BREASTFEEDING CONNECTION: NEURODIVERSITY IN BREASTFEEDING P.34 ISSUE 112 MARCH 2024 I THE MAGAZINE OF THE NEW ZEALAND COLLEGE OF MIDWIVES MIDWIFERY-LED TRANSITIONAL CARE IN AOTEAROA P.18 COLLEGE AND NGĀ MAIA SIGN PARTNERSHIP P.10 NEURODIVERGENCE IN PREGNANCY P.24

FORUM
FROM THE CO-PRESIDENTS
4. FOUNDATIONS FOR THE NEW YEAR FROM THE CHIEF EXECUTIVE
5.
ANCIENT AND EVER-EVOLVING
8. YOUR COLLEGE / BULLETIN
10. A NEW PARTNERSHIP
12. YOUR UNION
14. YOUR MIDWIFERY BUSINESS FEATURES
16. NGĀ MAIA
17. PASIFIKA
18. MIDWIFERY-LED NEWBORN TRANSITIONAL CARE IN AOTEAROA
24. NEURODIVERGENCE IN PREGNANCY
28. COULD THIS BE SEPSIS?
30. THE ONLY CONSTANT IS CHANGE
32. PROVIDING MEDICAL CERTIFICATES
33. A NEW HOUSE
34. BREASTFEEDING CONNECTION: NEURODIVERSITY AND BREASTFEEDING
38. READING CORNER
40. TAKU WĀHI MAHI / MY MIDWIFERY PLACE DIRECTORY
EDITOR
Hayley McMurtrie
E: communications@nzcom.org.nz
ADVERTISING ENQUIRIES
Hayley McMurtrie
P: (03) 372 9741
MATERIAL & BOOKING
Deadlines for June 2024
Advertising Booking:
1 May 2024
Advertising Copy: 13 May 2024




ADVERTISING POLICY AND DISCLAIMER: The New Zealand College of Midwives maintains a schedule of guidelines to exclude advertisements for products or services that are not aligned with its principles and ethics. Every effort is made to ensure that advertising in the magazine falls within those guidelines.
Where advertising is accepted, this does not imply endorsement by the College of the product or service being promoted
Midwife Aotearoa New Zealand is published quarterly for the New Zealand College of Midwives. The articles and reports printed in this newsletter are the views of the authors and not necessarily those of the New Zealand College of Midwives, its publishers or printers. This publication is provided on the basis that New Zealand College of Midwives is not responsible for the results of any actions taken on the basis of information in these articles and reports, nor for any error or omission from these articles and reports and that the College is not hereby engaged in rendering advice or services. New Zealand College of Midwives expressly disclaims all and any liability and responsibility to any person in respect of anything and of the consequences of anything done, or omitted to be done, by any such a person in reliance, whether wholly or partially upon the whole or any part of the contents of this publication. The College acknowledges and respects diversity of identities through the language used in this publication. Te reo Māori is prioritised, in commitment to tāngata whenua and te Tiriti o Waitangi. To maintain narrative flow, the editorial style may use a variety of terms. Direct citation of others’ work maintains the original authors’ language, and contributing writers’ language preferences are respected. All advertising content is subject to the Advertising Standards Authority Codes of Practice and is the responsibility of the advertiser. Contents Copyright 2020 by New Zealand College of Midwives. All rights reserved. No article or advertisement may be reproduced without written permission. ISSN: 2703-4546.
ISSUE 112 MARCH 2024 | 3 18 24
34 40
10
MIDWIFERY:
MARCH 2024
ISSUE 112
Welcome to Issue 112 of Midwife Aotearoa New Zealand
Welcome to the first issue of Midwife Aotearoa for 2024, what better way to start the year than a partnership agreement between the College and Ngā Maia. This agreement provides a solid platform for our organisations to work together with the shared aim of benefiting the women and whānau who midwives care for and to strengthen and grow the Māori midwifery workforce (p.10).
Another significant milestone for midwifery is the creation of the position Chief Clinical Officer for Maternity within Manatū Hauora, on p.11 we congratulate midwife Heather Muriwai who will take up this inaugural position with a pōwhiri on 4 March.
MMPO’s article looks at what AI means for health and more specifically midwifery. Do the benefits of time conservation outweigh the depersonalisation of service? There is certainly some balancing required as AI enters the midwifery profession.
The first feature article in this issue looks at transitional care in Aotearoa and celebrates the successes of this not-so-new service (p.19). The clinical update on pages 28 and 29 reminds us of the early signs of infection in both māmā and pēpē and the practice guidance articles look at issuing medical certificates and the recertification changes proposed by the Te Tatau o te Whare Kahu | Midwifery Council.
Page 22 calls for abstracts for the Joan Donley Research Forum that will be held over 24 and 25 October in New Plymouth. The local College region look forward to welcoming you all and showcasing midwifery research and their beautiful city.
We are also excited to bring the brandnew feature to this issue: taku wāhi mahi/ my midwifery place, where we celebrate the unique qualities of different midwifery workplaces across the motu over each coming issue. If you would like us to feature your workplace or have any other feedback, please let me know.
Ngā mihi nui, Hayley square
 HAYLEY MCMURTRIE EDITOR & PUBLICATIONS MANAGER
Email:
HAYLEY MCMURTRIE EDITOR & PUBLICATIONS MANAGER
Email:
communications@nzcom.org.nz


from the co-presidents
“Ki te ngaro ngā tikanga, ka ngaro te reo, ki te ngaro te reo, ka ngaro tātou te Māori” (If we lose tikanga, we will lose te reo, if we lose te reo, we will be lost) - Na Dr Pita Sharples
(1994)
BEA LEATHAM
Ko Papatūānuku te aina o tōku whare korero, ko Ranginui te tuanui, ko ngā poupou tapu o ia mana ariki ngā maunga. Me rere te kororangi o Whetumatarau ki a ia Marae, kāinga huri noa. Taiparatia ki tō tatou āpōpōtanga e!
The first quarter of 2024 is nearly over and for our first official column as co-presidents, we thought it best to partner up and share our visions for the future with our membership.
Our predecessor Nicole laid strong foundations and a legacy that I don’t take lightly. I have high expectations - not just of our College, but our profession as a whole. Gone are the days of tokenism; co-presidency is the most significant step the College has taken towards proving this to its membership, and now it’s our collective responsibility to ensure this translates into tangible, positive changes for the whānau we serve in our communities.
Under Aotearoa’s new coalition government we will no doubt face challenges, but we have the tikanga to guide us as an organisation, keeping the College accountable and truly responsive - not just to our profession, but to Aotearoa: a nation built on a foundation of partnership.
Ngākau nui, ngākau whakaiti. square
DEBBIE FISHER
Tēnā koutou, Hello, Mālō e lelei, Talofa lava, Taloha ni, Kia orana, Fakaalofa lahi atu, Namaste, Ni sa bula.
Here we are in 2024 with a fresh start to an exciting year ahead.
I’m so pleased to see new graduate midwives commencing and know they’ll be truly welcomed into our teams.
This year we’ll continue the work commenced by Nicole and the Board, focusing on midwifery retention and recruitment. There are also practical things we can all do every day to retain midwives in our regions; things that help us feel connected, like taking coffee to a busy colleague.
The most important part of any positive team culture is you, and in order to achieve what we aspire to in our diverse roles, our wellbeing, self-awareness and personal development are all essential. So, take a moment to think about how you can work with your brain biology to maintain a healthy mind platter.
As your College co-presidents, we are here to serve you and work towards midwifery being the career that brings out the best in you, rather than demanding the life out of you. I hope you’re ready to come with us. square
4 | NEW ZEALAND COLLEGE OF MIDWIVES MAGAZINE FROM THE EDITOR 4 | MIDWIFE AOTEAROA FROM THE PRESIDENTS

MIDWIFERY: ANCIENT AND EVER-EVLOVING
This year we welcome 150 graduate midwives to the profession, bringing their kete of hard-earned midwifery knowledge as well as their life experiences from Aotearoa’s many communities. Due to the incredible success of Te Ara O Hine / Tapu Ora, we are also welcoming the highest proportion of Māori and Pasifika graduates over the past two years than we ever have previously.
Although we have some way to go, it is exciting to see the ethnicity of our graduates diversifying to better reflect our population. Delegates at last year’s conference will remember the excitement we all felt about the future of midwifery when the students presented, and the thrill of the AUT Pasifika midwifery students “cheehoo!” as they shared their achievements. To all those completing their degrees and registering as midwives, I offer my heartfelt congratulations and a very warm welcome to our profession which is both ancient and ever-evolving – Nau mai, haere mai.
The transition to practice is exciting and often nerve-wracking as the full weight of responsibility lands. The early years in our midwifery careers are formative ones.
As today’s graduates are younger they are more likely to change their careers than graduates of previous generations. The support our graduates receive is influential in shaping their experiences of entering the profession, and also how long they choose to remain within it.
Since 2007, the College’s Midwifery First Year of Practice (MFYP) programme has supported more than 2,000 graduate midwives to navigate the journey from competent to confident midwife. Modelled on the concept of partnership, the programme centres the needs of graduates, providing wrap-around support within the programme’s structure. Just as our profession is constantly adapting to accommodate changes in practice and evidence, technological advances, and

from the chief executive, alison eddy
ISSUE 112 MARCH 2023 | 5
It feels as if it must be far more complex to be a graduate midwife in 2024 than it was when I graduated in 1997. Women’s notes were in a physical book, there was less expectation to order tests and investigations, and women largely received information from books or through conversations with their midwife, not through the internet.
cultural and social norms or expectations so we can continue to meet the needs of women and whānau, the MFYP programme has been continuously updated over the years. A formal evaluation in 2017 found it was achieving its aim of meeting graduates’ needs.
In 2023 the College’s board commissioned a cultural review of the organisation to support its endeavours to work in a Tiriti o Waitangi-honouring way and ensure its services are culturally responsive for tangata whenua. At our conference in November, Whaea Moe Milne and Linda Thompson presented the recommendations that they and co-author Koha Aperahama made in their report. These recommendations provide a roadmap for the College’s work into the future, including a review of key programmes and services.
After MFYP’s 17 years of operation, the College recognised the need for a refresh of the programme to ensure it was fit for the contemporary midwifery context and
responsive to our diverse graduate cohort, hence the establishment of an MFYP co-leadership model within the College staffing structure. At the same time, Te Whatu Ora (the contract funder) announced that it would resource a full refresh and redesign of the MFYP programme in line with the Pae Ora legislation. It was perplexing that Te Whatu Ora opened the tender up as a full RFP (funding proposal), given this was not the case for other professions’ first year of practice programmes. The College and Ngā Maia Māori Midwives partnered together to undertake an extensive process to tender for the redesign contract.
I am very pleased to announce that the College and Ngā Maia were successful in winning the redesign contract and I would particularly like to thank Midwifery Advisors Elaine Gray and Jay WaretiniBeaumont and Ngā Maia General Manager Tamara Karu for their hard work in writing such a high-quality proposal. The redesign is one of the first actions we are undertaking under the auspices of our newly minted partnership agreement with Ngā Maia (see page 10), and in line with the Cultural Review recommendations. The team working on the re-design will be engaging with graduates and other stakeholders over the coming months as this work unfolds. It is anticipated that the re-designed programme model will be ready for graduates from 2025 onwards.
It feels as if it must be far more complex to be a graduate midwife in 2024 than it was when I graduated in 1997. Women’s notes were in a physical book, there was less expectation to order tests and investigations, and women largely received information from books or through conversations with their midwife, not through the internet. Whilst technology was present, it wasn’t a large focus of our work – nobody had a smart phone. The means by which women access information in 2024 is completely different – the hyperconnected world the internet has created has had an influence on expectations and norms around birth for our society. The role of the midwife is now more about helping women make sense of information overload, to critically unpick misinformation or help them contextualise information from other countries for our Aotearoa New Zealand setting, as opposed to providing oneon-one education.
Despite the challenges, it is clear that midwifery has made a lot of progress since 1997. We have a well-established midwives’
union, and midwifery senior leadership positions in every hospital or district and also nationally. The LMC model is well embedded and midwifery-led continuity of care is an established norm within our system and culture. The World Health Organization has endorsed midwifery-led continuity of care as the preferred model within the evidence base and is in the process of developing implementation guidance to support the global expansion of this model.
In spite of our success with midwifery-led care, it has been hard to resist the increase in medicalisation and technological influences that our health system is subject to. The parameters around what is considered ‘normal’ seem to be forever shrinking, childbirth interventions are increasing, and our workforce is under stress with many areas struggling with recruitment and retention. We have a similar number of births now to 1997 and approximately 1,000 more practising midwives, yet our workforce shortages seem to be more acute than ever.
Midwifery exists within the wider cultural, social and political landscape in which we work. It has always sought to adapt and evolve whilst embracing the core values of the midwifery philosophy and model of care, which allow the flexibility to adapt and centre the needs of those who we are caring for.
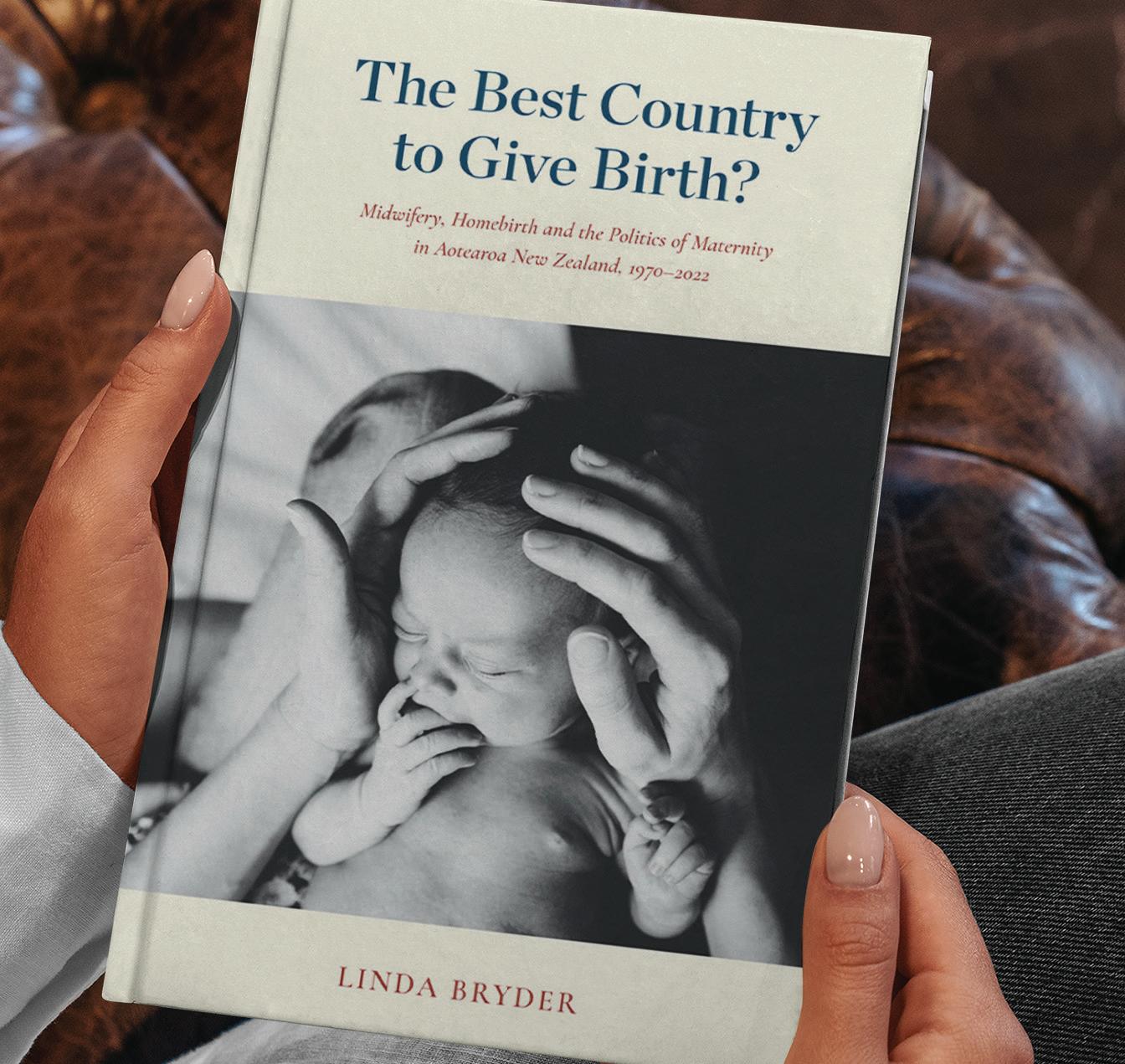
Health is inherently politicised as it affects every member of the population, and politicians are sensitive to how the public perceives health services to be functioning – none more so than maternity services. The very gendered nature of our work has meant that midwifery has had to be resilient in order to navigate its way through unfair criticism and unfavourable political climates. The recent publication of Linda Bryder’s book (see review page 38) shows that in spite of 30+ years of professionally autonomous practice, midwifery still faces discrimination and misrepresentation in how our profession and its history is interpreted. Midwifery has had to repeatedly prove the efficacy, safety and value of our services and now we also need to accommodate the challenges that globally connected information systems, exponential technological development, political polarisation and climate change are sending our way.
We are living in increasingly turbulent times both globally and within Aotearoa. War and civil unrest and increased climate-
6 | MIDWIFE AOTEAROA FROM THE CE

