Fourth branchial pouch sinus: A report of 7 cases and review of the literature
Age-related changes affecting the cricoarytenoid joint seen on computed tomography
Improved swallow outcomes after injection laryngoplasty in unilateral vocal fold immobility
Treatment outcomes in HPV-negative oropharyngeal cancer: Surgery plus radiotherapy vs. definitive chemoradiotherapy
www.entjournal.com A Vendome Publication AUGUST 2018 • VOL. 97, NO. 8





The new two-piece magnetically coupled solution for non-surgical closure Round Oval www.inhealth.com We speak ENT ©2017 InHealth Technologies Manufactured by Freudenberg Medical, LLC (161010.06) The voice of experience since 1978 Magnetic4
Nasal Septal Perforation Prosthesis
Closure
3
The #1 Most Profitable Ancillary Service for Private Practice ENTs
Y our peers wanted to share an update since adding a FYZICAL Balance Center to their ENT practice:

“This is the single best thing we’ve ever done in our practice. We can’t comprehend why an otolaryngologist would not do this. It’s a no-brainer and it’s taking our profession by storm."

vehicle."
ü We're seeing 40 - 4 5 patients per day for balanc e therapy only.
ü Our hearing aid sales have increased 59%.
ü Our total patient visits are up 15% for new patients and 5% for return patients.
ü Our allergy / immunotherapy population has grown 20% since joining.
"We couldn’t be more excited about our future. Get in touch with FYZICAL. You absolutely, positively, 100% need to see for your own eyes what this can do for your practice before it’s
Tuscaloosa ENT Group
"We can't stress enough how amazing of an opportunity this really is. You will grow every part of your practice through this
too late.”
Explore FYZICAL Balance at OTO Game Changer Discover the systems and procedures behind this opportunity. Call 941-227-4314
event.
seating
open to those with open
Discover more at www.BusinessofBalance.com
to register now or learn more about this
*Limited
and only
territories*
EDITORIAL BOARD
EDITORIAL BOARD MEMBERS
Editor-in-Chief
Robert T. Sataloff, MD, DMA, FACS
Professor and Chairman, Department of Otolaryngology–Head and Neck Surgery, and Senior Associate Dean for Clinical Academic Specialties, Drexel University College of Medicine Philadelphia, PA
Jean Abitbol, MD
Jason L. Acevedo, MD, MAJ, MC, USA
Jack B. Anon, MD
Gregorio Babighian, MD
Peter C. Belafsky, MD, PhD
Bruce Benjamin, MD
Gerald S. Berke, MD
Michael J. Brenner, MD
Kenneth H. Brookler, MD
Karen H. Calhoun, MD
Steven B. Cannady, MD
Ricardo Carrau, MD
Swapna Chandran, MD
Chien Chen, MD
Dewey A. Christmas, MD
Nicolle T. Clements, MS
Daniel H. Coelho, MD, FACS
David M. Cognetti, MD
James V. Crawford, MD
David H. Darrow, MD, DDS
Rima Abraham DeFatta, MD
Robert J. DeFatta, MD, PhD
Hamilton Dixon, MD
Paul J. Donald, MD, FRCS
Mainak Dutta, MS, FACS
Russell A. Faust, PhD, MD
Ramón E. Figueroa, MD, FACR
Charles N. Ford, MD
Paul Frake, MD
Marvin P. Fried, MD
Richard R. Gacek, MD
Andrea Gallo, MD
Frank Gannon, MD
Emilio Garcia-Ibanez, MD
Soha Ghossani, MD
William P. R. Gibson, MD
David Goldenberg, MD
Jerome C. Goldstein, MD
Richard L. Goode, MD
Samuel Gubbels, MD
Reena Gupta, MD
Joseph Haddad Jr., MD
Missak Haigentz, MD
Christopher J. Hartnick, MD
Mary Hawkshaw, RN, BSN, CORLN
Garett D. Herzon, MD
Thomas Higgins, MD, MSPH
Jun Steve Hou, MD
John W. House, MD
Glenn Isaacson, MD
Steven F. Isenberg, MD
Stephanie A. Joe, MD
Shruti S. Joglekar, MBBS
Raleigh O. Jones, Jr., MD
Petros D. Karkos, MD, AFRCS, PhD, MPhil
David Kennedy, MD
Seungwon Kim, MD
Robert Koenigsberg, DO
Karen M. Kost, MD, FRCSC
Jamie A. Koufman, MD
Stilianos E. Kountakis, MD, PhD
John Krouse, MD
Ronald B. Kuppersmith, MD, MBA, FACS
Rande H. Lazar, MD
Robert S. Lebovics, MD, FACS
Keat-Jin Lee, MD
Donald A. Leopold, MD
Steve K. Lewis, BSc, MBBS, MRCS
Daqing Li, MD
Robert R. Lorenz, MD
John M. Luckhurst, MS, CCC-A
Valerie Lund, FRCS
Karen Lyons, MD
A.A.S. Rifat Mannan, MD
Richard Mattes, PhD
Brian McGovern, ScD
William A. McIntosh, MD
Brian J. McKinnon, MD
Oleg A. Melnikov, MD
Albert L. Merati, MD, FACS
Joseph P. Mirante, MD, MBA, FACS
Ron B. Mitchell, MD
Steven Ross Mobley, MD
Jaime Eaglin Moore, MD
Thomas Murry, PhD
Ashli K. O’Rourke, MD
Ryan F. Osborne, MD, FACS
J. David Osguthorpe, MD
Robert H. Ossoff, DMD, MD
Enrique Palacios, MD, FACR
Michael M. Paparella, MD
Kourosh Parham, MD, PhD
Arthur S. Patchefsky, MD
Meghan Pavlick, AuD
Spencer C. Payne, MD
Kevin D. Pereira, MD, MS (ORL)
Nicolay Popnikolov, MD, PhD
Didier Portmann, MD
Gregory N. Postma, MD
Matthew J. Provenzano, MD
Hassan H. Ramadan, MD, FACS
Richard T. Ramsden, FRCS
Gabor Repassy, MD, PhD
Dale H. Rice, MD
Ernesto Ried, MD
Alessandra Rinaldo, MD, FRSM
Joshua D. Rosenberg, MD
Allan Maier Rubin, MD, PhD, FACS
John S. Rubin, MD, FACS, FRCS
Amy L. Rutt, DO
Anthony Sclafani, MD, FACS
Raja R. Seethala, MD
Jamie Segel, MD
Moncef Sellami, MD
Michael Setzen, MD, FACS, FAAP
Stanley Shapshay, MD
Douglas M. Sidle, MD
Herbert Silverstein, MD
Jeffrey P. Simons, MD
Raj Sindwani, MD, FACS, FRCS
Aristides Sismanis, MD, FACS
William H. Slattery III, MD
Libby Smith, DO
Jessica Somerville, MD
Thomas C. Spalla, MD
Matthew Spector, MD
Paul M. Spring, MD
Brendan C. Stack, Jr., MD, FACS
James A. Stankiewicz, MD
Jun-Ichi Suzuki, MD
David Thompson, MD
Lester D.R. Thompson, MD, FASCP
Helga Toriello, PhD, FACMG
Ozlem E. Tulunay-Ugur, MD
Galdino Valvassori, MD
Emre Vural, MD
Donald T. Weed, MD, FACS
Neil Weir, FRCS
Kenneth R. Whittemore, MD
David F. Wilson, MD
Ian M. Windmill, PhD
Ian J. Witterick, MD,MSc, FRCSC
Richard J. Wong, MD
Naoaki Yanagihara, MD
Eiji Yanagisawa, MD, FACS
Ken Yanagisawa, MD, FACS
Anthony Yonkers, MD
Mark Zacharek, MD
Joseph Zenga, MD
Liang Zhou, MD
CLINIC EDITORS
Dysphagia
Peter C. Belafsky, MD, PhD
Gregory N. Postma, MD
Facial Plastic Surgery
Anthony P. Sclafani, MD, FACS
Geriatric Otolaryngology
Kourosh Parham, MD, PhD, FACS
Karen M. Kost, MD, FRCSC
Head and Neck
Ryan F. Osborne, MD, FACS
Paul J. Donald, MD, FRCS
Reena Gupta, MD
Imaging
Enrique Palacios, MD, FACR
Ramón E. Figueroa, MD, FACR
Laryngoscopic
Robert T. Sataloff, MD, DMA, FACS
Otoscopic
John W. House, MD
Brian J. McKinnon, MD
Pathology
Lester D.R. Thompson, MD, FASCP
Pediatric Otolaryngology
Rande H. Lazar, MD
Rhinoscopic
Eiji Yanagisawa, MD, FACS
Dewey A. Christmas, MD
Joseph P. Mirante, MD, MBA, FACS
Ken Yanagisawa, MD, FACS
Special Topics
Robert T. Sataloff, MD, DMA, FACS
Thyroid and Parathyroid
David Goldenberg, MD
218 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018
Balloon dilation for Eustachian tube dysfunction
The superior, durable results your patients deserve. With
the safety you can count on.
A randomized, controlled trial comparing balloon dilation with ongoing medical therapy as treatment for persistent Eustachian tube dysfunction reported zero complications and significant symptom improvement through 12 months for patients treated with the XprESS™ ENT Dilation System.1
1 Meyer TA, O’Malley E, Schlosser RJ, et al. A randomized controlled trial of balloon dilation as a treatment for persistent Eustachian tube dysfunction with 1-year follow-up. Otol Neurotol. 2018. DOI: 10.1097/
MAO.0000000000001853
INDICATIONS FOR USE: To access and treat the maxillary ostia/ethmoid infundibula in patients 2 years and older, and frontal ostia/recesses and sphenoid sinus ostia in patients 12 years and older using a transnasal approach. The bony sinus outflow tracts are remodeled by balloon displacement of adjacent bone and paranasal sinus structures. To dilate the cartilaginous portion of the Eustachian tube for treating persistent Eustachian tube dysfunction in patients 18 years and older using a transnasal approach.
Please see Instructions for Use (IFU) for a complete listing of warnings, precautions, and adverse events as well as cleaning, sterilizing and care for surgical instruments.

CAUTION: Federal (USA) law restricts these devices to sale by or on the order of a physician.
ENTELLUS MEDICAL and XPRESS are trademarks of Entellus Medical, Inc.
DURABLE symptom improvement through 12 months
NEW CLINICAL DATA Read more at: go.ent.stryker.com/ETDRCT1YearData
©2018 Entellus Medical, Inc. 1738-762 rA 07/2018
Balloon Dilation (N=28) Control (N=27) Baseline (N=54) 6 Weeks (N=51) 3 Months (N=52) 6 Months (N=51) 12 Months (N=49) 1 2 3 4 5 6 7 0 1 2 3 4 5 6 7 4.6 2.1 2.12.1 2.1 MILD (NO PROBLEM) MODERAT E SEVERE M EAN OVERALL ETDQ-7 SCORE MEAN OVERALL ETDQ-7 SCORE ∆= -2.9±1.4 ∆= -0.6±1.0 p<0.0001 p<0.0001 for change from baseline to all follow-up periods BaselineFollow-up Baseline Follow-up ET balloon dilation
Balloon Dilation (N=28) Control (N=27) Baseline (N=54) 6 Weeks (N=51) 3 Months (N=52) 6 Months (N=51) 12 Months (N=49) 1 2 3 4 5 6 7 0 1 2 3 4 5 6 7 4.6 2.1 2.12.1 2.1 MILD (NO PROBLEM) MODERAT E SEVERE M EAN OVERALL ETDQ-7 SCORE MEAN OVERALL ETDQ-7 SCORE ∆= -2.9±1.4 ∆= -0.6±1.0 p<0.0001 p<0.0001
from baseline
follow-up periods BaselineFollow-up Baseline Follow-up ET balloon dilation with XprESS is SAFE
% COMPLICATION RATE
SUPERIOR to medical management
for change
to all
0
Editor-in-Chief Robert T. Sataloff, MD, DMA, FACS 219 N. Broad St., 10th Fl., Philadelphia, PA 19107 entjournal@phillyent.com Ph: 215-732-6100

Managing Editor Linda Zinn
Manuscript Editors Martin Stevenson and Wayne Kuznar
Associate Editor, Reader Engagement Megan Combs
Creative Director Eric Collander
National Sales Manager Mark C. Horn mhorn@vendomegrp.com Ph: 480-895-3663
Traffic Manager Eric Collander
Please send IOs to adtraffic@vendomegrp.com
All ad materials should be sent electronically to: https://vendome.sendmyad.com
Customer Service/Subscriptions
www.entjournal.com/subscribe Ph: 888-244-5310 email: VendomeHM@emailpsa.com
Reuse Permissions Copyright Clearance Center info@copyright.com Ph: 978-750-8400 Fax: 978-646-8600
Chief Executive Officer Jane Butler
Chief Marketing Officer Dan Melore
Vice President, Finance Bill Newberry
Vice President, Custom Media Jennifer Turney Director, Circulation Rachel Beneventi
ENT-Ear, Nose & Throat Journal (ISSN: Print 0145-5613, Online 1942-7522) is published 9 times per year in Jan/Feb, Mar, Apr/May, June, July, Aug, Sept, Oct/ Nov and Dec, by Vendome Group, LLC, 237 West 35th Street, 16th Floor, New York, NY 10001-1905.

