MĀ WHERO, MĀ PANGO

THE COLLEGE WELCOMES ITS FIRST MĀORI MIDWIFERY ADVISORS P.20

ELECTION'23: WHAT ARE THE MAIN PARTIES' MIDWIFERY POLICIES? P.24
CLIMATE CHANGE: FOOD SYSTEMS, ULTRA-PROCESSED FOODS, PLASTIC WASTE AND 'GREEN FEEDING’ P.28
BREASTFEEDING CONNECTION: TONGUE TIE P.32
ISSUE 110 SEPTEMBER 2023 I THE MAGAZINE OF THE NEW ZEALAND COLLEGE OF MIDWIVES
Early bird registration closes
Friday 15 September
02 - 04
NOVEMBER 2023
A conference to reconnect , re-energise and celebrate with your midwifery colleagues.
KEYNOTE PRESENTATIONS
• Rejuvenating Ngāi Tahu customary birthing practices - What does this look, sound and feel like? Dr Kelly Tiako
• Tū te turuturu o Hineteiwaiwa: Supporting maternal wellbeing in the context of whānau, whenua and wairua Naomi Simmonds

Whanaungatanga can change the world... one birth at a time
• The power of relationships in reclaiming birth Dr Rachel Reed
• Valuing vā and voice: Nurturing Pasifika relationships Talei Jackson
• Joan Donley Memorial Address Deb Pittam and Crete Cherrington
PANEL DISCUSSIONS
Perineal protection in Aotearoa - Holistic approaches and informed choice
Is induction of labour the latest pandemic? The future of the midwifery model of care
REGISTER ONLINE
midwife.org.nz/conference-2023
FORUM
FROM THE PRESIDENT
4. COURAGEOUS STEPS
FROM THE CHIEF EXECUTIVE
5. A DEEP AND ENDURING IMPRESSION
8. BULLETIN
10. YOUR COLLEGE

12. YOUR UNION
14. YOUR MIDWIFERY BUSINESS



18. NGĀ MAIA
Hayley McMurtrie
E: communications@nzcom.org.nz
ADVERTISING ENQUIRIES
Hayley McMurtrie
P: (03) 372 9741
MATERIAL & BOOKING
Deadlines for December 2023
Advertising Booking:
3 November 2023
Advertising Copy:
10 November 2023
ADVERTISING POLICY AND DISCLAIMER: The New Zealand College of Midwives maintains a schedule of guidelines to exclude advertisements for products or services that are not aligned with its principles and ethics. Every effort is made to ensure that advertising in the magazine falls within those guidelines. Where advertising is accepted, this does not imply endorsement by the College of the product or service being promoted Aotearoa New Zealand Midwife is published quarterly for the New Zealand College of Midwives. The articles and reports printed in this newsletter are the views of the authors and not necessarily those of the New Zealand College of Midwives, its publishers or printers. This publication is provided on the basis that New Zealand College of Midwives is not responsible for the results of any actions taken on the basis of information in these articles and reports, nor for any error or omission from these articles and reports and that the College is not hereby engaged in rendering advice or services. New Zealand College of Midwives expressly disclaims all and any liability and responsibility to any person in respect of anything and of the consequences of anything done, or omitted to be done, by any such a person in reliance, whether wholly or partially upon the whole or any part of the contents of this publication. The College acknowledges and respects diversity of identities through the language used in this publication. Te reo Māori is prioritised, in commitment to tāngata whenua and te Tiriti o Waitangi. To maintain narrative flow, the editorial style may use a variety of terms. Direct citation of others’ work maintains the original authors’ language, and contributing writers’ language preferences are respected. All advertising content is subject to the Advertising Standards Authority Codes of Practice and is the responsibility of the advertiser. Contents Copyright 2020 by New Zealand College of Midwives. All rights reserved. No article or advertisement may be reproduced without written permission. ISSN: 2703-4546.

ISSUE 110 SEPTEMBER 2023 | 3 20 24 28 32 37
16. CLASS ACTION UPDATE
17. JOYCE COWAN, ONZM FEATURES
ISSUE 110 SEPTEMBER 2023
19. PASIFIKA 20. MĀ WHERO, MĀ PANGO 24. ELECTION '23 28. CLIMATE CHANGE 32. BREASTFEEDING CONNECTION 36. BOOK REVIEW 37. FROM BOTH SIDES DIRECTORY
EDITOR
Welcome to Issue 110 of Midwife Aotearoa New Zealand
This issue celebrates the quality of midwifery in Aotearoa, highlighted by some hard-to-hear stories from around the globe, not least from midwives in war torn cities and those battling for recognition and any level of autonomy.
The ICM congress left a lasting impression on our CE and president and offered a different lens through which to view our own troubles. Understanding the importance and widereaching effects of a strong, effective and wellsupported system of midwifery care continues to be lost on many of our politicians (p. 24).
Workforce shortages continue to challenge our whole profession; in this issue MERAS urges its members to keep accurate and regular records in order to bring visibility to the current situation, while MMPO highlights the vital role of collegiality in times of significant understaffing.
We welcome two new Māori midwifery advisors and introduce them to you on page 20. They are both incredible wāhine doing important work and we are thrilled to have them on the team.

In our regular features, Breastfeeding Connection considers the issues that tongue tie presents for midwives with some helpful hints for assessment and management; meanwhile, the climate change article considers processed foods and introduces us to the concept of green feeding (p.28).
Don’t miss your chance to register for the College conference at the early bird prices (until 15 September). We are looking forward to being able to come together and to return to Christchurch for the first time post-quakes. Following a number of challenging years, it is exciting for midwives to have the opportunity to reconnect and re-charge. We hope to see you there.
As we go to print we are seeking nominations for co-presidents. Should multiple candidates apply for either role, members will be asked to vote via online ballot. Please keep an eye out for member emails and College e-news (Pitopito Kōrero) for important updates.
Haere pai, Hayley square
HAYLEY MCMURTRIE EDITOR & PUBLICATIONS MANAGER Email: communications@nzcom.org.nz

First clear off the weeds, then plant. Or if you do your work properly, those following can accomplish their task and together, everybody gets the job done. (Mead & Grove, 2001)
International gatherings always provide an opportunity for comparison and reflection, and ICM 2023 in Bali was no exception. The contrast between the status of tāngata whenua in Aotearoa and indigenous populations elsewhere in the world was unsurprisingly stark, as midwives and other health professionals shared stories of inequity, scarcity, and colonisers’ privilege.
Hearing these stories made me appreciative of the progress we’ve already made in Aotearoa, but they were also a poignant reminder of where we’ve been in the nottoo-distant past. In many ways, we are miles ahead of the rest of the world; Māori are now on the other side of struggles many indigenous populations are still fighting to have acknowledged. And yet, despite the significant progress made in Aotearoa, we are still nowhere near achieving equity.
One thing’s for sure: we cannot afford to become complacent. Healthy relationships require constant effort and energy, and this concept applies not only to our personal connections, but equally to our wider, collective relationships as a nation. Te Tiriti o Waitangi settlements and bi-lingual signage do not equate to cultural safety, and it may be some time before our mokopuna, Māori or tauiwi, no longer need to use terms like ‘te ao Māori’, because they won’t see or feel a divide. Reassuringly - and in perfect alignment with Matariki - two newly created Māori midwifery advisor roles were recently taken up by Te Paea (Shannon) Bradshaw and Jay
Waretini-Beaumont, affirming the College’s waka is pointed firmly in the right direction. This was further bolstered by overwhelming support from the membership to move to co-presidency; yet another tohu that Aotearoa midwives have no interest in looking back.
These are courageous steps, e te whānau; steps which shouldn’t be underestimated. As the whakatauki on pg. 22 illustrates, with red and black, the work is done. This points to the importance of collaboration - a concept midwives intuitively understand, due to the very nature of our mahi.
Not only do we know how important it is to collaborate and work harmoniously with each other as midwives, but in many instances the collaboration needs to happen outside of midwifery - with other health professionals, iwi, hapū and whānau. A classic example of this is hapū wānanga. There simply aren’t enough midwives to go around, and a number of hapū wānanga throughout the motu are being facilitated by non-midwives (supported by midwives), to ensure whānau don’t miss out on this vital service.
Thankfully, there are dedicated, passionate whānau out there willing to sacrifice their weekends and evenings to support the kaupapa. Although this responsibility shouldn’t fall on whānau, the reality is, it does. Until we achieve equity within our workforce and have enough midwives to deliver maternity services across all settings, collaborative ways of working will continue to be necessary, and we have whānau to thank for stepping up. square
4 | NEW ZEALAND COLLEGE OF MIDWIVES MAGAZINE FROM THE EDITOR 4 | AOTEAROA NEW ZEALAND MIDWIFE FROM THE PRESIDENT
from the president, new zealand college of midwives, nicole pihema (Ngāpuhi, Te Rarawa)
“E ngaki ana a mua, e tōtō mai ana a muri”
A DEEP AND ENDURING IMPRESSION
The International Confederation of Midwives (ICM) Council meeting and Congress (conference) in Bali which I attended in June has left a deep and enduring impression on me, and I have found myself frequently reflecting back on the whole experience over the past few weeks.


Established over 100 years ago, ICM is a representative organisation, whose membership consists of over 130 midwifery member associations. It is a ‘peak body’ which acts on behalf of its members and the midwifery profession globally, developing and setting standards for midwifery education, regulation and practice as well as advocating for the ongoing growth and development of the profession. Its overarching aim is to improve access to, and the quality of, maternal and newborn care through the advancement of the midwifery profession.
Unlike New Zealand, the vast majority of countries in the world don’t have well developed and mature midwifery education and regulation systems, let alone the health system settings which enable midwives to work autonomously across
all areas of their scope of practice. For many countries ICM’s resources are critical in supporting midwifery to achieve the necessary progress. New Zealand midwives have been represented by ICM since 1981, and its support and resources were used in our own journey to re-establish midwifery autonomy in Aotearoa in 1990.
In 2014, the Lancet published a series on Midwifery. One of the papers stated that “Midwifery with both family planning and interventions for maternal and newborn health could avert a total of 83% of all maternal deaths, stillbirths, and neonatal deaths” (Homer et al., 2014).
The World Health Organization (WHO) recognises that maternal mortality remains unacceptably high, with about 287,000 women dying during and following pregnancy and
ISSUE 110 SEPTEMBER 2023 | 5
from the chief executive, alison eddy
The newly elected ICM Board.
Although many challenges remain, the discussion at the Council meeting and presentations at the subsequent Congress reflected ICM’s success in supporting the scaling up our profession, and the provision of midwifery-led services and models of care.
childbirth in 2020. Almost 95% of all maternal deaths occurred in low- and lowermiddle-income countries in 2020, and most could have been prevented, with the most common causes being haemorrhage and sepsis. Scaling up midwifery has enormous potential to save lives, however it is no small feat, as it is estimated that there is a global shortage of close to 1 million midwives.


