WORKFORCE SURVEY
Leaders seek solutions to fortify the workforce
PLUS
❯ NAATP enforces ethics code
❯ How to add value
❯ Benefits of equine therapy
























































Leaders seek solutions to fortify the workforce
PLUS
❯ NAATP enforces ethics code
❯ How to add value
❯ Benefits of equine therapy























































BestCare® LIGATURE-RESISTANT fixtures ultimately reduce ligature points to ensure a safer and more secure behavioral healthcare environment.
TYPICAL BESTCARE® LIGATURE-RESISTANT PLUMBING FIXTURES & ACCESSORIES

DO YOU SEE THE LIGATURE POINTS?
LIGATURE POINTS IN A TYPICAL BATHROOM
In traditional restroom applications, ligature points are more common than you might realize. The arrows above indicate dangerous ligature points in existing bathrooms.
Did you know? Most inpatient suicides occur in the facilities bathrooms.

EDITORIAL
Editor in Chief Julie Miller
(216) 373-1204 • jmiller@iahbhc.com
Senior Editor Tom Valentino
(216) 373-1225 • tvalentino@iabhc.com
DESIGN
Creative Director Dave Villafañe
SALES
Director of the Institute for the Advancement of Behavioral Healthcare
Douglas J. Edwards (216) 373-1201 • dedwards@iabhc.com
Traffic Manager
Judi Zeng
(212) 812-8976 • jzeng@vendomegrp.com
Please send IOs to adtraffic@vendomegrp.com
All ad materials should be sent electronically to: https://vendome.sendmyad.com/
CUSTOMER SERVICE/SUBSCRIPTIONS
Call: 1-888-244-5310, email to: VendomeHM@emailpsa.com, or visit: www.iadvancebehavioralhealthcare.com/subscribe
REUSE PERMISSIONS
Copyright Clearance Center info@copyright.com Ph: 978-750-8400
Fax: 978-646-8600
ADMINISTRATION
Chief Executive Officer Jane Butler
Chief Marketing Officer Dan Melore
Vice President, Finance Bill Newberry
Vice President, Custom Media Jennifer Turney
Director, Circulation Rachel Beneventi
JILL SEDERSTROM BY ED JONESBehavioral Healthcare Executive (ISSN 1931-7093, Online 2167-9649) is published four times per year by Vendome Group, LLC, 237 West 35th St., 16th Floor, New York, NY 10001. ©2018 by Vendome Group.

Behavioral Healthcare Executive is a trademark of Vendome Group, LLC. All rights reserved. No part of Behavioral Healthcare Executive may be reproduced, distributed, transmitted, displayed, published, or broadcast in any form or in any media without prior written permission of the publisher. To request permission to reuse this content in any form, including distribution in educational, professional, or promotional contexts or to reproduce material in new works, please contact the Copyright Clearance Center at info@copyright.com or 978.750.8400.

EDITORIAL: Behavioral Healthcare Executive is the practical resource for intelligence that executives can apply to meet current leadership, financial, clinical, technology, and compliance needs Behavioral Healthcare Executive is indexed in the National Library of Medicine’s MEDLINE/ PubMed database. Articles and opinions published in Behavioral Healthcare Executive do not necessarily reflect the views of Vendome Group or the Editorial Advisory Board.
SUBSCRIPTIONS: For questions about a subscription or to subscribe, please contact us by phone: 888-244-5310, online: http://www.iadvance behavioralhealthcare.com/subscribe or email: VendomeHM@emailpsa. com. Subscription rate per year: $140 domestic, $169 outside the US. Single copies and back issues: $20 Domestic, $32 outside the US.
POSTMASTER: Send changes of address to: Behavioral Healthcare Executive, PO Box 11404, Newark NJ 07101-4014.




• Twitter: @BehavioralHlth
@Editor_JMiller | Editor in Chief Julie Miller
@ValentinoWrites | Senior Editor Tom Valentino
• Facebook.com/BehavioralHealthcare

April 2-5, 2018
National Rx Drug Abuse & Heroin Summit
Atlanta
The National Rx Drug Abuse & Heroin Summit is where solutions are formulated, stakeholders convene, and change begins. Be part of the international discussion on addressing the opioid crisis by attending the 2018 Summit.
https://vendome.swoogo.com/2018-rx-summit/
April 30-May 2, 2018
Treatment Center Executive & Marketing Retreat
Hilton Head, South Carolina
The second annual Treatment Center Executive & Marketing Retreat provides CEOs, CFOs, COOs, directors, senior marketing/business development/admissions leaders, and other executives with the tools they need to effectively and ethically grow their services in a rapidly changing market.

https://vendome.swoogo.com/2018-Executive-Marketing-Retreat
August 19-22, 2018
National Conference on Addiction Disorders
Anaheim, Calif.
Join addiction treatment and behavioral healthcare professionals of all types who are working together to advance recovery at the 2018 National Conference on Addiction Disorders.
https://vendome.swoogo.com/NCAD-2018
December 10-12, 2018
Treatment Center Investment & Valuation Retreat
Scottsdale, Arizona
The Treatment Center Investment & Valuation Retreat brings together owners and senior executives from the addiction treatment and recovery community to meet with key members of the investment and financial community for an exclusive three-day educational, business and networking event.
https://vendome.swoogo.com/TCIV-2018
For details on more upcoming events near you, visit: https://iadvancebehavioralhealthcare.com
Northern Kentucky University is the proud Platinum Sponsor of Education and Community for the 2018 National Rx Drug Abuse & Heroin Summit. When we come together, we can uncover breakthrough solutions to our society’s most challenging population health problems. We are excited to carry this mission forward when our Health Innovation Center opens this fall.

Learn more about NKU’s Health Innovation Center and our work to understand – and address – challenges to health and wellness.


Stop by Booth 802 during the conference in Atlanta April 2-5 or visit us online at
NKU.EDU/HICINFO
Kentucky’s drug death rate has risen 33% in the past five years and the state is ranked as having the 2nd highest number of deaths.
(America’s Health Rankings® Annual Report)
t’s clear that the behavioral health workforce is stretched to its limit. Truly the only way to fortify the workforce is to incentivize employable Americans to join the profession by offering decent wages and a reasonably comfortable lifestyle. But where is the money going to come from to supply the paycheck that ultimately will energize a new team of clinical workers? We have some choices.
1. Get more money from public sources. Many not-for-profits continue to struggle with underfunded programs and Medicaid rates that don’t even cover the cost of delivering services. When I was chatting recently with Linda Rosenberg from the National Council for Behavioral Health, she told me even the directors of the organizations themselves are thinking about career alternatives.
New appropriations of public funds to help pay workers to treat mental health and addiction disorders seems like a political longshot these days. It could happen in modest increments, but I wouldn’t count on major investment.
The best hope here is an expansion of Certified Community Behavioral Health Clinics, currently operating in eight states. Early in the demonstration phase, the clinics are working to create a flexible payment model that would absorb the cost of all the professionals required to provide the care a community needs.
2. Charge patients more. It’s not unusual for any provider to shift costs onto those who have the means to pay—such as those with decent health insurance or higher incomes. However, in behavioral health, the shift is already so great, it’s hard to image the market (or the mission) bearing much more. This is an extremely unlikely option for unearthing new funds that can be funneled toward the workforce.
3. Charge insurance companies more. Commercial payers want value propositions that demonstrate good clinical quality along with net cost savings. And the payers themselves will decide what qualifies as savings. Your call to action here is to understand your true delivery costs and your honest outcomes with incredible granularity. It’s tough negotiating with payers, but some providers have been successful.
Industry leaders and researchers agree that the pipeline of new clinical professionals will remain dry for the foreseeable future. Stakeholders must find a way to increase wages for experienced workers and develop a satisfying career path for new recruits.
David Chernof, MSW, LCSW, MBA
Consultant, Behavioral Help, LLC; Associate Clinical Director, Queen of Peace Center
Patrick Gauthier
Director, AHP Healthcare Solutions

Nancy Hale
Program Director, Operation UNITE
Andrew Kessler
Founder and Principal, Slingshot Solutions
Jean Krisle
Founder and CEO, 10,000 Beds
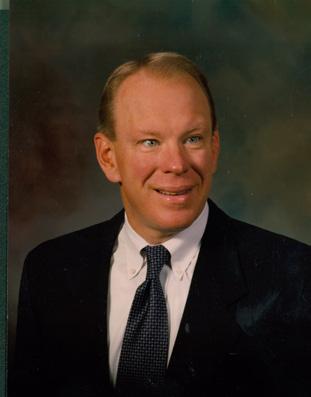
Edward R. Jones, PhD
Senior VP for Strategic Planning, Institute for Health and Productivity Management
Ron Manderscheid, PhD
Executive Director, National Association of County Behavioral Health and Developmental Disability Directors
Steven Millette Director, Gloo Inc.
Linda Rosenberg
President/CEO, the National Council on Behavioral Health
Raymond Tamasi
President, Gosnold on Cape Cod
Doug Tieman President/CEO, Caron Treatment Centers
Mary Woods CEO, WestBridge
Julie Miller, Editor-in-Chief