related and humanitarian crises are occurring. As I write this, it is the one-year anniversary of the significant Auckland, Hawke’s Bay and Tairāwhiti weather events. Although we are fortunate to live in a stable democracy, we are not immune to global political and social influences. The upheaval of the Covid-19 pandemic and its aftermath has acted as a lightning rod for anti-government sentiment across the world, which has been fuelled by political opportunists and contributing to lingering cracks in social cohesion. The recent change of government in Aotearoa has raised the temperature on debates about te Tiriti o Waitangi, how we address existing health inequities and how health services need to be provided to meet the needs of our people. These issues are complex and deserve thoughtful and respectful consideration.
The media environment we live with amplifies political rhetoric, hyperbole and emotive views, which only serve to increase division, leading to reduced tolerance and understanding. The impacts of colonisation and systemic discrimination continue to have a significant effect on the health and wellbeing of our people and we must continue to seek solutions to address this. It will be through identifying shared values that we will find a positive path forwards in working towards greater fairness and improved equity. We need to be able to have honest conversations, listen openly, seek to understand different points of view, examine why we feel uncomfortable, and foster tolerance as opposed to division and polarisation.
In spite of this turmoil, some things about midwifery will always remain the same. The creation of whānau, and the sense of satisfaction when you know you have made a difference to how a woman and her whānau experienced that journey remain deeply fulfilling. The mystery, adrenaline and excitement which surrounds birth, the collegiality that we share with each other, and our strong professional identity all nurture us in our work. It is the core tenets of midwifery practice, the philosophy and model of care that will support our profession and our graduates to remain resilient in the face of competing tensions and constant change. square


your college bulletin
quality assurance programme consultation
The College’s midwifery advisors, Te Paea Bradshaw and Brigid Beehan, are embarking on a consultation process centred on reviewing and redesigning the quality assurance programme for midwives, currently known as the Midwifery Standards Review. There will be various ways to participate in the consultation including virtual and face-to-face hui. The College values the voices of all midwives, whānau and stakeholders. Midwives are encouraged to actively participate in this process, providing valuable insights and perspectives to ensure that the revised Standards Review effectively addresses the needs of midwives, women and whānau. More information will be emailed to members over the coming months. square
international day of the midwife - 5th may 2024
This year International Day of the Midwife will fall on a Sunday. ICM have announced this year’s theme as 'Midwives - a vital climate solution'. More information and their promotional toolkit will be available from ICM shortly.
The Virtual International Day of the Midwife (VIDM) has a similar theme for 2024 - ‘Sustainable Midwifery: Caring for Tomorrow’s World’. This is VIDM’s 16th year providing a free 24-hour online conference held annually to celebrate International Day of the Midwife. For more information visit www.vidm.org square
ICM’s refreshed look and feel for their website
Over the last few months, the International Confederation of Midwives (ICM) has been hard at work reimagining their brand and revamping the website, giving them a fresh look and making them more accessible to more people - take a look at www. internationalmidwives.org square
maternity portfolio
Honourable Casey Costello has been announced as the Associate Minister of Health. Casey Costello, based in Pokeno, is a former Detective Sergeant, Vice-President of the Police Association, and spokesperson for Hobson’s Pledge. Costello first entered Parliament in 2023 and is the Minister of
Customs, Minister for Seniors, Associate Minister of Health, Associate Minister of Immigration, and Associate Minister of Police. Her health portfolio includes: Women's health (excluding cancer and cancer screening, perinatal and maternal mental health, workforce, and infrastructure); maternity health (including Plunket, but excluding perinatal and maternal mental health, workforce, and infrastructure); perinatal and maternal mortality; surgical mesh; sexual and reproductive health; the COVID-19 Inquiry; the Therapeutic Products Act 2023; emergency road and air services; family and sexual violence; surrogacy; dementia management; aged care.
Minister Reti has retained the health workforce portfolio, across all of the health professions, including midwifery. square
free online CBT courses for prenatal and postnatal wellbeing
Online mental health provider, Just a Thought, has launched its latest courses - Pregnancy Wellbeing and Postnatal Wellbeing. Using proven and effective cognitive behavioural therapy (CBT), these courses aim to provide
BULLETIN
8 | MIDWIFE AOTEAROA


Rural Student Midwifery Grant
Mary Garlick, a retired long standing rural midwife has generously granted a sum of money to the College to administer as an annual grant for midwifery students who intend to practise rurally on graduation. Applications will be accepted from students who are enrolled in the final year of a New Zealand Bachelor of Midwifery programme in 2024.
mothers who may be struggling with a tailored, accessible and highly effective treatment option without any cost or barriers to access.
These courses help empower new māmā with a kete of skills and strategies to support her wellbeing so she can focus on her growing whānau. For more information or to sign up and start prescribing these free courses, go to: justathought.co.nz/perinatalwellbeing square
family planning changes name after 85 years
Family Planning have rebranded as Sexual Wellbeing Aotearoa to better reflect the breadth of services they offer www. sexualwellbeing.org.nz square
national maternity clinical guideline webinars
Te Whatu Ora has published two clinician-led webinars to support the on-going implementation of the following national maternity clinical guidelines. The webinars and their transcripts can be found by scrolling to the bottom of the guidelines’ respective webpages:
1. Diagnosis and Treatment of Hypertension and Pre-eclampsia in Pregnancy in Aotearoa https://www.tewhatuora.govt.nz/ publications/diagnosis-and-treatment-of-hypertension-and-preeclampsia-in-pregnancy-in-aotearoa-new-zealand/
2. Guidelines for Consultation with Obstetric and Related Medical Services (Referral Guidelines) https://www.tewhatuora.govt. nz/publications/guidelines-for-consultation-with-obstetric-andrelated-medical-services-referral-guidelines/ square
Applications must be submitted via email to lynda.o@nzcom.org.nz by 1 May 2024, noting ‘Rural student grant application’ in the subject line. Further information and application forms are available on the College website www.midwife.org.nz
Midwifery students are eligible to apply for the annual grant if they meet the following criteria:
• Applicant must be a College member and enrolled as a final year student of an approved New Zealand Bachelor of Midwifery programme for 2024.
• Applicant must intend to practise as a rural midwife in New Zealand on graduation. Preference may be given to those intending to practise as an LMC.
To apply, applicants must:
• Demonstrate a commitment to rural midwifery practice on graduation
• Complete the application form and ask two referees to complete the relevant form. One referee must be a lecturerat the midwifery school in which the student is enrolled and the other, a midwife who the student has completed a clinical placement with.
NB: One grant will be awarded per annum.
The Midwifery Student Rural Grants Advisory Committee will award the grant.
college and ngā maia sign partnership agreement
Nāu te rourou, nāku te rourou, ka ora ai te iwi.
With my food basket and your food basket, the people will thrive.
The College has included Māori representation in its governance structure since 1992, with Mina Timutimu being the very first Māori midwifery representative to be appointed to the National Committee.
At that time there was no collective entity representing the interests of Māori midwifery, until the establishment of Ngā Maia in 1993. Since 1997 the College has included two dedicated places for Ngā Maia representatives within its governance structure – the National Committee (now the National Board) - alongside the position of kuia, which is now held by Crete Cherrington.
Over the years the College and Ngā Maia, two autonomous organisations, have sought to work together through various means with the shared aim of benefitting the women and whānau who midwives care for, and to strengthen and grow the Māori midwifery workforce. There have been some seminal events along the way, including the College’s adoption of Ngā Maia’s Turanga Kaupapa in 2007 alongside the Standards for Midwifery Practice to guide and support midwives in providing culturally safe care.
As the number of Māori midwives has grown, so too has the capacity, mauri and vitality of Ngā Maia. Following the
College’s cultural review last year, the College and Ngā Maia have been discussing the formalisation of our relationship through the establishment of a partnership agreement. The purpose of this agreement is to enhance and facilitate the aims of each organisation to ensure equitable outcomes for wāhine hapū and whānau Māori.
The agreement recognises the roles that each organisation plays within a partnership model, under Te Tiriti O Waitangi, recognising each party's responsibilities to support the best interests of each other’s organisations.
Specific actions each party is committed to include ensuring representation on each other’s governing bodies with ongoing Ngā Maia representation on the College’s board and a dedicated place being established for the College’s tangata whenua co-president on the Ngā Maia board. The agreement also recognises the need for the College regions and Ngā Maia regional roopu to work together to support our respective memberships at a regional level, as well as nationally.
This significant milestone in the relationship between Ngā Maia and the College occurred in Auckland on the 21st of February where the agreement was formally signed at a meeting of representatives from each organisation. square




10 | MIDWIFE AOTEAROA FORUM




Changing Birth Culture One
Birth At A Time
Apply now to become a Calmbirth® Educator in Aotearoa New Zealand. calmbirth.nz

opportunities available!

Are you looking for a new adventure? Would you like to join an enthusiastic and supportive team and community with a lifestyle second to none? We are a small secondary rural hospital focused on providing equitable women centred care with the opportunity to provide midwifery care across the scope.
If you are a Registered Midwife and want to be part of a dynamic and committed team of health workers providing an innovative approach to healthcare in a rural setting, and you are seeking a new challenge or to broaden your midwifery experience we may have the role for you!
We are interested in what hours of work may suit you. We are happy to accommodate a range of options including full or part-time, permanent
An attractive relocation package including accommodation and travel assistance is available for both domestic and international successful with further education and learning opportunities.
To learn more about the role, or for a friendly informal conversation please contact: Laura Ashwell, Interim Clinical Midwife Manager on Laura.Ashwell@wairarapa.dhb.org.nz +64 (6) 946-9800 ext. 4111
To apply or for a copy of the job description, please visit www.tewhatuora-wairarapa-careers.co.nz Vacancy Ref # 5473865
Image: Angela Scott Photography
 CAROLINE CONROY MERAS CO-LEADER (MIDWIFERY)
CAROLINE CONROY MERAS CO-LEADER (MIDWIFERY)
when things aren't going well in the workplace
Our workplaces are complex, dynamic places and there has been considerable change over the last two years since the transition from 20 district health boards to Health NZ - Te Whatu Ora. Part of that change has included the development of Te Mauri o Rongo | The NZ Health Charter.
The Charter outlines how workers can expect to be treated in the workplace and the engagement and relationship that should occur with unions. Whilst the intent of the Charter is positive, this might not be the reality that members are experiencing in the workplace. There are times when things are not going well for individual members or for members as a collective group in a workplace; examples of this can include:
The aspiration of Te Mauri o Rongo is to provide direction as to how people have told us they would like to be treated. It is a statement of the values, principles and behaviours that we want the health workforce to demonstrate individually, collectively and by the organisations.
For that to happen, Te Mauri o Rongo will need to shift all aspects of our thinking, decision making and operations to become an enduring influence, to improve relationships in the workplace and across the health sector. It must be a living document that guides us as we go.
Te Mauri o Rongo is my commitment to the health workforce to ensure that all health and care workers are supported, valued and respected, now and into the future. It is my recognition of the health workforce collective who work hard every day to improve the care of everyone, often under very challenging circumstances.
As a clinician, I want those coming through to have a better experience of work than I did.
- Minister of Health Hon Dr Ayesha Verrall - July 2023
CHANGES IN THE WORKPLACE
Change management processes are clearly outlined in the MERAS Collective Agreements. It is important that any changes proposed are clearly outlined in writing, that there is time for discussion and feedback and that genuine consideration is given to that feedback. Ideally MERAS representatives and organisers should be involved in reviewing the feedback and drafting the decision report. Simply being told about a change is not consultation.
Even on what might appear relatively minor changes in a workplace such as rearranging the office, it is important that changes proposed are discussed and there are opportunities for other ideas or options; often changes can be tried as a pilot and, if not working, other options explored.
Creating a workplace where staff feel able to make suggestions on changes that could occur in their workplace, and are able to lead the discussion with colleagues, contributes to creating positive workplaces where midwives feel valued and respected.
MERAS is not always advised of change occurring in a workplace so if change is occurring and this is causing concern, ensure your local MERAS workplace rep is aware of your concerns and they have also advised MERAS staff. If made aware of issues arising in your workplace MERAS are in the best position to support you.
Te Mauri o Rongo | The NZ Health Charter, is a requirement of the Pae Ora (Healthy Futures) Act 2022 and provides a clear steer on how the health workforce must be treated while at work.
12 | MIDWIFE AOTEAROA YOUR UNION
Te Mauri o Rongo | The NZ Health Charter
INCORRECT PAY
If you think you have received the incorrect pay (either over or under payment) report this as quickly as possible by email to your line manager. Doing this by email maintains a paper trail and if need be, you can also escalate and include the MERAS organiser in those emails.
EXPECTATIONS NOT BEING MET FOR NEW GRADUATE MIDWIVES OR NEW TO SERVICE STAFF
If you were given expectations at interview, for example of orientation, preceptors or being supernumerary for a set number of weeks and this does not occur, talk to your manager and local MERAS workplace representative as soon as possible. Clinical safety issues can arise if you are not well supported in your orientation period, and it impacts on the retention of new graduate or new midwives.
UNSAFE STAFFING
With the current midwifery workforce shortage there can be times when that shortage creates unsafe situations.
The Care Capacity Demand Management (CCDM) programme, which includes Trendcare and VRM/VIS, is intended to highlight escalating acuity or workforce pressures. There should be an escalation plan in your workplace and actions that should be taken when there is ‘unsafe staffing’. Incident reports (safety first or datix) should be completed in these situations, it is also important MERAS is informed if unsafe staffing situations are occurring on a regular basis as there is an expectation in the MERAS Collective Agreements that MERAS representatives will be involved in the

investigation and corrective measures of any unsafe staffing incident reports.
When things are not going well in your workplace it is important that those issues are discussed and a plan is put in place to address them. When issues are left unresolved it can impact on retention of staff and clinical safety. MERAS is here to support you in raising those concerns and working with you, local MERAS workplace representatives, your managers and Directors of Midwifery to resolve any issues and find solutions.
Don't hesitate to contact MERAS for support if things are not going well in your workplace. square

