






Americans have the worst health care among the world’s wealthy nations, a new report says.
People in the United States die the earliest and live the sickest lives out of 10 developed countries, even though the United States spends the most on health care, according to the annual report by health care thinktank The Commonwealth Fund.
Australia, the Netherlands and the United Kingdom rank highest out of the 10 countries included in “Mirror, Mirror 2024: A Portrait of the Failing U.S. Health System.”
“While other nations have successfully met their populations’ health needs, the U.S. health system continues to lag significantly,” said Reginald Williams II, vice president of international health policy and practice innovations with The Commonwealth Fund.
For the report, researchers compared nations’ health systems based on 70 specific measures across five

areas of performance. Other nations measured against the United States included Canada, France, Germany, New Zealand, Sweden and Switzerland.
The report found that:
• People in the United States have the shortest lives and the most avoidable deaths, ranking dead last on five out of six health outcome measures;
• Americans face the most barriers to obtaining health care. About 25 million people remain uninsured in this country, and nearly a quarter can’t afford care when they need it;
• The United States ranks lowest in health equity, with many low-income people unable to afford care and more groups reporting unfair treatment and discrimination when seeking care;
• Patients and doctors in the United States experience heavy administrative burdens when it comes to payment, billing and paperwork, with the system outranking only
Switzerland in its lack of efficiency.
The United States had just one bright spot in the report.
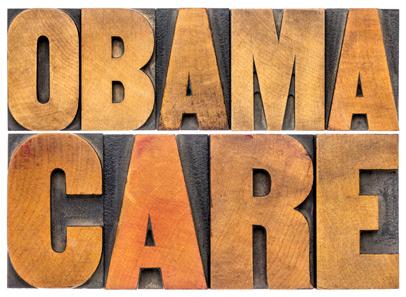
The nation ranked second among the countries in “care process,” which includes prevention, safety and patient engagement. The Affordable Care Act’s emphasis on patient safety and preventive services partly explains the high ranking, the researchers said.
“The U.S. is failing one of its principal obligations as a nation: to protect the health and welfare of its people,” said physician Joseph Betancourt, president of the Commonwealth Fund.
“The status quo — continually spending the most and getting the least for our health care dollars — is not sustainable,” Betancourt added in a Commonwealth Fund news release. “It isn’t about lack of resources — it’s clearly about how they are being spent. Too many Americans are living shorter, sicker lives because of this failure.”
The report argues that the United States could improve its health care comparative to other nations by:
• Extending coverage to the remaining uninsured and reforming health insurance to limit out-of-pocket expenses;
• Investing in primary care providers, so more are available to patients;
• Removing health inequities faced by minority and ethnic groups, rural residents and women;
• Curbing the uncontrolled consolidation of health care systems, which is driving prices higher;
• Address social drivers of health like poverty, homelessness, hunger, gun violence and substance use.
“This report shows that by adopting proven strategies and making smart investments, America can enhance its health system to better meet the needs of its people,” Williams said. “There’s no reason we can’t elevate our standing if we choose to do so.”



By Chris Motola

Andrea Shaw, M.D.
Physician was recently recognized for providing medical care to refugees. She talks about the influx of immigrants to Syracuse and how challenging it is for her team to deal with them
Q: You recently received the President’s Award from Catholic Charities for your work with local refugees.
A: Yes. So Catholic Charities is a longtime community partner in refugee resettlement. We’ve worked closely over the years to help facilitate getting refugees access to primary care, but also addressing the high-complexity needs of the population that can arise quickly in Syracuse.
Q: What does the refugee population generally look like in terms of age, overall health?
A: In general refugees have spent a long period of time in the transition process and have been in a country other than their country of origin for more than a decade before resettling in Syracuse. In that period of time they tend to have really limited access to healthcare and healthcare facilities. So often there’s an element of resilience. Healthy people do make it here, but we also see a higher risk of chronic disease after a lifetime of chronic stress and they’re usually coming from systems that have a poor ability to diagnose and manage those chronic diseases. So we see the whole range between people who are resilient and don’t need a lot of healthcare to people who really don’t have any insight into the chronic conditions that they have and have limited resources to management them.
Q: How quickly does this population need be examined by a doctor?
A: When people are coming to Syracuse, about 5%-10% of them are so sick that they need to be seen
within a week or two of landing. Another 20% should be seen within 30 days because they have a chronic medicine that needs follow-up. The remaining 70%-75% are generally healthy and don’t have chronic disease that they know of; they can be tucked into primary care within 90 days. The state does have a mandated request that we do health screenings for public health purposes within 90 days of arrival, which is hard to do in a healthcare system where the average wait time for a new primary care patient might be six to 12 months.
Q: Immigration and migration is politically a bit of a hot-button issue now. When the system is so stressed for existing citizens, how do you navigate helping this population in need while mitigating any potential resentment from underserved local populations?
A: We do certainly have folks who may look in on this system and say this isn’t fair. Local people are struggling to gain access to primary care, why do we have slot reserved for refugees? At the same time, our country is — through a formal refugee resettlement engagement with the United Nations — one of 30 countries that resettles refugees. So these are refugees who have fled persecution and have been deemed eligible and safe through a two-year vetting process for entry. Syracuse is one of the top three cities in the country for resettlement per capita and has a long history of welcoming immigrants and being a community that supports a safe space for diverse populations. So every year the
be their fourth or fifth language. So naturally a language barrier can be a social determinant of health. There are also cultural barriers in terms of how they perceive health and healthcare. And then there are very large systems issues. If you ask any American how they navigate their health insurance, the health office and navigate care, refugees have all those same issues times 10 because they’re just meeting this system for the first time. So if their child gets kicked out of school because they missed a physical or a vaccine, refugee families will be very confused about what’s happening and why. Of course everyone does their best to explain what’s happening and why, but there’s a lot to learn about healthcare and staying healthy in America.
Q: Which languages do you encounter the most? Do you have some on standby with regard to interpreters?
country accepts a certain number of refugees. We’re at around 100,000 this year. About 2% of what comes into the country comes into Syracuse. When people see 2,000 refugees come into Syracuse and are eligible for resources, it’s the same poverty-level resources that people in America have access to. So Medicaid, food stamps and housing support. These programs are designed to get refugees self-sufficient. Economic data shows that within 10 years their resilience and work ethic usually has gotten them out of poverty and contributing to our community.
Q: How does Upstate handle the intake of new arrivals?
A: So when you look at Upstate’s Center for International Health, what we try to do is center the resources. We’re a small but mighty clinic. We welcome two new families a week. We have built-in things like a reverse-translation line, live interpreters in the clinic and we do a lot to support their social needs along the way so that they can be on more of an equal plane with the U.S. population. And once they have their health insurance and primary care organized, they’ll graduate into other primary care clinics. So the local U.S. population has a lot of resources available to them whether it’s the ability to look at and transport themselves to other places, the ability to work and be eligible for types of insurance other than standard state Medicaid. Refugees have no systems experience and no language skills to navigate the arena. When we look at health equity, we try to give them a platform to launch from. If we don’t, the population becomes sicker within our midst and is less likely to be able to contribute to the community. So this is how we help their healthy assimilation.
Q: What are some of the challenges of treating refugees from the provider perspective?
A: None of our patients come with English as their first language. If they do know any English, it might
A: So actually this population is coming from all across the globe: Southeast Asia, the Middle East, sub-Saharan Africa and South America. We have over 50 languages registered within our clinic. By law, anyone billing Medicaid insurance needs to provide adequate translation services. We have access to a lot interpreter services, both live and phone consultations. There are a lot of creative ways across companies to book even limited language services ahead of patient visits. So we do our best to accommodate languages in a way that the patient is comfortable, in a dialect the patient understands. For example, we may have a patient who is only comfortable with a certain gender and they may want audio without video. They may prefer to work with a particular interpreter. One of the challenges is that many patients don’t come from a system where self-advocacy is their nature. They’ve lived a lifetime of persecution in very stagnant situations as refugees. So we need to be aware it’s going to take longer to work with this population. They need more to get to the same healthy playing field as the rest of us.
Q: You’re the medical director of international medicine at Upstate. What does that involve, apart from the refugee program?
A: The Center for International Health is a comprehensive primary care office. So we have folks who are trained in internal medicine, pediatrics and women’s health as well as mental health. We try to center those services in the same space because it’s really hard to get some of these primary care services to the patients if, say, they’re moved across town. So we do as much as we can to provide comprehensive care within our clinic at Upstate.
Name: Andrea Shaw, M.D.
Position: Medical director of Upstate University’s Center for International Health
Hometown: Manlius
Education: SUNY Upstate Medical University Affiliations: Upstate University Hospital
Organizations: American Academy of Pediatrics
Family: Husband, three children Hobbies: Travel, outdoor activities



























By George W. Chapman

The Inflation Reduction Act has already capped insulin at $35 a month for seniors on Medicare. In 2025, out-of-pocket costs for prescriptions will be capped at $2,000 a year. These alone will save members $1.5 billion a year. The Centers for Medicare and Medicaid Services (CMS) is just about done negotiating
While CMS finally negotiates drug prices for over 60 million Medicare recipients, commercial insurers that cover employees are on their own.
pricing with drug manufacturers for the first 10 drugs under the Inflation Reduction Act. The reduced prices will be in effect 2026. CMS will begin round two of price negotiations for another 15 drugs effective 2027. These savings on just 25 drugs will be in the billions for CMS and Medi-