he psychiatrist Thomas Szasz wrote a popular book in the 1960s, “The Myth of Mental Illness.” Mental illness is not a myth, but it is murky. People with serious conditions such as bipolar disorder and schizophrenia are most assuredly suffering from an illness. The National Alliance on Mental Illness (NAMI) was formed to support the individuals and families impacted by these illnesses, but we need to evaluate our scientific claims and our messaging for mental illness.
Psychiatrists have embraced a biological model of mental illness for decades and have prescribed a variety of psychotropic medications. However, skeptical researchers have evaluated many studies supporting antidepressants (including those submitted to the FDA) and have found that most of their benefits derive from placebo effect rather than chemical action.1 I remember simpler days of telling patients that their physician was prescribing their medication for a “chemical imbalance.” They would typically nod in acceptance of this simplistic biological hypothesis, which they mistakenly assumed to be well-validated, about what was impacting their lives.
Today, we have various neurotransmitters that are presumably unbalanced in various ways, and they are at the root of different solutions developed by the
pharmaceutical industry. The chemical balance explanation now makes little sense, and so we should come to terms with all the specious hypotheses that have been put forward about how medications work. At the same time, let’s not fail to raise the more fundamental question: H ow well do they actually work?
In this regard I would offer the thoughts of Richard A. Friedman, MD,2 professor of clinical psychiatry at Weill Cornell Medical College.
“American psychiatry is facing a quandary: Despite a vast investment in basic neuroscience research and its rich intellectual promise, we have little to show for it on the treatment front. With few exceptions, every major class of current psychotropic drugs— antidepressants, antipsychotics, anti-anxiety medications—basically targets the same receptors and neurotransmitters in the brain as did their precursors, which were developed in the 1950s and 1960s. Sure, the newer drugs are generally safer and more tolerable than the older ones, but they are no more effective.”
My question is whether every depressed person has an illness—a mental illness—on par with the cold and flu viruses people experience every year. Who asserts this? Proponents of biological psychiatry are the main standard bearers, be they from the pharmaceutical or psychiatric ranks, and they may simply advocate in a seemingly harmless way that a biological model will be validated at some future time. What are the benefits of assuming that all the disorders of mental health or emotional health are rooted in a mental illness? I would suggest none.
Prescribers often fall back on anecdotal evidence from their patients. Is the sad conclusion from medication research studies that we must admit that depression is a condition we really don’t understand after decades of study?
We can approach this from another angle. We know there
We must decide which one leads the way
BY ED JONES, PHD
are plenty of studies (and anecdotal reports) of people who “recovered” from depression after months of treatment with a clinician providing cognitive behavioral therapy. Was this recovery from an illness? Or was it recovery from a mental state that is not really an illness? Was it recovery from a negative state of mind learned over many years?
Many would argue that DSM diagnoses like addictions and eating disorders are illnesses. We certainly know why this is the case. We know how these conditions typically progress clinically and how they often result in death. Is there a physical progression underlying these conditions? Are they deteriorating mental states without a physical basis? We have theories, and yet we have few facts or conclusions. Again, the bias is to find a biological substrate for presumed mental illnesses along with bio-chemical solutions.
We know why there is a desire to place destructive patterns of thoughts, feelings and behaviors under the rubric of illness. The alternative has often been accepting moral judgments about personal failings, and just as worrisome, accepting limited funding for research and treatment for conditions that fall outside the medical model.
There is also a compelling logic to the model of illness. If we view addiction as being comparable to a chronic medical condition like diabetes, then we are more likely to develop a sensible, long-term treatment plan. Is it a problem that in many ways we understand the biology of diabetes better than the biology of addiction? Not if a curative addiction pill is on the horizon.
My point here is to be provocative— such a pill may be on the horizon for all I know—but I am challenging the assumption that it is wise to put most problems into the category of illness and wait for the new medications to arrive.
CleanSlate Centers offers hope for patients and families battling addiction, but we can’t do it alone.
Join our team by visiting us at CleanSlateCenters.com


We know why there is a desire to place destructive patterns of thoughts, feelings and behaviors under the rubric of illness
I would add one final critical thought, and it is about the dark side of marketing. Are we in the arena of science or marketing when we discuss mental illness?
When science is simply a bias about how we should validate a certain point of view—when marketing of that “science” has a financially-driven goal—when the medical model is more important than any findings—aren’t we are simply in the world of marketing? We are promoting ideas that may or may not have validity, but we are driven to support the dominating ideology, for financial value. This is a corrosive development.

My primary point is that we should discard the messaging about mental illness. We don’t really know what we are talking about if the assumption about illness is that we know biological causes. We should go in another direction. Mental health should be more highly valued and discussed.
It is a cornerstone to our overall health status. We should have no problem stating that we want to find ways to increase
our overall state of mental health. We might prefer to call it wellbeing or emotional health instead, but the point is the same—we want to enhance our general health status in a way that derives from our emotional health or our mental health.
Physicians have operated very well through the years by identifying the underlying biomedical cause for a condition and then treating it with surgery, medication, radiation, or an ever-expanding range of treatment options. While this may yet prove to be the model of psychological disorders, we are far from that point today.
Should we continue to assume that everything will be understood and resolved at a biological level? I think not, since we have few encouraging signs for persisting in this way. More importantly, we might benefit greatly from removing the focus on origins or causality. Let’s instead focus on mental health and emotional health.
I will be the first to applaud the development of medications that cure debilitating psychological conditions, or improve mood and/or cognitive functioning. However, our focus for research and our focus for care need not be the same.
Physician anesthesiologists are key to reduced opioid use during surgery and postoperative non-opioid pain control

• Ensure a physician anesthesiologist is involved in your pain care plan when undergoing surgery
• Regional anesthesia and analgesia with a multimodal approach is key to opioid free surgery; physician anesthesiologists have specialized training in these techniques and can assist with non-opioid postsurgical pain control
• Interventional therapies can be used to treat chronic pain and therefore prevent addiction to opioids
Contact your physician anesthesiologist when preparing for surgery asahq.org/resources
Let’s support research into the bio-psycho-social dimensions of illness, and yet let’s not forget that our primary focus as a society should be on improving health for all citizens today, not at some point in the future.
Let’s shift the discussion to mental health and away from mental illness, not only for scientific reasons, but also since our society will advance more from focusing on mental health than mental illness. Let researchers figure out the sources of illness in their laboratories, while we focus on advancing health in the face of all real-world challenges. Let’s identify paths to better health every day with an understanding that the validated sources of illness may be far off in our scientific body of evidence, and biological sources may be less prominent than we imagine.



The fundamental point is clear. We should embrace a discussion about mental health and emotional health, and we should leave the concept of mental illness for another day.

Let’s find everything we can do to improve health. Let’s embrace the non-stigmatizing terms of mental health and emotional health. Let’s wait to see what research determines is driving the development of the problems we treat.
We can help many people regardless of whether they suffer from bad genes, bad germs, bad habits, bad attitudes and so on. Messaging is important. Focus is important. Our field and our patients are better off focusing on enhancing health rather than battling illness.
Ed Jones, PhD, is senior vice president for the Institute for Health and Productivity Management.
2 Online link to New York Times Editorial by Dr. Friedman: https://www.nytimes. com/2015/07/19/opinion/psychiatrys-identity-crisis.html?rref=collection%2Fcolumn%2Frichard-a-friedman&action=click&contentCollection=opinion®ion=stream&module=stream_unit&version=latest&contentPlacement=10&pgtype=collection

In January, Behavioral Healthcare Executive surveyed its audience on industry-specific workforce issues. More than 600 treatment center professionals responded, and results indicate that clinical staffing remains the top workforce challenge not just to ensure quality of care but also to allow for future program growth.
The most surprising finding was that almost half of the audience with some knowledge of the business’s growth say that their organization at some point has abandoned service expansion plans because of concerns about finding the right clinical staff. It’s an issue that speaks to both the quantity and the quality of the available workforce in local areas.

When characterizing the various types of staff in comparison to current needs, respondents clearly sense there’s an inadequate supply of clinical employees. About 60% say their clinical departments are understaffed, and only 38% say such staffing is adequate.
“It doesn’t surprise me,” says Jeffrey Quamme, executive director of the Connecticut Certification Board. “Clinical staff is the hardest to recruit.”
By contrast, only 29.3% of respondents

