






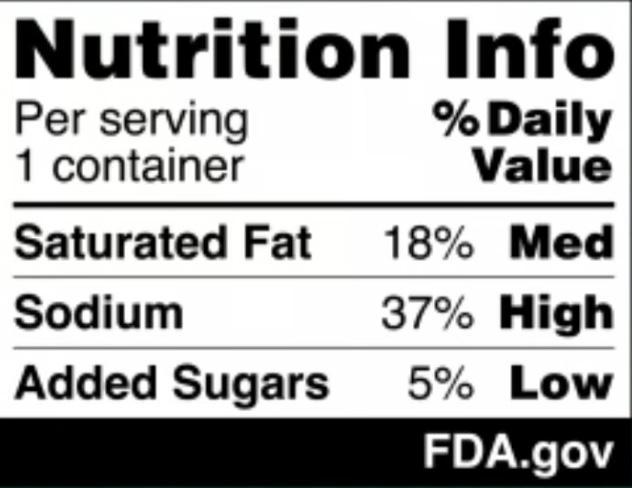
The U.S. Food and Drug Administration (FDA) has proposed a new rule requiring bold, easyto-read nutrition labels on the front of food and beverage packages.
These labels, which would highlight content of sugar, salt and saturated fat, aim to make it easier for shoppers to make healthier choices in the grocery aisle — helping to tackle the rising rates of obesity and conditions such as Type 2 diabetes, heart disease and high blood pressure, a media report from The New York Times states.
These chronic illnesses affect over 60% of American adults and contribute to an estimated $4.5 trillion in annual health care costs, according to the FDA.
“Nearly everyone knows or cares for someone with a chronic disease that is due, in part, to the food we eat,” physician Robert Califf, the commissioner of the FDA, said in a statement released by the administration. “It is time we make it easier for consumers to glance, grab and go.”
The black-and-white labels would appear on the front of products, unlike the current back-of-package Nutrition Facts panel, which lists dietary facts such as calorie counts, serving sizes and ingredients.
The new proposal is the result of three years of research by FDA scientists, who studied similar frontof-package labeling systems used in
Focus group testing of 10,000 people found that the proposed labels were easier to understand and effective at conveying nutrition information, according to the FDA. If the labels are finalized, food manufacturers would have up to four years to comply.
countries like Canada, the United Kingdom and Chile.
Focus group testing of 10,000 people found that these proposed labels were easier to understand and effective at conveying nutrition information, the FDA said.
If the labels are finalized, food manufacturers would have up to four years to comply.
The proposed rule has drawn praise and criticism.
“This proposal is a real step forward in our efforts to better inform
consumers, although we wish the administration had selected a nutrition warning format which is more likely to favorably affect purchasing decisions,” Peter Lurie, executive director of the Center for Science in the Public Interest, an advocacy group that first petitioned the FDA to require frontof-package labels in 2006, told The Times.
The food industry, however, pushed back. Sarah Gallo of the Consumer Brands Association said the labels lack important details, such as calorie counts and the presence of nutrients essential for a healthy diet.
Senator Bernie Sanders also criticized the plan, calling it “pathetically
weak” to address the real dangers of ultra-processed foods, which make up a majority of calories consumed by Americans regularly.
Some experts believe the frontof-package labels could encourage food companies to reformulate products to avoid “high” levels of sugar, salt or fat.
“If you're a retailer selling something that's just above the threshold, you have a lot of incentive to take a little bit of sugar out of your breakfast cereal so it doesn't bear the high label,” Anna Grummon, the director of the Stanford Food Policy Lab, told The Times. “That's a win for consumers.”


Don’t wait to get the care you need. When you visit the St. Joseph’s Health Cardiovascular Institute, you can expect the best. They’re rated high-performing in more heart procedures than all other area hospitals.* You’ll be back home and feeling better in no time.
*U.S. News & World Report



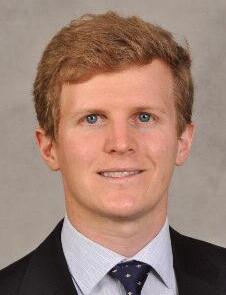
By Chris Motola
M.D.
New chief medical officer at Liberty Resources wants to build a larger medical team to serve the community. ‘We’re trying to build out a multidisciplinary model so the patient can get all of their routine care in one place,’ he says
Q: You are the new chief medical officer at Liberty Resources.
A: That is correct, as of Nov. 25. I recently started, so I’m getting to know Liberty right now. I came here from another position at FCHC [First Choice Health Centers] over in Connecticut. It’s a federally qualified health center with a lot of service lines. We took care of around 18,000 to 20,000 patients with diverse issues, facing a lot of challenges. It was a great experience. And then I moved over here to the Syracuse area for this great opportunity with Liberty Resources. So now I’m here.
Q: Liberty Resources has a heavy social services aspect to it. How does that factor into your role as CMO?
ing myself. So we’re able to provide more services, including pediatric services. I oversee the primary care side. I also oversee GYN services. It’s good. It’s exciting. We’re bringing on new staff, new nurses.
Q: Coming from another human services-oriented provider from another state, what are some of the differences in approaches between Liberty Resources in Syracuse and FCHC in East Hartford?
the same challenges when we’re screening patients for social determinants of health. Here everything’s integrated. We can screen from both sides. If I need to find a therapist for the patient I can just walk down the hallway to get a better idea of what’s going. On the primary care side, if a patient’s mental health isn’t being taken care of, I’m going to have a lot harder time fixing the physical side. And that’s goes both ways. If their diabetes is out of control, it’s going to affect their mental health. There are a lot of areas where we can collaborate. So we’re trying to build out that multidisciplinary model so the patient can get all of their routine care in one place.
Q: What’s your approach to building this model?
A: A lot of teamwork. A lot of networking. A lot of networking and teamwork and a lot of hard work. One thing I noticed with Liberty and a reason why I chose Liberty, is that there are a lot of great people who are innovative and want to make a difference. We do a lot of workshops, a lot of work groups. We target specific populations and work from there. Sometimes it’s trial and error, but it’s also assessing needs and matching services to needs for the population.
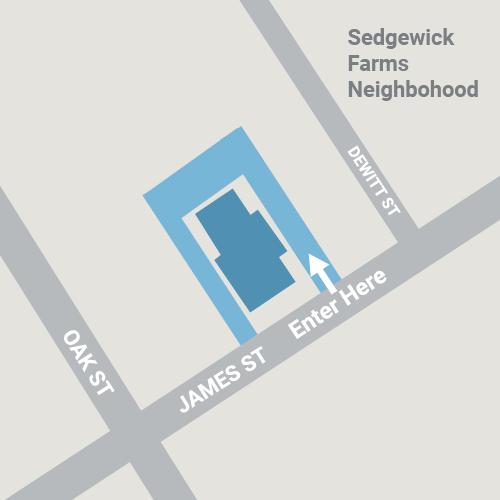
SIMEON DEWITT
150 E. 1st St. Oswego, NY 13126 315-343-0440
TOWPATH TOWERS
100 Rochester St. Fulton, NY 13069 315-598-4700
SPRINGBROOK APARTMENTS
4920 N. Jefferson St. Pulaski, NY 13142 315-298-6101
A: With the patient population that we see and Liberty’s crisis services and home-based services, we have a lot of home-based services. They’re a great network with great resources that we can utilize. The primary care arm that we’re trying to build out now will hopefully integrate and be able to utilize those services. A lot of the patients that we get have a lot of health issues. We take care of a lot of patients who are homeless, who have financial issues. So we have to bridge those barriers while taking care of their physical and mental health issues. It’s the challenge we’re trying to figure out. I think a lot of the resources that Liberty has are very well-positioned to take care of these patients in a more integrated manner, addressing gaps in care, reduc ing hospitalizations and getting quality outcomes.
cifically overseeing primary care?
seeing primary care. We’re just grow ing, so we just added on some new physicians — includ
A: So I can definitely say there are differences, but there are a lot of similarities, too. Hartford is a very urban setting. A lot of patients have issues with social determinants of health. There’s a lot of homelessness. That’s very similar to what we see here. But here, because of what Liberty Resources is known for, we see a lot more issues with patients with mental health issues that require mental health services. That’s the main difference. We also have some demographic differences. Syracuse has a large Nepalese demographic here that isn’t in Connecticut. I’m still getting to know the Syracuse area myself. There are differences in networking too. We have a lot of streamlined services with St. Joe’s as well as the ability to do a lot of things in-house.

Q: Mental health does get touched on by primary care, but it’s usually not a major focus. How does Liberty Resources go about integrated the two?
A: With a vast amount of resources. We have case managers. We have crisis coordinators. There are a lot of people here that we use to try to close our gaps in care. It’s been great to be able to use these resources for primary care. We have a lot of
Q: What got you interested in healthcare administration?
A: When I was first starting out I didn’t really know which area of medicine I wanted to go into. I wanted to do a little bit of everything. As an attending physician I came to see what patients were going through and became more interested in the system of health itself. How things work. How we deliver healthcare to patients. What we can do to keep patients out of the hospital. I went back for my healthcare-focused MBA over at Yale. It gave me an idea of how to do sustainable care delivery models. There’s a lot of innovation you can do. It’s a lot of fun.
Name: Sandeep Bhashyam, M.D.
Position: Chief medical officer at Liberty Resources
Education: Jacobs School of Medicine and Biomedical Sciences at University at Buffalo (2009); Yale University, executive Master of Business Administration, 2016; The American Board of Internal Medicine, board-certified in internal medicine; SUNY Stony Brook School of Medicine, residency in internal medicine, 2012; Rensselaer Polytechnic Institute, Bachelor of Science (BS) in biology and chemistry, 2004 (dean’s list)
Career: Chief medical officer, First Choice Health Centers, E. Hartford, Connecticut; associate medical director, Primary PartnerCare ACO, Great Neck; founder, We Excel Tech LLC, New York; chief medical officer; Conduet MED, New Haven, Connecticut
Hometown: Yonkers
Organizations: American Board of Internal Medicine, American Medical Association
Family: Wife, two sons
Hobbies: Basketball, tennis, movies





For many, coffee is a beloved morning ritual, fueling the day ahead. But what if the time you drink it could influence how long — and how well — you live?
New research published Jan. 8 in the “European Heart Journal” suggests that when you enjoy your cup of Joe might be just as important as how much you drink.
The study shows consuming coffee only in the morning was linked to a 16% lower risk of premature death and a 31% reduced risk of dying from cardiovascular disease compared to non-coffee drinkers.
"This is the first study testing coffee drinking timing patterns and health outcomes," lead study author Lu Qi, a professor of public health at Tulane University, said in a news release.
"We don't typically give advice about timing in our dietary guidance, but perhaps we should be thinking about this in the future."
Researchers analyzed data from over 40,000 adults aged 18 and up using dietary records collected between 1999 and 2018. Coffee consumption was divided into three timeframes: morning (from 4 a.m. to 11:59 a.m.), afternoon (from 12 p.m. to 4:59 p.m.), and evening (from 5 p.m. to 3:59 a.m.)
Results show that those who
drank coffee exclusively in the morning benefited the most in terms of longevity and heart health.
Meanwhile, folks who drank coffee throughout the day saw no significant reduction in risk.
The findings held true regardless of whether participants drank caffeinated or decaffeinated coffee, and the amount consumed — whether they drank less than one cup or more than three — didn't impact the benefits.
So, why does timing matter?
Experts agree that the timing of coffee intake may influence your circadian rhythm and hormone levels. Drinking coffee later in the day, even if we feel like we need it, may disrupt melatonin production, a hormone that regulates sleep and influences heart health.
According to study authors, some inflammatory markers in the blood have their own clocks. And the anti-inflammatory effects of coffee may be more effective when consumed in the morning, when these markers peak.
However, the study was observational and cannot prove causation, noted Vanessa King, a registered dietitian nutritionist and spokesperson for the Academy of Nutrition and Dietetics who wasn't involved in the study, told CNN.



