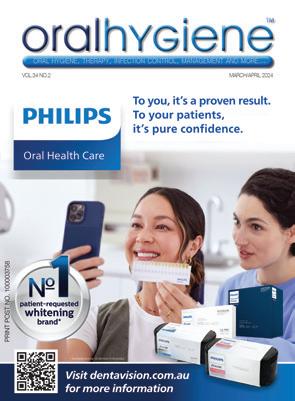
Oral Health Care


patient-requested whitening brand*




VOL.34 NO.2 MARCH/APRIL 2024 oral hygiene , therapy , infection control , management and more ...
PRINT POST NO. 100003758




FIRST CLASS IN EFFECTIVENESS AND TASTE
• Effective – quick desensitisation and fluoride release (5 % NaF ≙ 22,600 ppm)
• Excellent handling – moisture tolerant
• Aesthetic – tooth-shaded varnish
• Universal – available in tube version, SingleDose and cartridge
• Variety of flavours – mint, caramel, melon, cherry, bubble gum, cola lime and pina colada
Contact your VOCO Dental Consultant: VIC + TAS: Peter Kenda, Tel. 0409 390 194 | QLD: David Reyno, Tel. 0401 747 037 | NSW (North): Katrina Johnston, Tel. 0434 491 399 | NSW (South) & ACT: Buddy Ishak, Tel. 0438 065 400 | WA + SA + NT: Ronald Bangma, Tel. 0419 823 325






• B U M • • CHE Y •
Profluorid® Varnish VOCO GmbH · Anton-Flettner-Straße 1-3 · 27472 Cuxhaven · Germany · Freecall 00 800 44 444 555 · www.voco.dental
VOCO
On the cover...
Dentavision is now the preferred and only dental professional distribution partner for the Philips Zoom! professional teeth whitening range and Philips Sonicare oral care products in Australia.
Tabitha Acret looks
gender equality and the challenges faced by working mothers in particular


Catherine Pawloski and Dr Marie Fluent look at the advantages of using instrument cassettes in your practice




Yes! explains Prof. Laurie Walsh
Many components of infection prevention and control relates to what can be called “the problems of pipes” explains Prof. Laurie Walsh

Know your role in recognising and healing supervised neglect related to burnished calculus says Tami Wanless facebook.com/auxiliarynow twitter.com/auxiliarynow instagram.com/dentevents

Publisher & Editor: Joseph Allbeury
www.oralhygiene.com.au
Cammeray 2062
Oral Hygiene (formerly Auxiliary) ISSN 1323-4919 is printed in Australia and published six
per year by Main Street Publishing P/L ABN 74 065 490 655 • PO Box 586,
Telephone: (02) 9929-1900 Facsimile: (02) 9929-1999 Email:
© 2024. All rights reserved. The contents of this magazine are copyright and must not be reproduced without the written permission of the publisher. Permission to reprint may be obtained upon application. Correspondence and manuscripts for publication are welcome. Although all care is taken, the editor and publisher will not accept responsibility for the opinions expressed by contributors to this magazine, or for loss or damage to material submitted for publication. OH | CONTENTS Annual Subscriptions: Australia or NZ: OralHygiene $22.00 p.a. Overseas: A$38.00 p.a. Australasian Dental Practice (including OralHygiene) $99.00p.a. SUBSCRIBE ONLINE at http://shop.dentalpractice.com.au 4 BRIEFS 6 NEWS & EVENTS 16 CPD CENTRE 20 ABSTRACTS 12 CAN WE HAVE IT ALL?
times
info@dentist.com.au
at
14 TRAYS VS CASSETTES: CONSIDERATIONS WHEN PROCESSING DENTAL INSTRUMENTS
22 TOOTHPASTE
AND
FOR A RETHINK?
LABELLING
TESTING TECHNOLOGIES: TIME
26 THE PROBLEMS OF PIPES: A KEY CHALLENGE IN INFECTION PREVENTION AND
CONTROL
32 THE
MOST EFFECTIVE CALCULUS REMOVAL
READ ME FOR CPD READ ME FOR CPD
VOLUME 34 | NUMBER 2 MARCH/APRIL 2024 READ ME FOR CPD READ ME FOR CPD
New Cervitec Gel with optimized care formula
The new Cervitec Gel is recommended especially for the care of at-risk areas. The oral care gel with optimized care formula contains chlorhexidine, fluoride, xylitol and provitamin D-panthenol. With the new formula, Cervitec Gel protects the teeth, gums, peri-implant tissue and mucuous membrane with even more efficiency. Cervitec Gel supports the treatment of gingivitis, mucositis, denture stomatitis, periodontitis and peri-implantitis and helps combat elevated bacterial counts. It prevents inflammation and freshens breadth. Provitamin D-panthenol and xylitol moisturize and protect the gums and mucous membrane. Depending on the situation, the gel is applied either directly on the oral mucous membrane or removable restoration and distributed with an interdental brush or used to brush teeth. Given its smooth consistency, the clear gel can be optimally distributed on complex surfaces, e.g. implant restorations. Cervitec Gel can be applied in the dental office or at home. Cervitec Gel is widely accepted due to its mild taste. The soothing ingredients leave a pleasant feeling in the mouth. Available from Ivoclar on 1300-486-252 or visit www.ivoclar.com
3


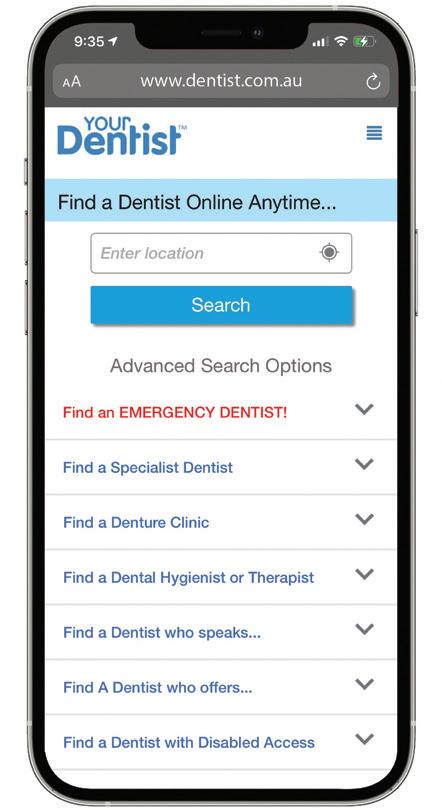
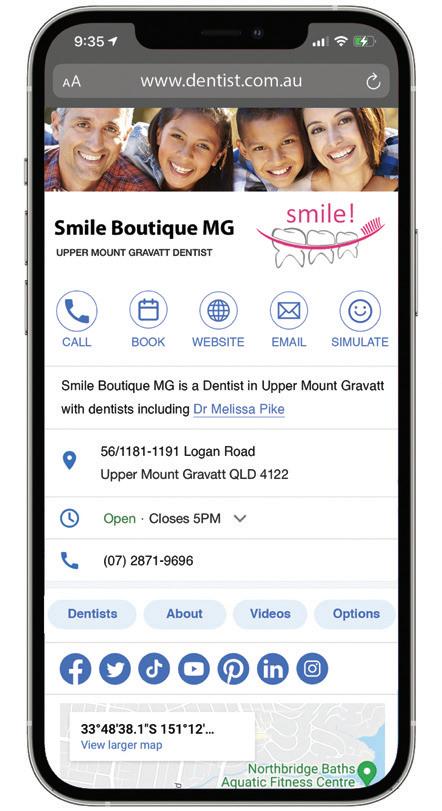
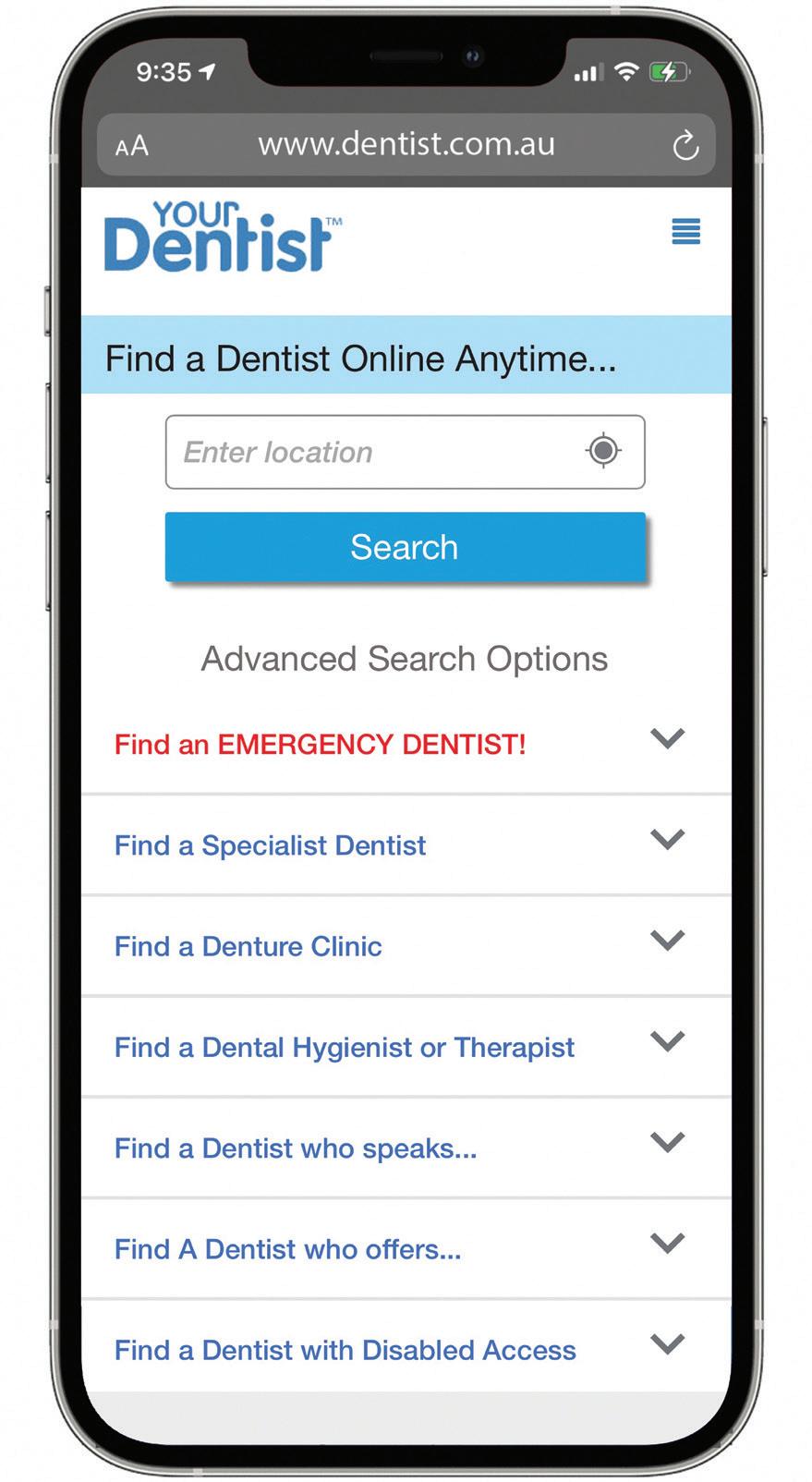
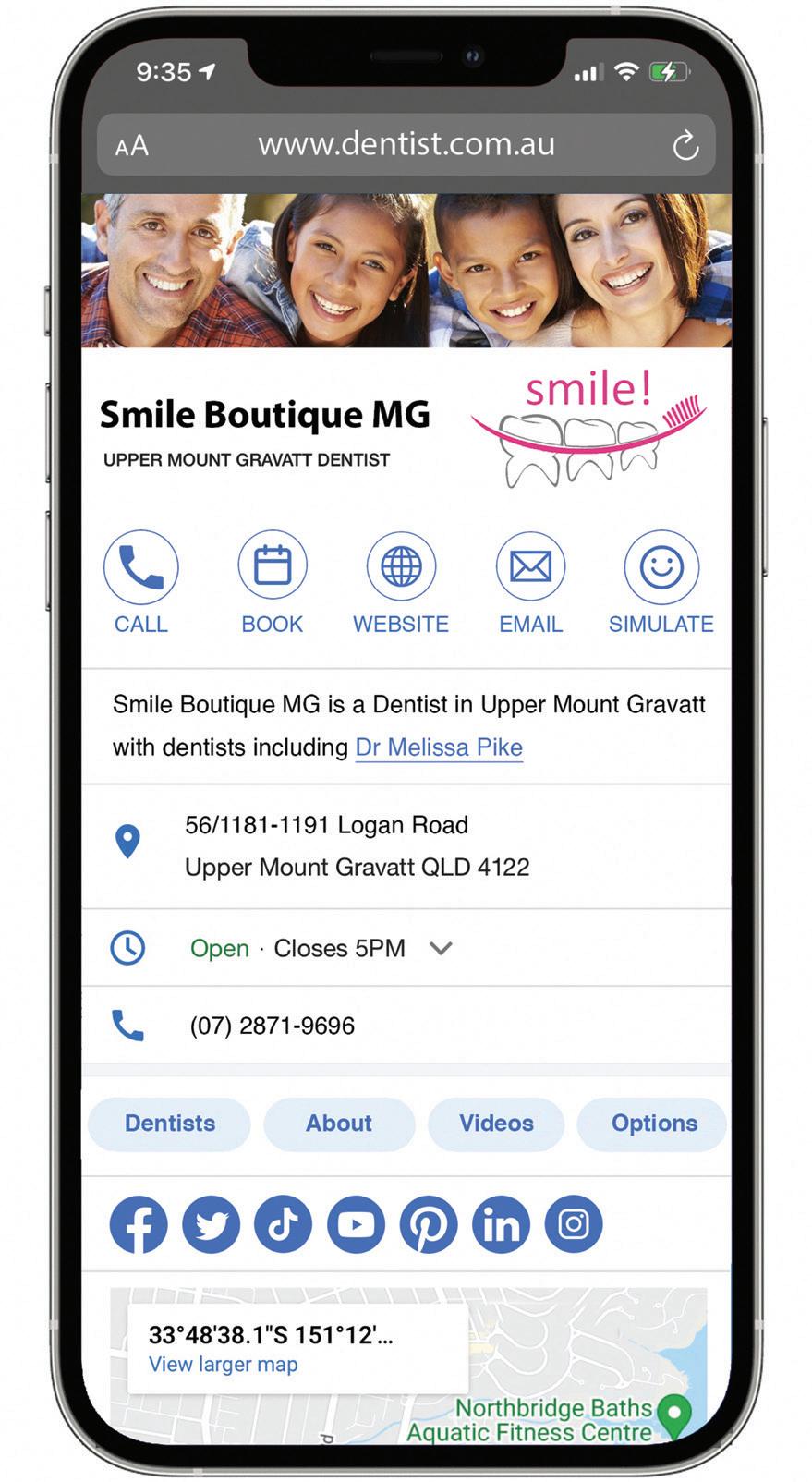
ways to get the most out of www.dentist.com.au
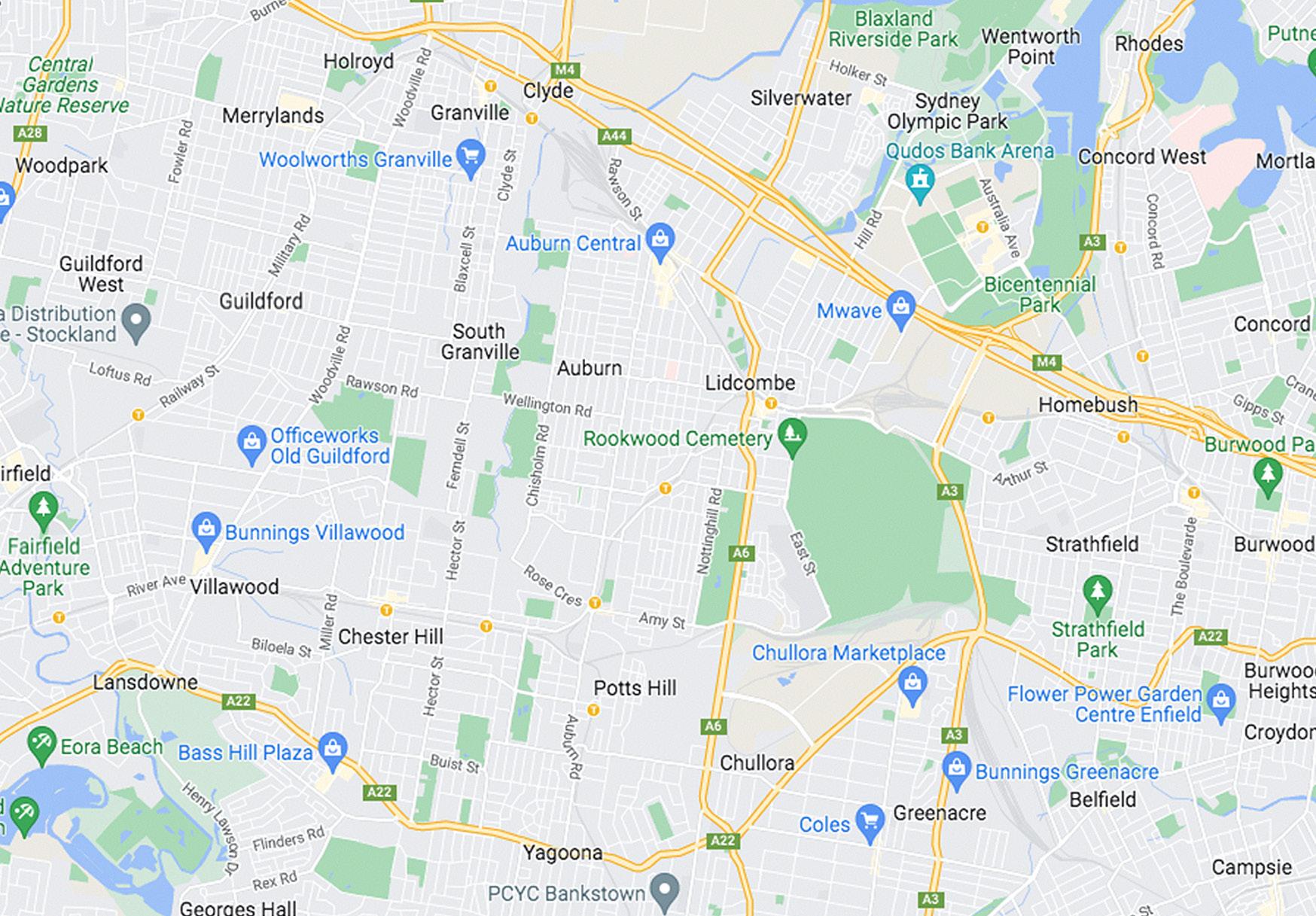
When people want to find a dentist, they mostly use the internet and Google “Dentist in...”. That’s what the research shows. Word of mouth is no longer king! Google only shows 3 or 4 individual dental practices on the first page of its search results. The other results returned are for, among other things, the website www.dentist.com.au. This directory lists all practices and practitioners and is searched a million times a year.
1 2 3
Get Listed! If you’re listed on dentist.com.au, your phone will ring! So just do it!
Upgrade your listing: Just like in Google, where your practice sits in the dentist.com.au search results list determines how often your phone rings. If you’re at the top of the list, then your phone will ring more often and if there is more detailed information listed about your practice, then this helps too. Unlike Google, you can increase your priority in searches for an annual fee. This increases your prominence in searches for your home suburb and often also in the surrounding suburbs. Plus you can add heaps of detailed information about your practice and practitioners.
Add your link for online bookings. If you accept online bookings, then once you’ve upgraded your listing, you can add the link to accept online bookings through your preferred booking engine and this will appear directly in the search results list. For details on how to upgrade, visit: dentist.com.au/information-for-dentists
During oral surgery there is a significant occupational risk of exposure to potentially harmful infectious diseases, transmitted through direct contact with body fluids and aerosolised splatters that may not be visibly detectable. Many of these exposures may be visually imperceptible. The aim of this study was to detect visually imperceptible blood contamination on personal protective equipment (PPE) and clinical working surfaces using the chemiluminescence agent luminol during oral surgical procedures. A total of 20 minor oral surgical procedures were performed. The procedures were subcategorized as aerosol-generating (surgical removal of impacted teeth) and non-aerosol generating (simple forceps extraction, intraoral incision and drainage, biopsy). Used PPE was scrutinised for traces of visually imperceptible blood contamination using luminol. The results of blood splatter on PPE and clinical surfaces were analysed. It was observed that visually imperceptible blood contamination in non-aerosol procedures was detected on the assistant’s PPE (46.7% of cases), the assistant’s face shield (40%), the suction apparatus (50%), the walls (30%) and the floor (56.7% of cases), after both aerosol-generating and non-aerosol generating procedures. The results of the study show undetected blood spillage can occur during aerosol-generating oral surgical procedures of 30 minutes and also during non-aerosol surgical procedures of more than 30 minutes. The contamination extends over an area of 1 metre horizontally and 1.6 metres vertically. These results emphasise the value of Personal Protective Equipment, especially the use of face shields, while performing oral surgical procedures in order to prevent cross infection. The results also stress the need for proper environmental cleaning of working surfaces in a consistent way after all procedures.
4 oral|hygiene March/April 2024
news | EVENTS
in | BRIEF
easiest dental marketing you will ever do!
1 million visitors a year...
9,675 dental practices...
27,690 clinicians... And counting... Get listed today!

