shut up about it.
That’s what happened with kiwis.
Oh, I knew they were beneficial all right — I just didn’t realize they had this particular benefit.
In a word, kiwis are “nature’s broom,” helping to unplug sluggish bowels with each delicious bite!
According to a recent study at Mayo Clinic, eating two kiwis per day was as powerful as prunes at increasing stool frequency and reducing straining. Physician Michael Camilleri, a gut motility specialist at the Mayo Clinic, said the sugar, fiber and other nutrients in kiwis can produce a laxative effect by increasing the water content and volume of stools.

Multiple studies also suggest that kiwis cause less gas, bloating and abdominal cramps than prunes.
Maybe that’s why kiwi-rich New Zealand is one of the happiest countries in the world: few are struggling with blocked bowels! As for here, well, so many are struggling with constipation, it’s our leading digestive complaint.
What’s no surprise is how high
these furry little fruits are in vitamin C, with one kiwi providing over 60% of our daily needs (more than an orange). Although widely known for its immune-boosting capabilities, vitamin C is also our skin’s best friend, creating derma-firming collagen, along with offering protection against age-accelerating sun damage. Research suggests that people who eat more vitamin C have fewer wrinkles.
Lastly, kiwis support heart health in impressive ways. They’re remarkably low in sodium, cholesterol and calories (only 44 per kiwi); they’re a good source of fiber, potassium, and folate (all associated with a lower risk of stroke); and they’re loaded with antioxidants, which help reduce the risk of chronic diseases by gobbling up damaging free radicals.
Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.

Skip artificial sweeteners if you're trying to lose weight, warns the World Health Organization (WHO), noting the sugar substitutes aren't effective for shedding pounds and may also cause harm.
Long-term use of sugar substitutes may cause "potential undesirable effects," according to new WHO guidance. This can include an "increased risk of Type 2 diabetes, cardiovascular diseases, and mortality in adults,” CBS News reported.
Consuming foods and beverages with ingredients like saccharin or sucralose or adding them to foods "does not confer any long-term benefit in reducing body fat in adults or children,” the WHO said after completing a systematic review.
Among the artificial sweeteners WHO officials considered were ace-

sulfame K, aspartame, advantame, cyclamates, neotame, saccharin, sucralose, stevia and stevia derivatives, according to the news report.
“People need to consider other ways to reduce free sugars intake, such as consuming food with naturally occurring sugars, like fruit, or unsweetened food and beverages," said Francesco Branca, WHO director for nutrition and food safety.
Artificial sweeteners "are not essential dietary factors and have no nutritional value. People should reduce the sweetness of the diet altogether, starting early in life, to improve their health," Branca added.
These recommendations do not apply to people who already have diabetes, according to the review. That group was not included in the review.
Dressing:
Choose plump, unblemished fruits that yield slightly to gentle pressure. Firm kiwis, stored at room temperature away from direct sunlight, take about 2-3 days to ripen. To hasten the ripening process, place kiwis in a paper bag with an apple or banana. Ripe kiwis can last up to 4 weeks in the fridge. For optimum health benefits, go ahead and eat the skin (but not if you have a history of kidney stones).
Serves 4-6
2 tablespoons balsamic or red wine vinegar
2 tablespoons fresh lemon juice
½ teaspoon salt
¼ teaspoon coarse black pepper
¾ teaspoon sugar
1 teaspoon Dijon mustard
1-2 cloves garlic, minced
1/3 cup olive oil
Salad:
4-6 kiwis, peeled (or not), sliced into half-moons
3 cups strawberries, quartered
1 cup blueberries
6-8 cups salad mix of choice
½ cup feta or gorgonzola crumbles
In a tightly covered container, shake dressing ingredients until well blended.
Cut all fruit as directed above.
To assemble individual salads, first place greens in salad bowls and drizzle on a little dressing. Then, add cut fruit and drizzle on a little more. This method keeps the lettuce crisp and the fruit bright. Garnish with cheese of choice.

This isn't the only time these artificial sweeteners have raised concerns. Recently, erythritol, an ingredient in the stevia sweetener Truvia, was singled out because of potential harms.
Cleveland Clinic researchers found months ago that people with
higher blood erythritol levels were at greater risk of heart attack or stroke and of dying prematurely. The study, involving 4,000 people, also found that the sugar substitute made it easier for blood clots to form. Those findings were published in the journal Nature Medicine.
Most people working on losing a significant amount of weight see prompt results when they first begin their efforts. With minimal effort such as walking each day or engaging in a short workout, the pounds seem to melt off at first.
As they progress in their weight loss program, it seems to become harder and harder to lose weight.
Even though they stick with their healthful, reduced calorie diet and exercise regimen, their weight loss plateaus for two reasons. First, they’re adding muscle while reducing fat so they may not see dramatically smaller numbers on the scale as they progress. Second, their body does not have to work as hard to carry around as much weight as when they first started losing weight. That’s where wearable weights can make their fitness activities more dynamic.
Wearing weights “can increase caloric expenditure for the same reason that someone with a high BMI can burn more calories with lower intensity exercise,” said Marilyn Buckley, master’s trained nurse at the Center for Weight Loss and Surgery at Oswego Health. “It can increase your heart rate.”
In addition to carrying hand weights such as kettle bells and dumbbells to bodyweight movements like squats and lunges, wearing weights can help. Donning a
weighted vest while engaging in activities like running or calisthenic movements increases the work level of the muscles involved. It mimics the effect of their heavier body weight, forcing their muscles to work harder.
Some weighted vests are as heavy as 40 pounds or more. However, “it is slow but steady when you increase your activity,” Buckley said, referring to wearing weight during exercise. “Start with one to two pounds, anywhere from 1%-2% of your body weight.”
Some wearable weights provide pockets to gradually fill as the user’s tolerance and strength increases. This can increase the usable life of wearable weights. It’s best to try on the devices in the store rather than purchasing them online (unless they’re returnable) to ensure a comfortable fit. Feeling wearable weights shifting during exercise is not ideal.