©2018 by Vendome Group, LLC. All rights reserved. No part of ENT-Ear, Nose & Throat Journal may be reproduced, distributed, transmitted, displayed, published, or broadcast in any form or in any media without prior written permission of the publisher. To request permission to reuse this content in any form, including distribution in education, professional, or promotional contexts or to reproduce material in new works, please contact the Copyright Clearance Center at info@ copyright.com or 978.750.8400.
EDITORIAL: The opinions expressed in the editorial and advertising material in this issue of ENT-Ear, Nose & Throat Journal are those of the authors and advertisers and do not necessarily reflect the opinions or recommendations of the publisher, editors, or the staff of Vendome Group, LLC. ENT-Ear, Nose & Throat Journal is indexed in MEDLINE/PubMed and Current Contents/Clinical Medicine and Science Citation Index Expanded. Editorial offices are located at 812 Huron Rd., Suite 450, Cleveland, OH 44115. Manuscripts should be submitted online at www.editorialmanager.com/entjournal. Instructions for Authors are available at www.entjournal.com.
SUBSCRIPTIONS: For questions about a subscription or to subscribe, please contact us by phone: 888-244-5310; or email: VendomeHM@emailpsa.com. Individual subscriptions, U.S. and possessions: 1 year $225, 2 years $394; International: 1 year $279, 2 years $488; Single copies $28; outside the U.S., $40.
POSTMASTER: send address changes to Ear, Nose & Throat Journal, PO Box 11404 Newark, NJ 07101-4014.
220 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018
ADVERTISER INDEX Pages Acclarent 223 Arbor .............................................. 246, 247 CANT Corporation ................................. 225 Compulink CVR3 Entellus .................................................. 219 Fyzical 217 InHealth Technologies ........................ CVR2 Lumenis ................................................. 221 McKeon Products CVR4, 241 Medtronic .............................................. 235 OmniGuide 253 Optim LLC ............................................. 229 Reliance Medical ................................... 231 RhinoWorld 237 SinOptim LLC ........................................ 243

ORIGINAL ARTICLES
236 Fourth branchial pouch sinus: A report of 7 cases and review of the literature
Indranil Pal, MS; Saumitra Kumar, MS; Ankur Mukherjee, MS, DNB; Bibhas Mondal, MS; Anindita Sinha Babu, MD
244 Age-related changes affecting the cricoarytenoid joint seen on computed tomography
Georges Ziade, MD; Sahar Semaan, MD; Sarah Assaad, MPH; Abdul Latif Hamdan, MD, EMBA, MPH
250 Improved swallow outcomes after injection laryngoplasty in unilateral vocal fold immobility
Steven Zuniga, MD; Barbara Ebersole, MA, CCC-SLP; Nausheen Jamal, MD
ONLINE EXCLUSIVES
E1 Treatment outcomes in HPV-negative oropharyngeal cancer: Surgery plus radiotherapy vs. definitive chemoradiotherapy
Dominique Rash, MD; Megan E. Daly, MD; Blythe Durbin-Johnson, PhD; Andrew T. Vaughan, PhD; Allen M. Chen, MD
E8 Protective effect of pentoxifylline on amikacin-induced ototoxicity
Mohammad Waheed El-Anwar, MD; Said Abdelmonem, MD; Ebtessam Nada, MD; Dalia Galhoom, MD; Ahmed A. Abdelsameea, MD
E13 Chronic otitis media with effusion in chronic sinusitis with polyps
Mary Daval, MD; Hervé Picard, MD, MSc; Emilie Bequignon, MD; Philippe Bedbeder, MD; André Coste, MD, PhD; Denis Ayache, MD, PhD; Virginie Escabasse, MD, PhD
E19 Ancillary medications and outcomes in post-tonsillectomy patients
Ashley P. O’Connell Ferster, MD; Eric Schaefer, MS; Jane R. Schubart, MBA, PhD; Michele M. Carr, DDS, MD, PhD
E25 Safety and utility of direct laryngoscopy and bronchoscopy in patients hospitalized with croup
Daniel P. Fox, MD; Julina Ongkasuwan, MD
E31 Inflammatory myofibroblastic tumor of the epiglottis excised with a carbon dioxide laser: Case report and literature review
Blake Raggio, MD; Neil Chheda, MD
E34 Visualized ethmoid roof cerebrospinal fluid leak during frontal balloon sinuplasty
Navdeep R. Sayal, DO; Eytan Keider, DO; Shant Korkigian, DO
E39 Dacryocystorhinostomy with a thulium:YAG laser—a case series
Christopher Tang, MD; Scott Rickert, MD; Niv Mor, MD; Andrew Blitzer, MD, DDS; Martin Leib, MD
E43 A rare case of odontoameloblastoma in a geriatric patient
Pratyusha Yalamanchi, MD, MBA; Orly Coblens, MD; Meejin Ahn, DO; Steven B. Cannady, MD; Jason G. Newman, MD
DEPARTMENTS
222 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018 EDITORIAL OFFICE Robert T. Sataloff, MD, DMA, FACS, Editor-in-Chief • 219 N. Broad St., 10th Fl. • Philadelphia, PA 19107 CONTENTS AUGUST 2018 • VOL. 97, NO. 8
220 Advertiser Index 224 ENT Journal Online 226 Editorial 227 Otoscopic Clinic 230 Imaging Clinic 233 Head and Neck Clinic E46 Guest Editorial E48 Rhinoscopic Clinics E52 Laryngoscopic Clinic
*In the U.S. only
ACCLARENT AERA® is intended for use by physicians who are trained on Acclarent technology. Eustachian tube balloon dilation has associated risks, including tissue and mucosal trauma, infection, or possible carotid artery injury. Prior to use, it is important to read the Instructions for Use and to understand the contraindications, warnings, and precautions associated with these devices. The safety of the device as used under local anesthesia has not been evaluated.

Caution: Federal (US) law restricts the sale, distribution or use of these devices to, by or on the order of a physician. Third party trademarks used herein are trademarks of their respective owners. This site is intended for visitors from the United States and published by Acclarent, Inc., which is solely responsible for its contents.
©2017 Acclarent, Inc. All rights reserved. 061003-170803
ACC L ARE NT AER A® Eustachian Tube Balloon Dilation System GO TO THE SOURCE.
only balloon dilation system*speci cally designed to address persistent Eustachian tube dysfunction at its source. OpenMyEars.com | Acclarent.com
The
JOURNAL ONLINE
Ear, Nose & Throat Journal's website is easy to navigate and provides readers with more editorial content each month than ever before. Access to everything on the site is free of charge to physicians and allied ENT professionals. To take advantage of all our site has to offer, go to www.entjournal. com and click on the “Registration” link. Once you have filled out the brief registration form, you will have full access. Explore and enjoy!
ONLINE EXCLUSIVES
Treatment outcomes in HPV-negative oropharyngeal cancer: Surgery plus radiotherapy vs. definitive chemoradiotherapy
Dominique Rash, MD; Megan E. Daly, MD; Blythe Durbin-Johnson, PhD; Andrew T. Vaughan, PhD; Allen M. Chen, MD
We performed a retrospective study to compare clinical outcomes among 51 consecutively presenting patients—38 men and 13 women, aged 46 to 74 years (median: 57)— with locally advanced human papillomavirus (HPV)-negative oropharyngeal cancer who were treated with either primary surgery followed by postoperative radiotherapy (S/RT group; n = 22) or definitive chemoradiotherapy alone (CRT group; n = 29). Within the cohort, 45 patients reported....
Protective effect of pentoxifylline on amikacininduced ototoxicity
Mohammad Waheed El-Anwar, MD; Said Abdelmonem, MD; Ebtessam Nada, MD; Dalia Galhoom, MD; Ahmed A. Abdelsameea, MD
We conducted an animal experiment to assess the effect of adding pentoxifylline to amikacin to prevent amikacin-induced ototoxicity. This research was conducted on 24 rats arranged in four groups of 6. One group was injected with 200 mg/kg of intramuscular amikacin once daily for 14 days (AMK-only group). Another received 25 mg/kg of oral pentoxifylline and 200 mg/kg of intramuscular amikacin once daily for 14 days (PTX-AMK 14/14 group). A third group received 25 mg/kg of oral pentoxifylline for 28 days and 200 mg/kg of intramuscular amikacin once daily for 14 days on days 15 through 28 of the pentoxifylline regimen (PTX-AMK 28/14....
Chronic otitis media with effusion in chronic sinusitis with polyps
Mary Daval, MD; Hervé Picard, MD, MSc; Emilie Bequignon, MD; Philippe Bedbeder, MD; André Coste, MD, PhD; Denis Ayache, MD, PhD; Virginie Escabasse, MD, PhD
The relationship between otitis media with effusion (OME) and chronic rhinosinusitis with nasal polyposis (CRSwNP) remains unclear. We conducted a cross-sectional study of 80 consecutively presenting patients—42 males and 38 females, aged 15 to 76 years (median: 48)—who were diagnosed with CRSwNP. Our aim was to ascertain the prevalence of OME in CRSwNP patients, to determine whether the severity of CRSwNP affected....
Ancillary medications and outcomes in posttonsillectomy patients
Ashley P. O’Connell Ferster, MD; Eric Schaefer, MS;
Jane R. Schubart, MBA, PhD;
Michele M. Carr, DDS, MD, PhD
To investigate the impact of medications on outcomes after tonsillectomy, a retrospective review using the MarketScan database was performed. A total of 306,536 privately insured children and adolescents (1 to 17 years old) who underwent tonsillectomy/adenoidectomy were identified from 2008 to 2012. Pharmaceutical claims identified patients who received outpatient prescriptions for ibuprofen, steroids, or topical anesthetics until discharge and for medications for the treatment of attention deficit hyperactivity....
Safety and utility of direct laryngoscopy and bronchoscopy in patients hospitalized with croup
Daniel P. Fox, MD; Julina Ongkasuwan, MD
Acute croup is a common admitting diagnosis for pediatric patients. If a patient is not responding to medical management for presumed croup, the otolaryngology team is occasionally consulted for direct laryngoscopy and bronchoscopy (DLB) to rule out tracheitis or another airway pathology. We conducted a study to determine if inpatient DLB in acute croup is safe and efficacious and to correlate preoperative vital signs with intraoperative findings. We reviewed the charts of 521 patients with an admitting diagnosis of acute tracheitis, acute laryngotracheitis, or croup. Of this group, 18 patients—11 boys and 7 girls, aged 1 month to 3.3 years (mean: 1.3 yr)—had undergone inpatient DLB. Comorbidities, complications, and level of care were also analyzed. Five patients (28%) had gastrointestinal reflux ....
Inflammatory myofibroblastic tumor of the epiglottis excised with a carbon dioxide laser: Case report and literature review
Blake Raggio, MD; Neil Chheda, MD
Inflammatory myofibroblastic tumor (IMT) is a benign neoplasm of intermediate biologic potential. It rarely occurs in the larynx, and it has not been previously reported in the epiglottis. We treated a 66-year-old woman who presented with progressive dysphonia and a mass on her suprahyoid epiglottis. The tumor was completely excised with a CO 2 laser; no adjuvant therapy was administered. Histopathology revealed that the mass was an IMT. No evidence of recurrence was noted after 6 months of follow-up. We present what we believe is the....
224 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018
www.entjournal.com
Visualized ethmoid roof cerebrospinal fluid leak during frontal balloon sinuplasty
Navdeep R. Sayal, DO; Eytan Keider, DO; Shant Korkigian, DO
Balloon sinus dilation (BSD) is generally accepted as a safe alternative to traditional sinus surgery. It is a unique technique designed to potentially minimize complications....
Dacryocystorhinostomy with a thulium: YAG laser—a case series
Christopher Tang, MD; Scott Rickert, MD; Niv Mor, MD; Andrew Blitzer, MD, DDS; Martin Leib, MD
We conducted a retrospective chart review of 27 patients—7 men and 20 women, aged 47 to 94 years (mean: 71.3)—with symptomatic epiphora secondary to dacryostenosis who....
A rare case of odontoameloblastoma in a geriatric patient
Pratyusha Yalamanchi, MD, MBA; Orly Coblens, MD; Meejin Ahn, DO; Steven B. Cannady, MD; Jason G. Newman, MD
Odontoameloblastoma is an extremely rare tumor derived from odontogenic epithelium and mesenchyme. In the fewer than 20 reported cases, odontoameloblastoma is described
as occurring in the maxilla or mandible of young men with a history of unerupted teeth. Here we report a case of a 73-year-old woman who presented to the dentist for routine cleaning and x-rays, which displayed a mandibular lesion....
ONLINE DEPARTMENTS
Guest Editorial: ENT Journal at the crossroads: Personal perspectives from an editorial board member
Rhinoscopic Clinics: A polyp originating in the middle turbinate and extending to the maxillary sinus ostium
Jae Hoon Lee, MD
Endoscopic view of postoperative maxillary sinus mucoceles separated by bony septum
Jae-Hoon Lee, MD
Laryngoscopic Clinic: Isolated lymphatic malformation of the postcricoid space
Douglas Sidell, MD; Arjun S. Joshi, MD; Christopher R. Kieliszak, DO; Steven A. Bielamowicz, MD
Reach More Patients.
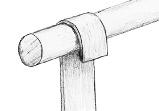
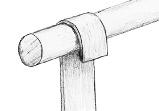
People come in different shapes and sizes.The same piece of equipment does not fit them all.Make oropharyngeal surgery easier with a simple extension.The CANT Corporation has created the Dedo Extension that fits between the Mayo Stand and the Crowe-Davis mouth gag so that it can be adjusted to fit larger patients.The DE98-A mounts to the square-sided Mayo Stand,while the DE98-B fits the tubular-sided support. The Dedo Extension - a simple but effective solution.


