









With summer in session, many of us are motivated to slip into our sneakers and head outside for a run. A good run enhances strength, contributes to cardiovascular fitness, builds muscle endurance and is a great way to shed pounds. It’s also a boost for your mental health. A recent study in Neuroscience News found aerobic exercise like running leads to an increase in levels of serotonin, dopamine and norepinephrine - chemicals that regulate your mood. It also helps promote better sleep, relaxes stress hormones and increases brain function.
So, take this as your sign to get out there! But, in addition to the right footwear, a killer playlist and an interesting route for your workout, it’s vital to focus on nutrition. Regardless of the distance or duration of your run, sports nutrition is an important key to your performance.
Most runners know they should get some carbs, protein, and stay hydrated. But how much, and when? Before, during or after your run? Dana Ryan, Ph.D., MA, MBA, director of Sports Performance, Nutrition and Education and Chair of the Fitness Advisory Board at Herbalife, offers these tips to get moving with good nutrition. Start with the basics. Whether you’re a distance runner or a new jogger working up to your first mile, a good basic diet is the building block for great performance. Fruits, veggies, lean protein, healthy fats and good carbohydrates are a must.
Pre-workout boost. As you near your run, you want to focus on liquids. One to two hours before your workout, drink a protein shake that includes carbohydrates. Protein helps your brain and body function and gives you an energy boost, and those carbs keep you going. Within 30 minutes of your run, a pre-workout drink that contains caffeine and nitric oxide precursors is a good option. The two things you want to avoid pre-workout are fiber and fat as they are hard for the body to digest.
Hydrate! This is vital before, during and after your workout. Proper hydration is essential not only for general body functions, but also boosts performance and mitigates dehydration during running. Runners need to maintain body water balance, because water provides nourishment that the body needs for almost every single function. It also helps limit changes in body temperature. For hydration, water alone is great. Water with electrolytes kicks it up a notch.
Carb it up. For many dieters, carbs are taboo. But for runners, or people who do other high-intensity workouts, carbs are key to performance. If you’ve ever run out of steam or hit a wall during a workout, it could be because you’re low on carbs. While running, it’s crucial to replace what the body is losing, namely carbohydrates and electrolytes. One’s body fatigues because of the depletion of carbohydrate reserves and dehydration due to loss of water and electrolytes in sweat, both of which hinder sports performance. So, for every hour of running, consume about 30 to 60 grams of carbohydrates through a sports drink.
Finish with protein. Immediately following the completion of a run, make sure to get some protein in. Within 30 minutes of finishing your workout, consume 20 to 40 grams of high-quality protein, no matter how long the run was. And for those longer runs, add in some carbohydrates to be closer to a 3:1 carbohydrate-to-protein ratio. Why? Protein after a run helps your muscles repair and recover. The amino acids in protein help build lean muscle, which is exactly what you want.

No matter your fitness level, nutrition is an important part of getting the most out of your workout. Now, get out there and move!
Source: Brandpoint

By d-mars.com News Provider
he summer heat can bring a range of illnesses due to increased outdoor activities, higher temperatures, and more travel. Here are some common summer sicknesses and tips to keep yourself healthy:
TCOMMON SUMMER SICKNESSES
Heat-Related Illnesses:
• Heat exhaustion and heatstroke can occur due to prolonged exposure to high temperatures.
• Prevention: Stay hydrated, wear loose and light clothing, avoid excessive sun exposure, and take breaks in the shade or indoors.
Food Poisoning:
• Higher temperatures can cause food to spoil faster, leading to bacterial growth.
• Prevention: Store food properly, cook meat thoroughly, avoid cross-contamination, and wash hands frequently.
Waterborne Illnesses:
• Swimming in contaminated water can lead to infections such as swimmer’s ear or gastrointestinal issues.
• Prevention: Avoid swallowing water from pools, lakes, or oceans, shower before and after swimming, and ensure swimming areas are clean and properly maintained.
Respiratory Infections:
• Changes in environments, such as air conditioning and travel, can spread viruses.
• Prevention: Practice good hygiene, wash hands regularly, and avoid close contact with sick individuals.
Vector-Borne Diseases:
• Diseases like Lyme disease and West Nile virus are spread by ticks and mosquitoes.
• Prevention: Use insect repellent, wear long sleeves and pants, avoid areas with high insect activity, and check for ticks after being outdoors.
GENERAL
Here are some tips that will help you stay healthy in the summer:
Hydration:
• Drink plenty of water throughout the day.
• Avoid excessive alcohol and caffeinated beverages as they can lead to dehydration.
Nutrition:
• Eat a balanced diet with plenty of fruits and vegetables.
• Avoid undercooked or raw foods that can spoil easily in the heat.
Sun Protection:
• Wear sunscreen with at least SPF 30, reapply every two hours or after swimming or sweating.
• Wear sunglasses, hats, and protective clothing.
Stay Active Safely:
• Exercise during cooler parts of the day, such as early morning or late evening.
• Gradually acclimate to higher temperatures if exercising outdoors.
Travel Smart:
•Check travel advisories and health recommendations for your destination.
• Pack the necessary medications and a first aid kit.
Cleanliness:
• Maintain good personal hygiene, especially when in public places.
• Sanitize hands and surfaces frequently, especially before eating.
By taking these preventive measures, you can experience a healthier and more enjoyable summer.