Buckley warned about using ankle or wrist weights for anyone with joint issues.
“The vest is certainly better for those kinds of patients with joint pain, but they shouldn’t use it if they have stomach or back issues or osteoarthritis that involves their spinal column,” she said.
The baseline fitness level and how one moves without wearing weights also matters. Wearing weight is inadvisable for someone who has been completely sedentary.
Austyn Affronti, president of Affronti Fitness in Rochester, believes that wearable weights can help burn more calories, but “if you’re just starting out, learn to use proper form,” he said. “Once you’re more advanced, you can use a weight vest. Otherwise, it can lead to joint inju-
ries. Putting more load on you will build more muscular strength and endurance and help people get in better shape.”
Always consult with a professional before undertaking a new fitness regimen or before increasing the level of activity.
In most households, women are the managers of their families’ health care needs.* Combined with the challenges associated with juggling child care and workplace demands – it can be a struggle to ensure women, quite literally, take care of themselves. FCMG can help. Available across CNY’s widest network of general practitioners and specialists – with short wait times, convenient hours and family-friendly offices – we make it easy to access a wide range of women’s care options, including:
• Reproductive health care and gynecology, including ultrasound exams
•Heart health, cholesterol management, and treatment of high blood pressure
•Type 1 and Type 2 Diabetes
•Chronic care and pain management
•Dermatology
•Bone density, including diagnosis and care of Osteoporosis
•Among others
To learn how FCMG can address women’s health care needs – for women of all ages – contact us today. New patients and families are welcome!
* Kaiser Women’s Health Survey (2017) indicated that 79% of the time, women are the one who take charge of health care responsibilities such as choosing their children’s provider; that 77% of the time, women take children to appointments; and that 77% of the time, women follow through with recommended family care.

A slow stroll with a dog on the park is always a healthy thing to do but it probably won’t cause people to lose weight.

You’re walking every day yet the number on the scale won’t budge.
What gives?
It’s likely that you’re not causing
a calorie deficit, you need to eat right and move more.
“In order to lose weight, you have to have a calorie deficit,” said Marilyn Buckley, master’s trained
They also don’t know what real exercise means.”
She added that the type of activity relies on the patient’s body mass index and how much they have to lose. The leaner the patients, the more calories they must expend to see numbers move on the scale.


“When you have to lose 10 to 15 pounds, the last few pounds are harder to get rid of as your body compensates for weight loss by lowering your resting metabolic rate,” Buckley said.
It’s also tricky for patients who begin to gain muscle as they lose fat. The number on the scale may not change, but they should notice a tighter body with less wobbly fat tissue.
Many people trying to lose weight ask if it’s better to exercise or improve their diet.
“You need both,” Buckley said. “Our bodies are designed to store fat.”
Taking leisurely stroll around the block may be a good way for deconditioned people to start and is certainly better than doing nothing. However, it’s no calorie torch. The American Heart Association recommends 150 minutes of moderate intensity exercise or 75 minutes of vigorous exercise weekly to maintain the same weight. To lose weight, one will need to decrease caloric intake and move more. It’s also important to engage in strength training twice weekly.
“A body that has more muscle burns more calories at rest,” said Alicia Olsen, nutritional counselor at the Center for Weight Loss and Surgery at Upstate. “It’s a more effi-




cient machine.”
Most smartphones come equipped with a fitness app that can help determine calories burned by activity based upon your weight. High calorie burners include running, martial arts, spinning, swimming, jumping rope and HIIT workouts. They involve major muscle groups and continuous movement.
Consuming a post-workout shake, protein bar or sports drink? If all you’re doing is a light workout, you need none of these as they negate the calories you’ve just burned. Instead, Olsen advises drinking water.

 By Deborah Jeanne Sergeant
By Deborah Jeanne Sergeant
Alicia Olsen, nutritional counselor at the Center for Weight Loss and Surgery at Upstate, offered 10 tips that result in weight loss:


1.Exercise and reduce calories


“It works better when we do both together. To lose weight, we figure out what your daily calorie needs are if they’re at rest. That’s your resting energy expenditure. We can figure it out with formulas and use some testing. Then we add in the activity factor. What do you do for activity? Let’s say by the time we add in the activity factor, you need 2,000 a day for your current weight. Subtract 500 a day to lose a pound a week. That deficit could come from exercise or eating less food or a combination of both. If you’re only walking at a slow rate for 20 minutes, you’re not burning 500 calories. If you’re eating habits don’t include the deficit, you might not meet that deficit.”
2.Eat balanced meals
“I like to ‘reduce by adding.’ I use the My Plate method. Add nutrient dense but low-calorie foods
that are high in fiber to keep you full longer.”
3.Don’t deprive yourself altogether, which is a setup for failure. “Eat a smaller serving of high calories items like meat, starches and fats.”
4.Avoid “diet” foods. “The best foods are foods you’re already familiar with.”
These include whole, unprocessed produce, lean sources of protein, and whole grains.
5.Don’t cook “special meals” for yourself. “I never want my patients to make a whole separate meal for themselves. Use the plate model to make your portions different. You can still offer the same foods but in a different proportion. Start with whole foods that aren’t processed.”
6.Hydrate calorie-free.

