Lessons Learned from a Boy with Autism


‘LOVE




‘LOVE


Playing with a dog for just 15 minutes can significantly reduce a person's stress, a new study reports.
Stressed students who interacted with a friendly dog reported less stress, had a reduced heart rate and had lower levels of the stress hormone cortisol in their saliva, researchers said in the journal PLOS One.
The experience also appears to be beneficial for dogs, researchers added. Fecal tests showed that canine cortisol levels were lower a week after hanging with a human.
“Even brief interactions with dogs can significantly reduce stress levels among university undergraduate students,” concluded the research team led by senior investigator Jaruwan Khonmee with Chiang Mai
University in Thailand.
For the study, researchers recruited six friendly dogs 3 to 6 years old to interact with college students. They included five chihuahuas raised by veterinarians and a Shetland sheepdog raised by a psychologist.
None of the dogs were certified for therapy work, researchers noted. This was the first time they'd participated in any sort of canine-assisted intervention, and they participated without the presence of their owner.
In the main library of Chaing Mai University, 122 students completed a stress assessment questionnaire, had their blood pressure and pulse taken, and provided a saliva sample for cortisol testing.
They then were given 15 minutes to play with a dog after being told the pooch's name, personality traits
and preferred interactions.
The students could do whatever they wanted — look at the dog, pet it, give treats, hug it, play with it.
Afterward, they went through another round of tests to assess their stress levels.
The dogs provided fecal and saliva samples before and after their time with students, to see whether the play benefited them as well.
Students showed self-reported and physical improvements in stress following their 15 minutes with a dog, results show.
“Compared to immediately before, students' self-reported stress levels decreased by 33.5% after interacting with the dog,” researchers reported.
The students also had improvements in their pulse rate and cortisol
levels, researchers noted.
There were no changes in salivary cortisol in the dogs on the day of play, but their fecal cortisol levels were lower a week after they spent time with the students, researchers said.
“Overall, these findings contribute to our understanding of the beneficial impact of human-dog interactions on human stress levels and highlight the importance of addressing stress in both humans and animals during targeted interventions,” researchers concluded.
“In contexts where certified dogs and handlers are not readily available, non certified dogs could still offer mental health benefits,” the team added.



Two groups focused on food safety and environmental toxins have sued Girl Scouts of America, claiming that their perennially popular cookies are tainted with pesticides and heavy metals.
GMO Science and Moms Across America filed court documents in March in New York, based on a December 2024 study that tested 25 cookie samples in three states, according to Tribune News Service. The suit names Girl Scouts of the United States and the two bakers that produce the tasty treats — ABC Bakers and Ferrero USA's Little Brownie Bakers.
The confections are ubiquitous during selling season, with more than a million members of the group hawking more than 200 million packages at stores, door-to-door and via QR code. The cookie campaign raises close to $1 billion a year for the organization, according to NPR.
In a blog post last month, the Girl Scouts responded to the study commissioned by the two groups, saying that heavy metals can occur naturally in soil and aren't a safety issue.
A Queens-area woman who bought several Girl Scout cookies since January, including Peanut Butter Patties and Adventurefuls, leads the suit.
"She believed that she was purchasing quality and safe cookies consistent with the Girl Scout's promise of ethical business practices and the representations published on the (organization's) websites," the lawsuit said, adding that she wouldn't have bought the cookies or would have paid less for them if the organization had "marketed their products accurately."
The suit seeks at least $5 million in damages for cookie buyers for alleged violations of consumer protection and labeling laws.
The study said Girl Scout cookies tested had higher than recommended levels of at least four of five heavy metals: arsenic, aluminum, lead, cadmium and mercury, GMO Science reported in December.
High levels of exposure can harm human health and the environment, experts say.
This isn't the first lawsuit tied to the presence of heavy metals in food products, according to the news agency Reuters. It noted that several chocolate makers, including Hershey's, have faced such legal actions.

By Chris Motola
Natalie Hartigan, D.O.
Q: Let’s get the important stuff out of the way first. Did you get that snowstorm you were hoping for when you moved back here from Florida?
A: You know, we did! I was pretty impressed. My parents still live in Upstate New York, so I had been visiting them. I hadn’t been too impressed by the snow the last few years, especially around the holidays, but this year I feel like we had a good amount of snow for a while. Though outside my office window I can see green grass already.
Q: They don’t make winters like they used to.
A: I always wonder if it’s just because when you’re a kid every snowstorm feels like a big snowstorm. I don’t know if I’m just older now and that’s the change, but I do think the winters have been different lately. I think one of the best things about Upstate New York is the change of seasons. I’m excited to see all of them come and I’m excited to see all of them go.
Q: How long have you been back?
A: I came back this fall. I started at HOA in October. We moved back a few weeks before that.
Q: What’s your experience with HOA been like so far?
A: It’s been great. It’s been a really wonderful place to work so far. I really enjoy collaborating with all the other doctors. There’s a lot of expertise, especially in the new physicians just starting out. I’ve been so welcome to ask questions and bounce cases off of them. They’ve been really supportive. But then all of the other support staff too, the nurses, the schedulers; everyone has just been great. I’m so impressed as I continue to learn about the services that HOA offers and the things we try to do for our patients. It just feels like a really comprehensive patient experience. Hopefully patients feel that way as well.
Q: How did you become interested in hematology and oncology?
A: So I really like getting to know patients and getting the opportunity to build a relationship with them over time. I like that I get to focus in on a few different problems. I think there are a few areas of medicine, including oncology, where there have been so many recent advances. They’ve really been game-changing. While a lot of sad things can happen here, there’s also so much hope and so many new opportunities. This industry was one way of really getting to know patients while staying at the cutting edge of research.

referrals from different people in the community. So I’ve just been slowly building my practice that way. I see a lot of general oncology, but have been starting to see more GI oncology. GI includes some blood cancers. Some of the more chronic leukemias, though some of the more acute ones are better treated at a transplant center like University of Rochester. Though I might be their local liaison here as they’re getting care in both places. But some of the more chronic leukemias and lymphomas I take care of as well.
Q: Are blood cancers harder to manage than most other cancers? Easier?
A: Fortunately there are so many new developments that treating all cancers has become a lot more nuanced. We look for specific markers and use that to guide treatment, and with blood cancers there are a lot of specific things. It can be a little bit tricky, but overall I think we’re well-prepared for them.
Q: Is there much of a regional difference in the prevalence of certain cancers in Upstate New York relative to Florida?
A: I would say typically no, but I think they do see more skin cancer in Florida as people are exposed to more sun, but we do see a lot of skin cancers up here as well. Some cancers are more common in older people, so where the population is older we’ll see more of them.
Q: It’s a little bit of a stereotype, but D.O.s tend to be more associated with primary care, and you almost considered going into it yourself. Are there expectations you had to overcome?
Q: Are you involved in re-
A: It’s slow at first, but I’ve been shocked and impressed by how much research there is at HOA, how many clinical trials. As a new doctor here I’m slowly working my way into the research department. I have a couple patients on clinical trials, and I’m working closely with the department.
Q: How much of a patient base have you been able to build up so far?
A: There are a few patients who were transfers from physicians who moved to the Camillus office. So I’ve inherited them that way and through
A: No, I don’t think so. Historically D.O.s have leaned toward primary care, but over the last few decades that’s been evolving and changing. I never had any issues applying to jobs, fellowships or residencies that I was interested in. I think in general osteopathic medicine encourages treatment of the whole person, which can include manipulative medicine. I don’t include it in my day-to-day practice, but I do try to practice clear communication and how conditions affect people physically and mentally. When a patient comes in with a new cancer I try to make sure they’re connected to ancillary services and communicate goals and expectations rather than just telling people they have cancer and here is the chemotherapy they’re going to get. That’s one thing I like about HOA, they really try to take the whole patient into account.
Name: Natalie Hartigan, D.O.
Position: Medical oncologist
hematologist at HematologyOncology Associates of CNY
Hometown: Little Falls
Education: Lake Erie College of Osteopathic Medicine
Affiliations: Crouse Hospital, St. Joseph’s Health Hospital
Organizations: American Society of Clinical Oncology, American Board of Internal Medicine
Family: Husband, one child
Hobbies: Cooking, gardening, reading

olks facing surgery on a Friday may want to consider rescheduling if they can based on findings from a new study.
People who undergo surgery just before the weekend have a significantly increased risk of death and complications, researchers reported March 4 in JAMA Network Open.
This “weekend effect” occurred across 25 common procedures representing multiple surgical specialties, researchers said.
"Patients who underwent surgery immediately preceding the weekend had a significantly increased risk of complications, readmissions and mortality compared with those treated after the weekend," a team led by senior investigator, physician Raj Satkunasivam of Houston Methodist Hospital in Texas, concluded.
"It is important for health care systems to assess how this phenomenon may impact their practices to ensure that patients receive excellent care irrespective of the day," researchers added.
Hospitals and health care systems tend to operate with skeleton crews during the weekend, leading to concerns that patients are more likely to receive worse care on Saturday and Sunday, researchers said in background notes. This is commonly called the "weekend effect."
This weekend effect might also apply to people undergoing surgery immediately before the weekend, who will be in the hospital recuperating after their procedure, researchers explained.
To investigate this, researchers analyzed data on nearly 430,000 patients who underwent surgery in Ontario, Canada, between 2007 and 2019.
Results showed that people who underwent surgery prior to the weekend had a higher risk of death at 30 days (9% increase), 90 days (10%) and one year (12%) compared to surgeries performed after the weekend.
Pre-weekend surgical patients also fared worse on a composite score combining death, complications and need for rehospitalization, with a 5% increased risk at 30 days and one year following surgery.
In addition to reduced personnel, there are other reasons why hospitals might provide worse care close to the weekend, researchers said.
More junior surgeons with fewer years of experience operate on Friday compared with Monday, and doctors working the weekend have less access to more senior colleagues and specialists, researchers said.
"Furthermore, weekend teams may be less familiar with the patients than the weekday team previously managing care," researchers noted.
Doctors also might have less access to tests and scans that could better help guide their treatment of patients, researchers added.
"Further study is needed to understand differences in care that may underpin these observations and ensure that patients receive high-quality care regardless of the day of the week," researchers concluded.







