16 minute read
Jean Yuan '25
Radiation erapy and the E ects of is Type of Cancer Treatment
BY JEAN YUAN '25
Advertisement
Cover Image: is speci c machine uses external beam radiation therapy in which the radiation oncologist can target a certain area of the body with radiation and damage the cells in that area.
Image Source: Flickr What is Radiation erapy?
Radiation oncology refers to the eld in medicine in which doctors study and treat cancer with various methods of radiation therapy. Cancer cells, abnormal cells that are no longer responsive to body signals that control cellular growth and death, divide without control, leading to the invasion of nearby tissues (O’Connor & Adams, 2010). Radiation therapy involves targeting these cancer cells with regulated doses of high-energy radiation with the goal of killing these cells while also minimizing the amount of radiation dose to the normal cells, thereby preserving the organs and other healthy tissues. e therapy causes damage to the DNA of the cancer cells by ionization, leading to loss of the cell’s ability to reproduce and eventually leading to cell death (Baskar et al., 2012). Ionization is when ions are introduced to a certain part of the body in order to release their energy and remove an electron, ultimately causing damage to cells in that are. However, this kind of therapy also a ects the division of cells of normal tissues. Damage to normal cells can cause unwanted side e ects, such as radiation sickness (nausea, vomiting, diarrhea, etc.) and secondary cancer/malignancies. A radiation oncologist oversees nding the right balance between destroying cancer cells and minimizing damage to normal cells. Radiation therapy cannot kill the cancer cells immediately. It takes only ten to een minutes to conduct the treatment, but it can take up to eight weeks in order to see results. Even a er months post treatment, cancer cells will continue to die (Baskar et al., 2012; National Cancer Institute, n.d.).
Types of Radiation erapy
ere are two types of radiation therapy: external beam radiation therapy and internal beam radiation therapy (Baskar et al., 2012; National Cancer Institute, n.d.). e type that is administered depends on a few di erent factors: “type of cancer,” location of the cancerous tumor, health and medical history of the patient, previous treatments of the patient, and age of the patient (National Cancer Institute, n.d.).
In external beam radiation therapy, a machine administers radiation at the a ected area and sends radiation to that area from various directions in order to target the cancerous tumor. is type of radiation therapy is spot treatment and only treats a speci c part of the body (Washington & Leaver, 2015). It is commonly used on cancers
of the breast, lung, prostate, colon, head, and neck. ere are many types of external beam radiation therapy (Schulz-Ertner & Jäkel, 2006). ey each rely on a computer to analyze the tumor in order to create an accurate treatment program. ere is 3-D conformal radiation therapy (3DCRT), intensity-modulated radiation therapy (IMRT), image-guided radiation therapy (IGRT), and stereotactic body radiation therapy. 3-D conformal radiation therapy (3DCRT) uses the radiation beams to allow for accurate tumor and matches the shape of the tumor in order to minimize the growth of the tumor and leave less room for error. Intensity-modulated radiation therapy (IMRT) is linear and utilizes linear accelerators, high-energy rays with pinpoint accuracy, in order to precisely distribute radiation at the cancerous tumor and to try to prevent damage to the healthy tissue (Baskar et al., 2012). Image-guided radiation therapy (IGRT) is used when the area that needs to be treated is in close proximity to a critical structure, such as moving organs. It takes images and scans of the tumor to help doctors position the radiation beams in the correct spot. Lastly, stereotactic radiation therapy uses 3-D imaging to focus the high doses radiation beams on the cancerous tumor in order to try preserve as much healthy tissue as possible. Due to the high dose treatment, the tissue around will be damaged, but it lessens the overall amount of healthy tissue damaged. is type has proven positive results for treatment in early-stage lung cancer for patients un t for surgery (Baskar et al., 2012; Sadeghi et al., 2010; Xing et al., 2005; National Cancer Institute, n.d.). as few healthy cells as possible (Washington & Leaver, 2015; National Cancer Institute, n.d.). If an implant is delivered, the type of implant depends on the type of cancer. If a permanent implant is administered, the radiation fades over time. Examples of the cancers it is used to treat include prostate, gynecological organ cancer, and breast cancer (Sadeghi et al., 2010; National Cancer Institute, n.d.).