It is against this backdrop that Nicole and I joined attendees at the ICM Council meeting which was held in Bali during the three days preceding the Congress. The Council is a key part of the ICM’s accountability to its members and a critical part of its governance structure. Once every three years, the Council meetings are held in person before the triennial Congress, with meetings held virtually in the interceding two years.
With member associations from over 100 countries across the world represented and proceedings translated into English, French and Spanish, the ICM Council meetings are comparable to the United Nations for midwifery. Attendees were randomly seated and Nicole and I found ourselves surrounded by delegates representing midwifery
associations from Finland, Indonesia, Namibia, Sweden and Japan. Council delegates considered a range of topics including the ICM annual and triennial reports, changes to the processes for selecting ICM board members and presidents, the impact of climate change on maternal and newborn health and what midwives can do to mitigate these effects, as well as a lively discussion on midwifery models of care.
ICM has six geographic regions (which align with those of the WHO). New Zealand is in the Western Pacific region and the Council agenda included a regional meeting where we connected with midwives from the Philippines, Papua New Guinea, Fiji, Indonesia, Australia, Japan, Taiwan, Hong Kong and South Korea. I have the privilege of being the incoming member for the Western Pacific region on the ICM board.
The challenges that many midwives face were brought into sharp relief for Nicole and I when during one of the breaks at the Council meeting, we communicated via Duolingo (smart phone app) with a French speaking midwife delegate from Côte d'Ivoire (Ivory Coast) in western Africa. A crude calculation of the number of births per annum in comparison with the number of practising midwives revealed that New Zealand has approximately one midwife per 20 births. Reliable estimates in countries such as Côte d'Ivoire are challenging due to incomplete birth registration and workforce data. In spite of these limitations our back of the envelope calculations estimated that the ratio for Côte d'Ivoire was something like one midwife for several hundred births. The difference in maternal mortality ratios said it all, with Côte d'Ivoire reporting 480 maternal
deaths per 100,000 livebirths in comparison with 7 per 100,000 in New Zealand.
I have been fortunate to attend an ICM Council meeting and Congress once before - nearly a decade ago in Prague, 2014. The progress our profession has made globally since then was clearly obvious as delegates animatedly shared their countries’ successes in advancing midwifery. ICM has grown significantly in the last six years under the leadership of its Chief Executive, New Zealand midwife Sally Pairman. It has expanded from a staff of approximately four, to nearly 30 staff from a diverse range of cultures around the world. It has successfully attracted funding from a wide range of partner organisations such as the Bill and Melinda Gates Foundation, World Health Organization and others, and has been able to expand its reach and influence as a result.
Although many challenges remain, the discussion at the Council meeting and presentations at the subsequent Congress reflected ICM’s success in supporting the scaling up our profession, and the provision of midwifery-led services and models of care. I attended presentations about the establishment and success of midwifery-led units in India, Afghanistan and western Africa. The presenters noted that demand for these services is overwhelming and they discussed the need to limit the number of women who could access them in order to maintain the standard or quality of care. The irony of this was not lost on me as we face the opposite issue in Aotearoa, one of inadequate utilisation of midwifery-led units and overutilisation of secondary and tertiary hospitals. Another highlight from the Congress was the showcasing of graduates from ICM’s Young Midwifery Leaders (YML)
and Neonatal
Specialists Request a complimentary trial of one or both beds and experience first hand the difference these beds make. activehealthcare.co.nz | 0800 336 339 | sales@activehealthcare.co.nz
Obstetric
Bed
Baby Cot
Request a free trial 6 | AOTEAROA NEW ZEALAND MIDWIFE FROM THE CE
Ave 2 Birthing Bed Natural birthing bed designed for improved outcomes.
programme. Peppered throughout the Congress were a variety of presentations from this group, who were selected from applicants from low resource settings to participate in a structured leadership development process. The results were impressive, with a range of young midwives from diverse countries and backgrounds demonstrating visible leadership and advocacy for the profession in their own countries as well as globally. I left the Congress determined to understand more about this work that ICM has undertaken and to learn how we can apply the principles here in Aotearoa.
The two most enduring reflections I have held onto following the Bali Council meeting and Congress are similar to those I experienced after Prague in 2014.
Firstly, our midwifery practice context in Aotearoa is far ahead of the majority of other countries around the world. This was evident in Bali with a number of New Zealand midwives presenting their impressive work, including president Nicole Pihema’s presentation on mentoring from te Ao Māori perspective. However, as a small country with a relatively small number of midwives (when considered on a worldwide scale) we don’t generate a lot of research. Thus we have limited capacity to share our knowledge and experiences on the global stage. There is so much more we could share if we had the resources to generate more home-grown research which is grounded in our model of care and professional context. We desperately need more research on ‘normal’ pregnancy and childbirth, how midwifery practice can protect and enhance it, and in particular within a continuity of care context.
Secondly, there is something truly inspirational about being amongst over 2,000 midwives from around the globe. The buzz and energy in the room during the opening ceremony, plenary sessions, break times and during the multiple conversations that occurred over the entire event (both the Council meeting and Congress) left me with an overwhelming sense of collective purpose, identity, emotion, connection and understanding. Midwifery is a global movement, and although within New Zealand we are incredibly privileged, there is an underlying similarity to the challenges that all midwives face. We have more in common than not with our worldwide midwifery colleagues. Our universally shared philosophy is our point of difference, it is what defines us and makes us unique and distinct as a profession. It is what enables an immediate and unspoken connection to occur between midwives - regardless of which country we are from, which language we speak, which culture we belong to or hold, or which ethnicity we identify with. This statement from the 2014 Lancet series provides a pertinent framing:
Although this Series is about midwives and midwifery services, the frames of reference are the needs of the woman and her newborn infant. The technical evidence this Series summarises is based on a particular set of values and a distinctive philosophy. These values include respect, communication, community knowledge and understanding, and care tailored to a woman’s circumstances and needs. The philosophy is equally important—to optimise the normal biological, psychological, social, and cultural processes of childbirth, reducing the use of interventions to a minimum. (Horton & Astudillo, 2014)
Coming back to Aotearoa, it can take a while to process all of these experiences, and get them into perspective. Although the scale of our concerns here may seem relatively miniscule at first glance when considered in the global context, they are ever present, very significant and complex to fix. Our motivation to resolve them must be firmly aligned with that of ICM, to improve access to and the quality of maternal and newborn care, through advancing the midwifery profession. square
ISSUE 110 SEPTEMBER 2023 | 7
therapeutic products bill: update
Although the Therapeutic Products Bill (TPB) has now passed, the Medicines Act 1989 (and Medicines Regulations) and Dietary Supplementary Regulations 1985 still apply until most of the TPB provisions come into force. These are scheduled to occur before 1 September, 2026.
These amendments:
• Create exemption mechanisms for certain small-scale natural health product manufacturers
• Remove many of the obligations that might apply to rongoā Māori practitioners and their services
• Strengthen provisions for the regulation of advertising, which includes some flexibility regarding direct-to-consumer advertising
• Allow for amendments to ensure consistency with international obligations regarding innovative medicines
Natural health products will still be available without a prescription, and practitioners will be able to provide care to clients. The College looks forward to taking part in the next consultation stage, which will
develop separate regulations for natural health products and provide a recognised list of specific ingredients.
For more information on this Bill, see the Manatū Hauora | Ministry of Health website.

To see the College’s Consensus Statement on Complementary and Alternative Therapies, go to https://www.midwife.org.nz/midwives/ professional-practice/guidance-for-practice/square
national cervical screening programme e-learning module
The National Cervical Screening Programme has produced a new series of four clinical training modules to help health professionals understand the upcoming changes to cervical screening.
On completion of the modules, accredited screen-takers, GPs and midwives should understand all clinical aspects of the new primary test for cervical screening and be able to successfully support participants to navigate cervical screening pathways.
To see the course content and enrol in the course, log in to https:// learnonline.health.nz/ square
bulletin 8 | AOTEAROA NEW ZEALAND MIDWIFE BULLETIN
upcoming education workshops
A-Z of Perineal Care
3 Oct, The Victoria Hotel, Ōtepoti / Dunedin
MESR (Midwifery Emergency Skills Refresher)
6 Oct, Waterford Birth Centre Limited, Kirikiriroa / Hamilton
A-Z of Perineal Care
16 Oct, Commodore Christchurch, Ōtautahi / Christchurch
Dotting the I's in a Digital Age: Record Keeping for Midwives
19 Oct, The Devon Hotel, Ngamotu / New Plymouth
MESR (Midwifery Emergency Skills Refresher)
20 Oct, Bithcare Auckland, Tāmaki-makau-rau / Auckland
MESR (Midwifery Emergency Skills Refresher)
17 Nov, Warkworth Birthing Centre, Tāmaki-makau-rau / Auckland
Dotting the I's in a Digital Age: Record Keeping for Midwives

22 Nov, The Pines, Te Whanga-nui-a-Tara / Wellington
MESR (Midwifery Emergency Skills Refresher)
30 Nov, Birthcare Huntly - 5 Onslow Street, Kirikiriroa / Hamilton
MESR (Midwifery Emergency Skills Refresher)
5 Dec, Warkworth Birthing Centre, Tāmaki-makau-rau / Auckland square
ISSUE 110 SEPTEMBER 2023 | 9
your college
section 94 update
When the Pae Ora (Healthy Futures) Act 2022 was passed last year on 1 July, the Primary Maternity Services Notice (previously Section 88 under the Public Health and Disability Act 2000) officially became a Section 94 of the Pae Ora Act. Therefore what was formerly known as “Section 88” is now in fact “Section 94”.
Prior to 1 July 2022, any increases into Section 94 needed to be specifically approved by Cabinet. Since the passing of the Pae Ora Act, the Te Whatu Ora board now have the autonomy to decide how health funding increases are allocated across the sector, and this year decided to apply a 5% funding uplift to Section 94.
The College was informed that as well as the 5% increase in the Section 94 Notice (which was applied differentially across the Notice), there was a significant underspend in the projected 2022/2023 Section 94 budget. We understood that this was due to conservative allocation of fees for the Additional Care Supplement (ACS) and Rural Practice Travel Supplement (RPATS).
The College recognises that the current RPATS funding does not adequately reflect the true cost associated with the travel required while providing midwifery services (rural services in particular), and has advocated consistently for this to be increased.
The ACS was a newly added component in Notice 21 and the initial fees were set conservatively in order to ensure the claims came within the allocated budget. The agreed view was that they would be modified or increased over time as Te Whatu Ora gathered information about how these modules were claimed and how effective they were at recognising and compensating midwives for the additional work required. The College has consistently lobbied for increased funding to be allocated to the ACS, and for increased recognition of acute call outs.
We had been led to believe that the Section 94 underspend from last year's budget would be re-allocated to increase the fees in both the ACS and RPATS. Unfortunately, we were subsequently informed that due to Te Whatu Ora now being a large consolidated entity, any unspent funds are
required to offset overspends in other services. This was deeply disappointing for the College and for midwives. If we had been aware of this possibility we likely would have advocated for a portion of the 5% increase to Section 94 be utilised to increase funding in the ACS and RPATS, rather than it all being allocated into the modules. The College will continue advocating strongly for the required uplifts and additions to the ACS and RPATS square
emergency and disaster relief fund
Following the significant weather events in the upper and middle North Island earlier this year, the Canterbury/ West Coast region proposed that the College establish an Emergency and Disaster Relief Fund (EDRF) to collect donations which could then be disbursed to members who had suffered significant loss or damage to property or belongings as a result of the weather events.
A Terms of Reference (TOR) was developed and an EDRF committee established. The committee membership includes the College CE and four members from the board. The TOR stipulate that the EDRF is formally accountable to the College’s board, thus its activities are overseen by the College’s governing body.
Large donations from three College regions (Canterbury/West Coast, Waikato and Wellington), as well as numerous donations from members, saw the EDRF grow to over $34,000. The EDRF called for applications and once these had been submitted, it met to assess them. All applications were anonymised to minimise the possibility of any bias. The EDRF noted that many applications demonstrated the ongoing nature of the disruption and stress that members were experiencing as a result of loss to property or changes in housing circumstances. A total of 13 applications were received and $29,500 disbursed in total. Every applicant received some financial support. The balance of $4,500 will remain in an interest bearing account, to use as seed funding for future emergency events. The EDRF committee is also considering ways in which it could continue to attract donations in order to have funds on hand should the need arise again. square
10 | AOTEAROA NEW ZEALAND MIDWIFE YOUR COLLEGE
Right: Following the significant weather events this year, it has been proposed that the College establish an ongoing Emergency and Disaster Relief Fund.
FREE Iron in Pregnancy booklet includes:
Evidence-based information
Key iron facts
Iron deficiency signs & symptoms
Top dietary iron tips
Iron-rich recipes
Scan the QR code to order your resources

Rangahau o Kahu pōkai
"Ko te manu e kai ana i te miro nōna te ngahere, ko te manu e kai ana i te mātauranga nōna te ao," The bird that partakes of the miro berry owns the forest, the bird that partakes of education owns the world.
The College and Ngā Maia have established a fund to support Māori midwifery researchers to share and present their mātauranga across Aotearoa and overseas at conferences, hui or wānanga. To be eligible to apply for the funding you need to be a registered midwife and whakapapa Māori and have or have planned to present your research within Aotearoa.


To apply visit www.ngamaiatrust.org/news-and-updates

CAROLINE CONROY MERAS CO-LEADER (MIDWIFERY)
 SAM JONES MERAS CO-LEADER (INDUSTRIAL)
SAM JONES MERAS CO-LEADER (INDUSTRIAL)
bringing visibility to midwifery shortages
A 40% average midwifery vacancy rate across maternity services has been reported in the recent Te Whatu Ora Health Workforce Plan. This will be no surprise to MERAS members, but this figure is only part of the story. What it does not reveal is that in some maternity units the figure has been, or is, more than 70% and challenges the ability to even maintain a maternity service.
The data obtained from Trendcare and other Care Capacity Demand Management components bring much greater visibility to the shortages and resulting pressures.
Our Midwife Aotearoa article in December 2022 highlighted the importance of Trendcare in capturing the work of midwives and the contribution this makes to FTE calculations. Now we focus on how the Variance Indicator Score (VIS) or Variance Response Management (VRM) tools can highlight the pressures that
midwives work under on each shift and actions that can be taken. The VIS score is usually completed at the beginning of each shift on maternity wards and birthing suites, and should be repeated during the shift as workload changes. The VIS score uses a traffic light model as shown in Table 1.
The VIS score reflects the ‘moment in time’ on any shift. The colour is displayed on the ‘Hospital at a Glance’ screens (HAAG) visible to the Duty Managers and highlights those areas with care capacity deficits. The VIS score can change several times during a shift and one of the challenges for the midwife coordinating a shift is to re-VIS whilst in the middle of an escalating acute or emergency event.
IS YOUR VIS NORMALISING THE SHIFT SHORTAGES?
There are criteria to be scored ‘yes/no’ as part of the VIS score. There is some concern that VIS scoring is reflecting the current roster and staffing shortages, rather than the agreed CCDM roster. Table 2 highlights considerations when scoring.
ACTIONS TO TAKE
Ideally a maternity ward or birthing suite should have a green VIS score. If the ward is in yellow, orange or red, the aim is to
take action that returns the ward to green as quickly as possible. Each maternity service should have a VRM Escalation Plan that outlines actions to take at yellow, orange or red, with a focus on increasing acuity in the middle of the night or at weekends when there are no midwife managers or senior midwives working. Possible actions include:
• delaying or deferring elective work such as IOL or elective sections
• calling in additional staff through an oncall roster, ‘senior midwives out of hours roster’ or an LMC roster
• delaying secondary care handover from LMCs
ACHIEVING VISIBILITY
Maternity CCDM working groups have been established in most maternity units. At these meetings the local MERAS workplace representatives, Midwife Managers, Directors of Midwifery, national CCDM maternity advisor and the MERAS Co-leader (Midwifery), review the information that is being obtained from Trendcare, the core data set and VIS/VRM for the month. Reports are developed to highlight the challenges and the actions needed to occur locally to support the midwives and achieve a safe workplace. This