GET LISTED
The
™ www.dentist.com.au SCAN to Add or Update Your Practice

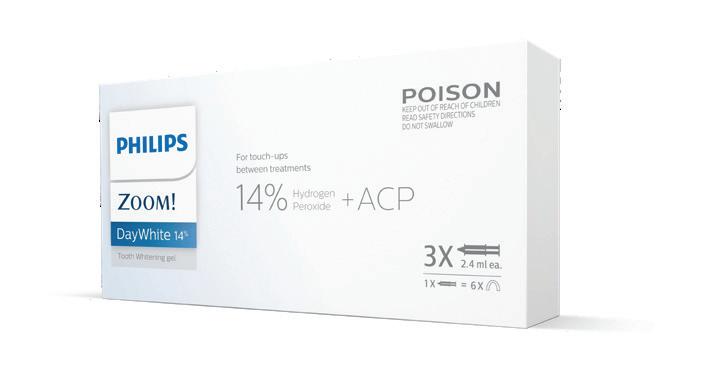
Philips appoints Dentavision as preferred oral healthcare distribution partner in Australia
Philips has announced it’s changing supply arrangements for the Philips Zoom! professional teeth whitening range and Philips Sonicare oral care products in Australia, appointing Dentavision as its preferred and only dental professional distribution partner.
The appointment of Dentavision, who will be the only distributor of Philips Zoom! in the market, will provide dental practices across the country with easier access to Philips’ market leading range of oral healthcare solutions.
“Dentavision is the perfect partner for Philips in Australia, with its marketleading position and extensive industry expertise,” said Simon Amor, Country Lead, Personal Health, Philips Australia. “Dentavision’s ethos also reflects Philips purpose, with patient-centric priorities of improving people’s health and well-being. Our partnership will expand access in Australia to Philips Zoom!, the #1 patient-
requested professional whitening brand,1 as well as Philips Sonicare power toothbrushes and power interdental products.”
“Dentavision are thrilled to announce our collaboration with Philips to deliver cutting-edge products to dental professionals in Australia,” said David Macnaughtan, Managing Director, Dentavision. “Philips’ industry leading range, coupled with Dentavision’s unparalleled sales and service team and product portfolio make us perfect partners for the journey ahead. Dentavision has a nationwide sales team that has extensive experience in training, education, marketing and supply of products and solutions for dental practices.”
The products
Philips’ flagship Zoom! WhiteSpeed in-chair system utilises advanced blue LED light-technology to accelerate the whitening process. In 45 minutes, teeth can be up to 8 shades whiter,2 reversing stains from food and drinks, ageing and even discolouration from some medications. Philips Zoom! DayWhite and NiteWhite complete the range with take home options in 6%, 9.5% and 14%
hydrogen peroxide and 10%, 16% and 22% carbamide peroxide respectively.
Philips Sonicare range of electric toothbrushes pulse fluid between the teeth and along the gum line while 62,000 brush strokes per minute gently and effectively remove plaque. The Sonicare range includes the Sonicare 9900 Prestige, Sonicare DiamondClean 9000, ExpertClean 7300, ProtectiveClean, Sonicare 3100 Series, Sonicare 2100 Series and Philips Sonicare For Kids.
Complementing these, the Sonicare Power Flosser range features a unique X-shaped nozzle that creates 4 streams for up to 99.9% plaque removal.3 The Quad Stream covers more area and requires less technique than a single stream nozzle, for fast and effective flossing.
1. Surveyed among 50 dentists in Australia.
2. Excludes preparation time. Research conducted in the US using 25% HP Zoom! Kit.
3. In an in-vitro study, actual results may vary.
For info visit www.philips.com.au/zoom
Dental practices can place orders for Philips products with Dentavision immediately. Call 1800-806-640 or visit www.dentavision.com.au

6 oral|hygiene March/April 2024 news | EVENTS
Oral Health Care


patient-requested whitening brand*




March/April 2024
Transform your dental practice with the Ultimate DIY Dental Marketing Pack
Let’s face it, the dental industry is bustling with competition and standing out is tougher than ever. But what if I told you that skyrocketing your practice’s visibility and attracting new patients could be both simple and cost-effective?
ENTER: The Ultimate DIY Dental Marketing Pack - your game-changer in navigating these challenging times.
Why you’ll love this marketing pack
Created by Angus Pryor and his dedicated team at Dental Marketing Solutions, after more than 10,000 hours of hands-on consulting with dental practices just like yours, this pack is more than a set of tools; it’s the secret ingredient to your practice’s success story. Incredible value for your investment: Imagine getting a treasure chest worth $8,080 for just $997. This is an amazing 88% off the original value!
Visit www.diy-marketing.com.au now
What’s Inside?
n 12-Month Marketing Calendar: Keep your marketing efforts focused and organised with themes, promotional activities and key dates so you always know what to do and when. $500 VALUE
n Social Media Mastery: With 24 professional social media templates (in Canva) and a library of customisable captions, you have literally hundreds of social media posts that will captivate and engage. $2400 VALUE
n Patient Engagement Emails: 24 professionally-written emails designed to keep your patients informed and interested, potentially unlocking thousands in additional revenue. $2400 VALUE


n Online Visibility Boost: Enjoy enhanced visibility on Dentist.com. au, ensuring your practice stands out strongly in Google especially in surrounding suburbs. $795 VALUE
n Effortless Tracking: An automated reminder system keeps your marketing efforts on track without the added stress. $360 VALUE
n Exclusive One-Off Bonuses: Enjoy a Google Business Profile Checklist, a 12-Point Website Self-Audit, a competitor audit and more. These bonuses are here to give you an edge over the competition. $1725 VALUE
Ready for a marketing revolution?
I magine having more time to focus on what you do best – providing top-notch dental care, while we handle the nitty-
gritty of marketing.
With The Ultimate DIY Dental Marketing Pack, you’re not just purchasing a product; you’re unlocking the full potential of your dental practice. This is your moment to shine, to stand out and to grow in ways you’ve never imagined.
Take the first step
Feeling excited? We are too! For one low price, packed with heaps of value, discover how the Ultimate DIY Dental Marketing Pack can revolutionise your practice. Remember, great marketing is the key to unlocking a floodgate of patients waiting to discover your practice. Embrace this opportunity to secure a bright and prosperous future for your dental practice.
Sign up at https://diy-marketing.com.au
8 oral|hygiene March/April 2024 news | EVENTS
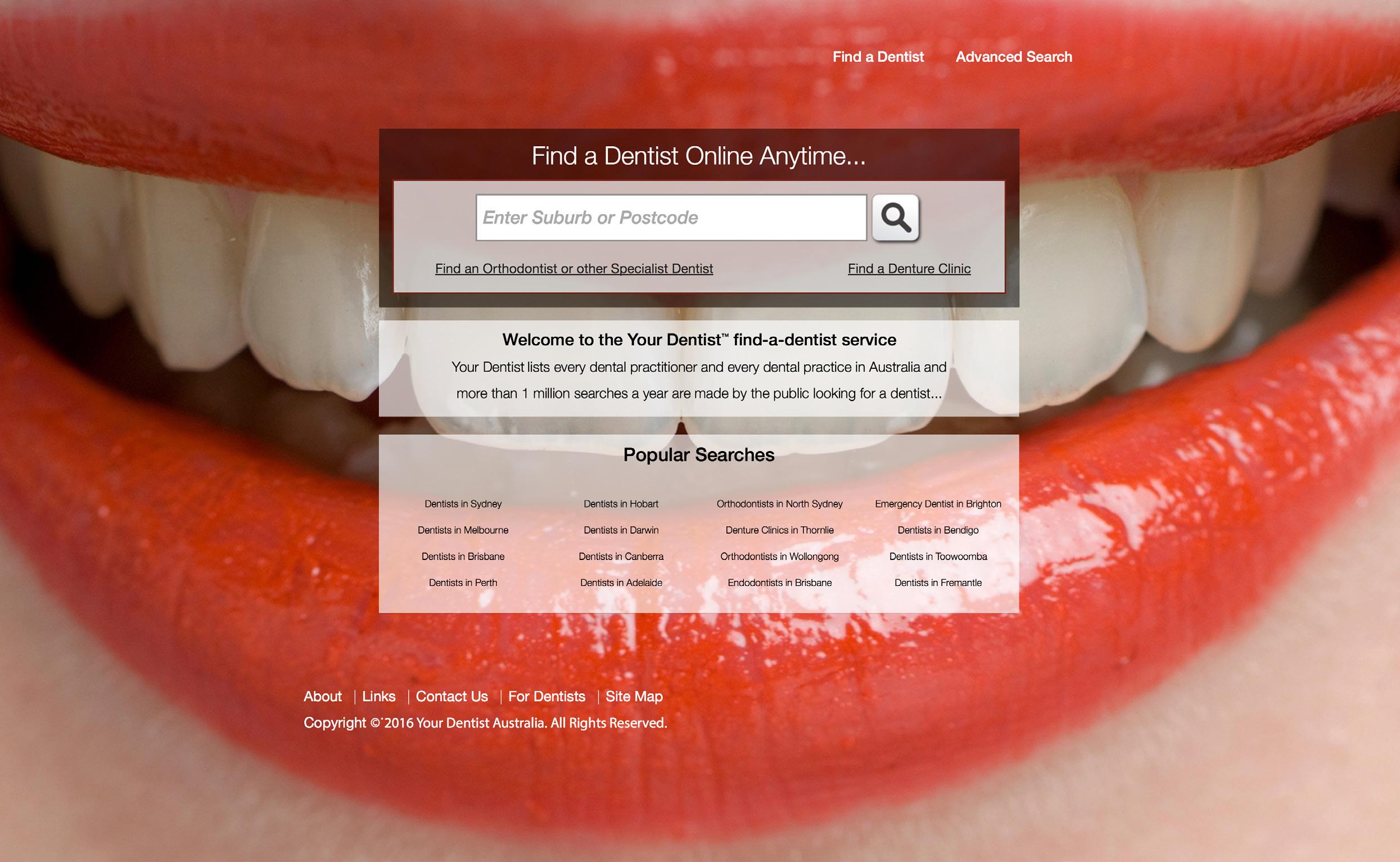
n Australia and New Zealand have over 25,000 dental practitioners
n dentist.com.au and dentist.co.nz lists every practitioner free of charge
n For 20 years, the Australian public has relied on www.dentist.com.au to find and connect with you. Now we have introduced the service to New Zealand
n Over 1 million searches are made every year
n Visit dentist.com.au or dentist.co.nz to check your details are correct
n Visit www.dentalcommunity.com.au and login to update your details any time without cost
Call (02) 9929 1900 or email info@dentist.com.au
every dentist in australia
dentist in new zealand
every dental practice...
every
and
™ www.dentist.com.au



THE ULTIMATE DIY DENTAL MARKETING PACK

Rise Above the Challenges – Elevate Your Dental Practice!
In today’s competitive landscape, dentists in Australia and New Zealand are navigating through increasingly challenging times. With growing competition and tighter economic circumstances, the need to stretch every marketing dollar further has never been more crucial.
That’s where The Ultimate DIY Dental Marketing Pack comes in – your comprehensive solution to not just survive, but thrive in these testing times.
Meticulously crafted for dental practice owners and managers in Australia and New Zealand, this pack isn’t just another marketing toolkit; it’s a strategic partner in your journey towards attracting new patients and securing your practice’s future.
WHY CHOOSE THIS?
Unprecedented Comprehensive Pack: Everything you need in one easy-to-use DIY package. Significant Savings: A $8,080 value for just $997! Act quickly and save over 90%! Prepared by experts: Heavily curated content based on more than 10,000 hours of 1 on 1 consulting with dentists in Australia and New Zealand by Angus Pryor and his team

88%!
– SAVE
READY TO ELEVATE YOUR PRACTICE? NEED MORE INFO? Use this QR code or visit DIY-marketing.com.au for more details and discover how you can revolutionise your dental practice today!

WHAT’S INSIDE?
PERPETUAL DIY MARKETING PACK
12-Month Marketing Calendar: plan and execute your marketing efforts with precision. Includes monthly marketing themes, promotional activities, list of key international days, and more. $500 value
24 Social Media Posts: engage and grow your audience all year. Includes caption library of over 100 customisable social media captions, professional image library, 24 professionally designed Canva templates to level up your practice's social media image. $2400 value
24 Professionally-Written Patient Emails: Keep your patients informed, interested, and thinking about you! Send just one of these emails to your patients and you could reap thousands in additional business. $2400 value
12-Month Dentist.com.au Upgrade: Enjoy thousands of additional views of your practice listing. Elevate your online presence and appear strongly in surrounding suburbs. $795 value
Automated Reminder System: Dental life gets busy, so this system helps you always know where you’re up to, allowing you to stay on track effortlessly. $360 value
ONE-OFF BONUSES
Google Business Profile Checklist: Appearing strongly in Google is Marketing 101 for dentists, and an essential part of your online presence is your Google Business Profile (formerly Google My Business). This checklist gives you the clear steps for success. $200 value
12-Point Website Self-Audit: Your website is a virtual calling card for your entire business. What does it say about you? This 5-minute check will give you everything you need to independently assess whether you practice comes across as a hero or a zero. $500 value
Competitor Assessment: Looking for answers about the competition in your local area? This 5-minute assessment will help you gauge your competition and suggest next steps. $995 value
The Dental Practice Profit System book: no.1 Amazon bestselling book from Australia’s no.1 Google-ranked dental marketer, Angus Pryor. $30 value
LIMITED TIME OFFER!
$8,080VALUE JUST $997!
This incredible offer is only available for a limited time. Seize the opportunity to elevate your dental practice!
“Definitely Angus has a great organisation. You will get value for money.”
Dr Claire Wilson, VIC
“My experience with Angus and the team has been really excellent. They’ve helped my business grow.”
Dr Brian Chen, NSW
“Honestly, it’s the best money I’ve ever spent. Because it’s all about return on investment. And this is the best return on investment I’ve ever done.”
Dr Geoff Hall, VIC


Can we have it all?
By Tabitha Acret, BOH, Grad.Cert (Public Health), Current Master’s Student

Being a working mum will always be one of the hardest juggles as its filled with guilt and hard work. In today’s life, it’s busy and there are many difficulties faced by working mums that are often compounded by pervasive double standards that judge us more harshly than our male counterparts. Despite progress towards gender equality, we are not there! There remains a deeply ingrained culture bias that scrutinises and devalues the choices and capabilities of working mums.
A glaring double standard is the contrasting expectations placed on working mothers and fathers. While working fathers isn’t even a term, it’s not something we mention or worry about and if we do, it’s usually as praise for their dedication to their career. On the other hand, working mothers are frequently criticised for prioritising a career and questioned over their mothering.
When I travel for work to speak at conferences, often people will ask me “Oh where are your kids today?” or “Who is looking after your kids?” but I never see them turn to my male counterparts and ask the same question. The one that infuriates me even further is when they say “Oh aren’t you lucky their dad can look after them while you work”. One, I never see anyone say that to men about women and two, no I am not lucky their
12 oral|hygiene March/April 2024
practice | MANAGEMENT

dad is fulfilling his role as a parent. I shouldn’t be excited as a woman that a male is helping with the load, it should be expected!
Why is it that men are praised for their dedication to their career, but a double standard is used and women are frequently questioned and criticised? Because I am questioned about my working, on the other hand when I say no to something as I need to prioritise kids, or one is sick, we are then criticised for our work ethics as mothers.
Why does society want me to work like I don’t have children and parent like I don’t have a job?
Society expects women to excel in both the professional and domestic spheres, while men are often given a pass when it comes to the household/parenting expectations. Or worse, put on a pedestal and praised for any small effort.
This disparity is often reflected in the workplace, where working mothers may face discrimination and bias based on outdated stereotypes. Studies have shown that mothers are less likely to be hired, promoted or offered equitable pay compared to their male counterparts. Furthermore, working mothers may encounter implicit bias from colleagues and supervisors who question their commitment and competence due to assumptions about their caregiving responsibilities.