By Frenetta Tate Contributing Writer
ental health is integral to our overall well-being because it profoundly affects how we think, feel, and act. It provides emotional resilience, enabling us to cope with life’s challenges, adapt to adversity, and recover from setbacks. Mental health is closely linked to physical health; poor mental health can lead to chronic stress, heart disease, and weakened immune function, while good mental health promotes healthier lifestyle choices and lessens the impact of stress-related illnesses.
Beyond individual resilience, our mental health significantly influences our social connections and productivity – how we relate to each other. Positive mental health fosters effective communication, empathy, and the ability to support others, which are crucial for maintaining strong personal and professional relationships. It also aids in managing conflicts constructively, enhancing relationship quality.
Finally, mental health is foundational to self-esteem, stress management, and overall quality of life. It enables individuals to view themselves positively, fostering confidence and a sense of competence. This self-esteem is crucial for making sound decisions, setting goals, and pursuing aspirations. Above all, good mental health enhances life quality by contributing to a sense of purpose, fulfillment, and joy.

While all of this is good to know, in many minority communities, mental health remains a topic wrapped in shame and misunderstanding. When the reluctance to openly discuss mental health issues is combined
with systemic barriers to accessing care – it results in significant disparities in mental health outcomes among minority populations. These disparities are rooted in various factors, including socioeconomic barriers, cultural stigmas, and systemic barriers. Socioeconomic status plays a significant role