By George W. Chapman

Lacking an organized approach to healthcare delivery in the U.S., we experience the highest cost per capita in the world and rank 40th in overall mortality. Now, our once formidable "front line" of primary care providers is battle weary and in retreat.
Thanks to the lack of any planning at the national level, coupled with decades of chronic underinvestment, providers are leaving the front line of primary care, favoring better resources (pay) and lifestyle (time) available in non primary specialties.
Fewer primary care providers (be they MD, PA, NP) results in longer wait times for appointments across all specialties; decreased access, especially in rural areas, and higher costs due to increased use of specialists and overwhelmed emergency rooms.
Of all the things that need fixing in healthcare, price transparency is way down on the list. Way, way down. Trump recently signed an executive order reinforcing the already existing rules on price transparency that were promulgated in his first term. Briefly, the rule requires insurers to post what they agreed to pay hospitals for 300 or so procedures. Then, in turn, hospitals are to post their prices for those same procedures. For the 92% of us covered by insurance, price transparency is nice but is practically useless. Price transparency means everything if you’re without insurance or your plan doesn't cover a certain procedure. For the vast majority of us, calling hospitals to check on their price for an MRI or outpatient procedure or finding out what your insurance pays the hospital for the procedure can be a waste of your time. In just about every case, you will be directed by your provider to an MRI site, hospital or outpatient center where the provider has privileges. Going elsewhere will be considered out-of-network and you could end up paying 100%. Medical billing and payment is very complicated. If we had a universal healthcare system, calling around for the best price would be totally unnecessary.
Consequently, premiums will rise across the board.
In 2022, primary care spending was only 5% of all healthcare costs. The number of primary care providers dropped from 106 per 100,000 people in 2022 to 104 per 100,000 in 2023. The trend is well established. Medical students are gravitating away from primary care (FP, Peds, OB-GYN) and toward specialties. Efforts by Medicare to "level the playing field" between primary care docs and specialists has been slow and inadequate. The best bet for a fledgling primary care resident is to avoid the economic and mental hassles of private practice and seek employment with a large hospital-centric healthcare system. And it's totally understandable. However, the trend toward the security of employ-
This is virtually the wild west of billing. If you have had to use an ambulance (and God bless our first responders who often keep you alive on the way to the ER) you probably owe more out of pocket for the ambulance ride than out of pocket for the hospital and physician services combined. Insurance coverage is all over the map (and calling ahead of your emergency for a price check is clearly not an option!) Most likely, you will end up negotiating after the bill arrives. Surprise billing regulations do not cover ambulances. These regs typically apply to bills from physicians who, unbeknownst to you, do not participate in your insurance plan even though the hospital ER does. In most cases, the hospital now pays the difference between what your plan would have paid and what the non-par doc charges. You are held harmless. Both volunteer and for-profit ambulance companies operate outside the competitive market place. Let's face it. They can because you are going to take whatever ambulance arrives first. That being said, 80% of ground ambulance rides are out of network. A case in California recently got a lot of notoriety. A jogger was struck by a car and taken via ambulance to a nearby ER just a
ment unintentionally exacerbates the shortage of providers because (ask any doc in private practice) employed docs work fewer hours than their private practice counterparts.
PCPs are the quarterbacks of healthcare. Without their involvement and direction, we will end up meandering our convoluted, confusing and disjointed "non-system" alone. Virtual visits and even AI may provide some relief and most patients who have experienced virtual care are OK with it. (Probably had no choice?) Without an adequate supply of MDs, PAs and NPs in primary care, patient frustration and premiums will invariably increase. If we are to fix healthcare, it has to start with the foundation of primary care.

few miles away. He was treated and released. The ambulance bill (again, God bless our first responders) was $13,000. After months of phone calls, the Blues [Blue Cross Blue Shield] acquiesced and paid $10,000 leaving the jogger with a $3,000 bill. After another few months of calls, this time with the commercial ambulance (and the press) the company waived the $3,000. The Center for Consumer Information and Insurance Oversight was involved. They were involved in more than 650,000 similar billing disputes in 2023. Unfortunately, 15% of their staff has been eliminated by DOGE, the Department of Government Efficiency. This is just another example of what could be fixed ahead of price transparency.
To put it mildly, things have been rather chaotic at CDC/FDA/ NIH/CMS since the election. As I'm writing this column, here it is where things stand in early March. The FDA abruptly cancelled a March 13 vaccine advisory committee meeting. The meeting is attended by experts — including drug designers, scientists, manufacturing, biologists and other healthcare stakeholders — to recommend the strains for next season's flu vaccine. The unexpected delay has raised concerns that unless a decision is made sooner than later
we won't have enough flu vax in the fall. Drug manufacturers face tight deadlines every year and this is exacerbating the problem. As of this writing in early March, 910,000 people have been hospitalized with the flu. 19,000 adults and 90 children have died from flu complications.
We spend about $5 trillion annually on healthcare or just over $14,000 per capita. It's by far more than any other country. It breaks down as the following: hospitals, 31%; other personal healthcare, 16%; physicians, 15%; drugs, 9%; clinical services. 5%; nursing homes. 4%; home care. 3%. The remaining 17% goes toward net cost of health insurance (basically overhead), investments and public health activities. For hospitals, revenue comes from three main payers: commercial insurance, 40%; Medicare, 30%; and Medicaid, 20%. The remaining 10% is self-pay, grants, investments, donations. Operating margins are razor thin for the majority of hospitals. The cuts to Medicaid will have a disproportionate impact on rural hospitals.
No one is spared from the recent purge of federal employees and our veterans are no exception. They comprise 30% of the VA workforce. The VA has been ordered to cut 80,000 jobs (nurses included) or 15% of the workforce. The goal is to return to the 2019 total of 400,000 employees. There are 170 VA hospitals and 1,380 outpatient healthcare facilities across the country making it our largest healthcare system. The VA cares for 15.8 million vets.
Congress has approved a federal budget that slashes $880 billion in Medicaid funding to indigent individuals, hospitals and nursing homes. Consequently, if the states are to continue the same level of services they must raise taxes. If the feds impose a suggested dollar per capita cap, the states will have to come up with between $700 billion and $1.1 trillion over the next 10 years. The states that would be most impacted are Arkansas, Kentucky, Louisiana, Mississippi, New Mexico and West Virginia. All these states are "red" except for New Mexico. In addition to a state tax increase, hospitals will most likely negotiate higher rates from commercial insurers to offset losses in Medicaid funding and the increase in uninsured patients seeking care in their clinics and emergency rooms.

George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse.

By Deborah Jeanne Sergeant
Deer ticks, also known as black legged ticks, can carry and transmit the bacteria that cause Lyme disease.
The illness was named for Lyme, Connecticut, where it was first identified in the US.
Unless tick bite patients infected with Lyme are treated early with antibiotics, the disease causes patients to experience swollen knees, paralysis, skin rashes, headaches and severe chronic fatigue.
Late-term use of antibiotics is not always as effective.
Not every tick transmits Lyme disease. Still, avoiding deer tick bites can prevent infection. Once the weather reaches above 40 degrees F., ticks can emerge. The New York State Department of Health states that deer ticks are most active from April through mid-May and also in early fall.
“The most effective way to prevent tick-borne diseases is by minimizing exposure to ticks,” said Saravanan Thangamani, SUNY Empire Innovation professor of microbiology and immunology at Upstate Medical University. “To lessen contact with ticks, steer clear of wooded areas and dense brush, especially where tall grass and leaf litter are present. While hiking, stick to marked trails and walk centrally to reduce the likelihood of encountering ticks.”
Thangamani directs the SUNY
Center for Environmental Health and Medicine and the Vector Biology Laboratories at Upstate. He is an expert in vector-borne diseases, specifically tick-borne and mosquito-borne diseases including those caused by pathogens such as the Lyme disease agent. The Upstate Tick Testing Laboratory (www.nyticks.org) also tests ticks.
“Before engaging in outdoor activities, apply insect repellent,” he said. “Treat your outdoor clothing and camping gear, including socks and shoes, with a 0.5% permethrin solution for long-lasting protection through several washes.”
Although it should not be applied directly to the skin but on clothing, backpacks and footwear, permethrin can help deter ticks. Keep permethrin away from cats. While it is wet, it’s highly toxic to cats.
“Additionally, tumble dry your clothes in a high-heat dryer for at least 10 minutes to eliminate ticks,” Thangamani said. “After coming home, shower promptly and perform a thorough tick inspection on your body and pets.”
It takes ticks 24 hours to crawl to where they typically like hiding. Since they’re so tiny and don’t typically tickle as they move, it’s easy to miss ticks on the body.
“Pay special attention to areas like underarms, behind the ears, around the hairline, inside the belly

button and between legs, as these are common places where ticks may attach,” said Kassandra Foley, regional director of Infection Prevention at St. Joseph’s Health and St. Peter’s Health Partners.
Another tick preventive is providing dogs with monthly prescription parasite medication such as drops or a Simparica Trio pill, which guards against ticks, fleas and heartworm.
“Even with collars and medication, double check them,” said Stephanie E. Waldron, director of environmental health assessment for Onondaga County. “On the bellies a lot of times you could see ticks. Animals seem to bring them indoors quite a bit. Use flea and tick control medication from your vet.”
Check the animal’s fur, especially between the toes and behind the ears, for ticks after time spent outdoors.
Although people tend to think of picking up ticks while hiking off-trail, the encroachment of wild animals near homes can mean simply gardening can expose homeowners to ticks. Foley said that maintaining the landscaping can help reduce this risk. Mow the lawn and trimmed bushes present an area less attractive to wildlife and a lower likelihood that ticks will be present since they prefer to wait on tall grasses for hosts to walk by. Keep wildlife away from the home by minimizing attractants like food, water and shelter. Leaving out pet food and water bowls invites wildlife to help themselves and bring along ticks. Block off any cracks where critters can crawl into outbuildings.
“Ticks thrive in areas with high
grass and dense vegetation, so creating a buffer between wooded areas and places where you and your pets spend time can help reduce the risk,” Foley said. “Consider creating areas of your yard that are less tick-friendly by using gravel, wood chips or cedar chips to create borders around gardens, play areas and patios. These act as barriers to ticks that typically do not like to cross hard, dry surfaces.”
Ticks can hide in moist organic debris such as leaf litter. Remove these regularly.
“Consider treating your yard with acaricides — pesticides designed to kill ticks — before the season starts,” Foley said. “There are both chemical and natural options available. Check with local garden centers or pest control companies for guidance on safe and effective treatments.”
Read the labels to make sure they’re safe for your pets.
Fortunately, Lyme disease is treatable, but prompt treatment is more effective. Foley said that Lyme disease presents with fever, fatigue, headache and a bull’s-eye rash.
“If you find a tick attached to your skin, remove it properly with fine-tipped tweezers, gripping as close to the skin as possible and clean the area with antiseptic,” Foley added. “If you develop any symptoms, contact your healthcare provider immediately for evaluation and potential testing.”
Diane Oldenburg, associate public health educator with Oswego County Health Department, recommends:
“EPA-registered insect repellents and always read the labels,” she said. “If you are using sunscreen, apply sunscreen first then insect repellent second.”
• products with DEET
• picaridin
• IR3535
• oil of lemon eucalyptus (OLE)
• para-menthane-diol (PMD)
• 2-undecanone
In addition, consider “light colored clothing, long sleeves, socks and closed toe shoes and pants tucked into socks,” she said.