Drug manufacturers are free to charge whatever they want. A senate committee recently grilled the CEO of Novo Nordisk, maker of Ozempic for Type 2 diabetes and Wegovy for weight loss. The difference in pricing between the U.S. and other countries is sickening if not criminal. In the U.S., Ozempic costs $969 a month. Yes — a month. It’s $59 in Germany; $71 in France; $122 in Denmark; and $122 in Canada.
In the U.S., Wegovy costs $1,349 a month. Again. A month. It’s $92 in the UK; $137 in Germany; $186 in Denmark; and $265 in Canada.
When pressed by the committee why, the CEO skirted the question and tried to put the entire blame on PBMs or pharmacy benefit managers. Really? While PBMs are another problem altogether, they are in no way accountable for the absurd differences in costs, (PBMs “negotiate” prices for their clients. But they get a payment of around 74 cents for every dollar eventually charged by Novo Nordisk. So, there is sort of a
perverse incentive against negotiating a really low price. The FTC has released a damning report on PBMs.)
The Novo Nordisk CEO absolutely knows the real reason why we pay so much more in the U.S. He just didn’t want to admit it. All the other countries have national health and negociate prices for every drug covered, including Ozempic and Wegovy, by their national plans for every citizen.
Not just 10 prices for their seniors. I’m sure there were a few senators on the committee sheepishly looking at their hands because they accept money from the ubiquitous and wealthy drug lobby.
Everyone at the hearing knew exactly what the answer was. And until we have a national plan, the drug lobby will grease palms and we will continue to be ripped off by drug manufacturers and PBMs.
Over 12 million of us purchase health insurance on the exchange. Premiums are discounted based on federal poverty guidelines. As an incentive to buy insurance, qualifying households are eligible for a premium tax credit. The average is about $800. The tax credit will expire next year. There is a bill
care recipients. Part D premiums will decrease next year from 2024 levels. For advantage plan members, the average monthly premium will decrease from $18.29 to $17. For Medicare members with traditional coverage, the average monthly premium will decrease from $41.63 to $40.
in congress that would make the tax credit premium for fear people will drop coverage without it. Overall, 45 million of us are covered by the ACA.
CVS ventured outside its pharmacy “lane” or area of expertise when it expanded into primary care clinics, pharmacy benefit management (Caremark) and insurance (Aetna Medicare) among other things. Their multifaceted business model intended to offer easy accessible, low cost, integrated care. As with many corporations, rapid overdiversification can lead to its downfall. CVS stock had fallen 20% from last year while the rest of the S&P has risen 21%. Industry experts surmise the negative press associated with PBMs and lower profits in their Medicare product could put both businesses on the chopping block.
‘I looked up hospitals in the broad region covering Watertown to Binghamton and Rochester to Albany. I didn’t find a 5-star facility. But I found four hospitals that received a 4-star rating: Guthrie in Cortland, Albany VA, St. Peter’s Albany and Cayuga Medical in Ithaca. All the other hospitals in the region received two or three stars.
seniors, employers must face cost reduction on their own. Premiums for commercial insurance could increase anywhere between 7% and 9% next year which means the U.S. will retain its ignominious lead in average per capita cost at $16,000. A recent survey found most employers are looking to cut costs thereby limiting cost shifting to their employees. A third of employers, however, say they will continue to shift costs to their employees via premium contributions, higher deductibles and higher copays. Twenty-one percent will offer drug discount cards and direct to consumer prescriptions and delivery. Forty-three percent will bid out their health plan. Thirty percent plan to explore narrower networks. Thirty-eight percent will reevaluate employee assistance programs like mental health. The top area of focus for all employers is drug costs, especially for weight management, cardiovascular health, cancer and women’s health.

CMS surveys our nursing homes and hospitals every two to three years. Hospitals receive a detailed report and must submit a plan of correction. Failure to improve can impact Medicare reimbursement. CMS uses a 5-star rating system. Metrics include quality, safety, staffing, etc. The average score for NYS hospitals is about 2.5 stars. Thirty-four of 133 NYS hospitals received one star. That’s 26%. The national average is 10%. You can look up a hospital or nursing home rating on Medicare.gov. I looked up hospitals in the broad region covering Watertown to Binghamton and Rochester to Albany. I didn’t find a 5-star facility. But I found four hospitals that received a 4-star rating: Guthrie in Cortland, Albany VA, St. Peter’s Albany and Cayuga Medical in Ithaca. All the other hospitals in the region received two or three stars.

Who isn’t? While Medicare is tackling costs via the Inflation Reduction Act and reducing premiums for

George W. Chapman is a healthcare business consultant who works exclusively with physicians, hospitals and healthcare organizations. He operates GW Chapman Consulting based in Syracuse.

Workplace anxiety. Who hasn’t experienced it?
However, if that anxiety is so strong that it hurts your performance or lingers for months, you might have a problem, one expert says.
Physician Asim Shah, executive vice chairman in the Menninger Department of Psychiatry and Behavioral Sciences at Baylor Colege of Medicine in Houston, explains what can trigger workplace anxiety, how to manage it and when to seek professional help.
“The goal is not to suffer and not let your anxiety affect work performance. About 60% of people experience workplace anxiety. It is common, which means you can do something about it,” Shah said.
Workplace anxiety can be caused by surly coworkers, a demanding supervisor, small, annoying tasks or overwhelming major projects.
If you have workplace anxiety, you might notice signs like:
• Feeling overly anxious or nervous;
• Experiencing excessive sweating or trembling;
• Obsessing about a task;
• Having a lack of interest in your work.
“The anxiety becomes so overwhelming that you are unable to focus and concentrate,” Shah noted in a Baylor news release. “These feelings can impair your daily work functions.”
If that continues for more than six months, Shah said it might be time to seek professional help.
“Some employers might offer an employee assistance program where you can go for help. You can also start talking to a therapist through psychotherapy or look into medication management for your workplace anxiety,” he said.
To manage it and help to reduce stress, Shah recommends:
• Break your tasks into small pieces;
• Set small goals throughout the work week and congratulate yourself for reaching them;
• Express your emotions. Journal how you feel. Talk, laugh or cry with someone you confide in;
• Start healthy habits and do things you enjoy;
• Work within your limits. Set boundaries with your workload.




By Eva Briggs, MD
Recently a friend asked me about the Inspire device to treat sleep apnea. I wasn’t familiar so I looked it up. Here is what I learned. Sleep apnea refers to stopped breathing occurring during sleep. There are several types: obstructive, central and mixed.
• Obstructive sleep apnea occurs when changes in the shape of the mouth and throat during sleep block air passage. It becomes more common with age. Examples include the tongue falling back against the soft palate or large tonsils. Symptoms include snoring or gasping during sleep, feeling drowsy during the day, trouble concentrating, dry mouth and headaches. But even children, such as those with enlarged tonsils or adenoids, can have OSA.
• Central sleep apnea occurs when the brain and nervous system fail to signal the body to breathe. Symptoms include daytime sleepiness, awakening feeling panicked or short of breath and insomnia. Causes include sedating drugs, sleeping at high altitudes and congestive heart failure. Some cases are idiopathic meaning there is no known underlying cause.
• Mixed sleep apnea combines both OSA and central sleep apnea.
The Inspire device treats OSA. Other treatments for OSA include CPAP (continuous positive airway pressure), surgical interventions to change the shape of the upper airway and oral appliances. The Inspire can treat patients that have tried and failed less invasive treatments.
The Inspire is designed to stimulate the genioglossus muscle, a muscle whose contraction moves the tongue forward thus opening the airway.
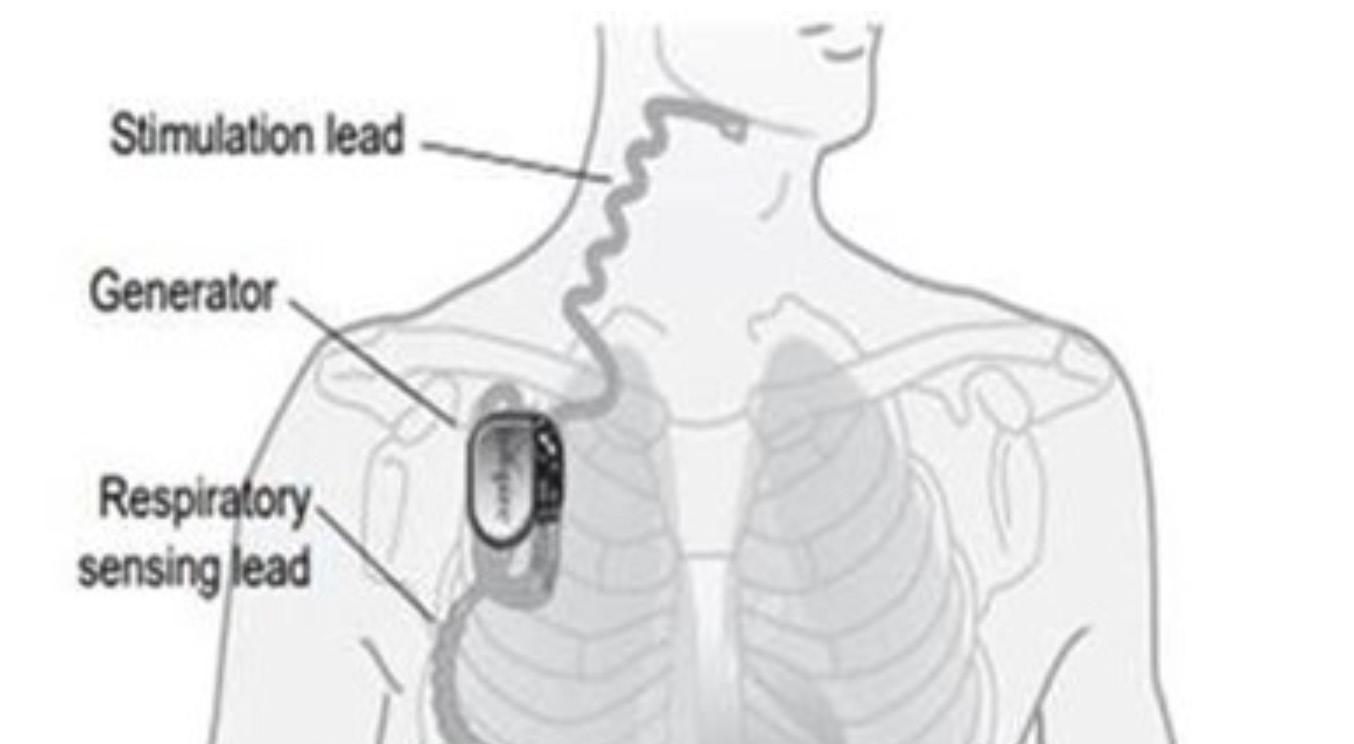
There are three components to the device. First is a small impulse generator, which is implanted under the collar bone. Second is a breathing sensor tunneled from the impulse generator to the chest wall muscles. This detects when the person is inhaling, telling the impulse generator to send a signal to the tongue to move forward. The third piece is a lead that tunnels from the impulse generator to a nerve stimulator lead placed on a branch of the hypoglossal nerve at the base of the tongue.
Candidates for this procedure must meet strict criteria. First is age, it’s used in adults older than 21. Second is moderate to severe OSA. The patient must have a body mass index less than 33. Patients must have first tried CPAP and have had trouble
Respiratory sensing lead Generator
tolerating it. Candidates for the procedure must not have significant additional medical problems such as neuromuscular disease, severe heart disease, severe lung disease or significant psychiatric illness. There should be no pronounced upper airway anatomic abnormalities. The patients must also undergo endoscopy during drug-induced sleep that demonstrates airway changes that could be helped by the device.
The procedure for eligible patients is as follows. It is done as an outpatient. There are two incisions. One is under the collarbone to place the battery-powered device. A second incision under the chin is used to place the lead wiring connecting to the nerve at the base of the tongue. The surgery takes about two hours and is performed with general anesthesia. The patient can go home the same day.
After one month, when sufficient healing has occurred, the patient returns for follow up at which time the device is activated. The patient can then use a remote to activate the device in the evening and turn it

off in the morning. The Inspire will require periodic adjustment. The battery is expected to last 10 years before requiring replacement.
As with any surgery, there are risks including bleeding, infection, tongue weakness, tongue numbness, facial weakness, voice change, lung collapse (pneumothorax), limitations of the ability to undergo MRI and tooth movement.
So, as you can see, it is not simple to determine who is a good candidate for the Inspire device. And it is a somewhat involved procedure. So, interested people would need to consult with an appropriately trained specialist.

Eva Briggs is a retired medical doctor who practiced in Central New York for several decades. She lives in Marcellus.