For MERAS Membership merasmembership.co.nz www.meras.co.nz
ISSUE 112 MARCH 2024 | 13 YOUR UNION
 WAYNE ROBERTSON EXECUTIVE DIRECTOR, MMPO
WAYNE ROBERTSON EXECUTIVE DIRECTOR, MMPO
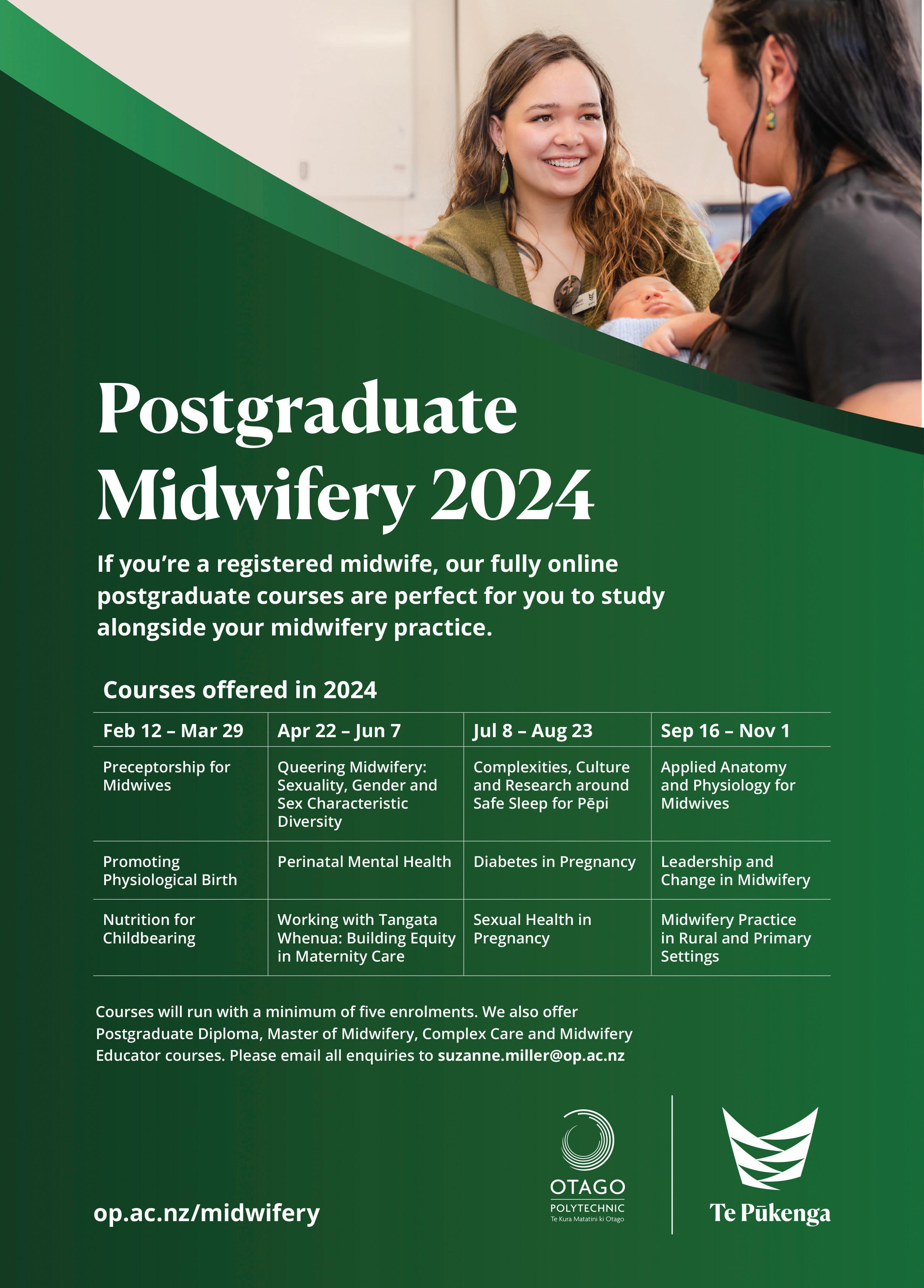
is there a future for midwifery and artificial intelligence?
In recent years, artificial intelligence (AI) has progressively edged into various sectors, wider healthcare being one of the most significant. ChatGPT, an AI chatbot developed by OpenAI, was launched to the public on November 30, 2022. By January 2023, it had become what was then the fastest-growing consumer software application (not just artificial intelligence) in history, gaining over 100 million users since its introduction.
WHY ALL THE HYPE ABOUT AI?
The anticipation surrounding AI is largely due to its transformative technological capabilities to process and learn from vast datasets. This learning enables efficiency improvements, innovation and enhanced decision-making that could directly contribute to improved outcomes and quality of life, fuelling the hype and optimism about its potential.
IS IT ALL HYPE OR ARE THERE REAL BENEFITS TO BE GAINED?
For a midwife providing care in Aotearoa the immediate benefits of properly designed AI would be the freeing up of their time to focus on more personalised maternity care (instead of less productive administration), improved decision-making and helping to achieve a better midwifery work-life balance.
Specific examples of how AI might help a midwife in Aotearoa in the future could be creating an initial personalised care plan for midwife review, predictive analytics for early risk detection (maybe incorporating smart digital wearables), access for māmā and whānau to virtual assistance for routine pregnancy questions, optimised scheduling for the midwife (based on their availability, geographical location and urgency of request), easier access to continuous learning and knowledge updates, and maybe routine diagnostic support.
The use of AI is provoking broad and challenging discussions. Not only is it early days for most people, but AI also comes with its own set of challenges, including:
14 | MIDWIFE AOTEAROA YOUR MIDWIFERY BUSINESS THE HYPE Greater Efficiency and Speed Increased Automation of Repetitive Tasks Better Data Analysis and Insights Supporting Greater Personalisation Enhanced Decision Accuracy and Precision
• The potential to disrupt the future of work: (including job displacement) particularly in sectors heavily reliant on routine tasks, leading to economic and social challenges.
• Ethical and privacy concerns: AI's ability to analyse and utilise personal data raises significant privacy issues, and the decisionmaking process of AI can sometimes lack transparency, leading to ethical dilemmas.
• Expected high cost of implementation: Developing, implementing and maintaining AI systems (including technology and training) can be expensive, particularly for small organisations, potentially widening the digital divide.
• Dependence on data: AI systems are only as good as the data they are trained on; biased or poor-quality data can lead to inaccurate outcomes, resulting in flawed decision-making.
• Risk of depersonalisation: Midwifery is deeply rooted in personal relationships and trust between the midwife and the māmā and whānau that they serve. There's a risk that an over-reliance on AI could lead to depersonalisation of care, where the midwifery response is dominated by technology.
• Lack of emotional intelligence: Despite advances, AI cannot currently replicate human empathy and emotional intelligence, potentially leading to a lack of warmth or understanding. Soft skills such as empathy, understanding, intuition and reassurance are crucial requirements to realise trust and delivery equity and best maternity care outcomes.
It is worth exploring the last two points more as they are critical midwifery ingredients to creating and maintaining a deep trusting relationship with the māmā and the whānau. Any failing or limitation because of AI (such as those detailed below) can make the delivery of equitable high quality midwifery care more challenging.
• Lack of genuine empathy: While AI can be programmed to recognise certain emotional cues and respond in predefined ways, it lacks the genuine empathy and deep emotional understanding that midwives offer. AI responses are based on algorithms and patterns, not on true emotional connection.
• Limited intuition: AI lacks the intuitive understanding that comes from human experiences and the subtle nuances of interpersonal communication. While AI can
analyse data to make predictions, it cannot sense emotions or read between the lines in the way a midwife can.
• Consistent but inflexible communication: AI can provide consistent information and support but lacks the ability to truly adapt its communication to the emotional needs of the moment. It may not always recognise the need to soften its approach or offer support beyond its programmed responses.
• Absence of physical reassurance: AI cannot replicate the physical presence and reassuring touch of a midwife. The lack of physical comfort and presence can be particularly felt in midwifery, where such gestures are an integral part of care.
THE CRITICAL IMPORTANCE OF MAINTAINING A BALANCE BETWEEN TECHNOLOGICAL ADVANCEMENT AND THE HUMAN TOUCH
AI’s future application in healthcare, and in particular midwifery, presents a unique and challenging intersection of technology and māmā (and whānau) centred midwifery care, with the thought-provoking potential of enhancing the care provided to māmā and whānau while, at the same time, supporting midwives in their roles.
While the potential of AI can complement equity, midwifery outcomes and midwife sustainability (and work-life balance) it falls short of replicating the personalisation of care and emotional intelligence of midwives.
Any future integration of AI must be approached with sensitivity to ethical considerations and a commitment to protecting and maintaining the irreplaceable human essence of midwifery, including emotional support, empathy and intuitive care that continues to be provided by midwives in Aotearoa.
As an aside, this article was written in balanced partnership between myself and ChatGPT. square

MMPO provides self employed community midwives with a supportive practice management system.
www.mmpo.org.nz
mmpo@mmpo.org.nz
03 377 2485
ISSUE 112 MARCH 2024 | 15 YOUR MIDWIFERY BUSINESS
 TAMARA KARU
NGĀ MAIA GENERAL MANAGER
TAMARA KARU
NGĀ MAIA GENERAL MANAGER
we need allies!
The proposed state sector cutbacks and coalition policies pose significant challenges for Māori health professionals. It is crucial to express support for your Māori colleagues at this time and actively advocate for their rights and contributions to the midwifery profession.
Māori health professionals and Māori providers are truly integral to the health sector. Their work goes beyond providing care, extending to advocacy, research and community engagement that improves the health and well-being of all communities.
The coalition agreement reads like an “Anti-Māori Manifesto” according to Māori in opposition. I agree it sets a clear agenda that this government intends to enable policies that uphold the privileged. Preserving privileges can be seen when people are in opposition to
things like the use of Te Reo Māori by government departments and by the blatant placing of Te Aka Whai Ora on the scrap heap. These actions give me no confidence in the ability of this government to reduce health inequity or be Te Tiriti honouring.
I am personally disturbed by the motivations of this government to reinstate pseudoephedrine availability while relaxing tobacco controls. Who benefits from this? It feels like sabotage. How can midwives reduce the rate of SUDI when we can almost predict a direct link between this government's policies and future SUDI rates. Roma Balzer once said “to be Māori, is to be political” when recalling a time when identifying as Māori meant being targeted, an outcast. Welcome to the past. Unfortunately, this is common ground for Māori. We are used to this behaviour; we confront racism daily. As Māori, we have no choice but to stand up for ourselves, stick our necks out. We have had to learn a set of skills, be defiant and to not allow noise to distract us from ensuring that the Māori communities receive culturally safe, equitable and accessible healthcare.

Hence, Ngā Maia are committed to the reinvigoration of Turanga Kaupapa training throughout 2024. We plan to do this in two cohorts: one for tangata whenua and one for tangata Tiriti, both virtual and face-to-face. We are also excited about working in partnership with the College to re-design the MFYP (Midwifery First Year of Practice) programme to better meet the needs of Māori new graduates.
The Māori health workforce and Māori providers deserve recognition for the many service innovations they have developed while working in a Western Eurocentric health system. Kaupapa Māori models are innovating across the country, where Western models fall short. Innovations such as Hapū Wānanga are thriving and influencing a new way of working.
Unity among Māori, coupled with the support of allies, can serve as a powerful force against what can only be described as the sabotage of Māori success. Unity among Māori is the call of Kīngi Tūheitia and the many that attended a Hui-ā-Motu at Tūrangawaewae Marae January 2024. It is therefore up to you to react and defend our whānau. Put simply, Māori communities and your Māori colleagues are suffering, you should tend to them. square
16 | MIDWIFE AOTEAROA NGĀ MAIA

capital gains
Whilst the majority of Pacific peoples reside in Tamaki Makaurau, there are also a number of midwives and students practising and studying in other city centres around the motu serving Pacific communities.
In Poneke Wellington, our profession is alive and well through the Pasefika Midwives Collective (PMC), consisting of Fana TemeseTo’omaga, Penina Fitisemanu and Therese Stowers, who have many years of practice between them either in core settings or as LMCs in the community.
Since 2020 PMC has been providing services specifically tailored for Pacific women in and around Porirua and greater Wellington. The first of their projects was the Tina (Māmā in Samoan) Initiative, providing antenatal classes in a Pacific context for women and their aiga (whānau). This service has been delivered through education and information talanoa (Samoan: discussion) in a familial environment conducive to reciprocal participation.
The Wellington region, with a Pacific population of 47,774 as at the 2018 Census, had not had antenatal classes provided with a Pacific lens before. PMC’s mission statement simply expresses that it provides opportunities for Pacific women to connect with and support each other through their pregnancy journey. The need for ‘connection’ to others was vital, as was ‘support’ in navigating the maternity system as well as the physiological process. PMC hope that this service will continue past the initial 3 years of funding it received.
Also in 2020, Te Ao Marama Midwifery Tapui Ltd (TAMM) was established to provide culturally responsive LMC care in Porirua. The Te Ao Marama Collective emerged through a desire to better support Māori and Pacific women through appropriate and accessible care, that was locally available - care for the community, in the community and by the community.
This team of Māori and Pacific midwives numbers 5 currently (Cherie Parai, Leilani Va’a, Wendi Robinson, Jardy Bridgeman and Fana Temese-To’omaga) with 3 new graduates (Anahera Ngatai, Kauia Tipene and Grethe Andersen).
Fana states, "we provide team care, and we work a 12-hour on call roster for labour and birth and make no apologies for this style of practice. Our desire is to serve our community and have a work/life balance for ourselves as well as supporting students through their training and increasing the workforce”. The purpose of TAMM is to:
• Provide a culturally appropriate service
• Provide continuity of care by, and for, Māori & Pasifika populations
• Improve early engagement with maternity services for Māori and Pacific women
• Improve quality and standards of care for Māori and Pacific women
• Support a sustainable LMC workforce
• Develop pathways and mentoring/coaching support for the Māori and Pacific midwifery workforce, particularly for new graduates
• To grow Te Ao Marama Midwifery as a model of care for Māori and Pacific people.
This year TAMM is expanding out to the Hutt Valley. Three of their midwives are from the Hutt, so it’s only fitting that they would eventually move in that direction.
They are feeling blessed to secure the fit-for-purpose Te Awakairangi Birthing Centre for the next 12 months as their Hutt base, and they are looking forward to serving families in the Hutt and working together with the wider community to support this direction. This will be a great opportunity to revive primary birthing in the area.
Finally, the presence of Pacific Midwifery Liaison roles for Otago Polytechnic Te Pūkenga and Te Herenga Waka Victoria University, by Esther Manville and Fana Temese-To’omaga respectively, under the National Te Ara o Hine - Tapu Ora programme, are fulfilling the support for workforce development and sustainability to curb attrition rates of the precious few Pacific students in the regions. Feedback from national fono (meetings) always have comments from students citing this valuable support on campus.
Tautua nei mo sou manuia taeao, Serve now for a better tomorrow! square
Since 2020 PMC has been providing services specifically tailored for Pacific women in and around Porirua and greater Wellington. The first of their projects was the Tina Initiative, providing antenatal classes in a Pacific context for women and their aiga.
PASIFIKA
FANA TEMESE-TO’OMAGA
ISSUE 112 MARCH 2024 | 17
TE AO MARAMA MIDWIFE