“Choose less sugary beverages. Go for water or flavored water over sweet tea, soda and juices.”
Prepared fancy coffee drinks, smoothies, shakes, eggnog and blended juices can contain hundreds of calories. If you really want one of these, watch the portion or make your own at home with tweaks to cut calories.
7.Minimize restaurant foods, which are often high in calories. “Cook more at home. Pack a lunch and avoid fast food.”
8.Move more. “It can be in any increments throughout the day. I count my 20-minute walk at lunch, walk the dog and an hour class at the gym. If I have a patient cancel, I do laps across the office. It’s as simple as that. It could be doing squats while helping the kids with homework. Or take the kids on a walk for family time. If you’re watching their football practice, walk laps around the stands.”
9.Seek workouts to find one you like. “There are plenty of great videos online or Netflix, Hulu or Amazon. Use your own body weight.”
10. Count calories. “Know how much you’re getting in for
the day. There are great apps on your phone to count your calories. But you need to know how many calories you need. But a dietitian can help you calculate your goals.”
 Alicia Olsen, nutritional counselor at the Center for Weight Loss and Surgery at Upstate
Alicia Olsen, nutritional counselor at the Center for Weight Loss and Surgery at Upstate

There must be something in the water in CNY.
Three sets of twins were born at St. Joseph’s Health Hospital June 10 and 11.
“In 32 years, I’ve never seen three sets of twins in 24 hours,” said Heather Shimer-Bero, director of women and infants service line. “Our labor and delivery and mother-baby colleagues showed incredible teamwork and managed all three deliveries beautifully.”

Pictured here from left to right: Kendall and Kamryn Burke, Theodore and Evelyn Kalina, and Haein and Haeyoon Jeon.

As of June 1, the FDA approved the first drug in its class to treat menopausal hot flashes. Veozah (fezolinetant) is an oral medication indicated for moderate to severe hot flashes.
Although hormone therapy is well-tolerated for some women, others do not want it or cannot have it. Hormone therapy has been linked with an increased risk of breast cancer and cardiovascular disease.
“It is good to have a non-estrogen product for women,” said pharmacist Sarah Driscoll, pharmacy operations supervisor at Oswego Health.
Veozah is a different class of medication than previous drugs used to treat hot flashes. It works by interrupting the pathways in the brain related to hot flashes, which is a different mechanism for reducing hot flashes than other prescription drugs. During its trial by week one those taking Veozah experience a 50% reduction of hot flashes and that continues to improve by week 12. The diversity of the trial, both in the ethnicity and BMI of the participants, bodes for a much broader efficacy than trials that include fewer types of women.

“Since it’s metabolized by the liver, if you have liver dysfunction, it’s probably not best for that patient,” Driscoll said.
Patients’ liver function is monitored every three months for the first year they use Veozah for this reason. Patients will need to shoulder these costs.
She added that side effects could include nausea, vomiting, and, because of liver dysfunction, yellowing of the eyes and skin. Veozah is contraindicated for women with liver disease or liver problems.
“It’s a conversation patients should have before starting it,” Driscoll said. “If patients have cirrhosis of the liver or end-stage renal disease, they should not take it.”
Sleepiness is another side effect of Veozah. However, many menopausal women struggle with sleep, so most women do not find that bothersome if they take their dose in the evening. Some women expe-
Women with abnormally heavy and painful menstruation should not ignore the issue.
Most women experience a period that lasts two to seven days and expel two to three tablespoons of blood over that timeframe. Minimal cramping or managing cramping with over-the-counter medication is normal. However, extremely painful, debilitating cramps are not. The latter can cause women to take sick leave.
For example, extreme bleeding can cause iron deficiency or chronic anemia. Women may experience chronic fatigue. It can even cause issues with mental health and cognition.
Many women delay seeking help for heavy periods. If it’s minimized, they may think they’re “being wimps” for speaking up and asking for help from their healthcare providers.
“Sometimes, it can be embarrassing for women to discuss the amount of bleeding or how much it’s affecting their quality of life,” said Keila Muniz, urogynecologist with St.
Joseph’s Health. “It can be difficult to get into see a clinician, depending on availability, office wait times and insurance coverage. Some patients have a fear of what the pelvic exam actually entails, especially if they’ve had a prior negative exam or history of abuse. The other thing is that sometimes unfortunately, a heavy bleeding episode can indicate a pregnancy or pregnancy loss.
“It’s something that patients need to come to terms with. It’s important for patients to advocate for themselves and if they get resistance, they need to insist they see a specialist who can help them with menstrual issues.”
Many women may also fear a diagnosis of uterine or cervical cancer or a disease in their reproductive system. But Muniz said that it’s more likely that the cause is a benign polyp, uterine fibroids, trauma or an injury or fall.
The thought of various treatments may prevent them from seeking help. However, Muniz said that treatment may include medication, surgery or other interventions.
rience nausea and gastrointestinal upset.
The medication should be a “tier 2” medication, indicating that most insurance will cover it with a moderate co-pay for patients. But if it is out-of-pocket, it could cost up to $600 per month. Driscoll said that would be a barrier for many women.
Keila Muniz, urogynecologist with St. Joseph’s Health, said that she offers menopausal patients numerous strategies
for dealing with hot flashes, including using air conditioning and fans and dressing in layers to tame the heat. Some non-hormonal medication may help, like selective serotonin reuptake inhibitors.

“These are used for depression but in low doses are good for just hot flashes,” Muniz said. “It’s a pleasant surprise when patients say that they didn’t know that would help.”
SSRI medication offers dual use. The North American Menopausal Society states on its website that women going through menopause are especially prone to depression and that they experience double the rate of depression of younger women.
“We have non-hormonal medication, hormonal medication and more,” said Michelle Chin, physician with Rochester Regional Health.
As to which is appropriate depends upon other health factors and the patient’s preference.
Heavy periods do not often indicate a serious issue. In fact, “most likely, there’s nothing seriously wrong and there’s a treatment that can give them relief,” said Carol Peterson, physician and assistant professor at URMC.