By George W. Chapman

As previously reported, the Inflation Reduction Act (IRA) caps out-of-pocket copays for drugs at $2,000 annually starting this year. This is great news for seniors, many of whom paid a lot more than $2,000 a month in copays.
Unfortunately, the $2,000 cap does not apply to consumers covered by employer commercial plans. Medicare is able to cover the additional cost associated with the $2,000 cap by paying billions less for drugs. That is accomplished by the Inflation Reduction Act (part two) which gives CMS the authority to finally negotiate prices with manufacturers.
Until the IRA, negotiating drug prices was literally prohibited by law which is testament to the power wielded by the drug manufacturers lobby. CMS is allowed to negotiate the price of 10 drugs effective next year. Congress has begrudgingly agreed to allow CMS to negotiate. Why not negotiate all drugs, you ask? It might have a little to do with campaign contributions from the drug lobby. In 2023, members of both sides of the aisle received an average of $57,000. Be that as it may, 10 is better than nothing. If the new administration is looking to cut costs, then what Medicare pays for drugs is a great place to start.
Medical debt has forced many people into personal bank ruptcy. The $2,000 cap on out-of-pocket costs for drugs estab lished by the Inflation Reduction Act may well prevent many bankruptcies for seniors in the future. The Federal Consumer Financial Protection Bureau just issued regulations which (at least) bars medical debt from affecting your credit rating. Credit agencies cannot include your medical debt on credit reports. The regulation also precludes lenders from considering medical debt when considering loans for borrowers. But despite the media

The chart below shows the negotiated price, deemed the MFP or maximum fair price, (fair to whom?) of the 10 drugs prices effective next year, versus the average price paid by countries with universal healthcare. (I couldn't find the current 2025 price per drug paid by Medicare.)
Despite our best effort at negotiations, we are still paying way more than other countries. Imagine the copay for Imbruvia at $10,619 a dose without the $2,000 cap!
The second chart shows the approximate total population in millions of the countries that pay (still) far less than the US despite our-soonto-be "reduced" 2026 price. Medicare
alone covers 70 million people. That is more than the total population of seven of the 10 countries listed. Where is our strength in numbers when it comes to negotiations? Where is our volume discount? The amount of money that would be saved if Medicare could negotiate on behalf of our total population (335 million) would be hundreds of billions. I'm including the savings that would also be achieved by commercial insurers as well. But until the stranglehold the drug lobby has on congress is eliminated, don't expect much improvement in healthcare costs let alone delivery.
if any patients are directly impacted by physician charges as third-party insurance establishes physician reimbursement. Withdrawing from Medicare and commercial insurance and going 100% self-pay is financial suicide. Compounding the Medicare cut is the potential for commercial carriers to mimic Medicare reimbursement and lower their physician payments. The Medicare cut is just another reason for physicians to eschew private practice.
Hacking patient records costs U.S. healthcare almost $2 million a day. In the past six years, breaches have cost U.S. healthcare almost $22 billion. Healthcare organizations incur 17 days of down time per occurrence, according to a report by Comparitech. Six hundred and thirty-four attacks in the last six years affected more than 88 million patient records. Razor-thin operating margins make total cyber security impossible. Medicare and commercial payments do not take into consideration the added costs of cyber security. The advent of AI will only make it easier for the bad guys to hack into information systems. To add insult to injury, Medicare actually penalizes healthcare organizations when they are hacked.
Jardiance $204 $52 $152
Farxiga $182 $54 $128
Eliquis $249 $76 $173
Enbrel $2,335 $764 $1,571
Januvia $117 $39 $78
Novolog $134 $50 $84
Xarelto $200 $82 $118
Entresto $314 $139 $175
Imbruvia $10,619 $5,670 $4,949
Stelara $4,490 $2,822 $1,668
frenzy and uproar over healthcare equity created by the murder of United Healthcare CEO Brian Thompson, don't expect any substantial changes to how healthcare is delivered for the foreseeable future.
Understandably, post-COVID-19, we are hyper aware of any potential epidemic. Bird flu has been getting a lot of attention lately. As of early January, there has been just one death attributed to bird flu or the H5N1 virus. The deceased was a senior (older than 65) resident of Louisiana with multiple underlying medical conditions. He was exposed to a backyard flock of wild birds. To date, there has been no indication the virus
is spreading person to person.
The January bill to fund the govern ment another three months did not include a provision to halt an illogical and unfair 2.8% cut in Medicare physician reimbursement. Considering that inflation is hovering around 3%, the 2.8 % reduction is tantamount to a 5.8% cut. Like all businesses, medical practices content with increasing labor, supply and insurance costs. But unlike other businesses, medical practices cannot compensate for rising costs by increasing charges. Few
If you're having trouble finding a mental health provider, you're not alone. Roughly half of mental health providers accept insurance and almost as many don't accept new patients. According to a Wall Street Journal survey, only 44% of Ph.D.s and psychologists accept insurance, let alone new patients. Many people are frustrated because the dearth of in-network providers creates long wait times of often several months. Online therapy is attempting to fill the void. Forbes Health has rated online providers. The top nine are: BetterHealth, Talkiatry, Cerebral, Talkspace, Brightside, Regain, Team Counseling, Faithful Counsel and Our Ritual. Services include depression, anxiety, stress, anger management, insomnia, panic attacks, eating disorders, trauma, relationships, life counseling, bereavement and more. Per Forbes, the best online therapy options were broad telehealth sites that include therapists: Amwell, Doctor On Demand and MD Live. You can get traditional therapy appointments focused on live video sessions. Ongoing therapy may require a subscription. It is best to contact your insurer before proceeding.


George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse.

The cancer death rate continues to decline in the U.S. but new cases are rising among women, potentially undermining progress against the nation's second-leading killer, according to a new report from the American Cancer Society (ACS).
The cancer death rate declined by 34% between 1991 and 2022, representing about 4.5 million deaths averted by early detection and improved treatments, the ACS said in its Cancer Statistics 2025 report published today.
However, new cancers among women and younger adults are increasing, the report found.
What's more, Native American and Black people still have much higher cancer death rates than whites.
“Continued reductions in cancer mortality because of drops in smoking, better treatment and earlier detection is certainly great news,” lead researcher Rebecca Siegel, senior scientific director of surveillance research at the American Cancer Society, said in a news release.
“However, this progress is tempered by rising incidence in young and middle-aged women, who are often the family caregivers, and a shifting cancer burden from men to women, harkening back to the early 1900s when cancer was more common in women,” Siegel said.
For example, cancer rates among women 50 to 64 have now surpassed those of men, with about 832 versus 830 cases for every 100,000 people, the report says.
And women younger than 50 now have an 82% higher cancer rate than men that age, about 141 versus 77 cases for every 100,000.
This shift can be partially blamed on increases in breast and thyroid cancers, which make up nearly half of all cancers in this age group and mostly impact women, the report stated.
Cancer rates in men younger
kidney and leukemia — but are offset by declines in cancers like melanoma, non-Hodgkin lymphoma and prostate.
Additionally, “alarming inequalities in cancer mortality persist,” an ACS press release says.
Native American people bear the highest cancer death rates, and are two to three times higher than white people to die from kidney, liver, stomach, and cervical cancers, the report says.
And Black people are twice as likely as white people to die of prostate, stomach, and uterine corpus cancers, and 50% more likely to die from cervical cancer, which is preventable, according to the report.
“Progress against cancer continues to be hampered by striking, wide static disparities for many racial and ethnic groups,” senior researcher Ahmedin Jemal, a physician and senior vice president of surveillance and health equity science at ACS, said in a news release.
“It's essential to help end discrimination and inequality in cancer care for all populations. Taking this step is vital to closing this persistent gap and moving us closer to ending cancer as we know it, for everyone,” Jemal added.
Other findings from the report:
• Progress is lagging against pancreatic cancer, which is the third-leading cause of U.S. cancer deaths. New cases and deaths are both increasing, and the five-year survival rate now stands at just 8% for nearly all cases.
• New colon cancer cases are rising among men and women younger than 65.
Cervical cancer cases have increased in women 30 to 44.
• Cancer cases among children 14 and younger have declined in recent years, but continue to increase among teens 15-19.
• Cancer death rates have dropped by 70% in kids and 63% in


By Gwenn Voelckers
By Gwenn Voelckers
In 1993, I purchased the home I still live in today.
At the closing, I became the proud owner of someone else’s dream home, complete with bright green shag carpet, a Pepto Bismal pink powder room and lacy bedroom curtains hanging in the living room.
What was I thinking?!
But I was convinced of the home’s potential and began a gradual, thoughtful and very rewarding process of making this home my own.
Looking back, I now realize that creating a home that is joyful, inspiring and uniquely mine was one of the most empowering things I did for myself after my divorce.
It was an essential part of starting my life over as a woman on her own.
If you are now living alone — whether due to a divorce, the loss of a partner or some other major life change — know that, while daunting, a fresh start can be incredibly liberating.
Designing your space for the person you are now, not the person you used to be, can support your journey toward happiness and fulfillment.
Let your home be your launchpad for the next phase of your life.
So, how do you design a space that reflects your singular style and spirit, especially if you are navigating
life on your own for the first time?
Here are some insights and tips that have helped me along the way.
Intuitively, I knew I needed to walk through my new front door and into my very own “warm embrace,” a place where I would be surrounded and uplifted by all things familiar and friendly.
So, I set out to create a retreat — a personal sanctuary where I could feel safe and sound, inspired and creative.
One of the first things I did when I bought my home (after I tore out the green shag carpet) was to frame and display photographs of family and friends. I wanted to see their faces when I entered a room, to be reminded of good times and the love that surrounds me.
In addition to photos, I adorned my living space with original pieces of art (now more boho!) and artifacts or souvenirs I collected on my travels. These cherished mementos and images lifted my spirits back then and continue to do so.
I encourage you to surround yourself with treasured items that reinforce both who you are and who you want to become. Whether it’s art, books you love, fresh flowers or
a favorite blanket, infuse your space with décor and possessions that make you smile.
Japanese author and organizer Marie Kondo’s famous phrase, “Does it spark joy?” became my mantra when I started the process of decluttering.
As she instructed, I took a deep breath and asked myself: "Does this truly make me happy? Does this piece of furniture, these old clothes, or that vase from my wedding still bring me joy?"
It was hard at first. There were items that carried sentimental value or that I thought I should keep because "that’s what you do." But once I embraced the idea of letting go of anything that didn’t spark joy, I felt an incredible weight lift off my shoulders.
If an object doesn’t bring you joy, let it go. By clearing your space of things that no longer align with who you are today, you make room for the things that truly do resonate with the person you aspire to be.
I’ll get to the point: Anything that makes you feel bad when you look at it should be thrown out, donated or repaired. Ratty dishtowels, old lampshades and faded curtains, for example, can dampen your mood and erode your self-esteem.
Don’t underestimate the negative power of unsightly or outdated objects.
I walked into my kitchen last week and cringed (for the 100th time) when I looked at my faded and frayed kitchen mat. I threw it out and grabbed a small oriental rug from my guest bedroom to put in its place.
It looks and works great! Yes, it’s a little unconventional for the kitchen, but I feel good every time I see it. What took me so long? I need to
follow my own advice!
Create Spaces That Inspire, Lift You Up and Nurture Personal Growth
One of the most powerful things about living alone is that you have the freedom to design your home exactly how you want it. No compromises, no negotiations. You get to choose every color, every piece of furniture and every layout.
Over the years, I’ve come to realize that my home is more than just a place to live — it’s a place that inspires and supports my continuously evolving self.
For example, as my passion for music grew, my home gradually transformed into a tangible expression of this newfound love.
My living room now sports my drum kit, bongos and assorted percussion instrument. Again, unconventional, but it reflects who I am today.
Designing spaces in your home that nurture your growth — whether it’s a meditation corner, a cozy writing desk or a place for artistic expression — can help you move forward.
Creating a home that is joyful, authentic and aligned with your true self is one of the most empowering things you can do for yourself.
Remember, you are not defined by your past, your circumstances or your former relationships. Your home can become an oasis of creativity and independence — a place that’s unconditionally yours, absent of compromise. Claim it.
Once you make your personal space your own, there’s no place like home!
Gwenn Voelckers is the author of "Alone and Content," a collection of inspiring essays for those who live alone. She welcomes your comments about this column and topic suggestions for future columns at gvoelckers@rochester.rr.com
Too much screen time can sabotage preschoolers' sleep, potentially turning them into terrors around the house, a new study warns.
Bad sleep can exacerbate children's struggles with poor attention, hyperactivity and moodiness, researchers reported Dec. 12 in the journal “Early Child Development and Care.”
Worse, kids can wind up in a downward spiral, with screen time and poor sleep feeding off each other.
“Our results suggest the presence of a positive feedback loop, wherein increased screen time and sleep disturbances exacerbate each other
through cyclic reinforcement, heightening the risk of hyperactive attention problems, anxiety and depression,” said researcher Bowen Xiao, an expert in children's socio-emotional functioning and developmental psychopathology with Carleton University in Canada.
For the study, researchers surveyed the mothers of 571 preschool children between the ages of 3 and 6 who were attending seven public kindergartens in Shanghai.
Moms reported the amount of time their kids spent with a TV, smartphone, computer or other screen device. They also answered questions to assess any behavioral

problems their kids might have, as well as the quality and duration of their sleep.
“Our results indicate that excessive screen time can leave the brains of preschool children in an excited state, leading to poor sleep quality and duration,” said researcher Yan Li, an expert in preschool education from Shanghai Normal University.
Researchers also noted that prior research has indicated that screen time can lead to hyperactivity and emotional problems among kids.
This study suggests that screen time might be the reason why, researchers said.
“This poor sleep may be due
to postponed bedtimes caused by screen viewing and the disruption of sleep patterns due to overstimulation and blue-light exposure,” added lead author Shujin Zhou, a doctor of psychology with Shanghai Normal University.
“Screen use might also displace time that could have been spent sleeping and increase levels of physiological and psychological arousal, leading to difficulties in falling asleep,” Zhou said in a journal news release.
These results could point the way toward future treatments for hyperactivity and mood problems among young children, Zhou said.
By Eva Briggs, MD

How can alcohol cause cancer? There are at least four known ways.
• First, alcohol breaks down in the body to a chemical called acetaldehyde. This substance harms DNA. Damaged DNA can allow a cell to grow uncontrollably leading to cancer.
• Second, alcohol also produces reactive forms of oxygen leading to oxidative stress which damages DNA, proteins and cells.
• Third, alcohol alters many hormones. It increases estrogen levels which increases the risk of breast cancer.
• Fourth, alcohol dissolves other cancer-causing chemicals such as those found in cigarette smoke. It also alters the cells of the mouth and throat. This makes those toxic substances more easily absorbed, raising the chance of mouth and throat cancers.
Drinking alcohol increases the risk of seven types of cancer:
1. Mouth and oral cavity 2. throat (pharynx), 3. esophagus, 4. voice box (larynx), 5. breast, 6. liver, 7. colon and rectum
Over my career I have cared for patients with every one of these cancers.
Quitting or reducing alcohol won’t prevent all of these cancers. But all of them are so unpleasant that reducing the chance of acquiring any of these diseases is worth considering.
How significant is the risk of cancer from drinking alcohol?
The risk that a woman who drinks less than one drink per week will develop cancer in her lifetime
Upstate's revitalized and growing heart services provide benefits to you.
From six cardiology outpatient sites to the arrival of our new heart surgeons, and more doctors and advanced providers for procedures such as caths and TAVRs, we are here to work with you. Learn more about what The Upstate Advantage can do for you.
is about 17 per 100 individuals. One drink per day increases that risk to 19 per 100 individuals and two drinks per day further increases the risk to 22 per 100 people. That means that five more women out of 100 (or one out of 20) who drink higher levels of alcohol will develop cancer during their lifetime.
For men, the risks are about 10% for those who drink less than one drink per week, to 11% for those who drink one drink per day and 13% for those who drink two drinks daily.
The surgeon general report made the following suggestions for steps to reduce alcohol-related cancers.