say their administrative departments are understaffed. When looking at only the treatment center organizations that include marketing departments—more than half—about a third of those respondents indicate that they could use more marketing staff.
It’s clear that treatment professionals with clinical education and experience represent the greatest human resource need. In fact, an overwhelming majority (81.5%) of respondents say as much.
Angela J. Beck, PhD, MPH, professor and assistant dean for the University of Michigan School of Public Health and director of its Behavioral Health Workforce Research Center, says the BHE findings are consistent with national studies that estimate the workforce shortage. For example, in a November 2016 report, the Health Resources and Services Administration estimates that by 2025, the United States will experience a shortage of 250,000 workers in the field.
“We’re not expecting a huge influx of behavioral health workers,” Beck says. “But that doesn’t mean we should give up on pipeline programs.”
What the field does have going for it in terms of recruitment is the personal investment of its many workers who have experienced mental health and addiction treatment themselves and feel a calling to give back, improve the system and share their fellowship of recovery.
“This work is tremendously missional, and it’s work in which people have a lot of passion for helping others,” says Dawne Carlson, vice president of human resources for Hazelden Betty Ford Foundation. “And because it is such deeply felt work, it
can sometimes feel heavy.”
Carlson says those who care for patients and clients can get burned out easily, and that’s why the turnover rates can be rather high in comparison to other health specialties. Self-care is imperative, she says.
More than 28% of the BHE survey respondents indicate that their clinical staff turnover rates are higher than industry average.
“I don’t have statistics on clinical staff turnover in behavioral health, but anecdotally, we know it’s pretty high,” says Beck. “This is a field in which burnout is high, compensation is comparatively low, and there’s still some stigma attached to working in mental health and addictions. That three-quarters of your respondents are reporting turnover at the industry average or more than industry average would be concerning.”
About half of survey respondents say their organization offers tuition reimbursement or similar education benefits. Such perks can help retain workers while also increasing clinical competencies. Additionally, nearly 17% believe that student loan forgiveness or academic scholarships would be the best solution to help attract more workers to the behavioral health field—second only to strategies that would increase workers’ pay.
In terms of solutions, Carlson says Hazelden Betty Ford offers a graduate school program that helps create a direct link from education to active clinical work at its facilities. Talent can be replenished close to home, and new openings can be filled by the graduating students who are already familiar with the organization.
Experts fully agree that good pay certainly doesn’t hurt.
“It’s important that we seek to pay competitively—that’s one of our solutions,” Carlson says. “That said, in every clinical aspect, we don’t necessarily lead the pay scale, but it’s important if you want good clinicians that you help them grow and continue to learn.”
She believes good leadership also makes a difference in retaining employees. More workers leave their jobs because they don’t care for the managers than those who leave because they don’t care for the job itself, she says.
Quamme says the rise in private, for-profit treatment centers has caused a noticeable shift of workers away from the traditional not-for-profit agency setting. Part of the attraction is likely higher pay.
“The industry does have a hard time keeping people,” he says. “Workers will jump for that one job with that $1 per hour more.”
Of the survey respondents with some knowledge on the subject, more than half report that their organization has seen a staff reduction at some point in the past two years attributed to financial strains. Even with its long established programs, Hazelden Betty Ford has had to cut staff in the past, according to Carlson.
“Healthcare as an industry is in such a state of change continuously, it’s challenging to be able to set the right levels of staff and be able to provide excellent care when margins are reducing,” Carlson says.
While some solutions can be implemented at the organization level, broader strategies might be needed to extend the reach of the workforce. For example, Beck says clinical professionals could have more impact right now if policies were in place to allow them to leverage all of their practice skills.
“It’s an area where legislators can get involved to address capacity issues in their states by ensuring the workforce they have is working up to the full scope of their practice,” she says. “It’s an issue of how you best utilize the staff you have.”
For example, a nurse might be limited by state restrictions, causing a physician’s time to get tied up in delivering services that the nurse otherwise is trained for and capable of providing.
Additionally, telehealth has been held up as a tool that could extend the workforce. Digital visits could solve some access issues, connecting more patients with behavioral health services, especially in rural areas. However, barriers to adoption—such as licensing requirements when patients and providers aren’t located
APRIL 2-5, 2018 | ATLANTA, GA
in the same state—continue to drag down telehealth’s progress.
Be part of the discussion at the largest national address the opioid crisis. Prevention, treatment, exchange best practices and hear from state and www.nationalrxdrugabusesummit.org
Beck says telehealth providers need to know who they can treat and where, taking licensing and reciprocity into account. Meanwhile, providers that are philosophically open to the idea of conducting telehealth visits might decide against it if they’re already overbooked with office visits.
AUGUST 19-22, 2018 | DISNEYLAND,
“And there are still the questions about alleviating perceptions about the quality of care with telehealth: Can you treat someone as sufficiently as with in-person care?” says Beck.
Addiction professionals annually convene at NCAD from thought leaders on delivering treatment, organizations learn how to run more effective, www.ncadcon.com
According to Quamme, clinical competency has evolved in behavioral health. While its origin might be one of fellowship or spiritual support, system pressures today increasingly call for evidence-based practice that has the science to back up its efficacy. However, there’s room for both, he says.
“I’d like to see the field put certification in higher esteem because we are the ones who guarantee competence, as opposed to permission to practice,” says Quamme. “I think they go hand-in-hand.”
NOVEMBER 12-14, 2018 | FORT LAUDERDALE,
The opioid crisis is making headlines, but another communities: stimulants. Join other stakeholders stimulant use.
In the future, as the healthcare system at large seeks greater integration, clinicians might also find themselves on large care teams. And how the teams are comprised matters, according to Beck. Sometimes it’s difficult to ensure that behavioral health professionals are equitably included in a team-based care provision—and equitably reimbursed.
www.stimulantsummit.com
DECEMBER 10-12, 2018 | SCOTTSDALE, Senior executives of treatment centers, and those growth strategies and market dynamics at this networking event.
www.treatmentcenterretreat.com
APRIL 30-MAY 2, 2018 | HILTON HEAD, TCEM provides CEOs, CFOs, COOs, directors, admissions leaders, and other executives with grow their services in a rapidly changing market. www.executiveandmarketingretreat.com
Interested in attending an event? Contact Ellen Kelley at ekelley@iabhc.com
ccording to a survey conducted last year by Behavioral Healthcare Executive, industry leaders believe that ethical standards should be enforced primarily by associations. The National Association of Addiction Treatment Providers (NAATP) is starting off the year with an updated code of ethics as well as a pledge to enforce it.
Executive Director Marvin Ventrell says that NAATP is taking a bold step by making ethical business and clinical operations requisites of membership for the first time.