Excess care capacity Significant care capacity deficit Critical care capacity deficit Early variance Staffing meets demandcapacity and demand matched VIS Colour Definition TABLE 1: VARIANCE INDICATOR SCORING (VIS) TOOL 12 | AOTEAROA NEW ZEALAND MIDWIFE YOUR UNION
Variable Factors to consider
Missed meal breaks
The first meal breaks should occur within five hours of the shift commencing. To achieve this, meal breaks should be started or planned by four hours into the shift. If it is going to be difficult achieving meal breaks, this should be escalated to the midwife manager or duty manager. Re-VIS when it is evident that there will be missed meal breaks
Skill mix Indicate where staff on duty do not have the required skills set for that maternity area or where there is no senior midwife on duty in a secondary or tertiary unit ward. Re-VIS if a midwife has left the ward (e.g., to theatre, escort, ED) and this has impacted on available skill mix
Staff mix
It is important that roster gaps are not normalised. Indicate when:
• the staffing on the shift does not reflect the approved CCDM roster. This may differ from the actual number of staff rostered. In most maternity units the registered staff should be 100% midwifery.
• the HCA or clerical staff are absent and midwives are doing these tasks.
• there are casual or locum midwives working who are unfamiliar with the ward area
• you have a midwife ‘on-call’ due to roster shortages and this is not part of the CCDM roster model for your ward. Re-VIS if a midwife has left the ward to go to theatre, do an escort or go to ED, as this has changed the staff mix on the ward
Negative variance
Positive variance
Delayed care
Deemed professionally unsafe
The negative or positive variance is automatically generated from the patient type predictions and data on the allocate screen. Re-VIS when new admissions or acute assessments have been added to Trendcare or to the Allocate Staff screen or patients have been discharged, as this will change workload and influence the variance
Indicate if there is delay in providing care to women or babies on the ward, or if an IOL or elective section is delayed due to acuity
Indicate if as the coordinating midwife you believe the clinical situation is unsafe. This might be a situation where the number of midwives on the shift is less than the agreed minimum staffing, there is no experienced or senior midwife to coordinate, or the workload exceeds available staff. Re-VIS as situations arise and if possible complete a datix or safety 1st form to highlight the situation and actions taken.
is then reported to the CCDM Council and the hospital senior management.
A focus is reducing the orange and red VIS that occur afterhours when there is less support available. Actions that can be taken include:
• prioritising night shift and weekend rostering
• discussions with medical staff to manage number of IOL or elective sections per day based on available staff
• non-clinical senior midwives agreeing to work some clinical days each week
• increasing clerical and HCA support after hours to allow midwives to focus on midwifery
• increasing the number of clinical midwife managers, clinical midwife coordinators or clinical midwife coaches so that new graduate midwives and other staff are supported during shifts and there is good coordination of the maternity services across 24 hours
The workforce shortages create significant challenges but using the tools available within CCDM each shift brings a focus to midwifery and maternity service needs. Completing VIS scoring each shift, and as the acuity changes on each shift, is important.
There is currently a pilot project underway at several maternity units, trialling a revised VIS scoring tool adapted specifically for birthing suites. MERAS will provide updates as information becomes available.
HOLIDAYS COMPLIANCE REVIEW
The work reviewing the way hospital payroll systems have interpreted the Holidays Act is close to finishing. The annual leave and public holiday payments over the last 10 years have been reviewed. District hospitals are expected to start paying out monies owing to staff from August, starting with the Auckland region, and this will continue into 2024.
A website will be established so that ex-employees can calculate if they are owed any money and how they make an application.
PAY EQUITY DISCUSSIONS
At the time of going to print MERAS is in discussions with Te Whatu Ora to recommence pay equity discussions, with the aim of reaching a final proposed settlement to vote on.
MERAS is also working closely with employers of the primary units and services outside of Te Whatu Ora to progress a pay equity claim for midwives employed in these units. square
For MERAS Membership merasmembership.co.nz
www.meras.midwife.org.nz

ISSUE 110 SEPTEMBER 2023 | 13 YOUR UNION
TABLE 2: FACTORS TO CONSIDER WHEN DOING VIS
WAYNE ROBERTSON EXECUTIVE DIRECTOR, MMPO
enhancing the group practice structure: better sustainability and continued collegiality

As the midwifery workforce faces significant understaffing and individual midwives grapple with stress and deteriorating work-life balance, a positive, proactive group practice can play a pivotal role in increasing sustainability and enhancing collegial behaviour.
A strong midwifery group practice creates and maintains an environment where midwives feel supported and motivated. Prioritising things such as sharing a common sense of purpose, effective communication, shared responsibility and flexible scheduling, helps ensure sustainability and protects collegial behaviour, despite challenges such as stress and burnout.
Sharing a common sense of purpose is key to both personal fulfilment and collective success, supporting motivation, collaboration and unity. On an individual level, a strong sense of purpose fuels job satisfaction and resilience. When this aligns with the collective purpose, it strengthens the practice’s function, enhancing cooperation, effectiveness, efficiency and sustainability.
Effective communication maintains a healthy and sustainable working environment. Various strategies support this:
• Regular practice meetings provide a platform for discussing cases, changes in procedures or guidelines, administrative matters or any challenges facing the team. Regular meetings foster collective problemsolving and decision-making.
• Making best use of digital technology that facilitates real-time communication makes collaboration and information sharing more
effective. It is vital to consider how digital tools are used, secured and kept private.
• Building and maintaining strong interprofessional relationships with maternity facilities and other health professionals enables midwives to extend their practice's capacity.
• Engaging with the communities they serve can help midwives understand the unique needs and challenges of whānau in their area. Such engagement also raises the profile of midwives in the community, increasing the value of their services and thereby promoting sustainability.
Sharing responsibility in a midwifery practice is when all midwives contribute to the tasks, decisions and outcomes in an equitable way. This can take on several forms:
• Reasonable workload: Responsibilities are distributed among practice members, considering their skills, experience and capacity.
• Group decision-making: Important decisions are made collectively. Each midwife has a voice and their opinions are considered and respected.
• Collegial caseload care: While a midwife lead will be assigned to each māmā, the team collectively ensures access to support continuity of care.
• Peer support and mentoring: All midwives in the practice support and learn from one another. More experienced midwives mentor less experienced ones, while newer midwives can bring fresh perspectives and knowledge.
• Crisis management: In challenging situations, the midwifery practice comes together to manage the crisis. This may involve reallocating tasks, providing extra support to those in need or seeking external assistance.
Flexible scheduling and time off involves accommodating individual midwives’ varying needs and circumstances. For example:
• Supporting part-time options: For those unable to work full-time due to personal responsibilities or health reasons, part-time options can help retain experienced staff who might otherwise leave the profession, and also opens up the possibility of hiring more midwives who prefer part-time work.
• Implementing an equitable on-call system: Midwives could be placed on-call during certain periods or on rotation.
• Flexible leave: Flexible time off helps midwives maintain a good work-life balance. Similarly, providing extended leave for personal reasons will help sustain practice,
14 | AOTEAROA NEW ZEALAND MIDWIFE YOUR MIDWIFERY BUSINESS
reinforcing the message that self-care is not a luxury, but a necessity.
Supporting continued professional development involves creating an environment that encourages learning and growth. Ensuring equitable professional development opportunities, even when a practice is under pressure, is critical for the overall growth and well-being of the team. Strategies include:
• Access to varied learning methods, including in-person and online workshops
• Providing resources to support learning
• Support from experienced midwives to less experienced colleagues
• Flexible policies that encourage midwives to take time off for professional development activities, including during high-stress periods.
DEVELOPING DIGITAL LITERACY
Midwives can leverage an evolving range of technologies to support their practice:
• Digital platforms (such as Microsoft 365 and Teams) enable virtual and remote meetings and a direct means of communication, helping overcome the mobile nature of midwifery care and the use of multiple communication modes.
• Digital records (e.g., clinical records, practice files and midwife calendars) assure better information sharing and coordination among practice midwives.
• Digital applications such as Microsoft OneDrive, online banking and Xero accounting software help with managing self-employed business-related needs. However, simply having access to digital technologies is not enough; midwives also need to ensure they have the skills to use these tools effectively. This involves a commitment to training and understanding the importance of maintaining digital privacy and security.
Finally, the induction of graduate (new) midwives into a midwifery group practice can be conducted in a way that positively supports their first touch to, and the sustainability of, the midwifery profession (Figure 1).
A welcoming and supportive environment that provides comprehensive orientation, preceptorship, constructive feedback, continuing education, and work-life balance support can help new graduates smoothly transition into their roles and foster their growth in the profession.
And, conversely, a new entrant to a group practice can also contribute significantly to support more experienced midwives in their group practice (Figure 2).
Creating a more sustainable midwifery practice, amid workforce shortages and increased stress, requires commitment but can be achieved by encouraging and executing a balanced, tailored mixture of the key components that suit you and your practice.
Over time, small but deliberate steps will help support and enhance ongoing sustainability, resilience and longevity in the midwifery profession. square
Supportive
Supportive
Induction of a Graduate (New) Midwife
How can a graduate or new midwife help the group practice
MMPO provides self employed community midwives with a supportive practice management system. www.mmpo.org.nz
mmpo@mmpo.org.nz I 03 377

2485
FIGURE 1. INDUCTION OF A GRADUATE MIDWIFE
ISSUE 110 SEPTEMBER 2023 | 15 YOUR MIDWIFERY BUSINESS Positive
Process
FIGURE 2. HOW A GRADUATE OR NEW MIDWIFE CAN HELP THE PRACTICE
Onboarding and Orientation
Access to Continuing Education
Midwifery Practice from more experienced midwives Regular and Constructive Feedback and Evaluation Open and Supportive Peer Connections
Work-Life Balance
Adapt Quickly Embrace Responsibilities Stay Updated and Share Knowledge Offer Tech Support Open Communications Maintain a Positive Attitude Resilience and Self-care
M i d w i fery F irst Year ofPracticeProgramme
important development: class action update
The work to prepare for the Class Action, which the College lodged in the High Court last year, is progressing well. The case will be heard in August 2024 and, although this may sound like a long time to wait, it is relatively quick timing for a case of this sort.
It’s been heartening to see so many midwives supporting the case, with over 1,300 originally signed in. Last month more members were given the chance to be added to the action. However, the litigation is now entering a new phase which requires considerable financial resources.

The Government is defending the case and there is every reason to believe it will continue to deny that it ever made any promises that LMCs should have fair and reasonable pay, and that it will launch a vigorous legal defence to try to deny midwives their rights. We want to give ourselves the best chance of success, and we can achieve this by mounting the strongest possible legal challenge. As a result, the case involves considerable money –potentially millions of dollars.
It is for this reason that the College’s National Board has decided to enter into an agreement with a third party disputes funder, Omni Bridgeway, who will provide funding for the legal, expert and other expenses associated with the case. The agreement we have made with Omni Bridgeway means that it will pay all of the costs (including any costs awarded against the College in the event that
the claim is unsuccessful). Omni Bridgeway is a reputable international company which has the confidence of our legal team.
The College’s Board has undertaken this step because it strongly believes that it provides significant advantages to the College and that it is in the best interests of the organisation and its members for the following reasons:
• The funding will enable us to mount the strongest possible case. We maximise our chances of success and also the likely amount of any settlement or funding awarded. Without the funding, the case would proceed but the funding the College could provide on its own is limited, and this may be reflected in the outcome. As well as ensuring that the College can access the best legal team and best experts, the Class Action funder has access to considerable legal and other expertise which will strengthen the case overall. It is in their interests for our case to be successful, and their involvement to date has already strengthened the case’s legal merits.
• By working with a funder, the College does not need to use its own financial reserves
to fund the case. As not all our members are signed into the action, it is therefore fairer for all of our members if independent funding is used to fund the costs of the case. We want to be completely transparent with midwives who have joined the Class Action about this change in circumstances. In return for providing the funding for the litigation and for taking the associated risks, Omni Bridgeway will be entitled to recover the litigation costs as well as a proportion of any monetary award or settlement achieved as a result of the case. The amount or proportion it will be entitled to depends on the length of time it takes for the case to be settled and the total amount awarded. Omni Bridgeway will fund the Class Action on a “no-win, no-fee” basis.
This means that if (as a result of the case) a midwife becomes entitled to monetary compensation, some of the compensation will be reduced for project/litigation costs paid, and for Omni Bridgeway’s return on its investment. We are advised by our lawyers that the percentage shares we have negotiated with Omni Bridgeway are more than reasonable in comparison with other funded cases.
16 | AOTEAROA NEW ZEALAND MIDWIFE FORUM
WHAT DOES THIS MEAN FOR MIDWIVES WHO ARE PARTICIPATING IN THE CLASS ACTION?
Midwives who have joined the Class Action signed a document – a Participation Notice which gave the College exclusive authority to enter into arrangements such as funding. However, as this is a new and significant development which may affect the final amount received by Participating Midwives, last month the College entered into a process to ensure midwives had the opportunity to have full information about the funding arrangement. Last month the College ran a series of webinars to enable questions about the arrangement. All of the information about the change in conditions, including a copy of the funding agreement, is available in the portal for members to view. We urge all midwives participating in the action to log into the members’ portal, consider the information in there and follow the instructions to indicate your support to the updated conditions in the Participation Notice.
It is vital that we get enough midwives taking this positive step – at least 75% of those who originally joined the Class Action – to ensure we have the funding that the Board believes is necessary for ensuring your and the College’s claim against the Government can proceed with the best possible chance of success.
This is an important case. We are taking it against the Ministry of Health in order to protect the legal rights which you were afforded in the various settlement agreements that we have had with the Government. This is not only about fair and reasonable pay. It is also about ensuring that midwives have the right to negotiate the conditions which are necessary to sustain you in the important work that you do. We are now almost one year in to our newly reformed health system and it’s fair to say that there is still no clarity about what future contracting models for community midwives will look like. As a small female-dominated profession, history has shown that we experience discrimination and that, as a result, we need to stand strongly and together to ensure our voices are heard and our rights are protected. Your participation in the action matters, so we urge you to log into the portal and indicate your ongoing support so that we can continue to receive funding and stand strongly together. square
If you have any questions, please email us at classaction@nzcom.org.nz
CELEBRATING JOYCE COWAN, ONZM – FIVE DECADES IN MIDWIFERY
Dr Joyce Cowan is a recognisable face to many in our profession due to her many roles over a long career. This year Joyce was recognised for her important contribution to the profession and to the health of women and babies with her award as an Officer of the New Zealand Order of Merit (ONZM). As Joyce hangs up her Pinnard stethoscope in retirement, she shares some thoughts about her five decades of midwifery practice.
After a few years of nursing, Joyce undertook her midwifery education at St Helen’s in Auckland and qualified as a midwife in 1972. For the next 17 years she worked at Middlemore as a staff midwife, taking short periods of maternity leave after birthing each of her four children.
Joyce recalls the inspiration she drew from Joan Donley as a home birth midwife and professional leader - when she heard Joan’s ‘Midwives or Moas?’ conference speech in the late 1980s calling midwives to action, Joyce took out her chequebook and signed up as a founding College member the same day.
Joyce was a trail-blazer in community midwifery, starting as a home birth midwife in 1989. She recalls the joy of continuity of care which was enabled by the 1990 Nurses Amendment Act: “Women were so powerful. The partnership model was something we loved and grasped. When the phone went I was so excited about going to the woman I knew - so different from my experience of working in hospital.” Joyce was deeply embedded in her community, working alongside women and childbirth educators to increase options for pregnancy and birth care.
Joyce is recognised as a leading midwifery expert in pre-eclampsia. She co-founded the charity, New Zealand Action on Preeclampsia (NZ APEC) in 1994, which raises awareness and provides education for health professionals about pre-eclampsia and supports whānau.

