

Post- Pregnancy
Mood & Sleep
Research based, post-pregnancy formula to support positive mood, calm and sleep.



EDITOR
Hayley McMurtrie
E: communications@nzcom.org.nz
ADVERTISING ENQUIRIES
Hayley McMurtrie
P: (03) 372 9741
MATERIAL & BOOKING
Deadlines for December 2024
Advertising Booking: 1 November 2024
Advertising Copy: 11 November 2024




Welcome to Issue 114 of Midwife Aotearoa New Zealand
At the time of writing the College is leading a Class Action on behalf of members in the High Court. This is set to become a significant moment in the history of New Zealand midwifery and of the College. We do not know what the outcome will be, but we do know we can be very proud of all of those who have taken the stand on behalf of the profession and we take this opportunity to thank them all. Whilst primarily the debate relates to LMC midwives, midwifery is one profession, and regardless of how and where midwives work with women and whānau, if all midwives are supported and their work valued and respected, the whole profession will be better for it.
There is also much discussion within Te Whatu Ora and within this issue of Midwife Aotearoa about the continuity of care model. As we approach this period of potential change it is beneficial to remember the beginnings of this model and the woman-led, whānau-centred core of the midwifery model that we are lucky enough to have in Aotearoa today.
Change is also reflected in the number of practice updates we have in this issue, including prescribing updates (p.12), Vitamin D recommendations (p.14), Pulse Oximetry requirements (p.15) and TXA (p.16). The College midwifery advisors are available to assist with any clarification around what these updates mean for you in practice, whether you are working in a core or LMC environment.
Spring is in the air and here at the College we are preparing to welcome many of you to the Joan Donley Research Forum (p.9), a fabulous opportunity to see first-hand the quality research that is taking place in Aotearoa, as well as to catch up with colleagues in the wonderful New Plymouth.
Ngā mihi nui, Hayley Square

HAYLEY MCMURTRIE
COMMUNICATIONS MANAGER
Email: communications@nzcom.org.nz
from the co-presidents

"Ki te tika te tauira, ka tika te whāia mai' If the example is appropriate, then they will follow in the appropriate manner
- Sir Timoti Karetu (Ngāti Kahungunu, Tuhoe)
'Models of care’ is an interesting phrase. For me personally, it’s lacking in clarity or substance. And despite its firm embedment in the modernday midwifery vernacular, it’s not possible to know what difference our current ‘model of care’ has made to outcomes for whānau. Especially for the whānau whose stories filled the pages of the latest PMMRC report.
I don’t believe the solutions lie in developing or designing new ‘models of care’. In my experience, these constructs aren’t what keep people accountable. True accountability and responsibility have nothing to do with buzz words, and everything to do with something more deeply, intrinsically human.
In this sense, responsibility refers to one’s ability to respond. As midwives, our ability to respond is, quite literally, in our hands. It’s also contained within the vast body of mātauranga we’ve acquired either through the passing down of intergenerational wisdom, or our modern midwifery education, or both.
In te ao Māori, we speak of tīpuna and mokopuna in the same vein; they are one and the same. Tīpuna doesn’t just refer to ancestors passed, but ancestors yet to come.
And irrespective of whether we share biological whakapapa with whānau we’re caring for, every mokopuna is valued equally and as if they’re our own.
So it’s our tīpuna and mokopuna that I and other Māori midwives look to for guidance in our practice. And it’s these mokopuna we respond to. We don’t need words like ‘continuity’ or ‘partnership’, because our values and senses supersede these words; the
behaviours are inherent, imprinted in our DNA.
In other words, Māori midwives are already working in ways that meet the needs of whānau and have been for some time now. And naturally, we’re best positioned to share our perspectives and ways of being.
I’ve cared for my own whānau, including my own daughter, as my mokopuna have entered this world. Had I ignored my own inner compass and followed the so-called professional boundaries outlined to me as a midwifery student, I would have been denying the very fabric of my being and, in our world, nothing could be more damaging.
The solution does not lie in the development of new models. The solution lies in ensuring that the system in which midwives work enables us to be guided by our tipuna so that we are not constrained in the way we can practice. Whether working at policy level in Te Whatu Ora, or in the community alongside birthing whānau, we need to value and respond to each mokopuna as if they are our own. Square

‘Models of care’ is something of a buzz phrase in health this year. However it can mean many things, depending on the setting in which it is used.
Within the International Confederation of Midwives’ consensus statements it refers to a philosophy of care which centres the needs of the recipient of care within their wider cultural, social and psychological context. Whereas within our own recently released Government Policy Statement on Health 2024-2027, the term refers to wider system settings which could enable such care to be provided.
The latest PMMRC report states in no uncertain terms that if we continue to do what’s already been done, nothing will
change. Ensuring the cultural responsiveness of the health system and providing culturally safe care at an individual practitioner level are essential things we can do to play our part in addressing inequities.
Rethinking service delivery, including the role so-called ‘models of care’ have to play, is more pressing than ever and who better placed to design these models, than midwives?
The Midwifery Insights survey, a joint project between Kahu Taurima and Te Whatu Ora, provided midwives with this opportunity - to reflect and feed back on potential models of care across different maternity settings and what those could look like. I hope all of you had your say.
We already have a strong, legislated foundational model of midwifery care based on the principles of continuity, partnership and autonomy. These principles are the core of our work as midwives, however, within this national model we also have examples of local models that recognise and acknowledge the uniqueness of different communities and the extent to which needs vary between groups.
But what does the concept mean to you and your colleagues? As a staff midwife working at a maternity facility, this might look and feel different to the commonly referenced ‘model of care’ often associated with LMC communitybased care. In reality, staff midwives and LMC midwives are interconnected and rely upon one another to deliver a service; both are equally integral to the design of any model. So what is the model of maternity care you work within? And what’s great about it?
What do whānau/families tell you about their experiences of the model you’re currently working in?
I believe a sustainable and effective model of midwifery care must include all of midwifery across community and hospital settings and take into consideration local midwives’ availability and local facilities. It must also be developed in partnership with the whānau/ families you care for, keeping their needs at the centre. Square
Bea Leatham
Debbie Fisher

CLASS ACTIONOUR DAY IN COURT
The College’s legal case against the government is being heard in the High Court in Wellington from 5 August for a six-week period. The proceedings allege breach of contract; breaches of equitable representations by the government; and also claim unlawful gender-based discrimination under the New Zealand Bill of Rights Act 1990.
The circumstances which have led to the current case being taken date back to the College’s initial judicial review claim against the Ministry of Health (the Ministry) in 2015 and include two subsequent Settlement Agreements between the College and the Ministry, one of which is the centre of the present breach of contract claim.
The current case is being taken as a class action, with over 1,400 midwives participating. It is being funded by an international class action funder. As the case and the matters under dispute are currently before the court, the College is limited in what it can publicly say about it. In the fullness of time, we will ensure that there is a coherently documented narrative of the convoluted chain of events that have brought us to this point, for the record.
The College’s decisions to pursue legal actions against the Ministry have not been easy decisions to make. These decisions have only ever been motivated by the desire to ensure that the profession is treated fairly and equitably – and so that we can continue to recruit midwives and retain them in the workforce, under conditions enabling them to provide the care that women and whānau need and deserve. Throughout every step, foremost in the board’s decision-making processes has been consideration of the profession’s future, including those who are new in our profession or yet to join it. Although MERAS has the mandate to negotiate on behalf of employed midwives, in the absence of any other entity with the mandate to negotiate for LMC midwives, the College has been forced to take

from the chief executive, alison eddy
Preparation for the case to be heard in court has been intense and involved the work and commitment of many. Heartfelt thank you to the mediation team witnesses Karen Guilliland, Nicole Pihema and Deb Pittam, all of whom have all been involved throughout legal and Settlement agreement processes which lead to these proceedings.
the issues forward by standing up for working conditions that will support retention, sustainable high quality equitably accessible care, and pay which fairly recognises the responsibilities and skills LMC midwives hold.
Preparation for the case to be heard in court has been intense and involved the work and commitment of many. Heartfelt thank you to the mediation team witnesses Karen Guilliland, Nicole Pihema and Deb Pittam, all of whom have all been involved throughout legal and Settlement agreement processes which lead to these proceedings. The breadth of your testimony, traversing content from the 1993 Maternity Benefits Tribunal in Karen’s case, to the present, including Nicole’s description of her practice as a Māori midwife in rural Te Taitokerau demonstrated the intricate and complex nature of the issues which the case is seeking to resolve. To our midwife witnesses, Yvonne Hiskemuller, Fiona Hermann, Bex Tidball, Sheryl Wright, Kendra Short the profession thanks you for your courage and willingness to put yourself on the record, with at times moving testimony about the work of midwives.
These midwives provide us with a great example of parrhesia (an ancient Greek word which means speaking truth to power). Midwifery has never been shy of speaking truth to power in advocating for women’s
rights, and in this case, these midwives are speaking up for our own profession’s rights to be treated fairly. I also acknowledge and thank the many other midwives; including Sally Pairman (who provided a written brief of evidence to the court), while not appearing in court, generously assisted our legal team with their time and knowledge.
To our legal team – including Robert Kirkness, Dr Mark Hickford, Kate Cornegé, Kerryn Webster, Taz Haradasa, Nerys Udy, Rosalie Reeves and Carla Humphrey – your work and commitment to bring the case to this point has been amazing to observe and bear witness to. The case preparation has involved hours and hours of complex and detailed work, combing through documents, drafting and redrafting briefs, critical thinking and mind mapping to draw the intricate web of facts and evidence of events which have occurred over nearly a decade (and even prior) into a comprehensive and coherent case. Whatever the outcome, members can be assured that with the calibre and fortitude of our midwife witnesses, and expertise of the legal team who have represented us, we have most certainly put the best possible case forward.
By the time this edition of the magazine goes to print, it is expected that the court hearing will be in its final weeks. Most of the evidence will have been presented with witnesses examined and cross examined. Her Honour Justice Cheryl Gwyn, who is presiding over the case, will then retire to consider the evidence. Her judgment is anticipated to be delivered some time in 2025.
I sincerely hope that once this case is concluded, the future is set for self-employed,
publicly funded midwives’ rights to negotiate fair and reasonable working conditions and for that work to be valued fairly. I hope that the College and its members will be able to draw a line in the sand, leaving this challenging decade behind us and, for the sake of those whom we care for, be able to look forward to a future in which our profession can flourish and thrive. Square
governance of the college
For some months now, the College’s board has been deliberating on our current governance model and how well it is serving our organisation’s needs. This discussion commenced as the board was developing our current strategic plan and continued as the recommendations and themes from the cultural review were considered. The work included reviewing the governance models of a range of other professional membership associations and unions.
Our current board is highly unusual in that it is large and appointments are entirely on a representative basis. It includes a total of 25+ individuals:
• Kuia and Elder
• two co-presidents
• 11 regional chairpeople (two for Auckland and one each for other regions)
• two Ngā Maia representatives
• two Pasifika representatives
• two midwifery student representatives
• up to four consumer representatives
• the College CE
• an ex-officio education consultant
• an independent Finance Committee member
There are often additional ex-officio (non-voting) attendees at board meetings too, including incoming or outgoing chairs, sub-regional chairs and staff members. It is not unusual for there to be 30 or more people in attendance at any given meeting.
Although some aspects of our current model are highly valued (including broad representation which brings a diversity of perspectives and skills, networking and relationships), there are some aspects that don’t work so well. A considerable portion of the time spent at board meetings is on information sharing rather than governance-related matters. This means board meetings, which currently take place three times a year in person, take two full days each. The turnover of board membership is high as regional chair roles commonly have two-year terms. In the 20+ years I have worked for the College and attended almost every board meeting, I have never attended a meeting whereby exactly the same people were in attendance at consecutive meetings. This can lead to challenges with decision making as important historical context can be lost from meeting to meeting.
Although our current model served us well as a grassroots and fledgling organisation in our past, it is time to ask ourselves whether it is still serving our needs as best it can. Over the years we have grown and matured as an organisation. We now have over 4,000 members and hold significant responsibilities for the delivery of contracted workforce support services. As the College is an Incorporated Society with charitable status, the board holds legal and financial accountability for the College and, with such a large board, it is sometimes challenging for each board member to maintain a line of sight to this accountability. Because regional chairs form a critical part of our national governance structure, they hold dual responsibilities with both regional and national governance accountabilities, which can also be challenging. It is therefore timely to also consider whether we have the best model and support for our regional structures.
As for all organisations, effective governance is essential to steer the College at a strategic level. It strengthens our organisation, and helps us to manage the risks and challenges that we face. Good governance will ensure that we are effective in meeting our members’ needs and in achieving our mission and objectives. The board has agreed to commission a report on our governance model which will consider options for change for the future.
This work will be undertaken over the coming months within a te Tiriti partnership, and a report is planned to be tabled at the board’s November meeting. Any recommendations for change will be brought to members for their views and perspective before any changes are agreed or implemented. Change can be exciting but also challenging; however, we owe our members the assurance we can adapt and change in response to our organisation’s needs, to make sure we are fit for purpose for today’s world. Square
Although our current model served us well as a grassroots and fledgling organisation in our past, it is time to ask ourselves whether it is still serving our needs as best it can.

your college
MSR and education administration
Alys Pullein has joined the College as Administrator for Midwifery Standards review and Education. She spent several years working in the UK before returning to her Aotearoa home. Alys takes over from Saili who held this position for fourteen years. Saili will be missed by her colleagues and the reviewers and educators throughout the country. Square
college statement on Abortion Reversal
At its July meeting, the National Board approved a statement about a non-evidence-based and potentially harmful practice known as'abortion reversal' which has been reported as having arrived in Aotearoa. The statement has been published on the College’s website, in the practice guidance section. Square
eLearning
By the time members receive this issue of Midwife Aotearoa the College’s long awaited eLearning programme will be live. We are excited to announce the first two courses available through the platform: Practicalities of Mentoring in Aotearoa; and Te Tiriti o Waitangi. Many more courses are in progress and will be launched in the coming months. Square
maternity care for refugee women
The inaugural Refugee Health Community of Practice forum was held at Te Āhuru Mōwai Refugee Resettlement Centre in Māngere on 20-21 June. Midwives Claire MacDonald, Shaqaiak Masomi and Amber Izzard were invited as speakers at the forum. Their presentation was about the College’s work on supporting access to and acceptability of maternity care for former refugee women, and the e-learning module about midwifery care for former refugee whānau which Te Whatu Ora has funded the College to develop. Along with Shaqaiak and Amber, the subject matter expert midwives informing the education development are Sonia Azizi and Louise Nibarema. The forum was an opportunity for stakeholder engagement with the refugee health community to inform the e-learning module, and for the College team to make
Above: Attendees at the inaugural Refugee Health Community of Practice forum in June.
connections and learn about the amazing mahi that is being done across the motu to support former refugees into their new homes and lives in Aotearoa. Square
upcoming workshops
The following dates are available now for face-to-face workshopsbook online www.midwife.org.nz to secure your place.
Tāmaki Makaurau | Auckland
MESR Midwifery Emergency Skills Refresher: 13 September, 18 September, 20 November A-Z of Perineal Care: 3 October
Ōtautahi | Christchurch
A-Z of Perinatal Care: 14 October
Dotting the I's in a Digital Age: Record Keeping for Midwives: 4 November
Te Whanganui a Tara | Wellington A-Z of Perineal Care: 11 November
Ahuriri | Napier
Dotting the I's in a Digital Age - Record Keeping for Midwives: 8 October
Kirikiriroa | Hamilton
MESR Midwifery Emergency Skills Refresher: 8 November
A-Z of Perineal Care: 25 November
Ōtipoti | Dunedin
Dotting the I’s in a Digital Age - Record Keeping for Midwives: 19 November
Maruawai | Gore
Dotting the I’s in a Digital Age - Record Keeping for Midwives: 20 November