Don’t wait to get the care you need. When you visit the St. Joseph’s Health Cardiovascular Institute, you can expect the best. They’re rated high-performing in more heart procedures than all other area hospitals.* You’ll be back home and feeling better in no time.
*U.S. News & World Report

By Gwenn Voelckers
Thanksgiving is around the corner, marking the beginning of the holiday season — a time filled with food, family, joy and sometimes stress.
For many, it’s also a time of adjustment to a new way of living, especially if you’re newly on your own after a divorce or the loss of a spouse.
Maybe this is your first holiday season solo and you’re discovering that the freedom to make your own choices is both exhilarating and overwhelming.
One of the most critical lessons I’ve learned on this journey is that living alone successfully requires more than just setting the table for yourself — it requires the strength to set boundaries and say “no, thank you” when necessary.
Why is it so hard to set boundaries?
Setting boundaries, especially around the holidays, can feel incredibly challenging. I can remember not wanting to disappoint others, feeling guilty for saying no or worrying that people would think I was selfish.
Setting boundaries isn’t about being selfish; it’s about being selfaware. By saying no to certain things, you’re saying yes to your peace of mind, your health and your happiness.
You’re establishing healthier relationships by communicating your needs clearly and honestly. You’re guarding your heart and building self-respect.
The truth is, boundaries allow us to show up more fully in the relationships and activities that matter most. Without them, we spread ourselves too thin, risking burnout and
resentment.
So, this Thanksgiving, along with the turkey and pumpkin pie, let’s serve up a healthy helping of selfcare by learning how to say no when we need to.
The first time I said no to a party invitation that I didn’t feel like attending, I felt an odd mixture of guilt and relief. It wasn’t that I didn’t like the people throwing the party — I did. But the truth was, I just didn’t have the steam to go.
Here’s how I handled it: “Thank you so much for inviting me! I really appreciate being included and love spending time with you. However, I’m going to have to pass this time. I’ve been feeling overwhelmed lately and need to take some ‘me time’ to recharge my batteries. I look forward to connecting with you when life slows down.”
By expressing gratitude for the invitation and suggesting a future connection, I was able to decline in a way that felt comfortable and respectful.
Then there was the late-night request from a friend: “Can you pick me up from the airport?” The flight landed at 11:30 p.m. and while I used to be the kind of person who would bend over backward to help out, I realized that driving across town late at night was more than I was willing (or felt safe) to do.
My response? “I’d love to help, but I’m not comfortable driving that late in the evening. Can I help you
find a taxi or ride-sharing service?” By offering an alternative solution, I was still helpful without sacrificing my own comfort and safety.
Boundaries don’t just come into play with friends and family.
Sometimes, they’re necessary with neighbors or acquaintances. Like when my widowed neighbor started showing up at my house unannounced, asking for my opinions on fall cleanup and other light-hearted matters.
It was innocent at first — friendly chats, small favors — but then it started to feel uncomfortable.
One afternoon, he asked if I’d like to go to dinner. It took me by surprise and I told him, “I’m very flattered. Let me think about it.”
I knew I wasn’t interested in taking the relationship further and needed to set a boundary.
After going over several scenarios in my head, I finally arrived at what I wanted to say. With a kind smile, I simply said, “I’m sorry but I have to decline your very nice offer to take me to dinner. I value our friendship too much to do anything that might disrupt what we have. You’re a great friend and I like things just the way they are! I hope you understand.”
Yes, I was nervous, but I managed to keep my voice friendly and calm.
Thankfully, he nodded “OK” with a smile and I felt enormous relief as well as pride for setting a very challenging boundary.
Tip 4: Opting out of gift exchanges
Holidays often come with traditions that no longer feel right, like gift exchanges.
A good friend and I had exchanged gifts every year for decades. But last year, I realized it was beginning to feel more like an obligation than a joyful tradition.
I approached her with honesty: “I’ve loved our gift exchanges over the years, but I’m trying to simplify things this holiday season. How about we skip the gifts this year and just do something fun together instead?”
She was relieved! As it turned out, she’d been feeling the same way but hadn’t known how to bring it up.
Tip 5: Saying no to hosting a guest
Lastly, there’s the ever-persistent request from friends or family to stay at your place when they’re in town. For some people, it’s no problem, but for others, hosting can be overwhelming, especially during the holidays when life is already hectic. When a family member asked to “crash” at my place for several days, I had to be honest.
“I’d love to see you, but I’m not able to host this time around. This holiday season will be a busy one for me this year with band rehearsals and concerts. I know I’m going to need my own space to relax, practice my music and prepare for our upcoming performances. Let me help you find a nearby hotel.”
It’s important to protect your space and energy, especially when you’re still adjusting to living alone.
Encouragement for the season
As we head into the holiday season, I want to remind you — and myself — that setting boundaries is an act of self-love.
So, as you set the table this Thanksgiving, remember that you’re also setting the table for your own well-being. Say yes to what fills your heart and brings you joy and say no, thank you, to the things that drain you. This holiday season, may you find peace, joy and the courage to prioritize yourself. Happy Thanksgiving!

Gwenn Voelckers is the author of “Alone and Content: Inspiring, empowering essays to help divorced and widowed women feel whole and complete on their own.” She welcomes your thoughts on this column as well as topic suggestion for future essays at gvoelckers@rochester. rr.com.
Astudy tracking almost 10,000 9- and 10-year olds for two years finds a link between time spent watching TV and other screens with a higher odds for ADHD and depression.
“Screen use may replace time spent engaging in physical activity, sleep, socializing in person and other behaviors that reduce depression and
anxiety,” said study lead author, physician Jason Nagata, of the University of California, San Francisco (UCSF). His team published its findings Oct. 7 in the journal BMC Public Health.
As Nagata’s group noted, mental health issues have been on the rise among adolescents.
“Adolescents are 50% more likely to experience a major depres-
sive episode and 30% more likely to commit suicide today than they were 20 years ago,” according to a UCSF news release.
At the same time, the average U.S. tween spends 5.5 hours per day looking at a screen, the researchers said, and that rises to 8.5 hours for teenagers.
Could there be a link?
To find out, Nagata’s team tracked data for 2016 through 2018 for 9,538 adolescents aged 9 and 10 enrolled in a major child brain development study. The children’s daily screen time and their rate of diagnoses for conduct disorders, depression, ADHD and other mental health issues were monitored.
The study couldn’t prove cause and effect, but the team did find small but significant associations.
“Higher total screen time was associated with all mental health symptoms,” the researchers reported.
Kids with the highest levels of
daily time spent staring at screens had a 10% higher odds for depression, a 7% higher risk for conduct issues, and a 6% higher risk for ADHD, compared to children with lower rates of screen use.
“The specific screen types with the greatest associations with depressive symptoms included video chat, texting, videos and video games,” Nagata and colleagues noted.
The effect also seemed stronger for white adolescents than for Black adolescents.
“For minority adolescents, screens and social media may play a different role, serving as important platforms to connect with peers who share similar backgrounds and experiences,” said Nagata, an associate professor of pediatrics at UCSF. “Rather than displacing in-person relationships, technology may help them expand their support networks beyond what’s accessible in their immediate environment.”
Annual mean wage for a physician assistant in the area is $123,850
By Deborah Jeanne Sergeant
Helen Williams, a physician assistant with Oswego Health, had always felt drawn to working in some type of medical profession.
However, it wasn’t until she had worked as an athletic trainer specializing in strength and conditioning, that she felt like she wanted to be able to provide more care for patients.
Earning her physician assistant Master of Science degree in August from Upstate Medical University enabled her to work as a PA.
“In my previous career, there was only so much that I could do and help with,” Williams said. “Becoming a PA allowed me to do significantly more.”
As an athletic trainer, she could diagnose injuries and treat them, but couldn’t prescribe medications or order MRIs or physical therapy. Like many other PAs, she likes the flexibility in the career. If she wants to shift gears from orthopedics and specialize in oncology or hematology, she can do so through on-the-job training, unlike the physician with whom she works.
“It’s a profession that’s attractive to a lot of people who aren’t sure
what they want to do,” Williams added.
It’s also a plus that for most people, earning a master’s degree to work as a PA takes only two years of additional studies beyond their bachelor’s degree.
Becoming a medical doctor would take an additional seven more years after achieving a bachelor’s degree. The PA career path requires providers to take on less debt. Since this is a second career for Williams, less debt is an especially important feature of the PA career path.
Most schools require around 900 hours of healthcare related volunteer or paid employment with direct patient contact. It’s helpful to have good communication skills and experience in some kind of medical field. After completing the degree, candidates must pass a physician assistant national examination within the next six years and within six attempts. Every two years, PAs must complete 100 continuing education credits, plus recertify every 10 years.
Williams likes the work-life balance of the PA. She doesn’t receive phone calls at 2 a.m. When she leaves work, she leaves work (although some specialties do require on-call

responsibilities).
“There’s tremendous growth which is why it’s so competitive to get into school,” Williams said.
She noted that US News & World Report has ranked PAs as the second-best healthcare job.
Colleen Krug, physician assistant at Upstate Urology at Oswego Health, has known many who, like Williams, enter a PA program as a second career after working in some facet of healthcare.
“This profession draws people who are not only interested in practicing medicine but those looking for a fulfilling career to provide a much-needed service to our communities using a team approach working alongside doctors, nurses and others in the medical field,” Krug said.
PAs work in hospitals, medical offices, urgent cares, nursing homes
and more. Their services can include performing physical exams, diagnosing and treating illnesses, performing procedures, assisting in surgery and providing patient education and counseling.
“The high demand for PAs and the flexibility to pursue different specialties and medical settings without having to go back to school allow for ample growth opportunities,” Krug said. “There are also opportunities in leadership roles, research and academia.”
According to the Bureau of Labor Statistics, the career’s employment should grow by 28% between 2023 and 2033. The annual mean wage for a physician assistant in the Central New York area is $123,850. Their employment can include hospitals, doctor’s offices, surgical centers, specialty offices and at institutions such as schools.


