

PLUS ❯ Meet the 2018 Behavioral Healthcare Champions ❯ 7 tips for better payer contracts SUMMER 2018 • VOL. 39, NO. 3 • WWW.BEHAVIORAL.NET Live coverage from NCAD at behavioral.net Led by Alan B. Miller, UHS aims to avoid taking on too much too fast SEEKING SENSIBLE





2018 Title Sponsor National Conference on Addiction Disorders Furthering recovery by engaging clinicians in conversations based on analytics, cutting-edge research, and trust Learn more about Dominion Diagnostics online at: www.dominiondiagnostics.com | @domdiag Part of the addiction treatment and recovery community for more than two decades, Dominion Diagnostics delivers the most sophisticated, actionable clinical information to treatment professionals, and supports them with the latest technologies and best education available as they work to improve outcomes.

EDITORIAL Senior Editor Tom Valentino tvalentino@iabhc.com
Editor Gary A. Enos genos@iabhc.com
SALES
All inquiries please contact Katrina Hall khall@iabhc.com
All ad materials should be sent electronically to: https://www.hmpglobal.com/ads/
North American Center for Continuing Medical Education, LLC an HMP Company 104 Windsor Center Drive, Suite 200, East Windsor, NJ 08520 609.371.1137 www.naccme.com
BUSINESS
President Randy Robbin

Director, Institute for The Advancement of Behavioral Healthcare Doug Edwards
Associate Director, Production Andrea Steiger
Graphic Designer Karen Copestakes
Production/Circulation Director Kathy Murphy
Audience Development Manager Bill Malriat
Circulation Manager Bonnie Shannon
Behavioral Healthcare Executive (ISSN 1931-7093, Online 2167-9649) is published 4 times per year by NACCME, 104 Windsor Center Drive, Suite 200, East Windsor, NJ 08520.
Behavioral Healthcare Executive is a trademark of NACCME. All rights reserved. No part of Behavioral Healthcare Executive may be reproduced, distributed, transmitted, displayed, published, or broadcast in any form or in any media without prior written permission of the publisher. To request permission to reuse this content in any form, including distribution in educational, professional, or promotional contexts or to reproduce material in new works, please contact Katrina Hall: khall@iabhc.com.
EDITORIAL: Behavioral Healthcare Executive is the practical resource for intelligence that executives can apply to meet current leadership, financial, clinical, technology, and compliance needs. Behavioral Healthcare Executive is indexed in the National Library of Medicine’s MEDLINE/ PubMed database. Articles and opinions published in Behavioral Healthcare Executive do not necessarily reflect the views of NACCME or the Editorial Advisory Board.
SUBSCRIPTIONS: For questions about a subscription or to subscribe, please contact us: 888-244-5310, http://www.iadvance behavioralhealthcare.com/subscribe, or VendomeHM@emailpsa.com. Subscription rate per year: $140 domestic, $169 outside the US. Single copies and back issues: $20 Domestic, $32 outside the US.
POSTMASTER: Send changes of address to Behavioral Healthcare Executive, 70 E Swedesford Rd, Suite 100, Malvern, PA 19355.
© 2018, North American Center for Continuing Medical Education, LLC, an HMP Company. All rights reserved. Reproduction in whole or in part prohibited. Opinions expressed by authors, contributors, and advertisers are their own and not necessarily those of NACCME, the editorial staff, or any member of the editorial advisory board. HMP is not responsible for accuracy of dosages given in articles printed herein. The appearance of advertisements in this journal is not a warranty, endorsement or approval of the products or services advertised or of their effectiveness, quality or safety. Rapid advances in medicine may cause information contained here to become outdated, invalid or subject to debate. Accuracy cannot be guaranteed. NACCME disclaims responsibility for any injury to persons or property resulting from any ideas or products referred to in the articles or advertisements. Content may not be reproduced in any form without written permission.
CONTENTS | SUMMER 2018 2 SUMMER 2018 BEHAVIORAL HEALTHCARE EXECUTIVE WWW.BEHAVIORAL.NET IN THIS ISSUE EDITOR'S LETTER 4 Behavioral Healthcare Champions’ clinical roots guide their success as executives BY TOM VALENTINO PERSPECTIVES 6 Compliance is the heart of your organization BY MAEVE O’NEILL, MED, LCDC, LPC-S, CDWF 10 Federal, state sober-living regulations intersect BY LILLIE SINGH, ESQ NEED TO KNOW 8 An NIH study shows medication reduces overdose risk BY JULIE MILLER MANAGEMENT 15 2018 Behavioral Healthcare Champions BY TOM VALENTINO 19 Seven tips for better payer contracts BY BRIAN ALBRIGHT POLICY 24 Raids cause larger concern for MAT providers BY JULIE MILLER CLINICAL TRENDS 28 Minimize risk when patients leave AMA BY JILL SEDERSTROM DESIGN FOCUS 33 Consider protections for specific patient populations BY JOANNE SAMMER TECHNOLOGY 36 Experts debate 42 CFR Part 2’s modern role BY ALICIA HOISINGTON COVER STORY Led by Alan B. Miller, UHS aims to avoid taking on too much too fast BY JULIE MILLER 12
Fort Lauderdale, FL Bonaventure Resort & Spa
The opioid crisis is making headlines, but another category of drugs continues to devastate communities: stimulants. Cocaine is ooding Southern states as production increases to record levels in South America. Meth remains an omnipresent scourge. And college students across the country continue to misuse prescription drugs to boost academic performance. Together these “twin epidemics” are overwhelming law enforcement and treatment providers.
Yet there are many reasons for hope, as this crisis is not going unnoticed. Clinical professionals, whether part of larger systems or in private practice, are in an ideal position to discuss with their clients why stimulants are no less dangerous than opioids, as well as address the trauma and shame histories that often lead to substance use. Law enforcement of cials are taking steps to educate their teams and communities about effective strategies for removing these drugs from the streets. And multiple stakeholders are working together to prevent stimulant use, provide access to treatment, and ensure that stimulants are part of larger societal discussions about addressing drug use.
Featured Speakers



Jim Hall, PhD Nationally Recognized Epidemiologist, Center for Applied Research on Substance Use and Health Disparities, Nova Southeastern University



Who Should Attend
• Private Practice Therapists

• Psychologists
• Clinicians, counselors, social workers, interventionists

• Law enforcement: Chiefs of police, sheriffs, detectives
• Public health and prevention of cials
• Federal, state, and local of cials and lawmakers
Justin L. Miller, PhD Field Intelligence Manager, DEA Miami Field Division

John Dyben, DHSc, MCAP, CMHP Distinguished Clinical Trainer on Addiction and Recovery
Siobhan Morse MHSA, CRC, CAI, MAC Leading Addiction Treatment and Outcomes Researcher David Fawcett, PhD, LCSW Author and Expert on Meth Use in LGBT Community

NOVEMBER 12-14, 2018
Full agenda, speaker bios, and more, visit: www.StimulantSummit.com
Mark S. Gold, MD Internationally Recognized Cocaine and Addiction Researcher
Be part of the discussion. Be part of the solution. Join us for the inaugural National Cocaine, Meth & Stimulant Summit.
Champions' clinical roots guide success as executives
ach year, Behavioral Healthcare Executive sets out to recognize some of the industry’s finest leaders with its Behavioral Healthcare Champions awards program. This year’s winners, all profiled in this issue, are an especially diverse bunch—geographically and demographically, representing both for-profit and not-for-profit organizations and various sectors of the field. Speaking with each winner, though, a common thread emerged: They might have corner offices now, but each relies heavily on clinical experience to guide their business decision-making.
“I have to make sure we pay our bills and do what we need to do on the business side of things, but whenever there are financial vs. clinical decisions, I feel like I can speak to both and hopefully make the best decision,” says New Vista Behavioral Health CEO Stephen Odom, LMFT, PhD. “It’s helped a lot with my teams that they see me as someone who has been in the trenches where they are.”
Not only has Odom been in the trenches, he still is. Shortly before taking the time to speak with Behavioral Healthcare Executive on a recent Monday afternoon, he met with his staff to discuss a current case. In addition to being the CEO, Odom remains New Vista’s chief clinical officer.
David Vennes, MPNA, LADC, is rightfully proud of the turnaround he has overseen at NUWAY since taking over as executive director and CEO. But his first year back in the field after working through his own 10-year battle with addiction was spent as a counselor at NUWAY. Looking back, he considers the experience “a wonderful time” in which he got back to his roots. “I hadn’t done clinical work in forever,” Vennes says.
In New Orleans, the clinical background of Rochelle Head-Dunham, MD, has been integral in the overhaul of the operations at the Metropolitan Health Services District. Even today, Head-Dunham, MHSD’s executive director and medical director, says she is a psychiatrist first and foremost.
“At the end of the day, understanding people and how to relate to them, and read situations and settle situations in a manner that allows for the ship to keep sailing has been tremendously advantageous,” she says.
The work these three leaders are doing is remarkable, and we celebrate their accomplishments in this issue of Behavioral Healthcare Executive. We invite you to do the same by joining us when we honor the 2018 Behavioral Healthcare Champions at the National Conference on Alcohol & Addiction Disorders, which will be held Aug. 19-22 at Disneyland in Anaheim, Calif.
Tom Valentino, Senior Editor
ADVISORY BOARD
David Chernof, MSW, LCSW, MBA

Consultant, Behavioral Help, LLC;
Associate Clinical Director, Queen of Peace Center
Patrick Gauthier
Director, AHP Healthcare Solutions
Nancy Hale
Program Director, Operation UNITE
Andrew Kessler
Founder and Principal, Slingshot Solutions
Jean Krisle
Founder and CEO, 10,000 Beds
Edward R. Jones, PhD
Senior VP for Strategic Planning, Institute for Health and Productivity Management
Ron Manderscheid, PhD
Executive Director, National Association of County Behavioral Health and Developmental Disability Directors
Steven Millette
Director, Gloo Inc.
Linda Rosenberg
President/CEO, the National Council on Behavioral Health
Raymond Tamasi
President, Gosnold on Cape Cod
Doug Tieman
President/CEO, Caron Treatment Centers
Mary Woods CEO, WestBridge
70 E. Swedesford Rd., Suite 100 Malvern, PA 19355 800.237.7285 www.hmpglobal.com
ADMINISTRATION
Chairman & Chief Executive Officer Jeff Hennessy
Executive Vice President Of Operations Anthony Mancini
Senior Vice President Of Finance
Greg Salter
Controller Meredith Cymbor-Jones
VICE PRESIDENT OF MARKETING & PUBLIC RELATIONS Kelly McCurdy
Senior Director, Digital Strategy And Media Tim Shaw
Senior Creative Director Vic Geanopulos
Senior Manager, IT Ken Roberts
LETTER FROM THE EDITOR 4 SUMMER 2018 BEHAVIORAL HEALTHCARE EXECUTIVE WWW.BEHAVIORAL.NET