bulletin
midwifery insights survey
Under its Kahu Taurima work programme, Health New Zealand | Te Whatu Ora has recently undertaken a survey to inform possible future funding models for community midwives. Alternative contract options may be developed, however, the Primary Maternity Services Notice will remain as an option for LMC midwives who wish to continue working as they are now. Kahu Taurima also aims to address the reality that some whānau are not currently able to access LMC midwifery care, and there are also inequities in whānau choice, and outcomes for māmā and pēpi. Any new alternatives need to be sustainable for midwives, and achieve improved access, experience and outcomes for whānau.
The purpose of the survey was to learn what midwives value in alternatives to the current funding model, to inform the development of new national settings for enhanced workforce support for community midwifery and to achieve improved access, outcomes and experiences of care for whānau. Health NZ have confirmed that continuity of care will continue to be a cornerstone of any future Kahu Taurima service. Midwives are a vital and valued workforce within our health services and will continue to lead in the provision of primary maternity care.
The College hosted two member webinars
in July to explain and discuss the survey and both webinars were well attended with strong engagement from midwives. Health New Zealand have agreed to share the survey results with the College. Square
national perinatal pathology service online training
The National Perinatal Pathology Service will be inviting midwives to participate in their new online course that is being launched in the last quarter of 2024. The service has worked with subject matter expert, Dr Vicki Culling, to develop an online course that provides information and resources to health professionals, who interact with bereaved parents and whānau after the death of a baby, and introduce the post-mortem procedure to them.
The course provides information about what the perinatal post-mortem entails and the referral process, and participants hear from perinatal pathologists from around the country. It also provides information on discussing post-mortem in a supportive, culturally safe way. The course includes interviews with bereaved whānau – some who chose to have a post-mortem for their baby, and some who chose not to and why.
The approximately 5 hour course is free for health professionals and can be used as CPD.
Register your interest at perinatalpathology@ adhb.govt.nz Square
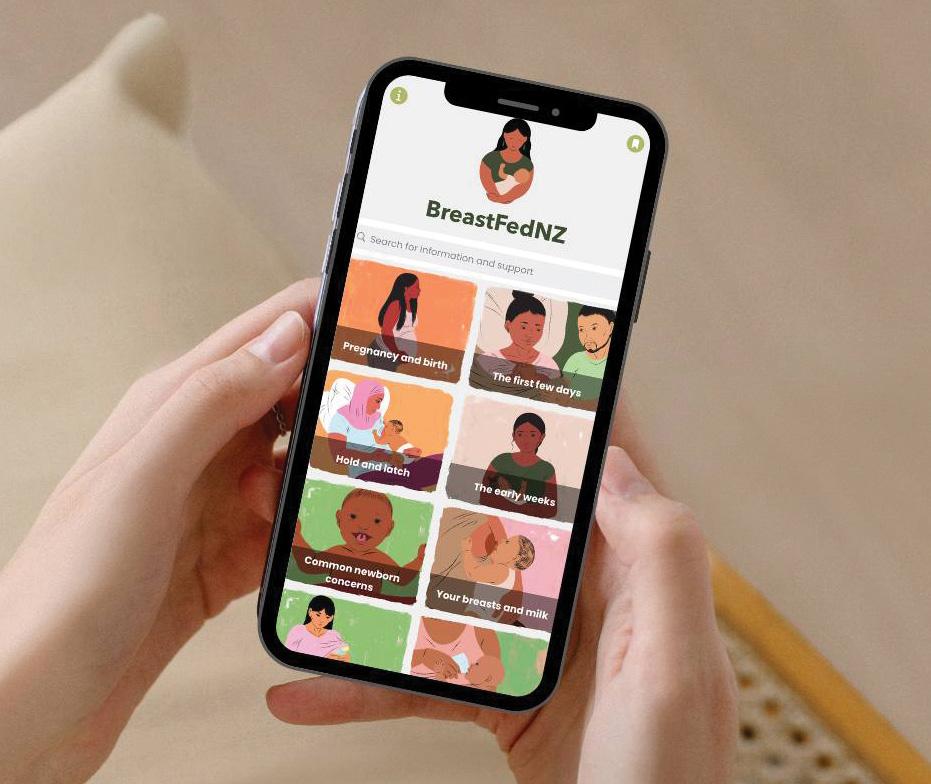
breastfeeding apps
The BreastFedNZ app has had a major overhaul and has been relaunched. The project was originally initiated by the five Midland DHBs with midwife and lactation consultant Karen Palmer developing content as part of a wide consultation process. The easy to use resource is designed for consumers and health practitioners - particularly midwives.
The updated Mama Aroha app, developed by midwife and lactation consultant
Amy Wray in collaboration with the New Zealand Breastfeeding Alliance and Hāpai Te Hauora, puts breastfeeding information into a user-friendly format for health professionals, mothers and whānau. Both apps are available for download from Google Play and App store. Square
telehealth (COVID) number is no longer active
The Covid Telehealth clinical advice line was decommissioned on 1 July 2024. Guidance for Health Professionals can now be found on the Health NZ website https://www.tewhatuora. govt.nz/health-services-and-programmes/ infection-prevention-and-control/ Square
CE Alison Eddy with Laura Aileone, Chief Midwife, Health NZ
BreastFedNZ App

jane cartwright is moving on from the new zealand breastfeeding alliance
After seven years as CEO of the New Zealand Breastfeeding Alliance (NZBA), Jane is now leaving this role to take on a new part-time role as Regional Integration Team Lead with Te Waipounamu. Jane's relationship skills, commitment to strengthening communities, and dedication to working in partnership, have supported the Baby Friendly Hospital Initiative to flourish. This year Jane became a Member of the NZ Order of Merit (MNZM), for her services to health governance. The College is sorry to see Jane leave the NZBA, but we wish her all the best for her new role. Square
chief midwife appointed
Laura Aileone has recently been appointed as the new Chief Midwife within the Clinical leadership directorate in Health New Zealand. As Tāngata o Te Moana-nui-a-Kiwa, Ngāti Hāmoa, Laura is passionate about addressing the inequities in our healthcare system, and ensuring both clinical and whānau voices are at the heart of midwifery service design and delivery. Having spent over 20 years in healthcare as a midwife, in midwifery and maternity service development, and in leadership and advisory roles across Aotearoa, Laura brings a wealth of experience to the role. The College CE and Advisors have met with Laura and look forward to working with her in this newly permanent role. Square
thank you deb
The College acknowledges the work of Deb Pittam who was seconded into the Interim Chief Midwife position when it was established last year. Deb led the profession in this role throughout particularly challenging times, as the health system adjusted to its new structure and with midwifery workforce shortages ever present. Throughout her tenure in the Chief Midwife role, Deb displayed innovative problemsolving skills, clear leadership and advocacy for women and whānau who access midwifery and maternity services, as well as for the midwifery profession. The profession thanks you for your service and wishes you all the best for the future. Square

Deb Pittam, former interim Chief Midwife

VIOLET CLAPHAM MIDWIFERY ADVISOR
PRESCRIBING UPDATE FOR MIDWIVES
Health New Zealand | Te Whatu Ora has recently published the latest version of the Pharmacy Procedures Manual (available at www.tewhatuora.govt.nz), which sets out rules and requirements for prescribing in Aotearoa New Zealand.
REINSTATEMENT OF CO-PAYMENTS ON PRESCRIPTIONS
The Government ended universal free prescriptions on 15 July 2024, with the $5 copayment restored for most New Zealanders. However, prescriptions will remain free for people with Community Services Cards,

people under 14 and people aged 65 and over. The Prescription Subsidy Card will continue to limit the total number of co-payments an individual or family will pay to 20 per year (the pharmacy year is 1 February to 31 January).
MIDWIFERY PRESCRIBING
Registered midwives take responsibility for the care of a woman throughout her pregnancy, childbirth and postnatal period. Registered midwives may claim maternity, pharmaceutical and other related benefits relevant to pregnancy and childbirth. Midwives are not able to prescribe for an underlying medical condition, such as asthma or hypertension but they may prescribe for the treatment of a patient under their care:
• any pharmaceutical for the woman, providing it is during pregnancy, labour and the postpartum period up to six weeks
• for the baby during this six-week period
• morphine, tramadol, fentanyl and pethidine, but no other controlled drug
As per the College’s consensus statement on Midwife Prescribing, midwives are expected to have knowledge regarding the effects, side effects, interactions and contra-indications of the drugs prescribed. The College expects midwives to prescribe within the level of their knowledge and expertise. However, midwives are not expected to prescribe for all antenatal, labour, birth and postnatal situations.
In relation to a preterm baby, the Midwifery Council defines the six-week postpartum period as commencing from the expected date of birth rather than the actual date of
birth. In other words, for preterm babies, the postpartum midwifery role may extend beyond six calendar weeks.
LEGAL AND CONTRACTUAL REQUIREMENTS OF A PRESCRIPTION FORM
The information supplied on a prescription form must be legible and indelible (written in pencil, for example, is not acceptable) and must include all the following:
• Prescriber’s usual signature in their own handwriting (not being a facsimile or other stamp) – subject to the Signature Exempt Prescription provisions
• The date on which the prescription form was signed
• Prescriber details, which include:
- Prescriber’s full name
- Prescriber’s physical work address, or postal address for those who do not have a place of work
- Prescriber’s telephone number
• Patient details, which include:
- Surname and each given name of the patient
- Physical address of the patient
- Patient’s date of birth if the prescription form is for a child under 14 years
• Pharmaceutical details, which include:
- Name of the pharmaceutical
- Strength of the pharmaceutical to be dispensed (where appropriate)
(0-13 years)
(14-17 years)
(18-64 years)
- Total amount of pharmaceutical or the total period of supply to be dispensed - Dose and frequency of the dose for internal pharmaceutical
- Method and frequency of use for external pharmaceutical
The Temporary Authorisation from Signatures on Prescriptions without NZePS (i.e., no barcode), which has been in place since October 2022, continues to allow non-NZePS signature-exempt prescriptions to be issued if the requirements under the Temporary Authorisation are met.
Midwives are entitled to verbally communicate prescription forms in an emergency situation.
MIDWIFE PRESCRIBING RULES FOR CONTROLLED DRUGS (CLASS B AND CLASS C)
Within the controlled drug categories, midwives may only prescribe tramadol, pethidine, morphine or fentanyl. The maximum period of supply is one month, and every controlled drug prescription form must state ‘for midwifery use only’. Midwives may not prescribe any other controlled drugs, such as codeine and benzodiazepines. Controlled drugs must be first dispensed no more than four days after the date of the prescription and repeats must be dispensed no more than four days after the previous supply is exhausted.
PRACTITIONER SUPPLY ORDERS
Midwives are entitled to use a Practitioner's Supply Order (PSO) form to order pharmaceuticals within their scope of practice. PSOs must be supplied in accordance with Pharmaceutical Schedule Rules. Pharmac publishes a list of funded pharmaceuticals which may be obtained by a midwife on a PSO. The list is updated monthly and can be found on the Pharmac website (www.pharmac.govt.nz). Square
YOUTH (AGES 0 TO 13 YEARS) – Y CODE
ADULT (AGES 18 TO 64 YEARS) – A CODE

VIOLET CLAPHAM MIDWIFERY ADVISOR
PRACTICE UPDATE –VITAMIN D
Health New Zealand | Te Whatu Ora have published a new national maternity companion statement titled: Companion Statement on Vitamin D and Sun Exposure in Pregnancy and Infancy in Aotearoa New Zealand – Tauākī Āpiti mō te Huranga Hihirā me te Huaora D i te Hapūtanga me te Nohinohitanga i Aotearoa. This statement, developed by a multidisciplinary steering group with sector-wide consultation, supersedes previous versions. The full version is available on www. tewhatuora.govt.nz
The Companion Statement should be read in conjunction with the Consensus Statement on Vitamin D and Sun Exposure in New Zealand (Ministry of Health and Cancer Society, 2012), the Ngā Paerewa Health and Disability Services Standard 8134:2021 (Standards New Zealand, 2021) and the corresponding sector guidance.
Midwives are advised to read the companion statement and supporting content to comprehensively understand this update and implications for practice. The companion statement is expected to be implemented within maternity services and professional practice to the best of one’s ability, ensuring clear documentation and rationale when there is an inability to do so. The key changes for midwives to be aware of are:
• Universal vitamin D supplementation is now recommended for all exclusively or partially breastfed babies
• Supplementation for infants should be commenced by four weeks of age and continue until 12 months of age
• The recommended daily supplement for babies is 400 IU colecalciferol 188mcg/mL orally per day (1 drop)
• Midwives should screen pregnant women to determine risk of vitamin D insufficiency
• Supplementation should be offered to pregnant women if they have any of the following risk factors:
- Live south of Nelson during winter or spring
- Naturally dark skin tone
- Spend limited time outdoors and/or have minimal sun exposure due to religious, cultural, personal or medical reasons. Square
References available on request.
practice points for midwives
DEFINING INSUFFICIENCY/ DEFICIENCY

In this companion statement Vitamin D insufficiency is defined as a level of <50 mmol/L, Vitamin D deficiency is defined as a level of <25 mmol/L.
MATERNAL HEALTH OUTCOMES
There is some evidence to suggest the health outcomes, gestational diabetes and pre-eclampsia. are linked to vitamin D insufficiency.
INFANT HEALTH OUTCOMES
There is sufficient evidence to suggest bone health is linked to adequate optimal vitamin D status. There is some evidence indicating the health outcomes, low birth weight, dental caries and acute respiratory infections are linked to vitamin D insufficiency or deficiency.
Discuss the following with whānau during pregnancy and infancy:
Maternal and infant risk factors for vitamin D deficiency or insufficiency; Testing asymptomatic pregnant people and infants for vitamin D insufficiency is not routinely recommended; Testing may be appropriate for: pregnant people with a known history of vitamin D deficiency/insufficiency; pregnant people with unexplained raised serum alkaline phosphatase, low calcium phosphate, atypical osteoporosis, unexplained bone pain, unusual fractures, or other evidence suggesting metabolic bone disease; infants presenting with seizures where hypocalcaemia is implicated, or unexplained raised serum alkaline phosphatase.
Recommendations for supplementation
Pregnancy: Offer vitamin D supplementation during pregnancy if they have any of the listed risk factors. Prescribe 400-800 IU Colecalciferol 188 microgram/ mL oral liquid per day. Individuals with all three risk factors during pregnancy may be at a higher risk of vitamin D deficiency and testing may be considered. Where vitamin D insufficiency or deficiency is confirmed through testing, follow the advice from New Zealand Formulary.
Infancy: Offer to prescribe vitamin D supplements to all exclusively or partially breastfed babies. Supplementation should begin by 4 weeks and continue until 1 year of age. Prescribe 400 IU Colecalciferol 188 microgram/mL oral liquid per day.
Sun safety advice: Discuss the following messages with whānau where appropriate: Follow the same sun safety messages as for the general population during pregnancy; Always avoid sunburn; There is no safe threshold of UV exposure from the sun that avoids skin damage and ensures sufficient vitamin D synthesis; Sunscreen should only be used on small areas of a baby's skin and should not be the only form of protection from the sun: use shade, protective clothing, broad-brimmed hats, and sunglasses; Young children, once mobile, should follow the same sun safety advice as for the general population.
RISK FACTORS IN PREGNANCY
There is an increased risk of vitamin D deficiency during pregnancy if the pregnant person has any of the following: naturally dark skin tone; live south of Nelson/Marlborough during winter or spring; spend limited time outdoors and/or have minimal sun exposure due to religious, cultural, personal or medical reasons.
SUPPORTING BREASTFEEDING
Breastmilk is the ideal food for infants and contains antibodies which protect infants against illness whilst providing all the energy and nutrients that the infant needs for the first months of life. There is strong evidence on the benefits of breastfeeding for both the mother and infant. Everyone should be encouraged and supported to breastfeed.
FURTHER RESEARCH
Further evidence is important to strengthen the understanding of vitamin D and sun exposure on health outcomes in pregnancy and on infants.