“It’s important to pay attention to this because most of us don’t have lifestyles that can sustain four to five days of cramps and misery,” she added.
Very heavy periods could also indicate fibroids, endometriosis or cancer. Even these more serious diagnoses can potentially be treated. But the first step is to seek help from a provider.
“Talk with your doctor and figure out what’s going on,” Peterson
said. “You can take medication that help decrease the flow. We have a lot of ways to treat heavy periods. You may have a form of hemophilia, which is treated in a different way. Some just have very heavy periods but can be treated.”
For very heavy bleeding, tampons and pads may need changing more than is convenient. Washable period underwear can also provide an additional barrier of protection against leaks.
Menstrual cups and disks require less frequent attention and are reusable, saving money and landfill space. Using a cup can also help women know exactly how much they’re bleeding as some cups include measuring marks. This information can be helpful when talking with a healthcare provider.
Women should discuss with their healthcare provider how to address heavy periods and how treatments relate to their other health concerns and any medications.
Extreme bleeding can cause iron deficiency, chronic anemia and fatigue. It can even cause issues with mental health and cognition
As the parent of two children who enjoy making music, the end of the school year meant quite a few concerts.
The music in these concerts left much to be desired. My ears were accosted by squeaks and squawks, massively out-of-tune notes, early and late entries, rhythmless rhythms, painful syncopations and monotone singing.
Yet, I loved every second of those performances.
In all of that novice playing and terrible cacophony, there was such beauty. In fact, it was so beautiful, I found myself tearing up at several points. I wasn’t moved by the beauty of the music; I was moved by the beauty of their beginnings. Their novice playing reminded me how terribly important it is to be terrible at things.
As adults, we often forget that it’s OK to be bad at things. Most of us stick to things we are good at. Our brains are aging and less pliable, thus we’re less receptive to learning new
things. Those rough-around-the-edges musical performances reminded me of something I’d almost forgotten: when you learn something new, you almost always start at terrible, and that’s OK.
The more I think about this concept, the more I think I should be talking to my kids about it. Most humans, regardless of their age, want to skip over terrible and move right on to talented.
But it doesn’t work like that.
When you learn something new, you’re training your brain and learning new habits. That’s really hard work, but it’s worth it.
These musical performances got me thinking about my role as a coach in my children’s lives. How do I help them understand the hard work is worth it? How do I help them see the beauty in the fumble and struggle? How do I model that behavior as a parent?
I don’t have all of the answers, but I have some ideas. Here are some ways to encourage your kids to em-
bark on the journey from terrible to talented (and empowered).
The only way to believe they can do hard things is to do those things.
It seems so basic; yet it’s so hard to embrace. If we want our kids to believe in themselves, we need to give them proof they can do it. As coaches, we need to nudge our kids to do difficult things and come out on the other side.
When they start learning something new, that’s the worst they’ll ever be.
It doesn’t get any worse than day one, and there is a strange sort of solace in that. We should help our kids find that solace. We need to reinforce that practice will make them better, and better will feel good. There’s nowhere to go but up.
They’ll feel more pride than they thought possible.
We should teach our kids that they don’t need to wait until mastery to feel proud of themselves. There is no accomplishment too small to feel proud of. We need to help them see how their small accomplishments add up to meaningful and great achievements. However, the small accomplishments are where the most joy can be found.
When they look back, they’ll be impressed by how far they’ve come.
We can help our kids understand how far they’ve come if we actually track their progress. We can help them track their progress in a notebook, photographs, videos or an app. If we let them see for themselves where they were a week, month or year ago, they will feel better about today. The evidence will help them inspire themselves.
When they start out with a team, that team gets less terrible together.
Sometimes, progress is bigger than one person. When our kids are part of bands, teams or groups, we should strive to help them see the beauty in collective progress. When people work hard and make progress together, they accomplish beautiful and meaningful things.
Learning doesn’t stop when they’re a grownup, so practice now.
As parents, we need to reinforce that learning is a lifelong practice. There isn’t a certain age where someone magically knows everything. We need to model that it’s OK to be terrible at something when one is 8 years old or 88 years old. We need to demonstrate we’re lifelong learners who are still terrible at things and help them see how awesome that is.
The act of learning is likely more fun than the act of mastery.
When they’re learning something new, they’re free to fail at it. As parents, it’s our job to coach our kids on how to enjoy the ride. Mastery can be a tedious exercise, but starting a new journey is an act of optimism and hope. We can help our kids see that light.
Conclusion
The next time your kid is hesitant to be terrible at something, remind them how cool it is to be terrible and what they will get out of the journey to good. Learning something new and getting better at it can actually be a lot of fun. Let’s talk to our kids about the beauty in beginnings and help them see all of the beautiful possibilities that lie in the terrible beginnings.


Men and women can experience a variety of issues related to problems in what’s called the pelvic floor, the network of muscles and ligaments around the pelvis.
Fortunately, strengthening therapy can get these problems under control.
A urologist from Baylor College of Medicine in Houston explains how this works.
“Like physical therapy is helpful for a knee or shoulder injury, pelvic floor therapy works the muscles in the pelvic floor to rehabilitate those muscles from injury or destruction,” physician Rotimi Nettey, an assistant professor in the department of urology, said in a school news release.
The pelvis is bordered by the hip bone and pubic symphysis — the joint between your left and right pelvic bones. It supports internal organs, including the intestines, bladder and rectum. In women, it also supports the uterus and vagina; in men, the prostate. This network is important for urination, bowel movements, supporting sexual function and childbirth.
Urinary and fecal incontinence, constipation, pelvic organ prolapse, pain with intercourse and sexual dysfunction are conditions that can
be treated with pelvic floor therapy. For women, this can be helpful after childbirth or during pregnancy. Men may seek out therapy after prostate surgery, Nettey said.
Pregnancy is the most common cause of injury to the pelvic floor because the uterus can compress various muscles and nerve groups, straining them as they are relied upon for more support. Vaginal delivery can bring trauma to the pelvic floor ligaments and muscles, causing lacerations or tears.
Pelvic floor therapists use a variety of techniques. These can include relaxation and “down” training exercises for those with an overactive bladder or a tense, high tone pelvic floor. Myofascial release -- a type of gentle massage -- can be helpful for patients with pelvic floor pain. Biofeedback therapy is another option.
“Pelvic floor therapy helps empower patients because they can do it on their own once they see a therapist who can extend those lessons they learn in therapy,” Nettey said. “It’s beneficial and harmless to patients and is pretty noninvasive compared to other therapies offered. Patients who are interested in learning more about pelvic floor therapy should consult their urologist or gynecologist.”