Visit Booth 514 For more information, visit VIVITROL.com/hcp ALKERMES and VIVITROL are registered trademarks of Alkermes, Inc. ©2017 Alkermes, Inc. All rights reserved. VIV-002837 Printed in the U.S.A. vivitrol.com/hcp YES... IT IS STILL A GOOD TIME TO FIRE THAT SEO GUY & HIRE DREAMSCAPE MARKETING. S earch E ng ine O ptimi zation. Content Marketing. Web Desi g n & De velopmen t. PP C A dver ti sin g. CALL US AT (888) 307-7304
Compliance is the heart of your organization
Our daily work impacts our patients
hen I was first talking with Addiction Campuses about a potential job, I said I wanted the title “chief heart officer.” When the organization offered me a position as vice president of compliance, I joked, “What says ‘heart’ more than compliance?”
But, it turns out I was right. And the lessons I have learned in my compliance leadership position over the past year have continued to reinforce the idea that as behavioral health professionals, we could all benefit from a heart-focused compliance and ethics program in our organizations.
Over my 30 years working in behavioral health, the compliance department has either not existed in the organization at all, or if it did exist, it was a reactive program to address the issues at hand, such as a confidentiality breach, a patient incident or staff misconduct. Certainly, the current state of our industry, which includes ethical complaints, court cases and legal battles, indicates that we have a critical need for more preventive and less reactive compliance programs.
It has been a huge learning experience as I research compliance programming in other industries to fully understand what is needed for a model behavioral healthcare compliance program. Since our daily work impacts the lives of our patients, their families, their collateral contacts and our staff, it seems imperative to build a program that is heart-centered that truly prevents, identifies and fixes problems just as the Health Care Compliance Association recommends.
When we commit the resources of a person or a department focused on compliance that is able to provide all the needed
BY MAEVE O’NEILL, MED, LCDC, LPC-S, CDWF
components and hardwire the concepts in all levels of the organization, we can avoid ethical problems or minimize their impact. As behavioral health executives, our goal is to build organizations that are financially and clinically sound with positive patient and staff outcomes.
It seems to me this is where the heart-focused compliance function is a necessity. It starts with policies and procedures that are seen as guides to our daily behaviors. When was the last time you read and used your policy manual? Consider regular oversight of the daily practices that implement the policies. At Addiction Campuses, we do this with monthly calls with each operational department to review policies, practices and any current issues. And ongoing staff education and training on all things compliance ensures staff can ask questions, bring up concerns and learn from each other.
We in behavioral health can bring genuine heart to our industry through compliance. I am so grateful that I get to do this work and bring my clinical and executive experience to the job. It truly is my heart and my mission over the next 30 years of my career to contribute to building a model behavioral health compliance program.
If we can encourage every conference and event to include the topics of compliance and ethics from a heart perspective, we can share best practices. This will help us all engage staff, empower teams and enhance organizational cultures based on compliance and ethics that are embedded in our services to support quality, safe care for patient and staff outcomes.
PERSPECTIVES 6 SUMMER 2018 BEHAVIORAL HEALTHCARE EXECUTIVE WWW.BEHAVIORAL.NET
Maeve O’Neill, MEd, LCDC, LPC-S, CDWF, is vice president of compliance for Addiction Campuses.
RENOVATE / DESIGN YOUR NEW BATHROOM
BestCare® LIGATURE-RESISTANT fixtures ultimately reduce ligature points to ensure a safer and more secure behavioral healthcare environment.
TYPICAL BESTCARE® LIGATURE-RESISTANT PLUMBING FIXTURES & ACCESSORIES

DO YOU SEE THE LIGATURE POINTS? LIGATURE POINTS IN A TYPICAL BATHROOM
In traditional restroom applications, ligature points are more common than you might realize. The arrows above indicate dangerous ligature points in existing bathrooms.
Did you know? Most inpatient suicides occur in the facilities bathrooms.
FOR MORE INFORMATION: whitehallmfg.com •1-800-782-7706

6 4 5 1 2 3 7 9 8 11 12 10 3 9
1. Showers
2. Soap Dishes
3. Grab Bars
4. Sinks
5. Shelves
6. Mirrors
7. Paper Towel Dispensers
8. Tank Style Toilets
9. Towel/Clothes Hooks
10. Spindle-less Toilet Paper Holders
11. Linear Drains
12. Floor Drains
SPONSORED CONTENT
NEED TO KNOW Medication reduces overdose risk
Buprenorphine and methadone can help patients at risk for fatal overdose
BY JULIE MILLER
A National Institutes of Health (NIH) study found that treatment of opioid use disorder with either methadone or buprenorphine following a nonfatal opioid overdose is associated with significant reductions in opioid-related mortality. The research, presented in June in the Annals of Internal Medicine, is the first study to look at the association between medication assisted treatment and mortality among overdose patients.
Study authors analyzed data from 17,568 adults in Massachusetts who survived an opioid overdose between 2012 and 2014. Compared to those not receiving medication assisted treatment, opioid overdose deaths decreased by 59% for those receiving methadone and 38% for those receiving buprenorphine in one year’s time. The authors were unable to analyze naltrexone in the same study.
Despite clinical evidence that medication assisted treatment can help many people recover from opioid addiction, the modality remains greatly underutilized. Less than one third of patients were provided any medication. In the one-year study period, only 11% received methadone, 17% received buprenorphine and 6% received naltrexone. Authors note 5% received more than one medication.
The median use of methadone was five months, buprenorphine was four months, and naltrexone was one month.
Authors were concerned that 34% of people who experienced an overdose were subsequently prescribed one or more prescriptions for opioid painkillers over the next 12 months, and 26% were prescribed benzodiazepines.
In an editorial commenting on the study, Nora Volkow, MD, and Eric Wargo, PhD, of the National Institute on Drug Abuse, called for changing policies to make the medications that treat opioid use disorder more accessible. They called for educating primary care and emergency providers on the fact that opioid addiction is a medical illness that must be treated aggressively with the tools that are available.
Source: National Institutes of Health, Annals of Internal Medicine, http://annals.org/aim/article-abstract/2684924/medication-opioid-use-disorder-after-nonfatal-opioid-overdose-association-mortality
8 SUMMER 2018 BEHAVIORAL HEALTHCARE EXECUTIVE WWW.BEHAVIORAL.NET
SPONSORED CONTENT
Federal, state sober-living regulations intersect
here have been many news stories and other reports that suggest federal laws prohibit state and local governments from regulating sober living facilities. That is not entirely true.
The Fair Housing Act (FHA) and Americans with Disabilities Act (ADA) are two federal laws that prevent discriminatory housing practices against individuals with disabilities. Substance use disorders are a cognizable “disability” for the purposes of both the FHA and ADA, and individuals suffering from the disorders constitute a “protected class.”
Under the FHA, state and local governments are prohibited from enacting or enforcing land use or zoning laws that discriminate against persons because of a legally protected characteristic. Meanwhile, the ADA prohibits discrimination against individuals with disabilities in all areas of public life, including public accommodations. Both the FHA and ADA require public entities to grant “reasonable accommodations” so that individuals with disabilities can access equal housing opportunities.
Given the protections of these federal laws, state governments are indeed limited in what they can do when it comes to individuals with substance use disorders.
For example, a state government or a local municipality could not prohibit treatment centers from operating in circumstances where they allowed treatment facilities for other conditions. They could not create a public housing program that excluded individuals that struggled with alcohol use in the past. Yet, it is worth noting that the disability protections do not protect individuals engaged in active drug use, regardless of the individuals’ diagnosis. States are still free to prohibit illegal drug
use, public intoxication or driving while under the influence.
Courts play close attention to sober living-related laws that are challenged as violations of the FHA, ADA or comparable state protections. In general, laws may be either “facially discriminatory,” where a law directly targets a protected class, or laws may be discriminatory “as applied,” where the law has the effect of hurting a specific group or where the law was enacted with discriminatory intent.
Until recently, many of the laws aimed at regulating or limiting sober living houses had neutral language and purported to treat all group residences with certain occupancy rates the same. These facially neutral laws did not mention sober living facilities specifically. In the last few years, however, there are more laws that target sober living facilities explicitly.
For example, the rules may require recovery residences to abide by certain health and safety standards or to obtain optional certification to receive referrals from licensed treatment providers in the state.
The exact tests and levels of scrutiny that courts apply when evaluating an allegedly discriminatory law vary by jurisdiction and by the circumstances. Violations of the federal protections may occur where, for example, there is:
1. Disparate treatment or intentional discrimination;
2. Disparate impact of a law, practice, or policy on a protected class; or
3. A failure by the local government to make reasonable accommodations in rules, policies or practices so as to afford people with disabilities an equal opportunity to live in a dwelling.
In general, courts have held that laws may treat a protected class differently if the restriction is intended to benefit the protected group or responds to legitimate safety concerns
PERSPECTIVES 10 SUMMER 2018 BEHAVIORAL HEALTHCARE EXECUTIVE WWW.BEHAVIORAL.NET
The Fair Housing Act and Americans with Disabilities Act are two federal laws that prevent discriminatory housing practices
BY LILLIE SINGH, ESQ.
raised by affected individuals. At the same time, there must be reasonable accommodations granted under the FHA and ADA where the accommodations or legal exceptions are necessary to afford individuals with disabilities an equal opportunity to use and enjoy housing.



The boundaries of the federal protections under the FHA and ADA are not always clear, especially when it comes to regulating sober living houses, which offer no treatment services. Lawyers for sober living operators have argued violations of the FHA and ADA resulting from laws that required sober living homes to abide by strict, burdensome and prohibitively expensive requirements, like mandates to have a doctor on premises 24 hours a day or fire codes that would cost hundreds of thousands of dollars in housing repairs to satisfy. These types of rules and regulations are often held to be invalid as applied because they prevent people in recovery from obtaining the housing they needed to deal with their disability and have the effect of harming a class of individuals protected by federal and state laws.






Refusing to grant a reasonable accommodation to such a provision, as would be necessary to afford the residents an equal opportunity to use and enjoy a dwelling, may constitute a violation of federal law. Some sober living operators who successfully challenged these types of laws in court have been awarded damages against the cities or other government entities that tried to prevent them from operating.






There have been few challenges to the new crop of state laws requiring sober living residences to obtain some level of licensure or certification from the state in order to receive certain referrals, apply for state funding, or to operate at all. Operators of sober living facilities are eagerly awaiting further clarification on whether voluntary and mandatory licensure requirements will be upheld if they are challenged as violations of federal laws like the ADA and FHA.

























PERSPECTIVES WWW.BEHAVIORAL.NET 11
800. 969. 4100 www.furnitureconcepts.com info@furnitureconcepts.com FURNITURE CONCEPTS DURABLE Secure Furniture Wood, Metal & Molded Plastic Bedsrooms. Mattresses, Dining, Seating and More. ® ® n f o Me al Beds & Casegoods Ma resses L ob bies & C ommon Rooms Solid Wood Furni ure Comple e Bedrooms An i-Con raband Dependable Uphols ered Sea ing Dining Super Rugged Beds Bedbug Solu ions! Affordabe Furn iure Furni ure for Secure Environmen s S ylish & Func ional Incon inence-Fluid Solu ions Limi ed Mobili y Furniture_Concepts_Behavioral_Health_Ad.qxp_Furniture_Concepts_Ad 4/25/18 5:05 PM Page 1
Lillie Werner Singh is an attorney focusing healthcare matters and serves as a consulting attorney for the Behavioral Health Association of Providers.
SEEKING SENSIBLE
Led by Alan B. Miller, UHS aims to avoid taking on too much too fast

 BY JULIE MILLER
BY JULIE MILLER
COVER STORY 12 SUMMER 2018 BEHAVIORAL HEALTHCARE EXECUTIVE WWW.BEHAVIORAL.NET
Alot has changed in the healthcare landscape since 1979, when Alan B. Miller founded Universal Health Services (UHS), an organization that has become one of the largest providers in the nation with revenue now exceeding $11 billion. Whole-person care has now become a strategic expectation, meanwhile, value propositions are ever more important as stakeholders look for the best balance of quality and cost.
By all accounts, the business is on a consistently upward trajectory. UHS’s 300 behavioral health sites have been recording a continuous rise in admissions, licensed beds and patient days. Most notably, in September 2015, UHS completed its $350 million deal to acquire Foundations Recovery Network—one of the legacy brands in addiction treatment. Additionally, last year alone, UHS added more than 400 behavioral health beds as part of its ongoing capital expansion. The division reported 3% growth in the first quarter of 2018.
As chairman and CEO, Miller still speaks of the almost 40-year-old enterprise as if it were a small entrepreneurial business.