BRIGID BEEHAN MIDWIFERY ADVISOR
NEW NATIONAL GUIDELINES FOR NEWBORN PULSE OXIMETRY SCREENING
Pulse oximetry is a simple, non-invasive screening tool that can detect critical congenital heart disease in newborns before symptoms appear. Health NZ I Te Whatu Ora has published a new national guideline, titled Pulse oximetry screening guidelines for newborn babies, to provide a consistent and evidence-based protocol for practitioners to follow. The guideline supports local health services, including all midwives providing birth and early postnatal care, to implement this screening.
Midwives are recommended to familiarise themselves with the guidelines, along with the algorithm, data collection form, and an information sheet for parents and whānau, all of which are available on the Health New Zealand | Te Whatu Ora website.
Developed for health practitioners involved in the assessment, screening, and treatment of newborns in Aotearoa New Zealand, these guidelines have been endorsed by the National Maternity Monitoring Group. Districts are responsible for implementing these guidelines and ensuring they meet their obligations under Te Tiriti o Waitangi to deliver equitable services.
The College was represented on the guideline development group and the draft guideline underwent member consultation. The College advocated for their implementation to enable screening to be equitably available to all whānau regardless of birth setting. This includes addressing challenges regarding access to appropriate
pulse oximetry equipment for midwives providing homebirth services.
KEY POINTS FOR MIDWIVES
• Motion-tolerant pulse oximeters that measure functional oxygen saturation levels are recommended.
• Parents, whānau, and guardians of well newborns born at 35 weeks gestation or more should be offered screening.
• Depending on the birth setting, the optimal time for the pulse oximetry screen is between 2 and 24 hours of age.
• Health practitioners should provide full, accurate, and unbiased information to help parents make an informed decision, ideally before the baby is born.
• Test results should be documented in the newborn’s clinical notes. If screening is declined, this should be recorded in both maternal and newborn clinical notes.
• Babies should not be discharged from a facility unless their oxygen saturation is greater than 95%. If their oxygen saturation is less than 95%, refer to the algorithm.
• For home births, screening should be undertaken before the midwife leaves the home, where possible.
The College understands that districts are at different stages of implementing this guideline. We recognise the importance of equitable access to this screening and are advocating for locally designed strategies to ensure that the place of birth does not become a barrier.


BRIGID BEEHAN MIDWIFERY ADVISOR
PRACTICE UPDATE: TRANEXAMIC ACID (TXA) IN POSTPARTUM HAEMORRHAGE MANAGEMENT
In 2022, the Ministry of Health | Manatū Hauora (MOH) published the Postpartum Haemorrhage (PPH) Consensus Guidelines, accompanied by the Treating Postpartum Haemorrhage poster. A notable update in these guidelines included specific recommendations for the administration of Tranexamic Acid (TXA) in the early management of PPH. This change means that midwives are now prescribing and administering TXA as part of the early recognition and proactive management of PPH. This article serves as a recap and practice update for TXA prescribing and administration, providing practical points to ensure effective and safe use in various practice settings.
WHAT IS TXA?
Tranexamic Acid (TXA) is an antifibrinolytic drug that inhibits the enzymatic breakdown of fibrin blood clots – known as fibrinolysis. It has been widely used in medical fields, including emergency trauma and surgical care. The 2020 WHO WOMAN (World Maternal Antifibrinolytic) trial significantly influenced PPH management worldwide. This large, randomised, controlled trial, involving over 20,000 women in 21 countries, provided robust evidence supporting the use of TXA in PPH management. The trial demonstrated that TXA reduces the risk of death due to bleeding by 30%, without increasing the risk of thromboembolic events, and reduces the risk of urgent surgery to control bleeding by 35%, thus shaping global and national guidelines, including those in Aotearoa.
KEY FACTORS
The 2022 National PPH guideline stresses the need for immediate action without
delay when PPH is suspected, including early recognition and assessment with swift management, including drug treatment. It is important to know that TXA is most effective when administered early, alongside other management and treatment measures. It's crucial to understand that TXA is not a replacement for uterotonics but rather an adjunctive treatment. Uterotonics stimulate uterine contractions to reduce blood loss. In contrast, antifibrinolytics temporarily slow the breakdown of clots and prevent further bleeding. Both drug classes play essential roles in the comprehensive management of PPH.
PRESCRIBING AND ADMINISTRATION
For PPH, TXA is recommended to be administered intravenously. The dosage is 1g/10ml IV at 1ml per minute. A repeat dose may be given if bleeding continues after 30 minutes or resumes within 24 hours of the initial dose. Square
Tranexamic acid

Dosage for PPH
1g/10ml IV at 1ml per minute
Action IV acts in 5-15 mins, effects last 3 hours and dosage can be repeated after 30 mins. There is no benefit of giving TXA after 3 hours from onset of bleeding.
Side effects and contraindications
Nausea, vomiting and diarrhoea are common. Do not use if a woman/ person has:
• A known thromboembolic event
• A history of coagulopathy
• Active intravascular clotting
• A known hypersensitivity to tranexamic acid
practice points for midwives
• TXA is within the midwife’s scope to prescribe and administer, and plays a crucial role in improving maternal outcomes when used effectively and safely. When prescribing a new medication, the College expects the midwife to do the necessary professional development to be competent to prescribe and administer the medication.
• The College recommends midwives add TXA to their homebirth pharmaceutical kit.
• IV TXA is not currently included in the Pharmac practitioner supply order. The College has been advocating for Pharmac to include TXA on the PSO schedule. Currently, 5 vials cost around $20.
• TXA is most effective when administered early after the onset of a PPH. TXA has no benefit after 3 hours. Early administration within 3 hours significantly improves survival rates and reduces the need for hysterectomy. Delays decrease survival by 10% for every 15 minutes.
• Ensure accurate dosage, using the appropriate concentration and administration rate (1g/10ml IV at 1ml per minute).
• Consultation and caution must be considered with contraindications for the medication: Do not administer TXA to women with active thromboembolic disease, a history of coagulopathy, or known hypersensitivity to the drug.
• Ensure TXA administration and subsequent care are culturally safe and respectful. Engage with the woman’s whānau and respect cultural practices and beliefs.
• The principles of Te Tiriti o Waitangi should guide interactions and care plans to achieve equitable health; TXA for PPH should be offered in all birth settings, including home.
• For comprehensive guidance on managing PPH, midwives should refer to the MOH Postpartum Haemorrhage (PPH) Consensus Guidelines and poster, alongside any regional guidelines.


CAROLINE
CONROY MERAS CO-LEADER (MIDWIFERY)
SAM JONES MERAS CO-LEADER (INDUSTRIAL)
changes in the workplace… how should this occur?
At some time most midwives have experienced changes in their workplace. These can include:
• Environmental changes such as renovations or changes in the use of rooms
• Relocation of services
• Changes to hours of work or shift patterns
• Changes to role, duties, expectations, service reviews or restructuring of services
• Creation of new roles or disestablishment of roles
• New or revised policies and guidelines

Change managed well in a workplace can be positive, providing opportunities for midwives to contribute ideas and to feel part of any change, which in turn has a positive effect on staff morale. Managed badly, change can have a negative impact on the retention of staff, adversely affect morale and breaking down trust between managers and employees. The MERAS Collective outlines how change should occur in the workplace, capturing key principles which are also included in legislation.
HOW SHOULD CHANGE BE MANAGED?
Changes should occur with some level of consultation with MERAS and the affected workers. The level of consultation may differ depending on the significance and impact of the change, but it must occur. Depending on the nature of the change or provisions of your employment agreement, your consent may be required.
Key principles required in change management processes include:
• Presenting proposals for change of a decision which is not yet finalised.
• Providing relevant information to enable adequate understanding of the proposed change, along with substantive input by affected employees and their Union.
• Ensuring reasonable timeframes that enable the consultation to occur.
• Maintaining open and transparent communication between the parties.
• Giving consideration to the feedback prior to any decision being made.
WHAT HAPPENS IF THIS PROCESS IS NOT FOLLOWED?
If midwives are experiencing change in their workplace or are aware of change that is about to occur, and the requirements outlined above are not evident, they should talk to their local MERAS workplace representatives and MERAS staff. Don’t assume that MERAS has been advised of the change occurring.
If change is occurring and there has not been consultation with midwives and MERAS, then MERAS will raise concerns with managers and highlight the expectations within the Collective and legislation. Any change should not occur until after there has been genuine consultation.
WHAT HAPPENS IF THERE IS A FORMAL CONSULTATION PROCESS?
There are times when midwives and MERAS representatives have been involved in the discussions and development of proposed changes that form the ‘proposal for change’. In other cases the proposal for change is a complete surprise to midwives and MERAS.
When MERAS is advised of a proposal for change, staff talk to local MERAS workplace representatives and affected midwives to gauge their views on the proposal. Feedback is drafted and circulated to members to ensure all their concerns and ideas are reflected. Following the feedback period, midwives, MERAS workplace representatives and MERAS staff may be invited to be part of the review of the feedback and recommendations.
At other times this is just done by managers with midwives and MERAS advised of the outcome.
THE IMPACT OF CHANGE
Sometimes change in a workplace can have a significant impact on an individual midwife or a group of midwives. If this occurs MERAS staff are available to

support midwives through any change nd ensure they are aware of the options available to them. There must be reasonable time for employees to explore these options and for notice to be given prior to any change after consultation has occurred. Do not hesitate to contact MERAS if change is proposed or occurring in your workplace. Square For MERAS Membership merasmembership.co.nz www.meras.co.nz
MERAS/Te Whatu Ora Collective Employment Agreement
Clause 27.1
Management of Change
a. The parties to this Collective Agreement accept that change in the health service is necessary in order to ensure the efficient and effective delivery of health services. They recognise a mutual interest in ensuring that health services are provided efficiently and effectively, and that each has a contribution to make in this regard.
b. Regular consultation between the employer, its midwives, and the union is essential on matters of mutual concern and interest. Effective communication between the parties will allow for:
• improved decision making;
• greater co-operation between employer and midwives; and
• a more harmonious, effective, efficient, safe, and productive workplace.
c. Therefore, the parties commit themselves to the establishment of effective and ongoing communications on all midwife relations matters.
d. The employer accepts that MERAS representatives are a recognised channel of communication between the union and the employer in the workplace.
e. Prior to the commencement of any significant change to staffing, structure or work practices, the employer will identify and give reasonable notice to employees who may be affected and to MERAS to allow them to participate in the consultative process so as to allow substantive input.
f. Reasonable paid time off at T1 shall be allowed for midwife representatives to attend meetings with management and consult with employees to discuss issues concerning management of change and staff surplus.
g. Prior approval of such meetings shall be obtained from the employer and such approval shall not be unreasonably withheld.
Clause 27.2
a. Consultation involves the statement of a proposal not yet finally decided upon, listening to what others have to say, considering their responses and then deciding what will be done. Consultation clearly requires more than mere prior notification.
b. The requirement for consultation should not be treated perfunctorily or as a mere formality. The person(s) to be consulted must be given sufficient opportunity to express their view or to point to difficulties or problems. If changes are proposed and such changes need to be preceded by consultation, the changes must not be made until after the necessary consultation has taken place.
c. Both parties should keep open minds during consultation and be ready to change. Sufficiently precise information must be given to enable the person(s) being consulted to state a view, together with a reasonable opportunity to do so - either orally or in writing.
d. Consultation requires neither agreement nor consensus. The parties accept that consensus is a desirable outcome, however the final decision shall be the responsibility of the employer.
e. From time to time directives will be received from government and other external bodies, or through legislative change. On such occasions, the consultation will be related to the implementation process of these directives. In considering the period of consultation the parties will agree on a period of time for the parties to engage with each other.
f. The process of consultation for the management of change shall be as follows:
1. The initiative being consulted about should be presented by the employer as a 'proposal' or 'proposed intention or plan' which has not yet been finalised.
2. Sufficient information must be provided by the employer to enable the party/parties consulted to develop an informed response.
3. Sufficient time must be allowed for the consulted party/parties to assess the information and make such response, subject to the overall time constraints within which a decision needs to be made.
4. Genuine consideration must be given by the employer to the matters raised in the response.
5. The final decision shall be the responsibility of the employer.

WAYNE ROBERTSON EXECUTIVE DIRECTOR, MMPO
reflecting on the integration of the BadgerNet Maternity Suite into New Zealand’s maternity care system
New Zealand’s maternity system has historically faced challenges due to fragmented and disconnected clinical data-recording practices. Recent advancements maintain the drive towards a unified clinical maternity data system, primarily centred around the continued implementation of the BadgerNet maternity suite of products.
The system is expected to be fully adopted by most North Island maternity facilities, in addition to the existing Lead Maternity Carer (LMC) midwife users across Aotearoa. This will mean that more maternity data and information will be seamlessly shared between LMCs providing community care and midwives based in maternity facilities. But how will this benefit māmā, pēpi, whānau and LMCs?
KEY FEATURES AND BENEFITS
• Better clinical decision-making support, leading to more responsive maternity care
• More efficient and effective integration of healthcare services (community and facility)
• Greater māmā and whānau empowerment and engagement
• Greater provision of education and resources
• Better data analytics and reporting, leading to improved insights and innovation
• Continuous improvement to training and support
The current BadgerNet suite offers a unified system through access to contrasting functions and views. These are:
MĀMĀ, PĒPI AND WHĀNAU ACCESS AND VIEW (BADGERNOTES – MULTI LANGUAGE)
This enables secure and private online digital access (through any digital device) to important parts of the woman’s pregnancy record, plus digital access to key resources (including online leaflets) as the pregnancy progresses.
Available pregnancy notes can be securely shared with other health professionals for a limited time. Women control their notes' sharing and can grant up to 1-hour access that can be cancelled anytime, with an audit trail of invitees and access usage.
BadgerNotes integrates with BadgerNet, tracking when leaflets/resources are opened and when the māmā/whānau completes birth plans.
LMC COMMUNITY MIDWIFE ACCESS AND VIEW (AVAILABLE TO THE MIDWIFE NOW)
This gives LMCs the ability to document, review and manage the full pregnancy from the first registration visit, to labour and birth and through until handover to Well Child and general practice.
To ensure safe practice standards, the implementation of included features like
offline mode, partner present mode and robust login support are essential. Offline mode allows continuous documentation even without internet access, ensuring no data loss. Partner present mode controls the visibility of sensitive and confidential data and information during consultations, enhancing support and safety. Secure login mechanisms are crucial for maintaining an accurate audit trail, safeguarding whānau data and ensuring accountability.
Additionally, charts such as MEWS (Modified Early Warning Score), NEWS (National Early Warning Score), GROW (Gestation Related Optimal Weight), Partogram, and biometric charts are accessible and play a vital monitoring and management role.
MATERNITY FACILITY MIDWIFE ACCESS AND VIEW
This gives maternity facility midwives the ability to document, review and manage the pregnancy during the labour and birth stage. The LMC midwife has complete visibility of all data and information updated while the māmā and pēpi are in any maternity facility that uses the BadgerNet maternity system.
NATIONAL DATA VIEW (PERINATAL SPINE) MANAGED BY BADGERNET
The Spine is a national data repository of certain data points and fields (based on the HISO Maternity Care Summary Standard) and sourced from digital records maintained by all LMC midwives (including non-BadgerNet digital vendors) and facility midwives.
Currently, only some booking data, including basic demographic data, are being sent to the Perinatal Spine. No clinical notes or additional context is sent unless the midwife is providing the required information directly in the BadgerNet Raw Care record (through the MMPO and certain facility users).
As data is progressively added to the Spine, māmā and their whānau will no longer need to repeatedly provide detailed medical history, and it will facilitate smoother claims if there is a change in LMC, as the subsequent midwife will not need to start from scratch.
The Spine's implementation is being rolled out in four phases:
• Phase 1 has already been delivered.
• Phase 2 is in testing and includes labour and birth data, newborn baby data and functionality for external parties to
retrieve data, with a release date still to be confirmed.
• Phase 3 will cover postnatal data.
• Phase 4 will include remaining antenatal data and a 'Do Not Share' feature, which is a Health NZ function requiring women to contact Health New Zealand, with the process details yet to be released.
UNIFIED DIGITAL MATERNITY
SYSTEM – BADGERNET DIGITAL
SUITE CLINICAL AND PROFESSIONAL OVERSIGHT
The MMPO Clinical Reference Group (CRG), composed of current midwife users, plays a crucial role in ensuring that the digital maternity system is fit for purpose by focusing on functionality, features, and clinical requirements.
Furthermore, the MMPO regularly engages with the College to seek professional advice and guidance, ensuring that the system aligns with the most up-to-date clinical standards and best practices.
Finally, the MMPO actively participates in broader maternity sector groups such as Health New Zealand's Expert Clinical Advisor (ECA) groups, which include representatives from midwifery, obstetrics and gynaecology, neonatal practitioners, and anaesthetists. These interactions ensure that the needs and perspectives of midwives are well-represented and integrated into the ongoing development and enhancement of the system.
From a wider sector view to ensure the ongoing maintenance of clinical and professional standards, as well as the functionality of the digital maternity system, various sector groups play vital roles. Health New Zealand's ECA groups report to the National Maternity and Neonatal Data and Digital Steering Group (MNDDSG) under Te Whatu Ora.
This steering group is responsible for submitting requests as the system evolves in response to user needs and maintaining high standards of clinical care.
IN SUMMARY
The integration of the BadgerNet Maternity Suite into New Zealand's maternity care system marked a pivotal advancement towards unified clinical data and streamlined care coordination. By integrating maternity data and facilitating seamless sharing between LMC midwives and facility midwives, the
system significantly enhances clinical decision support, efficiency, and patient engagement. Key features such as offline mode, partner present mode, and secure login ensure safe practice standards, while tools like MEWS, NEWS, GROW, Partogram, and biometric charts provide comprehensive maternal and fetal health monitoring. The phased implementation of the national Perinatal Spine further simplifies data sharing and continuity of care.
Through ongoing professional oversight and collaboration across the sector, the BadgerNet Maternity Suite promises to elevate the quality of maternity services, ensuring better outcomes for māmā, pēpi, whānau and the midwifery community. Square