Internal radiation therapy, which is also more commonly known as brachytherapy, is more invasive in that an oncologist inserts radioactive materials at the site of the cancer. is radioactive material emits a high dose of radiation directly at the tumor, but also keeps the nearby tissue safe by a radioactive implant that is placed in or in close proximity to the tumor. e bene t of brachytherapy is the ability to deliver high doses of radiation to the tumor without damaging the surrounding healthy tissues. is method harms Dosage
Since normal cells are also exposed to the radiation during treatment of the cancerous cells, the dose of radiation is very important in determining the maximum dosage that can safely be administered. Multiple doses of a smaller amount of radiation are less damaging to the normal cells than one dose equivalent to the total dose (Xing et al., 2005; National Cancer Institute, n.d.). e concept of the therapeutic ratio, a ratio that compares the blood concentration at which a drug becomes toxic and the concentration at which the drug is e ective, becomes an important parameter when trying to achieve an acceptable probability of complications in the healthy tissue from the radiation and the probability of controlling the tumor (Tamarago et al., 2015). A key factor in the development, safety, and optimization of a certain treatment is to make sure there is a balance between the toxic and e ective concentrations, which is why the therapeutic ratio is an integral part of radiation therapy. ere must be balance between the dose prescribed, the tumor volume, and the organat-risk (OAR) tolerance levels (called isotoxic dose prescription (IDP)) (Zindler et al., 2018). IDP allows the radiation dose prescribed to be a prede ned balance between the normal tissue complication (estimates of the tolerance of the dosage for speci c organs and tissues) and the probability of controlling the tumor (Washington & Leaver, 2015; Zindler et al., 2018).
e goal of the radiation therapy plays a large role in what kind of radiation therapy is needed. When only a small dose of treatment is needed, usually to ease cancer symptoms, it is de ned as palliative care, in which the goal is to prevent or treat any symptoms or side e ects of cancer as early as possible in order to improve the quality of life and reduce pain (National Cancer Institute, n.d.). Too much radiation can cause unwanted side e ects due to the fact that radiation can kill healthy cells that are nearby. ere is a limit as to how much radiation a body can receive (usually the limit of radiation in a lifetime for one person is about 400 millisieverts, and annual radiation limits is about 20 millisieverts (National Cancer Institute, n.d.; Hall et al., 2006)). Any more than the recommended amount of radiation can lead " ere are two types of radiation therapy: external beam radiation therapy and internal beam radiation therapy."
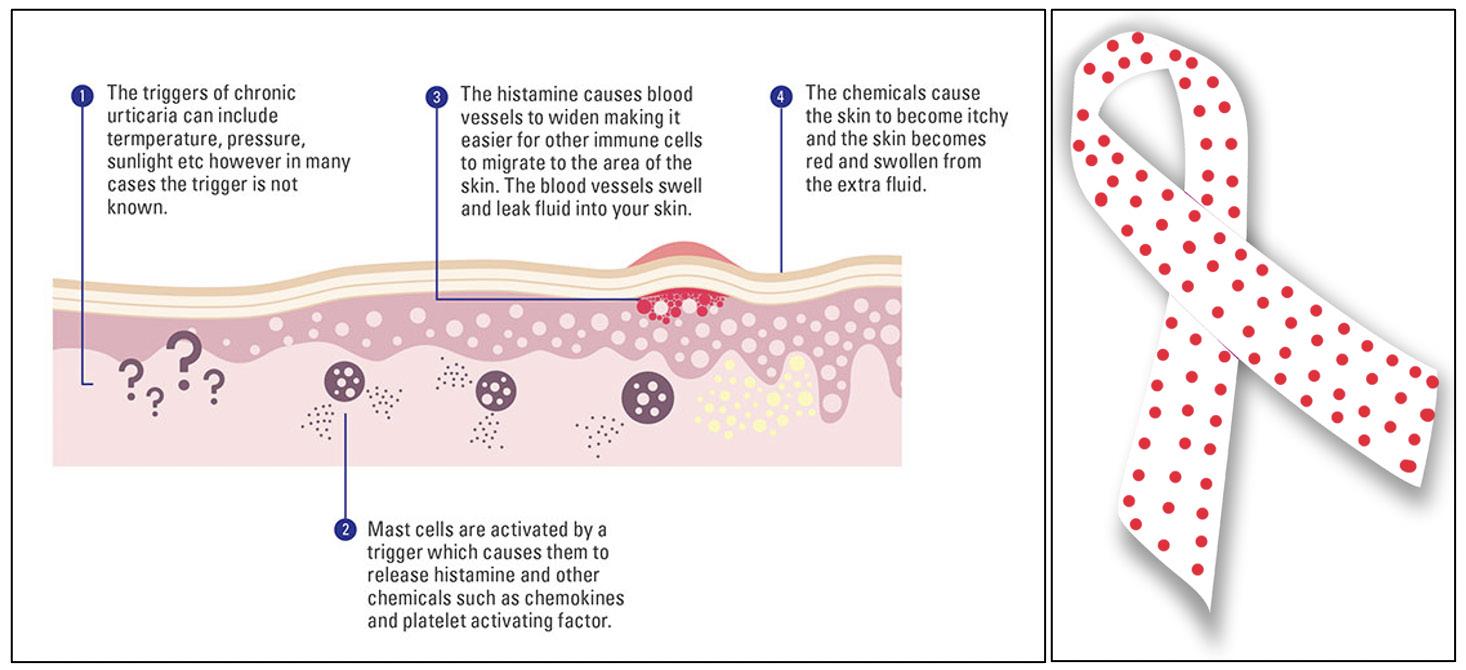
Image 1: Los Angeles, Route 101. Los Angeles is known for its extensive network of freeways around and within the city. Unfortunately, the construction of freeways heavily negatively impacted minority communities in the city, much like most others in the United States.