“We’re not concerned with being the biggest,” Miller tells Behavioral Healthcare Executive. “We just want to have the most efficient patient care aspects.”
He believes too many prominent healthcare companies have failed because they outgrew their capabilities and failed to deliver on what they promised. Miller wants UHS to remain an organization that never takes on more than it can manage, in spite of the constant flow of new investment opportunities in mental health and addiction treatment services today.
There are no immediate plans to build additional locations under the Foundations brand. Instead, Miller says, the staffing level is being built up and training is being offered.
”We can only expand when we feel we have excellent staff that can properly address the patients’ needs,” he says. “We’re not interested in dazzling Wall Street. We’re interested in taking care of patients, and Wall Street will follow. Obviously we need investors’ money, but we’re in a very strong financial position—I think without question, the strongest in the industry.”
A publicly traded company, UHS also operates acute care facilities and a healthcare real estate investment trust. The behavioral health operations saw $810 million in profits before taxes last year on $4.9 billion in net revenue. By comparison, the acute-care facilities saw $459 million on $5.5 billion in revenue.
PARTNERSHIP MODELS
On July 9, UHS opened the $30 million Lancaster Behavioral Health Hospital in Pennsylvania—a facility operated as a 50/50 partnership between UHS and Penn Medicine Lancaster General
Health. With a total of six units and 126 beds, the freestanding Lancaster facility will offer services for co-occurring disorders on the psychiatric-medical unit, as well as service in intensive adult and women’s trauma units.
“What we’re finding now is that the future [includes] people believing we’re going to have affordable care networks,” Miller says. “Big nonprofits realize they have concentrated well on acute care and have not paid attention to mental health. So when they want to expand and cover their portfolio, they come to us to partner and handle the mental health portion.”
UHS is advancing additional partnerships—including a $31 million, 100-bed psychiatric hospital near Des Moines, Iowa, slated to open in 2020—as well as other strategies for integration. Looking toward the future, the healthcare system at large is increasingly relying on comprehensive health measures for quality reporting and value-based payment models.
“We’ve always talked about the fact that when people are physically better from some acute care operation or treatment, but mentally, they’re not up to it, then then they’re not well,” Miller says.
The same is true for addiction treatment. He says he regards addiction as a chronic condition and recovery as a journey.
“In mental health or addiction treatment, people don’t talk about a cure,” he says. “They talk about being well.”
CHRONIC CONDITION CARE
Clinicians agree that recovery requires a lifelong care plan. Karen E. Johnson, UHS senior vice president, clinical services and division compliance officer, says that medication assisted treatment is one way of forwarding patients’ progress in recovery.
“We’re starting to see it more broadly in our hospitals, in our drug and alcohol treatment centers and in our outpatient centers,” Johnson says. “And that has become a more prevalent treatment modality over the years that we’ve utilized.”
WWW.BEHAVIORAL.NET 13
She says UHS mostly offers buprenorphine, but some of its Foundations Recovery Network facilities are using naltrexone. It’s a treatment choice that represents a potential growth area for UHS, she says.
Telehealth is also emerging for the substance use disorder patient population. UHS has leveraged the remote service capability for its psychiatric hospitals and plans to expand its use.
“With a focus on addiction as a chronic illness, telehealth allows us to connect and do family work, which is key to creating a network around each individual and a support system that allows people to fully engage,” Johnson says.
In most markets, payer protocols tend to favor more outpatient treatment for behavioral health services. Telehealth could be a less costly touchpoint that helps patients remain engaged, however, reimbursement will continue to be the main driver of telehealth adoption.
“I don’t see how someone with a serious problem can have
a few days’ stay and expect to recover with outpatient visits at best,” Miller says. “Many don’t go [to outpatient appointments] or only go for a short time, and they don’t follow up.”

WHAT’S NEXT
For the future, the outlook for UHS will continue to include the acute and behavioral health sides of the business. It’s the key differentiator that defines the company, Miller says.
“Over the years, I’ve heard advice saying we should sell the psychiatric division because acute care is more revenue and people will always be sick or injured,” Miller says. “I chose not to. I also heard other advice saying that mental health is the future, so why sell? We’ve been stubborn and stuck with both.”
His advice for treatment center operators is to hire good people and a build a reputation that resonates with communities.
WWW.BEHAVIORAL.NET
COVER STORY Our buying power. Your savings. commercialsales @mfrm.com mattressfirm.com/ commercialsales GET STARTED BY GETTING IN TOUCH 855.734.6484 Your patients deserve a great night’s sleep, and we’ll deliver it nationwide. Fast. • Wholesale pricing at your service • Fast nationwide delivery • Fast emergency replacements • No minimum purchase requirement • Removal and setup of old and new bedding WITH US, YOU’LL GET: MFCS_BehavioralHC_Care_7x4_875_FINAL.indd 1 7/10/18 5:25 PM
Julie Miller is a freelance writer based in Ohio.
2018 BEHAVIORAL HEALTHCARE CHAMPIONS
 BY TOM VALENTINO
BY TOM VALENTINO
Behavioral Healthcare Executive is proud to announce the outstanding leaders who have been selected as 2018 Behavioral Healthcare Champions. These three individuals are being honored for their dedication to the field, as well as their commitment to influence positive change and help more people in treatment on their road to recovery. Through their business achievements, the Champions have also been successful in advancing the mission and vision of their respective organizations.
The 2018 Champions were selected from an outstanding collection of nominees, each of whom are making a difference in the development, delivery and effectiveness of mental health and substance use disorder treatment services. Drawing from their clinical backgrounds, each of this year’s honorees have proven they can expand treatment services, be responsive to the needs of the communities they serve, and provide strong leadership that fuels strategic growth.
The 2018 Behavioral Healthcare Champions are:
• Rochelle Head-Dunham, executive director and medical director, Metropolitan Human Services District, New Orleans
• Stephen Odom, CEO and chief clinical officer, New Vista Behavioral Health
• David Vennes, executive director and CEO, NUWAY
JOIN US
TheBehavioralHealthcareChampionswillberecognized ataspecialceremonyduringtheNationalConferenceon AlcoholandAddictionDisorders(NCAD),whichwillbe heldAug.19-22inAnaheim,Calif.Formoreinformation, visit: vendome.swoogo.com/NCAD-2018
MANAGEMENT WWW.BEHAVIORAL.NET 15
Rochelle Head-Dunham, MD Executive Director and Medical Director, Metropolitan Human Services District, New Orleans
Since stepping into her role as executive director and medical director of the Metropolitan Human Services District in New Orleans in March 2016, Rochelle Head-Dunham, MD, has put a focus on strengthening the agency’s continuum of care, particularly for the area’s underserved minority population that is eligible for treatment. Along the way, she has built an empowered, educated clinical staff that is putting patients first, too.

Dunham describes the agency she inherited as having “a lean business model” that relied heavily on outside contractors to provide care so as to be nimble in the event of budget cuts. Dunham says developing a person-centric mindset on providing services has been a priority since she has taken over.
“Missing from the agency was a commitment to providing the entire con-
tinuum of care for a behavioral health population, which includes mental illness, substance use and everything in between,” Dunham says. “Not having the adequate staff employed by the agency to deliver services for anybody who walks in the door, it’s important since we are funded to do that, that we have that continuum in our clinic.”
To that end, Dunham added licensed addiction counselors to the agency’s staff and entered into a working relationship with Louisiana State University’s addiction fellowship program. The agency also has been able to partner with local substance use disorder provider agencies and hire resource coordinators through a Medication-Assisted Treatment-Prescription Drug and Opioid Addiction (MAT-PCOA) grant from the Substance Abuse and Mental Health Services Administration.
Dunham has also created an academic faculty curriculum that includes clinical guidance on a weekly basis and lunchand-learn style programs in which staff members can earn CEUs.

“I don’t want my staff to be stressed by leaving the agency to get CEUs or spending inordinate amounts of time or money to get their CEUs,” Dunham says.
“If I can incorporate that into the normal activity in our agency, I know that will serve them better.”
Lastly, Dunham has overseen the development of a recovery-oriented system of care (ROSC) that aligns stakeholders in the mission of being ready to provide service to patients when they are ready to receive treatment. It might not always offer staff members the dependability of set schedules, but it ultimately drives better outcomes for patients.
“Our work is to help our community partners understand this approach to care to empower people to take control of their lives so we can all get better outcomes from the services we provide,” Dunham says.
Dunham says that while implementing the changes to MHSD’s structure and service model, she has observed a positive change in the agency’s staff.
“I’m most proud of the cohesiveness that has developed amongst my team and the pride that they are beginning to take in the work they’re doing that ultimately is translating into providing a much better service to the people we’re trying to help. I’m very proud of the turnaround,” she says. “It’s been my goal to help them come into their own [and believe] in their own capabilities, and to challenge them to believe they can do more. I see that happening. That is probably the thing that is most important to me because it translates into a much better service for the general public, who we’re responsible for helping.”
MANAGEMENT 16 SUMMER 2018 BEHAVIORAL HEALTHCARE EXECUTIVE WWW.BEHAVIORAL.NET
Stephen Odom, LMFT, PhD
CEO and Chief Clinical Officer, New Vista Behavioral Health
Whether it was founding Simple Recovery or now serving as CEO and chief clinical officer of New Vista Behavioral Health, Stephen Odom, LMFT, PhD, has operated under a straightforward philosophy: Try to be the very best at what you do, but don’t try to do everything.

Each New Vista program – Avalon Malibu, Avalon Integrative Wellness, Center for Professional Recovery and Simple Recovery, which moved under the New Vista banner in 2016 – is designed with a specific purpose to foster recovery with specific populations. Services offered by New Vista, which is based in Costa Mesa, Calif., include mental health, addiction and co-occurring disorders.
Odom, who had spent much of his 30-year career working in large hospital systems, brought a similarly focused approach to the launch of Simple Recovery
in 2012, aiming to create a treatment facility that offered a more residential feel so that “people could get clean and sober in the community where they live.”
“I love working in hospital systems. At the same time, it’s treatment inside the four walls of a hospital. It seemed to me that we would do good treatment, provide great care and then have an excellent discharge plan,” says Odom. “But invariably, patients wouldn’t execute the discharge plan. Next thing you know, they were in trouble and relapsing—either their behavioral health or chemical dependency—and would need to come back again.”
An in-network provider with most major payers, Simple Recovery was designed to focus on re-establishing living skills, identifying potential triggers and helping patients integrate back into their environments and relationships in ways that are safe and will help them stay sober.

A group of investors later approached Odom about creating a new organization, putting the wheels in motion on the launch of New Vista in 2016. New Vista has been built on many of the concepts that led to Simple Recovery's success, with the other programs in the New Vista portfolio providing self-pay and out of network options.
While New Vista aims to deliver treatment to various niche populations, the
company isn't hesitant to refer potential clients to other facilities if they feel the fit elsewhere will improve their chances of recovery.
“We’re good friends to other treatment centers in the industry,” he says. “We refer a lot to other places because we believe they’re really good at what they do, and we believe they will find us to be the best at what we do. It’s a reciprocal, professional relationship. That’s how we do what we do at New Vista.”
Odom says he takes pride in continuing to work “in the trenches” with his clinical teams as New Vista’s chief clinical officer, being viewed by both staff and patients as trustworthy, approachable, and a “therapist who’s not a therapist.”
“People can just have conversations with me,” he says. “I like that, and I really love what we’re doing today.”
MANAGEMENT WWW.BEHAVIORAL.NET 17
Executive Director and CEO, NUWAY
While putting his own career back on track after a 10-year battle with addiction, David Vennes, MPNA, LADC, revitalized a community-based provider in Minnesota along the way.
Minneapolis-based NUWAY is thriving under Vennes, the organization’s executive director and CEO. But when Vennes was handed the reins a decade ago, he took over a company in dire straits.