MMPO provides self employed community midwives with a supportive practice management system.
www.mmpo.org.nz
mmpo@mmpo.org.nz
03 377 2485

TAMARA KARU NGĀ MAIA GENERAL MANAGER
Enhancing Support for Māori Midwives: A Tiriti Honouring Approach
TRANSFORMING THE GRADUATE SUPPORT PROGRAMME
The Graduate Support Programme for Qualified Midwives in Aotearoa (New Zealand) is undergoing a major transformation. This redesign is a collaborative effort with the New Zealand College of Midwives (the College) and Ngā Maia Trust. From the beginning, this process has been deeply rooted in honouring Te Tiriti o Waitangi, ensuring the articles and the principles of partnership, protection, participation and equity are top of mind.
As we near the completion of this redesign process, I am hopeful the new and improved version of the Graduate Support Programme will expand its view of the traditional elements such as mentoring, professional development and clinical support, as well as enhance and strengthen the cultural support component. This integration is crucial to creating a culturally responsive environment that meets the needs of all midwives, particularly Māori midwives, tangata whenua (people of the land).

TŪRANGA KAUPAPA AND CULTURAL SAFETY
We are thrilled to share that the Tūranga Kaupapa Education Programme 2024-2028 has received endorsement from the Midwifery Council. The Trust is working diligently to prepare the enrolment pathway for both a face to face and a live online learning schedule. The aim is to make the process smooth and accessible. We feel it best that our primary focus is to first train midwifery educators, midwifery leaders and MSR reviewers, ensuring they are all well-prepared to integrate the anticipated learning outcomes into their respective areas.
CLINICAL COACHING OPPORTUNITY
Ngā Maia is excited to support Te Whatu Ora (formerly Te Aka Whai Ora) in offering a pilot programme to explore the benefits of clinical coaching for Māori midwives. The expectation is that clinical coaching will improve recruitment and retention.
Ngā Maia Trust now offers professional support to practising midwives (Kahu Pōkai) to help them thrive in their work, by their design. Due to the need for both rapid and short-term actions (6 months), we are launching this service immediately with five trusted Clinical Coaches: Lisa Kelly, Crete Cherrington, Jacqueline Martin, Victoria Roper and Tamara Karu. Eligibility for the pilot requires that midwives be beyond their first two years of practice. However, if you have a significant need for clinical coaching or are about to complete MFYP, we would like to hear from you on admin@ngamaiatrust.org.
If you're interested in free clinical coaching, peer mentoring or clinical practice support in a culturally responsive manner, register your interest via your membership portal on our website ngamaiatrust.org/services. Coaching can be delivered face-to-face by arrangement, via phone call or via online hui, depending on availability. Sessions will be strictly confidential. Ngā Maia are required to provide quantitative data and themes; however, these do not include identifiers. Our goal is to offer clinical coaching to 100-130 midwives with up to 8 sessions (1 hour each) per eligible midwife. For urgent matters (within 24 hours), please contact Tamara Karu, phone 0276353566. Square
Heather Muriwai's pōwhiri to the MOH.

Sweet Fruit of Labour
Pasifika Midwives Aotearoa was established well over a decade ago (2012) by the small number of Pacific midwives in the workforce at the time. One of the driving factors for the group’s creation was to halt the alarming attrition rates of Pacific students during their first year of the midwifery degree - hence the ‘Aunties’ mentoring was initiated.
Over the years, whilst we have celebrated the increased numbers of Pacific midwifery students in the programme, the most joyous moments have been watching the colourfully adorned graduates walk across the stage, amidst impromptu cheers from those kin they represent.
The following is the reflection of one of PMWA’s members – fruition of the group’s purpose.
‘Fakaalofa lahi atu ki mutolu oti ko e higoa haku ko Whitney Amadia, mo e ko au ko e fifine Niue Samoa fakahekeheke. Ko au ne hau mai he tau kaina ko Alofi mo Mutalau i Niue mo Safune i Samoa. Ko au ko e māmā mo e fakamālohi ke he fāmili, ko e tokoua au ke he tau fānau he hōhā e 4, ko Emma-Jade, Madison, Leilani mo Ava, mo e tāgata fakamālohi haku ko Jordan.
Greetings to everyone, my name is Whitney Amadia, and I am a proud Niue Samoa woman. I come from the villages of Alofi and Mutalau in Niue and Safune in Samoa. I am a mum to four beautiful daughters, Emma-Jade, Madison, Leilani and Ava, and partner and soon-to be wife of Jordan Slade.
My journey into midwifery began when I had my second baby, Madison Grace, in 2011. For the first time, I experienced what it was like to have the care of a Lead Maternity Carer (LMC), as with my eldest baby I had my local doctor.
In 2019, I took a significant step forward by enrolling into midwifery at Auckland University of Technology (AUT). Although returning to study after over a decade was daunting, I felt a profound sense of certainty that this was the path I was meant to follow. During my first placement, I had the honour of witnessing my first birth. In that transformative moment, immersed in the birthing experience, I knew without a doubt that I was exactly where I belonged.
During my studies at AUT, I had the incredible opportunity to represent my fellow Pasifika students as the Pasifika Student Representative. This role allowed me to be a voice for Pasifika students, advocating for their needs and ensuring our cultural perspectives were recognised and respected within the academic environment. It was a rewarding experience that deepened my commitment to supporting Pasifika communities.
Throughout the degree, there have been numerous challengesbalancing motherhood, placements and assignments, and navigating a pandemic (COVID-19). Despite these hurdles, I would not change a thing, as it was during this time that I met friends who have become family, and networked with many of my future colleagues.
While my goal in pursuing this degree was to become an LMC within the Pasifika community, I realised the importance of understanding the complexities of midwifery care. I wanted to gain the skills to identify when the normal presents with complications. After graduating from AUT, this understanding took me to Te Toka Tumai (Auckland City Hospital), where I completed the New Graduate Programme. It was here that I gained hands-on experience with complex care situations, providing a strong foundation for my midwifery practice and enhancing my ability to provide comprehensive care to māmā and whānau. Te Toka Tumai has been an incredible experience, and I am immensely grateful for the time I spent there. The insights and skills I gained were invaluable, and if I were to return to a facility, I would choose Te Toka Tumai again without hesitation. I have embarked on a new journey as an LMC at the Nga Hau Birthing Centre in Māngere. This role has been a blessing, allowing me to care for Pasifika māmā within the South Auckland community while learning and adapting to this new environment. I am deeply grateful for the support of Tyra Fitisemanu, my midwifery partner and sister, and the exceptional Southside Aiga Midwives. Their support and collaboration have been crucial during this transition. Fulfilling my goal of working within my own community, I feel privileged and honoured to walk alongside these amazing māmā and whānau. I am excited to contribute to the health and well-being of Pasifika and Māori māmā in this vibrant community.
Midwives need midwives to mentor and nurture each other throughout their entire career paths. It strengthens collegiality, provides safe spaces and sustains the profession. When this ethic is applied, it will ultimately translate to quality care for whānau Square

WHITNEY AMADIA (NAMALAU’ULU TISH TAIHIA)
Whitney with her beautiful whānau.
TE WHETŪ ORANGA: AN INTEGRATED HEALTH HUB WITH A MIDWIFERY HEART
Kahu Taurima, the joint Te Aka Whai Ora and Te Whatu Ora approach to the First 2,000 Days, has seen millions of dollars disbursed to various health organisations throughout Aotearoa over the past year. And while a number of Kahu Taurima funding recipients have sought midwifery input at various stages, one in particular has been entirely midwiferyled from the outset. Amellia Kapa shares the story of three Māori midwives in Tokoroa who’ve stopped at nothing to bring their vision to life.

AMELLIA KAPA REGISTERED MIDWIFE
Māori midwife Kimai Cure knows the town –and hāpori (community) – of Tokoroa like the back of her hand. Born and raised in the South Waikato town, Kimai’s Ngāti Raukawa whakapapa not only links her directly to the whenua, but many of the whānau living upon it.
Gaining her midwifery degree in 2014 while living in the Hawke’s Bay, Kimai practised in the region for a couple of years before the call of her papakainga became too loud to ignore, and she returned home to Tokoroa in 2017 to put her new skills to use in her own hāpori.
Upon her return, Kimai crossed paths with Tracey White (Ngāti Toa), another Māori midwife based in Tokoroa, and the following year the pair officially joined forces, forming an LMC partnership. 'One weekend we sat down and came up with a plan for Te Whetū Oranga Midwives,' Kimai explains, the name of which stemmed from a painting she had created for an assignment during her degree. Kimai had created a visual representation of the standards of practice, Tūranga Kaupapa and Te Pae Mahutonga (Mason Durie’s health framework model), and named the image Te Whetū Oranga. It seemed the perfect fit for
Above: Kimai Cure's Te Whetū Oranga.
the pair’s shared vision and model of care.
'When we first started out, we attended all of our births together, and that carried on right up until Covid-19 hit,' Kimai explains.'Then, in 2020, Jackie arrived as a student and by that time Tracey and I were getting burnt out. Covid-19 was rough and especially rurally, things were disconnected and we were having to constantly adapt our practice due to the number of emergencies we experienced over that time.'
The pair knew something needed to change, not just for themselves, but for whānau too. The arrival of Jackie Simpkins (Ngāti Rangiwewehi, Ngāti Koata) as a student was pivotal and her official addition to the practice as a registered midwife in 2021 marked the beginning of a new phase, as her own vision and tikanga aligned perfectly with Kimai and Tracey’s long-held dream.
'We could see the gaps in Tokoroa, between discharge from midwifery care and other health services,' Jackie explains. 'Our whānau were coming back to us well after being discharged from our care, saying they hadn’t been visited by Well Child, or that they didn’t have any contraception. We’d already identified those holes in the system and knew something needed to be done. We had a vision but, at that stage, we weren’t quite sure how we could achieve it.'
The first step, Jackie details, was converting the status of their practice in preparation for what was to come. 'The year I started with Te Whetū Oranga Midwives, we decided to convert our business into a company. We were already steering that way because we knew we’d need to expand if we were to offer more support to whānau. And even though we didn’t know the specifics of how we’d achieve it, we just knew we needed to start. So we created a company – that was the first step. The following year, after six months, we went from Te Whetū Oranga Midwives to Te Whetū Oranga Health.'
On a day-to-day level, everything remained the same and the three midwives continued to toil away, caring for their caseload but knowing all the while, the right opportunity would present itself. And sure enough, when they least expected it, they stumbled across a funding opportunity.
'We were doing things like driving rural whānau to Tokoroa for appointments, or putting petrol in their cars,' Jackie recalls. 'We knew that gap needed to be filled so badly. Then we found Kahu Taurima and it was exactly what we’d been looking for; a way
of wrapping all of these extra services and resources around the whānau we were caring for, but maternity based. So we went for it.'
Pulling the initial proposal together was a collective effort, Jackie and Kimai say, laughing as they reflect on their antics.
'My cousin is the ED nurse manager at Tokoroa, so I asked her to come and help us,' Kimai says. 'She came and sat with us until midnight – until we’d finished it and sent it in. A month later, we were offered an interview and got through to the next stage, which was a presentation.'
It was a lengthy process. Kimai explains the trio still needed to meet their primary responsibilities as caseloading midwives, while dedicating every other spare minute to ensuring they presented a worthy case. 'All throughout the process we were still working as midwives, so in some instances we’d been up all night birthing, hadn’t had any sleep, and had to front up for meetings so that we could get it over the line. We were running on empty. Then on the 2nd of June, we found out we’d got the funding.'
The next challenge, the pair explain, was asking people – mostly whānau – to work for free while they waited for the funds to be disbursed. 'We had to make a start before we’d actually received the funds,' Jackie explains. 'So we found people to work for us for free and we funded the rest of it ourselves for the first few months. But they were our whānau, and that’s the Māori model, so they did it willingly,' she adds proudly.
'We got up and running in November 2023,' Jackie recalls. 'We had to move to new premises because our old space was too small, and we’ve already outgrown it. We have a Well Child nurse, a social worker, we contract a counsellor and we now have a general manager as well as an administrator who also does our PR. Our GM and administrator both worked for free in those early months, and their skillsets are amazing. We didn’t know how to set up job descriptions, for example, but they took those things off our plate.'
The organisation has gone from strength to strength, as Jackie illustrates. 'This year we got cold-chain accredited for immunisations and now we have an immunisations contract, supported by South Waikato Pacific Islands Community Services (SWPICS). We’ve also employed a Clinical Nurse Lead, who still works as an ED nurse manager. We realised we didn’t understand nursing and knew that aspect
One of our greatest success stories is our Well Child programme. When our nurse goes to her training sessions, the other nurses are in awe; she’s almost ready to close her books and that’s because it’s so seamlessly integrated.

of the service was going to grow, so we needed to bring someone on board with that expertise.'
And that’s not all. The list of services available to whānau is extensive, just as the midwives had always envisaged. 'We have hapū wānanga, Wai Ū breastfeeding support that includes a Pasifika lactation consultant, and Pēpi and You, which is a fourth trimester programme. We also serve as a drop-in centre; we have breast pumps for hire and we always have free stuff at the front for whānau to take. The other thing is transport; we can organise transport for women who can’t get to scans or appointments. So that bridges another gap.'
A bustling hub, Te Whetū Oranga Health has been well received by the community and engagement is at an all-time high, Jackie demonstrates. 'One of our greatest success stories is our Well Child programme. When our nurse goes to her training sessions, the other nurses are in awe; she’s almost ready to close her books and that’s because it’s so seamlessly integrated. The women come in for their antenatal appointments with us, then the Well Child nurse pops in to meet them. So that whakawhānaungatanga starts in pregnancy, before that pēpē is even born.'
Jackie Simpkins, Tracey White and Kimai Cure.
The convenience of having multiple needs addressed in the same appointment removes yet more barriers for whānau. 'It’s become a one-stop shop,' Jackie explains. 'If a woman says they haven’t had something like the pertussis vaccination, I pop out and find a nurse who can talk to them about it while we’ve got them there and we get it booked in.'
Having a strong midwifery core is what makes Te Whetū Oranga Health so unique, Kimai explains. 'I think that’s our point of difference; this all started with midwives. Being so intimately involved with whānau and holistic in our view means we’ve always been able to see what’s been missing. Our own midwifery work is still funded by Section 94, just like any other midwifery practice. But the Kahu Taurima funding covers everything else that surrounds the core of midwifery care. And it’s important to make that distinction; the midwifery team is at the centre, and everything else wraps around it, not the other way around,' she emphasises. Being so well integrated in their community is another reason why whānau are consistently engaging with services, Kimai explains. 'We’ve
been established here in this community for 13 years. There’s a real sense of partnership and trust, so when we embarked on this journey, our hāpori followed.'
Another success story could have ended very differently but Kimai and Jackie point to the power of an integrated approach.
'A young 17-year-old client of ours came to us in a psychotic state, which was druginduced,' Kimai begins, 'and we needed to care for her antenatally. We were so out of our depth but, in addition to the other referrals, we got our social worker and counsellor on board to support her. The social worker went and worked with her whānau, discussing why she needed to be on medication, sharing more information so that they understood the rationale and what support she needed to keep her and baby safe. And then together we all made a collaborative plan for her postnatal care. That young woman came out of the psychosis and is no longer on drugs. I was so terrified she might take her life during that pregnancy but, with an integrated approach and by involving the whānau in her care, a tragedy was avoided.'