“The preamble states clearly that members must comply with all elements of the code so there’s no confusion,” he says. “As a condition of membership, they agree to be removed if they do not comply.”
Of course, the goal is not to exclude organizations but rather to drive compliance across the industry with clear expectations. Ignorance is no longer an excuse for crossing the line on ethics.
“We might get smaller before we get larger,” says Doug Tieman, president and CEO of Caron Treatment Centers and one of the architects of the NAATP code.
Tieman says the high road might not be
BY JULIE MILLEReasy and might lead to legal snarls down the road, but NAATP is prepared to defend its position. The hope is that members removed will ultimately comply and become members reinstated.
The most significant updates in the code address marketing standards. For example, standards expressly forbid patient brokering or any form of remuneration for referrals.
“There is no buying and selling of leads—that needs to be said,” Ventrell tells Behavioral Healthcare Executive
Guidelines for marketing also demand transparency about the center’s identity in terms of name, location, services, licensing, accreditation and staff credentials. Online directories, for example, must include each featured center’s direct phone number.
“There are sites that pose as directories or resources, when in fact they are feeder sites to a particular organization,” Ventrell says. “It’s not clear to the consumer because the center’s name isn’t even on the page. They think it’s a clinical resource that leads to the best treatment.”
Similarly, transparency extends to statements made about licensing. Centers must be clear about what type of treatment they are licensed for and in which states. According to Ventrell, the specificity is important for consumer protection, and it’s no longer acceptable for treatment centers to gloss over their licensing details on websites and in marketing materials.
Tieman says too often treatment centers were justifying their own actions as ethical while judging their competitors as unethical. Now the code creates a common definition for marketing standards.
“The beauty of this is that we lay out ethical marketing
behavior instead of allowing everybody to interpret it for themselves,” he says.
Using a patient’s testimonial, image or identity as marketing tool while the patient is still in treatment also is prohibited by NAATP. Testimonials are usually appropriate further along the recovery path—with the patient’s written consent, of course— and many centers use them in their marketing materials.
However, Ventrell notes that some popular television talk shows are known to follow individuals in crisis and might ask a treatment center to cooperate with the show producers. NAATP members must avoid any situation that would exploit a patient for what is essentially entertainment, however, upholding ethics as they relate to media interaction might be evaluated on a caseby-case basis, he says.
And clearly, the show shouldn’t have any financial ties to the treatment center.
“There’s nothing wrong with Dr. Phil or anyone referring
someone to a center for assessment and treatment as long as there’s no payment for that referral,” he says.
NAATP is planning to offer in-person and online training sessions for members, according to Tieman. In time, the association also will compile a list of providers that have completed training and pledge to follow the ethics code. That list could be valuable to third-party payers looking to contract with the best quality providers.
“You’ve got a built-in advantage because you can say you’re doing things the right way,” Tieman says.
In his experience, payers are skeptical of most providers because they all claim to be high quality but have no way to verify it.
Tieman anticipates that NAATP membership could serve as that verification and ultimately offer a competitive advantage in the market.
dding value is something that Turnbridge President and CEO David Vieau talks about regularly with his peers in the field.
“It’s been an interesting ride in this industry through the conferences and listening to other CEOs speak,” says Vieau. “I’ve been hearing ‘adding value’ for a long time. We’re talking about how a corporation can grow and expand. I’ve always thought this industry needed to treat adding value differently than the electronics industry or the IT industry. We have a unique responsibility that we’re treating people in what could be fatal situations.”
“Value” in the context of behavioral healthcare largely is defined by the priorities of the stakeholder, and creating added value in many instances comes down to speaking the language of various constituents and delivering measurable results that reflect their needs, says Siobhan Morse, division director of clinical services for Foundations Recovery Network.
Whereas providers want efficient operations, and payers might be most interested in rates of client readmissions, patients’ family members might care more about the number of times clients have had significant conflicts with loved ones within the past month.
BY TOM VALENTINOBasic economics will tell you that value is a function of price vs. quality, Morse says.
“When you talk about value, you have two options,” Morse says. “You can decrease the price, which no one wants to do, or you can increase the integer in that formula that is associated with quality. Given the current price, how can I improve the quality of my product? How can I add something that speaks to the quality of my product? What can I add that is going to, in effect, make the price seem lower?”
Morse says providers across the industry have been less than stellar in defining their quality of care and answering the questions of stakeholders by speaking objectively and answering questions in an empirical, fact-based manner.
Morse refers to the six domains of healthcare quality that have been established by the Institute of Medicine and are recognized by the Agency for Healthcare Research and Quality. The domains say healthcare should be:
• Safe
• Effective
• Patient-centered
• Timely
• Efficient
• Equitable
For Turnbridge, which has 187 extended care beds at 16 facilities in the New Haven, Conn., area, analyzing its efficacy and efficiency begins with its robust system for monitoring its patient data.
Understanding ways to increase value for all parties can ultimately make the difference on providers’ bottom lines.
Vieau estimates that Turnbridge employs between 60 and 80 staff members who are measuring data on an hourly basis and sharing data with care team members. Patients’ responses to treatment are evaluated against others with a similar disorder acuity within the same socio-economic demographics.
There is a slogan often repeated around the halls of The Abbey Addiction Treatment Center in Bettendorf, Iowa: “Our job is to help get people into treatment, not keep them out.”
Founder Joseph Lemon Jr. says the first way in which The Abbey looks to improve its value proposition is by prioritizing access and affordability of care because it believes taking in clients at the moment they are ready to enter treatment enhances their odds for successful outcomes.
“You want to strike while the iron is hot with their readiness to change,” Lemon says.
For The Abbey, that means accepting insurance and working with clients to structure payments over an extended period, defraying costs up front, if necessary.
Having well-measured results that can clearly demonstrate a program’s efficacy eases relations when working with insurers, Vieau says.
Turnbridge does not have call centers, and it spends just “a very small percentage” of its top-line revenue on marketing. Vieau says the organization has found better value in putting its money into research and developing efficacy, which has resulted into targeted programming that fits a select population.
By design, Turnbridge works only with young people in gender-specific programs. Vieau says concentrating a targeted population instead of casting a wide net with a one-size-fits-all approach has directly correlated with success at its various sites.
“Not only do we want the right program and the right fit, but also for the right people in the right places,” Vieau says.
“Commercial insurance is saying, ‘Why should we pay X?’ ” Vieau says. “Efficacy is critical going forward.”
While some value propositions appeal to a specific subset of stakeholders, offering complementary continuing care is one strategy that has proven beneficial for all parties in the treatment equation for The Abbey, Lemon says.
Several opportunities for alumni participation are baked into the provider’s programming. This keeps past clients engaged in their recovery and helps current clients see where their next steps can lead. Past clients are also welcomed to return for a day or two when they self-identify symptoms for a potential relapse. Alumni receive “a booster shot" of programming that reintroduces principles of their treatment to stave off a physical relapse, Lemon says.
He acknowledges that patients aren’t the only ones who find value in the complementary continuing care.
“It’s a much less expensive way to care for patients—they miss less work and time with their family if they can be with us for a day or two instead of a month or two,” he says, “And if we can do anything to enhance their success, it reflects well on our program.”
Tom Valentino is Senior Editor of Behavioral Healthcare Executive.Having wellmeasured results that can clearly demonstrate a program's efficacy eases relations when working with insurers.
he practice of sending insurance reimbursement for services directly to a patient, rather than the provider who performed the services, significantly impairs a provider’s ability to collect the payment and ultimately could create access issues for patients themselves. While experts say this practice isn’t necessarily common in the industry, it can occur during denial reviews or in cases where a patient has used an out-of-network provider. Even though more treatment centers are going innetwork, a large number of residential centers remain uncontracted. Reduced provider choices for patients can cause an increasing number of disputes on coverage, says Randy Notes, principal in the Healthcare Life Sciences Practices at KPMG.
In these situations, payers may decide to adjudicate the claim and send payment to the patient instead, making it difficult for a provider to be reimbursed for the services it already provided.
“The odds of collecting that are really low,” Notes says, adding that once a bill surpasses the 120 or 180 day mark on the books, it’s unlikely to ever be paid.
According to Tami Mark, senior director of behavioral health financing for RTI International, consumers are three times more likely to go out-of-
BY JILL SEDERSTROMnetwork than in-network for psychiatric services due to a lack of available providers. Mark and her colleagues recently examined reimbursement disparities between in-network and out-of-network providers for a study published in Psychiatric Services in 2017.
Tactics that make collecting reimbursement more challenging for providers will only continue to reduce access for patients.
“We’ve set up this system where we have the providers on one side who are trying to charge as much as possible and make as much income as possible, and then we have the insurers on the other side who are trying to pay as little as possible and make as much income as possible,” Mark says. “And we have these little patients who are crushed in between or just trying to get care and not go bankrupt.”
Some providers have started to fight back against the practice of sending reimbursement directly to patients.
In the summer of 2016, Blue Cross and Blue Shield of Georgia faced two separate lawsuits from two different providers who accused the payer of sending reimbursements for emergency room services directly to the patients.
The Polk Medical Center, one of the providers suing the insurer, claimed that the practice was being used in retaliation for not agreeing to be part of the insurer’s network, according to a Kaiser Health News article written at the time of the lawsuit.
In both cases, the providers claimed the practice had significantly hurt their institutions financially.
According to Notes, collecting payment later from the patient can often be difficult for hospitals or other providers because by the time a provider tries to collect, patients may have already spent the money they received, which in some cases could be several thousand dollars.
“That’s not to say that patients are dishonest, but they get paid the money, then they don’t understand why. So they may spend it,” he says.
Hospitals can go after the patient for payment—and in some cases send the bill to collections.
“Most hospitals do not like to do that because the fallout usually is worse,” Notes says.
Providers who are impacted the most are those who are obligated to make sure a patient is stabilized and treated under the Emergency Medical Treatment and Labor Act (EMTALA) regardless of their insurance status or provider. Once services are provided, the provider is then left to try to recoup payment on their own from the patient. Too often the unpaid bill is accounted as bad debt.
Payers know all too well the challenges providers have in collecting payments from patients who receive reimbursement directly and may choose to capitalize on that during contract disputes in the hopes that a provider may return to the negotiating table and be more agreeable in reaching a deal.
“It really presents all sorts of issues for the provider in particular,” Notes says.
Certainly, there are ethical concerns with sending patients large sums of money while they are trying to maintain sobriety. Imagine a person with just a few weeks’ recovery time getting an unexpected, unexplained check for $2,000 or more. It’s all too tempting to spend the money on bad choices.
Notes says adopting policies or procedures that don’t incentivize behavioral healthcare providers to participate in in-network agreements, such as sending reimbursement to the patient, may ultimately hurt the patients seeking treatment services.
“The real devastating component of tactics like this in the behavioral health arena would be around access,” he says.
Providers who aren’t obligated to treat a patient under EMTALA could force patients to go to another provider, come back when they have insurance that is accepted at the facility or require payment upfront for services.
According to data from Mental Health America, one out of five adults with a mental illness already reports being unable to get the treatment they need.
Many behavioral healthcare providers already choose not to participate in in-network arrangements with insurers. One reason for this is the lack of incentives to participate in such arrangements.
For instance, in her latest study, Mark found that psychiatrists received $91 for moderate to high severity evaluation and management services provided in an in-network setting. However, the rate was $122 for psychiatrists performing the same services out-of-network.
“What I would predict if this goes across the board with your third party payers like Aetna, UnitedHealthcare, Blue Cross, etc., and becomes trend, then you are going to find them aggressively carving out [psychiatry] and not covering it, because it was a money-losing business anyway,” Notes says.
But while access may be decreased, the need for behavioral healthcare services continues to grow as the country battles the opioid crisis and struggles to meet the needs of the growing population who now has access to healthcare services under the Affordable Care Act.
Mark says payers and providers will have to reach some type of agreement in the years ahead about how they can work together to meet the needs of population.
“Out-of-pocket costs are rising so fast for consumers, particularly when they go out-of-network, that it’s really not sustainable,” she says. “At some point to continue to be a viable practice, [providers] are going to have to figure out how they are going to provide services in-network.”
Jill Sederstrom is a freelance writer based in Kansas.
esidential facilities that house patients overnight are at risk for a rarely recognized nuisance: bed-bug infestations.
But experts say remaining vigilant and proactive about the tiny pests can make a world of difference for a problem that can easily get out of hand and become costly.
“The nature of treatment centers puts them at risk for infestations in the facility. Patients may freely move between a variety of activities and other patients’ rooms,” says Angela Tucker, an expert in pest management and manager of technical services at Terminix. “In addition, some patients may leave the treatment center for off-site therapy or family visits.”
Bed bugs can be found virtually anywhere people gather, according to Cindy Mannes, vice president of public affairs for the National Pest Management Association.
Because bed bugs are found everywhere people are and due to their “hitchhiking” nature, these pests often tag along on a person’s belongings, according to Tucker.
“Bed bugs do not have wings and cannot fly; nor do they jump,” she says. “Their primary mode of movement is walking or running.”
Adult bed bugs are reddish-brown in
color, oval shaped, flat and measure about one-fourth of an inch long, Tucker says. Young nymphs are smaller and could be white or yellow-orange in color. Bed bug eggs are tiny and white, and the adult female will glue her eggs inside cracks and crevices, which can make them difficult to see.
Because of bed bugs’ traveling nature, Tucker says it’s necessary for residential centers to establish protocols that address the pests, such as inspection of personal belongings and furniture within the facility. Policies also should include what to do if a staff member finds bed bugs. It’s equally important that the policies are explained to patients, family members, caseworkers and other visitors, she says.
Mannes agrees that facilities should develop a written action plan in advance of any problems. The action plan should include specific procedures and responsibilities for responding to an incident. Likewise, she says facilities should provide an information sheet to everyone that explains how to avoid bringing bed bugs into a facility.
Some tips for avoiding an infestation, according to Mannes, include:
• Prohibit the use of secondhand furniture;
• Require furniture, luggage and other personal belongings be inspected by a professional and declared free of bed bugs, or heat treated or fumigated before coming into the facility;
• Regularly vacuum or steam areas prone to bed bugs;
• Seal cracks, crevices and holes near beds;
• Repair or replace peeling wallpaper or paint; and
• Keep the clean and dirty linens separate.
Tucker says that infestations are often localized, and early detection can at least reduce their movement throughout the facility. Thus, it’s important to not only have policies in place that help avoid the pests but also ones that help to reduce the chance of making a small infestation a larger one.
“A potential policy may be that when bed bugs are identified in a patient room, that person’s cloth items should be washed, dried and placed in plastic bags,” she says. “Only items that are washed and dried should be worn outside of the patient room.”
If a bed-bug infestation is suspected, there are some ways team members can check to confirm.
“Bed bugs have evolved to feed on human blood. They also have no real defense against humans and cannot fly away. These two facts mean that bed bugs are typically found near humans, particularly near our resting areas,” Tucker says.
That’s why it’s important to routinely inspect areas such as head boards, bed frames, mattresses, box springs, sofas, group rooms and other areas where patients may rest.
Mannes advises to check for small red to reddish-brown fecal spots on mattresses, upholstery or walls. Team members, armed with a small flashlight for assistance, can pull back sheets and inspect mattress seams and box springs, particularly at the corners, for pepper-like stains or shed bed-bug skins.
Another indication will be evident on the patients—red, sometimes itchy, bite marks that appear, especially on the legs, arms and other body parts that are exposed while sleeping, she says. Additionally, heavily infested areas could have a sweet odor.
Experts say that it’s important to call a licensed professional if signs of an infestation are discovered. A professional can help confirm the infestation and recommend a treatment plan.
“Identification is critical, as some states have regulations that prevent [pest-] product use without the confirmation of pests,” Tucker says. “Perhaps most importantly, operators should remember not to panic and to follow their planned policy.”
The time frame will depend on the size of the population, control methods used and the availability of the pest-management staff, Tucker adds.
“The use of heat may take anywhere from a half-day to several days based on the size of the area that must be treated. Chemical products will take less time, and often require more than one application to be successful,” she says. “In addition, the chemicals must be applied in accordance with their instructions.
For example, if a chemical can be reapplied every seven to 10 days, then the treatment schedule must reflect that.”
Mannes says rooms that have been serviced for bed bugs should be rescheduled for follow-up inspection, reserviced as needed and kept offline until the bed bugs have been controlled successfully. Additionally, affected and adjacent rooms should be inspected for the next two to three months to make sure that no isolated pockets of the pests remain.
“Also inspect waiting rooms, laundry rooms, lounges, cafeterias, children’s play areas and other areas as appropriate,” Mannes adds.
When it comes to affected personal belongings, Mannes advises to wash all clothes and linens, including ones that haven’t been worn or used, in hot water. Then, they should be dried on high heat to ensure that all bed bugs and their eggs have been removed.
“To many people’s surprise, best management practices discourage the disposal of items infected with bed bugs, as this may result in the spread of bed bugs to new locations,” she says.
According to Kathryn Edgerton, partner at Nelson Hardiman and who has represented 70 facilities, addiction treatment centers are required to keep their properties clean, safe, sanitary and in good repair, free of flies and other types of insects. That said, anyone can request that a facility be inspected. If a complaint is filed, the department of healthcare services must initiate an investigation within a specified time.
“If the investigator finds a deficiency—one example would be a bed-bug infestation—the investigator will notify the facility of the deficiency, provide a date by which it needs to be corrected and any civil penalty assessed,” Edgerton says.
A bed-bug infestation would be considered a Class B deficiency, Edgerton says. This type of deficiency relates to the operation or maintenance of a facility that has a direct or immediate relationship to the safety, or the physical or mental health of residents. These types of deficiencies must be corrected within 30 days unless the investigator assigns a shorter time frame. If facilities take care of infestations according to investigators’ instructions, license revocation shouldn’t be a concern. Revocation of a license could come into play if a facility has multiple Class B deficiencies with failures to correct them.
It all started with one One Agency that knew there had to be a better way
One Agency that knew technology could be a resource, an ally, a simplifier.
One Agency Partnering with One visionary young company.
Both committed to increasing the Quality of Care and Life for all in Behavioral Health
Eighteen years later, One Partner Agency in One State is now over 350, in 35 states.
Credible thanks each and every one of our Partner Agencies for their service and commitment
C Credible drives each and every one of our Partner Agencies to further leverage technology
Credible encourages our Partners to join together to push the bounds of collaboration and cooperation to new levels.
Credible is proud to Partner with so many quality Agencies from coast to coast
The Power of One, delivering Benefits to Many.
In June of 2000, Credible Behavioral Health started for one reason:
U Use technology to improve the quality of care 18 years and 350 Agencies later, Credible is the first Enterprise SaaS company delivering fast, secure, clinical, billing, mobile, reporting, and data mining functionality. And Credible delivers software efficiently while implementing in as little as 4.5 months.
Credible delivers real, tangible benefits to our Partner Agencies:
l A proven, reliable, secure and easy to use web-based solution
l Monthly innovation, real state specific service, live phone help