“We were doing less than a million dollars a year. It was a couple rundown halfway houses, and the state had changed the way it reimbursed,” Vennes says. “When I got involved, we were $350,000 in the red to the IRS. It looked pretty dire.”
But facing adversity was nothing new for Vennes. Prior to joining NUWAY, Vennes spent 10 years battling addiction and going in and out of prison, collecting six felony charges along the way. Vennes got sober in 2002 and got back into the
field with NUWAY a few years later after re-earning his license. Vennes spent one year as a counselor before being tapped for a leadership role.
Vennes, who had 16 years in the field from the late 1970s to the early 1990s before relapsing, says his personal experiences helped him shape a course for NUWAY’s rebound.
“I had burned a lot of bridges and dug a deep hole for myself,” Vennes says. “This time, being in a leadership role, I have that perspective of the tremendous need that’s out there for people cycling in and out of treatment and the chronic relapsing folks that have burned all their bridges. That’s what NUWAY was designed for and envisioned to serve: the clients that needed more than 28 days, and there was nothing available back then.”
Under Vennes’ direction, NUWAY has become the first organization in the U.S. to adopt the Co-Occurring Disorders Program created by Dartmouth Medical School in association with the Hazelden Betty Ford Foundation, and it has developed the RISE (Recovery in Supportive Environments) model, which links outpatient treatment with recovery residence support.

“In Minnesota, there is a ton of highquality, short-term intensive treatment centers,” Vennes says. “The majority of the growth has been in the short-term, high-
intensity part of the continuum. That creates even more need in the extended care piece. Some people need more than 21 or 28 days. Rather than cycling them in and out of short-term programs, which is so expensive, we’ve tried to fill that gap and be there to augment those short-term programs by offering extended care.”
NUWAY’s extended care treatment continuum includes a medium-intensity residential program for men and outpatient with recovery residence support for both men and women. All NUWAY programs offer individualized lengths of stay based on client need and address co-occurring disorders.
Overall, NUWAY operates five clinics, has a network of more than 160 sober living affiliates, and works with more than 700 clients.
Vennes credits those around him at NUWAY for the organization’s turnaround.
“From the board of directors, the leadership, the staff, we’ve had such a missionminded, focused staff. Sometimes, when I get to one of our treatment centers, my heart flutters when I see our staff interact with clients. It takes my breath away. It’s humbling to be a part of.”
MANAGEMENT 18 SUMMER 2018 BEHAVIORAL HEALTHCARE EXECUTIVE WWW.BEHAVIORAL.NET
David Vennes, MPNA, LADC
Tom Valentino is Senior Editor of Behavioral Healthcare Executive.
7 tips for better payer contracts
Economics of being out-of-network makes going in-network an increasingly attractive choice, experts say
he prospect of joining health insurance or managed care networks is increasingly attractive to behavioral healthcare providers. In part, that’s because the economics of being out-of-network versus in-network have been turned on their head. In an effort to better control their own costs and profits, payers have been cutting their out of network reimbursements, so that in many cases it makes more sense to go in network.
“With the past few years, insurers have reduced what they pay to out of network providers, almost to the point where it is equivalent or less to be out of network compared to in network,” says Anelia Shaheed, an attorney with the Law Offices of Julie W. Allison, who specializes in managed care and insurance reimbursement. “That has led to a dramatic increase of providers who want to go in network.”
All treatment centers need to weigh the pros and cons of their network status, but experts agree the final decision comes down to the ultimate financial impact.
“[Payers] cut down drastically their reimbursement levels for out of network providers,” says Nathaniel Weiner, an attorney with the Polsinelli law firm in San Francisco. “They also began to audit providers to see if the practices they were using were consistent with what payers view as medically necessary.”
Joining a network can translate to a reduced financial burden on patients, while providing a more reliable revenue stream to providers and potentially result in new referrals. However, for providers new to the process, contract negotiations can be challenging. If not handled correctly, they could even result in the provider reducing their own reimbursements.
Most payers are also narrowing their provider networks to
BY BRIAN ALBRIGHT
focus on the most efficient providers and cut away the more costly ones. That means it can be more difficult initially for a provider to join those networks. Gaining access and then having enough leverage during the contract negotiation to ensure an acceptable reimbursement rate will require treatment centers to differentiate themselves in the market, back up their claims with data on outcomes, and avoid common contracting pitfalls.
“You can’t be another face in the crowd,” Weiner says. “Research what their networks look like and if possible create something new that might fit the network need at that time. Some providers won’t have that flexibility if they are already licensed and staffed in a particular way. But the payer’s language now is data. Show us what your data is for outcomes, how you can improve the cost curve and provide better care.”
Once the provider obtains network access, the contract negotiation process can take anywhere from three to six months as providers and payers haggle over reimbursement rates and other contract terms. In the current environment, negotiating leverage comes almost entirely from providers offering unique and provably effective services that can help reduce overall costs.
IS IT WORTH IT?
Negotiating a contract with a payer can be time-consuming and frustrating. So why do it at all?
The primary benefit is that providers can stabilize their reimbursements, while also being listed in the payer’s online provider directory. That listing can help bring in new patients and revenue.
However, those listings need to be accurate. Insurer directories often include out of date information, including indications of whether the practice is accepting new patients, services provided, and in-network status. This is despite federal rules that would levy penalties and removal from marketplace portals if
MANAGEMENT WWW.BEHAVIORAL.NET 19
It all started with one. One Agency that knew there had to be a better way.
One Agency that knew technology could be a resource, an ally, a simplifier.
One Agency Partnering with One visionary young company.
Both committed to increasing the Quality of Care and Life for all in Behavioral Health.
Seventeen years later, One Partner Agency in One State is now over 375, in 34 states.
Credible thanks each and every one of our Partner Agencies for their service and commitment
C Credible drives each and every one of our Partner Agencies to further leverage technology
Credible encourages our Partners to join together to push the bounds of collaboration and cooperation to new levels.
Credible is proud to Partner with so many quality Agencies from coast to coast.
The Power of One, delivering Benefits to Many.
There is room for more.
In June of 2000, Credible Behavioral Health started for one reason:
U Use technology to improve the quality of care. 18 years and 375+ Agencies later,
Credible is the first Enterprise SaaS company delivering fast, secure, clinical, billing, mobile, reporting, and data mining functionality. And Credible delivers software efficiently while implementing in as little as 4 5 months
Credible delivers real, tangible benefits to our Partner Agencies:
l A proven, reliable, secure and easy to use web-based solution
l Monthly innovation, real state-specific service, live phone help

l An independent, financially strong, lasting company; founder owned and founder run
l Mission-based and built to stay that way
301.652.9500 | partnership@credibleinc.com | credibleinc.com
The Power of One. The Benefits to Many. Now It