in mental health outcomes. Our socioeconomic status is like a score or a measure of a person’s economic and social position based on their income, education and occupation, compared to others. In comparison to other communities, minority communities often face higher rates of poverty, unemployment, and underemployment, which can worsen mental health issues. Financial constraints limit access to quality mental health services, leading to untreated conditions and declining health.
Cultural beliefs and stigmas surrounding mental health significantly impact minority communities. In many cultures, mental health issues are seen as a sign of weakness or failure. This stigma can discourage individuals from seeking help, leading to people feeling ashamed and experiencing worsened conditions, isolation and increased stress. For example, in many Black and Latino communities, mental health struggles are often kept within the family, and seeking outside help can be perceived as a betrayal or failure.
Systemic barriers, including a lack of culturally competent healthcare providers, contribute to the disparities in mental health care for minorities. Many mental health professionals lack the training to understand and address the unique cultural contexts and experiences of minority patients. This cultural disconnect can lead to misdiagnoses, ineffective treatment plans, and a general mistrust of the healthcare system.
Myth 1: Mental Health Issues Are a Sign of Weakness
One of the most pervasive myths is that mental health issues signify personal weakness. This belief is particularly damaging in minority communities where strength and resilience are highly valued. It is essential to understand that mental health conditions are medical issues, similar to physical ailments, and seeking help is a sign of strength, not weakness.
Myth 2: Mental Health Problems Can Be Overcome with
Another common myth is that mental health problems can be solved with sheer willpower, positive thinking, or praying it away. While a positive outlook is beneficial, mental health conditions often require professional intervention, including therapy and medication.
Therapy is often stigmatized as something only necessary for severe mental illnesses. However, therapy can be beneficial for anyone experiencing stress, anxiety, or other emotional challenges. It provides a safe space to explore feelings, develop coping strategies, and improve overall mental health.
• Mental health maintenance refers to the ongoing practices and activities that help individuals manage stress, cope with challenges, and maintain a balanced state of mental well-being. Access to and maintenance of mental health is essential for overall well-being, yet minority communities often face significant barriers in obtaining the support that they need.
• Education is a powerful tool in combating mental health stigma. Community programs and public health campaigns can raise awareness about the importance of mental health and the benefits of seeking help.
• To better serve minority communities, healthcare providers must be trained in cultural competence. This training includes
understanding cultural beliefs, values, and practices related to mental health.
• To address financial barriers, it is crucial to expand access to affordable mental health services. Community health centers, sliding scale fees, and telehealth options can make mental health care more accessible.
• Support networks are vital for mental health maintenance. Encouraging open conversations about mental health within families and communities can reduce stigma and promote early intervention. Peer support groups, both in-person and online, offer a sense of community.
• Self-care is an essential component of mental health. Self-care is not selfish, it’s necessary. Activities such as exercise, meditation, getting adequate rest, and hobbies can significantly improve mental well-being, reduce stress and add joy to life.
• Recognizing when professional help is needed is paramount. Therapy and counseling can provide valuable tools and strategies for managing mental health conditions. It is important to research and find culturally competent providers who can understand and respect cultural backgrounds.
• Mindfulness practices, such as meditation and deep breathing exercises, can help manage stress and regulate emotions. Incorporating these practices into daily routines can enhance overall mental health.
Addressing the mental health disparities in minority communities requires a multifaceted approach that includes increasing awareness, enhancing cultural competence, and expanding access to services. By debunking myths and promoting open conversations about mental health, we can reduce stigma and encourage more individuals to seek the help they need. Ultimately, improving mental health within minority communities leads to a stronger and more resilient society.
Frenetta Tate is an award-winning author, inspirational orator, and certified women’s empowerment coach. Follow @frenettatate on social media.

