

















Helps provide deep repair* and long-lasting protection against dentine hypersensitivity** 1-4
NO.1 BRAND FOR SENSITIVE TEETH5

Builds a strong hydroxyapatite-like layer deep within the tubules of exposed dentine for deep repair* and protection** 1,3,6-9
Reparative* hydroxyapatite layer is harder than underlying dentine and resistant to dietary acid and physical brushing 2,4,7,10

Proven for effective relief and long-lasting protection against dentine hypersensitivity** 11-13


*Forms a protective layer over the sensitive parts of the teeth. Brush twice a day for lasting sensitivity protection **With twice-daily brushing. Always read label and follow the directions for use.
References: 1. Greenspan DC. J Clin Dent 2010; 21:61–65. 2. Burwell A et al. J Clin Dent 2010; 21:66–71. 3. LaTorre G, Greenspan DC. J Clin Dent 2010; 21:72–76. 4. Earl JS et al. J Clin Dent 2011; 22:68–73. 5. GSK Consumer Healthcare calculation based in part on data reported by NielsenIQ and IQVIA through the IQVIA™ & NielsenIQ© RMS Sell Out] Service for the Oral Health Database, Sensitive Segment for the 52 week period ending 17/08/2021 for the Australia Grocery Pharmacy market according to the client defined product hierarchy. 6. Earl et al; J Clin Dent 2011; 22(3): 62-67(A). 7. Parkinson C et al. J Clin Dent 2011; 22(3): 74-81. 8. GSK Data on File; In vitro study number ML880; G7215/018; 2018. 9. GSK Data on File, Addendum to in vitro report ML880; 2021. 10. Wang Z et al. J Dent 2010; 38: 400-410. 11. Hall C et al; J Dent 2017; 60: 36–43. 12. GSK Data on File; Clinical Study number RH01748, 2013. 13. Hall, C et al; J Dent Res, 2017; 96 B:062 BSODR. Trade marks are owned by or licensed to the GSK group of companies. © 2022 GSK group of companies or its licensor. GlaxoSmithKline Consumer Healthcare Pty Ltd, Sydney, Australia. PM-AU-SENO-22-00121.
On the cover...
The new MyLunos air polishing handpiece from Dürr Dental sits comfortably in your hand due to its ergonomic design and interchangeable powder chambers eliminate the need to refill mid-treatment.

The COVID-19 pandemic has brought much greater attention to the risk factors that operate in the dental clinical setting and the importance of respiratory protection as one of the layers of defence explains Prof. Laurie Walsh
Running a practice takes a lot of work. Although all practices are different and face unique challenges, one common issue is optimal instrument management.
One of the most common things that we do is to detect white spot lesions and monitor their progress to determine if they are progressing towards cavitation, undergoing arrest, or regressing explains Prof. Laurie Walsh

Signature Series Tubs are designed to match Hu-Friedy IMS instrument cassette rail colours and feature antimicrobial product protection.
facebook.com/auxiliarynow twitter.com/auxiliarynow instagram.com/dentevents








Publisher & Editor: Joseph Allbeury
www.oralhygiene.com.au

Oral Hygiene (formerly Auxiliary) ISSN 1323-4919 is printed in Australia and published six times per year by Main Street Publishing P/L ABN 74 065 490 655 • PO Box 586, Cammeray 2062 Telephone: (02) 9929-1900 Facsimile: (02) 9929-1999 Email: info@dentist.com.au © 2022. All rights reserved. The contents of this magazine are copyright and must not be reproduced without the written permission of the publisher. Permission to reprint may be obtained upon application. Correspondence and manuscripts for publication are welcome. Although all care is taken, the editor and publisher will not accept responsibility for the opinions expressed by contributors to this magazine, or for loss or damage to material submitted for publication.


The new Cervitec Gel is recommended especially for the care of at-risk areas. The oral care gel with optimized care formula contains chlorhexidine, fluoride, xylitol and provitamin D-panthenol. With the new formula, Cervitec Gel protects the teeth, gums, peri-implant tissue and mucuous membrane with even more efficiency. Cervitec Gel supports the treatment of gingivitis, mucositis, denture stomatitis, periodontitis and peri-implantitis and helps combat elevated bacterial counts. It prevents inflammation and freshens breadth. Provitamin D-panthenol and xylitol moisturize and protect the gums and mucous membrane. Depending on the situation, the gel is applied either directly on the oral mucous membrane or removable restoration and distributed with an interdental brush or used to brush teeth. Given its smooth consistency, the clear gel can be optimally distributed on complex surfaces, e.g. implant restorations. Cervitec Gel can be applied in the dental office or at home. Cervitec Gel is widely accepted due to its mild taste. The soothing ingredients leave a pleasant feeling in the mouth. Available from Ivoclar on 1300-486-252 or visit www.ivoclar.com
The Dental Community website offers members of the dental profession a range of tools to make your life easier and more prosperous. You can sign up for free and enjoy a range of online tools. Here are just 3...
Marketing! Login to list your practice - or update your details - on the hugely popular www.dentist.com.au website used by the public to find dentists, dental hygienists and oral health therapists. Not only can you manage your personal and practice details on the site, you can also view Google Analytics data about how your listing is performing on the website. As a dental hygienist or oral health therapist, you can ensure your profile is up-to-date and linked to all the practices where you work... and if you change jobs, you can immediately update dentist.com.au.
Track your CPD: With a new CPD cycle beginning, now is the perfect time to start logging the CPD you complete as you do it so in 3 years time, you’ll know exactly where you stand. Not only can you do this at www.dentalcommunity.com.au, the website also does some of it for you automatically. Any course you register to attend through Dentevents.com (such as with Ivoclar, Geistlich, GC, etc), your CPD is automatically recorded (and you can download the CPD certificate and your receipt any time). It’s also quick and easy to log any other courses you have completed too.
Complete CPD Questionnaires. If you’re a paid subscriber to Oral Hygiene (it’s only $22 a year), you can complete dozens of CPD Questionnaires from past editions - and a new questionnaire for each new edition - and receive 2 hours of CPD for each. Simply read the four CPD articles in each edition and then log in and complete the 20 questions. All the articles from past editions are also available to read online. And the CPD from the questionnaires is automatically logged in your CPD diary.
Personal protective equipment (PPE) worn by healthcare providers is exposed to SARS-CoV-2 while caring for infectious patients, in turn increasing the chances of fomite transmission of the virus during PPE doffing or reuse without prior disinfection. A pilot study modelled the stability of SARS-CoV-2 on common PPE worn in hospitals to simulate a moderate-dose SARS-CoV-2 transmission event that might occur during a high-risk airway procedure on a COVID-19 patient. The objective of this study is to relate SARS-CoV-2 concentrations on surfaces to predict the exposure of a single healthcare worker over an 8-hour shift and estimate the effects of doffing mistakes and number of care episodes per shift on inoculated dose per shift. They modelled the stability of SARS-CoV-2 on PPE commonly worn in hospitals when carrying out high-risk airway procedures. Evaluated PPE included the visors and hoods of two brands of commercially available powered air purifying respirators, a disposable face shield and Tyvek coveralls. Samples were collected at 4, 8, 24, 48 and 72 hours postexposure. A 72-hour time frame was selected as it coincides with a common work schedule observed by many intensive care unit personnel who may need to reuse PPE due to shortages. SARS-CoV-2 displayed prolonged stability on those PPE materials evaluated in this study, all of which had infectious SARS-CoV-2 present at least 72 hours postexposure. Following an exposure to 4.3 log10 plaque-forming units (PFUs) of SARS-CoV-2, all materials displayed a reduction in titre of > 4.2 log10 by 72 hours postexposure, with detectable titres at 72 hours varying by material (1.1-2.3 log10 PFU/mL). Although we found the predicted half-life of SARS-CoV-2 on PPE ranged from 6.74 to 10.05 hours (depending on the PPE material), it is important to note that between 1.9 and 2.3 log10 PFU/mL of infectious virus remained on those PPE evaluated in this study at 72 hours postexposure. This is in contrast to SARS-CoV-2 viability on cloth fabric (i.e., 50/50 nylon/cotton ripstop fabric), which decreased rapidly and was not recoverable at 24 hours postexposure. The results highlight the need for proper doffing and disinfection of PPE, or disposal, to reduce the risk of SARSCoV-2 contact or fomite transmission.





I’ve been spending a big chunk of my time over the last few weeks talking to practices who are scared to death of the potential risks from cyber attacks and rightfully so, considering these days it’s not a matter of if, but when.
Some of the classic responses I get when talking about security with clients range from a complete understanding of what they need to do to achieve their goals down to a completely opposite nonchalant attitude of “she’ll be right”...
1. Hackers aren’t interested in our little practice…
BUT THEY ARE!
It’s easier to compromise 1000 smaller businesses then it is to hit one big one; if only 10% of those pay a ransom of $10,000 then that’s a million dollars right there.
2. Securing our network is too expensive...
It’s not too expensive. In the current landscape, especially with the Optus and Medibank Private breaches recently, we’re going to see government agencies start to really come down on businesses that are compromised and have been negligent in securing their networks.
3. I don’t need all this security mumbo jumbo!
You absolutely need this security mumbo jumbo.
4. I have good backups, I’ll be fine...
That’s great, however do you want to be fined if you do have a data breach?
But let’s look at it from a different angle because a fine is only money.
How do you recover from the reputational damage that is caused when you have to tell all your patients that their personal and medical data has been breached and possibly out on the dark web to be sold to the highest bidder?
Cost is a big factor in a lot of the decisions that are made in regards to protection but considering the reputational damage that can be caused by a breach and losses due to downtime, it shouldn’t be, provided you’re investing in the right
security “stack” to minimise your exposure in line with your goals.
So what should an ideal security stack look like?
anaged services are the cornerstone of any good solution. They will usually include some form of support, anti-virus and “patch” management along with a proactive approach to looking at your hardware to minimise downtime.
HOWEVER, not all managed service plans are created equally; an ideal plan will include more than just antivirus and patch management; ideally they will be working to get your practice to an “Essential Eight” maturity level and include things like ransomware protection, persistent foothold protection and a good quality cloud backup solution.
We often put our security stack on to the networks of new clients only to find them riddled with viruses, malware and RATs.
Your firewall is the equivalent of building a massive brick wall on the internet connection to your practice. Now as effective as a brick wall is at stopping things, we come across the problem of also needing to let things through it.
So we decide to put a door in the brick wall. This allows things to go through it, but now we have the problem where things are coming through it unchecked, so like a nightclub, we need a bouncer.
Although I think most of us have had a good night ruined by a bouncer at a nightclub at some point, a good one will only let in people that aren’t there to ruin the party and keep out the riff-raff.
A good Next-Gen firewall will have a bouncer that checks what is going through it using live cloud databases and also study the behaviour of what that traffic is trying to do.
We recently had a discussion with a practice who pulled out one of the cheapest modems on the market and pointed to the part where it said “firewall”.
Yes, it has a firewall function included, but it is only a basic brick wall with a door in it and no bouncer–basically completely ineffective and this is what we come across every day. If you have a modem provided by your internet provider, it is ineffective to protect you against pretty much everything.
At Teamwork, we recommend Cisco Meraki firewalls as they’re fully cloud managed and provide one of the best levels of security for your network.
In addition to this, they will actually alert you if something is not right, for example if your internet goes down or if you have a device on your network that is doing something odd.
Spam is one of the key vectors of attack for any business, not just dental. By stopping the majority of spam from hitting your network, you not only increase productivity but also plug one of the biggest security holes for your practice.
Spam protection is quite inexpensive and using a third party such as Mailguard will not just give you industry leading protection but insights in to how much junk mail you’re actually receiving.
So what does it all cost to protect a five computer practice at this level?
Realistically, upfront, a good network firewall is around $2000-$3000 installed with a three year licence.
As for the ongoing costs for the managed services and spam protection, the industry average should be around $500-$700 a month depending on the IT provider you use and the overall level of security and value they provide.
Whilst this may not be the be all and end all of your security stack, they definitely give you a great foundation to elevate the security of your network and significantly reduce your attack surface.
We believe practices should learn and understand what security they require and how it works for them.
For more info, call Teamwork Technology on 1300-456-901.