Applicable Procedures
• T&A’s
The Crowe-Davis mouth
• Uvuloplasty
• Palatoplasty
• All oropharyngeal procedures using a Crowe-Davis mouth gag
Volume 97, Number 8 www.entjournal.com 225 ENT JOURNAL ONLINE
The Dedo Extension
The Mayo Stand
gag
337 • 233 • 2666, ext.9 • www.jrcant.com • PO Box 3522 • Lafa yette,LA 70502 Extension “DE98-B” also available for tubular support Extension “DE98-A” A B Dedo Ext 9 (ENT1/18/05) 1/19/05 1:51 PM Page 1
Telemedicine: Part II
[Note: This is Part II of a two-part Editorial. Part I was published in the July 2018 issue. It has been adapted with permission from Rubin J, Sataloff RT, Korovin G. Telemedicine. In: Rubin J, Sataloff RT, Korovin, G (eds). Diagnosis and Treatment of Voice Disorders. 4th Ed. San Diego: Plural Publishing, Inc.; 2014:781-4.]
A 2012 Guest Editorial for Ear, Nose & Throat Journal outlines ENT-related usages of telemedicine.15 Some examples include: Louisiana in the aftermath of Hurricane Katrina, where a telemedicine service was developed for neurotology patients,16 and Anchorage, Alaska, where a remote video-otoscopy service has been devised for post-tympanotomy tube insertion patients.17 There are several potential benefits of telemedicine for patients with voice disorders and their providers, including remote readings of strobovideolaryngoscopic and high-speed imaging, as well as provision of voice therapy.18 Telemedicine has several issues that still must be addressed if it is to become a pillar of medical care. Initial issues included difficulty in use, expense, limited reach, and slowness of service. Many of these issues have been resolved as technology has improved. Concerns regarding patient confidentiality, security, and regulatory challenges remain, however. Reimbursement issues also are still problematic in many areas, placing the investment burden on the hospital healthcare system or physician. Furthermore, cultural barriers are not easy to overcome as patients and doctors need to adapt to telemedicine paradigms for most effective use of the new techniques. There also are legal issues that remain a substantial impediment, especially in the United States, where medical licensure is on a state-by-state basis. Problematic examples can be envisioned readily. For example, if a physician is performing a remote examination on a patient who is physically in the state of California while the physician is working in and only licensed to practice medicine in the state of New York, is the physician liable for practicing medicine in California without a license? At present, the answer is yes. The location of practice is defined as the location of the patient, not the physician. Clarification also is required for analysis of biosignals, such as radiologic examinations that are stored in one state but reviewed in another. Similar queries could be posited for physicians practicing remotely between countries. As of the time of writing this editorial, the underlying suppositions that telemedicine is cost-effective and that it improves well-being are still unproven. The Whole
System Demonstrator Programme was launched by Great Britain’s Department of Health in May 2008. It is the largest randomized, controlled trial of telehealth and telecare in the United Kingdom, involving (according to the Department of Health in its “Early Headline Findings”)19 6,191 patients and 238 general practices across three sites: Newham, Kent, and Cornwall. In total, 3,030 people with one of three conditions (diabetes, heart failure, or chronic obstructive pulmonary disease) were included in the telehealth trial. For the telecare element of the trial, people were selected using the Fair Access to Care Services criteria.19
The results are still being analyzed. The UK Department of Health states: “If used correctly, telehealth can deliver a 15% reduction in A&E [accident and emergency department] visits, a 20% reduction in emergency admissions, a 14% reduction in elective admissions, a 14% reduction in bed days, and an 8% reduction in tariff costs. More strikingly…a 45% reduction in mortality rates.”19
In 2012, Steventon et al described 179 general practices and 3,230 people with diabetes, chronic obstructive pulmonary disease, or heart failure recruited from practices between May 2008 and November 2009 and concluded that telehealth is associated with lower mortality and emergency admission rates.20 The reasons for the short-term increases in admissions for the control group are not clear, but the trial recruitment processes could have had an effect. However, as Gornall stated, “Whether telehealth can help to reduce NHS costs, chiefly by reducing admissions and freeing up beds for closure, remains a complex question.”21
The BBC website, on March 21, 2013, ran the headline, “NHS remote monitoring ‘costs more.’”22 In this article, they stated, “The cost per quality—adjusted life year—a combined measure of quantity and quality of life of telehealth—was £92,000 when added to usual care. This is way above the threshold of £30,000 that the National Institute for Health and Clinical Excellence has set. A bestcase scenario considering that the price of equipment was likely to fall over time and that services were not running at full capacity during the trial, saw the probability that the service was cost-effective rise from 11% to 61%.”
In 2016, Gunter et al published a systematic review of the current use of telemedicine for postdischarge surgical care.23 Their review provided 72 references, including seven articles that studied clinical outcomes associated with telemedicine. All reported either no difference in the numbers of complications in the telemedicine group versus the group receiving usual care, or slightly higher
Continued on page 228
226 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018
EDITORIAL
Persistent stapedial artery with ankylosis of the stapes footplate
Fiona C.E.
A 46-year-old man presented to the Otolaryngology Department with a 10-year history of right-sided hearing loss. He denied any prior ear problems or family history of hearing loss. An audiogram demonstrated a right maximal conductive loss and a Carhart notch. Computed tomography (CT) demonstrated a 2-mm lucency on the oval window (figure 1). The opinion of the radiologist was that this was in keeping with an otosclerotic plaque.
The patient gave consent for middle ear exploration and stapedectomy. His malleus and incus were mobile. A large, pulsating vessel was found passing through the crura of the stapes, consistent with a persistent stapedial artery (PSA) (figure 2). His stapes footplate was found to be fixed. Because of the large PSA, stapedectomy was abandoned, despite the presence of a fixed stapes.
Postoperatively, the CT images were reviewed and the lucency that had previously been identified on the
stapes footplate was determined to be a PSA. The patient also was noted to have an absent foramen spinosum, one of the features of PSA (figure 3).
Given the position and size of the patient’s PSA, his treatment options were either hearing aids or ablation of the PSA followed by a stapedotomy. Because of the theoretical risks of ablation, including bleeding and injury to the facial nerve, the patient decided to use hearing aids to manage his conductive hearing loss.
PSA is a rare congenital vascular anomaly with a prevalence of 0.02% to 0.5%.1 It may present as a pulsatile middle ear mass or may appear as an incidental finding during middle ear surgery. Most patients with a PSA are asymptomatic. The classic CT findings suggestive of a PSA include a soft-tissue prominence in the region of the tympanic segment of the facial nerve and the absence of the ipsilateral foramen spinosum. These findings also can include a small canaliculus

Volume 97, Number 8 www.entjournal.com 227
From the Department of Otolaryngology Head and Neck Surgery, The Royal Victorian Eye and Ear Hospital, East Melbourne, Victoria, Australia (Dr. Hill and Mr. Tykocinski); and the Department of Otolaryngology Head and Neck Surgery, The Alfred Hospital, Melbourne, Victoria, Australia (Dr. Bing and Mr. Tykocinski). The case described in this article occurred at The Alfred Hospital.
OTOSCOPIC CLINIC
Hill, MBBS; Bing Teh, MBBS; Michael Tykocinski, FRACS
Figure 1. CT demonstrates the opacification over the stapes footplate (arrow), originally reported as a sclerotic plaque but determined to be a PSA.
originating from the carotid canal and enlargement of the tympanic segment of the facial nerve canal or a separate canal paralleling the facial nerve. In the present case, the presence of the soft tissue on the stapes footplate initially gave the appearance of an otosclerotic plaque. This case illustrates an unusual presentation of a PSA and demonstrates the importance of thorough middle ear assessment in the management conductive hearing loss.
Reference
1. Moreano EH,
D,
Continued from page 226 complication rates in the telemedicine group, although they could not relate those complications causally to the use of telemedicine. The greatest financial savings noted in their review accrued to the patients, particularly savings related to travel time and costs, although savings to healthcare systems were found, as well.
The role of telemedicine is increasing. Newer technologies such as mobile phone messaging applications, short message service, and multimedia message service have become readily available. Such technologies lend themselves to telemedical approaches. However, the future standing of telemedicine in medicine in general and in otolaryngology specifically remains unclear.
References
15. Garritano FG, Goldenberg D. Telemedicine in otolaryngology–head and neck surgery. Ear Nose Throat J 2012;91(6):226–9.

16. Arriaga MA, Nuss D, Scrantz K, et al. Telemedicine- assisted neurotology in post-Katrina Southeast Louisiana. Otol Neurotol 2010;31(3):524–7.
17. Kokesh J, Ferguson As, Patricoski C, et al. Digital images for postsurgical follow-up of tympanostomy tubes in remote Alaska. Otolaryngol Head Neck Surg 2008;139(1):87–93.

18. Rubin, J, Sataloff, RT, Korovin, G. Telemedicine. In: Diagnosis and Treatment of Voice Disorders, 4th edition. San Diego: Plural Publishing, Inc.; 2014:781-4.
19. Department of Health. Whole System Demonstrator Programme: Headline findings. December 2011. https://www.gov.uk/government/ publications/whole-system-demonstrator-programme-headlinefindings-december-2011. Accessed June 11, 2018.
20. Steventon A, Bardsley M, Billings J, et al. Effect of telehealth on use of secondary care and mortality: Findings from the Whole System Demonstrator cluster randomised trial. BMJ 2012;344:e3874.
21. Gornall J. Does telemedicine deserve the green light? BMJ 2012;345:e4622.
22. No authors listed. NHS remote monitoring ‘costs more.’ BBC News. March 21, 2013. www.bbc.co.uk/news/health-21874978. Accessed July 12, 2018.
23. Gunter RL, Chouinard S, Fernandes-Taylor S, et al. Current use of telemedicine for post-discharge surgical care: A systematic review. J Am Coll Surg 2016;225(5):915-27.
John S. Rubin, MD, FACS, FRCS
Royal National Throat Nose and Ear Hospital
National Hospital for Neurology and Neurosurgery
University College London Hospitals NHS Trust
School of Health Sciences
City, University of London
Department of Surgery
University College of London
London, United Kingdom
Robert T. Sataloff, MD, DMA, FACS
Editor-in-Chief
Ear, Nose & Throat Journal
1994;104(3 Pt 1):309-20.
Department of Otolaryngology–Head and Neck Surgery
Drexel University College of Medicine
Philadelphia
228 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018
CLINIC
EDITORIAL OTOSCOPIC
Figure 2. In this photograph down the external auditory canal with the tympanic membrane elevated, the pulsatile stapedial artery can be seen running over the stapes footplate, between the anterior and posterior crura. The stapedius tendon and chorda tympani nerve are seen in the foreground.
Figure 3. CT reveals the bilateral foramen ovale (red arrows) and the foramen spinosum on the left (yellow arrow), which is absent on the right.
Paparella MM, Zelterman
Goycoolea MV. Prevalence of facial canal dehiscence and of persistent stapedial artery in the human middle ear: A report of 1000 temporal bones. Laryngoscope
Portability Redefined
ENTity
Protects endoscope from damage during transport


Crash cart compatible
Shoulder strap offers mobility to move throughout hospital
ENTity™ XL Flexible Laryngoscope Everywhere ENT Clinicians Need to Be Outpatient Clinic | ICU | Bedside | ER | Radiation Oncology | OR TM Designed to empower ENT clinicians with the visibility & mobility they need Powerful innovation. proven performance. All-in-one, portable, flexible ENT scopes for clinic and bedside Contact Us Today : 800.225.7486 / sales@optim-llc.com Find out how to make the transition to portability with our endoscope trade-in program* *Program valid through September 30, 2018 | Mention offer code: GetTheBest www.optim-llc.com/entitygetthebest you’ve seen the rest now get the best Trade-in Promo Flexible Laryngoscopes No cables. No additional equipment. No Limits.
EndoCarrier
Transport System
ENTity XL & ENTity SDXL Laryngoscope Brightest, long-lasting patented LED lighting technology Durable craftsmanship and design with industry leading two-year warranty Standard and small diameter options to meet patient needs Get the Best - End the summer by adding the new generation ENTity XL Flexible Laryngoscope to your practice. Trade in your old endoscope for a credit towards the purchase of a brand new ENTity XL or SDXL Laryngoscope featuring our latest next generation LED illumination.
Powerful Innovation
IMAGING CLINIC
Bilateral massive pharyngoceles
Norair Adjamian, DO; Lyndsay L. Madden, DO; Libby J. Smith, DO
A 20-year-old collegiate man presented for evaluation of progressively worsening throat pain and left-sided neck bulging that occurred while he was playing the trumpet. He rated the pain as moderate and compared it to a sore throat one would experience with a common cold. The pain and neck fullness completely subsided when he was not playing the trumpet. He denied having associated dysphagia or dyspnea. His physical examination demonstrated a large, soft, left, easily compressible lateral neck fullness when he puffed his cheeks. Flexible laryngoscopy demonstrated no abnormalities of vocal fold motion or laryngeal lesions.
Based on these findings, a fine-cut, contrast-enhanced computed tomography (CT) imaging study of the larynx was acquired. Imaging was first taken with the patient at rest and then with his achieving positive pharyngeal pressure by exhaling through pursed lips, mimicking playing the trumpet. The results revealed normal anatomy at rest (figure 1) and massive bilateral pharyngoceles with positive pharyngeal pressure when exhaling (figure 2). CT showed no evidence of an underlying mass, fluid, or infection.
Reports of pharyngoceles are uncommon in the literature. They also have been described as lateral pharyngeal diverticulum, pharyngeal pouch, aerocele, pulsion pouch, and pulsion diverticulum.1 Dysphagia is described as the most common presenting complaint, followed by neck swelling and food regurgitation.2 Therefore, the differential diagnosis can be vast, and misdiagnosis often can occur without proper imaging studies.
The etiology of pharyngoceles often has been associated with elevations in intrapharyngeal pressure, as seen in individuals who play wind instruments; however, it has been postulated that pharyngoceles also can be a manifestation of a branchial arch anomaly, specifically a branchial sinus outpouching that may dilate over time.3

Nonsurgical treatment measures have provided excellent outcomes in symptomatic patients.4 A compressive neck wrap worn when he was playing the trumpet provided symptomatic relief to our patient. When surgery is required, external or endoscopic approaches are used.5 With proper history acquisition, physical exam, and imaging studies with normal and elevated pharyngeal pressures, pharyngoceles can be correctly diagnosed and treated appropriately.
From the Department of Medicine, Kansas City University of Medicine and Biosciences, Kansas City, Mo. (Dr. Adjamian); the Department of Otolaryngology Head and Neck Surgery, Wake Forest Baptist Medical Center, Wake Forest University Center for Voice and Swallowing, Winston-Salem, N.C. (Dr. Madden); and the Department of Otolaryngology Head and Neck Surgery, University of Pittsburgh Medical Center, University of Pittsburgh Voice Center, Pittsburgh, Pa. (Dr. Smith). The case described in this article occurred at the University of Pittsburgh Voice Center.
230 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018
Figure 1. Postcontrast axial CT section at the level of the hyoid bone (triangle) and pharynx (asterisk) demonstrates normal hypopharyngeal anatomy without positive pharyngeal pressure.
Since 1898, Reliance Medical Products has had an unmatched reputation for reliability and craftsmanship, building everything from exam chairs to ENT cabinets and accessories that stand up to anything. Including the test of time. And we’d like to thank all the doctors along the way who’ve helped us reach this proud milestone.




Learn how our history of excellence can help build a stronger future for you. Stop by our booth #1732 at the AAO-HNSF annual meeting.

BUILT TO LAST. AND LAST. AND LAST. A REPUTATION 120 YEARS IN THE MAKING.
Builttosupport.com © 2018 Haag-Streit USA. All Rights Reserved.
800.735.0357 |
2018 Reliance 710 Premiere Chair
1962 Reliance Model 630 Chair
1926 Reliance Barber Chair
Figure 2. A: Postcontrast axial CT section at the level of the hyoid bone (triangle), mandible (circle), and pharynx (asterisk) demonstrates bilateral pharyngoceles with positive pharyngeal pressure. B: This postcontrast axial CT section demonstrates massive bilateral pharyngoceles at the level of the pharynx (asterisk), below the hyoid.