Come join us!
Are you a skilled midwife looking to make a meaningful impact in the lives of whānau?
We’ve got exciting opportunities in our midwifery-led, stand-alone birth unit, and postnatal facility in Parnell, Auckland. At Birthcare we provide a supportive environment where your expertise is valued, and quality care is our focus.
Take the next step in your career with us.
The stories are countless, with Jackie recalling another scenario the team have faced many times over, which can now be remedied quickly and easily. 'We had another woman who came to us around 20 weeks pregnant, who hadn’t had a dating scan because they didn’t have enough money for groceries, let alone petrol to get to scans or appointments. We did a grocery shop and took the kai straight over to her home. We can now fix these issues immediately and connect women in these situations with a social worker to address the underlying issues and help lift these whānau up.'
Like most significant journeys, it’s been multi-faceted and Kimai describes just how personal it’s been at times. 'I’ve always struggled with whether I’m a Māori midwife, or a midwife who’s Māori. And now I know, I’m a Māori midwife. As a Māori midwife, you can connect with whānau in a really different way, because if you can make a whānau feel safe, they’ll open up. And we find that they do, all the time.'
Jackie agrees, demonstrating once again the importance of whānaungatanga and how midwifery care leads to meaningful connections. 'The biggest joy I get is birthing multiple generations within the same whānau. The trust is already established and when you visit their homes, their kids call you ‘Aunty’ or ‘Nanny’. There’s whakapapa between us, so they’re more like whānau, but a professional whānau.'
Initially awarded a 12-month contract, Te Whetū Oranga Health has since been approved a further year of Kahu Taurima funding, taking them through to 2025. But these highly motivated midwives aren’t resting on their laurels; there’s more to come, they say. 'Next on the agenda is sexual health, contraception and GPs. We’ve also got a physiotherapist who wants to work with us, and kairongoā (traditional Māori health practitioners) are in the pipeline,' Kimai explains.
Kimai is clear, there has been a personal cost attached to their achievements but she wouldn’t have it any other way. 'We love it. We’re burnt out, but we love South Waikato, we love rural midwifery and we really love each other. It’s been a hard year trying to navigate it all but it’s bigger than us.'
Jackie echoes the sentiment. 'We’ve all had moments of feeling exhausted and wanting to quit, but it’s beyond us and we all see that bigger picture.'
Expanding their team to five midwives next year will hopefully bring some relief and a semblance of work-life balance, which Kimai and Jackie both believe lies in collective approaches to care. 'No-one’s going to save us,' Jackie says,'so we need to figure out how to save ourselves, which we believe can only be done by a team approach.'
Kimai’s parting words leave a lasting impression. 'I’ve got two mokopuna, aged five and seven, and they say, ‘When I grow up, I want to be a midwife like my Nan’, so I want to make the future of our profession better for them, so that it can be sustainable and fulfilling.' Square

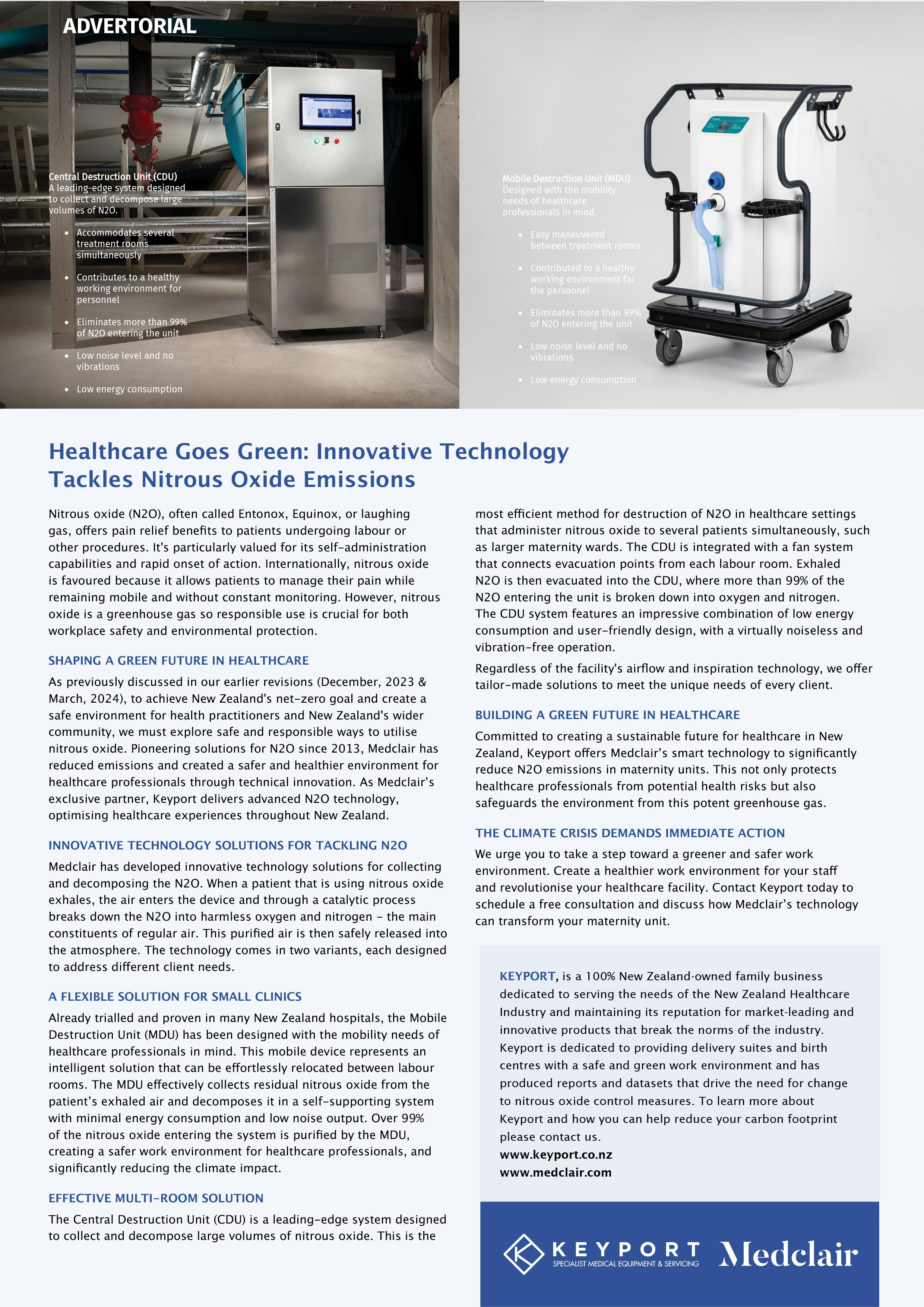

Left: Amy Carter with two newborns.
MIDWIVES WORKING OVERSEAS
Taking up an opportunity to work overseas is something many midwives consider doing at some stage in their career. The College has recently spoken with two midwives who have undertaken overseas missions with Médecins Sans Frontières. This type of work often involves travelling to countries where health systems are under significant strain and other factors, such as conflict and disease, impact on wellbeing. Providing midwifery care in these situations is vastly different to working in Aotearoa and midwives must adjust to the context and resourcing available to them. Overseas work can be both stressful and rewarding for midwives, and as you will see from the stories shared with us the experience has a profound impact. Sincere thanks to Amy and Linley for sharing their amazing stories with us.

amy carter - yemen, an adventurous soul
Midwife Amy Carter is currently working with Médecins Sans Frontières in Yemen, a country at war and facing ongoing threat of attack and destruction. Her journey to where she is today has been one of adventure and exploration. After moving to New Zealand from her home country of Ireland in 2011, Amy worked for seven years in Hawke’s Bay, providing complex midwifery care and working as a flight midwife. She then travelled to Qatar on a one-year sabbatical that turned into three years as she enjoyed the experience of working there despite the significant culture shock. Returning to Aotearoa in 2020, Amy worked in Auckland for a year, before joining the Fetal Maternal Medicine team, focusing on the provision of abortion care and contraceptive services. However, her itchy feet again led her to explore overseas opportunities. Applying to Médecins Sans Frontières (MSF) in June 2023, she underwent a rigorous recruitment process including a three hour interview, lots of paperwork, and finally approval to join. She then had
to wait six months for a mission to come up and, when it did it took another eight weeks to complete preparations that included applying for visas, permits and receiving numerous vaccinations and malaria shots.
YEMEN
Yemen’s civil war began in 2014 and continues today. The conflict has taken a heavy toll on civilians, making Yemen the world’s worst humanitarian crisis. The United Nations estimates that:
• 60% of the estimated 377,000 deaths in Yemen between 2015 and the beginning of 2022 were the result of indirect causes like food insecurity and lack of accessible health services.
• Two-thirds of the population (21.6 million Yemenis, including 11 million children) remain in dire need of assistance.
• 4.5 million people have been displaced.
• 5 million are at risk of famine.
• A cholera outbreak has affected over one million people.
• All sides of the conflict are reported to have violated human rights and international humanitarian law.
ARRIVING IN YEMEN
Amy was deployed to work in a remote rural village as a midwifery manager within a multidisciplinary MSF team. The hospital she works in was rebuilt by MSF in 2015 after being destroyed by bombing. Speaking very little Arabic, Amy has found communication to be a major challenge. General practitioners and paediatricians usually speak English, and at times there is a translator available that Amy can work with but, otherwise, she has had to find other effective ways of communicating with women and local midwives. The women’s department of the hospital is responsible for women’s health and paediatric cases and the scope of emergency care is limited. The nearest specialist service for referrals is 1.5 hours away. Local midwives are skilled breech birth practitioners as caesarean section is rarely available.
Caesarean section is reserved for life preserving cases only, and only after first gaining consent from the woman’s husband, then the Ministry of Health, and finally the hospital director. Requests are usually declined. There are no obstetricians at this hospital, and on the rare occasion that a caesarean section is approved, it is performed by a general surgeon.
Amy was deployed to work in a remote rural village as a midwifery manager within a multidisciplinary MSF team. The hospital she works in was rebuilt by MSF in 2015 after being destroyed by bombing. Speaking very little Arabic, Amy has found communication to be a major challenge. General practitioners and paediatricians usually speak English, and at times there is a translator available that Amy can work with but, otherwise, she has had to find other effective ways of communicating with women and local midwives.
THE REALITIES OF BIRTH AND DEATH IN YEMEN
During her time in Yemen Amy has witnessed frequent maternal and perinatal deaths. Many women have no antenatal care at all and are seen for the first time during or after their labour. Some birth at home and then come to the hospital having suffered a catastrophic postpartum haemorrhage – often the medical team cannot save their lives at that point. Amy recalls one woman arriving at the hospital (following the birth of her 10th baby) with a haemoglobin of 1 and no signs of life. Sadly, resuscitation efforts were unsuccessful, and they could not save the mother. Many babies also don’t survive birth, and when this happens the baby is wrapped in a towel and taken home by the family. There are no mementos taken for the parents, and no official processes in relation to the death.
The birthing room has two beds with a curtain between. Minimal equipment is available in the hospital; the midwives have two Dopplers to use for monitoring fetal wellbeing in labour, and not much else, and there is no analgesia available for women giving birth. There are no incubators in the hospital and no specialist neonatal care equipment. Cholera is prevalent and has to be diagnosed by a stool test, processed on admission. Laboratory services are patchy and of low quality and, if women test positive for cholera, they have to give birth in a tent outside the building.
MIDWIFERY IN YEMEN
Amy has learned a lot from the Yemeni midwives and has been impressed with their skills for coping with challenging clinical situations. There is not much they haven’t seen, and they have had to become resilient to the high rate of perinatal mortality and lack of sufficient resourcing.
Women have minimal antenatal care and chronic malnutrition, 67% of pregnant women in Yemen are malnourished. The World Food Programme were providing support to improve the health of mothers but have pulled out of the country due to ongoing safety concerns.
‘NO FREEDOM HERE’
Women in Yemen have a female caretaker who accompanies them everywhere – they are never on their own. The lack of choice and consent is the biggest difference Amy has noticed, and something that never sits
comfortably with her. Contraception and termination of pregnancy are not allowed, and the authorities are controlling and autocratic. It is in this context of a highly charged political environment that Amy must balance the needs of women with the realities of her situation. Women sometimes ask her to provide contraceptive services or abortion care, but this must be handled very discreetly as she cannot trust that other hospital staff won’t tell the hospital director.
ISOLATION
The village where Amy lives and works is an eight-hour drive from Sana’a (the capital), so although they can, in theory, leave at any time, the reality of making the trip is complicated. Communication networks can be patchy and internet service tends to cut out during storms. The speed of the internet is very slow so sharing photos and videos is not always possible. Sometimes there is no hot water or electricity. Each team member travels to Sana’a for a break every six weeks but missile attacks are frequent there, as it is the central conflict zone. It is during these six-weekly breaks that Amy usually contacts her family and updates them on her wellbeing.
POLITICAL ENVIRONMENT AND RISK
Due to the state of war in Yemen there is a significant mistrust of foreigners, and fair-skinned people are often assumed to be American. Each day a call to prayer goes out through the town and the messaging broadcast via the loudspeakers includes antiAmerican and anti-Semitic sentiments.
In June 2024 authorities arrested over 30 UN and MSF workers and accused these people of spying and espionage. The outlook is not positive for these captives and their arrest has been kept quiet by the media.
LIVING CONDITIONS
The MSF workers must walk in pairs to and from their shifts at the hospital, and everyone is subject to a strict 6pm curfew. Within the multi-disciplinary team Amy works in, there is a paediatrician, a physiotherapist, a logistics specialist, a human resources member and a co-ordinator. The team all live together in a shared house and have a cook who provides their meals. The camaraderie and shared experience of the team has been one of the highlights for Amy, and she has enjoyed meeting people from other parts of the world who have a similar desire to help where their skills are useful.
WORKING FOR MSF
MSF team members are paid a weekly rate for their services and flights and accommodation costs are covered. Workers have one twoweek holiday during their mission and can choose from six countries to be flown to for a break – Amy chose to go to Greece. The MSF organisation has a legal team which provides indemnity cover and also offers counselling and debriefing services for team members during and after their mission.
ADVICE TO OTHER MIDWIVES
Despite the extreme conditions and adversity, Amy has found it to be a powerful experience and would consider volunteering again in the future. Her advice to other midwives considering humanitarian work is to think seriously about what you will experience when you go on a mission. She advises there will be things you can’t unsee and things you can’t forget.
Talking with other midwives who have done this work is hugely valuable when considering your own path, as is having a good amount of practice experience under your belt, strong support networks and confidence in your own leadership skills. Being able to speak French or Arabic is also very helpful. Square
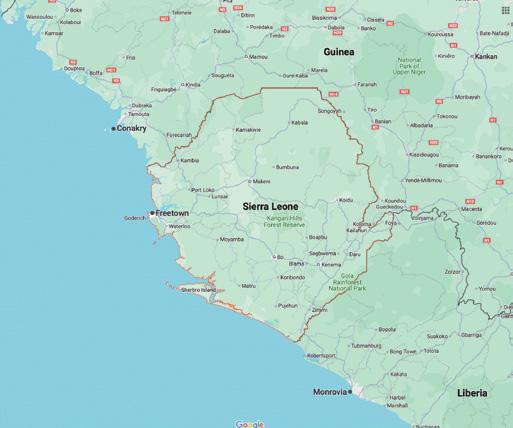
linley taylorsierra leone, fulfilling a lifelong goal
Linley Taylor has wanted to undertake humanitarian work since she was a teenager. With this goal in mind she first undertook a nursing degree, then, realising her heart lay with midwifery, she completed a midwifery degree as well.
Linley researched the various organisations that run humanitarian missions and decided on Médecins Sans Frontières (MSF), particularly because of their principles and the support offered to their teams. She says that after applying to join a mission with MSF, you have an interview and then, once accepted, there is generally a period of waiting for an opportunity to come up, so you need to have some flexibility in when you can leave. For Linley, this meant winding down her LMC caseload and making arrangements for her house while she was away.
She says you also need to be flexible about where you go. MSF workers can determine the countries which they are not willing to travel to but, other than that, you don’t get to choose your location. She adds that speaking French or another language is a big advantage as in many MSF destinations English is not the first language.
Prior to her departure, Linley had to complete a lot of paperwork, find a travel GP (which was tough) and be vaccinated against a wide range of diseases (this cost $1200, which was later reimbursed by MSF). She advises starting the vaccination process early as it takes some time to have all the required shots. Finally, she flew out to Sierra Leone in June 2023 to undertake her four-month mission.
SIERRA LEONE
Disease outbreaks – including of Ebola, COVID-19 and Lassa fever – and years of civil war have devastated the healthcare system in Sierra Leone, leaving it severely understaffed. Child and maternal death rates are exceptionally high, so humanitarian activities focus on children under five, pregnant women and lactating mothers, especially in Kenema in the country’s east where Linley was based. Across all age groups, malaria is the country’s single biggest killer and accounts for 38% of hospital admissions. Children and pregnant women are particularly vulnerable to malaria.
FITTING IN
Arriving in Sierra Leone, Linley’s first challenges were facing the massive context shift and learning how to become accepted in a foreign environment. Language was a significant barrier and, before she could do anything else, it was crucial to develop relationships and build a team atmosphere. It took about six weeks to be able to communicate well, with Linley having to adjust her speech, which caused her to sound slow and robotic (the Kiwi accent was particularly hard for people to understand).
The first part of the mission was the hardest as she was treated with some suspicion and wonder as to how she had such a high level of clinical knowledge and adept critical thinking in comparison to her African colleagues. She credits the New Zealand midwifery education and model of care.
‘EXTREME STUFF EVERY DAY’
Confronting Linley almost immediately was a steady stream of major emergency situations. Many women in Sierra Leone
have anaemia due to malaria, contributing to a high incidence of postpartum haemorrhage. She saw severe postpartum haemorrhages every day and found it distressing to realise that these were often preventable with critical thinking. Newborn resuscitation skills were also sorely lacking. Linley found it hard to watch aggressive suctioning of newborns, incorrect airway positioning, and a lack of use of oxygen when it was clinically required. She herself was not permitted to perform cardiac compressions on babies who required it. There was no CPAP available in the hospital, just nasal prong oxygen.
Linley saw so many extreme clinical situations that she had to be realistic about what could be achieved. These experiences took a lot of time and debriefing for her to process. Linley witnessed and was directly involved in resolving cord prolapses, eclampsia and dissemination intravascular coagulopathy, plus all of the women giving birth had been subjected to female genital mutilation when they were young girls. This resulted in bilateral episiotomy being performed and numerous cervical tears due to the common practice of applying fundal pressure to expedite the birth of the baby. One woman was nearly sent home with an unrepaired fourth degree tear and no pain relief from a birth overnight. Upon arrival in the morning Linley found her sitting in a pool of blood, yet another PPH. It was used as a learning opportunity with the local midwives to use critical thinking on the 4 Ts, use pain relief and discover why. Once stabilised she was sent to OT where it took the obstetrician 2.5 hours to repair it.
DIFFERENCES IN TRAINING
Local MSF-trained midwives in Sierra Leone have 18 months of theory-based training in Ghana and have a significantly different skill set compared to NZ-trained midwives. There is no medical training in Sierra Leone, rather there are Community Health Officers (CHOs) who are generally very young (mid-20s) and, although they are given high status, their skills are not welldeveloped. Linley quickly realised she was much more highly trained than most of the local health workers, which caused some degree of suspicion and mistrust in the initial stages. She was able to perform newborn resuscitation, treat postpartum haemorrhage, know what drugs to prescribe, diagnose and complete perineal repair work, and have knowledge and skill in emergencies.