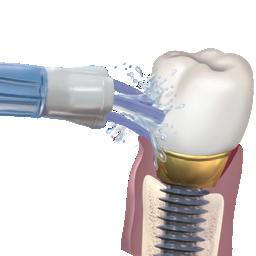
Dürr Dental has launched its portable powder handpiece in Australia. MyLunos, which has been available overseas since 2017, offers simple, powerful and ergonomic assistance when you need to remove discolouration, deposits and biofilms. Depending on the nozzle, it is ready for either supra- or subgingival applications.
The MyLunos handpiece sits comfortably in your hand due to its ergonomic design and interchangeable powder chambers, eliminating the need to refill in the middle of treatment. It also has the added benefits of allowing you to change from supra- to subgingival cleaning with a quick change of the nozzle.

In terms of reprocessing, all components are autoclavable and can be placed in the ultrasonic bath, reducing risk of clogging and ease of maintenance.
The primary benefits of subgingival air polishing are its gentler application and shorter treatment time in comparison to hand and ultrasonic instrumentation.
One of the low-abrasive powder materials, a non-cariogenic disaccharide, trehalose, has demonstrated equivalent outcomes to ultrasonic scaling over 12 months in terms of reducing periodontal pockets and bleeding on probing in patients with pocket depths of 5-9mm.

This was conducted using the new sterile perio tip designed by Dürr Dental, which has a small flexible diameter, allowing easy entry into the periodontal pocket, providing a much more comfortable experience for the patient compared to ultrasonic scaling. In contrast to an apical streaming tip, the single opening on the lateral surface of the tip enables
optimal redirection of the compressed air towards the root surface, lowering the risk of emphysema.
Trehalose, which is substantially less abrasive than glycine and sodium bicarbonate, has also demonstrated the best efficacy for supragingival stain and biofilm removal.
The MyLunos supra nozzle allows easy removal of plaque and stains using trehalose that can be integrated into routine hygiene visits, cleaning around orthodontic brackets or preparing for fissure sealants.
There are three flavours of the trehalose-containing Gentle Clean powder for supragingival application: orange,
spearmint and neutral. Additionally, a neutral-flavoured Perio Combi powder is offered as a one-for-all powder for both supragingival and subgingival treatments. Patients no longer need to feel the unpleasant grittiness commonly associated with air polishing due to trehalose’s exceptional water solubility, along with a pleasant tasting experience.
1. Morawietz, M.; Sarembe, S.; Kiesow, A.; Hänel, K.; Hartl, J.: Air-Polishing: Investigation of Cleaning Performance and Abrasiveness of Different Powders; Poster 2020 IADR/AADR/ CADR (Washington, D.C., USA); 2020; Presentation ID 2984.
2. Kruse, A.B., Wölki, B.J., Woelber, J.P. et al. Subgingival air polishing with trehalose powder during supportive periodontal therapy: use of a conical shaped tip during a randomized clinical trial. BMC Oral Health 22, 70 (2022). https:// doi.org/10.1186/s12903-022-02109-1.


in terms of cell response and in contrast to Glycine-based prophylaxis powder.
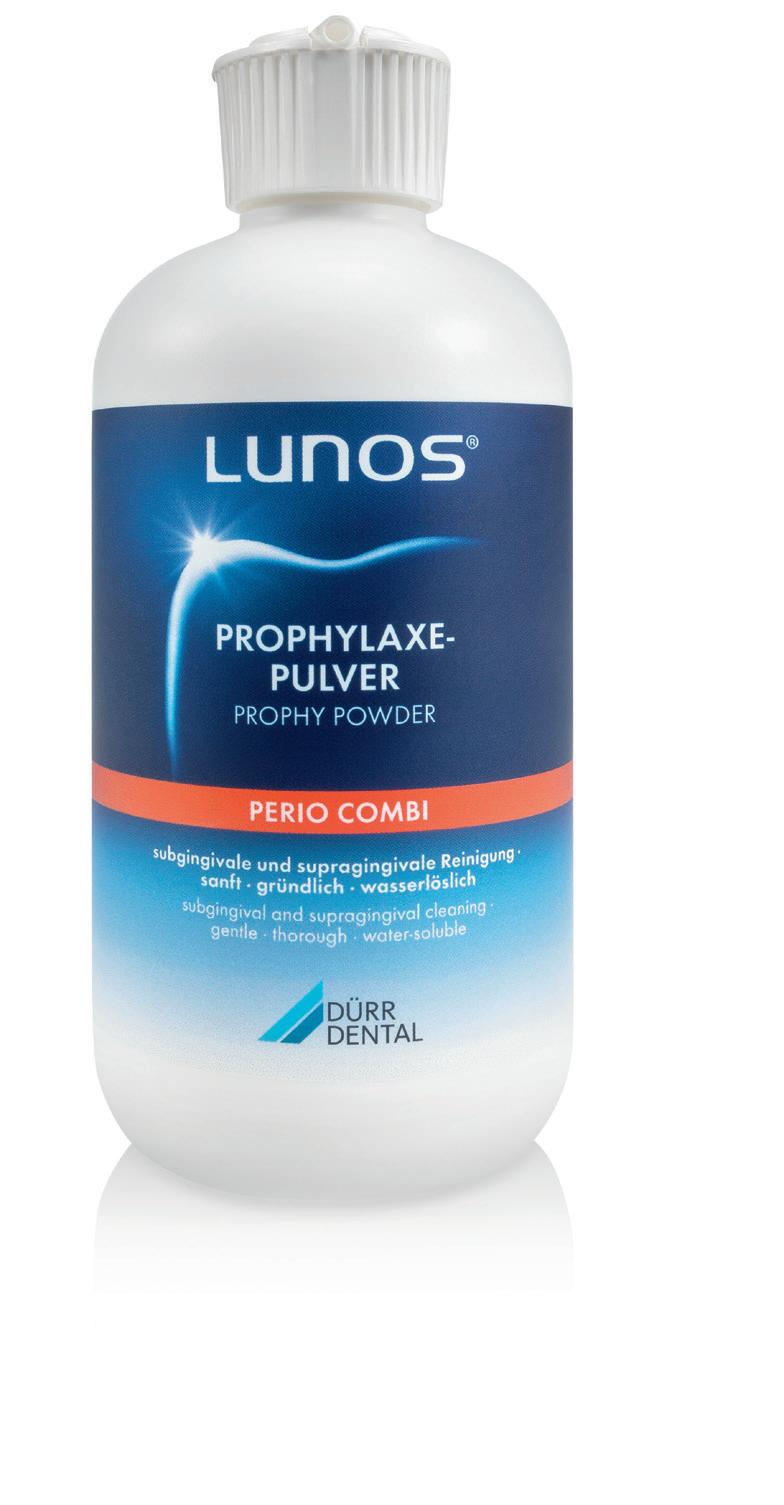
Lunos® Prophy Powder Perio Combi, based on trehalose, can be used for supra- and subgingival air-polishing in prophylaxis as well as to support periodontal or periimplantitis therapy. ▪ effective ▪ highly soluble ▪ pleasant taste for patients ▪ low abrasive
A recent in-vitro study (Weusmann et al. 2021) has shown that trehalose has no pro-inflammatory and no pro-apoptotic effects on human gingival fibroblasts. Wound healing of gingival tissue is, in contrast to glycine, not negatively influenced (Fig. 1).
Wound closure (%)
Time (h) 0 0 10 20 30 40 50 60 70 6 12 24 36 48
Control
Trehalose
Glycine
Fig. 1: Wound closure of human gingival fibroblasts (HGF) in the presence of glycine and trehalose over 48 h. *significant difference from all groups °significant difference to control Derived from (Weusmann et al. 2021).
Thus, the authors suggest that in terms of cell response, trehalose-based air-polishing powder might be more beneficial than glycine- based powder for air-polishing.
Weusmann, Jens; Deschner, James; Imber, Jean-Claude; Damanaki, Anna; Leguizamón, Natalia D. P.; Nogueira, Andressa V. B. (2021): Cellular effects of glycine and trehalose air-polishing powders on human gingival fibroblasts in vitro. In: Clinical oral investigations. DOI: 10.1007/s00784-021-04130-0.



Barnes CM, et al. J Clin Dent, 2005; 16(3): 71-77. Study conducted at the University of Nebraska Medical Center, College of Dentistry, Lincoln, Nebraska.
To evaluate the ability of a Waterpik® Water Flosser paired with either a power or manual toothbrush and a manual toothbrush and floss, to reduce gingivitis, bleeding and supragingival plaque biofilm.
One hundred and five (105) subjects participated in this four-week study. One group used a Waterpik® Water Flosser with a manual toothbrush and a second group used the Waterpik® Water Flosser with a power toothbrush. The control group used a manual toothbrush and floss. Subjects brushed twice daily and used either the Water Flosser or dental floss once daily. Plaque biofilm, bleeding and gingivitis were evaluated at two and four weeks.
At four weeks, the addition of a Waterpik® Water Flosser resulted in significantly better oral health, regardless of toothbrush type used over manual brushing and flossing. Adding the Waterpik® Water Flosser was up to 93% better in reducing bleeding and up to 52% better at reducing gingivitis than traditional dental floss.

he Waterpik® Water Flosser is an effective alternative to traditional dental floss for reducing gingivitis.












The day to day running of any dental practice is hectic, there are always a million and one things on your “to do” list and not to mention trying to balance your working life with your home commitments.
We all crave a little more time in our lives, so have you ever thought about how your practice management software could help
Dentally’s cloud-enabled dental software will streamline your processes, reduce your practice admin, deliver great patient care and help you manage your team. It is easy to use, secure and allows your team to work effectively to deliver the best possible care to your patients. Our team use the latest tech to innovate and develop our software to ensure you have the best tools at your fingertips. We listen to our customers and are always striving to make their lives easier. Patient management is all about ease
n Save time - manage your team and your practice admin seamlessly (whether staff are onsite or working remotely) with features such as task lists, automated communications, effective automated recalls and Dentally chat.
n Stay connected - keep patient communications open with Dentally to keep your practice running smoothly and develop better relationships with your patients. Communications are clear, concise and automated meaning you always have complete visibility and a detailed correspondence history for each patient.

n Effortless Patient journey - provide a seamless (contactless) patient journey from start to finish with tools such as Dental Portal including online appointment booking, customisable medical history, self check in and payments, plus straightforward clinical records, easy to use charting and patient treatment plans.
n Powerful real time reporting - Dentally sifts through your data quickly to produce clear, easy to interpret and analyse reports, so you can make informed decisions.
your reclaim some time and make things a little easier?
When you’re in the business of dentistry, patient care comes first and the daily demands of practice admin can seem endless, but that is where Dentally’s cloud enabled practice management software can help.
Dentally from Henry Schein One, is designed to make your day-to-day practice management simple - and sometimes just finding a short moment in your busy day to take a closer look at something new is worth every second invested!
with Dentally, saving you time and resources by taking care of all your admin, tracking tasks, automating your patient communications, managing finances and all aspects of your day-today processes.
n Save money - There’s no need for expensive hardware and servers. All data is stored securely on the cloud, to keep your practice running smoothly and cost-effectively. All you need is to Chrome and go! It is stable and high performing, updates automaticallyand will never slow you down!
n Easy onboarding - simple to switch, all your data will be converted from your existing system so you have all the patient info you need backed by comprehensive training for your team.
n Elevate - a customer success programme designed to support you in sustaining and growing your dental practice, that you won’t find anywhere else!
Dentally understand that running your dental practice is so much more than appointments, charting and financial. Visit their website to find out more at dentally.com.au - and remember not all dental practice management software in Australia is the same!
Transform your business with our cloud-based software, putting patients and simplicity at the heart of your practice.
Save money and stay secure, without the need for hardware or servers - all your data is stored securely on the cloud.
Our contactless reception keep things safe and simple, from online medical history to self-check-in and payment links.
Giving your patients a safe and simple experience, whilst ensuring your practice runs smoothly and securely.
Visit dentally.com.au to find out more.
Save time with our task list feature and manage your practice from any location, using automation and Dentally chat.
Stay connected with patients direct from their records and through automated communications.