The societal judgement of working mothers also extends to their parenting decisions. Mothers who choose to prioritise a career may face criticism for being “selfish” or “neglectful” of their children, while fathers who make similar decisions are praised for their ambition and dedication. The double standard perpetuates the idea that women’s primary role is to nurture and care for their families, while men are expected to be the breadwinners.
In addition to facing judgement from others, what’s even worse is the internalised guilt and self-doubt that comes from the societal pressures and questions. The pressure to meet societal expectations while navigating the competing demands of work and family can take a massive toll on mental and emotional wellbeing. Many working mothers, myself included, struggle with feelings of inadequacy and the fear of not measuring up in either role.
So, this leads us to the question, can we have it all? And the answer is yes and no. I believe as women we should make choices based on our individual needs. Based on what you personally want and your family needs. I love that I get to follow my passion for my career and still raise my kids, but I am not always winning and usually never both at the same time. Often when I am smashing some career goals, I am dropping some balls on
the home front and the same can be said when the wins are reversed. But guess what, you don’t always have to be winning. Sometimes surviving is a win!
The biggest thing to take away is be kind to people trying to juggle. Don’t put the expectations of everything on one gender, these should be shared roles. And don’t ask me where my kids are unless you care about the answer.
About the author
Tabitha Acret is a dedicated and passionate award-winning Dental Hygienist. She studied a Bachelor or Oral Health at Newcastle University , Graduate Certificate in Public Health and is a current Masters student. Tabitha has become one of the most sought-after Hygienists and Educators in Australia and internationally with a fast-growing and loyal customer base of patients, dental professionals and media. Tabitha was previously the National Vice-President for the Dental Hygienists Association of Australia and has volunteered in many roles since graduation for the Association. She also has a passion for educating with students, working as a Clinical Educator at Sydney University and Newcastle University as well as working in private clinical practice and as a Clinical Educator within the dental industry.
March/April 2024 oral|hygiene 13
MANAGEMENT
practice |
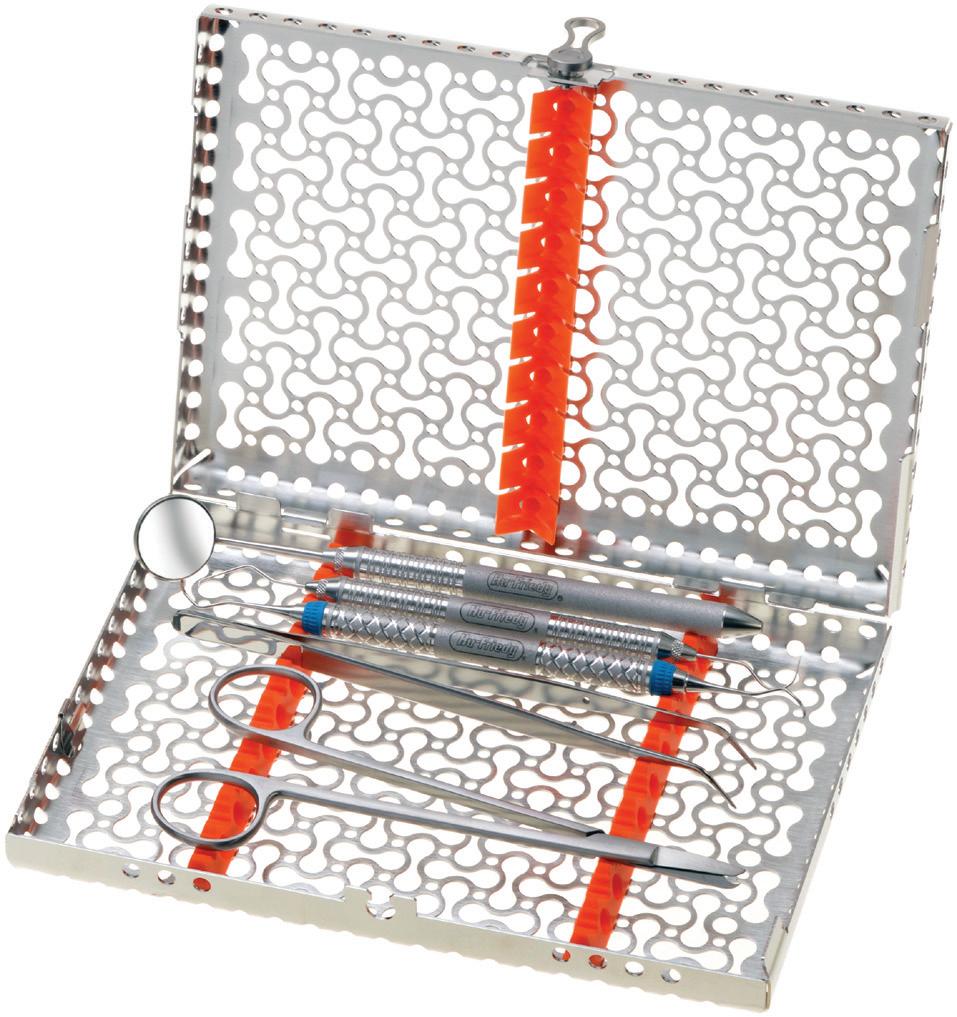
Trays vs cassettes: Considerations when processing dental instruments
By Catherine L. Pawloski, RDH and Marie T. Fluent, DDS
There are two main ways to process and transport dental instruments - process loose instruments in pouches, place onto trays and deliver to and from the operatory; or secure instruments in a locked sterilisation cassette to be packaged, processed and transported to the operatory and back to the sterilisation area. The decision to use trays versus cassettes involves a number of factors, including the occupational safety of dental healthcare personnel (DHCP) such as dental assistants; productivity and efficiency of instrument reprocessing; packaging integrity; professional appearance; and overall cost.
Infection control guidelines
Prior to the investment in any infection prevention and safety product, dental personnel should first and foremost consider compliance with the ADA Infection Control Guidelines and the Australian Standards for instrument reprocessing (AS/NZS 4815 and 4187). All of these recommend against manual cleaning and recommend steps to minimize handling of loose contaminated instruments.
Staff training and safety
P roper training of dental personnel who process instruments is important. General training requirements include ways to reduce risk of contracting an illness or injury on the job; policies and procedures for reporting occupational injuries; and obtaining the necessary follow-up medical care. It is necessary to train DHCP on all processing steps, including instrument transport, cleaning, inspection, packaging, sterilisation, monitoring of sterilisation and storage of sterilized items. DHCP must also be trained to follow all manufacturer instructions for use (IFU) for specific products. Policies, procedures and manufacturer reprocessing and maintenance instructions for reusable instruments and dental devices must be available in or near the instrument reprocessing areas to ensure that all equipment is used properly and is working correctly. When processing loose instruments, DHCP handle contaminated instruments more often than when using cassettes. This poses more vulnerability, as there is an increased risk for sharps injury and/or exposure to blood-borne pathogens, despite them wearing heavy duty utility gloves. In contrast, cassettes minimise the handling of loose instruments in all phases of reprocessing.

14 oral|hygiene March/April 2024 infection | CONTROL READ ME FOR CPD
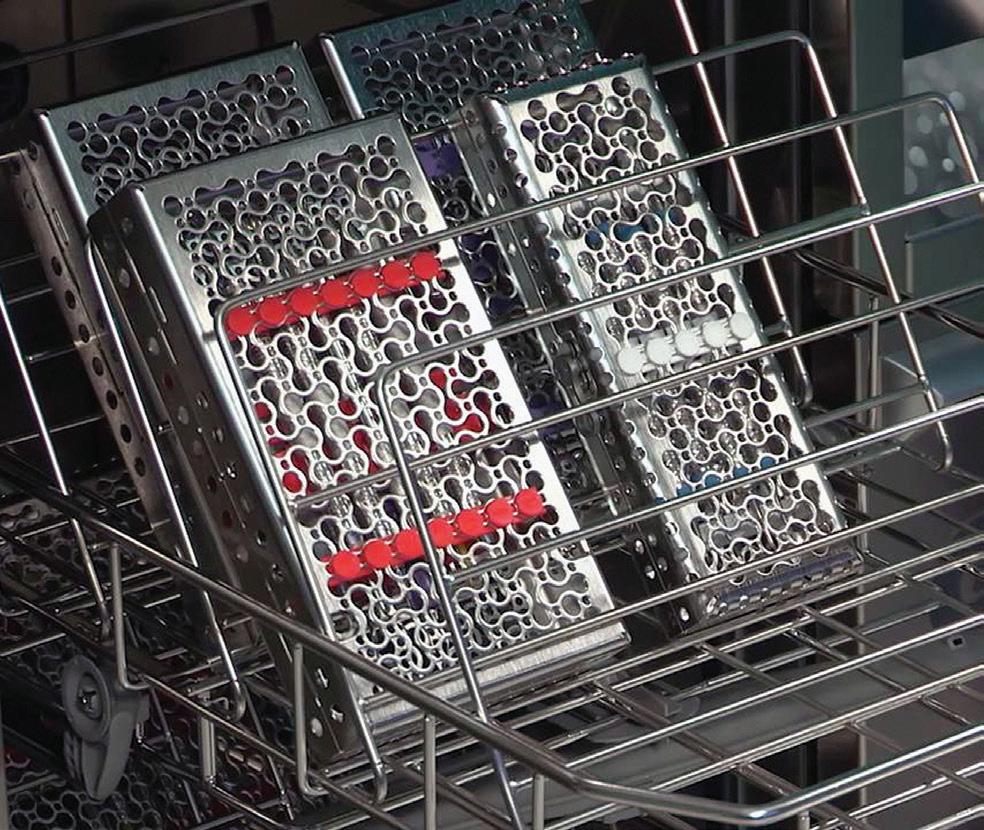
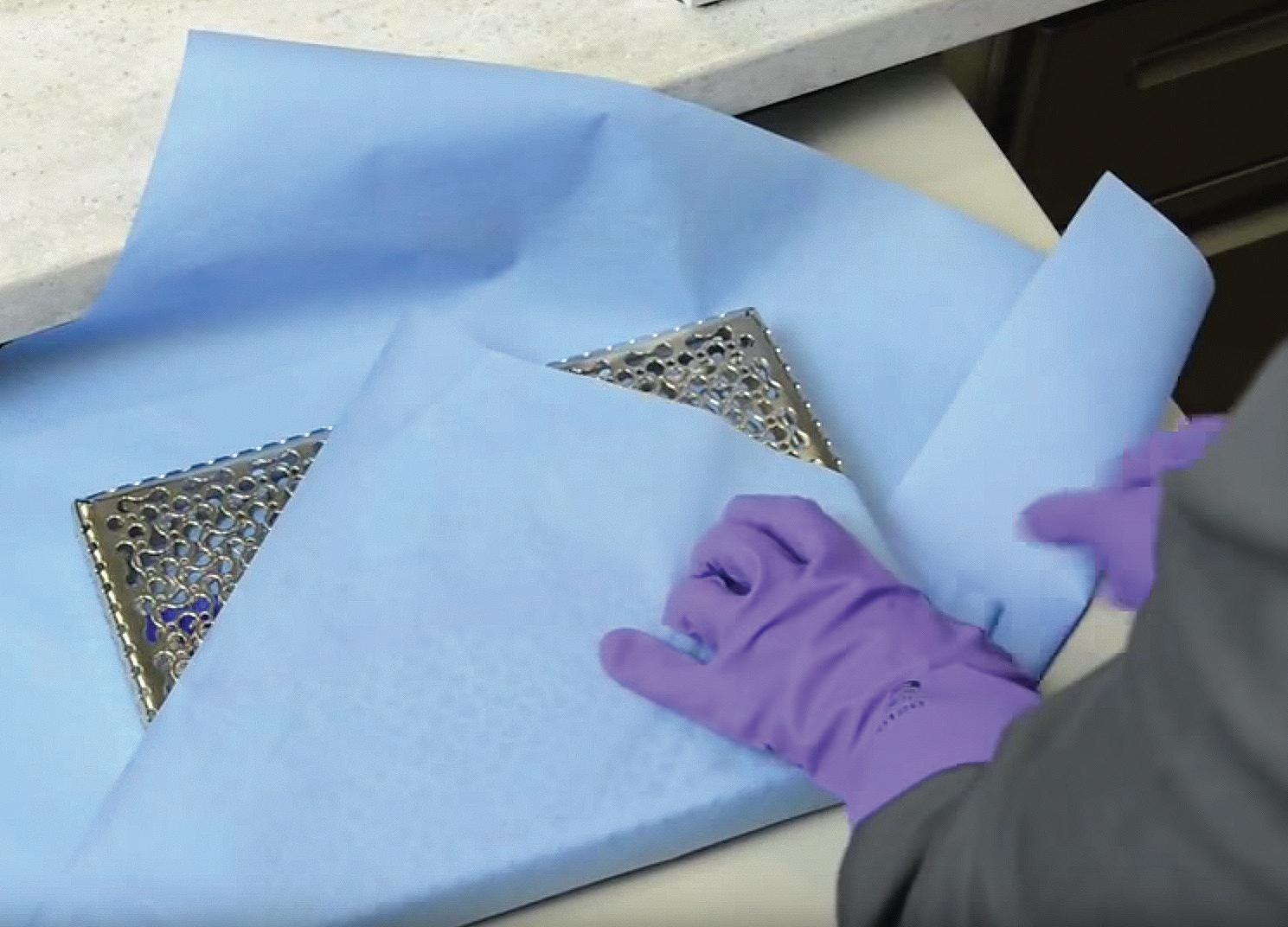
Figures 1 and 2. Hu-Friedy Infinity Series instrument cassettes.
Efficiency and productivity
When loose instruments are placed into different pouches, organisation and storage can be compromised. Staff must check each pouch to observe whether it is indeed the correct set-up and whether all instruments are present. As pouches are emptied on to a tray in the clinic, the contents spill out in random order and may even find their way to the floor. In contrast, sterilisation cassettes have racks which ensure that instruments are aligned and remain in sequence, ready for use in the clinic. After the procedure, DHCP return the various instruments to their correct location in the cassette and they remain in that place throughout reprocessing.
Instrument preservation and packaging integrity
During manual processing of loose instruments, individual items can move about freely, causing damage to their tips or to other items in the load. It is common for mouth mirrors to become scratched while being cleaned in an ultrasonic unit and for the tips of explorers and probes to become damaged, distorted or bent. In contrast, in cassettes, all instruments are held securely in place, preventing damage or loss of instruments.
Pouches with many loose instruments or instruments with sharp tips are more likely to suffer from a pouch perforation. When this happens, the contents of the pouch are no longer considered sterile and the instruments must be removed and reprocessed. In contrast, instruments in a wrapped cassette cannot compromise the packaging as their sharp tips are securely contained within.
Pouches and cassettes may also be compromised due to moisture that remains after sterilizing, or splashes of fluid onto sterilized packages. Dental personnel must keep all instrument packages away from any splashes or other contamination to ensure sterility is maintained during storage.
CAdditional considerations
assettes may hold unit dose supplies. These can be added after instrument cleaning, rinsing and drying. Having required supplies such as cotton rolls in the cassette eliminates the need to touch cabinets, drawers and containers during treatment.
Both pouches and cassettes are available in a multitude of sizes to accommodate all types of instrument set-ups. When using cassettes, it is important to ensure that the cassette size is compatible with the size of the washer disinfector, ultrasonic bath and steam steriliser.
While it may appear that the use of pouched instruments on trays may be a lower cost approach than using cassettes, there are considerable time and cost savings during instrument processing (in addition to benefits of improved safety, efficiency and productivity). Cassettes are easier to store and provide a more professional and up-to-date appearance. Regardless of which type of delivery systems is used, whether bagged instruments on trays or instruments in cassettes, compliance with infection control guidelines and the safety of staff and patients should remain the top priority.
About the authors
Catherine L. Pawloski, RDH, currently works in clinical practice in Michigan, USA. She has written articles relating to the topics of infection control in the dental office.
Marie T. Fluent, DDS, practised general dentistry for 25 years. She is currently an infection control adviser and has written a range of articles on infection control compliance and antibiotic stewardship in dentistry.
Article courtesy of “Inside Dentistry”. Thank you to Professor Laurie Walsh for editing content to ensure compliance with Australian standards and guidelines.
March/April 2024 oral|hygiene 15 infection | CONTROL
Figure 3. Instruments remain within cassettes during cleaning in thermal washer disinfector units or ultrasonic baths.
Figure 4. Following cleaning, the instruments, still in the cassettes, are packaged, sterilised and stored ready for use.
oral|hygiene CPD CENTRE
Trays vs cassettes: Considerations when processing dental instruments
By Catherine L. Pawloski, RDH and
DDS


Question 1. During reprocessing, using cassettes prevents:
a. Instrument tips from being damaged.
b. Mouth mirrors from becoming scratched.
c. Explorers and probes becoming damaged, distorted or bent.
d. All of the above.
Question 2. Pouches with many loose instruments or instruments with sharp tips are more likely to suffer from a pouch perforation and require reprocessing:
a. True
b. False
Question 3. Instruments remain within cassettes during:
a. Cleaning in thermal washer disinfector units or ultrasonic baths.
b. Autoclaving.
c. Transport to and from the operatory.
d. Storage.
e. All of the above.
Question 4. Sterilisation cassettes help:
a. Prevent instruments from becoming misplaced or lost.
b. Prevent sharps injuries during the reprocessing cycle.
c. Prevent instruments from being damaged during reprocessing.
d. Keep instruments in ordered procedural set-ups.
e. All of the above.
Question 5. Instrument cassettes deliver considerable time and cost savings during instrument processing in addition to benefits of improved safety, efficiency and productivity:
a. True
b. False


Question 6. Toothpaste ingredients are listed...
a. In alphabetical order.
b. Descending order based on weight percentage.
c. By active ingredients.
b. Ascending order based on weight percentage.
Question 7. A sweetener found in toothpaste is...
a. Sugar
b. Stevia
c. Xylitol
d. Aspartame
e. Any of the above
Question 8. Blue covarine is used in toothpaste to...
a. Give the toothpaste a white colour.
b. Create coloured stripes.
c. Make your teeth look whiter.
d. As a surfactant.
Question 9. Limonene and benzoates in toothpaste can cause...
a. Pellicle staining.
b. A risk of dental erosion.
c. Allergic reactions.
d. The pH to adversely change.
e. All of the above.
Question 10. When discussing toothpaste, PCR stands for...
a. Polymerase Chain Reaction.
b. Pellicle Cleaning Ratio.
c. Please Clean Regularly.
d. Perform Cleaning Regularly.
INSTRUCTIONS:
14 ora hygiene March/April 2024 infection CONTROL READ ME FOR CPD T here are two main ways to process and transport dental instruments - process loose instruments in pouches, place onto trays and deliver to and from the operatory; or secure instruments in a locked sterilisation cassette to be packaged, processed and transported to the operatory and back to the sterilisation area. The decision to use trays versus cassettes involves a number of factors, including the occupational safety of dental healthcare personnel (DHCP) such as dental assistants; productivity and efficiency of instrument reprocessing; packaging integrity; professional appearance; and overall cost. Infection control guidelines Prior to the investment in any infection prevention and safety product, dental personnel should first and foremost consider compliance with the ADA Infection Control Guidelines and the Australian Standards for instrument reprocessing (AS/NZS 4815 and 4187). All of these recommend against manual cleaning and recommend steps to minimize handling of loose contaminated instruments. Staff training and safety Proper training of dental personnel who process instruments is important. General training requirements include ways to reduce risk of contracting an illness or injury on the job; policies and procedures for reporting occupational injuries; and obtaining the necessary follow-up medical care. It is necessary to train DHCP on all processing steps, including instrument transport, cleaning, inspection, packaging, sterilisation, monitoring of sterilisation and storage of sterilized items. DHCP must also be trained to follow all manufacturer instructions for use (IFU) for specific products. Policies, procedures and manufacturer reprocessing and maintenance instructions for reusable instruments and dental devices must be available in or near the instrument reprocessing areas to ensure that all equipment is used properly and is working correctly. When processing loose instruments, DHCP handle contaminated instruments more often than when using cassettes. This poses more vulnerability, as there is an increased risk for sharps injury and/or exposure to blood-borne pathogens, despite them wearing heavy duty utility gloves. In contrast, cassettes minimise the handling of loose instruments in all phases of reprocessing.
Figures 1 and 2. Hu-Friedy Infinity Series instrument cassettes. 22 ora hygiene March/April 2024 Toothpaste labelling and testing technologies: Time for a rethink? By Emeritus Professor Laurence J. Walsh AO When strolling through the toothpaste aisle in a major supermarket, one cannot help but be impressed by the extent of available choices that faces the modern consumer when choosing a toothpaste. There is a wide variety of products available, both across major brands and within any given brand. However, when one breaks down the details to look at the individual product formulations, differences between some of them are relatively small. Many patients and colleagues tell me that they are confused when trying to work out which toothpaste is best for their particular situation, given the sheer number of choices available on the shelves. The purpose of this article is to help clinicians understand the technology of toothpastes, the role of the various ingredients and appreciate how the performance of toothpastes is assessed in the laboratory. READ ME FOR CPD clinical EXCELLENCE
Marie T. Fluent,
OralHygiene™ is now offering PAID subscribers the ability to gain 2 Hours CPD credit from reading articles in this edition of the magazine and answering the questions above. To participate, contact OralHygiene for your Username and Password. Then log into the Dental Community website at www.dentalcommunity.com.au and click on the CPD Questionnaires link; select the Oral Hygiene Mar/Apr 2024 questionnaire and then click START. A score greater than 80% is required to PASS and receive CPD.