’s Your Turn!
directories are not up-to-date.
New business from the directory also isn’t guaranteed. Some providers also think that insurance companies themselves will direct referrals to the practice, but that is not the case. Depending on state insurance law, the payers may actually be prohibited from recommending specific providers.
Another potential benefit is reducing administrative complexity. Going in-network can help streamline claims disputes. Providers may also have access to the payer’s medial director to resolve some questions.
“Unfortunately, in many cases the same patient who goes to an in network provider may get an authorization much more easily than with an out of network provider, even with the same criteria,” Shaheed says. “You can save time and money on authorizations.”
The New Haven, Conn.-based Turnbridge treatment center joined the Anthem network roughly one year ago. While CEO and founder David Vieau says that he hasn’t noticed Anthem’s approvals being measurably faster, reimbursements have been accelerated. “Once you are in network, those claims go to a different department and to a team of individuals you are working with on a regular basis,” Vieau says. “The processing is easier, even if the number of denials doesn’t really change.”
Ultimately, in-network status can also be a true help to clients.
“We have a responsibility to the consumer,” Vieau says. “If cost is a barrier to entry, then the provider has to think about that. As out of network deductibles have increased, the average American can’t afford them. Being in network stabilizes that to a certain degree. The consumer is spending less money on the front end to satisfy insurance requirements, and that makes more money available to provide help later in the process.”
BE SELECTIVE
While there are benefits to being in-network, the value of those benefits will vary by payers. Providers should carefully select potential networks based on availability (can they join the network at all?) as well as their current patient and payer mix. How much business the provider already does with an insurer (or how much business they may be turning away because they are out-of-network) can guide that selection process.
Find out about the rate of physician or provider turnover for the plan. A 2017 Health Affairs report found that narrow network Medicaid managed care plans experienced three-percentagepoint higher turnover rates in one year, and a 20-percentage-
point-higher rate in five years compared to non-narrow network plans, for example. Those metrics could give providers an idea of how they might be treated while in-network.
Also, look at your own claims data with that particular payer over time. How much revenue have they provided across different services? Investigate how they handled denials. Talk to your admin staff as well and find out what their experience has been like when dealing with a specific payer.
At Turnbridge, Vieau says he’s been evaluating plans based on their focus on effectiveness.
“Our approach is focused on efficacy, we believe that the longer a person is engaged in some form of treatment, that increases probability they stay sober,” Vieau says. “Our focus on efficacy has played an instrumental role in our decision to go in-network or out-of-network."
Turnbridge completed a lengthy contract negotiation process with Anthem that was heavily reliant on data from the provider and a willingness on Anthem’s part to consider that when determining a reimbursement rate.
According to Vieau, data on their success rates (97% reach their one-year sobriety milestone, for example) helped move the needle.
“We talked to them, showed them our results, and said the standardized rate wouldn’t be fair,” Vieau says. “We struck a deal. Other insurance companies have varying degrees of enthusiasm around efficacy. They aren’t going to shift from their reimbursement model unless you give them a reason to do so.”
CONTRACT TERMS
Negotiating a contact with an insurance company should be a team effort. “The biggest mistake I see in contracting is not having the billing department and medical director or the clinical team included in the discussion,” Shaheed says. “The billing staff can tell you if you forgot codes or if a doctor is not credentialed.”
Providers may feel they don’t have much leverage with payers, but Shaheed says there are ways to negotiate from a position of strength. If the provider is receiving a significant amount of out-of-network compensation from the insurer, they may be more willing to compromise, provided there’s an opportunity to save money. Data on success rates and unique advantages the provider can bring to the network are also key negotiating points.
“If you have no history or you’re a new facility, it can be more difficult to get a contract,” Shaheed says.
MANAGEMENT 22 SUMMER 2018 BEHAVIORAL HEALTHCARE EXECUTIVE WWW.BEHAVIORAL.NET
There are several other key contract components to watch for, including:
Providers need to know their costs to effectively compare them with reimbursements and determine whether the relationship is financially viable. “Going in network is going to financially ruin you if you don’t know your costs," Shaheed says.
is in network, but it hasn’t been added to their contract yet,” Shaheed says.
Always negotiate a rate increase in the contract, otherwise the provider may be stuck with the same rate for several years. “Look at the terms,” Shaheed says. “Make sure you know ancillary services and the codes. Look at the percentage paid of the Medicare allowable rate as well. If Medicare changes the rate from one year to the next, and you are contracted at the Medicare rate, then you are going to get the same percentage of a lower reimbursement.”
Weiner says that language around medical necessity can be a “big trap” for providers. “Definitions vary, and there are some things they can put in the contract that allow them to take another bite of the apple,” Weiner says. “If they’re asking for the lowest-cost treatment, that can lead to a lot of denials.” He also says that during negotiations the medical necessity language should be subject to objective criteria, and that there is a reciprocal sunset on the finality of a claim. Payers should negotiate rates before they go through the credentialing process with the insurer. “When you get to the credentialing stage, it’s important to make sure the licensing is correct, that you know all of the codes and services that will be billed, and that you know what you need to ask for or carve out,” Shaheed says. Waiting until the end to complete those processes could lead to the provider not having the right credentials in place, or forgetting to include specific services in the contract.
1 2 3 4 5
Also pay attention to language around take-backs (when insurers can reclaim money already paid), and the length of term of the contract. If the provider is dissatisfied with the contract over time, what are the rules governing cancellation of the contract? Are there fines associated with early termination?
Providers should also determine how the contract will apply to new lines of business or insurance products that are introduced after the contract is established. This can be particularly important for companies that offer ACA marketplace plans. “Get them to agree to automatically include you in those new lines of business, otherwise there may be patients purchasing ACA plans and thinking the provider
For payers that offer Medicaid or Medicare managed care offerings, providers need to make sure they can meet the state and federal audit requirements. “Enforcement tools are more stringent, and revenues can be automatically reversed if it turns out the provider has team members on the exclusion list or federal debarment list,” Weiner says.
The strategic plan the provider has for the organization is also an important component of contract negotiations. If the goal is to build up the business and sell it, there may be some limitations in the contract that could affect their ability to terminate. “There are also ‘least favored nation’ rates,” Weiner says. “That means if you are sold to another provider or you buy another provider, and one of you has a lesser rate with that payer, the lower rate automatically applies to both businesses.”
FOCUSING ON OUTCOMES
With the increased focus on data and outcomes, there has been some interest in establishing value-based reimbursement programs. The Centers for Medicare and Medicaid Services are already experimenting with value-based or outcome-based reimbursements, and private payers are beginning to follow their lead.
Shaheed says she has recently worked on several value-based payment contracts, but they are the first of their kind that she has dealt with. “The clients are just now evaluating along with the payer to see if this type of contract works for them,” Shaheed says.
She has also worked on all-inclusive contracts, in which the provider receives a flat fee for a certain package of services. In both case, the providers came up with a rate that they would require in order to reach the best outcome for the patient.
While outcomes-based reimbursement contracts are still rare, having outcomes data is still an important negotiating tool. “If you have 97% of individuals remaining sober, we’re making assumptions about what that does for overall health in terms of fewer emergency room visits or treatment of chronic diseases,” Vieau says.
Weiner expects more treatment centers to join payer networks. For providers, the key to successfully negotiating those payer contracts will be reliable data and the ability to make themselves stand out to insurers who are shrinking their networks.
“You need a differentiated success rate model if you want a differentiated reimbursement model,” Vieau says.
MANAGEMENT WWW.BEHAVIORAL.NET 23
Brian Albright is a freelance writer based in Ohio.
Raids cause larger concern for MAT prescribers
Some industry observers believe certain federal actions have been too aggressive
BY JULIE MILLER
s the nation attempts to combat the opioid crisis, some industry observers believe certain federal actions taken in the past few months have simply gone too far. In recent cases, agents executed search warrants on medication assisted treatment (MAT) providers with no obvious rationale.
The raids were unwarranted, according to Michael Barnes, managing partner at DCBA Law & Policy, who represents providers. He tells Behavioral Healthcare Executive he’s concerned that Attorney General Jeff Sessions and the Department of Justice (DOJ) are out of alignment with the Trump administration’s current position on the opioid crisis.
“Health and Human Services Secretary Alex Azar is onboard, and [the president’s counselor] Kellyanne Conway is doing a great job at supporting this—so is the Food and Drug Administration and the National Institutes of Health,” Barnes says. “Everyone except DOJ.”
In a letter to the president, DCBA Law & Policy calls for the dismissal of Sessions, the suspension of DOJ criminal investigations against physicians prescribing MAT, and the development of a process to ensure criminal investigations are conducted only with referrals from state licensing boards.
PRACTICES TARGETED
What’s especially concerning to Barnes is the fact that two of the providers are, in his assessment, clearly reputable providers. Stuart Gitlow, MD, MPH, MBA, DFAPA, the past president of the board of the American Society of Addiction Medicine (ASAM) was the target of one of the raids in March.
Gitlow, who is a general, forensic and addiction psychiatrist
and prescribes MAT drugs, confirms to BHE that his home and his private practice were raided by FBI agents with search and seizure warrants.
Federal agents recently also searched Watauga Recovery Centers in Virginia and Tennessee and seized patient records. Ralph Thomas Reach, MD, president and founder of the organization, is also the past president of the Tennessee Society of Addiction Medicine. He helped craft the state law for MAT, and is on the ASAM legislative committee.
He told the Johnson City Press that there are no medications kept at the treatment centers, and the organization doesn’t work with any federal or state health insurance programs that might be under the purview of special fraud investigation teams.
“These are not criminal cases,” Barnes says. “These are cases where the Department of Justice is going after some of America’s best addiction physicians for questionable medical conduct at best.”
He believes the intent is to create a chilling effect on the use of MAT drugs, even though the Trump administration has overtly favored access to MAT as a policy to address the opioid crisis.
“There is excessive enthusiasm on the part of Jeff Sessions to raid doctors,” Barnes says.
STATE BOARD OVERSIGHT
Ordinarily, questionable medical conduct, such as suspected diversion or overprescribing might be a case for state medical boards to examine. Physicians violating accepted standards would be investigated by a board of professionals to distinguish whether the offense warrants suspension of the license to practice or action from law enforcement.
“When there is any medical question about a prescriber’s conduct, that question should be referred to the state professional licensing board, which can then conduct an investigation and
POLICY 24 SUMMER 2018 BEHAVIORAL HEALTHCARE EXECUTIVE WWW.BEHAVIORAL.NET
refer criminal conduct to law enforcement,” Barnes says. “That’s what should be happening. Period.”
But not all boards have the resources to follow up on every situation. That’s why Barnes believes some of the federal opioidrelated funds should be funneled to medical boards for that purpose. He says his firm is working pro-bono to advance a policy for medical-board-referral requirement before federal investigation/prosecution.
The Federation of State Medical Boards prepared a brief in 2009 that had the support of attorneys general, the Drug Enforcement Agency (DEA) and others in law enforcement. While it was framed specifically to position best practices in investigating potential diversion of pain medications, Lisa Robin, chief advocacy officer of the federation, tells BHE the approach certainly applies to the medications used to treat addiction disorders.
“The principles of cooperation between regulatory bodies that oversee professionals and law enforcement are critical regardless
of what the issue is,” Robin says. “It doesn’t matter if it’s opioids or Suboxone or anything else. The principles are still solid.”
She emphasizes the fact that the federation’s template calls for medical expertise to evaluate a physician’s conduct.
“We worked for years with DEA and state medical boards and law enforcement, urging that there be cooperation in the investigations, that you look at the practice, and that there be expertise in the medical field to gauge if the provider was negligent or strayed away from standard of care,” she says.
The bottom line for treatment providers is that at the very least they must reduce their risk by keeping excellent documentation when prescribing MAT drugs. There’s also an opportunity to advocate for policies that balance the significant need for access to addiction treatment with the need to ambush those engaging in diversion.

POLICY WWW.BEHAVIORAL.NET 25
SCOTTSDALE, AZ DEC 10-12, 2018 OMNI SCOTTSDALE RESORT AND SPA AT MONTELUCIA Register now at www.TreatmentCenterRetreat.com/2018 INVESTING IN ADDICTION TREATMENT AND RECOVERY The Treatment Center Investment & Valuation Retreat is the premier event for executives who want to grow, invest in, and transform their businesses, and offers a series of panel discussions, expert presentations, and formal and informal networking opportunities. REGISTER TODAY
Julie Miller is a freelance writer based in Ohio.


Minimize risk when patients leave AMA
The process should begin when patients first arrive
atients who leave against medical advice are putting their own health at risk. Additional risks for the treatment center could include liability for patient self-harm, overdose, suicide or injury from a lack of basic safety. Such risk can be minimized, however, when provider organizations adopt wellcrafted policies and procedures that go beyond simple intake forms. The process must begin the moment a patient walks through the door to better protect the patient and the business.
Leaving against medical advice (AMA), or against treatment advice (ATA), is a universal struggle for most treatment centers.
A Treatment Episode Data Set (TEDS) report released by the Substance Abuse and Mental Health Services Administration (SAMHSA), examined discharge data from addiction treatment facilities in 2014—the most recent data available. SAMHSA found that 25.8% of the 1.4 million discharges examined included people who had dropped out of treatment. Treatment completion rate overall was 43%.
Kevin J. Malone, an attorney at Epstein Becker Green, says leaving against medical advice is a more significant concern for mental health and addiction treatment providers than any other provider setting, including hospitals, in large part because of the vulnerable populations they serve.
“There’s significant business risk to the treatment provider because they are losing the revenue from this patient, and they are faced with a potential liability associated with harm that may happen to that person,” Malone says. “And at this point in the trajectory of our country and with the issues that the opioid crisis has created, prosecutors are looking for anybody
BY JILL SEDERSTROM
to go after.”
According to Malone, prosecutors have become aggressive in trying to place blame for overdose deaths. Even if treatment centers did everything they could to help a particular patient, Malone says an investigation alone can carry with it a significant cost to the business.
For these reasons, it’s important that treatment centers are proactive and establish policies and procedures that limit their own liability.
CRAFT INTAKE FORMS
Risk mitigation should begin as soon as a patient walks in the door. Most treatment centers have forms for patients to fill out when they leave against medical advice, but experts say having carefully crafted intake forms that consider that possibility of AMA are just as important. Patients in the process of leaving might not be amenable to signing documents as they depart.
“Facilities may not have invested the time in making sure that their original informed consent intake forms protect them legally,” Malone says. “It varies by state what you can do on the intake side and on the AMA side.”
If states allow it, he says treatment centers should include binding arbitration provisions as part of the intake paperwork. Such forms should also include clear consent forms, particularly for 42 CFR Part 2 regulations, in order to give treatment facilities the authority to reach out to other providers or family members in the event a patient leaves AMA.
ESTABLISH COMPETENCY PROTOCOL
In addition, Malone says treatment centers also need to have an established policy to address the patient’s own ability to make a rational decision on continuing treatment. A professional
CLINICAL TRENDS 28 SUMMER 2018 BEHAVIORAL HEALTHCARE EXECUTIVE WWW.BEHAVIORAL.NET
assessment is potentially required by law.
“You don’t want to allow someone to leave against medical advice if they don’t have the capacity to make that decision,” he says. “If you don’t have a policy in place for how and when and who is qualified under state law to make that assessment, you are in a really bad situation.”
Smaller providers that don’t have a psychiatrist on staff, for example, need to determine how to carry out an assessment if necessary.
IDENTIFY PATIENTS AT HIGH RISK FOR AMA
Providers also need to have policies during the early stages of treatment that help clinicians identify which patients might be at the greatest risk of leaving AMA. For example, young adult patients might resist treatment when parents insist on it. Individuals opting for treatment through drug courts might have less motivation to be well in recovery than to simply avoid jail time.
Greg Hobelmann, MD, MPH, chief medical officer at Ashley Addiction Treatment in Maryland, says there are certain warning signs that may make a person more likely to leave AMA, such as someone who voices ambivalence about treatment, having a prior history of AMA or a having history of not following clinical advice.
JourneyPure, an addiction treatment center in Nashville, has incorporated an AMA risk assessment tool into part of its pre-admission screening process. Professionals ask patients five simple questions designed to assess the likelihood a patient will leave treatment against advice. Patients are then given a score from 0 to 5 based on their risk, and staff members determine
who might need extra intervention during treatment.
“We’ve found so far that the tool is fairly good in terms of its ability to predict one’s predisposition to leaving against our advice,” says Brian Wind, PhD, chief of clinical operations for JourneyPure.
CREATE A CULTURE THAT PREVENTS AMA
Patients are motivated to leave treatment for any of a long list of reasons, including cravings, intense emotions, fear of losing a job or lifestyle, or pressure from others to return home. Experts say treatment facilities need to create a warm and welcoming culture that promotes safety and alleviates fear.
JourneyPure uses a specific blocking protocol to prevent AMA departures and trains its staff to report any language or action they observe in a patient that could signal an AMA departure might be imminent. All staff are trained to use motivational interviewing techniques and avoid power struggles with the patients they serve.
“We’ve had some great people who are experts in AMA departure prevention that come around regularly to educate our staff,” Wind says. “We frequently do staff collaboration meetings and interdisciplinary meetings that center around AMA departures.”
The result is what Wind considers a low AMA departure rate at the JourneyPure facilities.
ALERT FAMILY OR HEALTH PROFESSIONALS
Even with signed forms and patient acknowledgement of AMA, Malone cautions that providers aren’t necessarily absolved from liability when the patient walks away.
“You need to be doing everything you possibly can to prevent them from leaving, and then to prevent harm after the person leaves, whether they sign the paperwork or not,” he says.
One way to try to reduce the potential harm to a patient after an AMA departure is alerting family members or other healthcare professionals who have referred the patient or treated them in the past.
Many providers mistakenly believe that HIPAA prevents them from notifying family about a dire situation, but HIPAA does allow communication when a patient is in danger. Clinicians can disclose information to family members “to the extent that the provider perceives a serious and imminent threat to the health or safety of the patient or others, and the family members are in position to lessen the threat,” according to federal guidance.