222 nanometre lighting




Far-UVC lighting is an autonomous and continuous sanitation system that is safe for humans and animals – using 222-nanometer wavelength, and is also maintenance free.
Far-UVC lighting is an autonomous and continuous sanitation system that is safe for humans and animals – using 222-nanometer wavelength, and is also maintenance free.
Far-UVC lighting is an autonomous and continuous sanitation system that is safe for humans and animals – using 222-nanometer wavelength and is also maintenance free.
Together with the two primary methods for minimising exposure to airborne diseases (including COVID-19) – wearing a mask and social distancing, far-UVC has been proven to effectively sanitise the indoor air around us.
Together with the two primary methods for minimising exposure to airborne diseases (including COVID-19) – wearing a mask and social distancing, far-UVC has been proven to effectively sanitise the indoor air around us.
Together with the two primary methods for minimising exposure to airborne diseases (including COVID-19) – wearing a mask and social distancing, far-UVC has been proven to effectively sanitise the indoor air around us.
Far-UVC can be widely applied to safeguard populated spaces such as shopping centres, hospitals, schools, offices, public transport systems and gyms.
Far-UVC can be widely applied to safeguard populated spaces such as shopping centres, hospitals, schools, offices, public transport systems, gyms... and dental surgeries.
Far-UVC can be widely applied to safeguard populated spaces such as shopping centres, hospitals, schools, offices, public transport systems and gyms.
For more information on FAR UVC AFRICA and this immediately available and highly cost-effective solution, please visit www.faruvcafrica.com or contact: 082 578 3755
Available in Australia from Medisupply Pty Ltd Unit 33/110 Inspiration Drive, Wangara WA 6065 www.medisupply.net.au | info@medisupply.net.au
For more information on FAR UVC AFRICA and this immediately available and highly cost-effective solution, please visit



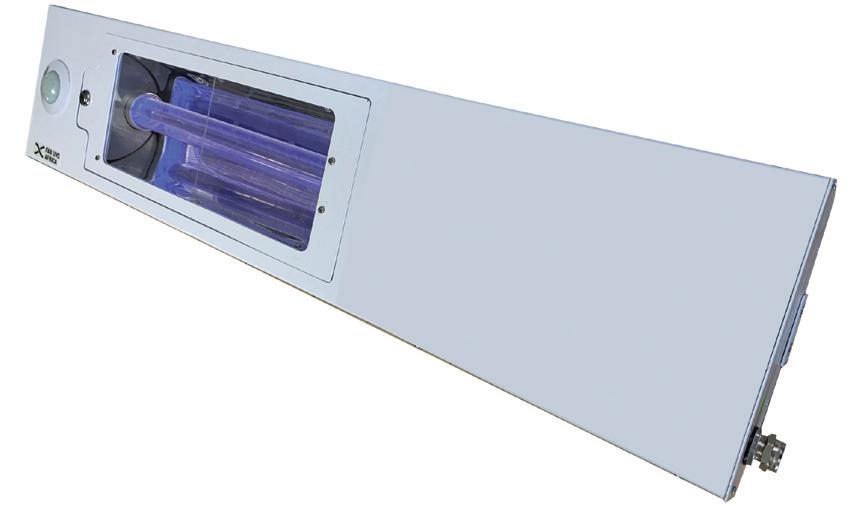
FAR UVC light at 222nm destroys viruses and bacteria and is the only product that offers REAL TIME air and surface sanitation.

UVC light at 222nm is effective against viruses including SARS-CoV-2 (COVID) and Influenza together with multi-drug resistant bacteria in the air, on living human tissue and on surfaces.
Unlike UVA and UVB light, UVC does not penetrate the stratum corneum of the skin nor the cell membrane of a human cell.
The placement of fixed or mobile UVC lighting units in dental treatment rooms including during invasive, implant and oral surgical proceduces can add a further line of defence to your infection control protocols.


FAR-UVC lighting is the first safe, effective, autonomous and continuous disinfection system for occupied spaces.
Visit www.medisupply.net.au for product and technical information, scientific research and studies, recent installations and more...
infection CONTROL
The COVID-19 pandemic has brought much greater attention to the risk factors that operate in the dental clinical setting because of droplets and aerosols and thus the importance of respiratory protection as one of the layers of defence.1,2 Masks and respirators perform multiple functions. This article will explore each of these functions and then go on to discuss some new antimicrobial technologies used in masks and respirators.
Containment Firstly, masks and respirators contain the secretions of the wearer and reduce the generation of droplets and aerosols into the immediate environment. This principle explains the use of these during pandemics to contain these on the face of
the user, rather than having them dispersed into the environment where they can infect others. Over the last three years, research in aerobiology has shown clearly that infectious aerosols are generated by the act of breathing, with an increased load of viruses produced during speaking, shouting, singing, coughing and sneezing, in increasing orders of magnitude. For this first purpose of containment, it is essential that the mask or respirator is adapted closely to the face so that expired air does not leak in large amounts from the periphery. Due to variations in facial shape, some individuals are unable to be properly fit tested with a surgical respirator and achieve a fully airtight fit for their respirator.
An example of proper adaptation is shown in Figure 1. Surgical masks are not designed to be airtight, but rather to be adapted closely against the skin of the face. Not folding the mask out fully and not adapting the insert that covers the bridge of the nose are two common errors that result in air being directed away from the face of the wearer and into the general environment.

22 ora hygiene September/December 2022
Question 1. The largest amounts of both splatter and aerosol are generated by:
a. Air polishing and ultrasonic scaling b. Triplex syringe c. High-speed handpieces d. Low-speed handpieces
Question 2. Level 3 fluid resistance is...
a. 60 mm Hg b. 120 mm Hg c. 180 mm Hg d. 240 mm Hg
Question 3. The antimicrobial properties of some masks is achieved by incorporating antimicrobial metals into their manufacture including: a. Selenium b. Silver or Gold c. Zinc d. Copper e. All of the above
Question 4. The outermost and innermost layers of modern masks and respirators are produced using: a. Injection moulding b. 3D printing c. Electrospinning d. Thermoforming
Question 5. To be rated as P2/N95, a surgical respirator must be able to filter particles of 0.2 µm in size by over:
a. 90% b. 93% c. 95% d. 97%
1. Characteristic appearance of enamel

By Emeritus Professor Laurence J. Walsh AO


In clinical dental practice, one of the most common things that we do is to detect white spot lesions and monitor their progress to determine if they are progressing towards cavitation, undergoing arrest, or regressing. This article summarises, from the perspective of the author, some of the main lessons about watching white spot lesions and provides a number of clinical hints in interpreting what is happening in these lesions.
Hidden beneath An active white spot lesion will each day be undergoing numerous cycles of mineral loss followed by remineralisation. Because an active white spot is covered by a cariogenic dental plaque biofilm that is producing multiple organic acids, the fluid in direct contact with the surface is not the saliva of the patients mouth but rather the plaque fluid. If using technologies that can detect acid production by dental plaque, such as GC TriPlaque ID gel, active white spot lesions will be found beneath the plaque which is producing the highest amounts of acid following a challenge with sucrose or another suitable substrate.4,5
26 ora hygiene September/December 2022
Question 6. What percentage of the buccolingual width of a tooth must be affected by mineral loss for it to appear on a biteway x-ray?
a. 10% b. 17% c. 23% d. 33% e. 50%
Question 7. Once detected, white spot lesions should be monitored to determine if they are: a. Progressing towards cavitation b. Undergoing arrest c. Regressing d. All of the above
Question 8. The application of a high concentration fluoride product can cause a white spot lesion to: a. Progress towards cavitation b. Undergo arrest c. Regress d. Become “frozen in time” e. All of the above
Question 9. Subsurface regeneration of white spot lesions, leading to their visible reversal, can be achieved using: a. A high concentration fluoride product. b. CPP-ACP via various delivery systems. c. Fluoride varnish. d. Silver fluoride.
Question 10. An active white spot is covered by: a. Saliva b. A cariogenic dental plaque biofilm c. An invisible layer of benign plaque d. Oral mucosal transudate
OralHygiene™ is now offering PAID subscribers the ability to gain 2 Hours CPD credit from reading articles in this edition of the magazine and answering the questions above. To participate, contact OralHygiene for your Username and Password. Then log into the Dental Community website at www.dentalcommunity.com.au and click on the CPD Questionnaires link; select the Oral Hygiene Sep/Oct 2022 questionnaire and then click START. A score greater than 80% is required to PASS and receive CPD.
Keeping up with expansion
As Floss & Co. began to get busier, staff struggled at first to manage an increase in patients. There were simply not enough scalers to keep up and all instruments were either in use or in reprocessing. At first, Dr Izzy Naem looked to solve the problem by purchasing more instruments, but the real issue wasn’t the number of instruments. It was about improving process efficiencies and finding better ways to keep instruments better organised.
So, when Dr Naem instead decided to switch to the IMS system, the practice was able to save 15 minutes per patient per chair, relieving some of the stress that the staff were experiencing. “We don’t have to think about the instruments,” Dr Naem said. “Where they’re at, where to put them, where to store them. It’s all in the cassette. It was safer and it was easier.”
With improved efficiency and organization, the practice was able to continue expanding and saw a 40 percent increase in new patients. By switching to IMS, Dr Naem was able to increase revenues and provide a better experience for his staff and growing patient base.
Improving efficiency
When Dr Edward Lin and his team at Orthodontic Specialists expanded from three doctors to four, the number of instruments used in their facility rose accordingly. Additionally, Dr Lin was concerned about protecting his investment in premium instruments. After trying other solutions with unsatisfactory results, the team began using IMS, enabling them to see 60 to 120 patients a day efficiently.
Simplifying complexity
For Dr Steven Koos of ORA Oral Surgery & Implant Studio, proper organisation is key to practice success. Since ORA specialises in various oral surgery procedures, it’s important to have setups ready for each unique procedure and organising the correct instruments can be complicated and time-consuming.
Adopting IMS simplified instrument prep with the introduction of versatile and customisable cassettes that keep instruments organised and in one place for each procedure, from chairside to cleaning to storage. “My surgical team has really embraced the Hu-Friedy IMS Cassette System because it’s enabled them to combine the cleaning and sterilisation and organisation and storage of a vast array of instruments into one integrated package and it works well,” Dr Koos said. Additionally, implementing cassettes has made it easier to hire and train new team members and open new locations without affecting the quality of care provided to patients.
Where can you improve?
expanded it to more locations to verify the findings, which generated identical results. With such positive outcomes, Hu-Friedy worked with PDS to implement IMS in over 100 practices. “Now that we’ve implemented these cassettes in approximately 100 locations, the feedback continues to be the same,” said one PDS compliance manager. “Staff really love the cassettes. They love the efficiencies of the cassettes.”
Cassettes were fundamental to enabling Dr Lin’s practice to successfully expand: “To work without the Hu-Friedy IMS System would be pure chaos,” Dr Lin said. “I couldn’t tolerate it because instruments are going to get lost. Instruments will get damaged. It would be physically impossible to be able to see the number of patients that we see in a clinical day without the IMS System.”
Chairside efficiency is the key to a productive practice. Maximizing this efficiency is possible when the exact procedural set ups needed for each patient are always at your fingertips. Hu-Friedy’s dental Instrument Management System standardises and combines the cleaning, sterilisation, storage and organisation of instruments in one integrated cassette system, creating real results that can save your practice up to 5-10 minutes per procedure. There are numerous advantages to adopting IMS and while each practice profiled here chose to make the switch for different reasons, the results are universal: better efficiency, improved safety, enhanced patient experience and an increased bottom line.
If your practice does not already use an instrument management system, you can request more information from a Hu-Friedy representative on how a cassette-based system can directly benefit your practice.
Question 11. Using an Instrument Management System can:
a. Reduce sharps injuries. b. Enhance organisation. c. Reduce costs due to reduced instrument damage. d. All of the above.
Question 12. After implementing an Instrument Management System, Pacific Dental Services’ sharps injuries were reduced to: a. 0 b. 1 per month c. 1 per year d. 2 per year
Question 13. implementing cassettes at ORA Oral Surgery & Implant Studio has made it easier to hire and train new team members and open new locations without affecting the quality of care provided to patients.
a. True b. False
Question 14. Using an Instrument Management System, Floss & Co improved process efficiencies per patient by:
a. 8 minutes b. 10 minutes c. 12 minutes d. 15 minutes
Question 15. Thanks to improved efficiency and organisation from using an Instrument Management System, Floss & Co’s new patients increased by:
a. 10% b. 20% c. 30% d. 40%
To retrieve your FREE Dental Community Login: Call (02) 9929 1900 or Email info@dentist.com.au