Update the health warning label on alcoholic beverages to warn about cancer risks. Reassess the recommended limits for alcohol consumption. Increase efforts to expand general awareness and educate the public. Inform patients during clinical encounters about the link between alcohol consumption and cancer risk.
We already know from past experience — prohibition — that making alcohol illegal is not the answer. But it’s up to us health care providers to make the public aware of these facts so that people can make informed decisions.

By Mary Beth Roach
Maryann Roefaro will step down as CEO of the Hematology-Oncology Associates of CNY on Feb. 14 after 23 years in the position. Assuming the leadership role will be Jen Pichoske, who came to the practice in 2012 as director of nursing. She was named chief clinical director in 2020 and has been HOA’s chief operating officer since 2023.
HOA is a private practice providing care for people with blood disorders and cancer since 1982. Roefaro noted that it is unique in that it is not affiliated with a supergroup or large hospital system. Last year alone, HOA recorded 133,479 patient visits, including visits to doctors, advanced practice providers, physical therapists, labs, cancer genetics and lung cancer screenings.
The number of employees is approximately 335, including 21 physicians and 34 advanced practice providers.
For the past two-plus decades, Roefaro has brought her boundless energy to her job. Her tenure has been marked by building — and rebuilding — virtually every facet of the organization — constructing brick-and-mortar facilities, rebranding the practice, enhancing the workplace environment, bringing in new therapy programs and introducing initiatives to help relieve some of the stresses that their patients experience.
organization to be known in the market and our turnover became low and our applicants became many.”
She realized, too, the need for what she called “long-term sustainability and success,” which she believed would come about through greater community awareness. To that end, she was responsible for creating the current HOA logo; investing marketing dollars into sponsorships for cancer-related foundations; and involving the HOA in various events that would give the organization more exposure. She also connected with boards in the area, such as Hospice of CNY, the CNY Komen Foundation; Syracuse Home and McHarrie Towne, to name a few.
Roefaro noted, too, that she is proud of that HOA has been able to maintain state-of-the art equipment and therapies.
Among those is CyberKnife radiation treatment, the only provider in Central New York to offer the treatment. She offered an example of its efficacy: prostate treatments are done in five days instead of 45 conventional treatments, adding that with such great outcomes it has become a standard of therapy for prostate cancer in the industry.
And as integrative or complementary therapy programs to augment cancer care became popular, often they were only available at large, prestigious cancer centers across the country. However, she noted, HOA was the first in Central New York to develop a complementary therapy program that included massage, acupuncture, reiki, foot reflexology and other energy healing modalities.
“I knew it was difficult for our patients to pay for these services while dealing with the financial stressors of cancer therapy, so I wanted to do something to help them. With the support of our physicians, I created CancerConnects, Inc. — originally known at Unique Connections,” she added.
retirement.
While she doesn’t have any specific retirement plans, she is looking forward to sleeping past 4:30 a.m., the time this avid runner usually got up so she could do a run before heading to work. She is working on her fourth book, “Transitions of Hope,” which she said is about half done; she plans on spending time with her husband, Tom Carranti, their family and her two dogs, Millie and Bella. She’s also considering taking up golf and starting a podcast with friend Mary Schechter.
And she said she may do her seventh marathon when she turns 70.
As she leaves HOA, she believes that Pichoske “is not only brilliant and truly understands operations, patient’s needs and cancer care, her heart and soul was made for HOA.”
Pichoske brings both professional and personal experience to her new role and her goals are to continue to develop staff morale; invest in new technologies and therapies; build partnerships; and to see HOA become more active politically.
Pichoske has been in hematology and oncology care for nearly 30 years as a nurse, nurse practitioner and instructor at the Crouse Hospital School of Nursing. She has an executive MBA from the Quantic School of Business and Technology and a Master of Science in nursing from the University at Buffalo and she is an advanced oncology certified nurse practitioner. In addition, because family members have had cancer, she has first-hand knowledge of a patient’s journey through the disease.
“I understand all the complexities that it takes to support the healthcare professional in every way and to help patients and families look at their mortality, keep them motivated through hope,” she said.
Shortly after becoming CEO, she helped to expand its Brittonfield space, which had first housed its radiation operation, to 65,000 square feet, bringing the entire practice under one roof. She was instrumental in opening a center in Auburn in 2012 and a Patient Rx Center in 2013. More recently, she oversaw the opening of a massive new 21,000- squarefoot comprehensive cancer center in Camillus.
She called the cancer center in Camillus her “last hurrah.”
“We opened our doors to this state-of-the-art facility in August. I put so much love into selecting the colors, furniture and artwork — every time I drive by, my heart smiles.”
However, she noted that one of her first orders of business 23 years ago was to build new staff morale.
“My first objective was to change the culture of our practice,” she explained. “The doctors were and still are fabulous — which only underscores the importance of good leadership. Culture is everything in an organization and it’s not one and done — it’s a continual effort. One of my first successes is that within a year, our culture improved significantly. My leadership and I supported by our physicians — created a culture of love, integrity, trust, transparency and accountability. The employees knew they had a voice and were appreciated — it did not take long for the personality of our
She secured its 501 (c)(3) status and it provides free complementary therapy sessions (like reiki, etc.) and assist cancer patients with all their financial burdens through their journey. These could include supplemental insurance payments, insurance co-pays, financial assistance for daycare, mortgages, rent, groceries, gas and other necessities.
CancerConnects also saw expansion during Roefaro’s tenure. As she explained, staff social worker Gussie Sorensen felt it was essential to create a mentoring program for cancer patients — trained volunteers that would assist in the journey and Roefaro brought it under the CancerConnects umbrella. In addition, the program has partnered with the Saint Agatha Foundation, which provides financial support for breast cancer patients. Additional support for CancerConnects comes through fundraising events held by the HOA Fun Committee, which Roefaro started.
She is also proud of her work with John Gullo, hematology-oncologist specialist, to develop the Breast Care Partners LLC, which is unique in that it brings together breast health specialists — regardless of the healthcare institution they’re affiliated — to provide, as its website states, “an organized, comprehensive, multidisciplinary, team approach to breast care that is now considered best practice to improve clinical and psychological outcomes for all patients.”
The energy that Roefaro brought to her work will not be lost in her
She noted too, that although she and Roefaro had been working together for the past two years to facilitate a smooth transition, it is still a big change for the staff. So she said she is going to continue to work on employee morale.
“Without them, we couldn’t get anything done,” she said.
Among her other goals, she said, is to have “the latest and greatest therapies” in medical oncology, radiation oncology and diagnostic imaging, which, with the ever-changing technological advances in the field, is a continual work in progress.
And she wants to continue to build the organization’s ongoing network of partners, especially, as she noted, since there have been some delays in services because of the pandemic.
HOA partnerships can only be enhanced Pichoske’s involvement with various boards.
She serves as vice president of the board for Hospice of CNY and the Finger Lakes, a local board member for Breast Care Partners, LLC and Cancer Connects, Inc. and a national board member of the Community Oncology Alliance.
She explained that COA is active in lobbying lawmakers, taking part in Hill Days three or four times a year and she wants to bring an increased presence on the state level.
“I’m going to continue to foster and promote political activism for cancer care nationally and statewide,” she said. “We’re going to get really active in that and go to Albany and make sure patients have everything that they need and access to care when it comes to cancer care.”


























Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMENT GROUP




Hybrid Nurse Aide Training Program ELEMENTAL MANAGEMENT GROUP







Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Equip your facility with our unstoppable HYBRID CNA program, empower your team to deliver top-notch care with the strength of a champion.
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking for an innovative way to attract CNA students? We have your answer
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to minimize and most importantly eliminate agency use? We have your solution
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to improve morale by increasing your direct care PPD? Reach out to us to hear more
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today
Are you looking to captivate and motivate the newer generation by offering unique and rewarding training opportunities? Look no further contact us today

CONTACT:

Peg Reith BSN, RN
Phone: 315-529-3267
CONTACT:
Email: CNA_Training@elementalmgt.com
Peg Reith BSN, RN
Phone: 315-529-3267
Email: CNA_Training@elementalmgt.com










By Anne Palumbo
Ahem. Before I enumerate the powerful benefits of eating beans, I’d like to ask you a personal question: Do you suffer from “bean hesitancy,” a common phenomenon marked by a reluctance to eat beans for fear of increased flatulence?
Yes?
Rest easy, you’re not alone. No thanks to jokes, children’s songs, and personal experience, many shy away from this “musical fruit.”
Let’s hope after reading this month’s column, you will—to paraphrase John Lennon—“give beans a chance.” That’s all we are saying.
To begin with a bang: Black beans have a nutritional profile like no other bean. While high in plantbased protein like most beans, black beans contain a unique slew of nutrients that other beans either lack or have negligible amounts.
• Diabetes warrior: According to medical experts, Type 2 diabetes is a national epidemic, with more chil-
dren, teens and young adults developing Type 2 diabetes than in the past due to rising obesity rates and unhealthy diets. Black beans help manage blood sugar levels in three remarkable ways: their low GI (glycemic index) won’t spike blood sugar levels and cause an aggressive insulin response; their high fiber content slows down digestion and the release of glucose into the bloodstream; and, lastly, their particular antioxidants support blood sugar control. Takeaway? Managing this disease can improve life expectancy.
• Sleep promoter: When it comes to better sleep, consuming black beans may be your express ticket to the land of Nod, and, according to the Mayo Clinic, a longer life. Thanks
to an abundance of three important nutrients—tryptophan, magnesium and fiber—your sleep may improve with regular consumption of this soporific bean. Specifically, tryptophan contributes to the production of sleep-boosters serotonin and melatonin, magnesium helps regulate melatonin production and muscle relaxation, and fiber helps prevent disruptive energy crashes by regulating blood sugar levels.
• Heart protector: Eating black beans has been shown to reduce high blood pressure, high cholesterol and obesity, which are all key risk factors for heart disease and premature death. How exactly do beans aid weight loss? Because this mighty legume teems with two nutrients that take longer to digest—protein and fiber—they often enhance feelings of fullness, which can result in eating less. Hearts also love black beans for their bounty of folate, a B vitamin that helps the heart

Drain and rinse canned beans thoroughly (to reduce both sodium and the production of gas). Scour labels and select canned beans with reduced or no sodium. Rest assured that 95% of food cans are now BPA-free.
stay healthy by reducing an amino acid that can damage artery walls and increase the risk of heart disease and stroke.
Circling back to the toots: I now present some valuable intel from the Bean Institute. 1) The more beans you eat on a regular basis, the less likely you’ll experience gas. 2) Drinking more water as you eat more beans helps your body better process a bean’s fiber. 3) Gas in the gut is generally considered a good sign because it indicates that healthy bacteria are hard at work!


Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.
Ingredients
Serves 6-8 Adapted from Eatingwell.com
1 tablespoon oil
2 medium sweet potatoes, washed
1 medium onion, chopped
1 garlic clove, minced
1 teaspoon chili powder (or more if you like heat)
1 teaspoon ground cumin
½ teaspoon salt (or less) ¼ teaspoon coarse black pepper
Directions
1. Preheat oven to 400 F. Lightly coat a 9 x 13 baking dish with oil or cooking spray.
2. Soften sweet potatoes in microwave: Pierce skin with a fork, then place on a microwave-safe plate and microwave for about 5-6 minutes, until sweet potatoes are soft enough to easily peel and cut into ½ cubes. Transfer to a large bowl.
3. Heat oil in a small nonstick skillet over medium heat. Add chopped onions; cook, stirring occasionally, until soft and golden, 4-6 minutes. Add minced garlic; cook 1 minute more, then add chili powder, cumin, salt and pepper; cook, stirring con-
1 (14.5 oz can) petite diced tomatoes, drained
1 (4 oz can) mild diced green chiles, drained
1 (15 oz can) reduced-salt black beans, drained and rinsed (or 2)
1 (8.5 oz can) sweet corn, drained
1 tablespoon lime juice
1¼ cups shredded cheese of choice
Optional garnish: cilantro, avocado slices, sliced scallions, lime wedges
stantly, for 30 seconds.
4. Transfer contents of skillet to bowl with sweet potatoes; gently stir in diced tomatoes, diced chiles, black beans, corn, lime juice, and ¾ cup cheese. Transfer this mixture to the prepared baking dish. Scatter the remaining ½ cup cheese on top. Cover dish with foil; bake for 15 minutes. Remove the foil; bake until the sweet potatoes are tender and the cheese is melted, about 10 minutes more. (Quickly broil if you like a crispier top.) Garnish with toppings of choice.
Note: Want some crunch? Add a layer of tortilla chips or broken-up taco shells before sprinkling the last ½ cup of cheese.
Philip Smith is a registered dietitian at Oswego Health: “New beginnings can occur at any time of the year and don’t need to fall off like so many New Year’s resolutions do.”
The New Year is often filled with hope and high expectations. By the end of the month, all that can turn to disappointment.
That occurs because people put all their efforts into living their best life and year in the early weeks and when things slightly fall off, they become dejected. However, health professionals want you to know your healthy journey can always be reset.
“While the new year is a great opportunity to kick start your new health goals, it’s not the only time you can make a change. New beginnings can occur at any time of the year and don’t need to fall off like so many New Year’s resolutions do,” said Philip Smith, a registered dietitian at Oswego Health. “Lifestyle changes are an ever-evolving process that requires work day by day. Start small, make realistic goals that are measurable and achievable and don’t get discouraged by small setbacks.”
It’s easy to lose weight on a diet. But as soon you stop following the restrictive rules of that diet you gain it all back and then some. Most diets work on the basis of limitations by cutting out entire food groups. Despite their strict guidelines, these diets remain effective only because they reduce your overall calories.
“What they fail to do is foster a
positive mind set, establish a healthy relationship with food or achieve sustainable weight loss,” said Smith. “In the end it mostly boils down to consistent behavior changes with slow manageable goals and setting in place repeatable habits.”
Healthy eating seems daunting. It requires constant perfection without any room for the foods that you enjoy. This perspective gets in the way of feeling able to succeed, leading many to get discouraged at the slightest missteps and unwilling to make changes that seem so unattainable.
“The truth is that eating healthy doesn’t look the same for everyone and it doesn’t work as a one-size-fitsall approach,” said Smith. “It begins as a unique approach with individual goals that reflect each person’s situation including their economic status, time constraints, support system, geographic location and personal motivation. What you see on social media doesn’t reflect what is best or healthiest for you. The latest and greatest superfood or exercise regimen may be enticing, but it is not likely to be the quick fix solution that will change your life.”
In addition, Smith suggests meal prep, eating balanced meals with lean protein and non starchy vegeta-
By Ernst Lamothe Jr
bles and drinking water.
Oftentimes healthy living makes people creative in a negative way. They look to shortsighted, shortcuts to achieve success.
“We see a lot of people who perform unhealthy habits such as skipping meals to get their desired results,” he added.
In addition, you should stay away from time-honored nutrition pitfalls. “Make sure you are not eating late at night before bed, extra calories from drink and eating fast food several times a week,” he said.
Many physicians recommend using the American Heart Association guideline of 150 minutes of moderate intensity aerobic activity every week. Moderate intensity exercise should elevate your heart rate and make you start to sweat. Walking doesn’t cost a thing and can be done just about anywhere. It is also important to add in weight and resistance training for muscle and bone health and stretching for flexibility.
“It is undeniable the necessity of exercise in our health. Physical activity plays a crucial role in our overall well being. It improves our functional ability, strength, focus, resilience, mental health and ability to live in-
dependently,” said Smith. “It is also a necessary component to sustaining weight loss and weight maintenance. Exercise has benefits even in small doses. It only takes 30-45 minutes of exercise three to four days per week to see improvements. Physical activity comes in different forms including cardio, flexibility, stretching and weight resistance. Benefits come from a combination of all three but most of us today will benefit from the simple inclusion of more movement into our daily routine.”
5.Why should you care?
Lifestyle decisions early in life play major roles in the conditions we deal with later on. Rates of conditions like diabetes, heart disease, hypertension and obesity are all drastically increasing.
“These chronic conditions aren’t in the immediate impact of one single decision today but are compounded by the little choices and habits we engage with every day.” said Smith. “Making small changes today can have a huge impact on our health in the future by helping us to avoid frequent hospital stays, take endless medication, suffer from compounding conditions and allow us to be able to live our lives independently.”