Joyce moved into education as an AUT midwifery lecturer in 2000 and carried on with a small practice for several years. She gained her Master's degree in 2006, researching women’s experiences of early-
onset pre-eclampsia, which provoked her interest in fetal growth restriction. Joyce established a postgraduate paper on fetal wellbeing and attended a fetal growth conference in 2013 in Baltimore which led to an invitation to undertake GAP educator training in Birmingham, UK. Joyce provided education on GROW for several years and became the GAP NZ Lead when ACC funded a national implementation rollout.
Joyce completed her DHSc in 2020, looking at the effect of implementation of the GAP in Counties Manukau on maternal and neonatal outcomes and has presented her research findings at several national and international conferences.
Considering her career, Joyce reflects, “It’s a huge journey isn’t it? I think it’s a real privilege to have been a midwife. It has given me a lot of joy. It has been challenging at times but I’m very grateful to my midwifery and obstetric colleagues.” Her advice to new midwives is to find balance with work and time for their own familiesit’s important that midwives look after their own wellbeing. This includes building close, reciprocal midwifery relationships.
Joyce is clear that nobody ever succeeds alone, and considers her ONZM as an award for midwifery. square
ISSUE 110 SEPTEMBER 2023 | 17 FORUM
DANI GIBBS – NGĀ MAIA NGĀ MAIA TRUST COLLEGE REPRESENTATIVE
Ngā Maia: honouring both ways of knowing

The International Confederation of Midwives Congress 2023, in the beautiful Nusa Dua, Bali, was exceptional. To be surrounded by passionate midwives, excited to share their matauraka was inspiring to say the very least; the joy in the room during the opening flag ceremony was palpable.

We set off on our haereka to Bali in the wee hours: four Ngā Maia Board of Trustees members and pēpi Kahurangi, all congregating at the gate in Auckland. Our plane was dominated by midwives, the 'off call going on a holiday' kind, the kind that make a plane run out of alcohol. We landed and parted ways with our gleeful colleagues only to reunite daily at the conference; everyone was always giddy with excitement to see each other.
The ICM delivered exceptional speakers; the plenary sessions had people on the edge of their seats most days. Birthing in humanitarian crises was a particularly confronting panel with representatives from the UN, WHO, Haiti and Ukraine discussing their experiences of being a midwife in unimaginable circumstances. Standing ovations were necessary.
Our neighbours in Australia spoke in multiple sessions about indigenising their health system to become culturally safe for the Aboriginal and Torres Strait people of Australia. It was inspiring and relatable to see so many similarities, and made me feel a strong sense of solidarity knowing that the same changes need to occur in order for our health system to be safe for Māori across Aotearoa. There was kōrero about the importance of ‘Birthing on Country’ with indigenous midwives and birth workers, rather than having to travel to distant locations that felt isolating and unfamiliar.
I reflected on the importance for Māori to be connected to our whenua and tupuna during our birth experiences and how birth is whakapapa; our pēpi are celestial taoka, gifted to us by our ancestors. I reflected on our current health statistics for Māori being disproportionally representative of poor health outcomes and it affirmed for me that the health reforms, co-governance restructures and emphasis on equitable healthcare are not just justifiable but absolutely essential. The impact that colonisation has had on our indigenous people, Māori, is no longer deniable and we have a responsibility as a profession to embrace indigenisation in order to see an equitable start to life for our precious taoka.
The Congress saved the best for last and the core reason for the Ngā Maia Board of Trustees members to travel to Bali: our College President Nicole Pihema’s presentation “A Māori perspective on mentoring in midwifery in Aotearoa New Zealand”. Nicole spoke with mana and did us so proud in the mentoring session, boldly delivering a kōrero about the current midwifery and maternity system that was not designed for us (Māori) to be successful in. Nicole gave enriching kōrero to our international colleagues about kaupapa Māori ways of being and challenged our New Zealand colleagues in leadership that, in order for us to achieve equity for takata whenua, a Māori model of mentoring, such as Tuakana Teina, needs to be widely integrated and realised. Kā mihi nui taku aroha ki te rakatira.
The 2023 ICM was an incredible opportunity and my learnings are extensive. I could go on for a long time! square
18 | AOTEAROA NEW ZEALAND MIDWIFE
NGĀ MAIA
TISH TAIHIA CLINICAL MIDWIFE MANAGER, NGĀ HAU

Pasifika: cultural keepsakes
The term Pasifika (Pasi-fi-ka) has become more widely used as we see the steady increase of peoples identifying their ethnicity (or part of it) as being from one of the myriads of isles spanning the South Pacific Ocean.
In the landscape of Aotearoa, it has also collectively come to describe those of a second generation born and raised and also those who are multi-ethnic. In the 2018 census Pacific Peoples reporting one ethnic group was 59.4%, a figure that is predicted to decrease with 2023’s census results.
Within growing numbers of Pasifika midwives and students over the past decade, putea from Te Ara o Hine - Tapu Ora has enabled us to explore activities that connect us not only professionally but with the ‘arts’ of our island origins, attempting to close the ‘Va’ (space) for our diaspora.
Pasifika Midwives Aotearoa - Tamaki Makaurau region, with the largest membership, participated in two workshops over the past year. Flagged as ‘Aunty-Niece’ team building activities, they gave rise for an opportunity to gather together and embrace collegial, creative and cultural sharing.
HIAPO PRINT – PATTERNS OF POLYNESIA (TUPUMAIAGA A NIUE TRUST)
Hiapo is the Niuean term given to the generic art of using bark cloth as the ‘canvas’ of each island’s identity. The print designs come from the beauty of nature and people, being rich motifs of environment and culture. However, for the hands-on workshop, lino prints designed by Trust artists were utilised on fabrics. As the morning unfolded it was clear that there was evidence of co-operation, communication and concentration occurring - key skills required in midwifery practice. The sense of achievement and pride at our finished works was so warmly positive, that you could forget that it was wet wintry and cold outside the Metro Theatre in Māngere East.
FALELALAGA VILLAGE (SAMOAN CULTURAL AND EDUCATION CENTRE)
The concept of the first workshop was familiar to many; however, in attending the Falelalaga Village fala pepe (baby mat) session, it was clear that this was a time to be spent as observers of the skilled art of weaving by Samoan master weavers.

We heard of the long process to grow the laufala and vulu (plants)harvesting, cutting, drying, washing and stripping. Then the weaving of the fala pepe that would be done amongst the women of the family
seated on the floor around the pregnant woman in the village fale (house). It was a time to give blessings and prayers to the wellbeing of the unborn child and the characteristics they hoped the child would have. The fala pepe was woven to withstand its many uses - sleeping, playing, nappy-changing.
For our day, the village setting was created by having us all close to the weavers on the floor watching the deft of their hands, donning an ‘ie lavalava’ (sarong) as is customary, smelling the coils of laufala, observing the most senior weaver stripping the long leaves as accurately as possible for consistency, hearing spoken Samoan and clapping to the impromptu song and dance of these supple elder women.
For us as guests, it was a therapeutic time of quietening the mind from work and study, to connect the body and soul. Midwifery takes us to those places when we ‘loiter around’ at homebirths and in the latent phases of labour in the still of the night in a birthing unit - it was indeed an experience of shifting mindset.
When we think of the development and retention of our workforce, we are forced to look at creative ways of sustaining the wellbeing of each other and our junior colleagues so that in the bigger scenario, solutions can be sought in care provision for our communities. square
PASIFIKA
MĀNGERE
O fanau a manu e fafga I fuga o la’au, o fanau a tagata e fafaga I upu (Samoan)
ISSUE 110 SEPTEMBER 2023 | 19
Birds feed their young seeds, while people nurture their young with words.

20 | AOTEAROA NEW ZEALAND MIDWIFE
AMELLIA KAPA REGISTERED MIDWIFE
MĀ WHERO, MĀ PANGO
The College’s first Māori Midwifery Advisors were welcomed to the team in July, with a mihi whakatau at the national office in Ōtautahi. Jaydeen (Jay) WaretiniBeaumont and Te Paea (Shannon) Bradshaw generously share with Amellia Kapa their midwifery journeys and aspirations for their new roles here.
Te Paea Bradshaw (Ngāti Kahungunu ki Wairarapa) was born and raised in Masterton and was inspired to become a midwife through her own experiences as a young māmā Māori.