Sgnature Series Tubs are designed to match Hu-Friedy IMS instrument cassette rail colours and feature antimicrobial product protection. Together, procedure tubs and cassettes create the most efficient and organised system for managing instruments and consumable products.
The time savings achieved by using IMS (Instrument Management System) cassettes and procedure tubs allow staff to spend time on more value-added activities in the dental practice.
Procedure tubs can be used as portable operatory drawers to store, organise and transport consumable materials to and from the storage/sterilisation area and the operatory. All of the materials needed for a specific procedure can be stored in the tub. A different tub and colour can be used for each different procedure type (e.g. crown & bridge, composite, etc). The Signature Series procedure tubs are available in colours that match IMS cassette rails, which allow the staff to match the tubs and cassettes by procedure.
An example of how it works:
Blue cassette rails and a blue tub may represent a composite procedure. All of the consumable materials for composite procedures can be stored and organised in the blue tub and instrumentation stored in the cassette with blue rails, allowing for quick identification.
Microban® Antimicrobial Product Protection
Microban protection is integrated into the tub and tub components during the manufacturing process. Microban technology works by interrupting key cell functions that allow the microorganisms to function, grow and reproduce. Microban protection begins to work as soon as the microorganism comes into contact with the product surface and works continuously to inhibit the growth of microbes that can cause stain, odours and product degradation - for the lifetime of the product.
Standardises material set-up for every type of procedure
The Hu-Friedy IMS and Tub System increases efficiency of materials management and eliminates time-consuming tray preparation for every procedure. Tubs may be configured to meet your practice needs or are available as a complete tub. Procedure tub colours match Hu-Friedy IMS cassette rail colours...
Increasing practice organisation and workflow efficiency. Allowing for quick identification of consumable products.
Providing
34 ora hygiene September/December 2022
Question 16. Signature Series Tubs are designed to store: a. All the instruments required for a procedure type. b. All the materials required for a procedure type. c. Both the instruments and materials required for a procedure type.
Question 17. Microban technology interrupts key cell functions that allow microorganisms to function, grow and reproduce: a. True b. False
Question 18. Signature Series procedure tubs are available in: a. Primary and secondary colours only. b. Custom colours to match your practice. c. ISO standard colours for dental procedures. d. Colours that match IMS cassette rails.
Question 19. Signature Series procedure tubs are designed to: a. Increase practice organisation. b. Increase workflow efficiency. c. Save on procedure set-up times. d. Safely store materials. e. All of the above.
Question 20. Locking lids protect tub contents from airborne materials during transportation to the operatory and during storage: a. True b. False
POWERED BY THE
Professor Laurence Walsh AO is a clinically active specialist in special needs dentistry who is based at the University of Queensland in Brisbane. Laurie has been teaching infection control and clinical microbiology for over 25 years at postgraduate level and has been the chief examiner in microbiology for the RACDS for the past 20 years. He has presented invited courses and lectures on infection control across Australia and internationally. Laurie has written over 60 articles on infection control and in addition published over 320 journal papers and a further 190 technical reports and literature reviews. He serves on two committees of Standards Australia (personal protecting equipment; and instrument reprocessing) and in recent years has been an adviser to the Communicable Diseases Network of Australia and the Australian Commission on Safety and Quality in Health Care. Laurie has been a member of the ADA Infection Control Committee since 1998. He has contributed to various protocols, guidelines and checklists and manuals used in Australia.










 By Emer. Prof. Laurence Walsh AO
By Emer. Prof. Laurence Walsh AO
Dental professionals are at high risk of exposure to communicable diseases during clinical practice, but many dental clinics provide clinical care in closed spaces. Therefore, it is essential to develop efficient ventilation methods in dental clinics that do not rely on natural ventilation. Although some reports have described the evaluation of contaminant dilution in naturally ventilated dental clinics, dental clinics usually have air conditioners running at all times to ensure the comfort of the staff and patients. To maximise the effectiveness of air conditioners and to avoid the interference caused by sunlight and wind, staff and patients spend long hours with the windows and curtains closed, necessitating an efficient ventilation method that does not rely on natural ventilation. In this study, to clarify the factors that cause air retention in dental offices, computational flow dynamics simulations were conducted focusing on (1) the flow path from the entrance to the exhaust port and (2) the presence of partitions. A three-dimensional model of a dental clinic with three dental chairs was created and simulations were conducted for scenarios with and without partitions with different entrance and exhaust port positions. Evaluation of these simulations on the basis of the age of air, an indicator of ventilation efficiency, showed that the value of the air age near the partition was locally high in the scenarios with partitions. In the scenarios where the exhaust port was located close to the entrance, the air age near the exhaust port was high, regardless of the presence of a partition. In addition to wearing protective clothing and sterilising instruments, it is important to consider air quality improvement as a countermeasure against airborne and droplet infections, such as virus infections, in dental clinics. Since the location of the entrance and exit points has been shown to affect the concentration of indoor air pollutants, appropriate positioning of the exhaust port may be important in dental offices. However, since changes in the positioning of the exhaust vent cannot be easily performed in an existing dental office, it is necessary to examine whether increasing or decreasing the ventilation volume can improve air quality. Nambu E, et al. Numerical simulation of air age in dental offices. Sci Rep. 2022; 12: 14120.
Self-contamination during doffing of personal protective equipment (PPE) is a concern for healthcare workers (HCW) following SARS-CoV-2-positive patient care. Staff may subconsciously become contaminated through improper glove removal; so, quantifying this exposure is critical for safe working procedures. HCW surface contact sequences on a respiratory ward were modelled using a discrete-time Markov chain for: IV-drip care, blood pressure monitoring and doctors’ rounds. Accretion of viral RNA on gloves during care was modelled using a stochastic recurrence relation. In the simulation, the HCW then doffed PPE and contaminated themselves in a fraction of cases based on increasing caseload. A parametric study was conducted to analyse the effect of: (1a) increasing patient numbers on the ward; (1b) the proportion of COVID-19 cases; (2) the length of a shift; and (3) the probability of touching contaminated PPE. The driving factors for the exposure were surface contamination and the number of surface contacts. The results simulate generally low viral exposures in most of the scenarios considered including on 100% COVID-19 positive wards, although this is where the highest self-inoculated dose is likely to occur with median 0.0305 viruses (95% CI = 0-0.6 viruses). Dose correlated highly with surface contamination, showing that this can be a determining factor for the exposure. The infection risk resulting from the exposure is challenging to estimate, as it will be influenced by the factors such as virus variant and vaccination rates. Regardless of the number of COVID-19-positive patients on a ward, notable decreases in predicted infection risk were associated with less self-contamination during doffing. For example, for scenarios involving all COVID-19 patients, the mean infection risk for 10% probability of self-contamination while doffing was 0.4%, while the mean infection risk for an 80% probability of self-contamination while doffing was more than a 420% increase at 2.1%. This emphasises the importance of adequate training for PPE use. The practical implications are that the infection risk from selfcontamination during doffing PPE is an important concern in healthcare settings, especially on a COVID-19 ward. Fatigue during high workload shifts may result in an increased frequency of mistakes and hence the risk of exposure. Length of staff shift and a number of COVID-19 patients on a ward correlate positively with the risk to staff through self-contamination after doffing. Cleaning of far-patient surfaces is equally important as cleaning traditional “high-touch surfaces”, given that there is an additional risk from bioaerosol deposition outside the patient zone.
King MF, et al. Modelling fomite-mediated SARS-CoV-2 exposure through personal protective equipment doffing in a hospital environment. Indoor Air. 2022; 32(1): e12938