Central Square resident shares experience after a regular screening showed a spot on her right lung
By Mary Beth Roach
This has been quite a year for Debbie Young. She started a job at Hematology-Oncology Associates of Central New York last October when a persistent co-worker encouraged her to take advantage of HOA’s free community lung cancer screenings, which are held in November in recognition of lung cancer awareness month.
The co-worker kept insisting; Young kept refusing.
Young, now 62, said she didn’t have any symptoms and that she and her husband, Central Square residents, were walking three miles every weekend.
“I thought I was fine,” she recalled.
But Young met at least two of the criteria for the screening. She is between 50 and 80 and she had been a smoker.
She said she and her husband quit 16 years prior when her daughter announced she was pregnant. In addition, both Young’s grandmother and mother had died of lung cancer. Her mom died when she was 60, one year younger than Young was when she was screened.
Finally, she agreed. These days, Young calls that same co-worker her guardian angel.
The screening showed a spot on her right lung. She followed up with a PET scan, a biopsy and a CT with contrast scan. She was diagnosed with non-small cell cancer, which makes up 80% to 85% of all lung cancers, according to the American Cancer Society.
She said she opted for surgery instead of doing chemo first. In February, she underwent surgery and had the top half of her right lung removed. During the surgery, doctors
found a second spot.
So, she followed up with four six-hour rounds of chemo, every 21 days. She’s currently on Keytruda, which she takes every three weeks for a year. She had a follow-up last month and was told she was cancer-free.
Despite that the screening results were not at all what she expected, she remained optimistic throughout her journey.
“God put me where I needed to be,” she said.
She returned to work this past spring, and working at the front desk at HOA, she helps to check patients in. Her cancer experience, she believes, has allowed her to perhaps better relate to the patients.
“We’re the first people that see them,” she said. She recounted how one female patient arrived at the offices quite despondent. Her husband did most of the talking for her. Young told the woman that whatever was going on with her wasn’t as bad as she was imagining. The woman admitted that she was not handling her circumstances well.
“I told her, ‘I had cancer. And not one time did I think this is the end.’ By the time I was done chatting with her, she was smiling,” Young said.
Young is hopeful that her story will lead at least one person to get the testing done.
These screenings are being offered for free by HOA and CRA Medical Imaging from 8 a.m. to 2 p.m. on Nov. 2, in three locations: HOA, 5008 Brittonfield Parkway, East Syracuse; HOA, 5490 Cobbler Way, Camillus; and Diagnostic Imaging Center, 37 W. Garden St., Auburn.
Appointments are required by calling 315-472-7504, extension 1301. Walk-ins aren’t allowed.

are quitting smoking (or not starting) and the number of deaths continues to drop, due to fewer people smoking and advances in early detection and treatment, according to a press release from HOA.
According to 2018-20 statistics provided by HOA, a total of 507 people in Onondaga, Cayuga and Oswego counties had lung cancer or 7.5% of the entire population.
This free lung cancer screening is available for people at high risk for lung cancer, meaning they must meet all the following criteria:
• Are 50 to 80 years old.
• Are currently a heavy smoker or one who has quit within the last 15 years. Heavy smoking is defined as one pack of cigarettes per day for 20 years; two packs of cigarettes per day for 10 years and has NOT previously received a free lung cancer screening through this program.
Those unsure if they meet the guidelines can take a simple quiz at hoacny.com/lungscreening.
This annual clinic is absolutely free as a community service from HOA and CRA. Lung cancer screenings are also available for anyone who meets the above criteria at any other time convenient to them, according to a media release from HOA. In most cases, the procedure is covered by insurance. The procedure also can be paid out-of-pocket for approximately $250.
Lung cancer, according to the American Cancer Society, occurs mostly in older people. Most diagnosed with it are 65 or older; a very small number of people diagnosed are younger than 45. The average age of people when diagnosed is about 70.
The American Cancer Society’s estimates for lung cancer in the U.S. for 2024 are about 234,580 new cases of lung cancer (116,310 in men and 118,270 in women).
Lung cancer is the leading cause of cancer death in the US, accounting for about one in five of all cancer deaths. Each year, more people die of lung cancer than of colon, breast and prostate cancers combined. However, the number of new cases continues to decrease, partly because more people
“The value of annual lung screenings is the opportunity to find lung cancer at an early stage where we have the greatest likelihood of curing it,” said physician Richard Cherny, a medical oncologist and hematologist from HOA.
Hematology-Oncology Associates of Central New York and and CRA Medical Imaging are offering free lung cancer screening from 8 a.m. to 2 p.m. on Nov. 2, in three locations: HOA, 5008 Brittonfield Parkway, East Syracuse; HOA, 5490 Cobbler Way, Camillus; and Diagnostic Imaging Center, 37 W. Garden St., Auburn.
Appointments are required by calling 315-472-7504, extension 1301. Walk-ins aren’t allowed.
This free lung cancer screening is available for people at high risk for lung cancer, meaning they must meet all the following criteria:
• Are 50 to 80 years old.
• Are currently a heavy smoker or one who has quit within the last 15 years. Heavy smoking is defined as one pack of cigarettes per day for 20 years; two packs of cigarettes per day for 10 years and has NOT previously received a free lung cancer screening through this program.
Those unsure if they meet the guidelines can take a simple quiz at hoacny.com/ lungscreening.

Program and volunteer manager at Upstate Oasis discusses the variety of courses the program offers to those over 50
By Mary Beth Roach
Q: For those who are not familiar with Upstate Oasis, how would you briefly describe it?
A: It’s a national nonprofit ed ucational organization designed to enhance the quality of life of adults 50 and older.
Q: Are you seeing an increase over the last few years in the number of people enrolling in your programs? And if so, why do you think that is?
A: Pre-COVID, we had a very robust program, and we were actu ally offering a lot of classes off site because we ran out of room in person to hold classes. And then COVID happened, and unfortunately, things changed. We pivoted to online classes. Now we’re still rebuilding post-COVID. We still offer online classes as well as in-person classes. We’re seeing more and more people every trimester. We run trimester. Obviously, COVID hurt, but then also it really showcased how im portant our program is for people to have that connection, to learn, to stay active. It hurt us in ways, but it also has helped us prioritize what healthy aging looks like.
Q: Can you give an overview of the pro grams that you offer?
A: We have art classes, art his tory, literature, writing, performing arts, all different types of history classes, current events. We offer science classes. We have a lot of environmental classes, which people are particularly interested in. We also have personal development classes; five different languages, currently Spanish, French, Italian, Russian and Irish; classes, like coping with stress, meditation. We offer cheese classes with The Curd Nerd [a local cheese

Fall is a busy time of year in Upstate New York, with loads of reasons to be outdoors. It’s also a busy time of year for the ticks that transmit illnesses including Lyme disease.
While most tick bites occur in the summer, it’s possible to get Lyme disease in the fall, especially if the weather is unseasonably warm.
“Lyme disease is a bacterial infection caused by the bite of an infected deer tick,” says physician Nicholas Massa, vice president of medical affairs at Excellus BlueCross BlueShield. “Untreated, the disease can cause health problems, including painful arthritis, swelling of the joints, and heart and central nervous system problems.”
When the infection is identified early, antibiotic treatment can result in a quick and complete recovery, according to Massa. The big issue, he says, is that Lyme disease often goes undiagnosed, which can lead to chronic symptoms that are hard to resolve.
Preventing tick bites is the best way to protect against Lyme disease and other tick-borne illnesses.
The New York State Department of Health offers these tips:
• Know where to expect ticks — Ticks prefer shady, moist areas at ground level. They cling to tall grass, brush and shrubs, usually no more than 18-24 inches off the ground. They also live in lawns and gardens, especially at the tree line. When

gardening, keep long hair tied back. When hiking, stick to well-cleared paths.
• Reduce ticks in your yard — Keep lawns mowed and edges trimmed. Clear away brush, leaf debris and tall grass from around the house and at the edges of gardens and stone walls. Stack woodpiles neatly away from the house, and preferably off the ground. Keep the ground under bird feeders clean so as not to attract small animals that can carry ticks into your yard. Locate children’s swing sets and other play equipment in sunny, dry areas of the yard, away from wooded areas.
• While outside, dress to protect To spot ticks easily, wear light-colored clothing with a tight weave.

By Deborah Jeanne Sergeant
Wear enclosed shoes, long pants, and a long-sleeved shirt. Tuck pant legs into socks or boots, and shirts into pants. Check clothes and any exposed skin frequently for ticks.
• Consider using repellent — The NYS Health Department recommends using EPA-registered insect repellents. For skin, products that have DEET (20% or more) or picaridin (5 to 20% of the active ingredient) can be applied. For clothes, shoes, and camping gear, treat, or purchase pretreated clothing with permethrin, but never apply permethrin to skin.
• After being outside, check yourself and your clothes — Do a final, fullbody tick check at the end of the day (also check children and pets) and remove ticks promptly. If available, put your clothes in a dryer on high heat for 15 minutes to kill any ticks that may be attached.
Submitted by Excellus BCBS
as they’re all interconnected. Altman listed managing stress, building mindfulness practices and developing healthier coping mechanisms as some of the practices health coaches instill in clients.
“By addressing the core of unhealthy habits and offering personalized support, they empower you to make meaningful changes that last a lifetime,” Altman said.
Working with a health coach doesn’t mean a long-term commitment to seeing someone every week for life. Diana Modera, registered nurse and certified health and wellness coach serving Central New York, said that coaches like her try to find the root cause of what’s happening with clients, whether it’s trauma, stress, health habits or other things.
“It’s not a quick fix like a fad diet. You work on one lifestyle habit at a time,” she said. “It does work for most people.”
After taking a medical history and learning about the client’s desired outcomes, she works with the client to develop a plan with both short-term and long-term goals. Some meet with her weekly, every other week, monthly or once they’ve reached their goals, as needed.
Just as an athletic coach wants to help athletes excel, a health and wellness coach wants clients to improve their wellbeing.
Most health and wellness coaches receive certification in facets of health so they can offer clients expertise that will benefit their health.
“As a health and wellness coach my job is to meet clients where they’re at and get familiar with their health challenges and goals,” said Cassie Schinto, owner of Cassie Schinto Holistic Wellness in Syracuse. “Every client is different but the common thread in every personalized program — whether the focus is increasing physical strength and mobility, relieving and mitigating chronic pain, cooking healthier and more nutritious meals, etcetera — is presenting a range options, information and experiences so that clients can figure out for themselves what works best for them, their lifestyle and their needs.”
It’s one thing to tell clients what
they need to do to be healthy. Schinto hopes to both empower clients and keep them accountable so they can reach their goals.
“Working with a wellness coach can help people feel more hopeful, informed, and motivated as they begin or continue their health and wellness journey,” she said.
Health coaches use consultations to learn clients’ history and goals so they can learn what will help support good health. Then they suggest steps that can help them reach their goals. These could include movement, yoga, meditation, therapy and energy work, depending on the practitioner.
Tracy W. Altman, certified health and life coach and owner of Mind Your Wellness in Phelps, views coaches as a support for the entire person’s health and not simply to address the symptoms individual problems once they’ve become extreme, as is typical of the medical model of care.
“In today’s fast-paced world,
many people struggle to maintain a healthy lifestyle,” Altman said. “Balancing work, family and personal wellbeing can feel overwhelming, leading to poor habits in areas like nutrition, sleep, exercise and stress management. This is where health coaches play a vital role.”
She said that personalized guidance is what makes a difference for clients as coaches develop a therapeutic and supportive role in their clients’ journey towards health. Instead of only addressing symptoms — a hallmark of many in the medical world — coaches take a holistic approach.
“They consider mental, emotional and even spiritual aspects of wellbeing,” Altman said. “This holistic approach encourages balance in all areas of life, helping you build sustainable healthy habits for the long term.”
In addition to supporting physical health, health coaches also support mental and emotional health,
The cornerstone of her practice is helping clients develop healthful eating habits. She also helps them identify physical activities they enjoy, ways to manage stress and improve their sleep.
The services are not covered by insurance. That’s why Modera tries to keep her rates low with most clients spending about $200 to $300 initially.
She refers clients to other specialists as needed and tells clients to continue seeing their healthcare providers and taking their medications as directed.
Modera has decades of experience in the medical field and also works as a private nurse.
“In the hospital, you see the same patients going in and out, in and out,” she said. “The focus now is more on preventative care.”
In addition to helping clients proactively plan for good health and to improve their health, coaches like Modera also provide a wealth of support to clients.
“One guy told me, ‘I just like that I’m not alone now,’” she said.
Inever liked cauliflower as a kid.
Boiled to a tasteless mush, it made me gag.
If that wasn’t bad enough, it stunk up the entire house for hours with its clingy odor molecules that followed me to school.
Fast forward a few decades, and I can’t get enough of this nutritious stuff.
Why the change of heart?
I learned ways to prepare it that didn’t set off the stink alarm, and I realized its powerful health benefits.
Cauliflower, like other members of the cruciferous family (broccoli, cabbage, and Brussels sprouts), may help reduce the risk of heart disease and cancer, the two leading causes of death in the United States. Research has found a link between a high intake of cruciferous vegetables and a lowered risk of inflammation, high blood pressure and hardening of the arteries. Some evidence suggests that cauliflower may also slow the growth and spreading of certain cancer cells.
This year-round vegetable has been found to contribute to weight loss and obesity prevention. High in fiber (2 grams per cup) but low in calories (27 per cup), cauliflower can help you feel full faster and eat less. Studies show that a diet high in fiber-rich vegetables like cauliflower is important for digestive health and
may lower the risk of several chronic illnesses, including diabetes.
Surprisingly, pale cauliflower is rich in vitamins C and K, which work together to protect bones and joints from damage and prevent bone loss. Separately, immune-boosting vitamin C helps the body grow and repair tissues while vitamin K helps blood to clot as well as prevent the hardening of arteries that can contribute to heart disease.