“When I was pregnant with my first daughter, I was 20 years old and living in Wellington,” Te Paea begins. “I had a wonderful group of Māori and Pasifika midwives providing my care, and I had the best experience. Then we moved to Auckland and I struggled to find a Māori midwife for my second daughter. There was an overall shortage of midwives, let alone Māori midwives, so that prompted me to pursue a career in midwifery – to be able to provide care for women like myself.”
Jay Waretini-Beaumont (Ngāti Rangi, Ngāti Uenuku, Ngāti Apa) grew up in Ōtautahi and was also inspired by earlier interactions with midwives. “I was an only child until I was eight years old and then Mum got hapū. I didn’t want to be a big sister, but Mum’s midwife came into our whare with a
bag of tricks and let me be involved. I could hear Mum labouring from my bedroom, got to have the first cuddle, and the midwife really helped my mum carve out that big sister space for me. So that’s how I decided. I was also a young mum myself and had a straight-talking midwife who, after baby number two, told me to get on with the rest of my life and come back to having more babies later. She encouraged me to do my midwifery, so I enrolled.”
Te Paea completed her midwifery degree in Tāmaki Makaurau at AUT and started her new graduate programme at Middlemore Hospital, but transferred down to the Hawke's Bay part way through. “My kids were missing their cousins and due to start school,” she explains, “and we were thinking about where we’d buy a home. I whakapapa back to Wairarapa and my husband’s whakapapa traces back to Te Wairoa, so we thought Hastings would be a perfect place to settle and raise our kids – right in the middle of both of our whānau.”
ISSUE 110 SEPTEMBER 2023 | 21 FEATURE
Left: Te Paea Bradshaw (L), Jay Waretini-Beaumont (R).
Te Paea’s vision for her mahi, which will include a specific focus on reviewing and improving the MSR process, is clear.
“I perceive this role as bringing a Māori worldview into the systemic decisions the College makes, advising specifically within the MSR process."
“After my new grad year, I went out LMC with a group of Māori midwives here in the Hawke’s Bay,” Te Paea continues. “Our caseload was probably 95% Māori and I did that for a few years, until the Māori midwifery consultant role came up at the DHB – the first in the country. My colleagues pushed me into that job, which is how we roll. You don’t do things of your own accord –you do it because your whānau support it, or your tīpuna push you to do it.”
And while Te Paea – now a māmā of five children – was studying and launching her career in Te Ika-a-Māui, Jay was doing the same in Te Waipounamu, completing her degree at Ara and diving in to the mahi. “I graduated and then worked as an LMC for a couple of years before finishing up to have Mihi – the only baby I had as a midwife – which was a lovely healing homebirth,” Jay says.
After taking 18 months off to focus on being a māmā to her three daughters, Jay went back to LMC practice in a different model, caring for a shared caseload and alternating on-call responsibilities weekly. “Then on my weeks off I started providing locum support in Kaikōura to the only LMC there, which led to me creating a different model of continuity – between the remote-rural region the wāhine lived in and the urban location they’d need to come to if they required any secondary care. I’d work a week in Kaikōura, meet all the women, then come back to Christchurch and be here to receive them if they needed to come to hospital.”
Jay has a particular passion for supporting tauira Māori and Māori new graduate midwives, evidenced by the roles she has already taken on. “I picked up a casual contract at Christchurch Women’s Hospital to help out, and I’d time my shifts to line up with when Māori students were on, so they could shadow me. Then at the beginning of 2022, I started mahi as a Te Ara Ō Hine Māori Liaison at Ara.”
Having MFYP in her new portfolio at the College is therefore a perfect fit for Jay, who has also added chairperson of Māori Midwives ki Tahu and Ngā Māia board member to her impressive list of responsibilities in recent years. “Because MFYP focuses on sustaining tauira and new graduates, which in turn will fix the profession one day, it aligns beautifully with what I want to be doing.”
Equally well-equipped for the role, Te Paea worked
as acting midwifery director at Hawke’s Bay DHB for a year, before returning to the Māori midwifery consultant role. She has also worked as a Turanga Kaupapa facilitator, an MFYP mentor, been an active Ngā Māia member, completed Māori clinical leadership programme Ngā Manukura o Apōpō, and plans to start her Master’s this year.
After completing her Post-Graduate Diploma in Midwifery last year, Te Paea has had ample opportunity to identify where the systemic gaps are and what she can do to bring about change. “I believe I was chosen to be a midwife and I’ve been guided along my midwifery career by the world and my tīpuna, and this role came at just the right time. Last year in my post-grad studies I was looking at Māori health – critiquing the system – and then this role came up. People in my community told me to go for it and I thought you know, I can either continue to critique or I can actually come and help.”
Te Paea’s vision for her mahi, which will include a specific focus on reviewing and improving the MSR process, is clear. “I perceive this role as bringing a Māori worldview into the systemic decisions the College makes, advising specifically within the MSR process. I also see my role as advising the College in general on how we can make midwifery better for all midwives – making sure cultural safety isn’t just a tick-box exercise, but is meaningful for the benefit of the whānau we care for. If we can get that right, we’ll be able to make some real change in health outcomes for whānau Māori accessing midwifery services.”
Jay’s post-graduate study has also clearly shaped the way she perceives her new role. “My Master’s in Māori and Indigenous Leadership has prepared me for working my way up the ladder and being a creative cog of systemic change in our profession. My dissertation was on what sustains me as a Māori midwife, so I see my new role as an opportunity to work together with the College, to be more culturally responsive to the needs of its Māori members, and to make MFYP a safer place for the increased number of Māori and Pasifika midwives coming through, thanks to Te Ara Ō Hine. The other hats I wear –Māori Midwives ki Tahu and Ngā Maia – in combination with this new role, will work to increase whānaungatanga, which can only be a good thing, especially in actioning the recommendations of the cultural review.”
“From this position,” Jay continues, “I’m able to help guide the College to have conversations that better benefit Māori, not to mention being a Māori voice on the end of the phone for Māori members when they call in. The power of that can’t be underestimated.”
Both midwives and mothers, Jay and Te Paea also have a passion for revitalising te reo Māori, which will no doubt alter the oro (vibration) of the entire team and its mahi going forward. Te Paea sums up the dawning of this new era with a fitting whakatauki: “Mā whero, mā pango, ka oti te mahi” – by red and black together, it is done. Or in other words, when we each play our part, the entire collective serves to benefit and ultimately thrive. square
22 | AOTEAROA NEW ZEALAND MIDWIFE FEATURE
Ngā Maia Trust
Māori Midwives Ō Aotearoa
Hui Ā Tau 2023
Whiringa-ā-Nuku 25-27
Maungatapu Marae, Tauranga
Pre-registrations 9am, Pōwhiri 11am
Theme - Wairuatanga
REGISTRATIONS OPEN NOW FOR NGĀ MAIA MEMBERS
Date: 25 to 27 October 2023
Venue: Maungatapu Marare, Tauranga
Cost: Practising Midwife: $250
Non practising Midwife: $150
Tauira & whanau member: $100
Register at www.ngamaiatrust.org/news-and-updates
Upskill in midwifery
If you’re a registered midwife, our fully online postgraduate courses are perfect for you to study alongside your midwifery practice.
Sign-up for our upcoming courses in September:
• Applied anatomy and physiology for midwives
• Hypertension in pregnancy
• Global midwifery - practical steps
• Staying connected - digital technology in midwifery education.

op.ac.nz/midwifery
suzanne.miller@op.ac.nz
election'23: what are the main parties' midwifery policies?
The recent release of Te Whatu Ora and Te Aka Whai Ora Health Workforce Plan 2023/24 has provided an outline of some potential solutions to the current health workforce crisis; however, it is light on detail especially in relation to what we can expect for maternity. With a 40% shortfall in midwifery FTEs it is clear that opening borders and improving training opportunities is not going to be enough to ensure midwifery is a sustainable career into the future and that our pēpi have the best start in life.
We asked the five political parties currently in parliament what we can expect for midwifery if they are elected on 14 October. Te Pāti Māori hadn’t responded at time of going to press.
Q. What do you believe the role of midwifery is in achieving the aims of the health system reform?
Labour: The Labour Party values the significant role that midwives play in our health system. The care of a midwife can make a huge difference to the safety and quality of care for mothers and their whānau during pregnancy, birth, and the postnatal period.
The health system reforms ensure that midwifery care is provided on the basis of need for all New Zealanders, no matter who they are, their ethnicity, or whether they’re urban or rural. These reforms are working to end the postcode lottery - meaning that the healthcare you received depended on where you lived.

National: Midwifery has always had a very important role to play in a health system providing guidance and skills to patients at the maternal care interface. However, the health reforms are a failed model in centralisation and “government knows best” that has done no
favours to midwifery. This is the consequence of when major structural reforms are undertaken in the middle of a pandemic.
ACT: ACT acknowledges that midwives play a crucial role in providing quality care and support for women and their families prior to, during, and after childbirth, reducing pressure on our hospitals, and ensuring a healthy start for the next generation.
Green: Midwifery, when properly prioritised, funded, and supported with facilities, can act as a role model for the broader aims of Te Whatu Ora and Te Aka Whai Ora.


The goal of the system transformation is to achieve a more equitable, accessible, cohesive, and people-centred health system, by weaving together all health services to ensure continuity of services and of care. Midwives have always embodied and practiced this continuity of care model, and therefore serve as an exemplary model of that vision for the broader health system.

Labour Hon Dr Ayesha Verrall ACT Brooke van Velden Green Jan Logie 24 | AOTEAROA NEW ZEALAND MIDWIFE FEATURE National Dr Shane Reti

FEATURE
Q. What do you consider are the top three challenges facing the profession at the moment?
Labour: New Zealand’s midwives are committed to the wellbeing of women and whānau, but they’re facing significant challenges. A shrinking workforce despite increasing demand for midwifery services and expertise has put enormous pressure on midwives across the country. Decades of underfunding of primary maternity services and hospital facilities has placed a massive strain on staff. We know that Māori and Pasifika midwives are under-represented. It’s important that our midwifery workforce reflects the diversity of the mothers, babies and whānau they care for.
National: Workforce is one of the key issues facing the health sector, with the Government releasing information that New Zealand is currently short 1,050 midwives. We acknowledge that wages, salary and terms and conditions are also challenges facing the sector.

ACT: ACT acknowledges that New Zealand is in a health workforce crisis. ACT identified that, in 2022 alone, 421 midwives chose not to renew their practising certificates.
Tight immigration settings, better working conditions overseas, and a health system in crisis are all challenges which have impacted upon the attractiveness of the midwifery profession in New Zealand.
Green: The ongoing pay equity process must finally be fully settled, ensuring that midwives are paid what they deserve. The funding model for midwifery services creates unfair financial pressures. The present acute shortage of midwives, particularly of kaupapa Māori and Pacific services, is one of the worst in our entire health workforce.
Q. What is your strategy for supporting the midwifery workforce to overcome these challenges?
Labour: Growing and supporting the workforce is a key priority for us. We acknowledge that there are shortages in our midwifery workforce, and we are committed to training more midwives to address that. Our recently announced Workforce plan will tackle longstanding health workforce issues. We’ve given registered midwives an immediate pathway to residence and funded the Return to Practice programme allowing a path back for midwives. We want to ensure
the midwifery workforce is representative of the populations it serves, which is why the Te Ara ō Hine programme and discretionary hardship fund for students aim to retain more Māori and Pasifika midwives.
National: National will pay nurses’ and midwives’ student loan repayments up to $4,500 a year for the first five years of their career. A nurse or midwife would be $22,500 better off and increases take-home pay by $87 a week. To access the scheme, they will need to enter into a five year bonding agreement after they graduate.
National will also allow qualified overseas nurses and midwives to come here on a sixmonth temporary visa to look for work and to bring their immediate family with them. We will also offer relocation grants worth up to $10,000 to support their move.
ACT: ACT will repeal the Accredited Employer Work Visa Scheme and replace it with a simple open work visa scheme. This will ensure that qualified midwives overseas have a simplified and clear pathway for entry into both New Zealand and our health workforce, providing they meet professional standards.
Green: The Green Party will finalise and resource the Women’s Health Strategy,
26 | AOTEAROA NEW ZEALAND MIDWIFE FEATURE
including implementing a fair funding model for midwives that prioritises high quality care and increases social services during pregnancy and following childbirth. We will increase entrants into health professions, the retention of practitioners in the workforce, and placements for on-the-job learning. While a Green MP was Minister for Women, primary maternity services received their largest ever funding boost, targeted to recognise the work midwives do caring for pregnant people who live rurally, and those with high-needs pregnancies. We will continue to deliver for midwives who work incredibly hard to care for pregnant people and their babies in Aotearoa.
Q. Employed midwives are currently going through a pay equity process led by MERAS, the midwives’ union. How would your party ensure that this is successfully concluded?
Labour: A wage increase ratified in July gave more than 1,150 midwives employed by Te Whatu Ora a 15% pay boost and a lump sum payment of at least $3,000. The hardworking and predominantly female midwives of Te Whatu Ora are another step closer to getting the pay they deserve. This agreement means the wages of our largest group of midwives have increased by about 45% since 2017. Graduate midwives in public hospitals will start work on almost $73,000 per year before overtime and allowances, while experienced midwives will be on a base rate of almost $97,000 before overtime and allowances.
National: National can proudly stand on our history of pay equity - it was a National Government that concluded the very first pay equity, Terra Nova, home care and support workers settlement. The specifics of current negotiations are only available to the Government and the opposition is not privy to that information.
ACT: Any pay equity process negotiations are ultimately a matter between Te Whatu Ora and MERAS.
Green: The Green Party values the critical work that midwives do, and recognises that they, along with other health and care workers, have long been underpaid, overworked, and undervalued. We have been very active in pay equity campaigns and see this work as essential to addressing discrimination and properly valuing caring work. To reflect this, we will meet union demands for fair wages, pay parity, a
reasonable workload, and conditions that support the wellbeing of health workers and the quality of care of their patients. A strong health system depends on the wellbeing of its healthcare workers: the Green Party will ensure that the workforce is properly valued and supported to stay in the job, including Māori who provide essential care for whānau, hapū and iwi.
Q. How do you see pay equity principles applying to self-employed community midwives (lead maternity carers/LMCs)?
Labour: We want kids to have the best possible start in life. In July, we launched the Kahu Taurima programme for maternity and early years. To improve access to Neonatal Retinal Screening for premature babies, and to protect young eyes, we are purchasing 20 new paediatric retinal cameras. This investment means at least one portable retinal camera will be available in every tertiary hospital in New Zealand. Budget 2020 provided the largest funding boost to primary maternity services, including payment for a broader range of services.
National: Pay equity in the public sector often sets remuneration levels that other similar roles in the private sector seek alignment with. This discussion is similar to GP practice nurses where the public sector achieves pay equity and private then seeks pay parity.
ACT: How pay equity principles are applied to self-employed community midwives (lead maternity carers/LMCs) is ultimately a matter for self-employed community midwives and funding providers, such as Te Whatu Ora.
Green: The Green Party will implement stronger protections for self-employed midwives. We will ensure they can be covered by Fair Pay Agreements and join other industry-specific collective bargaining. While the interim agreement reached by Te Whatu Ora and the midwives it employs is an important start, self-employed midwives - who are also publicly funded by Te Whatu Ora - are unable to take industrial action. Pay equity is about ensuring that people who do such important work for our communities are paid what they deserve - and that must be extended to self-employed midwives.
Q. What will midwifery look like in 2026 under your government?
Labour: The Chris Hipkins Government will continue to strengthen the midwifery
workforce. By 2026, we want to see an increase in the number of midwives in New Zealand. This will ease pressure on the existing workforce and ensure that whānau have access to quality medical care throughout the pregnancy and birthing journey.
Labour wants to see midwives paid a sustainable, equitable income. We believe that the pay our midwifery workforce receive should reflect the enormous contribution that midwives make to our whānau and communities. A Labour Government will continue to support midwives and the important work that they do.
National: In 2026 there will be more midwives and midwifery students in New Zealand who have been supported and bonded through National’s plan, or have arrived in the country through our plan to make it a more attractive destination for migrant midwives. This will help ease some pressures on the health sector and help deliver better services for expecting parents.
ACT: ACT is developing its health policies, and these will be released closer to the election.
Green: Our vision is for pregnant people (and, when appropriate, their whānau) to be able to easily access a midwife who is a good cultural fit for them; that all midwives are supported to provide the best possible care, backed up by strong community/health services where needed; that whānau are in warm, dry homes with adequate incomes.
We envision a diverse, sufficient, resilient, and collaborative workforce, in which all midwives earn what they deserve and enough to live a good life; a fair funding model has been implemented, and better work conditions and pay keep existing midwives in practice and encourage new midwives to the profession; workforce pathways for Māori and Pasifika have been strengthened, and midwives trained overseas have a clear pathway to residency and to practising in Aotearoa. square
Saturday, 14 October 2023
ISSUE 110 SEPTEMBER 2023 | 27 FEATURE
The New Zealand general election will be held on
CAROL BARTLE POLICY ANALYST