Question 11. The “S” in ARSPT stands for...
a. Sterilisation
b. Steam
c. Sensitivity
d. Stringent
Question 12. Older dental handpieces will not be compatible with washer disinfectors because...
a. The couplings are not supported.
b. The internal piping is too narrow.
c. The highly alkaline detergents used will cause corrosion.
d. Rubber O-rings are used.
Question 13. Oxidation of the isoprene polymer structure of natural rubber latex o-rings results from using...
a. Ozonated water.
b. Ultrafiltration in the water system.
c. Shock treatments.
d. Chelating agents.
Question 14. Hydrogen peroxide gas vapour is an alternative to using moist steam for sterilisation:
a. True
b. False
Question 15. The term “hollow load type A” remains in the new AS 5369 standard:
a. True
b. False
 By Tami Wanless
By Tami Wanless

Question 16. Burnished calculus is smoothed, partially removed subgingival calculus that no longer contributes to disease:
a. True
b. False
Question 17. In patients with a oral hygiene routine, burnished calculus will be evidenced by:
a. Isolated areas of tissue colour change.
b. Slight inflammation.
c. Bleeding on probing.
d. All of the above.
Question 18. Research supports evidence demonstrating that blind root planing is only effective to:
a. 2mm
b. 3mm
c. 4mm
d. 5mm
Question 19. To remove burnished calculus:
a. Use sharp instruments.
b. Ensure that the blade-to-tooth angle is optimal.
c. Use a modified-pen grasp to ensure the correct pressure is applied.
d. All of the above.
Question 20. Burnished calculus is more likely to be found in areas on the root surface with:
a. Developmental grooves
b. Depressions
c. Furcations
d. At the cemento-enamel junctions
e. All of the above
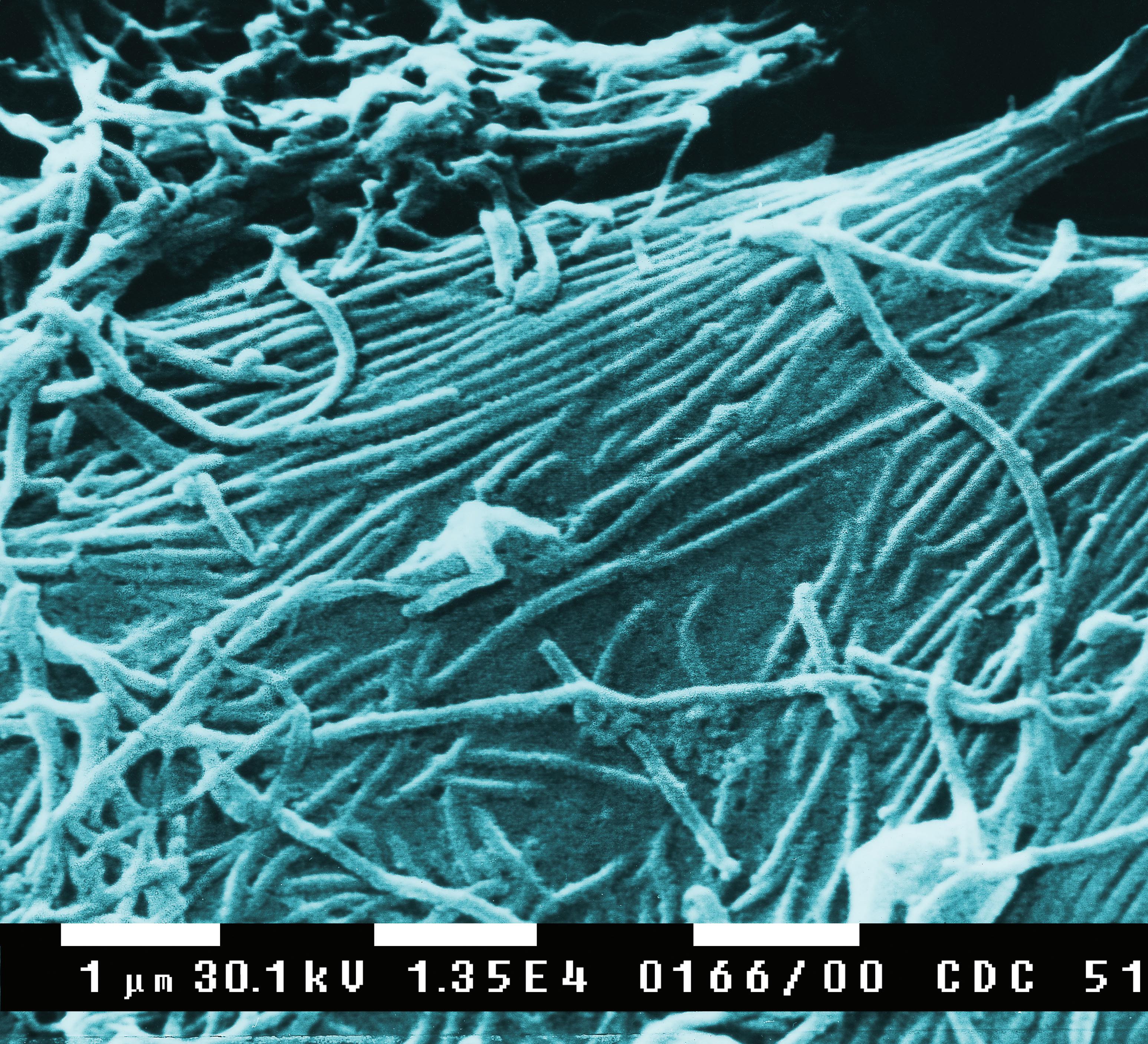
READ THE ARTICLES BELOW AND ANSWER THE QUESTIONS ONLINE AT WWW.DENTALCOMMUNITY.COM.AU - 2 HOURS OF CPD 26 ora hygiene March/April 2024 The problems of pipes: A key challenge in infection prevention and control By Emeritus Professor Laurence J. Walsh AO Many components of infection prevention and control in dental practice relates to what can be called “the problems of pipes” - preventing pipes from becoming blocked, removing hard mineralised and soft microbial deposits and bioburden from pipes, effective cleaning of pipes and sterilisation of pipes (Table 1) This article explores several of these elements and highlights the implications for everyday infection control protocols. Triplex tips Water which runs through dental units is not free of ions and most dental units use reticulated water (tap water), to which various chemicals are added to slow the growth of microbial biofilms. With a metal triplex tip which is of the DCI design, one pipe sits within another pipe and the inner pipe is held in place by crimping of the outer pipe. This creates a situation where tap water can be retained within the metal triplex tip when it reaches the chamber of the steam steriliser (autoclave). This then creates the possibility READ ME FOR CPD infection CONTROL 32 ora hygiene March/April 2024 READ ME FOR CPD Supervised neglect is defined by Mosbys Dental Dictionary as a case in which a patient is regularly examined and shows signs of a disease or other medical problems, but is not informed of its presence or progress (Mosby’s Dental Dictionary: Edition 2, 2007).1 A sound clinician would never intentionally leave calculus, let alone burnished calculus, but what if you learned today that you were leaving deposit contributing to chronic gingival disease? Are you practising Supervised Neglect? Whether you’re a new graduate or a seasoned professional, here is what you need to know to start making positive changes on your next patient. What is burnished calculus? When describing calculus attachment to my patients, like to use the analogy that the calculus attaches to the tooth like a barnacle attaches to a boat. Barnacles actually produce cement that is released through the tips of their antennules to attach themselves. Calculus attaches by mechanically interlocking to the crystals of the tooth using the acquired pellicle. Burnished calculus is a subgingival deposit that has had its outermost layer shaved off and not fully removed, so the surface is smooth, but is still attached to the tooth surface contributing to disease.4,5 When a clinician does not recognise or remove burnished calculus, they are practising Supervised Neglect. One wouldn’t “plane away” a barnacle off a boat, nor should you “shave away” calculus from a tooth; in either scenario you will leave the source of the irritant. How does tissue respond to a burnished deposit? These areas of burnished deposits will contribute to persistent gingival inflammation and bleeding in addition to providing a constant food source for more bacteria to attach. This vicious cycle will continue until you completely remove ALL the calculus. We set our patients up for failure when we tell them to brush and floss to reduce recurrent bleeding when we leave burnished deposit subgingivally every six months. The most effective calculus removal Your role in recognising and healing supervised neglect related to burnished calculus
clinical EXCELLENCE
POWERED BY THE To retrieve your FREE Dental Community Login: Call (02) 9929 1900 or Email info@dentist.com.au
dentevents presents...
Infection Control BOOT CAMP
29 VIDEOS - 8+ HOURS OF EDUCATION
Presented by Emeritus Professor Laurence Walsh AO BDSc, PhD, DDSc, GCEd, FRACDS, FFOP (RCPA), FFDT (RCS Edin)
8
Learn from Australia’s leading authority on infection prevention and control in dentistry about recent changes in infection control including from the Dental Board of Australia (July 2022), the ADA (4th edition guidelines August 2021 and the ADA Risk management principles for dentistry during the COVID-19 pandemic (October 2021)), the new guidelines from NHMRC (May 2019), Hand Hygiene Australia (Sept 2019) and the CDNA (Dec 2018) as well as recent changes in Australian Standards and TGA regulations that are relevant to infection control. The course provides a summary of how those changes interlink with one another and also covers practical implementation of the new requirements and what it means for everyday dental practice. Hear about the why and the how and keep up-to-date with the changes that are happening.
COURSE TOPICS
This one day course will cover changes in regulations and guidelines from 2018 to 2022 including:
n Risk-based precautions.
n Hand hygiene and hand care practices.
n Addressing common errors in personal protective equipment.
n Biofilm reduction strategies.
n Efficiency-based measures to improve workflow in instrument reprocessing and patient changeover.
n Correct operation of mechanical cleaners and steam sterilisers.
n Wrapping and batch control identification.
n Requirements for record keeping for instrument reprocessing.
n Correct use of chemical and biological indicators.
Register Now: www.boosterinjection.com.au
HOURS CPD
ON DEMAND ONLINE LEARNING PROGRAMME






Laurie Walsh is a specialist in special needs dentistry who is based at the University of Queensland in Brisbane, where he is an emeritus professor. Laurie has been teaching and researching in the areas of infection control and clinical microbiology for over 25 years and was chief examiner in microbiology for the RACDS for 21 years. His recent research work includes multiple elements of infection control, such as mapping splatter and aerosols, COVID vaccines and novel antiviral and antibacterial agents. Laurie has been a member of the ADA Infection Control Committee since 1998 and has served as its chair for a total of 8 years, across 2 terms. He has contributed to various protocols, guidelines and checklists for infection control used in Australia and represented dentistry on 4 committees of Standards Australia and on panels of the Communicable Diseases Network of Australia and of the Australian Commission on Safety and Quality in Health Care.



REGISTRATION INCLUDES
n On-Demand access to 29 Online Learning Videos (Over 8 hours of education).
n Watch and re-watch at your leisure 24/7
n Digital Online Learning Companion.
n Digital Suggested Reading Material.
n Online Questionnaire to earn 8 Hours of CPD.
Register Now: www.boosterinjection.com.au REGISTRATION FEES Dentists $660 inc gst Others $330 inc gst
Infection Contol Boot Camp is presented by Dentevents, a division of Main Street Publishing Pty Ltd ABN 74 065 490 655 • www.dentevents.com • info@dentist.com.au Tel: (02) 9929 1900 • Fax: (02) 9929 1999 • Infection Contol Boot Camp™ and Dentevents™ are trademarks of Main Street Publishing P/L © 2023 Main Street Publishing Pty Ltd FULL UPDATE! All the changes to Infection Control Updated in 2022 dentevents.tv
Oral Hygiene Abstracts 2024
By Emer. Prof. Laurence Walsh AO
Oral infections and joint prostheses

The surgical replacement of joints, especially hip and knee using an endoprosthesis (EP) is a frequent and highly successful treatment option to reduce pain and increase function in case of advanced joint diseases. Joint replacement surgery is one of the most frequently performed elective orthopaedic surgical procedures in the world. However, EP infections are a severe complication, causing enormous morbidity. Whether or not oral diseases contribute to the development of EP infections has been controversial. There is a large discrepancy between the prevalence of oral foci of disease and EP infections. EP infections are rarely occurring events; overall, 0.3%-2% of patients develop an EP infection. An overall prevalence of oral focus-related infections between 0.009% (3% of 0.3% at minimum) and 0.26% (13% of 2% at maximum) should be expected. This narrative review explores two hypotheses for oral disease-associated EP infections: (1) In case of an acute exacerbation during the early healing period after EP surgery (the first 3 months); and (2) Coincidental in the context of late EP infections (after successful initial healing), where an initial periprosthetic inflammation can be colonised secondarily by oral microorganisms. In both settings, oral foci are not primarily causative for EP infection, but represent an important reservoir for EP colonisation. Immunological conditions (locally and systemically) are crucial for the onset of an EP infection. Risk increases for factors such as high BMI, previous use of immunosuppressant, diabetes mellitus, rheumatoid arthritis, depression, steroid use, male gender, age and alcohol abuse. All of those co-morbidities can affect systemic immunity, resulting in a higher susceptibility to infections. Moreover, these parameters are also related to oral health, especially periodontitis. Thus, the occurrence of oral diseases in patients with EP infections might be coincidental rather than causal. Patients with risk factors for EP infection should be orally rehabilitated prior to EP surgery. A radical dental clearance is not a favourable approach for these patients. Usage of antibiotic prophylaxis during the first 3 months after EP implantation (initial healing period) has no reliable evidence to support it. Overall, patients with EP should receive increased attention in terms of preventive measures, because they show a high dental and periodontal treatment need.
Schmalz G, Ziebolz D. The hypotheses of oral disease-associated perioprosthetic joint infections to understand the role of oral health for endoprostheses - a narrative review. Spec Care Dentist. 2024 Mar-Apr;44(2):328-338.
UK IE guidelines are badly out of step
Infective endocarditis (IE) is a devastating infection of the heart valves, with a 30% first-year mortality. Its incidence continues to increase in the UK, driven by multiple factors including an ageing population, increasing numbers of high-risk individuals (due to medical interventions), increased awareness of IE and a reduction in the use of antibiotic prophylaxis (AP) before invasive dental procedures (IDPs). In 2023, the European Society of Cardiology (ESC) updated its infective endocarditis (IE) guidelines strongly endorsing antibiotic prophylaxis (AP) before invasive dental procedures (IDPs) for high-risk patients, elevating their recommendation to Class I. The American Heart Association (AHA) is aligned with this view and reaffirmed the need for AP to prevent IE in those at high-risk in its 2021 guidelines. Similar guidelines have existed in Australia for many years, which stratify cases according to the risk of the procedure and the risk to the patient. In contrast, since 2015 the UK’s National Institute for Health and Care Excellence (NICE) has recommended against routine AP use for IE, even in high risk cases. Despite considerable new evidence, NICE has not reviewed this recommendation since 2015. In 2015, an observational study found high compliance with the NICE guidance in the UK and identified an 88% decline in AP prescribing since 2008. It also found a significant increase in IE incidence following the change. At that time, NICE methodology required randomised controlled trial (RCT) evidence to support any change in recommendations and, following review, it reiterated its guidance stating that “antibiotic prophylaxis against infective endocarditis is not recommended for people undergoing dental procedures”. The ESC reviewed the same evidence in 2015 but continued to recommend AP for high-risk patients. In 2016, however, without explanation or review, NICE changed the wording of its guidance as follows: “antibiotic prophylaxis against infective endocarditis is not routinely recommended for people undergoing dental procedures”. The word “routinely” made the UK guidance ambiguous and has caused confusion for dentists, cardiologists and patients. This study reviewed the new evidence that has arisen since 2015. The analysis establishes the association between IDPs and IE and shows that AP is both safe and effective in reducing the IE-risk following IDPs in those at high-risk. Data also show that AP is cost-effective and would result in significant cost savings and health benefits if it was re-introduced into the UK’s National Health Service for highrisk patients. Given these insights, the study argues it is time NICE reviewed its guidance so that high-risk patients in the UK receive the same protection against IE that is afforded to patients in the rest of the world.
Thornhill M et al. Endocarditis prevention: time for a review of NICE guidance. Lancet Reg Health Eur. 2024 Mar 5:39:100876. doi: 10.1016/j.lanepe.2024.100876.
20 oral|hygiene March/April 2024 abstracts | 2024


When you SHOCK, let ICX RENEW.
Unwanted visitors like bacteria love to colonise in your dental unit waterlines. A daily waterline maintenance protocol with A-dec ICX® waterline treatment tablets, along with periodic ICX Renew™ shock treatments, will help reduce these nasty microorganisms.