Image Source: Wikimedia Commons
Image 2: An image of the machine that can execute the external beam radiation therapy. is machine uses beams from three types of particles: photons, protons, and electrons (Baskar et al., 2012; National Cancer Institute, n.d.). Photon beams “do not stop” until they reach the cancerous tumor, travelling through normal tissue as well. Proton particles can also reach the deep tumors, but they “do not scatter radiation” as the photon beams do (National Cancer Institute, n.d.). However, there is a higher price for these machines, making the use of these very limited. Electron particles cannot travel as deep as the photon and proton beams and are mainly used for surface tumors (Schulz-Ertner et al., 2006; Washington & Leaver, 2015; National Cancer Institute, n.d.). Image Source: Flickr to long-term problems, such as a secondary cancer, which is a cancer that has either originated from the rst kind and has mediatized to another location of the body, or a secondary type of cancer that was caused from the treatments of the rst (which is more common with radiation therapy). Extreme amounts of radiation can even lead to death. e quantity of radiation can be determined by the concentration of radiation photons and the energy of the individual photons. If one area of a body has received the limit of radiation, another part of the body can only be treated with radiation therapy if it is far enough from the previous area (Sadeghi et al., 2010; National Cancer Institute, n.d.).
Dosage is more of a concern in internal radiation therapy. ere are two types of treatment: high-dose rate brachytherapy and low-dose rate brachytherapy (Xing et al., 2005; National Cancer Institute, n.d.). In high-dose rate (HDR) brachytherapy, the patient is treated for several minutes at a time with a powerful radiation source that is inserted in the body. e source is removed a er ten to twenty minutes and can be repeated a few times per day or once a day over a course of a few weeks, depending on the type of cancer and the type of treatment needed. For lowdose rate brachytherapy, an implant is le in for one to a few days, in which it emits lower doses of radiation over a longer period of time, and then removed. Usually, patients stay in the hospital while being treated. If permanent implants are needed, once the radiation is no longer present, they are harmless and there is no need to take these implants out (Sadeghi et al., 2010; National Cancer Institute, n.d.). Radiation erapy Alongside Other Cancer Treatments
Radiation therapy can be used as the only treatment for certain cancers, or it may be used in conjunction with chemotherapeutic agents and/ or surgery (Baskar et al., 2012; National Cancer Institute, n.d.; American Society of Clinical Oncology, n.d.). However, the point at which the radiation therapy can be administered depends on the type of cancer and whether the therapy is to ease or treat the cancer symptoms. About 50% of all cancer patients receive radiation therapy (Baskar et al., 2012). Medical oncologists and radiation oncologists work together to combine chemotherapy and radiation therapy in order to create a treatment plan where chemotherapy can be used to weaken the cancer cells in order for radiation therapy to work e ectively (Peters et al., 2000). Before surgery, radiation is combined in order to shrink the cancer (National Cancer Institute, n.d.). Combined surgery and radiation therapy, intraoperative radiation therapy administers radiation therapy to the tumor during surgery using either an external or internal radiation beam. It aids surgeons in moving away healthy tissue before administering the radiation and preserves the vital organs (Khaira et al., 2009). Radiation before surgery can even aid the surgery procedure by shrinking the tumor and making it easier to remove during surgery (National Cancer Institute, n.d.).
Side E ects of Radiation erapy
Side e ects of radiation therapy depend on the type of cancer, the location of the cancer, the radiation therapy dosage, and general health.