Our free services include:
◘ Private, one-on-one counseling about health insurance options
◘ Answering your questions related to Medicaid and long term care.
◘ Helping you decide what plan is right for you.

◘ Helping you solve problems with your managed care plan.
◘ Meeting with you over the phone or in-person.
◘ Conducting educational sessions for consumers, caregivers, and professionals
By Norah Machia
If there is one message Caron Grossman hopes to convey in her new book, “Listen to Your Heart Song: Navigating the Unexpected,” it’s that women are their best health advocates, especially when it comes to their hearts.
Her book, published this February by Wildebeest Publishing, focuses on how women experiencing a heart attack may present with different symptoms than men and why it’s important to take those symptoms seriously.
Grossman knows how these symptoms often look different in women. Although she is a registered nurse, Grossman learned firsthand from personal experience.
Her mother died of a heart attack at age 39 after doctors attributed her symptoms to a hiatal hernia. At age 58, Grossman herself experienced a heart attack that started with “somewhat benign symptoms,” she said. “There was no chest pain, left arm pain or shortness of breath that we mostly associated with a heart attack.”
At the time, Grossman was speaking on the phone with a friend when she started to experience an odd sensation on both sides of her jaw.
“It was like an electrical current,” she said. A dull ache was also starting in the base of her neck. “At first I joked that my jaw was hurting because I was talking too much,” she added.
But after getting off the phone, the neck pain worsened and Grossman quickly realized something was seriously wrong. Although she was at a healthy weight and didn’t smoke, drink or eat sugar, Grossman sensed she might be having a heart attack based on her family history.
Along with her mother, her great-grandmother and two greataunts also died at a young age from heart attacks and her father had undergone quadruple bypass surgery in his 60s (although he lived into his 80s).

Caron Grossman is a registered nurse at Crouse Hospital. She wrote a book — “Listen to Your Heart Song: Navigating the Unexpected” — after she had a heart attack.
Grossman called 911 and was transported to Crouse Health, where she works as a registered nurse in the one-day surgery department. Medical tests showed that a coronary artery was nearly 100% blocked.
After undergoing a procedure to have stents placed in the artery to keep it open, “my heart is good,” Grossman said.
Following her heart attack, Grossman was surprised by the reaction from many people who asked about her story and did not realize that heart attack symptoms may present differently in women.
She began writing a book about her experience to help educate other women and encourage them to “listen to their bodies” if they believe something is seriously wrong, she said.
“Last year, I started thinking that people need to know some of the heart attack symptoms that may present in women,” she said. “It could be extreme fatigue and shortness of breath to jaw pain and dizziness.”
Because women are typically the primary caregivers of the household, they may not take the time to

get those health issues checked by a doctor or think they have an illness, like the flu, she added.
“We have to advocate for ourselves; we have to ask questions and get answers or rephrase the questions,” Grossman said. “We know our bodies better than anybody.”
According to the American Heart Association, a heart attack strikes someone about every 40 seconds in the United States. Although heart disease is considered the leading cause of death among women in the U.S., it’s common for women to attribute their symptoms to conditions that are not as life-threatening, such as acid reflux, the flu or normal aging.
“Many women think the signs of a heart attack are unmistakable,” according to the agency’s website. “But the signs may not be as obvious and might be confusing. Even when the signs are subtle, the outcomes can be deadly, especially if the person doesn’t get help right away.”
Both men and women may experience common heart attack symptoms, including chest pain and discomfort (or uncomfortable pressure or squeezing in the chest that may come and go). Other symptoms could include pain or discomfort in the arms, back, neck, jaw or stomach, shortness of breath, cold sweats or lightheadedness, according to the organization.
Some symptoms that women may experience, which are typically less associated with a heart attack, are anxiety, upset stomach, back pain or unusual tiredness or weakness.
Grossman is hoping that she can increase awareness because “I don’t want anyone else to say to me they had no idea it could have been a heart attack when they heard about my symptoms,” she said.
“This book is both a memoir and a vital resource, shedding light on a critical health issue that affects millions of women worldwide,” Grossman added.
A book launch party is scheduled for Feb. 7 from 5 to 8 p.m. at Northbound Mind and Body, 116 N. Main St., Minoa. Grossman will give some readings, and heart-healthy snacks will be served.
The book, released in February to coincide with Heart Health Month, will be sold at the Minoa location and available online at Amazon and Barnes & Noble.
For more information: www.carongrossman.com



By Deborah Jeanne Sergeant
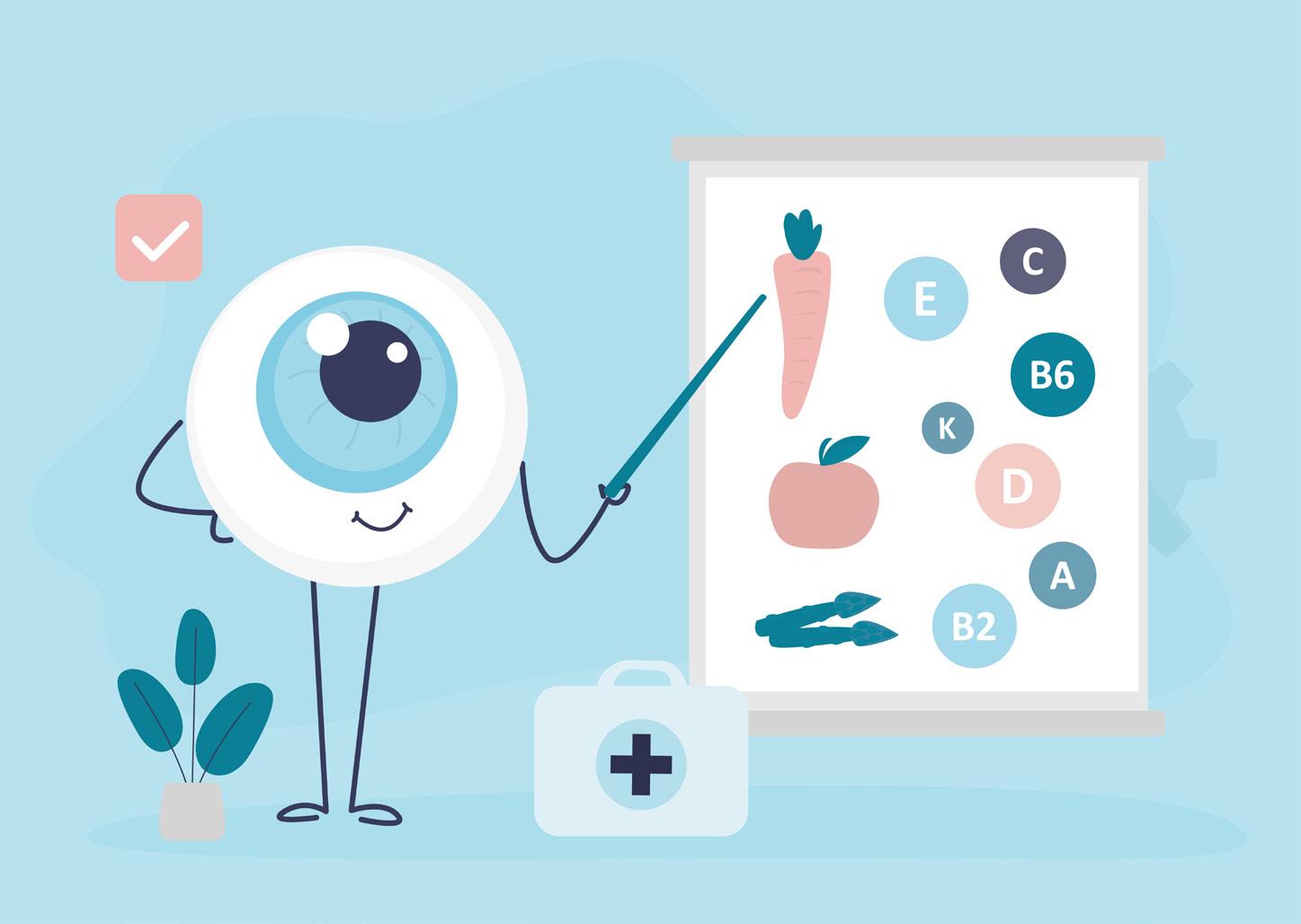
Eating right supports the body’s health, including the eyes.
Kelly Springer, registered dietitian and owner of Kelly’s Choice in Skaneateles, recommended “foods with lycopene are best for vision
pene. But that’s not the only type of nutrient that supports eye health.
“Spinach has been found to be one of the highest food sources for lutein and zeaxanthin and it also contains a moderate amount of vitamin C, vitamin A and folic acid,” said Laurel Sterling, registered dietitian, nutritionist and national educator for Carlson Laboratories in Canastota.
She explained that lutein and zeaxanthin are carotenoids, which promote healthy vision. These nutrients are found in yellow, orange and green leafy foods like sweet potatoes, carrots and kale.
“Kale is a power-packed veggie too,” Sterling said.
She recommends adding it to salad, eating dehydrated kale chips and adding it to soups and other dishes. Spinach is good in salad and shredded into frittatas, omelets and smoothies.
Sterling noted that one cup of chopped, raw kale 26 mg. of lutein and zeaxanthin, more than 6 mg. of beta carotene and more than 10,000 IU of vitamin A.
Other lutein-rich vegetables include collard greens, turnip greens, romaine lettuce and broccoli.
sources of vitamin A include orange and yellow fruits and vegetables. Some higher sources of beta-carotene are sweet potatoes, squash, carrots and pumpkin.”
Snack on raw carrots or yellow and orange pepper strips with hummus or dip. Or add carrots to a smoothie, soup, stews and casseroles.
“Pumpkin makes a delicious soup, muffins, bread and it can be a power-packed addition to smoothies,” Sterling said.
Vitamin C is also important for healthy vision.
“Vitamin C is an antioxidant that works to scavenge free radicals, as well as aiding in capillary and blood vessel health,” she said.
These actions can help keep your eyes working well.
Sterling noted many types of produce contain vitamin C, including red and green bell peppers, winter squash, Brussels sprouts, cauliflower, cabbage, turnip greens, spinach, other leafy greens, broccoli and sweet potatoes.
health. Some great food choices that have lycopene are guava, tomatoes, grapefruit, red bell peppers, watermelon and papaya.”
Sterling also recommends consuming foods rich in beta carotene. An important antioxidant, beta carotene helps the body produce vitamin A.
“Vitamin A is important for healthy vision as it plays an important role in helping the eyes adapt to light changes,” Sterling said. “Food
9.75” WIDE X 6.69” HIGH
In general, most produce that’s red contains some amount of lyco-
To increase your intake of colorful produce, try serving more than one vegetable at a meal, cooking up vegetable-based soup and stew a few times a week, adding veggies to a breakfast omelet or scrambled eggs, serving produce for snacks and including fruits and vegetables in smoothies and juices. Make it fun for your children by tracking how many colors of produce you consume daily and try to “eat the rainbow” every day.

At Hematology-Oncology Associates of CNY, you are never just a diagnosis or a number. We see you...the whole person, with passions, hopes, dreams, histories, and loved ones who share in your journey. From diagnosis, to treatment, to survivorship – our personalized care focuses on truly understanding and planning for your unique needs. We provide genuinely compassionate support, collaborating with you, your family, and caregivers every step of the way. Learn more about HOA today. We’ll see you and care for you – body, mind and spirit.