There was a sense that she was acting like a doctor rather than a midwife. It was a big realisation for Linley to appreciate the very high level of competency our system provides compared to some other countries.
THE BODY KEEPS SCORE
Linley had to take anti-malaria medication throughout her time in Sierra Leone, and dietary changes also took a toll. She lost 10kg in weight and half her hair fell out.
CULTURAL DIFFERENCES
Food was a challenge at times for Linley. Although there was a cooked meal available twice a day, she found the local meat unpalatable. A big luxury for Linley was to buy some food from the supermarket. The supermarkets there are owned by rich Lebanese families, and the food is
exorbitantly priced (mostly because foreign NGO workers can afford to pay for it, but the side effect is that local people can’t). One day Linley and her teammates splashed out and bought ingredients for a full roast chicken (imported!) and vegetable dinner. She would often make home-made pizza from scratch with her Norwegian colleague and the Lebanese morning espresso (infused with cardamon) was a definite highlight.
Linley was struck by the strong sense of community amongst the Sierra Leone people, and the religious harmony across different faiths. She learned a lot about Muslim culture while there. She also recognised that our mental health and wellbeing in Aotearoa is very poor in comparison, and the concept of being ‘traumatised’ by a birth experience is not in the social consciousness there. This
is despite the fact that on her arrival it was common practice for midwives to yell at women while they were giving birth, slap the woman’s legs open, and ‘yank’ the baby out. Linley did have success in gently encouraging the midwives to use alternative techniques to support women, and also in encouraging informed consent.
‘CRAZY AND AMAZING’
Linley says that she would do it all again and may volunteer for another mission in the future. Her time in Sierra Leone was ‘crazy and amazing’ and gave her a totally new perspective on our midwifery model of care and our well-resourced, generally healthy birthing population. Having seen the reality of poor population health, chronic disease and an under-resourced, under-trained health system, she realises how lucky we are.
In Sierra Leone there is a common saying that ‘the first baby belongs to death’ because it is very common for a first-born child to die during birth. If a first-born baby does survive it is seen as a miracle. Linley experienced this when supporting one family with the birth of their first baby – the sheer joy and celebration in the room was infectious, and all the women in the family were dancing around and singing when they saw the mother and baby come out of the delivery room alive. Women birthed without support people, who waited outside, sometimes for days, and slept on cardboard.
MSF EXPERIENCE
Linley felt a strong sense of camaraderie with her mission teammates and bonded with them during their time together. She felt so fortunate to work with the one or two obstetricians based there, as they understood and shared a similar knowledge base and critical thinking skill set.
ADVICE TO OTHER MIDWIVES
Linley’s advice is to be really sure about why you want to do this type of work. She says, ‘it will challenge you in areas unrealised’ and ‘you can’t unsee what you see’, so strong support networks are needed to help process the experiences. Having varied life experiences and a good amount of practice experience in NZ (at least five years) is recommended, as is having a broad range of practice experience –she says being an LMC was helpful as she was used to practising autonomously and trusting her own judgement. ‘You’ll find yourself in situations where you are the most experienced and you have to be ready to embrace the fear and go for it,’ she says. Square
Linley Taylor and her team mates.



TRUSTED • SAFE • UNIQUE
EPI-NO is clinically proven to of an intact per ineum, reduce episiotomy, and is safe to use
EPI-NO is a dual pur pose CE approved medical device designed muscles from ear ly in pregnancy, and again postpar tum The per ineal stretching exercises commence concur rently after Week 36.
EPI-NO Childbir th Tr aining has been accepted in Austr alia & New Zealand for over 15 year s as an effective prepar ation for women choosing a natur al vaginal bir th
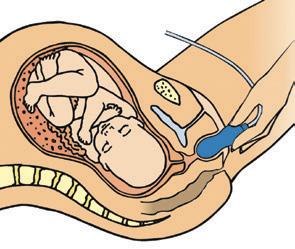
Over 65,000 EPI-NO births in Austr alia and New Zealand. Available in over 20 countr ies wor ldwide www.starnbergmed.co.nz


More restful, safer sleep and helps prevent flat head
• More restful, safer sleep limb and hip movement
• Ensures swaddling, sleepwear, Sleepingbag use is safer and cosier
Goes over any type of swaddling, sleeping bag or sleepwear, for a snug and more restful sleep Natural, flexible body, limb and hip movement Comfort and safety for babies newborn-2 years
• Excellent for babies requiring varied sleep positions or cot elevation
Helps keep young babies comfortably o the tummy; older babies turn freely within the wrap

Available online with shipment from Auckland and at selected phar macies.
EPI-NO Patient Brochures can be requested for New Zealand via info@starnbergmed.co.nz Germany
‘The human body performs to maximum trained and prepared. Childbir th is no exception ’ Dr Wilhelm Hor kel, Star nberg (EPI-NO inventor)




TE PAEA BRADSHAW MAORI MIDWIFERY ADVISOR
'Kaupapa driven, Wairua led' Supporting Māori birthing practices
The benefits of innovative Kaupapa Māori frameworks, and targeted initiatives to improve health equity between Te Tiriti o Waitangi partners, have been well researched over the last three decades. Concurrently, with the revitalisation of Te Reo me ona Tikanga (The Māori language and the correct way of doing things), there has been a surge of Mātauranga Māori (Māori knowledge bases) published, as the indigenous people of Aotearoa attempt to reclaim traditional practices within spaces where colonisation has been thriving. Midwifery is one of these spaces.
One way of growing and/or disseminating knowledge is to hold hui or wānanga. The inaugural Global Indigenous Midwives Hui was held in January 2024, hosted by the haukāinga of Hinetemoa Marae in Waimārama, Hawke's Bay. Whilst there, I had the opportunity to interview a handful of the Māori midwives. Three simple questions were asked: How do you know about traditional Māori birthing practices? Why are these important? Are there things that either help or hinder your ability as a midwife to support these?
This article does not intend to educate about specific traditional practices but rather how one may begin to learn, understand and support them.
HOW DO YOU KNOW ABOUT TRADITIONAL MĀORI BIRTHING PRACTICES?
Some explained that they ‘grew up with whānau who were either doing it, discussing it or learning about it’. The teaching was often informal and ‘just being discussed by Kuia and Kaumatua (Māori elders)’. The midwives agreed that ‘working with other Māori midwives’ helped them to gain knowledge, as they would freely share between themselves what they knew.
All participants agreed that reading research completed by Māori authors was highly valued and understood to be a useful tool. One participant stated, ‘even if it was from other rohe (regions), seeing how they do things, those talks and readings inspire you, you feel it, he oranga ngākau, he hikina wairua (rejuvenating on a physical and spiritual sense)’. This participant went on further to suggest that ‘we will get that this weekend at this hui, when your heart feels good, it’s inspiring, living, sharing and breathing it (the Kaupapa)’.
With that said, attending any hui ā Māori (Māori gatherings) such as Wānanga Hapūtanga (kaupapa Māori pregnancy & parenting programme), kura reo (conference to speak and learn Māori) or indigenous research forums, such as the one held at Waimārama, was also described as being helpful. Books, writings or presentations by Ngahuia Murphy, Naomi Simmonds or Kelly Tikao come highly recommended by the participants.
WHY ARE MĀORI BIRTHING PRACTICES IMPORTANT?
They were described as being important because they ‘connect you to whenua (land), our culture, and taonga tuku iho (treasured
knowledge consciously handed down through the generations)’. Midwives interviewed felt a responsibility to their whānau and hapori (community) to learn about these practices or at the very least to hold the space to allow whānau to incorporate what they knew. Knowledge that has survived the onslaught of colonisation, and resurfaced through meticulous research, has been found through kōrero (talks), waiata (songs), haka, moteatea (traditional chant) and carvings.
There was a unanimous sense of duty to ensure mātauranga Māori will not perish, ‘it’s like the reo, if we don’t value it and use it, it will die; our role is to keep enabling & supporting these practices’. Most of the midwives agreed that the Māori community are hungry for these tikanga (practices). The midwives are getting asked more and more by the whānau they care for to incorporate these practices that are uniquely Māori, ‘especially now as the Kōhanga (Māori immersion preschool), Kura Kaupapa (Māori immersion primary/intermediate school), and Wharekura (Māori immersion high school) generation of our people are at the age of having babies’.
This new generation has grown up immersed in Te Reo Māori, and within the language are Māori values and Māori ways of doing things
to ensure that the potential of Te Ao Māori (Māori world, including the environment, people, animals, language and culture) is met. Unsurprisingly, this is flowing into all facets of life, including the maternity realm.
ARE THERE THINGS THAT HELP OR HINDER YOUR ABILITY AS A MIDWIFE TO SUPPORT MĀORI BIRTHING PRACTICES?
It was felt that ‘being a rōpū’ helps, whether it’s your direct practice group, affiliations to Ngā Maia, or other regional Māori midwifery groups: ‘helping each other and sticking together’ and having a place to have ‘safe, non-judgemental conversations about our mahi (work)’. Tūranga Kaupapa has helped acknowledge that as Māori we consider different aspects of our midwifery provision to be valuable.
Wānanga Hapūtanga was also identified to be helpful, as the knowledge is being shared and whānau feel confident to use what they know. One midwife explained that the muka ties (a Māori alternative to plastic cord clamps)
she is seeing appears to be better quality compared to previous years. ‘The whānau have been taught how to harvest it, how to prepare it, and come out that day with one that has been made properly, so it becomes normal’. There are also places like Te Wānanga o Aotearoa and others around, that have free raranga (weaving) courses, ‘you have to go out and learn it, learn one, make one, teach one’.
Politics, policies and the environment were hindering factors. Facilities or people that don’t understand what we’re doing, ‘and sometimes I don’t want to, or don’t have the energy to, explain it’. A midwife gave the example of when she first starting using muka ties, ‘initially I just did it at homes, it was easier, no need to justify to anyone what we were doing’. There was a general sense that people or places are fearful of practices that are not mainstream or that ‘written policies don’t allow’. A contentious example shared was, how ‘the number of support people allowed in labour used to be dictated by the units’.
Some midwives shared that its not always tauiwi (non-Māori) who make it difficult to
incorporate Māori birthing practices ‘but sometimes it’s our own’, and the reason for this appears to be that ‘yeah they might have whakapapa Māori (Māori genealogy), but they’re too colonised’ Another midwife shared her sense of burden, that ‘I’m tired, I’m burnt out, but I can’t stop. I work hard for my clients because I know they won’t be supported and welcomed by others (staff and systems)’.
It is clear, the lived experience of tikanga (correct way of doing things) is slightly different for all. But for these Māori midwives it was central to their moral compass. Enabling and supporting Māori birthing practices is part of their duty as a Māori midwife. It is not a competency or standard that one must adhere to, but rather it exemplifies their proud connection, understanding and commitment to their environment, their people and their culture.
The role of a Māori midwife is 'Kaupapa driven, and Wairua led' (Whaea Crete Cherrington/Koha Aperahama). Square