Common site-speci c side e ects of radiation therapy on the head and neck include nausea, mouth sores, hair loss, tooth decay, and di culty swallowing (Coia & Tepper, 1995; American Society of Clinical Oncology, n.d.). Side e ects of radiation therapy on the chest include di culty swallowing, shortness of breath, nipple soreness, shoulder sti ness, cough, fever, and radiation brosis (Gross, 1977; American Society of Clinical Oncology, n.d.). Radiation brosis is caused by permanent lung scars from untreated radiation pneumonitis, which is in ammation of the lung due to radiation therapy aimed at the chest. Radiation pneumonitis is seen in around 5 to 15 percent of patients with breast cancer, lung cancer, or patients with mediastinal tumors (Berkey, 2010; American Society of Clinical Oncology, n.d.). Side e ects of radiation therapy on the stomach and abdomen include loss of appetite, nausea, vomiting, bowel cramping, and diarrhea (Coia & Tepper, 1995; American Society of Clinical Oncology, n.d.). ese side e ects make it di cult to eat which is detrimental to the healing process since the body uses a lot of energy during radiation therapy. Patients need to consume a higher-than-normal amount of calories and protein to maintain body weight during therapy. Side e ects of radiation therapy on the pelvis include diarrhea, rectal bleeding, loss of bladder control, bladder irritation, sexual problems, and lowered sperm count or changes in menstruation (Berkey, 2010; Coia & Tepper, 1995; American Society of Clinical Oncology, n.d.). ese reactions begin around the second or third week of treatment and can last several weeks a er treatment ends. Palliative care is used here to ease these symptoms (Baskar et al., 2012; American Society of Clinical Oncology, n.d.).
Common physical side e ects of radiation therapy include skin changes and fatigue (Berkey, 2010; American Society of Clinical Oncology, n.d.). Skin changes may include dryness of the skin, itching, and blisters, depending on which part of the body received the therapy (radiation dermatitis). is is a common side e ect of radiation therapy to the breast, prostate, head, and neck. ese side e ects usually decrease a few weeks a er treatment ends. However, some side e ects, such as a second cancer, become long term e ects a er treatment. Second cancer is a new type of cancer that develops due to the treatment, usually around 10 to 15 years a er the initial treatment. e common emotional side e ects include coping with uncertainty, stress, anger, anxiety, depression, fear, and guilt. e prevalence of this goes from 0 to 60 percent, depending on the population being studied (Berkey, 2010).
Side e ects vary depending on the person and the type of cancer, which is why it is important to stay alert when receiving treatment and to be in touch with a healthcare team in order to watch for these side e ects. ese side e ects happen due to the fact that the radiation is killing not only the cancer cells, but also damaging healthy cells. is damage to the healthy cells is what is causing the side e ects. It is also important to stay in touch with a dietitian in order to keep the caloric and protein intake up to par and maintain weight (Berkey, 2010; Peters et al., 2000; National Cancer Institute, n.d.; American Society of Clinical Oncology, n.d.).
Image 3: is is an image of Brachytherapy in the prostate. Radioactive seeds, or pellet, are implanted into the prostate gland in order to kill the prostate cancer. ese seeds are able to emit high or low amounts of radiation depending on the cancer. Image Source: Wikimedia Commons
Baskar R, Lee AK, Yeo R, Yeoh KW. (2012 Feb 27). Cancer and Radiation erapy: Current Advances and Future Directions. Chicago, Illinois. International Journal of Medical Sciences. Retrieved from https:// www.medsci.org/v09p0193.htm.
Berkey FJ. (2010 August 15). Managing the Adverse E ects of Radiation erapy. Penn State College of Medicine, Hershey, Pennsylvania. American Family Physician, 82 (4): 381-388. Retrieved from https:// www.aafp.org/afp/2010/0815/p381.html.
Brachytherapy to Treat Cancer. (n.d.). National Cancer Institute. Retrieved from https://www. cancer.gov/about-cancer/treatment/types/radiationtherapy/brachytherapy.
Coia LR MD., Tepper JE MD. (30 March 1995). Late e ects of radiation therapy on the gastrointestinal tract. International Journal of Radiation Oncology Biology Physics, 31 (5): 1213-1236. Retrieved from https://www.redjournal.org/article/03603016(94)00419-L/pdf.