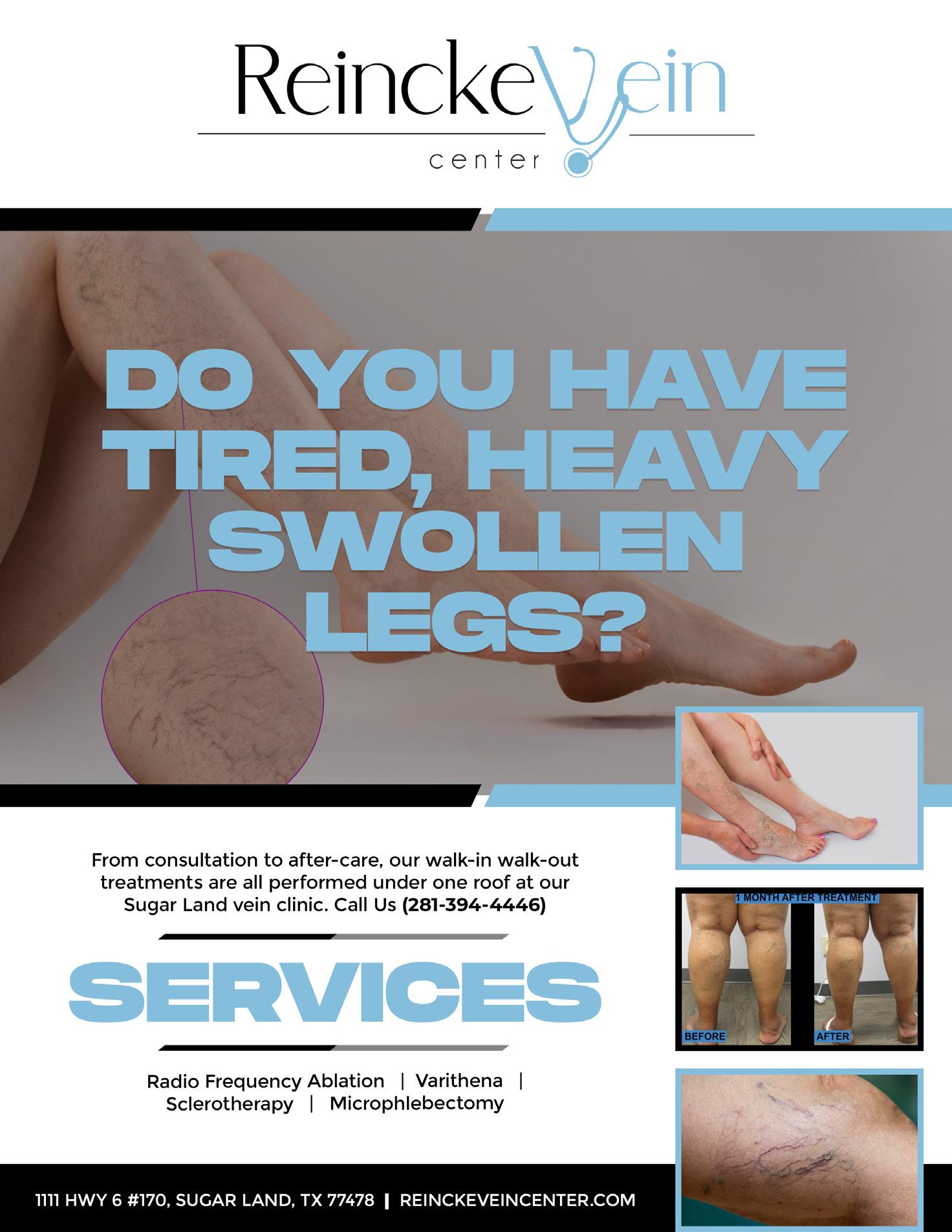
ein health and mental health are critical yet often overlooked aspects of overall well-being. Within minority communities, these issues are compounded by unique social, economic, and cultural challenges. Understanding the interplay between vein health and mental health in minority populations can illuminate pathways to more effective healthcare interventions and support.
Vein health primarily concerns the efficiency and condition of veins, which are responsible for returning deoxygenated blood back to the heart. Vein disease can lead to symptoms such as swelling, pain, and in severe cases, life-threatening complications such as blood clots.
Maintaining vein health involves regular physical activity, a balanced diet, proper hydration, and avoiding prolonged periods of standing or sitting. However, access to preventative care and treatment can be influenced by socioeconomic factors, often disproportionately affecting minority communities.

Mental health disparities in minority communities are well-documented. Factors such as socioeconomic status, discrimination, and lack of access to culturally competent care contribute to higher rates of depression, anxiety, and other mental health issues among minorities. Despite these challenges, minority populations are less likely to receive mental health services, often due to stigma, distrust of healthcare systems, and financial barriers.
Physical health issues like vein disease can exacerbate mental health problems, creating a vicious cycle of declining wellness. Chronic pain and quality of life issues from vein disease can lead to increased stress, anxiety, and depression. Conversely, poor mental health can negatively impact physical health behaviors, such as exercise and diet, further compromising vein health. For minorities, the compounded effect of systemic healthcare inequities can intensify this intersection. Socioeconomic barriers often limit access to both vein health specialists and mental health care providers. Additionally, cultural stigma surrounding mental health can deter individuals from seeking the necessary support, exacerbating both physical and mental health issues.
PATHWAYS TO WELLNESS
Addressing the intertwined issues of vein health and mental health in minority communities requires a multifaceted approach:
1. Community Outreach and Education:
Raising awareness about the importance of vein health and mental health is crucial. Community programs that educate about risk factors, prevention, and treatment options can empower individuals to seek care early.
2. Culturally Competent Care:
Healthcare providers must be trained in cultural competency to understand and respect the unique needs of minority patients. Culturally sensitive care can improve patient trust and engagement, leading to better health outcomes. This includes understanding cultural attitudes towards health and illness, and building trust within the community.
3. Integrated Healthcare Services:
Combining mental health services with general healthcare, including vein health, can provide more comprehensive care. Integrated care models ensure that both physical and mental health needs are addressed simultaneously.
4. Policy and Advocacy:
Advocating for policies that improve access to healthcare for minority communities is essential. This includes expanding insurance coverage, increasing funding for community health centers, and implementing policies that promote equity in healthcare delivery.
5. Support Networks: Encouraging the formation of support networks within minority communities can provide emotional and practical assistance. Peer support groups can help individuals manage both vein health and mental health challenges, fostering a sense of community and resilience.