By Gwenn Voelckers

remember the morning of Sept. 11, 2001, as if it were yesterday.
I was at work at the time, when we were summoned into the conference room. That’s where my colleagues and I watched TV in uncomprehending horror as the first tower collapsed and then the second.
We sat there together in stunned silence, until several coworkers abruptly stood up and ran to their offices to make phone calls to check on loved ones in New York City.
Moments later, we were dismissed for the day.
Shaken to the core, we gathered our things, slowly dispersed and went our separate ways.
I returned home in the middle of the day to a quiet house. Alone.
I made a few phone calls, but my friends and family had no words. Nor did I. We were all in shock. So, I turned on the TV and clung to the coverage as if it were a life raft. Commentators were trying to make sense of the unthinkable attack. Public figures were asking for prayers and offering reassurance.
It was all I had.
I remember longing for someone to sit beside me, to help me process the enormity of what was happening, to reassure me that we were safe, that life would go on. But there was no one.
That was my first real taste of facing a crisis alone.
And now, more than two decades later, I find myself — like so many others — struggling with those same emotions. Today, the enemy is not foreign terrorists but something that feels even closer to home.
At least half the country is grap-
pling with an overwhelming sense of fear and vulnerability under the current administration in Washington DC.
Democratic norms are being disregarded, trusted experts removed, legal, environmental and consumer protections dismantled. Mass firings and deportations occurring and the stock market is tumbling as I write this.
Most alarming is the strategic shift toward Russia, undermining longstanding alliances and jeopardizing Ukraine’s future.
Once again, I find myself longing for someone by my side during all this chaos, but over the years, I have learned that living alone does not have to mean helplessness.
There are ways to cope, to stay resilient and to find a path forward — even when the world feels like it’s unraveling.
Here are some of the strategies that have helped me and I hope they help you, too.
First and foremost, embrace self-compassion. These are extraordinary times and it is OK to feel overwhelmed. It is OK to take a moment to step back and acknowledge whatever feelings you are experiencing.
Ask yourself:
• Am I treating myself with the same kindness I would offer a friend going through a hard time?
• Am I allowing myself time to rest, recharge, meditate and pray?
• What small comforts can I give myself today — a warm drink, a cat nap, a walk outside or short drive
Panel suggests avoiding flavored and sweetened milk, soda, caffeinated drinks
Got milk? It turns out, plain cow's milk, water and a bit of veggie juice are still the best drink choices for kids and teens.
That's the consensus of experts who recently issued healthy beverage recommendations for kids and teens aged 5 to 18.
The expert panel — convened by Healthy Eating Research, a national program of the Robert Wood Johnson Foundation — included members from the Academy of Nutrition and
in the country? Listening to audio books is my healthy distraction.
How can I create moments of peace within my day, even amid the chaos?
2) Connect with Trusted Friends,
Living alone does not mean being alone. You do not have to endure hard times in isolation. Connection is a lifeline, and it is more important now than ever.
Ask yourself:
• Who are the people in my life that make me feel heard and supported?
• Can I reach out to a friend today, even if it’s just a quick text, email or phone call?
• Are there local or online communities where I can engage in meaningful conversations?
• How can I be a source of support for others, knowing that connection is a two-way street?
While I believe in staying informed, I also recognize the need to protect my sense of well-being. For me, too much exposure can be emotionally draining.
Ask yourself:
• Am I consuming news in a way that informs me or in a way that overwhelms me? More and more, I’ve found that reading the news causes me less anxiety than watching it. I can do without the breaking news banners, sensationalized stories and traumatic imagery.
• Can I set designated times for news updates?
• What are some trusted, balanced sources of information that won’t amplify my anxiety?
Feeling helpless is something I struggle with during challenging times like this, but doing something — no matter how small — can be empowering.
Ask yourself:
• What causes or organizations align with my values, and how can I support them?
• Can I volunteer, donate or advocate in ways that will make an impact?
• How can I channel my frustration into constructive action? Writing this column serves this purpose. And I hope it motivates you and others to get involved.
• What practical steps can I take in my daily life to contribute to the change I wish to see?
5) Pursue Joyful Endeavors
Even in turbulent times, joy is not frivolous — it’s essential. Engaging in activities that bring you happiness can replenish your emotional reserves.
Ask yourself:
• What hobbies or creative pursuits bring me a sense of fulfillment?
• Can I set aside time to read, watch a movie or listen to music without guilt?
• How can I incorporate small moments of beauty into my day — a lit candle, fresh flowers, a beautifully wrapped package, a birdsong, a heartfelt thank you.
• What places or experiences make me feel at peace and how can I seek them out? You’ll often find me at the Lamberton Conservatory in Highland Park.
You Are Not Alone:
The truth is, these strategies can be applied to any crisis, whether it is a political upheaval, a personal loss or a medical emergency.
So, if you are living alone and struggling with uncertainty, know this: There are countless others who share your fears, your frustrations and your hopes for a better future. By reaching out, taking action and caring for yourself, you can ease the burden of solitude and cultivate a renewed sense of purpose and resilience.
Remember — you are not alone. We will find a way forward. And we will do it together.

Gwenn Voelckers is the author of "Alone and Content," a collection of inspiring essays for those who live alone. She welcomes your comments about this column and topic suggestions for future columns at gvoelckers@ rochester.rr.com
Dietetics, the American Academy of Pediatric Dentistry, the American Academy of Pediatrics and the American Heart Association.
Its recommendations follow a five-month review of scientific literature, according to The Washington Post.
Unsurprisingly, the panel said water should be “primary beverage for meeting hydration needs,” with the recommended daily intake ranging from 16 ounces to 88 ounces,
depending on a child's age and sex.
Tap water, the panel wrote, is preferred because it's affordable, eco-friendly and often has fluoride added to prevent tooth decay.
Plain pasteurized milk — preferably low-fat or fat-free — was also recommended for its essential nutrients.
The panel said 100% fruit or vegetable juice is acceptable but should be limited due to its high calorie content.
The panel also said plant-based milks, like almond or oat, lack key nutrients and should only replace dairy if medically necessary.
It said flavored and sweetened milk should be avoided or limited.
Sugar-sweetened beverages, like sodas and sports drinks, “are not recommended as part of a healthy diet for children and adolescents,”

the panel concluded.
Caffeinated drinks, which can disrupt sleep, mental health and heart health, are also not recommended.
“Choosing healthy beverages for children is just as important as choosing healthy foods,” Amy Reed, a pediatric dietitian and the Academy of Nutrition and Dietetics' spokeswoman, said in a news release.

By Jolene Cleaver
contact while being fed lessened and he needed more support to sit up.

Every week, he receives at least 25 hours of applied behavior analysis therapy plus occupational speech and physical therapy and adapted physical education.
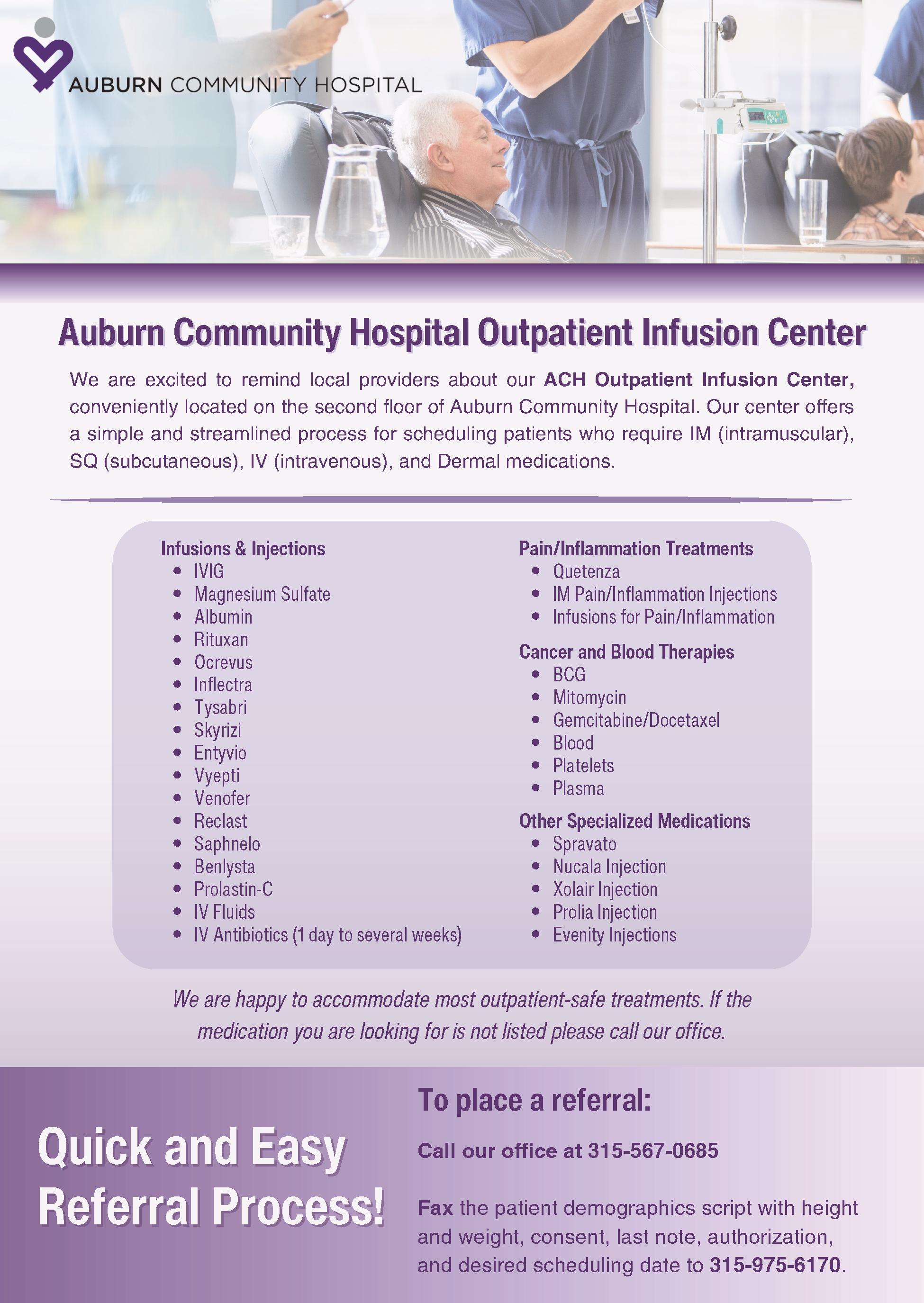
Jennifer and Benjamin Bailey have four children: three daughters and their youngest — a son, 7-year-old Connor.
Though the youngest, he has managed to teach his family the most life lessons.
This is his story.
The Oneida, Madison County, resident was diagnosed at 19 months old with profound autism.
According to a report released in 2023 by the Centers for Disease Control and Prevention (based on data collected from 2000-16), 26.7% of people diagnosed on the autism spectrum have profound autism.
His mom said that from the very beginning, the family was able to jump feet first into the pool to find resources for Connor.
When he was formally diagnosed, the family had a collective, “Oh, this is who he is now,” Jennifer remembered.
In the very beginning, as the family was acclimating, the mother said habilitative services were key in helping her family enter Connor’s world and help him connect with his environment at his pace, instead of the reverse where he would be tasked to constantly try to fit into the world around him.
But the journey to that mental point started several months prior, as questions about his development as an infant began to rise.
“When he was around 9 months old, his babbling stopped,” she said.
Then there were the missed developmental benchmarks — his eye
Along the road to getting diagnosed, doctors briefly thought he might have a hearing deficit. Testing ruled that out. A few months after that, doctors assessed all the data and made the diagnosis.
Then, the real work for the family began.
“We had to figure out a way to make the world ‘less’ so he could engage,” she said. “Today is just so demanding.”
Part of that came in the form of learning that her son had a love of the outdoors. Wind and water being tactile sensory engagements that he craves. So now, splash parks, lakes, beaches, hikes all factor in his world where he can relax and be himself.
She can visibly see Connor’s shoulders relax when watching waves splash on a lake or walking on a path through the woods.
Along the way, the family learned to slow down, To take respite and retreat opportunities. To look at the world around them as a unit.
The current day
“Connor’s never still,” his mother said. “He’s often jumping, moving, stimming.”
The challenge is getting his body to coordinate with what his mind wants to do, she added.
He is non speaking —which is different from being non verbal, she pointed out — and attends Willard Prior Elementary School in a specialized classroom. He can say words with an effort, his mother said. But he largely uses an augmentative and alternative communication (AAC) unit to converse.
Among services, through the New York State Office for People With Developmental Disabilities, he attends respite at the ARC of Madison Cortland’s kids club, attended a week-long camp at ARISE at the Farm in Chittenango last summer and engages in programming through Families FIRST, an organization which provides person-centered support for people living with disabilities.
He also regularly has appointments for neurology, a developmental pediatrician, pulmonary, geneticist, infectious disease, an ear, nose and throat specialist, an optometrist — the list can go on.
The Baileys also work full time. Jennifer is an occupational therapist and Benjamin works remotely for The Hartford.
But the family makes their busy schedule work.
“That’s our non stop lives that we never anticipated. Profound autism has changed everything and it’s certainly been an adjustment. Our Connor was diagnosed at 19 months old and I could name off all his milestones, but what the paperwork won’t say is how he’s changed us from the inside out. We faced questions of faith, justice and what love really meant. Connor has an incredible capacity for joy. He is a sensory seeker and the experiences that bring him joy are so full of light and depths of belly laughter, you can’t help but be moved,” she said.
“It is also heartbreaking to watch him crumble under the weight of a lack of ability to communicate. His ability and intelligence in navigating electronic devices, picking up on vocabulary and even to spell and read are incredible. Functional
communication, daily life skills and sensory regulation are challenges that wreak havoc on his life daily. We watch, pray and support as best we can to help him to grow through it,” she added.
Over the years the family has grown right along with Connor.
“His sisters’ compassion has grown. Their awareness has grown. As a family, we’ve slowed down and take in more. We’re the lucky ones, but you don’t process that unless you slow down,” she said.
She added that her son — who is on permanent disability — will need support for the rest of his life. So, while families need to live in the moment and the day-to-day to help family members with autism achieve goals, there are always long-range plans that need consideration and work, she said.
Her advice to parents of children who receive a diagnosis: “Remember to love your kid where they are at. And it’s the hardships [in life] that help reveal the beauty underneath.
“The thing with autism is you have to expect the unexpected and find those special moments to enjoy.”
Like the splashing of waves. The wind between your fingers. Or the sun on your face. And sharing it together with your family.
The Bailey family will host an autism walk at 10 a.m., April 26. at Higinbotham Park, 116 Broad St. in Oneida. The city of Oneida is co-sponsoring. Get more details here: https://tinyurl.com/2fahfn86
By Deborah Jeanne Sergeant
The COVID-19 pandemic highlighted the need for greater availability of nursing home and assisted and independent living opportunities for older adults.
Too few staff and too few residences mean that this population has few choices when they begin to need more support.
The same is true of people with developmental disabilities as they come of age.
As parents of people with disabilities grow older and die, parental support will not be available. But those who want to and are able to live independently of their families as young adults have few places to go.
Group homes are in short supply as are workers who support them.
Typical setups include a private bedroom and bathroom for each resident with shared living rooms and kitchens. Workers staff the group home 24-7 with the level of assistance needed to help residents with activities of daily living.
The Office for People with Developmental Disabilities in Albany provides certified housing support to more than 35,000 people with developmental disabilities statewide. The