By Melissa Stefanec MelissaStefanec@yahoo.com
ebruary is the month of love.
So please allow me to put my rose-colored glasses on for this month’s column.
I want to reflect on the most beautiful parts of the toddler and preschool years, because there were a lot of them.
Don’t get me wrong. Those years were really tough. I remember the impossible meltdowns. I remember being in a state of high alert and constant vigilance. I remember swiping strange things out of kids’ mouths and potty time. I remember not sitting down much or finishing many adult conversations. I remember crying in the bathroom when I felt overwhelmed. I remember losing my cool and hating myself for it. I remember feeling incredibly ill-equipped and wondering if I would ever get things right.
Those were some very trying years. If you are currently in the midst of them, I’m not going to tell you these are the best years of your life or that you should stop feeling overwhelmed, angry or exhausted. When people say things like this, I think their hearts are in the right place. However, they are being dis-
missive and failing to recognize the complexities of the parenting experience. I encourage parents of toddlers to feel how you need to feel at any given moment.
What I will do instead, is share what I still carry with me from my kids’ younger years. It’s been a decade since my oldest was a toddler. But I often think about moments from her and her brother’s younger years. Many of those moments still give me joy. Those memories can turn around a bad day. Those memories are treasures beyond value.
My hope is that by sharing these fond memories, I can help parents in the midst of the trying toddler years find some pockets of joy.
Joy can help you through the exhausting days. It is lifeblood.
• Beautiful moment: The way my kids mispronounced or misused words
My daughter had the most wonderful way of saying owl. I will be 80 years old and still hear her little voice mispronouncing that word in the most beautiful way. My son called his lacrosse pads his armor. There was no correcting him. When he suited up for the field, he was going to fight
and needed his armor.
• Beautiful moment: The way they took my hand in public
There comes a point where kids don’t want to hold hands with their parents anymore, which is good. But every once in a while, I still reach for their hands when walking through a parking lot. I miss the days where I could protect them from most of the dangers in the world.
• Beautiful moment: The way they brought all of their problems to me
As annoying as all-encompassing reports from toddlers and preschoolers can be, I miss the days where I knew almost everything about their lives. It was nice to solve most of their problems. Things were less complex then. Coaching kids to solve their middle-school problems is tough. I miss the days when a kiss took most of the pain away.
• Beautiful moment: Dressing them in adorable clothes
Sure, my kids fought me to wear their favorite clothes when they were young. But I got to pick out most of those clothes. I’m glad my kids are picking out their own clothes nowadays and finding themselves. But every once in a while, I wish I could put them in something adorable.
• Beautiful moment: When they said something funny that I should not have laughed at
This still happens, but not in the same way. Kids get edgier as kids get older. I miss the days when my children said something so obstinate or clairvoyant that I had to laugh. Granted, I had to direct them afterward, but I usually appreciated their fiery spirits.
• Beautiful moment: When they brought me simple gifts My kids used to bring me special presents on almost every walk we took. I have a tin of these presents. They brought me things like the first flowers in spring. A special rock. A leaf with a spot of color. Those gifts were from the heart and given without the expectation of anything but a smile in return.
• Beautiful moment: When they found pure joy in the simplest things I remember my kids finding temporary, all-consuming joy in the simplest things. An unusually large apple. A towering cone of ice cream. A squirrel being a squirrel. My kids still do this, but it’s not an hourly occurrence. If you have young kids, I really encourage you to find the joy that they find and experience it with them. That is one piece of advice I will stand by.
• Beautiful moment: The way they belly-laughed
Belly laughs are one of the greatest gifts a child has to share with the world. I remember my son laughing in public places and strangers joining him, because they simply could not help themselves. I remember my daughter telling nonsensical jokes and cracking herself up and others joining in the fun. Those belly laughs are a treasure. They are the medicine for the tantrums.
I hope this list of memories helps parents find a little extra joy when they are in the toddler and preschool trenches. Because, as a parent, you should be allowed to feel all of the emotions and do so without guilt.


The ‘DXA’
By Deborah Jeanne Sergeant
Of course, you will likely receive an X-ray if you break a bone so the provider can set the bone.
But did you know that there’s a diagnostic scan that can look at your bones’ density?
The DXA (also called a “dexa”) scan looks at the mineral content of your bones to help providers determine if you have osteopenia or osteoporosis.
It’s important to know if you have weak bones in case of a fall.
“What’s a simple fall as a toddler is more complicated event as you get older,” said geriatrician
Imaging offers providers a glimpse inside our bodies without opening up the skin. But what are the differences among the various types of exams?
Efficient and painless, X-rays are typically used to get a good look at the bones and soft tissues. Patients may lie, stand or sit near the equipment for about 15 minutes. Because radiation is used, providers will not be present in the room. Repeated exposure such as X-raying patients daily could cumulatively endanger providers. The patient may wear a lead covering to protect areas that do not need to be X-rayed, such as the apron available at dentist’s offices. Typically, X-rays focus on the area in question. Providers note X-rays in their patients’ charts to ensure that they do not receive unnecessary X-rays. Any imaging involving X-rays is not recommended for pregnant women.
A computer uses numerous X-ray images to create a 3D style image with the CT scan. Providers can look at bones, soft tissues, tumors and clots. Some of these procedures
Sharon Brangman. “It can result in life-changing injuries.”
She added that a broken spine or hip contributes to deconditioning and loss of independence in many older adults. Among older adults who experience a broken hip, more than 20% die within a year because of complications from the injury.
Brangman serves on the faculty at SUNY Upstate Medical University and is a distinguished service professor, chairwoman of geriatric medicine and director of the Upstate Center of Excellence for Alzheimer’s Disease.
Using low level radiation, the
DXA typically scans the spine and pelvic area, which are common areas for bone breaks in older adults. But other populations may want to ask their providers about a DXA as well.
Physician Carole Peterson, who provides women’s healthcare at URMC’s Perinton Medical Center, said that the risk factors include being a small-framed, post-menopausal woman; celiac disease; being a man over age 65; decreased bone density from medications; anorexia, wheelchair use; family history of bone breaks and metabolic disease. Other factors could include some autoimmune diseases; tobacco use;
By Deborah Jeanne Sergeant
require patients to have a contrasting dye in their system, either through an IV or by drinking it. Patients lie on a table in a room separated from the technician. The table slides into a large tube and then the X-ray equipment moves around the patient. The whole process takes about 15 minutes. Like standard X-rays, providers are not in the room to prevent cumulative radiation damage.
MRIs use magnets, radio waves and a computer to take a look at organs and soft tissues. Similar to CT scans, patients lie on a table that moves into the MRI equipment, which can be noisy at times. The scan can take up to an hour to complete. Providers can use MRIs to diagnose conditions such as aneurysms, multiple sclerosis, strokes, spinal cord
more than three servings of alcohol daily; vitamin D deficiency; and use of certain medications. These include corticosteroids, some kinds of cancer medication, some types of immunosuppressants, hormone suppressants, some types of seizure medications, proton pump inhibitors that treat acid reflux and GERD, and heparin, a blood thinner.
“It’s important to have the scan,” Peterson said. “There are 200 million in the US who have osteoporosis, and a significant number will have a fracture. People who fracture the spine or hip, their fatality rate is 20% in the next year. They may lose independence. As we age, we lose bone. DEXA is an intervention.”
The scan doesn’t treat fragile bones, however, it can give providers and patients and idea of whether the bones are at risk for fracture and what steps they can take to reduce that risk.
The scan takes mere minutes and is painless. Patients may eat and drink normally but are asked to forgo any calcium supplements for 24 hours before the test. Pregnant women should not receive a DXA scan. Patients must also wear loose, comfortable clothing without metal trim or closures like zippers or buckles.
According to the Cleveland Clinic, the best ways to strengthen your bones are:
Exercising more often: Regular physical activity strengthens your bones. Walking, yoga and strength training are great ways to stay active and prevent bone loss.
Supplements or eating specific foods: Your provider might suggest that you take a vitamin D or calcium supplement to support your bone health. You might need to eat more foods high in certain vitamins and minerals.
Medication: Your provider might prescribe medications that help slow down bone loss and prevent fractures. Some medications for osteoporosis may help build your bone density.
sound to detect fetal development in pregnant women. The technician lubricates the skin with gel and uses a handheld probe against the skin with firm pressure. Ultrasound procedures can take 30 to 60 minutes, depending upon the reason for the ultrasound, which can include diagnosing a plethora of diseases, blood flow problems, genital issues, tumors and more. Ultrasound can also help guide providers taking a biopsy.
problems, tumors and injuries to the joints or tendons.
To watch movement inside the body in real time, providers may use fluoroscopy. This type of imaging uses pulses of X-ray beams along with dye to help diagnose heart or intestinal diseases, guide surgery or injections or in orthopedics. Regular X-rays are like still photos, but fluoroscopy is more like videography. Providers can look in organs, joints, muscles and bones.
As the name denotes, ultrasound uses sound waves to develop images (sonograms) of organs within the body. It’s commonplace to use ultra-
PET scans (positron emission tomography) use a safe, radioactive tracer to help providers find diseased cells, typically for cancer, heart disease and conditions affecting the brain. Like the CT scan, the patient lies on a table that passes into the examination equipment. The radiotracer helps create images of the diseased cells because they absorb larger amounts of the material than healthy cells. The scan can take up to two hours. Some providers may use both the PET and MRI at the same time to make high contrast images, typically for tracking cancers in soft tissue areas.

oil options abound, but which is best?
By Deborah Jeanne Sergeant
Grocery stores offer olive oil, canola oil, sunflower oil and many more.
But which is best for heart health?
In general, the oil types are divided into olive oil — oil that is pressed from olives — and “seed oils,” those extracted and processed from seeds, such as rapeseed (canola) and sunflower seeds, and other plants like soybeans and peanuts.
Olive oil and canola are the top two oils.
“As far as oils, olive oil is definitely the best choice for heart health,” said Kelly Springer, registered dietitian and owner of Kelly’s Choice in Skaneateles. “It is composed of monounsaturated fats (MUFAs), primarily oleic acid.”
She explained that these fats have been shown to lower levels of LDL “bad” cholesterol, which can lower the risk of plaque buildup in arteries as well as raise HDL “good” cholesterol, which helps clear excess cholesterol from the bloodstream.
In addition, extra virgin olive oil (EVOO) also contains polyphenols. Springer said that these plant compounds offer “powerful anti-inflammatory and antioxidant properties. These compounds help reduce oxidative stress, a key contributor to heart disease and protect against endothelial dysfunction, which can lead to arterial stiffness and atherosclerosis.”
EVOO does have a few drawbacks. Its low smoke point means that it’s hard to cook with EVOO at high temperatures. It also tends to lend a distinctive flavor that doesn’t go with some uses. But its robust flavor complements Mediterranean-inspired dishes and for dips and salad dressings. Avoid using EVOO to stir fry vegetables at high temperatures. For use in higher heat, refined olive oil but realize that it contains less of the beneficial properties of EVOO.
About canola oil, Springer said that “particularly refined varieties, has minimal antioxidant content and lacks the bioactive compounds found in EVOO.
“Canola oil, while also containing MUFAs has a higher proportion of omega-6 fatty acids. Excessive omega-6 intake relative to omega-3s may contribute to inflammation, which is a risk factor for cardiovascular disease.”
Laurel Sterling, registered dietitian, nutritionist and national educator for Carlson Laboratories in Canastota, lauded olive oil’s omega-9 oleic acid and polyphenols because of their antioxidants.
“Antioxidants help protect the cells in your body from free radical damage,” Sterling said.
“Free radicals can cause your cells to oxidize and as a result perform poorly.”
EVOO is a good source of polyphenols, along with tea, chocolate, fruits and vegetables. Sterling noted that like other antioxidants, polyphenols promote healthy inflammation balance.
Canola oil offers a neutral flavor and higher smoke point, meaning it can be used in a greater variety of ways than olive oil. Compared with canola, olive oil is more expensive. But canola oil has a few drawbacks.
“To be clear, there are ‘healthy’ omega-6s and ‘unhealthy’ omega-6s,” Sterling said. “Unfortunately, in modern day society, people in America consume far too many of the unhealthy omega-6s which are major contributors to increased inflammation levels in our bodies.
“These unhealthy omega-6s sources typically come from convenience foods and fast-food. They typically include corn, canola, soy and cottonseed oils. The preferred omega-6 choices would be flaxseed, hempseed, sunflower, pumpkin seed, borage oil, evening primrose oil and black currant seed oil.”
For a healthy heart, it’s also important to incorporate aerobic activity and strength training into one’s routine and to mitigate stress.