The health of our veins and our minds are more connected than we often realize, especially in minority communities where the burdens of chronic health conditions and mental health disparities intersect. It is important to see the right physicians that are willing to implement these cultural strategies. Reincke Vein Center works with the community to make sure every vein patient is treated individually taking into account each patient’s needs. By fostering a comprehensive approach that addresses both physical and mental health, and by ensuring access to culturally competent care, we can pave the way for healthier, more resilient communities.

By Letrice Mason, MSN, APRN, FNP-C Contributing Writer
terine fibroids are a form of noncancerous growth that can grow inside and outside of your uterus. Fibroids do not always create symptoms, but when they do, they may cause heavy menstrual bleeding, back pain, frequent urination, and sex pain. Small fibroids rarely require treatment, while bigger fibroids may require medication or surgery.
UFibroids are a form of pelvic tumor that is fairly frequent. Fibroids affect between 40 and 80% of women. Many women, however, are unaware that they have fibroids since they do not feel any symptoms. This can happen if you have little fibroids that are asymptomatic, meaning they don’t give you any discomfort.
If you’re interested in learning more about uterine fibroids or suspect you might have some type, this article will come in handy. Below you can find useful information about what causes uterine fibroids to develop, the different types and side effects as well as what to do if you experience pain.
Fibroids are noncancerous uterine growths that commonly arise during pregnancy. Uterine fibroids, also known as leiomyomas or myomas, aren’t linked to an elevated risk of uterine cancer and usually never develop into cancer. They can range in size from tiny seedlings that are undetectable to enormous masses that deform and expand the uterus. You can have only one fibroid or several, which having multiple fibroids can cause the uterus to enlarge to the point where it reaches the rib cage, causing weight gain. Uterine fibroids affect many women at some point in their life. However, because uterine fibroids seldom cause symptoms, you may be unaware that you have them. During a pelvic exam or a prenatal ultrasound, your doctor may uncover fibroids by chance.
Fibroids have been connected to the hormone estrogen, however, the specific etiology is uncertain (the female reproductive hormone produced by the ovaries). Fibroids most commonly appear during a woman’s reproductive years (around the ages of 16 to 50), when estrogen levels are at their maximum.
After estrogen levels are low, such as during menopause, when a woman’s monthly periods finish, they decrease.
Uterine fibroids are thought to arise from a stem cell in the uterus’ smooth muscle tissue (myometrium). A single cell divides many times, eventually forming a solid, rubbery mass that is separate from surrounding tissue. What’s more, fibroids have a variety of growth patterns: they might grow slowly or quickly, or they can stay the same size. Some fibroids experience growth spurts, while others may diminish on their own.
TYPES
Three main types of uterine fibroids can grow anywhere in the womb and have various sizes that can range from very little to considerably big (think about a pea and a melon, for example).
COMMON
• Intramural Fibroids – It is the most common type of fibroid and develops in the muscle wall of the womb.
• Subserosal Fibroids – Fibroids that sprout outside the womb’s wall and into the pelvis and can grow to be quite enormous.
• Submucosal Fibroids – These fibroids originate in the muscular layer beneath the womb’s inner lining and grow into the cavity of the womb.
Subserosal or submucosal fibroids are sometimes linked to the womb by a thin stalk of tissue. Pedunculated fibroids are what they’re called.
SIDE
There are many side effects of uterine fibroids that can seriously compromise your health if not detected and treated properly. Intramural fibroids’ symptoms can range from mild to painful for those who suffer from them. Lower back pain, heavy periods lasting more than 10 days, bleeding between periods, pelvic pain, and exhaustion are all possible side effects.