Similar to its cruciferous cousins, cauliflower is packed with an abundance of antioxidants that protect our cells from harmful free radicals and inflammation. These unique nutrients have been shown to reduce the risk of cancer and heart disease, slow age-related cognitive decline, and lower the risk of premature aging.

Anne Palumbo is a lifestyle columnist, food guru, and seasoned cook, who has perfected the art of preparing nutritious, calorie-conscious dishes. She is hungry for your questions and comments about SmartBites, so be in touch with Anne at avpalumbo@aol.com.
It’s called the MIND diet and its primary aim is to help guard against thinking and memory declines as you age. But does it work?
Yes, claims new research that found following the MIND diet for 10 years produced a small but significant decrease in the risk of developing thinking, memory and concentration problems.
“With the number of people with dementia increasing with the aging population, it’s critical to find changes that we can make to delay or slow down the development of cognitive problems,” lead study author, physician Russell Sawyer, an assistant professor of clinical neurol-
ogy and rehabilitation medicine at the University of Cincinnati’s Gardner Neuroscience Institute, said in a news release on the study. “We were especially interested to see whether diet affects the risk of cognitive impairment in both Black and white study participants.”
How does the diet work its magic?
The MIND (Mediterranean-DASH Intervention for Neurodegenerative Delay) diet joins elements of the Mediterranean diet and the DASH diet, which focuses on reducing blood pressure.
“Among the MIND diet components are 10 brain-healthy food
Select firm, heavy cauliflower heads with compact, cream-colored florets and few brown spots (a sign that the head is getting old). Unwashed cauliflower lasts about a week in the refrigerator; precut cauliflower florets should be consumed within one to two days. If cauliflower gives you gas, eat small amounts to begin. And if you’re prone to kidney stones, you might have to limit your intake of cauliflower, which is a high-oxalate food.
1 large head of cauliflower, cut into medium florets
4 tablespoons butter (or olive oil), divided ¼ cup yellow onion, chopped 2 cloves garlic, minced
3 tablespoons all-purpose flour
1 teaspoon salt
1. Preheat oven to 375 F.
2. Cook the cauliflower florets in a large pot of boiling salted water for 4-5 minutes, until tender but still firm. Drain, pat dry, and set aside.
3. Meanwhile, melt 2 tablespoons of the butter in a medium saucepan over medium heat. Add chopped onion and garlic and sauté until tender, about 3-4 minutes. Reduce heat to low; add flour, stirring constantly with a wooden spoon for 2 minutes. Pour the hot milk into the saucepan and stir until it comes to a boil, increasing heat if necessary. Boil, whisking constantly for 1 minute, or until thickened.
4. Off the heat, add salt,
groups — green leafy vegetables, other vegetables, nuts, berries, beans, whole grains, seafood, poultry, olive oil and wine,” Sawyer told CNN.
Meanwhile, five unhealthy food groups — red meats, butter and stick margarine, cheese, fried and fast foods, and pastries and sweets — are very limited in the MIND diet, Sawyer added.
“The MIND diet has all the key features — notably an emphasis on real food, mostly plants — required to reduce systemic inflammation, facilitate weight loss, improve the health of the microbiome, ameliorate insulin resistance, lower elevated blood lipids [fats], and slow atherogenesis [clogging of arteries],” physician David Katz, a specialist in preventive and lifestyle medicine
½ teaspoon coarse black pepper
1 teaspoon thyme or rosemary
2 cups 2% milk, hot
¾ cup shredded Gruyere cheese, divided
½ cup grated Parmesan
½ cup whole-wheat panko breadcrumbs
pepper, thyme or rosemary, ½ cup of the Gruyere and the Parmesan, mixing until fully melted and smooth.
5. Pour 1/3 of the sauce on the bottom of an 8-by-11 or 9-by13 inch baking dish. Place the drained cauliflower on top and then spread the rest of the sauce evenly over the top. Combine the breadcrumbs with the remaining ¼ cup Gruyere cheese and sprinkle on top. Melt the remaining 2 tablespoons butter and drizzle over the gratin (optional).
6. Bake for 25 to 30 minutes, until the top is browned. Broil for 2-3 minutes to brown the top more (watch carefully).
Note: Sharp cheddar can be substituted for Gruyere.
who founded the lifestyle as medicine nonprofit True Health Initiative, told CNN.
“That such effects would translate into protection of the brain is anything but a surprise,” Katz added. “This study of association does not, by itself, prove that the MIND diet protects cognitive health, but given the clear mechanisms in play, it certainly suggests it does.”
People who followed the MIND diet more closely were 4% less likely to develop memory and thinking problems than those who did not adhere to it, the study found. The finding held even after factoring in exercise, education, smoking, body mass index, medical conditions, age and anxiety or depression.

By Melissa Stefanec MelissaStefanec@yahoo.com

By the time most people are reading this article, the 2024 presidential election should have been decided. Some of us will be angry and some of us will be relieved.
Most of us will have something to say about it and some of us will have a lot to say about it.
But what are we saying in front of our kids?
That is something we should all be considering.
So much of politics is subjective. Most political problems don’t have a clear right and wrong or a true hero and villain — no matter how many devil horns are drawn on political mailers and ads. It’s not that easy; there is a lot of nuance.
But when we talk about politics, many of us don’t explore the nuance. It’s far more common for us to de-
monize the other side and blowhard our opinions as facts.
I have concerns about how we talk about politics, especially in front of children and teenagers. We should be encouraging our children to question our beliefs and learn.
However, I think too many of us want to raise ideological clones who fall in line — clones that love what we love and hate what we hate.
When you say that out loud, it sounds dangerous. That’s because it is. We owe our kids more than programming and inherited hate. We should be encouraging them to think independently, as that’s what actually facilitates freedom.
This post-election season, I’m encouraging us parents to do something different. Instead of discussing politics with our children on the sidelines, let’s bring our kids into the
discussion and improve the way we have those discussions. It’s time for us adults to police our own political behavior as much as we police those with opposing viewpoints.
I don’t pretend I have all of the answers, but I can offer some starting points.
Here are some ideas for talking to children about politics that will make for a more informed and respectful (current and future) electorate.
• Don’t draw devil horns on those you disagree with — You aren’t right about everything. Most people you disagree with aren’t evil. Let’s stop making compromise a dirty word and demonizing the other side. One of the things that makes America great is the diversity of thoughts, beliefs and approaches to problem-solving. Any ideology that is left unchecked can quickly become dangerous and damage our society.
• Invite your kids into the conversation by asking them questions — Don’t lead the witness or ask loaded questions. Give your children some unbiased information. Research pros and cons of specific political issues and the proposed solutions. Present the different sides of an argument and ask them for their thoughts. For example, you could research how increased banking regulations have some upsides and downsides. Present your findings and engage them in a conversation. Talk to them about concerns from the other side of the aisle. Teach them that every decision has good and bad consequences. We can’t rally for the good consequences and bury our heads in the sand when it comes to the bad ones.
• Check your own emotions — It’s really difficult to keep emotions out of political discourse, especially when it feels like there is so much on the line. But when it comes to talking about politics in front of our kids, we should play fair. That means checking our biases and negative patterns at the door. Encourage kids to see politicians as whole people. We should talk about what specific policies accomplish instead of how certain policies make us feel. We shouldn’t be telling our kids how to judge. Instead, we should be giv-

ing them objective information and coaching them in making decisions based on that information. Letting your emotions rule you in front of your children isn’t good form.
• If nothing else, do your homework — There are many news outlets that publish, broadcast and circulate opinions as news. Worse yet, many outlets make claims based on piecemeal or wholly inaccurate information. This happens on both sides of the political spectrum. If someone is telling you what to think or using a lot of adjectives, it probably isn’t news. If what you’re interacting with reaffirms everything you believe in, it probably isn’t news. Finding objective and accurate information is truly challenging. If we challenge ourselves to do this, everyone wins.
To help you find less biased news sources, I highly recommend typing “ad fontes media bias chart” into your favorite search engine or going directly to the site at: https://adfontesmedia.com/interactive-media-bias-chart/.
Ad Fontes Media is a non-partisan organization that wants to help people on both sides of the political spectrum understand media bias. Its media bias chart is a great tool to explore with your children. It will give you options for less biased news sources, which is something we can all benefit from. We need to be teaching our kids to search for the truth, not to be spoon-fed stories that reaffirm their own beliefs and confirm their fears.
• Be human — Politics should never dehumanize. We should not talk about politics with hate, anger and fear. That’s no way to nurture a republic, build a democracy or raise a child. We need to teach our children that every human being has the same basic needs as everyone else. We shouldn’t teach them to label people as democrats, republicans, Haitians, city folk or country folk. The first label we should apply to everyone is human. Then, we should realize that each human gets all of the good and true things that come along with that label. Whether or not our kids are in earshot, we need to take the cheap shots out of politics.
n
n
n
(music listening, hunting, motor sports, landscaping) and occupational (professional musicians, fire and police personnel) activities.
n
aid selection, fittings and repairs
n Tinnitus evaluations and treatment.
n If you have any questions or concerns regarding your hearing or how to protect it.