l An independent, financially strong lasting company founder owned and founder run
l Mission based and built to stay that way

nimal-assisted therapy has grown in popularity over the past few decades, with both psychologist and physical therapists using a variety of critters— including dogs and dolphins—to help their patients. Horses are increasingly part of the mix, with hundreds of facilities offering equine therapy for a wide range of conditions.
While evidence is still largely anecdotal, equine programs are gaining popularity, particularly for treatment of post-traumatic stress disorder (PTSD) symptoms and autism. Like domestic dogs, horses are highly intuitive and have a unique historical relationship with humans that lends itself to a therapy setting.
“Their prey nature makes them highly attuned to their environment in order to ensure their safety, which is what makes them intuitive and emotionally sensitive to the slightest gesture, body posture or tension, tone of voice, or glance that we humans may unknowingly communicate,” says Liz Dampsey, PhD, clinical psychology post-doctoral fellow at Sierra Tucson. “They respond to our non-verbal behaviors and feelings through their body language.”
Many existing equine programs are based on the model established by the Equine Assisted Growth and Learning Association (Eagala), a ground-based model that now has 2,500 certified members in 40 countries. The model does not include riding, so horses do not have to perform in a certain way. They can behave more naturally.
Another organization, the Professional Association of Therapeutic Horsemanship International (PATH International), has created a program that does involve riding the horses for both
BY BRIAN ALBRIGHTphysical therapy as well as behavioral health applications. The organization has roughly 880 member centers, although many of those are focused on physical therapy.
Equine therapy programs are found at both large and small providers and can either be operated on-site or contracted out in the case of providers that don’t want to absorb the expense of boarding their own horses.
The Ranch treatment center has a large Eagala-based equine program that includes three barns, 25 horses, two equine psychotherapists and two equine specialists on staff.
There are group and individual sessions. According to psychotherapist Danielle Sukenik, group sessions start with some group work in a separate room in which participants are given a loosely structured exercise, such as building a jump in the arena for the horse. They then have to move the horse to the jump without touching the animal.
“We’re looking at how they problem solve and communicate,” Sukenik says. “Then we go back to the group room and process what happened.”
Sukenik says that equine therapy has been integrated with programming for Ranch clients across the board, including those being treated for addiction, trauma, sex addiction, eating disorders, depression/anxiety and other applications.
At Cumberland Heights, a not-for-profit, 12-Step-based treatment center, the equine program launched thanks to a donor.
“We had several staff members who had a passion for equine therapy. They began to use the new arena, and we built the program from there,” says Tammy Stone, associate clinical officer at Cumberland Heights.
The equine program is one of several expressive therapies (music, art, ropes courses, etc.) aimed at getting clients away from the typical circle of folding chairs.
“If patients are sitting around in a circle looing at each other, we only reach about 50% of them if we’re lucky,” Stone says. “If we get them outside and into an element they might be excited about, they get focused on that element and their defenses start to drop. They get more open to therapy, and we can reach them at a different level.”
The facility doesn’t keep its own horses; instead, they contract with an Eagala-trained and certified therapist. The only cost to Cumberland has been making sure they have the correct liability insurance in place and that staff remain certified and trained. However, later this year the facility plans to create a new adolescent program based on the PATH approach, and will begin keeping horses on the property.
The majority of equine-based psychotherapy programs were launched by providers who saw equine therapy in action. It’s unclear, though, how much of the benefit comes specifically from the horse versus other factors—being outside, being engaged in additional physical activity, or even the presence of the equine specialist in the therapy session.

One study, published in Psychiatric Services in Advance in 2015, did compare Eagala-based therapy with canine-assisted therapy, enhanced social skills psychotherapy, and regular hospital care among 90 patients at a state psychiatric hospital with recent in-hospital violent behavior or highly regressed behavior.
The animal-assisted approaches resulted in the largest decrease in violent behavior, with the Eagala approach being the more effective of the two.
However, a literature review ordered by the U.S. Department of Defense to investigate the use of equine therapy for veterans with PTSD symptoms found an “insufficient body of evidence to determine the effectiveness and safety of equine therapy.”
According to the providers interviewed for this article, patients do respond positively to this type of therapy, and the presence of a 1,000-pound animal in the session certainly leaves an impression. They believe equine encounters can help patients improve communication skills, overcome fears and anxieties and gain new insights into their own maladaptive behaviors.
Horses will react differently to people depending on whether they are relaxed, anxious or aggressive. A horse will walk away from a person who is exhibiting negative emotions, for example, which can be revealing in a therapy session.
“You can begin to regulate yourself to get the horse to cooperate,” Stone says. “The horse is mirroring back your nervousness or fear, and you can start to think about how your response to other people in similar situations in the past.”
For practices interested in tapping into this modality, there are a variety of requirements and costs involved. You don’t have to have your own horse and barn, but staffing, liability and insurance reimbursement issues are factors.
• Staffing and Facilities: In the Eagala model, the equine program must include both a licensed mental health

professional and an equine specialist for each session. You also need access to a corral or arena in which to conduct the session.
• Animals: The cost of stabling and caring for horses will vary, but some estimates put the cost to care for a single horse between $2,000 to $3,000 per year. Providers that don’t want to keep their own horses can also contract with an outside specialist, who absorbs the cost of caring for the horses and can provide access to suitable facilities for the sessions.
• Liability: Programs may also need to have equine liability insurance in addition to their standard liability coverage. At Sierra Tucson, for instance, the program is covered under general liability insurance.
• Insurance Reimbursement: Billing for treatment can be tricky and may require some extensive documentation depending on the insurance carrier. “There isn’t a code to bill insurance specifically for equine-assisted psychotherapy
similar to other types of therapy modalities and techniques —it is one of the processes used in a psychotherapy session,” says Lynn Thomas, CEO of Eagala. However, Stone says at Cumberland Heights, equine therapy is wrapped around services. “We just bill it as a regular therapy session,” she says.

• Marketing: These programs often market themselves— providers that offer equine services to specific clientele like veterans frequently wind up in the media. Some facilities also use their websites, blogs or other channels to promote equine therapies. Eagala also offers a Horses Help mobile app.
For providers that are unsure whether equine therapy would benefit their clients, experts say contracting with an outside equine specialist can provide an opportunity to see if this approach can be integrated with their practice.