OPWDD invests more than $5 billion annually to maintain and develop more housing options for people with developmental disabilities.
“Frontline staff, such as direct support workers, are critical to helping people with developmental disabilities reach their goals and be active and inclusive members of our communities, as well as ensuring people’s health, safety and wellbeing,” said Jennifer O’Sullivan, director of communications for OPWDD.
Despite these efforts, housing options remain tight for people with disabilities, according to Eric Boye, vice president of mental health services and employment program at Access CNY in Syracuse.
“There is limited space for people with disabilities to find a housing placement,” Boye said. These programs tend to be permanent, so once people get into a housing support program, they’re able to keep it. The challenge is getting placed. The need outweighs capacity.”
Access CNY offers community habilitation programs and individual support services to help people with disabilities access rent support and other services. One of the problems Access CNY encounters is buildings
Attention-deficit/hyperactivity disorder (ADHD) diagnoses have increased among adults in recent years, while remaining stable among teenagers.
ADHD diagnoses among adults increased by 15% between 2020 and 2023, after declining by nearly 11% from 2016 to 2020, researchers reported in a new study published in the journal Psychiatric Research and Clinical Practice.
At the same time, teen ADHD rates remained stable between 2018 and 2023, following a significant 26% decline between 2016 and 2018. These trends “are likely due to a complex interplay of various factors,” said the research team led by physician Erick Messias, chairman of psychiatry and behavioral neurosciences at St. Louis University School
of Medicine, said.
ADHD is more widely known and is less stigmatizing as a diagnosis, researchers said. There’s also increased access to health care services that could lead to diagnosis.
“As knowledge about ADHD symptoms improves among healthcare providers, parents and teachers, more cases may be identified and diagnosed,” researchers wrote.
In addition, an expansion of diagnostic guidelines for ADHD might have contributed to the increase.
For the study, researchers reviewed medical records for more than 144,000 patients with the Sisters of Saint Mary health care system, which has locations in Illinois, Missouri, Oklahoma and Wisconsin.
The study represents one of the largest efforts to investigate new
that were not constructed with accessibility in mind. Many of the more affordable homes are older construction and not accessible.
Although new construction is accessible, it’s less affordable. Boye said that sometimes, neighbors object to the presence of a group home or supported apartment, even though only two to four people would occupy the residence.
“Driving by, you’d never know it was supported living,” Boye said. “Being part of the community helps people have inclusion.”
Dave Devendorf, program director with supported employment programs with Access CNY said that supported living options should be better funded.
“Everyone does their best with the funding available but there’s more funding than people,” he said.
The OPWDD maintains that potential funding increases and other efforts should improve the situation.
“New York has taken aggressive action over the past several years to counteract the workforce shortage being experienced by OPWDD and our provider agencies, as well as most human services organizations across the country, including
enhanced wages and bonuses, professionalization of the workforce and through our #MoreThanWork recruitment campaign,” O’Sullivan said.
The state’s executive budget proposes a 2.1% targeted inflationary increase for all OPWDD providers to further address rising operating costs and cost of care. O’Sullivan said that when added to funding that has been provided since 2022 for cost-of-living increases, rate updates, bonuses, and American Rescue Plan projects, the proposals add up to almost $4 billion invested in the developmental disabilities service system over the last four years.
Training support workers is also a big priority to OPWDD, which has been working with SUNY and National Alliance for Direct Support Professionals to offer credentialing and certification to direct support workers.
These efforts “improve retention among staff and professionalizing the career,” O’Sullivan said. “More than 2,000 DSPs and frontline supervisors having earned their national certification — as well as college credits and stipends — in the last year.”

ADHD diagnoses among teens and adults before, during and after the COVID-19 pandemic, researchers noted.
Adult ADHD can be more difficult to spot, according to the Cleveland Clinic. Symptoms can include forgetfulness, procrastination, chronic restlessness, lack of follow-through and frequently misplacing items.
“Findings from this study support future investigation in identifying potential modifiable risk factors, ensuring sufficient treatment resources, developing targeted interventions, and addressing diagnostic disparities,” the researchers concluded. The findings were published Jan. Thirteenth.

At Hematology-Oncology Associates of CNY, you are never just a diagnosis or a number. We see you...the whole person, with passions, hopes, dreams, histories, and loved ones who share in your journey. From diagnosis, to treatment, to survivorship – our personalized care focuses on truly understanding and planning for your unique needs. We provide genuinely compassionate support, collaborating with you, your family, and caregivers every step of the way. Learn more about HOA today. We’ll see you and care for you – body, mind and spirit.



By Deborah Dittner
Asimple quote I found that says it all — “Love your feet, love yourself.”
If you take care of your feet, you are actually looking after your whole self. Of course, there is more to it than that. However, looking at proper foot health will guide you to improved mobility later in life. Your feet carry you through life from very young in age to very old. Without proper foot care, you may miss out on certain life situations. So…how do you care best for your feet?
• Walking, or better yet, barefoot walking can help you connect with the earth. There are numerous sensory receptors on the bottoms of your feet needing to “feel” the ground and
allowing you to freely move your toes. You can’t always be barefoot so finding proper fitting shoes is essential. There are athletic shoes, dress shoes, work shoes, boots, sandals and more but finding those which suit your feet and any anatomical issues can be challenging. Some may have high arches and others may have flat feet. Bunions also create challenging footwear needs.
The footwear you choose should be comfortable and support the foot’s regular position. Some may need a wide toe box especially if bunions are a concern. A proper fitting shoe will allow your toes to move and not limit the front of the foot.
The amount of cushioning depends on the activity. If you are
By Deborah Jeanne Sergeant
Without any warning, you suddenly experience a sharp pain on the bottom of your foot.
Upon examination, you discover a corn: a small, deep formation of dry skin with a hard center surrounded by swollen skin.
Although a corn is deeper than a callous and more likely to cause pain, friction causes both of them to form.
People should seek help from someone experienced in caring for corns, especially if they are immunocompromised, diabetic or have peripheral neuropathy or peripheral vascular disease, according to Ryan D’Amico, podiatrist and founder and co-owner of Syracuse Podiatry.
“I’ve seen them treat at home and come in with a raging infection,” he said.
Corn removal pads from drugstores typically contain salicylic acid to burn off the dead skin but D’Amico warned that these can go too deep and harm healthy skin along with removing the corn. It’s also likely that the pads won’t entirely remove the corn. A professional such as a podiatrist can remove the corn manually
walking on cement for hours on end, you will want a shoe with increased cushioning and the wide toe box.
• Strength training for your feet. There are many exercises to choose from with numerous benefits such as improving flexibility, balance, reducing discomfort and overall strength. Here are some to consider:
Toe raises — standing on your toes for a few seconds then lower back down (great for strengthening the calves).
Heel raises — opposite of toe raises.
Toe spreads — spreading your toes wide apart, hold a few seconds, then release.
Toe taps — tap your toes individually or all together from forward to side to back (great for balance).
Toe curls — curl your toes under, hold for a few seconds then release. You can also place a towel under your feet and grasping the towel with your toes to gather.
Tree pose (yoga) — stand on one leg with the other foot held at the ankle, the calf or the thigh (never at the knee). Build up the time as your balance and strength increase.
Massage — place a tennis ball under your arch and move the ball around in a circular motion then reverse. No tennis ball? Use your hands to massage the foot. This works out tension, increases circulation and decreases any tightness.
With any type of exercise, begin slowly and increase the repetitions as tolerated. These can be done on a daily basis or at least several times a week. If any pain occurs, stop the exercise and check in with your healthcare provider.
Problem issues can also arise requiring immediate action:
• Blisters — often caused by improperly fitted shoes or shoes that did not supply the necessary support
for the activity. Shoes that support the arches and allow for proper foot alignment will help keep blisters at a minimum.
• Plantar fasciitis — the band of tissue supporting the arch of your foot becomes inflamed causing heel pain and decreased mobility. Stretching prior to and after exercising is important as this may result in discomfort up your legs and as far up as your neck. Follow up with your healthcare provider.
• Bunions — the bony bump at the base of your big toe. It is often said that bunions are caused by tight, narrow fitting and high-heeled shoes. Properly fitted footwear is the best prevention. Using toe spacers may also prevent and relieve the discomfort of bunions.
Most importantly — pay attention to any discomfort your feet may experience.
If your feet hurt at the end of the day or you have developed knee or hip discomfort, consider any changes that have occurred in your footwear.
The sooner these issues are addressed, the better the healthcare of your feet adding improved function and mobility. So before any issues occur, wear proper fitting, wider toe box shoes, use toe spacers, strengthen your feet with exercise and walk barefoot whenever you can. Your feet (and body) will thank you!