Is it possible to collect Social Security benefits from my ex-spouse? We were married for 12 years but have been divorced for almost 20 years now.
Never Remarried
Yes, depending on your specific circumstances, you may very well be eligible for divorced spouses Social Security benefits. Here’s what you should know.

A divorced spouse can collect a Social Security retirement benefit on the earnings record of their ex-husband (or ex-wife) if you are at least age 62, were married for at least 10 years, are unmarried, and are not eligible for a higher benefit based on your own earnings record.
In order to collect, your former spouse must also be at least 62 and eligible for Social Security benefits. But he doesn’t have to be receiving them in order for you to collect divorced spouse’s benefits, as long as you’ve been divorced for at least two years.
Even if your ex is remarried, it won’t affect your right to divorcee benefits, nor will it affect your ex’s retirement benefits or his current spouse’s benefits.
A divorced spouse can receive up to 50% of their ex’s full Social Security benefit, or less if they take benefits before their full retirement age, which is 66 for people born in 1945-1954 but is gradually increased to age 67 for people born in 1960 or later. To find out your full retirement age and see how much your benefits will be reduced by taking them early see SSA.gov/benefits/retirement/ planner/agereduction.html.

Keep in mind though, that if you qualify for benefits based on your own work history, you’ll receive the larger of the two benefits. You cannot receive benefits on both your record, and your ex’s work record too.
To find out how much your retirement benefits will be, see your Social Security statement at SSA.gov/ myaccount. And to get an estimate of your ex’s benefits, call Social Security at 800-772-1213. You’ll need to show your marriage certificate and divorce decree to prove your marriage lasted at least 10 years along with his Social Security number to get it.
You also need to be aware that working can affect your divorced spouse’s benefits. If you start taking benefits while working, and are under full retirement age, your benefits will be reduced $1 for every $2 you earn above the annual limit, which is $21,240 in 2023. In the year you reach full retirement age, however, the annual limit increases to $56,520 and the reduction lowers to $1 for every $3 above that limit. See SSA. gov/pubs/EN-05-10069.pdf for more details.
Another factor that can reduce your divorced spouse’s benefits is receiving a pension from an employer that did not withhold Social Security taxes (like a government). This is a rule know as Government Pension Offset (see SSA.gov/benefits/retirement/planner/gpo-calc.html) which can reduce your benefits by twothirds of the amount of your pension.

You also need to know that when your ex-spouse dies (and if you were married for 10 or more years), you become eligible for divorced survivor benefits, which is worth up to 100% of what your ex-spouse was due.
Survivor benefits are available to divorced spouses as early as age 60 (50 if you’re disabled). But if you remarry before 60, you become ineligible unless the marriage ends. Remarrying after age 60 will not affect your eligibility.

Also note that if you are receiving divorced spouses benefits when your ex-spouse dies, you will automatically be switched over to the higher paying survivor benefit.
For more information visit SSA. gov/benefits/retirement/planner/ applying7.html and click on “Benefits for Your Divorced Spouse.”


Every July, we take pride in celebrating our nation’s independence. For nearly 90 years, our programs have helped provide financial independence to millions of hardworking people. We have useful online tools like the Social Security Statement (statement) and our benefits estimator tool that help people not yet receiving benefits. The statement shows the benefits that you and your family may be entitled to includes personalized fact sheets tailored to your age and earnings situation. The benefits estimator tool allows you to get estimates based on different ages you want to begin receiving benefits. These tools can help you plan for financial independence in retirement.
Don’t receive benefits? You can get the most out of your online experience if you have a personal My Social Security account. You can:
• Get your statement instantly.
• Request a replacement Social Security card (in nearly every state and the District of Columbia).
• Find out if you qualify for benefits.
• Appeal a decision we made on
Q.: Will my retirement benefits increase if I wait and retire after my full retirement age?

A: Yes. You can increase your Social Security retirement benefit in two ways:
• You can increase your retirement benefit by a certain percentage if you delay receiving retirement benefits. We will add these increases automatically from the time you reach full retirement age until you start receiving benefits or reach age 70.
• If you work, each additional year you work adds another year of earnings to your Social Security record. Higher lifetime earnings may result in higher benefits when you do retire.

For more information, visit www. ssa.gov/pubs to read, print, or listen to our publication, “When to Start Receiving Retirement Benefits.” You also can use our “Retirement Estimator” at www.ssa.gov/estimator to determine your estimated future benefits.
Q.: Will my Social Security disability benefit increase if my condition gets worse or I develop additional health problems?
A: No. We do not base your Social Security benefit amount on the severity of your disability. The amount you are paid is based on
your claim.
Already receiving benefits? If so, you can use your personal my Social Security account to:
• Request a replacement Social Security card (in nearly every state and the District of Columbia).
• Get an instant benefit verification letter for Social Security, Medicare, and Supplemental Security Income (SSI).
• Start or change your direct deposit (Social Security beneficiaries only).
• Check your information and benefit amount.
• Change your address (Social Security beneficiaries only).
• Request a replacement Medicare card.
• Get a replacement SSA-1099 or SSA-1042S instantly for tax season.
• Report your wages if you work and receive disability benefits or SSI.
You can create your personal My Social Security account at www.ssa. gov/myaccount.
With so many services and helpful information available online, we are here for you when it’s convenient for you. Be sure to tell friends and family about all they can do at www.ssa.gov.
your average lifetime earnings before your disability began. If you go back to work after getting disability benefits, you may be able to get a higher benefit based on those earnings. In addition, we have incentives that allow you to work temporarily without losing your disability benefits. For more information about disability benefits, read our publications “Disability Benefits and Working While Disabled — How We Can Help.” Both are available online at www.ssa. gov/pubs.
Q.: My grandfather, who is receiving Supplemental Security Income (SSI), will be coming to live with me. Does he have to report the move to Social Security?
A: Yes. An SSI beneficiary must report any change in living arrangements before the 10th day of the following month. If you do not report the change, your grandfather could receive an incorrect payment and have to pay it back, or he may not receive all the money that he is due. Failure to report a change to us could result in the deduction of a penalty from his SSI benefits. Your grandfather also needs to report the new address to us to receive mail from us. You can report the change by mail or in person at any Social Security office or call us toll-free at 1-800-772-1213 (TTY 1-800-325-0778). You
get more
We applaud our laboratory professionals. Those who have recently joined us and the dedicated employees who have been with Laboratory Alliance since we began 25 years ago. They all play a vital role in health care and patient advocacy.