State officials are seeing the effects addiction and overdose deaths have on other public systems— not the least of which is foster care. Increasingly, grandparents and other relatives are taking care of children who have lost their parents to overdose or have been removed from a home where opioids and other drugs are misused. Many kids are in foster homes. While the national system’s data collection process isn’t optimized to make a specific link between the opioid crisis and the number of children entering foster care as a result, there is clear evidence of a trend.
60 %
The percentage of child removals in Florida in 2017 attributed to substance use issues in the home—nearly double what it was four years prior. It is the No. 1 reason why children are removed in the state.
437,500
The number of children in the foster care system nationwide—for any reason—in fiscal year 2016, the most recent data available. More than 117,700 were waiting to be adopted.
15,100
The number of children who were removed from the home for circumstances involving parents’ alcohol use in fiscal year 2016. This represents a slight increase over the previous year’s nearly 15,000.
34 %
The percentage of children in the foster care system in fiscal year 2016, whose removal from the home was associated with circumstances involving parents’ drug abuse. The previous year’s percentage was 32%.
92,100
The number of children in the foster care system in fiscal year 2016, whose removal from the home was associated with circumstances involving parents’ drug abuse. Compare this to the previous year’s 85,900 children with the same reason for removal, and it’s a 7.2% increase.
Sources: Tampa Bay Times, January 8, 2018; U.S, Department of Health and Human Services’ Adoption and Foster Care Analysis and Reporting System, October 20, 2017; NBC News, August 28, 2017
Knowing that the millennial generation—those in the age range of 18 to 35—is now the largest generation in the United States, it’s smart for behavioral healthcare executives to tailor their marketing messages and consider the clinical care needs of millennials. The generation now numbers about 75 million to 80 million people, and it’s important to note that 98% of them own smartphones.
According to a Centers for Disease Control and Prevention Data Brief (No. 294), rates of drug overdose deaths in 2016 were highest among those in the 25 to 34 year-old age group, with 34.6 deaths per 100,000. Additionally, the year-to-year rise in overdose deaths was greatest in the 25 to 34 year-old age group at 29%, followed by 15 to 24 year-olds with a 28% rise in 2016. It’s clear that the millennial generation is being impacted by substance use disorders.
According to Nielsen, about 42% of millennials are multicultural—AfricanAmerican, Asian-American and Hispanic. They tend to consider connections to their multicultural heritage as mainstream.
In terms of education, more than 36% of millennials have obtained a bachelor’s degree or more, outranking their baby boomer and generation X counterparts. Interestingly, millennial women are more likely than millennial men to have such education, yet their median earnings are lower, according to the U.S. Census Bureau.
Millennials are the generation most likely to be living at home with their parents compared with previous generations of young adults, according to the Pew Research Center. Among those ages 25 to 35 years old, 15% are living in their parents’ home, compared to 10% of those in generation X who were a similar age and living at home in the year 2000. This generation moves less often and might be influenced by the job market and debt obligations.
The generation gap also demonstrates significant political divides. Millennials are the most likely group to identify as liberal Democrats or Democraticleaning at 27% of the population, compared to 21% of generation X and 17% of baby boomers. Additionally, the Pew Research Center reports that nearly one-third of baby boomers and 36% of the silent generation (age 71 to 88) described themselves as conservative Republicans or Republican-leaning in 2016, compared to 17% of millennials.
Sources: Nielson Insights, Nov. 15, 2016; Centers for Disease Control and Prevention Data Brief (No. 294), December 2017; Nielson Insights, Jan. 18, 2017; U.S. Census Bureau, “The State of Young Adults in the Labor Force”; Pew Research Center, May 5, 2017; Pew Research Center, March 20, 2017.
It’s a generation of digital tools and political divides
The National Rx Drug Abuse & Heroin Summit is where solutions are formulated, stakeholders convene, and change begins. Be part of the international discussion on addressing the opioid crisis by attending the 2018 Summit.


Who Attends:
• Clinicians, counselors, social workers, therapists, psychologists, interventionists
• Physicians, psychiatrists, nurses, pharmacists, dentists
• Advocates, families, and people in recovery
• Law enforcement personnel
• Public health and prevention officials
• Federal, state, and local officials and lawmakers
• Education specialists and researchers
• Treatment center owners and operators
• Lawyers
www.NationalRxDrugAbuseSummit.org
AMHSA offers an online treatment services locator to help consumers find behavioral health providers in their region. But this web tool also demonstrates the shortage of substance use treatment providers in many rural areas.
Meanwhile, between 1999 and 2015, opioid-related overdose death rates in rural areas quadrupled among those 18 to 25 years old and tripled for females, according to the Centers for Disease Control and Prevention.
“Looking at SAMHSA’s map of Michigan, pretty much anywhere above Grand Rapids, there is only a dot here or there. And there is a huge need for mental health services and substance use treatment,” says Scott Smith, MA, LPC, CAADC, a clinical supervisor at Pine Rest Christian Mental Health Services in Traverse City.
With a grant from SAMHSA, Pine Rest has launched a telehealth program to provide assessment and therapy to expand outpatient treatment for substance use disorders and co-occurring conditions to adults in underserved rural areas in northern Michigan.
Pine Rest offers counseling with a certified addiction counselor through an online video connection using a computer, tablet or smartphone to
BY DAVID RATHSindividuals living in eight counties.
“Instead of having to travel a long way in bad weather, this allows people to go online for treatment,” says Smith, who is supervising the grant for Pine Rest. Another benefit, he says, is that it provides an added element of confidentiality for professionals who work as physicians, first responders or police officers in small communities. When dealing with substance use issues, they might compromise their professional standing if they’re seen entering a treatment center.
SAMHSA continues to support programs that address the potential connection between telehealth and the opioid crisis in rural America. The federal Health Resources and Services Administration’s (HRSA) Office of Rural Health Policy has given grants to three organizations to establish a Substance Abuse Treatment Telehealth Network.
“Substance abuse treatment is an excellent use of telehealth,” says William England, director of HRSA’s Office for the Advancement of Telehealth.
Particularly relevant in addiction treatment is the convenience factor for patients who otherwise would travel long distances to see a provider. And telehealth can enable them to get the care that they might otherwise skip, he says, helping to reduce relapse rates.
In September 2017, Avera Health in Sioux Falls, S.D., was awarded a three-year grant of $746,000 as part of the HRSA program.
“There are a lot of different ways we measure shortages, but by most of those measures, South Dakota is one of the states most desperately in need of more services,” says Matthew Stanley, a psychiatrist at Avera Medical Group University Psychiatry Associates in Sioux Falls. “A large percentage of our counties are in shortage areas. We don’t have enough
psychiatrists for our population. A twoor three-hour drive is not unusual, and it can be a two-month wait to get an appointment.”
He says primary care doctors often feel overwhelmed by the number of health issues they are being asked to screen for, treat and monitor. With telehealth, family physicians can refer to a specialist quickly for supporting care services.
Avera’s telehealth has helped to create an easy handoff to a mental health professional in Sioux Falls from primary care providers in other areas of the state.
“The local practice or community might not be large enough to have those practitioners. [With telehealth,] we can
connect them to Sioux Falls, where we do have the resources,” he adds. “We are trying to extend SBIRT [Screening, Brief Intervention and Referral to Treatment] a little bit by having a licensed chemical dependency counselor available in our central hub.”
The providers who conduct telehealth sessions in the Avera network are duallicensed—mental health and chemical dependency—so they can go through an extensive intake interview and determine the best treatment plan for that patient.
“Beyond that, we have extended medication-assisted treatment,” Stanley says. “That is probably the harder but more necessary service with the opioid crisis. We
can connect a patient to medication-assisted treatment through telemedicine.”













Avera also is providing access to nalox-one prescriptions directly to consumers through its mobile app, AveraNow.






“Naloxone is a big lifesaver if you can get it to people experiencing acute overdose,” Stanley says. “We want people to have an opportunity to have naloxone—like having an EpiPen around if you have an allergy.”
By signing up on a smartphone, consumers can directly talk to a physician who will review the criteria, determine the need and issue a prescription to a local pharmacy if the consumer is determined to need naloxone. The cost is $49.
Large integrated health systems with rural service areas also are looking to add telehealth treatment of substance use disorders. David Hasleton, MD, is a practicing emergency physician and associate chief medical officer for Intermountain Healthcare in Salt Lake City. With its large, rural geography in two states, Intermountain is increasingly turning to telehealth for specialist care, and Hasleton says planning has begun on including substance use treatment in the array of telehealth services it offers.
“With medication-assisted treatment, which is one aspect of treating opioids, the hard part is that the practitioner has to be licensed in a particular way,” he says.
“We are working through a bunch of legal questions around that. There are some challenges, but it is doable.”

Ensuring proper licensing is essential for telemedicine of any kind. According to the Federation of State Medical Boards, physicians who treat or prescribe through online services sites are practicing medicine and must possess appropriate licensure in all jurisdictions where patients receive care. It’s the location of the patient that determines the licensing requirements.
Another challenge telehealth pioneers face is the uneven reimbursement landscape. For example, the Medicaid policies involving telehealth vary state
by state.
“Some insurers will cover mental health or psychiatry via telehealth but not substance use treatment,” says Pine Rest’s Smith. In Michigan, Blue Cross Blue Shield will cover substance use treatment via telehealth now, but Medicaid will not.
“Medicaid patients are probably the largest population in rural areas that deal with substance use issues,” he says. “That hurt us in the first year—not being able to take Medicaid clients.”
Also, rural areas are likely to experience a lack of broadband Internet access, which can make connecting telehealth sessions difficult. For the patient population most in need of services, internet access can be costly as well.
“There is not a lot of high-speed Internet in Northern Michigan,” Smith says. “Some clients have to sit in a certain part of their house just to get a signal. It is ironic because there are areas up there with multimillion-dollar homes, but they just switched from dial-up not too long ago.”
Conducting substance use treatment assessments and sessions via telehealth also requires some extra training for providers. Smith says it’s important to set up web cameras so the patient and the provider can see each other at eye level, for example. “Also, you have to make sure the client is in a place where they feel safe and secure—not in a dorm room with friends or in a public library.”