For complete trademark information, visit a-dec.com/legal/trademarks.
australia.a-dec.com © 2021 A-dec Inc. All rights reserved. Unwanted guests in your waterlines?
To find out more, visit

Toothpaste labelling and testing technologies: Time for a rethink?
By Emeritus Professor Laurence J. Walsh AO

When strolling through the toothpaste aisle in a major supermarket, one cannot help but be impressed by the extent of available choices that faces the modern consumer when choosing a toothpaste. There is a wide variety of products available, both across major brands and within any given brand. However, when one breaks down the details to look at the individual product formulations, differences between some of them are relatively small.
Many patients and colleagues tell me that they are confused when trying to work out which toothpaste is best for their particular situation, given the sheer number of choices available on the shelves. The purpose of this article is to help clinicians understand the technology of toothpastes, the role of the various ingredients and appreciate how the performance of toothpastes is assessed in the laboratory.
22 oral|hygiene March/April 2024
READ ME FOR CPD clinical | EXCELLENCE
Finding ingredient information
Toothpastes that are sold through supermarkets and pharmacies often have their ingredients and other information (such as specific instructions for use) on the website for that supermarket or pharmacy chain. This is often the fastest and easiest way to access such information. While some toothpaste manufacturers have set up a dedicated website for professionals, sometimes these require a user to log in and becomes an enrolled user in order to access this information, which seems an unnecessary step.
How the label information is arranged
Australian consumer law requires that ingredients are listed in descending order of their weight percentage, i.e. from the most dominant ingredient to the least. The position of an ingredient in the overall sequence is an important consideration when one spots an ingredient that might seem problematic. When an ingredient is included towards the end of the list of the ingredients, the amount is very small. Common examples are phosphoric acid and sodium citrate. Both chemical agents form parts of buffer systems and this is why they are used in toothpastes. Their inclusion brings the toothpaste to the correct near-neutral pH and ensures that the pH of the product when it is diluted in the mouth by saliva is appropriate. Thus, they pose no risk of dental erosion when used in this way.
Active ingredients
Product labelling will feature key active ingredients. These could be agents that assist with remineralisation, chemical plaque control, lowering the formation of dental calculus or removing external stains.
For a fluoride toothpaste, the chemical form of the fluoride compound makes a difference to its bioavailability and its performance in terms of remineralisation. As shown in Table 1, several standardised tests are used to assess the remineralising ability of toothpastes and these are described in the US FDA monograph series for toothpastes. These tests include fluoride uptake into incipient
enamel lesions and remineralisation of the enamel surface after a lactic acid challenge. Data from such tests typically indicate that when matched for parts per million (ppm) of fluoride ions, stannous fluoride products do better in these standardised assays than sodium fluoride. However, from the perspective of the consumer, product labelling does not state the level of fluoride in the toothpaste in terms of parts per million. Without knowing the chemical formula of the fluoride form that is used, it is not simple to calculate the ppm level from the information that is given on the product label. This creates a challenge for both dental professionals and patients.
(RDA) of the toothpaste. The RDA number comes from a complex calculation involving how well particular toothpaste compares to using a reference material when used in many thousands of cycles with standardised force in a toothbrushing jig.1-7 For a summary of RDA values for some common toothpastes, see reference 10. Typical examples are Oral-B Pro-Health and 3D-White, which have RDA values of around 170 and 180. There is an inherent compromise between the abrasivity of a toothpaste and its ability to remove external stains, i.e. stained pellicle. Toothpastes with aggressive abrasive properties will be better at removing stained pellicle, but
ISO 11609:2017 Dentifrices - Requirements, test methods, and marking.
ANSI/American Dental Association Standard No. 130.
Remineralisation of caries like lesions using the White method (White DJ. Caries Res. 1987;21(2):126-140. and White DJ. Caries Res. 1988;22(1):27-36).
US FDA Monograph Part 29 for soluble available fluoride concentrations.
US FDA monograph Part 21 for fluoride uptake into incipient enamel lesions.
US FDA monograph Part 33 for enamel solubility reduction.
For details and examples of fluoride and remineralisation tests, see references 13-19.
Vehicle components
By weight, the greatest components of toothpastes are found in the mixture of glycerin and water that comprises the vehicle. The glycerin serves several purposes. It is hygroscopic and so allows the toothpaste to retain moisture if the lid or cap is not closed fully. As a viscosity modifier, glycerin is the main ingredient which allows the toothpaste to flow evenly from the tube. It also contributes a slight sweet taste to the toothpaste.
Abrasives
The types of abrasives used in toothpastes vary over a wide range, both by their chemical composition and by their physical size. Common abrasives include perlite, calcium pyrophosphates, silica and calcium carbonate. Generally speaking, the smaller the particle size, the lower the relative dentine abrasivity
their long-term use can cause abrasion of roots and exposed dentine. This is why the international standard for toothpastes (ISO 11609:2017) stipulates a maximum relative dentine abrasivity (RDA) score of 250. Surprisingly, there are several toothpastes on the market that have abrasivity scores that are above 250. Not surprisingly, longterm use of highly abrasive toothpastes will cause abrasion of the dental hard tissues. Using such products also increases the likelihood of abrasion of the attached gingiva.
The blend of abrasives also influences the viscosity of the toothpaste and thus how much it will flow when a squeezing force is applied to the sides of the toothpaste tube. Products with higher levels of abrasive will be more viscous and will be less likely to flow in a consistent manner when pressure is applied, due to shear thinning. They may also feel grittier when used, if the particle size is sufficiently large that it can be detected by the tongue (e.g. 50 microns or larger).
March/April 2024 oral|hygiene 23 clinical | EXCELLENCE
Table 1. Key standard laboratory methods for performance testing of toothpastes
Surfactants
Most common toothpastes use sodium lauryl sulphate (SLS) as their surfactant. This is a high foaming agent and is responsible for the froth that is created during toothbrushing. SLS has some antibacterial actions and can assist in dislodging biofilm stacks from the pellicle. Residues of SLS are irritant to soft tissues, which explains why leaving residues of toothpastes behind can lead to irritation of the oral soft tissues.
Several studies have linked the presence of SLS in toothpastes with elevated prevalence rates for recurrent aphthous ulceration and this has driven several toothpaste manufacturers to introduce versions that either have reduced levels of SLS or where the SLS has been replaced completely with another surfactant. Low foaming surfactants used in toothpastes ensure that less froth and foam is generated during the toothbrushing action and that there are lower levels of soft tissue irritancy.
Flavours
The traditional flavour of toothpastes has been based on a mint taste, such as peppermint or spearmint. These are both relatively strong flavours and this can cause issues with patients who are unable to tolerate strong flavours, such as those with autism spectrum disorders. Some flavours are problematic because of allergy (e.g. limonene). Recently toothpastes have been developed with novel non-mint flavours (e.g. Hismile). This can help improve compliance with toothbrushing as it makes the experience more enjoyable.
Sweeteners
I ntense sweeteners are used widely in toothpastes to improve their overall taste and also to balance out the astringency of mint and some other flavours. Somewhat surprisingly, in some parts of the world, sugar is used rather than an alternative sweetener. Some toothpastes use stevia or natural polyols such as sorbitol or xylitol as part of their mixture of sweeteners, while others use modified forms of sugar (such as sucralose) or intense artificial sweeteners such as aspartame.
Colouring agents
Some toothpastes contain agents that give the toothpaste a white colour (such as titanium dioxide), while others contain various dyes that generate coloured stripes or enhance the reflection of blue or violet light from the surfaces of teeth (e.g. blue covarine CI74160) for as long as those dyes are bound to the pellicle layer. It is always useful to know what the dye is being used for, but rarely is this stated in the product information. The use of dyes is highly regulated, which is why certain markets will not permit the use of particular dyes.
“A toothpaste may make whitening claims because of its removal of stained pellicle. This needs to be distinguished from a situation where an actual oxidising agent (such as hydrogen peroxide or PAP) is present, which can decolourise external stains, rather than remove them...”
Preservatives
Antimicrobial agents are included in toothpastes to prevent overgrowth by microorganisms and thus provide a suitably long shelf life for the product. Sometimes these preservatives elicit problems including allergies. Benzoates are the most common preservative type that can lead to issues. Taking a careful history will reveal that a person who has an allergy to benzoate preservatives will mount responses to a range of foods and cosmetics where these are used.
Cleaning performance
It would be useful to both everyday consumers and dental professionals if the cleaning performance of a particular
toothpaste was stated using relatively simple metrics. A widely used laboratory-based method to assess the removal of stained pellicle is the pellicle cleaning ratio (PCR) assay.8-12 Based on clinical data, a PCR value of at least 50 is needed to provide acceptable extrinsic stain removal. Having a high PCR is important for individuals whose diet includes frequent intake of foods and beverages that can cause external staining.
By combining the information from the PCR with the dentine abrasivity, the cleaning efficiency index can be calculated. The actual equation is...
CEI = (RDA + PCR – 50) ÷ RDA
The cleaning efficiency index emphasizes the importance of effective stain removal properties and low dentine abrasion. Hence, if one was to degenerate the performance of the toothpaste to just one simple single number, this would be the number to use.
Whitening claims
Atoothpaste may make whitening claims because of its removal of stained pellicle. This needs to be distinguished from a situation where an actual oxidising agent (such as hydrogen peroxide or PAP) is present, which can decolourise external stains, rather than remove them. Given the short period of time that toothpastes are used for during toothbrushing, it is unlikely that oxidising agents will have sufficient time to penetrate into the enamel and oxidise any coloured molecules which are there.
Most consumers do not understand that whitening claims for toothpastes inherently are connected to the removal of external stains. This is why having greater transparency in labelling around the pellicle cleaning ratio and the cleaning efficiency index would greatly improve informed decisions around toothpastes. Those individuals whose diet has a high frequency of tea, coffee, red wine and other sources of external stain could then look for a toothpaste with a high PCR, to help reducing the accumulation of stained pellicle, while at the same time looking to see that the product has a high cleaning efficiency index, so that it is achieving removal of stained pellicle without causing a problematic amount of dental hard tissue abrasion.
24 oral|hygiene March/April 2024
clinical | EXCELLENCE
Use instructions
This is an area where considerable improvements can be made. The volume of toothpaste that is required will vary according to the size and number of teeth that are to be cleaned. Clear advice showing the proper amount of toothpaste to be applied to a toothbrush should be given by the manufacturer, for example, on the box or on the toothpaste container itself.
Table 2. Suggestions for greater transparency in toothpaste advertising and improved product support
• State clearly on the product that brushing should be for at least 2 minutes twice daily.
• State the level of fluoride in parts per million on the packaging.
• State the dentine abrasivity score and pellicle cleaning ratio, or the cleaning efficiency index on the packaging.
• On manufacturer websites for professionals, provide comparison tables for products within the brand, for ready reference by dental professionals. Ensure that these sites do not require logging in or enrolment to access such data.
• Make information on the pellicle cleaning ratio and the cleaning efficiency index available for dental professionals in marketing materials to facilitate their decision-making around which toothpaste to recommend to patients.
Moreover, there should be explicit instructions that toothbrushing needs to be conducted twice daily and for at least 2 minutes for each brushing episode, since the removal of dental plaque biofilm and the removal of stained pellicle are both highly responsive to brushing time.
Conclusions
Having now reached the end of this short journey, one can appreciate that, as dental professionals, we need to better understand the components of toothpaste and the performance of
toothpaste in order to make appropriate recommendations to our patients. While many of us will feel quite comfortable giving instructions on brushing techniques and interdental cleaning, some of us will
struggle when asked by a patient, “Which toothpaste do you recommend for me, and why?” Better product information and labelling (as summarised in Table 2) would greatly assist us in this task.
About the author
Emeritus Professor Laurence J. Walsh AO is a specialist in special needs dentistry who is based in Brisbane, where he served for 36 years on the academic staff of the University of Queensland School of Dentistry, including 21 years as Professor of Dental Science and 10 years as the Head of School. Since retiring in December 2020, Laurie has remained active in hands-on bench research work, as well as in supervising over 15 research students at UQ who work in advanced technologies and biomaterials and in clinical microbiology. Laurie has served as Chief Examiner in Microbiology for the RACDS for 21 years and as the Editor of the ADA Infection Control Guidelines for 12 years. His published research work includes over 400 journal papers, with a citation count of over 20,000 citations in the literature. Laurie holds patents in 8 families of dental technologies. He is currently ranked in the top 0.25% of world scientists. Laurie was made an Officer of the Order of Australia in January 2018 and a life member of ADAQ in 2020 in recognition of his contributions to dentistry.
References
1. Hefferren JJ. A laboratory method for assessment of dentifrice abrasivity. J Dent Res. 1976; 55(4): 563–573. DOI: 10.1177/0022034576055004030
2. Stookey GK, Muhler JC. Laboratory studies concerning the enamel and dentin abrasion properties of common dentifrice polishing agents. J Dent Res. 1968;47(4): 524-532. DOI: 10.1177/00220345680470040301
3. ADA Council on Dental Therapeutics. Abrasivity of current dentifrices. J Am Dent Assn 1970; 81(5): 1177-1178. PMID: 5272984
4. Grabenstetter RJ, Broge RW, Jackson FL, Radike AW. The measurement of the abrasion of human teeth by dentifrice abrasives: a test utilizing radioactive teeth. J Dent Res. 1958;37(6):1060-1068. DOI: 10.1177/00220345580370060601
5. Sabrah AHA, Lippert F, Kelly AB, Hara AT. Comparison between radiotracer and surface profile methods for the determination of dentifrice abrasivity. Wear 2013; 306 (1-2): 73-79. DOI: 10.1016/j.wear.2013.07.001. 6. ISO 11609: 2017. Dentifrices - Requirements, test methods and marking. URL https://www.iso.org/ standard/70956.html
7. González-Cabezas C, Hara AT, Hefferren J, Lippert F. Abrasivity testing of dentifrices - challenges and current state of the art. Monogr Oral Sci. 2013;23:100-7. doi: 10.1159/000350476.
8. Pontefract H, Courtney M, Smith S, Newcombe RG, Addy M. Development of methods to enhance extrinsic tooth discoloration for comparison of toothpastes. 1. Studies in vitro. J Clin Periodontol. 2004 Jan;31(1):1-6. doi: 10.1111/j.0303-6979.2004.00423.x.
9. Pontefract H, Courtney M, Smith S, Newcombe RG, Addy M. Development of methods to enhance extrinsic tooth discoloration for comparison of toothpastes. 2. Two-product clinical study. J Clin Periodontol. 2004;31(1):7-11. doi: 10.1111/j.0303-6979.2004.00422.x.
10. Schemehorn BR, Moore MH, Putt MS. Abrasion, polishing, and stain removal characteristics of various commercial dentifrices in vitro. J Clin Dent 2011;22:11-18. PMID: 21290981.
11. Stookey GK, Burkhard TA, Schemehorn BR. In vitro removal of stain with dentifrices. J Dent Res. 1982; 61(11): 1236-1239. doi: 10.1177/00220345820610110501.
12. American Dental Association Health Foundation Research Institute. Clinical methods for determining dentifrice-cleaning ability. J Am Dent Assoc. 1984;109(5):759-62. PMID: 6593364.
13. White DJ. Use of synthetic polymer gels for artificial carious lesion preparation. Caries Res. 1987;21(3):228–242. DOI: 10.1159/000261026.
14. White DJ. Reactivity of fluoride dentifrices with artificial caries I. Effects on early lesions: F uptake, surface hardening and remineralization. Caries Res. 1987;21(2):126-140. DOI: 10.1159/000261013.
15. White DJ. Reactivity of fluoride dentifrices with artificial caries. II. Effects on subsurface lesions: F uptake, F distribution, surface hardening and remineralization. Caries Res. 1988;22(1):27-36. DOI: 10.1159/000261079.
16. Duckworth RM, Lynch RJ. Fluoride uptake to demineralised enamel: A comparison of sampling techniques. Caries Res. 1998;32(6):417-21. doi: 10.1159/000016481.
17. Karlinsey RL, Mackey AC, Walker TJ, Frederick KE, Blanken DD, Flaig SM, Walker ER. In vitro remineralization of human and bovine white-spot enamel lesions by NaF dentifrices: A pilot study. J Dent Oral Hyg. 2011;3(2):22-29. PMID: 21643437.
18. Cate JM, Timmer K, Shariati M, Featherstone JD. Effect of timing of fluoride treatment on enamel deand remineralization in vitro: a pH-cycling study. Caries Res. 1988;22(1):20-6. doi: 10.1159/000261078.
19. Sakkab NY, Cilley WA, Haberman JP. Fluoride in deciduous teeth from an anti-caries clinical study. J Dent Res. 1984 Oct;63(10):1201-5. doi: 10.1177/00220345840630100601.

The problems of pipes: A key challenge in infection prevention and control
By Emeritus Professor Laurence J. Walsh AO