References
1. Norris CW. Pharyngoceles of the hypopharynx. Laryngoscope 1979;89(11):1788–1807.
2. Naunheim M, Langerman A. Pharyngoceles: A photo-anatomic study and novel management. Laryngoscope 2013;123(7):1632–8.
3. Chang CY, Furdyna JA. Bilateral pharyngoceles (branchial cleft anomalies?) and endoscopic surgical considerations. Ann Otol Rhinol Laryngol 2005;114(7):529–32.

4. Daultrey C, Colley S, Costello D. “Doctor I have a frog in my throat”: Bilateral pharyngoceles in a recreational trumpet player. Journal of Laryngology & Voice 2013;3(1):18-21.
5. Yılmaz T, Cabbarzade C, Süslü N, et al. Novel endoscopic treatment of pharyngocele: Endoscopic suture pharyngoplasty. Head Neck 2014;36(8):E78–80.
232 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018
A B IMAGING CLINIC
HEAD AND NECK CLINIC
Castleman disease
A 57-year-old man presented with a 3-year history of a left anterior neck mass. It was nonpainful and did not cause dysphagia, hoarseness, or difficulty breathing. Physical examination was significant for a firm, well-circumscribed, nonulcerating mass at left level 1B, with no overlying skin changes. Additionally, he had asymmetric left tonsillar hypertrophy. Flexible fiberoptic laryngoscopy revealed no abnormalities. Computed tomography (CT) of the neck with contrast revealed lymphadenopathy involving left level 1B measuring 3.1 cm (figure 1) and left supraclavicular

fossa measuring 2.1 cm, as well as asymmetric fullness of the left palatine tonsil. The patient proceeded with bronchoscopy, esophagoscopy, direct laryngoscopy, tonsillectomy, and open neck biopsy. Right tonsil, left tonsil, and level 1B lymph node surgical specimens were sent for review.
Histologically, the lymph node showed an overall increase of small atrophic follicles. The mantle zone was expanded, forming an “onion-skin” appearance that was penetrated by hyalinized vessels at a right angle (figure 2, A). Two atrophic germinal centers within a single
From the Department of Otolaryngology–Head and Neck Surgery, Philadelphia College of Osteopathic Medicine, Philadelphia (Dr. Cohn); and the Department of Otolaryngology–Head and Neck Surgery (Dr. Cohn and Dr. Hu) and the Department of Pathology (Dr. Zhou), Drexel University College of Medicine, Philadelphia. The case described in this article occurred at Hahnemann University Hospital, Philadelphia.
Volume 97, Number 8 www.entjournal.com 233
Jason E. Cohn, DO; Jing Zhou, MD, PhD; Amanda Hu, MD
Figure 1. Left level 1B lymphadenopathy measuring 3.1 cm is seen on contrastenhanced CT of the neck.
mantle zone were frequently seen. Interfollicular areas showed paracortical plasmacytosis (figure 2, B). The histology of the tonsils revealed lymphoid hyperplasia with some atrophic germinal centers with an expanded mantle zone. Interfollicular areas also showed increased hyalinized vasculature and plasma cells.
Immunohistochemistry of the tissues was negative for human herpesvirus 8 (HHV-8). Additionally, Epstein-Barr virus RNA in situ hybridization was negative. Flow cytometry revealed normal cell populations. Given these clinical findings, the patient was diagnosed with Castleman disease (CD).


CD, also known as angiofollicular lymph node hyperplasia or giant lymph node hyperplasia, is a rare lymphoproliferative disease characterized by benign, localized enlargement of lymph nodes.1 CD presents more commonly as a solitary mass with a benign course, known as the localized type. Less commonly, patients can present with a more aggressive form involving constitutional symptoms, hepatosplenomegaly, and laboratory abnormalities, referred to as the multicentric type. The multicentric type is usually associated with infection or malignancy such as human immunodeficiency virus (HIV), HHV-8, Kaposi sarcoma, or lymphoma.1,2
Most individuals affected by CD are young to middle-aged, with males and females equally affected. Most cases are asymptomatic, unicentric, and are the hyaline-vascular tissue type.2 The etiology of CD is believed to involve the overproduction of cytokine IL6, which has been shown to increase the proliferation and survival of B cells.1 Therefore, CD is usually treated with immunotherapy.3
Although there have been cases of CD involving the tonsils,4 this is rare. Our case also is unique because the patient’s disease was multicentric and the mixedtype (both hyaline-vascular and plasma-cell type),
and he tested negative for HIV (serology) and HHV-8 (immunohistochemical staining). HIV-negative CD has been associated with certain conditions including autoimmune disease, collagen vascular disorders, pulmonary arterial hypertension, and glomerulopathy. In some instances, the etiology is unknown.3 Once an underlying cause is identified, proper targeted therapy can be instituted.
References
1. Newlon JL, Couch M, Brennan J. Castleman’s disease: Three case reports and a review of the literature. Ear Nose Throat J 2007;86(7):414-18.
2. Wu PW, Lee TJ, Huang CC, et al. Intermittent hemoptysis and blood-tinged sputum. Castleman disease (CD), hyaline-vascular type. JAMA Otolaryngol Head Neck Surg 2013;139(7):743-4.
3. Muskardin TW, Peterson BA, Molitor JA. Castleman disease and associated autoimmune disease. Curr Opin Rheumatol 2012;24(1):76-83.
4. Thakral B, Zhou J, Medeiros LJ. Extranodal hematopoietic neoplasms and mimics in the head and neck: An update. Hum Pathol 2015;46(8):1079-1100.
234 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018
Figure 2. A: Histology shows a regressed germinal center surrounded by an expanded mantle zone (“onion skin”). The hyalinized vessel is penetrating small atrophic follicles. B: Expanded interfollicular zones show paracortical plasmacytosis. Some atypical binucleated forms and enlarged morphology are seen.
A B
HEAD AND NECK CLINIC
IRRIGATION. SUCTION. SYNCHRONIZATION.
Now there’s a better way to provide saline washes. The HydroCleanse™ Sinus Wash Delivery System from Medtronic combines pressurized sinus irrigation with builtin suction capability for a more efficient procedure. Disposable and easy to use, it allows you to irrigate the sinuses while limiting pooling and effluent discharge.
§ Disposable and easy to use
§ 360° fan spray
§ Pressurized saline irrigation
§ Built-in suction capability
§ Choice of angled catheter tips

HydroCleanse™ Sinus Wash Delivery System
IMPROVE THE SALINE WASH EXPERIENCE. CHOOSE HYDROCLEANSE.
Rx only. Refer to product instruction manual/package insert for instructions, warnings, precautions and contraindications.
For further information, please call Medtronic ENT at 800.874.5797 or consult Medtronic’s website at www.medtronicent.com.
© 2018 Medtronic. All rights reserved. Medtronic, Medtronic logo and Further, Together are trademarks of Medtronic. All other brands are trademarks of a Medtronic company. UC201902765 EN 07.2018
Fourth branchial pouch sinus: A report of 7 cases and review of the literature
Indranil Pal, MS; Saumitra Kumar, MS; Ankur Mukherjee, MS, DNB; Bibhas Mondal, MS; Anindita Sinha Babu, MD
Abstract
A fourth branchial pouch sinus often manifests quite late in life as a recurrent neck abscess, suppurative thyroiditis, or pseudothyroiditis. Demonstration of the sinus opening in the piriform fossa by hypopharyngoscopy in combination with ultrasonography of the neck provides adequate information to justify proceeding to surgery. The sinus tract usually courses through the thyroid cartilage. The most effective treatment is surgical excision of the tract up to the piriform fossa through the cartilage. This procedure is associated with very low complication and recurrence rates. A fourth branchial pouch sinus is an uncommon condition. Even so, it is still underdiagnosed as a result of poor awareness of its existence by medical practitioners, including otolaryngologists. Part of the reason is a lack of adequate coverage of this topic in otolaryngology and surgery textbooks. In this article, we add to the literature by describing our experience with 7 patients—4 males and 3 females, aged 5 to 45 years (mean: 25.6)—who were diagnosed with a fourth branchial pouch sinus over a 6-year period. The diagnosis was confirmed by identifying the sinus opening at the apex of the piriform sinus during hypopharyngoscopy. Definitive treatment consisted of surgical exploration of the neck and excision of the tract.
Introduction
Branchial cleft anomalies are not uncommon in clinical practice. Most of these (~95%) originate in the second branchial cleft.1 The remainder originate in the first, third, or fourth clefts.2
From the Department of Otorhinolaryngology (Dr. Pal, Dr. Kumar, Dr. Mukherjee, and Dr. Mondal) and the Department of Pathology (Dr. Babu), College of Medicine & JNM Hospital, West Bengal University of Health Sciences, Kalyani, Nadia, West Bengal, India.
Corresponding author: Dr. Indranil Pal, Department of Otorhinolaryngology, College of Medicine & JNM Hospital, West Bengal University of Health Sciences, Kalyani, Nadia, West Bengal 741235, India. Email: thisisindranil@yahoo.co.in
Fourth branchial cleft anomalies are rarely encountered, poorly understood, and often misdiagnosed. As a result, patients with this condition often undergo multiple consultations, referrals, and interventions before a definitive diagnosis is made and treatment instituted. The reason for this is a lack of awareness about this condition among the medical community— specifically, among otolaryngologists, general surgeons, and pediatricians, who are generally the first to attend these patients after referral by a general practitioner.
Fourth branchial pouch anomalies clinically manifest as a recurrent neck abscess, suppurative thyroiditis, or pseudothyroiditis.3 They are almost always located on the left side of the midline in the anterior part of the neck. They present as a sinus tract with a proximal opening in the floor of the piriform fossa; from there they extend upward for various distances in the neck.
In this article, we report our experience with 7 cases of fourth branchial pouch sinus, and we discuss their presentation, diagnosis, and treatment. We also discuss the possible reasons for delays in establishing a definitive diagnosis, and we offer our suggestions for making an early diagnosis.
Patients and methods
Patients. Over a period of 6 years at our institution, 7 patients—4 males and 3 females—were diagnosed with and operated on for a fourth branchial pouch sinus by the team of authors. For this study, we retrieved their medical records and compiled, in addition to the demographic data, information on their patient profile, their age at the onset of symptoms, the type of symptoms, the interval between symptom onset and the definitive diagnosis, the side of the sinus, the number of symptomatic episodes, and the number and type of previous surgical interventions performed before the definitive diagnosis was established.
Surgical procedure. All patients were treated under general anesthesia with surgical excision of the sinus
236 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018 ORIGINAL ARTICLE































RHINOWORLD CHICAGO June 6-9, 2019 Sheraton Grand Chicago THE PREMIER CONGRESS FOR RHINOLOGISTS Combined International Rhinology Meeting Robert Kern MD - 2019 ISIAN President Brent Senior MD - 2019 IRS President James Palmer MD - 2019 ARS President David Kennedy MD - ISIAN General Secretary Metin Onerci MD - IRS General Secretary Joseph Jacobs MD - ARS EVP For questions or more information visit RhinoWorld2019.com Contact: Wendi Perez, Executive Administrator, ARS +1-973-545-2735 ext. 6 | wendi@amrhso.com Polly Rossi, CMP-HC, CMM, Meeting Logistics +1-219-465-1115 | polly@meetingachievements.com Kevin Welch MD, Rakesh Chandra MD & David Conley MD - Program Chairs Featuring Pre-Course Dissections on June 5, 2019 SAVE THE DATE Registration opens October 1, 2018
tract through a neck incision. In the operating room, patients were placed in the supine position with the neck extended. An incision was made in equal lengths on both sides of the midline in a transverse neck crease roughly corresponding to the lower end of the lesion. Subplatysmal flaps were raised superiorly and inferiorly for adequate exposure. Superiorly, the exposure extended to the upper border of the thyroid cartilage. The strap muscles were retracted, and the upper pole of the thyroid lobe was exposed.

All the sinus tracts ended roughly at the upper pole of the thyroid gland. The sinus tract was identified and carefully dissected out. The recurrent laryngeal nerve was dissected if the sinus tract extended below the level of the cricothyroid joint. The superior laryngeal nerve was dissected and preserved whenever possible. Thyroid lobectomy was not required in any of our cases because the tract could be dissected free off the thyroid gland in all of them. The tract was then traced superiorly.
In all cases, the tract was found to pierce the thyroid cartilage at its lower end before opening into the piriform fossa. Therefore, a small sliver of thyroid cartilage was cut from the posterior border of the thyroid ala to trace the sinus tract up to the floor of the piriform fossa (figure 1). The tract was then excised as close to the piriform fossa as possible, and the stump was ligated with nonabsorbable sutures. The wound was then closed in layers. No drains were required.
Postoperative recovery was uneventful in all patients, and nonsteroidal anti-inflammatory drugs were the only necessary prescribed medications.
Results
Patients’ age at the onset of symptoms ranged from 3 to 40 years (mean: 20.3), and their age at diagnosis ranged from 5 to 45 years (mean: 25.6) (table 1).
The most common manifestation was recurrent neck abscess, which was seen in 5 of the 7 patients and which required multiple drainings. Recurrent thyroiditis or pseudothyroiditis was seen in 4 patients. One patient (patient 6) also had a pharyngeal fistula in addition to a recurrent abscess and thyroiditis; the fistula developed after she had undergone a total thyroidectomy at another institution for the treatment of suspected medullary thyroid cancer (table 1).
In all cases, the definitive diagnosis was made by viewing the sinus tract opening on the floor of the ipsilateral piriform sinus near its apex (figure 2). In the first 4 patients we tested, a barium swallow examination failed to demonstrate the sinus tract, even after the Valsalva maneuver, so we decided against administering a barium swallow test to the succeeding 3 patients.
Computed tomography (CT) was obtained in patients 1, 2, 3, and 4, followed by ultrasonography of the neck;
both demonstrated a hypodense area in relation to the thyroid gland. Since CT provided no information beyond what we saw on ultrasonography, we did not obtain CT in patients 5, 6, and 7, and we relied on just the ultrasonographic findings.
As described, definitive treatment entailed surgical exploration of the neck and excision of the tract. The tracts were easily dissected off the thyroid lobes, and thyroidectomy of any description was not required in any patient. Electrocautery was attempted in 3 patients (patients 1, 6, and 7), but it was unsuccessful in resolving the symptoms.
Follow-up ranged from 2 months to 6 years. No patient experienced any significant postoperative complications or recurrence (table 2).
Of the 7 patients, only 2 demonstrated the presence of lining epithelium, but all 7 exhibited inflammatory tissue and a tract lumen. The lining epithelium in both cases was stratified squamous epithelium; a focal presence of columnar epithelium was also seen in 1 of these 2 patients. However, even in the absence of any epithelial lining, the presence of a lumen and the preoperative demonstration of a tract opening in the piriform sinus left no doubt about the diagnosis.