Deborah Dittner is a family nurse practitioner and health consultant. Her mission is to transform as many individuals as possible through nutrition and lifestyle changes. www. debdittner.com
without damaging the healthy tissue near the growth.
“Remove the source of the corn,” D’Amico said. “Otherwise, It won’t be affective. You’re spitting in the wind and it will come back.”
He explained that like a callus, a corn is a normal response from the skin to protect against damage to that area that is being compressed. But unlike most calluses, corns can form very painful, pointed structures that poke at the tender skin underneath.
Ill-fitting and worn-out footwear is nearly always to blame for corns. Many people keep wearing shoes as long as the uppers look good but worn soles and overall tight fit can cause corns and other problems. Some wear the same pair of shoes every day. Alternating among a few pairs can help reduce the risk of corns since each pair fits slightly differently.
Replace shoes more frequently and ensure the new ones fit right. Check to see if the shoe slips on the heel and if it is tight against the toes. Good-fitting shoes should feel secure on the heel and allow room for toes to move.

“Go to a place that will fit you like Fleet Feet where they’ll spend some time assessing your feet,” said Douglas Dickson, podiatrist and owner of Oswego-Fulton Foot Care. “A lot of shoe stores don’t sell service. Go to a full-service shoe store. As long as the friction continues, they’ll keep coming back.”
Synthetic materials in socks prevent the feet from breathing and
trap moisture against the skin. That contributes to friction, as do seams. Look for socks with minimal seams.
Because Dickson uses sharp instruments to shave off corns, he advises against their home treatment. It’s easy to go too deep. The sharp tools are tricky to use right and corn pads can cause chemical burns.
“If it keeps coming back, we can do surgery,” Dickson added.
By Anne Palumbo

Basmati rice is my go-to rice, and here’s why: it’s healthier than popular white rice; it boasts a subtle, nutty flavor; and it’s slightly lower in arsenic than most rice.
Let’s begin with why it’s healthier than America’s most-consumed rice.
White rice has a high glycemic index, meaning it can cause rapid blood sugar spikes. These yo-yo spikes, while unhealthy for all, are particularly harmful for those with diabetes or insulin resistance. Basmati rice, on the other hand, especially

whole-grain brown basmati rice, is considered a low-to-medium glycemic index food.
Consuming foods that are lower on the glycemic index is important for many reasons.
It helps regulate blood sugar levels, potentially reducing the risk of developing diabetes (one of the top 10 leading causes of death in the U.S.). It can help with weight control by promoting satiety and reducing the urge to eat during blood-sugar fluctuations. And it may reduce the risk of heart disease, certain cancers
and other chronic conditions, according to trusted studies.
Basmati rice, like most rice, is enriched with certain nutrients to help boost its nutritional value. In particular, basmati boasts decent amounts of iron, B vitamins like folic acid, thiamine and niacin, which together help convert food into energy, and selenium, a powerful antioxidant that helps keep cells healthy.
I always opt for whole-grain brown basmati rice over the refined white version because it’s got more fiber: about 2-3 grams per serving versus less than 1 gram in white. In addition to the obvious benefits of keeping us regular, fiber is your heart’s best friend: it lowers cholesterol; it lowers blood pressure; it helps with weight management; and it improves blood sugar control. Top your basmati with some legumes and vegetables and you’ve created a trifecta of fiber goodness!
In addition to the nutrients listed above, an average 1-cup serving of brown basmati rice has about 200
Serves 6
3 cups cooked basmati rice, cooled
3 tablespoons olive oil
2 leeks, thinly sliced (white and light green parts)
12 ounces asparagus, sliced on the diagonal in one-inch pieces
2 garlic cloves, crushed
2 teaspoons dried basil
Salt and pepper to taste
1 cup shelled edamame, defrosted if frozen
lemon juice and zest
¼ teaspoon red pepper flakes
(optional)
Turns out, Americans may be drinking less coffee, soda and tea, but they're getting more caffeine than ever.
A new study of more than 49,000 U.S. adults found that while fewer are sipping caffeinated drinks, those who do are choosing much stronger doses, with coffee taking the lead.
The result? Caffeine intake is rising, even though the average consumption is still below 400 milligrams of caffeine per day. That's the amount health experts consider safe.
“We are all aware that the
caffeinated beverage market has changed dramatically over the past 10 years, yet no comparable, comprehensive caffeine intake data have been published in recent years," study author Diane Mitchell of the Institute for Advancing Health through Agriculture, Texas A&M AgriLife, said in a news release.
Coffee now accounts for 70% of total caffeine consumption, up 15% from the previous 2010-2011 survey, Mitchell's team reported.
What's more, carbonated soft drinks now contribute only 15% of
½ cup nut of choice, chopped (optional)
1. Prepare rice according to instructions. Let cool. (Can be made a day ahead.)
2. In a large non-stick skillet, heat 2 tablespoons olive oil to medium. Add the sliced leeks and sauté until wilted, about 2 minutes (okay if some get crispy). Next, add asparagus and cook for 5 minutes more, stirring frequently, until the asparagus is
Consider reducing your rice consumption if arsenic levels concern you. According to many studies, big rice eaters (about ½ cup of rice per day) have consistently high arsenic levels, no matter the type of rice. Research has shown that, over time, arsenic can harm your health and potentially increase your risk of certain cancers. To reduce arsenic, some suggest rinsing raw rice before cooking and using a large amount of water to cook rice, which is then drained.
calories, 4g of protein, and 34g of carbohydrates (the complex kind that take more time to break down).

tender-crisp.
Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.
3. Add garlic, basil, salt and pepper and stir for 1 minute more. Gently mix in edamame. Remove from pan and set aside.
4. With heat still on medium, add the remaining tablespoon of olive oil to pan, swirl around, then add rice, pressing down to make a single layer to brown rice. Let the rice cook, undisturbed for 5 minutes. Stir in vegetable mixture and cook until heated up, about 2 minutes more.
5. Serve; sprinkle with some lemon juice and zest; garnish with optional ingredients. Enjoy!
caffeine intake, a 27% decrease from a decade ago.
Tea consumption has also dropped significantly, with 50% fewer tea drinkers overall.

However, the remaining tea drinkers nearly doubled their caffeine intake from tea, suggesting those who stuck with the beverage are, in fact, drinking more. Energy drinks, which were less common a decade ago, now account for 6% of total caffeine intake, as the
number of available brands has jumped from 559 to 970. Despite these shifts, average caffeine intake remains below the federal government's recommended limit of 400 milligrams per day — about two to three 12-ounce cups of coffee.
“With a constantly evolving market of caffeinated beverages and the potential impact it has on beverage consumption patterns, continued monitoring of caffeine intakes is warranted," the authors concluded.
While tonsillitis may be considered a nuisance, it can cause great pain.
Tonsillitis is an inflammation of the tonsils that affects two lymph nodes located on each side of the back of your throat.
A common condition that mostly strikes children, people must understand the impact because patients can experience varying degrees of severity that can impact their daily life and become a serious health issue if left untreated.
It’s essential for individuals experiencing symptoms of tonsillitis to consult a healthcare provider for an accurate diagnosis and treatment plan. Maintaining good oral hygiene and practicing preventive measures, such as handwashing, can help reduce the risk of infections contributing to tonsillitis.
“The estimated cost of just pediatric streptococcal tonsillitis alone in the US is $224–$539 million per year, which includes indirect costs related to parental work losses,” said Melanie Groch, ear, nose and throat physician for Lakeshore ENT, which is part of Oswego Health. “Untreated tonsillitis can lead to complications of a tonsil abscess that may need to be drained surgically.”
Here are five issues with tonsillitis.
The Centers for Disease Control and Prevention doesn’t keep statistics on tonsillitis. However, the most common bacterial cause of tonsillitis is strep throat. It typically occurs in the colder months of autumn and winter, particularly among children between the ages of 5 and 15. Symptoms of tonsillitis include sore throat, difficulty swallowing, red and swollen tonsils, white or yellow coating on the tonsils, fever and even ear pain.

By Ernst Lamothe Jr
In young children who are unable to describe how they feel, signs of tonsillitis manifest in drooling due to difficult or painful swallowing, refusal to eat and unusual fussiness.
“Other complications include the spread of inflammation to the jugular vein in the neck causing a clot, high fever, throat and neck pain, and breathing difficulty,” said Nick Groch, ear, nose and throat physician with Lakeshore ENT — and husband of ENT physician Melanie Grotch. “The inflammation from streptococcal tonsillitis can also spread to the heart causing rheumatic heart disease, long-term kidney damage or autoimmune inflammation of the brain leading to obsessive compulsive disorder or other neuropsychiatric conditions.”
Severe or recurrent tonsillitis can lead to complications, such as abscesses or systemic infections, making it essential to take it seriously. People may consider surgical removal of the tonsils for several reasons. Experts say if you have frequent episodes of tonsillitis, which is more than one per year, it could be time to consider surgery. Those who have sleep apnea or breathing difficulties occasionally connect their condition to enlarged tonsils. Tonsillitis can significantly impact an individual’s quality of life, leading to missed school or work and complications if untreated.
“The most common indications for tonsillectomy are recurrent or chronic tonsil infections, loud snoring with sleep apnea, causing pausing in breathing while asleep that affects the quality of sleep,” said Nick Groch. “We also see bothersome tonsil stones causing throat pain and bad breath. In the United States, more than 530,000 pediatric tonsillectomies are performed annually with



acute or chronic tonsillitis being the third most common reason that kids see an ENT.”
The primary difference becomes recovery time. Children generally recover faster from tonsillectomy than adults. The pain and recovery period may last longer for adults. Adults face higher risks of complications, such as bleeding or infection, after surgery compared to children. Also adults might have different considerations regarding work and responsibilities during recovery compared to children.
“In general, tonsil removal during childhood is better tolerated than when done during adulthood due to increased pain and longer recovery time from surgery,” said Melanie Groch.
Recovery from tonsil surgery typically lasts about seven to 14 days. During this time, patients may experience throat pain, difficulty swallowing and ear pain. It’s essential to follow post-operative care instructions, stay hydrated and con-

sume soft foods. Pain management may also be necessary and follow-up appointments with the healthcare provider are important to monitor healing.
“We generally recommend being off from work or school for one week, a softer diet for two weeks and no exercise, gym class and lifting or straining for two weeks following surgery,” said Melanie Groch.
It’s essential to know that tonsillitis can be caused by more than simply strep throat. While bacterial infections like strep can cause tonsillitis, many viral infections can also lead to the condition. Also not all cases of tonsillitis require surgery and many can be managed with conservative treatment such as rest and medication.
“One common myth related to tonsillitis is that poor oral hygiene or cold weather can lead to infections. Another myth is that your tonsils can grow back following tonsillectomy. The tonsils have a capsule surrounding them and as long as all tonsil tissue including the capsule are removed, your tonsils can not grow back,” said Nick Groch.