WWW.BEHAVIORAL.NET 29
Events
The Institute is a trusted educational resource that helps address daily challenges. Our conferences convene thought leaders that share clinical best practices, discuss how to effectively and ef ciently operate a behavioral healthcare organization, and strategize solutions for addressing the opioid epidemic. Join us at an upcoming event to network with peers and take home valuable tools. Learn more about us and how we can help you at www.iadvancebehavioralhealthcare.com.
National Events
APRIL 22-25, 2019 | ATLANTA, GA
Be part of the discussion at the largest national gathering of stakeholders working together to address the opioid crisis. Prevention, treatment, law enforcement, public health, and many others exchange best practices and hear from state and federal of cials at the annual Rx Summit. www.nationalrxdrugabusesummit.org

AUGUST 19-22, 2018 | DISNEYLAND, CA
Addiction professionals annually convene at NCAD to share what’s working: Clinicians hear from thought leaders on delivering treatment, while executives of behavioral healthcare organizations learn how to run more effective, more ef cient, and ethically minded businesses. www.ncadcon.com
NOVEMBER 12-14, 2018 | FORT LAUDERDALE, FL
The opioid crisis is making headlines, but another category of drugs continues to devastate communities: stimulants. Join other stakeholders to explore how to address and treat stimulant use.
www.stimulantsummit.com


DECEMBER 10-12, 2018 | SCOTTSDALE, AZ
Senior executives of treatment centers, and those investing in these enterprises, discuss growth strategies and market dynamics at this exclusive, three-day educational and networking event.
www.treatmentcenterretreat.com
2019 DATE AND LOCATION COMING SOON
TCEM provides CEOs, CFOs, COOs, directors, senior marketing/business development/ admissions leaders, and other executives with the tools they need to effectively and ethically grow their services in a rapidly changing market.

www.executiveandmarketingretreat.com
Interested in attending an event? Contact Ellen Kelley at ekelley@iabhc.com or 216-373-1223.
Photography: Pete Winkel GPA and Chris Williams Zoeica Images
President Barack Obama addressed Institute attendees in 2016.
Matt Bevin, Governor of Kentucky, addressed Institute attendees in 2017.
and CE
CE Hours CE Hours
CME
Hours
President Bill Clinton addressed attendees in 2018.
National-Regional Events
CE Hours
Local Events
The Summits for Clinical Excellence bring together thought leaders on cutting-edge topics in multi-day national and regional conferences. Summits on mindfulness, trauma, process addiction, and shame appeal particularly to private practice behavioral healthcare professionals. Other Summits address the national opioid crisis from a regional perspective and engage a diverse group of stakeholders. Many Summits offer treatment ethics continuing education credits.
• ATLANTA, GA October 18-21, 2018
Brain Matters: Shame, Trauma, and Process Addictions
www.atlantasummitconference.com
• NEW ENGLAND November 8-9, 2018
The Opioid Crisis: Strategies for Treatment and Recovery www.newenglandopioidsummit.com

• PHOENIX, AZ February 20-22, 2019
The Opioid Crisis: The Clinician’s Role and Treatment Practices www.arizonaopioidsummit.com
• CHICAGO, IL March 6-7, 2019
The Opioid Crisis: Strategies for Treatment and Recovery www.chicagoopioidsummit.com
• CHICAGO, IL March 6-9, 2019
The National Conference on Trauma, Addictions, and Mindfulness: Where Freud Meets Buddha www.chicagosummitconference.com
• PITTSBURGH, PA June 3-4, 2019
The Opioid Crisis: The Clinician’s Role and Treatment Practices www.pittsburghopioidsummit.com
The National Conference on Alcohol and Addiction Disorders convenes panel discussions across the country in a lunch & learn format. Clinicians hear about treatment practices, while those on the business side of the field share strategies for managing and marketing behavioral healthcare organizations. www.iabhc.com/local
Virtual Events
Interested in attending an event? Contact Ellen Kelley at ekelley@iabhc.com or 216-373-1223.
events: Baltimore Chicago Columbus, OH Denver Detroit King of Prussia, PA Long Island Memphis Nashville New Orleans Phoenix Pittsburgh Providence Salt Lake City San Diego Washington, DC
Upcoming
CE Hours
from experts on clinical, managerial, and other topics in our frequent, free-to-attend Webinars. www.iabhc.com/webinars
Hear
CE Hours
Ashley Addiction Treatment chief medical officer Greg Hobelmann MD, says at Ashley, staff will inform all patients at intake that while they can later choose to remove consent to some of their contacts, patients cannot renege on their consent for an emergency contact, even in the case of an AMA departure.
“We always contact the emergency contact to let them know what’s going on,” he says.

MAINTAIN CONTACT AFTER DEPARTURE
Treatment providers should also give patients departing AMA a reasonable chance at success by supplying them with other community resources where they can find help or by giving them a way to reconnect with the facility.
“You should have a follow-up policy as well, especially if you have an outpatient program,” Malone says. “You don’t just ignore the person.”
JourneyPure has developed a smartphone app that acts as a

daily guide for recovery and includes a built-in communication system. The app, which Wind describes as HIPAA-compliant secure messaging with recovery coaches, is installed on the patient’s phone before they leave the facility.
The recovery coaches then remain in contact with the patient even after they leave.
“It feels like a safe private space by which to communicate with someone who loves them and cares about them in early recovery,” Wind says.
More than half of the people who leave JourneyPure AMA later return to the facility to re-enter treatment, Wind says.
“We still maintain a sense of connectivity with them, and even if they leave against our advice, we make it really clear in letting them know that there is no judgment. We’re still here for you,” he says.
Good Room design puts patients at e a s e a n d a l l ows t h e m to w i l l i n g l y enter treatment. So, what constitutes good room design in a healing environment? Facilities should include common areas designed for group sessions, semiprivate areas for family visits, spaces for one - on- one counseling, and safe, private areas for reading, resting, and contem-
plation. Non institutional, welcoming furniture is a cornerstone of a facility designed with healing in mind.


A natural assumption of many executives is that contrac t quality furniture will be too institutional and lack the charac ter of residential furniture. The truth is that contrac t seating, dining, and b e d ro o m s a re n o t o n l y ava i l a b l e i n h u ndreds of st yles but contrac t furniture also
s

and self-harm risk not offered by retail furniture providers.
Contrac t furniture complies with all consumer safety standards, state and loc al public use codes, as well as licensing & accreditation requirements like Joint Commission. In addition, contrac t furniture providers offer fabrics and finishes that are de -
signed to stay fresh and clean under constant use Replacement c ycles can be reduced to 5 –7 years or more. S ome facilities repor t more than 10 years with the right quality furniture.
800 969 4100 info@furnitureconcepts.com w w w.furnitureconcepts.com

CLINICAL TRENDS 32 SUMMER 2018 BEHAVIORAL HEALTHCARE EXECUTIVE WWW.BEHAVIORAL.NET
® FURNITURE CONCEPTS Home of TOUGH STUFF!
Jill Sederstrom is a freelance writer based in Kansas City
r e l i a b i l i t y fo r co nce r n s l i ke behavioral o u t b u r s t s
p r o v i d e
safet y and
and
l l
Advertorial_BH_ furniture Concepts.qxp_Layout 1 7/20/18 3:00 PM Page 1 SPONSORED CONTENT
First IMPRESSIONS When Patients Enter a Behavioral Healthcare Treatment Facility can really SET THE STAGE FOR RECOVERY.
Design for safety Consider protections
for specific patient populations
BY JOANNE SAMMER
o say patient safety is a priority for behavioral healthcare facilities is an understatement. Federal, state and local laws and regulations offer an array of requirements for facilities to meet, but behavioral healthcare organizations also bring their own patient safety standards to the table. New inpatients are often at their most vulnerable, and self-harm protections must be considered. However, experts say design doesn’t have to be hampered by the need for safety.
When America’s Rehab Campuses designs a new facility, the organization is often repurposing a former hotel or resort. From a safety perspective, that means that each new facility brings its own challenges. “We walk through and are prepared to adapt everything,” says Michelle Carrasco, the organization’s chief administrative officer in Tucson, Ariz. That could mean removing a hedge to eliminate hiding places and improve sightlines to patients to removing the materials left behind, like spring
mattresses, that could endanger patients if someone removed a spring to use as a weapon. “We bring in fresh eyes—our CEO, chief nursing officer, CFO and our facilities people—to offer opinions on potential changes,” she says.
Carrasco notes that the design focus at America’s Rehab Campuses goes above and beyond legal requirements, for example, by making detox units completely anti-ligature. That means making significant investments to ensure that every element of the design uses anti-ligature products, including air conditioning unit, plumbing and lighting fixtures, hardware, window coverings and so on.
“We spend a lot of money but the detox unit is built specifically for its purpose and that is not inexpensive,” she says.
The fact is, facility design has a tremendous impact on patient safety. It impacts how people move through the building, how much of a given area staff can see at one time and how people feel when they are in specific spaces.
“It is important to live a ‘day in the life’ of a facility and develop an open dialogue about what is going on,” says Mitch Hoefer, founder and CEO of HoeferWysocki, an architecture,

DESIGN FOCUS WWW.BEHAVIORAL.NET 33
ArtistrenderingcourtesyHoeferWysocki
planning and interior design firm in Kansas City, Mo. Questions to consider include:
• How does the facility receive patients?
• How does the intake process flow?
• What is the average length of stay?
• What size is the patient population and what are its demographics?
• How much does the patient census fluctuate and does the facility need to accommodate an ebb and flow of patients?
UNIQUE DESIGNS FOR UNIQUE TREATMENT
Safety begins well before a patient picks something up and throws it at someone or slips and falls or attempts to self harm. An effective design for a treatment facility can help patients remain calm and minimize opportunities for patients to be destructive or self harm. Bedrooms and bathrooms can be particularly dangerous places for vulnerable patients so keeping patients active and out of their rooms is a common goal.
“To keep patients from lingering in their rooms, you can minimize its sense of place,” says Hoefer. “By providing only the basics, bedrooms become only a place to sleep.”
Other design choices will depend on the unique treatment philosophy of each facility.