238 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018
PAL, KUMAR, MUKHERJEE, MONDAL, BABU
Figure 1. The tract of the right-sided fourth branchial pouch sinus in patient 5 extends behind the ala of the thyroid cartilage and enters the apex of the piriform sinus. A sliver of thyroid cartilage was excised to trace the tract into the piriform fossa (SCM = sternocleidomastoid muscle).
Figure 2. Endoscopic views show the proximal openings of sinus tracts at the apex of the right piriform fossa (A) and the left piriform fossa (B)
Table 1. Clinical data obtained at presentation
Discussion
Although it is theoretically possible, the presence of a complete fourth branchial cleft or pouch fistula has never been demonstrated. It generally presents as a sinus with a proximal opening in the apex of the piriform fossa and with the distal end extending to any point along the theoretical extent of the tract—that is, beginning at the piriform fossa, passing between the thyroid (fourth arch) and cricoid (fifth arch) cartilages, descending between the superior laryngeal nerve and the cricothyroid muscle (fourth arch), and thereafter extending between the trachea and the recurrent laryngeal nerve.
The tract then loops around the aortic arch on the left side and around the subclavian artery on the right side and rises in the cervical area posterior to the common carotid artery. Then it loops over the hypoglossal nerve and finally descends and opens on the skin of the lower neck along the anterior border of the sternocleidomastoid muscle.4
Based on the difference between the theoretical course and the actual course of the sinus tract, Thomas et al suggested that the branchial sinuses arising from the piriform sinuses do not originate in the true third or fourth arch pouches but that they are sinuses arising from a patent thymopharyngeal duct.5 None of the fistulas described in their report were congenital; all were acquired secondary to infection and abscess formation, which was followed by spontaneous rupture or surgical drainage. The lone patient in our series who presented with a fistula had developed it secondary to a thyroidectomy performed at another hospital.
Lu et al suggested that there could be three different emerging pathways for the sinus tract from the piriform fossa.6 The tract could emerge by penetrating either the thyroid cartilage near the inferior cornu, the inferior constrictor muscle of the pharynx, or the cricothyroid membrane as it emerges from the pharynx. In our series, all seven tracts emerged by penetrating the thyroid
cartilage. This probably indicates that this is the most common course.
A third branchial pouch sinus is similar to a fourth branchial pouch sinus in its course and presentation. The difference is that the third pouch sinus opens in the cranial part of the piriform sinus, while the fourth opens more caudally at the apex of the piriform fossa.7 The third pouch sinus then courses superiorly through the thyrohyoid membrane cranial to the superior laryngeal nerve, posterior to the carotid vessels, and deep to the sternocleidomastoid muscle.4 In our series, all the sinus tracts were located caudal to the superior laryngeal nerve, and all opened at the apex of the piriform sinus.
A fourth branchial pouch sinus, like most congenital conditions, is generally believed to manifest as symptoms during the first or second decade of life.8,9 In our series, however, only 3 of the 7 patients experienced an onset of symptoms within the first decade. In the other 4 patients, the initial symptoms manifested late—at the age of 20, 28, 37, and 40 years.
By far, most fourth branchial pouch sinuses occur on the left side, probably as a result of the asymmetry in vascular development in this arch.1 They are rarely seen on the right side, and there are only occasional reports of bilateral sinuses.10 In our series, only 1 of the 7 was located on the right side.
The most common presentation is recurrent deep neck infections, 3 followed by thyroiditis-like features (pseudothyroiditis).11 Two uncommon presentations that have been reported were stridor in a neonate12 and suspected esophageal perforation in a 14-year-old boy.13 Our study yielded similar findings, although we had the 1 case of iatrogenic fistula.
A fourth branchial pouch sinus should be high on the list of differential diagnoses for patients with recurrent thyroiditis or recurrent neck abscess, especially on the left side. The recommended investigations for confirming the diagnosis include a barium swallow examination, sonography with a Valsalva maneuver, fiberoptic
Volume 97, Number 8 www.entjournal.com 239 FOURTH BRANCHIAL POUCH SINUS: A REPORT OF 7 CASES AND REvIEw OF THE LITERATURE
Pt. Sex/age at presentation, yr Age at onset, yr Symptom Side Symptomatic episodes, n Previous surgeries, n 1 M/20 20 RT Left 2 0 2 F/5 3 RNA Left 4 3 3 M/45 40 RNA Left 5 2 4 M/10 8 RNA Left 3 1 5 M/30 28 RT + RNA Right 4 3 6 F/29 6 RT + RNA + fistula Left 6 5 7 F/40 37 RT Left 4 3
Key: RT = recurrent thyroiditis or pseudothyroiditis; RNA = recurrent neck abscess.
Table 2. Investigations, treatments, and outcomes
laryngoscopy, CT, magnetic resonance imaging (MRI), and hypopharyngoscopy under general anesthesia.
In our series, the most definitive diagnosis was made by viewing the sinus tract opening on the floor of the ipsilateral piriform sinus near its apex. Barium swallow examination failed to demonstrate the sinus tract, even after the Valsalva maneuver in our first 4 patients, so we decided against performing this test in the 3 patients who presented later. The reason for the low yield of barium swallow skiagrams is probably because they require a quiescence of inflammation of the tract for the entry of the barium contrast into the sinus.
CT was performed in our first 4 patients, and it demonstrated a hypodense area in relation to the thyroid gland. Ultrasonography of the neck was also performed on these 4 patients, and the findings were similar to those of CT. Since CT provided no additional information beyond what we saw on ultrasonography, we decided that it was unnecessary for the final 3 patients, and we used only the ultrasonographic findings. MRI was not available at our institution.
We believe that the demonstration of the sinus opening in the apex of the piriform sinus with a flexible fiberoptic laryngoscope or bronchoscope or with an upper gastrointestinal endoscope is a simple, highly sensitive, and highly specific procedure for confirming the diagnosis of a fourth branchial pouch sinus. We also conclude that ultrasonography of the neck performed by an experienced and competent radiologist is sufficient to identify the extent of the sinus tract. The two procedures together provide us with adequate information with which to proceed to surgery. Other radiologic investigations yielded little additional information over and above what these two procedures did.
The most noteworthy finding of our study was that almost all of our patients presented with two or more episodes of pseudothyroiditis or abscess in the neck that required multiple drainings. One of our patients (patient 6) had undergone five previous surgical interventions
at different hospitals, including a total thyroidectomy that led to the development of a nonhealing fistula in her neck, and yet a precise diagnosis was not made.

In an attempt to understand the low level of suspicion among physicians when it comes to recognizing and diagnosing fourth branchial pouch sinuses, we reviewed the world literature as available on PubMed. We found that the interval between the first appearance of symptoms and the final diagnosis ranged from 2 to 10 years,14,15 excluding neonatal presentations12,16 and incidental presentations.13 In a case published in 2012, a young boy experienced 10 episodes of neck abscess during a 10-year span, and he had undergone seven surgical interventions before a diagnosis was finally reached.6 This fact is astonishing given that more than 100 cases of fourth branchial sinus have been indexed on PubMed, with the first case having been reported more than 40 years ago.2
We also reviewed 6 reference books on otorhinolaryngology and head and neck surgery and found only 1 that contained a complete description, which consisted of 27 lines of text.17 We found 3 to 8 lines of text tucked away in four other books.18-21 We also checked 3 reference books in surgery along with 10 different textbooks used by undergraduate medical students in otorhinolaryngology, and none of them contained any mention of this condition. We believe that the description of this condition should not be limited to articles in peer-reviewed journals, but should be included in detail in all future textbooks, for undergraduates as well as for postgraduates, to raise the level of awareness of this condition.
The definitive treatment for a fourth branchial pouch sinus is an excision of the tract via a neck incision, sometimes accompanied by a hemithyroidectomy,6,9 an endoscopic transpharyngeal excision with a CO2 laser, 22 chemocauterization with 10% trichloroacetic acid, 23 endoscopic monopolar
240 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018
PAL, KUMAR, MUKHERJEE, MONDAL, BABU
diathermy,24 or
endoscopic tissue fibrin glue biocauterization.25
even KTP-laser–assisted
Pt. Scope findings* Site of tract exit Thyroid lobectomy Vocal fold paralysis Follow-up Recurrence 1 Opening identified Thyroid cartilage Not done No 6 yr No 2 Opening identified Thyroid cartilage Not done No 4 yr No 3 Opening identified Thyroid cartilage Not done No 3 yr No 4 Opening identified Thyroid cartilage Not done No 3 yr No 5 Opening identified Thyroid cartilage Not done No 2 yr No 6 Opening identified Thyroid cartilage Not done No 3 mo No 7 Opening identified Thyroid cartilage Not done No 2 mo No
* Hypopharyngoscopy.


www.macksearplugs.com *Independent research as completed by Business Research Group, February 2014. Pillow Soft® comfort only from Mack’s®, the original moldable silicone putty earplug. Mack’s ® is the #1 Doctor Recommended earplug brand to help prevent otitis externa and to get a good night’s sleep when sleeping with a snoring spouse.* Available at pharmacies.
We managed all of our patients with surgical excision of the tract through a neck incision. In all cases, we could dissect the sinus tract from the thyroid gland and surrounding tissues, and therefore we did not have to perform a thyroid lobectomy in any patient.
The sinus tract is said to be lined with columnar epithelium. In our series, most patients exhibited a denudation of the epithelial lining, owing to recurrent inflammation. Two of our patients had a stratified squamous epithelium. This might have been attributable to a metaplastic change in the normal columnar epithelial lining of the branchial sinus secondary to recurrent inflammation.3,26 In such a circumstance, histopathology provides little clue as to the diagnosis of a fourth branchial pouch sinus.
In conclusion, a fourth branchial pouch sinus is an uncommon yet underdiagnosed condition. Awareness of its existence is low, and thus so is a suspicion for it among medical practitioners, including otolaryngologists. The problem is compounded by a lack of adequate coverage of this topic in otorhinolaryngology and surgery textbooks, a deficiency that needs to be corrected in the future.
The most common presentation of this condition is a recurrent neck abscess on the left side. Symptoms often manifest quite late in life, unlike the case with most congenital sinuses, fistulae, and cysts.
A fourth branchial pouch sinus is best diagnosed by demonstration of the sinus opening in the piriform fossa. Hypopharyngoscopy in combination with ultrasonography of the neck provides adequate information with which to proceed to surgery.
The tract most commonly courses through the thyroid cartilage. Surgical excision of the tract up to the piriform fossa through the cartilage is the most effective treatment, and it is associated with very low complication and recurrence rates.
References
1. Rosenfeld RM, Biller HF. Fourth branchial pouch sinus: Diagnosis and treatment. Otolaryngol Head Neck Surg 1991;105(1):44-50.
2. Tucker HM, Skolnick ML. Fourth branchial cleft (pharyngeal pouch) remnant. Trans Am Acad Ophthalmol Otolaryngol 1973;77(5):ORL368-71.
3. Godin MS, Kearns DB, Pransky SM, et al. Fourth branchial pouch sinus: Principles of diagnosis and management. Laryngoscope 1990;100(2 Pt 1):174-8.
4. Liston SL. Fourth branchial fistula. Otolaryngol Head Neck Surg 1981;89(4):520-2.
5. Thomas B, Shroff M, Forte V, et al. Revisiting imaging features and the embryologic basis of third and fourth branchial anomalies. AJNR Am J Neuroradiol 2010;31(4):755-60.
6. Lu WH, Feng L, Sang JZ, et al. Various presentations of fourth branchial pouch sinus tract during surgery. Acta Otolaryngol 2012;132(5):540-5.
7. Franciosi JP, Sell LL, Conley SF, Bolender DL. Pyriform sinus malformations: A cadaveric representation. J Pediatr Surg 2002;37(3):533-8.
8. Yang C, Cohen J, Everts E, et al. Fourth branchial arch sinus: Clinical presentation, diagnostic workup, and surgical treatment. Laryngoscope 1999;109(3):442-6.
9. Madana J, Yolmo D, Kalaiarasi R, et al. Recurrent neck infection with branchial arch fistula in children. Int J Pediatr Otorhinolaryngol 2011;75(9):1181-5.
10. Rea PA, Hartley BE, Bailey CM. Third and fourth branchial pouch anomalies. J Laryngol Otol 2004;118(1):19-24.
11. Contencin P, Grosskopf-Aumont C, Gilain L, Narcy P. Recurrent pseudothyroiditis and cervical abscess. The fourth branchial pouch’s role. Apropos of 16 cases [in French]. Arch Fr Pediatr 1990;47(3):181-4.
12. Nathan K, Bajaj Y, Jephson CG. Stridor as a presentation of fourth branchial pouch sinus. J Laryngol Otol 2012;126(4):432-4.
13. Jeyakumar A, Hengerer AS. Various presentations of fourth branchial pouch anomalies. Ear Nose Throat J 2004;82(9):640-2, 644.
14. Mehrzad H, Georgalas C, Huins C, Tolley NS. A combined third and fourth branchial arch anomaly: Clinical and embryological implications. Eur Arch Otolaryngol 2007;264(8):913-16.
15. Hamoir M, Rombaux P, Cornu AS, Clapuyt P. Congenital fistula of the fourth branchial pouch. Eur Arch Otolaryngol 1998;255(6):322-4.
16. Leboulanger N, Ruellan K, Nevoux J, et al. Neonatal vs delayed-onset fourth branchial pouch anomalies: Therapeutic implications. Arch Otolaryngol Head Neck Surg 2010;136(9):885-90.
17. Gleeson M, ed. Scott-Brown’s Otorhinolaryngology, Head and Neck Surgery. 7th ed. London: Hodder Arnold; 2008:1779-80.
18. Bailey BJ, Johnson JT, Newlands SD, eds. Head & Neck Surgery–Otolaryngology. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2006:1211.
19. Flint PW, Haughey BH, Lund VJ, John K, et al. Cummings Otolaryngology Head and Neck Surgery. 5th ed. Philadelphia: Mosby Elsevier; 2010:2585.
20. Wetmore RF, Muntz HR, McGill TJ. Pediatric Otolaryngology: Principles and Practice Pathways. 2nd ed. New York: Thieme; 2012:849-50.
21. Watkinson JC, Gilbert RW, eds. Stell & Maran’s Textbook of Head and Neck Surgery and Oncology. 5th ed. London: Hodder Arnold; 2012:222.
22. Parker KL, Clary MS, Courey MS. The endoscopic approach to a fourth branchial pouch sinus presenting in an adult. Laryngoscope 2013;123(11):2798-2800.
23. Stenquist M, Juhlin C, Aström G, Friberg U. Fourth branchial pouch sinus with recurrent deep cervical abscesses successfully treated with trichloroacetic acid cauterization. Acta Otolaryngol 2003;123(7):879-82.
24. Wong PY, Moore A, Daya H. Management of third branchial pouch anomalies—an evolution of a minimally invasive technique. Int J Pediatr Otorhinolaryngol 2014;78(3):493-8.
25. Huang YC, Peng SS, Hsu WC. KTP laser assisted endoscopic tissue fibrin glue biocauterization for congenital pyriform sinus fistula in children. Int J Pediatr Otorhinolaryngol 2016;85:115-19.
26. Takimoto T, Yoshizaki T, Ohoka H, Sakashita H. Fourth branchial pouch anomaly. J Laryngol Otol 1990;104(11):905-7.
242 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018
PAL, KUMAR, MUKHERJEE, MONDAL, BABU