climate change issues: food systems, ultra-processed foods, plastic waste and 'green feeding’
It is becoming increasingly clear that not only is our current food system a significant contributor to chronic disease, it is also a driver of climate change, which in turn is affecting food security. As Ora Taiao, NZ Climate and Health Council, stated in a 2019 submission to the Ministry of Health about healthy food and drink: "Healthy eating, including increased intake of plant-based foods and less consumption of red meat and animal fat (particularly highly processed animal products), would both help reduce greenhouse gas emissions and lead to significant improvements in health.”
There are numerous issues to consider, including food waste, different dietary choices, the proliferation of unhealthy ultra-processed foods, equity in terms of affordability and access to good nutritious food, and taking care of fertile land to ensure it remains healthy and able to sustain the nutritional needs of the
Ultra-processed foods, which are ready-to-eat, cheap and accessible products with little to no whole foods, with added sugar, salt, fats, additives and preservatives, have been engineered to be addictive and to encourage over-consumption.
population. Transformation means changing practices to support land regeneration and to support sustainability. Environmental systems and processes have been pushed beyond safe boundaries by industrial food production, and there have been calls for a global transformation of our food systems (Willett et al., 2019). Jones (2019) has described how the climate crisis will affect the health of indigenous peoples due to a range of factors already recognised, which include relationships with the natural environment, socioeconomic deprivation, issues with access to quality health care and political marginalisation.
The Intergovernmental Panel on Climate Change (IPCC) reports that climate change is affecting food security through increasing temperatures, changing precipitation patterns and greater frequency of some extreme events (Mbow et al., 2019), while at the same time our industrial food
systems are causing greenhouse gas emissions from land use, food storage, transport, packaging and processing. Transforming the global food system is one of the ways to address climate threats, alongside addressing issues of health, wellbeing and equity.
ULTRA-PROCESSED FOODS, PLASTICS AND THE CLIMATE
Ultra-processed foods, which are ready-toeat, cheap and accessible products with little to no whole foods, with added sugar, salt, fats, additives and preservatives, have been engineered to be addictive and to encourage over-consumption. There is a need to shift the blame for their consumption and negative health effects away from individuals and populations, on to aggressive marketing and corporations (van Tulleken, 2023). Conflicts of interest relationships between politicians, doctors and industry also hamper
28 | AOTEAROA NEW ZEALAND MIDWIFE CLIMATE CHANGE

ISSUE 110 SEPTEMBER 2023 | 29 CLIMATE CHANGE
positive progress, and government inaction on food affordability continues to disappoint. The food industry playbook of strategies and tactics which cast doubt on unfavourable research and lobby against public health recommendations includes commercial milk formula marketing as well as the promotion of other ultra-processed foods (Nestle, 2023).
The current food system which is driven by demands for cheaper ultra-processed food is not only unsustainable but it is a driver of carbon emissions and environmental damage (van Tulleken, 2023). Ultra-processed food also damages the environment through the production and use of plastic and packaging. The theme for World Environment Day on 5 June 2023 focused on solutions to plastic pollution (https://www. worldenvironmentday.global). More than 400 million tonnes of plastic are produced every year, half of which is designed to be used only once. Coca-Cola, PepsiCo and Nestle were the top plastic polluters for the third year in a row in 2020 (van Tulleken, 2023). These companies, plus Unilever, sell single-use plastic bottles, sachets and packets in non-Western countries, despite the industry awareness that waste is not able to be managed efficiently in these countries and it becomes pollution (Tearfund Report, 2020). The New Zealand Government has been making some slow efforts to reduce single use plastics, and from 1 July 2023 some items have now been banned, such as plastic drinking straws (with exceptions for people with disabilities), single-use plastic produce bags and non-compostable plastic produce labels.
Medical plastic waste is a difficult issue, complicated by concerns about infection prevention and control. Cleaning up plastics in healthcare waste is a hot topic of discussion, with suggestions that health professionals should strive for alternatives
as part of their mission to improve health (Rasheed & Walraven, 2023). Action by health professionals is viewed as a potential strategy to send market signals to industry to encourage the production of environmentally friendly products for healthcare usage. It is inspiring to note that a ‘Green Maternity Intervention’ in Victoria, Australia, led by midwives at Western Health’s Joan Kirner Women’s and Children’s Hospital, resulted in a 71% decrease in clinical waste and a 48% reduction in waste management costs. The intervention involved a range of initiatives, including midwife sustainability champions, staff education, information posters, monthly newsletters and incentives to promote engagement with the intervention (https:// www.deakin.edu.au/research/research-newsand-publications/articles/midwives-go-green).
A related issue which is not often considered is the cost incurred from the many unnecessary tests and procedures that occur in our health system. The Choosing Wisely campaign has drawn attention to the medical tests, treatments and procedures that provide little or no benefit, and which could also cause patient harm, but the issue of the generation of more healthcare waste has not been addressed as part of this initiative.
PREGNANCY: NUTRITION AND FOOD INSECURITY
In terms of ultra-processed foods in Aotearoa, a report from the University of Auckland found that 69% of the 13,000+ packaged foods they surveyed were categorised as ultraprocessed. This included snack foods, bread products, meat alternatives, and sauces and dressings (Mackay et al, 2019). A NZ study looking at ultra-processed food intake in children aged 12, 24 and 60 months found that these foods contributed 45%, 42% and 51% respectively to children’s diets (Fangupo et al., 2020).
When connecting the topic of food systems to issues that concern the work of midwives, a key consideration is the health of women during pregnancy. Socioeconomic status can impact maternal and newborn health and wellbeing. Midwives understand the importance of healthy eating in pregnancy, and the challenges of poverty and access to nutritious foods, as opposed to unhealthy, inexpensive and convenient fast ultraprocessed foods. Ultra-processed foods contribute to the overall population health burden, and there is a link to climate change and environmental degradation. Poverty, near-poverty and hardship around the time
of pregnancy was explored in a large study of women included in the postpartum survey data from California’s Maternal and Infant Health Assessment (n=18,332) and from the CDC Pregnancy Risk Assessment Monitoring System (n=143,452) (Braveman et al., 2010). The researchers extrapolated their findings to the US overall, and suggested that approximately 800,000 pregnant women annually in the US are likely to experience food insecurity. The Best Start Ontario resource manual interviewed women who lived in poverty during their pregnancies, and provided feedback from these women participants on a range of topics (Best Start, undated). The main issues of concern reported by these women were a lack of access to healthy food and to the recommended prenatal vitamins. Food security was considered to be the number one barrier that interfered with a healthy pregnancy by many low-income women. A comment from one of the women participants made it clear that the barriers she experienced were not related to a lack of awareness or education:
“Don’t lecture me about do’s and don’ts. I already know them. If I could do them I would. If I’m not, there’s a reason. Usually I try, but when there’s no money, there’s no money.”
Diets contribute significantly to critical issues such as greenhouse gas emissions and water consumption, as well as their health impacts; and, while changing dietary patterns could have many positive environmental impacts, these benefits will be hampered due to barriers to healthy carbon-light food affordability and accessibility. Sustainable solutions will need to be underpinned by an equity lens. Promoting a shift to sustainable, nutritious food production and consumption, without supporting and protecting population access to this food, is unethical and not the answer. It is also unethical to promote breastfeeding without providing support for women who wish to breastfeed and protection of their rights to breastfeed.
A recent review of reports, plans and strategies in Aotearoa (Kore Hiakai, Zero Hunger Collective, 2023) concludes that food insecurity is an entrenched problem in Aotearoa and that realising food security and sustainable food systems are priority actions. Agency, stability, long term sustainability, access, availability and utilisation are highlighted as dimensions of food security. It is unfortunate that organisations who are
30 | AOTEAROA NEW ZEALAND MIDWIFE CLIMATE CHANGE
When connecting the topic of food systems to issues that concern the work of midwives, a key consideration is the health of women during pregnancy. Socioeconomic status can impact maternal and newborn health and wellbeing.
involved in advocacy for healthy food, food security and climate action consistently fail to factor infant feeding into their discussions and documents. Breastfeeding provides food security for infants while supporting optimal nutrition and immune protection, and the significance of its inclusion in discussion about food security and sustainability should be recognised.
BREASTFEEDING | INFANT AND YOUNG CHILD FEEDING: GREEN FEEDING
How the world’s infants and young children are fed is of significance to our collective wellbeing, and the sheer volume of milk formula powder, the lack of protection of breastfeeding and the damage inflicted on the environment are interrelated issues which are often not acknowledged or addressed. This is not about formula not having a role when needed, but rather a concern about the rapid expansion of formula milk production, inappropriate marketing and inadequate policies and legislation to support women who wish to breastfeed. Women’s contributions to food production and food security are often overlooked (Smith et al., 2023) and the focus of Green Feeding is on the need for Government action to improve their policies and programmes to protect, promote and support breastfeeding women, and to regulate the marketing of commercial milk formula.
Green Feeding is an initiative which is described as climate action from birth. It encompasses optimal breastfeeding and complementary feeding practices for infants and young children aged from 0-36 months (IBFAN, GIFA, WBTi, 2019). This initiative aims to raise awareness of the links between infant and young child feeding to the climate emergency to bring about transformative change. A recently launched user-friendly Green Feeding Tool has been designed to calculate the carbon and water footprints of commercial milk formula (CMF) to help illustrate the carbon offset that could be achieved by increasing breastfeeding and reducing commercial milk formula use (Smith, 2023). The Green Feeding Tool is designed to provide countrylevel estimates of greenhouse gas emissions from CMF to help bring the importance of breastfeeding and achieving global breastfeeding targets to the attention of governments, environmentalists and climate change scientists. Priority actions, including investment in breastfeeding, are outlined

in the Green Feeding document and the protection of bottle-fed babies is described as a priority due to the large percentage of babies who consume powdered formula reconstituted with water that is likely to become increasingly contaminated (IBFAN, GIFA, WBTi, 2019).
CONCLUSION – TRANSITION AND TRANSFORMATION
Our industrial food systems are fragile and will continue to be threatened by climate change and unpredictable weather events. The economist E. F. Schumacher (1974) suggests, in his study of economics, “As if People Mattered,” that “nothing makes economic sense unless its continuance for a long time can be projected without running into absurdities.” Reducing the use of plastics, the transport, packaging and processing of food and the mismanagement of land will support healthy people and a healthy planet. Agroecology is a set of practices that integrates ecological principles into agriculture. It starts with reducing toxic techniques like chemical fertilisers and pesticides, and using alternative practices like crop rotation, compost and cover crops (Bittman, 2022). According to Bittman, the next stage involves shortening the food supply chain and reducing the distance between growers and eaters, and making our food systems sustainable and equitable for everyone. It is also timely to consider that breastfeeding represents the shortest food mile and that, “a woman can
produce hundreds of litres of the super-fluid breastmilk for a zero-carbon footprint” (Palmer, 2009).
Catherine Knight writes about a transition to an “economy of enough” rather than the constant striving for more economic growth (Knight, 2023). Moving towards a sustainable – and survivable – future, and avoiding catastrophic ecological and climate breakdown by making sufficiency a central guiding principal of our economy, while living within the biophysical limits of our country and the planet, is proposed. As Knight says:
“Key to making progress towards the transitions we need for a more survivable future will be the building of bridges. Not ones made of concrete and steel, but ones of ideas.”
The IPCC Synthesis Report recognises the interdependence of climate, ecosystems, biodiversity and human societies, as well as diverse forms of knowledge (2023). The report notes that sustainable and healthy diets promote all dimensions of individual and population health and well-being. Recognising the importance of accessible, affordable, culturally acceptable, safe and equitable food systems which are community-led, and which recognise food sovereignty and the essential contribution of women, is a positive step forward. square
References available on request: communications@nzcom.org.nz
ISSUE 110 SEPTEMBER 2023 | 31 CLIMATE CHANGE
CAROL BARTLE POLICY ANALYST