The people behind the laboratory report are critical players in the diagnostic process. While most patients do not have contact with our laboratory professionals, they play key roles in the detection, diagnosis and treatment of disease.



We have positions available for qualified New York state-licensed medical technologists and technicians. Join our team and make a positive difference in the lives of others.




Internal Medicine Associates of Auburn, located at 77 Nelson St., has placed in the top tier for excellence out of primary care groups in the Upstate New York market in 2022.
Through participation with the UnitedHealthcare MA-PCPI and MCAIP (Medicare Advantage Primary Care Physician Incentive) performance programs, the practice is focused on patient and provider collaboration, patient engagement, preventive medicine, early disease management and chronic disease management.

The practice achieved a near perfect performance score of 4.64 out of a possible five-star rating in 2022, based on the Centers for Medicare and Medicaid Services five-star qual ity rating system.
“We are honored to earn this outstanding recognition for the 2022 performance year,” practice officials stated in a press release. “The achievement is a direct result of a determined and systematic approach toward managing our patient population. The process is an ‘all in’ team commitment at the practice level, as well as thoughtful collaboration with our patients. Additionally, we value shared communication within our medical community as we all strive to improve the health of our mutual patients.”
Serving the Auburn community since 1975, Internal Medicine Associates of Auburn includes four medical doctors board certified in internal medicine, five nurse practitioners certified in adult or family medicine and thirty-six support staff.
The practice serves over 12,000 patients from Auburn and the surrounding areas.
For the third year in a row, Life
time Benefit Solutions (LBS) has been inducted into the Circle of Excellence by WEX, the global commerce platform.
a full suite of ancillary benefits and specialty programs to help round out employer’s traditional benefits. Each is built with scalability and flexibility in mind, providing added security to help both businesses and employees grow.
“The achievements and accomplishments of our Circle of Excellence members inspire us all to reach higher and do more,” says Robert Deshaies, chief operating officer of the Americas, WEX. “These organizations repeatedly rise to challenges and serve as catalysts for innovation. We are honored and humbled to celebrate their successes.”
To learn more about LBS, visit www.LifetimeBenefitSolutions.com.

Nancy Williams has been hired
management from Walden University, a Bachelor of Science degree in nursing from Syracuse University’s College of Nursing, and a Bachelor of Science degree from SUNY Brockport.
Nancy is an Auburn native and resides in Tully with her husband and family.

Board-certified and fellow
vascular neurosurgery at the State University of New York at Buffalo.
After completing his fellowship training, Eller joined the faculty at Thomas Jefferson University department of neurosurgery, where he has served for several years as a clinical assistant professor and cerebrovascular and endovascular neurosurgeon at the AtlantiCare Neurosciences Institute, a member of the Jefferson Neurosciences Network. In this capacity, Eller has helped develop several neurosurgical service lines at AtlantiCare, including a comprehensive stroke center, multidisciplinary neuro-oncological and skull base surgery as well as providing general neurosurgical trauma care in support of the institution’s trauma center. Eller also earned a master’s in business administration from Widener University in Pennsylvania.
Trish Mooney
Syracuse-based LBS, with offices in Rochester and Buffalo, is an industry leader in designing, developing, and deploying reimbursement accounts, COBRA, retirement accounts and other employee wellness-related plans that promote employee health while safeguarding a company’s financial health.
“This honor places LBS among the top echelon of third-party administrators,” says LBS President Trish Mooney. “We are so proud of our team!”
Lifetime Benefit Solutions offers
as the new chief people officer at Loretto. Williams was previously the director of patient experi ence and logistics for Crouse Hospital, and is a long-term Loretto board member. In her new role at Loretto, she will be responsible for the newly restructured human resources, shared services and talent management teams.
ship-trained cerebrovascular and endovascular neurosurgeon Jorge Eller, who previously served as a member of the team at Crouse Medical Practice Neurosurgery, has recently returned to the practice.
“Dr. Eller is highly regarded, and we’re proud to offer his experience, education and advanced training to our patients once again,” said President and CEO Seth Kronenberg, MD.
“Nancy brings a wealth of indepth experience to this position, including several advanced leadership positions at Crouse spearheading experience programs, managing diverse teams, leading strategic planning initiatives and driving significant process improvement projects to improve system throughput and quality care,” said Kimberly Townsend, president and CEO at Loretto.
Williams has an extensive clinical background and managed several large clinical teams during her tenure, including expertise in complaint and formal grievance management. She joined Crouse Hospital in 2000 as an registered nurse on the intensive care unit and graduated from management of the cardiac care center into her broader roles in patient experience and people leadership.