Age-related changes affecting the cricoarytenoid joint seen on computed tomography
Georges Ziade, MD; Sahar Semaan, MD; Sarah Assaad, MPH; Abdul Latif Hamdan, MD, EMBA, MPH
Abstract
We conducted a retrospective chart review to compare four characteristics—cricoarytenoid joint ankylosis, narrowing, erosion, and density increases—in patients younger and older than 65 years. Our study population was made up of 100 patients, who were divided into two groups on the basis of age. The younger group (<65 yr) comprised 49 patients (27 men and 22 women), and the older group (≥65 yr) was made up of 51 patients (25 men and 26 women). Findings on computed tomography (CT) of the neck were used to determine whether each of the four characteristics was present or absent. Overall, we found only one statistically significant difference between the two groups: ankylosis was significantly more common in the older group (p = 0.036). When we looked further at the side of these anatomic changes, we found that the older group had significantly more right-sided and left-sided ankylosis than did the younger group (p = 0.026 for both), as well as significantly more left-sided narrowing (p = 0.028) (some patients had bilateral involvement). When we analyzed age as a continuous variable, older age was again associated with significantly more ankylosis (p = 0.047) and narrowing (p = 0.011). We conclude that CT can be useful for assessing radiologic changes in the cricoarytenoid joint in elderly patients during the workup of dysphonia and abnormal movement of the vocal folds.
Introduction
With age, many changes affect the laryngeal structures; among them are the cricoarytenoid joints. These diarthrodial joints are formed by the articular facets of both the cricoid and arytenoid cartilages apposed in a multiaxial form.1 In the elderly—which for the purposes of this study we defined as those aged 65 years and older—the articulation begins eroding and the perichondrium becomes thicker, which affects the precise movement of the arytenoid cartilages over the cricoid cartilage and alters the position of the vocal folds during phonation. These histologic and structural changes result in a change in voice quality.2-4
Among the different laryngeal imaging modalities, computed tomography (CT) is the best for assessing the cricoarytenoid joint. With its rapid image acquisition and low susceptibility to artifact induced by breathing and swallowing, it is considered by many to be the standard diagnostic imaging study for the evaluation of organic voice disorders.5 Modern CT scanners allow for a reconstruction of high-quality images in multiple planes and orientations, and they provide excellent spatial resolution.5
From the Department of Otolaryngology–Head and Neck Surgery (Dr. Ziade and Dr. Hamdan) and the Department of Radiology (Dr. Semaan), American University of Beirut Medical Center, Beirut, Lebanon; and the Department of Public Health and Primary Care, University of Cambridge, Cambridge, U.K. (Miss Assaad). The study described in this article was conducted at the American University of Beirut Medical Center.
Corresponding author: Abdul Latif Hamdan, MD, Department of Otolaryngology–Head and Neck Surgery, American University of Beirut Medical Center, PO Box 110236, Beirut, Lebanon. Email: ah77@aub.edu.lb
While numerous reports have been published on the acoustic changes and voice symptoms often experienced by patients with presbyphonia, we found only two studies in the English-language literature that have described CT changes in the cricoarytenoid joint brought about by aging.6,7 To the best of our knowledge, no other radiologic study has examined age-related changes affecting the cricoarytenoid joint using CT. In this article, we describe what we believe is only the third study of radiologic changes at the level of the cricoarytenoid joint as they relate to age.
Patients and methods
We retrospectively reviewed the charts of all patients who underwent CT of the neck at our medical center from July 2015 through March 2016. After excluding patients with rheumatologic disease, vocal fold paraly-
244 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018 ORIGINAL ARTICLE
sis, laryngeal lesions, and a history of laryngeal cancer, laryngeal surgery, or irradiation, our study population was made up of 100 patients.
We analyzed this population on the basis of age, using 65 years as the cutoff threshold. A total of 49 patients (27 men and 22 women) were younger than 65 years and 51 (25 men and 26 women) were aged 65 or older. There were no significant differences between the two groups in the overall number of patients in each group or the number of men and women in each group.
Axial, coronal, and sagittal CT images of the neck were obtained on a 64-slice machine (SOMATOM Sensation 64; Siemens; Erlangen, Germany). The images were displayed at a window level of 150 Hounsfield units (HU) and a width of 650 HU to optimize the evaluation of the cartilage and surrounding soft tissues. The scans were reviewed by an experienced radiologist, who made anatomic measurements at the level of the cricoarytenoid joint to determine the presence and degree of ankylosis, narrowing, erosion, and density changes.