“Good designers understand the goals, objectives and principles of a behavioral healthcare practice, its program and its philosophy for providing care,” says Rebecca Sanders, a
healthcare principal with design firm HGA in Minneapolis. “Creating a safe environment is one piece of that.”
The Virginia Treatment Center for Children in Richmond, Va., has built its treatment philosophy around never using mechanical restraints on its patients. To fulfill that goal, the staff and patients need an environment where staff can prevent situations from escalating as much as possible. To that end, the facility has 130 cameras that can be monitored at the nurses station and that staff can turn on using their identification badges. This allows staff members to respond more quickly to emergencies and help avoid dangerous and violent situations.
“Our philosophy is to build a relationship with each child and understand his or her trauma,” says Alexandria Lewis, Ed.D., the facility’s executive director. “We want them and their families to partner with us in their own treatment.”
Making sure the design team understood this philosophy and the facility’s resulting priorities for patient safety was the essential starting point for designing a new facility. She and her team visited similar facilities to see how they approach design and how various design approaches work in a real-life clinical setting. However, they also recognized the need to adjust any safety-related design solutions they saw during these visits to accommodate their treatment philosophy because many of these facilities used mechanical restraints.
“Avoiding mechanical restraints is not a common approach,” she says.
DESIGN FOCUS 34 SUMMER 2018 BEHAVIORAL HEALTHCARE EXECUTIVE WWW.BEHAVIORAL.NET
PhotocourtesySteveHenkeStudios
CREATING BALANCE
Balance is an important consideration in both design and patient safety. For example, a key part of creating a safe environment for patients is also creating a safe environment for staff. How staff members interact with a space and with patients in that space can have a tremendous impact on patient safety. If staff feel safe and confident that they can handle situations, their actions and decision making are likely to be more effective.
One consideration in design is ensuring that staff can move around a facility safely. That means having clear pathways to leave a room or other area to call for assistance when necessary. It also means having clear sightlines to patient areas and feeling comfortable as they go about their work. For example, one acute care facility created a separate dining area for staff with natural light and clear sightlines and access to the patient dining room.
“It is a place for staff to rest and have respite while still being aware of what is happening in the main dining room,” says
Sanders.
By having their own space, staff can relax during a meal without having to interact directly with patients unless it is necessary to do so.
Balance is also needed when designing for everyday activities. Behavioral healthcare organizations may end up designing a facility with a worst-case scenario in mind rather than focusing on the environment they want to create in a given area or for a facility as a whole. Sanders noted that many behavioral healthcare organizations tend of emphasize the durability of materials.
“Their philosophy focuses more on protecting the facility from the patients rather than understanding how the environment can provide dignity for the patient,” she says.
While a focus on protecting against the worst-case scenarios is essential when designing private spaces like bathrooms and bedrooms, behavioral healthcare leaders can reach for middle ground in more communal areas for dining, group activities, recreation and conversation.
“This is where they can think differently about design and not just focus on the worst-case scenario,” says Sanders.
One adolescent treatment facility created a multi-use space for patients that included a pool table, a television, space for reading and playing games and lounge furniture with each area separated by glass surrounds to contain the noise from the various activities while also providing clear sight for the staff. “Everyone needs something different—space for reflection, personal space, community,” says Sanders.
Virginia Treatment Center for Children incorporated abundant natural light and outside spaces into its design to help patients heal from trauma.
“We have a number of courtyard areas that we include in therapy so that children don’t feel that they are being held within a building,” says Lewis. “They can go outside.” The facility design also relies on curves to avoid sharp edges and increase the flow of the layout.
To create these types of spaces that meet patient and staff needs, Sanders suggested that behavioral healthcare leaders set parameters for design. That means evaluating the floor plan to identify the most critical and noncritical areas of the facility, including public areas, and identify materials acceptable for each one with more specific guidelines for bathroom design. Experts agree, there is no one size fits all.

DESIGN FOCUS WWW.BEHAVIORAL.NET 35
Joanne Sammer is a freelance writer based in New Jersey.
ArtistrenderingcourtesyHoeferWysocki
Experts debate 42 CFR Part 2’s modern role
Recent changes to the rule have kept it top of mind for providers
BY ALICIA HOISINGTON
lthough changes to 42 CFR Part 2 took place in recent months, the rule has always been top of mind for treatment centers. And now that legislation passed in June to align privacy for substance use disorder patients with HIPAA, the rule continues to make waves.
On June 20, the U.S. House passed the Overdose Prevention and Patient Safety Act, or HR 6082, which allows authorization to disclose—as long as it is in line with HIPAA—the records of patients with substance use disorders without written patient consent to a covered entity for treatment and payment purposes, healthcare operations, and to a public health authority. In May, the House Energy and Commerce Committee passed a similar bill, HR 5795.
Corey Waller, chair of the American Society of Addiction Medicine’s Legislative Advocacy Committee, says that rolling 42 CFR Part 2 into HIPAA with added protections—and the bills that support this—is the way to go.
“HR 5795 is a good option because it maintains the criminal justice protection,” he says. “It mandates training for people on how to maintain these records, and it adds criminal penalties if you release the records. Now if under 42 CFR Part 2 you release them, it’s only civil and no criminal.”
Deborah Reid, senior health policy attorney at the Legal Action Center, and her team strongly oppose HR 5795 because Reid says it doesn’t offer enough protection for certain patients.
“That bill basically is eliminating Part 2’s federal confidentiality protection for the disclosure of information and further disclosure of substance use disorder information for the purposes of treatment, payment and healthcare operations and it
replaces it with a weaker HIPAA standard that has no patient consent,” she says. Reid adds that while the bill offers some anti-discrimination provisions, it doesn’t protect people with disorders who are using illegal substances.
“It’s based on current civil rights laws like the Americans with Disabilities Act or the Fair Housing Act. They don’t protect people who are using illegal substances against discrimination,” she says.
Pamela Greenberg, president and CEO of the Association for Behavioral Health and Wellness, says that legislation working to align Part 2 with HIPAA for covered entities will actually strengthen standards set forth in Part 2. The association is part of the Partnership to Amend 42 CFR Part 2, a coalition of more than 40 healthcare organizations committed to aligning Part 2 with HIPAA to allow appropriate access to patient information.
“One of the criticisms very early on as we talked about wanting to move to the HIPAA standard was what about these protections that exist in Part 2 that may not be as strong in HIPAA that ensure people’s substance use disorder records aren’t used against them in an employment or housing situation, or a child custody case?” she says. “In the legislation, we keep all of those protections and actually strengthen them.”
MORE CHANGE NEEDED
Even so, sources say legislation to change 42 CFR Part 2 is moving along due to the rule’s antiquated regulations. Part 2 was introduced in the 1970s, and many believe it has since become outdated in today’s world of electronic health records and increasing need to provide services amid epidemics such as the opioid crisis.
Greenberg says Part 2 is a great hindrance when it comes to electronic health records because there is no good way to segment information.
“Electronic health record vendors are interested in seeing
TECHNOLOGY 36 SUMMER 2018 BEHAVIORAL HEALTHCARE EXECUTIVE WWW.BEHAVIORAL.NET
W
a change toward a HIPAA standard as well because most, if not all, electronic health records are not able to accommodate separation of the substance use records from the rest of the medical records,” she says. “SAMHSA has tried with some version of a record, but my understanding is nobody is using it, and it’s costly and complicated. It didn’t end up being a good solution.”
And Waller says that in theory the recent changes SAMHSA made to Part 2 were to help improve the movement of information. But when information needs to be segmented and shared, the data within the system can become costly for the entities that own it. In turn, that can make those entities simply not want to own the information.
“The issue is re-disclosure. This is what scares hospitals off,” he says. “If I take on somebody’s Part 2 information and make it a part of the medical record, it’s now up to me to go find that patient again, if someone requests their medical record, to get a separate release of information.”
He says that can pose a problem if the patient is difficult to get in contact with because he or she doesn’t have a phone or might be homeless, for instance. He says if that information is released anyway, it goes against the regulations put in place by 42 CFR Part 2, which can be a costly decision.
“So even though you’re not a covered entity by yourself, you’re re-disclosing covered-entity data. That’s why hospitals are not willing to start a lot of internal programs because it costs millions of dollars to build electronic infrastructure to separately house addiction information,” Waller says. “And then when you separately house it, it still cuts off that piece of information from the people who really need it that are treatment providers.”
But even more detrimental than the cost of building an electronic infrastructure to accommodate the regulations of Part 2 is the harm that can come to patients when medical records can’t be shared with treatment providers, says Waller, who has experience with the negative effects of the rule.
Waller treated a patient who came in via the emergency room for a broken wrist. He asked the patient whether there was a history of substance use disorder, including alcohol, opioids or other issues with pain medications. The answer from the patient was no, so Waller wrote a prescription for three days worth of pain medication with instructions for orthopedic follow-up. The next day, the patient received a daily dose of methadone from a clinic. “My treatment plan for them would have been much different if I had known they were in a methadone clinic,"
Waller says. “But right now there’s no provision for disclosing within the medical record so that I can just see it. For every other disease, I can just see it.”
PROTECTING PATIENTS
But Reid says Part 2 is important when it comes to protecting patients who might not seek treatment if they aren’t sure where their information is going.
“The risks are really great, particularly during the nation’s opioid crisis. You’ll have people who are afraid to go into treatment because they’re afraid where that treatment information might go,” she says, adding that moving away from Part 2 opens patient information up to more disclosures and re-disclosures to a variety of entities without consent.
“They may know their information going for treatment purposes, but they won’t know who. It may be some physician or some other type of provider who treated them badly in the past,” she says. “We all want patients to get better care. We all want patients who need substance use disorder treatment to get it. …
“What we disagree on is the line of patient consent. Do you believe in patient consent? If you do, then you would support 42 CFR Part 2,” she says.
Reid says it’s true that people who seek treatment for general care probably aren’t thinking about their medical records, but the same doesn’t hold true for patients with substance use disorders.
“If I have a substance use disorder, for example, an alcohol problem or any type of drug problem … I’m going to care where my information goes,” she says. “It’s because society is still stigmatizing the illness and also because there’s still discriminatory treatment against people who have certain illnesses, unfortunately.”
But Waller says he’d like to see the data that shows people won’t seek treatment because they are concerned about where their medical records will end up.
“Not one piece of data supports that argument, not one memo, not a case report,” he says.
Waller does agree that there is a problem with stigma in society that needs to be tackled, however.
“Once we handle the stigma by normalizing the fact that this is ultimately a chronic neurobiological disorder and we’re going to treat it as a chronic disease—and if you have it, we recognize it and we treat it, and we move on—then that won’t be an issue,” he says.
TECHNOLOGY WWW.BEHAVIORAL.NET 37
Alicia Hoisington is a freelance writer based in Ohio.
ARCHITECTS
BWBR
Saint Paul, MN
Contact: Richard Dahl, AIA (651) 222-3701
marketing@bwbr.com www.bwbr.com
Corbin Russwin

Berlin, CT
Contact: Wayne Falce (860) 225-7411
wayne.falce@assaabloy.com www.corbinrusswin.com
FURNITURE/FURNISHINGS
CR Goodman Associates

Annapolis, MD
Contact: Sandy Goodman (410) 841-2570
info@crgoodmanassociates.com www.crgoodmanassociates.com
ESa (Earl Swensson Associates)
Nashville, TN
Contact: Sandy Dickerson (615) 329-9445 sandyd@esarch.com www.esarch.com
NK Architects
Morristown, NJ
Contact: Ben Lee (973) 539-5353 leeb@nkarchitects.com www.nkarchitects.com/
DOOR HARDWARE
Accurate Lock and Hardware
Stamford, CT
Contact: Monica Nunez (203) 348-8865 monica@accuratelockandhardware.com www.accuratelockandhardware.com

Accurate Lock and Hardware offers an extensive range of ligature resistant and ADA-compliant products that positively contribute to healing environments. Accurate’s team of experts are dedicated to developing innovative solutions for specific challenges including retrofit scenarios, custom openings and safety compliance. Designed with patient care and staff safety in mind, all Accurate products are made entirely in the USA, which allows the ability to quickly adjust, adapt and produce the best solutions to meet the everchanging needs of the healthcare industry. Simply put, your challenge is Accurate’s challenge.
As healthcare facilities transform, Corbin Russwin’s Behavioral Health Series is providing products with a superior design that are safer for patients, while maintaining a modern aesthetic. With products that provide a unique combination of aesthetics, safety, security, and durability that is unmatched in the industry, Corbin Russwin products have a unique style that brings healthcare and design together with the ability to withstand the most abusive environments.
Carstens Inc.
Chicago, IL
Contact: Mike Cook (800) 782-1524
carstens@carstens.com

www.carstens.com
Carstens' WALLAroo® storage cabinets and computer workstations, mobile carts, and chart racks with locking doors are ideal for behavioral health facilities focused on workflow improvement and enhanced patient care. WALLAroos are designed for securely storing computers used for EHR and/or medications and supplies. Carstens' chart racks have locking doors to aid with HIPAA compliance, secure patient records and protect patient privacy. Carstens is a certified womanowned small business and manufactures products in the USA.
Sargent Manufacturing Company
New Haven, CT
Contact: David Higginson (800) 727-5477
david.higginson@assaabloy.com www.sargentlock.com

With ligature-resistant door locks and hardware, SARGENT Manufacturing’s Behavioral Health Series sets the standard for safety and security in a healthcare setting. The innovative designs provide users with durable, versatile products that are easy to use while increasing patient safety. These products can be used in the most demanding environments; combining safety and reliability with design and transforming the patient experience.
FLOORING, RESILIENT
nora systems, inc.
Salem, NH
Contact: Customer Service (800) 332-6672
healthcare-us@nora.com
www.nora.com

Furniture Concepts
Cleveland, OH
Contact: Katie Krizek (800) 969-4100
info@furnitureconcepts.com
www.furnitureconcepts.com


TECHNOLOGY GUIDE 38 SUMMER 2018 BEHAVIORAL HEALTHCARE EXECUTIVE WWW.BEHAVIORAL.NET
Spec Furniture
Toronto, ON
Contact: Dubravka Milinkovic (888) 761-7732
specit@specfurniture.com

www.specfurniture.com


Spec Furniture(r) is recognized as a market leader in the quality, design, and engineering of healthcare seating and tables products, focusing on a wide range of lounge and occasional seating designs. Spec's behavioral health product has been recognized as product of excellence at the 2017 Nightingale and 2018 Best of NeoCon awards. Every Spec product is supported by an industry leading warranty and a dedication to outstanding customer service.