By Deborah Jeanne Sergeant
Working as an occupational therapist might seem like the same thing as a physical therapist, but the two careers have important differences.
“OT is similar to PT, but there are different areas you’re working on,” said Jenny Dickinson, director of special children services at Onondaga County Public Health.
Typically, OT focuses on regaining the skills to perform activities of daily living and work (if the patient is employed). But PT is more about helping patients improve their range of motion, regain strength and mobility and lower their pain. OT can also include cognitive function and sensory processing.
After learning about occupational therapy while a freshman in college, Kelly Christensen, now an
occupational therapist for Finger Lakes Health, knew that was the career path for her.
“I love having the opportunity to help people achieve even the smallest milestone,” she said.
At Finger Lakes Health, the organization offers short-term rehabilitation, long-term care and out-patient rehabilitation. In each of those areas, occupational therapists can help patients strategize ways to use their arms and hands to complete activities of daily living, especially those related to self-care.
“We look at what’s needed for that individual to return home,” she said.
In general, occupational health can serve patients from youngsters in early intervention through end-of-life care.
Although physical therapists treat patients of all ages, American Physical Therapy Association states that most physical therapy patients (36.1%) are older than 65. As that cohort of the population increases, it’s clear that the demand for physical therapists isn’t going down anytime soon.
Younger people also need PT.
“We have massive wait lists for children needing PT,” said Jenny Dickinson, director of Special Children Services for Onondaga County Public Health.
She added that the program requires a bachelor’s and then doctorate degree, but doesn’t have a master’s.
“Working in this field with these ages, you really are affecting public health in such a positive way for years and generations,” Dickinson said. “Children who without the intervention wouldn’t be nearly as successful in their later lives.
“There’s a genuine feeling of accomplishment because it’s an altruistic career as you’re in service of young children and their families.”
Falls and other injuries, deconditioning from hospital stays and recovery from surgeries are among
“The profession is great for those looking to help someone,” Christensen said. “There’s a component of teaching too, so we’re often teaching a new way to do a skill. The ability to talk with people is important. And the ability to form relationships. When people are at their worst or lowest is when we’re helping them. Something hard has happened to them. We’re working with them in a vulnerable space. Being able to bond with them is helpful.”
The career requires a master’s level education and doctorate and post-professional doctorate programs are also available.
Julie Kunisch, doctor of occupational therapy, clinical associate professor and chair and program director of the Department of Occupational Therapy at Nazareth University, noted that the Bureau of Labor Statistics foresees that occupational employment is expected to grow “faster than average” and that “U.S. News & World Report named OT number 4 in the best healthcare careers.”
She believes that the aging population represents a key reason for this expansion. People want to remain independent and at home as they age and OT can help. The higher awareness of mental health is also fueling this growth.
“OTs are essential mental health providers and can help people develop coping strategies to engage in meaningful activities,” Kunisch said. “More and more people are living with chronic conditions and disabilities. OTs are experts in promoting independence using adaptive strategies and environmental modifications.”
The healthcare world is also shifting to a prevention and early intervention model. Kunisch views OTs are important for these emphases. As holistic practitioners, they treat the whole person, not just the aspect of their health that hampers their ability
to function independently.
In addition to aiding young children and older adults, OTs also work with people of all ages who have injuries and disabilities. Because medical technology has advanced to allow more people to live, OTs can help rehabilitate patients and foster a greater ability to live independently.
“As these trends continue to evolve, the demand for OTs is expected to keep growing, making it a dynamic and rewarding career,” Kunisch said.
She has been working in the field since 1996 and finds it fulfilling because of “the overall meaningful impact of the work and the personal rewards of the profession. OTs make a direct difference by helping others regain independence, improve their quality of life and achieve their goals which is highly rewarding.”
She also likes that occupational therapy is a dynamic field in which practitioners continuously learn and adapt to new research, techniques and technology.
“This professional growth and opportunities to specialize in different areas like pediatrics, mental health, hand therapy and geriatrics support a fulfilling career,” Kunisch said. “OT is fulfilling work because it allows practitioners to make a profound impact on people’s lives, fosters meaningful relationships, offers variety and professional growth and provides meaningful rewards from seeing tangible improvements in people’s wellbeing and quality of life.”
According to the Bureau of Labor Statistics, the annual mean wage for an occupational therapist in the Syracuse area is $84,030.
the top reasons many older adults need physical therapy.
Maureen Loyal, physical therapist and director of rehabilitation and physical therapy for Finger Lakes Health, has worked as a physical therapy supervisor for 25 years, mentoring young physical therapists and teams.
In addition to treating older patients, physical therapists treat athletes and children with motor delays in schools and “weekend warrior” adults in clinics. They also work in home health, delivering care to people recovering from surgery or injury and in long-term care facilities to help “keep folks functionally mobile and safe,” Loyal said. “Having physical therapy in your house can help keep you mobile there. That’s a great place to work.”
Physical therapists who travel to clients’ homes can better assess their daily living environment for safety and tailor exercise regimens that use familiar items they already own. They can address the particular challenges their homes present, such as front steps, a dimly lit hallway or an uneven floor.
Physical therapists “assess, plan, organize and participate in rehabili-

tative programs that improve mobility, relieve pain, increase strength and improve or correct disabling conditions resulting from disease or injury,” states the Bureau of Labor Statistics.
Loyal felt drawn to the profession of physical therapy as a young athlete. She experienced knee surgery which required subsequent physical therapy. She appreciated the efforts of her physical therapist and felt she also wanted to “help get people back to their life,” Loyal said.
She has always worked in a hospital or acute setting. Many of her patients have had strokes or amputations.
“Getting those folks so they will get over that mentally and physically and get them mobile and home again has been so rewarding,” Loyal said.
“You’re helping people and also you have to challenge your mind to have a successful outcome.”
She likes that physical therapists have direct access so that most insurance companies do not require a referral from a physician and will cover 30 days or 10 visits, whichever comes first.
“Having that autonomy, we should be able to in the future order MRIs,” Loyal said.
According to the Bureau of Labor Statistics, the annual mean wage for a physical therapist in the Syracuse area is $88,990.
By Eva Briggs, MD
Pharmacists are an often-overlooked part of the healthcare team. Many people think that a pharmacist’s job is limited to counting pills or measuring liquids, putting them into bottles and handing them to the patient. But the role of a pharmacist is actually much more involved.
First, what education or training is required? Pharmacy school is four years long and leads to a Pharm. D. degree. The prerequisite to entering pharmacy school is generally a minimum of two years of college courses, although many students complete three years or finish a fouryear undergraduate college degree. Prerequisite courses include anatomy, physiology, biology, chemistry, biochemistry, microbiology, physics,
$43,610 for non residents. And that does not include room and board or other living expenses or the cost of the undergraduate education.
The average student graduates with about $171,000 of debt (that is a January 2024 figure so it’s probably more now.)
There are also programs leading to Master of Science and Ph.D. degrees in pharmaceutical science.
Once a student starts pharmacy school, they will complete a rigorous academic program with courses in pharmacology, pharmacokinetics, pathophysiology, genetics, microbiology, immunology, delivery of care, professional communication and pharmaceutical calculations. There are also courses related to pharmacotherapy for specific organ systems:
tinuing education course. In New York state a minimum of 45 contact hours (at least 23 live) is required in each three-year registration period. This includes at least three credits of formal continuing education on strategies and techniques to reduce medication and prescription errors and at least three credits of formal continuing education pertaining to pharmaceutical compounding.
Most people are aware of pharmacists that work at retail pharmacies. But pharmacists also work in hospitals, helping clinicians choose the correct medications, helping calculate the correct dose and monitoring for drug interactions. Some pharmacists work in specialized hospital units and clinics, such as oncology (cancer care) and mental health.
Poison control centers employ pharmacists. Some work in veterinary medicine. Other facilities that employ pharmacists include rehabilitation centers, long-term care facilities, nursing homes and hospice. There are also pharmacists who teach and others involved in research.
So please remember to be kind to your pharmacist. They are highly trained and collaborate with physicians, nurses and other health care professionals.
SIMEON DEWITT
150 E. 1st St. Oswego, NY 13126 315-343-0440
TOWPATH TOWERS
100 Rochester St. Fulton, NY 13069 315-598-4700
4920 N. Jefferson St. Pulaski, NY 13142 315-298-6101

The following services are included in your rent
• Trash Collection • Free Wi-Fi
• Bus for shopping/groceries
• Heat, Electricity & Hot Water
• Snow Removal & Lawn Care
• Planned Activities
• All repairs & maintenance Applications are now being accepted! 62+ No smoking!
Preference given for veterans & spouses of veterans.
Endocrinology, including diabetes testing, care and education
• Sleep lab and sleep disorder treatment
• Clinical Programs (Chronic Intensive, Transitional, and Palliative Care Management)
• Among many others!
All provided in one of over two dozen comfortable, conveniently-located, and family-friendly offices across CNY! Call 315.802.5178 or visit fcmg.org today!

Upstate's revitalized and growing heart services provide benefits to you.
From six cardiology outpatient sites to the arrival of our new heart surgeons, and more doctors and advanced providers for procedures such as caths and TAVRs, we are here to work with you. Learn more about what The Upstate Advantage can do for you.