The COVID-19 pandemic has brought much greater attention to the risk factors that operate in the dental clinical setting because of droplets and aerosols and thus the importance of respiratory protection as one of the layers of defence.1,2
Masks and respirators perform multiple functions. This article will explore each of these functions and then go on to discuss some new antimicrobial technologies used in masks and respirators.
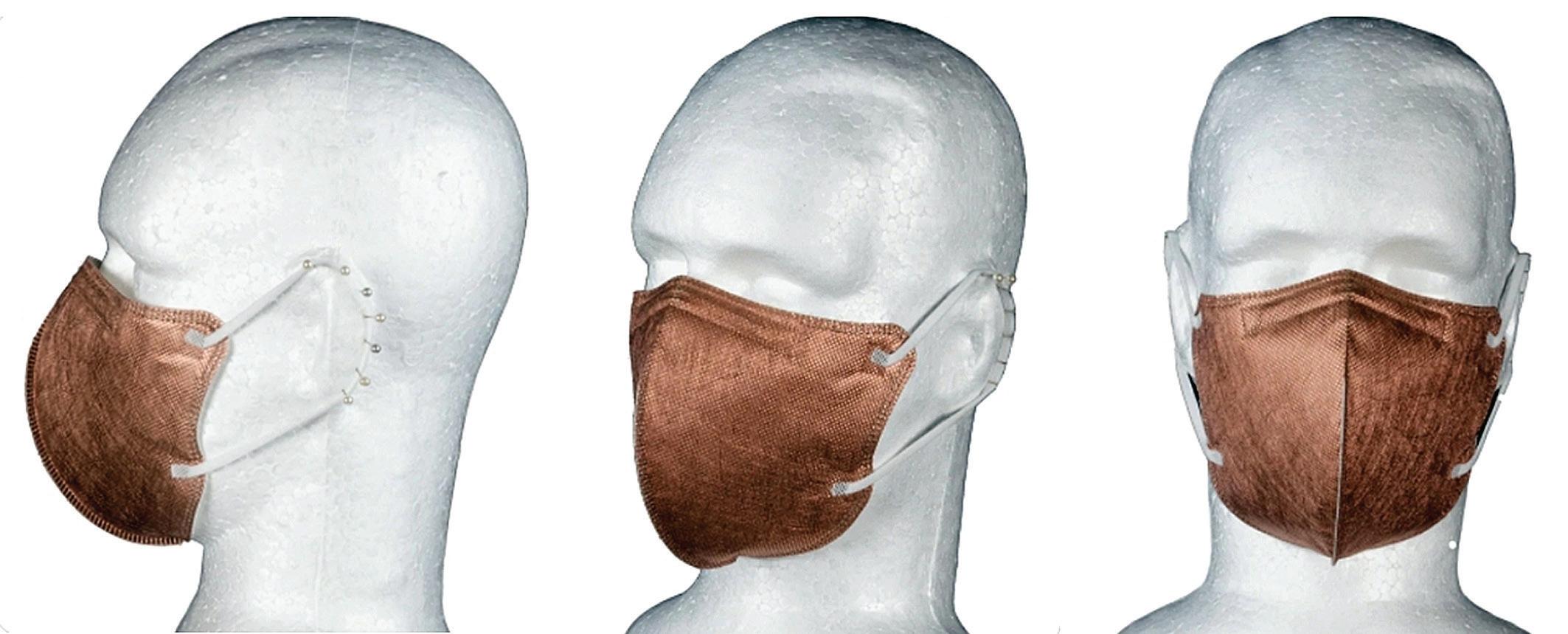
Firstly, masks and respirators contain the secretions of the wearer and reduce the generation of droplets and aerosols into the immediate environment. This principle explains the use of these during pandemics to contain these on the face of
the user, rather than having them dispersed into the environment where they can infect others. Over the last three years, research in aerobiology has shown clearly that infectious aerosols are generated by the act of breathing, with an increased load of viruses produced during speaking, shouting, singing, coughing and sneezing, in increasing orders of magnitude. For this first purpose of containment, it is essential that the mask or respirator is adapted closely to the face so that expired air does not leak in large amounts from the periphery. Due to variations in facial shape, some individuals are unable to be properly fit tested with a surgical respirator and achieve a fully airtight fit for their respirator. An example of proper adaptation is shown in Figure 1. Surgical masks are not designed to be airtight, but rather to be adapted closely against the skin of the face. Not folding the mask out fully and not adapting the insert that covers the bridge of the nose are two common errors that result in air being directed away from the face of the wearer and into the general environment.
ing. Panels A-C are 42X magnification images of the outer, middle and inner layers, respectively. The 3D printed nature of the outer and inner surfaces is evident. Panels D and E are 520X magnification images of the outer, middle layers, respectively. Note the differences in size and arrangement between the outer fibres, which are 3D printed, and the inner fibres, which are electrospun. Several small particles which appear white can be seen at hearing to the fibres.


Asecond feature of masks and respirators is that they are a disposable surface that covers the face and the upper neck. This is important when one is being exposed to fluid splashes, as frequently occurs in dental practice. Several studies have explored the extent of contamination and the most recent evidence shows clearly that dental assistants during their normal work receive greater splashes to the face and upper chest region then do dental clinicians. The nature of the equipment being used also has a powerful influence, with air polishing and ultrasonic scaling producing the largest amounts of both splatter and aerosol, followed by the triplex syringe and high-speed and low-speed handpieces, respectively.1,2 Knowing the outer surface of the mask or respirator becomes highly contaminated during a clinical procedure underpins the importance of removing this in a way that does not lead to contamination of the fingertips.
For use in a clinical setting, masks and respirators require resistance to splashes of fluid. Synthetic blood is the test liquid used to assess resistance to fluid penetration through the mask and resistance to penetration is expressed in terms of pressure in millimetres of mercury, so that it corresponds to blood pressure. Requirements for these are specified in AS 4381:2015 and the test protocol for fluid resistance is in ISO 22609. Level I fluid resistance is 60 mm Hg and this suits environments where little or no exposure to fluid is expected, because the triplex syringe or powered instruments are not being used at any stage of the procedure. Level 2 fluid resistance is 120 mm Hg and is more than sufficient for all routine surgical and nonsurgical dental procedures. Level 3 fluid resistance is 180 mm Hg. This is designed to cover situations of extreme exposure to arterial squirting during surgical procedures (such as orthopaedic or cardiac surgery and limb amputations). It is very rare for arterial squirting to occur in oral surgery procedures undertaken in an office-based setting.
The third feature is that of filtration of particles. This occurs in two directions, trapping expired particles as they leave the mouth and the nose and also trapping particles from the external environment as the wearer is breathing in. The outer most and innermost layers of modern masks and respirators are produced using 3D printing, with dense aggregates of fibres and linking regions that provide strength and support. Typical examples of this structure are shown in Figure 2. Surgical masks and respirators have one or two central layers of very fine electrospun fibres that are designed for filtration of small particles. The filtration occurs both through straining out of larger particles that are intercepted as they attempt to pass through the forest of fine fibres, as well as attraction of smaller particles through electrostatic interactions with the fibres themselves. To achieve this second mechanism, the polypropylene fibres are treated with a high voltage as a final stage of manufacturing the mask.
Understanding these two filtration approaches is important for assessing the quality of a surgical mask. Filtration of larger particles of 2 µm in size (i.e. bacteria) is expected to be a minimum bacterial filtration efficiency (BFE) of either 95% or 98% for surgical masks under AS 4381. Filtration of small particles is not a requirement under this particular standard. High-quality surgical masks, such as those with four layers, can achieve significant filtration of small particles and in this case they will be labelled with their particle filtration efficiency (PFE). For surgical respirators, under AS 1716, filtration of particles of 0.2 µm in size (i.e. viruses causing respiratory infections) must exceed 95% for the mask to be rated as a P2/N95.
n addition to serving as a passive filter, in recent years several technologies have been developed so that masks can have active antimicrobial effects against bacteria and viruses. This is typically achieved by using one of the antimicrobial metals, or their compounds, such as those based on selenium, silver, gold, zinc or copper.3-10 Nanoparticles of the metal can be incorporated into the melt so that during 3D printing or electro spinning, the particles are integrated into the polypropylene,



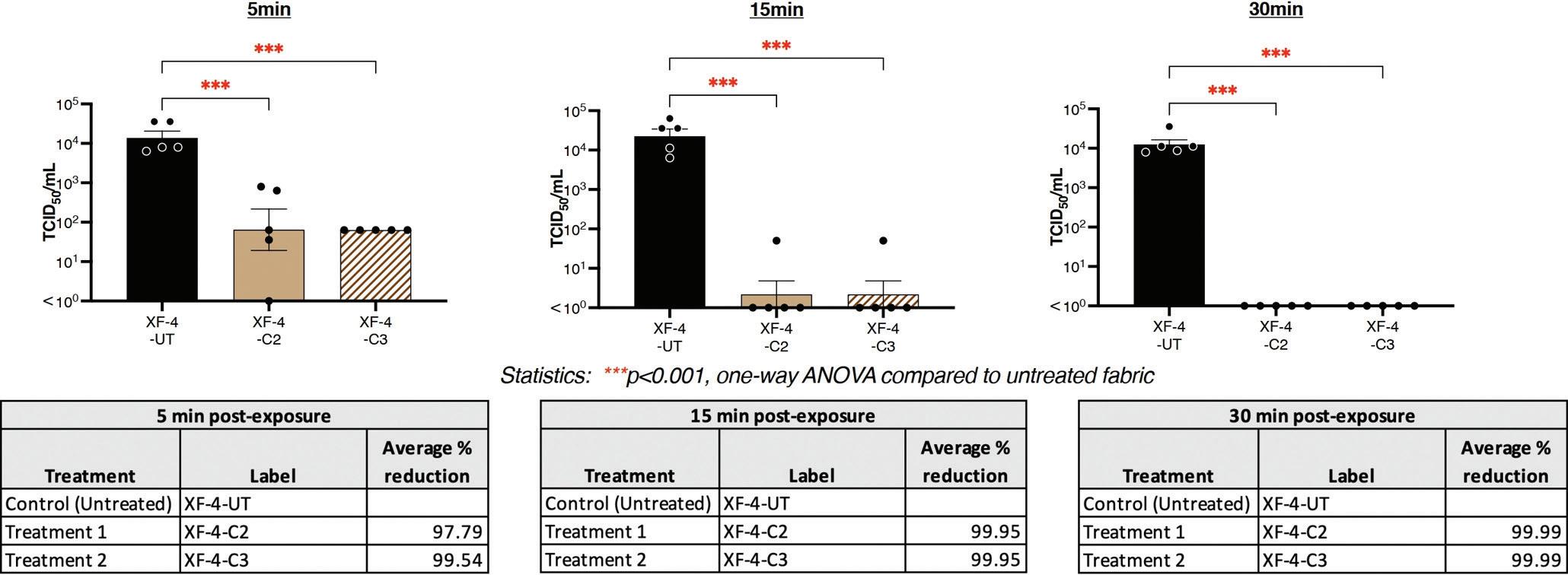
Figure 3. Testing of the surfaces of a Survivon™ Copatac mask with copper coating against a clinical isolate of SARS-CoV-2 by the Doherty Institute at Melbourne (conducted on March 4, 2021). Details of the mask are at https://www.survivon.com/copper-masks. The graphs compare the tested surfaces with a control and the percentage reduction is shown in the tables for the three time points of 5, 15 and 30 minutes. Each 10 mm X 10 mm sample was exposed to 50µL of SARS-CoV-2 to simulate large droplet contamination of material. After 5, 15 and 30 mins incubation at room temperature, exposed samples were washed 8 times with media, then the eluate collected and assayed for infectious viral load via performing a tissue culture infectious dose (TCID50) assay. The infectious titre was then determined 3 days later upon examination of virus induced cytopathic effects. The samples exhibited significant viricidal activity within 5 mins as a lower SARS-CoV-2 infectious titre (TCID50/mL) was measured. The average percent reduction in infectious titre was more than 97% at 5 min post-exposure. By 15 minutes post-exposure, the eluate had non-detectable infectious SARS-CoV-2 present and achieved an average of a 99.95% reduction in infectious titre. At 30 minutes post-exposure, the samples had non-detectable infectious SARS-CoV-2, reducing the infectious titre by 99.99%.
with some of these being on the outside of the fibres, where they can come into direct contact with bacteria or viruses. Alternative approaches are to use various vapour deposition processes to deposit at the nanoscale the relevant antimicrobial metal onto the surface of the fibres, or to spray on a polyurethane coating that has the metal nanoparticles within it. Regardless of the method, including such metals can change the appearance of the mask, giving it an unusual or distinctive colour.
One particularly popular strategy has been to use copper metal or copper compounds such as copper iodide. Copper exerts drawn antimicrobial, antifungal and antiviral actions and readily inactivates SARS-CoV-2 and human influenza viruses. The Survivon™ Copatac brand is an example of Australian-made masks and respirators that incorporate this type of copper technology. An example of test results for inactivation of SARS-CoV-2 is shown in Figure 3. The inactivation process occurs within a short time frame. The same type of concept using antimicrobial metals can also be applied to various textiles and this has been an active area of investigation in recent years as attempts have been made to develop personal protective equipment with active protection mechanisms.
Emeritus Professor Laurence J. Walsh AO is a specialist in special needs dentistry who is based in Brisbane, where he served for 36 years on the academic staff of the University of Queensland School of Dentistry, including 21 years as Professor of Dental Science and 10 years as the Head of School. Since retiring in December 2020, Laurie has remained active in hands-on bench research work, as well as in supervising over 15 research students at UQ who work in advanced technologies and biomaterials and in clinical microbiology. Laurie has served as Chief Examiner in Microbiology for the RACDS for 21 years and as the Editor of the ADA Infection Control Guidelines for 12 years. His published research work includes over 390 journal papers, with a citation count of over 18,300 citations in the literature. Laurie holds patents in 8 families of dental technologies. He is currently ranked in the top 0.25% of world scientists. Laurie was made an Officer of the Order of Australia in January 2018 and a life member of ADAQ in 2020 in recognition of his contributions to dentistry.
1. Han P, et al. Splatters and aerosols contamination in dental aerosol generating procedures. Appl Sci. 2021; 11 (4): 1914.
2. Pulich A, et al. Simulated and clinical aerosol spread in common periodontal aerosol-generating procedures. Clinical Oral Investigations 2022; ;26(9): 5751-5762.
3. Borkow G, et al. A novel anti-influenza copper oxide containing respiratory face mask. PLoS ONE 2010; 5(6): e11295.
4. Fujimori Y, et al. Novel antiviral characteristics of nanosized copper(I) iodide particles showing inactivation activity against 2009 pandemic H1N1 influenza virus. Appl Env Microbiol. 2012; 78(4): 951-955.
5. Takeda Y, et al. Application of copper iodide nanoparticle-doped film and fabric to inactivate SARS-CoV-2 via the virucidal activity of cuprous ions (Cu1). Appl Environ Microbiol 2021; 87: e01824-21.
6. Jung S, et al. Copper-coated polypropylene filter face mask with SARS-CoV-2 antiviral ability. Polymers 2021; 13: 1367.
7. Foffa I, et al. A copper nanoparticles-based polymeric spray coating: Nanoshield against SarsCov-2. J Appl Biomater Funct Mater. 2022; 20: 22808000221076326.
8. Jung S, et al. Sustainable antibacterial and antiviral high-performance copper-coated filter produced via ion beam treatment. Polymers 2022; 14: 1007.
9. Wang WB, Clapper JC. Antibacterial activity of electrospun polyacrylonitrile copper nanoparticle nanofibers on antibiotic resistant pathogens and methicillin resistant Staphylococcus aureus (MRSA). Nanomaterials 2022; 12: 2139.
10. Purniawan A. Synthesis and assessment of copper-based nanoparticles as a surface coating agent for antiviral properties against SARS-CoV-2. Sci Rep. 2022; 12(1): 4835.
Unwanted visitors like bacteria love to colonise in your dental unit waterlines. A daily waterline maintenance protocol with A-dec ICX® waterline treatment tablets, along with periodic ICX Renew™ shock treatments, will help reduce these nasty microorganisms.