INTERIOR DESIGNERS
Pickett Design Associates

Walnut Creek, CA
Contact: Christine Hardin (310) 558-5500

chardin@pickettdesigns.com
www.pickettdesigns.com
WASHROOM/LAVATORY
Bradley Corporation
Menomonee Falls, WI
Contact: Abigail Heppe (262) 532-6072
abigail.heppe@bradleycorp.com
www.bradleycorp.com


WWW.BEHAVIORAL.NET 39
DANBROWNCONSULTING.COM LEARN MORE. Since 1987, Brown Consulting, Ltd. has assisted hundreds of mental health and addictions treatment organizations in successfully reaching their goals. We provide a full range of consulting services. Specialist in Regulatory Compliance. Give us a call today! 1-800-495-6786 RESULTS! NOT PROMISES. Pages Pages Accurate Lock and Hardware 1, 9 Alkermes 5 Brown Consulting ............................................................... 39 Credible Behavioral Health Software CVR4, 20, 21 Dominion Diagnostics CVR2 Dreamscape Marketing 5 Furniture Concepts 11, 32 Institute 2-page Spread Ad 30, 31 Mattress Firm 14 Spread House Ad 26, 27 TCIV house ad 3 This End Up 39 Whitehall Manufacturing CVR3, 7 ADVERTISER INDEX thisendup.com (800) 979-4579
FYIPEOPLE
AWARDS
AWARDS
Oxford Treatment Center has named Mark Sawyer CEO and Mark Stovall, CAT, CMHT, chief operating officer.
POLICY PROGRAMS
Spectrum Health Systems announced it has received its sixth consecutive CARF accreditation for its continuum of care, including its inpatient, outpatient and residential services.
Desert Hope Treatment Center has been awarded the Joint Commission’s Gold Seal of Approval for its services.
Mental Health News
Education presented its 2018 Leadership Award to Jim Spink, Beacon Health Options Mid-Atlantic, market president.
The Rosecrance substance abuse program has earned an Aetna Institute of Quality designation for behavioral health.
PEOPLE PEOPLE
Doug Foote has been named chief operating officer of The Emily Program, an eating disorder treatment provider.
JourneyPure has named Stephen Loyd, MD, medical director for four outpatient clinics and one residential facility in Tennessee.
Bethany Kassar, MSW, LCSW, has been named executive director of Liberation Behavioral Health LLC, to manage operations of its Liberation Way programs in its Pennsylvania addiction treatment facilities in Bala Cynwyd, Fort Washington and Yardley.
Rosecrance appointed Elizabeth Ellison as the new executive director at the Lakeview Recovery Home and Facility in Chicago.
AWARDS
Recovery Centers of America has named Adam Brickner CEO of its Waldorf, Md., facility that serves the southern Maryland and Washington, D.C., area. RCA also announced that Theresa Donovan has joined its Danvers, Mass., facility as quality manager.
POLICY PROGRAMS FUNDING
Cynthia Hollingsworth, LCSW, DHSc, has been named clinical director at Sunspire Health Recovery Road.
The Baltimore Station, a residential treatment program supporting veterans and others transitioning from homelessness and addiction to self-sufficiency, has added five new members to its board of directors: Jay Larson, Frank McNeil Jr., Joseph Salek-Nejad, Adam Skolnik, CPM, ARM and Lawrence “Eric” Wyss, CFP, AEP, CTFA
Delphi Behavioral Health Group has appointed Linda S. Earhart as the company's new chief operations officer
and Heather Ata as its chief marketing officer.
AWARDS
TRT Holdings Inc. has named longtime executive Jim Caldwell president and CEO of Origins Behavioral HealthCare.
PROGRAMS
PEOPLE POLICY
PROGRAMS FUNDING
Addiction Policy Forum has launched a confidential resource line for those in Ohio struggling with substance use disorder, as well as their loved ones. The line can be reached at 1-833-301-HELP (4357).
The American Indian College Fund, in partnership with United Health Foundation, has launched the United Health Foundation Tribal Wellness Scholarship Program to create a pipeline of mental health and substance abuse professionals in North Dakota to serve remote and rural communities.
Seabrook addiction treatment center has applied to the state of New Jersey, DHS, Office of Licensing, to add an additional 13 licensed residential detox beds to its existing 37 licensed beds at its Bridgeton, New Jersey, location.
Beacon Health Options announced it has raised its minimum pay rate to $15 per hour.
Center For Discovery has
opened Discovery Austin, an outpatient eating disorder treatment program in Austin, Texas.
Lancaster Behavioral Health Hospital has opened a 126-bed behavioral health facility in Lancaster, Pa. The facility will serve adolescents, adults and older adults, and will also feature a dedicated women’s trauma unit.
Beacon Point Recovery Center has opened a detoxification and residential addiction treatment facility in the Port Richmond area of Philadelphia.
Constellation Behavioral Health announced the opening of the BrightQuest Nashville mental health facility in Tennessee.
Delphi Behavioral Health Group announced it has acquired Family Recovery Specialists, a Miami, Fla.based outpatient program.
Fairhaven Treatment Center in Memphis, Tenn., has been acquired by Refresh Mental Health.
Rosecrance announced that it has agreed to a merger with Iowa-based Jackson Recovery Centers that is expected to be finalized in mid-2019.
Private equity firm BelHealth Investment Partners has finalized a deal to acquire Beach House Center for Recovery with facilities in Palm Beach County, Fla.
40 SUMMER 2018 BEHAVIORAL HEALTHCARE EXECUTIVE WWW.BEHAVIORAL.NET
BestCare® LIGATURE-RESISTANT fixtures ultimately reduce ligature points to ensure a safer and more secure behavioral healthcare environment.
DO YOU SEE THE LIGATURE POINTS?
LIGATURE POINTS IN A TYPICAL BATHROOM

In traditional restroom applications, ligature points are more common than you might realize. The arrows above indicate dangerous ligature points in existing bathrooms.
Did you know? Most inpatient suicides occur in the facilities bathrooms.

6 4 5 1 2 3 7 9 8 11 12 10 3 9
1. Showers
2. Soap Dishes
3. Grab Bars
4. Sinks
5. Shelves
6. Mirrors
7. Paper Towel Dispensers
8. Tank Style Toilets
9. Towel/Clothes Hooks
10. Spindle-less Toilet Paper Holders
11. Linear Drains
BESTCARE®
PLUMBING FIXTURES & ACCESSORIES RENOVATE / DESIGN YOUR NEW BATHROOM
12. Floor Drains
TYPICAL
LIGATURE-RESISTANT
MORE INFORMATION: whitehallmfg.com •1-800-782-7706
FOR

Hundreds of Partners. One at a Time. Now it’s your Turn. The Power of One. The Benefits to Many. Now It ’s Your Turn. 301.652.9500 | partnership@credibleinc.com | credibleinc.com

























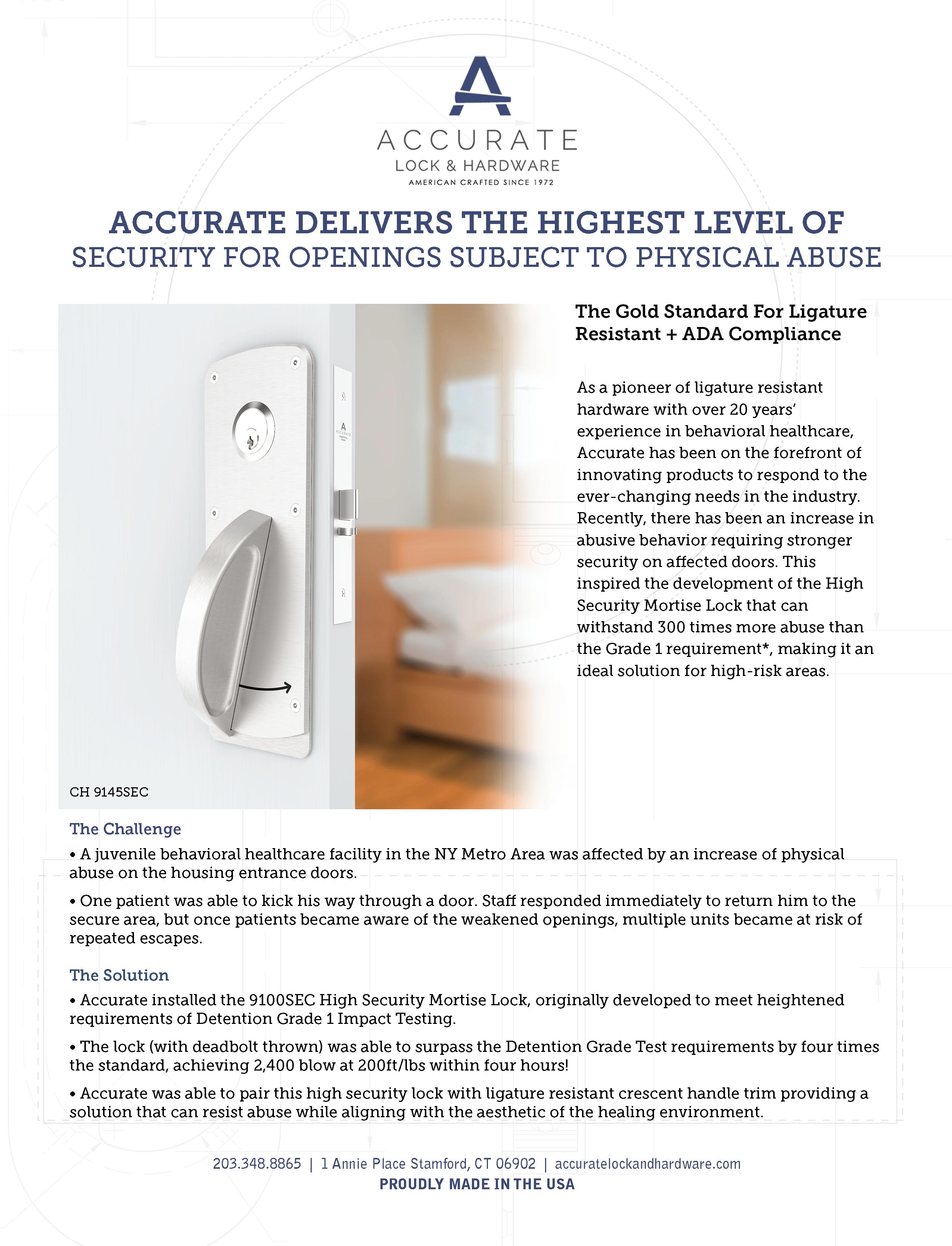




























 BY JULIE MILLER
BY JULIE MILLER


 BY TOM VALENTINO
BY TOM VALENTINO






