In addition to serving as a trustee for the Loretto Management Corporation board for more than five years, she is active in many community and human service organizations, including the Schwartz Center for Compassionate Healthcare, the Association for Patient Experience, the Beryl Institute, the American Nurses Association, and Administrators of Volunteer Services (AVS). She also served as a board member for Sarah’s Guest House for six years and remains an active supporter of the organization, and served as a member on several St. John Fisher College dissertation committees.
Williams holds a Doctor of Education degree in executive leadership from St. John Fisher College, a Master of Science in nursing, leadership and
Eller returns to Crouse from Eisenhower Neuroscience Institute in California. He is board-certified by the American Board of Neurological Surgery since 2008 and is a member of the American Association of Neurological Surgeons and the Congress of Neurological Surgeons. “I’m pleased to have returned to Central New York to practice at Crouse, which has been deeply committed for many years to the delivery of advanced neurosurgical techniques in the area’s most state-of the-art facility,” said Eller.
He specializes in the treatment of brain, spinal and peripheral nerve pathologies in general, such as brain and spinal tumors; pituitary tumors; cervical or lumbar disc herniations; cervical or lumbar spinal stenosis; and carpal tunnel or ulnar nerve entrapment. In addition, he uses advanced microsurgical and minimally invasive endovascular treatment of cerebrovascular pathologies, such as intracranial aneurysms; arteriovenous malformations and fistulas; carotid stenosis or dissections; intracranial vascular stenosis and strokes, as well as chronic subdural hematomas, facial pain and trigeminal neuralgia.
After earning his medical degree from the Federal University of Espirito Santo Medical School in his native Brazil, Eller completed an internship in general surgery and residency in neurological surgery at SUNY Upstate Medical University. After his residency, he completed a fellowship in stereotactic and functional neurosurgery at Oregon Health and Science University in Portland, Oregon, where he subsequently served as an assistant professor of neurological surgery and chief of neurosurgery at the Portland VA Medical Center. In 2010, he joined the neurosurgical faculty at Saint Louis University, where he completed a fellowship in cerebrovascular and skull base surgery, followed by a fellowship in endo-
St. Camillus has recently been recognized as a 5-star rated facility by the Centers for Medicare & Medicaid Services, (CMS)
CMS developed the 5-star quality rating system to provide consumers, families and caregivers with an easy way to search for nursing homes and to help them decide which facilities to consider. The tool helps individuals compare nursing homes more easily and is an important resource in navigating the quality ratings for each facility.
According to the CMS website, CMS.gov, its nursing home care compare feature highlights a quality rating system that gives each nursing home a rating of between 1 and 5 stars. Nursing homes with 5 stars are considered to have much above average quality and nursing homes with 1 star are considered to have quality much below average. There is one overall 5-star rating for each nursing home, and separate ratings for health inspections, staffing and quality measures.
“Achieving this 5-star rating by CMS is an incredible accomplishment. We couldn’t have done it without our dedicated, compassionate staff who consistently go above and beyond the call of duty to enrich the lives of our residents and the tireless support of the entire St. Camillus community,” said Michael Schafer, president of St. Camillus. “It is truly a testament to the quality of services and standard of care we are committed to providing to our residents each and every day.”
“The 5-star rating system is increasingly used by consumers, regulators, insurers and provider networks to make informed decisions about engaging with the facility. We are thrilled to share this 5-star rating with our community and celebrate our staff’s commitment to excellence in quality of care” said Kathy Barber, vice president of quality management.
St. Joseph’s Health recently
welcomed physician Andrew Call to St. Joseph’s Physicians Primary Care in Cicero.
According to St. Joseph’s, Call is a welcome addition to the team of family medicine physicians and staff. Having practiced for many years in the Rochester area, he brings a passion for applying his medical knowledge and skills in the diagnosis and prevention of illness.

“I’m really enjoying working in Cicero. The entire team sincerely cares about our patients, and each other. We have a stellar group of colleagues working together to support our patient’s health goals,” said Call. “I have felt very supported during my transition to work and life in Syracuse and am happy to be a part of this community.”
Upstate Medical University
officially opened the Nappi Wellness Institute in a ribbon-cutting ceremony Friday, June 2.

The five-story, 209,615-squarefoot building will be the centerpiece of Upstate’s outpatient care, bringing key ambulatory services under one roof. The innovative floor plan features 240 exam and consult rooms with workstations located to facilitate and foster provider interactions.
The building’s unique design features the integration of preventive medicine with an emphasis on wellness. The facility has been built to WELL Building Standards with design features to address air, comfort, fitness, light, mind, nourishment, water, movement, sound and community. Once certified, the Nappi Wellness Institute will be the first WELL certified building in Central New York.
The building is named for Sam and Carol Nappi, whose $8 million gift to the Upstate Foundation is the largest monetary gift in the foundation history.
“The Nappi Wellness Institute is a transformative health care facility that we are proud to have as part of our campus,” said Upstate Medical University President Mantosh Dewan, MD. “Wellness is indeed its middle name for healing and wellness is reflected throughout the facility, in its design, in its mechanics, in its operations, in the way our health care professionals work and in the way our patients will be cared for.
“We are grateful to so many who have made this moment a reality,”
Dewan continued. “To Sam and Carol Nappi for their support, to the hundreds of workers who have spent more than three years—most of that time during the pandemic—building this structure, to our great team here at Upstate for ensuring that this facility is the source of the very best care in our region.”
Physician Robert Corona, CEO of Upstate University Hospital, joined Dewan in echoing the facility’s focus on wellness. “The inspiring nature of the Nappi Wellness Institute is the focus on wellness in every aspect of its design and operation—and that benefits our patients and supports our providers,” he said.
The Nappi Wellness Institute houses an array of services, practices and programs, including adult and pediatric primary care, geriatrics, radiology, laboratory services, behavioral health, family medicine, pediatrics, the Center for International Health, Inclusive Health Services and the Joslin Center for Diabetes (adults and pediatrics), which has relocated from its East Genesee Street location three miles away. The building also features several supportive ancillary services and Connect Care to ensure seamless post-acute follow-up for patients.
Primary care, behavioral health, specialties, palliative care and social supports will be integrated to reduce fragmentation and promote patient-centered multidisciplinary care in a single location. Primary care and behavioral health providers will share in the care of patients, development of care plans and education of
patients and families.
A key feature of the building will be the expansion of Upstate’s Center of Excellence for Alzheimer’s Disease, which has its clinical site within geriatrics. Several clinical services will collaborate to enhance the care to these patients including a cognitive neurologist, additional space for neuropsychological testing, physical therapy and convenient space for families to drop off and pick up patients.
“The greater Syracuse area has the highest concentration of older adults in New York state, so we are excited to amplify the services we can offer to this expanding population,” said SUNY Distinguished Service Professor and Geriatric Medicine Chair Sharon Brangman, MD. “We anticipate that we will see patients with dementia and Alzheimer’s disease in greater numbers. This facility will ensure that we have the space to care for patients, consult with families and provide us immediate access to other specialists.”
Wellness isn’t just the purview of practitioners; the building itself is defined by wellness.
“The goal in pursuing WELL certification for the Nappi Wellness Institute is to create a world class health care facility that promotes the health of all those it serves and those who work there,” said Marylin Galimi, Upstate’s chief operating officer.
The building is located on the corner of Sarah Loguen and East Adams streets, across the street from the Upstate Cancer Center.
In addition to the gift from the Nappis, funding for the $158 million project came from a $70.6 million grant as part of the State Department of Health’s Capital Restructuring Financing Program and Essential Health Care Provider Support Program. An additional $70.6 million in matching bonds was issued by New York state.
Upstate broke ground on the project in early 2020.
Call earned his medical degree from Mount Sinai School of Medicine (now Icahn School of Medicine at Mount Sinai) and his undergraduate degree in biology from SUNY Alfred. Following a family medicine internship, Call completed his residency at the University of Rochester/ Highland Hospital family medicine residency in Rochester, where he served as chief resident. He is boardcertified by the American Board of Family Medicine.
St. Joseph’s Physicians
announced physician Renee Groetz recently joined its hospitalist team.