By Jim Miller
Dear Savvy Senior,
What are the risk factors for kidney disease? My mother died from kidney failure a few years ago at age 75 but didn’t even know she had a problem until it was too late.
Inquiring Daughter
Dear Inquiring,
Anyone who has diabetes, high blood pressure, heart problems or has a family history of the disease is at increased risk for chronic kidney disease, a condition in which the kidneys can no longer effectively filter your blood.
According to the Centers for Disease Control and Prevention, around 37 million U.S adults have chronic kidney disease, and millions more are at risk of developing it, yet most people don’t realize it.
That’s because kidney disease develops very slowly over many years before any symptoms arise. But left untreated, the disease can eventually require people to spend hours hooked up to a dialysis machine or get a kidney transplant. Even mild kidney problems can double a person’s risk of heart attack and stroke, as well as cause anemia and bone disease.
The reason kidney disease has become so widespread today is because of the rise of obesity, Type 2 diabetes and high blood pressure which all strain the kidneys.
Another factor is the increasing number of people who take multiple medications, which can overtax the organs. People over age 60 are especially vulnerable both because they tend to take more drugs, and because kidney function normally declines somewhat with age.
Because kidney disease is often symptomless, it’s usually undiagnosed. The only way to catch it before it advances is to have a routine blood and urine test by your doctor. So, anyone that has diabetes, high blood pressure or heart disease, or is age 60 or older needs to be tested annually.
If your lab tests show a decline in kidney function for more than three months in a row, you might be diagnosed with kidney disease and referred to a nephrologist. You also need to know that while kidney damage cannot be reversed, there are a number of effective lifestyle steps and treatments that can help contain the damage, including:
• Control your blood pressure: If you have high blood pressure, get it under 130/80. If you need medication to do it, ACE inhibitors and

ARBs are good choices because of their proven ability to protect the kidneys.
• Control your diabetes: If you have diabetes, keep your blood sugar as close to normal as possible. Diabetes medications called SGLT-2 inhibitors have also shown to be effective in helping slow the progression of kidney disease, even in non diabetic patients.
• Adjust your diet: This usually means reducing the amount of protein and phosphorus you eat and cutting back on sodium, sugar and possibly potassium. Your doctor can help you determine an appropriate eating plan, or you may want to talk to a dietitian.
• Watch your meds: Dozens of commonly used drugs can damage the kidneys, especially when taken in high doses over long periods — most notably NSAIDs like ibuprofen and naproxen. Proton pump inhibitor (PPI) medications taken for heartburn and GERDS, and herbal supplements can also be problematic. Talk to your doctor about all the prescription, over-the-counter and herbal products you take to identify potential problems and find alternatives.
• Exercise and lose weight: If you’re overweight and inactive, start an aerobic fitness routine (walk, swim, cycle, etc.) that gets your heart pumping. This will help lower blood pressure, control diabetes and help you lose excess weight all of which will help your kidneys.
• Stay hydrated: Dehydration can affect kidney function, so try to drink at least six to eight 8-ounce glasses of water per day.
• Quit smoking: If you smoke, quit. Smoking damages the kidneys and doubles the rate of progression to end-stage renal failure.

Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.
Local News Inc. is hiring a driver to distribute copies of In Good Health newspaper in the Oswego-Pulaski area. It’s not a regular job. Once or twice a month. No heavy lifting. The job consists of getting the monthly publication in Oswego and distribute it to various locations. The job needs be performed during the day, roughly from 9 to 5 from Monday through Wednesday. $15.50/hr plus .30 cents per mile. It amounts to about $200 per job. Great for active retirees and for stay-at-home moms.

Please call (315) 751-2320 and ask for Mr. Dotto.
Do you qualify for
Do you have enough $$$ set aside for your funeral?


www.ballardassoc.com




By Warren Beck Social Security District Manager in Syracuse.
ou may be able to get Supplemental Security Income (SSI) even if you already receive Social Security benefits.
About 2.5 million adults and children get SSI and Social Security at
We pay Social Security benefits to workers and their eligible family members based on the worker’s earnings. SSI is a needs-based program that provides payments to people with little or no income and

Gary Lewis, the son of legendary comedian Jerry Lewis, talks to
‘My dad was
he says.
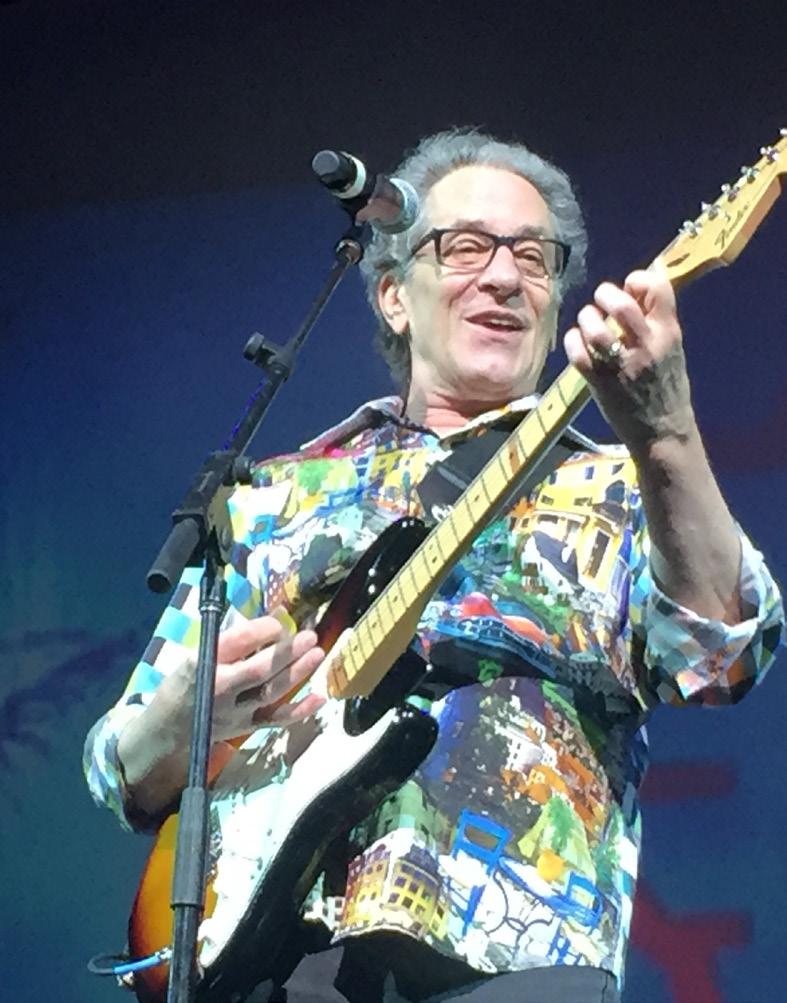
People younger than 65 must be blind or have a disability and meet SSI income and resource limits, while people 65 and older do not have to have a disability. About 1.4 million people 65 and older receive both SSI and Social Security.
What do we mean by “little or no income”?
In 2025, you may be eligible for SSI if your total income — including your Social Security benefit — is less than $987 per month (the 2025 SSI monthly federal benefit rate plus
We consider income from all non-work sources, including pen-
Q.: What is the estimated average Social Security payment that a person receives each month?
A.: The estimated average monthly Social Security benefit for a retired worker in 2025 is $1,976.00. The average monthly Social Security benefit for a worker with a disability in 2025 is $1,580.00.
Q.: Why should I sign up for a personal My Social Security online account?
A. My Social Security is a personal online account you can securely use to check your Social Security information and do business with us. With a personal my Social Security account you can:
• Keep track of your earnings and verify them every year.
• Get an estimate of your future benefits if you are still working.
• Request a replacement Social Security card in most states.
• Get a letter with proof of your benefits if you currently receive them.
sions, veterans’ benefits, unemployment and Social Security disability, retirement and survivor benefits. We also count some — but not all — earnings from work, including self-employment.
What do we mean by “few resources”?
Resources are things that you own that you could change to cash and use to support yourself. They include vehicles (if you own more than one) and money in bank accounts, stocks and bonds. We do not count your home and the land it’s on, as long as you live there. To be eligible for SSI, your resources cannot be worth more than:
– $2,000 for a single person.
– $3,000 for a married couple living together.
For more information visit our blog article, You May Be Eligible for SSI and Social "Security Benefits" at blog.ssa.gov/you-may-be-eligible-for-ssi-and-social-security-benefits.
Please share this information with others who may benefit – and post it on social media.
• Manage your benefits:
– Change your address or telephone number. (Social Security beneficiaries only)
– Start or change your direct deposit. (Social Security beneficiaries only)
– Get a replacement Medicare card.
– Get a replacement SSA-1099 or SSA-1042S for tax season.
To find all the services available and set up an account, go to www. ssa.gov/myaccount.
Q.: I plan to retire soon. When are Social Security benefits paid?
Social Security benefits are paid each month. Generally, new retirees receive their benefits on either the 2nd, 3rd, or 4th Wednesday of each month, depending on the day in the month the retiree was born. If you receive benefits as a spouse, your benefit payment date will be determined by your spouse’s birth date. Here’s a chart showing how your monthly payment date is determined:
Karen Callahan has been ap

pointed chief clinical officer at Hematology-Oncology Associates of CNY overseeing all nursing, research, radiation and administrative teams across HOA’s three centers: East Syracuse, Auburn and Camillus. Since 2022 Callahan served as HOA’s director of research operations.
With Master of Science and Bachelor of Science degrees in nursing from Keuka College, Callahan has spent her entire nursing career providing and directing care for patients with cancer and blood disorders. Some of her accomplishments include serving as a preceptor to SUNY Morrisville and Utica University nursing programs, as a board member for Premier Oncology Hematology Management Society and as a member of the American Organization of Nursing Leadership.
“With Karen’s extensive experience and commitment to advancing
patient care, she will be instrumental in shaping the future of our clinical operations,” says HOA Chief Executive Officer Jennifer Pichoske. “Her leadership will further strengthen our mission to provide the highest quality, personalized cancer care each patient deserves, close to home.”
Two physicians have joined Crouse Medical Practice – Cardiology. They are:
• Pratap Arasu — he specializes in cardiovascular disease. He obtained his medical degree from Maulana Azad College in New Delhi, India. He completed his residency and fellowship in cardiovascular at SUNY Upstate Medical University. He also completed a fellowship in interventional cardiology at Strong Memorial Hospital in Rochester.
• Avneet Singh — he received a Master in Health Administration degree from Cornell University and obtained his medical degree from Maulana Azad College in New Delhi, India. He completed his residency and fellowship at SUNY Upstate Medical University.
Both providers are currently welcoming new patients.
CMP offers primary care and specialty care in 19 locations through-
Two new cancer doctors with expertise in melanoma and bone cancer and stem cell transplantation have join Upstate Cancer Center
Jade Homsi will serve as division chief of hematology and oncology and associate director of adult hematology-oncology at the Upstate Cancer Center as well as an associate professor of medicine.
Zheng Zhou has been named the director of stem cell transplantation and cellular therapy program as well as an assistant professor of medicine.
“The addition of these new physicians to the Upstate Cancer Center strengthens and enhances our ability to treat cancers like melanoma and sarcoma and leukemia,” said Cancer Center Interim Director Thomas Vandermeer. “It also broadens our range of treatments, including stem cell transplantation and cellular therapies, while introducing cutting-edge options such as CAR T-cell therapy. Their addition to our cancer-fighting team speaks highly of our center’s reputation in bringing the best practitioners to Central New York.”
Before joining Upstate, Homsi was an associate professor of internal medicine and the clinical chief of the hematology and oncology at the University of Texas Southwestern Medical Center in Dallas. He was the leader of the melanoma and
out Central New York. In addition to primary care, clinical services offered through CMP include general surgery; cardiology; OB-GYN; endocrinology; pulmonology; neurosurgery; neurovascular; diabetes care; stroke care; bariatric; maternal fetal medicine; plastic surgery.
Physician Tarek Sousou, He