18 | AOTEAROA NEW ZEALAND MIDWIFE

 AMELLIA KAPA REGISTERED MIDWIFE
AMELLIA KAPA REGISTERED MIDWIFE
MIDWIFERY-LED NEWBORN TRANSITIONAL CARE IN AOTEAROA
Midwifery-led newborn transitional care isn’t a new concept. In fact, Robynne Hubbard and Caroline Conroy were providing it in a primary maternity setting before it even had a name. Counties Manukau remains the only rohe in Aotearoa where this model of care is being provided in primary birth units, but a dedicated unit now exists at Auckland City Hospital, with more services emerging nationally. Amellia Kapa talks to midwives working in this specialised area about why it’s vital for whānau.
It was 2002 and Midwife Manager of Papakura Birthing Unit Robynne Hubbard took a phone call, not realising just how pivotal it would turn out to be. “The paediatric consultant from Middlemore Hospital called and asked if we could take a baby. He was pre-term and didn’t need intensive care anymore, but still needed to transition from nasogastric (NG) tube feeds to breastfeeding,” she begins. “As a midwife, I’d never thought about looking after a premature baby and I still remember the night they arrived, which was a Friday. He must have been just over two kilograms and I freaked out initially,” she laughs.
“It was pretty innovative,” Caroline Conroy elaborates, “and a reflection of Robynne’s leadership, as well as the dynamics of the unit at the time.
The baby’s mum was self-employed - running a business with her husband - and struggling to be at Middlemore Hospital for any length of time because she had other children, which was making it hard to establish breastfeeding. She’d indicated it would be much easier if baby could come to Papakura, because she only lived just down the road.”
Distances in Auckland aren’t just about kilometres, as Caroline points out, and can be particularly problematic when babies are requiring specialised care. “Papakura’s a 30-minute drive from Middlemore, but it often takes longer in Auckland traffic and it’s quite a convoluted route once you get off the motorway. The train also takes 30 minutes, so either way it’s an hour round-trip, which not only has a time impact, but a significant cost impact too.”
ISSUE 112 MARCH 2023 | 19 FEATURE
The answer to the consultant’s request was therefore an obvious one, as Robynne explains. “If mothers can’t get in to NICU, they’re not bonding with their baby, and nor is the rest of the whānau. So we said, ‘Yeah, let’s do this. It’s easier for this mum and we have the space, so why not? It’s within the midwifery scope of practice; it’s about establishing breastfeeding’. A few of the midwives had also worked in tertiary settings, so we were familiar with NG tubes and it didn’t phase us.”
Obvious as the solution was, it was still controversial at the time, and Robynne explains the decision was met with understandably mixed responses. “There were lots of conversations and questions around whether it could even be called midwifery care, because the baby was already 85 days old when he came to us, having been born at 30 weeks gestation. But it was about getting those longterm neonates out of NICU and transitioning closer to home, where the siblings could also visit. That was - and still is - the gold standard; to improve the overall family dynamic by keeping the mother and baby together as that breastfeeding dyad, while ensuring mum is still supported to care for the rest of her whānau if she needs to pop home and settle older children at night, for example.”
The experience was a success and the rest is history, as Robynne reflects. “The care went really well, so then NICU asked us if we could take another baby, and we decided we could take a maximum of two transitional care babies at any one time. They’re generally with us for around one to two weeks, so it does mean those rooms are occupied.”
Over time, it became obvious that both whānau and staff could benefit from the development of consistent guidelines, so unit staff took the lead. “We developed some principles of care outlining what we did,” Caroline explains, “from the decision points prior to admission, through to what needed to be done at admission depending on factors like whether mum was a boarder or an in-patient; the importance of assessing the first feed; how top-ups were to be given; and how often the babies would be weighed, so that everyone was always on the same page.”
Other primary units in Counties Manukau followed suit, with Botany and Pukekohe also opting to provide transitional care so that whānau could be closer to home sooner, rather than later. South Auckland midwives could have been forgiven for believing the model had been adopted nationwide, but in her role as MERAS Co-Leader, Caroline was visiting maternity facilities all throughout Aotearoa and knew otherwise. Years after Papakura had accepted their first transitional care baby, Counties Manukau remained an anomaly, so Caroline suggested they
present the work they had been doing at the 2016 New Zealand College of Midwives conference in Auckland.
“I realised we hadn’t actually recognised how innovative we’d been. Nowhere else in the country was providing transitional care in a primary setting. We’d already been doing it for years at that point, but we’d taken it for granted; it was just business as usual for us and we’d accepted it as normal. Then when we’d get new staff from other units and it was quite funny watching their reaction, because they’d never seen or done it anywhere else.”
“In our presentation at the conference workshop we talked about transitional care being: the transition of the mother from visitor to primary caregiver; the transition from care in a neonatal unit to care in a maternity service; and the transition from a medical model of care to a midwifery-led model of care. And that’s what defines it as midwifery-led; we’re growing the mother’s confidence in being the primary caregiver, supporting breastfeeding, and making sure she’s got all of the parenting knowledge she needs.”
Following the conference workshop, Robynne and Caroline were invited to Auckland City Hospital, to speak to their neonatal unit about the work they were doing, and Caroline recalls the team being impressed. “It was pretty radical,” she emphasises. “It was an equitable approach before equity was being talked about in those terms.”
Robynne concurs that providing transitional care in primary settings is certainly more equitable than the alternative, although underlying systemic issues are still at play. “I certainly believe we’re working well towards it, but I still feel there’s a long way to go because although it might seem equitable, some mothers still don’t get to pop home because they don’t have the petrol to go back and forth. We’re meeting the needs in terms of keeping mum and baby together, but those wider socio-economic factors are still impacting the whānau.”
Having spent her entire 30-year midwifery career at Papakura’s birthing unit, Robynne is very well integrated in her community and understands its needs better than most. “Papakura is definitely a high deprivation area. These whānau can’t afford not to breastfeed, so the reason we do things the way we do is to maintain the mum-baby dyad and support the mum’s mental health, in the real world. In her real world.”
More than 15 years after Robynne and her team pioneered midwifery-led transitional care in Papakura, a national review of neonatal care was commissioned by the Ministry of Health and published in 2019. The report affirmed what Robynne and her colleagues already knew, highlighting the provision of transitional neonatal care as a potential solution to ameliorate the nationwide pressure on NICUs.
In November 2021, Te Toka Tumai-Auckland City Hospital responded with the opening of Whitinga Ora Pēpi - its own transitional care unit. Bringing together expertise from midwives, neonatologists, NICU nurses and the wider multi-disciplinary team in a hybrid model, Whitinga Ora Pēpi is a collaboration between Starship’s NICU
20 | MIDWIFE AOTEAROA FEATURE
The New Zealand Midwifery Council (2019) defines the six-week postnatal period as commencing from the expected date of birth, rather than the actual date of birth, meaning it is within a midwife’s scope of practice to provide care for pre-term babies beyond six calendar weeks.

and the tertiary hospital’s high-risk antenatal/postnatal maternity ward.
Co-charge of Whitinga Ora Pēpi and Midwife Manager Rebecca Clark explains the unit’s unique approach. “We’re whānau-centred and whānau-led,” she begins, “with wraparound support from our midwifery, nursing and wider multi-disciplinary team. NICU and the Women’s Health department have worked side-by-side for many years, but this is the first time we’ve formally collaborated. We had to truly integrate the care to provide this service.”
An eight-bed unit made possible with funding from the Starship Foundation, Whitinga Ora Pēpi is staffed by both midwives and NICU nurses, and Rebecca explains the result is a seamless, cohesive service that’s able to cater to wāhine still requiring obstetric care. “Through this approach, midwives and nurses are able to share their expertise with each other, so there’s real collaboration happening every day.”
Rebecca explains Whitinga Ora Pēpi ensures pēpi are receiving care that is appropriate for their age and stage. “We knew there was a need for a unit like this and we had a lot of international evidence to support the provision of transitional care. The goal is to keep whānau and pēpi together in a unit that’s focused on empowering and supporting whānau to care for their own pēpi as they transition to home.”
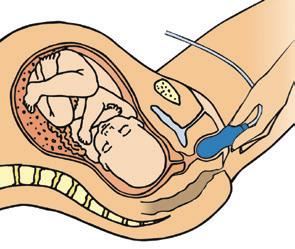
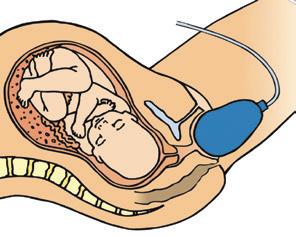
“In general,” she clarifies, “the criteria for admission to Whitinga Ora Pēpi is that the baby is late pre-term or small for gestational age, weighing more than 1800g, and no longer requiring any intensive monitoring or breathing support. These pēpi are not quite ready to go home, but also not needing intensive care and the focus is on establishing breastfeeding - transitioning from NG tube to oral feeds - and instilling confidence in whānau to care for their baby and take them home.”
In 2022, Whitinga Ora Pēpi cared for 265 māmā and 320 pēpi, with a significant number of twins admitted to the unit. A survey offered to all whānau who stayed in the unit in its first 12 months reveals the positive difference the unit has already made, with 85% of respondents saying they felt that being able to room-in 24/7 with their pēpi helped with bonding and attachment, and 87% saying they felt Whitinga Ora Pēpi helped build confidence in preparation for going home.
“We’re whãnau-centred and midwifery-led,” Rebecca explains. “Whānau are at the centre, taking the lead in the care of their pēpi, with a midwife specialist planning the care alongside them, and nursing staff delivering the care and supporting the teaching. So even though we have input from a multi-disciplinary team when needed, it’s the midwife specialist who guides care and discharge plans with whānau.”
As her passion project, Rebecca was excited to take on the role of managing Whitinga Ora Pēpi after years
FEATURE ISSUE 112 MARCH 2023 | 21
of already working on the hospital’s high-risk postnatal ward. “Whitinga Ora Pēpi is dear to my heart. I’ve seen the positive impact it’s had and its continued success is really important to me not just as a manager, but as an individual.”
The ripple effect for her entire team is also evident. “The feedback from our midwives is that they love working in Whitinga Ora Pēpi because they have the time to provide high-quality care and feel as though they’re making a real difference. They can see that evolution from admission to discharge and how their involvement has helped ease the journey home for a whānau. Job satisfaction has increased dramatically as a result,” she beams.
After more than 22 years of experience in the area, Robynne’s belief in the transitional care model is unwavering. “If we didn’t have transitional care, a lot more babies would be sitting in ‘feed and grow’ units, not being visited, and with very limited access to what a baby needs: whānau input and cuddles. I believe every primary unit should be providing transitional care and if regions don’t have that capacity, consideration should be given to how midwifery-led transitional care could be provided.”
With planning for the provision of transitional care currently under way in a number of regions throughout Aotearoa, a national resource has now been developed with input from Caroline Conroy and College Policy Analyst
and Lactation Consultant, Carol Bartle. The working group also included other midwives, neonatologists, NICU nurses and paediatricians, with the resource aimed at offering information to help guide health professionals providing newborn transitional care. In addition to defining principles of care, the resource includes generalised criteria (although these will vary depending on setting) and kōrero surrounding culturally safe practice.
Caroline argues transitional care is relevant now more than ever. “Because neonatal care has extended to earlier and earlier gestations, it means the babies receiving intensive care are even more complex now than they used to be, so despite the expansion of Middlemore’s NICU and other NICUs around the country, transitional care in primary units is absolutely still needed.”
Like Robynne, Caroline agrees Aotearoa needs more transitional care provision, specifically in primary maternity settings. “This can be midwifery-led,” she insists, “and that’s where we need to challenge the status quo, I believe. In secondary or tertiary units there’s always that potential for everything to still require medical oversight, whereas babies in our primary units are exclusively under midwifery care. If we have any concerns, we simply phone the neonatal unit in the same way we would for any other baby, but it’s primarily about establishing breastfeeding, which sits entirely within the realm of the midwife. And that’s what we need to remember.” square
22 | MIDWIFE AOTEAROA
C ALL FOR ABSTRACTS NOW OPEN The purpose of the forum is to provide an opportunity for midwives and others to share ideas, experiences and knowledge t hrough research, audits and p ostgraduate studies relating to m idwifery and maternity care. N EW PLYMOUTH PLYMOUTH INTERNATIONAL HOTEL 11t h B i e n n i al Joan Donley miDWiFe r Y researCh ForUm 2 4 & 25 Oc to b e r 202 4 For further information and submission guidelines visit our website midwife.org.nz Call for abstracts closes 19 April 202 4 FEATURE

Midwifery Postgraduate Education Grants
Midwives who are engaged in formal postgraduate education (at Level 8 or above on the NZQA framework) may apply for a grant towards the cost of their postgraduate study. These grants are funded by Te Whatu Ora - Health New Zealand and administered by the College to subsidise the costs of fees, some travel, and accommodation. Applications are prioritised on a first come first served basis.
For more information and to apply visit: www.midwife.org.nz.
Student Midwifery Grants 2024
The College is offering grants to assist students at each midwifery school who are currently undertaking a Bachelor of Midwifery programme. Grants are available for each school of midwifery. Please refer to the College website for further information and application forms: www.midwife.org.nz
Applications open on 1 May 2024
Funded by:

ISSUE 112 MARCH 2023 | 23


neurodivergence in pregnancy
Everyone has communication or sensory differences, but neurodivergent whānau face additional challenges and obstacles in these areas, which can impact their midwifery experience. This article offers advice on accommodating such differences, broadly applicable to all neurodivergent whānau.
WHAT IS NEURODIVERGENCE?
To be neurodivergent or have neurodivergence is to have a brain that has developed or functions differently from the majority. Current estimates suggest that as many as 20% of the population are neurodivergent.
While autism/Takiwātanga and ADHD/Aroreretini are the most widely recognised neurodivergent conditions, Tourette’s syndrome, dyslexia, and anxiety fall under this umbrella. While most neurodivergent conditions are congenital, some conditions (e.g. PTSD) are acquired, meaning that in certain circumstances neurodivergence can be temporary depending on the aetiology of the condition and its treatment.
NEURODIVERSITY AND NEUROAFFIRMING MIDWIFERY CARE
NEUROAFFIRMING COMMUNICATION
Our ability to communicate clearly and effectively is not just impacted by traditional norms of fluency, literacy and health knowledge, it also depends on the environment, stressors brought on by social demands, and changes in our circumstances and physical health.
Midwives may find a large variation in how a neurodivergent client communicates from one appointment to the next. Someone who speaks fluently
Kupu Māori provide some insight
during a routine visit may need help to use speech effectively or be supported to use hand signals in an emergency. Others can be overwhelmed by verbal instructions or wordy handouts and get more information out of visual guides.
DOUBLE EMPATHY PROBLEM
Overcoming communication challenges isn’t solely the responsibility of the neurodivergent client. It is still a widely held misunderstanding that autistic people lack empathy. Coined by Dr Damian Milton, The Double Empathy Problem argues that this isn’t true, but rather that autistics simply express themselves differently to those who are not autistic.
A study by Morrison et al. in 2020 concluded that autistic and neurotypical individuals struggle to communicate because they do not understand each other's cognitive and communication styles. They reasoned that if autistic adults had poor communication skills, they would find it difficult to speak to everyone, autistic or not. But Morrison found no communication issues within the autistic groups, suggesting that their matching cognitive and communication styles were the key to success. In mixed neurotypical/autistic dyads, each participant struggled to understand their partner's different communication style.
Māori scholars have highlighted that the concept of neurodiversity aligns with indigenous views on disability (Simpson, 2021); strength-based constructs of neurodivergence are reflected in the following kupu Māori: Takiwātanga (Autism) meaning “in my own time and space”; Aroreretini (ADHD) meaning “mind/attention on many things” (Opai, 2019).
24 | MIDWIFE AOTEAROA FEATURE
BRONWYN RIDEOUT REGISTERED MIDWIFE AMY TAYLOR REGISTERED MIDWIFE
ISSUE 112 MARCH 2024 | 25 FEATURE
EXAMPLES OF SENSORY ACCOMMODATIONS
HYPOSENSITIVE
Olfactory Co-create plans for noticing signs of infection or illness
Auditory Louder volumes for alarms and phone calls; Written summary of any discussion
Interoception (The ability to understand the body’s internal signals)
Proprioception (Awareness of position and movement of the body)
Encourage reminders for eating, drinking and toileting; Utilise schedules and routines; Check/ask clients about awareness of infection or illness symptoms; Careful co-planning for monitoring fetal movements
HYPERSENSITIVE
Reduce use of scents and perfumes for personal and cleaning
Sound reduction: set up any necessary equipment outside of the room; Blocking sounds: noise cancelling headphones; Manage noise in shared rooms
Validate experience; Consider earlier pain relief during labour or for procedures; Consider anti-anxiety medication for procedures: in consultation with mental health team or GP
Pregnancy-safe tight clothing; Normalise the client’s need to move; Massage/deep touch; Weighted blanket; Extra coaching on holding baby during feeds
Visual Lamps with multiple colour options
Tactile Tactile stimming tools; Hands-on learning; Robust consent conversations
Below are some recommendations to improve communication between yourself and neurodivergent whānau:
• Processing speed - Give people time to process what has been said, answer questions and communicate the decision at a later time. If possible, schedule longer appointments or follow-up later. Encourage clients to prepare notes in advance about what they want to discuss.
• Literal and precise language - Avoid metaphors, asking vague questions or hinting/implying. Where possible, avoid using words like maybe, soon, possibly, etc. When using open-ended questions, provide prompts or a list of possible answers.
• Non-verbal communication - Your client may have difficulty understanding vocal tones, facial expressions or body language.
Reflect on the use of abdominal support belts/wraps and tubular bandages. Avoid unnecessary physical contact or fast physical activities
Reduce lighting; Close curtains; Sunglasses; Keep clinical spaces clutter-free
Avoid unnecessary physical contact; Communicate before physical contact; Enable alternatives to standard hospital bedding and sonography gel; Encourage stimming, sensory aids or distraction techniques during uncomfortable procedures or during feeds
In addition, their body language and facial expressions may not match your expectations. Listening and focusing will look different, so don’t worry about lack of eye contact or if they appear disinterested; instead, focus on the client's words.
• Planning and organising - Manage mutual expectations about cancelling or rescheduling appointments. If appropriate, encourage using alarms, lists or apps to remind clients of appointments or other critical pregnancy/parenting tasks.
• Modes of communication - Consider visual or easy-read versions of handouts or policies if available. Neurodivergent clients may stop speaking when overwhelmed but can still communicate. Having simple hand signals will ensure your client's wishes are still honoured. Many people struggle
with phone calls; consider video calls for emergencies and email or text messaging for non-urgent matters. Follow-up verbal discussions with a written summary.
SENSORY AFFIRMING CARE
Differences in sensory processing can also make the sensory environment of healthcare facilities challenging. Pioneering occupational therapist, psychologist and neuroscientist
A. Jean Ayres likened sensory processing challenges to a neurological “traffic jam” that prevents certain brain parts from receiving the information needed to interpret sensory information correctly.
• Hypersensitivity/over responsiveness can result in sensory avoidance behaviours.
• Hyposensitive/under responsiveness to a stimulus may engage in sensory-seeking behaviours.
26 | MIDWIFE AOTEAROA FEATURE
A person can be hyposensitive to stimuli such as hearing but hypersensitive to touch. Hypersensitivities can contribute to distraction and are frequently part of a broader multisensory issue; hyposensitivities can entail an impaired response to noxious or unusual stimuli and require strategies to overcome this.
Sensory processing can also go askew. While non-tactile stimuli like lights and sounds can elicit a pain response, broken bones and internal infections or organ troubles might go unnoticed. Such experiences significantly negatively impact personal well-being and daily life, with participants describing fatigue, stress and hindrances in day-to-day activities. Sensory sensitivity can also heighten during pregnancy and persist for months after birth.
Framing a sensory difference as a challenge or an advantage depends on the situation. While a person with auditory sensitivities might struggle with the noises of the machinery in the birthing suite, they may also be quicker to interpret what their baby needs by their cries.
DIETARY CONSIDERATIONS
Dietary advice is a significant part of the healthcare midwives provide and it is easy to overlook eating as a sensory experience: how the food feels/tastes in the mouth, the smell, the texture and the visual. Other elements also add to eating challenges, e.g., body signals not communicating hunger cues or fullness cues (interoception), chronic anxiety (hard to feel hungry), demand avoidance and self-medicating due to low dopamine levels.
Unsurprisingly, the neurodivergent population experiences a significantly increased rate of disordered eating and eating disorders. This includes conditions such as avoidant food intake disorder (ARFID), binge eating disorder, anorexia and so on. Food is personal and can be accompanied by feelings of guilt and shame when one is judged for eating the same “safe” foods and meal routines every day, wanting to eat alone or needing food presented in a specific way.
NEURODIVERGENCE AND ANTENATAL EDUCATION
Group social environments can be challenging to manage for neurodiverse whānau. Due to communication and sensory differences, they may not benefit in the
same way from social networking as their neurotypical peers.
OVERWHELM, MELTDOWN AND SHUTDOWN
Everyone, midwives and clients alike, has experienced sensory overwhelm or had a meltdown or shutdown at some point in their life. Sensory overwhelm can be a result of months, weeks, days or hours of coping with unexpected changes, lack of sleep and/or social/sensory overload.
When we are overwhelmed but still have control over our actions, the fight/flight/ fawn/freeze response might be engaged until the cause of the overwhelm passes or burnout occurs.
Sometimes, sensory overwhelm does not abate and can cascade into a meltdown and/ or a shutdown phase.
• Meltdowns are uncontrolled outward explosions of emotion. They are distinct from tantrums because the person has no control over their actions nor are they trying to achieve a goal or seek an audience. Removing or reducing the offending stimuli can help with recovery.
• Shutdowns are when a person withdraws, dissociates, becomes unresponsive or becomes lethargic and does not want to move.
Shutdowns and meltdowns affect both neurodivergent and non-neurodivergent people. Sarah Hampton (2020) found that during birth her non-autistic group were more likely to experience a meltdown, while her autistic participants were equally likely to have a meltdown or shutdown. This has significant implications in labour when it comes to ascertaining informed consent and timely delivery of analgesia when required.
Supportive care is important. Keep questions to a minimum and don’t tell your client to stay calm. Having tissues, fluids and light snacks ready, encouraging them to rest and having their preferred comfort items nearby can all be helpful. If they are clinically safe to leave unattended, give them as much space as possible to recover. Keep the space free of shame. You can lay the groundwork antenatally if you have a client who is familiar with how they respond to sensory overwhelm and can include that in the birth plan.
Every neurodivergent person is unique: start asking all whānau if they have specific sensory or communication needs. Include this in booking forms and review regularly. square
about the authors
Bronwyn Rideout and Amy Taylor are hosts of the recently published Neurobirth Podcast series available on Amazon Music / Audible, Deezer, Google Podcasts, iHeart Radio, Spotify, Spreaker.
The Neurobirth Podcast is a seven episode, limited series about the childbearing journey, from preconception through to the early weeks of parenting, through the lenses of ADHD and Autism.
Both from Wellington, Bronwyn is a Core Midwife and Amy works in the community as an LMC.
Each episode in the Neurobirth Podcast focuses on a different topic pertaining to pregnancy, and how sets of neurodivergent traits and behaviours may present and impact perinatal care:
Episode 1: Neurodiversity 101 - What is neurodiversity, what it means to be neurodivergent, intersectionality, and who is missing out on timely diagnosis?
Episodes 2 & 3: The senses - A twoparter which covers sensory processing, hypo- and hypersensitivity, stimming, and controversies around weighted blankets and fidget toys.
Episode 4: Communication - Tips on improving communication between healthcare providers and neurodivergent consumers, Spoon Theory, the Double Empathy problem.
Episode 5: General/preconception health - What current research says about health outcomes for people with autistim/ Takiwatanga and ADHD/Aroreretini and the implications for perinatal care.
Episode 6: Antenatal, labour and birthWhat does research tell us and where are the gaps?
Episode 7: Postnatal and early parentingMental health, infant feeding, adjusting to parenting, and contraception.
Midwives can claim time spent listening and reflecting on the podcast as part of their Continuing Education requirements for recertification.
References available on request.
ISSUE 112 MARCH 2024 | 27 FEATURE