Many components of infection prevention and control in dental practice relates to what can be called “the problems of pipes” - preventing pipes from becoming blocked, removing hard mineralised and soft microbial deposits and bioburden from pipes, effective cleaning of pipes and sterilisation of pipes (Table 1).
This article explores several of these elements and highlights the implications for everyday infection control protocols.
Triplex tips
Water which runs through dental units is not free of ions and most dental units use reticulated water (tap water), to which various chemicals are added to slow the growth of microbial biofilms. With a metal triplex tip which is of the DCI design, one pipe sits within another pipe and the inner pipe is held in place by crimping of the outer pipe. This creates a situation where tap water can be retained within the metal triplex tip when it reaches the chamber of the steam steriliser (autoclave). This then creates the possibility
26 oral|hygiene March/April 2024
READ ME FOR CPD infection | CONTROL
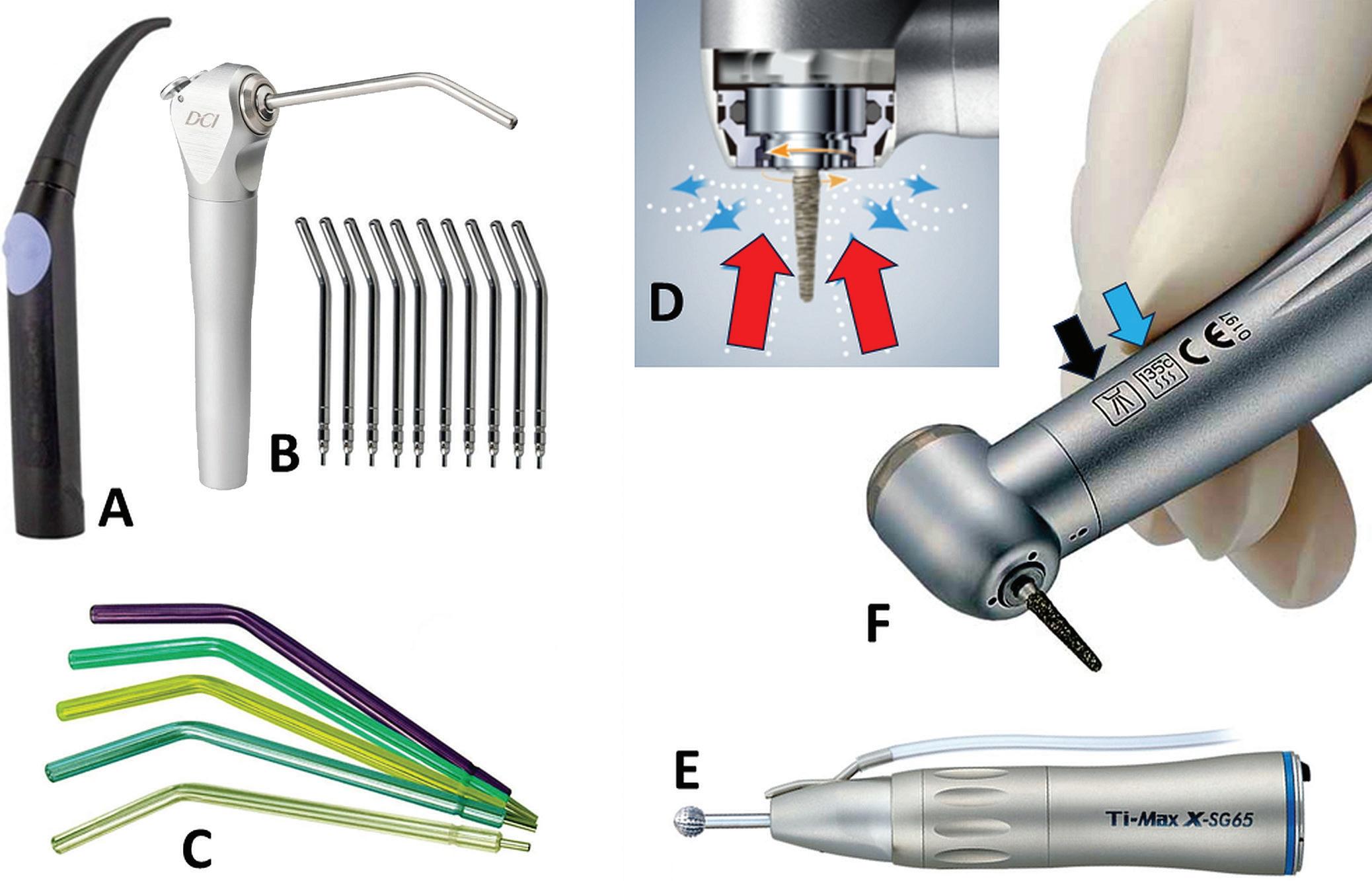
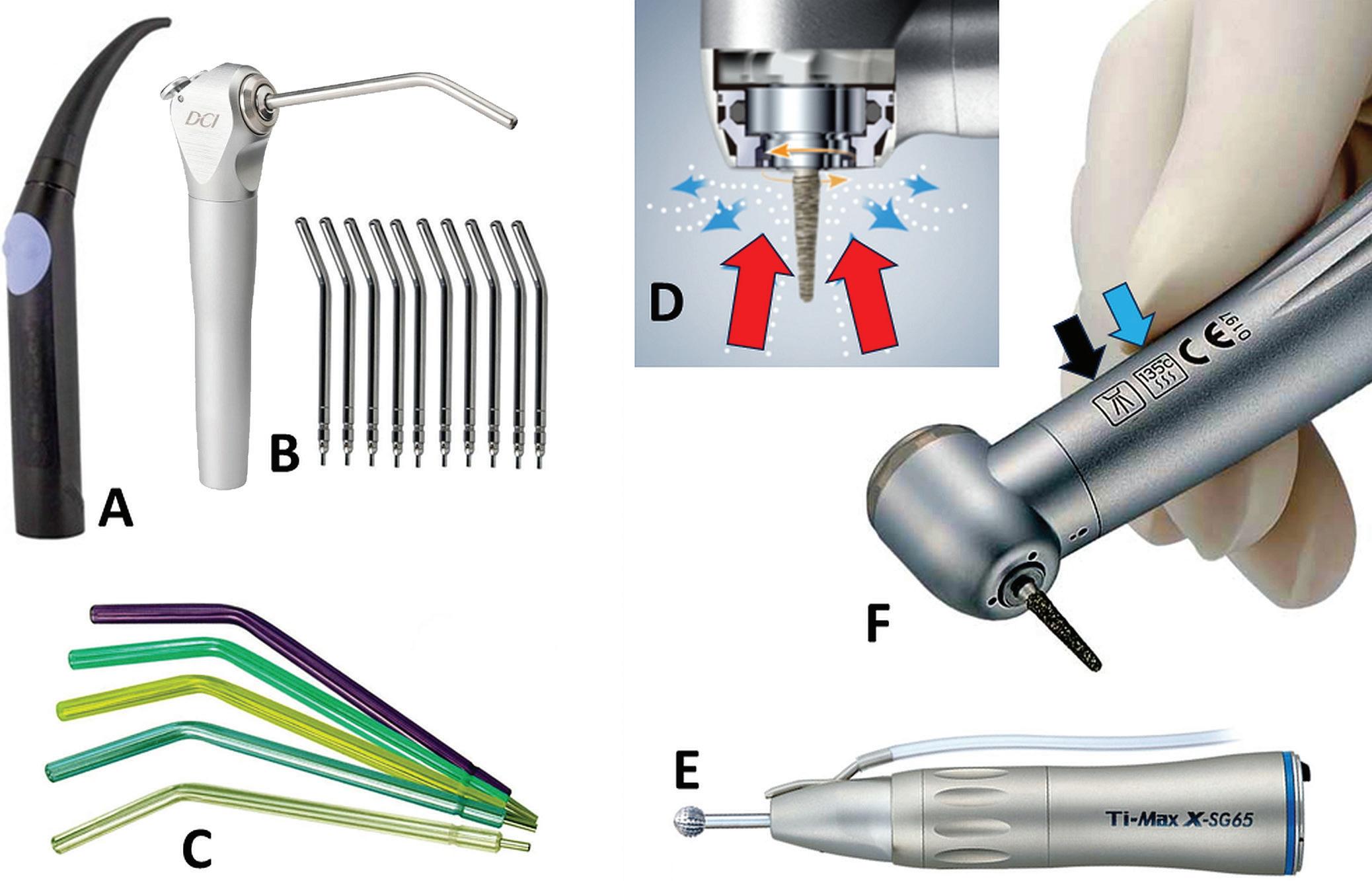
Figure 1. A. A specially designed triplex tip where the water and air pipes are kept separate. B. A traditional DCI triplex with metal tips (one pipe inside the other). C. Disposable plastic triplex tips. D. Air movements during the operation of an air turbine handpieces, with air moving outwards during use (blue arrows) and then air moving inwards as the pressure collapses when the handpieces turned off (red arrows). E. Surgical handpiece with external pipe for irrigation fluids. F. Restorative handpiece showing the symbols for reprocessing in a washer-disinfector (black arrow) and steam sterilisation (blue arrow).
for the precipitation of mineral scale within the metal triplex tip during the drying phase of the steam steriliser cycle.
Careful examination of metal triplex tips used in large clinics has documented the ubiquitous presence of such deposits.1 As they build up, they occlude the proper flow of water and air through the metal triplex tip. This is the reason why the use of metal DCI triplex tips has become less common over the past decade. Several European dental chair manufacturers have addressed the issue by having triple syringe designs where there are completely separate water and air lines (Figure 1A), thereby avoiding the capillary effect which traps fluid in the traditional DCI design (Figure 1B). There are disposable triplex tips (Figure 1C) and also several systems for converting the fittings to use other types of disposable plastic triplex tips.
Dental handpieces
When an air turbine is being used, the rotating burr creates aerosols that move away rapidly from the
Table 1. Key problems of pipes in the dental practice setting
Location Deposit type Implications
Triplex tip Mineral scale Partial or complete occlusion lowers air and water flow. Not possible to remove with chemical agents. Need to replace metal DCI/A-dec tips regularly.
Handpieces Lubricants Residues cause impaired sterilisation.
Residues expressed into the mouth contaminate treated teeth. Must run handpiece after lubrication to remove lubricant.
Bioburden Retraction of material from patients entering internal aspects. Routine use of anti-retraction systems. Sterilisation of handpieces using air removal processes.
Autoclave Mineral scale Impaired steam flow causing failed cycles. Must use only demineralised water for steam generation.
Waterlines Biofilms Health risk to patients and staff from aerosolized irrigants. Must use chemical treatments, monitor and shock when needed.
Suction Mineral scale Impaired evacuation because of lowered air flow. Weekly use of chelators to remove mineral scale.
Biofilms Creates unpleasant odours in the clinical working area. At least daily use of suction cleaners with disinfecting actions.
March/April 2024 oral|hygiene 27
handpiece.2-5 When the foot control is released, as the burr decelerates to reach a complete stop, negative pressure is generated around the head of the handpiece (Figure 1D).
This can draw material into the internal aspects of the handpiece. It is possible for patient material (e.g. fragments of DNA) and oral microorganisms to be found in the turbine capsule following use. This drove the universal use of anti-retraction valves on handpiece couplings, flushing between patients and also the development of anti-retraction systems within air turbine handpieces (so-called “clean head” designs).6
A further consequence was the routine steam sterilisation of air turbine handpieces between patients seen in dental practices in Australia and in North America.7,8 Somewhat surprisingly, there are still parts of the world, including in Europe, where air turbine handpieces are not sterilised routinely between patients and the accompanying research in such places has demonstrated the potential for cross contamination to occur, with the dental handpiece being the vector for that.9
Steam sterilisers
Within a steam steriliser, there are a range of different pipes, which carry steam and remove air. To prevent the buildup of mineral scale within the pipes of a steam steriliser, the level of ions must be sufficiently low that precipitation will not occur.
Most modern steam sterilisers have a circuit which checks the electrical conductivity of the water which is added to the steam steriliser for steam generation, to give a fault signal and prevent a cycle from starting when the level of ions in the feed water is excessive. Simple, low-cost handheld digital meters can also check water conductivity, e.g. by measuring total dissolved solids (TDS). Using such a meter is essential as a quality check when dental practices purchase demineralised water, e.g. from a local supermarket.
Regrettably, if the quality of feed water is poor and mineral scale deposits do form in the steam lines, there is no simple procedure which can be done by the end user to address this problem. Hence, the focus is on prevention from the outset.
Waterlines
The fundamental problem in waterlines that carry irrigation fluids is stagnation. Water flow only occurs at low volumes and is irregular. This provides ample time for microorganisms to settle onto the walls of the tubing and to form biofilms.10,11
Waterlines that carry irrigation fluids are found in a range of benchtop devices (such as stand-alone ultrasonic scalers) as well is in dental chairs. Hence, it is important to consider how to prevent biofilm overgrowth occurring in any lines that carry irrigation fluids.
The feed water supplied to dental chairs can be rendered sterile by ozonation or by ultrafiltration. This prevents repeated inoculation of the waterlines with waterborne bacteria.
The dental chair manufacturer’s instructions will often provide advice on suitable additives and treatment protocols for waterline maintenance.
These can vary from one brand to the next, because of the compatibility of the internal components. For example, if the dental chair (or benchtop device) contains O-rings which are made from natural rubber latex, those systems will be unsuitable for ozonated water, since this will attack by oxidation the isoprene polymer structure of natural rubber latex. On the other hand and as is usually the case, the O-rings may be made from a synthetic rubber (such as neoprene) and ozonated water can be used without concerns of damage.
Treatment agents for waterlines fall into 2 major types: those that inhibit the growth of biofilms and those that disrupt and detach biofilms.10-14 These different effects can be achieved by changing the chemical composition of the treatment agent, its concentration or the exposure time. This is why shock treatments (also known as disinfection or sanitising treatments) employ high concentrations of chemical agents and often prolonged exposure times from several hours to overnight.
In some cases, chelating agents are included in shock treatment products. These are designed to break down any mineralised deposits that may have formed deep in the biofilm and to interfere with the binding of biofilms onto the walls of tubing.
Suction systems
Plentiful exposure to water, saliva and blood makes suction lines ideal for microbial growth. Repeated exposure to oral microorganisms inoculates these lines on a frequent basis. Extensive growth of microorganisms can lead to coloured microbial deposits and the generation of unpleasant odours when the biofilms are nourished with blood. This reinforces the need for frequent flushing of suction systems with water, not only at the end of a patient appointment, but during a patient appointment. During oral surgical procedures, flushing sterile saline or sterile water can be undertaken.
Products designed for the maintenance of suction systems will typically have 2 different formulations available. One of these will be designed for use at least once per day or more often and will contain low foaming surfactants and low-level disinfectants. The second formulation will be designed for use once per week and will contain agents that dissolve mineral scale, such as sulfamic or other acids. In situations where a practice is doing frequent perio and oral surgical procedures where bleeding will be occurring, it may be necessary to flush the lines with the daily product several times during the day to prevent the development of odours from the suction lines when they are not being used. Likewise, in locations where the tap water that is fed into the dental unit is moderately hard, the weekly product which dissolves mineral scale may need to be used more often.
Cleaning pipes
Devices that have pipes, channels or lumens are much more difficult to clean than those with flat surfaces. Lumened items are not cleaned effectively by ultrasonic cleaners. This reinforces the value of washer-disinfectors, since these can be fitted with specific couplings to connect the flushing system of the WD with the item of interest, whether that be a dental handpiece, relative analgesia tubing or high velocity evacuation/suction tips. Several modern brands of high-speed air turbine handpieces and low-speed contra-angle handpieces are designed for cleaning in a WD and are marked with a “flushing” symbol to indicate this (Figure 1F).15-17
28 oral|hygiene March/April 2024
infection | CONTROL
Older dental handpieces will not be compatible with the highly alkaline detergents that are used in a WD and will undergo corrosion. Hence, it is essential for staff to check compatibility of items and to follow the handpiece manufacturer’s instructions for reprocessing.
The challenges of cleaning items with smaller narrow pipes is not unique to dentistry. The rise of minimally invasive surgical approaches using endoscopes has led to numerous developments for devices and technologies that can better clean the channels of endoscopes and render these free of patient tissue remnants, blood and microorganisms.18 A range of highly sensitive protein soil tests and borescopes have been developed specifically to evaluate how well devices such as automated endoscope reprocessors (AERs) are achieving their stated aim.19,20
A range of novel technologies have been developed to clean endoscope channels by using nanotechnology approaches. The foremost of these, known as “Nanoclean”, involves flushing the channels with water containing microfibrillated cellulose (MFC) with low levels of embedded silica abrasives. As the water flows through the channel, these MFC nanoparticles move along the walls where they scour away bioburden.21-24 The MFC are from a natural source and are classified as “generally recognised as safe”, which means that ingestion is not problematic, since cellulose is the normal form of dietary fibre.
With some minor modifications, the same nanoparticle cleaning concept can be applied to pipes in a dental setting. In a proof-of-concept study (Figure 2), biofilms were developed in the waterlines of a small dental unit under defined laboratory conditions, using stagnation. The biofilm deposits in the tubing were then stained using crystal violet dye. “Biopsy” segments of the transparent tubing were taken. Flushing through Nanoclean removed the biofilm deposits in a short time period (less than 2 minutes), replicating what had been seen when this same approach is used to clean endoscope channels. With further optimisation and validation, this approach could provide a worthwhile strategy for dental units. By achieving the physical removal of biofilm, the need for more aggressive chemical treatments such as shocking could be reduced.