Seniors’ risk of dementia is more than double what was previously thought.
The risk of developing dementia after age 55 is more than 42% among Americans, researchers reported in a study published Jan. 13 in the journal Nature Medicine.
That’s more than twice the risk reported by older studies.
“Our study results forecast a dramatic rise in the burden from dementia in the United States over the coming decades, with one in two Americans expected to experience cognitive difficulties after age 55,” said senior investigator and physician Josef Coresh, founding director of the Optimal Aging Institute at NYU Langone Health.
That dementia risk translates into an estimated half-million cases this year — and will increase to 1 million new cases annually by 2060, researchers stated.
This increase is directly tied to the aging of the U.S. population, along with a better understanding of other factors related to dementia — genetics, high blood pressure, diabetes, obesity, unhealthy diet, lack of exercise and poor mental health.
For the study, researchers exam-
ined data from an ongoing study that has tracked heart health and brain function among nearly 16,000 participants as they age.
Between 1987 and 2020, more than 3,200 participants were diagnosed with dementia, researchers said.
That translates to an overall lifetime dementia risk of 42% — 35% for
men and 48% for women.
Women live longer than men on average and thus are more likely to develop dementia during their lifetimes, researchers said.
Further, the lifetime risk of dementia increases to more than 50% for people older than 75.
Results also showed a higher risk among Black people, as well as in those who carry a mutation of the APOE4 gene that’s been previously linked to Alzheimer’s disease risk.
The APOE4 mutation is considered the single biggest genetic risk factor for developing
late-onset Alzheimer’s, researchers noted.
These findings place added emphasis on the need for policies aimed at preventing dementia.
“The pending population boom in dementia cases poses significant challenges for health policymakers, in particular, who must refocus their efforts on strategies to minimize the severity of dementia cases, as well as plans to provide more health care services for those with dementia,” Coresh said.
For example, previous studies have shown that preventing heart disease and diabetes should also slow brain decline.
Loss of hearing among seniors has also been linked to an increased risk of dementia, researchers added. However, only a third of Americans with hearing loss use hearing aids.
More monitoring of hearing loss, and programs to make hearing aids more widely available, could help stem the coming tide of dementia, Coresh said.
Resources also are needed to address racial inequities in health care.
While dementia is expected to double among white people during the next four decades, it’s expected to triple among Black seniors, Coresh concluded. Efforts to improve childhood education and nutrition in Black communities now could stave off cognitive decline later.


By Deborah Jeanne Sergeant
Born between 1946 and 1964, the oldest members of the baby boomer generation will turn 80 in 2026.
Does the CNY area have sufficient resources available to meet their needs in older age?
Geriatrician Sharon Brangman, on the faculty at SUNY Upstate Medical University and a distinguished service professor, discussed what is available in CNY and what is still lacking.
“The biggest issue is transportation,” said Brangman, who is also chairwoman of geriatric medicine and director of the Upstate Center of Excellence for Alzheimer’s Disease. “We’re still a community where the single private car is the main source of transportation. It’s important for getting to doctor appointments, pharmacies and socializing. We don’t have that infrastructure support for public transportation.”
Poor vision, slower reflexes and limited range of motion mean giving up the keys. However, older adults still need to get to doctor’s appointments, social engagements and the grocery store. Riding a bus can make













running an errand take all day, as riders must wait for others to board and get off the bus at each stop. Bus and taxi services typically do not offer any help with packages or stepping on and off the bus. And bus routes do not go to every location a person may want to go.
Ride share services can help provide transportation. However, “most older adults don’t have a smart phone, so they don’t use ride share apps,” Brangman said. “Some will have their adult children order it for them, but they feel like a burden because they’re bothering their kids.”
Some older adults continue to drive even if they are no longer safe driving because they have no other convenient means of transportation — not a good option, considering their higher rate of death and injury should they be involved in a car crash. According to the Centers for Disease Control and Prevention, drivers aged 70 and older have a higher crash death rate than those aged 35 to 54.
Services like GoGoGrandparent.com function like a concierge, helping people link with ride sharing














and food delivery. A live operator takes the call and summons help for a convenience fee, plus the cost of the service.
As people age, they tend to rely upon healthcare resources more than they did when they were younger. Considering the healthcare worker shortage exacerbated by the pandemic — when 20% of healthcare workers quit the industry — the incoming flux of older adults needing more healthcare resources may overwhelm the system.
Another way in which technology can help is telehealth, which can reduce staffing woes for healthcare providers. Telehealth is one example of ways that the healthcare system can reduce urgent care and emergency department visits. Many providers are turning to automated systems to facilitate visit reminders and prompt prescription filling. Although some older people resist using technology for telehealth, as younger Boomers age, this won’t be as big of a problem. People who retired 30 to 40 years ago were likely using technology in their day-to-day work lives.


































Living in an assisted living community helps with transportation and with other types of assistance. However, not everyone wants to live in or can afford assisted living.
Aging in place at home appeals to most older adults. However, Brangman said it’s “not always feasible because of repairs that are needed and there are so few home health aides. A study showed that one of the main reasons that older adults can stay in their home is a good handyman to help when things break.”
It can also help to prepare for older age. For example, “automating” tasks such hiring a lawn care and snow removal company can prevent injury from these activities. Scheduling regular delivery of groceries and supplies can make shopping simpler. Signing up for automatic payments ensures these bills won’t be skipped.
“Get services that augment support for people to stay in their own homes, like service jobs, homecare, handyman services and food delivery,” Brangman said.


Age, family genetics and gender make it nearly impossible for older adults to avoid becoming a chronic disease statistic.
According to NCOA research, 94.9% of adults aged 60 and older have at least one condition, while 78.7% have two or more.
You probably have a parent or grandparent who is managing a condition right now or perhaps you are managing one yourself.
And obesity, which impacts about 42% of adults 60 and older, can increase your risk for conditions like heart disease, Type 2 diabetes, and some cancers.
With these kinds of odds, you might wonder if there is anything you can do to prevent the onset of a chronic medical condition or make managing an existing one easier. The answer is yes.
Here are 10 common chronic conditions adults 65-plus on Medicare were treated for in 2018, and what you should know about each.
Nearly 12% of older adults on Medicare were treated for Alzheimer’s disease or another form of dementia. Alzheimer’s disease is one specific type of dementia — a condition that causes memory loss and difficulty thinking or problem-solving to the point that it interferes with every day activities. Dementia is not a normal part of aging and is caused by changes in the brain over time.
The biggest risk factors for these chronic conditions are things you often can't control, including age, family history and genetics. But studies have suggested incorporating the following habits into your lifestyle could slow or prevent onset:
• Exercise. Staying active isn't just good for your heart; it's also great for your brain.
• Sleep. Your brain does important stuff while you are sleeping, so getting at least seven hours of deep sleep a night is crucial. Upgrading to the best mattress for you could help.
• Be smart about your diet. Research suggests that some foods can negatively affect your brain.
Sixteen percent of older adults sought treatment for depression — a treatable medical condition that is not a normal part of aging. Depression causes persistent feelings of sadness, pessimism, hopelessness, fatigue, difficulty making decisions, changes in appetite, a loss of interest in activities and more.
Steps you can take to help with depression include:
• Manage stress levels. Reach out to family and friends during rough spells and consider regular meditation.
• Eat a healthy diet. What you put into your body can affect your mood, so focus on foods that are high in nutrients and promote the release of endorphins and those "feel good" chemicals, and limit consumption of things like alcohol, caffeine, artificial sweeteners, and highly processed foods.
• Routine exercise. Exercise has a number of physical and psychological benefits, including improving your mood through the release of endorphins and other "feel good" brain chemicals, boosting self-confidence and self-worth through meeting goals and improving your physical appearance, and increased socialization through interactions at gyms and group classes.
• Talk to your doctor. If you've ex-
Nearly 95% of adults 60 and older have at least one chronic condition, while nearly 80% have two or more.
perienced any of the warning signs of depression, talk to your doctor, and ask about your treatment options. Antidepressant medications or psychotherapy could be right for you.
If you’re in severe emotional distress, one of the first things you should do is tell someone else about it — such as a trusted friend or family member. You can also dial or text 988 from your phone to speak with a counselor who is specially trained in suicide prevention. The 988 service is free, confidential, and available to everyone in the United States 24 hours a day, seven days a week.
About 5% of older adults were treated for heart failure — a condition that occurs when the heart cannot adequately supply blood and oxygen to all of the organs in the body. The heart might become enlarged, develop more muscle mass or pump faster in order to meet the body’s needs, causing you to feel tired, light headed, nauseous, confused, or lack an appetite.
Steps you can take to prevent or diminish symptoms of heart failure:
• The best prevention is to follow a doctor's recommendations to decrease your risk for coronary heart disease and high blood pressure.
Nearly 25% of older adults were treated for chronic kidney disease (CKD) or a slow loss in kidney function over time. People dealing with CKD have an increased risk for developing heart disease or kidney failure.
Steps you can take to prevent or diminish symptoms of CKD:
• Understand what damages your
kidney. Diabetes and high blood pressure are the greatest risk factors for kidney damage, so taking steps to prevent these diseases is your best strategy.
• Early detection and treatment. Talk to your doctor regularly, stay current on screenings, and keep up on prescriptions you need to diminish symptoms.
Twenty-seven percent of older adults were treated for diabetes — a disease that occurs when your body is resistant to (or doesn’t produce enough) insulin. Insulin is what your body uses to get energy from food and distributes it to your cells. When this doesn’t happen, you get high blood sugar, which can lead to complications such as kidney disease, heart disease, or blindness. Chances of having diabetes increases after age 45.
Steps you can take to keep you from developing diabetes or to manage this condition:
• Eating a healthy diet, including monitoring your carbohydrate and calorie intake, and talking to your doctor about alcohol consumption.
• Exercising for 30 minutes five times a week to keep your blood glucose levels in check, and to control weight gain.
• Safely losing 5-7% of body weight if you are diagnosed with pre-diabetes.
Nearly 29% of older adults were treated for ischemic heart disease — a condition that is caused by a build-up of plaque that narrows the arteries leading to the heart. Narrow

or blocked arteries decreases the amount of oxygen-rich blood delivered to the heart. This can cause other complications like blood clots, angina or a heart attack.
Steps you can incorporate to help if you have ischemic heart disease:
• Avoid saturated and trans fats, and limit sugar and salt intake
• Get seven to eight hours of sleep each night
• Keep your stress levels in check
• Do regular cardio exercises
• Abstain from smoking
• Talk to your doctor about the major risk factors, including high cholesterol and high blood pressure
About 35% of older adults were treated for arthritis — an inflammation of your joints, which causes pain and stiffness and is more common in women.
Steps you can take to delay the onset of arthritis or manage the symptoms:
• Exercise at least five times per week, for 30 minutes each time, to improve function and decrease pain. Try to include a mixture of aerobic, strength-building, and stretching movements.
• Stay within the recommended weight for your height — losing one pound can remove four pounds of pressure on your knees.
• Make sure your back, legs and arms are always supported.
• Take precautions to avoid joint injuries.
• Do not smoke.
About 40% of adults 65 and older are living with obesity, a chronic disease linked to more than 200 chronic conditions. The National Council on Aging (NOAA) is pressing to define quality obesity care as a universal right. That includes the right to coverage for treatment with access to the full range of treatment options.
Tips for addressing obesity include:
• Understanding what obesity treatments are covered by Medicare
• Empowering yourself with knowledge about nutrition
• Educating others and being your own advocate
More than 50% of older adults were treated for high cholesterol — a condition that occurs when your body has an excess of bad fats (or lipids), resulting in your arteries getting clogged, which can lead to heart disease.
Steps you can take to prevent or manage high cholesterol:
• Abstain from smoking and
Another common chronic conditions for adults over 65 is chronic obstructive pulmonary disease (COPD), which includes two main conditions: emphysema and chronic bronchitis. COPD makes it hard to breathe and causes shortness of breath, coughing, and chest tightness.
Steps you can take to manage COPD include:
• The best way to prevent COPD — or slow its progression — is to quit or avoid smoking. Also try to avoid secondhand smoke, chemical fumes and dust, which can irritate your lungs.
• If you already have COPD, complete the treatments that your doctor has prescribed, get the flu and pneumonia vaccines as recommended by your doctor, and continue to remain active.
This article was published in May 2024 on the website of the National Council on Aging (NOAA), www.ncoa.org.
excessive alcohol consumption
• Be active each day
• Manage your weight
• Minimize saturated fats and trans fats in your diet
blood pressure)
Nearly 60% of older adults were treated for hypertension — a common condition that involves both how much blood your heart pumps, as well as how resistant your arteries are to the blood flow. When your heart pumps a lot of blood, and you have narrow arteries which resist the flow, that’s when you get high blood pressure, also known as hypertension. The danger of hypertension is not only that you can have it for years and not know it, but it can cause other serious health conditions, like stroke and heart attacks.
Steps you can take to prevent or reduce high blood pressure:
• Maintain a healthy weight. Losing just 10 pounds can reduce blood pressure
• Regulate your stress levels
• Limit salt and alcohol consumption
• Exercise daily, including a combination of moderate to vigorous-intensity aerobic activities, flexibility and stretching, and muscle strengthening
• Check your blood pressure regularly—the quicker you catch pre-hypertension, the more likely you are to prevent high blood pressure
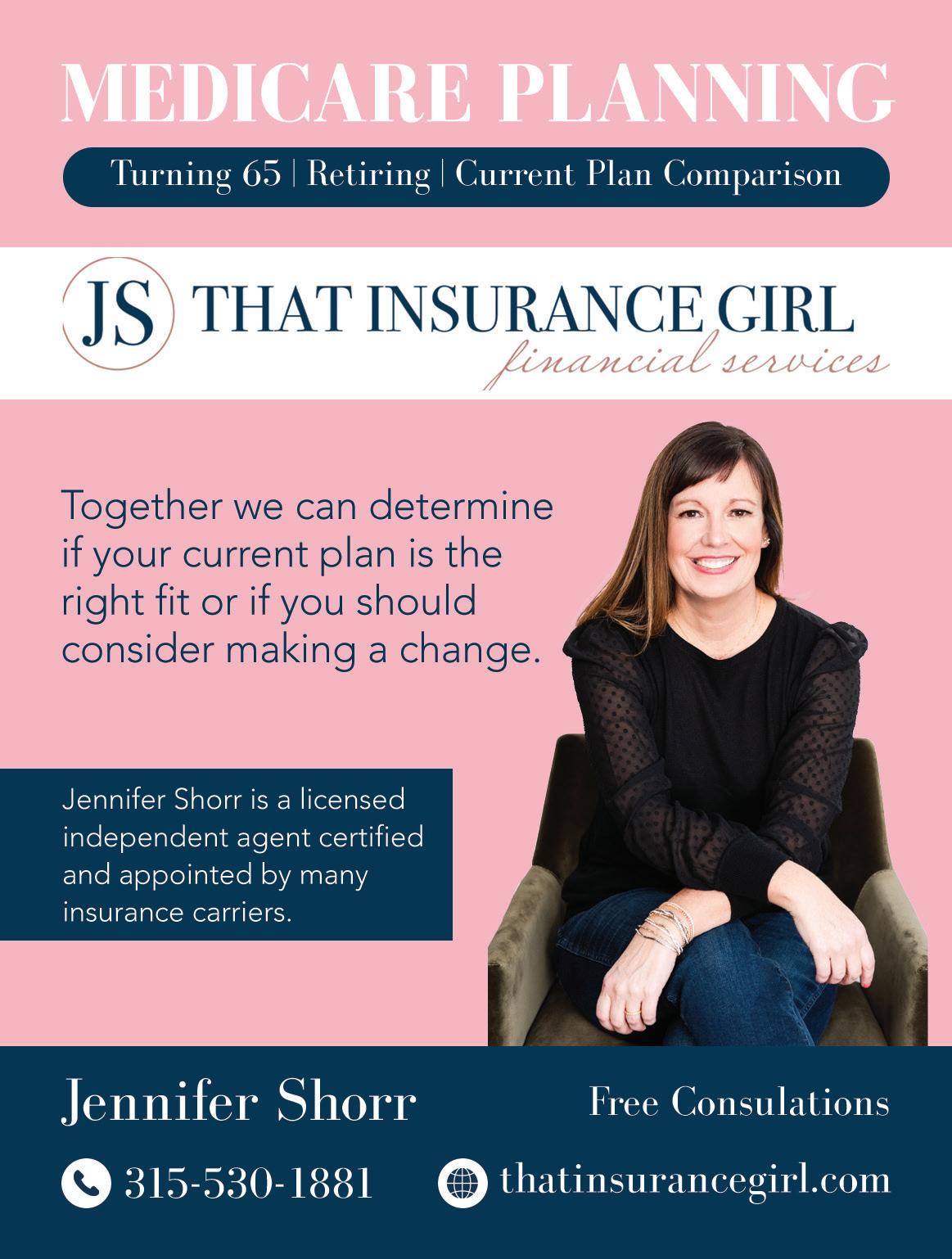