sepsis | mate whakatāoke: could this be sepsis?
Sepsis is a serious condition, which can develop rapidly and have catastrophic health outcomes. It is a leading cause of maternal deaths worldwide and is the third most common cause of death in newborn babies. Midwives, as with other maternity care providers, have a responsibility to identify early signs of infection in women and babies, provide appropriate midwifery care and activate referral.
Many midwives will have seen the impact of infection when providing midwifery care for women | wāhine | pēpē, particularly as this group of people are at higher risk of developing sepsis. This article aims to act as a refresher on sepsis for midwives.
Cheyne (2022) highlights that the majority of cases of maternal and infant infection are likely to occur in the postnatal period and that most maternal deaths from sepsis occur postnatally. In Aotearoa we are fortunate to be able to provide postnatal care up to 6 weeks after birth, supporting access to an essential primary care service that many countries do not prioritise. In both hospital and community midwifery practice we need to remain vigilant for signs of sepsis while women are an inpatient or at home, especially as women are discharged home early and we navigate rising intervention rates and inequitable health outcomes.
Midwives play a leading role in the recognition of sepsis, its diagnosis, management and early referral throughout the childbirth continuum. Information sharing with whānau relating to signs and symptoms of infection enable them to know when to be concerned and what action needs to be taken and when to seek help from their
midwife. Any concerns shared by women during pregnancy and in the postnatal period need to be taken seriously. Recurring themes in perinatal and maternal mortality show the disproportionate impact on Māori, Pacific and Indian women, those under 20 years old and the effects of increasingly severe socioeconomic deprivation on these outcomes (PMMRC, 2020).
Much work on sepsis awareness has and continues to be undertaken by national entities in Aotearoa: Te Tāhū Hauora Health Quality & Safety Commission, ACC, and the Best Practice Advocacy Centre New Zealand (bpacnz guidelines). This guidance has been used to inform this article.
WHAT WE KNOW ABOUT SEPSIS
Sepsis is a multisystem disorder that can cause end organ damage, multi-organ failure, and mortality induced by infection (Vaught, 2018). Sepsis with shock is a life-threatening condition that is characterised by low blood pressure despite adequate fluid replacement, and organ dysfunction or failure.
Sepsis is difficult to diagnose with certainty. Although people with sepsis may have a history of infection, one important fact
to remember is that fever is not always present in all cases. The signs and symptoms of sepsis can be very non-specific, so the first consideration for anyone presenting with a possible infection is ‘could this be sepsis?’ Midwives need to always be cognisant that physiological changes related to pregnancy can mask early indicators of sepsis in order to avoid a ‘normalisation’ of possible sepsis.
SIGNS AND SYMPTOMS
Sepsis can occur because of pregnancy/ birth/postpartum-related infections or other infections during the childbirth continuum, e.g., pneumonia. Many people can initially look well despite being septic and can deteriorate very quickly. Early recognition and suspicion of sepsis is therefore crucial. During pregnancy - non-specific:
• Malaise
• Lethargy
• Confusion
• Reduced appetite
• Urinary symptoms
• Productive cough
• Flank/back pain
28 | MIDWIFE AOTEAROA CLINICAL UPDATE
FEVER
AND CHILLS - RIGORS
DISTRESS watch out
CONFUSION RESPIRATORY
for...

PAIN/PHYSICAL
• Diarrhoea and or vomiting
• Uterine and/or renal pain and tenderness
• Abdominal or chest pain
• Fever and chills - rigors
• Fetal tachycardia
Postnatal: all of the above plus
• Pain that is ‘out of the normal expectations of pain’
• Breast engorgement/redness
• Increase in lochia (delay in involution)
• Cellulitis around surgical wound and/or discharge
• Perineal trauma signs of infection/ breakdown/haematoma/increased pain
• Offensive vaginal discharge/lochia (offensive may indicate anaerobes, serosanguinous, streptococcus infection) This demonstrates the importance of visually assessing the woman’s perineum throughout the postnatal period to assess healing when there has been perineal trauma at the time of birth. Signs of slow healing or infected tissues may alert the midwife to the need for additional care to prevent sepsis from developing.
PĒPĒ | NEWBORN BABIES
Primary sepsis infection is usually bacterial in nature in newborn babies; however, in rare cases it could also be due to a viral or fungal infection. Pēpē may become infected via vertical transmission from the pregnant wahine antenatally or during birth or less commonly from the immediate/surrounding environment (Cheyne, 2022). Bacteria that are known to cause sepsis in pēpē include E.coli, group B streptococcus, neisseria meningitis, salmonella, haemophilus influenza type b, and listeria monocytogenes. The
herpes simplex virus can cause a viral infection. An existing medical condition may also trigger sepsis.
Signs may vary according to the type of infection, however pēpē may present with: Fever, hypothermia and/or temperature instability; Respiratory distress; Increased irritability and unusual behaviour; Lethargic movements or floppy motions; Apnoea and bradycardia; Tachycardia; Cyanotic episodes; Unexplained jaundice; Eyes may have a sunken appearance; Decrease in urination; Abdominal distension; Bulging of the fontanelle; Umbilical flair and skin rashes.
TOOLS AND REFERRAL PROCESSES TO SUPPORT MIDWIVES IN PRACTICE
In recent years tools have been created in Aotearoa to support decision making and to identify acute illness and deterioration. These tools include the Maternity and Newborn Early Warning System charts (HQSC). Such tools are specifically designed to support care however they should be utilised with a thorough midwifery assessment which may include wider considerations not identified in the tool. Midwifery clinical judgement is the most important factor and is supported by such tools.
Multiple infectious diseases and conditions are described in the 2023 Referral Guidelines (Te Whatu Ora). These categories guide midwives to instigate to obstetric and paediatric colleagues. Maternal sepsis (code 7006) is categorised as a transfer of clinical responsibility, once discussions and exploration have occurred with the affected person. Maternal sepsis is described as: temperature >38°C or <36°C; heart rate > 100 beats per minute; respiratory rate > 25 breaths per minute; systolic blood pressure < 90 mmHg; new onset of pain;
altered mental state. The Referral guidelines for pēpē are more generic and relate to various clinical signs and symptoms, however the urgency of referral is as important.
SUMMARY
Sepsis is the body’s response to severe infection and develops as a result of undetected and unchecked infection. It can develop with rapid speed and is a significant cause of maternal and neonatal morbidity and mortality. Midwives play a crucial role in vigilance during pregnancy and particularly in the postnatal period. square
References available on request.
“Could this be sepsis?”
(Adapted from the UK Sepsis Trust)
Does the wahine or pēpē look unwell?
• Was there a known antenatal infection e.g. group B strep?
• Has there been recent trauma e.g. perineal trauma repair?
• Has there been an invasive procedure e.g. caesarean section?
• Has there been an invasive procedure during labour and birth e.g. application of FSE?
• Was there anything that you had concerns about in the pregnancy/labour/ birth or postnatal period?
Could this be due to an infection relating to:
• Infected perineal wound
• Infected caesarean section wound
• A breast abscess
• A urinary tract infection
• Retained placental productsendometritis
ISSUE 112 MARCH 2024 | 29 CLINICAL UPDATE
TACHYCARDIA AND BRADYCARDIA
CLAMMY OR SWEATY SKIN
DISCOMFORT

 BRIGID BEEHAN MIDWIFERY ADVISOR
BRIGID BEEHAN MIDWIFERY ADVISOR
MIDWIFERY PRACTICE GUIDANCE: THE ONLY CONSTANT IS CHANGE
The midwifery landscape in Aotearoa New Zealand is evolving and, with it, the College's commitment to workforce is stronger than ever. In 2023 Te Tatau o te Whare Kahu | Midwifery Council (the Council) surveyed midwives to gauge the profession’s thoughts and ideas to strengthen the Recertification Programme’s elements. Although the final version of the next Recertification Programme cycle is still not fully confirmed, this article explores an overview of the proposed changes announced by the Council in December 2023, for the period 2024-2027. These changes, affecting all midwives holding an Annual Practising Certificate (APC), are designed to adapt to the dynamic nature of midwifery, addressing both traditional practices and emerging challenges. The Council anticipate that the overall changes to the current cycle will commence 1 July 2024 although it is likely that some may occur in April.
OVERVIEW OF RECERTIFICATION CHANGES
The recertification process is one of the cornerstones of professional development, ensuring that midwives remain at the forefront of best practices and quality care. While the core components like professional activities and education hours continue, the introduction of new elements marks a significant stride towards enhancing the scope and depth of midwifery education.
Understanding these changes is crucial for every practising midwife, as they reflect both the evolving landscape of healthcare and the ongoing commitment to excellence in midwifery practice.
CULTURAL SAFETY EDUCATION
A significant and positive addition to the new cycle will support all midwives’ engagement in cultural safety education. This education
will be a combination of a day workshop on Tūranga Kaupapa provided by Ngā Maia and an additional 4 hours of cultural safety education. The College is hosting a hybrid e-learning opportunity exploring Te Tiriti o Waitangi which will be available to midwives shortly.
MIDWIFERY SCOPE OF PRACTICE EDUCATION
The College (along with all midwives) is awaiting the final version of the Scope of Practice to be gazetted and for the Council to provide sufficent clarity about what the proposed changes will mean for midwifery practice. The Council is yet to release the updated revised draft.
The competencies are also in the process of being updated and these will provide further clarity about what potential changes to the Scope will mean. We are eager to see and be
invloved in any education that follows and will support midwives to transition through understanding and application of requirements within the new Scope.
MIDWIFERY STANDARDS REVIEW
Midwifery Standards Review (MSR) is one of the many components of the Recertification Programme which supports midwives to maintain their competency to practise. 2023 was a landmark year with the College introducing a co-leadership model for the MSR portfolio in its advisory team. This approach, involving both tangata whenua and tangata Tiriti aligns with cultural review recommendations. This model is not just a procedural change but a significant cultural shift, paving the way for the process to update the MSR to be co-led.
The College intends to start national hui with midwives, Ngā Maia and other
ELAINE GRAY MIDWIFERY ADVISOR
30 | MIDWIFE AOTEAROA PRACTICE GUIDANCE
stakeholders to explore what a quality assurance programme should look like in 2024. The objective is to create a programme that not only maintains high professional standards but also resonates with the diverse and individual needs of midwives. Alongside this, a quality assurance programme needs to meet the Council’s requirement for Recertification, reassuring the public that midwives are providing safe and effective care to wāhine and whānau.
The consultation process, spearheaded by the two MSR midwifery advisors, is set to begin in early 2024, marking the start of a collaborative effort towards revising the MSR to ensure it reflects the needs of midwives and the environment in which they practise in 2024. The Council has stated that the current MSR will remain in place for 2024-2025 while the next steps for a quality assurance programme are considered.
MIDWIFERY EMERGENCY STUDY REFRESHER
The annual Midwifery Emergency Study refresher workshops are pivotal in preparing midwives for emergency situations, directly impacting maternal and neonatal health outcomes.
The Council announced that the Midwifery Emergency Skills Refresher (MESR) annual update will remain part of the Recertification programme for the next three years.
They identified that common childbirth emergencies will remain included in the days, with the addition of broader topics that directly influence and inform safety in practice for midwives, and the experiences of wāhine and whānau. Additional topics will be embedded into MESR over the next three years, including maternal mental health, midwife wellbeing, and communication as a response to the broader challenges faced in the field. This holistic approach ensures that midwives are not just technically proficient but also equipped to handle the psychological and emotional aspects of their roles.
The College facilitates MESR education nationwide and has a designated education team delivering the content. The College delivers the MESR mostly in primary birthing units (rural and urban) and predominately in Auckland. Sometimes, the College supports Te Whatu Ora hospitals nationally with MESR workshops when educators cannot deliver the emergency days within the hospital setting.
In April 2024, the College will host a 2-day national educators forum for all Te Whatu
Ora educators to enable exploration and discussion of the content of MESR, share resources and plan a consistent approach to the first-year education content around mental health. The forum provides a platform for educators to collaborate, share resources and plan the approach to the new triennial of MESR days.
CONTINUING MIDWIFERY EDUCATION
Continuing education is the backbone of professional growth. However, accessibility for some members remains a challenge, particularly for those in rural areas and experiencing current workforce shortages. The Council announced that the requirements of 8 hours per year of continued education would remain. The College will continue to provide face-to-face education nationwide and is in the process of developing new workshops over 2024. The exciting addition of our e-learning platform will further enhance the College’s education calendar and we look forward to seeing you all in the virtual world.
PROFESSIONAL ACTIVITIES
The recognition of professional activities as a part of a midwife’s development journey is a significant aspect of the recertification process. The Council’s decision to broaden the scope of these activities reflects an understanding of midwives’ diverse roles. Be it mentorship, preceptorship, professional or representative appointments, many activities that midwives engage in create opportunities for meaningful professional development. They offer platforms for learning, sharing, and growing together as a community, reinforcing the collaborative spirit of the profession.
The Council provides some guidance on their website and ideas under 5 overarching topics:
• Working with colleagues
• Engagement with the profession
• National and regional appointments
• Council appointments
• Teaching and learning
The Council plans to broaden the definition of professional activities for the next triennium and provides the most up-to-date information about professional development activities on their website.
COLLEGE RESOLUTION SUPPORT
It is timely to remind midwives about the benefits and professional responsibility of
discussing the College resolution support service for women and people in their care, regardless of whether the midwife identifies a need.
In 2023, Resolution Committees were renamed Resolution Support Service. Each region nominates a consumer and midwife representative to offer support to wāhine who require further clarification, conflict resolution or have questions about the midwifery care they have received.
Within this service, Māori resolutions members will offer support to Māori consumers when requested. Unfortunately, this valuable service is underutilised, and the College reminds LMC midwives of their responsibilities to inform wāhine and whānau about this service, and to ensure they understands its purpose and benefit.
The resolutions support service provides benefits for midwives by offering a supportive environment, listening ear, the opportunity for the midwife to reflect on the care they have provided, and the facilitation of effective conflict resolution that supports consumers and mitigates low-level complaints being escalated to the Council and/or HDC.
The Resolutions service encourages open nonbiased confidential communication for wāhine to discuss their midwifery care and, when the midwife is involved, this enhances their professional development, enabling midwives to learn from experiences and continuously improve their practice. square