A normal-appearing cricoarytenoid joint was defined as one with a clearly visible soft-tissue plane between the articular surface of the cricoid cartilage and the surface of the arytenoid cartilage on two or more orthogonal planes, with homogeneous density of the cartilage (figure 1).
Ankylosis was defined as a complete fusion of the joint secondary to severe joint space narrowing, which was defined as the loss of the radiolucent intercartilaginous space between the cricoid and arytenoid cartilages (figure 2). Erosion was defined as the destruction of the articular cartilage at its surface (figure 3). Finally, density changes were defined as areas of increased density, particularly calcification at the articular surface of the cricoarytenoid joint (figure 4).
These four variables were classified as either present or absent. Because the cricoarytenoid joint is a multiaxial joint and cannot be completely visualized in a single slice, the presence of any variable needed to be identified on two or more planes.
Statistical analysis. Statistical analysis was performed with the Statistical Package for the Social Sciences software (v. 23). The association between age group and each variable was examined with the chi-square test and the Fisher exact test (for expected counts <5), and p values were reported.
Further analysis was conducted to examine associations according to which side of the neck was affected. Finally, age was also studied as a continuous measure. With the age distribution significantly deviating from normality (p <0.05; Shapiro-Wilk test), the nonparametric Mann-Whitney U test was used to examine the differences in median age between the two groups in terms of whether findings were present or absent. A p value of <0.05 was considered significant.
Volume 97, Number 8 www.entjournal.com 245 AGE-RELATED CHANGES AFFECTING THE CRICOARyTENOID JOINT SEEN ON COMPUTED TOMOGRAPHy
Figure 1. CTs demonstrate a normal-appearing cricoarytenoid joint, with preserved intra-articular soft-tissue spaces seen in each plane (arrows).
Figure 3. Erosion is demonstrated as an irregularity of the articular surface and areas of hypodensity (arrows).
Figure 4. Density changes are seen as areas of significant increased density (arrows), with coarse calcification at the articular surface.
Figure 2. Joint ankylosis manifests as a loss of soft-tissue density between the cricoid and arytenoid cartilages (arrows) secondary to severe joint space narrowing, which creates areas of focal fusion.
ARBOR PRINT
ARBOR PRINT
Ethical considerations. Before the initiation of our analysis, the study protocol was approved by the Institutional Review Board of the American University at Beirut Medical Center.
Results
The prevalence of cricoarytenoid joint ankylosis was significantly higher in the older group (p = 0.036). Joint narrowing was more common in the older group, but the difference did not reach statistical significance (p = 0.112). Only a slightly greater prevalence of joint erosion and increased density was seen in the older group (table 1).
With respect to the side of diagnosis (some patients exhibited bilateral involvement), the only significant difference on the right side was the presence of ankylosis, which was more prevalent in the older group (p = 0.026). On the left side, the older group had significantly more ankylosis (p = 0.026) and narrowing (p = 0.028) (table 2).
When age was taken as a continuous variable, the mean age of patients with ankylosis and narrowing was significantly higher than the age of those in whom these variables were absent (table 3).
Discussion
The laryngeal cartilage is of the hyaline type, and its ossification process begins around the age of 20 years; it occurs secondary to the progressive replacement of the cartilaginous tissue by lamellar bone and hematopoietic tissue.3 In elderly patients, the perichondrium of the cricoid and arytenoid cartilages becomes thicker, as the formation of cartilaginous fibrillations can be seen on light microscopy.8
Furthermore, the cricoarytenoid joint exhibits erosion and roughening of its surfaces, which worsen progressively as the formation of chondrocyte clusters leads to exposure of the collagenous fibers.8-10 These changes, along with a decrease in the adherent properties of the joint capsule, affect the precise movement of the arytenoid cartilage over the cricoid cartilage, which in turn ultimately affects vocal fold movement and quality of voice.4,11
CT is frequently used for laryngeal imaging. As previously mentioned, CT changes in the cricoarytenoid joint with age were previously looked at in two studies, but both carried some limitations. 6,7 In 1982, Yeager et al published a cadaveric study of 30 adult larynges. 6 Specimens had been obtained from 16 men and 14 women, all of whom were 50 years of age or older. The authors looked at patterns of ossification in the cricoarytenoid joint on CT. Twenty-one of 32 cricoarytenoid joint specimens showed
a complete ossification of the vocal process, and 23 of 31 specimens exhibited some ossification of the arytenoid body.
As for the cricoid cartilage, their study found a difference in ossification between the inner and outer surfaces in the male donors; complete ossification was present on the inner surface in 12 specimens and on the outer surface in only 7. 6 Less ossification was seen at the level of the cricoid arch. No correlation was found between patterns of ossification and age. In addition, the pattern of ossification was more prominent on the left side than on the right, which led the authors to conclude that patterns of ossification are mainly asymmetric. No other radiologic features of the cricoarytenoid joint were looked at in this study.
A few years later, Cérat et al reported their histologic and radiologic examination of 8 cadaveric larynges using 1.5-mm contiguous CT slices.7 They described the radiologic appearances of the cricoarytenoid joints as being either radiolucent or radiopaque . In 2 cases, the cricoid and arytenoid cartilages lacked calcification and were not visible. In addition, the cricoarytenoid joint could not be assessed in 3 other cases because the cartilages had not mineralized enough. In the 3 remaining cases, the cricoarytenoid joint was either radiolucent or radiopaque whenever the cricoid and arytenoid cartilages were overlapping.
248 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018
ZIADE, SEMAAN, ASSAAD, HAMDAN
n (%) Variable <65 yr (n = 49) ≥65 yr (n = 51) p Value Sex 0.543 Male 27 (55.1) 25 (49.0) Female 22 (44.9) 26 (51.0) Ankylosis 0.036 Present 4 (8.2) 12 (23.5) Absent 45 (91.8) 39 (76.5) Narrowing 0.112 Present 23 (46.9) 32 (62.7) Absent 26 (53.1) 19 (37.3) Erosion 0.488 Present 3 (6.1) 6 (11.8) Absent 46 (93.9) 45 (88.2) Increased density 0.665 Present 20 (40.8) 23 (45.1) Absent 29 (59.2) 28 (54.9)
Table 1. Distribution of sex and the four variables by age group
Table 2. Distribution of the four variables by age and to the side of diagnosis*
The Cérat study was limited because only axial views were used to assess the cricoarytenoid joints, which hindered the possibility of evaluating the joint in a three-dimensional fashion.7 Cartilage cortices are obliquely oriented and cannot be well evaluated on axial cuts. This is in addition to the limitations of their small sample size in that the radiologic evaluation of the joint was made on only 3 larynges.
Both of these studies failed to examine anatomic changes such as cricoarytenoid joint ankylosis, erosion, and soft-tissue changes. The results of our investigation indicate a significantly higher prevalence of ankylosis in our older group than in our younger group, as well as a trend toward joint narrowing in the older group. Our findings corroborate the results of histopathologic
studies performed on the aging cricoarytenoid joint in which erosion and roughening of the joint surfaces were observed.10,12
Increased ankylosis and joint narrowing can also be attributable to changes affecting the synovial membrane, which constitutes the internal lining of the joint. The synovial membrane undergoes many histopathologic changes with age, including its replacement by chondrocyte clusters and a loss or decrease in its blood capillaries, macrophages, and lymphocytes.8,12
Our study found an asymmetry in changes affecting the cricoarytenoid joint with age. Specifically, narrowing in the aged joint was statistically significant only on the left side, which is consistent with the findings of Yeager et al, who reported an increased ossification of the cartilages and joint on the left.6 Based on these findings, we concur that patterns of ossification affecting the cricoarytenoid joint are mainly asymmetric.
To the best of our knowledge, our study is the first to look at multiple radiologic parameters of the cricoarytenoid joint in association with aging. Nevertheless, it does have some limitations that might be addressed in future research projects. One is its
Volume 97, Number 8 www.entjournal.com 249 AGE-RELATED CHANGES AFFECTING THE CRICOARyTENOID JOINT SEEN ON COMPUTED TOMOGRAPHy
n (%) Variable <65 yr (n = 49) ≥65 yr (n = 51) p Value Right side Ankylosis 0.026 Present 3 (6.1) 11 (21.6) Absent 46 (93.9) 40 (78.4) Narrowing 0.112 Present 23 (46.9) 32 (62.7) Absent 26 (53.1) 19 (37.3) Erosion 0.488 Present 3 (6.1) 6 (11.8) Absent 46 (93.9) 45 (88.2) Increased density 0.718 Present 19 (38.8) 18 (35.3) Absent 30 (61.2) 33 (64.7) Left side Ankylosis 0.026 Present 3 (6.1) 11 (21.6) Absent 46 (93.9) 40 (78.4) Narrowing 0.028 Present 20 (40.8) 32 (62.7) Absent 29 (59.2) 19 (37.3) Erosion 1.00 Present 2 (4.1) 3 (5.9) Absent 47 (95.9) 48 (94.1) Increased density 0.649 Present 18 (36.7) 21 (41.2) Absent 31 (63.3) 30 (58.8)
* Some patients exhibited bilateral involvement.
Age, yr, mean ± SD Variable Present Absent p Value Ankylosis 65.5 ± 14.3 54.6 ± 18.9 0.047 Narrowing 60.2 ± 17.8 51.6 ± 18.7 0.011 Erosion 63.1 ± 23.9 55.7 ± 18.0 0.137 Increased density 57.9 ± 18.1 55.2 ± 19.0 0.497 Continued on
256
Table 3. Mean age of patients with and without the presence/absence of the four variables
page
Improved swallow outcomes after injection laryngoplasty in unilateral vocal fold immobility
Steven Zuniga, MD; Barbara Ebersole, MA, CCC-SLP; Nausheen Jamal, MD
Abstract
While the impact of injection laryngoplasty on voice outcomes in unilateral vocal fold immobility has been well characterized, there is a relative paucity of literature investigating its influence on swallow function and outcomes. We performed a retrospective chart review of patients presenting to an academic cancer center between January 2014 and January 2016 to evaluate the clinical impact of percutaneous injection laryngoplasty on reduction of aspiration risk, patient perception of swallowing, and recommended safe diet in patients with vocal fold immobility after head and neck and thoracic surgery. A consecutive sample of patients diagnosed with unilateral vocal fold immobility with patient- or clinician-identified abnormal swallow function who underwent bedside or in-office vocal fold injection was included in the study. Fiberoptic endoscopic evaluation of swallowing, Eating Assessment Tool-10 scores, Functional Oral Intake Scale scores, and patient perceptual assessment of swallow were evaluated pre- and postinjection. Twenty-one patients with newonset unilateral vocal fold immobility who underwent injection laryngoplasty were evaluated. Median Eating Assessment Tool-10 and Functional Oral Intake Scale scores postinjection were significantly improved from preinjection. Patients who initially required restricted oral diets, or were nil per os, were able to advance their diet after injection laryngoplasty. Injection laryngoplasty is a safe and effective intervention for improvement of dysphagia in patients with unilateral vocal fold immobility. A single treatment may markedly reduce or eliminate risk of aspiration and potential sequelae.
From the Department of Otolaryngology–Head and Neck Surgery, Lewis Katz School of Medicine at Temple University, Philadelphia (Dr. Zuniga, Ms. Ebersole and Dr. Jamal); and the Department of Speech Pathology (Ms. Ebersole) and Department of Surgical Oncology (Dr. Jamal), Fox Chase Cancer Center, Temple Head and Neck Institute, Temple University Health System, Philadelphia.
Corresponding author: Steven Zuniga, MD, Department of Otolaryngology, Lewis Katz School of Medicine at Temple University, 3440 N. Broad St., Kresge West #300, Philadelphia, PA 19140. Email: Steven.Zuniga@tuhs.temple.edu
Introduction
Unilateral vocal fold immobility (UVFI) is a known complication of head and neck and thoracic surgery, resulting from manipulation or transection of the recurrent laryngeal nerve (RLN).1 As a result, the ipsilateral true vocal fold may assume a paramedian or lateral position, putting the patient at risk for dysphonia, poor cough reflex, exercise intolerance, dysphagia, and aspiration.1 Videofluoroscopic swallowing studies have demonstrated aspiration rates of 23 to 53% in patients with UVFI, with loss of laryngopharyngeal motor and sensory function thought to play predominant etiologic roles.1
Several techniques have been developed to address the glottic insufficiency caused by UVFI, including voice therapy, medialization thyroplasty, arytenoid adduction, and injection laryngoplasty.1 As techniques have become more refined, data have become available demonstrating the safety and efficacy of injection laryngoplasty.2 This intervention not only bypasses a costly trip to the operating room, but it also avoids the danger of putting patients with myriad medical comorbidities under general anesthesia.3 Many studies have described the utility of injection laryngoplasty in improving voice quality in patients with UVFI, but studies solely assessing its efficacy in improving swallow outcomes have been limited.
Many of the patients in the authors’ clinical practice develop UVFI because of thoracic and head and neck cancers and/or related surgical procedures; these patients are often chronic smokers with compromised pulmonary status related to their disease or treatment, making the sequelae of aspiration potentially even more detrimental in this patient population. The aim of this study, therefore, is to evaluate the impact of injection laryngoplasty on patient swallow outcomes, including diet advancement, in patients with swallowing complaints after onset of UVFI; those requiring behavioral modifications during swallow; or those designated nil per os (NPO) because of the presence of an unsafe swallow.
We hypothesize that an improvement in subjective and objective measures of swallow function will be
250 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018 ORIGINAL ARTICLE
demonstrated in patients suffering from UVFI after medialization of the immobile true vocal fold via injection laryngoplasty.
Case report
Approval for this study was granted by the Fox Chase Cancer Center (FCCC) Institutional Review Board. A retrospective chart review was completed on all patients diagnosed with new-onset UVFI at FCCC between January 2014 and January 2016. Diagnosis was made by an otolaryngologist via flexible fiberoptic laryngoscopy, typically within 1 week of surgical insult for inpatients, or within 1 month of voice change in outpatients, who were in the interim diagnosed with locoregionally aggressive or metastatic disease.
To be included in the study, patients had to meet the following criteria: presence of UVFI associated with patient- or clinician-identified abnormal swallow function, performance of successful injection laryngoplasty, and presence of pre- and postinjection fiberoptic endoscopic evaluation of swallowing (FEES) results and Eating Assessment Tool-10 (EAT-10) scores. Patients who were lost to follow-up, who had incomplete preand postinjection survey results, and those who had received injections for voice rehabilitation only were excluded from the study.
Injection laryngoplasty was performed at bedside or in the office for inpatients and outpatients, respectively, by the same attending otolaryngologist using a percutaneous transcartilaginous (thyroid cartilage) or transmembranous (cricothyroid membrane) technique with carboxymethylcellulose (Prolaryn Gel; Merz; Raleigh, N.C.).
Circle the appropriate response.
Pre- and postinjection EAT-10 scores were assigned for all patients included in the study, as validated by Belafsky et al for patients with swallow disorders (table 1).4 Preinjection EAT-10 scores were collected immediately before injection. Postinjection EAT-10 scores were collected during the 1-month postinjection follow-up outpatient visits.
Upon receiving a diagnosis of UVFI, patients underwent FEES by a speech and language pathologist (SLP) to assess swallow dynamics, to interrogate laryngopharyngeal sensation, to investigate for the presence of aspiration or penetration, and to determine a safe diet. Functional Oral Intake Scale (FOIS) score was assigned, as described by Crary et al, based on FEES findings.5 Injection laryngoplasty was performed 1 to 7 days after the initial FEES and, immediately after injection, a repeat FEES was performed to assess for improvement in swallow and eligibility for safe diet advancement.
Statistical analysis was completed using the Statistical Package for the Social Sciences (ver. 24). Pre- and postinjection FOIS and EAT-10 data were compared with a Wilcoxon signed rank test, which is a nonparametric hypothesis test used to compare matched samples.
Results
The charts of 48 patients diagnosed with UVFI within the study period were identified, 21 of whom met the inclusion criteria. Patients excluded had incomplete pre- and postinjection diet and swallow data, were lost to follow-up, or declined intervention with injection laryngoplasty. Patient demographic data, etiology of UVFI, indication for injection laryngo -
To what extent are the following scenarios problematic for you? 0 = No problem 4 = Severe problem
*A version of the EAT-10, a 10-item self-administered instrument validated by Belafsky et al4 and used to assess subjective dysphagia complaints.
Volume 97, Number 8 www.entjournal.com 251 IMPROvED SwALLOw OUTCOMES AFTER INJECTION LARyNGOPLASTy
IN UNILATERAL vOCAL FOLD IMMOBILITy
Table 1. Eating Assessment Tool (EAT-10)*
My swallowing
0 1 2 3 4
My swallowing problem interferes with my ability to go out for meals. 0 1 2 3 4
Swallowing liquids takes extra effort. 0 1 2 3 4 4. Swallowing solids takes extra effort. 0 1 2 3 4 5. Swallowing pills takes extra effort. 0 1 2 3 4 6. Swallowing is painful. 0 1 2 3 4
The pleasure of eating is affected by my swallowing. 0 1 2 3 4 8. when I swallow, food sticks in my throat. 0 1 2 3 4 9. I cough when I eat. 0 1 2 3 4 10. Swallowing is stressful. 0 1 2 3 4 Total EAT-10
1.
problem has caused me to lose weight.
2.
3.
7.
Key: VFI = vocal fold immobility
plasty, and injection material used were similar in all included patients (table 2).
The mean patient age at the time of diagnosis of UVFI was 65 years (±11 years). Eleven men and 10 women comprised the study cohort. Ninety percent of patients suffered left-sided UVFI. Table 2 outlines the distribution of etiologies for UVFI, the majority being the result of iatrogenic surgical injury or malignant invasion by local or metastatic malignancy.
The indication for injection for all patients in the study was dysphagia with or without dysphonia. FEES was performed by an experienced SLP to determine aspiration risk and safe oral diet based on FOIS scoring. One of 21 patients was made strictly NPO before injection laryngoplasty (FOIS score 1); the remainder tolerated a regular diet or were required to adhere to behavioral modifications with oral intake (FOIS scores 5 to 7) (tables 3 and 4).
All 8 patients who initially required restricted diets (FOIS score 5) were able to advance to a regular diet without the use of behavioral modifications (FOIS score 7). The 1 patient who was NPO before injection (FOIS score 1) was able to safely tolerate a PO diet with behavioral modification after injection laryngoplasty (FOIS 5) (table 4). The remaining 12 patients did not require dietary modification preinjection, but they did experience subjective dysphagia, as demonstrated by their abnormal EAT-10 scores.
A statistically significant difference was observed between patients’ pre- and postinjection FOIS and EAT-10 scores, with improvement noted after injection ( p = 0.004 and p = 0.04, respectively) (tables 5 and 6).
Discussion
Several studies have demonstrated that injection laryngoplasty improves subjective and objective measures of voice, including scores on the voice-related quality of life (VRQOL); the Grade of Dysphonia, Roughness, Breathiness, Asthenia, Strain (GRBAS) scale; and maximum phonation time (MPT).6
Although the benefits of injection laryngoplasty regarding improvement of vocal quality have been well studied, the specific contribution that medialization procedures may have on improvement of swallow function has been less thoroughly evaluated. The aim of this study, therefore, was to evaluate objective and subjective measures of swallow before and after intervention with injection laryngoplasty in patients newly diagnosed with UVFI to determine potential benefits to swallow function.
Although the incidence of penetration and aspiration events in patients with UVFI varies considerably in the literature, the general consensus is that these patients are at heightened risk for dysphagia and aspiration.7 Previous investigations have reported that approximately 60% of patients with UVFI complain of dysphagia, which may represent a wide range of swallow impairment, from no objective impairment to gross aspiration.7 The most potentially devastating consequence of UVFI is aspiration-related pulmonary sequelae; thus, prompt identification and evaluation is prudent.
Many of the patients in our cohort developed UVFI as a result of a thoracic surgical procedure. Patients who undergo thoracic surgery often possess compromised pulmonary status and decreased pulmonary reserve because of disease, treatment, or other medical comorbidities, making the sequelae of aspiration potentially more detrimental in this patient population,
*Regular diet: Patient able to safely tolerate regular solids and thin liquids without behavioral modifications (i.e., chin tuck, head turn, etc.).
†Thickened diet: Refers to a diet allowing for thickened liquids (no thin liquids).
Key: NPO = nil per os.
252 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018 ZUNIGA,
JAMAL
EBERSOLE,
Demographic n (%) Sex Male 11 (52) Female 10 (48) Side of vFI Left 19 (90) Right 2 (10) Etiology of vFI Thoracic malignancy 9 (43) Thoracic surgery 6 (29) Metastases 3 (14) Idiopathic 3 (14)
Table 2. Patient demographics (N = 21)
Preinjection Postinjection Diet n (%) (%) NPO 1 (5) 0 (0) Regular diet* 12 (57) 20 (95) Regular diet with behavioral modifications 7 (33) 0 (0) Thickened diet† 1 (5) 1 (5)
Table 3. Pre- and postinjection diet of study participants (N = 21)
The BEACON Advanced Energy Laser combines our industry-leading Enhanced Safety Fibers with free beam energy delivery, giving you the versatility to choose.
System Features:

Versatile: Industry-leading enhanced safety fibers + Line of Sight (LOS) capabilities.
Easy-to-Use: OR workflow inspired user interface with smartphone like navigation.
Built for Performance: Innovative design ensures mobility with integrity. Multiple laser modes enable desired tissue interaction.

OmniGuide’s polymer-based Enhanced Safety Fibers feature multiple layers of highly reflective mirrors, which efficiently transmit laser energy the length of the fiber.