Writer recalls the hours before hurricane
Milton hit Florida … and right after it. ‘The massive destruction this storm left behind is devastating,’ she writes
By Barbara Pierce
Tuesday: Oct. 8: “There’s a category 5 hurricane coming this way!” my daughter says as I answer her call. “We’re evacuating. You should, too.”
Oncoming hurricane Milton is rapidly intensifying, surprising everyone with its rapid buildup. Hurricanes are rated category 1 to 5 — 5 being the worst.
“Catastrophic,” “life threatening,” “unprecedented,” are the words I hear when I turn on TV to learn more.
I’m sitting right in the path of where it’s expected to make landfall.
I’m in an evacuation zone, meaning I’m in a most vulnerable area and should not stay during the hurricane.
I’ve been through several hurricanes in Florida, my home state. It was difficult to sit there with the wind howling, the rains pouring and no power. But what I found much worse was the days after the hurricane, when I saw the devastation done. When I couldn’t drive down the street because of the trees down and no street lights. The road to my house was under water. My house was OK as it was on stilts.
It’s not getting through hour and hour of the hurricane’s fury — it’s the aftermath that’s heartbreaking.
I am not leaving for this hurricane. I have severe back pain. I’d spent the last days and nights in a recliner, positioned at exactly the right level, with an ice pack as that was the only thing tolerable. I couldn’t sit in my car and drive, with hundreds of others, to go to someplace strange. And hotels don’t offer recliners to sleep in.
I meet others in my building. “Are you leaving?” wee ask each other. “We’re staying,” was often the answer. “We’re troupers. We’ve got this. We’re not scared.”
I’ve been through hurricanes before. I can do this. But they keep saying there’s never been such a powerful, forceful one. This one does seem different.
And I’m scared, very scared.
The email from Florida Power and Light suggests I prepare for power outages, probably of long duration. I bought protein bars and other food that doesn’t require refrigeration.
Several of my neighbors pack
their cars, load their dogs and drive off. “You should leave,” they tell me. I drive downtown. Traffic in downtown is usually gridlocked, moving slowly along. Now there are one or two other cars. It’s eerie. Very creepy.
My brother calls from the other side of Florida. “Come stay with me. It’s not safe for you there.”
My ex calls several times. “You must leave now,” he commands. “Why aren’t you leaving?”
I can’t drive anywhere as the pain of driving would be intolerable after only a short time.
I talk to my few friends. We wish each other well. We’re all scared, really scared. “Stay safe,” we say to eachother.
Our building is only 10 years old. It seems sturdy; I should be safe here. I’m on the fourth floor. I’ll be OK if the river next to the building overflows. I’ll hide in an interior bathroom to keep safe if I need to.
As flooding is likely, I take my car out of the first-floor garage and move it to the second floor.
Wednesday, Oct. 9: Rain steady all day. By afternoon, the wind sounds like a train going overhead, hour after hour, rumbling, growling, growing louder and louder. Rain becomes intense a steady, heavy downpour.
I was fortunate because my power didn’t go out until about 10 p.m. I could watch the storm on TV. The landfall came right over us; the wind and rain stopped as we were in the eye.
“Things will get worse after the eye,” warns the weatherman, who had by now lost his voice from talking for many hours.
I’m hearing reports of tornados, all over the state, not only destroying
buildings but killing people in their path.
After the power goes out, I sit in my recliner, hearing the loud, loud wind battering the roof. When I get up, the floor shakes from the vibrations of the wind. I trusted this sturdy building; the floor shouldn’t be trembling.
Thursday, Oct. 10: I wake up. Much to my happy surprise, my power is already back on. I watch TV with tears as I see that trees are down, power lines are down. It’s not safe to go out. The roads are blocked by downed trees and there are no traffic lights. Many homes are without power. Mobile homes have been destroyed or roofs gone. Several neighborhoods are flooded; people have lost everything.
The massive destruction this storm left behind is devastating. It’s a bright sunny day. That makes me very angry!
Florida, you lured us here with your seductive sunshine, balmy winters, glorious blue skies and lovely fluffy white clouds. Behind this beautiful façade lies the cruelty of hurricanes, a threat becoming more and more powerful and intense each year, destroying the lives of so many people. I’m done. Time to leave Florida.



An arthritis sufferer’s joints start to get ornery when the weather turns colder, getting stiff and achy as the mercury drops.
Cold weather doesn’t cause arthritis, but it can make it worse, experts say.
“Our joints operate best in temperate weather,” said physician Mariko Ishimori, interim director at the Cedars-Sinai Division of Rheumatology in Los Angeles. “When the
weather gets cooler, the synovial fluid that acts like motor oil in our joints becomes more like sludge.”
Frigid temperatures also can increase a person’s pain sensitivity, slow their blood circulation, and promote muscle spasms, the Arthritis Foundation says.
And if that weren’t enough, your joints detect and respond to changes in air pressure that accompany weather fronts.
“A drop in barometric pressure can cause muscles and tendons to expand, which can put more stress on an already crowded joint,” Ishimori said in a Cedars Sinai news release.
“When your joint cap expands, you can feel that.”
But there are some simple steps that people with arthritis can take to protect themselves against joint pain caused by cold weather, experts say.
• Stay warm. Wear hats, gloves
and scarves, and use heating pads and blankets to keep warm while napping. A hot bath also can soothe stiff joints.
• Get moving. Exercise can keep joints loose, boost energy and release a flood of feel-good hormones. Aim for at least 150 minutes of moderate-intensity exercise weekly, including two rounds of strength training.
• Stretch. Be sure to stretch your muscles regularly, especially prior to exercise. Roll the wrists and ankles, do some knee bends and stretch out the fingers and hands.
• Eat healthy. A good diet can help reduce inflammation and boost the immune system, as well as strengthening bones. Be sure to get enough omega-3 fatty acids, which reduce inflammation, as well as bone-strengthening vitamin D.
• Maintain a healthy weight. The more weight a person carries, the more pressure placed on bones, joints and tissues. Dropping some pounds can help reduce pain and stiffness.
• Tread carefully. A simple fall can cause lasting pain, and a person’s sense of balance can be altered by arthritis-damaged joints. Take your time while walking, and wear proper footwear.
These recommendations will vary between people. Ishimori recommends that each person explore how cold weather affects their joints, then pursue the lifestyle changes most apt to make them feel better.
“There’s a lot we can do to ease joint pain and stiffness,” Ishimori said. “You don’t need to suffer in silence.”




By Deborah Jeanne Sergeant
Information released this summer by FAIR Health indicates that in a population of people 65-plus who have commercial health insurance, diagnoses of sexually transmitted diseases increased by almost 24% during the COVID-19 pandemic compared with just 5% in the population overall.
Those between 55 and 64 represented the next largest group with a 16% jump. These statistics mirror those published by the Centers for Disease Control and Prevention for those 55 and older between 2012 and 2022.
The information doesn’t shock physician Sharon Brangman, faculty at SUNY Upstate Medical University, distinguished service professor, chairwoman of geriatric medicine and director of the Upstate Center of Excellence for Alzheimer’s Disease.
“There’s a stereotype about older people and sexual activity,” Brangman said. “Sexual activity doesn’t stop just because you’re older.”
While their parents’ generation slowed down in the bedroom once libido and physical limitations

hampered them, current older adults have no such restrictions.
“With erectile dysfunction medication, many older men have more than one partner,” Brangman said. “Women can take hormones and creams to help them be more likely to be sexually active, so they can have sex without pain.”
A generational gap in STI knowledge also contributes. No longer fearing pregnancy, older adults may erroneously feel freer to engage in promiscuous sex. Brangman said that physician guidelines for STI screenings don’t exist for older adults’ PCP visits.
“Ageism makes us think it’s not an issue for older people,” Brangman said.
Even worse, the typical older adult already has some health issues that Brangman said mimic some STI symptoms. Or an older adult can assume everything’s fine since some STIs present as asymptomatic initially.
“People who are recently widowed or divorced are dating and they may not have the sex ed we give

Anew, large study from France underscores the link between adult hearing loss and dementia.
“Given the major burden of cognitive decline and the absence of curative treatment, identifying modifiable risk factors is of importance,” a team led by physican Baptiste Grenier, of the Université Paris Cité, wrote
to younger people,” Brangman said. “They can’t get pregnant, so they’re not thinking of safe sex. They may have multiple partners.”
That only exacerbates the spread.
A National Institutes of Health study that indicated people aged 6594 held many misconceptions about STIs.
Jenna Weintraub, sex educator for Rochester Center for Sexual Wellness, guessed that greater longevity may have something to do with why more older adults are getting STIs.
“People are living longer and staying healthier until older ages,” she said. “Many can maintain an active sex life for many more years.”
During the pandemic, many people made a major life shift such as separation and divorce, closing a small business or retiring. Reevaluating one’s life trajectory can cause changes in behavior and not all of those are good.
Better attention to healthcare has caused more people to maintain better health later in life. During the retirement years, with more time on their hands and “gray divorce”
increasing, more older adults are entering sexual relationships with multiple partners: a huge risk factor for the spread of STIs.
More than ever, older adults access dating apps, which allows them to cross paths with more random encounters with veritable strangers instead of meeting a friend-of-afriend for lunch and developing a relationship naturally from serendipitous interactions. Weintraub also indicated that living in intentional communities geared towards older adults increases their dating pool, as does the tendency for women to outlive their husbands.
Not only do older adults have more opportunity for exposure to STIs, but those factors directly related to their age also increase their risk.
“Since menopause causes the vagina skin to become thinner, less acidic and cervical mucous diminishes, this makes the skin more prone to infection,” Weintraub said.
Weintraub encourages more medical providers to screen their patients for STIs and start conversations about sexual health.
Oct. 1 in the journal JAMA Network Open. They said thinking skills may decline not only because people with hearing loss become socially isolated but also because they go for a long periods without auditory input.
In addition, hearing loss is linked to loss of volume in critical areas of the brain.
Even so, researchers said hearing aids for patients with disabling hearing loss should be prescribed based on potential benefit to quality of life and not to ease cognitive decline. For that, they wrote, more research is needed.
For the study, Grenier’s team analyzed data from more than 62,000 people in France (average age 57)
recruited between January 2012 and December 2020. Participants aged 45 and older underwent cognitive testing at the outset.
In all, 49% had normal hearing; 38% had mild hearing loss; and 10% had disabling hearing loss but did not use a hearing aid; 3% wore a hearing aid.
Participants took both hearing and cognitive tests.
In all, 27% of participants with mild hearing loss and 37% with disabling hearing loss had cognitive scores indicative of impairment. That compared to 16% of participants whose hearing was normal.
Researchers found no meaningful difference in the risk of cognitive impairment between individuals with disabling hearing loss who wore a hearing aid and those who did not.
A related analysis suggested that hearing aids may reduce the risk of cognitive impairment in people who have disabling hearing loss as well as depression.