ISSUE 112 MARCH 2024 | 31 PRACTICE GUIDANCE
 VIOLET CLAPHAM MIDWIFERY ADVISOR
VIOLET CLAPHAM MIDWIFERY ADVISOR
MIDWIFERY PRACTICE GUIDANCE: PROVIDING MEDICAL CERTIFICATES
Midwives may at times be asked by pregnant women for medical certificates. For a Work Capacity Medical Certificate, the woman needs to be more than 27 weeks pregnant or have complications related to pregnancy.
All medical certificates certified by health practitioners are legal documents, and these certificates are described as needing to be honest and made in good faith (Work and Income). Work and Income also provide guidelines about what needs to be written, what should be shared, and what needs to be clearly identified on the certificate.
The obvious key point is legibility when writing a paper form, and the need to minimise medical terms to make the certificate easier to read is also suggested. Information shared needs to be accurate and based on the health practitioner’s clinical observations, with the date of examination and when the woman’s work capacity is expected to be reassessed clearly identified. The Work Capacity Medical Certificate is
The Work Capacity Medical Certificate also gathers information about any diagnosis that impacts on ability to work, what could support a person to work and if a person could work in a more suitable role with support.
designed to gather information about what the barriers to and/or limitations to work are; this includes non-medical related barriers or limitations.
The Work Capacity Medical Certificate also gathers information about any diagnosis that impacts on ability to work, what could support a person to work and if a person could work in a more suitable role with support. The most common reasons a medical certificate may be requested during pregnancy include:
• Proof of sickness or injury
• Paid parental leave applications
• Benefit requirements (Work and Income)
• Alteration of work duties
• For airline travel
OTHER KEY POINTS
An employer may ask an employee for proof of sickness or injury. Proof is usually in the form of a medical certificate from a doctor stating that the employee is sick or injured (or their spouse, partner or dependant is sick or injured) and is not able to work.
An employer is not allowed to tell an employee which doctor or practice they should go to for a certificate. If an employee is sick or injured, or cannot attend work because their spouse, partner or dependant is sick or injured, for less than three days,
and an employer asks for proof of sickness or injury, they must ask the employee for proof as soon as possible and pay the employee back for the cost of a visit to the doctor to obtain the proof.
If the employee is sick or injured three or more days in a row, even if these three days are not all days the employee would have otherwise worked, and the employer asks for proof, then the employee needs to meet the cost of obtaining the proof.
WORKPLACE ACCOMMODATIONS FOR PREGNANCY
As pregnancy progresses, considerations such as modified workstations, reduced physical demands and adjustments to working hours may be necessary to ensure the well-being and safety of the pregnant worker. Employers have a legal obligation to manage workplace hazards wherever possible. Knowing that an employee is pregnant allows the employer to reassess the workplace risks and make the necessary adjustments to protect the pregnant worker. Pregnant women who are affected by hyperemesis gravidarum may be unable to work at times.
WORK AND INCOME MEDICAL CERTIFICATES
In some situations, the midwife may not have access to the woman’s previous medical history, or the woman may have a complex
32 | MIDWIFE AOTEAROA PRACTICE GUIDANCE
medical condition and the Work Capacity Medical Certificate may be better completed by the woman’s doctor. The need to refer to the doctor may also be present if the midwife is placed in a situation of conflict - either through duress or because the person has a complex social or financial situation. The midwife can signal on the medical certificate to suggest that a second opinion may be more appropriate, if there are any concerns about the provision of a diagnosis, providing an opinion about capacity for work, or the cost associated with a health condition and/ or disability.
WORK AND INCOME BENEFITS
Pregnant women may be receiving a benefit from Work and Income which requires them to look for work (the Job Seeker Benefit). Pregnant women are no longer required to actively seek work after 27 weeks of pregnancy but Work and Income require proof of the woman’s expected due date. Midwives may provide a medical certificate in this situation. If the woman has a Work and Income client number, this should be included on the certificate. The assessment from a health practitioner is also used by Work and Income to enable the right financial assistance and support to be provided. square
useful information
Midwives can purchase Medical Certificate pads from the College website: www.midwife.org.nz/product/medicalcertificates/
Further information is available at: Work and Income: www.workandincome. govt.nz/providers/health-and-disabilitypractitioners/medical-certificates. html#null
The Ministry of Business, Innovation and Employment website: www.employment. govt.nz/leave-and-holidays/sick-leave/ requirement-for-medical-examination/
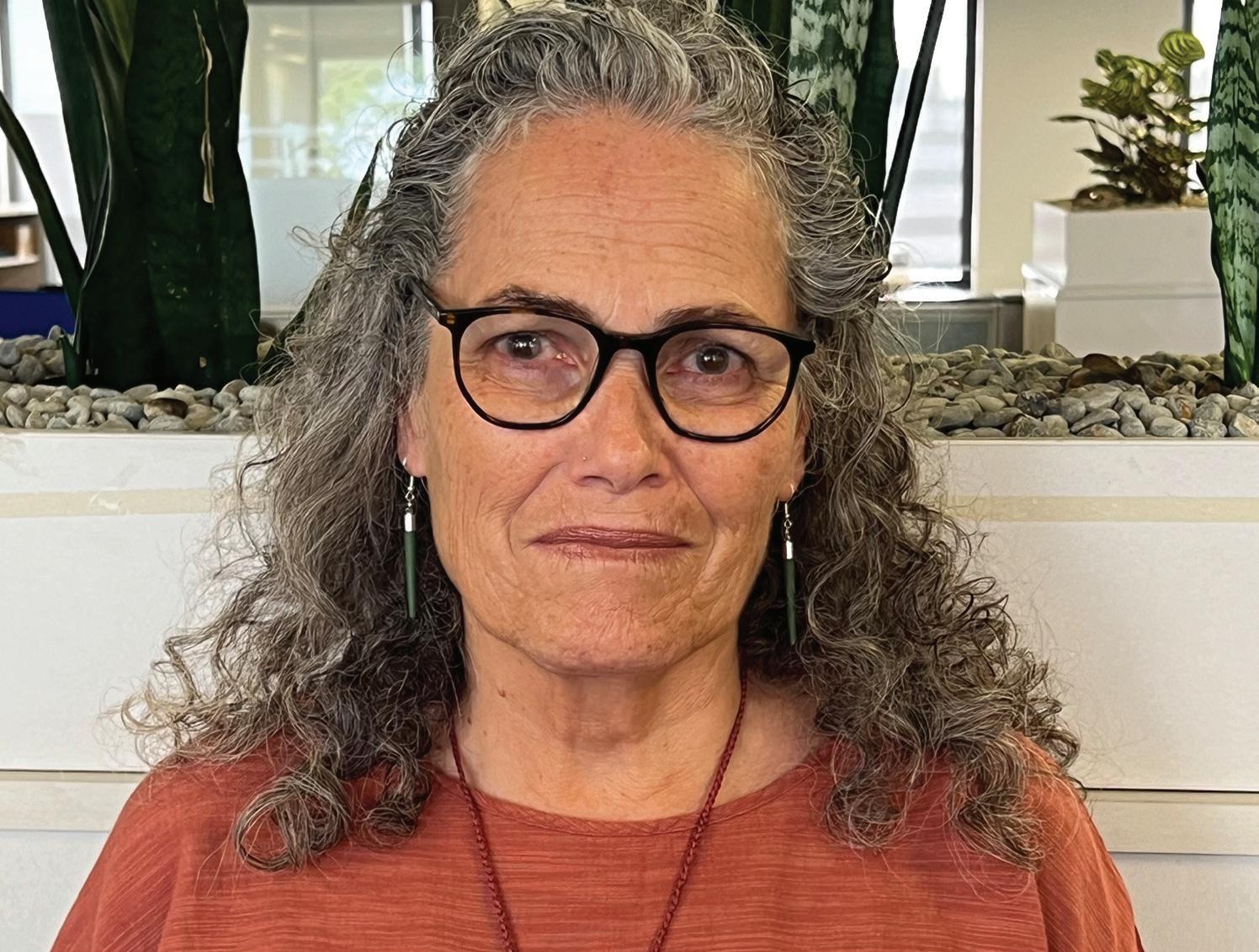
A NEW HOUSE
Heather Muriwai (Tangahoe, Ngāti Ruanui) has been selected for the inaugural position of Chief Clinical Officer for maternity at Manatū Hauora | Ministry of Health. Hayley McMurtrie caught up with Heather about her role and aspirations for it.
“At my interview”, Heather states, “I was asked why I applied for the role, and without really thinking I said, ‘because I haven’t finished’, within the current political climate I needed a new house to continue the mahi for birthing whānau”.
Heather believes her new role, which she will take up on March 4, provides the opportunity to drive policy and strategy across the whole of the maternity sector, aligning closely with Kahu Taurima and Heather’s goal of seamless care for birthing whānau. Not naturally comfortable in the political arena Heather says she can only be herself, a determined wahine with a clear goal to see improved outcomes for birthing whānau, however Heather is quite clear that this is not the world according to Heather, she is the māngai (voice) for birthing whānau.
Heather has been active in the maternity sector for over 25 years, most recently as Chief Clinical Officer Midwifery, Te Aka Whai Ora and has worked in a variety of clinical settings as well as education, leadership and management. Heather, together with Midwifery Advisor Elaine Gray, authored and facilitated the workshop Birthing Across Cultures, which may have been quite revolutionary at the time and is what Heather considers her first opportunity to influence hearts and minds in her goal of achieving equity. Heather says she is not afraid to have those courageous conversations that are needed to bring change.
Pleased that Manatū Hauora has recognised a need for a maternity position of this kind and honoured that they have chosen a midwife to fill it, Heather states, “We should start at the beginning with birth - it influences your life oranga story”.
Humbled and honoured to take on this position, Heather is also rightly proud. She is excited to have taken on an inaugural position where she can set the scene herself, guided by her own vision to steer the role.
Midwives cannot rest on their laurels though; Heather has huge expectations for the profession to fulfil her vision of midwives becoming active participants of Kahu Taurima. Heather says, “midwives do not operate alone, we are part of a network that sets the tamariki on the right path… Midwives acknowledge their love of their vocation, so prioritising continuity of care as the cornerstone of our midwifery model will enable an improvement in our birthing and maternity outcomes”.
Heather’s appointment is the first time maternity and midwifery has been represented at such a strategic level and we know that Heather’s experience and focus on whole whānau care and support will serve Aotearoa’s birthing whānau well.
We wish Heather all the best in her new role. square
ISSUE 112 MARCH 2024 | 33
 CAROL BARTLE POLICY ANALYST
CAROL BARTLE POLICY ANALYST
NEURO DIVERSITY AND BREAST FEEDING
Pregnancy, birth and breastfeeding are significant events in the lives of many women, and all can be associated with some anxiety, particularly in first-time mothers. Thinking about unknown experiences, browsing on the internet and listening to stories from well-meaning people – stories that may swerve into horror stories – can all add up to some degree of concern. But for some women there may be added anxieties for other reasons.
Neurodiversity as a term has been described as a movement that emerged in the 1990s to increase the acceptance and inclusion of all people while embracing neurological differences (Baumer & Frueh, 2021). Merriam-Webster defines neurodiversity as individual differences in brain functioning regarded as normal variations within the human population. Neurodiversity has often been associated with disability or mental illness, although now it is generally better understood to be about the way that human brains differ. Neurodevelopmental conditions include attention deficit/hyperactivity disorder (ADHD), autism, communication disorders, intellectual development disorders, motor disorders and specific learning disorders. Autism and ADHD are the two more commonly known neurodiverse conditions and the range of issues that can be experienced with both conditions are persistent and varied.
Autism is a neurodevelopmental condition which is characterised by differences in reciprocal social interaction and communication, restricted and repetitive behaviours, and sensory processing difficulties (Hampton et al., 2022). Autism and ADHD are described as impairments in diagnostic reference manuals but for many neurodivergent people the strengths and quirks of their own neurodivergence are seen as important parts of who they are. Autism may also present with co-occurring psychiatric conditions such as depression and anxiety (Rumball et al., 2020) which can complicate care. The potential for neurodivergence to cause difficulties and be disabling in some circumstances does exist, and an awareness of what aspects of the maternity experience may present as challenging is necessary for midwives. A lack of public understanding of social communication, behavioural and other differences can lead to stigmatisation for individuals (Clarke et al., 2024).
Women who are neurodiverse may all present differently during their midwifery care, and communication difficulties may cause challenges but, fortunately, individualised relational care which is a foundation of midwifery care is flexible, creative, supportive and tailored to meet the needs of all women. The midwifery continuity of care model supports issues that may face women who are neurodiverse, and indeed all women in the maternity system, to ensure challenges can be successfully navigated.
In a previous Midwife Aotearoa article (March 2023) the impact of disability on breastfeeding was explored to identify barriers to breastfeeding and to ascertain how women with disabilities wished to be treated. Women with disabilities in one study wanted “to just fit in” and to receive care in a similar or identical manner to those without disabilities. They resented an “at risk” label on account of their disabilities when it was not medically indicated (Blair et al., 2022). An issue identified by Joanna Grace, a breastfeeding woman who is autistic and who founded “The Sensory Projects”, is the invisibility of autism, which led her to being fearful of people making negative assumptions about her capabilities, despite her being a competent human being preferring to be considered as having low support needs (Grace, 2021).
The New Zealand Disability Strategy 2016-2026 states: New Zealand is a nondisabling society – a place where disabled people have an equal opportunity to achieve their goals and aspirations, and all of New Zealand works together to make this happen. Non-disabling is a term that was used to recognise the importance of removing the barriers in society for disabled people who have impairments of any kind. Another nondisabling strategy is building recognition that neurodivergent people may have brains that work differently but with the right support this should not result in barriers to care, or traumatising experiences.
There is some work that specifically looks at neurodivergence and women’s needs
34 | MIDWIFE AOTEAROA BREASTFEEDING CONNECTION

when pregnant, birthing, breastfeeding and parenting, although most relate primarily to autism. There are numerous articles about breastfeeding a baby with sensory difficulties which will be addressed in a future article.
NEURODIVERGENCE AND BREASTFEEDING
Research shows that the reasons women do not meet their own goals for breastfeeding, or the optimal recommendations for breastfeeding, are because of barriers which are mostly out of the control of the individual woman. These barriers include insufficient maternity protection, unsupportive workplaces, difficulties in accessing ongoing support for breastfeeding, economic pressures and the spread of misinformation (Brown, 2017). These challenges to breastfeeding affect many women regardless of health, experiences, neurodiversity or disability. However, factors such as neurodivergence are described as having the potential to cause difficulties but as being less recognised (Grant et al., 2022). Challenges faced by breastfeeding autistic women are noted to be related to sensory issues, communication and pain, with the more typical barriers to breastfeeding being exacerbated by an inaccessibility of support services and a lack of social support (Grant et al., 2022).
Research shows that the reasons women do not meet their own goals for breastfeeding, or the optimal recommendations for breastfeeding, are because of barriers which are mostly out of the control of the individual woman. These barriers include insufficient maternity protection, unsupportive workplaces, difficulties in accessing ongoing support, economic pressures and the spread of misinformation (Brown, 2017).
ISSUE 112 MARCH 2024 | 35 BREASTFEEDING CONNECTION