Visit www.omni-guide.com/beacon or call 888.666.4484 for

for
co2
delivery.
MaxiMuM versatility
precise
energy
© 2018 OmniGuide, Inc. All rights reserved. 1-0168-074-00-00 rev.0
additional information.
*FOIS Scale is described as: (1) nil per os; (2) tube-dependent with minimal per oral (PO) intake; (3) tube-dependent with consistent PO intake; (4) total PO diet of single consistency; (5) total PO diet of multiple consistencies but requiring special preparation/compensation; (6) total PO diet without special preparation/compensation but with specific food limitation; (7) total PO diet with no limitations.
as well as in chronic smokers with head and neck cancer. The need for alternate enteral access in those with an unsafe swallow also produces a detriment to patient quality of life and levies a psychological burden on patients already suffering from other serious disease processes. 8
FEES was the investigative modality of choice to interrogate swallow function in our patient population. Videofluoroscopic examination of swallow (VFS) has long been considered the “gold standard” in assessment of pharyngeal swallow function; however, several studies have demonstrated numerous advantages afforded by FEES over VFS.9–11 Specifically, Langmore et al showed an acceptable level of sensitivity, specificity, positive predictive value, and negative predictive value in identifying aspiration, penetration, bolus residue, and spillage during FEES compared with the results
of the VFS study done on the same individuals.9 The increasingly ubiquitous availability of this technology in clinical practice combined with the expanding cohort of clinicians becoming facile with both the administration and interpretation of this modality makes it a reliable and generalizable diagnostic technique.
The FOIS allows quantitative description of diet advancement after injection laryngoplasty. All patients in our study who were initially prescribed a restricted diet due to their UVFI were able to have their diet advanced immediately after injection laryngoplasty. This improvement in FOIS scores from pre- to postinjection was statistically significant (table 5), supporting an improvement in swallow safety after injection laryngoplasty. Graboyes et al demonstrated similar findings in their series of 20 patients in which 90% of their cohort were recommended for strict NPO before injection. Of these, 94% were allowed an oral diet and 67% tolerated a regular diet after injection.12
Given the relatively high rate of subjective reports of dysphagia in UVFI, the EAT-10 instrument was used to measure changes in patient perception of swallow. EAT-10 was validated by Belafsky et al in a group of patients with known reflux, voice disorders, oropharyngeal dysphagia, head and neck cancer, or esophageal dysphagia, with dysphagia etiologies ranging from neurologic disease to esophageal webs and stricture.4
In the current patient population, a statistically significant improvement was demonstrated when comparing pre- and postinjection EAT-10 scores (table 6), supporting improvement in patient perception of swallow, even in the absence of the need for dietary modification. The degree of improvement represents a meaningful benefit, as dysphagia is a well-documented detriment to quality of life.13
Cates et al demonstrated similar findings to ours in their evaluation of 44 patients who underwent either injection laryngoplasty or medialization thyroplasty for UVFI, demonstrating a durable and statistically significant improvement in EAT-10 after the medializa-
*FOIS Scale is described as: (1) Nil per os; (2) Tube-dependent with minimal per oral (PO) intake; (3) Tube-dependent with consistent PO intake; (4) Total PO diet of single consistency; (5) Total PO diet of multiple consistencies but requiring special preparation/compensation; (6) Total PO diet without special preparation/compensation but with specific food limitation; (7) Total PO diet with no limitations.
†p = 0.004; Wilcoxon paired samples test was used to calculate p value for the median change before and after injection
Key: IL = injection laryngoplasty.
254 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018 ZUNIGA, EBERSOLE, JAMAL
Patient no. Preinjection FOIS score Postinjection FOIS score 1 5 7 2 5 7 3 1 5 4 5 7 5 5 7 6 5 7 7 5 7 8 5 7 9 5 7
Table 4. Functional Oral Intake Scale (FOIS)* scores pre- and postinjection for patients who required preinjection diet modification
Minimum Maximum Mean Median FOIS score Pre-IL 1 5 4.56 (±1.33) 5 FOIS score Post-IL 5 7 6.78 (±0.67) 7 Change in FOIS score 2 4 2.22 (±0.67) 2†
Table 5. Functional Oral Intake Scale (FOIS)* scores pre- and postinjection for patients requiring preinjection diet modification
tion procedure.13 In contrast to our study, however, the Cates study does not report objective measures of diet advancement or behavioral diet modifications before or after surgical intervention.
Although intact motor and sensory function is clearly necessary to mediate the complex sequence of events during swallow, the individual contribution and importance of these unique motor and sensory mechanisms is difficult to elucidate. Improvement in glottic valving likely plays a role in improving intrabolus pressure generation, and these mechanisms in combination may reduce aspiration while increasing bolus clearance.14
Bhattacharyya et al evaluated swallow impairment in patients with UVFI via VFS and noted laryngeal penetration during and after swallow due to bolus residue in the pharynx.7 They postulated that an incompetent glottic valve may impair the necessary negative hypopharyngeal pump pressure needed to propel the bolus through the pharynx, thus predisposing the patient to aspiration.7 However, although glottal competence is paramount to swallow safety during deglutition, intact sensory function is essential for the coordination of events during the swallow, as well as to elicit reflex clearance of materials from the hypopharynx, larynx, and trachea.1 Further, other biomechanical factors, including pharyngeal strength and upper esophageal sphincter opening, have been demonstrated to significantly influence swallow efficiency.
Nayak et al investigated patterns of failure after medialization procedures for UVFI, suggesting that pharyngeal transport defects and bolus residue in persistent penetration or aspiration play leading roles in failure, despite glottic competence.15 Domer et al demonstrated significantly prolonged pharyngeal transit time and decreased pharyngeal strength in patients with UVFI, thus supporting the notion that mechanical factors other than glottal competence contribute to the increased incidence of penetration and aspiration in this patient population.16
Because swallowing is a complex, multistep process that requires various motor and sensory inputs, swallow outcomes after medialization procedures in patients with UVFI have yielded diverse results. The findings of our study suggest a greater derived benefit than in
several prior studies. The greater benefit realized in our study may be explained by isolated unilateral RLN injury as the etiology of UVFI in patients included in our cohort, in contrast to similar studies, which have included patients with UVFI resulting from radiation, cerebrovascular accident, skull base pathology, or central nervous system dysfunction.2,7,17-19
Patients suffering from multiple cranial neuropathies or central nervous system dysfunction may receive less benefit from medialization procedures given multiple levels of laryngeal dysfunction.16 Despite the etiologic homogeneity of our study population, our findings remain pertinent as surgical trauma to the RLN is the most commonly cited etiology of UVFI.16
Interestingly, 57% of patients in our study did not have aspiration associated with their dysphagia. Why some patients experience aspiration with UVFI while others do not also remains poorly understood. The authors suspect that baseline swallowing efficiency, degree of glottic closure post-UVFI development, impaired laryngeal sensation, and pulmonary status likely play a role. Further research is required to better understand the risk factors for developing aspiration after UVFI.
Our study has several methodologic limitations. The limitations inherent to any retrospective study are present in this study, including incomplete follow-up data in many patients. To compensate, we designed our study with rigid inclusion criteria to optimize the accuracy and integrity of the presented data. As a result, however, of the 48 patients diagnosed with UVFI during the study period, only 21 patients had complete data for objective and subjective swallow outcomes for pre- and postinjection laryngoplasty.
Unfortunately, as all patients included had head and neck or thoracic cancer, a considerable number of patients were unable to complete adequate follow-up because of disease progression, disability, or death. As a result, small sample size was another weakness of our study. Our study also did not feature a control group to which we might have compared swallow outcomes. Finally, a selection bias may also be present in that patients included suffered from significant swallow detriment due to their UVFI and were thus more likely to desire treatment.
Volume 97, Number 8 www.entjournal.com 255 IMPROvED SwALLOw OUTCOMES AFTER INJECTION LARyNGOPLASTy IN UNILATERAL vOCAL FOLD IMMOBILITy
Minimum Maximum Mean Median EAT-10 score before IL 0 30 8.62 (±8.78) 5 EAT-10 score after IL 0 15 3.86 (±4.50) 2 Change in EAT-10 score –25 8 –4.76 (±8.21) –2*
Table 6. Eating Assessment Tool-10 scores pre- and postinjection laryngoplasty
* p = 0.04; Wilcoxon paired samples test was used to calculate p value for the median change before and after injection laryngoplasty.
Key: EAT-10 = Eating Assessment Tool-10, IL = injection laryngoplasty.
References
1. Tabaee A, Murry T, Zschommler A, Desloge RB. Flexible endoscopic evaluation of swallowing with sensory testing in patients with unilateral vocal fold immobility: Incidence and pathophysiology of aspiration. Laryngoscope 2005;115(4):565-9.
2. Anderson TD, Mirza N. Immediate percutaneous medialization for acute vocal fold immobility with aspiration. Laryngoscope 2001;111(8):1318-21.
3. Mathison CC, Villari CR, Klein AM, Johns MM. Comparison of outcomes and complications between awake and asleep injection laryngoplasty: A case-control study. Laryngoscope 2009;119(7):1417-23.
4. Belafsky PC, Mouadeb DA, Rees CJ, et al. Validity and reliability of the Eating Assessment Tool (EAT-10). Ann Otol Rhinol Laryngol 2008;117(12):919-24.
5. Crary MA, Mann GD, Groher ME. Initial psychometric assessment of a functional oral intake scale for dysphagia in stroke patients. Arch Phys Med Rehabil 2005;86(8):1516-20.
6. Chhetri DK, Jamal N. Percutaneous injection laryngoplasty. Laryngoscope 2014;124(3):742-5.
7. Bhattacharyya N, Kotz T, Shapiro J. Dysphagia and aspiration with unilateral vocal cord immobility: Incidence, characterization, and response to surgical treatment. Ann Otol Rhinol Laryngol 2002;111(8):672-9.
8. Mayre-Chilton KM, Talwar BP, Goff LM. Different experiences and perspectives between head and neck cancer patients and their care-givers on their daily impact of a gastrostomy tube. J Hum Nutr Diet 2011;24(5):449-59.
9. Langmore SE, Schatz K, Olson N. Endoscopic and videofluoroscopic evaluations of swallowing and aspiration. Ann Otol Rhinol Laryngol 1991;100(8):678-81.
10. Rao N, Brady S, Chaudhuri G, et al. Gold-standard? Analysis of the videofluoroscopic and fiberoptic endoscopic swallow examinations. 2003. https://www.scienceopen.com/ document?vid=4ab613e2-80f7-4a6a-aca5-c709660b6e72. Accessed March 13, 2017.
11. Hiss SG, Postma GN. Fiberoptic endoscopic evaluation of swallowing. Laryngoscope 2003;113(8):1386-93.
12. Graboyes EM, Bradley JP, Meyers BF, Nussenbaum B. Efficacy and safety of acute injection laryngoplasty for vocal cord paralysis following thoracic surgery. Laryngoscope 2011;121(11):2406-10.
13. Cates DJ, Venkatesan NN, Strong B, et al. Effect of vocal fold medialization on dysphagia in patients with unilateral vocal fold immobility. Otolaryngol Head Neck Surg 2016;155(3):454-7.
14. Ruddy BH, Pitts TE, Lehman J, et al. Improved voluntary cough immediately following office-based vocal fold medialization injections. Laryngoscope 2014;124(7):1645-7.
15. Nayak VK, Bhattacharyya N, Kotz T, Shapiro J. Patterns of swallowing failure following medialization in unilateral vocal fold immobility. Laryngoscope 2002;112(10):1840-4.
16. Domer AS, Leonard R, Belafsky PC. Pharyngeal weakness and upper esophageal sphincter opening in patients with unilateral vocal fold immobility. Laryngoscope 2014;124(10):2371-4.
17. Heitmiller RF, Tseng E, Jones B. Prevalence of aspiration and laryngeal penetration in patients with unilateral vocal fold motion impairment. Dysphagia 2000;15(4):184-7.
18. Carrau RL, Pou A, Eibling DE, et al. Laryngeal framework surgery for the management of aspiration. Head Neck 1999;21(2):139-45.
19. Flint PW, Purcell LL, Cummings CW. Pathophysiology and indications for medialization thyroplasty in patients with dysphagia and aspiration. Otolaryngol Head Neck Surg 1997;116(3):349-54.
Continued from page 249
retrospective nature, which limited our ability to acquire information on our patients’ phonatory behavior, voice quality, and endoscopic laryngeal findings. Another is the absence of indirect laryngeal examination, which would have been of value in excluding other possible laryngeal pathologies such as vocal fold paresis and in allowing us to draw other conclusions of possible clinical significance.
In conclusion, ankylosis and narrowing of the cricoarytenoid joint are commonly observed with aging. CT can be used to measure these changes and assist in the workup of elderly patients with dysphonia and abnormal vocal fold movement disorders.
References
1. Logeman JA. Upper digestive tract anatomy and physiology. In: Bailey BJ, Johnson JT, Newlands SD, eds. Head & Neck Surgery–Otolaryngology. 4th ed. Philadelphia: Lippincott Williams & Wilkins; 2006.
2. Sasaki C, Kim Y. Anatomy and physiology of the larynx. In: Snow JB, Ballenger JJ, eds. Ballenger’s Otorhinolaryngology: Head and Neck Surgery. 16th ed. Hamilton, Ont.: B.C. Decker; 2003:1090.
3. Sakai F, Gamsu G, Dillon WP, et al. MR imaging of the larynx at 1.5 T. J Comput Assist Tomogr 1990;14(1):60-71.
4. Segre R. Senescence of the voice. Eye Ear Nose Throat Mon 1971;50(6):223-7.
5. Huang BY, Solle M, Weissler MC. Larynx: Anatomic imaging for diagnosis and management. Otolaryngol Clin North Am 2012;45(6):1325-61.
6. Yeager VL, Lawson C, Archer CR. Ossification of the laryngeal cartilages as it relates to computed tomography. Invest Radiol 1982;17(1):11-19.
7. Cérat J, Charlin B, Brazeau-Lamontagne L, Mongeau CJ. Assessment of the cricoarytenoid joint: High-resolution CT scan study with histo-anatomical correlation. J Otolaryngol 1988;17(2):65-7.
8. Meller SM. Functional anatomy of the larynx. Otolaryngol Clin North Am 1984;17(1):3-12.
9. Sellars I, Sellars S. Cricoarytenoid joint structure and function. J Laryngol Otol 1983;97(11):1027-34.
10. Paulsen FP, Tillmann BN. Degenerative changes in the human cricoarytenoid joint. Arch Otolaryngol Head Neck Surg 1998;124(8):903-6.
11. Dedivitis RA, Abrahão M, de Jesus Simões M, et al. Cricoarytenoid joint: Histological changes during aging. Sao Paulo Med J 2001;119(2):89-90.
12. Kawamoto-Hirano A, Honkura Y, Shibata S, et al. Cricoarytenoid articulation in elderly Japanese with special reference to morphology of the synovial tissue. Ann Otol Rhinol Laryngol 2016;125(3):219-27.
256 www.entjournal.com ENT-Ear, Nose & Throat Journal August 2018
ZUNIGA, EBERSOLE, JAMAL ZIADE, SEMAAN, ASSAAD, HAMDAN














































SMART is Better TRANSFORM YOUR PRACTICE WITH ARTIFICIAL INTELLIGENCE Our Advantage SMART Practice™ suite of All-in-One Solutions use real-time data from your clinic to optimize efficiency, improve outcomes, and increase revenue. EHR | PM | RCM | ASC ANALYTICS | PATIENT ENGAGEMENT TELEHEALTH | 2015 ONC CERTIFIED ENT SPECIFIC EHR & PM Leader for 33 Years Request a demo TODAY www.compulinkadvantage.com/ENTEHR | 800.456.4522
The #1 Doctor Recommended Earplug Brand to get a good night’s sleep with a snoring spouse.*



“Mack’s® Earplugs saved our marriage.”
*Business Research Group, February 2014.
Tammy
& Tim Paczkowski Richmond, MN