CLAIRE MACDONALD MIDWIFERY ADVISOR
16TH PMMRC REPORT RELEASED
He matenga ohorere, he wairua uiui, wairua mutunga-kore.
The grief of a sudden, untimely death will never be forgotten (PMMRC, 2024).
The 16th report of the Perinatal and Maternal Mortality Review Committee (PMMRC) | te Komiti Arotake Mate Pēpi, Mate Whaea Hoki, reporting mortality data from 2021, is the last report under the longstanding Committee structure.
Following then-Minister of Health Andrew Little’s review of the national mortality review function, the governance of national perinatal and maternal mortality (PMM) data shifted to the new National Mortality Review Committee (NMRC) from July 2023 and PMMRC members were renamed subject matter experts (SME). SMEs were contracted to continue in their roles for one more year after this shift, to complete the 16th report. Due to delays that occurred during the transition process, this report is shorter and later to be published than previous reports.
PMMRC reports include descriptive data and commentary about perinatal related mortality (stillbirths, terminations of pregnancy and neonatal deaths of babies from 20 weeks’ gestation to 28 days after birth), neonatal encephalopathy (babies born ≥35 weeks) and maternal mortality (the death of a woman/ person while pregnant or within 42 days of the end of pregnancy).
The production of a PMMRC report is a collective effort from midwives, obstetricians, neonatologists, paediatricians, and neonatal nurses who care for bereaved whānau and carefully enter their data into the dataset. In addition to supporting bereaved whānau, local co-ordinators often play a key role in local mortality review and in ensuring the data is complete. The national co-ordinator oversees
data quality and provides education for local coordinators, while Te Tāhū Hauora | Health Quality and Safety Commission (HQSC) senior specialist advisor co-ordinates the SMEs and the report’s production.
Data scientists, clinicians, hauora Māori experts and consumers review the data in the Committee/SME group, identifying modifiable risks and system factors to inform recommendations to the sector and government, with the aim of effecting positive change. The report is peer reviewed by epidemiology and sector experts.
The PMMRC reports are upheld internationally as being of high standard, with robust data collection, analysis and reporting. Statutory confidentiality and data collection provisions mean that we can be confident the reports contain as full and high quality a dataset as possible. This is particularly important when considering adverse and relatively rare outcomes like PMM, as small errors can make a major difference to results.
Since their first publication in 2007, PMMRC reports have been an integral element of the midwifery information landscape, informing undergraduate, continuing and postgraduate education; the Midwifery First Year of Practice programme; College guidance; strategic planning; and advocacy work to improve services for whānau who access maternity services.
PMM data governance also includes considering and approving data access requests by researchers, who can investigate and contribute to the evidence about where interventions to reduce mortality may be most effective.
FINDINGS
FROM THE 16TH REPORT AND OVERALL REPORTING
SERIES
The report opens with karakia and mihi, and acknowledges that each data point represents the death of a whānau member. A content warning is included to explain that the report may be distressing and challenging; the same applies to this article as findings are discussed. High level findings are summarised here, and midwives are encouraged to read the full report which includes detailed analyses of PMM by population group and cause: https://www. hqsc.govt.nz/assets/Our-work/Mortalityreview-committee/PMMRC/Publicationsresources/16thPMMRCReport_FINAL.pdf.
WHAT HAS CHANGED?
Some improvements have been made over the years of data collection. A reduction in stillbirth occurred early in the reporting series, decreasing from pre-2009 rates and remaining relatively consistent since 2010. There has been a small downwards trend in neonatal mortality for extremely premature babies born before 28 weeks, which the 16th report notes may have been influenced by improved care and technology and 2019 guidance on periviability.
The greatest proportional change has been in direct maternal mortality, due to a reduction in obstetric-related causes like amniotic fluid embolism (AFE), which the 16th report notes is now an incredibly rare event. In the 9th report, it was recognised that Aotearoa had a 5-fold higher AFE death rate than the UK, which signposted an area for change and
improvement in clinical management. To come to a detailed understanding of the situation in Aotearoa, the then-PMMRC undertook an indepth analysis of AFE cases in the 10th report. Practice points on AFE were included in the 10th and 11th reports, presented at the PMMRC conference, and education was rolled out around the motu. The overall downward trend in direct maternal mortality has continued since then, suggesting that the PMMRC programme may have contributed to women’s lives being saved.
Overall termination of pregnancy (ToP) rates (≥20 weeks) have increased since 2020, when the law changed, attributable mainly to an increase in ToP for maternal conditions. The report notes, 'the proportion of terminations at >20 weeks’ gestation in Aotearoa was <1% in 2021, which is lower than the 1-2% reported in other countries where abortion is available as a health care procedure, such as Sweden and the UK' (p. 19). This suggests a possibility that the rate could increase further in coming years. Congenital anomalies were the most frequent cause of perinatal related mortality in the decade to 2021, and those pregnancies mostly ended by ToP.
There was some evidence of a small increase in NE in the last three reporting periods, which is a shift from the apparent downward trend from 2010 to 2018. Although the report asks whether this reflects a true increase or improved diagnosis since the 2019 national NE consensus statement was implemented, one of the hallmarks of the PMMRC reports has always been high case ascertainment. The possibility that it could be a true increase warrants further investigation, closer monitoring and an understanding of what has happened since 2021 when the most recent data was published.
WHAT HAS NOT CHANGED?
While there has been year-to-year variation in morbidity and mortality measures, many of the trends in the reported adverse outcomes and their causes demonstrate no change over the years of reporting. This is most evident when considering inequities. The fact that the ongoing burden of higher rates of adverse outcomes continues to be borne by Māori, Pasifika and Indian whānau led to a wero | challenge being laid down by the PMMRC in the 14th report, to implement the outstanding PMMRC recommendations from the reporting series; more than half still require action.
For perinatal related mortality in 2021, when compared with wāhine Māori as the reference group (RR 1.0), higher rates were experienced by Indian (RR 1.35, 95% CI 1.22–1.48) and Pacific
peoples (RR 1.18, 95% CI 1.08-1.22); with lower rates for Other European (RR 0.58, 95% CI 0.52–0.65) and Other Asian women/people (RR 0.80, 95% CI 0.73-0.88); whereas NZ Europeans experienced a similar rate (RR 0.99, 95% CI 0.93-1.05). Differences between NZ Europeans and Māori were evident in mortality type; although stillbirth rates were reasonably similar, neonatal death rates were higher for Māori, while ToP rates were higher for NZ Europeans. The 16th report also provides an indication of how the inequities by ethnic group differ according to gestation at birth.
Women/people aged <20 or >40 years old experienced more baby loss than those aged 25-34. Those living in areas of high deprivation experienced more loss than those in wealthier quintiles, driven particularly by much higher rates of preterm labour/preterm rupture of membranes (which could therefore be a key area for preventive measures).
Although a rare event, the starkest inequities were evident in maternal mortality with all other ethnic groups experiencing lower rates than Māori and Pacific women/people. Suicide tragically remained the leading cause of direct maternal death, and affected wāhine Māori more than any other group.
Neonatal encephalopathy (NE) rates and cooling treatment did not differ significantly by maternal prioritised ethnic group and there is still room for improvement in the use of cooling treatment for babies with NE. Action is needed to address the inequities in MRI investigation before discharge for Māori babies compared with all other ethnicities.
WHY DO WE NEED SURVEILLANCE DATA?
Health inequities represent a breach of the Crown’s obligations under Te Tiriti o Waitangi. Health equity needs to be a focus across the Government’s policy programme from macroeconomic, social and public policies, to the structures it funds like education, housing and, of course, health. The health system is one of the key determinants of health, so all health professionals have a responsibility to ensure care is culturally safe, accessible, acceptable and evidence-informed: we are all part of the solution when we work in a Tiriti-honouring way. Surveillance data fulfil several key functions within maternity and the wider health system. At a foundational level, mortality and morbidity are baseline indicators for the function of not only our health services, but also our social services and wider government policy settings as they affect the social determinants of health. Reporting the data provides transparency for
both clinicians and the public. And surveillance data is hypothesis-generating, providing the questions for epidemiologists, case reviewers and researchers to investigate to support improvements in care, processes and systems (as demonstrated in the case of AFE).
Intelligence from data collection and reporting makes an important contribution to understanding where outcomes can be improved. Achieving the necessary improvements requires strategy, action (at district, regional, national and government levels) and lines of accountability. It is hoped and anticipated that the new National Mortality Review governance structure will develop processes within the system to ensure the PMMRC recommendations can be fully implemented.
The 16th report’s recommendations reflect the findings from the 2021 data and add to the existing suite of recommendations which still stand. They include action on preterm birth; national guideline implementation; embedding cultural safety across standards, regulation, service provision arrangements and personal responsibility; and prioritising complete and robust data collection and appropriate use, maintaining Māori data sovereignty.
As of July 2024, the future of PMMR reporting is unknown, and SME contracts are ending. Te Tāhū Hauora has commissioned an assessment of current and future data needs in relation to reviews of PMM. College representatives have advocated for, and strongly urge, the NMRC to maintain the PMMR infrastructure (including data collection and local review on each mortality), along with regular, independent reporting underpinned by epidemiological analysis and expert clinical and cultural review.
Mō tātou, me ā tātou uri e heke mai nei – For us and our children after us. Square

BREASTFEEDING AND DATA COLLECTION
Breastfeeding data needs to be accurately collected, carefully recorded and clearly reported, not only to establish exclusive breastfeeding rates, to show how breastfeeding initiation and duration are being supported (or not being supported) and whether the rates are trending upwards, downwards or staying static, but also to establish how modes of infant feeding impact on women's and children’s health and wellbeing, both short and long-term. Data also needs to be easily accessible by those working in maternal, infant and young child health.
WHY IS BREASTFEEDING IMPORTANT AND WHY DO WE NEED BREASTFEEDING DATA?
Exclusive breastfeeding to six months remains optimal and this is clearly shown in evidence of health outcomes. Exclusive breastfeeding in maternity facilities predicts longer duration of breastfeeding, which is significant for health equity, particularly for women of lower socioeconomic status (Vehling et al., 2018). Breastfeeding can promote equitable child health by reducing childhood illness and healthcare utilisation in the early years (Ajetunmobi et al., 2024) and is also associated with reduced childhood hospitalisations for common childhood illnesses (Ajetunmobi et al., 2015). Breastfeeding reduces costs to the health system, through a reduction in acute diseases in children (gastrointestinal and lower respiratory tract infections, acute otitis media and necrotising enterocolitis in preterm babies) (Pokhrel et al., 2015).
In 2015 the Commerce Commission attempted to estimate the healthcare costs/ savings related to breastfeeding rates in Aotearoa New Zealand, using a UNICEF UK report for reference (Commerce Commission, 2015; Renfrew et al., 2012). Looking at
incremental healthcare costs related to breast cancer, gastrointestinal infections, necrotising enterocolitis, lower respiratory tract infection and acute otitis media, the Commerce Commission estimated that two years of decreased breastfeeding rates would result in a cost of approximately $3.4 to $3.8 million for the treatment of the increased rate of ill health, if SIDS deaths were also included in the analysis. This was considered to be an underestimate of the harms that would arise in the event of a small decrease in breastfeeding rates.
It is clear that investment in public health, and in services that support women who want to breastfeed exclusively and for a longer duration, is cost saving. Any discussion about equality or equity that omits to address breastfeeding is failing to understand the significance of breastfeeding to health equity and positive population health. Breastfeeding is among the most cost-effective public health interventions available, and as previously noted it provides protection against several short and long-term health conditions for both mother and infant (Victora et al., 2016). Renfrew et al. pointed out in 2012 that research into the burden of disease associated with low breastfeeding rates continues to be
hampered by data collection methods and that this can be addressed by high quality data collection and research.
Breastfeeding data needs to provide insights into which women are experiencing challenges, when these challenges occur and why. Comparison of different system approaches to supporting breastfeeding, what the barriers to breastfeeding are, what strategies work, why they work, how they work, who they work for, and when they work, become difficult to ascertain without reliable data. The reporting of data, data indicators and access to data are hurdles that need to be overcome to enable evaluation of equity and how we are supporting, or not supporting, breastfeeding and breastfeeding women.
TARGETS AND INDICATORS
Breastfeeding and population level infant feeding practices need defined indicators and regular monitoring and evaluation. Indicators monitor progress – or lack of progress – towards a previously determined and specific goal. As described by Health New Zealand Te Whatu Ora (2024), “measuring the health and disability sector’s performance is critical to improve equity and for tracking progress towards better health and wellbeing”.
The Ministry of Health described breastfeeding targets 22 years ago in 2002. These targets were to increase the exclusive and full breastfeeding prevalence rate at six weeks to 74% by 2005 and 90% by 2010; to increase the exclusive and full breastfeeding prevalence rate at three months to 57% by 2005 and 70% by 2010; and to increase the exclusive and full breastfeeding prevalence rate at six months to 21% by 2005 and 27% by 2010 (National Breastfeeding Advisory Committee, 2008). The 2014 Well Child Tamariki Ora (WCTO) quality indicators reported exclusive and fully breastfeeding together and indicators #11-#14 were two weeks after birth, at discharge from LMC care, and at three months and six months of age (Health Quality and Safety Commission, 2014). Targets for breastfeeding were
CAROL BARTLE POLICY ANALYST