A thematic analysis by Hampton et al. (2022) found that the sensory aspects of birth, such as noise and touch, could be challenging for autistic women (semistructured interviews with 21 autistic women two to three months after birth). The importance of clear, direct communication was identified. Interestingly, Tint and Weiss (2018) found that autistic women reported being able to mask autistic characteristics,
Women value providers who consider their feelings and needs and appreciate a flexibility of approach... health providers needed to listen to what women tell them about what they want.
which led to an underestimation of their needs by health care professionals. It is possible that within a relational midwifery continuity of care model there would be more openness and trust which is conducive to discussion about difficult topics.
The sensory difficulties during childbirth such as lighting and noise should be relatively easy to modify in most birthing environments, particularly of course in home birth settings. Sensitivity to touch has been identified as an issue for both birth and breastfeeding. A theme of positive and negative birth experiences identified in the research by Hampton et al. (2022) included a subtheme titled the physical and emotional challenges of birth; The study included autistic and non-autistic women and the experiences across both groups of women were similar in that both groups found labour pains challenging, some had complicated births that did not meet their expectations, and both groups found it difficult to adapt to unexpected circumstances. In terms of
disclosure around autism, some autistic women said that they felt their disclosure was overlooked while others felt disclosure led to their needs being met. Both the autistic women and the non-autistic women in this study valued continuity of care for establishing a relationship and being understood. The vast majority of the 21 autistic women in this study had a co-occurring psychiatric condition, compared to a minority in the group of 25 who were not autistic. Breastfeeding issues were common to both participant groups. Participants in both groups found breastfeeding support groups useful although some women in the autistic group found the idea of joining a group and meeting other mothers too challenging. It is possible that individual mother-to-mother peer support could be valuable for breastfeeding support if the peer supporter also has personal experience of neurodiversity.
Gardner et al. (2016) explored the childbearing experiences of eight women
36 | MIDWIFE AOTEAROA BREASTFEEDING CONNECTION
with Asperger’s Syndrome and found four major themes: processing sensations, needing to have control, walking in the dark and motherhood on my own terms. Discussion of specific sensory experiences, counselling about coping strategies for sensory intrusions, targeted support and modifying the clinical environment were recommended as necessary for the provision of sensitive individualised care. It was noted in this article that some of the women in the study were described as having self-diagnosed, rather than being formally diagnosed by a clinician with expertise in autism. Regardless of a formal diagnosis, women who present with diverse needs can be accommodated during their midwifery care experiences.
Inaccessibility of infant feeding support was cited as an issue in the systematic review of “autistic women’s views and experiences of infant feeding” conducted by Grant et al. (2022). Sensory challenges, pain and interoceptive (perceptions of sensations from inside the body) differences made breastfeeding impossible for some women. Feeling “touched out” which can also be described as a sensory overwhelm was reported. Sensory-related issues such as health professionals sitting too close to women, touching without asking first, and causing pain during examinations were all described as challenging issues. Misunderstandings between health professionals’ spoken words and women’s understanding meant that opportunities for support were sometimes missed. Specific solutions included a partner holding the baby during breastfeeding to reduce sensory overwhelm, using tolerable devices such as a nipple shield to support breastfeeding continuance, reducing other sensory stimuli, and setting short-term breastfeeding goals.
Women value providers who consider their feelings and needs and appreciate a flexibility of approach. In a study by Blair et al. about disability (2022) one woman participant suggested that health providers needed to listen to what women tell them about what they want, should not request women to do things, but rather ask them if they can do things, and should not tell women about policies without explaining how they can be adapted, and/or why they are recommended in that way. For autistic women and neurodiverse women, further considerations may be necessary. Expressing and sensing pain differently and being unable
to accurately report these pain experiences, processing spoken language differently, losing the capability to articulate experience when stressed, and a limited capacity to process language during phone conversations were all described as challenging personal issues by Grace (2021).
CAN BIRTH PLANS HELP?
Birth plans were originally intended to empower women in labour and childbirth. In 1980 the first guidance about constructing birth plans was written by Simpkin and Reinke and produced by the International Childbirth Education Association (Ghahremani et al., 2023).
The development of a birth plan can support engagement, communication, expectations, and an exploration of the possible options for birthing women, as well as a discussion about preferences. Birth plans can also extend into the post-birth period and include breastfeeding/infant feeding. A scoping review about the role of birth plans found that they were seen as a tool for shared decision making, autonomy, sense of control, professionalism of care provider and trust (Shareef et al., 2023).
Birth plans invite participation in care, generate the development of a greater sense of control and engage the woman in decision making, with the aim being higher satisfaction with the birth experience (Waller-Wise, 2016). These are all key points for midwives who aim to provide support for all pregnant women to achieve satisfaction during their pregnancy, labour, birth and breastfeeding care. Discussion about the place of birth and women’s preferences is part of midwifery care and part of birth plan development.
CONCLUSION
Protecting birth physiology and supporting a positive childbirth experience has been a cornerstone of midwifery practice, with the aim of improving the health and wellbeing of all mothers and infants. Open, engaged reciprocal engagement and conversation, however slow it develops during the midwife-woman relationship due to communication difficulties, should aim to enable the development of a relationship and care model that will meet women’s diverse needs for birthing and breastfeeding. Many of the barriers described by neurodiverse women are barriers to breastfeeding which apply to other women also. Individual care delivery adaptation
whenever necessary and flexibility in care are the keys to meeting the needs of women during maternity care.
Grant et al. (2022) in their UK work looking at autistic women’s views and experiences of infant feeding in maternity systems recommend service improvement in general rather than setting up new bespoke separate services. Midwives in Aotearoa New Zealand protect the rights of women to control their pregnancy and birthing experiences and uphold the right to informed decision making and consent throughout the childbirth experience. This philosophy is consistent with autonomy, communication, and individualised care and, by definition, it should be able to meet the needs of all women regardless of any differences in their needs. square
References available on request
key points
Sensory issues need to be exploredfor example, lighting, sounds, and the environment may need some modification, and single postnatal rooms or home birth if it is a possibility.
Communication needs to be creativeit should be verbally clear and, for some women written information should also be available to reduce the likelihood of misunderstanding. Phone conversations may cause difficulties for some women.
Avoid making assumptions. Ask if there are any specific communication needs or preferences.
Consider that the processing of pain and the ability to describe pain may be challenging for some women.
Mother-to-mother breastfeeding peer support from mothers who have similar experiences may be helpful.
Mothers should not be touched during breastfeeding assistance without consent (Grant et al., 2022), and the mother’s personal space needs to be respected.
Breastfeeding support should be tailored to individual needs.
A birth plan can include breastfeeding and infant feeding and support engagement and communication.
The continuity of midwifery care model is flexible, creative, and supportive and it is tailored to meet the needs of all women.
ISSUE 112 MARCH 2024 | 37 BREASTFEEDING CONNECTION
 SIAN BURGESS
SIAN BURGESS
The Best Country to Give Birth? Midwifery, Homebirth and the Politics of Maternity in Aotearoa New Zealand 1970-2022
This revisionist history of maternity care in New Zealand is a depressing and heart-wrenching read. Writing 33 years after the 1990 Amendment to the Nurses Act, Linda Bryder details the events leading up to, during and following the changes to
maternity care in Aotearoa New Zealand that enabled midwives to regain autonomy.
Bryder is a medical historian whose central thesis questions whether Aotearoa is the best country to give birth. She focuses on the influence of homebirth, feminism and the
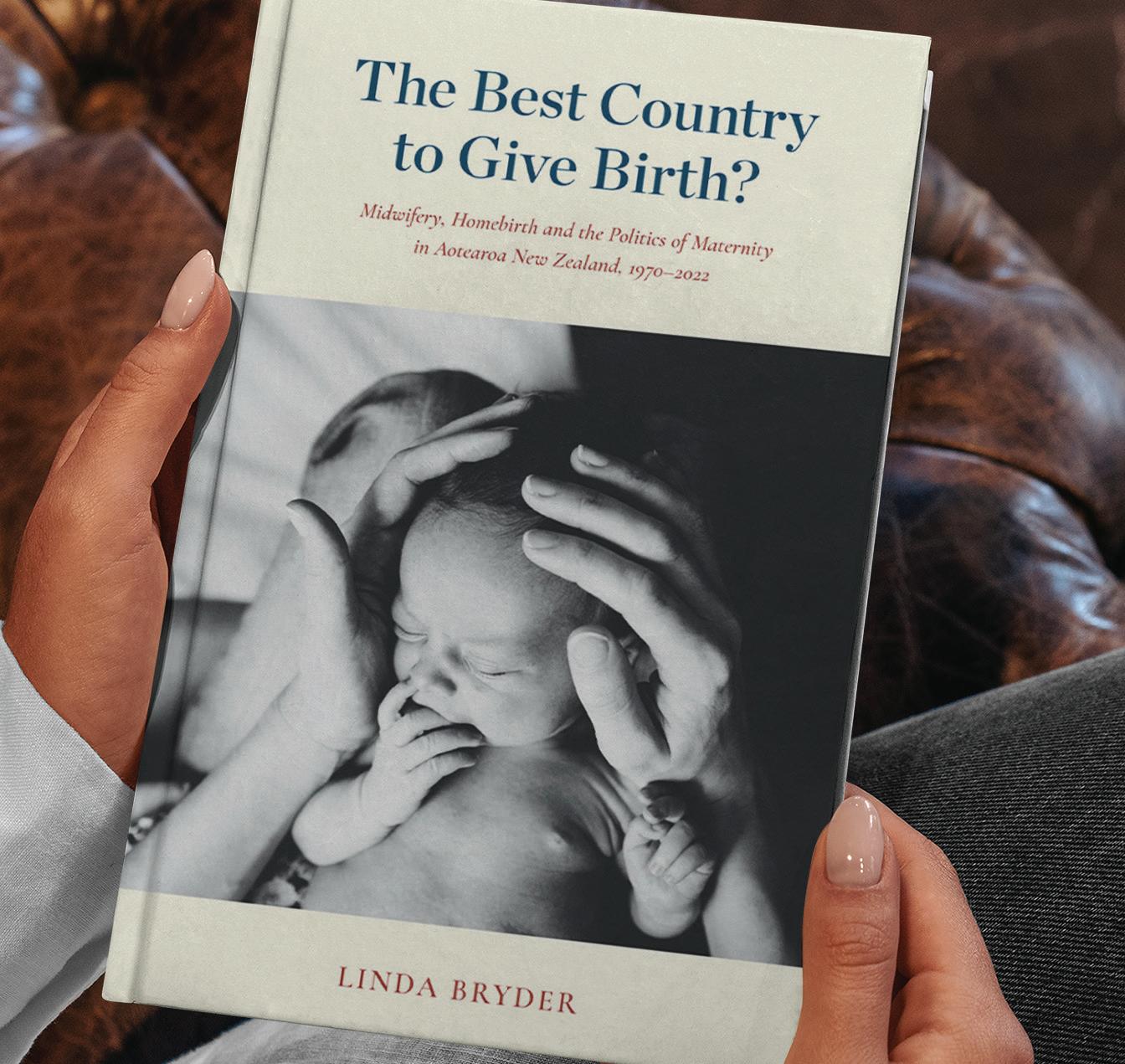
counterculture movement of the ‘70s and ‘80s, ignoring many of the other influences that supported the changes.
The impact of doctor-led hospital birth in the ‘70s and ‘80s receives scant mention and the very real need for change, given the experiences of women at that time, is completely ignored.
At that time, a "normal" birth would involve the mother undergoing a pubic shave, an enema, birthing flat on her back on a bed under bright lights, her partner requiring permission to be present and the baby being whisked off to the nursery to be washed and dressed - often before she could see or hold her baby.
Written through a lens that privileges the medical voice, this book follows a familiar formula Bryder has used previously to discredit the 1987-1988 Cartwright Inquiry in A History of the Unfortunate Experiment at National Women’s Hospital
As women’s health activist Lynda Williams wrote at the time, “A careful reading of her book reveals that it is possible to prove almost anything if you quote enough people, and quote them out of context. This applies to both health professionals and consumers - or as Bryder refers to some of us - 'feminist health activists'."
Just as Bryder said then that there was no experiment and that Judge (now Dame) Silvia Cartwright, who presided over the 1987 enquiry into whether women were mistreated, got it wrong, she now uses
38 | MIDWIFE AOTEAROA READING CORNER
A PERSONAL REFLECTION
similar logic to assert that Helen Clark and Ministry of Health officials were captured by this small vociferous midwives' voice. The vast majority of women, she asserts, did not want the changes that the Act enabled.
Whilst the Act gave autonomy to all midwives, it was thought that it was mainly homebirth midwives who would pick it up.
However, women did want the care that the changes to the Act enabled, and midwives left hospital employment to work in the community as the offer of continuity of midwifery care was quickly taken up by the vast majority of women. The ability to know your midwife and have greater autonomy was a boon both for pregnant women and midwives.
Coming to NZ in 1979, I worked at St Helen’s Hospital in Auckland until the birth of my first daughter. The influence of my midwife and the ability to continue working with my baby in tow encouraged me to join the ranks of the homebirth midwives in 1980. It was a marvellous time to be a midwife and to be able to deliver womencentred care - no more shaves or enemas, or separating mothers from their babies.
Homebirth was part of my training in the UK and the influence of people like Sheila Kitzinger, Frederique Leboyer and Michel Odent formed my views of birth at home. The simple reality and privilege of being in the mother’s space where she was in charge, compared to a hospital environment where she wasn’t, enabled a safer and more respectful place to birth for most women.
The shock of reading Bryder’s interpretation of that time has been profound and distressing. My overwhelming reaction is that ‘it just wasn’t like that’. I loved being a midwife and I am immeasurably proud of the changes to maternity care that took place during this time.
Bryder makes the case that we were a bunch of feminist ideologues for whom place of birth was part of our antiestablishment values; that it came with a distrust of doctor-centred medicine; and that it was accompanied by a desire to extend this ideological influence to all mothers.
She also suggests that the relationship between doctors and midwives was not constructive - which is simply not the case. Prior to the changes to the Act, we worked amicably and respectfully with GPs who supported homebirth for many years.
Readers who want a more accurate herstory of maternity over this time are strongly recommended to read midwife Joan Skinner’s Labour of Love which stands in stark contrast to Bryder’s version of history. I could see myself on every page of Labour of Love; reading Bryder's history felt like entering a constructed reality that was nothing like my lived experience of this time.
In her book criticising the Cartwright enquiry, Bryder states that our Education Act enshrines "academic freedom to put forward new ideas and state controversial or unpopular opinions". Whilst this may be true, I was left wondering in her current book why she felt the need to disparage midwifery. What does this history of maternity contribute?
Bryder’s sustained onslaught on midwives is a controversy with no real cause. If you seriously wanted to make maternity care safer, then you would make the case for better support for midwives, for the midwifery model that both holds up internationally and is why NZ is seen as The Best Country to Give Birth. square


taku wāhi mahi my midwifery place
Laura Ashwell is interim Clinical Midwife Manager of Wairarapa Ata Rauru (Wairarapa Hospital Maternity Unit) in Masterton and can’t speak highly enough of her team and workplace. In the first instalment of our new series Taku wāhi mahi | My midwifery place, Laura shares what makes Wairarapa Ata Rauru so special with Amellia Kapa.
After 10 years in LMC practice, Laura - who was born and raised in Masterton - was surprised to find herself signing up for shifts at Wairarapa’s secondary maternity unit in 2021. “My practice partner of 10 years had decided to retire, so we were winding up our practice, I was having another baby, and I’d grown tired of the weight of on-call responsibility. I felt like I needed a change, so I started casual shifts at the hospital toward the end of my pregnancy.”
 AMELLIA KAPA REGISTERED MIDWIFE
AMELLIA KAPA REGISTERED MIDWIFE
To her amazement, Laura enjoyed the change in pace and environment more than she could have anticipated. “I was pleasantly surprised by how much I enjoyed it. I went straight into LMC practice as a new graduate midwife, so I didn’t realise how isolating LMC work had been until I got there. I had an incredible practice partner - she’s my best friend and midwifery mum - but you’re not together all day.
You’re with women and even though you might be conversing all day, it can still be lonely work. I didn’t realise how much I’d been missing until I was part of a bigger team.”
Following the birth of her son, Laura returned to the hospital in a permanent capacity, starting quality work and other projects, in addition to shifts. “The clinical midwife manager at the time was going overseas, so I expressed my interest as interim clinical manager and, seven months later, here I am in that role and loving it.”
Named Wairarapa Ata Rauru by local kaumātua Mike Kawana, the unit sees around 450-500 births per year and when asked what makes it such a great place to work, Laura is clear. “It’s our people; it’s the women, our community and whānau. It’s our core team, our senior midwifery leadership team, our
40 | MIDWIFE AOTEAROA FEATURE
Michelle Thomas and Laura Ashwell (interim Clinical Midwife Manager) Wairarapa Te Whatu Ora