CDC: More than 14 million older people (25%) report falling — it has become the top cause of injury-related death for people over 65
By Deborah Jeanne Sergeant
The Centers for Disease Control and Prevention reports that falls are the top cause of injury-related death for people 65 and older. Falls in this age cohort are common.
The CDC states that more than 14 million older people (25%) report falling — and that does not include those who fall but do not report it.
“The age-adjusted fall death rate increased by 41% from 55.3 per 100,000 older adults in 2012 to 78.0 per 100,000 older adults in 2021,” the CDC states.
But why are falls so harmful to older adults?
“As we get older, we have less reserve. Its physiological reserve, the cushion to draw upon when our body is stressed,” said geriatrician Sharon Brangman. “As you get older, that cushion gets thinner and thinner so even a small incident like a fall is a bigger impact. The minute we start to limit mobility it leads to lower bone mass and muscle mass. You get weaker.”
Brangman serves on the faculty at SUNY Upstate Medical University and is a distinguished service professor, the chairwoman of geriatric medicine and the director of the Upstate Center of Excellence for Alzheimer’s Disease.
“As we get older, the bones are often thinner and more brittle,” Brangman added. “You’re more likely to have a fracture with a fall.”
After a fall, many frail older adults do not regain the same level of vitality as they had before, even if they did not experience a bone break. Beyond the pain experienced during a fall, the consequences of falling can be severe for older adults as their bodies decondition while they’re laid up. Preventing falls can help avoid these outcomes.
The reasons for falling are complex.
“Part of it is the natural changes as we get older put us at risk for falls and make us more vulnerable for a bad outcome if we fall,” Brangman said.
Many older adults have a harder time lifting their feet high enough. Their vision may be dimmer and their reaction time is slower. Instead of catching themselves before falling, they respond too slowly and fall.
“Generalized weakness, especially core muscles that keep us erect and help with balance, those muscles get weaker with age and you need to do specific exercises,” Brangman said. “It’s the same with leg muscles. A lot of people who fall have a fear of falling and move less and that increases their chance of falling because their muscles are weaker, shorter and tighter.”
In addition, many older people experience momentary dizziness upon rising as the blood vessels going to the head constrict. Some older people take medication that worsens
By Jim Miller
Excessive amounts of earwax can cause problems in elderly seniors including hearing loss or ringing in the ears.
Some people experience vertigo, which increases the risk of falling. And there’s also a correlation between hearing loss and cognitive decline and depression.
Earwax — which is not really wax at all, but a substance called cerumen that binds with dirt, dust and debris — is normally produced by the body as a way to clean and protect the ears. In most people, the self-cleaning process works fine. But in others, including more than 30% of elderly people, the wax collects to the point where it can completely block
or impact the ear canal.
Those that are most affected are elderly seniors, especially those living in nursing homes or assisted living centers that provide substandard hygiene. And those highest at risk are hearing-aid users because the devices push wax down into the canal.
Earwax Removal
Usually, earwax moves up and out on its own so the best way to control it is to leave it alone. But that advice can backfire for those who accumulate excessive amounts of earwax.
The symptoms of an earwax problem can include an earache, a
this effect.
How people move can make a difference in whether or not they fall. For example, shuffling may seem like a safer way to walk. However, since it reduces their base of support, they’re more likely to be unable to catch themselves if they stumble. A longer, more natural stride is safer.
Becoming less active to prevent falls is counterproductive, according to Maureen Loyal, physical therapist and director of rehabilitation and physical therapy with Finger Lakes Health.
“Fear of falling has you do less outside the home,” she said. “You become deconditioned and it’s a cycle. Do the opposite of what people do, which is confine themselves to their homes and have people do errands for them. People who are older should park farther away so they’re walking more. ‘Use it or lose it’ is important. It’s never too late to have balance exercises.”
She encourages older adults to seek help to improve their endurance, strength, flexibility and balance if they begin to experience instability while walking. Too many people reach for a cane or walker early on when improving their physical condition would prevent that reliance.
Instead of performing random exercise movements, Loyal focuses on functional movement that will help people better carry out activities of daily living like carrying grocery
feeling of fullness in the ear, hearing loss, tinnitus, dizziness, an ear infection, ear itchiness or cough due to pressure from the blockage stimulating a nerve in the ear.
If you or your elderly loved one’s experience any of these symptoms, try using a softening agent to help the wax leave the ear or to remove it more easily.
If you prefer the natural route, try baby oil or mineral oil. Using an eyedropper, apply a drop or two into your ear, tilting your head so that the opening of the ear is pointing up toward the ceiling. Stay in that position for a minute or two to let the fluid flow down to the waxy buildup. Then tilt your head in the opposite direction to let the fluid and wax drain.
Or try an over-the-counter earwax removal solution or kit, which are sold in most pharmacies. Solutions may contain oil or hydrogen peroxide, and some kits include a bulb syringe that you squeeze to flush your ear with warm water,
bags, standing and sitting and climbing stairs.
“We want to keep that function throughout life,” she said, “And you do that by keeping your strength. You may weigh the same, but you can see there’s more fat than muscle. You may think you have the same muscle capacity, but you don’t. I try to focus on functional exercises, not sitting in a chair and kicking your legs up. When do you ever do that movement?
“Do sit-to-stand exercises where you stand and then slowly sit down. If you can keep your quad muscles strong, it decreases risk for falls and keeps you independent in the community.”
The home environment makes an enormous difference. Poor lighting, clutter on the floor, throw rugs, uneven flooring and multi-level living spaces all contribute to a higher risk of falling. Upgrading the bathroom and bedroom — the most fall-prone rooms of the house — can reduce fall risk.
Grab bars by the shower and toilet also assist in stability, as does a bedrail in the bedroom.
Seeing where you’re going helps you stay on your feet. Place nightlights and lamps where they can be turned on upon entering the room. It can also make sense to outsource tasks that involve climbing on ladders or other activities that can cause falls.
if needed.
You may need to repeat this wax-softening and irrigation procedure several times before getting rid of the excess earwax. If, however, the symptoms don’t improve after a few treatments, you need to see an audiologist or ear, nose and throat (ENT) doctor to have the wax removed.
Earwax removal is one of the most common ENT procedures performed. They have a variety of tools that can remove hard, stubborn earwax.
It might be tempting to poke a cotton swab, bobby pin, pencil or finger into your ear to get the gunk out, but don’t go digging. Yes, it’ll remove some of the wax, but it may also push the rest deeper into the ear canal and increase your risk of injuring your eardrum and making the problem worse.
Jim Miller is the author of Savvy Senior, a column that is published in In Good Health every issue.
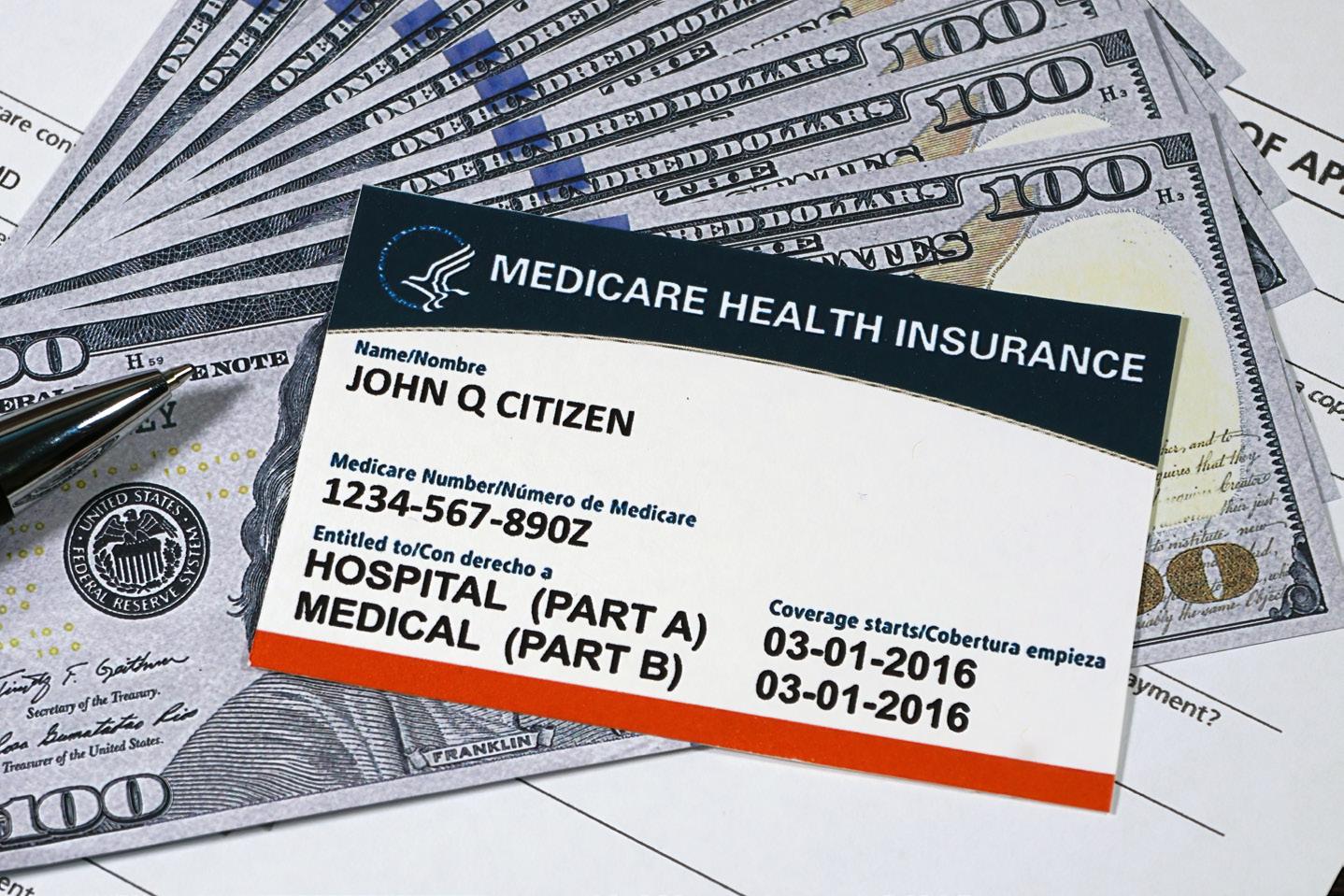
Which are the most overlooked Medicare benefits and how to take advantage of them
By Deborah Jeanne Sergeant
If you have a Medicare plan, chances are you don’t use the benefits as fully as you could.
Anthony Hinds-Fritz, certified financial planner and chartered financial consultant, owns Evolution Retirement Solutions, LLC in Syracuse. He shared a few examples of underused Medicare benefits, most of which emphasize preventive measures for maintaining good health rather than reactive benefits to mitigate health problems.
“Most plans have a gym membership and some offer benefits
for at-home exercise equipment,” Hinds-Fritz said. “That tends to be underutilized.”
Plans include coverage for gym memberships to encourage more cardiovascular activity and strength training, both of which are foundational for maintaining good health. Exercise can help improve fitness, functional movement, balance, flexibility and offer a social outlet.
The plan may dictate where you go and provide a list of covered facilities, but what you do there is up to you. Take a class, swim laps, lift
weights, pedal on an elliptical: it’s up to you.
Hinds-Fritz said that many plans include coverage for emergency response buttons. However, few people take advantage of these. People who feel comfortable summoning help with a cellphone won’t feel the need for the buttons (they’re for “old people.”) By the time someone is cognitively incapable of using a cellphone to call for help, it may be too late to adapt to use a response button either.
Hinds-Fritz said that dental coverage and allowances for eyewear and hearing aids are sometimes overlooked, as people not experiencing any difficulties in their current oral, visual or hearing health may make do. Part of the reason is that some people lack transportation for what they may view as unnecessary visits.
“Some plans even provide a transportation benefit if you need help getting to and from a provider’s office,” Hinds-Fritz noted.
Lack of transportation prevents some older adults from seeking medical care, from routine visits to appointments for treating chronic conditions.
Even those with perfect health can benefit from a baseline exam and following through with regular primary care visits. Many don’t feel the need to visit a doctor if they’re not sick or hurt. But a wellness visit can reveal issues while they are small and likely more readily treatable.
• Depression screening
• Gift card for completing surveys and health-related tasks like flu vaccination
• Cardiovascular risk reduction
• Tobacco cessation programs
• Mental health and substance

abuse services
• Home health care
• Hospice services
• Caregiver support such as respite care and caregiver training
• Chronic disease education
• Meal delivery (typically for a short period after a hospital discharge)
• Housing assistance
“These things do change and sometimes from year to year, you’ll see bigger changes,” Hinds-Fritz said. “It helps to check in with the broker.”
• 65,636,490 people are enrolled in Medicare.
• 7,716,192 people — roughly 11.8% of Medicare beneficiaries — are younger than 65.
• 34,073,277 beneficiaries are enrolled in original Medicare (Part A and Part B).
• 31,563,213 beneficiaries are enrolled in Medicare Advantage (Medicare Part C) or other Medicare health plans.
• 22,576,006 beneficiaries have a standalone Medicare Part D prescription drug plan (PDP).
• 28,816,577 beneficiaries get their Medicare drug coverage through a Medicare Advantage plan.
Source: MedicareAdvantage.com
n Baseline and monitoring testing for chemotherapy and other hearing – harmful medications
n Hearing measurements for personal (medical, communication) or occupational (OSHA, DOT, law enforcement) purposes.
n Hearing protection counseling and devices for loud recreational (music listening, hunting, motor sports, landscaping) and occupational (professional musicians, fire and police personnel) activities.
n Hearing aid selection, fittings and repairs
n Tinnitus evaluations and treatment.
n If you have any questions or concerns regarding your hearing or how to protect it.