Before they have experience, providers tend to think that a telehealth consult is going to be awkward or that they are not going to be able to read the patient well.
“But once they have done some telemedicine, both patients and practitioners describe being pretty satis-fied with the experience,” says Avera’s Stanley. “Because we operate this out of a hub where there are a lot of other telemedicine practitioners, we do a fair amount of orientation and walkthrough and make sure we are using validated tools.”
HRSA’s England says its grant program has asked grantees to report on an array
of metrics regarding the efficacy of pilot programs, and it’s the first time the agency has made an award in telehealth for substance use disorder treatment.
“This is one of the priorities for the department, and we are excited to be able to showcase what telehealth can do.”
One of HRSA’s goals is for the programs to attain sustainability, which largely depends on the reimbursement environment at the state level. Many states have made progress with legislation, England says, but it’s ultimately the reimbursement that will drive the adoption.
Ideally, 2018 should be the year of investment, according to Linda Rosenberg, president and CEO of the National Council for Behavioral Health. While the industry has long bemoaned the lack of public resources dedicated to treating addiction and mental health disorders, new pressures are emerging that sound a more urgent alarm for lasting solutions. Always the optimist, Rosenberg believes there are successes to celebrate, too.

She recently spoke to Behavioral Healthcare Executive, and here are a few items on Linda’s List for 2018.
Communities are struggling as they try to connect people in need with appropriate addiction and mental health resources. Even those who have insurance or the means to pay out of pocket still have ongoing access problems. Care is rarely immediate, and there are numerous barriers along the continuum.
This is the year of the community crisis, Rosenberg says.
“We’ve tried a number of things to solve the opioid crisis and serious mental illness, and one of the things we’ve learned so far is that beds alone are not the answer,” she says. “Expanding federally qualified health centers (FQHCs) alone is not the answer, and integration alone is not the answer.”
how we need to stop blaming community-based organizations for certain problems when we’ve not made any investment in them,” she says.
Additionally, Rosenberg says it’s irrational to expect not-forprofits to innovate and offer new services to respond to local needs when there’s no funding to back it up. By comparison, she says, it took Amazon about six years to make a profit even with substantial private investment. More cannot be expected of community organizations or their donors.
Rosenberg says the workforce shortage is a crisis that’s been brewing for years. Now with unemployment in check nationwide, attracting quality employees—particularly clinical employees—represents a competitive advantage.
“You’ve got millennials who have a huge number of career choices, who can work for companies that are getting big tax cuts and are announcing perks and pay raises, and then you’ve got a nonprofit sector of community organizations that have not benefitted at all from the tax breaks,” she says.
Linda RosenbergAt the ground level, the lack of investment is only made worse by historical shortfalls and increasing pressure on rates as the healthcare system at large shifts toward value models. She says the result is more providers closing down and fewer clinical workers entering the field.
“That’s what we need to tackle—honest conversations about
Even the Veterans Administration and FQHCs are able to pay employees more, and considering that workers need to earn a living and take care of their families, the choice becomes obvious for them. Offering training as the special employee perk just doesn’t cut it anymore.
“In the end, you have to pay people, and you have to treat millennials to snacks in the office, sabbaticals, weekly dinners, parties and other events,” she says. “That’s what for-profit companies do for millennials, meanwhile, nonprofits can barely afford to hire staff. We get what we pay for.”
As for solutions, Rosenberg believes career ladders for peer
Negley prides itself on developing customized coverage solutions, not simply providing off-the-shelf policies. We’ll work with your broker to understand the intricacies of your organization so we can tailor each coverage to meet your business risk exposure. And we’re always ready to offer the insights we’ve gained over the past 50 years –everything from the pitfalls of high coverage limits and additional insured endorsements, to why coverage for physicians should never be scheduled.
 Nicholas Bozzo, President, Negley Associates
Nicholas Bozzo, President, Negley Associates


coaches would be helpful because they’re a valuable and recognized resource that should be scaled up. However, the caution here is that commercial payers have embraced peer services largely because of the cost savings.
“They are an important part of the workforce, but payers like it because it’s cheap,” she says.
Rosenberg again calls for expansion of Certified Community Behavioral Health Clinics (CCBHCs). Still limited to eight states, the programs aim to create a payment model that ensures fair reimbursement for the actual cost of services. A number of federal policy proposals have attempted to expand the program incrementally, but none have been adopted yet.
“It was all about giving community mental health and addiction treatment the same investment that FQHCs have gotten for the last 20 years,” she says. “It’s a chance to get paid and have rates that are high enough to hire people and have things like tuition
reimbursement and to pay adequately and to pay for experts and supervision. None of that is allowable with the kind of rates community-based organizations are getting right now.”
Among the active CCBHCs today, workforce expansions have occurred in all the demonstration areas, with a total of 1,160 new staff hired—including psychiatrists and staff with addiction specializations. Additionally, 87% of the clinics report they have been able to serve more patients thanks to their new capabilities. These are the bright spots. And Rosenberg says progress must continue on the practice side and the policy side because both are needed.





The opioid crisis remains a designated public health emergency at the federal level with the original declaration now extended until late April. However, Rosenberg cautions that there are so many drivers of addiction today that a short-term focus won’t be enough to realistically combat the true scope of the problem.
For example, she says, adding residential treatment beds makes business sense for private equity investors in the market, and programs to reduce overprescribing of opioids certainly help to reduce the number of pills found in medicine cabinets. But those actions are perhaps low-hanging fruit.
“It is not necessarily true that all addictions are coming from overprescribing,” she says. “Most people who take opioids, need opioids and never get addicted.”
Rosenberg recommends strategies that support recovery, whether it’s housing, career training or ongoing care coordination for co-occurring disorders. Additionally, she wants to see a national strategy that creates the infrastructure to deliver such solutions with ongoing investment.

The Institute is a trusted educational resource that helps address daily challenges. Our conferences convene thought leaders that share clinical best practices, discuss how to effectively and ef ciently operate a behavioral healthcare organization, and strategize solutions for addressing the opioid epidemic. Join us at an upcoming event to network with peers and take home valuable tools. Learn more about us and how we can help you at www. iadvancebehavioralhealthcare.com.

APRIL 2-5, 2018 | ATLANTA, GA
Be part of the discussion at the largest national gathering of stakeholders working together to address the opioid crisis. Prevention, treatment, law enforcement, public health, and many others exchange best practices and hear from state and federal of cials at the annual Rx Summit.
www.nationalrxdrugabusesummit.org
AUGUST 19-22, 2018 | DISNEYLAND, CA
Addiction professionals annually convene at NCAD to share what’s working: Clinicians hear from thought leaders on delivering treatment, while executives of behavioral healthcare organizations learn how to run more effective, more ef cient, and ethically minded businesses. www.ncadcon.com
NOVEMBER 12-14, 2018 | FORT LAUDERDALE, FL
The opioid crisis is making headlines, but another category of drugs continues to devastate communities: stimulants. Join other stakeholders to explore how to address and treat stimulant use.
www.stimulantsummit.com

DECEMBER 10-12, 2018 | SCOTTSDALE, AZ
Senior executives of treatment centers, and those investing in these enterprises, discuss growth strategies and market dynamics at this exclusive, three-day educational and networking event.
www.treatmentcenterretreat.com
APRIL 30-MAY 2, 2018 | HILTON HEAD, SC
TCEM provides CEOs, CFOs, COOs, directors, senior marketing/business development/ admissions leaders, and other executives with the tools they need to effectively and ethically grow their services in a rapidly changing market.
www.executiveandmarketingretreat.com
Interested in attending an event? Contact Ellen Kelley at ekelley@iabhc.com or 216-373-1223.
Photography: Pete Winkel GPA President Obama addressed Institute attendees in 2016. Matt Bevin, Governor of Kentucky, addressed Institute attendees in 2017.CE Credits
The Summits for Clinical Excellence bring together thought leaders on cutting-edge topics in multi-day national and regional conferences. Summits on mindfulness, trauma, process addiction, and shame appeal particularly to private practice behavioral healthcare professionals. Other Summits address the national opioid crisis from a regional perspective and engage a diverse group of stakeholders. Many Summits offer treatment ethics continuing education credits.
• PHOENIX, AZ February 14-16, 2018
The Opioid Crisis: The Clinician’s Role and Treatment Practices - Featuring the 2nd Annual Arizona Opioid Summit
www.arizonaopioidsummit.com

• ORANGE COUNTY, CA March 1-2, 2018
East Meets West: Multiple Perspectives on Trauma and Addictions
www.iabhc.com/orangecounty2018
• CHICAGO, IL March 7-8, 2018
The Opioid Crisis: Strategies for Treatment and Recovery
www.chicagoopioidsummit.com
• CHICAGO, IL March 7-10, 2018
The National Conference on Trauma, Addictions, and Mindfulness: Where Freud Meets Buddha www.iabhc.com/chicago2018
• PITTSBURGH, PA June 25-26, 2018
The Opioid Crisis: The Clinician’s Role and Treatment Practices
www.pittsburghopioidsummit.com
• ATLANTA, GA October 18-21, 2018
Brain Matters: Shame, Trauma, and Process Addictions
www.iabhc.com/atlanta2018
• NEW ENGLAND November 8-9, 2018
The Opioid Crisis: Strategies for Treatment and Recovery
www.newenglandopioidsummit.com
CE Credits
WEBINARS
The National Conference on Addiction Disorders convenes panel discussions across the country in a lunch’n’learn format. Clinicians hear about treatment practices, while those on the business side of the field share strategies for managing and marketing behavioral healthcare organizations. www.iabhc.com/local
Upcoming events: Baltimore
Boca
Long
Salt
San
Washington,
Hear from experts on clinical, managerial, and other topics in our frequent, free-to-attend Webinars. www.iabhc.com/webinars
CE Credits
Contact Ellen Kelley at ekelley@iabhc.com or 216-373-1223.
ddiction treatment with a river view is not the only feature of Riverside Recovery’s new Tampa, Fla., facility. Many facets of the facility’s design are in sync with the recovery process, while also making the most of a setting on the banks of the Hillsborough River.
“Everything about the design was intentional and focused on promoting a sense of peace and calmness for our clients and creating a safe and efficient environment,” says Ashley Janes, the facility’s director of business development.