Figure 2. Proof of concept laboratory study for the removal of dental unit waterlines biofilms using micro-fibrillated cellulose (Novaflux NanoClean™). A, The small dental unit used in the study. B, Feed water tubing connected to a peristaltic pump, which was operated intermittently to create realistic use conditions. C, Scanning electron micrograph at 5,400X showing organisms growing on the walls of the dental handpiece tubing. D, Scanning electron microscope image at 20,000X showing the meshwork structure of the micro-fibrillated cellulose nanoparticles that were used to mechanically clean biofilm from the waterline tubing. E, A biofilm tubing cutout “biopsy” sample of clear waterline tubing stained with crystal violet dye, showing the intense purple colouration of the biofilm through the transparent tubing. F, A biofilm tubing sample immediately after 90 seconds of flushing using a solution of NanoClean, showing complete lack of staining. Complete removal of biofilm was confirmed by subsequent scanning electron microscope examination.
Sterilising pipes
Awide array of process challenge devices (PCDs) exist in the market, with some of these being designed explicitly as air removal and steam penetration tests (ARSPTs).25,26 With the release of ISO 11140.6 in November 2022,27 the older terminology of “hollow load type A” has now been replaced by referring to the level of challenge for air removal and steam penetration being equivalent to the reference hollow load of this same ISO standard.
The 2022 date of this ISO standard also explains why older standards, such as EN 13060 for small steam sterilisers28 and older operating manuals for steam sterilisers, use the older terminology of the “hollow load type A”, while AS 5369, which was published in December 2023, does not.
March/April 2024 oral|hygiene 29
infection | CONTROL
Several factors influence the performance of ARSPTs that use a pipe design, including those where, to reduce the overall size, the pipe has been formed into a coil. These factors include the material of manufacture of the pipe, its wall thickness, length and diameter. When the pipe is made of a plastic polymer, its performance as an ARSPT changes at a high number of use cycles due to thermal degradation of the polymer. This is why PCDs with plastic polymer pipes have a limited number of use cycles (e.g. 50 or 100), while those with metal pipes have an indefinite number of use cycles.
A range of processes can be used to sterilise items with pipes, with moist steam and hydrogen peroxide gas vapour (HPGV) being the two most well-known for officebased dental practice settings. Air can be removed from pipes in handpieces and other devices by either positive or negative pressure. In the case of positive pressure, bursts of steam from a small steam generator will gradually displace the air from the pipe; typically 2 or 3 bursts will be needed. This approach is used in several bespoke S cycle steam sterilisers, such as the SciCan Statim™ and the Nitram/Sirona DAC Universal™. Negative pressure employs a vacuum pump to evacuate the chamber before the sterilant (moist steam or HPGV) is introduced. Typically, 2 or 3 negative pressure vacuum cycles are used. It is essential that no air leaks into the chamber through the door seal or other locations during these vacuum phases and this is why vacuum/ air leak tests are used with pre-vacuum steam sterilisers. Overall, the pre-vacuum approach can deal with much greater challenges in terms of air removal and so is the preferred way for pipes that are longer and thinner, since these pose the most difficulty. This is the reason why the instructions for surgical dental handpieces state that they are to be sterilised in a pre-vacuum cycle.
Conclusions:
Preventing the problems of pipes
The many devices and items used in dentistry that contain pipes make it essential that staff understand issues of prevention, maintenance and reprocessing associated with these. All devices with pipes will present potential problems that need to be addressed by following the manufacturer’s instructions carefully and ensuring that the necessary performance checks are being undertaken.
References
1. Edwards C, Bennani V, Chandler N, Lowe B. Effectiveness of disposable (single-use) tips for dental air-water syringes. Eur J Prosthodont Restor Dent. 2015;23(4):187-91.
2. Gallagher JE, K C S, Johnson IG, Al-Yaseen W, Jones R, McGregor S, Robertson M, Harris R, Innes N, Wade WG.A systematic review of contamination (aerosol, splatter and droplet generation) associated with oral surgery and its relevance to COVID-19. BDJ Open. 2020;6:25.
3. Innes N, Johnson IG, Al-Yaseen W, Harris R, Jones R, Kc S, McGregor S, Robertson M, Wade WG, Gallagher JE. A systematic review of droplet and aerosol generation in dentistry. J Dent. 2021;105:103556.
4. Johnson IG, Jones RJ, Gallagher JE, Wade WG, AlYaseen W, Robertson M, McGregor S, K C S, Innes N, Harris R. Dental periodontal procedures: a systematic review of contamination (splatter, droplets and aerosol) in relation to COVID-19. BDJ Open. 2021;7(1):15.
5. Puljich A, Jiao K, Lee RSB, Walsh LJ, Ivanovski S, Han P.Simulated and clinical aerosol spread in common periodontal aerosol-generating procedures. Clin Oral Investig. 2022;26(9):5751-5762.
6. Montebugnoli L, Dolci G, Spratt DA, Puttaiah R. Failure of anti-retraction valves and the procedure for between patient flushing: a rationale for chemical control of dental unit waterline contamination. Am J Dent. 2005;18(4):270-4.
7. Cannata S, Bek M, Baker P, Fett M. Infection control and contaminated waste disposal practices in Southern Sydney Area Health Service Dental Clinics. Aust Dent J. 1997;42(3):199-202.
8. Molinari J. Dental infection control at the year 2000: accomplishment recognized. J Am Dent Assoc. 1999;130(9):1291-8
9. Sasaki JI, Imazato S. Autoclave sterilization of dental handpieces: A literature review. J Prosthodont Res. 2020;64(3):239-242.
10. O’Donnell MJ, Boyle MA, Russell RJ, Coleman DC. Management of dental unit waterline biofilms in the 21st century. Future Microbiol. 2011;6(10):1209-26.
11. Spagnolo AM, Sartini M, Cristina ML. Microbial contamination of dental unit waterlines and potential risk of infection: a narrative review. Pathogens 2020;9:651.
12. Ji XY, Fei CN, Zhang Y, Liu J, Liu H, Song J. Three key factors influencing the bacterial contamination of dental unit waterlines: a 6-year survey from 2012 to 2017. Int Dent J. 2019;69(3):192-199.
13. Lizzadro J, Mazzotta M, Girolamini L, Dormi A, Pellati T, Cristino S. Comparison between two types of dental unit waterlines: How evaluation of microbiological contamination can support risk containment. Int J Environ Res Public Health. 2019;16(3):328.
14. Allison JR, Dowson C, Jakubovics NS, Nile C, Durham J, Holliday R. Waterline disinfectants reduce dental bioaerosols: a multitracer validation. J Dent Res. 2022;101(10):1198-1204.
15. Offner D, Scholler J, Musset AM. Cleaning of dental handpieces and associated parameters: Internal and external cleaning, drying and rotation. Am J Dent. 2021;34(3):137-142.
16. Deasy EC, Scott TA, Swan JS, O’Donnell MJ, Coleman DC. Effective cleaning and decontamination of the internal air and water channels, heads and head-gears of multiple contra-angle dental handpieces using an enzymatic detergent and automated washer-disinfection in a dental hospital setting. J Hosp Infect. 2022;128:80-88. d
17. Coleman DC, Deasy EC, Swan JS, O’Donnell MJ, Scott TA. Direct evidence for effective cleaning and decontamination of the internal air and water channels, heads and head-gears of multiple contra-angle dental handpieces using an enzymatic detergent and automated washer-disinfection in a dental hospital setting. J Hosp Infect. 2023;135:204-205.
18. Chiu KW, Lu LS, Chiou SS. High-level disinfection of gastrointestinal endoscope reprocessing. World J Exp Med. 2015;5(1):33-9.
19. Ofstead CL, Smart AG, Hopkins KM, Wetzler HP. The utility of lighted magnification and borescopes for visual inspection of flexible endoscopes. Am J Infect Control. 2023;51(1):2-10.
20. Hopkins KM, Adams SJ, Lamb LA, Smart AG, Ofstead CL. Beyond endoscopes: pilot study of surgical instrument lumen inspection. Biomed Instrum Technol. 2024;58(1):2533.
21. Tabani Y, Labib ME. Method for cleaning hollow tubing and fibers. US patent No. 6,945,257. 2005.
22. Sohn SY, Alfa MJ, Lai R, Tabani Y, Labib ME. Turbulent fluid flow is a novel closed-system sample extraction method for flexible endoscope channels of various inner diameters. J. Microbiol. Methods 2020; 168:105782.
23. Labib ME, Duhkin SS, Tabani Y, Lai CY, Manganaro JL, Materna P, Roberston JC. Compositions for cleaning and decontamination. U.S. patent 10,266,793. 2019.
24. Labib ME, Duhkin SS, Tabani Y, Lai CY, Manganaro JL, Materna P, Roberston JC, Sohn SY. Cleaning com-position with superabsorbent polymer. U.S. patent 11,345,878. 2022.
25. Rodrigues SB, de Souza RQ, Graziano KU, Erzinger GS, Souza O. Performance evaluation of chemical, biological and physical indicators in the process of sterilization under the effect of non-condensable gases. J Hosp Infect. 2021;108:1-6.
26. Miguel EA, Laranjeira PR, Ishii M, Pinto TJA. Analysis of water quality over non-condensable gases concentration on steam used for sterilization. PLoS One. 2022;17(9):e0274924.
27. ISO 11140-6:2022. Sterilization of health care products. Chemical indicators. Part 6: Type 2 indicators and process challenge devices for use in performance testing of small steam sterilizers. URL https://www.iso.org/standard/66625.html
28. EN 13060 Small steam sterilizers (includes Amendment :2018). URL https://standards.globalspec.com/ std/13216824/DIN%20EN%2013060
About the author
Emeritus Professor Laurence J. Walsh AO is a specialist in special needs dentistry who is based in Brisbane, where he served for 36 years on the academic staff of the University of Queensland School of Dentistry, including 21 years as Professor of Dental Science and 10 years as the Head of School. Since retiring in December 2020, Laurie has remained active in hands-on bench research work, as well as in supervising over 15 research students at UQ who work in advanced technologies and biomaterials and in clinical microbiology. Laurie has served as Chief Examiner in Microbiology for the RACDS for 21 years and as the Editor of the ADA Infection Control Guidelines for 12 years. His published research work includes over 400 journal papers, with a citation count of over 20,000 citations in the literature. Laurie holds patents in 8 families of dental technologies. He is currently ranked in the top 0.25% of world scientists. Laurie was made an Officer of the Order of Australia in January 2018 and a life member of ADAQ in 2020 in recognition of his contributions to dentistry.
30 oral|hygiene March/April 2024
High-performance sterilization- and drying system

5“ high-resolution colour touch display for intuitive navigation
3-fold flexible fresh water supply with integrated quality control
All in view and documented thanks to connection to the practice network


With Hygoclave 50, Dürr Dental and A-dec offers dental practices a professional Class B solution that combines impressive performance with a well thought-out operating concept – for maximum efficiency and exceptional user friendliness designed to cope effortlessly with tough day-to-day working environments. Available with a volume of 17 or 22 litres. More information under www.duerrdental.com
Hygiene is in our DNA. The Hygoclave 50.
Contact your local A-dec dealer 1800 225 010 Contact your local A-dec dealer 1800 225 010
Integrated dust protection filter

The most effective calculus removal
Your
role in recognising and healing supervised neglect related to burnished calculus
By Tami Wanless
Supervised neglect is defined by Mosbys Dental Dictionary as a case in which a patient is regularly examined and shows signs of a disease or other medical problems, but is not informed of its presence or progress (Mosby’s Dental Dictionary: Edition 2, 2007).1
A sound clinician would never intentionally leave calculus, let alone burnished calculus, but what if you learned today that you were leaving deposit contributing to chronic gingival disease? Are you practising Supervised Neglect? Whether you’re a new graduate or a seasoned professional, here is what you need to know to start making positive changes on your next patient.
What is burnished calculus?
W hen describing calculus attachment to my patients, I like to use the analogy that the calculus attaches to the tooth like a barnacle attaches to a boat. Barnacles actually produce cement that is released through the tips of their antennules to attach themselves.2 Calculus attaches by mechanically interlocking to the crystals of the tooth using the acquired pellicle.3 Burnished calculus is a subgingival deposit that has had its

How does tissue respond to a burnished deposit?
outermost layer shaved off and not fully removed, so the surface is smooth, but is still attached to the tooth surface contributing to disease.4,5 When a clinician does not recognise or remove burnished calculus, they are practising Supervised Neglect. One wouldn’t “plane away” a barnacle off a boat, nor should you “shave away” calculus from a tooth; in either scenario you will leave the source of the irritant.
These areas of burnished deposits will contribute to persistent gingival inflammation and bleeding in addition to providing a constant food source for more bacteria to attach. This vicious cycle will continue until you completely remove ALL the calculus. We set our patients up for failure when we tell them to brush and floss to reduce recurrent bleeding when we leave burnished deposit subgingivally every six months.
32 oral|hygiene March/April 2024 READ ME FOR CPD
clinical | EXCELLENCE



Instrument reprocessing solutions
Instrument reprocessing solutions
Instrument reprocessing solutions
has revolutionised sterilisation by offering a compact, dedicated line that provides unparalleled performance!
Mocom has revolutionised sterilisation by offering a compact, fully dedicated line that provides unparalleled performance!
Mocom has revolutionised sterilisation by offering a compact, fully dedicated line that provides unparalleled performance!






Washing Drying Disinfection
Decontamination Washing Drying Disinfection
M: 0427 816 459 • F: (02)46328456 • sales@mocomaustralia.co m.au • www.mocomaustralia.com.au
Sterilisation
Decontamination Washing Drying Disinfection Sterilisation 459 • F: (02)46328456 sales@mocomaustralia.co m.au • www.mocomaustralia.com.au
ULTRA SAFETY PLUS TWIST
How do you diagnose burnished calculus?
F rank periodontal disease is easy to identify; detecting Burnished Calculus can be just as easy once you change your approach. The patient who pristinely brushes and flosses regularly but has isolated areas of tissue colour change, slight inflammation or bleeding upon probing may be leading you to a burnished calculus area. Despite their dedication they will never heal until you detect the burnished area and remove it. Change the way you examine your patient to determine if burnished deposit is present. Before you pick up a scaler;
Burnished calculus is more likely to be found in areas on the root surface with developmental grooves, depressions, furcations and also at the cementoenamel junctions.
safe & easy
How do I remove burnished calculus and avoid supervised neglect?
areas. Establish secure solid fulcrums as close to the working area as possible. Avoid supervised neglect by removing deposit the first time you scale it. Clean up your practice by detecting existing burnished calculus and removing it with sharp instruments.
> Protects you and your staff from needle stick injuries
> Complies with latest regulations
> Intuitive device
DBarnacles on a boat cause drag and slow the vessel down. Burnished calculus contributes to chronic disease and overall inadequate systemic health. Be part of your patients’ total body health solution and not the cause of chronic disease as they navigate through life’s waters!
> Available with either sterile single use or sterilisable handle
1. Prudently view the colour and consistency of the gingival tissues, paying close attention to interproximal areas and line angles (where the tooth curves and you need to pivot on your fulcrum while rolling your instrument to adapt). Look for red or blue shades as well as swelling. The bodies first line of defense from any foreign object is to send in the white blood cells to turn tissue angry red and inflamed;
ull instruments are a significant cause of burnished calculus. If a hand instrument is extremely sharp at the onset of removing the calculus and stays sharp, it will eliminate deposit and not just shave layers away, leaving burnished bumps. When continued scaling with a dull edge occurs, the clinician shaves the deposit and begins to smooth the calculus without removing all of the bacteria. To avoid this:
Passive or active aspiration: security for the patient
2. Use a generous amount of air and blow towards the cervical tissue at a 45 degree angle and allow the tissue to distend while you look into the sulcus. Many times I have noticed undetected a burnished deposit when I’m using the air polishing unit. Try polishing prior to scaling in an effort to support the newest clinical success while locating burnished calculus at the same time; and
Transparent barrel: aspiration is clearly visible
Sliding protective sheath: protection from needle stick injuries
3. Pick up your posterior explorer (11/12) and gently search for irregularities. Lighten up your grasp like you’re holding a fragile piece of china. Feel for the slightest elevation. You will not feel that “clickable” deposit; burnished calculus will be a smooth raised bump.
It wasn’t me!
Leaving burnished calculus is more common than you believe. Research supports evidence demonstrating that blind root planing is only effective to 4mm. Beyond 4mm, 30-50% of the subgingival root surface is still covered with undetectable burnished calculus.6
• Start by using the sharpest instrument available for the maximum success in removing all the calculus from the start. Everedge 2.0 by Hu-Friedy is by far the sharpest instrument on the market. I am actually more effective with deposit removal using EE2.0 than any other instrument - it’s that sharp. Clinically, I am using fewer strokes and lighter lateral pressure on the lower anterior areas specifically, because they are that strong and sharp. There is less hand fatigue at the end of the day and I don’t need to sharpen nearly as often. They hold a sharper edge longer. I have never used any other instrument this sharp to compare it to;
• Another principle for effective calculus removal is to ensure that the blade-totooth angle is correct. If the terminal shank of the instrument is not parallel to the surface being scaled, then the angulation is either too open (greater than 70°) or too closed (less than 70°). To aid in correct angulation, a visual cue is used to ensure the terminal shank of the instrument is parallel to the surface being scaled;
• An incorrect grasp can cause a lack of enough lateral pressure to ensure that the sharpened blade grabs onto the calculus. Use a modified-pen grasp, ensuring you have enough space between your thumb and index finger to allow for rolling into the line angle
About the author
Tami Wanless is Adjunct Faculty in the department of Dental Hygiene at the College of DuPage in Glen Ellyn, IL, USA. She has a Master’s Degree in Adult Education from Northern Illinois University. Tami has 27 years of experience in the dental field with 24 of these in both the clinical and educational arenas. In her current role at the College of DuPage, Tami is a clinical educator, the didactic instructor for Head and Neck Anatomy and Histology and the didactic and laboratory instructor in the Science of Dental Materials. Tami authored the lab manual for the Science of Dental Materials. She speaks on a multitude of dental hygiene related topics - predominately instrument sharpening and public health issues. Additionally, Tami is the founder of Sharp Advantage, a nationwide instrument sharpening business. When not educating, sharpening, scaling or active in professional organizations, you might find Tami plotting the next dental mission trip. Tami is committed to organised dentistry and quality patient care.
References
1. Mosby’s Dental Dictionary: Edition 2. (2007). St. Louis: Elsevier.
2. Grunbaum, M. (2010, March 22). How do Barnacles attach to Whales? Science Line.
Two different positions:
3. Roberts-Harry EA, C. V. (2000 ;28). Subgingival calculus; where are we know? Journal dent, 93-102.
Holding Position (reversible)
4. Pattison, A. (2011, August 9). Burnished Calculus at the CEJ. Dimensions of Dental Hygiene, p. 74.
Locking Position (irreversible)
5. Pattison, Anna. Keys to Effective Calculus Removal, Dimensions of Dental Hygiene. October 2011; 9(10): 50-53.
6. Carroll, J. (2015, June 01). Exposing one of dentistry’s dirty little secrets. Modern Hygienist.










34 oral|hygiene March/April 2024 VISIT US ONLINE ©2016 Hu-Fried y Mfg. Ensure predictable
WHY DENTISTS FIT IS
Orders 0800 808 VISIT US ONLINE ©2016 Hu-Fried y Mfg.
Orders 0800 808 VISIT US ONLINE ©2016 Hu-Fried y Mfg. Ensure predictable
when WHY DENTISTS FIT IS
the Orders 0800 808 VISIT US ONLINE ©2016 Hu-Fried y Mfg. Ensure predictable
FIT IS Find the Orders 0800 808
You’ll quickly discover Because when
Find the
Ensure predictable You’ll quickly discover Because when WHY DENTISTS
You’ll quickly discover Because
Find
You’ll quickly discover Because when WHY DENTISTS
first
final
clinical | EXCELLENCE
A LONG-PROVEN EFFICACY
OF



EVERYTHING the right one with Hu-Friedy

for you. when it comes to the perfect fit, Hu-Friedy is just right.
A study demonstrated that when introduced in a dental school, Ultra Safety Plus was a the key success factor for avoiding needle stick injuries. With Ultra Safety Plus, needle stick injuries decreased from an average of 11.8 to 0 injuries per 1,000,000 hours worked(1)
STEEL PEDO CROWNS:
Septanest : the first choice of dentists with over 150 million injections per year, provides you high quality you can trust










ONLINE AT Co., LLC. All rights reserved. predictable outcomes for your littlest patients with Hu-Friedy Stainless Steel Pedo Crowns. discover why dentists favor our impeccable fit. Perfect for your patients. Easy for you. it comes to the perfect fit, Hu-Friedy is just right. DENTISTS LOVE OUR STAINLESS STEEL PEDO CROWNS: IS EVERYTHING the right one with Hu-Friedy 808 855 ww ONLINE AT Mfg. Co., LLC. All rights reserved. predictable outcomes for your littlest patients with Hu-Friedy Stainless Steel Pedo Crowns. discover why dentists favor our impeccable fit. Perfect for your patients. Easy for you. when it comes to the perfect fit, Hu-Friedy is just right. DENTISTS LOVE OUR STAINLESS STEEL PEDO CROWNS: 808 855 ww ONLINE AT Co., LLC. All rights reserved. predictable outcomes for your littlest patients with Hu-Friedy Stainless Steel Pedo Crowns. discover why dentists favor our impeccable fit. Perfect for your patients. Easy for you. it comes to the perfect fit, Hu-Friedy is just right. DENTISTS LOVE OUR STAINLESS STEEL PEDO CROWNS: IS EVERYTHING the right one with Hu-Friedy 808 855 ww ONLINE AT Mfg. Co., LLC. All rights reserved. predictable outcomes for your littlest patients with Hu-Friedy Stainless Steel Pedo Crowns. discover why dentists favor our impeccable fit. Perfect for your patients. Easy
DENTISTS LOVE OUR STAINLESS
IS
808 855 ww
(1) J.M Zakrzewska et al. Introducing safety syringes into a UK dental school – a controlled study. Brit Dent J 2001 ; 190; 88-92.
Call 0508 486 252 www.ivoclar.com
FREQUENCY
NEEDLE STICK INJURIES YEAR 1 YEAR 2 YEAR 3 YEAR 4 YEAR 5 ULTRA SAFETY PLUS INTRODUCTION


Clean. Disinfect. Lubricate. Purge. Dry. In 12 minutes.


Disinfect. Lubricate. Purge. Dry. In 12 minutes. Replace Manual with Mechanical. Clean. Disinfect. Lubricate. Purge. Dry. In 12 minutes. Replace Manual with Clean. Disinfect. Lubricate. Purge. Dry. In 12 minutes. Replace Manual with Mechanical.
Replace Manual with Mechanical.



T o t a l H a n d p i e c e M a i n t e n a n c e .
M: 0427 816 459 | P: (08) 9244 4628 E: sales@mocomaustralia.com.au | W: www.mocomaustralia.com.au
Clean.


