As a hospitalist, Groetz cares for patients from the time they enter the hospital, to the time they’re discharged. She handles diagnosis, treatment, and coordination of care of needed specialists. This model of care improves the efficacy of care and patient outcomes leading to greater patient satisfaction, according to a hospital press release.
Renee Groetz
“I am excited to join the hospitalist team at St. Joseph’s Health Hospital and give back to the community I grew up in,” said Groetz. “I completed my residency at St. Joseph’s and decided to accept a position after graduation because of the supportive staff and colleagues I work with every day.”
Groetz holds a medical degree from Saint James School of Medicine, Park Ridge, Illinois. She earned an undergraduate degree in biomedical sciences graduating magna cum laude from the University at Buffalo. She completed her family medicine residency at St. Joseph’s Health Hospital where she served as chief resident.
Crouse recently welcomed five summer interns from MercyWorks’ Synergy internship program. They’ll be working Monday through Thursday until Aug. 3.
The Synergy Leadership Internship offers college-enrolled students the development, training and exposure they need to succeed. Through the 10-week internship, students are placed in a summer experience targeted toward their field of study.


Students are:


• Ahmed Ghanem, business administration–CPA program from Onondaga Community College (finance, Wes Sprague and Sean Barron)
• Chadani Timsina, pre-med, Dartmouth College (ED, Michelle Michael-Korn)

• Abdias Nguemadi, human resources, Niagara University (HR, Michelle Murphy)
• Mohamed Alhaj, information security, Syracuse University (IT, Aaron Armelino)

• Jamal Aden, information technology, Syracuse University (IT, Dan Turton)

MercyWorks is a nonprofit organization that operates the Clarence


The screening will be offered from 6:30 to 9:30 a.m. A 12-hour fast is required.
Jordan Vision
Their mission is to empower youth and under-served individuals in the community.

Oswego Health’s annual multi-organ blood analysis will be offered July 15th at the Fulton Medical Center in partnership with the Fulton Kiwanis Club.
This full battery of tests can help prevent potential health problems. The cost of the analysis is $55 and for every participant, Oswego Health
will donate $5 to the Fulton Kiwanis. Typically, these tests can cost more than $760.
In addition, there are two optional tests that each cost an additional $20. They include the prostate specific antigen (PSA) test, which is recommended to men older than age 50, as well as a vitamin D test.
Community members are encouraged to make their appointment online at www.oswegohealth.org/ bloodanalysis. Questions about the event, please call 315-532-5813 weekdays, 8 a.m. -3:30 p.m.






The Oswego Health Foundation announces its eighth annual “For Your Health 5K and Wellness Event,” presented by Excellus BlueCross BlueShield, will be held Saturday, Aug. 12. Runners and walkers of all ages and levels are encouraged to participate.
As a nonprofit healthcare system, Oswego Health relies on events such as this to support the healthcare needs and initiatives of the commu-

nity. The event will focus on overall wellness and feature community partners, local vendors, and resources to help strengthen the health of the community. In addition, the event will feature a kids’ fun run at 9 a.m. and the “For Your Health” 5K run/ walk will start at 9:30 a.m. at the scenic course on the Seneca Hill campus, between Fulton and Oswego, off Route 481 on Route 45A.
Awards will be presented to the top three overall male and female 5K finishers in both the walking and running divisions of the For Your Health 5K. Community members can register online at www.oswegohealth.org/5k.
Local businesses or organizations can also enter a team. For more information, contact Michele Hourigan at 315-326-3788.
This year’s presenting sponsor is Excellus BlueCross BlueShield.






Frank chose non-surgical CyberKnife® at HOA –offering 5 treatments instead of 35!

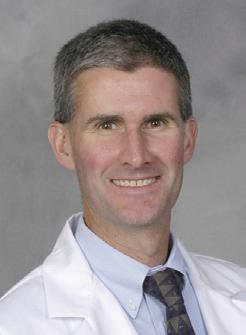










“The original diagnosis was to treat my prostate cancer with seven weeks of radiation, five days a week. I was kind of upset that I was never given the option of CyberKnife,” said Frank. “The precise radiation achieved by CyberKnife, far fewer treatments, and the personalized care I received from Dr. Chin and his team made my decision an easy one. Better, the treatment was a real success!”