“We are located on the river, so the interior follows the theme and design.”
The facility currently operates with 66 beds, including 15 beds for detox. Once all of the renovations to the 60,000 square-foot building are completed, the facility will nearly double its capacity to 120 beds. Its services include a 30-day residential program, detoxification, and intensive outpatient services for patients age 18 or older with substance misuse and co-occurring mental health issues. The length of stay varies according to patient needs, with an average stay of three to 10 days for detox, 30 to 90 days for residential care, and four to eight weeks for outpatient care.
The design and layout of the facility plays a role in the recovery experience as soon as patients walk in. The facility, which opened its doors to new patients last summer, is designed to make the
intake process as smooth and inviting as possible.
For example, the lobby reception area is sunny and open with high ceilings, a wall of windows and art on the walls. The tile flooring used in this area continues throughout the facility to ensure continuity. The tile itself resembles natural plank wood flooring but is more durable and easier to sanitize than real wood. The can lighting used in the lobby is also consistent throughout the facility and provides a softer ambiance and avoids an institutional feel that harsher fluorescent lighting can create.
“We didn't want the space to feel sterile or hospital-like,” says Janes. “We wanted the environment to feel safe, comfortable, welcoming, peaceful and supportive of the therapeutic process.”



To accomplish that, facility management chose a clean and crisp look for the interior spaces using natural materials, such as wood and leather. The artwork can also be described as

both abstract and natural with pictures of trees, river rocks, geodes and water elements. The color scheme of blue and gray hues are designed to promote peace and balance. Group meeting rooms and patient rooms have colorful fabrics to bring more warmth to those areas.
Once patients enter the lobby, they can immediately be escorted to the adjacent intake room. From there, patients move into their rooms—the men in Strength Hall and the women in Hope Hall. Patients who need increased medical
observation reside in Experience Hall, which is located close to the nurses’ station.

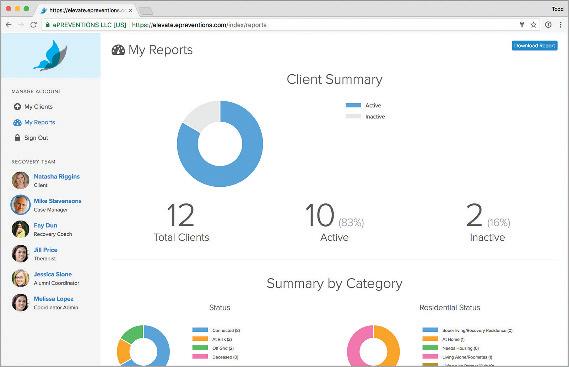

The detox area is as secluded as possible in the very back corner of the building. This ensures that patients and staff will have a quiet environment and necessary privacy away from the bustle of administrative activities and common areas. At the same time, the offices of the physician, nurse practitioner and director of nursing are all close by to ensure easier observation and to ensure patient safety. This part of the facility is appropriately named Beginnings Hall. During day-to-day activities, patients and staff can use several common areas set in different parts of the facility.

Given the importance of physical and social activities to recovery, Riverside offers indoor facilities, including a gym with a half basketball court and workout equipment, while also leveraging its riverside location to incorporate the outdoors. Patients have access to a new outdoor swimming pool, sand volleyball court, meditation garden, and fire pit and barbecue area.


The staff can now also incorporate the riverside setting into outdoor activities as much as possible. A new riverside dock allows patients to enjoy fishing and kayaking. All recreation activities are overseen by a certified recreation therapist.



















The Joint Commission has awarded Clearview Horizon in Heron, Mont., its Gold Seal of Approval for behavioral healthcare accreditation.
Beacon Health Options announced it has received full accreditation as a Managed Behavioral Health Organization (MBHO) from the National Committee for Quality Assurance (NCQA). Beacon has been an accredited NCQA MBHO since 2000.
Redonna Chandler, PhD, has been named director of the AIDS research program at the National Institute on Drug Abuse.
Sarah A. Wattenberg, MSW, has joined the National Association of Psychiatric Health Systems (NAPHS) as director of quality and addiction services.
Andrey Ostrovsky, MD, has been named president and CEO of Concerted Care Group in Baltimore. Ostrovsky is the recent chief medical officer for the Center for Medicaid and CHIP Services.
Caron Treatment Centers announced the following appointments: Sara Counes, CAP, ICADC, to vice president of admissions and business development; Kelli Grant, MS, CRC, as corporate director of business development and case management; and William P. Parfitt, CPA, as chief financial officer.
a Professionals Treatment Program at its Center for Professional Recovery in Santa Monica, Calif.
Advanced Recovery Systems (ARS) and the Miss Florida Scholarship Pageant have announced a collaboration to educate high school and college students about the dangers of drug and alcohol abuse. As the spokesperson for the partnership, Miss Florida 2017 Sara Zeng will be visiting schools across the state for a “Real Talk” with students.
Centerstone has named Shawny Robey as the company’s chief operating officer.
Michael Nanko, PhD, has been named American Addiction Centers president and chief operating officer.
Beacon Health Options has appointed Russell C. Petrella, PhD, as president and chief executive officer.
Sheppard Pratt Health System has named Donna Richardson, MBA, vice president and chief development officer.
Centerstone has promoted Brad Bills to vice president of systems development, Melissa Collette to vice president of enterprise services and Chuck Pegg to director of information technology infrastructure. Laura Clanton has joined the organization director of advancement at Centerstone Tennessee.
Addiction Campuses has hired Brett Martin as its public relations manager.
The National Association of Drug Court Professionals (NADCP) has named Melissa Fitzgerald as director of Advancing Justice, a new initiative to lead justice reform.
Lindner Center of HOPE, a not-for-profit mental health center based in Cincinnati, has received two grants totaling $75 million for its behavioral health programs. Cincinnati business leaders and philanthropists Linda and Harry Fath have pledged a $50 million, and Frances and Craig Lindner have pledged $25 million.
Regional Mental Health Center has opened Regional Health Clinic, a federally qualified health center, in Merrillville, Ind.
New Vista Behavioral Health announced the opening of The Point, a detoxification and residential substance abuse treatment facility in Huntington Beach, Calif. The organization has also announced the opening of
Spectrum Health Systems has opened new outpatient treatment centers in Millbury and Weymouth, Mass., and the company’s existing Pittsfield, Mass., program moved to a larger facility to adequately serve the local population.
Caron Treatment Centers has opened the Carole and Ray Neag Medical Center at its Berks County headquarters. The facility features an expanded detoxification center, rooms for medically compromised patients, and a new location for Caron's Older Adult Program.
Safe Landing has opened a private addiction treatment facility for adolescents in North Miami, Fla.
Morningside Recovery has opened Hand in Hand Recovery, an addiction and mental health inpatient center for couples seeking recovery, in Orange County, Calif.
Haven Behavioral Healthcare has announced an agreement to open a new, 72-bed psychiatric hospital in Meridian, Idaho. The hospital, which is expected to begin treating patients in early 2019, will provide inpatient psychiatric treatment to adults experiencing depression, anxiety,
psychosis or other severe behavioral problems.
Gateway Rehab in Pennsylvania announced it will expand its Westmoreland County residential addiction treatment facility, and relocate its South Hills outpatient office from Pleasant Hills to Whitehall.
Longbranch Healthcare has opened Longbranch Wellness Center, an outpatient medication-assisted treatment center in Old Metairie, La.
Seaside Healthcare has acquired Turning Point Family Services, adding another four locations to its operations in North Carolina.
Pharos Capital Group, LLC announced its acquisition of Behavior Care Specialists, an autism treatment service provider based in Sioux Falls, S.D.

Recovery Centers of America (RCA) announced it is launching gender-specific substance use disorder treatment programs for
young adults at two of its inpatient facilities, with similar programming to roll out at the rest of the provider’s locations throughout the year.
The CLARE Foundation and the Matrix Institute on Addictions have voted to merge into a new notfor-profit entity. Services include detox, residential and outpatient care, medication assisted treatment and sober living, with locations in Los Angeles and San Bernardino counties in California.
New Directions Behavioral Health announced it has acquired E4 Health, an integrated healthcare management company based in Irving, Texas.
BayMark Health Services has acquired 15 opioid treatment facilities from Health Care Resource Centers, Inc. (HCRC), located in three New England states. The transaction also includes a management deal
Universal Health Services (UHS) is acquiring three not-for-profit facilities in Mississippi, including a 109-bed inpatient center previously owned jointly by the City of Gulfport and Harrison County under the Memorial Hospital umbrella.
Centerstone Kentucky has announced plans to merge with Uspiritus, which offers two residential centers as well as community-based services
Meridian Behavioral Health has acquired New Beginnings Minnesota. The provider now operates more than 30 facilities across five states.
Odyssey Behavioral Healthcare has acquired Selah House, an eating disorder treatment center for women in Anderson, Ind.
Summit BHC announced an agreement with private
to acquire a controlling interest in the company from Flexpoint Ford and other investors.

Delphi Behavioral Health Group has completed a recapitalization with private investment firm the Halifax Group.
Strive Health of Greensburg (Pa.) announced that it will offer outpatient and intensive outpatient treatment programming for substance use