DOM and our LMCs; it really is the people that make our unit so amazing.”
“We all have the same focus,” she elaborates. “We want to provide the best care possible whether we’re in the community, sitting at a desk, or on the ward. Everyone’s striving towards the same goal of providing equitable, women-centred care.”
It’s not always smooth sailing, as Laura illustrates. “We’re not perfect. Like every area of NZ, issues crop up, but I think as a smaller team we’re able to address them and adapt relatively quickly - whether it’s changes in best practice, quality issues, interface issues, or personal issues. We’re able to move through challenges swiftly, which makes for positive relationships not just between our LMC and core midwives, but our wider team, including our obstetricians, social workers, administrative staff and health care assistants. We’re really lucky. It’s a great place to be and work.”
“We’re not immune to those wider workforce issues either,” she clarifies. “We still need to attract more midwives to the region and we’d love for our staff to be paid what they deserve, but we have a really healthy, proactive team here at the moment which I’m really proud to be a part of. It’s been truly rewarding to be part our senior leadership team, which I wasn’t expecting. I thought that feeling only came through one-on-one relationships with women; I wasn’t aware I could get it from a role like my current one. So that’s been really refreshing.”
Working in one of Aotearoa’s smallest secondary maternity units makes for close, meaningful connections, which Laura values above all else. “You can’t go anywhere without seeing a māmā, aunty, nana or child you know, which really fills my cup as a midwife. We’re constantly getting feedback from the people we care about the most and that’s part of being in our small-knit community - the rewards feel even greater.” square
Comfort and safety for babies newborn-2 years

More restful, safer sleep and helps prevent flat head
• More restful, safer sleep limb and hip movement
Goes over any type of swaddling, sleeping bag or sleepwear, for a snug and more restful sleep
• Ensures swaddling, sleepwear, Sleepingbag use is safer and cosier
Natural, flexible body, limb and hip movement
• Excellent for babies requiring varied sleep positions or cot elevation est 1992 Helps keep young babies comfortably o the tummy; older babies turn freely within the wrap
safely lasts two babies aged 0-2 yrs CLINICALLYPROVEN 100%SAFETYRECORDEST.1992

The World’s Safes t Baby Wrap
* s a f e l y l a s t s t w o b a b i e s a g e d a p p r o x i m a t e l y 0 -2 y r s
Use code ‘NZCOM’ for 20% OFF
* www.safetslee

TRUSTED • SAFE • UNIQUE
EPI-NO is clinically proven to of an intact per ineum, reduce episiotomy, and is safe to use EPI-NO is a dual pur pose CE approved medical device designed muscles from ear ly in pregnancy, and again postpar tum The per ineal stretching exercises commence concur rently after Week 36.
EPI-NO Childbir th Tr aining has been accepted in Austr alia & New Zealand for over 15 year s as an effective prepar ation for women choosing a natur al vaginal bir th
EPI-NO Patient Brochures can be requested for New Zealand via info@starnbergmed.co.nz
Over 65,000 EPI-NO births in Austr alia and New Zealand. Available in over 20 countr ies wor ldwide www.starnbergmed.co.nz
Available online with shipment from Auckland and at selected phar macies.
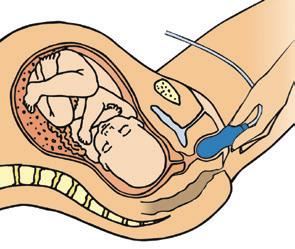
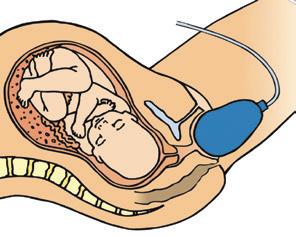

‘The human body performs to maximum trained and prepared. Childbir th is no exception ’ Dr Wilhelm Hor kel, Star nberg (EPI-NO inventor)


Germany
w w.safet sleep.com CLINICALLYPROV E N EFAS • DELLAIRT •

New Zealand College of Midwives Directory
National Office
PO Box 21-106, Christchurch 8140
Ph 03 377 2732 Fax 03 377 5662 nzcom@nzcom.org.nz www.midwife.org.nz
Auckland Office and Resource Centre
PO Box 24487, Royal Oak, Auckland 1345 Ph 09 625 9764 Fax 09 625 0187 auckadmin@nzcom.org.nz
College Membership Enquiries
Lisa Donkin membership@nzcom.org.nz 03 372 9738
Chief Executive
Alison Eddy
Co-Presidents
Beatrice Leatham bea.tangatawhenua.copres@nzcom.org.nz Debbie Fisher debbieF.tangatatiriti.copres@nzcom.org.nz
National Board Advisors
Kuia: Crete Cherrington
Elder: Sue Bree
Education Advisor: Tania Fleming
Regional Chairpersons
Auckland Jacquelyn Paki, Mel Nicholson auckchair@nzcom.org.nz
Bay of Plenty/Tairāwhiti
Cara Kellet chairnzcomboptairawhiti@gmail.com
Canterbury West Coast
Sheena Ross chairnzcom.cantwest@gmail.com
Central
Laura McClenaghan centralchair@nzcom.org.nz
Nelson Marlborough
Emma Neal tetauihunzcom@gmail.com
Northland
Shelley Tweedie
tetaitokerauchair@nzcom.org.nz
Otago
Jan Scherp, Charlie Ferris otagochair@nzcom.org.nz
Southland
Liz Whyte liz.whyte@netspeed.net.nz
Waikato Taranaki Jenny Baty-Myles chairwaikatonzcom@gmail.com
Wellington Suzi Hume nzcomwellington@gmail.com
Regional Sub-Committees
Hawke's Bay Sub-Committee
Linley Taylor midwife.linley@gmail.com
Horowhenua
Laura McClenaghan midwife.laura@hotmail.co.nz
Manawatu Sub-Committee
Megan Hooper-Smith megan.scott@live.com
Emma LeLievre emma@LMCmidwife.com
Taranaki Sub-Committee Ange Hill nzcom.taranaki@gmail.com
Wanganui Sub-Committee
Laura Deane laura.deane@wdhb.org.nz
Consumer Representatives
Home Birth Aotearoa
Bobbie-Jane Cooke bobbiejane.homebirth@gmail.com
Parents Centre New Zealand Ltd Liz Pearce e.pearce@parentscentre.org.nz
Royal New Zealand Plunket Society
Zoe Tipa zoe.tipa@plunket.org.nz
Student Representatives
Paytra Buckrell paybuc01@student.wintec.ac.nz
Te Rina Apelu sgp0097@aut.ac.nz
Ngā Maia Representatives www.ngamaia.co.nz
Dani Gibbs dani.midwife.maori@gmail.com
Lisa Kelly lisakellyto@yahoo.co.nz
Pasifika Midwives Representatives
Talei Jackson
Ph 021 907 588 taleivejackson@gmail.com
Ngatepaeru Marsters
Ph 021 0269 3460 lesngararo@hotmail.com
MERAS / General Enquiries & Membership
PO Box 21-106, Christchurch 8140 www.meras.co.nz
Ph 03 372 9738 meras@meras.co.nz
MMPO mmpo@mmpo.org.nz
Ph 03 377 2485 PO Box 21-106, Christchurch 8140
Rural Recruitment & Retention Services 0800 Midwife/643 9433 rmrr@mmpo.org.nz
Resources for midwives and women
The College has a range of midwiferyrelated books, leaflets, merchandise and other resources available through our website: www.midwife.org.nz/shop
ISSUE 108 MARCH 2023 | 43 DIRECTORY
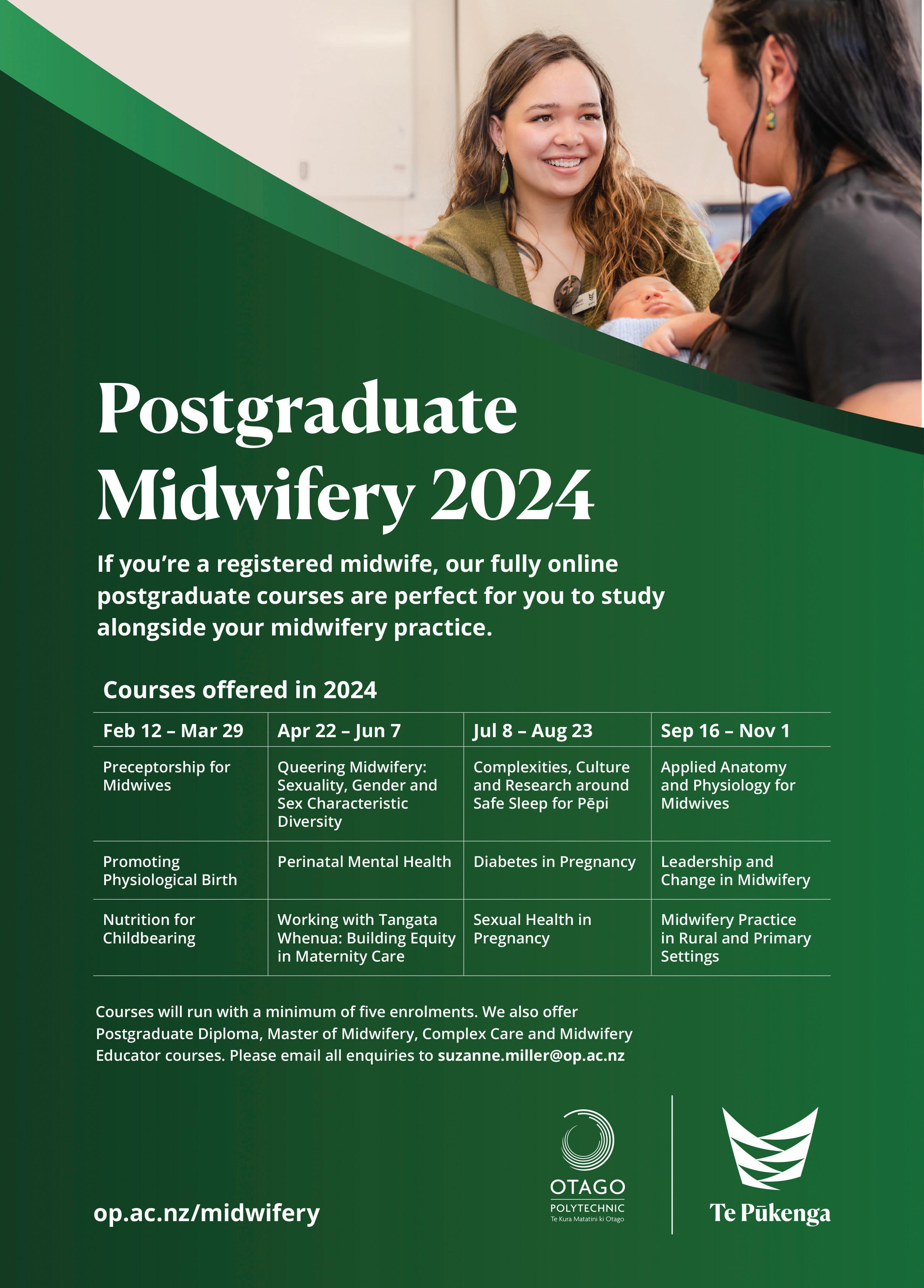






 HAYLEY MCMURTRIE EDITOR & PUBLICATIONS MANAGER
Email:
HAYLEY MCMURTRIE EDITOR & PUBLICATIONS MANAGER
Email:




















 CAROLINE CONROY MERAS CO-LEADER (MIDWIFERY)
CAROLINE CONROY MERAS CO-LEADER (MIDWIFERY)


 WAYNE ROBERTSON EXECUTIVE DIRECTOR, MMPO
WAYNE ROBERTSON EXECUTIVE DIRECTOR, MMPO

 TAMARA KARU
NGĀ MAIA GENERAL MANAGER
TAMARA KARU
NGĀ MAIA GENERAL MANAGER




 AMELLIA KAPA REGISTERED MIDWIFE
AMELLIA KAPA REGISTERED MIDWIFE








 BRIGID BEEHAN MIDWIFERY ADVISOR
BRIGID BEEHAN MIDWIFERY ADVISOR

 VIOLET CLAPHAM MIDWIFERY ADVISOR
VIOLET CLAPHAM MIDWIFERY ADVISOR
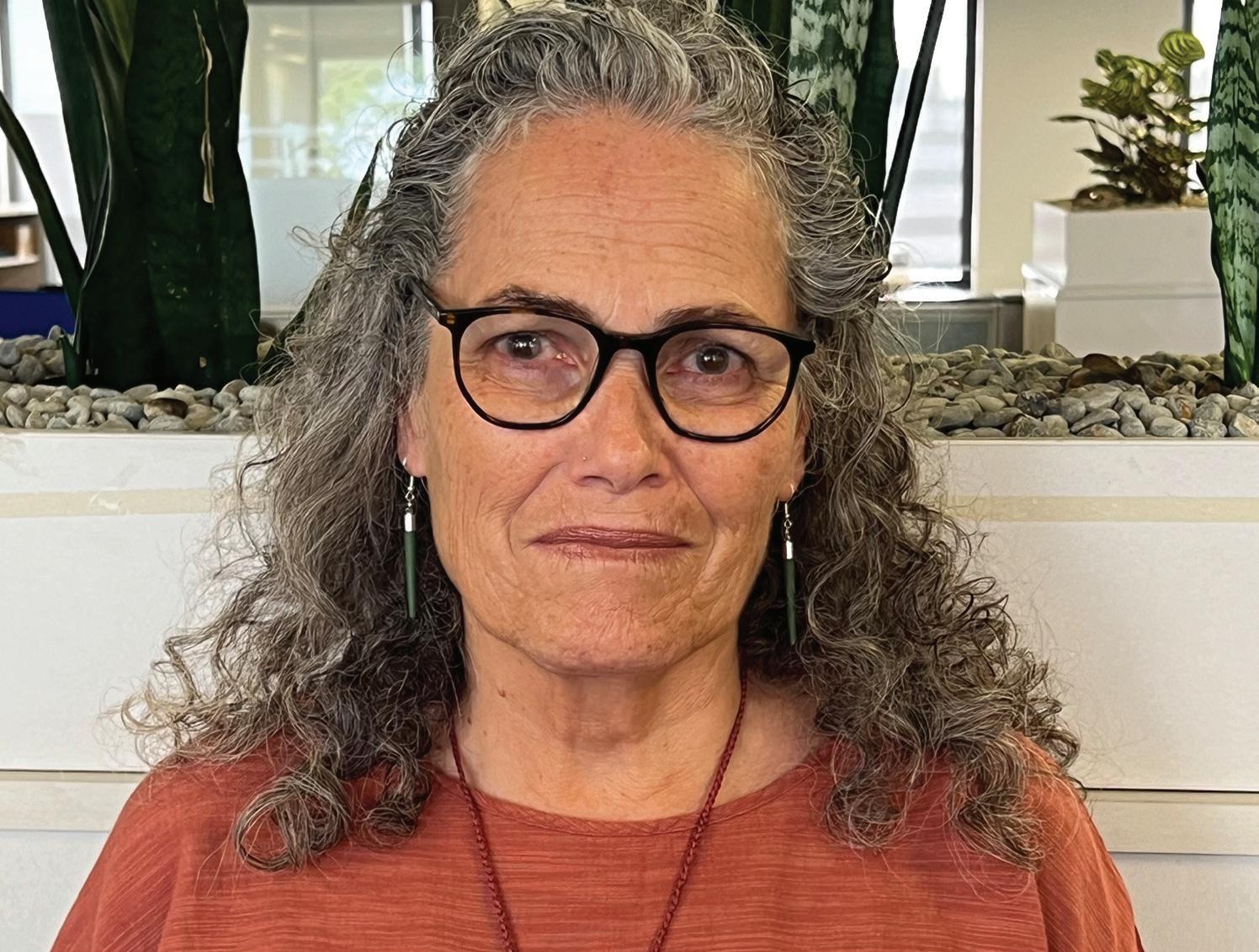
 CAROL BARTLE POLICY ANALYST
CAROL BARTLE POLICY ANALYST


 SIAN BURGESS
SIAN BURGESS