By Warren Beck Social Security District Manager in Syracuse.




When your child turns 18 years old, they legally become an adult. This is an important time to consider their financial future, especially if they need additional care into adulthood. Here are five things that may help you prepare for this milestone:

When your child legally becomes an adult, you can no longer make certain decisions for them about their health and welfare. However, you can stay involved through our representative payee program. Social Security will determine who best serves as a representative payee for your child’s benefits. To learn more about the representative payee program, read our webpage at www.ssa.gov/ payee/index.htm. Please note Social Security does not recognize power of attorney.
SSI provides monthly payments to adults and children with disabilities, as well as people 65 and older, who have little or no income and resources.
If your child receives SSI, when they turn 18 we will review their eligibility for continued SSI payments based on the disability rules for adults. For more information, please review the publication, “What You Need To Know About Your Supplemental Security Income (SSI) When You Turn 18” at www.ssa.gov/pubs/ EN-05-11005.pdf. Please be sure to review this with your child. We also encourage you to check out Social Security’s youth toolkit webpage at www.ssa.gov/youth.
If your child attends school, they have a few options to continue their education, such as pursuing:
• A diploma: They may pursue further education in college or trade programs with an individualized education program (IEP). More information on the IEP is available at www.ssa.gov/pubs/EN-64-118.pdf.
• A certificate: They may have the opportunity to continue in a transitional program in their high school even after they complete their senior year. Most are permitted to remain until they turn 22.
• Employment: Local vocation-
al rehabilitation services can assist with employment options during pre-graduation IEP meetings.
Once your child turns 18, they may choose or qualify for different living arrangements depending on the services they already receive. If your child receives therapy services at school, how will they receive them once they leave? They could receive them through a Medicaid waiver or private insurance.
Qualification for respite services may also look different. Respite services allow family caregivers time to step away from their duties. It is essential you understand all the benefits and options available to your child after they complete high school and before deciding on living arrangements and services.
• Special needs trust: Update estate planning documents before your child turns 18. Otherwise, inheritance may terminate your child’s governmental benefits.
• ABLE account: You can deposit funds into this account up to a certain limit each year. However, there are limits on what its funding covers. More information on ABLE accounts is available at www.ssa.gov/payee/ able_accounts.htm.
The above is informational only and does not constitute financial advice or an endorsement of ABLE products or ABLE organizations by the Social Security Administration. There may be other financial options that could be a better fit for some individuals. You must use your best judgement to determine which option is best for your situation.
Children receiving benefits on a parent’s record may continue to receive those benefits until age 19 if they’re a full-time elementary or secondary school student. People who have a disability that began before age 22 may also be eligible to receive child’s benefits at any age. For more information, please review the publication, “Benefits for Children” at www.ssa.gov/pubs/EN-05-10085. pdf. As your child enters adulthood, consider these issues while you navigate their financial future.
Please share this information with your friends and loved ones who may need it.
By Jim Miller

Dear Savvy Senior,
What types of mental health services does Medicare cover? I struggle with anxiety and depression, and my primary care provider recommended I see a therapist or psychiatrist.
Anxious Annie
Dear Annie,
Medicare actually covers both outpatient and inpatient mental health care services and programs to help beneficiaries with anxiety, depression and many other mental health needs. Here what you should know.
If you’re enrolled in original Medicare, your Part B coverage will pay 80% (after you’ve met your annual $257 Part B deductible) for a variety of counseling and mental health care services that are provided outside a hospital, such as in a doctor or therapist’s office, hospital outpatient department or community health center. These services can also be received via telehealth.
You or your Medicare supplemental (Medigap) policy is responsible for the remaining 20% coinsurance.
Medicare also gives you the expanded option of getting treat-
ment through a variety of health professionals such as psychiatrists, psychologists, clinical nurse specialists, clinical social workers, nurse practitioners, physician assistants, marriage and family therapists and mental health counselors.
To get this coverage, you’ll need to choose a participating provider that accepts Medicare assignment, which means they accept Medicare’s approved amount as full payment for a service.
If you choose a nonparticipating provider who accepts Medicare but does not agree to Medicare’s payment rate, you may have to pay more. And if you choose an opt-out provider that does not accept Medicare payments at all, you will be responsible for the entire cost.
To locate a mental health care professional in your area that accepts Medicare, go to “Medicare.gov/ care-compare,” click on “doctors & clinicians” and type in your location, followed by “clinical psychologist” or “psychiatry” in the “Name & Keyword” box. You can also get this information by calling Medicare at 800-633-4227.
If you happen to need mental health services in either a general or psychiatric hospital, original Medicare Part A covers this too, after you’ve met your $1,676 Part A deductible. Your doctor should determine which hospital setting you need. If you receive care in a psychiatric hospital, Medicare covers up to 190 days of inpatient care for your lifetime. And if you use your lifetime days but need additional care, Medicare may cover additional inpatient
care at a general hospital.
In addition to the outpatient and inpatient mental health services, Medicare also covers yearly depression screenings that must be done in a primary care doctor’s office or clinic. Annual depression screenings are covered 100 percent. And if you have a Medicare prescription drug plan, most medications used to treat mental health conditions are covered too.
If you get your Medicare benefits through a private Medicare Advantage plan, they too provide the same coverage as original Medicare does, but may impose different rules and will likely require you to see an in-network provider. You’ll need to contact your plan directly for details.
For more information, call Medicare at 800-633-4227 and request a copy of publication #10184 “Medicare & Your Mental Health Benefits,” or you can read it online at Medicare. gov.

Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.

Excellus BlueCross BlueShield recently announced the recipients of its Health Equity Innovation Awards, designed to support community programs and services that focus on combating racial and ethnic health disparities across Upstate New York.
Last fall, Excellus BCBS called on organizations to apply for grants that would fund initiatives, programs and research that confront the fundamental causes of health inequities, with an emphasis on the impact of structural racism. The health plan hopes the awards will help to enhance the physical and mental health of our communities, reduce social disparities in health care, and promote equitable access to health services.
The funding, which totals more than $500,000, will benefit 19 nonprofit 501(c)(3) organizations in the Central New York/Southern Tier, Rochester, and Utica/North Country regions.
From an application pool of nearly 300 submissions, recipients were selected based on their well-defined objectives and quantifiable results aimed at diminishing health disparities and advancing health equity.
In the Central New York/Southern Tier region, Excellus BCBS Health Equity Innovation Award funding will support the following initiatives:
• Cayuga County Community Health
Network, Inc.: Program will support the training of doulas, create opportunities for them to become Medicaid-certified providers and provide referrals to doulas for birthing individuals, increasing access to maternal health care for birthing individuals in Cayuga County.
• Cortland Area Communities That Care Coalition, Inc.: Program will support daytime spaces for individuals experiencing housing insecurity. The space will provide access to critical support services, including meals and hygiene facilities and connect participants to essential health-related services.
• Crouse Health Foundation: Program will support integrating community-based doulas into Crouse Health’s care team, creating a more inclusive and supportive environment that respects expectant families’ diverse needs and experiences. The project will emphasize collaboration and communication between health care providers and doulas to improve patient satisfaction, support safe pregnancies and childbirth, eliminate pregnancy-related health disparities, and improve health outcomes for new mothers and babies.
• Farnham Family Services: Program will support the Recovery Engagement and Access Coordinator for Health (REACH) team, consisting of a care coordination specialist,

vocational counselor, certified re covery peer advocate and counselor assistance, to focus on the social and economic factors that impact individuals’ health and well-being across their lifespan.
• Hopeprint, Inc.: Program will encourage community members to utilize a network of neighborhood spaces for community-based education and resources focused on maternal and mental health. This includes a non medical clinic that acts as a trusted hub for assistance in accessing maternal mental health and social determinants of health services.
• SAGE Upstate: Program will support the Take Care Together initiative to reduce health disparities by countering isolation. The initiative will engage over 50 participants in weekly social, fitness and health education activities and record their experiences to gain an understanding of the impact of social connection.
• Syracuse Community Health Center: Program will support a mental health early intervention program designed to help pregnant and postpartum women navigate the physical and emotional changes experienced during pregnancy. A psychiatric nurse practitioner will use a combination of evidence-based therapies delivered via individualized and monthly group sessions. The program will also provide educational
• Broome County Council of Churches: Program will tackle food insecurities by funding a mobile grocery bus that delivers access to food in underserved areas of Broome County.
• CareFirstNY: Program will address the need to support behavioral and mental health in the community by providing specialized support for those coping with loss and other grief-related matters for children and adults.
• Economic Opportunity Program: The Empowerment program will address known needs of women and girls in Chemung County by helping to meet the physical needs of women of in emergency situations.
• Family Service Society: Program will provide free behavioral health screenings to address the need to support behavioral and mental health in local youth.
• Meals on Wheels of Chemung County: Program will establish a cafe to address hunger and food insecurity in the community, by providing free meals-to-go with a focus on helping the elderly population.
For the latest information on Excellus BCBS’s community investments and partnerships, visit ExcellusBCBS.com/community.






If you're over 40 and raise your levels of exercise to that of the top 25% of your peers, you might gain an average of five more years of life, a new study calculates.
For over-40 folks in the lowest level of daily activity, a similar move could bring an average 11 extra years, the same report found.
The study results surprised even its Australian authors.
“Our findings suggest that [physical activity] provides substantially larger health benefits than previously thought,” wrote a team led by Lennert Veerman. He's a professor public health at Griffith University School of Medicine and Dentistry in Gold Coast, Queensland.
The new study focused on U.S. data: Information on daily physical activity gleaned from "activity trackers" worn by participants aged 40 and above in 2003 to 2006 federal health surveys; and data on U.S. deaths from 2017

and 2019, also recorded in federal databanks.
Veerman's team calculated that daily levels of physical activity (in whatever form) that placed people in the top 25% in terms of fitness was equal to about 2 hours and 40 minutes of normal-paced (3 miles per hour) walking.
The researchers calculated that if everyone over 40 suddenly matched this activity level, it would raise everyone's expected life span by five years — from the 78.6 years it's now estimated to be to nearly 84 years.
Of course that leap in fitness would be tougher for some than others. The Australian team said that moving folks in the lowest 25% up to the highest 25% would mean the equivalent of an extra 111 minutes of normal-paced walking daily.
There'd be a huge health payoff, though: Almost 11 extra years of expected life for this group, the team said.
Among this group as well, the researchers estimated that each extra hour spent walking each day would translate to an extra six hours of lifespan.
Vreeman's team stressed that the study couldn't prove cause and effect, only that extra physical activity seemed associated with living longer.
The findings were published Nov. 14 in the British Journal Of Sports Medicine.


Cover — Hockey hall of famer — Syracuse Crunch owner Howard Dolgon scores a goaaal! with team and community.
Volunteering — Retirees give back to the community.
Books — Book Buddies: Group puts the fun back into reading.
TheVoice — The man behind the voice: Dave Allen, host of ‘Syracuse’s Morning News with Dave Allen.’ Aging in Place — The overlooked downsides of aging in place.
Investing — Nest egg: Think hard before you raise your risk. Living — Senior community? What’s in it for you?
Turning 70 — So this is 70! Self-care, family connections, meaningful work and pursuing my passions all help set a course through this decade.
Dreams — Jesse Kline, acting director of the Auburn Downtown Business Improvement District, makes an impression.




Say hello to a convenient way to stay healthy in Oswego County. ConnnextCare offers a comprehensive set of services - family and internal medicine, pediatrics, dentistry, psychiatry, substance use disorder treatment and social work all under one medical group. Patients within our network can visit any of our seven locations at any time.
ConnextCare also offers medical, dental and mental health services at nine School Based Health Centers in five Oswego County school districts.
WALK-IN APPOINTMENTS NOW AVAILABLE IN THE PULASKI ACUTE CARE SUITE
MONDAY - FRIDAY 7:00AM - 6:00PM
ACCEPTING NEW PATIENTS AT ALL SCHOOL BASED HEALTH CENTERS! SCAN THE QR CODE FOR ENROLLMENT FORMS!