For complete trademark information, visit a-dec.com/legal/trademarks.
To find out more, visit australia.a-dec.com
Figure 1. Characteristic appearance of enamel white spot lesions on the cervical aspect of maxillary incisors. This site has low resting salivary flow and poor access to stimulated saliva. The image has been taken 2 weeks after an intensive oral hygiene regimen has been introduced. This explains why the following 3 features can be seen: (1) there are no visible deposits of dental plaque; (2) there is no gingivitis; and (3) a small rim of healthy enamel is seen at the cervical aspect of the white spot lesions, apical to the lower margin of the white spot lesions.


In clinical dental practice, one of the most common things that we do is to detect white spot lesions and monitor their progress to determine if they are progressing towards cavitation, undergoing arrest, or regressing. This article summarises, from the perspective of the author, some of the main lessons about watching white spot lesions and provides a number of clinical hints in interpreting what is happening in these lesions.
Hidden beneath
An active white spot lesion will each day be undergoing numerous cycles of mineral loss followed by remineralisation.1-4 Because an active white spot is covered by a cariogenic dental plaque biofilm that is producing multiple organic acids, the fluid in direct contact with the surface is not the saliva of the patients mouth but rather the plaque fluid. If using technologies that can detect acid production by dental plaque, such as GC TriPlaque ID gel, active white spot lesions will be found beneath the plaque which is producing the highest amounts of acid following a challenge with sucrose or another suitable substrate.4,5
Hence, it is essential to assess what is happening in the dental plaque biofilm before removing it to assess the surface. Practically, this means undertaking dental plaque assessment and disclosing should come before scoring the teeth for white spot lesions.
W
hen white spot lesions are viewed under wet conditions, only those lesions with large percentages of subsurface mineral loss will be visible. On the other hand, when enamel surfaces are clean and any saliva or water on the surface is removed with compressed air, it is much easier to detect the full extent of
“The reason why compressed air makes white spot lesions much more visible is that the compressed air causes desiccation (drying) of the surface and also of the more superficial parts of the white spot lesion. This removal of water changes the refractive index and hence the way that light passes through or reflects from the surface...”
white spot lesions that are present.7 This principle is the basis behind the ICDAS/ ICMS category 1 white spot lesion diagnosis - a lesion which can only be seen when the teeth are clean and dry, but is not evident when the tooth surface is wet.
The reason why compressed air makes white spot lesions much more visible is that the compressed air causes desiccation (drying) of the surface and also of the more superficial parts of the white spot lesion. This removal of water changes the refractive index and hence the way that light passes through or reflects from the surface. The greater scanner coefficient for visible light from the surface of the dry white spot lesion explains why the surface appears white.
Figure 2. Proper diagnosis of enamel lesions that can appear white is essential for their proper management. This plate shows typical examples of common conditions other than dental caries that can manifest with opacities in the enamel, as well as other changes in the surface topography. With mild fluorosis (upper left), changes are subtle and become more evident when teeth are dried. As fluorosis becomes more severe (upper right), surface pitting may be present and the uptake of exogenous stains can make the affected areas dark. When systemic factors affect enamel development (lower left), the location of affected sites vary according to the chronology of tooth development. A common local factor that drives localised changes such as enamel opacity of permanent incisor teeth (lower right) is pulpal infection of deciduous incisors because of advanced caries.