They can also cause anemia and iron deficiency as a result of blood loss during a woman’s menstrual cycle. Because intramural fibroids are located directly inside the uterine cavity, if they grow too large (more than 6 cm in diameter), they begin to take over the space normally reserved for an embryo to grow, causing many difficulties and jeopardizing fertility.
Subserosal fibroids can result in significant pelvic pain as well as pressure on the surrounding organs. Subserosal fibroids grow on the outside of the uterus, unlike intramural and submucosal fibroids, which grow on the inside of the uterus, causing different symptoms. The most significant difference is that subserosal fibroids appear to affect neighboring organs such as the bladder more than the uterus. Submucosal fibroids may obstruct and deform fallopian tubes, making sperm passage to the uterus for implantation impossible. For women with fibroids, this disruption is frequently what causes fertility problems. Furthermore, submucosal fibroids can cause pregnancy difficulties. There is insufficient room for the fetus to grow as the fibroids get larger and push into the uterine cavity. As a result, this problem could lead to a miscarriage or birth abnormalities.
If there are no symptoms, fibroids do not need to be treated. Without treatment, they usually decrease and disappear over time, especially after menopause. If you have fibroids-related symptoms, you will most likely be prescribed medication to help relieve them.
There are various medications that can aid in the reduction of fibroids. If these fail to work, surgery or other, less invasive techniques may be suggested.
Let us help and book an appointment with us. Access to medical care from the comfort of your home and with skilled professionals that are always looking after your health, with your emotional, physical, and spiritual wellness in mind.
Her Down There specializes in several important concerns such as birth control, STD testing, urinary tract infections, menopause, and more, assisting women and providing the care they need without having to move from their house. Her Down There aims to make women’s healthcare simple, quick, easy, and economical.
Letrice Mason, MSN, APRN, FNP-C, is an accomplished women’s health nurse practitioner and proud owner of the esteemed Her Down There Women’s Clinic. She is a trusted healthcare professional within the Houston community.
By d-mars.com
Provider
early 25 million people of all ages in the United States are living with asthma, a lifelong chronic disease that makes it harder to move air in and out of the lungs. Here’s what the American Lung Association wants everyone to know during summer, when extreme heat can make asthma harder to manage.
1. NEW CHALLENGES ARE EMERGING.
Beyond traditional asthma triggers like respiratory infections, secondhand smoke and pets, new challenges are emerging. The effects of climate change
tions, asthma-related hospitalization and asthma-related death, especially for children and women. Patients should limit time outdoors during heat waves, seek access to air conditioning and take steps to improve indoor air quality, as humidity allows dust mites and mold to thrive.
2. CITY DWELLERS ARE PARTICULARLY VULNERABLE.
Two-thirds of the average U.S. city is made up of roads, parking spaces, sidewalks and roofs. Since these surfaces are typically dark and non-porous, they contribute to flooding, increased air pollution, poor health and what is known as “urban heat,” a phenomenon in which cities experience warmer temperatures than surrounding areas. Urban heat, combined with pollutants from power plants, motor vehicles and other pollution sources, creates ozone pollution, also known as smog. Those with asthma can experience symptoms like shortness of breath, wheezing and coughing from both ground-level ozone and particle pollution, as well as from the impacts of extreme weather and airborne allergens. Sadly, these issues disproportionally impact certain communities. Due to a history of discriminatory practices like systematic denial of mortgages, insurance loans, and other financial services on the basis of race and ethnicity, Black and Indigenous people, and other people of color, are more likely to be living in areas impacted by urban heat and poor air quality.