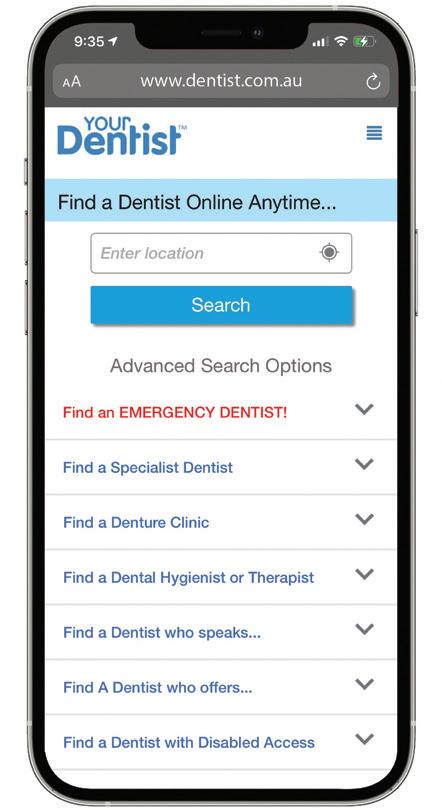
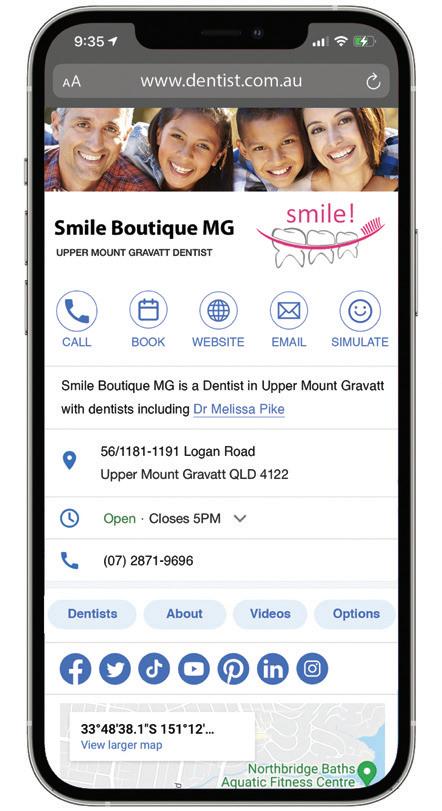
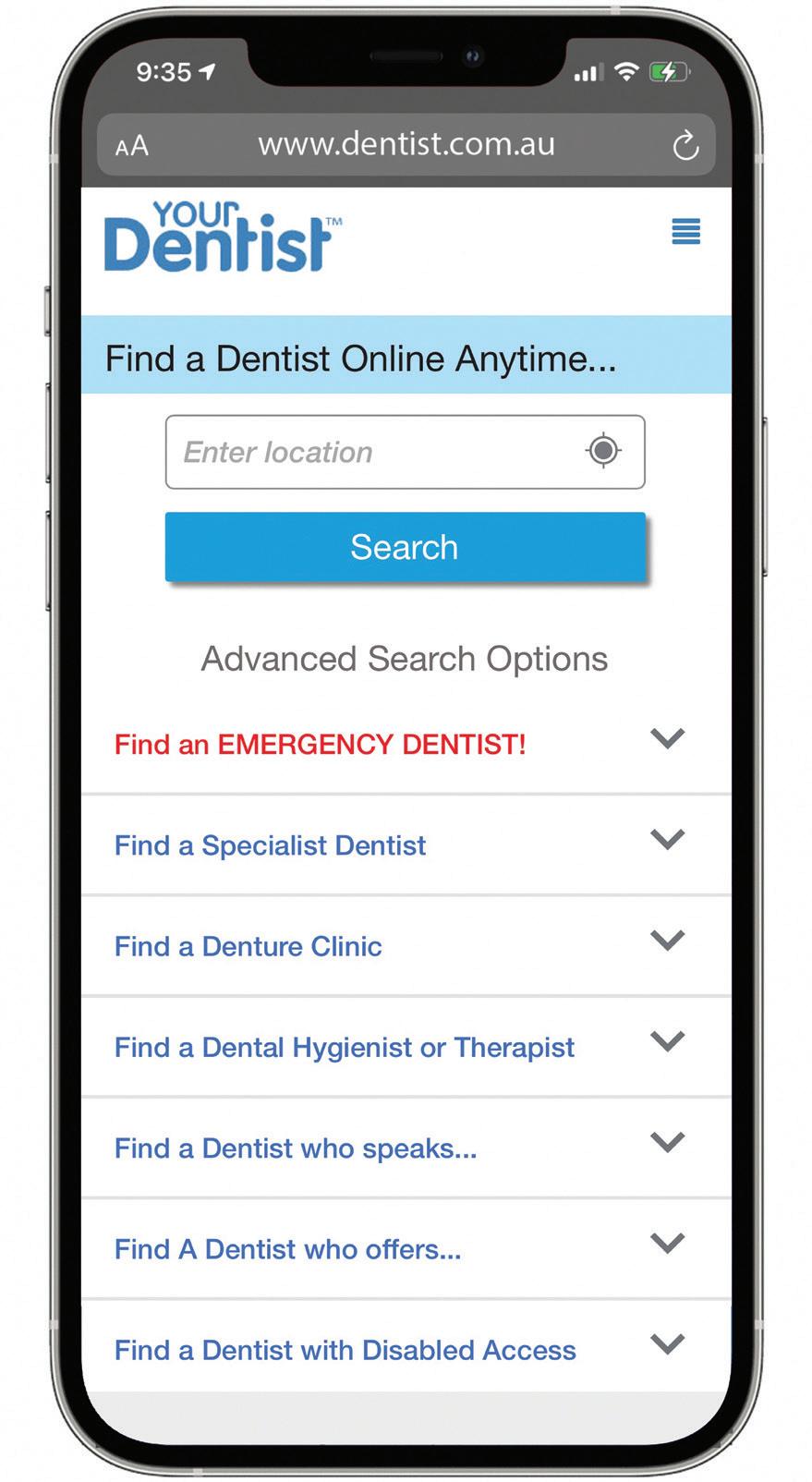
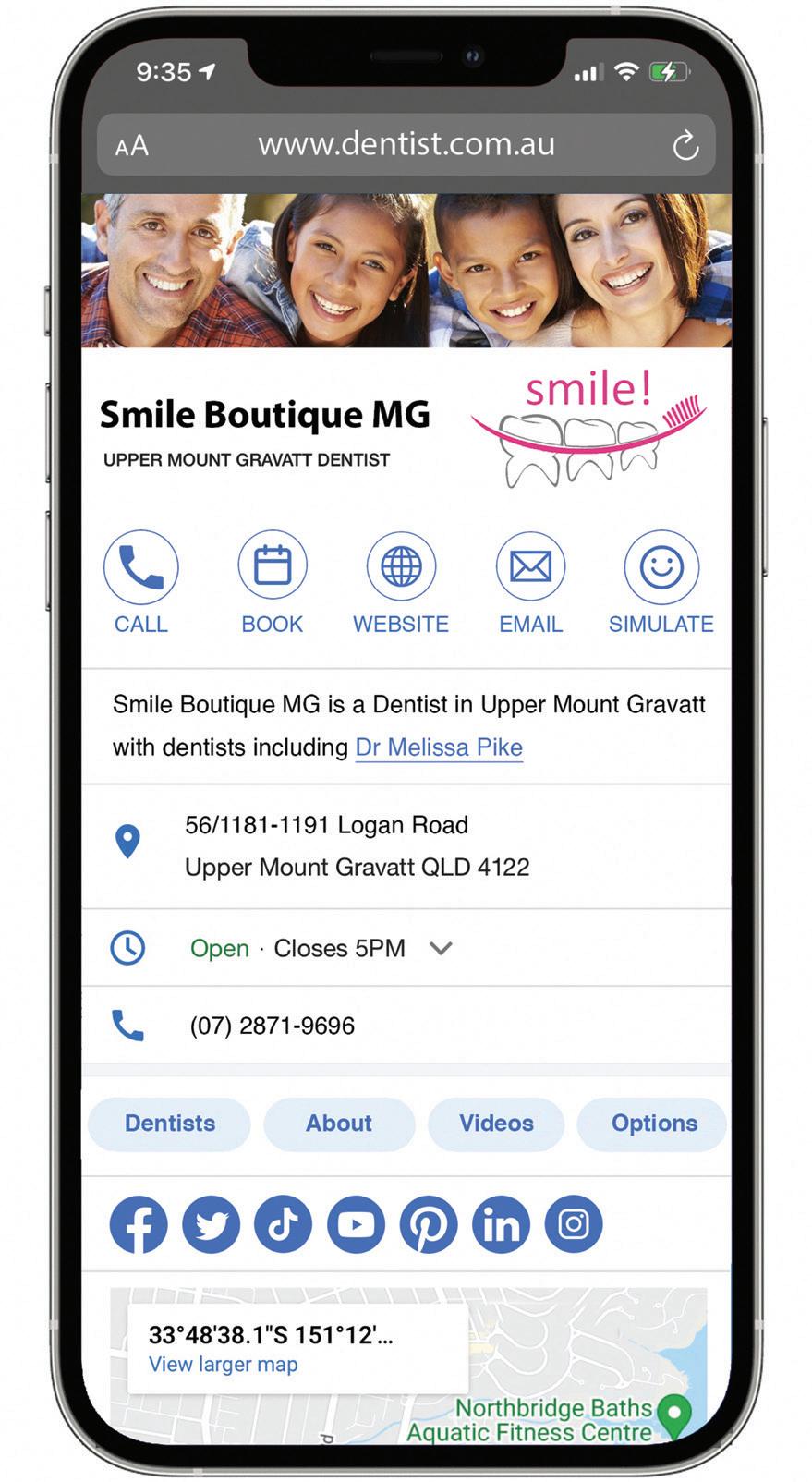
















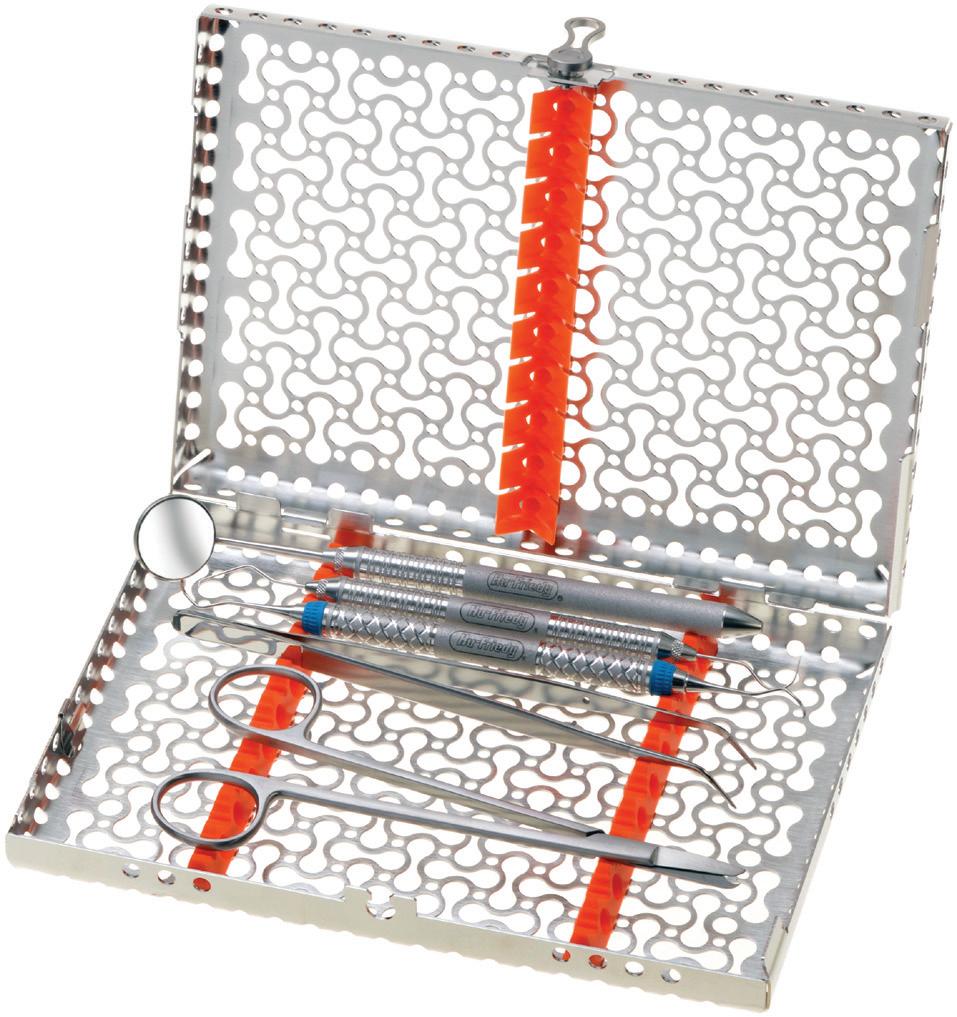
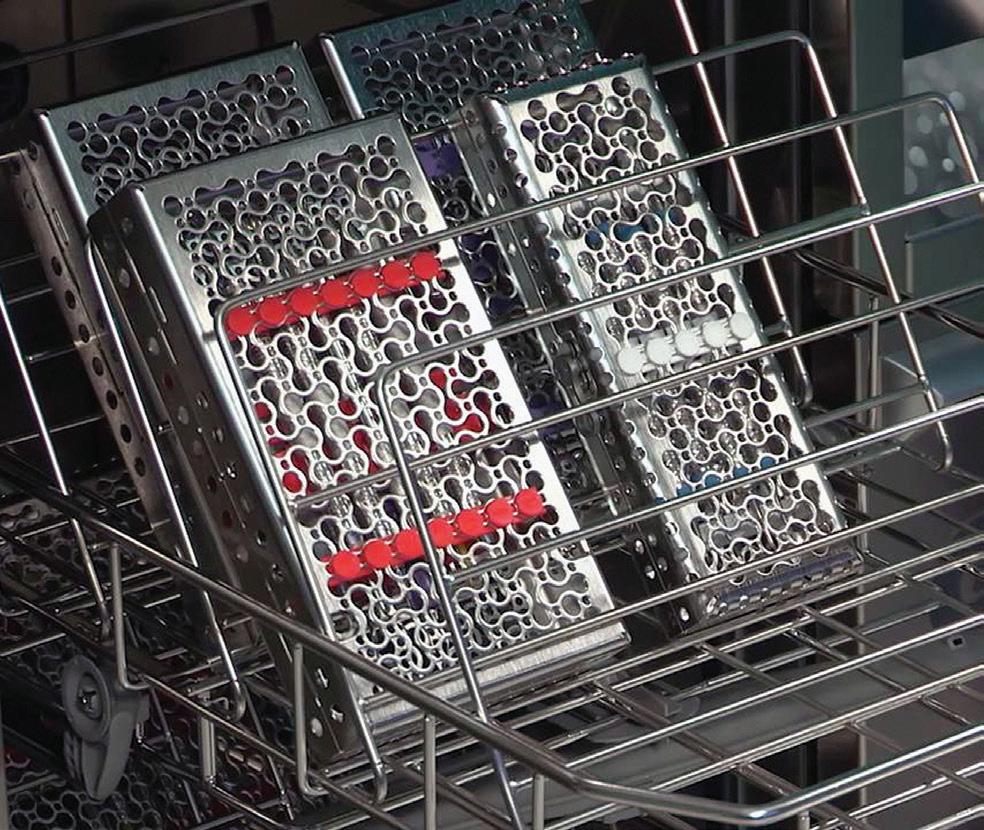
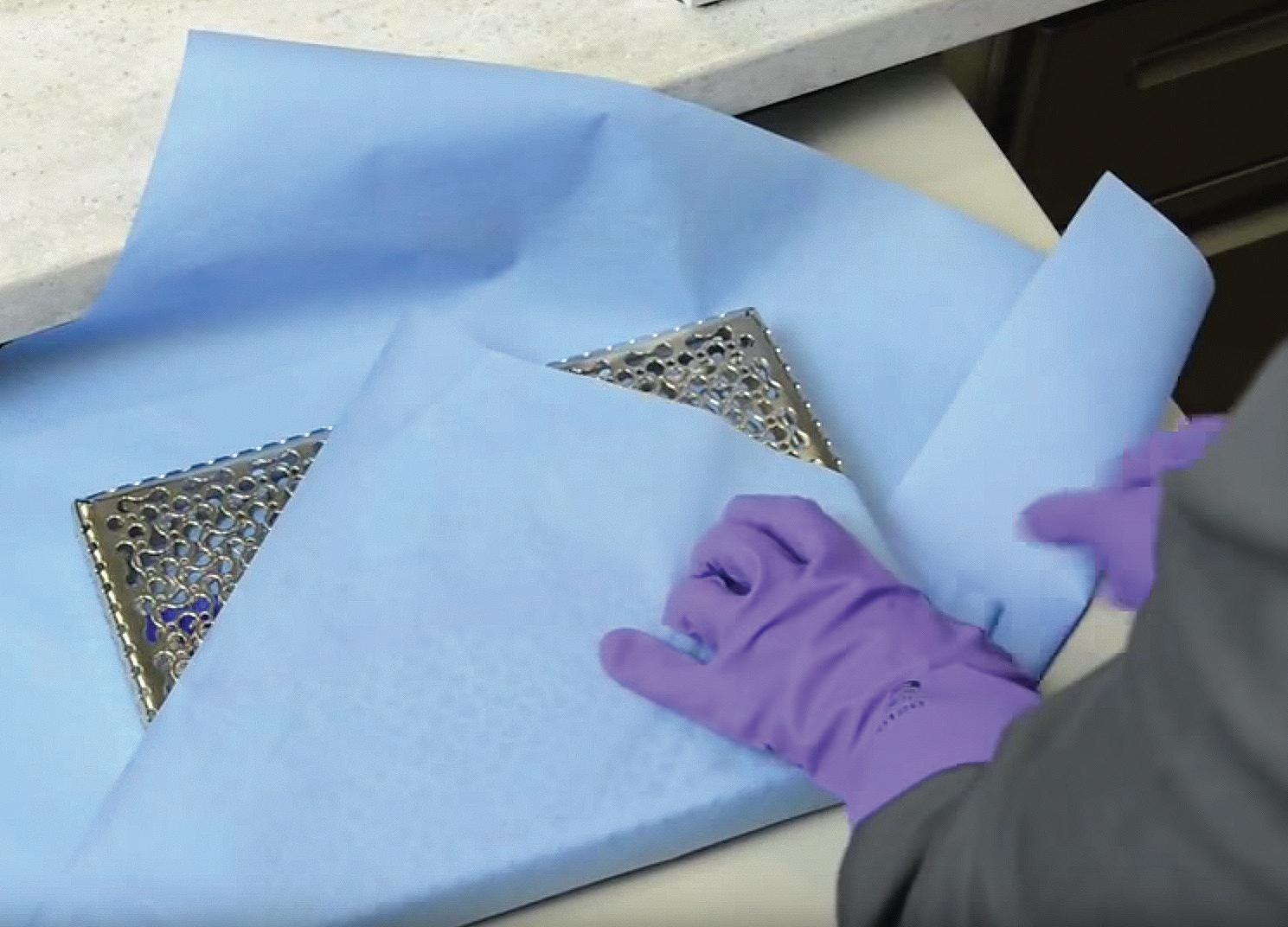





 By Tami Wanless
By Tami Wanless