When comparing anterior teeth, there is a large difference in the relative risk of labial surfaces of incisor and canine teeth for white spot lesions. The risk is much greater for the maxillary anterior teeth than for the corresponding mandibular anterior teeth.5 This difference is one of the reasons for the effectiveness of the “lift the lip” approach.
The reasons for the differences relate to the more hostile environment for the maxillary anterior teeth, which have little contact with stimulated saliva and which are covered by a saliva refill that is slowmoving and has relatively low buffer capacity when compared to its counterpart in the lower arch.8,9 As a result of the environmental influence of saliva, studies of plaque fermentation always show that plaque pH is lower for maxillary anterior teeth than for their mandibular tooth counterparts when one compares the same tooth surface on the labial aspect.5
The three laws of real estate apply strongly to the distribution of white spot lesions within the one arch. In the maxillary arch, it will be very rare to find white spot lesions on the buccal surfaces of first and second molar teeth, because of their proximity to the parotid salivary duct. This information is not new. In 1966, Otto Backer-Dirks reported a study in which 184 buccal surfaces of maxillary first molars were examined at age 7 and every second year for eight years until age 15. Areas diagnosed originally as white spot lesions in a number of cases subsequently appeared normal.10
Maxillary molar buccal tooth surfaces show an exceptional ability for mineral to be deposited, typically by mineralisation of the dental plaque biofilm to form supragingival calculus - and likewise, for remineralisation to occur. Hence, one would only see white spot lesions in such a location if there had been a particularly strong local caries risk factor, such as a molar orthodontic band making oral hygiene difficult and allowing plaque to stagnate, or a patient developing saliva gland hypofunction.
In the mandibular arch, it would be very uncommon to see white spot lesions on the lingual or labial surfaces of the
incisor teeth, since these would normally have exposure to saliva that pools on the floor of the mouth at rest.1,11 Hence, when white spot lesions are seen in these locations, there is a strong suspicion of depressed production of saliva at rest.
The iceberg concept of dental caries diagnosis is that when one sees a single visible white spot lesion, there will be more lesions present at a less advanced stage. Conversely, the number of visible cavitations of the enamel is typically less than the number of white spot lesions that are present.7,12
“One has to consider whether a white spot lesion that has formed on an approximal enamel surface that is evident on a bitewing radiograph has actually cavitated, or not. If it has not, then strategies for remineralisation that can stabilise the surface and arrest the progression of the lesion can be deployed. However, once the enamel surface collapses and a cavity forms, restorative intervention is required...”
The major implication that flows from this is that when assessing a patient’s caries history, if one only tracks cavities and past restorations, it is likely that the total caries experience of the patient will be underestimated. In populations of children, scoring white spot lesions on primary teeth as well as cavities and filled surfaces will elevate the DMFT approximately threefold, providing a rather more alarming total score.13,14 Similar principles apply in adults. An individual could have a low DMFT if one defines a decayed surface as having a frank cavitation in the enamel, but still have a very large number of active white spot lesions.
When a patient has numerous visible white spot lesions on the buccal tooth surfaces, one should immediately be suspicious of what is happening interdentally and check the patient for caries on the aproximal enamel surfaces. Typically, this is done using bitewing radiographs or digital imaging fiber optic transillumination (e.g. using the KaVo DiagnoCAM).15
A key point when assessing bitewing radiographs is to recall that approximately one third of the buccolingual width of the tooth must be affected by mineral loss for the change in mineral density to be reliably detected by radiographic examination. Practically speaking, this means that white spot lesions on a proximal enamel surfaces are much easier to detect on teeth where the contact points are narrow (e.g. incisors and premolars) rather than on teeth where contact points are wide, such as molars. An important point of dental anatomy is that contact points are wide on molar teeth but are placed further buccally as one goes more posterior in the mouth.
Furthermore, one has to consider whether a white spot lesion that has formed on an approximal enamel surface that is evident on a bitewing radiograph has actually cavitated, or not. If it has not, then strategies for remineralisation that can stabilise the surface and arrest the progression of the lesion can be deployed. However, once the enamel surface collapses and a cavity forms, restorative intervention is required, since the dental plaque biofilm within the cavity will now be in a protected space.7
The question is, are arrested enamel lesions on approximal enamel surfaces stable? Back to the studies of Otto Backer-Dirks in 1966 in the Netherlands. In a group of 45 male and 45 female children, mesial surfaces of upper and lower first molars on bitewing radiographs were tracked over 8 years. Some 26% of enamel lesions diagnosed at age 7 had not progressed after 8 years. This was in a non-fluoridated community and was prior to the advent of topical fluorides or modern remineralising therapies.10 So, the answer to the question of stability is yes.
Another aspect of the inside story of white spot lesions relates to the presence of bacterial products in the outermost poorest layers of the white spot lesion that make up its visible surface.
Current fluorescence technology based on the Diagnodent is sufficiently sensitive to be able to detect and measure such bacterial products in white spot lesions on tooth surfaces that have just undergone professional prophylaxis to remove all deposits of plaque. Tracking fluorescence scores over time on individual white spot lesions can provide clues as to their trajectory. If the fluorescence scores remain stable, it is highly likely that the lesion has stabilised, whereas when fluorescence scores are increasing, this indicates that more bacterial products from the overlying dental plaque have penetrated through the surface and into the body of the lesion. Increasing fluorescence scores over time correlate with cavitation occurring at a subsequent time point.13,14
An important consideration when assessing white spot lesions is whether the lesion is active or not. A range of parameters provide information to inform such a decision.7 An active white spot lesion will have a rough irregular surface that will look under magnification like white sand. The lesion will typically be beneath a mature dental plaque biofilm with high levels of acid production. Because of the dental plaque biofilm, the configuration of the lesion will reflect the patient’s oral hygiene in that location and there will be corresponding inflammatory changes in the adjacent gingiva. Typically, the lesion will be close to the gingival margin and there will be visible signs of gingivitis present.
On the other hand, an arrested white spot lesion will have a surface that is macroscopically smooth and shiny or polished in appearance. The lesion location is typically supragingival, rather than equi-gingival and on a surface that is free of dental plaque. The adjacent gingival soft tissues may be quite healthy. Lesions which have undergone arrest can trap pigmented substances within them, that originate from coloured foods and drinks in the diet.
It is important to have clear treatment goals for white spot lesions. If the intent is to cause these to arrest, making them “frozen in time” for the remainder of the patient’s life, then the application
of a high concentration fluoride product, particularly a fluoride varnish, can cause surface porosities to be blocked through the deposition of calcium fluoride.16 In this author’s view, such a strategy should only be considered when the lesion is not in an area of aesthetic importance.
Where white spot lesions are present in areas that are aesthetically important, particularly maxillary anterior teeth, the treatment goal should be to return the enamel to a completely normal appearance. Use of CPP-ACP through various delivery systems has been shown
“Orthodontic treatments carry a high risk of patients developing white spot lesions, so it is important to consider ways to prevent these lesions occurring during treatment, as well as to mitigate the impact of them at the end of treatment. A number of studies have shown that GC Tooth Mousse Plus used during orthodontic treatment lowers the risk of white spot lesion development, through both chemical as well as biological actions...”
to be highly effective for causing subsurface regeneration of white spot lesions, leading to their visible reversal.17-20 This happens progressively over time, as neutral ion species penetrate into the lesion. The enamel which forms has a high degree of resistance to acid dissolution, as well as an optimal appearance. Most commonly, such regeneration approaches involve repeated application of a topical crème such as GC Tooth Mousse Plus each day over a period of multiple weeks.
An important consequence of following this strategy is that the regenerated enamel has desirable aesthetic and chemical characteristics and is contiguous with the
previous unaffected enamel. As a result, should the teeth subsequently undergo dental bleaching, the result will be consistent across the surface of the tooth. Hence, the strategy of regeneration is preferred in situations where multiple white spot lesions are noted to be present when brackets are removed at the end of fixed orthodontic treatment, or at the end of a program of sequential plastic aligners.
Orthodontic treatments carry a high risk of patients developing white spot lesions,21,22 so it is important to consider ways to prevent these lesions occurring during treatment, as well as to mitigate the impact of them at the end of treatment. A number of studies have shown that GC Tooth Mousse Plus used during orthodontic treatment lowers the risk of white spot lesion development, through both chemical actions (including the release of optimal ratios of calcium, phosphate and fluoride ions) as well as biological actions (such as prebiotic effects).4,23
At the end of orthodontic treatment, if resin impregnation is used to treat white spot lesions that developed around brackets, some long-term issues could arise that must be considered. Historically, resin impregnation was developed for posterior teeth and its use on anterior teeth was not advised. Part of the thinking behind this was that any micro-scale or nano-scale leakage of fluid around the resin over time could be problematic. Moreover, later attempts to treat the tooth using in-office or at-home bleaching could result in irregular outcomes, since the presence of the resin would greatly affect the ability of reactive oxygen species to penetrate through the enamel. As well, long-term colour stability of the resin that had been infiltrated into the tooth could be an issue. Finally, from a purely structural point of view, having a tooth with an intact enamel surface with ideal mineral characteristics (true regeneration) is preferable to having weakened areas infiltrated with resin. This is because of the distribution of stress within the tooth and its concentration at interfaces and boundaries.
Some of the concepts described above can be adapted for the situation of the early or incipient root surface carious lesion.
In terms of location, the site with the greatest propensity for root surface caries to develop is the buccal surface of mandibular molar teeth, especially in the furcation region. On the other hand, the most protected sites in the mouth are the lingual surfaces of mandibular incisor teeth, since these normally sit in continuous contact with resting saliva.24 When root surfaces of mandibular incisor teeth are exposed because of periodontal attachment loss or gingival recession, these lingual surfaces should be the last ones in the mouth to develop dental caries. This is why the presence of dental caries in this site is highly suggestive of prolonged and severe saliva gland hypofunction, which removes the protection of the saliva at rest.1
Applying the iceberg concept, when cavitated root surfaces are found, one must always consider what is happening on the interdental root surfaces.25,26 Taking bitewing or periapical radiographs will often reveal lesions of root surface caries in locations that may not be readily accessible to probing. This results in the advice to always suspect that as many lesions of root surface caries may be present radiographically as may be present clinically.
In lesions of root surface caries, destruction of the surface occurs by multiple processes, including proteolysis of collagen as well as dissolution of mineral by organic acids. The combination of these two processes explains why lesions develop over a broad front beneath a cariogenic biofilm and why surface softening occurs a long time before physical breakdown of the surface.
Fluorescence can be tracked in incipient root surface lesions using the DIAGNOdent, and repeated applications of topical CPP-ACP have been shown to cause caries arrest.27 When this occurs, the fluorescence scores will stabilise or decline. The lesions may or may not change colour. When colour change does occur, it reflects a change in the metabolic state of key bacterial species that generate pigments, especially Acyinomyces odontolyticus. A colour change such as darkening may occur when a root surface lesion is treated, as the bacteria within the outermost regions of the dentine change their metabolic state. Unfortunately, such a colour change does not mean that the lesion has stabilised for an indefinite period of time.
Lastly, agents that may be used to arrest incipient or cavitated lesions of root surface caries can themselves cause discolouration of the tooth, with the classic example being silver diamine fluoride preparations. In this case, the colour change is caused by the silver component and it will mask any changes due to bacterial pigment production.
Emeritus Professor Laurence J. Walsh AO is a specialist in special needs dentistry who is based in Brisbane, where he served for 36 years on the academic staff of the University of Queensland School of Dentistry, including 21 years as Professor of Dental Science and 10 years as the Head of School. Since retiring in December 2020, Laurie has remained active in hands-on bench research work, as well as in supervising over 15 research students at UQ who work in advanced technologies and biomaterials and in clinical microbiology. Laurie has served as Chief Examiner in Microbiology for the RACDS for 21 years and as the Editor of the ADA Infection Control Guidelines for 12 years. His published research work includes over 390 journal papers, with a citation count of over 18,300 citations in the literature. Laurie holds patents in 8 families of dental technologies. He is currently ranked in the top 0.25% of world scientists. Laurie was made an Officer of the Order of Australia in January 2018 and a life member of ADAQ in 2020 in recognition of his contributions to dentistry.
1. Walsh LJ. A system for total environmental management (STEM) of the oral cavity, and its application to dental caries control. International Dentistry SA Australasian Edition 2008;3 (1):34-48.
2. Walsh LJ, Brostek AM. Minimal intervention dentistry principles and objectives. Australian Dental Journal 2013; 58 (1 Suppl): 3-16.
3. Brostek AM, Walsh LJ. Minimal intervention dentistry in general practice. Oral Health and Dental Management 2014;13(2):285-294. PMID.
4. Walsh LJ, Healey D. Prevention and caries risk assessment and management in teenage and orthodontic patients. Australian Dental Journal 2019 (Special Issue) Jun; 64 Suppl 1:S37-S45.
5. Walsh LJ, Tsang AKL. Chairside testing for cariogenic bacteria: current concepts and clinical strategies. International Dentistry 2008;10(2):50-65.
6. Walsh LJ. Caries diagnosis aided by fluorescence. In: Arkanslan Z (Ed) Dental Caries - Diagnosis and Management. Croatia: InTech Publishers, 2018. Chapter 7, pp. 97-115.
7. Walsh LJ. Maximum interception: things to try before you drill. Australasian Dental Practice 2007;18(5):90-98.
8. Walsh LJ. Preventive dentistry for the general dental practitioner. Australian Dental Journal 2000; 45(2): 76-82.
9. Walsh LJ. Clinical aspects of salivary biology for the dental clinician. International Dentistry 2007;9(4):22-41.
10. Backer Dirks O. Posteruptive changes in enamel. Journal of Dental Research 1966; 45(3): 503-511.
11. Walsh LJ. Minimal intervention management of the older patient. British Dental Journal. 2017; 223(3):151-161.
12. Ismail AI, Sohn W, Tellez M, Amaya A, Sen A, Hasson H, Pitts NB. The International Caries Detection and Assessment System (ICDAS): an integrated system for measuring dental caries. Community Dentistry and Oral Epidemiology 2007;35(3):170-178.
13. Walsh LJ, Clifford H. Changes in Diagnodent scores in smooth surface enamel carious lesions in primary teeth: a longitudinal clinical study. Journal of Oral Laser Applications 2008;8(3):157-164.
14. Walsh LJ, Groeneveld G, Hoppe V, Keles F, van Uum W, Clifford H. Longitudinal assessment of changes in enamel mineral in vivo using laser fluorescence. Australian Dental Journal 2006;51(4):S26.
15. Walsh LJ. Shining infrared light through teeth – Laser transillumination and the DIAGNOcam. Australasian Dental Practice 2014; 24(2):76-78.
16. Walsh LJ. In-clinic fluoride products: current concepts for maximal effectiveness. New Zealand Dental Therapists’ Association Journal; April 2008; 15:7-8.
17. Walsh LJ. White spots, GC Asia Dental, Singapore, 2007.
18. Walsh LJ. Strategies for remineralization. In: Limeback H (ed) Comprehensive Preventive Dentistry, Ames Iowa: Blackwell Publishing 2012, Chapter 17. Pp. 298-312.
19. Fontana M, Walsh LJ, Amaechi BT, Ngo HC. Aids to remineralization. In: Mount GJ, Hume WR, Ngo HC, Wolff MS (eds). Preservation and Restoration of Tooth Structure, 3rd edn. 2016. Chichester, West Sussex, UK: John Wiley. pp. 67-80.
20. Tran C, Walsh LJ. Assessment of mineral gain in white spot lesions using CPP-ACP and CPP-ACFP in different clinical protocols: A proof of concept study. Recent Progress in Materials. 2021, 3(4): 18.
21. Chang HS, Walsh LJ, Freer TJ. Effect of orthodontic treatment on salivary flow, pH, buffer capacity, and levels of mutans streptococci and lactobacilli. Australian Orthodontic Journal. 15(4), 229-234, 1999.
22. Chang HS, Walsh LJ, Freer TJ. Enamel decalcification during orthodontic treatment - aetiology and prevention. Australian Dental Journal1997; 42: 322-327.
23. Philip N, Leishman SJ, Bandara HMHN, Healey DL, WALSH LJ. Randomized controlled study to evaluate microbial ecological Effects of CPP-ACP and cranberry on dental plaque. JDR Clinical and Translational Research. 2020;5(2):118-126.
24. Walsh LJ. Root caries – The emerging challenge in dental caries management. Annals of the Royal Australasian College of Dental Surgeons 2014; 22: 60-63.
25. Walsh LJ, Gan A. Proximal root surface caries in an Australian periodontal population. Periodontology 1991; 12: 33-36.
26. Walsh LJ. The problems of furcations: what lies beneath. Auxiliary 2008;18(2):26-28.
27. Vlacic J, Meyers IA, Walsh LJ. Combined CPPACP and photoactivated disinfection (PAD) therapy in arresting root surface caries: a case report. British Dental Journal. 2007;203(8):457-459.





