New research shows that the dramatic increases in life expectancy seen during the 19th and 20th centuries have slowed
So much for the idea that most people born today will live 100 years or more.
New research shows that the dramatic increases in life expectancy seen during the 19th and 20th centuries have slowed considerably.
In the world’s longest-living populations, life expectancy at birth has risen just 6.5 years, on average, since 1990, after nearly doubling over the 20th century as a result of advances in preventing disease.
Humans appear to be hitting a biological limit to life, the evidence suggests.
“Most people alive today at older ages are living on time that was
manufactured by medicine,” said lead author S. Jay Olshansky, of the University of Illinois Chicago School of Public Health. “But these medical Band-Aids are producing fewer years of life even though they’re occurring at an accelerated pace, implying that the period of rapid increases in life expectancy is now documented to be over.”
A child born in the United States today can expect to live to 77.5 years. A baby girl has a lifespan of 80.2 years and a boy, 74.8, according to the National Center for Health Statistics.
Olshansky has been studying life expectancy for decades. He pub-
lished a paper in the journal Science in 1990 that said that people were approaching a ceiling for life expectancy at about 85. Others disagreed, forecasting that advances in health care would lead to further gains.
The new study — published Oct. 7 in the journal Nature Aging — forecasts that gains in life expectancy will continue to slow as more people experience the unyielding effects of aging.
It looked at data from Hong Kong and eight countries where life expectancy is the highest and at the United States, one of a few countries where life expectancy dropped during the period studied.
“Our result overturns the conventional wisdom that the natural longevity endowment for our species is somewhere on the horizon ahead of us — a life expectancy beyond where we are today,” Olshansky said in a university news release. “Instead it’s behind us — somewhere in the 30- to 60-year range. We’ve now proven that modern medicine is yielding incrementally smaller improvements in longevity even though medical advances are occurring at
breakneck speed.”
Even though more people may live to 100, they’ll be the exception, he said. That’s just the opposite of thinking among insurers and wealth-management firms, who make calculations based on the assumption that most people will live to be 100.
“This is profoundly bad advice,” Olshansky said.
While the study notes that science and medicine may produce further benefits, efforts to improve quality of life rather than extending it may make more sense. Researchers called for investment in geroscience, the biology of aging, arguing that it may be key to the next wave of health and life extension.
“This is a glass ceiling, not a brick wall,” Olshansky noted.
Reducing risk factors, working to eliminate disparities and encouraging people to embrace healthier lifestyles can enable people to live longer and healthier, he said.
“We can push through the glass health and longevity ceiling with geroscience and efforts to slow the effects of aging,” he added.

















Living to 100 is not only possible. It’s also possible to maintain good health into three-digit age. Beyond the oft heralded “don’t smoke, eat right and exercise” and a lucky set of genetics, a few other factors play into healthy longevity.
Tips from Diana Modera, registered nurse, private nurse and certified health and wellness coach serving Central New York:
1 “Sleep is big. It controls the hormones for your satiety center. Lack of sleep makes you crave carbs and increases cortisol levels. Not sleeping is stress for your body and it increases your fat storage.
2 “Find out what the stressors are. For one person, it was a toxic relationship. Or it could be suppressed trauma. Sometimes, if I think someone is traumatized to the point where they can’t function, I refer them out to a psychologist or psychiatrists. They need help in working through things.
3 “Many people have a lack of activity. Walking releases endorphins and we need to exercise for 30 minutes a few times a week, plus strength training.
4. “Get out in the sunshine. It helps your body generate and absorb vitamin D. We don’t have much sunshine here in the Northeast, so supplementing is important for D. I believe you can get almost all that you need in your food. I’m not a big supplement person. Supplements aren’t FDA-approved. They can print anything they want on the bottle. I’d run this by a registered dietitian to get supplements.
5. “Hydration is very key. Your body is 60% water. You have to drink enough water.
6. “It’s not just about avoiding junk, but eating enough of the good stuff. I call my eating plan the ‘rainbow plate’ because 50% should be fruits and vegetables, 25% lean protein and 25% whole grain. You can be healthy if 80% to 90% of the time, you stick with what works. If you have a celebration, don’t feel guilty. Enjoy it.
7. “Eat more whole foods. Processed foods are what’s killing America.”
Tips from physician Sharon Brangman, faculty at SUNY Upstate Medical University, chairwoman of geriatric med icine and director of the Up
The keys to healthy longevity are less obvious than you think
By Deborah Jeanne Sergeant
state Center of Excellence for Alzheimer’s Disease:
8. “You can be healthy and still have medical problems. The main thing we look for is someone who still has brain power and can get around for the most part. They might need a little help. It doesn’t mean you age without a medical problem.
9. “Everyone needs social engagement. Find something that has meaning and you find has value. So many older people feel marginalized and that they’re no longer contributing.
10 “Find something that you can do with others. Find something you want to learn more about, especially if it involves other people. We learned during the pandemic that people by themselves had increased risk of dementia and overall increase in diseases. Maintain that social engagement. It’s so important. It can be harder as you get older and friends die and family lives far away. Look to senior centers and other programs.”
Tips from geriatrician Ahmed Rab, affiliated with Rochester Regional Health:
pose have less dementia. Acquiring new skills supports brain health.
12 “Another thing that resonates well is being as functional as possible and keeping their minds sharp.
13 “Focus on cognitive fitness. Puzzles, reading and learning new languages can prevent cognitive decline. Those who stay mentally and physically active have lower risk of cognitive decline.
14 “Maintaining a safe home environment is extremely important. When people have falls and fractures, it sets them back in their ability to live independently at home. Add grab bars, add lighting, make sure the floor is clutter-free and avoid rugs that raise fall risk.
15 “Embrace technology. I have patients who order on Amazon at age 100.
16 “Get depression screenings and get help. As we get older, we lose a spouse. They maybe had experiences with war and kept their feelings buckled in. A lot of my patients are living in senior communities where they have others who have experienced these things. That can help.
17 “Take your medications. As we get older, remembering what to take is hard. We need reminders. I have a couple patients who have


By Deborah Jeanne Sergeant
Visiting a hospital’s emergency department isn’t routine healthcare and for most issues should not be the first response.
Depending upon the time of day, people should contact their primary care provider, the on-call nurse at their primary care physician’s office or an urgent care provider.
But some health issues cannot wait.
“The number one reason people this age should go to the ER is if they have a bad fall, especially if they hit their head,” said physician Sharon A. Brangman, faculty at SUNY Upstate Medical University. “So many falls can lead to an injury that can cause serious damage to the brain. There can be bleeding or breaking a bone in the neck.”
Brangman chairs geriatric medicine and directs the Upstate Center of Excellence for Alzheimer’s Disease. She also said that any stroke signs such as sudden onset of slurred speech, bodily weakness or blurred
vision require an ER visit, as does a seizure.
“They should go if there’s a fever of 101 or greater,” Brangman said. “A lot of these also depend on what other medical problems a person might have.”
Some other symptoms could indicate an older person needs emergency care.
“Severe pain in their belly that doesn’t go away or really bad pain anywhere in their body that comes on suddenly, get checked out,” Brangman said.
Abdominal pain could indicate appendicitis, for example.
It’s especially tricky for older adults to decide to go to the ER because they may have several health conditions and related medications that can have interactions. The symptoms could represent an urgent condition, but not an emergency.
Anyone unsure of whether they or a loved one should go to the ER should contact the primary care

provider or the on-call line during off hours to get a better idea of what to do next. Contacting an urgent care center within the patient’s medical system can help ensure that the providers can access medical records to improve continuity of care.
When reporting to the emergency room, it’s helpful to — if possible — select one within the patient’s medical system and provide a list of the patient’s medications and current and past health issues.
These can help providers determine what’s going on.
By Deborah Jeanne Sergeant
Most people haven’t experienced sitting with a loved one whose death is anticipated. Even those who have could still use support.
That’s where death doulas come in.
Also known as end-of-life doulas, these professionals make dying easier on the patient and family by offering a comforting, non-medical presence through practical, emotional and spiritual guidance during death.
Jesse Penorio, certified end-of-life doula and member of the National End-of-Life Doula Alliance, serves Onondaga County. She became interested in the dying process when she had to face it herself as a 17-yearold with Ewings sarcoma, a type of tumor that forms from a certain kind of cell in bone or soft tissue. After effective treatments, she survived the bone cancer on her pelvis and was able to pick up where she left off: going to college, moving to New York City and launching her life. But it bothered her that others face alone their own demise or that of a loved one.
When she returned to Central New York during COVID-19, she realized that she wanted to pursue certification to become an end-of-life doula. She has volunteered at hospic-
es and plans to formally launch her end-of-life doula business in 2025.
Volunteers with a hospice
“When you’re sick everyone wants to say, ‘It will be fine; you’ll get better,’” Penorio said. “But eventually death will happen to all of us. How can we make it easier? How can we help people to not make the end of life so scary?”
She believes that most people don’t want to die at the hospital alone. A couple generations ago, most people died at home, surrounded by loved ones. With a little support, many families can experience this as a more peaceful passing than in the institutional setting of the hospital.
direction it faces; what type of legacy items they want to leave behind, such as a journal, video recording or other gestures; and how they want their passing commemorated or their life celebrated.
The end-of-life doula may also serve as a liaison between the intown and out-of-town family members and suggest ways that they can offer support from afar.
“We don’t want to interfere, but there is something to be said for having a third party there who doesn’t know your Aunt Susie so she won’t be offended if I say, ‘I think it would be best to step away.’ I don’t care if she’s mad about that. I’m just trying to help my client,” Penorio said. Penorio hopes to become reiki certified in 2025 to add another tool to her client care toolbox.