Curative Radiation erapy. (n.d.). National Cancer Institute. Retrieved from https://training.seer.cancer. gov/treatment/radiation/therapy.html
External beam radiation therapy for cancer. (n.d.). National Cancer Institute. Retrieved from https:// www.cancer.gov/about-cancer/treatment/types/ radiation-therapy/externalbeam
Gross N.J M.D. (1977 January 1). Pulmonary E ects of Radiation erapy. Department of Medicine, Annals of Internal Medicine, 1-12. Retrieved from https://doi.org/10.7326/0003-4819-86-1-81.
Hall JD, Godwin M MD, Clarke T MD. (10 August 2006). Lifetime Exposure to Radiation from Imaging Investigations. U.S. National of Medicine National Institutes of Health, O cial Publication of e College of Family Physicians of Canada. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/articles/ PMC1781500/.
Khaira M, Mutamba A, Meligonis G, Rose GE, Plowman PN, O’Donnell H. (8 July 2009). e Use of Radiotherapy for the Treatment of Localized Orbital Amyloidosis. Taylor & Francis Online, 27 (6): 432-437. Retrieved from https://doi. org/10.1080/01676830802350216.
O'Connor, C. M. & Adams, J. U. (2010). Essentials of Cell Biology. Cambridge, MA. NPG Education, 9798. Retrieved from https://web.iitd.ac.in/~amittal/ Peters WA III, Liu PY, Barrett RJ II, Stock RJ, Monk BJ, Berek JS, Souhami L, Gringsby P, Gordon W Jr., Alberts DS. (2000). Concurrent Chemotherapy and Pelvic Radiation erapy Compared with Pelvic Radiation erapy Alone as Adjuvant erapy A er Radical Surgery in High-Risk Early-Stage Cancer of the Cervix. Journal of Clinical Oncology, 18 (8): 16061613. Lippincott Williams and Wilkins. Retrieved from https://ascopubs.org/doi/abs/10.1200/ JCO.2000.18.8.1606.
Radiation erapy to Treat Cancer. (n.d.). National Cancer Institute. Retrieved from https://www. cancer.gov/about-cancer/treatment/types/radiationtherapy#:~:text=Radiation%20therapy%20(also%20 called%20radiotherapy,your%20teeth%20or%20 broken%20bones.
Sadeghi M, Enferadi M, Shirazi A. (29 November 2010). External and internal radiation therapy: Past and future directions. Journal of Cancer Research and erapeutics, 6 (3): 239-248. Retrieved from https://www.cancerjournal.net/text. asp?2010/6/3/239/73324.
Schulz-Ertner D MD., Jäkel O PhD., Schlegel W PhD. (available online 27 September 2006). Radiation erapy With Charged Particles. Seminars in Radiation Oncology, 16 (4) Retrieved from https:// doi.org/10.1016/j.semradonc.2006.04.008.
Side E ects of Radiation erapy. (n.d.). American Society of Clinical Oncology (ASCO), Cancer.Net. (September 2020). Retrieved from https://www. cancer.net/navigating-cancer-care/how-cancertreated/radiation-therapy/side-effects-radiationtherapy
Tamarago J, Le Heuzey JY, Mabo P. (15 April 2015). Narrow therapeutic index drugs; a clinical pharmacological consideration to ecainide. U.S. National of Medicine National Institutes of Health, European Journal of Clinical Pharmacology. Retrieved from https://www.ncbi.nlm.nih.gov/pmc/ articles/PMC4412688/
Understanding Radiation erapy. (n.d.). American Society of Clinical Oncology (ASCO), Cancer.Net. (September 2020). Retrieved from https://www. cancer.net/navigating-cancer-care/how-cancertreated/radiation-therapy/side-effects-radiationtherapy
Washington CM, Leaver DT. (2015). Principles and Practice of Radiation erapy. 4th edition. Elsevier Mosby. 156, 293, 536. Retrieved December 2, 2021.
Xing L PhD., orndyke B PhD., Schreibmann E PhD., Yang Y PhD., Li TF PhD., Kim GY PhD., Luxton G PhD., Koong Albert MD. (21 December 2005). Overview of Image-Guided Radiation erapy. Stanford, CA. Medical Dosimetry, 1-22. Retrieved from https://doi.org/10.1016/j.meddos.2005.12.004.
Zindler, J.D., Schi elers, J., Lambin, P. (18 January 2018). Improved e ectiveness of stereotactic radiosurgery in large brain metastases by individualized isotoxic dose prescription: an in silico study. Strahlenther Onkol, 194, 560–569. Retrieved from https://doi.org/10.1007/s00066-018-1262-x