It is clear that investment in public health, and in services that support women who want to breastfeed exclusively and for a longer duration, is cost saving. Any discussion about equality or equity that omits to address breastfeeding is failing to understand the significance of breastfeeding to health equity and positive population health.
included and the two week target for combined exclusive/fully in 2014 was 72% and the target set for 2016 was 80%. The combined targets dropped to 68% for 2014 and 75% for 2016 in the LMC discharge category, the three months combined target for 2014 was 54% and 60% for 2016, and the six months category combined target for 2014 was 59% and 65% for 2016. In the Quality Improvement Framework report of 2016, the six month indicators were removed (Health New Zealand Te Whatu Ora, 2016). Targets would be more valuable for population health research purposes if exclusive and fully breastfeeding were separated in the indicators and targets.
The Health System Indicators Framework describes, “a new approach to health system performance measurement” (Health New Zealand Te Whatu Ora, 2024a). The high level indicators for child wellbeing include potentially avoidable stays in hospital for
children and immunisation rates (Health Quality and Safety Commission, 2022).
Data in Aotearoa New Zealand which would be necessary to assess mode of feeding and link this to paediatric or maternal health issues appears to be unavailable, or at least inaccessible.
DATA IN AOTEAROA NEW ZEALAND
Definitions of breastfeeding differ, depending on which country is collecting the data and how they define their categories. This makes cross-country examination of data complicated, if not impossible. We are fortunate to have the Baby Friendly Hospital Initiative (BFHI), as BFHI data reports exclusive and fully breastfeeding separately as well as partial breastfeeding and babies who are not breastfed. These definitions, which differ from other countries, are used as part of the BFHI assessments and represent critical information. Maternity facilities are required to achieve an exclusive breastfeeding rate of 75% at discharge for healthy full-term infants (New Zealand Breastfeeding Alliance [NZBA], 2023). Evidence shows that the BFHI has led to an increase in breastfeeding rates, including exclusive breastfeeding and breastfeeding duration (Perez-Escamilla et al., 2016; Patterson et al., 2018; Philipp & Radford, 2006; Spaeth et al., 2018; Thomsen et al., 2024), and has also produced social value greater than the cost of investment, demonstrating the economic gains that can be made as a public health intervention (Pramono et al., 2021).
The definitions of exclusive, fully and partial breastfeeding and formula feeding are defined by the Ministry of Health:
• Exclusive breastfeeding: the infant has never, to the mother’s knowledge, had
Definitions of breastfeeding differ, depending on which country is collecting the data and how they define their categories. This makes cross-country examination of data complicated, if not impossible.
any water, formula or other liquid or solid food. Only breastmilk, from the breast or expressed, and prescribed medicines have been given from birth.
• Fully breastfeeding: The infant has taken breastmilk only, no other liquids or solids except a minimal amount of water or prescribed medicines, in the past 48 hours.
• Partial breastfeeding: The infant has taken some breastmilk and some infant formula or other solid food in the past 48 hours.
• Artificial feeding: The infant has had no breastmilk but has had alternative liquid such as infant formula with or without solid food in the past 48 hours.
After mothers and babies are discharged from maternity facilities the data from that point on is either inaccessible to many and/or often hard to access. The concluding observations of the United Nations Convention on the Rights of the Child (2023), on their consideration of the sixth periodic report from New Zealand, recommended the strengthening of measures promoting, protecting and supporting breastfeeding, with a view to increasing the number of infants up to six months of age who are exclusively breastfed. With the current reporting on breastfeeding data some differences in health outcomes that may represent avoidable structural determinants are difficult to ascertain.
Breastfeeding data on discharge from maternity facilities is straightforward and easy to access thanks to the NZBA (2024) and the BFHI (NZBA, 2024). As yet this data is unable to describe how babies are being fed in terms of breastfeeding, breast milk feeding and use of donor milk, although recognition of donor breast milk is included in the definition – breast milk includes pasteurised and unpasteurised donor human milk.
LMC midwives are required to report on breastfeeding status for electronic fee claiming purposes. This includes reporting at 48 hours after birth, at two weeks and at discharge. The reporting is detailed and specifies exclusive breastfeeding at the mother’s breast; freshly expressed breast milk from the mother’s breast fed via syringe, cup, spoon or nasogastric tube; antenatally expressed breast milk from the mother’s breast, fed via syringe, cup, spoon or nasogastric tube; breastfeeding at someone else’s breast; donor breast milk fed via syringe, cup, spoon or nasogastric tube or supplemental nursing system. These are further classified as exclusive or fully.
This data is currently not reported on, but it could provide some valuable insight into whether babies are breastfeeding or breast milk feeding on discharge from maternity units, and whether the breast milk is all from the baby’s mother or from a donor mother/mothers. The use of donor breast milk may be quietly boosting the exclusive breastfeeding rates by inadvertently covering up breastfeeding initiation and early establishment issues. Insight into what the indications are for using donor breast milk for each recipient baby, and what is influencing the challenges with initiation and duration of breastfeeding, would be valuable. Dyads who are breast milk feeding rather than breastfeeding may be a group with some members more likely to discontinue breastfeeding sooner than they planned, but as this data is apparently not collected, and certainly not reported, outcomes are unknown apart from small numbers in research studies or anecdotally.
The Midwifery and Maternity Providers Organisation (MMPO) reports on New Zealand’s MMPO midwives and provided reports of data collected by midwives until 2016. This data reported exclusive and fully breastfeeding separately at discharge (both numerically and statistically, from place of birth – home, primary, secondary, and tertiary) and at two weeks of age (MMPO, 2016). Data collection from 2016 drastically changed with the introduction of a new programme but new reports are on track to contain the detailed categories collected by LMCs described above.
The Well Child Tamariki Ora quality improvement framework has three indicators related to breastfeeding and data is collected from two weeks of age, at discharge from the LMC and at three months (Health New Zealand Te Whatu Ora, 2024a). Data reporting from Well Child Tamariki Ora now stops at three months, despite data after this time still being collected, so ascertaining whether breastfeeding practices are meeting the Ministry of Health recommendations for optimal infant feeding – exclusive to six months, and then continued breastfeeding alongside the introduction of solid foods from around six months – is difficult to assess. It is not possible to find the median duration of breastfeeding in Aotearoa New Zealand and we have no reliable information about how many women continue to breastfeed up to two years and beyond, which is one of the infant and young child feeding recommendations of the World Health Organization (2023).
Ministry of Health data reported under the topic of nutrition (2023) includes exclusively breastfed until at least four months, and exclusively breastfed until at least six months. It also reports whether babies are given solids before four months and before six months (Ministry of Health, 2024). This data is reported from 2011/2012 until 2022/2023. Exclusive breastfeeding until four months old is recorded as 58.1% and at six months 9.5%. The NZBA 2023 BFHI data on infant feeding reported relatively constant exclusive breastfeeding rates at discharge from maternity facilities between 2021and 2023, and the 2023 rate was 77.06% nationally. The Māori exclusive breastfeeding rate was higher than the national average at 80.78% but decreases were reported in Pacific People, Asian and Indian populations since 2022.
Data on breastfeeding may also be collected by private businesses such as Karo Health (https://karo.co.nz/) and Reach Aotearoa/Health Stat (https://reach.co.nz/Services/Population+Health+Monitoring/HealthStat. html) but it is unclear what data these organisations are collecting, how large their cohort numbers are, what indicators they are using, who the data is being reported to, and where the data is being reported.
Currently, the Ministry of Health’s breastfeeding definitions and the available data only tell us half a story and, despite the reporting specifications required by LMC midwives, mothers and infants going home from a facility exclusively or fully breastfeeding at the breast are seen as no different in the data from a mother and infant documented as exclusively or fully breastfeeding when the baby has never managed, or barely managed, an effective latch at the breast. This means that mother-baby dyads may be taking home unresolved breastfeeding issues. The extra workload such as expressing/pumping breast milk to establish/protect milk supply, the infant being syringe/spoon/bottle-fed the expressed milk, and the mother and midwife continuing attempts to support the infant to latch – none of this can be ascertained from the available data. The available data says they are the same, but the reality for mothers and midwives is far from this, and the differences are not counted. The work involved in resolving these breastfeeding challenges is also invisible, except to those directly impacted and involved.
BREASTFEEDING OR BREAST MILK FEEDING?
There are reasons related to infant health and development outcomes, and health research, that highlight why data needs to be clear about whether a baby is breastfeeding or being fed breast milk – whether mother’s own milk or a donor's. Research has indicated that feeding breast milk via a bottle may not be equivalent to breastfeeding. There have been observed differences in a range of markers, which indicates accurate data is required to establish health outcomes. For example, infant weight gain (Azad et al., 2018), infant satiety (Li et al., 2010), asthma rates (Klopp et al., 2017) and memory (Pang et al., 2019). Pang et al. (2019) suggest that the developmental differences may be due to breastfeeding exerting effects through the physical and/or emotional contact between mother and infant during breastfeeding. Despite the potentially different impact of bottlefeeding breast milk, rather than breastfeeding, and despite the reduced bioactivity of expressed and stored human milk, breast milk continues to provide benefits compared with feeding infant formula (Azad et al., 2018; Klopp et al., 2017). Azad et al. propose that future research should be capturing the “complexity of modern human milk feeding practices, even among exclusively breast milk fed babies”. They also suggest it is critical to address the structural barriers that force some women to choose between pumping and stopping breastfeeding altogether. Collecting accurate data is significantly important to support such work.
References available on request
conclusion
Breast milk is much more than food, and nutrition is barely half the story (Bartle, 2012). As described by Garbes (2015), “it's potent medicine and, simultaneously, a powerful medium of communication between mothers and their babies. It's astonishing. And it should be—the recipe for mother's milk is one that female bodies have been developing for 300 million years”.
The science about the importance of breastfeeding is solid, it is evidence-based, and it is undeniable. However, while the science of breastfeeding is indisputable, the key issues for breastfeeding women or women trying to make decisions about how to feed their babies remain the same. This is not about women misunderstanding the importance of breastfeeding to themselves and their babies, as the majority do intend to breastfeed, but it is predominantly about removing the barriers to breastfeeding which are largely out of the control of individual women. These barriers include: the significant midwifery shortage and staffing issues in maternity facilities, which include the employment of nurses without breastfeeding education and of non-regulated health care workers; an increase in birth interventions; and an increase in birthing women with complex medical needs which may impact on breastfeeding. There are also continuing issues with insufficient maternity protection for many women, unsupportive workplaces, and economic pressures. Currently Aotearoa New Zealand has provided limited societal, governmental, institutional and cultural investment and support structures. The quality assurance measure of the Baby Friendly Initiative is a clear exception because without breastfeeding ‘getting off to a good start’, what follows may be more challenges for breastfeeding. Collecting robust breastfeeding data, and being able to link this to a range of indicators and trends which provide a fuller picture of the breastfeeding journeys for mothers and babies and their health, is an urgent country and global priority. As described by Amir and Smith (2020) the first step to seriously investing in breastfeeding is the funding of “proper data collection”. This should be done via routine data collection up to two years of age and regular in-depth national surveys. Exclusive breastfeeding is a key health indicator that needs collecting up to six months. The data about immunisation rates is rigorously collected and reported - breastfeeding is a baby’s first immunisation, and it protects against a range of infant and young child illnesses. The efforts taken to access data for this article have been significantly difficult and it is hard to understand why there is not one easily accessible database that collates all breastfeeding and infant feeding data.
As the Global Breastfeeding Collective states - “Behind every breastfeeding statistic is a mother trying to reach her breastfeeding goals” (2024). And therein lies the reason we need good data collection, coherent and easily accessible data reports, targets, and ongoing monitoring to create accountability and address challenges. Because mothers and babies matter, we need to know how they are doing, and we need to know about their health and wellbeing. Square

taku wāhi mahi my midwifery place
small but fundamental part of a network of maternity facilities serving the wider Wellington region. Gwen loves her workplace and explains its significance as a vital service for her local community.
Born and raised in Wellington city, Gwen moved to Kāpiti 35 years ago and hasn’t looked back. 'It was partly about affordability - it was cheaper to buy a house here than in Wellington and it’s by the beach, which I love,' she admits.
Gwen registered as a midwife in 2008 but had her own birth experience in the unit 31 years ago.' This place has been here for a long time,' she explains.' I had my oldest baby here - not in this same building, but on the same site, when it used to be a hospital.'
Her connection to the place is personal and, since becoming a midwife, Gwen has oscillated between LMC practice and core midwifery, accessing Paraparaumu Maternity Unit countless times over 14 years of LMC caseloading. In 2021, she joined the unit as a staff midwife and two years ago stepped into her current role of Midwife Manager.

'I loved it so much here, I saw it as a natural progression,' she says of her move into the managerial role. With one birth room and two postnatal rooms - extending to three postnatal rooms on weekends - the unit sees around 100-130 births annually and Gwen emphasises how essential the facility is for people who call Kāpiti home.
'Keeping low-risk people out of hospital is obviously a good thing. Being able to provide an alternative place of birth for our
local community who don’t want to be in hospital, but also don’t want to birth at home, is really important.'
Providing quality postnatal care for locals is another highlight of working at the unit, as Gwen explains.'We take postnatal people from both Wellington and Hutt Valley hospitals, which not only eases the pressure on the hospitals, but means local people can be closer to home for their postnatal stay. Having one midwife to two or three postnatal people means we can spend quality time supporting them and their whānau.'
When asked what makes the unit such a great place to work, Gwen doesn’t hesitate: 'the dedication of the midwives and their commitment to the unit, as well as the collegial relationships between staff midwives and LMCs. I think if you asked any midwife here, they’d say the same. LMCs often say it’s a really approachable team and that they feel comfortable coming here'
Her connection to the place is personal and, since becoming a midwife, Gwen has oscillated between LMC practice and core midwifery, accessing Paraparaumu Maternity Unit countless times over 14 years of LMC caseloading.
Unsurprisingly, it comes back to connection. 'Most of our team have worked here for a number of years and have developed long-standing relationships with midwifery colleagues and the local community. A lot of returns who come back remember the staff, and some even pop back in to show us their babies a few weeks or months down the track, which is special.' Square
Above: Gwen Ryan, Midwife Manager with Joanna Ramsay, Staff Midwife, Paraparaumu Marternity Unit.
AMELLIA KAPA
REGISTERED MIDWIFE
Gwen Ryan is Midwife Manager of the Paraparaumu Maternity Unit, a
New Zealand College of Midwives Directory
National Office
PO Box 21-106, Christchurch 8140 Ph 03 377 2732 nzcom@nzcom.org.nz www.midwife.org.nz
Auckland Office auckadmin@nzcom.org.nz
College Membership Enquiries
Lisa Donkin membership@nzcom.org.nz 03 372 9738
Chief Executive
Alison Eddy
Co-Presidents
Beatrice Leatham bea.tangatawhenua.copres@nzcom.org.nz
Debbie Fisher debbieF.tangatatiriti.copres@nzcom.org.nz
National Board Advisors
Kuia: Crete Cherrington Elder: Sue Bree
Education Advisor: Tania Fleming
Regional Chairpersons
Auckland Jacquelyn Paki, Tania Webb auckchair@nzcom.org.nz
Bay of Plenty/Tairāwhiti
Cara Kellet chairnzcomboptairawhiti@gmail.com
Canterbury West Coast Becky Bangma chairnzcom.cantwest@gmail.com
Central
Laura McClenaghan centralchair@nzcom.org.nz
Nelson Marlborough
Emma Neal tetauihunzcom@gmail.com
Northland
Ange Yendell tetaitokerauchair@nzcom.org.nz
Otago
Jan Scherp, Charlie Ferris otagochair@nzcom.org.nz
Southland
Liz Whyte liz.whyte@netspeed.net.nz
Waikato Taranaki
Michele Lord chairwaikatonzcom@gmail.com
Wellington Suzi Hume nzcomwellington@gmail.com
Regional Sub-Committees
Hawke's Bay Sub-Committee
Linley Taylor midwife.linley@gmail.com
Horowhenua Sub-Committee
Laura McClenaghan midwife.laura@hotmail.co.nz
Manawatu Sub-Committee
Megan Hooper-Smith megan.scott@live.com
Emma LeLievre emma@LMCmidwife.com
Taranaki Sub-Committee Ange Hill nzcom.taranaki@gmail.com
Whanganui Sub-Committee
Laura Deane laura.deane@wdhb.org.nz
Consumer Representatives
Home Birth Aotearoa
Bobbie-Jane Cooke bobbiejane.homebirth@gmail.com
Parents Centre New Zealand Ltd
Nicola Eccleton n.eccleton@parentscentre.org.nz
Royal New Zealand Plunket Society
Zoe Tipa zoe.tipa@plunket.org.nz
Student Representatives
Paytra Buckrell paytra_browne@windowslive.com
Te Rina Apelu tee_apelu@hotmail.com
Ngā Maia Representatives www.ngamaiatrust.org
Lisa Kelly lisakellyto@yahoo.co.nz
Pasifika Midwives Representatives
Talei Jackson Ph 021 907 588
taleivejackson@gmail.com
Ngatepaeru Marsters Ph 021 0269 3460 lesngararo@hotmail.com
MERAS
PO Box 21-106, Christchurch 8140 Ph 03 372 9738 meras@meras.co.nz www.meras.co.nz
MMPO
PO Box 21-106, Christchurch 8140 Ph 03 377 2485 mmpo@mmpo.org.nz
Rural Recruitment & Retention Services 0800 Midwife/643 9433 rmrr@mmpo.org.nz
Resources for midwives and women
The College has a range of midwiferyrelated books, leaflets, merchandise and other resources available through our website: www.midwife.org.nz/shop
ADVERTISING POLICY AND DISCLAIMER: The New Zealand College of Midwives maintains a schedule of guidelines to exclude advertisements for products or services that are not aligned with its principles and ethics. Every effort is made to ensure that advertising in the magazine falls within those guidelines. Where advertising is accepted, this does not imply endorsement by the College of the product or service being promoted
Midwife Aotearoa New Zealand is published quarterly for the New Zealand College of Midwives. The articles and reports printed in this newsletter are the views of the authors and not necessarily those of the New Zealand College of Midwives, its publishers or printers. This publication is provided on the basis that New Zealand College of Midwives is not responsible for the results of any actions taken on the basis of information in these articles and reports, nor for any error or omission from these articles and reports and that the College is not hereby engaged in rendering advice or services. New Zealand College of Midwives expressly disclaims all and any liability and responsibility to any person in respect of anything and of the consequences of anything done, or omitted to be done, by any such a person in reliance, whether wholly or partially upon the whole or any part of the contents of this publication. The College acknowledges and respects diversity of identities through the language used in this publication. Te reo Māori is prioritised, in commitment to tāngata whenua and te Tiriti o Waitangi. To maintain narrative flow, the editorial style may use a variety of terms. Direct citation of others’ work maintains the original authors’ language, and contributing writers’ language preferences are respected. All advertising content is subject to the Advertising Standards Authority Codes of Practice and is the responsibility of the advertiser.
Contents Copyright 2024 by New Zealand College of Midwives. All rights reserved. No article or advertisement may be reproduced without written permission. ISSN: 2703-4546.
You are kaitiaki for hapū māmā and pēpē

Maternal immunisation provides vital protection for pēpē and māmā before and during the most vulnerable first months of life. Your recommendation to immunise can save lives.
INFLUENZA
Pregnant people and their babies are at greater risk of serious influenza-related complications. Most young babies whose mothers were vaccinated during pregnancy are protected against influenza.
WHOOPING COUGH
Babies, particularly younger ones, can get very sick or even die from whooping cough. Most young babies whose mothers were vaccinated during pregnancy are protected against whooping cough.
COVID-19
COVID-19 vaccination in pregnancy protects against infection, severe disease, hospitalisation and death. Babies of immunised mothers receive some of that protection too.
Immunisation during pregnancy boosts disease-specific antibodies that not only protect hapū māmā, but also travel across the placenta and protect pēpē until their first three immunisations at six weeks old.
Influenza vaccination is recommended at any stage of pregnancy and is free during the influenza season COVID-19 vaccination is recommended and funded at any stage of pregnancy Tdap*
* Tdap is funded from the beginning of the 2nd trimester and is recommended from 16–26 weeks. † MMR post-delivery is recommended for those who haven’t had the MMR vaccine.