“Obviously, we can’t control everything that’s going to happen,” Penorio said. “What can we control?”
That might include who the person wants or doesn’t want near the bed; where their bed is and what
“When you’re dying, you’re not quite as in touch with your body in that state and it can be nice to have someone massage the limbs, hands and feet,” she said.
“A death doula is someone there to sit bedside if you have a caregiver who’s getting burned out. They can go grocery shopping, take a shower, do something with their kids. The person dying can know someone familiar with them. If they’re a religious person, they may want something like Bible verses read to them or some other religious practice.”
The services are not covered by
The Institute for Healthcare Policy and Innovation’s National Poll on Healthy Aging states that annually, people aged 50 and older make more than 40 million visits to the ER. In the organization’s 2020 survey, people aged 50-80 reported that 26% had an ER visit in the past two years; as did 32% of those aged 65-80 and 23% of those 50-64.
Of those going to the ER, 13% went because they could not receive care soon enough from a PCP or specialty office, although 63% contacted a PCP before going to the ER.

insurance as they’re not medical. However, some hospitals and hospices have end-of-life doulas as part of their staff.
Penorio hopes that more people plan for how they want to die so when it’s their time, they can have their own wishes fulfilled and also relieve their families of the burden of wondering if their loved one is comfortable.
She even started an Instagram account, @jess_themortal, to talk about death so more people prepare.
“We were always supposed to die; we were always supposed to do this,” Penorio said. “I think COVID-19 woke people up a little bit.”
By Jim Miller
Dear Savvy Senior,
I would like to arrange a simple cremation that doesn’t cost me, or my family, a lot of money. Can you offer any tips that can help me with this?
Still Kicking
Dear Kicking,
If you’re looking for a simple and affordable way to go, cremation is an excellent choice, and one that’s become exceedingly popular in the United States. About 60 percent of Americans are now choosing cremation over a traditional burial, versus only around 20 percent in the mid1990s.
Why the big shift? Price is a key reason. A basic cremation can cost as little as $700 to $1,200, depending on your location and provider, versus $7,500 or more for a traditional funeral and cemetery burial. Geography is another factor, as many families are spread across the country, making future gravesite visits less common.
Here are a few tips to help you arrange your cremation and ensure you get a good deal.
You can arrange a cremation through a funeral home or a cremation-only business, but it’s wise to shop around because prices vary widely. It’s not unusual for one funeral home to charge $1,000, while another charges $4,000 or more for the same service.
Call five or six funeral homes or cremation-only businesses in your area and ask them how much they charge for a “direct cremation,” which is the most affordable option there is. With direct cremation, there’s no embalming, viewing or memorial service. It only includes the essentials: transportation of the body; required paperwork such as death certificates; the cremation itself; and return of the ashes to the family, usually within a week.
If you want a viewing, memorial service or anything beyond what a direct cremation provides, ask the funeral home for an itemized price list so you know exactly what you’re paying for. All funeral providers are required by law to provide this.
To locate nearby funeral homes, Google “cremation” or “funeral” followed by your city and state. You can also shop and compare prices from funeral homes in your area at Funeralocity.com.
The urn is another item that can drive up your cremation costs. Funeral home urns usually cost around
$100 to $350, but you aren’t required to get one.
After cremation, your family will receive your ashes in a thick plastic bag inside a cardboard box. This is all they need if you intend to have your ashes scattered, but if your family wants something to display, Amazon.com and Walmart.com both sell a wide variety of urns for under $50.

If you’re an environmentally conscious person, there’s also a green cremation option you should know about called “alkaline hydrolysis” that chemically dissolve the body. This is a gentler, more eco-friendly process than traditional cremation, which uses combustion. It’s legal in more than 20 states, and costs around $2,000 to $3,500. Alkaline hydrolysis is not currently legal in New York state.
If you’re interested in a free final farewell, you may want to consider donating your body to a university medical facility.
After using your body for medical research or surgical practice they will cremate your remains for free, and either bury or scatter your ashes in a local cemetery or return them to your family, usually within a year.
In Upstate New York, the departments of anatomy of SUNY Upstate Medical Center and University of Rochester School of Medicine are some of the places that accept body donations. To find other medical schools that offer the service, the University of Florida offers an online directory at Anatbd.acb.med.ufl. edu/usprograms.
Whatever arrangements you end up making, make sure you tell your family your wishes so they will know what to do and who to call after your death. Also, if you have a written agreement with any funeral or cremation provider, give them a copy to let them know if you’ve prepaid or not.

Send your senior questions to: Savvy Senior, P.O. Box 5443, Norman, OK 73070, or visit SavvySenior. org. Jim Miller is a contributor to the NBC Today show and author of “The Savvy Senior” book.
SIMEON DEWITT
150 E. 1st St. Oswego, NY 13126 315-343-0440
TOWPATH TOWERS
100 Rochester St. Fulton, NY 13069 315-598-4700
4920 N. Jefferson St. Pulaski, NY 13142 315-298-6101
The following services are included in your rent
• Trash Collection • Free Wi-Fi
• Bus for shopping/groceries
• Heat, Electricity & Hot Water
• Snow Removal & Lawn Care
• Planned Activities
• All repairs & maintenance Applications are now being accepted! 62+ No smoking!
Preference given for veterans & spouses of veterans. Equal


813 Fay Road| Syracuse st-camillus.org/join-our-team




Baldwinsville, Camillus, Cazenovia, Cicero, East Syracuse, Fayetteville, Liverpool, Pulaski, Syracuse and Watertown
Visit our newest Patient Service Center located at 5000 Campuswood Drive in East Syracuse. Monday to Friday 8 am to 4:30 pm. Prompt, courteous and no appointment needed.

By Warren Beck Social Security District Manager in Syracuse.
It may have been years or even decades since you thought about how much you earned at your first job. Did you know that you can find out how much you made that first year? Or any year you worked and paid Social Security taxes?
Your earnings history is a record of your progress toward your future Social Security benefits. We track your earnings so we can pay you the benefits you’ve earned over your lifetime.
That is why it’s so important for you to review your earnings record.
Even though it’s your employer’s responsibility to provide accurate earnings information, you should review your earnings history and let us know if there are any errors or omissions. Otherwise, your future Social Security benefits could be lower than you should receive. It’s important to identify and report errors as soon as possible. If too much time passes, it could be hard for you to get older tax documents. Also, some employers may no longer exist or be able to provide past payroll information.
The best way to verify your earnings record is to visit www.ssa.gov/ myaccount and create or sign in to your personal My Social Security account. You should review your earnings carefully every year and confirm them using your own records, such as W-2 forms and tax returns. Keep in mind that earnings from this year and last year may not be listed yet. When you have a personal My Social Security account, we send you an email once a year, three months before your birthday, to remind you to check your earnings and to get future benefit estimates.
If your Social Security earnings record is incorrect and does not
Q.: I didn’t enroll in Medicare Part B back when my Part A started a few years ago. Can I enroll now?
A.: It depends. The general enrollment period for Medicare Part B (medical insurance) runs from Jan. 1 through March 31. Keep in mind that although there is no monthly premium for Medicare Part A, there will be a premium for your Medicare Part B. In most cases, that premium goes up each 12-month period you were eligible for it and elected not to enroll. If you are covered by a group health plan based on your employment or the employment of a spouse, you may be eligible for a special enrollment period. Special enrollment periods may be processed at any point during the year but require proof
match your personal records, you may be able to submit a correction request online using your personal My Social Security at www.ssa.gov/ myaccount. If that feature is available in your personal My Social Security account, you can use the online process to correct missing earnings, inaccurate earnings from a valid employer, or earnings from an employer you did not work for. You’ll need to provide:
• Your address if we need to contact you about your request.
• Details about your correct earnings and employer.
• Evidence or proof of correct earnings, if available.
You can electronically upload your proof (W-2, W-2C, tax return, wage stub, pay slip, etc.) in a JPG or PDF format. After you successfully submit your evidence, you can print or save a receipt.
Earnings corrections cannot be processed online if they are for:
• The current or prior year, which may not be recorded yet.
• Self-employment.
• Railroad Board.
• Certain years before 1978. Also, you cannot submit an earnings correction online if you:
• Receive Social Security benefits, Supplemental Security Income (SSI), or Medicare.
• Have applied for Social Security benefits or SSI.
If you cannot correct your earnings online, call us at 1-800-772-1213 (TTY 1-800-325-0778), Monday to Friday, 8:00 a.m. to 7:00 p.m. to request a correction.
Start a conversation today. Ask a family member or friend about their first job and let them know they can find out what they earned that year!
of coverage. To find out more about Medicare, visit www.medicare.gov or www.ssa.gov/medicare/sign-up.
Q.: My child, who gets Social Security, will be attending his last year of high school in the fall. He turns 18 in a few months. Do I need to fill out a form for his benefits to continue?
A.: Yes. You should receive a form, SSA-1372-BK, in the mail about three months before your son’s birthday. Your son needs to complete the form and take it to his school’s office for certification. Then, you need to return page 2 and the certified page 3 back to Social Security for processing. If you can’t find the form we mailed to you, you can find it online at: www.ssa.gov/forms/ssa-1372.pdf.










Currently, he serves as one of the team doctors for Syracuse University, providing sideline coverage for football, field hockey and women’s basketball, along with training room coverage for all SU athletes.
Hamilton Orthopaedics Spine and Sports Medicine, with offices in Hamilton and New Hartford, has become an official partner of Oneida Health.
With the new partnership, Hamilton Orthopaedics surgeons Rudolph Buckley and Russell LaFrance will begin performing most of Hamilton Orthopaedics’ hospital-based surgical procedures in the operating room at Oneida Health Hospital in Oneida.
“Hamilton Orthopaedics and Oneida Health have had a collaborative relationship for years focused on providing high-quality orthopedic services to patients in Central New York,” said Buckley. “Our new partnership will provide a centralized location for Hamilton Orthopaedics patients to receive the high level of quality hospital-based surgical care they are accustomed to in a stateof-the-art operating room at Oneida Health.”
Before the agreement with Oneida Health, the practice’s surgeons performed surgical services across multiple healthcare locations in Chenango, Madison and Oneida counties.
“There are many patient care and logistical advantages to providing hospital-based surgical care in a centralized location,” said LaFrance. “Together, we can create an efficient, cohesive team focused on the continuous growth of surgical outcomes and recovery for patients of Hamilton Orthopaedics through enhanced continuity of care.”
With the agreement, Hamilton Orthopaedics will continue maintaining and operating their out-patient offices. Oneida Health will also continue operating its orthopedic office, Oneida Health Orthopedics, in Oneida.
“We welcome Dr. Buckley and Dr. LaFrance to our Orthopedic Surgical team,” said physician M. Asad Khalid, chief of surgery and director of orthopedic surgery at Oneida Health. “Their addition to our orthopedic surgical team will increase access to more orthopedic services previously unavailable in Oneida for the communities we serve throughout Madison and Oneida counties.”
Mark Martens, MD • Amy MacDonald, MD
Tanya Paul, MD • Farkad Balaya, MD
At Auburn OBGYN & Women’s Health, we provide comprehensive, personalized care throughout every stage of your life. Our experienced team of physicians, certified midwives, and nurses offer a wide range of services, including routine well-woman exams, prenatal care, gynecological surgeries, and more.

“For many years, our community has needed increased access to orthopedic services,” said Felissa Koernig, president and CEO of Oneida Health. “The opportunity to partner with two locally renowned orthopedic surgeons, Dr. Buckley and Dr. LaFrance, and to bring their surgical services to Oneida only elevates the high level of orthopedic surgery Oneida Health already provides through Dr. Khalid and our Oneida Health Orthopedics team. With the development of this partnership and future growth, Oneida will soon become a destination for orthopedic surgical services throughout CNY.”





Say hello to a convenient way to stay healthy in Oswego County. ConnnextCare offers a comprehensive set of services - family and internal medicine, pediatrics, dentistry, psychiatry, substance use disorder treatment and social work all under one medical group. Patients within our network can visit any of our seven locations at any time.
ConnextCare also offers medical, dental and mental health services at nine School Based Health Centers in five Oswego County school districts.
WALK-IN APPOINTMENTS NOW AVAILABLE IN THE PULASKI ACUTE CARE SUITE MONDAY - FRIDAY 7:00AM - 6:00PM
Central Square (315) 675-9200 Fulton (315) 598-4790 Oswego (315) 342-0880 Pulaski (315) 298-6564 Parish (315) 625-4388 Phoenix (315) 695-4700 Mexico (315) 963-4133