matology-Oncology Associates of CNY board president, is the newest member of the board of directors for the Community Oncology Alliance (COA), a national nonprofit dedicated solely to advocating for independent community oncology practices and the patients they serve.
“We’re thrilled to have Dr. Sousou support COA’s mission with his unique expertise. He brings extensive experience and a passion for providing a caring environment for patients battling cancer,” said COA President Debra Patt, a practicing breast cancer
specialist in Austin, Texas, and executive vice president at Texas Oncology. “All members of COA’s board of directors come together under the shared mission of ensuring that patients have access to high-quality, affordable, cutting-edge cancer care close to where they live and work.”
A practicing medical oncologist, Sousou joins the COA board for a three-year term effective immediately. He fills the board vacancy created by Jennifer Pichoske, who stepped down from her position to serve on the COA Administrators’ Network (CAN) board as part of her new position as chief executive officer of Hematology-Oncology Associates of CNY.
COA is a nonprofit controlled by independent community oncologists and is dedicated to advocating for community oncology practices and, most importantly, the patients they serve. The officers, committees and board members of COA further its mission to protect and foster the community oncology delivery system in the United States through public policy, advocacy, and education.
HOA is a private community cancer center established in 1982 with a mission to provide the highest level of quality care in a healing environment for the body, mind and spirit of patients dealing with cancer and blood disorders. A member of the Community Oncology Alliance, HOA has offices in Auburn, Camillus and East Syracuse.
sarcoma disease-oriented team at University of Texas Southwestern’s Harold C. Simmons Comprehensive Cancer Center, an NCI-designated comprehensive cancer center. Prior to that, he was an assistant professor of cancer medicine at the University of Texas MD Anderson Cancer Center in Houston and the center affiliate in Arizona.
Homsi earned his medical degree in 1995 from Damascus University in Syria. He completed a clinical research fellowship in medical oncology-palliative medicine at the Cleveland Clinic in 2001, completed an internal medicine residency at Mercy Hospital in St Louis (2004) and a fellowship in hematology and oncology at the Moffitt Cancer Center/University of South Florida in Tampa (2007).
He is dedicated to patient-centered care using evidence-based medicine and novel therapies. Homsi specializes in treating patients with melanoma, advanced skin cancer and soft tissue and bone sarcomas. He is active in research related to melanoma and sarcoma with a focus on immunotherapy and early phase clinical trials. He has authored or co-authored more than 50 articles based on his research and won several awards for his work from the National Institute of Health and the American Society of Clinical Oncology.
Zhou graduated from medical


school at Shanghai Medical University in 1997 and received his internal medicine residency training at the University of Massachusetts Medical School. He earned his PhD in 2005 from McGill University. He then completed a fellowship in hematology and medical oncology at Northwestern University Feinberg School of Medicine in 2014.
Before coming to Upstate, he served as assistant professor of medicine at Tufts School of Medicine and associate director of the stem cell transplant and cellular therapy program at Tufts Medical Center
in Boston.
His clinical and academic interests are in hematological cancers utilizing transplantation and cellular therapy approaches. He has served as a principal investigator on multiple clinical trials and has authored more than 20 peer-reviewed publications in such journals as Blood, Blood Advances, Journal of NCCN, Leukemia and Lymphoma. He is an active member of several national professional societies and an inspector for the Foundation for the Accreditation of Cellular Therapy (FACT).
Physician Scott P. Albert has been

P. Albert named director of the breast program at Upstate Medical University. He also serves as assistant professor of medicine. Albert previously served at Upstate from 2013 to 2017 and held numerous roles, including as chief of the division of breast endocrine and plastic surgery and breast program leader. He also served as associate program director for the surgery residency program. He most recently served as a surgeon at St. Joseph’s Health Hospital.
Albert is board-certified in complex general surgical oncology, which is granted to surgeons who have completed advanced training and demonstrated expertise in the field of surgical oncology, specifically focusing on patients needing complex cancer surgeries or with rare or unusual cancers.
Albert has lectured and written on topics such as breast cancer, melanoma, thyroid diseases and has been published in numerous publications, such as Critical Care Medicine, Annals of Surgical Oncology and the Journal of Surgical Research, among others.
Albert earned his medical degree from Upstate Medical University in 2000. He was a general surgery resident and surgical research fellow at Upstate, before holding a surgical oncology fellowship at Ohio State University.
His honors include the Humanitarian Award from the Carol Baldwin Breast Cancer Research Fund.
Oswego Health has appointed

Bryan Jenkins as the new director of Springside, an independent senior living community in Oswego. Jenkins is no stranger to Oswego Health, having previously served as the director of social services at The Manor at Seneca Hill from 2022 to 2023.
Most recently, he served as a certified ombudsman for the New York state ombudsman program, advocating for over 1,000 residents in long-term care facilities across Oswego and Cayuga counties.
Before his role at The Manor, Jenkins held leadership positions with Morningstar and the state of Montana. As director of social services at Morningstar from 2019 to 2022,
Jenkins oversaw the implementation of essential programs for residents. His work as a career development specialist for the office of public assistance in Montana helped streamline training programs, reducing turnover and improving employee performance across the state.
Jenkins holds a Bachelor of Science in marketing management from Juniata College and an MBA from Robert Morris University.
As director of Springside, Jenkins will oversee the daily operations of the independent senior living community, managing all departments and ensuring that Springside continues to provide the highest standard of care and service to its residents.
Oswego Health Medical Practice,

a leading multi-specialty healthcare provider in Central New York, announced the addition of Raman Dhawan, a board-certified orthopedic and spine surgeon, to its orthopedic team. Dhawan brings over 18 years of experience in orthopedic surgery. After completing his orthopedic residency at Upstate Medical University from 1999 to 2004, Dhawan pursued a spine fellowship at University of California San Diego (2004-2005), where he honed his expertise in advanced spine care.
Prior to joining Oswego Health Medical Practice, Dhawan practiced at Crouse Hospital, where he served from 2007 until recently. Additionally, he has worked at Geneva General Hospital since 2008 and Community Memorial Hospital from 2005 to 2007.
“We are thrilled to welcome Dr. Dhawan to our team,” Oswego Health Medical Practice President Wajeeh Sana. “His extensive experience and dedication to providing personalized, world-class orthopedic care are a great addition to our practice. Dr. Dhawan shares our commitment to improving the health and well-being of our community, and we are excited to see the positive impact he will make.”
St. Joseph’s Health recently

announce the appointment of Julie Moore as its new chief nursing officer. Moore brings a distinguished career in nursing leadership, patient care excellence and healthcare operations to her new role, where
she will oversee the strategic direction of nursing services across the St. Joseph’s Health system.
With more than 15 years of progressive leadership experience, Moore is renowned for fostering a culture of safety, innovation and compassionate patient care. Her expertise spans critical care, emergency services, surgical services, infection prevention, and patient safety.
Most recently, she served as vice president of patient care services at JPS Health Network in Fort Worth, Texas, where she oversaw 3,500 colleagues, led transformative initiatives that enhanced patient outcomes, significantly reduced emergency department wait times, and improved operational efficiency.
“Julie is an exceptional leader whose track record demonstrates her dedication to quality care and staff engagement,” said Meredith Price, senior vice president of acute care at St. Joseph’s Health. “Her passion for innovation and team collaboration aligns perfectly with our mission to deliver world-class care to the communities we serve.”
Moore earned her Doctor of Nursing Practice in executive leadership from Baylor University, her MBA in healthcare management from Western Governors University, and her Bachelor of Science in nursing from the same institution. She holds certifications as a nurse executive advanced-board certified (NEA-BC) and a critical care registered nurse (CCRN).
In addition to her professional achievements, Moore has a strong commitment to community service, volunteering for initiatives such as feeding the homeless, supporting animal care organizations, and mentoring future nursing leaders.
Outside of work, she enjoys rescuing and fostering animals, reading, traveling, and most of all, spoiling her grandchildren.
St. Joseph’s Health recently

welcomed physician Megan Matott back to the hospital, where she will practice palliative medicine. Matott received her Bachelor of Science in biology from Nazareth College in Rochester, where she graduated summa cum laude. She earned her Doctor of Osteopathic Medicine from West Virginia School of Osteopathic Medicine and completed her family medicine residency training at St. Joseph’s Health Hospital.
She worked in primary care for two years, prior to completing her fellowship training in hospice and palliative medicine at Rochester General Hospital.
Matott is particularly interested in symptom management at the end of life and providing supportive en-
vironments for patients and families during these transitional periods.
“I feel a true calling to care for those with serious illnesses. I am honored and humbled every day to help improve quality of life for this population,” said Matott. “I am thrilled to be able to continue my career in a place where I already feel at home with an incredible team of colleagues.”
In her spare time, Matott as a self-proclaimed “health nut,” an athlete, lifter, dancer, cyclist, roller skater and low-carb diet enthusiast. She also runs a small custom cake business in her spare time. She loves all things outdoorsy, home renovations, DIY projects and reading an abundance of fiction novels.
Physician Jonathan Ramalho

Jonathan Ramalho recently joined St. Joseph’s Health Cardiovascular Institute. He is board-certified in internal medicine and cardiovascular disease. He practices electrophysiology. Ramalho received his Bachelor of Science in biology from Loyola University and graduated cum laude.
He was a Division I tennis athlete and selected to the Metro Atlantic Athletic Conference All-Academic Team.
He earned his medical degree from Ross University School of Medicine where he graduated with honors and completed his internal medicine residency and cardiovascular disease fellowship at SUNY Downstate Medical Center in New York City. He went on to complete a clinical cardiac electrophysiology fellowship at Westchester Medical Center.
“I am beyond thrilled to be joining the highly skilled medical team at St. Joseph’s Cardiovascular Institute,” said Ramalho. “The advancements in cardiovascular disease treatment, including novel ablative therapies in electrophysiology, make it an exciting time to be practicing.”
Ramalho is a member of the American College of Cardiology (ACC) and Heart Rhythm Society (HRS). He has been part of multiple research projects and written several publications, including some unique case reports on supraventricular tachycardia.
Ramalho is from Westfield, New Jersey, where his family still resides. Outside of work, Ramalho enjoys working out, cooking and trying new restaurants.
Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMEN OUP
Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMENT GROUP










Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMENT GROUP






Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities?
Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today


CONTACT:
CONTACT:
Peg Reith BSN, RN
Peg Reith BSN, RN
Phone: 315-529-3267
Phone: 315-529-3267
CONTACT:
Email: CNA_Training@elementalmgt.com
Email: CNA_Training@elementalmgt.com
Peg Reith BSN, RN
Phone: 315-529-3267
Email: CNA_Training@elementalmgt.com

















Say hello to a convenient way to stay healthy in Oswego County. ConnnextCare offers a comprehensive set of services - family and internal medicine, pediatrics, dentistry, psychiatry, substance use disorder treatment and social work all under one medical group. Patients within our network can visit any of our seven locations at any time.
ConnextCare also offers medical, dental and mental health services at nine School Based Health Centers in five Oswego County school districts.
WALK-IN APPOINTMENTS NOW AVAILABLE IN THE PULASKI ACUTE CARE SUITE
MONDAY - FRIDAY 7:00AM - 6:00PM
ACCEPTING NEW PATIENTS AT ALL SCHOOL BASED HEALTH CENTERS! SCAN THE QR CODE FOR ENROLLMENT FORMS!
Central Square (315) 675-9200 Fulton (315) 598-4790 Oswego (315) 342-0880 Pulaski (315) 298-6564 Parish (315) 625-4388 Phoenix (315) 695-4700 Mexico (315) 963-4133