ANKYLOGLOSSIA –TONGUE TIE: ADDRESSING THE ISSUES FOR MIDWIFERY AND BREASTFEEDING
Ankyloglossia is a congenital condition in which the lingual frenulum (the tissue that attaches the tongue to the floor of the mouth) is thickened, tightened and/or shortened, which may restrict or impact on newborn tongue mobility. As described by Mills et al. (2019), this is not a band, or a cord, but rather layers of tissue which form a diaphragm-like structure.
The topic of ankyloglossia has been a topic of some intense debate and disagreement for a number of years in both health and parent forums. These issues have not bypassed midwives of course. The conflicts caused by different approaches to evaluation, diagnosis, treatment and opinion have resulted in variances in management, and at times passionate discussion within midwifery practice and in dialogue with other health professionals. This article aims to look at clinical practice through a midwifery lens, while also attempting to address some of the ongoing ethical concerns.
Due to concerns about over-diagnosis, and the unnecessary treatment or overtreatment of tongue ties, guidance was developed by the Ministry of Health to provide clear and consistent guidance to the health sector to support identification, assessment, diagnosis and treatment (2020).
IS IT A TONGUE TIE?
Babies have many complex suck swallow breathe sequences to manage when they are initiating suckling. It “requires the function of six cranial nerves, six cervical nerves and a few thoracic nerves coordinating 31 muscles in the lips, cheeks, tongue, jaw, chin and
soft palate” (Smythe, 2015). Some in-utero influences, or birth events, may temporarily alter the jaw or oral cavity (including the tongue) shape, structure, or function, e.g., the fetal position in utero, birth interventions such as ventouse or forceps, and uterine influences such as fibroids and bicornate uterus. Waitematā DHB’s management and treatment of tongue tie document describes the potential relationship between difficult births and tongue restriction:
“The tongue it is a very vascular organ covered with mucosa. All body structures are held together by fascia tissue. There are theories that ‘over tight fascia’ may cause tongue tie. This can be seen in neonates following difficult births when head, jaw and neck tension may be felt and as the skull moulding and tension settles, the tongue restriction usually settles too. Heat and massage may be of value during this period” (Waitematā DHB Management and Treatment of Tongue Tie (ankyloglossia): Credentialing education for midwives). Some parents may be able to afford alternative therapies such as infant craniosacral work to support recovery from a difficult birth but, for many parents, this is not an option. An alternative initiative such
as skin-to-skin contact can encourage the baby to turn their head to each side. Skin-to-skin with the mother is preferable as this will also support milk supply and practice for latching, but skin-to-skin with a significant other is also of benefit. Deep baths where the baby can move about freely, and mirimiri (gentle massage) may help. Supporting the ‘tincture of time’ is also important.
These birth-related factors usually have a short-term influence, and breastfeeding and lactation support will be required until the baby can feed effectively. Growth patterns in utero may have an effect, as growth restricted babies often have limited cheek fat pads which may make maintaining a vacuum during breastfeeding more challenging. Once the baby has gained some weight, the feeding often improves on its own.
BREASTFEEDING AND TONGUE TIE
Common challenges that may occur when a baby has a tongue tie include problems with latching at the breast and retention of the latch, and painful feeding. There may also be poor milk transfer which can lead to subsequent poor weight gain and decreased milk supply, long breastfeeds with baby not behaving satisfied after a feed, or frequent short and inefficient feeds. Early difficult feeding experiences can lead to maternal and infant frustration and distress.
ASSESSMENT
Breastfeeding is an interaction between the mother and her baby, and there are many factors other than tongue-tie that need to be considered when managing breastfeeding difficulties. Midwives have the skills to assess and support breastfeeding, to assist with improvement of latch, positioning and milk supply issues, and to provide evidence-based information to parents.
Reviewing birth events is part of an assessment. Has there been some restricted growth issues, is the chin more receding than we expect to see in a newborn, does the face look asymmetrical, what is the baby’s muscle tone like, are all questions that can provide
32 | AOTEAROA NEW ZEALAND MIDWIFE BREASTFEEDING CONNECTION
KAREN PALMER MIDWIFE AND LACTATION CONSULTANT
some key insights into the evaluation/ assessment. When assessing a breastfeed, the latch and how the baby ‘holds’ the latch are important to note, as is the observation of nipple appearance when the nipple is released. Asking questions about pain during feeds, listening for any unusual noises made when the baby is suckling, and checking milk transfer for the full duration of the breastfeed – is it sustained for most of the feed or only when the milk is flowing – the answers add more information to the holistic observation.
Anatomy also needs to feature in the assessment as breasts and nipples come in all shapes and sizes and adjustments to latch and position may need to be made to ensure the ‘fit’ between mother and baby is as optimal as possible.
It is within the scope of practice of a midwife to identify and assess for tongue tie using an accredited tool, to provide information to parents and to treat or refer accordingly, using an informed consent model of care. Identification of a tongue tie which is causing feeding problems can be made by a midwife during a breastfeeding observation.
The assessment can be made using an evidence-based tool such as the Bristol Tongue Tie Assessment (BTAT; Ingram et al., 2015), Tongue Tie and Breastfed Babies (TABBY; Ingram et al., 2019), or the Hazelbaker Assessment Tool (Amir et al., 2006).
The TABBY Tool gives a good visual assessment guide that can be used confidently with parents.
Common challenges that may occur when baby has a tongue tie include problems with latching at the breast and retention of the latch, painful feeding usually resulting in some nipple damage, poor milk transfer which can lead to subsequent poor weight gain and decreased milk supply, long breastfeeds with baby not behaving satisfied after a feed, or frequent short and inefficient feeds.

ISSUE 110 SEPTEMBER 2023 | 33 BREASTFEEDING CONNECTION
TREATMENT – BREASTFEEDING SUPPORT
Skilled breastfeeding support and management takes precedence over surgical intervention, and this has been recommended as the first line of intervention – this includes clinical assessment, modifying the latch and the position of the baby, assessing the baby’s milk intake, treating sore or damaged nipples, and protecting lactation where necessary (Ministry of Health, 2020; Lefort et al., 2021; Watson-Genna et al., 2017). A baby with ankyloglossia may benefit from a style of feeding that supports instinctive behaviours and feeding cues (Brimdyr et al., 2020; Colson, 2005; Wang et al., 2021; Widström et al., 2020).
Positional instability can cause a baby to back arch, cry and fuss at the breast, and/ or refuse to breastfeed. Positional instability is when the baby signals either subtle or significant discomfort, and experiences challenges with motoric postural control. This usually occurs when the baby is desperate to feed and too distressed to stay in an optimal position (Douglas, 2016). There are modified cradle, laid back and side lying positions that can be utilised to support babies who are having difficulties with latching.
A baby needs to be well supported to adopt an instinctive posture to latch and feed well, be mostly prone and facing the mother’s body, with the head free to move. The baby’s head will instinctively tilt backwards to latch if there is no obstruction behind the head. The baby’s body needs to be in contact with the mother – knees, chest and chin – these are touch points that assist the baby to find the breast.
There is limited data on the incidence, treatment and follow-up outcomes of babies with tongue tie in Aotearoa New Zealand, despite ongoing concerns about over-diagnosis and treatment in some regions. The collection of collated national data identifying the short and long-term outcomes for babies who have had frenotomies is essential.
Working with an individual woman’s breast size and shape is important. Women with small breasts find an oblique position helpful, whereas larger breasted women may benefit from an across or underarm position. In some situations where there is anterior breast fullness, an inverted side lying position may be necessary for a few feeds until the breasts soften and the baby achieves some feeding success.
CONSERVATIVE MANAGEMENT
Ongoing support when breastfeeding is not effective or is painful may include appropriate use of nipple shields and/or pumping in some situations. An individual care plan developed with the mother is important to ensure a good outcome with the mother feeling supported in her choices. Different women will have different levels of self-efficacy with overcoming breastfeeding difficulties.
TREATMENT – FRENOTOMY
There will be documentation as to whether the baby has had intramuscular or oral Vitamin K administered at birth. Frenotomy needs to be delayed by at least 12 hours after the baby has received intramuscular Vitamin K, or 24 hours after the baby has received the first oral dose of Vitamin K. If the parents choose for their baby not to receive Vitamin K, continued breastfeeding support is advised instead of frenotomy (MOH, 2020).
Performing a limited simple lingual frenotomy using an approved assessment tool, and technique, is within the scope of midwives who have completed specific training, while babies with complex tongue ties or babies with any medical or relevant physical conditions require referral to a specialist. Posterior tie, upper lip ties, buccal ties, lower lip ties and after-treatment stretches have limited or no evidence to support treatment (Mills et al., 2019; NZ Dental Association, 2018; Shah et al., 2020). A frenotomy needs to be done in a clinical setting where two practitioners are present, and a process in place in case of unexpected bleeding.
ETHICAL DILEMMAS
Midwives have an obligation to provide evidence-based information and care for women, and to respect women’s rights to make uncoerced and informed decisions about their care and the care of their newborn babies (Midwifery Council –Code of Midwifery Professional Conduct).
Sometimes conversations about breastfeeding difficulties are complicated by parental expectations and their frustration about the inability to immediately find a quick ‘fix’ for feeding difficulties. Parents are influenced by what they read and see on social media, and it is difficult for them to separate out popular rhetoric from evidence-based information. It can be complex when dealing with situations where parents have been advised by another health professional that a tongue tie is present.
Dealing with these situations requires professional discretion. Many normal baby behaviours and scenarios have been attributed to tongue tie without good evidence – for example, wind, reflux, and spilling feeds – and this further complicates the conversations with parents. It is also hard to disagree with parents who are convinced there is a tongue tie, even when a midwife has assessed the baby and the breastfeeds, and found the issue is unlikely to be a tongue tie. Midwifery care is women-centred and relationship-based and when mother and baby dyads experience breastfeeding issues, consideration of how best to provide support can be a complicated clinical challenge at times. The surgical release of a tongue tie is only one of the treatment and support options available.
To address the rising rates of tongue tie diagnosis in Canterbury, local healthcare professionals were brought together in a working group. They reached consensus on a pathway for improving the management of infants with tongue tie and breastfeeding difficulties. This embedded an expert breastfeeding review and assessment of lingual function using a validated method, the Bristol Tongue Tie Assessment Tool (BTAT; Dixon et al., 2018). Frenotomy intervention rates were reported as reducing markedly from 11.3% in 2015 to 3.5% by mid-2017. Feeding methods were not different before or after surgery between infants who received a frenotomy and those who did not. The new clinical pathway was introduced based on best available evidence and multidisciplinary expert consensus, with the aim of ensuring that all possible causes for breastfeeding difficulties were considered early, and that tongue function and anatomy were assessed consistently and objectively. A key aspect of this initiative is full breastfeeding observation and the use of a validated tool for assessment. Unfortunately, numbers of babies who may
34 | AOTEAROA NEW ZEALAND MIDWIFE BREASTFEEDING CONNECTION
have been taken out of Canterbury by their parents for treatment are not possible to ascertain.
CONCLUSION
There has been limited data on the incidence, treatment and follow-up outcomes of babies with tongue tie in Aotearoa New Zealand, despite ongoing concerns about overdiagnosis and treatment in some regions. The collection of collated national data identifying the short and long-term outcomes for babies who have had frenotomies is essential. For midwives to feel comfortable with assessing a tongue tie, the use of a validated tool can support assessment before a management plan is developed, or referral for possible treatment is made. With the continuity of care model, the midwife has a breadth of knowledge about both the mother and baby to be able to provide a holistic assessment. Breastfeeding difficulties are common in the postnatal period and they are often multifactorial. They can be a challenge for midwifery practice as they require time, observation, knowledge and experience. Referral options will vary from region to region and there may be a free and accessible lactation consultant service to refer to in some centres when required, but this is not always the case. Judicial use of frenotomy is
important (when appropriate) but frenotomy without a firm diagnosis is an unnecessary intervention. Full informed choice and consent by parents is paramount.
There are health risks associated with not breastfeeding, and not being breastfed, and the very large majority of women in Aotearoa intend to breastfeed. Undiagnosed, incorrectly diagnosed and unmanaged breastfeeding problems, and the resultant weaning, can cause a grief response and put new mothers at increased risk of postnatal depression. If breastfeeding difficulties are assessed as being due to a tongue tie, a thorough assessment, treatment and/or timely referral for treatment are essential.

The development of a pathway and free services for assessment, referral and treatment is necessary for all regions of Aotearoa New Zealand. The College continues to support the provision of a free, equitable, accessible and timely service for the release of neonatal tongue tie if it is impacting negatively on breastfeeding, while also agreeing that frenotomy is not always necessary even when a tongue tie is diagnosed. square
References available on request: communications@nzcom.org.nz
Key Points
Degrees of ankyloglossia vary and, while most infants breastfeed successfully, there may be challenges for a small percentage of infants.
No accurate figures about tongue tie incidence are available - closest estimate is that 5% will require treatment.
There is a wide range of normal infant oral anatomy.
Uterine conditions and birth events can temporarily alter oral anatomy and abilities.
Not every breastfeeding difficulty is due to tongue tie and not every tongue tie causes a breastfeeding issue.
Position and latching - the ability to improve latch by careful positioning is significant.
Breastfeeding support needs to be offered if frenotomy is not chosen or not available.
Post-frenotomy breastfeeding assessment is necessary.
ISSUE 110 SEPTEMBER 2023 | 35
The S position - the ears, shoulders and hips are in alignment and the body forms an S curve to achieve a good feed.
Comfort and safety for babies newborn-2 years
More restful, safer sleep and helps prevent flat head
• More restful, safer sleep
Goes over any type of swaddling, sleeping bag or sleepwear, for a snug and more restful sleep


limb and hip movement
• Ensures swaddling, sleepwear, Sleepingbag use is safer and cosier
Natural, flexible body, limb and hip movement
• Excellent for babies requiring varied sleep positions or cot elevation
safely lasts two babies aged 0-2 yrs
Helps keep young babies comfortably o the tummy; older babies turn freely within the wrap
TRUSTED • SAFE • UNIQUE
EPI-NO is clinically proven to significantly increase the chances of an intact perineum, reduce episiotomy, and is safe to use.
EPI-NO is a dual purpose CE approved medical device designed to strengthen the pelvic floor muscles from early in pregnancy, and again postpartum. The perineal stretching exercises commence concurrently after Week 36.