3. FLOODING CAN HARM LUNG HEALTH.
Increased severe storms due to climate change results in more flooding, which can harm lung health. Chemicals, sewage, oil, gas and other dangerous substances found in floodwaters can pose health risks, and mold, associated with asthma attacks, can grow anywhere there is water or dampness.
4. ADVOCACY EFFORTS ARE UNDERWAY.
The Smart Surfaces Coalition is made up of 40 national and international organizations committed to making Smart Surfaces the global urban design standard. Smart Surfaces encompass a suite of cutting-edge technologies, including reflective (cool) roofs and pavements, green roofs, trees, solar panels and rain gardens. Designed to mitigate urban heat, enhance air quality and improve health, these transformative urban features can cool cities by 5 degrees F, reduce flooding, provide economic benefits and potentially advance environmental justice.
The American Lung Association, an active member of the Smart Surfaces Coalition, encourages cities to take these actions:
• Install light-colored roads, parking lots and driveways to reflect sunlight and reduce heat.
• Install solar panels to convert sunlight into electricity and provide shade for roofs.
• Plant trees to increase shade.
• Select porous surfaces to collect polluted stormwater, soak it into the ground, and filter out pollution.
Other strategies to reduce urban heat, air pollution and ozone levels include using public transportation carpooling, increasing green spaces and installing cooling centers in extreme conditions.
5. RESOURCES ARE AVAILABLE.
Educational programming can help people better manage the disease in summer and year-round. Patients can check out the self-management education programs, information and tools available at Lung.org/asthma or call the American Lung Association’s Lung Helpline at 1-800-LUNGUSA. Living with an illness, or being the caretaker to someone who is, can take a physical and emotional toll. Patients can get support and knowledge, and connect with others by joining the Lung Association’s Patient & Caregiver Network.
For the 24.8 million Americans living with asthma, extreme summer temperatures and emerging environmental threats can make life more difficult. Fortunately, new educational resources and expanded programming can help patients navigate new and old challenges alike.
Source: StatePoint
n today’s evolving reproductive health landscape, informed decision-making about contraception is crucial, particularly for women affected by inherited blood clotting conditions or thrombophilia. Selecting the right birth control method is pivotal, say experts who point to research that shows the risk for potentially life-threatening blood clots is 35 times greater among women with genetic clotting disorders who use estrogen-based contraceptives.
DYNAMIC
Recent advances in technology and healthcare policies have fueled debate around screening for thrombophilia, a condition characterized by an increased tendency to develop blood clots, before starting estrogen-based contraceptives. Current guidelines discourage universal thrombophilia testing, citing concerns such as costs and potential adverse psychological effects. Instead, selective screening, focused on individuals with personal or family histories of blood clots, is more likely to be embraced by the medical community. Also, concerns about unfair treatment by insurers or employers due to genetic disclosures underscore the complexities of this approach.
However, people in support of a more patient-centered approach to healthcare and this type of birth control decision making stress the importance of identifying individuals at higher risk for blood clots.
Each year, many hundreds of women in the United States alone lose their life due to blood clots linked to estrogen-based contraception, as studies demonstrate. Advocates for genetic testing emphasize its role in facilitating personalized healthcare decisions, potentially reducing the incidence of clot-related fatalities, and empowering women with information and a more patient-centric approach to reproductive healthcare.
Cost considerations remain a significant factor, but for many, the value of preserving health and saving lives far outweighs financial concerns. While insurance coverage for genetic testing varies, studies show a willingness among women to bear screening costs, underscoring the importance of informed decision-making. Despite the perceived low absolute risk for blood clots among individuals with genetic clotting disorders, personal factors must be considered. Tailored approaches to contraceptive decisions, guided by individual risk profiles, may be warranted, especially in certain popu lations with higher rates of genetic clotting disorders.
For individuals with genetic throm bophilia, contraceptive options such as copper IUDs or pro gestin-only pills offer effective alternatives without increas ing clotting risks. Prioritizing safety and effectiveness is paramount in contraceptive decision-making.
While genetic testing may cause some level of anxiety or concern, studies indicate that most individuals do not regret pursuing testing. Knowledge empowers individuals to make proactive decisions about their health, outweighing potential psychological burdens.
Despite legal protections, concerns about discrimination persist. Understanding the implications of genetic disclosures on insurance and employment can inform decision-making processes, though these concerns may rightfully deter some individuals from pursuing testing. Women interested in pursuing genetic testing should talk with their healthcare provider about their testing options. Genetic counselors can also provide valuable help. Women considering their contraception options and interested in learning more about genetic testing can get more information from the Rowan Foundation at www. alexrowanfoundation.org.

Genetic testing holds the promise of empowering women to engage in informed discussions with healthcare providers, fostering shared decision-making in reproductive healthcare. Informed choices, guided by genetic information, may pave the way for more personalized and patient-centered care.
Source: Brandpoint



continues to grow not just in student population but also in the construction of new buildings such as the John M. O’ Quinn Law Building and Tilman J Fertitta Family College of Medicine.
UH’s facilities growth includes the continuous need to procure a variety of non-construction goods and services, all of which undergirds UH’s recognition as an institutional “Powerhouse.”