Running a practice takes a lot of work. Although all practices are different and face unique challenges, one common issue is optimal instrument management.
For many practices, switching to an Instrument Management System (IMS®) provides innumerable benefits; however, practices may be reluctant to switch. Practices may have to reconfigure their sterilisation area, purchase new instruments or retrain employees, but the return is worth the investment! Whether it’s reduced sharps injuries, enhanced organisation, cost reductions, increased patient counts or another benefit, practices that adopt IMS see measurable results.
Large organisations like Pacific Dental Services (PDS) are always looking for measurable, data-driven ways to improve safety and ensure regulatory compliance across their network of dental practices. To better understand the impact of IMS, PDS identified two practices with an opportunity to reduce sharps injuries to trial the cassette-based system. After implementing IMS in those practices, PDS compared the results after a year with equivalent control practices.
The findings were unmistakable. Not only were sharps injuries reduced to zero for the two practices during the trial period, but both practices experienced improved efficiency, as instruments were reprocessed eight minutes faster on average, freeing up time to spend with patients.
Following this successful experiment, PDS expanded it to more locations to verify the findings, which generated identical results. With such positive outcomes, Hu-Friedy worked with PDS to implement IMS in over 100 practices.
“Now that we’ve implemented these cassettes in approximately 100 locations, the feedback continues to be the same,” said one PDS compliance manager. “Staff really love the cassettes. They love the efficiencies of the cassettes.”
As Floss & Co. began to get busier, staff struggled at first to manage an increase in patients. There were simply not enough scalers to keep up and all instruments were either in use or in reprocessing. At first, Dr Izzy Naem looked to solve the problem by purchasing more instruments, but the real issue wasn’t the number of instruments. It was about improving process efficiencies and finding better ways to keep instruments better organised.
So, when Dr Naem instead decided to switch to the IMS system, the practice was able to save 15 minutes per patient per chair, relieving some of the stress that the staff were experiencing.
“We don’t have to think about the instruments,” Dr Naem said. “Where they’re at, where to put them, where to store them. It’s all in the cassette. It was safer and it was easier.”
With improved efficiency and organization, the practice was able to continue expanding and saw a 40 percent increase in new patients. By switching to IMS, Dr Naem was able to increase revenues and provide a better experience for his staff and growing patient base.
When Dr Edward Lin and his team at Orthodontic Specialists expanded from three doctors to four, the number of instruments used in their facility rose accordingly. Additionally, Dr Lin was concerned about protecting his investment in premium instruments. After trying other solutions with unsatisfactory results, the team began using IMS, enabling them to see 60 to 120 patients a day efficiently.
Cassettes were fundamental to enabling Dr Lin’s practice to successfully expand: “To work without the Hu-Friedy IMS System would be pure chaos,” Dr Lin said. “I couldn’t tolerate it because instruments are going to get lost. Instruments will get damaged. It would be physically impossible to be able to see the number of patients that we see in a clinical day without the IMS System.”
or Dr Steven Koos of ORA Oral Surgery & Implant Studio, proper organisation is key to practice success. Since ORA specialises in various oral surgery procedures, it’s important to have setups ready for each unique procedure and organising the correct instruments can be complicated and time-consuming.
Adopting IMS simplified instrument prep with the introduction of versatile and customisable cassettes that keep instruments organised and in one place for each procedure, from chairside to cleaning to storage. “My surgical team has really embraced the Hu-Friedy IMS Cassette System because it’s enabled them to combine the cleaning and sterilisation and organisation and storage of a vast array of instruments into one integrated package and it works well,” Dr Koos said.
Additionally, implementing cassettes has made it easier to hire and train new team members and open new locations without affecting the quality of care provided to patients.
Chairside efficiency is the key to a productive practice. Maximizing this efficiency is possible when the exact procedural set ups needed for each patient are always at your fingertips. Hu-Friedy’s dental Instrument Management System standardises and combines the cleaning, sterilisation, storage and organisation of instruments in one integrated cassette system, creating real results that can save your practice up to 5-10 minutes per procedure. There are numerous advantages to adopting IMS and while each practice profiled here chose to make the switch for different reasons, the results are universal: better efficiency, improved safety, enhanced patient experience and an increased bottom line.
If your practice does not already use an instrument management system, you can request more information from a Hu-Friedy representative on how a cassette-based system can directly benefit your practice.
The most sophisticated solution for instrument management
The most sophisticated solution for instrument management
The most sophisticated solution for instrument management
The most sophisticated solution for instrument
That’s right, you deserve it. You deserve the peace of mind and confidence of knowing that you are employing the most contemporary method of processing instruments. As dentistry’s innovator of the cassette-based instrument management system, Hu-Friedy is proud to bring you the modern design and functionality of the Infinity Series Cassettes which include:
That’s right, you deserve it. You deserve the peace of mind and confidence of knowing that you are employing the most contemporary method of processing instruments. As dentistry’s innovator of the cassette-based instrument management system, Hu-Friedy is proud to bring you the modern design and functionality of the Infinity Series Cassettes which include:
Ensure predictable outcomes for your littlest patients with Hu-Friedy Stainless Steel Pedo Crowns. You’ll quickly discover why dentists favor our impeccable fit. Perfect for your patients. Easy for you. Because when it comes to the perfect fit, Hu-Friedy is just right.
That’s right, you deserve it. You deserve the peace that you are employing the most contemporary
Ensure predictable outcomes for your littlest patients with Hu-Friedy Stainless Steel Pedo Crowns. You’ll quickly discover why dentists favor our impeccable fit.
• An open hole pattern that promotes water flow throughout the cassette
That’s right, you deserve it. You deserve the peace of mind and confidence of knowing that you are employing the most contemporary method of processing instruments. As dentistry’s innovator of the cassette-based instrument management system, Hu-Friedy is proud to bring you the modern design and functionality of the Infinity Series Cassettes which include:
Ensure predictable outcomes for your littlest patients with Hu-Friedy Stainless Steel Pedo Crowns. You’ll quickly discover why dentists favor our
• An open hole pattern that promotes water flow throughout the cassette
WHY DENTISTS LOVE OUR STAINLESS STEEL PEDO CROWNS:
file. Available upon request.
• An open hole pattern that promotes water flow throughout the cassette

designs. Data on file. Available upon request.
• Color-coded silicone rail system that significantly reduces instrument contact and allows for more water flow while protecting the instruments during reprocessing
©2020 Hu-Friedy Mfg. Co., LLC. All rights reserved. HFL-482AUS/1220
• Ideal height and mesio-distal width





• Color-coded silicone rail system that significantly reduces instrument contact and allows for more water flow while protecting the instruments during reprocessing
• Color-coded silicone rail system that significantly reduces instrument contact and allows for more water flow while protecting the instruments during reprocessing
©2020 Hu-Friedy Mfg. Co., LLC. All rights reserved. HFL-482AUS/1220
• Pre-trimmed and pre-crimped for simple placement
• Easy-to-use, ergonomic latch that allows for one-handed opening
All
• Accurate occlusal anatomy that matches the natural tooth
• Easy-to-use, ergonomic latch that allows for one-handed opening Performing at your best means having confidence in what you do. Experience Infinity Series™ Cassettes, and improve the efficiency of your practice, while helping protect your patients, your staff and your instrument investment.

©2020 Hu-Friedy Mfg. Co., LLC. All rights reserved. HFL-482AUS/1220
To learn more about how IMS can enhance your practice visit Hu-Friedy.com/Infinity
VISIT US ONLINE AT HU-FRIEDY.COM/PerfectFit
Hu-Friedy Mfg. Co., LLC, 1666 E. Touhy Ave., Des Plaines, IL 60018 | Hu-Friedy.com
• Easy-to-use, ergonomic latch that allows for one-handed opening Performing at your best means having confidence in what you do. Experience Infinity Series™ Cassettes, and improve the efficiency of your practice, while helping protect your patients, your staff and your instrument investment. VISIT US ONLINE AT HU-FRIEDY.COM/PerfectFit
©2016 Hu-Fried y Mfg. Co., LLC. All rights reserved.
Performing at your best means having confidence in what you do. Experience Infinity Series™ Cassettes, and improve the efficiency of your practice, while helping protect your patients, your staff and your instrument investment. VISIT US ONLINE AT HU-FRIEDY.COM/PerfectFit
All company and product names are trademarks of Hu-Friedy Mfg. Co., LLC, its affiliates or related companies, unless otherwise noted.
©2016 Hu-Fried y Mfg. Co., LLC. All rights reserved.
©2017 Hu-Friedy Mfg. Co., LLC. All rights reserved.
©2016 Hu-Fried y Mfg. Co., LLC. All rights reserved.
©2021 Hu-Friedy Mfg. Co., LLC. All rights reserved.
Signature Series Tubs are designed to match Hu-Friedy IMS instrument cassette rail colours and feature antimicrobial product protection. Together, procedure tubs and cassettes create the most efficient and organised system for managing instruments and consumable products.
The time savings achieved by using IMS (Instrument Management System) cassettes and procedure tubs allow staff to spend time on more value-added activities in the dental practice.
Microban protection is integrated into the tub and tub components during the manufacturing process. Microban technology works by interrupting key cell functions that allow the microorganisms to function, grow and reproduce.
Microban protection begins to work as soon as the microorganism comes into contact with the product surface and works continuously to inhibit the growth of microbes that can cause stain, odours and product degradation - for the lifetime of the product.
Procedure tubs can be used as portable operatory drawers to store, organise and transport consumable materials to and from the storage/sterilisation area and the operatory. All of the materials needed for a specific procedure can be stored in the tub. A different tub and colour can be used for each different procedure type (e.g. crown & bridge, composite, etc). The Signature Series procedure tubs are available in colours that match IMS cassette rails, which allow the staff to match the tubs and cassettes by procedure.

Blue cassette rails and a blue tub may represent a composite procedure. All of the consumable materials for composite procedures can be stored and organised in the blue tub and instrumentation stored in the cassette with blue rails, allowing for quick identification.

The Hu-Friedy IMS and Tub System increases efficiency of materials management and eliminates time-consuming tray preparation for every procedure. Tubs may be configured to meet your practice needs or are available as a complete tub.
Procedure tub colours match Hu-Friedy IMS cassette rail colours...
• Increasing practice organisation and workflow efficiency.
• Allowing for quick identification of consumable products.
• Providing aesthetic integration with IMS cassettes.
• Protect items from airborne materials during transportation to the operatory and storage.
• Adhere to infection control standards Microban® Antimicrobial Product Protection.
• Microban inhibits the growth of microorganisms that can cause stains, odours and product degradation.
• Allow for storage in central sterilisation or each operatory.
• Tubs can be transported to the operatory prior to each procedure, eliminating inventory management of materials in each operatory.
For more information, visit www.hufriedygroup.com
Standardises material set-up for every type of procedure