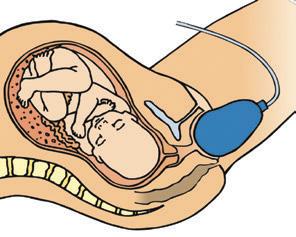

EPI-NO Childbirth Training has been accepted in Australia & New Zealand for over 15 years as an effective preparation for women choosing a natural vaginal birth
EPI-NO Patient Brochures can be requested for New Zealand via info@starnbergmed.co.nz
Over 65,000 EPI-NO births in Australia and New Zealand. Available in over 20 countries worldwide.
www.starnbergmed.co.nz



Available online with shipment from Auckland and at selected pharmacies.
‘The human body performs to maximum efficiency in any physical activity when correctly trained and prepared. Childbir th is no exception.’
Dr Wilhelm Horkel, Star nberg (EPI-NO inventor)
Germany

LABOUR
OF
LOVE: A PERSONAL HISTORY OF MIDWIFERY IN AOTEAROA
KAREN GUILLILAND CONSULTANT

Joan Skinner's recall of the midwifery history she experienced is a welcome contribution to the many events which shaped our midwifery history. She illustrates the changes (good, bad and challenging) through the decades with insight, gentle humour and political awareness. At times I was curious as to whom Joan was referring to when she used the term ‘we’ in relation to these events, and wondered if the book would have benefited from more acknowledgements of the dozens of colleagues throughout New Zealand who contributed to the midwifery story over the years.
That said, this is a lovely piece of writing that flows through from observation, description, analysis and reflection. Joan’s personal story especially is told in an insightful and honest way. Her whānau stories are very moving.
Joan’s adventures abroad as a Midwife Consultant for numerous Aid agencies are remarkable. Her descriptions of life for those women and midwives highlighted how privileged New Zealand is in comparison. The International Confederation of Midwives, (ICM), WHO, UNFPA, JPEIGO, the New Zealand College of Midwives and New Zealand Polytechnics and Universities have a significant and longstanding schedule of work supporting the developing world’s midwifery and maternity systems. Consultants are part of that work and Joan’s skills were appreciated and made positive change for many of her projects. However, she also reflected on the challenges of this role when in isolation and looks back and wonders what do aid projects really achieve when governments, whatever their rhetoric, still largely ignore the rights of women to effective maternity services. Her story of her North Korean experience is starkly illustrative of the political games played in order to get funding. The global examples of colonisation and medicalisation of birth Joan describes made sad and depressing reading. New Zealand too is rightly held to account for its decades of ignoring the real value of midwifery care.
Joan’s account is a personal story and as such relies on the individual’s experience, memory and perspective. This is one such tale skilfully recounted. No doubt many midwife readers will remember people’s roles and contributions slightly differently. I certainly do but then they are my memories!
Labour of Love is an easy read and keeps the reader's interest all the way. I recommend this unique and valuable story of the work of midwives to anyone with an interest in midwifery and women’s reproductive rights around birth. square

*
* s a f e l y l a s t s t w o b a b i e s a g e d a p p r o x i m a t e l y 0 -2 y r s The World’s Safes t Baby Wrap w w safet sleep com
www.safetslee
CLINICALLYPROV E N EFAS • DELLAIRT • CLINICALLYPROVEN 100%SAFETYRECORDEST.1992
est 1992
Use code ‘NZCOM’ for 20% OFF
36 | AOTEAROA NEW ZEALAND MIDWIFE BOOK REVIEW
my midwifery my midwife
Claire Casby is an Irish-trained midwife, currently practising as an LMC in Taranaki. While her journey to Aotearoa may have taken longer to materialise than originally planned, the experience has been well worth the wait.

Claire knew she wanted to be a midwife as a young girl, but made a conscious decision to wait for the right time before embarking on her midwifery journey. “I wanted to have more maturity and life experience first, so I decided to start when I was 30,” she explains.
Having learned of Aotearoa’s maternity system early on, Claire’s midwifery dream was always to practise here, although it took a bit longer to get here than she’d originally hoped. “I would’ve loved to have come to New Zealand years ago, but between one life thing and another I had to jump many hurdles. When we finally did get here in 2021, it was everything I’d hoped it would be.”
On arrival in Aotearoa, Claire and her husband settled on the Taranaki region as their new home. “It sounds cliché, but it was something about the mountain and the sea.”
Having come from the very medicalised, largely under-resourced Irish maternity system, Claire’s experience at Taranaki Hospital was a welcome breath of fresh air. “I had a really good orientation opportunity at Taranaki. I’d come from regularly looking after nine women a shift in Ireland, with no continuity of care. It was like a big revolving factory. At Taranaki I was able to provide actual care and feel like I was on a level team across the disciplines. It was a lot to get my head around the full scope of the LMC role, so doing the maternity systems course as part of my registration was very helpful."
The cultural competency training Claire received here was another confirmation that she’d chosen the right place. “Having moved many times as a child, I knew how it felt to be displaced and have a different cultural perception, which was not fully addressed with the recent immigrant population in my Irish setting. That created many safety issues. I also did my dissertation on positive safety culture in midwifery, which is another reason why the cultural competency training really struck a chord with me.”
Following a break in practice due to the vaccine mandate, Claire returned to midwifery in October 2022 and prepared to commence LMC practice, which she began early this year. “I am loving the fullness of autonomous practice here, moving in the community and in the hospital. I really appreciate all the support in getting me set up and the opportunity to really be with women.”
Now working out of a new clinic in Ōkato, Claire is fine tuning her work-life balance. “It’s an incredible system we’ve got here. I know there are many aspects that need review, but continuity-of-care is everything I dreamed of in this role.” square
Having experienced a high level of intervention in her first pregnancy and birth, Chrisy Sinclair’s goal for her second pregnancy was to experience the opposite. Choosing Claire Casby as her midwife was integral to experiencing a healing birth.

“With a first baby, you don’t really know how important it is to have the right midwife, or what you’re even looking for,” Chrisy explains. “This time, I really wanted someone who was aligned with our belief systems and spiritually on our wavelength. Claire had such a loving and gentle way about her, which we instantly liked. We felt her philosophy was aligned with ours, with a focus on keeping everything natural. She had a real heart connection as well, and we’re all about heart.”
Following a completely different path for her second pregnancy, Chrisy knew what she wanted and simply needed a midwife who could help facilitate that. “We did IVF to get pregnant with our first baby Grace and had a hospital birth, so it was beautiful to be able to follow the natural path all the way with our second daughter Alana. We wanted to have a homebirth and Claire really supported that.”
Her dream became a reality, turning out to be everything she hoped it would be. “It was such a contrast - our beautiful homebirth was so relaxed, peaceful and enjoyable. We had a really quick labouronly two hours. Claire got here and I don’t know how long it was afterwards, but baby was born in our dining room, surrounded by family. It was a beautiful and healing experience.”
Claire’s genuinely caring nature was what stood out for Chrisy. “She was there whenever we needed her. She made it very clear from the outset - to call if I had any worries or concerns at all - which was just amazing and so reassuring, especially when I was in a vulnerable place.”
Continuing to receive that standard of care after Alana was born was another gift. “The postnatal care was amazing too - having the same midwife for the birth and then all the way through, making sure baby and I were ok, felt so reassuring. She’s got a real heart for her work - it shines through in every aspect and she’s always so friendly, positive and helpful.”
Claire’s practice wisdom and neutrality were further pluses for Chrisy, who felt empowered throughout her maternity journey. “It’s obvious Claire really knows what she’s talking about. She shared lots of resources with us in a really balanced way, making sure she gave us all the information so we could make our own decisions and feel confident and secure in them.”
Chrisy’s future vote is clear. “I wouldn’t ever want to have any other midwife. Claire was incredible the whole way through.” square
ISSUE 110 SEPTEMBER 2023 | 37 FROM BOTH SIDES
New Zealand College of Midwives Directory
National Office
PO Box 21-106, Christchurch 8140 Ph 03 377 2732 Fax 03 377 5662 nzcom@nzcom.org.nz www.midwife.org.nz
Auckland Office and Resource Centre
Delia Sang, Administrator Yarnton House, 14 Erson Avenue PO Box 24487, Royal Oak, Auckland 1345 Ph 09 625 9764 Fax 09 625 0187 auckadmin@nzcom.org.nz
College Membership Enquiries
Contact Lisa Donkin membership@nzcom.org.nz 03 372 9738
Chief Executive
Alison Eddy
President
Nicole Pihema
Ph 021 609 011 nicolepihema@gmail.com
National Board Advisors
Kuia: Crete Cherrington
Elder: Sue Bree
Education Advisor: Tania Fleming
Regional Chairpersons
Auckland
Jacquelyn Paki, Mel Nicholson auckchair@nzcom.org.nz
Bay of Plenty/Tairāwhiti
Cara Kellet chairnzcomboptairawhiti@gmail.com
Canterbury West Coast
Sheena Ross chairnzcom.cantwest@gmail.com
Central
Laura McClenaghan centralchair@nzcom.org.nz
Nelson Marlborough
Emma Neal tetauihunzcom@gmail.com
Northland
Shelley Tweedie tetaitokerauchair@nzcom.org.nz
Otago
Jan Scherp, Charlie Ferris otagochair@nzcom.org.nz
Southland Liz Whyte liz.whyte@netspeed.net.nz
Waikato Taranaki Jenny Baty-Myles chairwaikatonzcom@gmail.com
Wellington Suzi Hume nzcomwellington@gmail.com
Regional Sub-Committees
Hawke's Bay Sub-Committee
Kerri Smith kerrijeansmith@aol.com
Horowhenua
Laura McClenaghan midwife.laura@hotmail.co.nz
Manawatu Sub-Committee
Megan Hooper-Smith megan.scott@live.com
Emma LeLievre emma@LMCmidwife.com
Taranaki Sub-Committee Ange Hill nzcom.taranaki@gmail.com
Wanganui Sub-Committee Laura Deane laura.deane@wdhb.org.nz
Consumer Representatives
Home Birth Aotearoa
Bobbie-Jane Cooke bobbiejane.homebirth@gmail.com
Parents Centre New Zealand Ltd
Liz Pearce e.pearce@parentscentre.org.nz
Royal New Zealand Plunket Society
Zoe Tipa zoe.tipa@plunket.org.nz
Student Representatives
Penny Martin pennymartin79@live.com
Ana Ngatai ana.olsen.ngatai@hotmail.co.nz
Ngā Maia Representatives www.ngamaia.co.nz
Dani Gibbs dani.midwife.maori@gmail.com
Lisa Kelly lisakellyto@yahoo.co.nz
Pasifika Representatives
Talei Jackson Ph 021 907 588
taleivejackson@gmail.com
Nga Marsters Ph 021 0269 3460 lesngararo@hotmail.com
MERAS / General Enquiries & Membership
PO Box 21-106, Christchurch 8140 www.meras.co.nz
Ph 03 372 9738 meras@meras.co.nz
MMPO mmpo@mmpo.org.nz
Ph 03 377 2485 PO Box 21-106, Christchurch 8140
Rural Recruitment & Retention Services 0800 Midwife/643 9433 rural@mmpo.co.nz
Resources for midwives and women
The College has a range of midwiferyrelated books, leaflets, merchandise and other resources available through our website: www.midwife.org.nz/shop
38 | AOTEAROA NEW ZEALAND MIDWIFE DIRECTORY




weleda.co.nz @weledanz
You are kaitiaki for hapū māmā and pēpē
Maternal immunisation provides vital protection for pēpē and māmā before and during the most vulnerable first months of life. Your recommendation to immunise can save lives.
INFLUENZA
Pregnant people and their babies are at greater risk of serious influenza-related complications. Most young babies whose mothers were vaccinated during pregnancy are protected against influenza.

WHOOPING COUGH
Babies, particularly younger ones, can get very sick or even die from whooping cough. Most young babies whose mothers were vaccinated during pregnancy are protected against whooping cough.
COVID-19
COVID-19 vaccination in pregnancy protects against infection, severe disease, hospitalisation and death. Babies of immunised mothers receive some of that protection too.
Immunisation during pregnancy boosts disease-specific antibodies that not only protect hapū māmā, but also travel across the placenta and protect pēpē until their first three immunisations at six weeks old.
Influenza vaccination is recommended at any stage of pregnancy and is free during the influenza season
COVID-19 vaccination is recommended and funded at any stage of pregnancy Tdap*
* Tdap is funded from the beginning of the 2nd trimester and is recommended from 16–26 weeks. † MMR post-delivery is recommended for those who haven’t had the MMR vaccine.
For more information, visit immune.org.nz
MMR post-delivery†
First trimester Second trimester Third trimester Post delivery





















 SAM JONES MERAS CO-LEADER (INDUSTRIAL)
SAM JONES MERAS CO-LEADER (INDUSTRIAL)